Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals

Chronic obstructive pulmonary disease articles from across Nature Portfolio
Chronic obstructive pulmonary disease (COPD) is a disease of the respiratory tract that is characterized narrowing of the small airways and destruction of lung tissue. This leads to poor airflow, shortness of breath, cough and frequent exacerbations, which are often due to infections. Smoking is the most common aetiologic factor.
Latest Research and Reviews
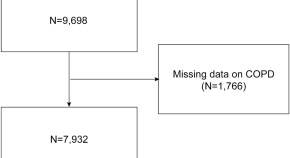
Association of hepatic steatosis and liver fibrosis with chronic obstructive pulmonary disease among adults
- Dayang Zheng
- Chunxiang Zhou
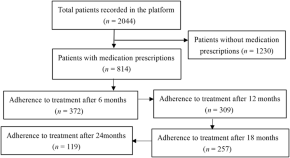
Pharmaceutical treatment status of patients with COPD in the community based on medical Internet of Things: a real-world study
- Yi-qun Jiang
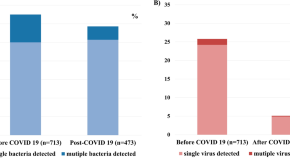
Respiratory pathogen and clinical features of hospitalized patients in acute exacerbation of chronic obstructive pulmonary disease after COVID 19 pandemic
- Soo Jung Kim
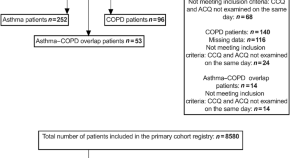
Measuring burden of disease in both asthma and COPD by merging the ACQ and CCQ: less is more?
- Liz J. A. Cuperus
- Cathelijne M. van Zelst
- Johannes C. C. M. in ’t Veen
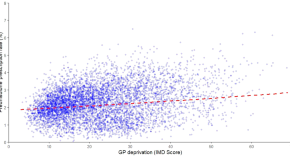
The relationship between prescription rates of oral corticosteroids for respiratory diseases and deprivation in England
- Erin Barker
- Jessica Pocock
- Richard Hudson
Risk of chronic obstructive pulmonary disease in a large cohort of Ontario, Canada workers
- Jeavana Sritharan
- Victoria H. Arrandale
- Paul A. Demers
News and Comment
Gold 2023: Highlights for primary care
- Alvar Agustí
- Antoni Sisó-Almirall
- Jadwiga A. Wedzicha
Have guidelines been oblivious to the obvious? Unmasking the positives from the COVID-19 pandemic
- K. Vishak Acharya
- B. Unnikrishnan
GPs should not try to detect mild COPD
- Paul Enright
- Carlos Vaz Fragoso
Let’s stop dumping cookstoves in local communities. It’s time to get implementation right
- Evelyn A Brakema
- Rianne Mjj van der Kleij
- Sian Williams
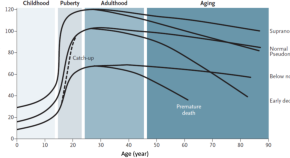
COPD’s early origins in low-and-middle income countries: what are the implications of a false start?
- E. A. Brakema
- F. A. van Gemert
Hollywood raising awareness of smoking-related diseases: can it proactively counteract the impact of smoking in movies?—the final mission of Star Trek’s Mr Spock
- Job FM van Boven
- Alan G Kaplan
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Study provides new insights into deadly acute respiratory distress syndrome (ARDS)
Mechanical explanation for instability in the lungs could lead to new treatments for illnesses such as covid-19.
Researchers at the University of Minnesota Twin Cities may have discovered a mechanical explanation for instability observed in the lungs in cases of acute respiratory distress syndrome (ARDS), particularly in the aftermath of respiratory illnesses such as COVID-19 or pneumonia.
The research was recently published in the Proceedings of the National Academy of Sciences (PNAS), a peer reviewed journal of the National Academy of Sciences.
Currently, there is no known cure for ARDS, a life-threatening lung injury that allows fluid to leak into the lungs. The researchers in this study say that as many as two thirds of all patients that passed away from COVID-19 had ARDS. There is not a clear reason on why specific people with a severe respiratory illness may develop ARDS, while others may not, but researchers in this study were looking to find that answer.
They identified the concentration of a lysolipid -- a byproduct of the immune response to viruses and bacteria -- that can have a major impact in adults suffering from ARDS. Increased concentration of this chemical eliminates the surfactant, a complex composed of fats and proteins generated in the lungs. The result is uneven lung inflation and, ultimately, respiratory distress in adults.
"This study looked into the correlation of the concentration of the lysolipid in the lungs. Once that fluid reached a certain level, it started to cause severe impacts," said University of Minnesota Department of Chemical Engineering and Materials Science Professor Joseph Zasadzinski and lead professor on the research.
"Your average everyday person usually won't need to think about this, but if a virus or infection is bothering your lung surfactant system and you end up in the hospital, then it could become top of mind very quickly," Zasadzinski added
There are a natural amount of these lysolipids that exist in the human body, and as long as those stay below a specific concentration, the average person can breathe normally. When someone has a bad infection, those lysolipids increase, which can lead to respiratory distress. Once a patient is headed in that direction, there are not many ways of reversing those symptoms.
"This research shows frequency dependence, or how quickly you open and close the lungs. This could help doctors try to tailor the treatment process for each specific patient," said Clara Ciutara, a 2023 Ph.D. chemical engineering and materials science graduate and first author of the study.
Previous research of neonatal respiratory distress syndrome (NRDS) in premature infants found that it could be treated by introducing replacement lung surfactant, but that was not the case in adults. It is the amount of lysolipid that determines the outcome of the surfactant in the lungs, not the breakdown of the existing lung surfactant.
The next step in the research will be to translate these ideas into a clinical environment and test to see if they can manipulate specific molecules to make them less active or stick to a specific place. This could help drop the concentration of the lysolipids to a threshold that may be able to reverse symptoms of ARDS and put people on the road to recovery.
In addition to Zasadzinski and Ciutara, the research team included University of Minnesota Department of Chemical Engineering and Materials Science NIH postdoctoral fellow Steven V. Iasella, undergraduate student Boxun Huang, and former postdoctoral associate Sourav Barman.
This work is supported by a grant from National Institutes of Health (NIH) Heart, Lung, and Blood Institute. All microscopy images were obtained at the University Imaging Center at the University of Minnesota.
- Lung Disease
- Lung Cancer
- Mental Health Research
- Diseases and Conditions
- Infectious Diseases
- Cystic Fibrosis
- Upper respiratory tract infection
- Severe acute respiratory syndrome
- Pulmonary alveolus
- Gas exchange
- Whooping cough
Story Source:
Materials provided by University of Minnesota . Note: Content may be edited for style and length.
Journal References :
- Clara O. Ciutara, Steven V. Iasella, Boxun Huang, Sourav Barman, Joseph A. Zasadzinski. Evolution of interfacial mechanics of lung surfactant mimics progression of acute respiratory distress syndrome . Proceedings of the National Academy of Sciences , 2023; 120 (51) DOI: 10.1073/pnas.2309900120
- Charles Maldarelli. Respiratory distress when a lung surfactant loses one of its two hydrophobic tails . Proceedings of the National Academy of Sciences , 2024; 121 (10) DOI: 10.1073/pnas.2320426121
Cite This Page :
Explore More
- High-Efficiency Photonic Integrated Circuit
- Life Expectancy May Increase by 5 Years by 2050
- Toward a Successful Vaccine for HIV
- Highly Efficient Thermoelectric Materials
- Toward Human Brain Gene Therapy
- Whale Families Learn Each Other's Vocal Style
- AI Can Answer Complex Physics Questions
- Otters Use Tools to Survive a Changing World
- Monogamy in Mice: Newly Evolved Type of Cell
- Sustainable Electronics, Doped With Air
Trending Topics
Strange & offbeat.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Global Impact of Respiratory Disease
Stephanie m. levine.
a University of Texas, San Antonio, TX
Darcy D. Marciniuk
b Department of Respirology, Critical Care and Sleep Medicine, University of Saskatchewan, Saskatoon, Canada
The third edition of the Global Impact of Respiratory Disease 1 begins with the statement “We take our breathing and our respiratory health for granted, but our lungs enable us to live, laugh, love, and enjoy activities.” At no time in our recent history has that truth become more evident and more relevant. The COVID-19 pandemic, in a short period of 24 months, has claimed the lives of > 5.7 million people, 2 largely all from respiratory causes. But even before the pandemic, three respiratory diseases were entrenched in the top 10 causes of death in the world.
COPD is the third-leading cause of death worldwide, killing 3.2 million individuals every year and accounting for an astounding 81.7% of the total number of deaths from chronic respiratory disease. Pneumonia is a leading cause of death among children < 5 years old outside the neonatal period and in adults > 65 years old. Lung cancer is the deadliest of nearly all cancers, with 5-year survival rates of only 10% to 20%, even in developed countries. We know that asthma is the most common chronic disease of childhood, and the prevalence of asthma has been rising for the past three decades. TB would be the greatest single infectious cause of death if it were not for the current COVID-19 pandemic, with an estimated 500,000 new cases of rifampicin-resistant or multidrug-resistant TB in 2019 alone. In addition to the top five conditions mentioned here, the report also highlights the significant global burden of sleep-disordered breathing, pulmonary hypertension, occupational lung diseases, in addition to the harmful effects of air pollution and climate change.
The Global Impact of Respiratory Disease 1 was compiled by the Forum of International Respiratory Societies, a coalition of the leading international professional societies in the world. Together, the American College of Chest Physicians, American Thoracic Society, Asian Pacific Society of Respirology, Asociación Latinoamericana de Tórax, European Respiratory Society, International Union Against Tuberculosis and Lung Disease (The Union), Pan African Thoracic Society, Global Initiative for Asthma, and the Global Initiative for Chronic Obstructive Lung Disease joined in the collective goal of empowering respiratory health worldwide through global advocacy. These societies continue to work hard to reduce the global burden of lung disease and to ensure everyone can and is able to breathe freely. The third edition of the Global Impact of Respiratory Disease is an important step; it provides the means for meeting those goals, outlines major causes of respiratory disease and death, and lays out clear recommendations for global action. The executive summary of the report has been translated into eight languages.
But the report goes far beyond only highlighting the problems and consequences. Representing > 100,000 professional members worldwide who care about lung health, the Forum of International Respiratory Societies also clearly identified the following eight essential actions to reduce the burden of respiratory disease and improve global health.
- 1. Improve public and policy makers’ awareness that respiratory health is vital to global health and that childhood respiratory disease has long-term negative consequences on adult health.
- 2. Reduce, and then eliminate, the use of all tobacco and smoking products.
- 3. Adopt and adhere to World Health Organization (WHO) standards, at a minimum, to reduce ambient, indoor, and occupational air pollution for all countries.
- 4. Implement universal access to quality health care, including the availability of affordable, quality-assured, essential medicines and universal coverage for all effective childhood and adult immunizations.
- 5. Improve the prevention and early diagnosis of respiratory diseases.
- 6. Increase education and training of health care professionals in respiratory disease worldwide.
- 7. Standardize the monitoring and reporting of the prevalence, severity, and management of respiratory diseases to enable development of better-informed national strategies through programs of WHO and governmental and nongovernmental organizations.
- 8. Boost funding for respiratory research to develop programs, tools, and strategies to better prevent and treat respiratory disease.
So you might be thinking “What can I do to help make a difference?” or maybe “This is so big and complicated: what can really be achieved?”
Those are great questions, as are the answers.
Imagine if, together, we could influence policies or decision-makers to further enable respiratory health? What impact could we make if we acted together to further reduce the harmful effect of tobacco and work towards completely eliminating smoking? What would be the impact of better trained and supported health care professionals working together and health care systems and policies that more effectively aided the prevention and optimal management of lung disease for all? What investment in respiratory research and researchers would lead to breakthroughs, to cures, and to a future in which our children, all around the world, could almost take their breathing for granted because lung diseases were not listed prominently in the top ten causes of death in the world? What more could we do, either as members of these societies or as individuals who fully appreciate the destructive forces of lung disease and the benefits of respiratory health, to advance these tangible outcomes?
Let’s talk specifics and specifics close to home.
Imagine better access to pulmonary rehabilitation and supplemental oxygen therapy, more available and affordable medications and therapies, and health care systems that are accessible and served everyone. Imagine equitable access to quality care and populations that we serve with descriptors that do not begin with “disadvantaged” or “underserviced.” Imagine funding for training and respiratory research that is equitable and aligned with the enormous burden of respiratory disease and that more completely nourishes the genuine possibilities of breakthroughs and cures afforded by our researchers and research teams. One easily could imagine even more.
The pandemic has highlighted starkly the reality that what is far away can become so close to home in a matter of days. The world’s issues are inexplicably our issues. The pandemic has also shown that what we do locally can help many far beyond our own borders. And all of us who have cared for patients know that someone who is short of breath, no matter where they live or work or play, is suffering.
The Global Impact of Respiratory Disease 1 has made clear the consequences, around the world, of lung diseases and the benefits and the path to respiratory health. Let us now together eliminate that suffering and amplify the benefits of working together in our own clinics and our own hospitals and laboratories, not only for those individuals we care for, but also for millions of other patients around the world.
The next edition of this report is proposed to be co-developed with the WHO for release in 2025 at the High-Level United Nations NCD Meeting. This publication will be aimed specifically at a target audience of high-level health care policy makers and will include an Executive Policy Briefing with recommendations directed at both global and national levels.
There is much work to be done before that next step.
FINANCIAL/NONFINANCIAL DISCLOSURES: The authors have reported to CHEST the following: S. M. Levine is an employee of the University of Texas and serves as Deputy Editor, Contributor Equity and Experience, CHEST . D. D. Marciniuk has undertaken consulting with Alberta Health Services, Canadian Foundation for Healthcare Improvement, Health Canada, Lung Association of Saskatchewan, Ontario Ministry of Health and Long-Term Care, Saskatchewan Health Authority, and Yukon Health and Social Services; has provided research advisory and received research funding (held and managed by the University of Saskatchewan) from AstraZeneca, Boehringer Ingelheim, Canadian Institute of Health Research, GlaxoSmithKline, Grifols, Lung Association of Saskatchewan, Lung Health Institute of Canada, Novartis, Sanofi, Saskatchewan Health Research Foundation, Schering-Plough; and is an employee of the University of Saskatchewan and serves as Deputy Editor. Outreach, CHEST .
Emerging Technological Trends and Advancements in Respiratory Medicine
- First Online: 24 March 2022
Cite this chapter

