
Quality Care
Publications, intimate partner violence and co-occurring substance abuse/addiction.substring(0, maxlength), intimate partner violence and co-occurring substance abuse/addiction.
Intimate partner violence (IPV) is a major public health concern. Recent national media attention has increased discussion regarding this significant health care issue.
Definition and Background
The Futures Without Violence Association (FWV) defines intimate partner violence (IPV) as “A pattern of assaultive and coercive behaviors that may include inflicted physical injury, psychological abuse, sexual assault, progressive social isolation, stalking, deprivation, intimidation and threats. These behaviors are perpetuated by someone who is, was, or wishes to be involved in an intimate or dating relationship with an adult or adolescent, and one aimed at establishing control by one partner over the other.”
Substance abuse has been found to co-occur in 40-60% of IPV incidents across various studies. Several lines of evidence suggest that substance use/abuse plays a facilitative role in IPV by precipitating or exacerbating violence. Some studies also suggest the benefit of interventions that focus on substance abuse/addiction in men who have histories of IPV.
Spousal abuse has been identified as a predictor of developing a substance abuse problem and/or addiction. Additionally, women in abusive relationships have often reported being coerced into using alcohol and/or drugs by their partners. Substance abuse and high-risk alcohol use/abuse are more prevalent among women who experience IPV compared to a cohort with no IPV experience. In a study of prenatal patients in North Carolina, victims of violence were significantly more likely to use multiple substances before and during pregnancy than those who had no experience of IPV ( American Journal of Public Health ). It is known that many episodes of IPV involve alcohol and/or illicit drug consumption. Research has found that on days of heavy drug and/or alcohol use, physical violence was 11 times more likely among IPV batterers and victims.
Greater than 20% of male perpetrators report using alcohol and/or illicit drugs prior to the most recent and severe acts of violence. Victims of IPV also report the offender had been consuming alcohol and/or using illicit drugs. Many studies find excessive alcohol use to be strongly associated with perpetrating partner violence, though there is debate as to whether heavy drinking causes men to be violent or whether it is used to excuse violent behavior.
The strong relationship between substance abuse and perpetration of IPV has been found in primary health care settings, family practice clinics, prenatal clinics, and rural health clinics. The incidence of IPV and relationship to substance abuse is frequently observed and reported among individuals presenting at psychiatric and substance abuse treatment settings.
The United States Bureau of Justice Statistics report on intimate violence found that 85% of victims are female.
Women are five to eight times more likely than men to be victimized by an intimate partner. Seventy-five percent of perpetrators are males. Of note, IPV also occurs in lesbian, gay, bisexual and transgender (LGBT) relationships.
There is a lack of much-needed research specific to IPV and the LGBT communities. In a recent survey of men in same-gender relationships, the lifetime prevalence of IPV was nearly 40%, with 22% of men reporting physical abuse in the past five years. Prevalence
According to Futures Without Violence , “On average, more than three women a day are murdered by their intimate partner in the United States,” and “Nearly one in four women in the United States report experiencing violence by a current or from a former spouse or boyfriend at some point in their life.” The most current data available from Centers for Disease Control and Prevention finds women experience over 2,000,000 injuries from intimate partner perpetrators. In the United States, the vast majority of nonfatal intimate partner victimizations of women (66%) occur in the home.
“15.5 million children in the US live in families in which partner violence occurred at least once in the past year,” ( Futures Without Violence ), and young women who were in shelters as children are now seeking protection from domestic violence situations themselves, according to the 2013 Mary Kay Truth about Abuse Survey.
Also of importance, nearly 50% of Native American women experience IPV in their life, the highest rate amongst US population groups. Health Consequences of IPV
“IPV is the leading cause of female homicides and injury-related deaths during pregnancy, and accounts for significant preventable injuries and ED visits by women,” ( Intimate Partner Violence and Healthy People 2010 Fact Sheet ). A 2002 study by the US Department of Justice found that most victims injured by an intimate partner did not report seeking professional medical treatment for their injuries.
Victims of IPV are at increased risk for suffering serious mental health problems; 56% of women who experience IPV are diagnosed with a psychiatric problem, and victims of IPV are more likely to use tobacco and marijuana. Several studies suggest a significant correlation between IPV, morbid obesity and disturbed eating behaviors. Victims of IPV are 70 percent more likely to drink alcohol heavily than the non-experienced IPV cohort. IPV is also linked to a variety of reproductive health issues.
The American College of Obstetrics and Gynecology Committee on Health Care for Underserved Women recommends with “clinical signs of depression, substance abuse, mental health problems, requests for repeat pregnancy tests when the patient does not wish to be pregnant, new or recurrent STIs, asking to be tested for an STI, or expressing fear when negotiating condom use with a partner” to assess the patient for IPV. Conclusions
Although intimate partner violence remains a public health concern, there have been advances in our basic understanding of how to treat perpetrators with co-occurring substance abuse and addiction. “For example, when substance use and IPV co-occur, research suggests that substance use plays a facilitative role in IPV by precipitating or exacerbating violence,” ( Psychiatric Times – The Role of Substance Abuse in Intimate Partner Violence ).
Hence, it is imperative to treat the substance abuse/addiction.
The United States is making progress in addressing this violence. Standard IPV interventions have shown to be ineffective, so referrals to substance abuse or mental health treatment are necessary ( Psychiatric Times – The Role of Substance Abuse in Intimate Partner Violence ).
Centers of higher educations are developing a stronger role in prevention as well, training students to intervene on behalf of one another and assist victims.
Addiction Medicine specialists can use therapeutic relationships with patients to: “identify intimate partner violence, make brief office interventions, offer continuity of care, and refer them for subspecialty and community-based evaluation, treatment, and advocacy,” ( American Family Physician - Intimate Partner Violence ).
Treat Addiction - Save Lives
References and Resources
Psychiatric Times – The Role of Substance Abuse in Intimate Partner Violence
American College of Obstetricians and Gynecologists – Intimate Partner Violence
American Psychological Association - Intimate Partner Violence Facts and Resources
US Dept. of Justice - Intimate Partner Violence, 1993-2010
American Journal of Public Health - Violence and Substance Abuse Among North Carolina Pregnant Women
Journal of Interpersonal Violence – Encouraging Responses in Sexual and Relationship Violence Prevention: What Program Effects Remain 1 Year Later?
Futures Without Violence
VetoViolence
Mary Kay Foundation
Office on Violence Against Women
Violence Prevention Evidence Database - World Health Organization
Hotlines National Domestic Violence Hotline: 1-800-799-SAFE (7233) Rape Abuse & Incest National Network (RAINN) Hotline: 1-800-656-HOPE (4673)
Additional Review Articles & Books Avery-Leaf, S., & Cascardi, M. (2002). Dating violence education: Prevention and early intervention strategies. In P. A. Schewe (Ed), Preventing violence in relationships: Interventions across the life span (pp.79-105). Washington, DC, US: American Psychological Association. Babcock, J. C., Green, C. E., & Robie, C. (2004). Does batterers' treatment work? A meta-analytic review of domestic violence treatment. Clinical Psychology Review, Jan;23(8):1023–1053. CDC Report on Intimate Partner and Sexual Violence in the U.S. Explores Victimization and Impact http://www.cdc.gov/violenceprevention/intimatepartnerviolence/ Foshee, V.A. & Reyes, H. L. M. (2009). Primary Prevention of Adolescent Dating Abuse Perpetration: When to Begin, Whom to Target, and How to Do It. In D. J. Whitaker and J. R. Lutzker’s Preventing partner violence: Research and evidence-based intervention strategies. Washington, DC: American Psychological Association, pp. 141–168. Hickman, L. J., Jaycox, L. H., & Aranoff, J. (2004) Dating violence among adolescents: Prevalence, gender distribution, and prevention program effectiveness. Trauma, Violence, and Abuse, 5, 123–142. Mitchell, C. & Anglin, D. (Eds.), (2009). Intimate partner violence: A health based perspective. New York: Oxford University Press. Nelson, H.E., Bougatsos, C., & Blazina, I. (2012). Screening women for intimate partner violence: A systematic review to update the 2004 U.S. Preventive Services Task Force recommendation. Annals of Internal Medicine, 156 (11), 796–808. Ruff, S., McComb, J.L., Coker, C.J., & Sprenkle, D.H. (2010). Behavioral Couples Therapy for the treatment of substance abuse: A substantive and methodological review of O’Farrell, Fals-Stewart, and colleagues’ program of research. Family Process, 49:439–456. Black, M.C., Basile, K.C., Breiding, M.J., Smith, S.G., Walters, M.L., Merrick, M.T., Chen, J., & Stevens, M.R. (2011). The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Whitaker DJ, Baker CK, & Arias I. (2007). Interventions to prevent intimate partner violence. In L. Doll, S. Bonzo, D. Sleet, J. Mercy & E. Hass (Eds.), Handbook of Injury and Violence Prevention (183–201).New York, NY: Springer. Whitaker, J.D. & Lutzker, J.R. (Eds.), (2009). Preventing partner violence: Research and evidence-based intervention strategies. Washington DC: American Psychological Association. Whitaker DJ., Morrison S., Lindquist CA., Hawkins SR, O'Neil JA, Nesius AM, Mathew A, Reese L. (2006) A critical review of interventions for the primary prevention of perpetration of partner violence.
Related Articles

ASAM applauds the election of Ilse R. Levin, DO, MPH & TM, FACP to the AMA Board of Trustees.
Aug 09 2021
ASAM and CARF Launch Transformative Residential Addiction Treatment Certification Nationwide
Amidst covid-19 crisis, asam releases updated national practice guideline for treating opioid use disorder, asam announces partnership with acog to provide waiver qualifying course on treatment for opioid use disorders, asam honors innovators and leaders in addiction medicine at the asam 51st annual conference, asam selects association strategies and tuft & associates to lead its ceo search.
ORIGINAL RESEARCH article
Exploring factors influencing domestic violence: a comprehensive study on intrafamily dynamics.

- 1 Departamento de Economía Cuantitativa, Facultad de Ciencias Escuela Politécnica Nacional, Quito, Ecuador
- 2 Institut de Recherche en Gestion et Economie, Université de Savoie Mont Blanc (IREGE/IAE Savoie Mont Blanc), Annecy, France
- 3 Department of Marketing, Universidad San Francisco de Quito USFQ, Quito, Ecuador
Introduction: This econometric analysis investigates the nexus between household factors and domestic violence. By considering diverse variables encompassing mood, depression, health consciousness, social media engagement, household chores, density, and religious affiliation, the study aims to comprehend the underlying dynamics influencing domestic violence.
Methods: Employing econometric techniques, this study examined a range of household-related variables for their potential associations with levels of violence within households. Data on mood, depression, health consciousness, social media usage, household chores, density, and religious affiliation were collected and subjected to rigorous statistical analysis.
Results: The findings of this study unveil notable relationships between the aforementioned variables and levels of violence within households. Positive mood emerges as a mitigating factor, displaying a negative correlation with violence. Conversely, depression positively correlates with violence, indicating an elevated propensity for conflict. Increased health consciousness is linked with diminished violence, while engagement with social media demonstrates a moderating influence. Reduction in the time allocated to household chores corresponds with lower violence levels. Household density, however, exhibits a positive association with violence. The effects of religious affiliation on violence manifest diversely, contingent upon household position and gender.
Discussion: The outcomes of this research offer critical insights for policymakers and practitioners working on formulating strategies for preventing and intervening in instances of domestic violence. The findings emphasize the importance of considering various household factors when designing effective interventions. Strategies to bolster positive mood, alleviate depression, encourage health consciousness, and regulate social media use could potentially contribute to reducing domestic violence. Additionally, the nuanced role of religious affiliation underscores the need for tailored approaches based on household dynamics, positioning, and gender.
1. Introduction
Intimate partner violence is a pervasive global issue, particularly affecting women. According to the World Health Organization ( 1 ), approximately 30% of women worldwide have experienced violence from their intimate partners. Disturbingly, recent studies indicate that circumstances such as the COVID-19 pandemic, which disrupt daily lives on a global scale, have exacerbated patterns of violence against women ( 2 – 4 ). Data from the WHO ( 1 ) regarding gender-based violence during the pandemic reveals that one in three women felt insecure within their homes due to family conflicts with their partners.
This pressing issue of intimate partner violence demands a thorough analysis from a social perspective. It is often insidious and challenging to identify, as cultural practices and the normalization of abusive behaviors, such as physical aggression and verbal abuse, persist across diverse socioeconomic backgrounds. However, all forms of violence can inflict physical and psychological harm on victims, affecting their overall well-being and interpersonal relationships WHO ( 5 ). Furthermore, households with a prevalence of domestic violence are more likely to experience child maltreatment ( 6 ).
In this context, the COVID-19 pandemic has had profound effects on individuals, families, and communities worldwide, creating a complex landscape of challenges and disruptions. Among the numerous repercussions, the pandemic has exposed and exacerbated issues of domestic violence within households. The confinement measures, economic strain, and heightened stress levels resulting from the pandemic have contributed to a volatile environment where violence can escalate. Understanding the factors that influence domestic violence during this unprecedented crisis is crucial for developing effective prevention and intervention strategies.
This article aims to explore the relationship between household factors and domestic violence within the context of the COVID-19 pandemic. By employing econometric analysis, we investigate how various factors such as mood, depression, health consciousness, social media usage, household chores, density, and religious affiliation relate to violence levels within households. These factors were selected based on their relevance to the unique circumstances and challenges presented by the pandemic.
The study builds upon existing research that has demonstrated the influence of individual and household characteristics on domestic violence. However, the specific context of the pandemic necessitates a deeper examination of these factors and their implications for violence within households. By focusing on variables that are particularly relevant in the crisis, we aim to provide a comprehensive understanding of the dynamics that contribute to intrafamily violence during the pandemic.
The findings of this study have important implications for policymakers, practitioners, and researchers involved in addressing domestic violence. By identifying the factors that either increase or mitigate violence within households, we can develop targeted interventions and support systems to effectively respond to the unique challenges posed by the pandemic. Furthermore, this research contributes to the broader literature on domestic violence by highlighting the distinct influence of household factors within the context of a global health crisis.
The structure of this paper is organized as follows. Section 2 provides a comprehensive review of the relevant literature on household violence. Section 3 presents the case study that forms the basis of this research. Section 4 outlines the methodology employed in the study. Section 5 presents the results obtained from the empirical analysis. Finally, Section 6 concludes the paper, summarizing the key findings and their implications for addressing domestic violence.
2. Literature review
2.1. violence at home.
Throughout human history, the family unit has been recognized as the fundamental building block of society. Families are comprised of individuals bound by blood or marriage, and they are ideally regarded as havens of love, care, affection, and personal growth, where individuals should feel secure and protected. Unfortunately, it is distressingly common to find alarming levels of violence, abuse, and aggression within the confines of the home ( 7 ).
Domestic violence, as defined by Tan and Haining ( 8 ), encompasses any form of violent behavior directed toward family members, regardless of their gender, resulting in physical, sexual, or psychological harm. It includes acts of threats, coercion, and the deprivation of liberty. This pervasive issue is recognized as a public health problem that affects all nations. It is important to distinguish between domestic violence (DV) and intimate partner violence (IPV), as they are related yet distinct phenomena. DV occurs within the family unit, affecting both parents and children. On the other hand, IPV refers to violent and controlling acts perpetrated by one partner against another, encompassing physical aggression (such as hitting, kicking, and beating), sexual, economic, verbal, or emotional harm ( 9 , 10 ). IPV can occur between partners who cohabit or not, and typically involves male partners exerting power and control over their female counterparts. However, it is crucial to acknowledge that there are cases where men are also victims of violence ( 11 ).
Both forms of violence, DV and IPV, take place within the home. However, when acts of violence occur in the presence of children, regardless of whether they directly experience physical harm or simply witness the violence, the consequences can be profoundly detrimental ( 12 , 13 ).
