An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward
Abukari kwame.
1 College of Graduate and Postdoctoral Studies, University of Saskatchewan, Saskatoon, Canada
Pammla M. Petrucka
2 College of Nursing, University of Saskatchewan, Regina Campus, Regina, Canada
Associated Data
Not applicable.
Providing healthcare services that respect and meet patients’ and caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns, beliefs, and contextual variables. Achieving patient-centered care and communication in nurse-patient clinical interactions is complex as there are always institutional, communication, environmental, and personal/behavioural related barriers. To promote patient-centered care, healthcare professionals must identify these barriers and facitators of both patient-centered care and communication, given their interconnections in clinical interactions. A person-centered care and communication continuum (PC4 Model) is thus proposed to orient healthcare professionals to care practices, discourse contexts, and communication contents and forms that can enhance or impede the acheivement of patient-centered care in clinical practice.
Providing healthcare services that respect and meet patients’ and their caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thus constituting patient-centered care. Care is “a feeling of concern for, or an interest in, a person or object which necessitates looking after them/it” [ 1 ]. The Institute of Medicine (IOM) noted that to provide patient-centered care means respecting and responding to individual patient’s care needs, preferences, and values in all clinical decisions [ 2 ]. In nursing care, patient-centered care or person-centered care must acknowledge patients’ experiences, stories, and knowledge and provide care that focuses on and respects patients’ values, preferences, and needs by engaging the patient more in the care process [ 3 ]. Healthcare providers and professionals are thus required to fully engage patients and their families in the care process in meaningful ways. The IOM, in its 2003 report on Health Professions Education , recognized the values of patient-centered care and emphasized that providing patient-centered care is the first core competency that health professionals’ education must focus on [ 4 ]. This emphasis underscored the value of delivering healthcare services according to patients’ needs and preferences.
Research has shown that effective communication between patients and healthcare providers is essential for the provision of patient care and recovery [ 5 – 8 ]. Madula et al. [ 6 ], in a study on maternal care in Malawi, noted that patients reported being happy when the nurses and midwives communicated well and treated them with warmth, empathy, and respect. However, other patients said poor communication by nurses and midwives, including verbal abuse, disrespect, or denial from asking questions, affected their perceptions of the services offered [ 6 ]. Similarly, Joolaee et al. [ 9 ] explored patients’ experiences of caring relationships in an Iranian hospital where they found that good communication between nurses and patients was regarded as “more significant than physical care” among patients.
According to Boykins [ 10 ], effective communication is a two-way dialogue between patients and care providers. In that dialogue, both parties speak and are listened to without interrupting; they ask questions for clarity, express their opinions, exchange information, and grasp entirely and understand what the others mean. Also, Henly [ 11 ] argued that effective communication is imperative in clinical interactions. He observed that health and illness affect the quality of life, thereby making health communication critical and that the “intimate and sometimes overwhelming nature of health concerns can make communicating with nurses and other healthcare providers very challenging” [ 11 ]. Furthermore, Henly [ 11 ] added that patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns. Given the prevalence of face-to-face and device-mediated communications and interactions in healthcare settings, we must explore and clarify who, what, where, when, why, and how interactions with individuals, families, and communities are receiving care and health services [ 11 ].
The value of effective communication in nurse-patient clinical interactions cannot be overemphasized, as “research has shown that communication processes are essential to more accurate patient reporting and disclosure” [ 12 ]. Respectful communication between nurses and patients can reduce uncertainty, enhance greater patient engagement in decision making, improve patient adherence to medication and treatment plans, increase social support, safety, and patient satisfaction in care [ 12 , 13 ]. Thus, effective nurse-patient clinical communication is essential to enhancing patient-centered care and positive care outcomes.
Patient-centered communication, also known as person-centered communication or client-centered communication, is defined as a process that invites and encourages patients and their families to actively participate and negotiate in decision-making about their care needs, as cited in [ 7 ]. Patient-centered communication is crucial in promoting patient-centered care and requires that patients and their caregivers engage in the care process. As McLean [ 14 ] observed, patient-centered care can be enhanced through patient-centered communication by valuing patients’ dignity and rights. Through open communication and collaboration, where information and care plans are shared among care providers, patients, and their families, care provision becomes patient-centered [ 14 ].
Given the interconnected nature of patient-centered care and communication, we must identify the barriers and enablers of patient-centered care and communication and proposed efficient ways to enhance that because patient-centered communication is essential in achieving patient-centered care. Our aim in this paper is to identify the barriers and facilitators of patient-centered care and communication and propose and present a patient-centered care and communication continuum (PC4) Model to explain how patient-centered care can be enhanced in nurse-patient clinical interactions. As Grant and Booth argued, critical reviews are often used to present, analyse, and synthesized research evidence from diverse sources, the outcome of which is a hypothesis or a model as an interpretation of existing data to enhance evidence-based practice [ 15 ]. Thus, this critical literature review study explores the questions: what are the barriers and facilitators of patient-centered care and how can patient-centered care be enhanced through effective clinical communication?
An earlier version of this study was submitted as part of author AK’s doctoral comprehensive exams in February 2021. An interdisciplinary doctoral committee recommended many of the included literature and the questions explored in this study based on the current discourse of patient-centered care advocated for in many healthcare facilities and in recognition of the universal healthcare access objective of the health sustainable development goal. Additional searches for literature were conducted between September and November 2020 using keywords such as barriers and facilitators of nurse-patient interaction, patient-centered care, patient-centered communication , and nurse-patient communication . Databases searched included CINAHL, PubMed, Medline, and Google Scholar. Included studies in this critical review were empirical research on nurse-patient interactions in different care settings published in English and open access. All relevant articles were read, and their main findings relevant to our review questions were identified and organized into themes and subthemes discussed in this paper. Other published studies were read, and together with those that addressed the review question, a model was developed regarding how to enhance patient-centered care through effective communication.
Barriers to Patient-Centered Care and Communication
Nurses constitute a significant workforce of care providers whose practices can severely impact care outcomes (both positive and negative). Nurses spend much time with patients and their caregivers. As a result, positive nurse-patient and caregiver relationships are therapeutic and constitute a core component of care [ 9 , 13 ]. In many instances, nurses serve as translators or patients’ advocates, in addition to performing their primary care duties. Although good nurse-patient relationships positively impact nurse-patient communication and interaction, studies have shown that several factors impede these relationships with significant consequences on care outcomes and quality [ 6 , 16 , 17 ]. Thus, these barriers limit nurses’ and other care providers’ efforts to provide healthcare that meets patients’ and caregivers’ needs. We categorize the barriers to patient-centered care and communication into four kinds: institutional and healthcare system-related, communication-related, environment-related, and personal and behaviour-related barriers. Although these barriers are discussed in separate subheadings, they are interlinked in complex ways during clinical practice.
Institutional and Healthcare System Related Barriers
Many barriers to providing patient-centered care and communication during nurse-patient interactions emanate from healthcare institutional practices or the healthcare system itself. Some of these factors are implicated in healthcare policy or through management styles and strategies.
Shortage of nursing staff, high workload, burnout, and limited-time constituted one complex institutional and healthcare system-level barrier to effective care delivery [ 18 , 19 ]. For instance, Loghmani et al. [ 20 ] found that staffing shortages prevented nurses from having adequate time with patients and their caregivers in an Iranian intensive care unit. Limitations in nursing staff, coupled with a high workload, led to fewer interactions between nurses, patients, and caregivers. Similarly, Anoosheh et al. [ 16 ] found that heavy nursing workload was ranked highest as a limiting factor to therapeutic communication in nurse-patient interactions in Iran.
In a study on communication barriers in two hospitals affiliated with Alborz University of Medical Sciences, Norouzinia et al. [ 21 ] found that shortage of nurses, work overload, and insufficient time to interact with patients were significant barriers to effective nurse-patient interactions. Similar factors are identified as barriers to nurse-patient communication and interactions in other studies [ 13 , 16 , 18 ]. For instance, Amoah et al. [ 16 ] reported that nursing staff shortage and high workload were barriers to patient-centered care and therapeutic communication among Ghanaian nurses and patients. Amoah and colleagues reported a patient’s statement that:
[B]ecause there are few nurses at the ward, sometimes you would want a nurse to attend to you, but he or she might be working on another patient, so in such case, the nurse cannot divide him or herself into two to attend to you both [ 16 ].
Nurses and patients and their caregivers have noted that limited time affects nurse-patient interactions, communication, and care quality. Besides, Yoo et al. [ 22 ] reported that limited visiting hours affected communications between caregivers and nurses in a tertiary hospital in Seoul, Korea. Since the caregivers had limited time to spend with patients, they had little knowledge about the intensive care unit and distrusted the nurses.
Although nursing staff shortage is a significant barrier to patient-centered care and communication that healthcare institutions and managers must know, some healthcare scholars have critique nurses’ complaints of time limitation. For instance, McCabe [ 7 ] argued that the quality of nurse-patient interactions is what matters and not the quantity of time spent with patients and their caregivers. McCabe maintained that “spending long periods with patients does not always result in positive nurse-patient relationships” [ 7 ]. He argued that implementing patient-centered care does not require additional time; hence, nurses’ perceptions of being too busy cannot excuse poor therapeutic communication during clinical interactions. Instead, nurses are encouraged to develop self-awareness, self-reflection, and a commitment to ensuring that patients receive the needed care.
Another institution-related barrier to patient-centered care and communication is the healthcare system’s emphasis on task-centered care. Care providers are more focused on completing care procedures than satisfying patients’ and caregivers’ needs and preferences. This barrier to patient-centered care and communication is acknowledged in several studies [ 7 , 14 , 20 , 22 , 23 ]. For example, McLean [ 14 ] studied dementia care in nursing homes in the United States. She found that patient-centered care and communication in one nursing home (Snow I) were severely affected when nurses, physicians, and care managers focused on completing tasks or observing care and institutional routines to the detriment of satisfying patients’ care needs. However, in the other care home (Snow II), patient-centered care was enhanced as nurses, physicians, and the care home managers focused on addressing patients’ needs and values rather than completing care routines and tasks.
Similarly, Yoo and colleagues [ 22 ] observed that nurse-patient communication was affected when the ICU nurses placed urgency on completing tasks linked directly to patients’ health (e.g., stabilizing vital signs) than communicating to addressed patients’ specific needs. This evidence shows that when nurses are more task-focused, patients and caregivers are treated as bodies and objects, on which medical and care practices must be performed to restore health. Research has shown that when nurses focus on task-oriented care, it becomes hard to provide holistic care to patients or teach and communicate with patients even when nurses are less busy [ 20 ].
Nursing managers and their management styles can affect patient-centered care and communication. Studies have revealed that the management styles that nursing managers implement can either facilitate or impede patient-centered care [ 14 , 22 ]. When nurse managers orient their nursing staff towards task-centered care practices, it affects nurse-patient interaction and communication. Moreover, when nurse managers fail to address their staff’s mental health needs and personal challenges, it influences how nurses attend to patients’ care needs. For example, nurses have indicated that nurse-patient communication is affected when nurse managers are unsupportive or unresponsive to their needs [ 20 ].
In a study exploring nursing and midwifery managers’ perspectives on obstacles to compassion giving and therapeutic care across 17 countries, Papadopoulos et al. [ 24 ] discovered that nurses and midwifery managers’ characteristics and experiences could facilitate or impede compassion and therapeutic interactions in nursing care. Negative personal attitudes, including selfishness, arrogance, self-centeredness, rudeness, lack of leadership skills, the desire for power, and feelings of superiority among nurses and midwifery managers, were obstacles to compassion building. The study further showed that managers who emphasize rules, tasks, and results do not prioritize relationship-building and see their staff as workers rather than team members [ 24 ]. Therefore, nurse managers and care administrators must monitor nurse-patient interaction and communication to address nurses’ concerns and support them, especially in resource-constrained and high patient turnover contexts [ 25 , 26 ].
Communication-Related Barriers
Effective communication is essential to providing patient-centered care. Studies have shown that poor communication between care providers and patients and their caregivers affects care outcomes and perceptions of care quality [ 7 , 16 , 27 , 28 ]. A consistent communication-related barrier in nurse-patient interaction is miscommunication, which often leads to misunderstandings between nurses, patients, and their families [ 20 ]. Other communication-related barriers include language differences between patients and healthcare providers [ 6 , 16 , 27 ], poor communication skills, and patients’ inability to communicate due to their health state, especially in ICU, dementia, or end-of-life care contexts [ 13 , 22 ]. For instance, in their maternity care study, Madula et al. [ 6 ] noted that language barriers significantly affected effective communication between nurses/midwives and expectant mothers. A patient in their study indicated that although many nurses were polite and communicated well, some nurses had challenges communicating with patients in the Chitumbuka language, which affected those nurses’ ability to interact effectively with patients [ 6 ].
Furthermore, Norouzinia et al. [ 21 ] asserted that effective communication could not be established when nurses and patients have a language difference. Moreover, the meanings of certain non-verbal communication acts (e.g., head nodding, eye gaze, touch) can invoke different interpretations across different cultures, which could impede the interactions between patients and nurses. Even in healthcare contexts where nurses and patients speak the same language, “differences in vocabulary, rate of speaking, age, background, familiarity with medical technology, education, physical capability, and experience can create a huge cultural and communication chasm” between nurses and patients [ 12 ]. In ICU and other similar care settings, nurses find it difficult to effectively communicate with patients because the mechanical ventilators made it hard for patients to talk [ 22 ].
To overcome the communication-related barriers, healthcare institutions must make it a responsibility to engage translators and interpreters to facilitate nurse-patient interactions where a language barrier exists. Moreover, nurses working in ICU and other similar settings should learn and employ alternative forms of communication to interact with patients.
Environment-Related Barriers
The environment of the care setting can impact nurse-patient communication and the resulting care. Thus, “good health care experiences start with a welcoming environment” [ 29 ]. Mastors believed that even though good medicine and the hands working to provide care and healing to the sick and wounded are essential, we must not “forget the small things: a warm smile, an ice chip, a warm blanket, a cool washcloth. A pillow flipped to the other side and a boost in bed” [ 29 ]. The environment-related barriers are obstacles within the care setting that inhibit nurse-patient interaction and communication and may include a noisy surrounding, unkept wards, and beds, difficulties in locating places, and navigating care services. Noisy surroundings, lack of privacy, improper ventilation, heating, cooling, and lighting in specific healthcare units can affect nurse-patient communication. These can prevent patients from genuinely expressing their healthcare needs to nurses, which can subsequently affect patient disclosure or make nursing diagnoses less accurate [ 13 , 18 , 21 ]. For instance, Amoah et al. [ 16 ] revealed that an unconducive care environment, including noisy surroundings and poor ward conditions, affected patients’ psychological states, impeding nurse-patient relationships and communication. Moreover, when care services are not well-coordinated, new patients and their caregivers find it hard to navigate the care system (e.g., locating offices for medical tests and consultations), which can constrain patient-centered care and communication.
Reducing the environment-related barriers will require making the care setting tidy/clean, less noisy, and coordinating care services in ways that make it easy for patients and caregivers to access. Coordinating and integrating care services, making care services accessible, and promoting physical comfort are crucial in promoting patient-centered care, according to Picker’s Eight Principles of Patient-Centered Care [ 30 ].
Personal and Behaviour Related Barriers
The kind of nurse-patient relationships established between nurses and patients and their caregivers will affect how they communicate. Since nurses and patients may have different demographic characteristics, cultural and linguistic backgrounds, beliefs, and worldviews about health and illnesses, nurses’, patients’, and caregivers’ attitudes can affect nurse-patient communication and care outcomes. For instance, differences in nurses’ and patients’ cultural backgrounds and belief systems have been identified as barriers to therapeutic communication and care [ 12 , 13 , 21 ]. Research shows that patients’ beliefs and cultural backgrounds affected their communication with nurses in Ghana [ 16 ]. These scholars found that some patients refused a blood transfusion, and Muslim patients refused female nurses to attend to them because of their religious beliefs [ 16 ]. Further, when nurses, patients, or their caregivers have misconceptions about one another due to past experiences, dissatisfaction about the care provided, or patients’ relatives and caregivers unduly interfere in the care process, nurse-patient communication and patient-centered care were affected [ 16 , 21 ].
Similarly, nurse-patient communication was affected when patients or caregivers failed to observe nurses’ recommendations or abuse nurses due to misunderstanding [ 20 ], while patients’ bad attitudes or disrespectful behaviours towards nurses can inhibit nurses’ ability to provide person-centered care [ 31 ]. The above-reviewed studies provided evidence on how patients’ and caregivers’ behaviours can affect nurses’ ability to communicate and deliver patient-centered care.
On the other hand, nurses’ behaviours can also profoundly affect communication and care outcomes in the nurse-patient dyad. When nurses disrespect, verbally abuse (e.g., shouting at or scolding), and discriminate against patients based on their social status, it affects nurse-patient communication, care outcomes, and patient disclosure [ 6 , 32 ]. For instance, Al-Kalaldeh et al. [ 18 ] believe that nurse-patient communication is challenged when nurses become reluctant to hear patients’ feelings and expressions of anxiety. When nurses ignore patients’ rights to share ideas and participate in their care planning, such denials may induce stress, discomfort, lack of trust in nurses, thereby leading to less satisfaction of care [ 18 ].
Furthermore, when nurses fail to listen to patients’ and caregivers’ concerns, coerce patients to obey their rules and instructions [ 16 , 17 , 20 ], or fail to provide patients with the needed information, nurse-patient communication and patient-centered care practices suffer. To illustrate, in Ddumba-Nyanzia et al.‘s study on communication between HIV care providers and patients, a patient remarked that: “I realized no matter how much I talked to the counselor, she was not listening. She was only hearing her point of view and nothing else, [and] I was very upset” [ 17 ]. This quote indicates how care provider attitudes can constrain care outcomes. Due to high workload, limited time, poor remunerations, and shortage of personnel, some nurses can develop feelings of despair, emotional detachment, and apathy towards their job, which can lead to low self-esteem or poor self-image, with negative consequences on nurse-patient interactions [ 13 , 18 ].
Given the significance of effective communication on care, overcoming the above personal and behaviour related barriers to patient-centered care and communication is crucial. Nurses, patients, and caregivers need to reflect on the consequences of their behaviours on the care process. Thus, overcoming these barriers begins with embracing the facilitators of patient-centered care and communication, which we turn to in the next section.
Facilitators of patient-centered care and communication
Patient-centered care and communication can be facilitated in several ways, including building solid nurse-patient relationships.
First, an essential facilitator of patient-centered care and communication is overcoming practical communication barriers in the nurse-patient dyad. Given the importance of communication in healthcare delivery, nurses, patients, caregivers, nursing managers, and healthcare administrators need to ensure that effective therapeutic communication is realized in the care process and becomes part of the care itself. Studies have shown that active listening among care providers is essential to addressing many barriers to patient-centered care and communication [ 7 , 13 ]. Although handling medical tasks promptly in the care process is crucial, the power of active listening is critical, meaningful, and therapeutic [ 22 ]. By listening to patients’ concerns, nurses can identify patients’ care needs and preferences and address their fears and frustrations.
Another facilitator of patient-centered care is by understanding patients and their unique needs [ 25 ], showing empathy and attending attitudes [ 7 , 13 ], expressing warmth and respect [ 22 ], and treating patients and caregivers with dignity and compassion as humans. For instance, McCabe [ 7 ] noted that attending, which obligates nurses to demonstrate that they are accessible and ready to listen to patients, is a patient-centered care process; a fundamental requirement for nurses to show genuineness and empathy, despite the high workload. Showing empathy, active listening, respect, and treating patients with dignity are core to nursing and care, and recognized in the Code of Ethics for Nurses [ 33 ], and further emphasized in the ongoing revision of the Code of Ethics for nurses [ 34 ].
Besides, engaging patients and caregivers in the care process through sharing information, inviting their opinion, and collaborating with them constitutes another facilitator of patient-centered care and communication. When patients and caregivers are engaged in the care process, misunderstandings and misconceptions are minimized. When information is shared, patients and caregivers learn more about their health conditions and the care needed. As McLean [ 14 ] argued, ensuring open communication between care providers and patients and their families is essential to enhancing patient-centered care. Conflicts ensue when patients or their families are denied information or involvement in the care process. As a result, the Harvard Medical School [ 30 ] identified patient engagement, information sharing, and nurse-patient collaboration during care as essential patient-centered care principles.
Finally, health policy must be oriented towards healthcare practices and management to facilitate patient-centered care and communication. These policies, at a minimum, can involve changes in management styles within healthcare institutions, where nurse managers and healthcare administrators reflect on nursing and care practices to ensure that the Code of Ethics of Nurses and patients’ rights are fully implemented. Resource constraints, staff shortages, and ethical dilemmas mainly affect care practices and decision-making. Nonetheless, if patients are placed at the center of care and treated with dignity and respect, most of the challenges and barriers of patient-centered care will diminish. Empowering practicing nurses, equipping them with interpersonal communication skills through regular in-service training, supporting them to overcome their emotional challenges, and setting boundaries during nurse-patient interactions will enhance patient-centered care practices.