- M. Yasasve 4 ,
- D. Manojj 5 &
- L. Ansel Vishal 5
702 Accesses
Pulmonology is a medical discipline concerned with a number of respiratory diseases also known as “respiratory medicine” or “chest medicine.” Respiratory medicine mainly deals with the diagnosis, management of a wide variety of lung conditions, their linings, blood vessels, muscles, and nerves used to respire. Medicines are the most effective and viable manner for treating respiratory conditions, whether they are inhaled (steroids) or orally or orally administered (antibiotics). A typical example is the use of inhalers in treating allergic lung disorders such as asthma or chronic pulmonary obstructive disease. Also, oxygen therapy with ventilator support is used during adverse respiratory situations like emphysema and idiopathic pulmonary fibrosis. Over the past 20 years, our conceptual understanding about the dynamics of respiratory disorders has changed due to clinical and molecular technological advancements. In light of this rapid growth, this chapter will highlight some of the recent advances in the clinical practice of respiratory medicine. Advancements in the fields of drug developments, biomarker technology, intervention medicine, imaging technology, and nanotechnology have paved the way for treating complicated lung diseases and lung disorders.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others
Introduction to Chronic Respiratory Diseases: A Pressing Need for Novel Therapeutic Approaches

New Technologies in COPD Management

Introduction to Lung Disease
Abedini A, Kiani A, Emami H, Touhidi MH (2019) Serum Procalcitonin level as a predictor of bacterial infection in patients with COPD exacerbation. Tanaffos 18:112–117
PubMed PubMed Central Google Scholar
Afonso Júnior JE, Werebe Ede C, Carraro RM, Teixeira RH, Fernandes LM, Abdalla LG, Samano MN, Pêgo-Fernandes PM (2015) Lung transplantation. Einstein (Sao Paulo) 13:297–304
Article Google Scholar
Balbi B, Bason C, Balleari E, Fiasella F, Pesci A, Ghio R, Fabiano F (1997) Increased bronchoalveolar granulocytes and granulocyte/macrophage colony-stimulating factor during exacerbations of chronic bronchitis. Eur Respir J 10:846–850
CAS PubMed Google Scholar
Bargagli E, Magi B, Olivieri C, Bianchi N, Landi C, Rottoli P (2011) Analysis of serum amyloid a in sarcoidosis patients. Respir Med 105:775–780
Article CAS PubMed Google Scholar
Barnes PJ (2008a) The cytokine network in asthma and chronic obstructive pulmonary disease. J Clin Invest 118:3546–3556
Article CAS PubMed PubMed Central Google Scholar
Barnes PJ (2008b) Immunology of asthma and chronic obstructive pulmonary disease. Nat Rev Immunol 8:183–192
Bartziokas K, Papaioannou AI, Loukides S, Papadopoulos A, Haniotou A, Papiris S, Kostikas K (2014) Serum uric acid as a predictor of mortality and future exacerbations of COPD. Eur Respir J 43:43–53
Bhowmik A, Seemungal TA, Sapsford RJ, Wedzicha JA (2000) Relation of sputum inflammatory markers to symptoms and lung function changes in COPD exacerbations. Thorax 55:114–120
Bozkaya D, Yiğit Ş, Yurdakök M (2019) Is serum procalcitonin level a reliable indicator in early diagnosis of congenital pneumonia? Turk J Pediatr 61:34–39
Article PubMed Google Scholar
Bullens DM, Truyen E, Coteur L, Dilissen E, Hellings PW, Dupont LJ, Ceuppens JL (2006) IL-17 mRNA in sputum of asthmatic patients: linking T cell driven inflammation and granulocytic influx? Respir Res 7:135
Article PubMed PubMed Central CAS Google Scholar
Butler CC, Gillespie D, White P, Bates J, Lowe R, Thomas-Jones E, Wootton M, Hood K, Phillips R, Melbye H, Llor C, Cals JWL, Naik G, Kirby N, Gal M, Riga E, Francis NA (2019) C-reactive protein testing to guide antibiotic prescribing for COPD exacerbations. N Engl J Med 381:111–120
Caramori G, Adcock IM, Di Stefano A, Chung KF (2014) Cytokine inhibition in the treatment of COPD. Int J Chron Obstruct Pulmon Dis 9:397–412
Chan JF, Yip CC, To KK, Tang TH, Wong SC, Leung KH, Fung AY, Ng AC, Zou Z, Tsoi HW, Choi GK, Tam AR, Cheng VC, Chan KH, Tsang OT, Yuen KY (2020) Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-PCR assay validated in vitro and with clinical specimens. J Clin Microbiol 58:e00310–e00320
Chee C, Sellahewa L, Pappachan JM (2014) Inhaled corticosteroids and bone health. Open Respir Med J 8:85–92
Article PubMed PubMed Central Google Scholar
Conway Morris A, Kefala K, Wilkinson TS, Moncayo-Nieto OL, Dhaliwal K, Farrell L, Walsh TS, Mackenzie SJ, Swann DG, Andrews PJ, Anderson N, Govan JR, Laurenson IF, Reid H, Davidson DJ, Haslett C, Sallenave JM, Simpson AJ (2009) Diagnostic importance of pulmonary interleukin-1beta and interleukin-8 in ventilator-associated pneumonia. Thorax 65:201–207
d’Alessandro M, Carleo A, Cameli P, Bergantini L, Perrone A, Vietri L, Lanzarone N, Vagaggini C, Sestini P, Bargagli E (2020) Correction to: BAL biomarkers’ panel for differential diagnosis of interstitial lung diseases. Clin Exp Med 20:217
Davis MD, Montpetit AJ (2018) Exhaled breath condensate: an update. Immunol Allergy Clin N Am 38:667–678
de Benedictis FM, Bush A (2012) Corticosteroids in respiratory diseases in children. Am J Respir Crit Care Med 185:12–23
Article PubMed CAS Google Scholar
De Coster DA, Jones M (2014) Tailoring of corticosteroids in COPD management. Curr Respir Care Rep 3:121–132
Donnelly JP, Baddley JW, Wang HE (2014) Antibiotic utilization for acute respiratory tract infections in U.S. emergency departments. Antimicrob Agents Chemother 58:1451–1457
Dua K, Shukla SD, de Jesus Andreoli Pinto T, Hansbro PM (2017) Nanotechnology: advancing the translational respiratory research. Interv Med Appl Sci 9:39–41
Eddy RL, Svenningsen S, McCormack DG, Parraga G (2018) What is the minimal clinically important difference for helium-3 magnetic resonance imaging ventilation defects? Eur Respir J 51:1800324
Eguiluz-Gracia I, Tay TR, Hew M, Escribese MM, Barber D, O’Hehir RE, Torres MJ (2018) Recent developments and highlights in biomarkers in allergic diseases and asthma. Allergy 73:2290–2305
Feltis BN, Wignarajah D, Zheng L, Ward C, Reid D, Harding R, Walters EH (2006) Increased vascular endothelial growth factor and receptors: relationship to angiogenesis in asthma. Am J Respir Crit Care Med 173:1201–1207
Fort MM, Cheung J, Yen D, Li J, Zurawski SM, Lo S, Menon S, Clifford T, Hunte B, Lesley R, Muchamuel T, Hurst SD, Zurawski G, Leach MW, Gorman DM, Rennick DM (2001) IL-25 induces IL-4, IL-5, and IL-13 and Th2-associated pathologies in vivo. Immunit 15:985–995
Article CAS Google Scholar
Francis NA, Gillespie D, White P, Bates J, Lowe R, Sewell B, Phillips R, Stanton H, Kirby N, Wootton M, Thomas-Jones E, Hood K, Llor C, Cals J, Melbye H, Naik G, Gal M, Fitzsimmons D, Alam MF, Riga E, Cochrane A, Butler CC (2020) C-reactive protein point-of-care testing for safely reducing antibiotics for acute exacerbations of chronic obstructive pulmonary disease: the PACE RCT. Health Technol assess 24:1-108. Doi:
Google Scholar
Frye L, Machuzak M (2017) Airway complications after lung transplantation. Clin Chest Med 38:693–706
Hu R, Han C, Pei S, Yin M, Chen X (2020a) Procalcitonin levels in COVID-19 patients. Int J Antimicrob Agents 10:106051
Hu Y, Sun J, Dai Z, Deng H, Li X, Huang Q, Wu Y, Sun L, Xu Y (2020b) Prevalence and severity of corona virus disease 2019 (COVID-19): a systematic review and meta-analysis. J Clin Virol 127:104371
Jenkins C (2017) Drugs for chronic obstructive pulmonary disease. Aust Prescr 40:15–19
Jiang C, Jiang L, Qin Q (2019) Conventional treatments plus acupuncture for asthma in adults and adolescent: a systematic review and Meta-analysis. Evid Based Complement Alternat Med 2019:9580670
Kakhki VR (2007) Positron emission tomography in the management of lung cancer. Ann Thorac Med 2:69–76
Kalender WA (2006) X-ray computed tomography. Phys Med Biol 51:R29–R43
Kany S, Vollrath JT, Relja B (2019) Cytokines in inflammatory disease. Int J Mol Sci 20:6008
Article CAS PubMed Central Google Scholar
Kelly HW, Van Natta ML, Covar RA, Tonascia J, Green RP, Strunk RC, CAMP Research Group (2008) Effect of long-term corticosteroid use on bone mineral density in children: a prospective longitudinal assessment in the childhood asthma management program (CAMP) study. Pediatrics 122:e53–e61
Kerstjens HA, Groen HJ, van Der Bij W (2001) Recent advances: respiratory medicine. BMJ 323:1349–1353
Kołodziej M, de Veer MJ, Cholewa M, Egan GF, Thompson BR (2017) Lung function imaging methods in cystic fibrosis pulmonary disease. Respir Res 18:96
Konradsen JR, Skantz E, Nordlund B, Lidegran M, James A, Ono J, Ohta S, Izuhara K, Dahlén SE, Alving K, Hedlin G (2015) Predicting asthma morbidity in children using proposed markers of Th2-type inflammation. Pediatr Allergy Immunol 26:772–779
Lai Y, Dong C (2016) Therapeutic antibodies that target inflammatory cytokines in autoimmune diseases. Int Immunol 28:181–188
Lange C, Abubakar I, Alffenaar JW, Bothamley G, Caminero JA, Carvalho AC, Chang KC, Codecasa L, Correia A, Crudu V, Davies P, Dedicoat M, Drobniewski F, Duarte R, Ehlers C, Erkens C, Goletti D, Günther G, Ibraim E, Kampmann B, Kuksa L, de Lange W, van Leth F, van Lunzen J, Matteelli A, Menzies D, Monedero I, Richter E, Rüsch-Gerdes S, Sandgren A, Scardigli A, Skrahina A, Tortoli E, Volchenkov G, Wagner D, van der Werf MJ, Williams B, Yew WW, Zellweger JP, Cirillo DM, TBNET (2014) Management of patients with multidrug-resistant/extensively drug-resistant tuberculosis in Europe: a TBNET consensus statement. Eur Respir J 44:23–63