Understanding the intricacies and dynamics of domestic violence and its impact on individuals and families is of paramount importance. The consequences of such violence extend beyond the immediate victims, affecting the overall well-being and social fabric of society. Therefore, it is crucial to explore the various factors that contribute to domestic violence, including those specific to the current context of the COVID-19 pandemic, in order to inform effective prevention and intervention strategies. In the following sections, we will examine the empirical findings regarding household factors and their association with domestic violence, shedding light on the complexities and nuances of this pervasive issue.
2.2. Drivers of domestic violence
As previously discussed, the occurrence of violence within the home carries significant consequences for individuals’ lives. Consequently, gaining an understanding of the underlying factors that contribute to this violence is crucial. To this end, Table 1 provides a comprehensive summary of the most commonly identified determinants of domestic violence within the existing literature.
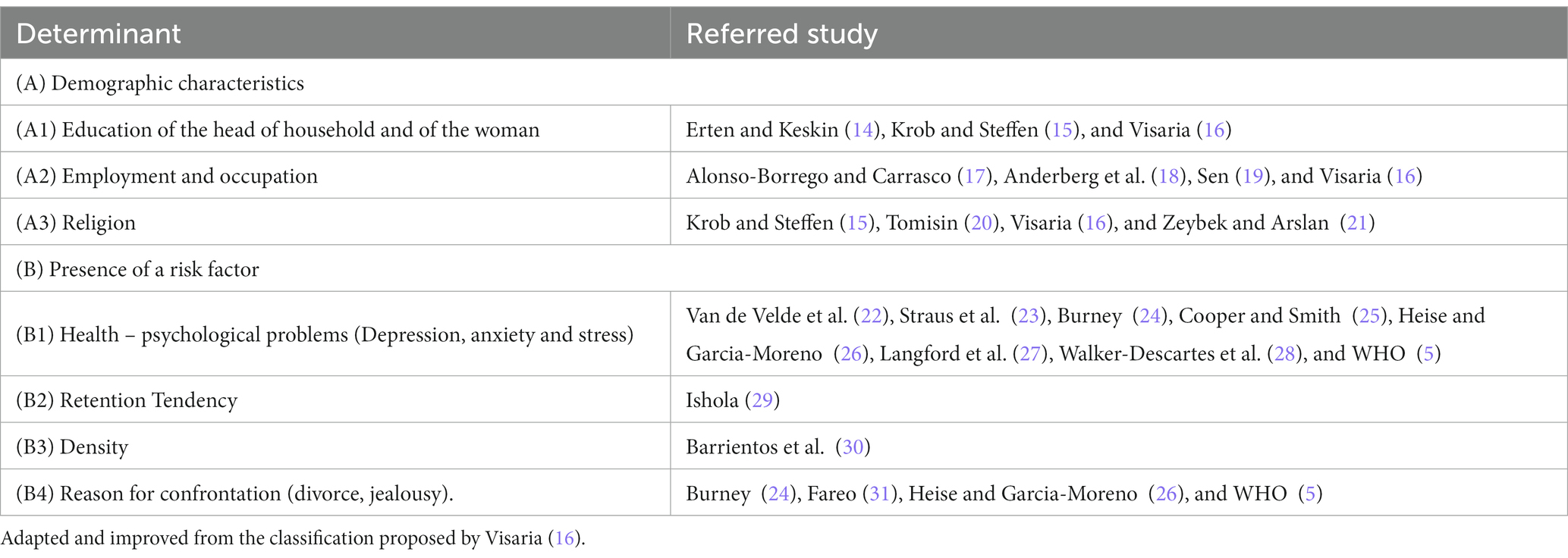
Table 1 . Determinants of domestic violence.
Identifying these determinants is a vital step toward comprehending the complex nature of domestic violence. By synthesizing the findings from numerous studies, Table 1 presents a consolidated overview of the factors that have been consistently associated with domestic violence. This compilation serves as a valuable resource for researchers, practitioners, and policymakers seeking to address and mitigate the prevalence of domestic violence.
The determinants presented in Table 1 encompass various variables, including socio-economic factors, mental health indicators, interpersonal dynamics, and other relevant aspects. By examining and analyzing these determinants, researchers have made significant progress in uncovering the underlying causes and risk factors associated with domestic violence.
It is important to note that the determinants listed in Table 1 represent recurring themes in the literature and are not an exhaustive representation of all potential factors influencing domestic violence. The complex nature of this issue necessitates ongoing research and exploration to deepen our understanding of the multifaceted dynamics at play. Thus, we categorize these factors into two groups to provide a comprehensive understanding of the issue.
Group A focuses on variables that characterize both the victim and the aggressor, which may act as potential deterrents against femicide. Previous research by Alonso-Borrego and Carrasco ( 17 ), Anderberg et al. ( 18 ), Sen ( 19 ), and Visaria ( 16 ) has highlighted the significance of factors such as age, level of education, employment status, occupation, and religious affiliation. These individual characteristics play a role in shaping the dynamics of domestic violence and can influence the likelihood of its occurrence.
Group B aims to capture risk factors that contribute to the presence of violence within the home. One prominent risk factor is overcrowding, which can lead to psychological, social, and economic problems within the family, ultimately affecting the health of its members. Research by Van de Velde et al. ( 21 ), Walker-Descartes et al. ( 23 ), Malik and Naeem ( 2 ) supports the notion that individuals experiencing such distress may resort to exerting force or violence on other family members as a means of releasing their frustration. Additionally, Goodman ( 32 ) have highlighted the increased risk of violence in households with multiple occupants, particularly in cases where individuals are confined to a single bedroom. These concepts can be further explored through variables related to health, depression, anxiety, and stress, providing valuable insights into the mechanisms underlying domestic violence.
By investigating these factors, our study enhances the existing understanding of the complex dynamics of domestic violence within the unique context of the pandemic. The COVID-19 crisis has exacerbated various stressors and challenges within households, potentially intensifying the risk of violence. Understanding the interplay between these factors and domestic violence is essential for the development of targeted interventions and support systems to mitigate violence and its consequences.
2.3. Demographic characteristics (A)
2.3.1. education level (a1).
According to Sen ( 19 ), the education level of the victim, typically women, or the head of household is a significant antecedent of domestic violence. Women’s access to and completion of secondary education play a crucial role in enhancing their capacity and control over their lives. Higher levels of education not only foster confidence and self-esteem but also empower women to seek help and resources, ultimately reducing their tolerance for domestic violence. Babu and Kar ( 33 ), Semahegn and Mengistie ( 34 ) support this perspective by demonstrating that women with lower levels of education and limited work opportunities are more vulnerable to experiencing violence.
When women assume the role of the head of the household, the likelihood of violence within the household, whether domestic or intimate partner violence, increases significantly. This has severe physical and mental health implications for both the woman and other family members, and in the worst-case scenario, it can result in the tragic loss of life ( 22 , 23 , 35 ).
Conversely, men’s economic frustration or their inability to fulfill the societal expectation of being the “head of household” is also a prominent factor contributing to the perpetration of physical and sexual violence within the home ( 36 ).The frustration arising from economic difficulties, combined with the frequent use of drugs and alcohol, exacerbates the likelihood of violent behavior.
These findings underscore the importance of addressing socio-economic disparities and promoting gender equality in preventing and combating domestic violence. By enhancing women’s access to education, improving economic opportunities, and challenging traditional gender roles, we can create a more equitable and violence-free society. Additionally, interventions targeting men’s economic empowerment and addressing substance abuse issues can play a pivotal role in reducing violence within the home.
2.3.2. Employment and occupation (A2)
Macroeconomic conditions, specifically differences in unemployment rates between men and women, have been found to impact domestic violence. Research suggests that an increase of 1% in the male unemployment rate is associated with an increase in physical violence within the home, while an increase in the female unemployment rate is linked to a reduction in violence ( 37 ).
Moreover, various studies ( 34 , 35 , 38 , 39 ) have highlighted the relationship between domestic violence and the husband’s working conditions, such as workload and job quality, as well as the income he earns. The exercise of authority within the household and the use of substances that alter behavior are also associated with domestic violence.
Within this context, economic gender-based violence is a prevalent but lesser-known form of violence compared to physical or sexual violence. It involves exerting unacceptable economic control over a partner, such as allocating limited funds for expenses or preventing them from working to maintain economic dependence. This form of violence can also manifest through excessive and unsustainable spending without consulting the partner. Economic gender-based violence is often a “silent” form of violence, making it more challenging to detect and prove ( 40 ).
Empowerment becomes a gender challenge that can lead to increased violence, as men may experience psychological stress when faced with the idea of women earning more than them ( 14 , 18 ). Lastly, Alonso-Borrego and Carrasco ( 17 ) and Tur-Prats ( 41 ) conclude that intrafamily violence decreases only when the woman’s partner is also employed, highlighting the significance of economic factors in influencing domestic violence dynamics.
Understanding the interplay between macroeconomic conditions, employment, and economic control within intimate relationships is crucial for developing effective interventions and policies aimed at reducing domestic violence. By addressing the underlying economic inequalities and promoting gender equality in both the labor market and household dynamics, we can work toward creating safer and more equitable environments that contribute to the prevention of domestic violence.
2.3.3. Religion (A3)
Religion and spiritual beliefs have been found to play a significant role in domestic violence dynamics. Certain religious interpretations and teachings can contribute to the acceptance of violence, particularly against women, as a form of submission or obedience. This phenomenon is prevalent in Middle Eastern countries, where religious texts such as the Bible and the Qur’an are often quoted to justify and perpetuate gender-based violence ( 20 ).
For example, in the book of Ephesians 5:22–24, the Bible states that wives should submit themselves to their husbands, equating the husband’s authority to that of the Lord. Similarly, the Qur’an emphasizes the importance of wives being sexually available to their husbands in all aspects of their relationship. These religious teachings can create a belief system where women are expected to endure mistreatment and forgive their abusive partners ( 15 ).
The influence of religious beliefs and practices can complicate a woman’s decision to leave an abusive relationship, particularly when marriage is considered a sacred institution. Feelings of guilt and difficulties in seeking support or ending the relationship can arise due to the belief that marriage is ordained by God ( 15 ).
It is important to note that the response of religious congregations and communities to domestic violence can vary. In some cases, if abuse is ignored or not condemned, it may perpetuate the cycle of violence and hinder efforts to support victims and hold perpetrators accountable. However, in other instances, religious organizations may provide emotional support and assistance through dedicated sessions aimed at helping all affected family members heal and address the violence ( 20 ).
Recognizing the influence of religious beliefs on domestic violence is crucial for developing comprehensive interventions and support systems that address the specific challenges faced by individuals within religious contexts. This includes promoting awareness, education, and dialog within religious communities to foster an understanding that violence is never acceptable and to facilitate a safe environment for victims to seek help and healing.
2.4. Presence of risk factor (B)
2.4.1. depression, anxiety, and stress (b1).
Within households, the occurrence of violence is unfortunately prevalent, often stemming from economic constraints, social and psychological problems, depression, and stress. These factors instill such fear in the victims that they are often hesitant to report the abuse to the authorities ( 42 ).
Notably, when women assume the role of heads of households, they experience significantly higher levels of depression compared to men ( 21 ). This study highlights that the presence of poverty, financial struggles, and the ensuing violence associated with these circumstances significantly elevate the risk of women experiencing severe health disorders, necessitating urgent prioritization of their well-being. Regrettably, in low-income countries where cases of depression are on the rise within public hospitals, the provision of adequate care becomes an insurmountable challenge ( 21 ).
These findings underscore the urgent need for comprehensive support systems and targeted interventions that address the multifaceted impact of domestic violence on individuals’ mental and physical health. Furthermore, effective policies should be implemented to alleviate economic hardships and provide accessible mental health services, particularly in low-income settings. By addressing the underlying factors contributing to violence within households and ensuring adequate care for those affected, society can take significant strides toward breaking the cycle of violence and promoting a safer and more supportive environment for individuals and families.
2.4.2. Retention tendency (B2)
Many societies, particularly in Africa, are characterized by a deeply ingrained patriarchal social structure, where men hold the belief that they have the right to exert power and control over their partners ( 31 ). This ideology of patriarchy is often reinforced by women themselves, who may adhere to traditional gender roles and view marital abuse as a norm rather than recognizing it as an act of violence. This acceptance of abuse is influenced by societal expectations and cultural norms that prioritize the preservation of marriage and the submission of women.
Within these contexts, there is often a preference for male children over female children, as males are seen as essential for carrying on the family name and lineage ( 43 ). This preference is also reflected in the distribution of property and decision-making power within households, where males are given greater rights and authority. Such gender-based inequalities perpetuate the cycle of power imbalances and contribute to the normalization of violence against women.
It is important to note that men can also be victims of domestic violence. However, societal and cultural norms have long portrayed men as strong and superior figures, making it challenging for male victims to come forward and report their abusers due to the fear of being stigmatized and rejected by society ( 16 ). The cultural expectations surrounding masculinity create barriers for men seeking help and support, further perpetuating the silence around male victimization.
These cultural dynamics underscore the complexity of domestic violence within patriarchal societies. Challenging and dismantling deeply rooted gender norms and power structures is essential for addressing domestic violence effectively. This includes promoting gender equality, empowering women, and engaging men and boys in efforts to combat violence. It also requires creating safe spaces and support systems that encourage both women and men to break the silence, seek help, and challenge the harmful societal narratives that perpetuate violence and victim-blaming.
2.4.3. Density (B3)
Moreover, the issue of overcrowding within households has emerged as another important factor influencing domestic violence. Overcrowding refers to the stress caused by the presence of a large number of individuals in a confined space, leading to a lack of control over one’s environment ( 44 ). This overcrowding can have a detrimental impact on the psychological well-being of household members, thereby negatively affecting their internal relationships.
The freedom to use spaces within the home and the ability to control interactions with others have been identified as crucial factors that contribute to satisfaction with the home environment and the way individuals relate to each other. In this regard, studies have shown that when households are crowded, and individuals lack personal space and control over their living conditions, the risk of violence may increase ( 45 ).
Furthermore, investigations conducted during periods of extensive confinement, such as the COVID-19 pandemic, have shed light on the significance of other environmental factors within homes ( 46 ). For instance, aspects like proper ventilation and adequate living space have been found to influence the overall quality of life and the health of household inhabitants.
These findings emphasize the importance of considering the physical living conditions and environmental factors within households when examining the dynamics of domestic violence. Addressing issues of overcrowding, promoting healthy and safe living environments, and ensuring access to basic amenities and resources are crucial steps in reducing the risk of violence and improving the well-being of individuals and families within their homes.
2.4.4. Reason for confrontation (B4)
Another form of violence that exists within households is abandonment and neglect, which manifests through a lack of protection, insufficient physical care, neglecting emotional needs, and disregarding proper nutrition and medical care ( 47 ). This definition highlights that any member of the family can be subjected to this form of violence, underscoring the significance of recognizing its various manifestations.
In this complex context, negative thoughts and emotions can arise, leading to detrimental consequences. For instance, suspicions of infidelity and feelings of jealousy can contribute to a decrease in the partner’s self-esteem, ultimately triggering intimate partner violence that inflicts physical, social, and health damages ( 32 , 48 ).
Furthermore, it is important to acknowledge the intimate connection between domestic violence and civil issues. Marital conflicts, particularly when accompanied by violence, whether physical or psychological, can lead to a profound crisis within the relationship, often resulting in divorce. Unfortunately, the process of obtaining a divorce or establishing parental arrangements can be protracted, creating additional friction and potentially exacerbating gender-based violence ( 49 ).
These dynamics underscore the complex interplay between domestic violence and broader social, emotional, and legal contexts. Understanding these interconnected factors is crucial for developing effective interventions and support systems that address the multifaceted nature of domestic violence, promote healthy relationships, and safeguard the well-being of individuals and families within the home.