In line with the above discussion, Camara et al. [ 25 ] identify three core dimensions that nurses, patients, and caregivers must observe to enhance patient-centered care: treating the patient as a person and seeing the care provider as a person and a confidant. Regarding the first dimension, care providers must welcome patients, listen to them, share information with them, seek their consent, and show them respect when providing care. The second dimension requires that the healthcare provider be seen and respected as a person, and negative perceptions about care providers must be demystified. According to Camara et al. [ 25 ], care providers must not overemphasize their identities as experts but rather establish good relationships with patients to understand patients’ personal needs and problems. Lastly, patients and caregivers must regard care providers as confidants who build and maintain patients’ trust and encourage patients’ participation in care conversations. With this dimension, patients and caregivers must know that nurses and other care providers have the patient at heart and work to meet their care needs and recovery process.
Camara et al.‘s [ 25 ] three dimensions are essential and position patients, their caregivers, and nurses as partners who must engage in dialogic communication to promote patient-centered care. As a result, effective communication, education, and increased health literacy among patients and caregivers will be crucial in that direction.
Enhancing Patient-Centered Care and Communication: A Proposed Model
Nursing care practices that promote patient-centered communication will directly enhance patient-centered care, as patients and their caregivers will actively engage in the care process. To enhance patient-centered communication, we propose person-centered care and communication continuum (PC4) as a guiding model to understand patient-centered communication, its pathways, and what communication and care practices healthcare professionals must implement to achieve person-centered care. In this PC4 Model, we emphasize the person instead of the patient because they are a person before becoming a patient. Moreover, the PC4 Model is supposed to apply to all persons associated with patient care; thus, respect for the dignity of their personhood is crucial.
Although much is written about patient-centered communication in the healthcare literature, there is a gap regarding its trajectory and what communication content enhances patient-centered communication. Also, little is known about how different clinical discourse spaces influence communication and its content during nurse-patient clinical interactions. Using evidence from Johnsson et al. [ 3 ], Murira et al. [ 23 ], and Liu et al. [ 35 ], among other studies, we outline the components of the PC4 Model and how different discourse spaces in the clinical setting and the content of communication impact patient-centered care and communication.
The proposed PC4 Model in this paper has three unbounded components based on the purpose of and how communication is performed among care providers, patients, and their caregivers. Figure 1 illustrates the PC4 Model, its features, and trajectory.

A Person-Centered Care and Communication Continuum (PC4 Model)
Task-Centered Communication
At the lowest end of the PC4 Model is task-centered communication. Here, the care provider’s role is to complete medical tasks as fast as possible with little or no communication with the patient and their caregivers. Patients and caregivers are treated as bodies or objects whose disease symptoms need to be studied, identified, recorded, treated, or cured. As Johnsson et al. [ 3 ] observed, communication content at this stage is mainly biomedically oriented, where nurses and other healthcare professionals focus on the precise medical information (e.g., history taking, medical examination, test results, medication, etc.) about the patient. With a task-centered orientation, nurses make journal entries about their patients’ disease state and ensure that treatment plans, diagnostic tests, and medical prescriptions are completed. Communication at this stage is often impersonal or rigid (see [ 23 ] for details). Care providers may address patients and their caregivers by using informal attributes (e.g., bed 12, the woman in the red shirt, card 8, etc.), thereby ignoring patients’ and caregivers’ personal and unique identities. Patients’ and caregivers’ nonverbal communication signs are mostly overlooked.
Motivations for task-centered communication can be attributed to time limitation, high workload, and staff shortage, thereby pushing nurses and other care providers to reach as many patients as possible. Moreover, the healthcare system’s orientation towards and preference for biomedically-focused care seems to favour task-centered communication [ 7 , 14 ].
Depending on the clinical discourse space under which patient-provider interactions occur, different forms of communication are employed. Clinical discourse spaces can be public (e.g., in the ward, patient bedside), private (e.g., consulting rooms, medical test labs, nurse staff station, etc.), or semi-private (e.g., along the corridor) [ 35 ]. In these clinical discourse spaces, nurse-patient communication can be uninformed (patients or caregivers are not informed about patients’ care conditions or why specific data and routines are performed). It can be non-private (others can hear what the nurse and patient are talking about) or authoritative (care providers demonstrate power and control and position themselves as experts) [ 23 ]. Finally, in task-centered communication, healthcare providers often use medical jargon or terminologies [ 3 ] since the goal of communication is not to engage the patient in the process. Usually, patients or their caregivers are not allowed to ask questions, or their questions get ignored or receive superficial, incomprehensible responses.
Process-Centered Communication
Process-centered communication is an intermediate stage on the continuum, which could slip back into the task-centered or leap forward into person-centered communication. Through process-centered communication, care providers make an effort to know patients and their caregivers as they perform care routines. Care providers ask patients or their caregivers questions to understand the care conditions but may not encourage patients or caregivers to express their thoughts about their care needs. Patients and caregivers are recognized as persons with uniques care needs but may not have the agency to influence the care process. Care providers may chit-chat with patients or their caregivers to pass the time as they record patients’ medical records or provide care. Unlike task-centered communication, there is informative and less authoritative communication between nurses and patients and their caregivers. The goal of process-centered communication could be a mixture of instrumental and relational, with less display of power and control by nurses.
Person-Centered Communication
This is the highest point of the PC4 Model, where patient-centered care is actualized. At this stage of the communication continuum, patients and caregivers are treated as unique persons with specific care needs and are seen as collaborators in the care process. As McLean [ 14 ] observed, caregiving becomes a transactional relationship between the care provider and receiver at the person-centered stage of the continuum. The care itself becomes intersubjective, a mutual relational practice, and an ongoing negotiation for care providers and receivers [ 14 ].
The content of communication at this stage of the continuum is both “personal” and “explanatory” [ 3 ]. Nurses and other healthcare providers create meaningful relationships with patients and their caregivers, understand patients’ concerns, needs, and problems, use open-ended questions to encourage patients or caregivers to express their thoughts and feelings about the care situation. Nurses and other healthcare professionals explain care routines, patients’ health conditions, and management plans in lay language to patients and caregivers through person-centered communication. Accomplishing this level includes employing alternative forms of communication to meet the needs of intensive care unit patients, deaf patients, and ventilated and intubated patients. For instance, it has been shown that “deaf people […] frequently do not have access to clear and efficient communication in the healthcare system, which deprives them of critical health information and qualified health care” [ 36 ]. Empathetic communication practices, including active listening, showing genuine interest in patients’ care, and respect and warmth, become a significant part of nursing care [ 3 , 7 , 14 , 22 ].
Different communication strategies are employed based on the care situation and context. Chit-chatting, as a form of personal communication [ 3 ], use of humor as a communication strategy [ 7 , 8 ], and even maintaining silence [ 28 ] are essential in enhancing person-centered care and communication. Both care providers and patients or their caregivers use relationship-building and -protecting humor (see [ 28 ] for details) to address difficult situations in the care process.
Implications of the PC4 Model for Nursing Practice
Given the values of effective communication in nurse-patient interactions and care outcomes, nurses and other healthcare providers must ensure that they develop therapeutic relationships with patients, their families, and caregivers to promote person-centered care and communication. Achieving that begins with knowing and reflecting on the barriers of therapeutic communication and ways to minimize them. The PC4 Model draws nurses and all healthcare providers’ attention to patient-centered care pathways and how effective communication is necessary. Healthcare professionals, including nurses, must be aware of how their communication orientation–––either oriented toward completing tasks, following care processes or toward addressing patients’ and their caregivers’ needs––can impact patient-centered care. Healthcare providers must observe the care context, patients’ unique situations, their non-verbal language and action, and whether they belong to historically marginalized groups or cultures.
Mastors [ 29 ] has offered healthcare providers some guidance to reflect on as they communicate and interact with patients and caregivers. Thus, (a) instead of asking patients, “What’s the matter?“ care providers must consider asking them, “What’s important to you?“ With this question, the patient is given a voice and empowered to contribute to their own care needs. Care providers should (b) check with patients in the waiting room to update patients whose waiting time has been longer than usual, based on the care context. They should also (c) try to remember their conversations with patients to build on them during subsequent interactions. This continuity can be enhanced by nurse managers reexamining how they deploy care providers to patients. The same nurse can be assigned to the same patients for the duration of the patient’s stay to help patients feel valued and visible [ 29 ].
Knowledge of cultural competence, sensitivity, humility, and interpersonal communication skills will help achieve and implement the PC4 Model. As Cuellar [ 37 ] argues, “[h]umility is about understanding and caring for all people [and] being empathetic.“ Cultural competence is a “dynamic process of acquiring the ability to provide effective, safe, and quality care to the patients through considering their different cultural aspects” [ 38 ]. The concept of cultural competence entails “cultural openness, awareness, desire, knowledge and sensitivity” during care [ 39 ]. It demands that care providers respect and tailor care to align with patients’ and caregivers’ values, needs, practices, and expectations, based on care and moral ethics and understanding [ 39 ]. Active listening and showing compassion as therapeutic relationship-building skills are essential, and continuous education and mentorship will be crucial to developing these skills among healthcare providers.
We invite qualitative and quantitative studies, especially on language use and communication strategies, to explore and evaluate the PC4 Model. Providing in-depth and experiential data on ways to increase its effectiveness as a tool to guide healthcare providers is highly desired. More knowledge can support healthcare providers in offering evidence-based patient-centered care in different healthcare settings and units.
Conclusions
Effective communication is an essential factor in nurse-patient interactions and a core component of nursing care. When communication in the nurse-patient dyad is patient-centered, it becomes therapeutic. It allows for trust and mutual respect in the care process, thereby promoting care practices that address patients’ and caregivers’ needs, concerns, and preferences. We have identified the barriers and facilitators of patient-centered care and communication and proposed a person-centered care and communication continuum (PC4 Model) to demonstrate how patient-centered communication intersects with patient-centered care.
Acknowledgments
We express our gratitude to the first author’s doctoral committee members for their valuable comments, suggestions, and critique of an earlier version of this paper. We are also grateful to the anonymous reviewers for the insightful comments and suggestions that have helped us improve the study’s quality.
Authors' information
Abukari Kwame is a Ph.D. candidate in Interdisciplinary Studies in the College of Graduate and Postdoctoral Studies, University of Saskatchewan, interested in patients' rights in nurse-patient clinical communications and interactions in the hospital setting. He holds two Master of Philosophy degrees in Indigenous Studies and English Linguistics. Abukari's research interests include language use in social interaction, health communication, First/Second language acquisition, African traditional medical knowledge, and Indigenous and qualitative research methodologies.
Pammla M. Petrucka is a professor in Nursing and has international research experience with many of her graduate students from Africa, Asia, and the Caribbean. Pammla has published extensively in the field of nursing. Her research interests are vast, including child and maternal health, Indigenous peoples' health, global health, and vulnerable populations, with extensive experiences in qualitative research and indigenous research methodologies. Pammla is co-editor of the BMC Nursing journal and a reviewer for many other academic journals.
Abbreviations
Authors’ contributions.
Both authors conceived the topic. PMP recommended the literature, AK searched and added more sources, and drafted the paper. PMP reviewed the paper for intellectual content. Both AK and PMP read and approved the final version.
The authors have not received any funding for the conduct, preparation, and publication of this paper.
Availability of data and materials
Declarations.
Not Applicable.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Open access
- Published: 16 May 2024
Competency gap among graduating nursing students: what they have achieved and what is expected of them
- Majid Purabdollah 1 , 2 ,
- Vahid Zamanzadeh 2 , 3 ,
- Akram Ghahramanian 2 , 4 ,
- Leila Valizadeh 2 , 5 ,
- Saeid Mousavi 2 , 6 &
- Mostafa Ghasempour 2 , 4
BMC Medical Education volume 24 , Article number: 546 ( 2024 ) Cite this article
286 Accesses
Metrics details
Nurses’ professional competencies play a significant role in providing safe care to patients. Identifying the acquired and expected competencies in nursing education and the gaps between them can be a good guide for nursing education institutions to improve their educational practices.
In a descriptive-comparative study, students’ perception of acquired competencies and expected competencies from the perspective of the Iranian nursing faculties were collected with two equivalent questionnaires consisting of 85 items covering 17 competencies across 5 domains. A cluster sampling technique was employed on 721 final-year nursing students and 365 Iranian nursing faculties. The data were analyzed using descriptive statistics and independent t-tests.
The results of the study showed that the highest scores for students’ acquired competencies and nursing faculties’ expected competencies were work readiness and professional development, with mean of 3.54 (SD = 0.39) and 4.30 (SD = 0.45), respectively. Also, the lowest score for both groups was evidence-based nursing care with mean of 2.74 (SD = 0.55) and 3.74 (SD = 0.57), respectively. The comparison of competencies, as viewed by both groups of the students and the faculties, showed that the difference between the two groups’ mean scores was significant in all 5 core-competencies and 17 sub-core competencies ( P < .001). Evidence-based nursing care was the highest mean difference (mean diff = 1) and the professional nursing process with the lowest mean difference (mean diff = 0.70).
The results of the study highlight concerns about the gap between expected and achieved competencies in Iran. Further research is recommended to identify the reasons for the gap between the two and to plan how to reduce it. This will require greater collaboration between healthcare institutions and nursing schools.
Peer Review reports
Introduction| Background
Nursing competence refers to a set of knowledge, skills, and behaviors that are necessary to successfully perform roles or responsibilities [ 1 ]. It is crucial for ensuring the safe and high-quality care of patients [ 2 , 3 , 4 , 5 ]. However, evaluating nursing competence is challenging due to the complex, dynamic, and multi factorial nature of the clinical environment [ 3 ]. The introduction of nursing competencies and their assessment as a standard measure of clinical performance at the professional level has been highlighted by the Association of American Colleges of Nursing [ 6 , 7 ]. As a result, AACN (2020) introduces competence assessment as an emerging concept in nursing education [ 7 ].
On the other hand, the main responsibility of nursing education is to prepare graduates who have the necessary competencies to provide safe and quality care [ 3 ]. Although it is believed that it is impossible to teach everything to students, acquiring some competencies requires entering a real clinical setting and gaining work experience [ 8 ]. However, nursing students are expected to be competent to ensure patient safety and quality of care after graduation [ 9 ]. To the extent that the World Health Organization (WHO), while expressing concern about the low quality of nursing education worldwide, has recommended investing in nursing education and considers that the future to require nurses who are theoretically and clinically competent [ 5 ]. Despite efforts, the inadequate preparation of newly graduated nursing students and doubts about the competencies acquired in line with expectations to provide safe care for entering the nursing setting have become a global concern [ 10 , 11 , 12 , 13 ]. The results of studies in this field are different. The results of Amsalu et al. showed that the competence of newly graduated nursing students to provide quality and safe care was not satisfactory [ 14 ]. Some studies have also highlighted shortcomings in students’ “soft” skills, such as technical competency, critical thinking, communication, teamwork, helping roles, and professionalism [ 15 ]. Additionally, prior research has indicated that several nursing students have an unrealistic perception of their acquired competencies before entering the clinical setting and they report a high level of competence [ 2 ]. In other study, Hickerson et al. showed that the lack of preparation of nursing students is associated with an increase in patient errors and poor patient outcomes [ 16 ]. Some studies also discussed nursing competencies separately; Such as patient safety [ 17 ], clinical reasoning [ 18 ], interpersonal communication [ 19 ], and evidence-based care competence [ 20 ].
On the other hand, the growing need for safe nursing care and the advent of new educational technologies, the emergence of infectious diseases has increased the necessity of nursing competence. As a result, the nursing profession must be educated to excellence more than ever before [ 5 , 21 , 22 ]. Therefore, the self-assessment of students’ competence levels as well as the evaluation of nursing managers about the competencies expected from them is an essential criterion for all healthcare stakeholders, educators, and nursing policymakers to ensure the delivery of safe, and effective nursing care [ 9 , 23 , 24 ].
However, studies of nurse managers’ perceptions of the competence of newly graduated nursing students are limited and mostly conducted at the national level. Hence, further investigation is needed in this field [ 25 , 26 ]. Some other studies have been carried out according to the context and the needs of societies [ 3 , 26 , 27 , 28 ]. The results of some other studies in the field of students’ self-assessment of perceived competencies and managers’ and academic staff’s assessment of expected competency levels are different and sometimes contradictory, and there is the “academic-clinical gap” between expected and achieved competencies [ 25 , 29 , 30 ]. A review of the literature showed that this gap has existed for four decades, and the current literature shows that it has not changed much over time. The academe and practice settings have also been criticized for training nurses who are not sufficiently prepared to fully engage in patient care [ 1 ]. Hence, nursing managers must understand the expected competencies of newly graduated students, because they have a more complete insight into the healthcare system and the challenges facing the nursing profession. Exploration of these gaps can reveal necessities regarding the work readiness of nursing graduates and help them develop their competencies to enter the clinical setting [ 1 , 25 ].
Although research has been carried out on this topic in other countries, the educational system in those countries varies from that of Iran’s nursing education [ 31 , 32 ]. Iran’s nursing curriculum has tried to prepare nurses who have the necessary competencies to meet the care needs of society. Despite the importance of proficiency in nursing education, many nursing graduates often report feeling unprepared to fulfill expected competencies and they have deficiencies in applying their knowledge and experience in practice [ 33 ]. Firstly, the failure to define and identify the expected competencies in the nursing curriculum of Iran led to the absence of precise and efficient educational objectives. Therefore, it is acknowledged that the traditional nursing curriculum of Iran focuses more on lessons organization than competencies [ 34 ]. Secondly, insufficient attention has been given to the scheduling, location, and level of competencies in the nursing curriculum across different semesters [ 35 ]. Thirdly, the large volume of content instead of focusing on expected competencies caused nursing graduates challenged to manage complex situations [ 36 ]. Therefore, we should not expect competencies such as critical thinking, clinical judgment, problem-solving, decision-making, management, and leadership from nursing students and graduates in Iran [ 37 ]. Limited research has been conducted in this field in Iran. Studies have explored the cultural competence of nursing students [ 38 ] and psychiatric nurses [ 39 ]. Additionally, the competence priorities of nurses in acute care have been investigated [ 40 ], as well as the competency dimensions of nurses [ 41 ].
In Iran, after receiving the diploma, the students participate in a national exam called Konkur. Based on the results of this exam, they enter the field of nursing without conducting an aptitude test interview and evaluating individual and social characteristics. The 4-year nursing curriculum in Iran has 130 units including 22 general, 54 specific, 15 basic sciences, and 39 internship units. In each semester, several workshops are held according to the syllabus [ 42 ]. Instead of the expected competencies, a list of general competencies is specified as learning outcomes in the program. Accepted students based on their rank in the exam and their choice in public and Islamic Azad Universities (non-profit), are trained with a common curriculum. Islamic Azad Universities are not supported by government funding and are managed autonomously, this problem limits the access to specialized human resources and sufficient educational fields, and the lower salaries of faculty members in Azad Universities compared to the government system, students face serious challenges. Islamic Azad Universities must pay exorbitant fees to medical universities for training students in clinical departments and medical training centers, doubling these Universities’ financial problems. In some smaller cities, these financial constraints cause students to train in more limited fields of clinical training and not experience much of what they have learned in the classroom in practice and the real world of nursing. The evaluation of learners in the courses according to the curriculum is based on formative and summative evaluation with teacher-made tests, checklists, clinical assignments, conferences, and logbooks. The accreditation process of nursing schools includes two stages internal evaluation, which is done by surveying students, professors and managers of educational groups, and external accreditation is done by the nursing board. After completing all their courses, to graduate, students must participate in an exam called “Final”, which is held by each faculty without the supervision of an accreditation institution, the country’s assessment organization or the Ministry of Health, and obtain at least a score of 10 out of 20 to graduate.
Therefore, we conducted this comprehensive study as the first study in Iran to investigate the difference between the expected and perceived competence levels of final year nursing students. The study’s theoretical framework is based on Patricia Benner’s “From Novice to Expert” model [ 43 ].
Materials and methods
The present study had the following three objectives:
Determining self-perceived competency levels from the perspective of final year nursing students in Iran.
Determining expected levels of competency from the perspective of nursing faculties in Iran.
To determine the difference between the expected competencies from the perspective of nursing faculties and the achieved competencies from the perspective of final-year nursing students.
This study is a descriptive-comparative study.
First, we obtained a list of all nursing schools in the provinces of Iran from the Ministry of Health ( n = 31). From 208 Universities, 72 nursing schools were randomly selected using two-stage cluster sampling. Among the selected faculties, we chose 721 final-year nursing students and 365 nursing faculties who met the eligibility criteria for the study. Final-year nursing students who consented to participate in the study were selected. Full-time faculty members with at least 2 years of clinical experience and nurse managers with at least 5 years of clinical education experience were also included. In this study, nursing managers, in addition to their educational roles in colleges, also have managerial roles in the field of nursing. Some of these roles include nursing faculty management, nursing board member, curriculum development and review, planning and supervision of nursing education, evaluation, and continuous improvement of nursing education. The selection criteria were based on the significant role that managers play in nursing education and curriculum development [ 44 ]. Non-full-time faculty members and managers without clinical education experience were excluded from the study.