Lee HW, Choi SM, Lee J, Park YS, Lee CH, Yim JJ, Yoo CG, Kim YW, Han SK, Lee SM (2019) Serum uric acid level as a prognostic marker in patients with acute respiratory distress syndrome. J Intensive Care Med 34:404–410
Li H, Xiang X, Ren H, Xu L, Zhao L, Chen X, Long H, Wang Q, Wu Q (2020) Serum amyloid a is a biomarker of severe coronavirus disease and poor prognosis. J Infect 80:646–655
Lin KH, Wang FL, Wu MS, Jiang BY, Kao WL, Chao HY, Wu JY, Lee CC (2014) Serum procalcitonin and C-reactive protein levels as markers of bacterial infection in patients with liver cirrhosis: a systematic review and meta-analysis. Diagn Microbiol Infect Dis 80:72–78
Liu Q, Gao Y, Ci X (2019) Role of Nrf2 and its activators in respiratory diseases. Oxidative Med Cell Longev 143:2062–2074
Liu F, Li L, Xu M, Wu J, Luo D, Zhu Y, Li B, Song X, Zhou X (2020) Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J Clin Virol 127:104370
Llor C, Bjerrum L (2014) Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf 5:229–241
Lu Z, Huang W, Wang L, Xu N, Ding Q, Cao C (2018) Exhaled nitric oxide in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 13:2695–2705
Ma JT, Tang C, Kang L, Voynow JA, Rubin BK (2018) Cystic fibrosis sputum rheology correlates with both acute and longitudinal changes in lung function. Chest 154:370–377
Manojj D, Yasasve M, Kanmani K, Ramesh AS (2020) In vitro cytotoxicity study and anti-Brucella activity of Tarenna asiatica (L). S Afr J Bot 128:54–61
Matsumoto H (2019) Roles of Periostin in asthma. Adv Exp Med Biol 1132:145–159
Matsuo Y, Ogawa E, Seto-Yukimura R, Ryujin Y, Kinose D, Yamaguchi M, Osawa M, Nagao T, Kurosawa H, Nakano Y (2019) Novel respiratory impedance-based phenotypes reflect different Pathophysiologies in chronic obstructive pulmonary disease patients. Int J Chron Obstruct Pulmon Dis 14:2971–2977
Mayeux R (2004) Biomarkers: potential uses and limitations. NeuroRx 1:182–188
Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, Cooley LA, Dean NC, Fine MJ, Flanders SA, Griffin MR, Metersky ML, Musher DM, Restrepo MI, Whitney CG (2019) Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med 200:e45–e67
Meyer KC (2018) Recent advances in lung transplantation. F1000Res 7:1684
Miller JD, Coughlin MD, Edey L, Miller P, Sivji Y (2000) Equipoise and the ethics of the Canadian lung volume reduction surgery trial study: should there be a randomized, controlled trial to evaluate lung volume reduction surgery? Can Respir J 7:329–332
Naylor S (2003) Biomarkers: current perspectives and future prospects. Expert Rev Mol Diagn 3:525–529
Newby PR, Crossley D, Crisford H, Stockley JA, Mumford RA, Carter RI, Bolton CE, Hopkinson NS, Mahadeva R, Steiner MC, Wilkinson TMA, Sapey E, Stockley RA (2019) A specific proteinase 3 activity footprint in α1-antitrypsin deficiency. ERJ Open Res 5:00095–02019
Oostveen E, MacLeod D, Lorino H, Farré R, Hantos Z, Desager K, Marchal F (2003) ERS task force on respiratory impedance measurements. The forced oscillation technique in clinical practice: methodology, recommendations and future developments. Eur Respir J 22:1026–1041
Park JS, Jang AS, Park SW, Lee YM, Uh ST, Kim YH, Cha JY, Park SM, Park CS (2010) Protection of leukotriene receptor antagonist against aspirin-induced bronchospasm in asthmatics. Allergy Asthma Immunol Res 2:48–54
Petousi N, Talbot NP, Pavord I, Robbins PA (2019) Measuring lung function in airways diseases: current and emerging techniques. Thorax 74:797–805
Póvoa P, Coelho L, Bos LDJ (2020) New biomarkers for respiratory infections. Curr Opin Pulm Med 26:232–240
Pruteanu AI, Chauhan BF, Zhang L, Prietsch SO, Ducharme FM (2014) Inhaled corticosteroids in children with persistent asthma: dose-response effects on growth. Evid Based Child Health 9:931–1046
Reese SE, Xu CJ, den Dekker HT, Lee MK, Sikdar S, Ruiz-Arenas C, Merid SK, Rezwan FI, Page CM, Ullemar V, Melton PE, Oh SS, Yang IV, Burrows K, Söderhäll C, Jima DD, Gao L, Arathimos R, Küpers LK, Wielscher M, Rzehak P, Lahti J, Laprise C, Madore AM, Ward J, Bennett BD, Wang T, Bell DA; BIOS consortium, Vonk JM, Håberg SE, Zhao S, Karlsson R, Hollams E, Hu D, Richards AJ, Bergström A, Sharp GC, Felix JF, Bustamante M, Gruzieva O, Maguire RL, Gilliland F, Baïz N, Nohr EA, Corpeleijn E, Sebert S, Karmaus W, Grote V, Kajantie E, Magnus MC, Örtqvist AK, Eng C, Liu AH, Kull I, Jaddoe VWV, Sunyer J, Kere J, Hoyo C, Annesi-Maesano I, Arshad SH, Koletzko B, Brunekreef B, Binder EB, Räikkönen K, Reischl E, Holloway JW, Jarvelin MR, Snieder H, Kazmi N, Breton CV, Murphy SK, Pershagen G, Anto JM, Relton CL, Schwartz DA, Burchard EG, Huang RC, Nystad W, Almqvist C, Henderson AJ, Melén E, Duijts L, Koppelman GH, London SJ (2019) Epigenome-wide meta-analysis of DNA methylation and childhood asthma. J Allergy Clin Immunol 143:2062–2074
Rosenwasser LJ (1998) Biologic activities of IL-1 and its role in human disease. J Allergy Clin Immunol 102:344–350
Ross MH, Zick BL, Tsalik EL (2019) Host-based diagnostics for acute respiratory infections. Clin Ther 41:1923–1938
Saito H, Morikawa H, Howie K, Crawford L, Baatjes AJ, Denburg E, Cyr MM, Denburg JA (2004) Effects of a cysteinyl leukotriene receptor antagonist on eosinophil recruitment in experimental allergic rhinitis. Immunology 113:246–252
Sethi GR, Singhal KK (2008) Pulmonary diseases and corticosteroids. Indian J Pediatr 75:1045–1056
Seyyedi SR, Malekmohammad M, Chitsazan M, Behzadnia N, Sadr M, Hashemian SM, Sharif-Kashani B (2017) Relationship between serum uric acid levels and the severity of pulmonary hypertension. Tanaffos 16:283–288
Silva M, Milanese G, Seletti V, Ariani A, Sverzellati N (2018) Pulmonary quantitative CT imaging in focal and diffuse disease: current research and clinical applications. Br J Radiol 91:20170644
Stellrecht KA, Cimino JL, Wilson LI, Maceira VP, Butt SA (2019) Panther fusion ® respiratory virus assays for the detection of influenza and other respiratory viruses. J Clin Virol 121:104204
Stirling RG, van Rensen EL, Barnes PJ, Chung KF (2001) Interleukin-5 induces CD34(+) eosinophil progenitor mobilization and eosinophil CCR3 expression in asthma. Am J Respir Crit Care Med 164:1403–1409
Tan C, Huang Y, Shi F, Tan K, Ma Q, Chen Y, Jiang X, Li X (2020) C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J Med Virol 92:856–862
Thomas PS, Yates DH, Barnes PJ (1995) Tumor necrosis factor-alpha increases airway responsiveness and sputum neutrophilia in normal human subjects. Am J Respir Crit Care Med 152:76–80
Tillu G, Chaturvedi S, Chopra A, Patwardhan B (2020) Public health approach of Ayurveda and yoga for COVID-19 prophylaxis. J Altern Complement Med 26:360–364
Utz JP, Hubmayr RD, Deschamps C (1998) Lung volume reduction surgery for emphysema: out on a limb without a NETT. Mayo Clin Proc 73:552–566
Valacer DJ (1999) New treatments for asthma: the role of leukotriene modifier agents. J Natl Med Assoc 91:26S–39S
CAS PubMed PubMed Central Google Scholar
Volpi S, Ali JM, Tasker A, Peryt A, Aresu G, Coonar AS (2018) The role of positron emission tomography in the diagnosis, staging and response assessment of non-small cell lung cancer. Ann Transl Med 6:95
Wang L (2020) C-reactive protein levels in the early stage of COVID-19. Med Mal Infect 50:332–334
WHO (2007) Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach. https://www.who.int/gard/publications/GARD_Manual/en/ . Accessed 30 July 2020
WHO (2018) Cancer fact sheet. https://www.who.int/news-room/fact-sheets/detail/cancer . Accessed 30 July 2020
Yang W, Sirajuddin A, Zhang X, Liu G, Teng Z, Zhao S, Lu M (2019) The role of imaging in 2019 novel coronavirus pneumonia (COVID-19). Eur Radiol 15:1–9
Yeh GY, Horwitz R (2017) Integrative medicine for respiratory conditions: asthma and chronic obstructive pulmonary disease. Med Clin North Am 101:925–941
Zhou Y, McLane M, Levitt RC (2001) Th2 cytokines and asthma. Interleukin-9 as a therapeutic target for asthma. Respir Res 2:80–84
Download references
Author information
Authors and affiliations.
Department of Biotechnology, Sri Venkateswara College of Engineering (Autonomous—Affiliated to Anna University), Sriperumbudur, Tamil Nadu, India
Department of Biotechnology, Sree Sastha Institute of Engineering & Technology (Affiliated to Anna University), Chennai, Tamil Nadu, India
D. Manojj & L. Ansel Vishal
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Department of Life Sciences, International Medical University, Kuala Lumpur, Malaysia
Dinesh Kumar Chellappan
Regulatory Affairs Coordinator, Bioproperties Pty Ltd, Glenorie, NSW, Australia
Kavita Pabreja
School of Pharmacy, Al-Karim University, Katihar, Bihar, India
Md. Faiyazuddin
Rights and permissions
Reprints and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Yasasve, M., Manojj, D., Vishal, L.A. (2022). Emerging Technological Trends and Advancements in Respiratory Medicine. In: Chellappan, D.K., Pabreja, K., Faiyazuddin, M. (eds) Advanced Drug Delivery Strategies for Targeting Chronic Inflammatory Lung Diseases . Springer, Singapore. https://doi.org/10.1007/978-981-16-4392-7_25
Download citation
DOI : https://doi.org/10.1007/978-981-16-4392-7_25
Published : 24 March 2022
Publisher Name : Springer, Singapore
Print ISBN : 978-981-16-4391-0
Online ISBN : 978-981-16-4392-7
eBook Packages : Biomedical and Life Sciences Biomedical and Life Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