Finally, despite the multitude of factors identified in the existing literature that may have an impact on gender-based violence, we have selected a subset of variables for our study based on data availability. Specifically, our analysis will concentrate on the following factors reviewed: (A3) religion, (B1) depression, health consciousness, and mood, (B2) retention tendency as reflected by household chores, and (B3) density.
The rationale behind our choice of these variables stems from their perceived significance and potential relevance to the study of domestic violence. Religion has been widely acknowledged as a social and cultural determinant that shapes beliefs, values, and gender roles within a society, which may have implications for power dynamics and relationship dynamics within households. Depression, as a psychological construct, has been frequently associated with increased vulnerability and impaired coping mechanisms, potentially contributing to the occurrence or perpetuation of domestic violence. Health consciousness and mood are additional constructs that have garnered attention in the context of interpersonal relationships. Health consciousness relates to individuals’ awareness and concern for their own well-being and that of others, which may influence their attitudes and behaviors within the household. Mood, on the other hand, reflects emotional states that can influence communication, conflict resolution, and overall dynamics within intimate relationships.
Furthermore, we have included the variable of retention tendency, as manifested through household chores. This variable is indicative of individuals’ willingness or inclination to maintain their involvement and responsibilities within the household. It is hypothesized that individuals with higher retention tendencies may exhibit a greater commitment to the relationship, which could influence the occurrence and dynamics of domestic violence. Lastly, we consider the variable of density, which captures the population density within the living environment. This variable may serve as a proxy for socio-environmental conditions, such as overcrowding or limited personal space, which can potentially contribute to stress, conflict, and interpersonal tensions within households.
By examining these selected factors, we aim to gain insights into their relationships with domestic violence and contribute to a better understanding of the complex dynamics underlying such occurrences. It is important to note that these variables represent only a subset of the broader range of factors that influence gender-based violence, and further research is warranted to explore additional dimensions and interactions within this multifaceted issue.
3. Data collection and variables
The reference population for this study is Ecuadorian habitants. Participants were invited to fill up a survey concerning COVID-19 impact on their mental health. Data collection took place between April and May 2020, exactly at the time of the mandatory lockdowns taking place. In this context governmental authorities ordered mobility restrictions as well as social distancing measures. We conduct three waves of social media invitations to participate in the study. Invitations were sent using the institutional accounts of the universities the authors of this study are affiliated. At the end, we received 2,403 answers, 50.5% females and 49.5% males. 49% of them have college degrees.
3.1. Ecuador stylized facts
Ecuador, a small developing country in South America, has a population of approximately 17 million inhabitants, with a population density of 61.85 people per square kilometer.
During the months under investigation, the Central Bank of Ecuador reported that the country’s GDP in the fourth quarter of 2020 amounted to $16,500 million. This represented a decrease of 7.2% compared to the same period in 2019, and a 5.6% decline in the first quarter of 2021 compared to the same quarter of the previous year. However, despite these declines, there was a slight growth of 0.6% in the GDP during the fourth quarter of 2020 and 0.7% in the first quarter of 2021 when compared to the previous quarter.
In mid-March, the Ecuadorian government implemented a mandatory lockdown that lasted for several weeks. By July 30, 2020, Ecuador had reported over 80,000 confirmed cases of COVID-19. The statistics on the impact of the pandemic revealed a death rate of 23.9 per 100,000 inhabitants, ranking Ecuador fourth globally behind the UK, Italy, and the USA, with rates of 63.7, 57.1, and 36.2, respectively. Additionally, Ecuador’s observed case-fatality ratio stood at 8.3%, placing it fourth globally after Italy, the UK, and Mexico, with rates of 14.5, 14, and 11.9%, respectively ( 50 ). As the lockdown measures continued, mental health issues began to emerge among the population ( 51 ).
The challenging socioeconomic conditions and the impact of the pandemic on public health have had significant repercussions in Ecuador, highlighting the need for comprehensive strategies to address both the immediate and long-term consequences on the well-being of its population.
3.2. Dependent variable
The dependent variable in this study is Domestic Violence, which is measured using a composite score derived from five items. These items were rated on a 7-point scale, ranging from 1 (never) to 7 (very frequent), to assess the frequency of intrafamily conflict and violence occurring within the respondents’ homes. The five items included the following statements: “In my house, subjects are discussed with relative calm”; “In my house, heated discussions are common but without shouting at each other”; “Anger is common in my house, and I refuse to talk to others”; “In my house, there is the threat that someone will hit or throw something”; and “In my house, family members get easily irritated.”
To evaluate the internal consistency of the measurement, Cronbach’s Alpha was calculated and found to be 0.7. This indicates good internal consistency, suggesting that the items in the scale are measuring a similar construct and can be considered reliable for assessing the level of domestic violence within the households under investigation.
3.3. Independent variables
3.3.1. mood.
The mood construct, based on Peterson and Sauber ( 52 ), is measured using three Likert scale questions. The respondents rate their agreement on a scale from strongly disagree to strongly agree. The questions included: “I am in a good mood,” “I feel happy,” and “At this moment, I feel nervous or irritable.” The Cronbach’s Alpha coefficient for this construct is 0.7757, indicating good internal consistency.
3.3.2. Depression
The depression construct, based on the manual for the Depression Anxiety Stress Scales by Lovibond S and Lovibond P, is measured by summing the results of 13 Likert scale questions. The scale ranges from strongly disagreeing to strongly agreeing. The questions include: “I feel that life is meaningless,” “I do not feel enthusiastic about anything,” “I feel downhearted and sad,” and others. The Cronbach’s Alpha coefficient for this construct is 0.9031, indicating high internal consistency.
3.3.3. Health consciousness
The health consciousness construct, based on Gould ( 53 ), is measured using four Likert scale questions. The respondents rate their agreement on a scale from strongly disagree to strongly agree. The questions include: “I’m alert to changes in my health,” “I am concerned about the health of others,” “Throughout the day, I am aware of what foods are best for my health,” and “I notice how I lose energy as the day goes by.” The Cronbach’s Alpha coefficient for this construct is 0.7, indicating acceptable internal consistency.
3.3.4. Household chores
The respondents were asked to rate their involvement in various household chores on a scale from “not at all” to “a lot.” The listed household chores include cooking, washing dishes, cleaning restrooms, doing laundry, home maintenance, and helping with children/siblings. It can serve as a proxy for Retention Tendency.
3.3.5. Density
It is measured as the number of people per bedroom, indicating the level of overcrowding within households.
3.3.6. Religion
The religion construct is measured as the sum of four Likert scale items based on Worthington et al. ( 54 ). The respondents rate their agreement on a scale from strongly disagree to strongly agree. The items include: “My religious beliefs lie behind my whole approach to life,” “It is important to me to spend periods in private religious thought and reflection,” “Religion is very important to me because it answers many questions about the meaning of life,” and “I am informed about my local religious group and have some influence in its decisions.” The Cronbach’s Alpha coefficient for this construct is 0.8703, indicating good internal consistency.
3.4. Control variables
3.4.1. social media.
The respondents were asked to indicate the number of hours they spend on social networks during a typical day. The scale ranges from “I do not review information on social networks” to “More than three hours.”
Sex is measured as a binary variable, where 1 represents female and 0 represents male.
Age refers to the age of the respondent.
3.4.4. Age of householder
Age of householder refers to the age of the individual who is the primary occupant or head of the household.
3.5. Describe statistics
Table 2 reports the means, standard deviation, and correlation matrix. Our dataset has not the presence of missing values.
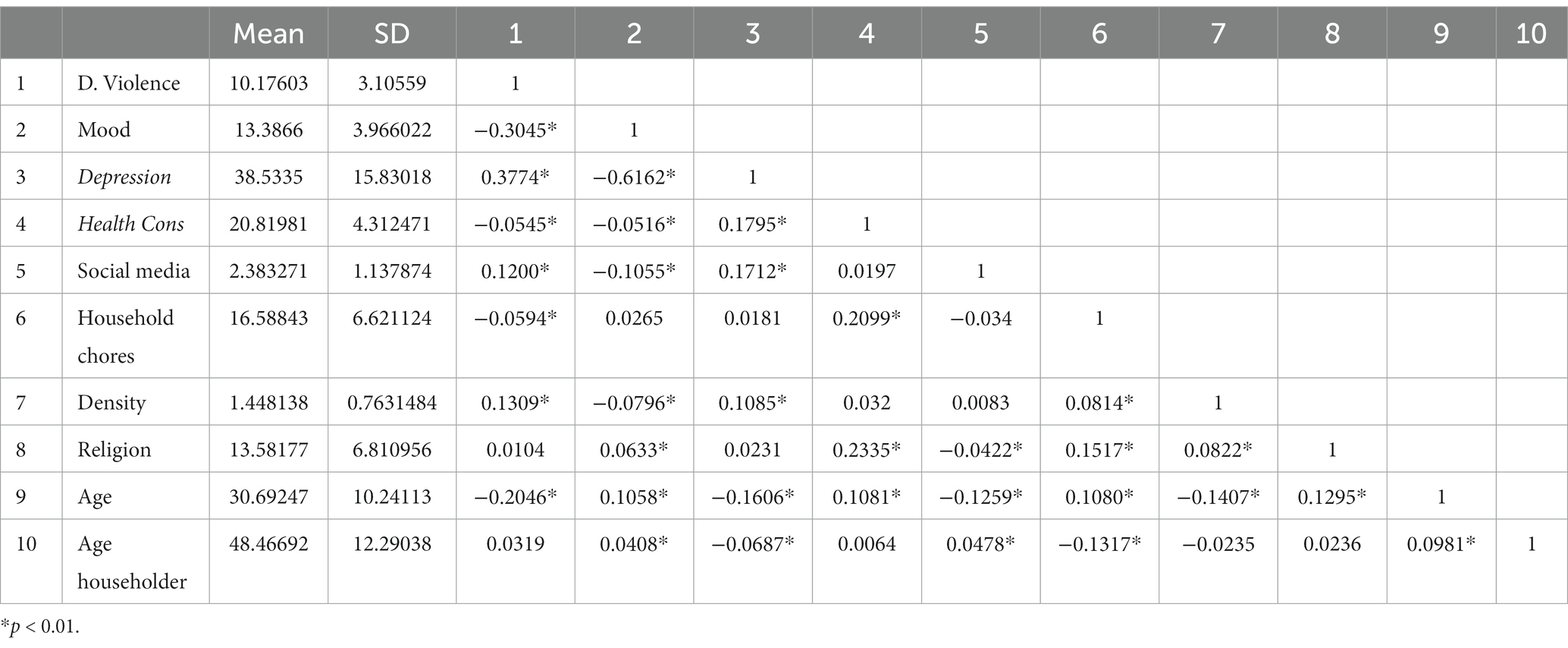
Table 2 . Summary statistics.
Descriptive statistics reveal that the variables in the sample exhibit a considerable degree of homogeneity, as evidenced by the means being larger than the standard deviations. Moreover, the strong correlation between Depression and mood suggests that these two variables should not be included together in the same model.
4. Methodological approach
Our empirical identification strategy comprises the following linear model:
We employed ordinary least squares (OLS) regression techniques to examine the relationship between our selected exogenous variables and household violence during the period of mandatory lockdowns. To ensure the robustness of our regression model, we conducted several diagnostic tests. Firstly, we tested for heteroscedasticity using the Breusch-Pagan test, yielding a chi-square value of 223.58 with a value of p of 0, indicating the presence of heteroscedasticity in the model. Secondly, we assessed multicollinearity using the variance inflation factor (VIF), which yielded a VIF value of 1.07, indicating no significant multicollinearity issues among the variables. Furthermore, we conducted the Ramsey Reset test to examine the presence of omitted variables in the model. The test yielded an F-statistic of 2.06 with a value of p of 0.103, suggesting no strong evidence of omitted variables. Lastly, we checked the normality of the residuals using the skewness and kurtosis tests, which yielded a chi-square value of 97.9 with a value of p of 0, indicating departure from normality in the residuals.
Hence, our analysis revealed the presence of heteroscedasticity issues and non-normality in the residuals. Consequently, it is imperative to employ an alternative estimation technique that can handle these challenges robustly. In light of these circumstances, we opted for Quantile Regression, as proposed by Koenker and Bassett ( 55 ), which allows for a comprehensive characterization of the relationship between the input variable(s) x and the dependent variable y.
4.1. Quantile regression
While an OLS predicts the average relationship between the independent variables and the dependent variable, which can cause the estimate to be unrepresentative of the entire distribution of the dependent variable if it is not identically distributed, Quantile Regression allows estimating parts of the dependent variable. Distribution of the dependent variable and thus determine the variations of the effect produced by the exogenous variables on the endogenous variable in different quantiles ( 56 ). The Quantile Regression methodology also presents the benefit that, by providing them with a weight, the errors are minimal. Quantile Regression is defined as follows:
where: Y i is dependent variable, X i is vector of independent variables, β(ϑ): is vector of parameters to be estimated for a given quantile ϑ, e ϑ i : is random disturbance corresponding to the quantile ϑ, Q ϑ ( Y i ) is qth quantile of the conditional distribution of Y i given the known vector of regressors X i .
The Quantile Regression model provides predictions of a specific quantile of the conditional distribution of the dependent variable and is considered the generalization of the sample quantile of an independent and identically distributed random variable ( 57 ). By considering a range of quantiles, Quantile Regression offers a more nuanced understanding of the conditional distribution, making it a valuable technique for analyzing various aspects of the relationship between variables.
The estimation results are reported in Table 3 . The regressions 1 and 3 consider individuals who are not household heads, while regressions 2 and 4 involve the respondent being the household head. In regressions 5 and 6, the respondent is not the household head and is also female, whereas in regressions 7 and 8, the respondents are household heads and male. The regressions exhibit a coefficient of determination ranging between 9 and 11.

Table 3 . Results.
The effects of the different variables studied on violence are presented below: Across all regressions, it can be observed that the mood of a person, which indicates whether they are in a good mood or feeling cheerful, nervous, or irritated, is statistically significant at all levels of confidence. This implies that violence decreases when the mood is good. On the other hand, depression has a positive and significant sign. This tells us that, on average, an increase of one unit in the depression, anxiety, and stress scale is associated with an increase in the measurement of conflict and intrafamily violence in a household, whether the respondent is a household head or not.
On the other hand, Health Consciousness has a negative and significant sign, indicating that violence decreases as Health Consciousness increases. However, it is noteworthy that it loses significance when the survey respondent is a woman, regardless of whether she is a household head or not.
Regarding Household chores, which refers to the time spent on household tasks, it can be observed that it is only significant and negative when the respondent is not a household head, and this significance holds even when the respondent is male. In other words, less time spent on household chores decreases violence in households where the respondent is not a household head.
The variable religion generally has a positive and significant sign in most regressions, but loses significance in regressions (1) and (5), where the respondent is not the household head and is female, respectively. This suggests that being religious would increase the levels of violence.
In general, density increases violence in the surveyed households, as indicated by a positive and significant sign. However, it is interesting to note that it is only significant again when the respondent is not a household head and is female, or when the respondent is a household head and is male.
As for the control variables, the variable Social media, which indicates the number of hours a person spends on social media, is positive and significant whether the respondent is a household head or not, and even when the respondent is male. This suggests that violence decreases with access to social media, possibly due to increased access to information. Finally, the variables sex, age of the respondent, and age of the household head were not significant.
6. Discussion
Interestingly, the prevalence and intensity of domestic violence appear to vary across different segments of society. Goodman ( 33 ) have highlighted the existence of variations in episodes of domestic violence among social strata. They have also identified several factors that act as deterrents to domestic violence, including income levels, educational attainment, employment status of the household head, household density, consumption of psychotropic substances, anxiety, and stress. These factors increase the likelihood of experiencing instances of violence within the home.