The instrument used in this study is a questionnaire developed and psychometrically tested in a doctoral nursing dissertation [ 45 ]. To design the tool, the competencies expected of undergraduate nursing students in Iran and worldwide were first identified through a scoping review using the methodology recommended by the Joanna Briggs Institute (JBI) and supported by the PAGER framework. Summative content analysis by Hsieh and Shannon (2005) was used for analysis, which included: counting and comparing keywords and content, followed by interpretation of textual meaning. In the second step, the results of the first step were used to create tool statements. Then the validity of the instrument was checked by face validity, content validity (determination of the ratio and index of content validity), and validity of known groups. Its reliability was also checked by internal consistency using Cronbach’s alpha method and stability using the test-retest method. The competency questionnaire comprises 85 items covering 17 competencies across 5 domains: “individualized care” (4 competencies with 21 items), “evidence-based nursing care” (2 competencies with 10 items), “professional nursing process” (3 competencies with 13 items), “nursing management” (2 competencies with 16 items), and “work readiness and professional development” (6 competencies with 25 items) [ 45 ]. “The Bondy Rating Scale was utilized to assess the competency items, with ratings ranging from 1 (Dependent) to 5 (Independent) on a 5-point Likert scale [ 46 ]. The first group (nursing students) was asked to indicate the extent to which they had acquired each competency. The second group (nursing faculties) was asked to specify the level to which they expected nursing students to achieve each competency.
Data collection
First, the researcher contacted the deans and managers of the selected nursing schools by email to obtain permission. After explaining the aims of the study and the sampling method, we obtained the telephone number of the representative of the group of final year nursing students and also the email of the faculty members. The representative of the student group was then asked to forward the link to the questionnaire to 10 students who were willing to participate in the research. Informed consent for students to participate in the online research was provided through the questionnaires, while nursing faculty members who met the eligibility criteria for the study received an informed consent form attached to the email questionnaire. The informed consent process clarified the study objectives and ensured anonymity of respondent participation in the research, voluntary agreement to participate and the right to revoke consent at any time. An electronic questionnaire was then sent to 900 final year nursing students and 664 nursing faculties (from 4 March 2023 to 11 July 2023). Reminder emails were sent to nursing faculty members three times at two-week intervals. The attrition rate in the student group was reported to be 0 (no incomplete questionnaires). However, four questionnaires from nursing faculty members were discarded because of incomplete responses. Of the 900 questionnaires sent to students and 664 sent to nursing faculties, 721 students and 365 nursing faculty members completed the questionnaire. The response rates were 79% and 66% respectively.
Data were analyzed using SPSS version 22. Frequencies and percentages were used to report categorical variables and mean and standard deviations were used for quantitative variables. The normality of the quantitative data was confirmed using the Shapiro-Wilk and Skewness tests. An independent t-test was used for differences between the two groups.
Data analysis revealed that out of 721 students, 441 (61.20%) was female. The mean and deviation of the students’ age was 22.50 (SD = 1.21). Most of the students 577 (80%) were in their final semester. Also, of the total 365 faculties, the majority were female 253 (69.31%) with a mean of age 44.06 (SD = 7.46) and an age range of 22–65. The academic rank of most nursing faculty members 156 (21.60%) was assistant professor (Table 1 ).
The results of the study showed that in both groups the highest scores achieved by the students and expected by the nursing faculty members were work readiness and professional development with a mean and standard deviation of 3.54 (0.39) and 4.30 (0.45) respectively. The lowest score for both groups was also evidence-based nursing care with a mean and standard deviation of 2.74 (0.55) for students and 3.74 (0.57) for nursing faculty members (Table 2 ).
Also, the result of the study showed that the highest expected competency score from the nursing faculty members’ point of view was the safety subscale. In other words, faculty members expected nursing students to acquire safety competencies at the highest level and to be able to provide safe care independently according to the rating scale (Mean = 4.51, SD = 0.45). The mean score of the competencies achieved by the students was not above 3.77 in any of the subscales and the highest level of competency achievement according to self-report of students was related to safety competencies (mean = 3.77, SD = 0.51), preventive health services (mean = 3.69, SD = 0.79), values and ethical codes (mean = 3.67, SD = 0.77), and procedural/clinical skills (mean = 3.67, SD = 0.71). The other competency subscales from the perspective of the two groups are presented in Table 3 , from highest to lowest score.
The analysis of core competencies achieved and expected from both students’ and nursing faculty members’ perspectives revealed that, firstly, there was a significant difference between the mean scores of the two groups in all five core competencies ( P < .001) and that the highest mean difference was related to evidence-based care with mean diff = 1 and the lowest mean difference was related to professional care process with mean diff = 0.70 (Table 4 ).
Table 5 indicates that there was a significant difference between the mean scores achieved by students and nursing faculty members in all 5 core competencies and 17 sub-core Competencies ( p < .001).
The study aimed to determine the difference between nursing students’ self-perceived level of competence and the level of competence expected of them by their nursing faculty members. The study results indicate that students scored highest in work readiness and professional development. However, they were not independent in this competency and required support. The National League for Nursing (NLN) recognizes nursing professional development as the goal of nursing education programs [ 47 ] However, Aguayo-Gonzalez [ 48 ] believes that the appropriate time for professional development is after entering a clinical setting. This theme includes personal characteristics, legality, clinical/ procedural skills, patient safety, preventive health services, and mentoring competence. Personality traits of nursing students are strong predictors of coping with nursing stress, as suggested by Imus [ 49 ]. These outcomes reflect changes in students’ individual characteristics during their nursing education. Personality changes, such as the need for patience and persistence in nursing care and understanding the nurse identity prepare students for the nursing profession, which is consistent with the studies of Neishabouri et al. [ 50 ]. Although the students demonstrated a higher level of competence in this theme, an examination of the items indicates that they can still not adapt to the challenges of bedside nursing and to use coping techniques. This presents a concerning issue that requires attention and resolution. Previous studies have shown that nursing education can be a very stressful experience [ 51 , 52 , 53 ].
Of course, there is no consensus on the definition of professionalism and the results of studies in this field are different. For example, Akhtar et al. (2013) identified common viewpoints about professionalism held by nursing faculty and students, and four viewpoints emerged humanists, portrayers, facilitators, and regulators [ 54 ]. The findings of another study showed that nursing students perceived vulnerability, symbolic representation, role modeling, discontent, and professional development are elements that show their professionalism [ 55 ]. The differences indicate that there may be numerous contextual variables that affect individuals’ perceptions of professionalism.
The legal aspects of nursing were the next item in this theme that students needed help with. The findings of studies regarding the legal competence of newly graduated nursing students are contradictory reported that only one-third of nurse managers were satisfied with the legal competence of newly graduated nursing students [ 56 , 57 ]. Whereas the other studies showed that legality was the highest acquired competence for newly graduated nursing students [ 58 , 59 ]. However, the results of this study indicated that legality may be a challenge for newly graduated nursing students. Benner [ 43 ] highlighted the significant change for new graduates in that they now have full legal and professional responsibility for the patient. Tong and Epeneter [ 60 ] also reported that facing an ethical dilemma is one of the most stressful factors for new graduates. Therefore, the inexperience of new graduates cannot reduce the standard of care that patients expect from them [ 60 ]. Legal disputes regarding the duties and responsibilities of nurses have increased with the expansion of their roles. This is also the case in Iran. Nurses are now held accountable by law for their actions and must be aware of their legal obligations. To provide safe healthcare services, it is essential to know of professional, ethical, and criminal laws related to nursing practice. The nursing profession is accountable for the quality of services delivered to patients from both professional and legal perspectives. Therefore, it is a valuable finding that nurse managers should support new graduates to better deal with ethical dilemmas. Strengthening ethical education in nursing schools necessitates integrating real cases and ethical dilemmas into the curriculum. Especially, Nursing laws are missing from Iran’s undergraduate nursing curriculum. By incorporating authentic case studies drawn from clinical practice, nursing schools provide students with opportunities to engage in critical reflection, ethical analysis, and moral deliberation. These real cases challenge students to apply ethical principles to complex and ambiguous situations, fostering the development of ethical competence and moral sensitivity. Furthermore, ethical reflection and debriefing sessions during clinical experiences enable students to discuss and process ethical challenges encountered in practice, promoting self-awareness, empathy, and professional growth. Overall, by combining theoretical instruction with practical application and the use of real cases, nursing schools can effectively prepare future nurses to navigate ethical dilemmas with integrity and compassion.
However, the theme of evidence-based nursing care was the lowest scoring, indicating that students need help with this theme. The findings from studies conducted in this field are varied. A limited number of studies reported that nursing students were competent to implement evidence-based care [ 61 ], while other researchers reported that nursing students’ attitudes toward evidence-based care to guide clinical decisions were largely negative [ 20 , 62 ]. The principal barriers to implementing evidence-based care are lack of authority to change patient care policy, slow dissemination of evidence and lack of time at the bedside to implement evidence [ 10 ], and lack of knowledge and awareness of the process of searching databases and evaluating research [ 63 ]. While the European Higher Education Area (EHEA) framework and the International Council of Nurses Code of Ethics introduce the ability to identify, critically appraise, and apply scientific information as expected learning outcomes for nursing students [ 64 , 65 ], the variation in findings highlights the complexity of the concept of competence and its assessment [ 23 ]. Evidence-Based Nursing (EBN) education for nursing students is most beneficial when it incorporates a multifaceted approach. Interactive workshops play a crucial role, providing students with opportunities to critically appraise research articles, identify evidence-based practices, and apply them to clinical scenarios. Simulation-based learning further enhances students’ skills by offering realistic clinical experiences in a safe environment. Additionally, clinical rotations offer invaluable opportunities for students to observe and participate in evidence-based practices under the guidance of experienced preceptors. Journal clubs foster a culture of critical thinking and ongoing learning, where students regularly review and discuss current research articles. Access to online resources such as databases and evidence-based practice guidelines allows students to stay updated on the latest evidence and best practices. To bridge the gap between clinical practice and academic theory, collaboration between nursing schools and healthcare institutions is essential. This collaboration can involve partnerships to create clinical learning environments that prioritize evidence-based practice, inter professional education activities to promote collaboration across disciplines, training and support for clinical preceptors, and continuing education opportunities for practicing nurses to strengthen their understanding and application of EBN [ 66 ]. By implementing these strategies, nursing education programs can effectively prepare students to become competent practitioners who integrate evidence-based principles into their clinical practice, ultimately improving patient outcomes.
The study’s findings regarding the second objective showed that nursing faculty members expected students to achieve the highest level of competence in work readiness and professional development, and the lowest in evidence-based nursing care competence. The results of the studies in this area revealed that there is a lack of clarity about the level of competence of newly graduated nursing students and that confusion about the competencies expected of them has become a major challenge [ 13 , 67 ]. Evidence of nurse managers’ perceptions of newly graduated nursing student’s competence is limited and rather fragmented. There is a clear need for rigorous empirical studies with comprehensive views of managers, highlighting the key role of managers in the evaluation of nurse competence [ 1 , 9 ]. Some findings also reported that nursing students lacked competence in primary and specialized care after entering a real clinical setting [ 68 ] and that nursing managers were dissatisfied with the competence of students [ 30 ].
The results of the present study on the third objective confirmed the gap between expected and achieved competence requirements. The highest average difference was related to evidence-based nursing care, and the lowest mean difference was related to the professional nursing process. The findings from studies in this field vary. For instance, Brown and Crookes [ 13 ] reported that newly graduated nursing students were not independent in at least 26 out of 30 competency domains. Similar studies have also indicated that nursing students need a structured program after graduation to be ready to enter clinical work [ 30 ]. It can be stated that the nursing profession does not have clear expectations of the competencies of newly graduated nursing students, and preparing them for entry into clinical practice is a major challenge for administrators [ 13 ]. These findings can be explained by the Duchscher transition shock [ 69 ]. It is necessary to support newly graduated nursing students to develop their competence and increase their self-confidence.
The interesting but worrying finding was the low expectations of faculty members and the low scores of students in the theme of evidence-based care. However, nursing students need to keep their competencies up to date to provide safe and high-quality care. The WHO also considers the core competencies of nurse educators to be the preparation of effective, efficient, and skilled nurses who can teach the evidence-based learning process and help students apply it clinically [ 44 ]. The teaching of evidence-based nursing care appears to vary across universities, and some clinical Faculties do not have sufficient knowledge to support students. In general, it can be stated that the results of the present study are in line with the context of Iran. Some of the problems identified include a lack of attention to students’ academic talent, a lack of a competency-based curriculum, a gap between theory and clinical practice, and challenges in teaching and evaluating the achieved competencies [ 42 ].
Strengths and limitations
The study was conducted on a national level with a sizable sample. It is one of the first studies in Iran to address the gap between students’ self-perceived competence levels and nursing faculty members’ expected competency levels. Nevertheless, one of the limitations of the study is the self-report nature of the questionnaire, which may lead to social desirability bias. In addition, the COVID-19 pandemic coinciding with the student’s first and second years could potentially impact their educational quality and competencies. The limitations established during the outbreak negatively affected the nursing education of students worldwide.
Acquiring nursing competencies is the final product of nursing education. The current study’s findings suggest the existence of an academic-practice gap, highlighting the need for educators, faculty members, and nursing managers to collaborate in bridging the potential gap between theory and practice. While nursing students were able to meet some expectations, such as value and ethical codes, there is still a distance between expectations and reality. Especially, evidence-based care was identified as one of the weaknesses of nursing students. It is recommended that future research investigates the best teaching strategies and more objective assessments of competencies. The findings of this study can be used as a guide for the revision of undergraduate nursing education curricula, as well as a guide for curriculum development based on the development of competencies expected of nursing students. Nursing managers can identify existing gaps and plan to fill them and use them for the professionalization of students. This requires the design of educational content and objective assessment tools to address these competencies at different levels throughout the academic semester. This significant issue necessitates enhanced cooperation between healthcare institutions and nursing schools. Enhancing nursing education requires the implementation of concrete pedagogical strategies to bridge the gap between theoretical knowledge and practical skills. Simulation-based learning emerges as a pivotal approach, offering students immersive experiences in realistic clinical scenarios using high-fidelity simulators [ 70 ]. Interprofessional education (IPE) is also instrumental, in fostering collaboration among healthcare professionals and promoting holistic patient care. Strengthening clinical preceptorship programs is essential, with a focus on providing preceptors with formal training and ongoing support to facilitate students’ clinical experiences and transition to professional practice [ 71 ]. Integrating evidence-based practice (EBP) principles throughout the curriculum cultivates critical thinking and inquiry skills among students, while technology-enhanced learning platforms offer innovative ways to engage students and support self-directed learning [ 72 ]. Diverse and comprehensive clinical experiences across various healthcare settings ensure students are prepared for the complexities of modern healthcare delivery. By implementing these practical suggestions, nursing education programs can effectively prepare students to become competent and compassionate healthcare professionals.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Huston C, et al. The academic-practice gap: strategies for an enduring problem . In nursing forum . Wiley Online Library; 2018.
Meretoja R, Isoaho H, Leino-Kilpi H. Nurse competence scale: development and psychometric testing. J Adv Nurs. 2004;47(2):124–33.
Article Google Scholar
Järvinen T, et al. Nurse educators’ perceptions of factors related to the competence of graduating nursing students. Nurse Educ Today. 2021;101:104884.
Satu KU, et al. Competence areas of nursing students in Europe. Nurse Educ Today. 2013;33(6):625–32.
World Health Organization. State of the world’s nursing 2020: investing in education, jobs and leadership. 2020 [cited 12 June 2023; https://www.who.int/publications-detail-redirect/9789240003279 .
Lee W-H, Kim S, An J. Development and evaluation of korean nurses’ core competency scale (KNCCS) 2017.
American Association of Colleges of Nursing. The essentials: core competencies for professional nursing education… 2020 [cited 2023; https://www.aacnnursing.org/Portals/0/PDFs/Publications/Essentials-2021.pdf .
Gardulf A, et al. The Nurse Professional competence (NPC) scale: self-reported competence among nursing students on the point of graduation. Nurse Educ Today. 2016;36:165–71.
Kajander-Unkuri S, et al. The level of competence of graduating nursing students in 10 European countries-comparison between countries. Nurs Open. 2021;8(3):1048–62.
Labrague LJ et al. A Multicountry Study on Nursing Students’ Self-Perceived Competence and Barriers to Evidence‐Based Practice 2019. 16(3): pp. 236–246.
Visiers-Jiménez L, et al. Clinical learning environment and graduating nursing students’ competence: a multi-country cross-sectional study. Nurs Health Sci. 2021;23(2):398–410.
Herron EK. New graduate nurses’ preparation for recognition and prevention of failure to rescue: a qualitative study. J Clin Nurs. 2018;27(1–2):e390–401.
Google Scholar
Brown RA, Crookes PA. What are the ‘necessary’ skills for a newly graduating RN? Results of an Australian survey. BMC Nurs. 2016;15:23.
Amsalu B, et al. Clinical practice competence of Mettu University nursing students: a cross-sectional study. Adv Med Educ Pract. 2020;11:791–8.
Song Y, McCreary LL. New graduate nurses’ self-assessed competencies: an integrative review. Nurse Educ Pract. 2020;45:102801.
Hickerson KA, Taylor LA, Terhaar MF. The Preparation-Practice gap: an Integrative Literature Review. J Contin Educ Nurs. 2016;47(1):17–23.
Huang FF, et al. Self-reported confidence in patient safety competencies among Chinese nursing students: a multi-site cross-sectional survey. BMC Med Educ. 2020;20(1):32.
Hong S et al. A Cross-Sectional Study: What Contributes to Nursing Students’ Clinical Reasoning Competence? Int J Environ Res Public Health, 2021. 18(13).
Mcquitty DJPE, Counseling. Teaching interpersonal communication concepts to increase awareness and reduce health disparities: Presenter (s): DaKysha Moore, NCAT, United States 2023. 109: pp. 25–26.
Lam CK, Schubert CF, Herron EK. Evidence-based practice competence in nursing students preparing to transition to practice. Worldviews Evid Based Nurs. 2020;17(6):418–26.
Lake MA. What we know so far: COVID-19 current clinical knowledge and research. Clin Med (Lond). 2020;20(2):124–7.
Shustack L. Integrating Google Earth in Community Health nursing courses: preparing globally aware nurses. Nurse Educ. 2020;45(2):E11–2.
Zeleníková R, et al. Self-assessed competence of final-year nursing students. Nurs Open. 2023;10(7):4607–18.
Hyun A, Tower M, Turner C. Exploration of the expected and achieved competency levels of new graduate nurses. J Nurs Manag. 2020;28(6):1418–31.
Kukkonen P, et al. Nurse managers’ perceptions of the competence of newly graduated nurses: a scoping review. J Nurs Manag. 2020;28(1):4–16.
Nilsson J et al. Nurse professional competence (NPC) assessed among newly graduated nurses in higher educational institutions in Europe. 2019. 39(3): p. 159–67.
Kajander-Unkuri S et al. Students’ Self-assessed Competence Levels during Nursing Education Continuum - A Cross-sectional Survey. Int J Nurs Educ Scholarsh, 2020. 17(1).
Salminen L, et al. The competence of nurse educators and graduating nurse students. Nurse Educ Today. 2021;98:104769.
Numminen O, et al. Newly graduated nurses’ competence and individual and organizational factors: a multivariate analysis. J Nurs Scholarsh. 2015;47(5):446–57.
Södersved Källestedt ML, et al. Perceptions of managers regarding prerequisites for the development of professional competence of newly graduated nurses: a qualitative study. J Clin Nurs. 2020;29(23–24):4784–94.
Ezzati E, et al. Exploring the social accountability challenges of nursing education system in Iran. BMC Nurs. 2023;22(1):7.
Farsi Z, et al. Comparison of Iran’s nursing education with developed and developing countries: a review on descriptive-comparative studies. BMC Nurs. 2022;21(1):105.
Salem OA et al. Competency based nursing curriculum: establishing the standards for nursing competencies in higher education. 2018. 5(11): p. 1–8.
Noohi E, Ghorbani-Gharani L. and A.J.S.i.D.o.M.E. Abbaszadeh, A comparative study of the curriculum of undergraduate nursing education in Iran and selected renowned universities in the world 2015. 12(3): pp. 450–471.
Rassouli M, Zagheri Tafreshi M. J.J.o.c.e. Esmaeil. Challenges Clin Nurs Educ Iran Strategies. 2014;2(1):11–22.
Riazi S, et al. Understanding gaps and needs in the undergratue nursing curriculum in Iran: a prelude to design a competency-based curriculum model %J payesh (Health Monitor). Journal. 2020;19(2):145–58.
ADIB HM, Mazhariazad F. Nursing Bachelor’s Education program in Iran and UCLA: A comparative study 2019.
Farokhzadian J, et al. Using a model to design, implement, and evaluate a training program for improving cultural competence among undergraduate nursing students: a mixed methods study. BMC Nurs. 2022;21(1):85.
Sargazi O, et al. Improving the professional competency of psychiatric nurses: results of a stress inoculation training program. Psychiatry Res. 2018;270:682–7.
Faraji A, et al. Evaluation of clinical competence and its related factors among ICU nurses in Kermanshah-Iran: a cross-sectional study. Int J Nurs Sci. 2019;6(4):421–5.
Atashzadeh-Shoorideh F, et al. Essential dimensions of professional competency examination in Iran from academic and clinical nurses’ perspective: a mixed-method study. J Educ Health Promot. 2021;10:414.
Purabdollah M, et al. Comparison of the Iranian and scandinavian bachelor of nursing curriculum (Sweden): a scoping review. J Educ Health Promotion. 2023;12(1):389.
Benner P. J.B.o.s., technology and society, using the Dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education . 2004. 24(3): p. 188–99.
World Health Organization. Nurse educator core competencies. Geneva, Switzerland: World Health Organization. 2016 [cited 23 June 2023; https://www.who.int/hrh/nursing_midwifery/nurse_educator050416.pdf .
Purabdollah M, et al. Competencies expected of undergraduate nursing students: a scoping review. Nurs Open. 2023;10(12):7487–508.