- Share facebook twitter google linkedin
Perspectives: Experts’ Consensus on the Management of Respiratory Disease Syndemic
- Weizhong Yang 1,2,3 , , ;
- Zhongjie Li 1,2,3 ;
- Ting Yang 4 ;
- Yanming Li 5 ;
- Zhengde Xie 6 ;
- Luzhao Feng 1,2,3 ;
- Zhibin Peng 7 ;
- Jue Liu 8 , ,
- management ,
- respiratory disease ,
- experts’ consensus
- Funding: Supported by the National Natural Science Foundation of China (Grant Numbers: 72122001 and 72211540398) and Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2022-I2M-CoV19-006; 2021-I2M-1-044)
Author Affiliations
School of Population Medicine and Public Health, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
State Key Laboratory of Respiratory Health and Multimorbidity, Beijing, China
Key Laboratory of Pathogen Infection Prevention and Control, Peking Union Medical College, Ministry of Education, Beijing, China
National Center for Respiratory Diseases, State Key Laboratory of Respiratory Health and Multimorbidity, National Clinical Research Center for Respiratory Diseases, Institute of Respiratory Medicine, Chinese Academy of Medical Sciences, Department of Pulmonary and Critical Care Medicine, Center of Respiratory Medicine, China-Japan Friendship Hospital, Beijing, China
Department of Pulmonary and Critical Care Medicine, National Center of Gerontology, Beijing Hospital, Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing, China
Beijing Key Laboratory of Pediatric Respiratory Infection Diseases, Key Laboratory of Major Diseases in Children, Ministry of Education, National Clinical Research Center for Respiratory Diseases, Research Unit of Critical Infection in Children, Chinese Academy of Medical Sciences, 2019RU016, National Key Discipline of Pediatrics (Capital Medical University), Beijing Pediatric Research Institute, Beijing Children's Hospital, Capital Medical University, National Center for Children's Health, Beijing, China
Chinese Center for Disease Control and Prevention, Beijing, China
Department of Epidemiology and Biostatistics, School of PublicHealth, Key Laboratory of Epidemiology of Major Diseases, Ministry of Education, Peking University Health Science Center-Weifang Joint Research Center for Maternal and Child Health,Peking University, Beijing, China
- Corresponding authors: [email protected] -->Weizhong Yang, [email protected] ; [email protected] -->Jue Liu, [email protected]
Online Date: February 23 2024
Issue date: february 23 2024, doi: 10.46234/ccdcw2024.029, proportional views, 通讯作者: 陈斌, [email protected].
沈阳化工大学材料科学与工程学院 沈阳 110142
Article Metrics
Article views( 1986 ) HTML views( 43 ) --> PDF downloads( 26 ) Cited by( ) Received: 02 January 2024 Revised manuscript received: Published in print: 23 February 2024 -->

- PDF Downloads( 26 )
- Abstract views( 1986 )
- HTML views( 43 )

Experts’ Consensus on the Management of Respiratory Disease Syndemic
- 1. School of Population Medicine and Public Health, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
- 2. State Key Laboratory of Respiratory Health and Multimorbidity, Beijing, China
- 3. Key Laboratory of Pathogen Infection Prevention and Control, Peking Union Medical College, Ministry of Education, Beijing, China
- 4. National Center for Respiratory Diseases, State Key Laboratory of Respiratory Health and Multimorbidity, National Clinical Research Center for Respiratory Diseases, Institute of Respiratory Medicine, Chinese Academy of Medical Sciences, Department of Pulmonary and Critical Care Medicine, Center of Respiratory Medicine, China-Japan Friendship Hospital, Beijing, China
- 5. Department of Pulmonary and Critical Care Medicine, National Center of Gerontology, Beijing Hospital, Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing, China
- 6. Beijing Key Laboratory of Pediatric Respiratory Infection Diseases, Key Laboratory of Major Diseases in Children, Ministry of Education, National Clinical Research Center for Respiratory Diseases, Research Unit of Critical Infection in Children, Chinese Academy of Medical Sciences, 2019RU016, National Key Discipline of Pediatrics (Capital Medical University), Beijing Pediatric Research Institute, Beijing Children's Hospital, Capital Medical University, National Center for Children's Health, Beijing, China
- 7. Chinese Center for Disease Control and Prevention, Beijing, China
- 8. Department of Epidemiology and Biostatistics, School of PublicHealth, Key Laboratory of Epidemiology of Major Diseases, Ministry of Education, Peking University Health Science Center-Weifang Joint Research Center for Maternal and Child Health,Peking University, Beijing, China
Corresponding authors: Weizhong Yang, [email protected] [email protected] -->; Jue Liu, [email protected] [email protected] -->
- Accepted: 2024-01-02
- Available Online: 2024-02-23
The global burden of respiratory diseases is a significant and increasing threat to individuals worldwide. In 2017, there were 544.9 million cases of chronic respiratory diseases, a 39.8% increase since 1990 ( 1 ). These diseases were the third leading cause of global mortality in 2017, accounting for 7.0% of all deaths, an 18.0% increase compared to 1990. In addition to chronic respiratory diseases, acute infectious respiratory diseases, including influenza, coronavirus diseases 2019 (COVID-19), and respiratory syncytial virus, pose significant public health concerns and cause both short-term and long-term health damages ( 2 – 3 ). The presence of complex coexisting diseases in the respiratory system further complicates treatment and increases the burden of disease. To effectively address these challenges, it is crucial to implement a comprehensive and robust management approach.
A syndemic refers to the co-occurrence of multiple diseases or health conditions within a population, where biological or behavioral factors worsen the negative health impacts of these conditions ( 4 ). Syndemic theory suggests that the combined presence of diseases, along with social and environmental factors, synergistically affects population health. This theory provides a valuable framework for understanding and addressing respiratory disease syndemics. Managing respiratory diseases from a syndemic perspective necessitates a deep understanding of the intricate interplay between biological, social, and environmental factors that contribute to the occurrence and progression of these diseases. By adopting a syndemic approach, the focus shifts from managing individual diseases to a collaborative model that prioritizes population-level interventions, including proactive diagnosis, comprehensive assessment of disease severity, and integrated management of conditions associated with respiratory diseases. The expert consensus on managing respiratory disease syndemics aims to support research and practical interventions in addressing these complex respiratory health challenges.