Within this context, the COVID-19 pandemic has had far-reaching implications for individuals and families worldwide, with significant impacts on various aspects of daily life, including domestic dynamics. This study explores the relationship between household factors and violence within the context of the pandemic, shedding light on the unique challenges and dynamics that have emerged during this period.
Our findings highlight the importance of considering mental well-being in the context of domestic violence during the pandemic. We observe that positive mood is associated with a decrease in violence levels within households. This suggests that maintaining good mental health and emotional well-being during times of crisis can serve as a protective factor against violence. With the increased stress and anxiety caused by the pandemic, policymakers and practitioners should prioritize mental health support and interventions to address potential escalations in violence within households.
Furthermore, our results indicate that depression exhibits a positive association with violence. As individuals grapple with the impacts of the pandemic, such as job loss, financial strain, and social isolation, the prevalence of depression may increase. This finding underscores the urgent need for accessible mental health resources and support networks to address the heightened risk of violence stemming from increased levels of depression.
The study also reveals that health consciousness plays a crucial role in reducing violence within households. As individuals become more aware of the importance of maintaining their health amidst the pandemic, violence levels decrease. This suggests that promoting health awareness and encouraging healthy lifestyle choices can serve as protective factors against domestic violence. Public health initiatives and educational campaigns aimed at fostering health-conscious behaviors should be emphasized as part of comprehensive violence prevention strategies.
Interestingly, our analysis uncovers a mitigating effect of social media usage on violence levels during the pandemic. With the increased reliance on digital platforms for communication and information sharing, access to social media may provide individuals with alternative channels for expression and support, ultimately reducing the likelihood of violence. Recognizing the potential benefits of social media, policymakers and practitioners should explore ways to leverage these platforms to disseminate violence prevention resources, provide support, and promote positive social connections within households.
Additionally, our findings highlight the role of household chores and density in shaping violence levels during the pandemic. Less time spent on household chores is associated with decreased violence, indicating that redistributing domestic responsibilities may alleviate tension and conflict within households. The COVID-19 pandemic has disrupted routines and added new challenges to household dynamics, making it essential to consider strategies that promote equitable distribution of chores and support mechanisms for individuals and families.
Moreover, the positive association between household density and violence emphasizes the impact of living conditions during the pandemic. With prolonged periods of confinement and restricted mobility, crowded living spaces may intensify conflicts and escalate violence. Policymakers should prioritize initiatives that address housing conditions, promote safe and adequate living environments, and provide resources to mitigate the negative effects of overcrowding.
In this line, our study delves into the intricate relationship between household factors and violence during the COVID-19 pandemic, primarily within our specific context. However, it is valuable to consider how our findings align or diverge when juxtaposed with research from developed countries, where economic, social, and healthcare systems are typically more advanced. In developed countries, the impact of crises, such as the pandemic, could manifest differently due to varying levels of financial stability, access to support networks, and well-established healthcare systems.
For instance, while we observe that maintaining mental well-being serves as a protective factor against violence, developed countries might have better access to mental health resources and support networks, potentially magnifying the impact of positive mental health on violence prevention ( 58 ). Similarly, the positive association between health consciousness and reduced violence levels could be influenced by different perceptions of health and well-being in developed countries, where health awareness campaigns are more prevalent ( 51 ).
The mitigating effect of social media on violence levels during the pandemic might also vary across contexts. Developed countries might have more widespread and equitable access to digital platforms, leading to a stronger impact on violence reduction through alternative channels for communication and support ( 59 ). Conversely, regions with limited digital infrastructure could experience a smaller effect.
Additionally, comparing the role of religious affiliation and its influence on violence with findings from developed countries could reveal cultural variations in the interplay between religious teachings, gender dynamics, and violence ( 60 ). While our study suggests the need for interventions promoting peaceful religious interpretations, it is crucial to examine whether similar efforts have been successful in developed nations with distinct cultural norms and religious landscapes.
In this context, this study makes a significant contribution to the field of gender-based violence research by intricately examining the intersection of diverse socio-economic and psychological factors within the backdrop of the COVID-19 pandemic. The uniqueness of this article lies in its holistic approach to comprehend domestic violence dynamics amidst a global crisis. By dissecting and analyzing how mental health, health awareness, social media utilization, household chore distribution, living space density, and religious affiliation interact to influence violence levels, this study provides a deeper and nuanced insight into the factors contributing to the manifestation and prevention of gender-based violence. Moreover, by pinpointing areas where traditional gender norms and religious beliefs might exacerbate violence, the article suggests novel avenues for research and intervention development that account for cultural and contextual complexities. Ultimately, this work not only advances the understanding of gender-based violence during a critical period but also offers practical and theoretical recommendations to inform policies and preventive actions both throughout the pandemic and in potential future crises.
In considering the limitations of our study, we acknowledge that while our findings provide crucial insights into the role of religious affiliation in shaping violence levels during the pandemic, there are certain aspects that warrant further investigation. Firstly, our analysis primarily focuses on the association between religious beliefs and violence without delving deeply into the underlying mechanisms that drive this relationship. Future research could employ qualitative methodologies to explore how specific religious doctrines and practices interact with broader cultural norms to influence gender dynamics and contribute to violence within households. Additionally, our study does not extensively address variations in religious interpretations across different communities, which could lead to distinct outcomes in terms of violence prevention efforts. To address these limitations, scholars could conduct comparative studies across religious affiliations and denominations to uncover nuanced insights into the interplay between religious teachings, cultural contexts, and violence dynamics.
Furthermore, while our study suggests that policymakers and practitioners should consider developing targeted interventions promoting peaceful religious interpretations to mitigate violence, the precise design and effectiveness of such interventions remain areas ripe for exploration. Future research could involve collaboration with religious leaders and communities to develop and test intervention strategies that align with both religious teachings and contemporary gender equality principles. This interdisciplinary approach could yield actionable insights into fostering cultural change and enhancing the role of religion in promoting non-violence within households.
In conclusion, our study provides valuable insights into the dynamics of domestic violence within households during the COVID-19 pandemic. The findings underscore the importance of addressing mental health, promoting health consciousness, leveraging social media, redistributing household chores, improving housing conditions, and considering the nuanced role of religious beliefs. By incorporating these findings into policy and intervention strategies, policymakers and practitioners can work toward preventing and mitigating domestic violence in the context of the ongoing pandemic.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
CL played a crucial role in this research project, being responsible for the data collection, conducting the econometric analysis, contributing to the literature review, introduction, and discussion sections of the manuscript. JD-S made significant contributions to the project and assisted in the data collection process, contributed to the literature review, and provided insights in the discussion section. FV assisted with the data collection process and reviewed the article for accuracy and clarity. All authors contributed to the article and approved the submitted version.
This project receives funding from Vicerrectorado de Investigación y Proyección Social, Escuela Politécnica Nacional.
Acknowledgments
The authors acknowledge the Escuela Politécnica Nacional for this support on this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. World Health Organization . (2021). Violence against women. Available at: https://www.who.int/es/news-room/fact-sheets/detail/violence-against-women
Google Scholar
2. Malik, Sana , and Naeem, K. (2020). Impact of COVID-19 pandemic on women: health, livelihoods & domestic violence. Sustainable Development Policy Institute. Available at: https://www.iassw-aiets.org/wp-content/uploads/2021/01/Covid19-impact-on-women.pdf
3. Manrique De Lara, A , and Arellano, MDJM . The COVID-19 pandemic and ethics in Mexico through a gender lens. J Bioethical Inquiry . (2020) 17:613–17. doi: 10.1007/s11673-020-10029-4
CrossRef Full Text | Google Scholar
4. Taub, A . A new COVID-19 crisis: Domestic abuse rises worldwide . New York, NY: New York Times (2020).
5. World Health Organization (2013). World health statistics 2013 . Available at: https://www.who.int/publications/i/item/9789241564588
6. Sepehrdoust, H . Health care analysis and regional disparities in different provinces of Iran. Iran. Econ. Rev. (2009) 14:113–34.
7. White, JW , and Bondurant, B . Gendered violence. Gendered relationships. (1996):197–210.
8. Tan, SY , and Haining, R . Crime victimization and the implications for individual health and wellbeing: a Sheffield case study. Soc Sci Med . (2016) 167:128–39. doi: 10.1016/j.socscimed.2016.08.018
9. Alvarez-Hernandez, LR , Cardenas, I , and Bloom, A . COVID-19 pandemic and intimate partner violence: an analysis of help-seeking messages in the Spanish-speaking media. J Fam Violence . (2021) 37:939–50. doi: 10.1007/s10896-021-00263-8
10. Moorer, O. (2021). Intimate partner violence vs. domestic violence–YWCA Spokane. Ywca Spokane Organization. Available at: https://ywcaspokane.org/What-Is-Intimate-Partner-Domestic-Violence/
11. Carmo, R , Grams, A , and Magalhães, T . Men as victims of intimate partner violence. J Forensic Legal Med . (2011) 18:355–9. doi: 10.1016/j.jflm.2011.07.006
12. McTavish, JR , MacGregor, JCD , Wathen, CN , and MacMillan, HL . Children’s exposure to intimate partner violence: an overview. Int Rev Psychiatry . (2016) 28:504–18. doi: 10.1080/09540261.2016.1205001
13. Wathen, CN , and MacMillan, HL . Children’s exposure to intimate partner violence: impacts and interventions. Paediatr Child Health . (2013) 18:419–22. doi: 10.1093/pch/18.8.419
14. Erten, B , and Keskin, P . For better or for worse? Education and the prevalence of domestic violence in Turkey. Am Econ J Appl Econ . (2018) 10:64–105. doi: 10.1257/app.20160278
15. Krob, DB , and Steffen, L . Religious influence on education and culture: violence against women as common sense. Procedia Soc Behav Sci . (2015) 174:2374–9. doi: 10.1016/j.sbspro.2015.01.903
16. Visaria, L . Violence against women in India: is empowerment a protective factor? Econ Polit Wkly . (2008) 43:60–6. doi: 10.1007/s40609-020-00186-0
17. Alonso-Borrego, C , and Carrasco, R . Employment and the risk of domestic violence: does the Breadwinner’s gender matter? SSRN Electron J . (2016) 49:5074–91. doi: 10.2139/ssrn.2748885
18. Anderberg, D , Rainer, H , Wadsworth, J , and Wilson, T . Unemployment and domestic violence: theory and evidence. Econ J . (2016) 126:1947–79. doi: 10.1111/ecoj.12246
19. Sen, P . Enhancing women’s choices in responding to domestic violence in Calcutta: a comparison of employment and education. Eur J Dev Res . (1999) 11:65–86. doi: 10.1080/09578819908426739
20. Tomisin, A . Culture, religion and help-seeking for intimate partner violence victims in Nigeria (a narrative review). African J Soc Sci Human Res . (2020) 3:56.
21. Zeybek, O , and Arslan, Examining cultural heritages harmed by religious fanaticism: sample of the Palmyra Ancient City. Bartın Orman Fakültesi Dergisi . (2017) 19:1–10.
22. Van de Velde, S , Bracke, P , and Levecque, K . Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Soc Sci Med . (2010) 71:305–13. doi: 10.1016/j.socscimed.2010.03.035
23. Straus, MA , Gelles, RJ , and Steinmetz, SK . Behind closed doors: Violence in the American family Routledge (2017).
24. Burney, VH . Applications of social cognitive theory to gifted education. Roeper Review. (2008) 30:130–9.
25. Cooper, A , and Smith, EL . Homicide trends in the United States, 1980–2008 . Washington, DC: Bureau of Justice Statistics (2011).
26. Heise, L , and Garcia-Moreno, C . Violence by intimate partners. World report on violence and health. (2002) 1:87–113.
27. Langford, L , Isaac, N , and Kabat, S . Homicides related to intimate partner violence in Massachusetts: examining case ascertainment and validity of the SHR. Homicide Stud . (1998) 2:353–77. doi: 10.1177/1088767998002004002
28. Walker-Descartes, I , Mineo, M , Condado, LV , and Agrawal, N . Domestic violence and its effects on women, children, and families. Pediatr Clin N Am . (2021) 68:455–64. doi: 10.1016/j.pcl.2020.12.011
29. Ishola, SA . Domestic violence: the Nigerian experience. Asia-Africa J Mission Ministry . (2016) 13:3–16. doi: 10.21806/aamm.2016.13.01
30. Barrientos, S , Kothari, U , and Phillips, N . Dynamics of unfree labour in the contemporary global economy. J. Dev. Stud. (2013) 49:1037–41.
31. Fareo, D . Domestic violence against women in Nigeria. Europ J Psychol Res . (2015) 371:1664. doi: 10.1016/S0140-6736(08)60723-0
32. Goodman, L , and Epstein, D . COVID-19 and the Loneliness Pandemic: Implications for Intimate Partner Violence Survivors (2020). Available at: https://dx.doi.org/10.2139/ssrn.3727674”http://dx.doi.org/10.2139/ssrn.3727674
33. Babu, BV , and Kar, SK . Domestic violence against women in eastern India: a population-based study on prevalence and related issues. BMC Public Health . (2009) 9:1–15. doi: 10.1186/1471-2458-9-129
34. Semahegn, A , and Mengistie, B . Domestic violence against women and associated factors in Ethiopia; systematic review. Reprod Health . (2015) 12:72. doi: 10.1186/s12978-015-0072-1
35. Farley, R . Homicide trends in the United States. Demography . (1975) 17:177–88.
36. Owoaje, ET , and OlaOlorun, FM . Women at risk of physical intimate partner violence: a cross-sectional analysis of a low-income community in Southwest Nigeria. Afr J Reprod Health . (2012) 16:43–53.
PubMed Abstract | Google Scholar
37. Bhalotra, S , Kambhampati, U , Rawlings, S , and Siddique, Z . Intimate partner violence: the influence of job opportunities for men and women. World Bank Econ Rev . (2021) 35:461–79. doi: 10.1093/wber/lhz030
38. Kargar Jahromi, M , Jamali, S , Rahmanian Koshkaki, A , and Javadpour, S . Prevalence and risk factors of domestic violence against women by their husbands in Iran. Global J Health Sci . (2015) 8:175–83. doi: 10.5539/gjhs.v8n5p175
39. Sen, S , and Bolsoy, N . Violence against women: prevalence and risk factors in Turkish sample. BMC Womens Health . (2017) 17:1–9. doi: 10.1186/s12905-017-0454-3
40. Croda, E , and Grossbard, S . Women pay the price of COVID-19 more than men. Rev Econ Househ . (2021) 19:1–9. doi: 10.1007/s11150-021-09549-8
41. Tur-Prats, A . Family types and intimate partner violence: a historical perspective. Rev Econ Stat . (2019) 101:878–91. doi: 10.1162/rest_a_00784
42. Straus, MA . Measuring intrafamily conflict and violence: the conflict tactics (CT) scales. Phys Violen Am Fam . (2019) 41:29–48. doi: 10.4324/9781315126401-4
43. Hsu, L , Kaufmann, P , and Srinivasan, S . How do franchise ownership structure and strategic investment emphasis influence stock returns and risks? J Retail . (2017) 93:350–68. doi: 10.1016/j.jretai.2017.04.004
44. Díaz-Sánchez, JP , Lanchimba, C , Velasco, F , and Paz, M . Associations between household density and mood during COVID-19 lockdowns: evidence from Ecuador associations between household density and mood during COVID-19 lockdowns: evidence from Ecuador. Cities Health . (2022):1–10. doi: 10.1080/23748834.2022.2135187
45. Porter, C , Favara, M , Sánchez, A , and Scott, D . The impact of COVID-19 lockdowns on physical domestic violence: evidence from a list randomization experiment. SSM Populat Health . (2021) 14:792. doi: 10.1016/j.ssmph.2021.100792
46. Diaz, A , Nucci-Sack, A , Colon, R , Guillot, M , Hollman, D , Brunelli, M, et al. Impact of COVID-19 mitigation measures on Inner-City female youth in New York City. J Adolesc Health . (2022) 70:220–7. doi: 10.1016/j.jadohealth.2021.10.015
47. Barbara, G , Facchin, F , Micci, L , Rendiniello, M , Giulini, P , Cattaneo, C, et al. COVID-19, lockdown, and intimate partner violence: some data from an Italian service and suggestions for future approaches. J Women's Health . (2020) 29:1239–42. doi: 10.1089/jwh.2020.8590
48. Piquero, AR , Riddell, JR , Bishopp, SA , Narvey, C , Reid, JA , and Piquero, NL . Staying home, staying safe? A short-term analysis of COVID-19 on Dallas domestic violence. Am J Crim Justice . (2020) 45:601–35. doi: 10.1007/s12103-020-09531-7
49. Lillard, LA , and Waite, LJ . A joint model of marital childbearing and marital disruption. Demography . (1993) 30:653–81. doi: 10.2307/2061812
50. Johns Hopkins Coronavirus Resource Center . (2020). Mortality analyses. John Hopkins University & Medicine. Available at: https://coronavirus.jhu.edu/data/mortality
51. Franklin, V , Cintya, L , Mariel, PM , and Pablo, DSJ . Mental health factors that guide individuals to engage in overconsumption behavior during the COVID-19 pandemic: a cross-cultural study between USA and Ecuador. Front Public Health . (2022) 10:1–12. doi: 10.3389/fpubh.2022.844947
PubMed Abstract | CrossRef Full Text | Google Scholar
52. Peterson, R , and Sauber, M . “A mood scale for survey research.” In: Handbook of marketing scales , eds. H Briggs, A Howland, DE Axelsen, N Kabakian (Sage Publications, Inc.) (1983). 188.