Bondy KN. Clinical evaluation of student performance: the effects of criteria on accuracy and reliability. Res Nurs Health. 1984;7(1):25–33.
NLf N. Outcomes for graduates of practical/vocational, diploma, associate degree, baccalaureate, master’s, practice doctorate, and research doctorate programs in nursing . New York 2010; 201]. https:api.semanticscholar.org/corpus ID: 68620057.
Aguayo-González M, Castelló-Badía M, Monereo-Font C. Critical incidents in nursing academics: discovering a new identity. Rev Bras Enferm. 2015;68(2):195–202. 219 – 27.
Scott Imus FJJNEP. Nurse anesthesia student’s personality characteristics and academic performance: A big five personality model perspective 2019. 9: pp. 47–55.
Neishabouri M, Ahmadi F, Kazemnejad A. Iranian nursing students’ perspectives on transition to professional identity: a qualitative study. Int Nurs Rev. 2017;64(3):428–36.
Zheng S, et al. New nurses’ experience during a two year transition period to clinical practice: a phenomenological study. Nurse Educ Today. 2023;121:105682.
Aryuwat P, et al. An integrative review of resilience among nursing students in the context of nursing education. Nurs Open. 2023;10(5):2793–818.
Ayaz-Alkaya S, Simones J. Nursing education stress and coping behaviors in Turkish and the United States nursing students: a descriptive study. Nurse Educ Pract. 2022;59:103292.
Akhtar-Danesh N, et al. Perceptions of professionalism among nursing faculty and nursing students. West J Nurs Res. 2013;35(2):248–71.
Keeling J, Templeman J. An exploratory study: student nurses’ perceptions of professionalism. Nurse Educ Pract. 2013;13(1):18–22.
Nilsson J, et al. Development and validation of a new tool measuring nurses self-reported professional competence–the nurse professional competence (NPC) scale. Nurse Educ Today. 2014;34(4):574–80.
Berkow S, et al. Assessing new graduate nurse performance. J Nurs Adm. 2008;38(11):468–74.
Lofmark A, Smide B, Wikblad K. Competence of newly-graduated nurses–a comparison of the perceptions of qualified nurses and students. J Adv Nurs. 2006;53(6):721–8.
Park E, Choi J. Attributes associated with person-centered care competence among undergraduate nursing students. Res Nurs Health. 2020;43(5):511–9.
Tong V, Epeneter BJ. A comparative study of newly licensed registered nurses’ stressors: 2003 and 2015. J Contin Educ Nurs. 2018;49(3):132–40.
Florin J, et al. Educational support for research utilization and capability beliefs regarding evidence-based practice skills: a national survey of senior nursing students. J Adv Nurs. 2012;68(4):888–97.
Reid J, et al. Enhancing utility and understanding of evidence based practice through undergraduate nurse education. BMC Nurs. 2017;16:58.
Phillips JM, Cullen D. Improving the adoption of evidence-based practice through RN-to-BSN education. J Contin Educ Nurs. 2014;45(10):467–72.
Stievano A, Tschudin V. The ICN code of ethics for nurses: a time for revision. Int Nurs Rev. 2019;66(2):154–6.
Ministry of Education and Research. Norwegian qualifications framework: levels and learning outcome descriptors… 2011 [cited 23 June 2023; https://www.regjeringen.no/contentassets/e579f913fa1d45c2bf2219afc726670b/nkr.pdf .
Chen Q, et al. Differences in evidence-based nursing practice competencies of clinical and academic nurses in China and opportunities for complementary collaborations: a cross‐sectional study. J Clin Nurs. 2023;32(13–14):3695–706.
Missen K, McKenna L, Beauchamp A. Registered nurses’ perceptions of new nursing graduates’ clinical competence: a systematic integrative review. Nurs Health Sci. 2016;18(2):143–53.
Leonardsen AL, et al. Nurses’ perspectives on technical skill requirements in primary and tertiary healthcare services. Nurs Open. 2020;7(5):1424–30.
Duchscher JE. B.J.J.o.a.n. Transition Shock: Initial Stage role Adaptation New Graduated Registered Nurses. 2009;65(5):1103–13.
Ajemba MN, Ikwe C, Iroanya JC. Effectiveness of simulation-based training in medical education: assessing the impact of simulation-based training on clinical skills acquisition and retention: a systematic review. World J Adv Res Reviews. 2024;21(1):1833–43.
Krystallidou D et al. Interprofessional education for healthcare professionals. A BEME realist review of what works, why, for whom and in what circumstances in undergraduate health sciences education: BEME Guide No. 83 Medical Teacher, 2024: pp. 1–18.
Sun Y, et al. Critical thinking abilities among newly graduated nurses: a cross-sectional survey study in China. Nurs Open. 2023;10(3):1383–92.
Download references
Acknowledgements
The authors extend their gratitude to all the nursing students and faculties who took part in this study.
This article is part of research approved with the financial support of the deputy of research and technology of Tabriz University of Medical Sciences.
Author information
Authors and affiliations.
Department of Nursing, Khoy University of Medical Sciences, Khoy, Iran
Majid Purabdollah
Medical Education Research Center, Health Management and Safety Promotion Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
Majid Purabdollah, Vahid Zamanzadeh, Akram Ghahramanian, Leila Valizadeh, Saeid Mousavi & Mostafa Ghasempour
Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Vahid Zamanzadeh
Department of Medical Surgical Nursing, Faculty of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran
Akram Ghahramanian & Mostafa Ghasempour
Department of Pediatric Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Leila Valizadeh
Department of Epidemiology and Biostatistics, Assistant Professor of Biostatistics, School of Health, Tabriz University of Medical Sciences, Tabriz, Iran
Saeid Mousavi
You can also search for this author in PubMed Google Scholar
Contributions
M P: conceptualized the study, data collection, analysis and interpretation, drafting of manuscript; V Z: conceptualized the study, analysis and interpretation, drafting of manuscript; LV: conceptualized the study, data collection and analysis, manuscript revision; A Gh: conceptualized the study, data collection, analysis, and drafting of manuscript; S M: conceptualized the study, analysis, and drafting of manuscript; M Gh: data collection, analysis, and interpretation, drafting of manuscript; All authors read and approved the final manuscript.
Ethics declarations
Ethics approval and consent to participate.
All the participants voluntarily participated in this study and provided written informed consent. The study was approved by the ethics committee of the Tabriz University of Medical Sciences (Ethical Code: IR.TBZMED.REC.1400.791) and all methods were performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Purabdollah, M., Zamanzadeh, V., Ghahramanian, A. et al. Competency gap among graduating nursing students: what they have achieved and what is expected of them. BMC Med Educ 24 , 546 (2024). https://doi.org/10.1186/s12909-024-05532-w
Download citation
Received : 23 November 2023
Accepted : 07 May 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s12909-024-05532-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nursing education
- Self-Assessment
- Nursing students
- Professional Competency Professional
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Fostering career interest in community nursing: early strategic approaches in education, clinical placements, and mentorship for nursing students are crucial
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Ayan Mack 1 ,
- http://orcid.org/0000-0002-7499-5050 Tanvir C Turin 1 , 2
- 1 Department of Community Health Sciences , University of Calgary Cumming School of Medicine , Calgary , Alberta , Canada
- 2 Department of Family Medicine , University of Calgary Cumming School of Medicine , Calgary , Alberta , Canada
- Correspondence to Dr Tanvir C Turin, Department of Community Health Sciences, University of Calgary Cumming School of Medicine, Calgary, Canada; turin.chowdhury{at}ucalgary.ca
https://doi.org/10.1136/ebnurs-2024-104076
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- Nurses- Community Health
Commentary on: Chee, JMP, Rusli KDB, Tan ZYA, Tan AJQ, Ang SGM, Lau ST, Seah B, Liaw SY. Perceptions of community care among nursing students: A cross-sectional study with implications to the nursing workforce. Nurse Education Today . 2024; 137:106162. 10.1016/j.nedt.2024.106162
Implications for education and research
With the shift towards delivering healthcare services in homes, communities and primary healthcare settings, nursing curricula should integrate community nursing early in the program and provide diverse placements with mentorship opportunities to highlight career paths in this specialty.
Future research should explore effective implementation strategies to enhance student perceptions of community care and address workforce challenges in this field.
The increasing demand for postacute and home-based care programmes creates an urgent need to expand the community nursing workforce. 1 However, a gap in attracting graduates into community care contributes to a problematic shortage of community nurses. 1 2 Nurse shortages can seriously affect community health by impeding healthcare access and worsening disparities leading to inferior health outcomes. Since nursing students represent the future workforce, their perspectives on community care remain important. 2 A cross-sectional study conducted by Chee et al 2 at Singapore University explored the perceptions of undergraduate nursing students regarding community care and their placement preferences to identify factors discouraging them from pursuing careers in community nursing. Identifying these deterrents can address the nursing workforce gap and improve community health and well-being.
With a 55.7% response rate (501/900), the majority of participants were first-year students(32.5%), females (82.8%) and of Chinese ethnicity (84.4%). Only one-third of the participants had positive perceptions of community nursing and preferred placement in community care settings. Most students preferred acute care hospitals (68.7%) for placement. Those who preferred home-based or intermediate long-term care placements had a more optimistic view of community nursing compared with those favouring acute care settings. Perceptions varied across students’ years. The results highlight the complexity of factors influencing students’ placement preferences and the connection of their preferences to their career aspirations.
Community health nurses play a critical role in delivering personalised precision healthcare services beyond the confines of traditional hospital settings. By reaching into communities, these nurses provide essential services tailored to the needs of individuals and families, promoting health and fostering wellness. 1 2 However, despite the increasing demand for their services, the field faces significant challenges in attracting graduates. This challenge stems from misconceptions about the roles and responsibilities of community nurses and perceived limited career advancement within this specialisation. 2 Consequently, many nursing students gravitate towards acute care hospital settings; as a result, there is a noticeable workforce gap in the community. 4
The preference of nursing graduates for acute care or specialty settings can significantly exacerbate workforce shortages in the community, widening health disparities and limiting access to quality healthcare, particularly in vulnerable populations. These factors indicate the emergence of a significant societal problem that urgently requires resolution. 1 Effectively mitigating this challenge demands concerted collaboration among nursing educational institutions, healthcare entities and policy-makers. Through strategic endeavours, we can improve the workforce deficit, cultivate a favourable perception of the field to attract new graduates and champion the pivotal role of community health nursing. 4
Key strategies to promote community nursing may include integrating community care experiences early into the nursing curriculum and providing exposure through structured programmes, workshops and quality community placement opportunities with positive role model mentors. 1 2 4 Immersing students in the unique responsibilities of community nurses can dispel misconceptions and inspire them to make a meaningful difference in the communities they serve. Additionally, offering quality placements in community settings through mentorship allows students to gain firsthand experience and develop competencies outside of traditional hospital environments, fostering an optimistic community nursing career outlook. 4 An influx of graduates, including culturally and linguistically competent nurses, into community nursing roles can enhance access to quality healthcare, particularly for underserved communities, significantly improving the long-term health and well-being of all communities.
- van Iersel M ,
- Latour CHM ,
- de Vos R , et al
- Rusli KDB ,
- Tan ZYA , et al
- Latour C , et al
- Frauendienst R
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:
This paper is in the following e-collection/theme issue:
Published on 22.5.2024 in Vol 26 (2024)
The Power of Rapid Reviews for Bridging the Knowledge-to-Action Gap in Evidence-Based Virtual Health Care
Authors of this article:

- Megan MacPherson, PhD ;
- Sarah Rourke, MSN
Fraser Health, Surrey, BC, Canada
Corresponding Author:
Megan MacPherson, PhD
Fraser Health
400-13450 102nd Avenue
Surrey, BC, V3T 0H1
Phone: 1 6045616605
Email: [email protected]
Despite the surge in popularity of virtual health care services as a means of delivering health care through technology, the integration of research evidence into practice remains a challenge. Rapid reviews, a type of time-efficient evidence synthesis, offer a potential solution to bridge the gap between knowledge and action. This paper aims to highlight the experiences of the Fraser Health Authority’s Virtual Health team in conducting rapid reviews. This paper discusses the experiences of the Virtual Health team in conducting 15 rapid reviews over the course of 1.5 years and the benefit of involving diverse stakeholders including researchers, project and clinical leads, and students for the creation of user-friendly knowledge products to summarize results. The Virtual Health team found rapid reviews to be a valuable tool for evidence-informed decision-making in virtual health care. Involving stakeholders and focusing on implementation considerations are crucial for maximizing the impact of rapid reviews. Health care decision makers are encouraged to consider implementing rapid review processes to improve the translation of research evidence into practice, ultimately enhancing patient outcomes and promoting a culture of evidence-informed care.
Introduction
Virtual health care services, which involve the delivery of health care through information and communication technologies, have gained popularity among health care providers, patients, and organizations. In recent decades, several initiatives have been undertaken to implement virtual care and improve the access, quality, and safety of health care delivery in Canada [ 1 ]; however, technological advancement and a rapidly expanding evidence base make supporting virtual care with research evidence challenging. Specifically, to adequately support virtual care, health care decision makers are expected to keep up with available technologies, their applications, and evidence of their effectiveness among a variety of health conditions.
Despite decision makers recognizing the need to consider research evidence in the context of public health problems [ 2 , 3 ], there is still a knowledge-to-action (KTA) gap between what is known and what is put into practice clinically [ 4 - 6 ], with health care professionals worldwide demonstrating suboptimal use of research evidence within clinical practice [ 7 - 14 ]. Further, it has been estimated that one-third of patients do not receive treatments that have proven efficacious, one-quarter receive treatments that are potentially harmful, and up to three-quarters of patients and half of clinicians do not receive the information necessary for research-informed decision-making [ 15 ]. Clearly, there is a need to improve the translation of research evidence into practice, particularly in the case of virtual care where technological innovations and research evidence are rapidly expanding.
Knowledge Translation
The field of knowledge translation (KT) strives to enhance the usefulness of research evidence through the design and conduct of stakeholder-informed, patient-oriented studies as well as the dissemination and implementation of research findings into practice [ 16 ]. The Canadian Institutes for Health Research defines KT as the ethical exchange, synthesis, and application of knowledge among researchers and users to accelerate the benefits of research for Canadian people [ 17 ]. The ultimate goal of KT has been further described as the facilitation of evidence-informed decision-making [ 18 ] and the integration of various forms of evidence into public health practice and policy.
The Canadian Institutes for Health Research describes 2 “Death Valleys” on the continuum from research to action, which contributes to the KTA gap [ 19 ]. Valley 1 refers to the reduced ability to translate basic biomedical research discoveries from the laboratory to the bedside and to effectively commercialize health innovations. Valley 2 refers to the reduced ability to synthesize, disseminate, and integrate research findings more broadly into clinical practice and clinical decision-making. To improve the utility of biomedical and clinical research, enhance health outcomes, and ensure an evidence-based and sustainable health care system, strategic attempts to bridge these valleys must be made.
Rapid Reviews
One way to help overcome the second valley is through evidence syntheses such as systematic, scoping, and rapid reviews [ 20 ]. Evidence syntheses have emerged as valuable methods for KT as they can compile large bodies of evidence into a single knowledge product, making them an essential tool for decision makers to enhance evidence-informed decision-making [ 21 , 22 ]. Systematic reviews offer a comprehensive synthesis of available evidence on a particular topic, playing an ever-expanding role in informing policy making and practice [ 23 , 24 ]; however, the resource-intensive nature of conducting systematic reviews, in terms of both time and cost, presents a significant obstacle to facilitating prompt and efficient decision-making [ 25 ].
Given the time constraints health care practitioners and policy makers often face [ 26 ], rapid reviews provide a more resource- and time-efficient means to conduct evidence syntheses that offer actionable evidence in a more relevant manner compared to other types of evidence syntheses such as systematic or scoping reviews [ 20 , 26 - 34 ]. Specifically, rapid reviews are a form of evidence synthesis in which systematic review steps are streamlined to generate actionable evidence within a condensed time frame [ 35 ]. To expedite the review process, rapid reviews often compromise on the rigor typically associated with systematic reviews, resulting in a less precise and robust evaluation in comparison [ 32 ]. That being said, rapid reviews have gained traction in health systems’ policy making, health-related intervention development, and health technology assessment [ 34 - 36 ]. This paper outlines the experiences of the Fraser Health (FH) Authority Virtual Health team in rapidly producing and disseminating rapid review results to date. Rapid reviews were chosen as they are often highly driven by end-user demands [ 37 ] and have been highlighted as a viable tool to disseminate knowledge within the rapidly growing field of virtual health [ 33 ].
FH Authority Context
As the largest regional health authority in British Columbia, Canada, FH serves more than 1.9 million people in Canada [ 38 ]. In recent years, FH has prioritized the expansion of virtual care [ 39 ], conducting over 1.9 million virtual visits between January 2019 and 2023 (roughly 27% of all visits). Within the Virtual Health department at FH, the “research and evaluation team” aims to improve the translation of research into practice while engaging in ongoing collaborative evaluation of existing Virtual Health programming. During Virtual Health strategic planning, rapid reviews have emerged as a central tool for knowledge dissemination and have been used to inform the development of frameworks, services, and program scale-up. This paper highlights FH’s experience in conducting 15 rapid reviews over the course of 1.5 years. This paper is meant to serve as an overview on the utility and feasibility of rapid reviews within a health authority; for more information on rapid review methods to aid in conducting reviews within a team-based setting, see MacPherson et al [ 33 ].
Rapid reviews are used within the Virtual Health team to provide an overview of available evidence addressing a research question related to a single topic produced within a short time frame (typically 1 week to 4 months). From October 2022 until March 2024, the Virtual Health team conducted 15 rapid reviews following published recommendations [ 33 ]. Questions posed to date include the following:
- What are the perspectives on virtual care among immigrant, refugee, and Indigenous people in Canada [ 40 ]?
- What virtual care solutions exist for people with heart failure [ 41 ]?
- What virtual care solutions exist for people with diabetes [ 41 ]?
- What virtual care solutions exist for people with chronic obstructive pulmonary disease (COPD) [ 41 ]?
- What are currently used decision guides or algorithms to inform escalation within remote patient monitoring services for people with heart failure?
- What barriers, facilitators, and recommendations exist for remote patient monitoring services within the context of respiratory care [ 42 ]?
- What virtual care or digital innovations are used by physicians in acute care [ 43 ]?
- What barriers and facilitators exist for patient-to-provider virtual messaging (eg, SMS text messaging) [ 44 ]?
- What is the existing evidence for centralized remote patient monitoring services [ 45 ]?
- What domains are included within virtual care frameworks targeting appropriateness and safety?
- What are patient and provider barriers to virtual care [ 46 ]?
- What is the evidence for virtual hospital programs [ 47 ]?
- What KT strategies exist that could be used by the Virtual Health research and evaluation team in their efforts to translate research findings into practice?
- What is the available evidence on virtual decision-making and clinical judgment?
- What is the available evidence for, and are there existing validated assessment criteria for nursing assessment frameworks?
Team members assisting with the rapid reviews included researchers, project leads, clinical leads, and students previously unfamiliar with the review process. Knowledge users within the Virtual Health team (eg, clinical leads and clinical directors) were involved throughout the entirety of the review process from developing the research questions to the presentation of research findings in Virtual Health team meetings and the implementation of findings into Virtual Health practice.
Similar to other rapid reviews [ 20 ], results were collated and narratively or visually summarized (eg, through infographics) and presented to Virtual Health team members. The final knowledge products were created to offer a high-level overview of the evidence arranged in a user-friendly manner, aiming to provide VH team members with a high-level understanding of the available evidence [ 41 ].
Experiences and Lessons Learned
The Virtual Health team’s journey in conducting 15 rapid reviews over the course of 1.5 years has provided valuable insights into the feasibility and utility of rapid reviews within a health authority setting. These lessons learned are from the perspectives of the authors of this paper. MM is the research and KT lead of the Virtual Health department at the FH Authority. Prior to creating the rapid review program within the Virtual Health department, she has prior experience conducting systematic, scoping, and rapid reviews. SR is a clinical nurse specialist within the Virtual Health department at FH. As a system-level leader, SR leverages evidence to informed clinical and service model changes to optimize patient care and outcomes and support strategic priorities. Prior to her involvement in the Virtual Health rapid review program, SR had no previous experience with conducting evidence reviews.
Importance of Defining a Clear and Actionable Research Question
Throughout this journey, one of the key lessons learned was about the importance of the research question being actionable to ensure that the results of rapid reviews can be readily integrated into practice. Initially, our reviews had broader scopes aimed at informing future Virtual Health service implementations across various populations such as COPD, diabetes, and heart failure. While these reviews were informative, they did not lead to immediate changes in Virtual Health practice and required strategic efforts to disseminate findings and integrate results into practice. Subsequently, we learned that focusing on specific programs or initiatives within the Virtual Health setting yields more actionable results. For instance, a review focused on identifying patient and provider barriers to virtual care was conducted with the explicit purpose of informing the development of a framework to improve video visit uptake among primary care providers. This targeted approach enabled us to directly address the identified barriers through the development of a framework focused on the uptake of safe and appropriate video visits within primary care.