The Process of Consensus Formulation
The research team utilized evidence-based medicine methodology to focus on studies pertaining to the management of respiratory diseases. A comprehensive literature search was conducted, encompassing both domestic and international sources, resulting in the collection of 7,085 relevant articles in the database up to December 2023. Through meticulous examination of these articles, relevant information pertaining to the research objectives was extracted. Rigorous criteria were applied to select representative studies, ensuring the robustness and comprehensiveness of the analysis. Expert input was integrated from various fields such as public health, disease prevention and control, and clinical respiratory science. This involved consolidating guidelines, consensus statements, and recommendations related to respiratory disease management. The consensus was developed through three rounds of expert discussions, incorporating advancements in research and practices for the prevention and treatment of respiratory disease syndemic. The consensus primarily consists of fundamental principles that facilitate practical application by healthcare professionals involved in the management of respiratory disease syndemic. Regular revisions will be made based on feedback from prevention and treatment practices in the future. The consensus was initiated and developed by the Chinese Academy of Medical Sciences and Peking University and has been registered on the international Practice Guideline Registration for Transparency platform (PREPARE, http://www.guidelines-registry.org ) in collaboration with the World Health Organization Guidelines Implementation and Knowledge Translation Center. The registration code for this consensus is PREPARE-2024CN181.
Concept and Impact
Recommendation 1: A respiratory disease syndemic is characterized by the concurrent presence and interconnectedness of multiple respiratory diseases within a population.
At the individual level, the concept of respiratory disease syndemic refers to the occurrence of one or more acute or chronic respiratory diseases within a specific time period in conjunction with pre-existing chronic respiratory disease. This includes chronic non-communicable respiratory diseases such as chronic bronchitis, chronic obstructive pulmonary disease (COPD), asthma, interstitial lung diseases, pneumoconiosis, sleep-disordered breathing, pulmonary arterial hypertension, as well as acute and chronic communicable respiratory diseases like influenza, tuberculosis (TB), and others. The interaction between these conditions is complex and can have implications beyond respiratory health, extending to organ diseases, mental health issues, geriatric syndromes, and other related problems that can significantly impact overall well-being. Clinical evidence has demonstrated bidirectional relationships between certain respiratory diseases; for example, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection may increase the risk of TB, while latent TB can worsen COVID-19 outcomes ( 5 ). Depression has also been associated with an increased risk of TB, with a complex biopsychosocial mechanism ( 6 ). In COPD, patients often have additional clinically relevant chronic diseases, particularly cardiovascular diseases and cancer, which significantly contribute to mortality ( 7 ). These interactions emphasize the importance of a comprehensive and integrated approach to the diagnosis, management, and overall care of patients with respiratory diseases.
Recommendation 2: It is essential to assess the impact of respiratory disease syndemics at both the individual and population levels.
Medical evaluation, which includes physical examinations and specialized tests such as pulmonary function tests and chest imaging, plays a crucial role in assessing the health of the respiratory system. These tests provide a comprehensive understanding of both respiratory and non-respiratory disorders, helping in the diagnosis of conditions like cardiac or neuromuscular diseases ( 8 ). However, it is important to note that pulmonary function tests, despite their effectiveness, carry a risk of generating aerosols that can lead to infection ( 9 ). Therefore, it is essential to prioritize the safety of all individuals involved and take measures to minimize infection risks when conducting these tests. In addition to pulmonary function tests, quality of life questionnaires like the St. George’s Respiratory Questionnaire (SGRQ) for COPD ( 10 ), the Asthma Quality of Life Questionnaire (AQLQ) for asthma ( 11 ), the Chronic Respiratory Questionnaire (CRQ) for chronic respiratory diseases ( 12 ), the Leicester Cough Questionnaire (LCQ) for cough symptoms ( 13 ), and the Short Form Health Survey (SF-36) ( 14 ) can provide valuable insights into the impact of respiratory disease syndemics on individuals. However, there is currently a lack of standardized scales to quantitatively measure this impact on patients' health and lives. Therefore, further research and development of relevant scales and diagnostic tools are necessary to comprehensively assess and quantify the impact of respiratory disease syndemics on populations. This may involve creating new scales or adopting comprehensive assessment approaches that combine existing scales to measure different aspects of the impact.
Recommendation 3: The presence of respiratory disease syndemics adds complexity to diagnostic and treatment procedures, which can lead to increased demands for healthcare services and complicated medication regimens. This poses long-term challenges for communities.
The simultaneous presence of multiple chronic health conditions necessitates a coordinated treatment approach, which adds complexity to medical decision-making. There are ongoing uncertainties regarding the mechanisms underlying the association between different respiratory diseases ( 15 ). Clinical interventions for one respiratory disease may have varying effects on coexisting comorbidities ( 16 ). It is crucial for individuals with respiratory disease syndemics to receive regular management, including consultations and adherence to healthcare professionals’ recommendations, in order to reduce the risk of disease progression and complications. Additionally, respiratory disease syndemics lead to increased healthcare expenditures, as the presence of intertwined co-infections reduces treatment efficacies and drives up costs ( 17 ). Due to the chronic nature of these diseases, regular medical assessments are necessary, leading to elevated expenses, especially during acute exacerbations. This increased spending creates financial pressure, thereby calling for the exploration of health insurance coverage, government assistance programs, patient support organizations, and prescription assistance programs ( 18 ). Developing a comprehensive financial plan with the assistance of advisors can provide effective strategies for managing healthcare expenses. Integrating regular management, education, and financial strategies into the treatment plan can help individuals and families better navigate the challenges, thus mitigating the overall impact of additional healthcare costs.
Management Targets
Recommendation 4: The main goal of managing respiratory disease syndemics is to proactively reduce the incidence of new respiratory diseases.
Respiratory comorbidities have a significant impact on both the respiratory and immune systems, making patients more susceptible to various irritants such as smoke, smog, viruses, bacteria, and mycoplasma. This susceptibility can worsen symptoms, lead to the development of new respiratory diseases, and increase the overall disease burden, thereby affecting patients’ quality of life and contributing to the transmission of respiratory infectious diseases ( 19 ). To mitigate these risks, it is essential to implement comprehensive medical assessments and personalized management plans that include rehabilitation services and the creation of a conducive environment. Furthermore, patients should adopt personal protective measures such as wearing masks and getting vaccinated to protect themselves against emerging respiratory infections ( 20 ). To effectively reduce the incidence of new respiratory diseases, mitigate the spread of infectious diseases, and safeguard overall health, it is imperative to enhance health education, implement preventive strategies, and provide timely medical interventions. This requires collaborative efforts to address the challenges posed by respiratory disease syndemics and to foster a healthier and more sustainable living environment.
Recommendation 5: Enhancing the overall health status and quality of life of populations with respiratory comorbidities is also a crucial objective in managing the syndemic of respiratory diseases.
The management of respiratory disease syndemics should go beyond focusing on individual diseases and avoiding integrated care to reduce costs and enhance patient safety. It is important to pay attention to patients and consider the impact of respiratory disease syndemics on their health needs ( 21 ). Patients with respiratory comorbidities often experience severe symptoms that significantly affect their quality of life ( 22 ). In cases of COVID-19, patients with comorbidities have been found to have worse clinical outcomes compared to those without comorbidities ( 23 ). Therefore, it is crucial to adopt patient-centered, integrated approach that includes personalized treatment plans and symptom-oriented rehabilitation services to improve the health status and overall well-being of patients ( 7 ). This approach should involve comprehensive medical evaluation, timely intervention, and continuous rehabilitation services. By prioritizing the patient in the management process and providing comprehensive care, we can empower patients to better cope with the challenges of respiratory disease syndemics, leading to a healthier and more fulfilling life.
Recommendation 6: Another crucial objective is to prevent deaths resulting from the syndemic of respiratory diseases.
Chronic respiratory diseases and respiratory infectious diseases contribute significantly to the global disease burden ( 24 ). The presence of multiple respiratory conditions, known as respiratory disease syndemics, has a profound impact on patients, increasing their risk of exacerbated symptoms and mortality ( 25 ). Early diagnosis, prompt medical intervention, and effective treatment strategies are pivotal in reducing mortality associated with respiratory disease syndemics. The BODE Index (Body mass index, airflow Obstruction, Dyspnoea, and Exercise capacity), which has been validated for assessing all-cause or respiratory mortality ( 26 ), holds promise in evaluating the prognosis of patients with respiratory comorbidities ( 25 ). Our commitment lies in providing active medical care and health management to reduce mortality, mitigate threats to life, and establish a safer and more sustainable healthcare environment for individuals affected by respiratory disease syndemics.
Management Principles
Recommendation 7: It is essential to consistently evaluate the health status and efficacy of treatment methods among populations affected by respiratory disease syndemics. This is important for early detection, optimizing treatment strategies, and effectively managing concurrent chronic non-communicable and communicable respiratory diseases.
Implementing routine health assessments within healthcare institutions is crucial for managing respiratory diseases at a population level ( 27 ). Clinical follow-up, systematic symptom assessments, and early detection of issues such as additional pulmonary diseases or heart failure necessitate adjustments in overall management strategies ( 28 ). The positive outcomes, including improved patient well-being and quality of life, underscore the efficacy of systematic health assessments. Integrating these principles into medical education emphasizes the indispensable role of regular health assessments in delivering comprehensive and patient-centered care. Additionally, considering the seasonality and climate sensitivity of respiratory diseases, particularly before peak seasons, conducting assessments for climate-sensitive respiratory diseases is essential. The escalating burden of chronic respiratory diseases emphasizes the need for innovative treatment approaches ( 29 ). Adapting treatment strategies in response to ongoing advancements ensures patients benefit from the latest medical knowledge ( 30 ). Given the complexity of patients contending with multiple chronic conditions, vigilant adjustments to treatment strategies accommodate the interaction and changes in these ailments over time ( 31 ). Periodic assessments address patient heterogeneity, leading to personalized medical services. Regular adjustments to treatment plans mitigate potential drug interactions, especially in cases of concurrent medication use. Close communication with patients, including feedback on experiences, symptoms, and quality of life, facilitates timely adjustments to treatment strategies, aligning with patient needs and expectations.
Recommendation 8: Surveillance plays a crucial role in the management of respiratory disease syndemics as it facilitates early detection and intervention.
Surveillance is essential for early detection, personalized intervention, and timely adjustments to treatment plans in the context of respiratory disease syndemics. It provides real-time prevalence data, contributing to better patient outcomes and overall public health ( 32 ). Genomic surveillance, such as the global INFORM-RSV study on Respiratory Syncytial Virus (RSV), is crucial for understanding RSV strain prevalence and genetic diversity across different countries ( 33 ). These genetic insights are important for early detection, understanding transmission dynamics, and evaluating vaccine and treatment effectiveness. Previous studies have underscored the often-overlooked aggregated impact of respiratory viruses, underlining the ongoing diversification of influenza variants as well as the critical need for surveillance of various respiratory viruses, at regional and international levels ( 34 ). Therefore, surveillance is fundamental in the management of respiratory disease syndemics as it facilitates early detection, tailored interventions, and prompt modifications to therapeutic strategies. This process is essential for gaining a critical understanding of the incidence and genetic variability of respiratory viruses.
Recommendation 9: Minimizing medication is a fundamental principle in the management of respiratory disease syndemics.
Optimizing patient care in respiratory disease syndemics requires a streamlined approach to medication management, considering the complexity of multi-morbidity and potential drug interactions ( 35 ). Inaccurate prescribing may occur due to the presence of comorbidities ( 36 ). As multi-morbidity becomes more prevalent with age, especially in the elderly population, simplifying medication regimens becomes crucial ( 37 ). Treatment burden, including multiple medication administration, negatively impacts health-related quality of life ( 38 ). Minimizing medication not only reduces treatment burden but also improves patient compliance, decreases the risk of adverse drug interactions, and enables a comprehensive and personalized approach to care. Emphasizing non-pharmacological interventions further contributes to better patient outcomes and quality of life. It is essential to regularly review medications to align with the current health status and optimize treatment strategies. Overall, a thoughtful and streamlined approach to medication management is pivotal in addressing the unique challenges posed by respiratory disease syndemics.
Recommendation 10: It is essential to establish an interdisciplinary team consisting of experts in infectious diseases, respiratory medicine, immunology, public health, and related fields. This team will play a critical role in the prevention, diagnosis, control, treatment, and rehabilitation of respiratory disease syndemics.
Interdisciplinary care has shown success in managing diseases such as diabetes despite barriers like hierarchical structures and financial constraints ( 39 ). Healthcare policies now prioritize interconnected factors to optimize patient outcomes, improve effectiveness, and reduce costs through integrated care delivery ( 40 ). The World Health Organization (WHO) emphasizes the importance of interdisciplinary teamwork in primary care as a key element in healthcare reform ( 41 ). Effective interdisciplinary teamwork relies on clear policies, explicit expectations, regular team meetings, open communication, and a dedicated focus on patient care ( 42 ). Smooth teamwork within interdisciplinary management teams is facilitated by clear divisions of labor, trust, mutual respect, and regular communication, whether face-to-face or electronic ( 43 ). In the comprehensive management of respiratory disease syndemics, establishing a thorough evaluation system is crucial for continuous improvement, adaptability, and improved patient outcomes.
Recommendation 11: Effective management of respiratory disease syndemics necessitates strong collaboration among hospitals, communities, families, and patients.
The collaboration between hospitals and the community has become increasingly important, particularly in light of the COVID-19 pandemic. Hospitals played crucial roles during the pandemic, conducting testing, monitoring, promoting workforce health, caring for the sick, and administering vaccines. This experience highlighted the vital connection between hospitals and community well-being. This connection extends beyond direct nursing care and is also an organizational characteristic. The strong ties between healthcare institutions at different levels and the community have positive effects on nursing personnel and patients within and beyond the hospital setting ( 44 ). Furthermore, involving families in decision-making for patients is considered crucial. Family members play significant roles in the decision-making process regarding patient care and other relevant matters ( 45 ). In summary, collaboration between hospitals, communities, families, and patients is crucial in managing respiratory disease syndemics.
Management Strategies
Recommendation 12: In the management of respiratory disease syndemics, it is essential to implement classification management based on the types of syndemics.
The classification management of respiratory disease syndemics follows the health management concept of “promotion, prevention, diagnosis, control, treatment, and rehabilitation.” It divides respiratory disease syndemics into three categories: co-infection of multiple acute respiratory infectious diseases, comorbidity of multiple chronic respiratory diseases, and chronic respiratory disease patients experiencing acute respiratory infections. This approach aims to comprehensively assess patients, determine their health and disease status, and tailor treatment strategies for more effective management. By emphasizing disease prevention, targeted interventions can be implemented. This classification management enables the medical team to accurately address patient needs, providing personalized and comprehensive services to control disease progression, improve prognosis, and promote overall health.
Recommendation 13: The management of co-infection of multiple acute respiratory infectious diseases should prioritize personalized treatment, disease transmission control, and disease prevention.
Patients require individualized treatment regimens that focus on medication and symptom management to control infection and support recovery. Disease control and prevention measures, such as essential quarantine, health monitoring, personal protection, and vaccination, are essential for minimizing transmission risks. Co-infection in respiratory infectious diseases, particularly during influenza pandemics, significantly burdens patients by worsening symptoms and impacting their quality of life ( 46 ). Managing co-infection should prioritize symptom improvement and individual preventive measures, taking into account the issue of antimicrobial resistance ( 47 ). It is crucial to practice rational drug use by avoiding unnecessary antibiotics and antivirals to prevent the development of antimicrobial resistance ( 48 ). Studies indicate that bacterial co-infection is rare among COVID-19 patients, reducing the need for empirical antibacterial treatment ( 49 ).
Improving symptoms requires a personalized medication regimen tailored to specific symptoms, taking into account the challenges posed by antimicrobial resistance and limited virus-targeting drugs ( 47 ). Disease surveillance and medical evaluation are essential for assessing disease prevalence and patient characteristics, which provide the foundation for implementing quarantine measures. Health monitoring, including regular testing, and epidemiological surveillance, play a pivotal role in controlling disease transmission ( 50 ). Adjusting treatment promptly based on monitoring conditions helps minimize the risk of transmission. For both individual patients and the population at large, personal protection measures such as wearing medical masks and N95 respirators, along with promoting vaccination, are critical for disease prevention ( 51 ). Vaccination is highly effective in preventing respiratory infectious diseases and their associated complications, including influenza and COVID-19 ( 52 ).
Recommendation 14: The management of comorbidity in patients with multiple chronic respiratory diseases should prioritize comprehensive pulmonary rehabilitation services and the prevention of infectious diseases.
Patients with multiple chronic respiratory diseases often experience severe symptoms that have a significant impact on their health. To address this, comprehensive care is needed ( 53 ). Integrated pulmonary rehabilitation services are crucial in managing both pulmonary and extrapulmonary aspects of comorbidity, leading to significant improvements in patients’ prognosis and quality of life ( 54 ). It is important to implement preventive measures such as personal protection and vaccination, considering the heightened vulnerability of these patients to respiratory pathogens ( 55 ). Pulmonary rehabilitation involves thorough assessments, personalized exercise programs, and education focused on self-management and health-promoting behavior change ( 54 ). This hospital-based approach, supported by an interdisciplinary team, ensures optimal outcomes for patients with multiple chronic respiratory diseases ( 56 ). The integration of pulmonary rehabilitation services with preventive measures is vital in effectively managing comorbidity and enhancing overall patient health.
Recommendation 15: The management of acute respiratory infections in patients with chronic respiratory diseases should prioritize infection control, prevention of disease worsening, mortality, and new infections. Additionally, comprehensive rehabilitation services should be provided to these patients.
Patients with chronic respiratory diseases are at a higher risk of developing acute respiratory infections, including bacterial and viral pathogens such as COVID-19. This increases the severity of their existing respiratory conditions ( 55 ). To address this vulnerability, it is crucial to prioritize infection control, prevention of exacerbations, and integrated rehabilitation services ( 57 ). Control measures should include rational drug use, health monitoring, personal protection, and vaccination. Symptom-oriented medication, including the use of antimicrobials when necessary, helps with timely infection control. Close health monitoring allows for prompt treatment adjustments. Personal protective measures, such as wearing masks, reduce the spread of infections and the susceptibility to new pathogens ( 58 ). Immunization plays a critical role in preventing new infections and associated complications, reducing the risks of severe illness and mortality. Additionally, timely integrated pulmonary rehabilitation services are recommended to improve the health status, quality of life, and mental well-being of patients. These comprehensive measures aim to alleviate symptoms, minimize disease severity and mortality risks, prevent new infections, and provide holistic health protection.
In conclusion, research on the management of respiratory disease syndemics is still in its preliminary stages, encountering challenges in practical application and inadequate research efforts. The establishment of this consensus is anticipated to act as a catalyst, fostering wider advocacy and practical implementation of concepts and methods for managing respiratory disease syndemics.
No conflicts of interest.
Qiao Liu and Shimo Zhang.
No.155 Changbai Road, Changping District, Beijing 102206, China
Tel:+86-10-63150701 Fax:+86-10-58900240 -->
Supported by: Beijing Renhe Information Technology Co., Ltd.
Export File