53. Gould, SJ . Consumer attitudes toward health and health care: a differential perspective. J Consum Affairs. (1988) 22:96–118. doi: 10.1111/j.1745-6606.1988.tb00215.x
54. Worthington, EL , Wade, NG , Hight, TL , Ripley, JS , McCullough, ME , Berry, JW, et al. The religious commitment Inventory-10: development, refinement, and validation of a brief scale for research and counseling. J Couns Psychol . (2003) 50:84–96. doi: 10.1037/0022-0167.50.1.84
55. Koenker, R , and Bassett, G . Regression Quantiles. Econometrica . (1978) 46:33. doi: 10.2307/1913643
56. Conyon, MJ , and He, L . Firm performance and boardroom gender diversity: a quantile regression approach. J Bus Res . (2017) 79:198–211. doi: 10.1016/J.JBUSRES.2017.02.006
57. Dimelis, S , and Louri, H . Foreign ownership and production efficiency: a quantile regression analysis. Oxf Econ Pap . (2002) 54:449–69. doi: 10.1093/oep/54.3.449
58. Betancourt, TS , and Khan, KT . The mental health of children affected by armed conflict: protective processes and pathways to resilience. Int Rev Psychiatry . (2008) 20:317–28. doi: 10.1080/09540260802090363
59. Mcdonald, P , Charlesworth, S , and Graham, T . Developing a framework of effective prevention and response strategies in workplace sexual harassment. Asia Pac J Hum Resour . (2015) 53:41–58. doi: 10.1111/1744-7941.12046
60. Ellison, CG , Bartkowski, JP , and Anderson, KL . Are there religious variations in domestic violence? J Fam Issues . (1999) 20:87–113. doi: 10.1177/019251399020001005
Keywords: domestic violence, depression, mood, religious affiliation, health consciousness, quantile regression, Ecuador, Covid-19
Citation: Lanchimba C, Díaz-Sánchez JP and Velasco F (2023) Exploring factors influencing domestic violence: a comprehensive study on intrafamily dynamics. Front. Psychiatry . 14:1243558. doi: 10.3389/fpsyt.2023.1243558
Received: 20 June 2023; Accepted: 24 August 2023; Published: 07 September 2023.
Reviewed by:
Copyright © 2023 Lanchimba, Díaz-Sánchez and Velasco. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cintya Lanchimba, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Study protocol
- Open access
- Published: 24 September 2015
Patterns of domestic violence and alcohol consumption among women and the effectiveness of a brief intervention in a household setting: a protocol study
- Carla Ferreira de Paula Gebara 1 ,
- Cleusa Pinheiro Ferri 1 ,
- Lelio Moura Lourenço 2 ,
- Marcel de Toledo Vieira 3 ,
- Fernanda Monteiro de Castro Bhona 2 &
- Ana Regina Noto 1
BMC Women's Health volume 15 , Article number: 78 ( 2015 ) Cite this article
8019 Accesses
11 Citations
8 Altmetric
Metrics details
Domestic violence and harmful alcohol consumption are considered major public health problems worldwide. These phenomena often co-occur, and they share several risk factors. Nevertheless, few in-depth studies have supported integrated interventions for both phenomena, in particular among Latin American women. This project will study the consumption of alcoholic beverages among women and its relationship with patterns of domestic violence; furthermore, it will assess the effect of a brief intervention (BI) aimed at modifying these behaviors using a community household sample.
Methods/design
This project is divided into two studies. Study 1 will employ a cross-sectional observational design and will be conducted using a household sample of adult women (approximate sample size = 1600) to assess harmful alcohol consumption and domestic violence patterns. Study 2, will be a randomized clinical trial based on specific cases from Study 1, assessing the effect of a brief intervention on women who exhibit harmful levels of alcohol consumption (AUDIT ≥ 8). Approximately 73 women will be assigned to one of two groups, either a treated group (TG) or a control group (CG). A sociodemographic questionnaire, a questionnaire concerning general health and substance use, and four other standardized instruments (i.e., the Alcohol Use Disorder Identification Test [AUDIT; used to investigate problems related to alcohol consumption], the Center for Epidemiologic Studies Depression Scale [CES-D; used to measure depressive symptoms], and the Revised Conflict Tactics Scales and Parent–child Conflict Tactics Scales [CTS2 and CTSPC; used to obtain information on violence among couples and between parents and children, respectively]) will be used to collect data.
The study protocol will employ a household survey of a representative sample from a neighborhood in a middle income country, where well-conducted household surveys remain rare. The present work represents a step toward a better understanding of violence in women’s lives and its interaction with alcohol consumption and expands the discussion on the potential strategies for public health actions seeking to prevent both domestic violence and harmful alcohol consumption.
Trial registration
Brazilian Clinical Trials Registry: RBR-7rjt4t . Registered 17 October 2013.
Domestic violence and harmful alcohol consumption are two key public health problems worldwide [ 1 ]. In addition to their high prevalence, both phenomena result in considerable biological, psychological, and sociological repercussions for individuals and the general population [ 1 , 2 ]. These phenomena often co-occur and share a complex set of psychosocial risk factors. However, in-depth studies aimed at supporting interventions to address both phenomena in an integrated manner remain scarce, especially among specific groups such as Latin American women.
Alcohol consumption among women
Although alcoholic beverage consumption remains higher among men, women have significantly increased their consumption because of society’s changing gender roles [ 3 ]. According to the Global Burden of Diseases, Injuries, and Risk Factors Study in 2010 [ 4 ], alcohol consumption is the third leading risk factor for illnesses and disabilities worldwide; furthermore, the World Health Organization (WHO) considered it to be the primary risk factor for “disability-adjusted life years” (DALYs) in Tropical Latin America, which encompasses certain Latin America countries including Brazil. Depending on consumption patterns, alcohol can affect individual’s health due to accidents, dependence, liver cirrhosis, cancer, and injury. Alcohol consumption can also affect the health of other people in community and family settings, specifically due to drinking and driving situations, work absenteeism, drinking during pregnancy, and cases of violence and neglect in the parent–child relationship [ 2 ].
Previous Brazilian surveys suggest that approximately 75 % of the population has consumed alcohol at least once in their lifetime [ 5 ], and nearly 25 % of respondents reported at least one type of drinking-related problem. Furthermore, 3 % meet the criteria for alcohol abuse, and 9 % are alcohol dependent [ 6 ]. These rates varied based on gender, age, marital status, educational level, income, and country region with approximately 4 % of women abusing alcohol or being alcohol dependent [ 7 ].
It has been suggested [ 3 ] that biological factors such as lower body weight and lower fat-to-muscle ratios contribute to faster and more intense effects of alcohol among women. Compared with men, harmful alcohol consumption among women has a disproportionate effect on their lives and health, including undesired consequences regarding reproductive function and pregnancy as well as the faster development of physical, cognitive, social, and psychiatric problems [ 3 , 8 , 9 ].
- Domestic violence
Like alcohol consumption, violence (specifically, domestic violence) has been identified as a priority for WHO actions. Violence is a major public health problem worldwide because it has serious implications for health (in both the short and long term) as well as the psychological and social development of individuals, families, and communities [ 10 , 11 ].
Domestic violence (or family violence) can be understood as “every act or omission committed by some family member in a position of power, regardless of where it occurs, which harms the well-being, physical or psychological integrity, or freedom and right to full development of another family member” [ 12 ]. Violent acts can be classified based on their type, including acts of physical, psychological, and sexual violence; alternatively, they can be expressed as forms of neglect or abandonment [ 11 ]. In the family setting, violence can occur within interpersonal relationships, including those with children, adolescents, men, women, and the elderly [ 13 – 15 ]. Despite the increased emphasis placed on victimized women within partnerships [ 11 ], researchers recognize that women can also be the aggressor in the marital relationship [ 13 , 16 , 17 ] and with regard to their children [ 18 , 19 ].
Some studies suggest that domestic violence is highly prevalent and has a complex network of associations. Some of the factors associated with domestic violence include younger age, lower education level, a history of physical violence in the family, childhood sexual abuse, depression, poor socioeconomic conditions, and problems related to alcohol consumption among one or both members of the couple [ 20 – 23 ]. The consequences of domestic violence can be identified at different levels of life, leading to physical and psychosocial impairments. [ 24 , 25 ]. Therefore, it becomes important to treat family violence as a complex phenomenon, one that tends not to be restricted to a single member of the family [ 22 ].
Domestic violence and alcohol
Although many studies relate alcohol consumption to violent behavior, it is not possible to establish a simple and unidirectional association because of the complexity of this relationship [ 1 , 26 – 29 ]. A population-based study in Brazil found that the aggressor was under the influence of alcohol at the time of the event in over half of the identified cases of domestic violence [ 14 ]. The literature includes several other studies that suggest an association between alcohol consumption and violent behavior among intimate partners [ 1 , 30 – 35 ].
Although some studies have suggested that alcohol consumption is more associated with the severity of violence acts than to increases in its occurrence [ 31 , 36 ], others have suggested that it should be related to both [ 35 ] and that the association between alcohol and violence becomes more powerful with increased consumption [ 26 , 29 ]. To better understand how alcohol consumption might be related to a greater severity of domestic violence, it is important to consider not only the pharmacological effects of alcohol but also the environmental and sociocultural factors that influence patterns of alcohol consumption and violent behaviors [ 31 ].
Alcohol is a risk factor for the occurrence of violent acts because it has direct effects on physical and cognitive performances, contributing to violence by reducing self-control as well as reducing judgment and the ability to recognize signs of danger. Moreover, individual and cultural beliefs that alcohol causes aggression can lead to its intake in preparation or as an excuse/justification for violent acts [ 1 ]. It is also possible that harmful alcohol consumption is a coping strategy adopted by victims to address the stress caused by violent situations [ 1 , 37 ].
Although strong associations seem exist between domestic violence and alcohol abuse among women, few studies have been conducted regarding the peculiarities of this association, especially in developing countries such as Brazil. Given this association, the WHO recommends measures to reduce the availability and the harmful consumption of alcohol as important strategies to prevent violence. There is some evidence on the success of brief interventions (BIs) in reducing various forms of violence, including domestic violence [ 1 ].
Early detection and intervention for harmful alcohol consumption
The early detection of alcohol abuse is essential in preventing the future consequences of this consumption, because it enables the early application of interventions [ 38 – 40 ]. Given that many users do not recognize they have a problem in the early stages, interventions that allow problems to be recognized and behaviors to be changed become necessary.
BIs that are targeted on primary or secondary prevention strategies among alcohol consumers focus on changing an individual’s behaviors through limited-time therapies that can be performed by professionals with different backgrounds [ 39 , 41 ]. Despite the variations in the forms of BIs application (e.g., in person, by phone, or online), the theoretical framework of motivational interviewing [ 42 ] and the principles of cognitive-behavioral therapy are usually employed.
Because BIs are an effective, low-cost strategy for treating problems related to alcohol and drugs, it is also a useful tool for prevention and a way to facilitate the referral of severe cases (e.g., those with alcohol dependence) to specialized treatments [ 38 , 41 , 43 ]. Previous studies have suggested that BIs work for different types of patients and that their effectiveness can be equal to or even better than those of interventions that require more time to complete [ 44 ]. Although BIs have been shown to be effective when performed by skilled professionals or researchers [ 41 , 45 ], in clinical settings or in the context of routine health services, there is a lack of studies regarding the use of these techniques in community household settings. Such an approach should reach populations who do not have access to or choose not seek out the healthcare system; furthermore, it represents an alternative to the difficulties of implementing BIs in the healthcare services.
A comprehensive review of the BIs applied in primary care concluded that this approach decreases alcohol use among men; however, these findings were not extended to women. Therefore, additional research regarding the most effective components of such interventions is needed among this specific population [ 43 ]. Moreover, another literature review [ 46 ] identified promising results for women, despite the significant heterogeneity observed among the analyzed clinical trials. Because the evidence for the effectiveness of BIs remains contradictory among women [ 43 , 46 , 47 ], a well-conducted study that establishes the effectiveness of BIs is necessary for this population group, especially within developing countries. The assessment of BIs in community household settings is especially relevant in Brazil because this country has a strong strategy for primary health services that is focused on providing home care to families.
The current protocol is designed to study the association between alcohol consumption and patterns of domestic violence among women. Study 1 aims to (1) estimate the rates of harmful alcohol consumption and domestic violence (within the couple and that directed toward children) among adult women; (2) assess the association between the sociodemographic and mental health factors with regard to the harmful consumption of alcoholic beverages; and (3) assess the association between the sociodemographic and physical and mental health factors as well as between alcohol consumption and the occurrence of domestic violence (within the couple and that directed toward children).
Nested within Study 1, Study 2 aims to evaluate the effectiveness of BIs on women with harmful alcohol consumption living in a community household setting in reducing their alcohol consumption and patterns of domestic violence (within couples and toward children).
Study design
Study 1 will employ a cross-sectional observational design to investigate the patterns of alcohol consumption and domestic violence using a household survey of women. Study 2 will be a randomized clinical trial (RCT) nested within Study 1 (i.e., the women identified as having harmful alcohol consumption in Study 1 will be invited to take part in the RCT.
The current study will be conducted in Juiz de Fora, Minas Gerais, southeastern Brazil; this city has approximately half a million inhabitants. The study will randomly select women living in two neighborhoods with different average monthly incomes per capita according to the Instituto Brasileiro de Geografia e Estatística (Brazilian Institute of Geography and Statistics; IBGE) census conducted in 2000. This categorization will be used to investigate two populations with different income profiles.
To calculate the sample size needed for this cross-sectional study, the data from a previous study (which estimated the prevalence of harmful alcohol consumption among women in Juiz de Fora as approximately 9.1 %) will be considered [ 48 ]. In addition, this study considered a maximum measurement error of 3 %, 95 % confidence intervals, a finite population correction based on the number of women residing in the randomly selected neighborhoods (consistent with the 2000 IBGE census), an effect of the sampling design equal to 2, and a 25 % refusal to participate rate. Thus, the initial sample size was estimated as 824 respondents (412 in each neighborhood).