Benefits and Challenges Involving Knowledge Users
The involvement of knowledge users such as clinical leads and directors in the rapid review process proved to be invaluable. First, they helped focus the scope of reviews by providing insights into the practical needs and priorities within the FH context. For example, the reviews focusing on virtual care solutions for patients with heart failure, COPD, and diabetes were initiated by 1 of the directors within Virtual Health and included an occupational therapist and clinical nurse specialist on the review team. The diverse insights offered by clinician team members helped shape the review questions, search strategy, and analysis, ensuring it addressed the practical needs in delivering virtual care to this specific patient population.
Second, the engagement of nonresearchers, students, and health care professionals in the review process not only enhanced the quality and relevance of the rapid reviews but also provided an opportunity for experiential learning and professional development. By participating in the rapid review process, students and other team members developed essential skills such as critical appraisal, evidence synthesis, and scientific communication. This approach has the potential to bridge the gap between research and practice by building a generation of clinicians who are well versed in evidence-based practice and can effectively translate research findings into clinical decision-making. For example, a team of nursing students participated in a rapid review focused on algorithms for care escalation within remote patient monitoring services for patients with heart failure. While they lacked prior review experience, their fresh perspectives and familiarity with health care practice as it relates to heart failure brought unique insights helping to shape the clinician-oriented KT efforts.
While involving knowledge users throughout the review process offers numerous benefits, it can also extend the time required to complete a review. This is often due to the necessity for these individuals to familiarize themselves with new software while simultaneously mastering the intricacies of conducting reviews and adhering to all associated steps. For instance, several Virtual Health team members have observed that during their initial and subsequent reviews, they encountered difficulties in efficiently navigating the study screening phase. The abundance of potentially relevant literature posed a challenge, with concerns arising about potentially overlooking papers containing valuable insights or “hidden gems.” This underscores the importance of establishing clear eligibility criteria and providing comprehensive training from the outset to ensure reviewers feel empowered to exclude papers confidently, even those that may initially appear intriguing.
Resources and Staff Time Involved
Readers interested in starting a rapid review program in their own health systems may find it helpful to understand the resources and staff time involved in our process. As the research and KT lead within the Virtual Health team, MM has been responsible for building the rapid review program, training team members, and leading rapid reviews. Her full-time role allows for dedicated focus on these as well as other research and KT-related activities, ensuring the smooth operation of the rapid review process.
Additionally, strong leadership support within the Virtual Health team has been instrumental in fostering a culture of evidence-informed decision-making and facilitating the integration of research evidence into practice. While we do not have a core team with a dedicated full-time equivalent specifically for rapid reviews, a call is put out to the Virtual Health department at the beginning of a review to identify who has the capacity to assist in a review. A testament to the value of these reviews is that VH team members have begun autonomously conducting rapid reviews with the research and KT lead acting as an advisor, not a lead on the reviews. For example, a nurse who was tasked with creating a framework for a virtual nursing assessment requested assistance in running a search for her team to complete a rapid review, to ensure that the resulting framework did not miss any key components seen in the literature.
Rapid Review Process
The overall process map for our team (an adaptation of MacPherson et al [ 33 , 48 ]) can be found in Figure 1 . Our journey in conducting rapid reviews has been accompanied by several challenges and the implementation of quality assurance measures to ensure the integrity of our findings. The overall process of reviews within the Virtual Health team includes Virtual Health team members submitting a request or having an informal meeting with the research and KT lead outlining the scope and purpose of the review, which is then refined to ensure that it will result in actionable evidence relevant to the Virtual Health team and is in alignment with organizational priorities.
Challenges or obstacles encountered during the rapid review process have included resource constraints. When there are not enough people to assist with a review, either the time to complete the review needs to be extended or additional constraints must be placed on the review question. Time limitations have also been a factor, especially when there is an urgent request. Clear communication on how the results will be used is needed to refine the review topic and search strategy to quickly produce actionable evidence. Given the wealth of research, we have started all reviews by first exploring if our questions can be answered by conducting a review of reviews. This has allowed for the timely synthesis of evidence instead of relying on individual studies. We have also found that decision makers value the most up-to-date evidence (especially regarding virtual health care technologies); as such, many of our reviews have imposed limitations to the past 5-10 years to ensure their relevance to decision makers. Additionally, difficulties in accessing relevant literature have been noted, as health authorities often do not have access to the same resources as academic institutions. This results in increased time to secure papers through interlibrary loans, which can be overcome by collaborating with academics.

Another strength of the Virtual Health team’s rapid review approach was the development of easily digestible knowledge products highlighting key data synthesized in the review. Rather than providing end users with lengthy reports that often go unread, clinicians within the Virtual Health team helped to create brief summaries and infographics highlighting the main findings and recommendations. This approach was aimed at improving the uptake of research evidence into practice by presenting the information in a format that was easily accessible and understandable for clinicians and other stakeholders. By creating visually appealing and user-friendly knowledge products, the Virtual Health team was able to efficiently communicate key takeaways from the rapid reviews, thus facilitating their dissemination and implementation within the FH context. This approach also helped to overcome a common challenge of KT, where research evidence can be difficult to access, understand, and apply in practice. By presenting the information in a format that was relevant and easily digestible, the Virtual Health team was able to enhance the applicability of the rapid reviews, thereby building clinician capacity and increasing their potential impact on patient outcomes.
Leveraging Rapid Reviews for Clinically Based Tools
Our most recent reviews were focused on developing a virtual nursing assessment and virtual nursing decision-making framework. Unlike traditional KT efforts used within other reviews, where the focus often lies on creating user-friendly summaries and infographics, our approach took a slightly different path. We aimed to directly inform the development of clinical decision support tools (DSTs).
Rather than developing traditional KT products, the raw data extracted from these reviews served as a foundational resource for the development of the clinical DSTs. Each piece of information was carefully referenced and integrated into the tool, providing evidence-based support for specific components and functionalities. This direct integration of research evidence into the tool development process not only strengthened the validity and credibility of the tool but also facilitated the transparent communication of the evidence behind each recommendation or feature.
Within these reviews, the active participation of those who were responsible for the development of the DSTs proved invaluable. Their involvement was crucial in ensuring understanding and confidence in the information as well as in merging research evidence with their own clinical expertise. By involving end users in the review process, we could tailor the outcomes to their specific needs and preferences, ultimately enhancing the relevance and applicability of the extracted evidence. This collaborative approach ensured that the resulting DSTs were not only evidence based but also resonated effectively with the clinical context they were intended for.
Principal Findings
The Virtual Health team’s experience with conducting 15 rapid reviews over the course of 1.5 years highlights the potential of rapid reviews as a time-efficient tool for improving the translation and uptake of research evidence into Virtual Health programming. Compared to more traditional review types (eg, systematic or scoping), which can take more than a year to complete [ 49 ], rapid reviews provide a practical way of synthesizing available evidence to inform clinical decision-making. The ability to produce a high-quality evidence summary in a shorter time frame can be particularly valuable in rapidly evolving areas of health care, such as virtual health. While rapid reviews are not new, our program offers insights into their application in a dynamic and rapidly evolving field such as virtual health. The lessons learned from FH’s rapid review program have important implications for evidence-based decision-making and KT within health care settings.
One of our primary lessons learned underscores the importance of establishing clear and actionable research questions. By outlining precise objectives, rapid reviews can ensure the relevance and applicability of their results, thus facilitating their seamless integration into clinical practice. Moreover, our experiences highlight the transformative impact of involving knowledge users throughout the review process. This collaborative approach not only enhances the quality and relevance of the evidence synthesized but also fosters a culture of evidence-informed decision-making within the organization. This type of early and continued engagement of knowledge users in research endeavors has been increasingly recognized as pivotal for establishing research priorities and enhancing the utility of research findings in real-world health care contexts [ 50 , 51 ]. In line with this, the overarching goal of knowledge-user engagement in health research is to coproduce knowledge that directly addresses the needs of decision makers. By involving knowledge users from the outset, research priorities can be aligned with the practical requirements of health care delivery, thereby increasing the relevance and utility of research outputs [ 52 - 54 ].
Limitations of Rapid Reviews
Despite its benefits, the rapid review approach is not without limitations. Loss of rigor, as mentioned earlier in this paper, remains a concern. The rapid nature of the process may compromise the depth and comprehensiveness of the literature search and synthesis, potentially leading to oversights or biases in the evidence presented. Furthermore, within the context of virtual health, the rapid pace of technological advancements poses a challenge. New technologies may outpace the generation of peer-reviewed literature, resulting in a lag between their implementation and the availability of robust evidence.
In response to the challenge posed by rapidly evolving technologies, FH’s Virtual Health department has used creative solutions to capture relevant evidence. While peer-reviewed literature remains a primary source, we have also incorporated gray literature, such as news articles, trade publications, and reports, from other health care authorities or departments within the review processes when applicable. Additionally, to supplement reviews and provide more contextual evidence, additional research and evaluation methodologies are used (time permitting) to inform Virtual Health service development such as consulting Patient and Family Advisory Councils within FH, conducting interviews with patient and clinician partners, and conducting analyses on existing data within FH.
Next Steps for FH’s Rapid Review Program
We remain committed to advancing the rapid review program to meet the evolving needs of the Virtual Health department at FH. While we have heard anecdotally that knowledge users value the user-friendly knowledge products developed for rapid reviews, the next steps of this program include an evaluation of our knowledge dissemination to assess the reach and impact the reviews are having within the Virtual Health department.
Conclusions
Rapid reviews are a valuable tool for the timely synthesis of available research evidence to inform health care decision-making. The Virtual Health team’s experience with conducting rapid reviews highlights the importance of involving a diverse range of knowledge users in the review process and the need to focus on implementation considerations. By engaging knowledge users beyond designated researchers, and particularly by involving clinicians across the research process, rapid reviews become more robust, applicable, and aligned with the practical needs of health care providers and organizations, which can help to bridge the KTA gap.
Conflicts of Interest
None declared.
- Goodridge D, Marciniuk D. Rural and remote care: overcoming the challenges of distance. Chron Respir Dis. 2016;13(2):192-203. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bowen S, Zwi AB. Pathways to "evidence-informed" policy and practice: a framework for action. PLoS Med. 2005;2(7):e166. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jacobs JA, Jones E, Gabella BA, Spring B, Brownson RC. Tools for implementing an evidence-based approach in public health practice. Prev Chronic Dis. 2012;9:E116. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Davis D, Evans M, Jadad A, Perrier L, Rath D, Ryan D, et al. The case for knowledge translation: shortening the journey from evidence to effect. BMJ. 2003;327(7405):33-35. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003;362(9391):1225-1230. [ CrossRef ] [ Medline ]
- Grol R, Jones R. Twenty years of implementation research. Fam Pract. 2000;17(Suppl 1):S32-S35. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Straus SE, McAlister FA. Evidence-based medicine: a commentary on common criticisms. CMAJ. 2000;163(7):837-841. [ FREE Full text ] [ Medline ]
- Mellis C. Evidence-based medicine: what has happened in the past 50 years? J Paediatr Child Health. 2015;51(1):65-68. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Villar J, Carroli G, Gülmezoglu AM. The gap between evidence and practice in maternal healthcare. Int J Gynaecol Obstet. 2001;75(Suppl 1):S47-S54. [ Medline ]
- Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001;39(8 Suppl 2):II46-II54. [ CrossRef ] [ Medline ]
- Schuster MA, McGlynn EA, Brook RH. How good is the quality of health care in the United States? Milbank Q. 1998;76(4):517-563. [ FREE Full text ] [ CrossRef ] [ Medline ]
- McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635-2645. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lauer MS, Skarlatos S. Translational research for cardiovascular diseases at the National Heart, Lung, and Blood Institute: moving from bench to bedside and from bedside to community. Circulation. 2010;121(7):929-933. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lang ES, Wyer PC, Haynes RB. Knowledge translation: closing the evidence-to-practice gap. Ann Emerg Med. 2007;49(3):355-363. [ CrossRef ] [ Medline ]
- Kitson AL, Straus SE. Identifying knowledge to action gaps. Knowledge Transl Health Care. 2013:97-109. [ FREE Full text ] [ CrossRef ]
- Graham ID, Logan JL, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26(1):13-24. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Knowledge translation strategy 2004-2009: innovation in action. Canadian Institutes of Health Research. 2004. URL: https://cihr-irsc.gc.ca/e/26574.html [accessed 2024-04-25]
- Ciliska D, Thomas H, Buffett C. A compendium of critical appraisal tools for public health practice. National Collaborating Centre for Methods and Tools. 2008. URL: https://www.nccmt.ca/uploads/media/media/0001/01/b331668f85bc6357f262944f0aca38c14c89c5a4.pdf [accessed 2024-04-25]
- Canada's strategy for patient-oriented research. Government of Canada. Canadian Institutes of Health Research. 2011. URL: https://cihr-irsc.gc.ca/e/44000.html#a1.1 [accessed 2023-04-06]
- Khangura S, Konnyu K, Cushman R, Grimshaw J, Moher D. Evidence summaries: the evolution of a rapid review approach. Syst Rev. 2012;1(1):10. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chambers D, Wilson PM, Thompson CA, Hanbury A, Farley K, Light K. Maximizing the impact of systematic reviews in health care decision making: a systematic scoping review of knowledge-translation resources. Milbank Q. 2011;89(1):131-156. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7(1):50. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bosch-Capblanch X, Lavis JN, Lewin S, Atun R, Røttingen JA, Dröschel D, et al. Guidance for evidence-informed policies about health systems: rationale for and challenges of guidance development. PLoS Med. 2012;9(3):e1001185. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Oxman AD, Lavis JN, Lewin S, Fretheim A. SUPPORT tools for evidence-informed health policymaking (STP). Norwegian Knowledge Centre for the Health Services. 2010. URL: https://fhi.brage.unit.no/fhi-xmlui/bitstream/handle/11250/2378076/NOKCrapport4_2010.pdf?sequence=1 [accessed 2023-11-22]
- Oliver K, Innvar S, Lorenc T, Woodman J, Thomas J. A systematic review of barriers to and facilitators of the use of evidence by policymakers. BMC Health Serv Res. 2014;14(1):2. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ganann R, Ciliska D, Thomas H. Expediting systematic reviews: methods and implications of rapid reviews. Implement Sci. 2010;5(1):56. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Moore G, Redman S, Rudge S, Haynes A. Do policy-makers find commissioned rapid reviews useful? Health Res Policy Syst. 2018;16(1):17. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Flores EJ, Jue JJ, Giradi G, Schoelles K, Mull NK, Umscheid CA. AHRQ EPC Series on improving translation of evidence: use of a clinical pathway for C. Difficile treatment to facilitate the translation of research findings into practice. Jt Comm J Qual Patient Saf. 2019;45(12):822-828. [ CrossRef ] [ Medline ]
- Hartling L, Guise J, Kato E, Anderson J, Belinson S, Berliner E, et al. A taxonomy of rapid reviews links report types and methods to specific decision-making contexts. J Clin Epidemiol. 2015;68(12):1451-1462.e3. [ CrossRef ] [ Medline ]
- Hartling L, Guise JM, Kato E, Anderson J, Aronson N, Belinson S, et al. EPC Methods: An Exploration of Methods and Context for the Production of Rapid Reviews. Rockville, MD. Agency for Healthcare Research and Quality; 2015.
- Hartling L, Guise JM, Hempel S, Featherstone R, Mitchell MD, Motu'apuaka ML, et al. Fit for purpose: perspectives on rapid reviews from end-user interviews. Syst Rev. 2017;6(1):32. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Featherstone RM, Dryden DM, Foisy M, Guise JM, Mitchell MD, Paynter RA, et al. Advancing knowledge of rapid reviews: an analysis of results, conclusions and recommendations from published review articles examining rapid reviews. Syst Rev. 2015;4(1):50. [ FREE Full text ] [ CrossRef ] [ Medline ]
- MacPherson MM, Wang RH, Smith EM, Sithamparanathan G, Sadiq CA, Braunizer AR. Rapid reviews to support practice: a guide for professional organization practice networks. Can J Occup Ther. 2023;90(3):269-279. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Watt A, Cameron A, Sturm L, Lathlean T, Babidge W, Blamey S, et al. Rapid reviews versus full systematic reviews: an inventory of current methods and practice in health technology assessment. Int J Technol Assess Health Care. 2008;24(2):133-139. [ CrossRef ] [ Medline ]
- Polisena J, Garritty C, Kamel C, Stevens A, Abou-Setta AM. Rapid review programs to support health care and policy decision making: a descriptive analysis of processes and methods. Syst Rev. 2015;4(1):26. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Harker J, Kleijnen J. What is a rapid review? A methodological exploration of rapid reviews in health technology assessments. Int J Evid Based Healthc. 2012;10(4):397-410. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Garritty C, Gartlehner G, Nussbaumer-Streit B, King VJ, Hamel C, Kamel C, et al. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol. 2021;130:13-22. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Fraser Health. 2023. URL: https://www.fraserhealth.ca/ [accessed 2023-04-06]
- Virtual Health. Fraser Health. URL: https://www.fraserhealth.ca/patients-and-visitors/virtual-health [accessed 2023-04-06]
- MacPherson M. Immigrant, refugee, and Indigenous Canadians' experiences with virtual health care services: rapid review. JMIR Hum Factors. 09, 2023;10:e47288. [ FREE Full text ] [ CrossRef ] [ Medline ]
- MacPherson M. Virtual care in heart failure, chronic obstructive pulmonary disease, and diabetes: a rapid review protocol. OSF Registries. 2023. URL: https://osf.io/xn2pe [accessed 2023-09-11]
- MacPherson M. Barriers, facilitators, and recommendations to inform the expansion of remote patient monitoring services for respiratory care: a rapid review. OSF Registries. 2022. URL: https://osf.io/asf2v/ [accessed 2024-04-25]
- MacPherson M. Virtual health services in the context of acute care: a rapid review. OSF Registries. 2023. URL: https://osf.io/ub2d8/ [accessed 2024-04-25]
- MacPherson MM, Kapadia S. Barriers and facilitators to patient-to-provider messaging using the COM-B model and theoretical domains framework: a rapid umbrella review. BMC Digit Health. 2023;1(1):33. [ FREE Full text ] [ CrossRef ]
- Chan L, MacPherson M. Remote patient monitoring: an evidence synthesis. OSF Registries. 2023. URL: https://osf.io/7wqb8/ [accessed 2024-04-25]
- Montenegro M, MacPherson M. Barriers to virtual care experienced by patients and healthcare providers: a rapid umbrella review. OSF Registries. 2023. URL: https://osf.io/nufg4/ [accessed 2024-04-25]
- Montenegro M, MacPherson M. Virtual hospitals: a rapid review. OSF Registries. 2023. URL: https://osf.io/m3a4b/ [accessed 2024-04-25]
- Attribution 4.0 International (CC BY 4.0). Creative Commons. URL: https://creativecommons.org/licenses/by/4.0/ [accessed 2024-05-13]
- Borah R, Brown AW, Capers PL, Kaiser KA. Analysis of the time and workers needed to conduct systematic reviews of medical interventions using data from the PROSPERO registry. BMJ Open. 2017;7(2):e012545. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Deverka PA, Lavallee DC, Desai PJ, Esmail LC, Ramsey SD, Veenstra DL, et al. Stakeholder participation in comparative effectiveness research: defining a framework for effective engagement. J Comp Eff Res. 2012;1(2):181-194. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bragge P, Clavisi O, Turner T, Tavender E, Collie A, Gruen RL. The Global Evidence Mapping Initiative: scoping research in broad topic areas. BMC Med Res Methodol. 2011;11(1):92. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Langlois EV, Montekio VB, Young T, Song K, Alcalde-Rabanal J, Tran N. Enhancing evidence informed policymaking in complex health systems: lessons from multi-site collaborative approaches. Health Res Policy Syst. 2016;14(1):20. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Vindrola-Padros C, Pape T, Utley M, Fulop NJ. The role of embedded research in quality improvement: a narrative review. BMJ Qual Saf. 2017;26(1):70-80. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ghaffar A, Langlois EV, Rasanathan K, Peterson S, Adedokun L, Tran NT. Strengthening health systems through embedded research. Bull World Health Organ. 2017;95(2):87. [ FREE Full text ] [ CrossRef ] [ Medline ]

Abbreviations
Edited by Z Yin; submitted 22.11.23; peer-reviewed by W LaMendola, M Willenbring, Y Zhang, P Blasi; comments to author 10.03.24; revised version received 15.03.24; accepted 13.04.24; published 22.05.24.
©Megan MacPherson, Sarah Rourke. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 22.05.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Best Nursing Research Topics for Students
What is a nursing research paper.
- What They Include
- Choosing a Topic
- Best Nursing Research Topics
- Research Paper Writing Tips

Writing a research paper is a massive task that involves careful organization, critical analysis, and a lot of time. Some nursing students are natural writers, while others struggle to select a nursing research topic, let alone write about it.
If you're a nursing student who dreads writing research papers, this article may help ease your anxiety. We'll cover everything you need to know about writing nursing school research papers and the top topics for nursing research.
Continue reading to make your paper-writing jitters a thing of the past.
A nursing research paper is a work of academic writing composed by a nurse or nursing student. The paper may present information on a specific topic or answer a question.
During LPN/LVN and RN programs, most papers you write focus on learning to use research databases, evaluate appropriate resources, and format your writing with APA style. You'll then synthesize your research information to answer a question or analyze a topic.
BSN , MSN , Ph.D., and DNP programs also write nursing research papers. Students in these programs may also participate in conducting original research studies.
Writing papers during your academic program improves and develops many skills, including the ability to:
- Select nursing topics for research
- Conduct effective research
- Analyze published academic literature
- Format and cite sources
- Synthesize data
- Organize and articulate findings
About Nursing Research Papers
When do nursing students write research papers.