A Patient’s Guide to Respiratory Disease
Learn about the symptoms, causes and treatment options in the respiratory disease condition guide at U.S. News and World Report.
This article is based on reporting that features expert sources.
Most people take effortless breathing for granted. When your lungs are healthy , they expand easily into your chest cavity as you inhale, taking in vital oxygen for your blood to deliver throughout your body. With each exhalation, your lungs deflate and release carbon dioxide, a respiratory waste product.
When you run to catch the bus or climb a steep flight of stairs, your breathing naturally adapts to meet the extra demand on your heart and lungs. You may feel slightly out of breath – but not actually short of breath – because healthy lungs have a breathing reserve (extra air volume you can use after a normal exhalation). On the other hand, shortness of breath, also called dyspnea, is a condition characterized by a feeling of extreme tightness in the chest, difficulty breathing and "air hunger" and is a hallmark sign of respiratory disease.
The lower respiratory system includes the windpipe (trachea), which separates into a pair of bronchial tubes. Within each lung, the bronchial tubes divide into multiple smaller branches called bronchioles. Stemming from these narrowing branches are small air sacs, called alveoli. Tiny blood vessels, called capillaries, surround the alveoli. These capillaries let oxygen and carbon dioxide pass back and forth between the lungs and bloodstream.
The respiratory system serves several functions, including delivery of oxygen to the blood, removal of carbon dioxide by exhalation and protecting the body from harmful substances and irritants.
Read More About Respiratory Disease

8 Surprising Facts About Asthma and Seasonal Allergies

Your Guide to Asthma Inhalers

Can Young People Get COPD?

Best Breathing Exercises for Asthma

What Are the Best Strategies for Living With COPD?