To calculate the clinical trial sample size, the following considerations will be made: (i) a significance level of 5 %; (ii) a statistical power of 80 % (to compare proportions of the two independent groups); (iii) a non-interview rate of 15 % due to refusal to participate or failure to locate the informant; (iv) the effect of the BI after 3 months (i.e., an expected reduction of at least 20 % in the number of women with harmful alcohol consumption; and (v) an effect of the sampling design equal to 2. Thus, the calculated sample size for each group (i.e., the treated group [TG] and control group [CG]) will be 73 women.
To make the second study possible, considering the prevalence of women with risky alcohol consumption in the two neighborhoods surveyed around the estimated above (ie, 9.1 %), there will be necessary an increase in the sample size for Study 1, which now has approximately 1600, with 800 in each of the neighborhoods.
To recruit the women who belong to the target population, a two-stage cluster sampling method will be adopted. The streets belonging to each neighborhood will be considered as primary sampling units (PSUs), and households will be considered as secondary sampling units (SSUs). To select PSUs, a simple random sampling method without replacement will be adopted, whereas the SSUs will be selected using systematic sampling. In each selected household, the field researchers will invites all women who met the inclusion criteria to participate in the study.
Inclusion criteria
Female residents in the two neighborhoods who are aged 18–60 years, literate, and without obvious cognitive impairments will comprise the target sample. Domestic violence behaviors will be investigated among women who have children of aged up to 18, husbands or partners, or both residing in the same household.
Measurements
Participant sociodemographic characteristics.
Information concerning ethnicity, age, education level, religion, occupation, marital status, and number of children will be obtained. Among women who are married or cohabitating, information regarding the duration of their relationship will be obtained along with the sociodemographic characteristics of their partners (e.g., age, education level, and occupation).
Alcohol consumption
Alcohol consumption will be assessed using the Alcohol Use Disorders Identification Test (AUDIT), a screening tool developed by the WHO [ 49 ] that consists of 10 questions: 3 concerning consumption amount and frequency, 3 regarding dependence symptoms, and 4 concerning personal and social problems related to alcohol abuse. The final score reflects the following alcohol consumption levels or patterns: abstainers/low risk (0–7 points), hazardous use (8–15 points), harmful use (16–19 points), and probable dependence (20–40 points). The AUDIT has been previously validated in several countries, including Brazil, and shows good sensitivity (mean = 0.90) and specificity (mean = 0.80) regarding the detection of harmful alcohol consumption [ 49 , 50 ].
Information concerning the respondents’ use of any healthcare service over the previous 3 months, the approach of health professionals regarding respondents’ alcohol consumption, respondent participation in any treatment for alcohol consumption, and the respondents’ perceptions of their partners’ alcohol consumption will also be obtained.
Consumption of other substances
Information regarding the consumption of tobacco, marijuana, amphetamines, benzodiazepines, antidepressants, and cocaine over the three months preceding the interview will be obtained.
A structured 15-question instrument concerning the respondents’ general health and the presence of specific diseases such as hypertension, diabetes, and heart problems will be administered.
The population-based screening scale for depression from the Center for Epidemiologic Studies (i.e., the CES-D) will be used. This screening instrument seeks to identify depressive symptoms within adult population-based studies [ 51 ]. Consisting of 20 items, its total score ranges from 0 to 60 points, with the higher scores indicating a greater amount of depressive symptoms. The cutoff of 16 points is often used to classify individuals as having possible depression. The CES-D has been previously validated for use in Brazil and shows satisfactory levels of reliability [ 52 , 53 ].
The Revised Conflict Tactics Scales (CTS2) will be employed to collect information on violence between intimate partners, whereas the Parent–child Conflict Tactics Scales (CTSPC) will be used to assess domestic violence by women against their children.
The CTS2 was designed to assess violence within couples, and it provides data on the respondent and her partner. This survey consists of 78 items, and each item is displayed in a set of two questions. The first question of each set refers to a possible behavior of the respondent, whereas the second refers to the same action but experienced by the partner. This instrument consists of 5 subscales that address the occurrence of negotiation, psychological aggression, physical violence, consequences of violence affecting the health of the respondent and her partner (i.e., injuries), and sexual coercion within the relationship. The CTS2 shows an internal consistency between 0.65–0.86 and an intra-observer reliability (kappa) above 0.75 when evaluated in Brazilian samples to assess its conceptual equivalence, semantic equivalence, and psychometric properties [ 54 – 56 ].
The CTSPC was designed based on the refinement of the previous instrument, and it addresses the parent–child relationship. This instrument is composed of questions regarding the occurrence of certain behaviors directed at children. Its 22 items are divided into three levels: nonviolent discipline (e.g., explaining errors and applying punishment), psychological aggression (e.g., swearing, screaming, threatening to kick the child out, or hitting), and physical assault (e.g., face slapping, throwing the child on the floor, or threatening with a knife); the latter was subdivided into corporal punishment, physical abuse, and severe physical abuse. The CTSPC had previously been cross-culturally adapted for use in Brazil; furthermore, prior work found that its internal consistency ranged from 0.49–0.68, and estimates of its intra-observer reliability (kappa) were above 0.75 [ 57 , 58 ].
According to Straus [ 59 ] (the author of the CTS2 and CTSPC), these instruments investigate the occurrence of behaviors that, unlike emotions, attitudes, and beliefs, are less susceptible to distortions with regard to the interpretation of facts. Importantly, the methodological choice for these assessments reflects an understanding of domestic violence as a complex phenomenon that tends not to remain restricted to only one member of the family [ 58 ]. Furthermore, research indicates that violent acts are typically reciprocal, i.e., the respondent might be both the aggressor and the victim [ 60 ].
The information regarding alcohol consumption provided by the respondent and her partner during episodes of violence will also be incorporated by adapting the violence scales. After each CTS2 and CTSPC item, the interviewer will ask whether one of the involved individuals was under the influence of alcohol when the event occurred.
The CTS2 and CTSPC will be self-applied, whereas all of the other instruments will be administered to participants during interviews. Except for the CES-D, which refers to the events of the previous week, all of the instruments will be adapted to consider a time period of three months.
Study 1: Household survey
A researcher will approach the participants at their homes; all of the instruments will be administered there. The interviews will take approximately 30 min to complete and will be held in a place as private as possible to allow the interviewees to freely answer questions and increase the credibility of their answers.
The researchers will be properly trained women who will initially approach the participants to invite them to volunteer for the survey, delivering a document that describes the study and its objectives. The training of the team will consist of attending lectures on domestic violence, alcohol consumption, BIs, the project details, a clarification of the study’s procedures, and an explanation of the questionnaires. Furthermore, the importance of research ethics will be emphasized. The researchers will gain familiarity with the instruments by administering them to a colleague. Training will be provided on the application of a BI via videos and role-playing techniques.
To locate the women living in the randomly selected households, at least three visits will be made to each household. When a resident is not found at her supposed address, the researchers will seek information from the neighbors to identify the existence of any women who meet the eligibility criteria for the study and the best days and times to approach them.
Study 2: Random clinical trial
The data collection for Study 2 will be conducted concomitantly using the women detected in Study 1. Women with AUDIT scores equal to or above 8 will be considered as hazardous alcohol users and randomly allocated into one of two groups: the TG or the CG. The TG will receive a single BI after the instrument is administered, whereas the CG will not receive BI until after the end of the study.
The participants will be allocated using a list of random numbers. Three months after the BI, all instruments except for the sociodemographic questionnaire will be re-administered to both groups. Because of ethical reasons, a BI session will also be offered to the CG after the second evaluation, at the end of the study. Independent interviewers will perform the baseline and the follow-up interview.
The intervention
The BI will be performed at the participants’ households in accordance with the model proposed by Miller and Sanchez [ 61 ], the principles of which are summarized by the acronym “FRAMES”. This acronym stands for “Feedback” (provide information regarding the score obtained on the screening instrument), “Responsibility” (the patient must take responsibility for changing their behavior), “Advice” (guidance on issues related to the use of substances and coping strategies), “Menu of options” (a list of options or alternative behaviors to substance use), “Empathy” (putting one’s self in another’s shoes based on one’s own assumptions to try to understand their behavior), and “Self-efficacy” (patients’ belief in their ability to change).
The timing of the BI will be controlled, ranging from 15 to 40 min. After administering the procedure, the researcher will record the approach used and the participant’s behavior during the intervention.
This study has been approved by Ethics Committee of the Federal University of São Paulo (Universidade Federal de São Paulo; UNIFESP- registration number 0699/10). The study has also been registered in the Brazilian Clinical Trials Registry (ReBEC; registration number: RBR-7rjt4t).
All participants will receive information about the study, and their participation will be voluntary. Each participant will be required to sign an informed consent document. At the end of the interviews, all participants will receive an informational leaflet regarding the use of alcoholic beverages, as well as a guide concerning health services and psychosocial assistance in cases of violence and alcohol dependence. After the follow-up assessment is performed three months after the screening, the BI will be applied to participants in the CG. Women who score in the range of “probable alcohol dependence” (i.e., 20 points or more on the AUDIT) will be instructed to seek specialized treatment, regardless of the group to which they are allocated.
Statistical analyses
Given the characteristics of the adopted sampling design, the data will be processed and analyzed using the statistical software STATA version 11.
Initially, exploratory bivariate analyses will be conducted to assess the associations between the variables of interest and the possible risk factors. Chi-square tests will be used to test the association between categorical variables, whereas Student’s t -test will be used to compare the means of continuous variables.
A logistic regression model will be used to examine the patterns of alcohol consumption with the response variable and the sociodemographic and health characteristics as explanatory variables. A separate logistic regression model will be used with the type of violence as dependent variable and the sociodemographic and health characteristics, and alcohol consumption patterns as explanatory variables.
The TG and CG will be compared using t-tests and generalized linear models with repeated-measures.
Both alcohol consumption among women and violence within the family are relevant public health problems which are mediated by cultural and contextual factors [ 20 ]. Despite the purported associations between these phenomena, studies providing information on their characteristics among women using community samples are scarce in Brazil [ 19 , 21 , 62 ].
This study includes a household survey with representative samples of two neighborhoods with different socioeconomic profiles in Brazil, a developing country where well-conducted household surveys remain rare. Although the cross-sectional design does not allow for the inference of causality, this approach will broaden the discussion on the relationship between alcohol consumption and violence, considering the individual and environmental aspects involved in these phenomena.
This study not only proposes to present a better understanding of violence in the lives of women (regardless of its association with alcohol consumption) but also expand the discussion regarding the possible public healthcare strategies and actions needed to prevent domestic violence and harmful alcohol consumption [ 1 ]. With regard to alcohol, the use of a BI in a community household setting represents a new method of prevention that could have indirect effects on domestic-violence-related problems.
We believe that this protocol has the potential to support supplementary studies aiming to promote knowledge regarding two of the most important public health problems from different perspectives: harmful alcohol consumption and domestic violence. Furthermore, we believe that the results of this study might influence both clinical practice and prevention efforts in the context of public health.
Abbreviations
Alcohol use disorders identification test
- Brief intervention
Center for epidemiologic studies depression scale
Revised conflict tactics scales
Parent–child conflict tactics scales
Disability-adjusted life years
Brazilian institute of geography and statistics
World health organization
World Health Organization. Violence prevention: The evidence. Preventing violence by reducing the availability and harmful use of alcohol. Geneva: World Health Organization; 2009. p. 18.
Google Scholar
World Health Organization. Global status report on alcohol and health. Geneva: World Health Organization; 2011. p. 286.
World Health Organization. Gender, health and alcohol use. Geneva: WHO Department of Gender, Women and Health; 2005.
Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–223.
Article PubMed Google Scholar
Galduroz JC, Carlini EA. Use of alcohol among the inhabitants of the 107 largest cities in Brazil--2001. Braz J Med Biol Res = Revista Bras Pesquisas Med Biol/Soc Bras Biofisica [et al]. 2007;40(3):367–75.
CAS Google Scholar
Laranjeira R, Pinsky I, Sanches M, Zaleski M, Caetano R. Alcohol use patterns among Brazilian adults. Rev Bras Psiquiatr. 2010;32(3):231–41.
Caetano R, Madruga C, Pinsky I, Laranjeira R. Drinking patterns and associated problems in Brazil. Adicciones. 2013;25(4):287–93.
Kay A, Taylor TE, Barthwell AG, Wichelecki J, Leopold V. Substance use and women’s health. J Addict Dis. 2010;29(2):139–63.
Nilsen P. Brief alcohol intervention to prevent drinking during pregnancy: an overview of research findings. Curr Opin Obstet Gynecol. 2009;21(6):496–500.
García-Moreno C, Jansen H, Ellsberg M, Heise L, Watts C. WHO multi-country study on women’s health and domestic violence against women. Geneva: World Health Organization; 2005.
Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002;360(9339):1083–8.
Shrader E, Sagot, M. Domestic violence: women's way out. Pan American Health Organization [PAHO]. Washington, DC. 2000. x, 124 p.
Dossi AP, Saliba O, Garbin CA, Garbin AJ. [Epidemiological profile of domestic violence: Complaints of aggression filed in a city in Sao Paulo State, Brazil from 2001 to 2005]. Cadernos Saude Publica. 2008;24(8):1939–52.
Article Google Scholar
Fonseca AM, Galduroz JC, Tondowski CS, Noto AR. Alcohol-related domestic violence: A household survey in Brazil. Rev Saude Publica. 2009;43(5):743–9.
Rodriguez Franco L, Lopez-Cepero J, Rodriguez Diaz FJ. [Domestic violence: A bibliographic and bibliometric review]. Psicothema. 2009;21(2):248–54.
PubMed Google Scholar
Archer J. Sex differences in physically aggressive acts between heterosexual partners: A meta-analytic review. Aggress Violent Behav. 2002;7(4):313–51.
Moore TM, Stuart GL, Meehan JC, Rhatigan DL, Hellmuth JC, Keen SM. Drug abuse and aggression between intimate partners: A meta-analytic review. Clin Psychol Rev. 2008;28(2):247–74.
Canha J. The child victim of violence. In: Machado C, Gonçalves RA, editors. Orgs.) [Violence and crime victims] (vol.2, 3rd edition,pp 17–37. Portugal: Editora Quarteto; 2008.
Zaleski M, Pinsky I, Laranjeira R, Ramisetty-Mikler S, Caetano R. Intimate partner violence and contribution of drinking and sociodemographics: The Brazilian National Alcohol Survey. J Interpers Violence. 2010;25(4):648–65.
Abramsky T, Watts CH, Garcia-Moreno C, Devries K, Kiss L, Ellsberg M, et al. What factors are associated with recent intimate partner violence? Findings from the WHO multi-country study on women’s health and domestic violence. BMC Public Health. 2011;11:109.
Article PubMed PubMed Central Google Scholar
d’Oliveira AFPL, Schraiber LB, Franca I, Ludermir AB, Portella AP, Diniz CS, et al. Factors associated with intimate partner violence against Brazilian women. Rev Saude Publica. 2009;43(2):299–310.
Reichenheim ME, Dias AS, Moraes CL. [The co-occurrence of physical violence against partners and their children in health services]. Rev Saude Publica. 2006;40(4):595–603.
Gilchrist G, Hegarty K, Chondros P, Herrman H, Gunn J. The association between intimate partner violence, alcohol, and depression in family practice. BMC Fam Pract. 2010;11:72.
Johnson MP: Differentiating among types of domestic violence. Marriage and family: Perspectives and complexities 2009:281–297.
Tolan P, Gorman-Smith D, Henry D. Family violence. Annu Rev Psychol. 2006;57:557–83.
Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, et al. Alcohol: No ordinary commodity. Research and public policy. Oxford: Oxford University Press; 2003.