You may need to write a research paper for any of the nursing courses you take. Research papers help develop critical thinking and communication skills. They allow you to learn how to conduct research and critically review publications.
That said, not every class will require in-depth, 10-20-page papers. The more advanced your degree path, the more you can expect to write and conduct research. If you're in an associate or bachelor's program, you'll probably write a few papers each semester or term.
Do Nursing Students Conduct Original Research?
Most of the time, you won't be designing, conducting, and evaluating new research. Instead, your projects will focus on learning the research process and the scientific method. You'll achieve these objectives by evaluating existing nursing literature and sources and defending a thesis.
However, many nursing faculty members do conduct original research. So, you may get opportunities to participate in, and publish, research articles.
Example Research Project Scenario:
In your maternal child nursing class, the professor assigns the class a research paper regarding developmentally appropriate nursing interventions for the pediatric population. While that may sound specific, you have almost endless opportunities to narrow down the focus of your writing.
You could choose pain intervention measures in toddlers. Conversely, you can research the effects of prolonged hospitalization on adolescents' social-emotional development.
What Does a Nursing Research Paper Include?
Your professor should provide a thorough guideline of the scope of the paper. In general, an undergraduate nursing research paper will consist of:
Introduction : A brief overview of the research question/thesis statement your paper will discuss. You can include why the topic is relevant.
Body : This section presents your research findings and allows you to synthesize the information and data you collected. You'll have a chance to articulate your evaluation and answer your research question. The length of this section depends on your assignment.
Conclusion : A brief review of the information and analysis you presented throughout the body of the paper. This section is a recap of your paper and another chance to reassert your thesis.
The best advice is to follow your instructor's rubric and guidelines. Remember to ask for help whenever needed, and avoid overcomplicating the assignment!
How to Choose a Nursing Research Topic
The sheer volume of prospective nursing research topics can become overwhelming for students. Additionally, you may get the misconception that all the 'good' research ideas are exhausted. However, a personal approach may help you narrow down a research topic and find a unique angle.
Writing your research paper about a topic you value or connect with makes the task easier. Additionally, you should consider the material's breadth. Topics with plenty of existing literature will make developing a research question and thesis smoother.
Finally, feel free to shift gears if necessary, especially if you're still early in the research process. If you start down one path and have trouble finding published information, ask your professor if you can choose another topic.
The Best Research Topics for Nursing Students
You have endless subject choices for nursing research papers. This non-exhaustive list just scratches the surface of some of the best nursing research topics.
1. Clinical Nursing Research Topics
- Analyze the use of telehealth/virtual nursing to reduce inpatient nurse duties.
- Discuss the impact of evidence-based respiratory interventions on patient outcomes in critical care settings.
- Explore the effectiveness of pain management protocols in pediatric patients.
2. Community Health Nursing Research Topics
- Assess the impact of nurse-led diabetes education in Type II Diabetics.
- Analyze the relationship between socioeconomic status and access to healthcare services.
3. Nurse Education Research Topics
- Review the effectiveness of simulation-based learning to improve nursing students' clinical skills.
- Identify methods that best prepare pre-licensure students for clinical practice.
- Investigate factors that influence nurses to pursue advanced degrees.
- Evaluate education methods that enhance cultural competence among nurses.
- Describe the role of mindfulness interventions in reducing stress and burnout among nurses.
4. Mental Health Nursing Research Topics
- Explore patient outcomes related to nurse staffing levels in acute behavioral health settings.
- Assess the effectiveness of mental health education among emergency room nurses .
- Explore de-escalation techniques that result in improved patient outcomes.
- Review the effectiveness of therapeutic communication in improving patient outcomes.
5. Pediatric Nursing Research Topics
- Assess the impact of parental involvement in pediatric asthma treatment adherence.
- Explore challenges related to chronic illness management in pediatric patients.
- Review the role of play therapy and other therapeutic interventions that alleviate anxiety among hospitalized children.
6. The Nursing Profession Research Topics
- Analyze the effects of short staffing on nurse burnout .
- Evaluate factors that facilitate resiliency among nursing professionals.
- Examine predictors of nurse dissatisfaction and burnout.
- Posit how nursing theories influence modern nursing practice.
Tips for Writing a Nursing Research Paper
The best nursing research advice we can provide is to follow your professor's rubric and instructions. However, here are a few study tips for nursing students to make paper writing less painful:
Avoid procrastination: Everyone says it, but few follow this advice. You can significantly lower your stress levels if you avoid procrastinating and start working on your project immediately.
Plan Ahead: Break down the writing process into smaller sections, especially if it seems overwhelming. Give yourself time for each step in the process.
Research: Use your resources and ask for help from the librarian or instructor. The rest should come together quickly once you find high-quality studies to analyze.
Outline: Create an outline to help you organize your thoughts. Then, you can plug in information throughout the research process.
Clear Language: Use plain language as much as possible to get your point across. Jargon is inevitable when writing academic nursing papers, but keep it to a minimum.
Cite Properly: Accurately cite all sources using the appropriate citation style. Nursing research papers will almost always implement APA style. Check out the resources below for some excellent reference management options.
Revise and Edit: Once you finish your first draft, put it away for one to two hours or, preferably, a whole day. Once you've placed some space between you and your paper, read through and edit for clarity, coherence, and grammatical errors. Reading your essay out loud is an excellent way to check for the 'flow' of the paper.
Helpful Nursing Research Writing Resources:
Purdue OWL (Online writing lab) has a robust APA guide covering everything you need about APA style and rules.
Grammarly helps you edit grammar, spelling, and punctuation. Upgrading to a paid plan will get you plagiarism detection, formatting, and engagement suggestions. This tool is excellent to help you simplify complicated sentences.
Mendeley is a free reference management software. It stores, organizes, and cites references. It has a Microsoft plug-in that inserts and correctly formats APA citations.
Don't let nursing research papers scare you away from starting nursing school or furthering your education. Their purpose is to develop skills you'll need to be an effective nurse: critical thinking, communication, and the ability to review published information critically.
Choose a great topic and follow your teacher's instructions; you'll finish that paper in no time.

Joleen Sams is a certified Family Nurse Practitioner based in the Kansas City metro area. During her 10-year RN career, Joleen worked in NICU, inpatient pediatrics, and regulatory compliance. Since graduating with her MSN-FNP in 2019, she has worked in urgent care and nursing administration. Connect with Joleen on LinkedIn or see more of her writing on her website.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.

Nursing Overview: Purpose of Nursing Papers
- Evidence Based Practice
- Purpose of Nursing Papers
- Writing Assignments by Class
- Nursing Journal Articles
- Nursing Texts
- How do I find this particular article?
- Other useful resources
- Lexicomp Drug Database
- APA 7-Citations
- APA 7-Layout
- APA 7 Style
- Word Tip Videos
- Plagiarism Tutorial
- HESI & NCLEX
- Faculty Resources
- Comments/Suggestions
- Movies About Health Care
- Scholarships
What is the purpose of nursing papers?
The purpose of the nursing paper is to give the student experience in solving nursing problems using evidence-based practice (EBP). The paper is the written proof that the student understands the EBP process. The student must apply skills in the following areas:
- Identifying a nursing problem
- Selecting appropriate resources
- Communicating in own words the “gist’ of the resources
- Presenting a solution to the nursing problem by suggesting appropriate nursing interventions
- Using APA format and style to communicate the process
Learning the terminology
- What is a nursing problem?
- What is evidence based practice?
- What is an empirical study?
- What is and what is not peer reviewed?
- What is a literature review?
- What is APA style and format?
- Quote vs. Cite
A nursing problem is one that can be solved by nurses, not doctors, therapists, or even the patients themselves. These solutions are referred to as nursing interventions and are usually presented in the care plan. The appropriate intervention is unique for each patient. It is the nurse's responsibility to customize the care plan for each patient.
Evidence based practice (EBP) involves using evidence derived from appropriate scientific experiments and applying it to nursing practice.
Before nurses do anything to or for patients, they must find evidence that it works. While evidence may be derived from personal experience, for the purposes of nursing school, evidence will come primarily from empirical (original) research. You will be looking for articles that feature experiments done by nurses.
You must read the empirical research for yourself--not someone else's interpretation of that research.
To ensure quality, the empirical research should be peer reviewed and less than 5 years old.
The best place to find peer reviewed EBP is through the library databases, where you can filter by peer reviewed , among other factors. The CINAHL database provides the most filter options and is the most user friendly. Be sure to include all relevant filters for your search, but not too many or you will eliminate many relevant articles.
What counts as evidence:
- Original research: "We counted...," "We studied...," "We surveyed..."
- (Do not be misled by articles where the authors conducted a literature search . In those articles, the authors will say that their methods included a search of databases and what keywords they used..)
What does not count as evidence:
- Commentary: "I think...," "I believe...," "I feel..."
- Continuing Education: "Here is what all nurses need to know..."
- Literature Review: "Here is what other people have researched..."
While other articles may provide quality background information or explanation of the topic that may be useful in your paper, they are not evidence .
How to use empirical research in evidence based resea rch
Once you have found an empirical study, figure out what it means for nursing. How can nurses provide better care because of the evidence presented in the study? There should be some kind of problem that the researchers attempted to solve. Your paper will present the information like this:
Introduction: What is the problem?
Body: How did the researchers try to solve the problem?
Conclusion: How can nurses solve the problem?
An empirical study follows the scientific method to find a solution to a question or problem.
How to tell if the article is an empirical study:
1. Look for headings such as: Objective/Aim, Method/Methodology, Data/Results, Discussion, Conclusion
2. Read the abstract. What did the authors DO? (The authors should have done something, not just read other articles.)
Even though an article may appear in a peer reviewed journal, it is not peer reviewed unless it is an actual empirical study. Articles that appear in a peer reviewed journal, but are not peer reviewed, include: letters to the editor, commentary, continuing education, overviews.
In a literature review, the author reads empirical studies by other researchers, summarizes them and discusses an intervention based on those studies. You will read about various databases like CINAHL, MedLine, PubMed, Scopus, LILACS, a mong others.
Most empirical studies have a literature review section at the beginning in order to explain how the study will be different or to explain the background of research in the area.
As the actual research was not done by the authors of the article, you cannot use the information presented because it is not directly from the people who conducted that research.
APA format refers to what the paper looks like, i.e. the margins, font, spacing, etc. It also refers to how you write your references page and how you refer to your sources within the paper.
APA style refers to what you actually say in your paper. It guides how you phrase your sentences and how you explain your ideas.
QUOTE means word-for-word what someone else said. When you use 3 or more words directly from a source, that is a quote, and the words MUST be within quotation marks, and the in-text citation must include a page number.
Ex: "nursing students dislike writing papers" (Toups, 2019, p. 35)
CITE means whose idea it was. Even when you put ideas into your own words (paraphrase), you must still give credit to the person whose ideas they are (cite).
Ex. Nursing students prefer hands-on work as opposed to papers (Toups, 2019).
Do not substitute each word in a sentence with a synonym and think you have paraphrased.
- << Previous: Evidence Based Practice
- Next: Writing Assignments by Class >>
- Last Updated: May 20, 2024 2:13 PM
- URL: https://libguides.tccd.edu/nursing
- Open access
- Published: 03 September 2021
A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward
- Abukari Kwame 1 &
- Pammla M. Petrucka 2
BMC Nursing volume 20 , Article number: 158 ( 2021 ) Cite this article
376k Accesses
161 Citations
97 Altmetric
Metrics details
Providing healthcare services that respect and meet patients’ and caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns, beliefs, and contextual variables. Achieving patient-centered care and communication in nurse-patient clinical interactions is complex as there are always institutional, communication, environmental, and personal/behavioural related barriers. To promote patient-centered care, healthcare professionals must identify these barriers and facitators of both patient-centered care and communication, given their interconnections in clinical interactions. A person-centered care and communication continuum (PC4 Model) is thus proposed to orient healthcare professionals to care practices, discourse contexts, and communication contents and forms that can enhance or impede the acheivement of patient-centered care in clinical practice.
Peer Review reports
Providing healthcare services that respect and meet patients’ and their caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thus constituting patient-centered care. Care is “a feeling of concern for, or an interest in, a person or object which necessitates looking after them/it” [ 1 ]. The Institute of Medicine (IOM) noted that to provide patient-centered care means respecting and responding to individual patient’s care needs, preferences, and values in all clinical decisions [ 2 ]. In nursing care, patient-centered care or person-centered care must acknowledge patients’ experiences, stories, and knowledge and provide care that focuses on and respects patients’ values, preferences, and needs by engaging the patient more in the care process [ 3 ]. Healthcare providers and professionals are thus required to fully engage patients and their families in the care process in meaningful ways. The IOM, in its 2003 report on Health Professions Education , recognized the values of patient-centered care and emphasized that providing patient-centered care is the first core competency that health professionals’ education must focus on [ 4 ]. This emphasis underscored the value of delivering healthcare services according to patients’ needs and preferences.
Research has shown that effective communication between patients and healthcare providers is essential for the provision of patient care and recovery [ 5 , 6 , 7 , 8 ]. Madula et al. [ 6 ], in a study on maternal care in Malawi, noted that patients reported being happy when the nurses and midwives communicated well and treated them with warmth, empathy, and respect. However, other patients said poor communication by nurses and midwives, including verbal abuse, disrespect, or denial from asking questions, affected their perceptions of the services offered [ 6 ]. Similarly, Joolaee et al. [ 9 ] explored patients’ experiences of caring relationships in an Iranian hospital where they found that good communication between nurses and patients was regarded as “more significant than physical care” among patients.
According to Boykins [ 10 ], effective communication is a two-way dialogue between patients and care providers. In that dialogue, both parties speak and are listened to without interrupting; they ask questions for clarity, express their opinions, exchange information, and grasp entirely and understand what the others mean. Also, Henly [ 11 ] argued that effective communication is imperative in clinical interactions. He observed that health and illness affect the quality of life, thereby making health communication critical and that the “intimate and sometimes overwhelming nature of health concerns can make communicating with nurses and other healthcare providers very challenging” [ 11 ]. Furthermore, Henly [ 11 ] added that patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns. Given the prevalence of face-to-face and device-mediated communications and interactions in healthcare settings, we must explore and clarify who, what, where, when, why, and how interactions with individuals, families, and communities are receiving care and health services [ 11 ].
The value of effective communication in nurse-patient clinical interactions cannot be overemphasized, as “research has shown that communication processes are essential to more accurate patient reporting and disclosure” [ 12 ]. Respectful communication between nurses and patients can reduce uncertainty, enhance greater patient engagement in decision making, improve patient adherence to medication and treatment plans, increase social support, safety, and patient satisfaction in care [ 12 , 13 ]. Thus, effective nurse-patient clinical communication is essential to enhancing patient-centered care and positive care outcomes.
Patient-centered communication, also known as person-centered communication or client-centered communication, is defined as a process that invites and encourages patients and their families to actively participate and negotiate in decision-making about their care needs, as cited in [ 7 ]. Patient-centered communication is crucial in promoting patient-centered care and requires that patients and their caregivers engage in the care process. As McLean [ 14 ] observed, patient-centered care can be enhanced through patient-centered communication by valuing patients’ dignity and rights. Through open communication and collaboration, where information and care plans are shared among care providers, patients, and their families, care provision becomes patient-centered [ 14 ].
Given the interconnected nature of patient-centered care and communication, we must identify the barriers and enablers of patient-centered care and communication and proposed efficient ways to enhance that because patient-centered communication is essential in achieving patient-centered care. Our aim in this paper is to identify the barriers and facilitators of patient-centered care and communication and propose and present a patient-centered care and communication continuum (PC4) Model to explain how patient-centered care can be enhanced in nurse-patient clinical interactions. As Grant and Booth argued, critical reviews are often used to present, analyse, and synthesized research evidence from diverse sources, the outcome of which is a hypothesis or a model as an interpretation of existing data to enhance evidence-based practice [ 15 ]. Thus, this critical literature review study explores the questions: what are the barriers and facilitators of patient-centered care and how can patient-centered care be enhanced through effective clinical communication?
An earlier version of this study was submitted as part of author AK’s doctoral comprehensive exams in February 2021. An interdisciplinary doctoral committee recommended many of the included literature and the questions explored in this study based on the current discourse of patient-centered care advocated for in many healthcare facilities and in recognition of the universal healthcare access objective of the health sustainable development goal. Additional searches for literature were conducted between September and November 2020 using keywords such as barriers and facilitators of nurse-patient interaction, patient-centered care, patient-centered communication , and nurse-patient communication . Databases searched included CINAHL, PubMed, Medline, and Google Scholar. Included studies in this critical review were empirical research on nurse-patient interactions in different care settings published in English and open access. All relevant articles were read, and their main findings relevant to our review questions were identified and organized into themes and subthemes discussed in this paper. Other published studies were read, and together with those that addressed the review question, a model was developed regarding how to enhance patient-centered care through effective communication.
Barriers to Patient-Centered Care and Communication
Nurses constitute a significant workforce of care providers whose practices can severely impact care outcomes (both positive and negative). Nurses spend much time with patients and their caregivers. As a result, positive nurse-patient and caregiver relationships are therapeutic and constitute a core component of care [ 9 , 13 ]. In many instances, nurses serve as translators or patients’ advocates, in addition to performing their primary care duties. Although good nurse-patient relationships positively impact nurse-patient communication and interaction, studies have shown that several factors impede these relationships with significant consequences on care outcomes and quality [ 6 , 16 , 17 ]. Thus, these barriers limit nurses’ and other care providers’ efforts to provide healthcare that meets patients’ and caregivers’ needs. We categorize the barriers to patient-centered care and communication into four kinds: institutional and healthcare system-related, communication-related, environment-related, and personal and behaviour-related barriers. Although these barriers are discussed in separate subheadings, they are interlinked in complex ways during clinical practice.
Institutional and Healthcare System Related Barriers
Many barriers to providing patient-centered care and communication during nurse-patient interactions emanate from healthcare institutional practices or the healthcare system itself. Some of these factors are implicated in healthcare policy or through management styles and strategies.
Shortage of nursing staff, high workload, burnout, and limited-time constituted one complex institutional and healthcare system-level barrier to effective care delivery [ 18 , 19 ]. For instance, Loghmani et al. [ 20 ] found that staffing shortages prevented nurses from having adequate time with patients and their caregivers in an Iranian intensive care unit. Limitations in nursing staff, coupled with a high workload, led to fewer interactions between nurses, patients, and caregivers. Similarly, Anoosheh et al. [ 16 ] found that heavy nursing workload was ranked highest as a limiting factor to therapeutic communication in nurse-patient interactions in Iran.
In a study on communication barriers in two hospitals affiliated with Alborz University of Medical Sciences, Norouzinia et al. [ 21 ] found that shortage of nurses, work overload, and insufficient time to interact with patients were significant barriers to effective nurse-patient interactions. Similar factors are identified as barriers to nurse-patient communication and interactions in other studies [ 13 , 16 , 18 ]. For instance, Amoah et al. [ 16 ] reported that nursing staff shortage and high workload were barriers to patient-centered care and therapeutic communication among Ghanaian nurses and patients. Amoah and colleagues reported a patient’s statement that:
[B]ecause there are few nurses at the ward, sometimes you would want a nurse to attend to you, but he or she might be working on another patient, so in such case, the nurse cannot divide him or herself into two to attend to you both [ 16 ].
Nurses and patients and their caregivers have noted that limited time affects nurse-patient interactions, communication, and care quality. Besides, Yoo et al. [ 22 ] reported that limited visiting hours affected communications between caregivers and nurses in a tertiary hospital in Seoul, Korea. Since the caregivers had limited time to spend with patients, they had little knowledge about the intensive care unit and distrusted the nurses.
Although nursing staff shortage is a significant barrier to patient-centered care and communication that healthcare institutions and managers must know, some healthcare scholars have critique nurses’ complaints of time limitation. For instance, McCabe [ 7 ] argued that the quality of nurse-patient interactions is what matters and not the quantity of time spent with patients and their caregivers. McCabe maintained that “spending long periods with patients does not always result in positive nurse-patient relationships” [ 7 ]. He argued that implementing patient-centered care does not require additional time; hence, nurses’ perceptions of being too busy cannot excuse poor therapeutic communication during clinical interactions. Instead, nurses are encouraged to develop self-awareness, self-reflection, and a commitment to ensuring that patients receive the needed care.
Another institution-related barrier to patient-centered care and communication is the healthcare system’s emphasis on task-centered care. Care providers are more focused on completing care procedures than satisfying patients’ and caregivers’ needs and preferences. This barrier to patient-centered care and communication is acknowledged in several studies [ 7 , 14 , 20 , 22 , 23 ]. For example, McLean [ 14 ] studied dementia care in nursing homes in the United States. She found that patient-centered care and communication in one nursing home (Snow I) were severely affected when nurses, physicians, and care managers focused on completing tasks or observing care and institutional routines to the detriment of satisfying patients’ care needs. However, in the other care home (Snow II), patient-centered care was enhanced as nurses, physicians, and the care home managers focused on addressing patients’ needs and values rather than completing care routines and tasks.
Similarly, Yoo and colleagues [ 22 ] observed that nurse-patient communication was affected when the ICU nurses placed urgency on completing tasks linked directly to patients’ health (e.g., stabilizing vital signs) than communicating to addressed patients’ specific needs. This evidence shows that when nurses are more task-focused, patients and caregivers are treated as bodies and objects, on which medical and care practices must be performed to restore health. Research has shown that when nurses focus on task-oriented care, it becomes hard to provide holistic care to patients or teach and communicate with patients even when nurses are less busy [ 20 ].