A Patient’s Guide to Pulmonary Fibrosis
Various respiratory conditions, including chronic and infectious conditions, can hinder your ability to breathe. Diseases that affect the lungs include cancer, pneumonia and other inflammatory diseases. Chronic lung diseases fall into one of two main classes: obstructive or restrictive.
People with weakened lungs and immune systems are more vulnerable to infectious respiratory conditions. Some individuals have multiple lung conditions.
Obstructive Conditions
Obstructive lung diseases lead to blocked or narrowed airways, making it difficult for the lungs to exhale and exchange air.
Chronic obstructive pulmonary disease (COPD)
Chronic obstructive pulmonary disease (COPD) makes airways and air sacs less elastic, inflames the airway walls and clogs the lungs with excess mucus. It encompasses emphysema , a condition in which the tiny air sacs of the lungs are damaged, and chronic bronchitis , which involves inflammation of the air sacs and excessive mucus production in the lungs.
In the U.S., about 16 million adults are diagnosed with COPD annually, according to the Centers for Disease Control and Prevention. COPD is the sixth leading cause of death in the country.
"COPD is a horrible disease," says Dr. Kyle Hogarth, professor of medicine and co-director of the Lung Cancer Screening Program at University of Chicago Medical Center . "It slowly robs you of your breath and your activity." He notes that it is the third leading cause of death worldwide.
However, COPD is preventable and treatable. COPD death rates have decreased significantly for men but only slightly for women. For people with COPD over the age of 25, the death rate for men declined by 22.5% from 2000 to 2014. However, the death rate for women only declined by roughly 4% during that period.
Alpha-1 antitrypsin deficiency (AATD)
Alpha-1 antitrypsin deficiency (AATD) is a genetic condition that puts people at risk for lung and liver disease. Alpha-1 antitrypsin is a protein produced by the body to protect various organs from damage caused by the body's own immune system. AATD is not an uncommon disease, says Dr. Brooks Kuhn, assistant professor of medicine and co-director of the Comprehensive COPD Clinic at UC Davis Health in Sacramento, California.
"The sad reality is we have only identified probably a very small fraction of patients with alpha-1 antitrypsin deficiency," says Kuhn, who also serves as the director of the UC Davis Comprehensive COPD Clinic and director of the Alpha-1 Foundation designated Clinical Resource Center. "We probably have about 12,000 or so identified currently."
Although it can lead to COPD, AATD requires a different specialized type of treatment.
Asthma , also called reactive airway disease, involves inflammation of the airways, usually in response to triggers, such as pollen or dust, cold weather, stress or chemical fumes. More than 25 million people in the U.S. have asthma, according to the CDC .
There are different types of asthma, including allergic, non-allergic, occupational and cough-variant asthma (asthma that presents with cough), says Dr. Luis Javier Peña-Hernández, a lung health specialist at the Pulmonary, Critical Care & Sleep Disorders Institute of South Florida in Palm Beach, Florida.
Bronchiectasis
Bronchiectasis causes abnormal widening of the airways, making it difficult to rid the lower airways of mucus and phlegm, which raises the risk of infection.
Cystic fibrosis
Cystic fibrosis is a genetic condition that causes mucus in organs, including the lungs, to become thick and sticky. Respiratory complications include infections, inflammation and respiratory failure.
Restrictive Conditions
Restrictive lung disease reduces the volume of air that the lungs can hold. Lungs can lose their elasticity or the ability to expand.
Pulmonary fibrosis
Pulmonary fibrosis scars and stiffens lung tissue, restricting lung movement and function. It is a type of interstitial lung disease, the umbrella term for more than 200 disorders that cause progressive and usually irreversible scarring, called fibrosis, of the lungs.
"That causes the volume of the lungs to get smaller and smaller," says Dr. Jared Chiarchiaro, clinical chief for pulmonary and critical care medicine at Oregon Health & Science University in Portland, Oregon.
The most common type of pulmonary fibrosis is called idiopathic pulmonary fibrosis (IPF), a condition in which the cause is unknown, rather than being a complication of another condition. Overall, about 250,000 people in the U.S. live with pulmonary fibrosis, according to an estimate by the Pulmonary Fibrosis Foundation.
Sarcoidosis
Sarcoidosis is a rare condition that can arise in different parts of the body. Sarcoidosis involves the growth of tiny inflammatory cells that may affect a number of organs, most often the lungs.
Lung cancer
Lung cancer affects the lungs in multiple ways. Tumors may block airways, or fluid can collect around either lung, making expansion difficult. Lung cancer can also cause inflammation in the respiratory system.
Infectious Conditions
Infectious lung conditions are usually temporary, although some respiratory infections can become chronic or frequently recur.
Pneumonia is a lung infection most commonly caused by bacteria or viruses. People with chronic respiratory conditions, like COPD, are more vulnerable to developing pneumonia .
Tuberculosis
Tuberculosis is a bacterial infection that affects the lungs and other parts of the body. TB can be latent for many years.
Certain factors are known to contribute to respiratory disease.
- Smoking : Smoking is a leading cause of lung cancer and COPD, and it can worsen asthma and trigger attacks. Secondhand smoke increases asthma attacks and upper respiratory infections in children and adults alike.
- Environmental: Air pollution and environmental triggers like pollen contribute to asthma risk and flares .
- Autoimmune conditions : Certain immune-compromising conditions, like scleroderma and rheumatoid arthritis , can lead to pulmonary fibrosis. Scleroderma involves hardening of the skin and connective tissue. Rheumatoid arthritis affects the joints and sometimes other parts of the body.
- Genetic: Cystic fibrosis and AATD are caused by inherited genetic defects.
Pediatric Respiratory Conditions
Croup (laryngotracheobronchitis) is a respiratory infection that generally occurs in young children less than 5 years of age, usually around age 2, says Dr. Michael D. Cabana, physician-in-chief at the Children's Hospital at Montefiore in New York City. Viruses that may cause common cold symptoms in an adult or older child can also cause some mild swelling in the airways in young children. Because kids have smaller airways, this can cause a high-pitched inspiratory sound, called stridor, or a " barking cough ," like the sound a seal makes, Cabana says.
Typically, doctors tend to diagnose this condition during colder weather by conducting an exam of the child that includes listening to their chest with a stethoscope. Chest radiographs can also be helpful in diagnosis. If you are concerned about your child’s breathing, contact your physician. Chest radiographs (X-rays) can sometimes be helpful for the diagnosis.
Treatment may consist of corticosteroids or epinephrine.
Respiratory syncytial virus (RSV)
One of the most common respiratory conditions that affects children is respiratory syncytial virus (RSV), which infects the lungs and breathing passages. In the U.S., virtually all children have been infected with RSV by age 2, according to the National Institute of Allergy Infectious Diseases. RSV is the most common cause of bronchiolitis , which is inflammation of the small airways in the lungs in children younger than 1 year old. Annually, it causes about 58,000 hospitalizations among children under age 5.
RSV frequently causes illness in children, typically in the late fall and winter, says Dr. Joanne M. Nazif, attending physician at Children's Hospital at Montefiore in New York City. While RSV usually causes common cold symptoms in older children, infants and toddlers younger than 2 may experience more severe respiratory symptoms due to their smaller airways.
These symptoms may include:
- Fast breathing.
- The use of extra muscles during breathing, such as those of the abdomen and between the ribs.
Parents should seek medical attention if they notice any of these symptoms in their child.
Doctors typically diagnose RSV based on its usual signs and symptoms. Rapid testing by nasal swab can be performed if confirmation is needed.
Treatment consists of supportive measures, such as clearing the nasal passages using saline drops and suctioning, as well as ensuring adequate hydration . If the infection is severe, hospitalization for additional therapies may be needed. While medications are not typically used to treat RSV, very premature infants can receive prophylaxis with antibodies to prevent severe illness.
The worldwide COVID-19 pandemic broke out in early 2020. As of April 12, 2023, more than 104 million cases of COVID-19 have been reported in the U.S., according to the CDC . Many people infected with COVID-19 have suffered respiratory distress, ranging from mild to severe.
When SARS-CoV-2, the virus that causes COVID-19, gets into your body, it comes into contact with mucous membranes that line your nose, mouth and eyes. It uses the healthy cells it comes into contact with to make more copies of the virus, explains David Souleles, director of the COVID-19 response team and the Master's in Public Health program at the University of California, Irvine. The virus can then travel down through your respiratory system into your lungs infecting additional cells which can lead to inflammation in the lungs, and COVID-19 respiratory related symptoms. In more severe cases, the lungs may fill with fluid.
COVID-19 is particularly concerning to people with asthma.
Common COVID-19 respiratory symptoms can include:
- Congestion.
- Difficulty breathing.
- Runny nose.
In more severe cases, a person may experience COVID-19 pneumonia , bronchitis and – in very acute instances – acute respiratory distress syndrome (ARDS), a condition in which patients are often unable to breath on their own and may require a ventilator to help them breathe.
"We saw these more severe symptoms more frequently in the early days of COVID-19 before the widespread availability of vaccines and treatments , which can help to both prevent infection and reduce the severity of illness if you do become infected," Souleles says.
A COVID-19 test is the best way to determine if you are infected. PCR tests performed in a laboratory may be available from your provider or local clinics. COVID-19 home antigen tests are also a good test to use to determine if you have COVID-19 and are widely available and only take about 15 minutes to get results.
If you are diagnosed with COVID-19 and are experiencing more severe respiratory symptoms, your health care provider may order additional tests, including chest X-rays, to determine the severity of your respiratory complications.
Individuals ages 50 and older and people with compromised immune systems are at greater risk of getting sick.
Having these underlying diseases also puts individuals at greater risk of severe disease:
- Chronic lung disease.
It's important to stay up to date with your COVID-19 vaccines, including boosters .
Antiviral treatments, such as Paxlovid and remdesivir, are available from your health care provider or local clinic by prescription . These medications can reduce your risk of severe symptoms, hospitalization and death. To be most effective, treatment should be started within days of developing symptoms.
Symptoms can vary by the type of respiratory condition, but some symptoms are common to several disorders.
- Shortness of breath with activity.
- Persistent cough .
- Wet cough with mucus (COPD, cystic fibrosis).
- Dry, unproductive cough (pulmonary fibrosis).
- Chest tightness.
- Rapid, shallow breathing.
- Hoarseness.
- Recurring respiratory infections.
A correct diagnosis is essential to treat respiratory disease promptly and appropriately. Diagnosis can be straightforward; however, misdiagnosis, under-diagnosis and delayed diagnosis can occur due to the complexity of the disease and overlapping symptoms.
In 2021, the Global Initiative for Chronic Obstructive Lung Disease updated its guidelines regarding diagnosis and treatment of respiratory disease.
Physicians typically diagnose COPD using a combination of spirometry and medical history, which includes risk factors like smoking, and occupational or environmental exposures. When assessing symptoms, it's important to consider other possible diagnoses, such as COVID-19, because symptoms may appear similar.
Spirometry is a noninvasive, readily available and objective measure of airflow limitation. Spirometry is required to make an official diagnosis of COPD. The new GOLD guidelines recommend the use of spirometry be limited just to patients who need urgent or essential testing for a diagnosis and/or to assess lung function for surgery and other procedures. Such testing carries the risk of a possible viral transmission.
The GOLD categories classify patients into four categories:
- GOLD 1 (mild).
- GOLD 2 (moderate).
- GOLD 3 (severe).
- GOLD 4 (very severe).
Physicians can use other tools and methods to approach various kinds of respiratory diseases:
- Chest X-ray: A chest X-ray can show evidence of lung conditions, such as COPD, cystic fibrosis and lung cancer.
- CT scan: A chest CT scan can help doctors identify a pattern of fibrosis in the lungs. One particular pattern is very typical of idiopathic pulmonary fibrosis.
- Pulmonary function tests: These tests measure your lung volume and capacity, airflow rates and gas exchange. PFTs can be done in two ways. Spirometry is a diagnostic test that uses a device called a spirometer with a mouthpiece connected to a small machine. With plethysmography, you enter an airtight, booth-like chamber to perform the breathing test.
- Bronchial provocation/methacholine challenge PFT: For asthma, standard PFTs may not be enough. Someone with asthma may have normal lung sounds and test results because they are being tested when they feel fine, not in the middle of an attack. Specialized PFTs use an aerosolized drug, called methacholine, to irritate or challenge the lungs and measure a decrease in lung function that occurs in those with asthma.
- Pulse oximetry: This quick, noninvasive test uses a small device called a pulse oximeter. This device shines pulsating light through your finger to measure the oxygen level of your blood. A normal reading is about 90% or above.
- Arterial blood gas: An ABG is a more invasive, but more accurate test to determine oxygen, carbon dioxide and other respiratory-related measurements using a blood sample taken from your artery.
- Alpha-1 antitrypsin blood test: Decreased levels of ATT in the blood can identify alpha-1 antitrypsin deficiency. Any patient with evidence of COPD should be tested.
- Bronchoscopy: This test uses a bronchoscope, a flexible tube with a fiber-optic system that connects to a video camera, to help diagnose some lung disorders.
- Lung cancer screening: If you're a heavy smoker or former heavy smoker age 50 or older, you may be a candidate for lung cancer screening , which involves a yearly, low-dose CT scan to detect and treat lung cancer in its early stages. This has shown to reduce mortality from the disease.
Depending on your respiratory condition, medications can include an assortment of inhalers, oral drugs and intravenous treatments. Your doctor should explain why specific medications are prescribed, and their potential benefits and side effects. Some examples include:
Inhalers and nebulizers are key components of asthma treatment. Long-term asthma control medications include inhaled corticosteroids (ICS), leukotriene modulators (like montelukast) that decrease inflammation and prevent asthma symptoms. Beta agonists, or LABAs, that relax airway muscles (like Serevent). Combination inhalers include both a LABA and corticosteroid. LABA are contraindicated to be used alone and should be used in combination with ICS. Quick relief or rescue asthma medications provide rapid, short-term symptom relief during asthma flares. Albuterol and Atrovent are types of inhaled rescue drugs. Oral and IV steroids may be prescribed on a short-term basis to treat severe asthma symptoms.
A wide range of inhalers, nebulizers, oral medications and injections are used to treat COPD, depending on severity and symptoms. Clinicians use the GOLD guidelines, to prescribe COPD medications.
Idiopathic pulmonary fibrosis
Two oral medications are currently approved by the Food and Drug Administration to treat idiopathic pulmonary fibrosis: pirfenidone (Esbriet) and nintedanib (Ofev).
Alpha-1 antitrypsin deficiency
Augmentation therapy, also referred to as replacement therapy, is used to treat people with AATD by using alpha-1 antitrypsin protein from healthy donors to increase AAT levels in patients. It consists of a weekly IV infusion.
There's no cure for cystic fibrosis, but treatment may mitigate the symptoms.
Treatments for cystic fibrosis include:
- Antibiotics to prevent and mitigate the effects of lung infections.
- Anti-inflammatory medications to lessen inflammation in the airways of the lungs.
- Inhaled medications , known as bronchodilators, can relax muscles around the bronchial tubes, which helps keep airways open.
- Targeted therapy is a type of medication that targets gene mutations. One medication combines three drugs to treat the most common genetic mutation that causes cystic fibrosis.
- Oral pancreatic enzymes , which assist the digestive tract absorb nutrients.
Other options for cystic fibrosis treatment include:
- Lung transplant can be an option in severe cases. It may be a treatment for individuals with life-threatening lung complications, severe breathing issues and end-stage lung disease.
- Sinus and nasal surgery may help remove nasal polyps that interfere with breathing. Sinus surgery may help treat chronic or recurrent surgery.
- Oxygen therapy may be recommended if your oxygen level declines. Your health care provider may suggest that you breathe air with additional oxygen to help oxygenation and assist with breathing. Some patients in end-stage lung disease may need noninvasive ventilation with or without oxygen.
Advanced Procedures
- Interventional bronchoscopy uses a bronchoscope to allow minimally invasive treatment for respiratory conditions, such as severe asthma and emphysema, and to treat lung tumors.
- Lung transplant is an option for some patients with severe, progressive conditions. Without therapies to reverse idiopathic pulmonary fibrosis, which can progress rapidly and unexpectedly, patients should be evaluated for a possible lung transplant as early as possible.
Stem Cell Caution
There is growing interest in stem cell therapy to treat respiratory conditions. However, there is not enough evidence to support this form of therapy.
"We get a lot of questions about stem cells, for IPF in particular," Chiarchiaro says. "We generally recommend against it outside of a clinical research study."
Although researchers are continuing to investigate stem cell therapy, insurance will not cover these types of interventions because they have not been supported by evidence.
Self-Management
Over the long term, you can take steps to stay on top of respiratory conditions and reduce their impact on your day-to-day life. For example, quitting smoking is an essential lifestyle change for those with lung disease who still smoke. In some cases, disease progression can lead to unavoidable lifestyle changes.
Patient education, digital technology and asthma action plans can improve asthma control and quality of life.
If you're diagnosed with asthma, there's a lot to learn. Education on how to take medications, the difference between rescue and control medications, how to use medication spacers and respiratory peak flow meters and avoiding environmental triggers are essential.
Having a personalized asthma action plan in place can help control your asthma and prevent attacks. An asthma action plan outlines your known environmental triggers, instructions for the prescribed controller and rescue medications, when to use them and potential side effects, medication use around exercise, and when to call your health care provider or go immediately to the emergency room. You can download asthma action plan forms from the CDC website.
Smartphone apps can improve asthma self-management, medication reminders and other resources.
Health Care Providers
Your treatment team may include the following clinicians:
- Pulmonologist .
- Allergist .
- Oncologist .
- Rheumatologist .
- Ear, nose and throat specialist.
- Patient educator.
- Primary care physician.
- Nurse practitioner.
- Pulmonary care nurse.
- Respiratory therapist.
If you have COPD, ongoing support can help you manage better at home and avoid a cycle of frequent disease exacerbations and hospital readmissions.
The UC Davis Reversible Obstructive Airway Disease Program, like similar COPD programs, takes a multidisciplinary approach to individualizing treatment, educating patients and following up with calls after discharge to help with the transition to home. Having a landing spot for patients when they leave the hospital and getting them into the clinic early when symptoms arise can help people with COPD stay out of the hospital, Kuhn says.
For any chronic respiratory condition, joining an online or in-person support group lets you meet peers and share information and resources. Medical centers that focus on less-common conditions can connect you with related support groups.
Related Articles
Patient Advice
What Are the Symptoms of RSV in Adults?
Learn about the respiratory syncytial virus in adults, including its causes, common symptoms and available treatment options.
Christine Comizio June 15, 2023