Bennett L, O’Brien P. Effects of coordinated services for drug-abusing women who are victims of intimate partner violence. Violence Against Women. 2007;13(4):395–411.
Laranjeira R, Duailibi SM, Pinsky I. [Alcohol and violence: Psychiatry and public health]. Rev Bras Psiquiatr. 2005;27(3):176–7.
Moreira TC, Belmonte EL, Vieira FR, Noto AR, Ferigolo M, Barros HM. Community violence and alcohol abuse among adolescents: A sex comparison. J Pediatr (Rio J). 2008;84(3):244–50.
Boden JM, Fergusson DM, Horwood LJ. Alcohol misuse and violent behavior: Findings from a 30-year longitudinal study. Drug Alcohol Depend. 2012;122(1–2):135–41.
Graham K, Bernards S, Wilsnack SC, Gmel G. Alcohol may not cause partner violence but it seems to make it worse: A cross-national comparison of the relationship between alcohol and severity of partner violence. J Int Violence. 2011;26(8):1503–23.
Kaplan LM, Hill TD, Mann-Deibert GR. Does alcohol consumption exacerbate the mental health consequences of interpersonal violence? Violence Against Women. 2012;18(3):289–308.
Selic P, Pesjak K, Kersnik J. The prevalence of exposure to domestic violence and the factors associated with co-occurrence of psychological and physical violence exposure: A sample from primary care patients. BMC Public Health. 2011;11:621.
Tartakovsky E, Mezhibovsky S. Female immigrant victims of domestic violence: A comparison between immigrants from the former Soviet Union in Israel and Israeli-born women. J Fam Violence. 2012;27(6):561–72.
Tumwesigye NM, Kyomuhendo GB, Greenfield TK, Wanyenze RK. Problem drinking and physical intimate partner violence against women: Evidence from a national survey in Uganda. BMC Public Health. 2012;12:399.
Leonard KE. Alcohol and intimate partner violence: When can we say that heavy drinking is a contributing cause of violence? Addiction. 2005;100(4):422–5.
Kaysen D, Dillworth TM, Simpson T, Waldrop A, Larimer ME, Resick PA. Domestic violence and alcohol use: Trauma-related symptoms and motives for drinking. Addict Behav. 2007;32(6):1272–83.
Babor TF, Higgins-Biddle JC. Brief interventions for alcohol abuse in primary health care. Ribeirão Preto: PAI-PAD; 2003.
Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT): Toward a public health approach to the management of substance abuse. Subst Abus. 2007;28(3):7–30.
Ronzani TM, Mota DC, Souza IC. Alcohol prevention within primary care in municipalities in the state of Minas Gerais, southeastern Brazil. Rev Saude Publica. 2009;43 Suppl 1:51–61.
Nilsen P, Kaner E, Babor TF. Brief intervention, three decades on. Nordic Stud Alcohol Drugs. 2008;25:6.
Miller WR, Rollnick S: Motivational interviewing: Preparing people for change. New York: Guilford press; 2002.
Kaner EFS, Dickinson HO, Beyer FR, Pienaar E, Campbell F, Schlesinger C, Heather N, Saunders JB, Burnand B, Pienaar ED. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database of Systematic Reviews 2007(2), DOI: 10.1002/14651858.CD004148.pub3 .
Formigoni MLOS, Ronzani TM. [Effectiveness and cost-benefit ratio of brief interventions] in: [national antidrug secretariat – senad. (org.) system for the detection of theabuse, use of and addition to psychoactive substances - SUPERA]. 2ed. Basília Senad - Governo Federal. 2008;4:58–63.
Aasland OG, Nygaard P, Nilsen P. The long and winding road to widespread implementation of screening and brief intervention for alcohol problems: A historical overview with special attention to the WHO initiatives. Nordic Stud Alcohol Drugs. 2008;25(6):469–76.
Gebara CF, Bhona FM, Ronzani TM, Lourenco LM, Noto AR. Brief intervention and decrease of alcohol consumption among women: A systematic review. Substance Abuse Treat Prevent Policy. 2013;8:31.
Floyd RL, Weber MK, Denny C, O’Connor MJ. Prevention of fetal alcohol spectrum disorders. Dev Disabil Res Rev. 2009;15(3):193–9.
Amato TC, Silveira PS, Oliveira JS, Ronzani TM. Use of alcoholic drinks, religion and other sociodemographic characteristics in primary health care patients - Juiz de Fora, MG, Brazil - 2006. SMAD Revista Eletrônica Saúde Mental Alcool Drogas. 2008;4(2):00.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG: The alcohol-use disorders identification test. Guidelines for use in primary care, Second Edition, Department of Mental Health and SubstanceDependence, World Health Organization; 2001.
Lima CT, Freire AC, Silva AP, Teixeira RM, Farrell M, Prince M. Concurrent and construct validity of the audit in an urban Brazilian sample. Alcohol. 2005;40(6):584–9.
Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401.
Fleck MP, Lima AF, Louzada S, Schestasky G, Henriques A, Borges VR, et al. [Association of depressive symptoms and social functioning in primary care service, Brazil]. Rev Saude Publica. 2002;36(4):431–8.
Silveira DX, Jorge MR. [Psychometric properties of the epidemiologic screening scale for depression (CES-D) in clinical and non-clinical populations of adolescents and young adults]. Psiq Clin. 1998;25:251–61.
Moraes CL, Hasselmann MH, Reichenheim ME. [Portuguese-language cross-cultural adaptation of the Revised Conflict Tactics Scales (CTS2), an instrument used to identify violence in couples]. Cadernos de Saude Publica. 2002;18(1):163–76.
Moraes CL, Reichenheim ME. Cross-cultural measurement equivalence of the Revised Conflict Tactics Scales (CTS2) Portuguese version used to identify violence within couples. Cadernos Saude Publica. 2002;18(3):783–96.
Reichenheim ME, Klein R, Moraes CL. Assessing the physical violence component of the revised conflict tactics scales when used in heterosexual couples: An item response theory analysis. Cadernos Saude Publica. 2007;23(1):53–62.
Reichenheim ME, Moraes CL. [A Portuguese-language cross-cultural adaptation of the parent–child conflict tactics scales (CTSPC), an instrument used to identify parental violence against children]. Cadernos Saude Publica. 2003;19(6):1701–12.
Reichenheim ME, Moraes CL. The psychometric properties of the Portuguese version of the Conflict Tactics Scales: Parent–child version (CTSPC) used to identify child abuse. Cadernos Saude Publica. 2006;22(3):503–15.
Straus MA. Blaming the messenger for the bad news about partner violence by women: The methodological, theoretical, and value basis of the purported invalidity of the conflict tactics scales. Behav Sci Law. 2012;30(5):538–56.
Whiting JB, Simmons LA, Havens JR, Smith DB, Oka M. Intergenerational transmission of violence: The influence of self-appraisals, mental disorders, and substance abuse. J Fam Violence. 2009;24(8):639–48.
Miller WR, Sanchez V. Motivating young adults for treatment and lifestyle change. In: Howard G, editor. Issues in alcohol use and misuse by young adults. Notre Dame IN: University of Notre Dame Press; 1993.
Zanoti-Jeronymo DV, Zaleski M, Pinsky I, Caetano R, Figlie NB, Laranjeira R. [Prevalence of physical abuse in childhood and exposure to parental violence in a Brazilian sample]. Cadernos Saude Publica. 2009;25(11):2467–79.
Download references
Acknowledgments
This study is developed with the support of the following agencies: the São Paulo Research Foundation (FAPESP; Fundação de Amparo à Pesquisa do Estado de São Paulo; processes no.: 2010/51094-7 and no.: 10/51837-0), the National Council of Technological and Scientific Development (CNPq; Conselho Nacional de Desenvolvimento Cientifico e Tecnológico, process no.: 400675/2010-2) and the Research Incentive Fund Association (AFIP; Associação Fundo de Incentivo à Pesquisa).
This study has been funded by the São Paulo Research Foundation (FAPESP; Fundação de Amparo à Pesquisa do Estado de São Paulo; processes nº: 2010/51094-7 and nº: 2010/51837-0) and the National Council of Technological and Scientific Development (CNPq; Conselho Nacional de Desenvolvimento Cientifico e Tecnológico, process nº: 400675/2010-2). The study also has been developed with the support of the Research Incentive Fund Association (AFIP; Associação Fundo de Incentivo à Pesquisa).
Author information
Authors and affiliations.
Department of Psychobiology, Research Center on Health and Substance Use (NEPSIS), Universidade Federal de São Paulo (UNIFESP), Botucatu St., 862-First floor, São Paulo, SP, 04023-062, Brazil
Carla Ferreira de Paula Gebara, Cleusa Pinheiro Ferri & Ana Regina Noto
Department of Psychology, Center for Studies on Violence and Social Anxiety (NEVAS), Universidade Federal de Juiz de Fora (UFJF), Juiz de Fora, MG, Brazil
Lelio Moura Lourenço & Fernanda Monteiro de Castro Bhona
Department of Statistics, Universidade Federal de Juiz de Fora (UFJF), Juiz de Fora, MG, Brazil
Marcel de Toledo Vieira
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Carla Ferreira de Paula Gebara .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
CG, AN, LL and FB participated in the study design and the definition of objectives and goals of the study. MV was responsible for the sample design. CF made the proposal of the statistical analyzes. CG, AN and CF drafted the manuscript and made the final revision of the text. All authors read and approved the final manuscript.
Authors’ information
CG was a PhD student from the Department of Psychobiology of Universidade Federal de São Paulo (UNIFESP). FB is a PhD student from the Department of Psychology of Universidade Federal de Juiz de Fora (UFJF). MV is a professor from the Department of Statistics of UFJF and LL is a professor from the Department of Psychology of UFJF. CF and AN are professors from the Department of Psychobiology of UNIFESP. CG, AN and CF are researchers of Research Center on Health and Substance Use (NEPSIS), FB and LL are researchers of Center for Studies on Violence and Social Anxiety (NEVAS).
Availability of data and materials
Not applicable.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Gebara, C.F.d.P., Ferri, C.P., Lourenço, L.M. et al. Patterns of domestic violence and alcohol consumption among women and the effectiveness of a brief intervention in a household setting: a protocol study. BMC Women's Health 15 , 78 (2015). https://doi.org/10.1186/s12905-015-0236-8
Download citation
Received : 19 December 2014
Accepted : 17 September 2015
Published : 24 September 2015
DOI : https://doi.org/10.1186/s12905-015-0236-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Search Menu
- Advance articles
- Author Guidelines
- Submission Site
- Open Access
- About Epidemiologic Reviews
- About the Johns Hopkins Bloomberg School of Public Health
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Abbreviations, introduction, acknowledgments.
- < Previous
Drug Use Disorders and Violence: Associations With Individual Drug Categories
- Article contents
- Figures & tables
- Supplementary Data
Shaoling Zhong, Rongqin Yu, Seena Fazel, Drug Use Disorders and Violence: Associations With Individual Drug Categories, Epidemiologic Reviews , Volume 42, Issue 1, 2020, Pages 103–116, https://doi.org/10.1093/epirev/mxaa006
- Permissions Icon Permissions
We conducted a systematic review that examined the link between individual drug categories and violent outcomes. We searched for primary case-control and cohort investigations that reported risk of violence against others among individuals diagnosed with drug use disorders using validated clinical criteria, following Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. We identified 18 studies published during 1990–2019, reporting data from 591,411 individuals with drug use disorders. We reported odds ratios of the violence risk in different categories of drug use disorders compared with those without. We found odds ratios ranging from 0.8 to 25.0 for most individual drug categories, with generally higher odds ratios among individuals with polydrug use disorders. In addition, we explored sources of between-study heterogeneity by subgroup and meta-regression analyses. Cohort investigations reported a lower risk of violence than case-control reports (odds ratio = 2.7 (95% confidence interval (CI): 2.1, 3.5) vs. 6.6 (95% CI: 5.1, 8.6)), and associations were stronger when the outcome was any violence rather than intimate partner violence (odds ratio = 5.7 (95% CI: 3.8, 8.6) vs. 1.7 (95% CI: 1.4, 2.1)), which was consistent with results from the meta-regression. Overall, these findings highlight the potential impact of preventing and treating drug use disorders on reducing violence risk and associated morbidities.
confidence interval
Drug misuse is a global public health concern ( 1 , 2 ). Worldwide, around 70 million individuals were diagnosed with a drug use disorder ( 1 ). Drug use disorders have been associated with a wide range of adverse outcomes, including suicide, comorbid mental illness, and premature mortality ( 3–5 ). In addition, drug use disorders increase risk of violence against others ( 3 , 6–9 ). Further, the prevalence of drug use disorder in prison ranges from 10% to 61% in men and 30% to 69% in women ( 10 ), which is substantially elevated compared with the prevalence, ranging from 0.6% to 4.0% in men and 0.3% to 2.9% in women, in the general population ( 11 ).
The prevalence differs between individual categories of drug use disorders. Globally, the prevalence rate per 100,000 people is 65 for stimulants such as amphetamines, 78 for cocaine, 290 for cannabis, 353 for opioids, and less than 52 for other drugs including hallucinogens and sedatives ( 12 ). Although research has consistently found increased violence risk in drug use disorders, individual studies have shown that the magnitude of this increased risk varies depending on the drug category. For example, when compared with the general population, odds ratios of violence in cannabis use disorder have ranged from 1 to 7 ( 13–17 ), and in cocaine, they have varied from 2 to 11 ( 18–21 ). This might be due to different methodologies adopted and specific outcomes used in different studies. Furthermore, it has been suggested that certain type of stimulants, such as crack cocaine, that are associated with irritability and aggressiveness ( 7 , 22 ), might have a higher risk of criminal behavior than others, including less-strong forms of cannabis that might reduce risks due to sedative and calming effects ( 23 , 24 ). This is important to clarify further in that more precise estimates would allow for risk stratification, better treatment allocation (especially if liaison with criminal justice agencies is required), and more evidence-based estimates of the population impact of certain drug policies.
Previous reviews have explored associations between general drug misuse and violence against others but have mostly investigated selected samples, such as prisoners ( 25 ) or psychiatric patients ( 26–29 ). In addition, most existing reviews have not used standardized clinical criteria to identify drug use disorders ( 22 , 30 ). This could introduce bias given that self-report of the extent of drug use is often unreliable ( 31 ). Validated diagnostic tools based on validated criteria (such as the Diagnostic and Statistical Manual of Mental Disorders or International Classification of Diseases ) can identify individuals with a severe form of drug misuse, who might present to clinical and addiction services, and for whom there is evidence-based treatment available. In addition, diagnostic categories enable consistent communication between clinicians and researchers because the criteria are widely known and validated cross-culturally with decent reliability measures ( 32 , 33 ). Furthermore, the most recent review that examined the link between general drug use disorders and violence was conducted more than 2 decades ago ( 34 ) and did not explore potential source of between-study heterogeneity or differences between individual categories of druguse.
The link between drug use and violent outcomes is complex; a wide range of factors—such as experiences of violence including both as victim and perpetrator, the comorbidity of other mental disorders, and social determinants such as sex, ethnicity, and poverty—might moderate and mediate this link. For instance, previous violence victimization might trigger development of drug use disorders, which might in turn lead to later perpetration of violence ( 35–39 ). Moreover, structural causes of drug use problems are relevant, given that they have been linked to criminalization ( 23 ), as well as factors such as poverty ( 40 ), poor mental health ( 4 , 41 ), treatment availability ( 42 ), and homelessness ( 43 ). In addition, physical and psychological effects of drugs can lead to agitation, aggression, and cognitive impairment that might in turn heighten risk of violence. Individuals with drug use disorders might also turn to violence to finance their drug use, and disputes within illegal drug markets might be associated with violence ( 44 ). To address these gaps in the evidence, in this review, we aimed to synthesize the odds of violence in individual drug use disorders and explore sources of heterogeneity between studies.