Nursing managers and their management styles can affect patient-centered care and communication. Studies have revealed that the management styles that nursing managers implement can either facilitate or impede patient-centered care [ 14 , 22 ]. When nurse managers orient their nursing staff towards task-centered care practices, it affects nurse-patient interaction and communication. Moreover, when nurse managers fail to address their staff’s mental health needs and personal challenges, it influences how nurses attend to patients’ care needs. For example, nurses have indicated that nurse-patient communication is affected when nurse managers are unsupportive or unresponsive to their needs [ 20 ].
In a study exploring nursing and midwifery managers’ perspectives on obstacles to compassion giving and therapeutic care across 17 countries, Papadopoulos et al. [ 24 ] discovered that nurses and midwifery managers’ characteristics and experiences could facilitate or impede compassion and therapeutic interactions in nursing care. Negative personal attitudes, including selfishness, arrogance, self-centeredness, rudeness, lack of leadership skills, the desire for power, and feelings of superiority among nurses and midwifery managers, were obstacles to compassion building. The study further showed that managers who emphasize rules, tasks, and results do not prioritize relationship-building and see their staff as workers rather than team members [ 24 ]. Therefore, nurse managers and care administrators must monitor nurse-patient interaction and communication to address nurses’ concerns and support them, especially in resource-constrained and high patient turnover contexts [ 25 , 26 ].
Communication-Related Barriers
Effective communication is essential to providing patient-centered care. Studies have shown that poor communication between care providers and patients and their caregivers affects care outcomes and perceptions of care quality [ 7 , 16 , 27 , 28 ]. A consistent communication-related barrier in nurse-patient interaction is miscommunication, which often leads to misunderstandings between nurses, patients, and their families [ 20 ]. Other communication-related barriers include language differences between patients and healthcare providers [ 6 , 16 , 27 ], poor communication skills, and patients’ inability to communicate due to their health state, especially in ICU, dementia, or end-of-life care contexts [ 13 , 22 ]. For instance, in their maternity care study, Madula et al. [ 6 ] noted that language barriers significantly affected effective communication between nurses/midwives and expectant mothers. A patient in their study indicated that although many nurses were polite and communicated well, some nurses had challenges communicating with patients in the Chitumbuka language, which affected those nurses’ ability to interact effectively with patients [ 6 ].
Furthermore, Norouzinia et al. [ 21 ] asserted that effective communication could not be established when nurses and patients have a language difference. Moreover, the meanings of certain non-verbal communication acts (e.g., head nodding, eye gaze, touch) can invoke different interpretations across different cultures, which could impede the interactions between patients and nurses. Even in healthcare contexts where nurses and patients speak the same language, “differences in vocabulary, rate of speaking, age, background, familiarity with medical technology, education, physical capability, and experience can create a huge cultural and communication chasm” between nurses and patients [ 12 ]. In ICU and other similar care settings, nurses find it difficult to effectively communicate with patients because the mechanical ventilators made it hard for patients to talk [ 22 ].
To overcome the communication-related barriers, healthcare institutions must make it a responsibility to engage translators and interpreters to facilitate nurse-patient interactions where a language barrier exists. Moreover, nurses working in ICU and other similar settings should learn and employ alternative forms of communication to interact with patients.
Environment-Related Barriers
The environment of the care setting can impact nurse-patient communication and the resulting care. Thus, “good health care experiences start with a welcoming environment” [ 29 ]. Mastors believed that even though good medicine and the hands working to provide care and healing to the sick and wounded are essential, we must not “forget the small things: a warm smile, an ice chip, a warm blanket, a cool washcloth. A pillow flipped to the other side and a boost in bed” [ 29 ]. The environment-related barriers are obstacles within the care setting that inhibit nurse-patient interaction and communication and may include a noisy surrounding, unkept wards, and beds, difficulties in locating places, and navigating care services. Noisy surroundings, lack of privacy, improper ventilation, heating, cooling, and lighting in specific healthcare units can affect nurse-patient communication. These can prevent patients from genuinely expressing their healthcare needs to nurses, which can subsequently affect patient disclosure or make nursing diagnoses less accurate [ 13 , 18 , 21 ]. For instance, Amoah et al. [ 16 ] revealed that an unconducive care environment, including noisy surroundings and poor ward conditions, affected patients’ psychological states, impeding nurse-patient relationships and communication. Moreover, when care services are not well-coordinated, new patients and their caregivers find it hard to navigate the care system (e.g., locating offices for medical tests and consultations), which can constrain patient-centered care and communication.
Reducing the environment-related barriers will require making the care setting tidy/clean, less noisy, and coordinating care services in ways that make it easy for patients and caregivers to access. Coordinating and integrating care services, making care services accessible, and promoting physical comfort are crucial in promoting patient-centered care, according to Picker’s Eight Principles of Patient-Centered Care [ 30 ].
Personal and Behaviour Related Barriers
The kind of nurse-patient relationships established between nurses and patients and their caregivers will affect how they communicate. Since nurses and patients may have different demographic characteristics, cultural and linguistic backgrounds, beliefs, and worldviews about health and illnesses, nurses’, patients’, and caregivers’ attitudes can affect nurse-patient communication and care outcomes. For instance, differences in nurses’ and patients’ cultural backgrounds and belief systems have been identified as barriers to therapeutic communication and care [ 12 , 13 , 21 ]. Research shows that patients’ beliefs and cultural backgrounds affected their communication with nurses in Ghana [ 16 ]. These scholars found that some patients refused a blood transfusion, and Muslim patients refused female nurses to attend to them because of their religious beliefs [ 16 ]. Further, when nurses, patients, or their caregivers have misconceptions about one another due to past experiences, dissatisfaction about the care provided, or patients’ relatives and caregivers unduly interfere in the care process, nurse-patient communication and patient-centered care were affected [ 16 , 21 ].
Similarly, nurse-patient communication was affected when patients or caregivers failed to observe nurses’ recommendations or abuse nurses due to misunderstanding [ 20 ], while patients’ bad attitudes or disrespectful behaviours towards nurses can inhibit nurses’ ability to provide person-centered care [ 31 ]. The above-reviewed studies provided evidence on how patients’ and caregivers’ behaviours can affect nurses’ ability to communicate and deliver patient-centered care.
On the other hand, nurses’ behaviours can also profoundly affect communication and care outcomes in the nurse-patient dyad. When nurses disrespect, verbally abuse (e.g., shouting at or scolding), and discriminate against patients based on their social status, it affects nurse-patient communication, care outcomes, and patient disclosure [ 6 , 32 ]. For instance, Al-Kalaldeh et al. [ 18 ] believe that nurse-patient communication is challenged when nurses become reluctant to hear patients’ feelings and expressions of anxiety. When nurses ignore patients’ rights to share ideas and participate in their care planning, such denials may induce stress, discomfort, lack of trust in nurses, thereby leading to less satisfaction of care [ 18 ].
Furthermore, when nurses fail to listen to patients’ and caregivers’ concerns, coerce patients to obey their rules and instructions [ 16 , 17 , 20 ], or fail to provide patients with the needed information, nurse-patient communication and patient-centered care practices suffer. To illustrate, in Ddumba-Nyanzia et al.‘s study on communication between HIV care providers and patients, a patient remarked that: “I realized no matter how much I talked to the counselor, she was not listening. She was only hearing her point of view and nothing else, [and] I was very upset” [ 17 ]. This quote indicates how care provider attitudes can constrain care outcomes. Due to high workload, limited time, poor remunerations, and shortage of personnel, some nurses can develop feelings of despair, emotional detachment, and apathy towards their job, which can lead to low self-esteem or poor self-image, with negative consequences on nurse-patient interactions [ 13 , 18 ].
Given the significance of effective communication on care, overcoming the above personal and behaviour related barriers to patient-centered care and communication is crucial. Nurses, patients, and caregivers need to reflect on the consequences of their behaviours on the care process. Thus, overcoming these barriers begins with embracing the facilitators of patient-centered care and communication, which we turn to in the next section.
Facilitators of patient-centered care and communication
Patient-centered care and communication can be facilitated in several ways, including building solid nurse-patient relationships.
First, an essential facilitator of patient-centered care and communication is overcoming practical communication barriers in the nurse-patient dyad. Given the importance of communication in healthcare delivery, nurses, patients, caregivers, nursing managers, and healthcare administrators need to ensure that effective therapeutic communication is realized in the care process and becomes part of the care itself. Studies have shown that active listening among care providers is essential to addressing many barriers to patient-centered care and communication [ 7 , 13 ]. Although handling medical tasks promptly in the care process is crucial, the power of active listening is critical, meaningful, and therapeutic [ 22 ]. By listening to patients’ concerns, nurses can identify patients’ care needs and preferences and address their fears and frustrations.
Another facilitator of patient-centered care is by understanding patients and their unique needs [ 25 ], showing empathy and attending attitudes [ 7 , 13 ], expressing warmth and respect [ 22 ], and treating patients and caregivers with dignity and compassion as humans. For instance, McCabe [ 7 ] noted that attending, which obligates nurses to demonstrate that they are accessible and ready to listen to patients, is a patient-centered care process; a fundamental requirement for nurses to show genuineness and empathy, despite the high workload. Showing empathy, active listening, respect, and treating patients with dignity are core to nursing and care, and recognized in the Code of Ethics for Nurses [ 33 ], and further emphasized in the ongoing revision of the Code of Ethics for nurses [ 34 ].
Besides, engaging patients and caregivers in the care process through sharing information, inviting their opinion, and collaborating with them constitutes another facilitator of patient-centered care and communication. When patients and caregivers are engaged in the care process, misunderstandings and misconceptions are minimized. When information is shared, patients and caregivers learn more about their health conditions and the care needed. As McLean [ 14 ] argued, ensuring open communication between care providers and patients and their families is essential to enhancing patient-centered care. Conflicts ensue when patients or their families are denied information or involvement in the care process. As a result, the Harvard Medical School [ 30 ] identified patient engagement, information sharing, and nurse-patient collaboration during care as essential patient-centered care principles.
Finally, health policy must be oriented towards healthcare practices and management to facilitate patient-centered care and communication. These policies, at a minimum, can involve changes in management styles within healthcare institutions, where nurse managers and healthcare administrators reflect on nursing and care practices to ensure that the Code of Ethics of Nurses and patients’ rights are fully implemented. Resource constraints, staff shortages, and ethical dilemmas mainly affect care practices and decision-making. Nonetheless, if patients are placed at the center of care and treated with dignity and respect, most of the challenges and barriers of patient-centered care will diminish. Empowering practicing nurses, equipping them with interpersonal communication skills through regular in-service training, supporting them to overcome their emotional challenges, and setting boundaries during nurse-patient interactions will enhance patient-centered care practices.
In line with the above discussion, Camara et al. [ 25 ] identify three core dimensions that nurses, patients, and caregivers must observe to enhance patient-centered care: treating the patient as a person and seeing the care provider as a person and a confidant. Regarding the first dimension, care providers must welcome patients, listen to them, share information with them, seek their consent, and show them respect when providing care. The second dimension requires that the healthcare provider be seen and respected as a person, and negative perceptions about care providers must be demystified. According to Camara et al. [ 25 ], care providers must not overemphasize their identities as experts but rather establish good relationships with patients to understand patients’ personal needs and problems. Lastly, patients and caregivers must regard care providers as confidants who build and maintain patients’ trust and encourage patients’ participation in care conversations. With this dimension, patients and caregivers must know that nurses and other care providers have the patient at heart and work to meet their care needs and recovery process.
Camara et al.‘s [ 25 ] three dimensions are essential and position patients, their caregivers, and nurses as partners who must engage in dialogic communication to promote patient-centered care. As a result, effective communication, education, and increased health literacy among patients and caregivers will be crucial in that direction.
Enhancing Patient-Centered Care and Communication: A Proposed Model
Nursing care practices that promote patient-centered communication will directly enhance patient-centered care, as patients and their caregivers will actively engage in the care process. To enhance patient-centered communication, we propose person-centered care and communication continuum (PC4) as a guiding model to understand patient-centered communication, its pathways, and what communication and care practices healthcare professionals must implement to achieve person-centered care. In this PC4 Model, we emphasize the person instead of the patient because they are a person before becoming a patient. Moreover, the PC4 Model is supposed to apply to all persons associated with patient care; thus, respect for the dignity of their personhood is crucial.
Although much is written about patient-centered communication in the healthcare literature, there is a gap regarding its trajectory and what communication content enhances patient-centered communication. Also, little is known about how different clinical discourse spaces influence communication and its content during nurse-patient clinical interactions. Using evidence from Johnsson et al. [ 3 ], Murira et al. [ 23 ], and Liu et al. [ 35 ], among other studies, we outline the components of the PC4 Model and how different discourse spaces in the clinical setting and the content of communication impact patient-centered care and communication.
The proposed PC4 Model in this paper has three unbounded components based on the purpose of and how communication is performed among care providers, patients, and their caregivers. Figure 1 illustrates the PC4 Model, its features, and trajectory.
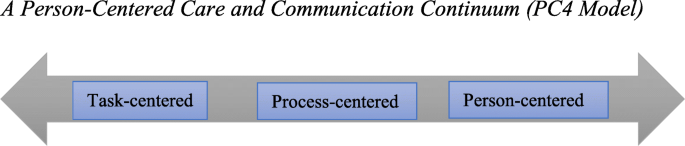
A Person-Centered Care and Communication Continuum (PC4 Model)
Task-Centered Communication
At the lowest end of the PC4 Model is task-centered communication. Here, the care provider’s role is to complete medical tasks as fast as possible with little or no communication with the patient and their caregivers. Patients and caregivers are treated as bodies or objects whose disease symptoms need to be studied, identified, recorded, treated, or cured. As Johnsson et al. [ 3 ] observed, communication content at this stage is mainly biomedically oriented, where nurses and other healthcare professionals focus on the precise medical information (e.g., history taking, medical examination, test results, medication, etc.) about the patient. With a task-centered orientation, nurses make journal entries about their patients’ disease state and ensure that treatment plans, diagnostic tests, and medical prescriptions are completed. Communication at this stage is often impersonal or rigid (see [ 23 ] for details). Care providers may address patients and their caregivers by using informal attributes (e.g., bed 12, the woman in the red shirt, card 8, etc.), thereby ignoring patients’ and caregivers’ personal and unique identities. Patients’ and caregivers’ nonverbal communication signs are mostly overlooked.
Motivations for task-centered communication can be attributed to time limitation, high workload, and staff shortage, thereby pushing nurses and other care providers to reach as many patients as possible. Moreover, the healthcare system’s orientation towards and preference for biomedically-focused care seems to favour task-centered communication [ 7 , 14 ].
Depending on the clinical discourse space under which patient-provider interactions occur, different forms of communication are employed. Clinical discourse spaces can be public (e.g., in the ward, patient bedside), private (e.g., consulting rooms, medical test labs, nurse staff station, etc.), or semi-private (e.g., along the corridor) [ 35 ]. In these clinical discourse spaces, nurse-patient communication can be uninformed (patients or caregivers are not informed about patients’ care conditions or why specific data and routines are performed). It can be non-private (others can hear what the nurse and patient are talking about) or authoritative (care providers demonstrate power and control and position themselves as experts) [ 23 ]. Finally, in task-centered communication, healthcare providers often use medical jargon or terminologies [ 3 ] since the goal of communication is not to engage the patient in the process. Usually, patients or their caregivers are not allowed to ask questions, or their questions get ignored or receive superficial, incomprehensible responses.
Process-Centered Communication
Process-centered communication is an intermediate stage on the continuum, which could slip back into the task-centered or leap forward into person-centered communication. Through process-centered communication, care providers make an effort to know patients and their caregivers as they perform care routines. Care providers ask patients or their caregivers questions to understand the care conditions but may not encourage patients or caregivers to express their thoughts about their care needs. Patients and caregivers are recognized as persons with uniques care needs but may not have the agency to influence the care process. Care providers may chit-chat with patients or their caregivers to pass the time as they record patients’ medical records or provide care. Unlike task-centered communication, there is informative and less authoritative communication between nurses and patients and their caregivers. The goal of process-centered communication could be a mixture of instrumental and relational, with less display of power and control by nurses.
Person-Centered Communication
This is the highest point of the PC4 Model, where patient-centered care is actualized. At this stage of the communication continuum, patients and caregivers are treated as unique persons with specific care needs and are seen as collaborators in the care process. As McLean [ 14 ] observed, caregiving becomes a transactional relationship between the care provider and receiver at the person-centered stage of the continuum. The care itself becomes intersubjective, a mutual relational practice, and an ongoing negotiation for care providers and receivers [ 14 ].
The content of communication at this stage of the continuum is both “personal” and “explanatory” [ 3 ]. Nurses and other healthcare providers create meaningful relationships with patients and their caregivers, understand patients’ concerns, needs, and problems, use open-ended questions to encourage patients or caregivers to express their thoughts and feelings about the care situation. Nurses and other healthcare professionals explain care routines, patients’ health conditions, and management plans in lay language to patients and caregivers through person-centered communication. Accomplishing this level includes employing alternative forms of communication to meet the needs of intensive care unit patients, deaf patients, and ventilated and intubated patients. For instance, it has been shown that “deaf people […] frequently do not have access to clear and efficient communication in the healthcare system, which deprives them of critical health information and qualified health care” [ 36 ]. Empathetic communication practices, including active listening, showing genuine interest in patients’ care, and respect and warmth, become a significant part of nursing care [ 3 , 7 , 14 , 22 ].
Different communication strategies are employed based on the care situation and context. Chit-chatting, as a form of personal communication [ 3 ], use of humor as a communication strategy [ 7 , 8 ], and even maintaining silence [ 28 ] are essential in enhancing person-centered care and communication. Both care providers and patients or their caregivers use relationship-building and -protecting humor (see [ 28 ] for details) to address difficult situations in the care process.
Implications of the PC4 Model for Nursing Practice
Given the values of effective communication in nurse-patient interactions and care outcomes, nurses and other healthcare providers must ensure that they develop therapeutic relationships with patients, their families, and caregivers to promote person-centered care and communication. Achieving that begins with knowing and reflecting on the barriers of therapeutic communication and ways to minimize them. The PC4 Model draws nurses and all healthcare providers’ attention to patient-centered care pathways and how effective communication is necessary. Healthcare professionals, including nurses, must be aware of how their communication orientation–––either oriented toward completing tasks, following care processes or toward addressing patients’ and their caregivers’ needs––can impact patient-centered care. Healthcare providers must observe the care context, patients’ unique situations, their non-verbal language and action, and whether they belong to historically marginalized groups or cultures.
Mastors [ 29 ] has offered healthcare providers some guidance to reflect on as they communicate and interact with patients and caregivers. Thus, (a) instead of asking patients, “What’s the matter?“ care providers must consider asking them, “What’s important to you?“ With this question, the patient is given a voice and empowered to contribute to their own care needs. Care providers should (b) check with patients in the waiting room to update patients whose waiting time has been longer than usual, based on the care context. They should also (c) try to remember their conversations with patients to build on them during subsequent interactions. This continuity can be enhanced by nurse managers reexamining how they deploy care providers to patients. The same nurse can be assigned to the same patients for the duration of the patient’s stay to help patients feel valued and visible [ 29 ].
Knowledge of cultural competence, sensitivity, humility, and interpersonal communication skills will help achieve and implement the PC4 Model. As Cuellar [ 37 ] argues, “[h]umility is about understanding and caring for all people [and] being empathetic.“ Cultural competence is a “dynamic process of acquiring the ability to provide effective, safe, and quality care to the patients through considering their different cultural aspects” [ 38 ]. The concept of cultural competence entails “cultural openness, awareness, desire, knowledge and sensitivity” during care [ 39 ]. It demands that care providers respect and tailor care to align with patients’ and caregivers’ values, needs, practices, and expectations, based on care and moral ethics and understanding [ 39 ]. Active listening and showing compassion as therapeutic relationship-building skills are essential, and continuous education and mentorship will be crucial to developing these skills among healthcare providers.
We invite qualitative and quantitative studies, especially on language use and communication strategies, to explore and evaluate the PC4 Model. Providing in-depth and experiential data on ways to increase its effectiveness as a tool to guide healthcare providers is highly desired. More knowledge can support healthcare providers in offering evidence-based patient-centered care in different healthcare settings and units.
Conclusions
Effective communication is an essential factor in nurse-patient interactions and a core component of nursing care. When communication in the nurse-patient dyad is patient-centered, it becomes therapeutic. It allows for trust and mutual respect in the care process, thereby promoting care practices that address patients’ and caregivers’ needs, concerns, and preferences. We have identified the barriers and facilitators of patient-centered care and communication and proposed a person-centered care and communication continuum (PC4 Model) to demonstrate how patient-centered communication intersects with patient-centered care.
Availability of data and materials
Not applicable.
Abbreviations
Intensive Care Unit
Institution of Medicine
Person-Centered Care and Communication Continuum
Etheredge HR. “Hey sister! Where’s my kidney?“ Exploring ethics and communication in organ transplantation in Gauteng, South Africa, Ph.D. dissertation, Johannesburg. University of the Witwatersrand; 2015.
Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. National Academy Press; 2001.