Is It Safe to Take Allergy Medicine While Pregnant?
Some allergy medicines are generally considered safe during pregnancy. Learn which.
Ruben Castaneda and Michael O. Schroeder May 2, 2022

What Is Coronavirus Pneumonia?
This dangerous lung infection has new features and treatments with COVID-19.
Elaine K. Howley and Lisa Esposito April 28, 2022

What Are the Symptoms of Omicron?
Although upper respiratory symptoms are more common, COVID-19 cases aren't always mild.
Lisa Esposito Jan. 19, 2022

How to Wear a Face Mask Safely and Comfortably in Summer
Yes, it’s hot, sticky and uncomfortable. But wearing a mask is critical to fighting COVID-19.
David Levine July 8, 2020

The U.S. News Health team delivers accurate information about health, nutrition and fitness, as well as in-depth medical condition guides. All of our stories rely on multiple, independent sources and experts in the field, such as medical doctors and licensed nutritionists. To learn more about how we keep our content accurate and trustworthy, read our editorial guidelines .
Cabana is physician-in-chief at the Children's Hospital at Montefiore in New York City
Chiarchiaro is clinical chief for pulmonary and critical care medicine at Oregon Health & Science University in Portland, Oregon.
Nazif is ending physician, Division of Hospital Medicine at Children's Hospital at Montefiore in New York City.
Peña-Hernández a lung health specialist at the Pulmonary, Critical Care & Sleep Disorders Institute of South Florida in Palm Beach, Florida.
Souleles is director of the COVID-19 response team and the Master's in Public Health program at the University of California, Irvine.
health disclaimer »
Disclaimer and a note about your health ».
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Signs and Symptoms
- How It Spreads
- About Non-Polio Enteroviruses
About Hand, Foot, and Mouth Disease
- Hand, foot, and mouth disease (HFMD) is common in children under 5 years old, but anyone can get it.
- The illness is usually not serious, but it is very contagious.
- To prevent spreading HFMD, wash your hands often, clean and disinfect surfaces, and avoid close contact with others.

HFMD is a common illness that usually causes fever, mouth sores, and skin rash. It can spread quickly at schools and day care centers. Most people get better on their own in 7 to 10 days.
Signs and symptoms
Most children have mild symptoms for 7 to 10 days. Symptoms may include:
- Sore throat
- Painful mouth sores that blister
- Rash commonly found on the hands and feet
Complications from HFMD are rare.

Who is at risk
HFMD is most common in infants and children younger than 5 years old.
If you are pregnant, contact your doctor if you think you may have been exposed to HFMD. Complications from HFMD are rare. However, your own medical history and how far along you are in your pregnancy can affect the situation.
How it spreads
HFMD is caused by viruses. A person infected with one of these viruses is contagious. This means they can pass the virus easily to other people.
HFMD can spread through contact with:
- Droplets with virus particles made after person sneezes, coughs, or talks
- Objects and surfaces that have virus particles
- Fluid from blisters
HFMD is very contagious. To help prevent catching or spreading HFMD:
- Wash your hands often with soap and water for at least 20 seconds, especially after changing diapers, using the toilet, and coughing, sneezing, or blowing your nose.
- Help children wash their hands and keep blisters clean.
- Avoid touching your face with unwashed hands, especially your eyes, nose, and mouth.
- Clean and disinfect frequently touched surfaces and shared items, including toys and doorknobs.
- Avoid close contact with an infected person, such as hugging or kissing them
There is no vaccine in the United States to protect against the viruses that cause HFMD.

Treatment and recovery
HFMD is usually not serious. Most people get better on their own in 7 to 10 days with minimal or no medical treatment. You can take steps to manage symptoms while you or your child are sick.
Manage symptoms at home
Relieve pain and fever. Take over-the-counter medications to relieve fever and pain caused by mouth sores. Never give aspirin to children.
Prevent dehydration (loss of fluids). You can take steps to relieve symptoms and prevent dehydration while you or your child are sick. Drink enough liquids. Mouth sores can make it painful to swallow, so your child may not want to drink much. Make sure they drink enough to stay hydrated.
When to return to school
Because HFMD is normally mild, children can continue to go to child care and schools as long as they:
- Have no fever.
- Feel well enough to participate in class.
- Have no uncontrolled drooling with mouth sores.
Talk with your child’s healthcare provider if you are still not sure when it is okay for them to return. Sometimes, the local health department may require children with HFMD to stay home to control an outbreak.
- When and How to Wash Your Hands
- Hand Hygiene in Healthcare Settings
- A Guide to Clinical Management for HFMD | WHO
Hand, Foot, and Mouth Disease (HFMD)
HFMD is very contagious and usually causes fever, mouth sores, and skin rash. It is common in children under 5 years old, but anyone can get it.

IMAGES
VIDEO
COMMENTS
Therefore, all nations should come together to conduct research, make efforts to prevent the spread of these diseases, and develop appropriate treatments and vaccines. From the Spanish flu to the severe acute respiratory syndrome, Middle East respiratory syndrome, and COVID-19, the unmasking of the virus responsible for these epidemics stands ...
Of 38,353 persons interviewed, 595 were found to have undiagnosed COPD or asthma and 508 underwent randomization: 253 were assigned to the intervention group and 255 to the usual-care group.
Respiratory tract diseases are illnesses that affect components of the respiratory system, including the nasal passages, the bronchi and the lungs. They range from acute infections, such as ...
Background: In response to the COVID-19 pandemic, new evidence-based strategies have emerged for reducing transmission of respiratory infections through management of indoor air. Objectives: This paper reviews critical advances that could reduce the burden of disease from inhaled pathogens and describes challenges in their implementation. Discussion: Proven strategies include assuring ...
Recently, significant innovations in the diagnosis and management of respiratory diseases have been developed [1,2,3,4].All aspects of respiratory medicine have seen significant progress in increasing the innovation and precision and reducing the invasiveness of all instruments and technologies used in the diagnosis and management of pulmonary diseases [1,2,3,4].
In The Lancet Respiratory Medicine, Eric Lim and colleagues 1 present results of the MARS 2 trial, which sought to answer the question of whether (extended) pleurectomy decortication has an effect on survival and quality of life of patients with resectable pleural mesothelioma. The principal evidence for surgery before the MARS 2 trial was retrospective case series, and no controlled trials ...
Research funding for these five respiratory infectious diseases increased to US$58,969 million and US$1093,769 million in 2020-2021, from the NSF and NIH, respectively.
Therapeutic Advances in Respiratory Disease is a peer-reviewed open access journal which focuses on pioneering efforts and innovative studies across all areas of respiratory disease. View full journal description. This journal is a member of the Committee on Publication Ethics (COPE).
Despite decades of advances in clinical management protocols and new antibiotics, pneumonia continues to be a leading cause of morbidity and mortality worldwide. The 2019 Global Burden of Disease Study indicated that lower respiratory infections, including pneumonia, were the fourth leading cause of disability-adjusted life-years across all ages.1 People at the extremes of age, specifically ...
These lead to local lung diseases, such as tracheitis, chronic obstructive pulmonary disease (COPD), acute lung injury/acute respiratory distress syndrome (ALI/ARDS), and pneumonia. These respiratory injuries and diseases can lead to life-threatening conditions, hospitalization, and high mortality, [ 8 ] which cause healthcare, economic, and ...
Chronic obstructive pulmonary disease (COPD) is a disease of the respiratory tract that is characterized narrowing of the small airways and destruction of lung tissue. This leads to poor airflow ...
University of Minnesota. "Study provides new insights into deadly acute respiratory distress syndrome (ARDS)." ScienceDaily. ScienceDaily, 12 March 2024. <www.sciencedaily.com / releases / 2024 ...
E-health includes a wide range of subdomains, such as wearables, smart-inhalers, portable electronic spirometers, digital stethoscopes, and clinical decision support systems. E-health has been consistently shown to enhance the quality of care, improve adherence to therapy, and allow early detection of worsening in chronic pulmonary diseases.
The Forum of International Respiratory Society has identified acute lower respiratory infections, chronic obstructive pulmonary diseases (COPDs), asthma, tuberculosis (TB) and lung cancer as the big five RDs that mainly contribute to the increased global burden (Wisnivesky and De-Torres 2019).To focus on the needs of respiratory disease patients in poor and middle-income countries, the WHO ...
This work is supported by the Singapore Ministry of Health's National Medical Research Council under the Clinician-Scientist Individual Research Grant MOH-001356 (S.H.C.) and a Clinician-Scientist Award MOH-000710 (S.H.C) and Transition Award MOH- 001275-00 (P.Y.T) and the Singapore Ministry of Education under its AcRF Tier 1 Grant (RT1/22 ...
COPD is the third-leading cause of death worldwide, killing 3.2 million individuals every year and accounting for an astounding 81.7% of the total number of deaths from chronic respiratory disease. Pneumonia is a leading cause of death among children < 5 years old outside the neonatal period and in adults > 65 years old.
Pulmonology is a medical discipline concerned with a number of respiratory diseases also known as "respiratory medicine" or "chest medicine." ... thereby making their management very hard ... Ariani A, Sverzellati N (2018) Pulmonary quantitative CT imaging in focal and diffuse disease: current research and clinical applications. Br J ...
A randomised controlled experimental study was conducted in 220 patients with a medical diagnosis of COVID-19 and more than 5 months of evolution, dyspnoea or perceived fatigue, including olfactory and gustatory perception problems, of whom 200 patients completed the study. 100 patients were randomly assigned to the intervention group, consisting of an inspiratory training treatment plan ...
HTML; The global burden of respiratory diseases is a significant and increasing threat to individuals worldwide. In 2017, there were 544.9 million cases of chronic respiratory diseases, a 39.8% increase since 1990 ().These diseases were the third leading cause of global mortality in 2017, accounting for 7.0% of all deaths, an 18.0% increase compared to 1990.
Congestion. Difficulty breathing. Runny nose. In more severe cases, a person may experience COVID-19 pneumonia, bronchitis and - in very acute instances - acute respiratory distress syndrome ...
Washing your hands is easy, and it's one of the most effective ways to prevent the spread of germs. Follow these five steps every time. Wet your hands with clean, running water (warm or cold), turn off the tap, and apply soap. Lather your hands by rubbing them together with the soap. Lather the backs of your hands, between your fingers, and ...
Prevention. HFMD is very contagious. To help prevent catching or spreading HFMD: Wash your hands often with soap and water for at least 20 seconds, especially after changing diapers, using the toilet, and coughing, sneezing, or blowing your nose.. Help children wash their hands and keep blisters clean.. Avoid touching your face with unwashed hands, especially your eyes, nose, and mouth.