Johnsson A, Wagman P, Boman A, Pennbrant S. What are they talking about? Content of the communication exchanges between nurses, patients and relatives in a department of medicine for older people: An ethnographic study. J Clin Nurs. 2018 Apr;27(7–9):e1651-9. doi: https://doi.org/10.1111/jocn.14315 .
Long KA. The Institute of Medicine report on health professions education: A bridge to quality. Policy Polit Nurs Pract. 2003 Nov;4(4):259–62. doi: https://doi.org/10.1177/1527154403258304 .
Crawford T, Candlin S, Roger P. (2017). New perspectives on understanding cultural diversity in nurse-patient communication. Collegian, 2017 Feb 1;24(1):63 – 9. https://doi.org/10.1016/j.colegn.2015.09.001 .
Madula P, Kalembo WF, Yu H, Kaminga CA. Healthcare provider-patient communication: A qualitative study of women’s perceptions during childbirth. Reprod Health. 2018 Dec;15(135):1–10. https://doi.org/10.1186/s12978-018-0580-x .
McCabe C. Nurse-patient communication: An exploration of patients’ experiences. J Clin Nurs. 2004 Jan;13(1):41–9.
Schöpf AC, Martin GS, Keating MA. Humor as a communication strategy in provider-patient communication in a chronic care setting. Qual Health Res. 2017 Feb;27(3):374–90. doi: https://doi.org/10.1177/1049732315620773 .
Joolaee S, Joolaei A, Tschudin V, Bahrani N, Nikbakht NA. Caring relationship: the core component of patients’ rights practice as experienced by patients and their companions. J Med Ethics Hist Med. 2010;3(4):1–7.
Google Scholar
Boykins AD. Core communication competences in patient-centered care. The ABNF J. 2014 Apr 1;25(2):40 – 5.
Henly SJ. Health communication research for nursing science and practice. Nurs Res [Editorial] 2016:257–8. doi: https://doi.org/10.1097/NNR.0000000000000171 .
Ruben BD. Communication theory and health communication practice: The more things change, the more they stay the same. Health Commun. 2016 Jan 2;31(1):1–11. doi: https://doi.org/10.1080/10410236.2014.923086 .
Bello P. Effective communication in nursing practice: A literature review. BSc Nursing Thesis. Arcada; 2017. Available at https://core.ac.uk/download/pdf/84798372.pdf Accessed 20 Jan 2021.
McLean A. The person in dementia: A study of nursing home care in the US. Toronto, University of Toronto Press; 2007.
Grant MJ, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info Libraries J. 2009;26:91–108. Doi: https://doi.org/10.1111/j.1471-1842.2009.00848.x .
Article Google Scholar
Amoah KMV, Anokye R, Boakye SD, Acheampong E, Budu-Ainooson A, Okyere E, Kumi-Boateng G, Yeboah C, Afriyie OJ. A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nurs. 2019 Dec;18(4)1–8. https://doi.org/10.1186/s12912-019-0328-0 .
Ddumba-Nyanzia I, Kaawa-Mafigiria D, Johannessen H. Barriers to communication between HIV care providers (HCPs) and women living with HIV about childbearing: A qualitative study. Patient Educ Couns. 2016 May 1:99(5):754–9. https://doi.org/10.1016/j.pec.2015.11.023 .
Al-Kalaldeh M, Amro N, Qtait M. Barriers to effective nurse-patient communication in the emergency department. Emerg Nurse. 2021 Mar 2;29(2). doi: https://doi.org/10.7748/en.2020.e1969 .
Sethi D, Rani MK. Communication barrier in health care setting as perceived by nurses and patient. Int J Nurs Educ 2017 Oct. 2016;9(4):30. doi: https://doi.org/10.5958/j.2320-8651.2.1.001 .
Loghmani L, Borhani F, Abbaszadeh A. Factors affecting the nurse-patients’ family communication in intensive care unit of Kerman: A qualitative study. J Caring Sci. 2014 Mar;3(1):67–2. doi: https://doi.org/10.5681/jcs.2014.008 .
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci. 2016 Jun;8(6):65–4. https://doi.org/10.5539/gjhs.v8n6p65 .
Yoo HJ, Lim OB, Shim JL. Critical care nurses’ communication experiences with patients and families in an intensive care unit: A qualitative study. PLoS One. 2020 Jul 9;15(7):e0235694. https://doi.org/10.1371/journal.pone.0235694 .
Murira N, Lützen K, Lindmark G, Christensson K. Communication patterns between healthcare providers and their clients at an antenatal clinic in Zimbabwe. Health Care Women Int. 2003 Feb 1;24(2):83 – 2. https://doi.org/10.1080/07399330390170060 .
Papadopoulos I, Lazzarino R, Koulouglioti C, Aagard M, Akman O, Alpers L-M, Apostolara P, Araneda Bernal J, Biglete-Pangilinan S, Eldar-Regev O, Gonzalez-Gil MT, Kouta C, Zorba A. Obstacles to compassion-giving among nursing and midwifery managers: An international study. Int Nurs Rev. 2020 Aug;11:1–13.
Camara BS, Belaid L, Manet H, Kolie D, Guilard E, Bigirimana T, Delamou A. What do we know about patient-provider interactions in sub-Saharan Africa? A scoping review. Pan Afr Med J. 2020;88(88):1–13. doi: https://doi.org/10.11604/pamj.2020.37.88.24009 .
Kwame A, Petrucka PM. Communication in nurse-patient interaction in healthcare settings in sub-Saharan Africa: A scoping review. Int J Afr Nurs Sci. 2020 Jan 1;12:100198. https://doi.org/10.1016/j.ijans.2020.100198 .
Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. Int Nurs Rev. 2009 Jun;56(2):243–9.
Vuković M, Gvozdenović BS, Stamatović-Gajić B, Ilić M, Gajić T. Development and evaluation of the nurse quality of communication with patient questionnaire. Srp Arh Celok Lek. 2010;138(1–2):79–4. doi: https://doi.org/10.2298/SARH1002079V .
Article PubMed Google Scholar
Mastors P. (2018). What do patients want, need, and have the right to expect? Nurs Adm Q. 2018 Jul 1;42(3):192-8. doi: https://doi.org/10.1097/NAQ.0000000000000297 .
Harvard Medical School. The Eight Principles of Patient Centered Care; 2015 Nov 18. Available from OneView: https://www.oneviewhealthcare.com/the-eight-principles-of-patient-centered-care/ Accessed 28 Dec 2020.
White J, Phakoe M, Rispel LC. ‘Practice what you preach’: Nurses’ perspectives on the Code of Ethics and Service Pledge in five South African hospitals. Glob Health Action. 2015 Dec 1;8(1):26341. https://doi.org/10.3402/gha.v8.26341 .
Kruger L-M, Schoombee C. The other side of caring: abuse in a South African maternity ward. J Reprod Infant Psychol. 2010 Feb 1;28(1):84–101. doi: https://doi.org/10.1080/02646830903294979 .
International Council of Nurses. ICN Code of Ethics for Nurses; 2012. Available from www.icn.ch/images/stories/documents/about/icncode_english.pdf . Accessed 20 Dec 2020.
Stievano A, Tschudin V. The ICN code of ethics for nurses: A time for revision. Nurs Health Policy Perspect. 2019 Jun;66(2):154–6.
Liu W, Manias E, Gerdtz M. Medication communication during ward rounds on medical wards: Power relations and spatial practices. Health 2012 Mar. 2012;17(2):113–34. doi: https://doi.org/10.1177/1363459312447257 .
Hoglind TA. Healthcare language barriers affect deaf people, too. 2018 Oct 11. Retrieved from Boston University [BU] School of Public Health: Available from https://www.bu.edu/sph/news/articles/2018/healthcare-language-barriers-affect-deaf-people-too/ Accessed 15 Jan 2021.
Cuellar NG. Humility. A concept in cultural sensitivity. JTranscult Nurs [Editorial]. 2018 Apr 26; 29(4):317. https://doi.org/10.1177/1043659618772384 .
Sharifi N, Adib-Hajbaghery M, Najafi M. Cultural competence in nursing: A concept analysis. Int J Nurs Stud. 2019 Nov 1;99(103386):1–8. https://doi.org/10.1016/j.ijnurstu.2019.103386 .
Henderson S, Horne M, Hills R, Kendall E. Cultural competence in healthcare in the community: A concept analysis. Health Soc Care Community. 2018 Jul;26(4):590–603. doi: https://doi.org/10.1111/hsc.12556 .
Download references
Acknowledgments
We express our gratitude to the first author’s doctoral committee members for their valuable comments, suggestions, and critique of an earlier version of this paper. We are also grateful to the anonymous reviewers for the insightful comments and suggestions that have helped us improve the study’s quality.
Authors' information
Abukari Kwame is a Ph.D. candidate in Interdisciplinary Studies in the College of Graduate and Postdoctoral Studies, University of Saskatchewan, interested in patients' rights in nurse-patient clinical communications and interactions in the hospital setting. He holds two Master of Philosophy degrees in Indigenous Studies and English Linguistics. Abukari's research interests include language use in social interaction, health communication, First/Second language acquisition, African traditional medical knowledge, and Indigenous and qualitative research methodologies.
Pammla M. Petrucka is a professor in Nursing and has international research experience with many of her graduate students from Africa, Asia, and the Caribbean. Pammla has published extensively in the field of nursing. Her research interests are vast, including child and maternal health, Indigenous peoples' health, global health, and vulnerable populations, with extensive experiences in qualitative research and indigenous research methodologies. Pammla is co-editor of the BMC Nursing journal and a reviewer for many other academic journals.
The authors have not received any funding for the conduct, preparation, and publication of this paper.
Author information
Authors and affiliations.
College of Graduate and Postdoctoral Studies, University of Saskatchewan, Saskatoon, Canada
Abukari Kwame
College of Nursing, University of Saskatchewan, Regina Campus, Regina, Canada
Pammla M. Petrucka
You can also search for this author in PubMed Google Scholar
Contributions
Both authors conceived the topic. PMP recommended the literature, AK searched and added more sources, and drafted the paper. PMP reviewed the paper for intellectual content. Both AK and PMP read and approved the final version.
Corresponding author
Correspondence to Abukari Kwame .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kwame, A., Petrucka, P.M. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs 20 , 158 (2021). https://doi.org/10.1186/s12912-021-00684-2
Download citation
Received : 05 May 2021
Accepted : 18 August 2021
Published : 03 September 2021
DOI : https://doi.org/10.1186/s12912-021-00684-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient-centered care
- Therapeutic communication
- Nurse-patient interactions
- Clinical discourse space
- Patient-centered care and communication continuum
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Health Care Access & Coverage
Top 5 Reasons Why U.S. Nurses Are Leaving Their Jobs
Study suggests hospitals could improve working conditions to retain nursing staff, julia hinckley, jd.
- Share this page on Twitter
- Share this page on Facebook
- Share this page on LinkedIn

The seismic departures in the nursing workforce threaten to impair access and quality of care across the country. And these trends concerned health care leaders and policymakers even before the major disruptions of the COVID-19 pandemic.
Today, hospitals continue struggling to fill openings even though the U.S. has never had more actively-licensed nurses (5.6 million), driven by record-breaking graduations from schools and a robust job forecast.
To understand what is driving the exodus, Penn LDI researchers surveyed more than 7,800 nurses who left employment between 2018 and 2021, and published their findings in a recent study in JAMA Network Open .
Here are the top five reasons why nurses left their jobs:
- Planned retirement . Of those surveyed, 30% left employment for a retirement they had planned.
- Burnout. About 1 in 4 respondents reported that they left because of burnout.
- Insufficient staffing. Related to experiencing burnout, 21% of those surveyed identified a lack of sufficient staffing as the cause of their departure.
- Poor work-life balance. The inability to balance restrictive and often unpredictable work schedules with family life led about 18% of respondents to depart from their jobs.
- Concerns related to COVID-19. Of those surveyed, 17% said concerns about COVID-19, including concern about family member exposure, led to their departure.
The researchers point out that all of these reasons (aside from planned retirement) are factors within the control of the institutions. They argue that substantive improvements to work conditions could ease the nursing retention crisis.
The study, “ Top Factors in Nurses Ending Health Care Employment Between 2018 and 2021 ,” was published on April 9, 2024 in JAMA Network Open . Authors include K. Jane Muir , Joshua Porat-Dahlerbruch, Jacqueline Nikpour , Kathryn Leep-Lazar, and Karen B. Lasater .

Director of Policy Strategy
More on health care access & coverage, fda needs to reboot rules for less harmful tobacco alternatives after biden’s delay of the menthol ban.
Modified Risk Tobacco Products Need a Faster Approval System to Help More Smokers Quit
- Andy Tan, PhD, MPH
In Their Own Words
What Nurses Really Need is Better Staffing
The Common Strategies to Raise Nurse Morale Need an Update
- Karen Lasater, PhD, RN
- Jane Muir, PhD, APRN
Bipartisan Support Grows To Solve One of Health Care’s Biggest Problems
Dually Eligible Americans on Medicare and Medicaid Are Getting the Attention They Deserve
- Rachel M. Werner, MD, PhD

Future Bundled Payment Models Need To Engage Physician Group Practices
Looking Forward, LDI Fellows Offer Their Perspectives and Expertise
- Austin Kilaru, MD, MSHP
- Aidan P. Crowley
- Amol S. Navathe, MD, PhD
- and Qian (Erin) Huang, MPH

How Can We Improve Telemedicine for Patients with Gynecologic Cancer?
Fewer Than 30% of Patients Used Telehealth Even During the Pandemic
- Chris Tachibana, PhD, MS

Eileen Lake and Salimah Meghani Named to International Nurse Researcher Hall of Fame
Cited for Their Work’s Significant Impact on Nursing and Patient Care
- Hoag Levins
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Guidelines and Guidance Library
- Core Practices
- Isolation Precautions Guideline
- Disinfection and Sterilization Guideline
- Environmental Infection Control Guidelines
- Hand Hygiene Guidelines
- Multidrug-resistant Organisms (MDRO) Management Guidelines
- Catheter-Associated Urinary Tract Infections (CAUTI) Prevention Guideline
- Tools and resources
- Evaluating Environmental Cleaning
What to know
This guideline provides recommendations for isolation precautions in healthcare settings.
Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007)
Print Version of Guidelines
Updates, infection control.
CDC provides information on infection control and clinical safety to help reduce the risk of infections among healthcare workers, patients, and visitors.
For Everyone
Health care providers, public health.

IMAGES
VIDEO
COMMENTS
Care providers are more focused on completing care procedures than satisfying patients' and caregivers' needs and preferences. This barrier to patient-centered care and communication is acknowledged in several studies [7, 14, 20, 22, 23]. For example, McLean studied dementia care in nursing homes in the United States. She found that patient ...
Journal of Research in Nursing. Journal of Research in Nursing publishes quality research papers on healthcare issues that inform nurses and other healthcare professionals globally through linking policy, research and development initiatives to clinical and academic excellence. View full journal description.
Exploring all aspects of nursing research, training, education, and practice, BMC Nursing is a well-established open access peer-reviewed journal. ... commitment, job stress, and nursing work environment on patient safety management activities in comprehensive nursing care service units during the covid-19 pandemic. ... 1.428 - SNIP (Source ...
SUBMIT PAPER. Global Qualitative Nursing Research. Impact Factor: 1.7 / 5-Year Impact Factor: 4.6 . JOURNAL HOMEPAGE. SUBMIT PAPER. Close ... (2017). Employing a qualitative description approach in health care research. Global Qualitative Nursing Research, 4, 2333393617742282. Crossref. PubMed. Google Scholar.
Parse categorized nursing theories into totality and simultaneity paradigms, with the former viewing the person as a combination of biological, psychological, social and spiritual features, in constant interaction with the environment to accomplish goals and maintain balance: The goals of nursing in the totality paradigm focus on health promotion, care and cure of the sick, and prevention of ...
The Future of Nursing is an ambitious and motivational report that includes 11 chapters focused on a variety of topics, including social determinants of health; health equity; the role of the nurse in improving health care access, quality, and health equity; and educating nurses for the future. A key theme is preparing current and future nurses at all levels to understand and address health ...
This paper described how nurses crafted and shaped new roles with an experimental process. It revealed the implications of developing a distinct VN role and the possibility to enhance the BN role in coordination tasks and in steering and supporting EBP quality improvement work. ... A framework for nursing, midwifery and care staff. 2016. https ...
2. De-implementing inappropriate or harmful healthcare interventions. International research on this topic connects the concepts of de-implementation, low-value care, and de-adoption, often characterised as unproven, inappropriate, or harmful (Dunsmore et al., Citation 2023; Norton & Chambers, Citation 2020).This is significant to nursing, considering the use of devices, implementation of ...
Nursing Research has a long and distinguished record in the history of nursing science. Since its launch in 1952, Nursing Research has been a "cooperative venture" of scientists, professional organizations, publisher, editorial staff, and readers to circulate scientific papers in nursing to improve care, alleviate suffering, and advance well-being.
The shortage of the nursing workforce is a chronic issue that needs to be addressed effectively. Prompted by the findings on the nursing shortage, it impacted the health service delivery throughout the population (Ministry of Health (MOH), 2018). Although strategies have been implemented in the past to address the issues, the shortage of ...
Between January 2022 (Volume 31, Issue 1) and the current May 2023 journal issue (Volume 32, Issue 3), AJCC published 71 reports of original research. These recent papers addressed a wide range of research topics, including bedside patient care, palliative and end-of-life care, intensive care unit (ICU) survivorship, measurement and prediction of patient problems, family concerns ...
Nursing Research is a peer-reviewed journal celebrating over 60 years as the most sought-after nursing resource; it offers more depth, more detail, and more of what today's nurses demand. Nursing Research covers key issues, including health promotion, human responses to illness, acute care nursing research, symptom management, cost-effectiveness, vulnerable populations, health services, and ...
The purpose of this paper is to provide a clear definition of nursing care quality that contributes to the formulation, application, and measurement of quality nursing outcomes for patients ...
This concept paper aims to describe the burnout concept and reflect. on the impact on nurses. Our intention with this reflection, considering the burnout impact on nurses, is to support a ...
Nursing competence refers to a set of knowledge, skills, and behaviors that are necessary to successfully perform roles or responsibilities [].It is crucial for ensuring the safe and high-quality care of patients [2,3,4,5].However, evaluating nursing competence is challenging due to the complex, dynamic, and multi factorial nature of the clinical environment [].
Commentary on: Chee, JMP, Rusli KDB, Tan ZYA, Tan AJQ, Ang SGM, Lau ST, Seah B, Liaw SY. Perceptions of community care among nursing students: A cross-sectional study with implications to the nursing workforce. Nurse Education Today . 2024; 137:106162. 10.1016/j.nedt.2024.106162 ### Implications for education and research The increasing demand for postacute and home-based care programmes ...
A 2007 study by Woodward and colleagues in the Journal of Research in Nursing found that nurse clinicians engaged in research often perceive a lack of support from nurse managers and resentment from colleagues who see the research as taking them away from clinical practice. The distinction often drawn between nursing research and clinical ...
Attempts to shape nursing work have lacked understanding of how nurses contribute to healthcare, with negative consequences. For example, the recent introduction of Nursing Associate roles (Department of Health and Social Care, 2017) in the UK, ostensibly to be a compassionate, patient-facing role and reduce costs, overlooks evidence that replacing registered nurses with other providers leads ...
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on CRITICAL CARE NURSING. Find methods information, sources, references or conduct a literature review ...
Despite the surge in popularity of virtual health care services as a means of delivering health care through technology, the integration of research evidence into practice remains a challenge. Rapid reviews, a type of time-efficient evidence synthesis, offer a potential solution to bridge the gap between knowledge and action. This paper aims to highlight the experiences of the Fraser Health ...
1. Clinical Nursing Research Topics. Analyze the use of telehealth/virtual nursing to reduce inpatient nurse duties. Discuss the impact of evidence-based respiratory interventions on patient outcomes in critical care settings. Explore the effectiveness of pain management protocols in pediatric patients. 2.
The purpose of the nursing paper is to give the student experience in solving nursing problems using evidence-based practice (EBP). The paper is the written proof that the student understands the EBP process. The student must apply skills in the following areas: Identifying a nursing problem. Selecting appropriate resources.
Nurses and patients and their caregivers have noted that limited time affects nurse-patient interactions, communication, and care quality. Besides, Yoo et al. [] reported that limited visiting hours affected communications between caregivers and nurses in a tertiary hospital in Seoul, Korea.Since the caregivers had limited time to spend with patients, they had little knowledge about the ...
The seismic departures in the nursing workforce threaten to impair access and quality of care across the country. And these trends concerned health care leaders and policymakers even before the major disruptions of the COVID-19 pandemic. Today, hospitals continue struggling to fill openings even though the U.S. has never had more actively-licensed nurses (5.6 million), driven by record ...
Appendix A: Type and Duration of Precautions Recommended for Selected Infections and Conditions. Appendix A: Table 1. History of Guidelines for Isolation Precautions in Hospitals. Appendix A: Table 2. Clinical Syndromes or Conditions Warranting Empiric Transmission-Based Precautions in Addition to Standard Precautions. Appendix A. Table 3.
CAR T-cell immunotherapy changes these collected T cells to produce chimeric antigen receptors (or CARs) that adhere to tumors to destroy them. A recent study published in the New England Journal of Medicine, suggests CAR T-cell therapy could become a highly effective treatment for SLE patients who do not respond to current lupus therapeutics ...