Flowchart of systematic search strategy of primary studies on drug use disorders and violence in multiple countries, 1990–2019.
We conducted this review following the Meta-analyses of Observational Studies in Epidemiology (MOOSE) ( 45 ) and Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines ( 46 ). The study was registered with an international prospective register of systematic reviews (PROSPERO CRD42019119533).

Search strategy
We conducted searches in the following digital databases from the inception of the databases (dated from January 1, 1927) to February 18, 2019: PubMed, Web of Science, Embase, Ovid MEDLINE, PsycINFO, Global Health, and US National Criminal Justice Reference Service Abstract Database. We used a combination of search terms related to drug misuse (i.e., illegal drug OR illegal substance OR marijuana OR cocaine OR cannabis OR opioid OR heroin OR methamphetamine OR stimulant*) AND violence (i.e., violen* OR crim* OR homicide OR aggress* OR offen*) AND study design (i.e., cohort OR longitudinal OR follow-up OR prospective OR case-control). We included studies of both illegally and legally obtained drugs. There were no language restrictions, and non-English-language articles were translated. We also scanned reference lists in an attempt to identify additional articles. We searched for unpublished literature including conference proceedings, theses, and dissertations. The first author (S.Z.) conducted the initial screening of the titles and abstracts for inclusion and exclusion. S.Z. and R.Y. screened full-text publications for eligibility. Any uncertainties were discussed with S.F.
Study selection
Inclusion criteria were: 1) cohort and case-control studies that examined link between individual categories of drug use disorders and violent outcomes and provided data for calculation of odds ratio between individuals with and without the drug use disorder being studied, and eligible case-control studies were those that reported prevalence of drug use disorders in cases with and without violence perpetration; 2) investigations that reported drug use disorders (or, in older studies, equivalent diagnostic categories of drug abuse or dependence) meeting diagnostic criteria for Diagnostic and Statistical Manual of Mental Disorders and International Classification of Diseases ; and 3) studies that reported violent outcomes, including any violence and not being limited to context (e.g., community, domestic, intimate partner), type of crime (e.g., homicide, assault, threat or intimidation, and all sexual offenses), and measures (self-report, family report, or official/criminal records).
We excluded: 1) animal investigations; 2) experimental, cross-sectional, qualitative studies, or randomized controlled trials; 3) investigations with within-individual designs; 4) studies that used self-report ( 47 ) (e.g., Addiction Severity Index) or urine tests to identify drug use or that did not separate drug misuse from alcohol and nicotine misuse; 5) reports with recidivism or reoffending as outcomes ( 48 ); 6) studies in selected samples (e.g., offenders, cohorts with mental disorders) so we could increase the generalizability of risk estimates to the general population; 7) investigations that used the nonspecific outcome of all criminal behavior, antisocial behavior, or delinquency, which was not broken down for violence specifically; 8) studies that reported selected participants under medication (e.g., antidepressant, antipsychotic drugs, or other prescription drugs) or individuals undergoing other interventions for drug use disorders; or 9) case-series studies or reviews.
In case of duplicate samples, we included the study that was most recent, used the most common outcome, or had the largest sample. If a study reported outcomes at multiple time points, outcomes with the longest follow-up period were included.
Data extraction
We used a standardized form to extract data. The following information was recorded: study design, country, sample characteristics, diagnostic criteria, category of drug use disorders, type of drugs, comparison group, sex, age, years of follow-up, and study period. S.Z. conducted the initial data extraction. In case of uncertainties, R.Y. and S.F. were consulted.
Statistical analysis
Quality of the individual study was assessed using the Newcastle-Ottawa Quality Assessment Scale ( 49 ). Heterogeneity was estimated using I 2 . I 2 is reported as a percentage out of 100%, where 0%–40% represents low heterogeneity, 30%–60% might indicate moderate heterogeneity, 50%–90% might denote substantial heterogeneity, and 75%–100% might indicate considerable heterogeneity ( 50 , 51 ). All effect sizes were converted into odds ratios and converted from Pearson’s r and Cohen’s d using standard approaches ( 52 ). Sources of heterogeneity were explored using subgroup analyses and meta-regression analyses. Meta-regression was conducted to estimate the extent to which one or more measured covariates (the same variables as used in the subgroup analysis) explained the observed heterogeneity in risk estimates between primary studies ( 50 ). The same variables were used in the subgroup and meta-regression analyses, and only nonoverlapping samples were included in the analyses. When testing the effect of sample size, we excluded 2 studies that were disproportionately large ( 53 , 54 ). We set the years of follow-up as a continuous variable and also a dichotomous variable using the median period as the cut-off. Other analyses included estimating associations between drug use disorders and violence while excluding studies published before 2000 and subgroup analyses by different comparison groups. We tested publication bias using Egger’s test ( 55 ), with P < 0.05 indicating publication bias. Analyses were performed using STATA, version 13 (StataCorp LP, College Station, Texas).
We identified 18 eligible studies (for details, see Figure 1 and Table 1 ) that included 591,411 individuals with drug use disorders. Studies were from 5 countries: 14 from the United States ( n = 542,393, 91.7%) ( 53 , 54 , 56–67 ) and 1 each from New Zealand ( n = 182, 0.03%) ( 68 ), Denmark ( n = 43,403, 7.3%) ( 69 ), the Netherlands ( n = 5,303, 0.9%) ( 70 ), and Turkey ( n = 130, 0.02%) ( 71 ). Eight studies used case–control designs ( 53 , 54 , 56 , 58 , 63 , 66 , 67 , 71 ); the remaining 10 studies were longitudinal cohorts with a median follow-up of 9.5 years.
Summary of Included Studies on Risk of Violence in Drug Use Disorders
Abbreviations: DSM, Diagnostic and Statistical Manual of Mental Disorders ; ICD, International Classification of Diseases ; N/A, not available; WHO-CIDI; World Health Organization’s Composite International Diagnostic Interview.
a Non–drug, non–drug use disorder, and non–drug addicts served as a control group and they refer to people who might have used drugs before but did not meet diagnostic criteria for any drug use disorders. “Healthy volunteers without substance use disorders” refers to healthy volunteers without drug or alcohol use disorders.
In 16 investigations, diagnosis was made using the Diagnostic and Statistical Manual of Mental Disorders (version 3 onward). One study adopted the International Classification of Diseases , Eighth Revision ( 69 ), and 1 provided both International Classification of Diseases , Tenth Revision , and Diagnostic and Statistical Manual of Mental Disorders–IV diagnoses ( 63 ).
For outcome measurement, 2 studies used violent conviction from official records ( 65 , 69 ) and 1 reported intimate partner violence from the partner’s report ( 62 ). Most used self-report items in the Diagnostic Interview Schedule ( 56 ), PPC Delinquency and Criminal Behavior inventory ( 57 ), Aggression Questionnaire ( 58 ), Conflict Tactics Scale ( 63 ), physical aggression subscale in Buss-Perry Scale ( 71 ), and specially developed questionnaires ( 53 , 54 , 60 , 61 , 66 , 67 , 70 ). A combination of several measures (e.g., official records and self-report) was applied in 3 studies ( 59 , 64 , 68 ).
Any drug or polydrug use disorder
We identified 6 cohort investigations ( 57 , 60 , 64 , 65 , 69 , 70 ) and 6 case-control reports ( 53 , 54 , 56 , 63 , 66 , 67 ) that examined the risk of violence in any or polydrug use disorder. The odds ratios ranged from 1.3 (95% confidence interval (CI): 0.1, 13.0) to 25.0 (95% CI: 16.1–39.0) ( Figure 2 ). When excluding the 2 studies that were published prior to 2000, the odds ratio was 4.1 (95% CI: 3.0, 5.7).
Cannabis/marijuana use disorder
Six cohort studies ( 57 , 59 , 61 , 62 , 64 , 68 ) and 5 case-control investigations ( 53 , 54 , 56 , 67 , 71 ) examined the link between cannabis/marijuana use disorder and violence. The odds ratios ranged from 1.3 (95% CI: 1.1, 1.7) to 11.5 (95% CI: 7.8, 17.2). When excluding studies prior to 2000, the odds ratios ranged from 1.3 (95% CI: 1.1, 1.7) to 9.1 (95% CI: 8.5, 9.7). (See Figure 2 ).
Hallucinogen use disorder
Two cohort investigations ( 59 , 62 ) and 1 case-control report ( 54 ) tested the association between hallucinogen use disorder and violence. The odds ratios varied from 1.4 (95% CI: 1.3, 1.4) to 18.3 (95% CI: 14.9, 22.5). (See Figure 2 ).
Stimulant use disorder
We identified 5 studies that reported risk estimates for violence in stimulant use disorder, with 3 studies ( 59 , 61 , 62 ) using a cohort study design and 2 ( 54 , 58 ) using a case-control study design. All of these studies were conducted in the United States. The odds ratios ranged from 1.9 (95% CI: 1.4, 2.6) to 10.8 (95% CI: 9.3, 12.5). (See Figure 2 ).
Opioid use disorder
Three cohort investigations ( 59 , 61 , 62 ) and 2 case-control studies ( 54 , 67 ) reported the risk of violence in opioid use disorder, all of which were conducted in the United States. The risk estimates ranged from an odds ratio of 0.8 (95% CI: 0.5, 1.1) to 9.5 (95% CI: 8.7, 10.4). (See Figure 2 ).
Sedative use disorder
Two cohort investigations ( 59 , 62 ) and 1 case-control study ( 54 ) examined the association between sedative use disorder and violence. Odds ratios varied from 1.1 (95% CI: 1.1, 1.2) to 10.5 (95% CI: 9.1, 12.2). (See Figure 2 ).
Heterogeneity
No significant differences were found in risk estimates by sex, country, outcome measures, years of follow-up, and sample size in subgroup analyses ( Table 2 ). The risk estimates in cohort investigations (odds ratio (OR) = 2.7, 95% CI: 2.1, 3.5) were lower than in the case-control reports (OR = 6.6, 95% CI: 5.1, 8.6). No differences were found among violence by self-report (OR = 4.6, 95% CI: 3.0, 7.2), informant report/official records (OR = 3.2, 95% CI: 1.3, 7.8), and combined measures (OR = 4.4, 95% CI: 1.3, 14.5).
Risk Estimates for Violence in Drug Use Disorders According to Sample or Study Characteristics, Multiple Countries, 1990–2019
Abbreviations: CI, confidence interval; DSM, Diagnostic and Statistical Manual of Mental Disorders ; OR, odds ratio.

Odds ratios (ORs) and confidence interval (CIs) for the association between drug use disorders and violent outcome. Weights are from random effects analysis.
The odds ratios for intimate partner violence (OR = 1.7, 95% CI: 1.4, 2.1) were lower than for general violence (OR = 5.7, 95% CI: 3.8, 8.6) ( Table 2 ). When further exploring the associations of the comparison groups in studies of the association between drug use disorders and intimate partner violence, no significant differences were found. In the meta-regression analysis, we found that study design (cohort vs. case–control study) was associated with heterogeneity ( |$\beta $| = 0.8, t = 2.3, P = 0.04), as was the violent outcome (intimate partner violence vs. general violence; |$\beta $| = −1.2, t = −3.3, P = 0.004). No other variables examined explained the heterogeneity between studies. Egger’s test did not suggest publication bias ( t = 1.32, P = 0.20).
Main findings
This systematic review examined the association between drug use disorders and violence. We identified 18 eligible studies from 5 countries, with 591,411 individuals meeting diagnostic criteria for drug use disorders. There were 2 main findings. First, we found that individuals with a diagnosed drug use disorder have a 4- to 10-fold higher risk of perpetrating violence compared with general population or individuals without the drug use disorder being studied. All of the examined categories of drug use disorders—including cannabis, hallucinogens, stimulants, opioids, and sedatives—were associated with elevated violence risks. Of the total of 37 included studies, we found increased risk of violence in 34 studies with confidence intervals that did not cross 1. To examine the population impact, the odds of violence perpetration need to be seen in the context of general population prevalence of these disorders—which varies from 52 cases (per 100,000) of hallucinogen use disorders to 353 cases (per 100,000) of opioid use disorders ( 12 ). Second, there was substantial heterogeneity between studies, which was partially explained by study design and the type of outcome. Violence risk in drug use disorders was lower in cohort than in case-control studies, and when intimate partner violence was the outcome rather than general violence.
Implications
Although the odds of increased risk of violence in drug use disorders are not dissimilar to those in other neuropsychiatric conditions ( 72 ), their importance is greater from a public health perspective as drug use disorders are more prevalent than severe mental illnesses, such as schizophrenia or bipolar disorder. In addition, although drug use disorders are not more prevalent than disorders such as depression and anxiety, their risk of violence is usually higher ( 67 , 73 ). Therefore, drug use disorders have greater population impact when taking into account both prevalence and relative risk. This underscores the importance of treating drug use disorders as part of any public health approach to violence prevention. Notably, long-term methadone maintenance programs and behavioral treatments can reduce crime ( 74 ). In addition, there are studies that demonstrate reduced crime after drug treatment (e.g., opioid maintenance treatment, methadone, buprenorphine, and naltrexone) and nonmedical treatment (e.g., therapeutic communities, drug courts), among individuals using cocaine (75) and opioids ( 76–79 ), as well as with general drug use disorders ( 80–83 ). Moreover, prison-based interventions—such as therapeutic communities, opiate maintenance treatment, and pharmacotherapies for drug use disorders—are effective in reducing recidivism in prisoners ( 84–86 ). Despite this, most individuals with drug use disorders do not receive treatment. In the United States, among individuals with 12-month and lifetime drug use disorders, only 14% and 25% received treatment, respectively ( 87 ). Thus, more efforts should be made to improve accessibility of treatment for individuals with drug use disorders. Together, the treatability of drug use disorders, unmet needs, and risk of adverse outcomes present an opportunity to improve public health and safety.
A second implication, regarding study design, is that 2 aspects of design explained some of the between-study heterogeneity. Cohort studies had lower risk estimates than case-control investigations. This difference is likely because cohort studies are more likely to take into account the temporal sequence between drug use disorders and violent outcome. This allowed for a more accurate estimation of the associations than case-control studies. Future observational research should prioritize cohort designs to longitudinally follow individuals with drug use disorders and examine their violent outcomes. We also found that the association with intimate partner violence was less strong than with general violence. This might be because individuals with drug use disorders are less likely to have partners ( 87 , 88 ) and those who have partners might present with less severe symptoms of drug use disorders ( 89 ).
Strengths, limitations, and future directions
This review has several strengths. First, we included only studies that used validated diagnostic criteria to identify drug use disorders and excluded studies using self-report or other measures that might reflect short-term or recreational use. Second, we carefully explored heterogeneity using 2 methods (subgroup analyses and meta-regression). Third, we excluded studies examining drug use disorders and violent outcomes in selected samples such as offenders, cohorts with mental disorders, and individuals under treatment for drug use disorders, because not all individuals with drug use disorders are offenders or have other mental disorders, and the majority will not be subject to treatment. This likely increases the generalizability of our findings.
However, a number of limitations should be noted. First, all but one of the studies we included were conducted in high-income countries. We found an investigation from a middle-income country—Turkey—but no others, and none in Central Latin America, Tropical Latin America, and Southern sub-Saharan Africa, where violence is among the top 10 leading causes of disability-adjusted life-years ( 90 ). Many countries in these regions account for the majority of global drug manufacture, trafficking, and consumption ( 91 , 92 ). Therefore, more research on the link in these settings is needed. A second limitation was that the amount of information on individual categories was not sufficient to draw definite conclusions about differences by drug class. We identified 3 studies ( 54 , 59 , 62 ) of sedative use disorder and 5 each for stimulant use disorder ( 54 , 58 , 59 , 61 , 62 ) and opioid use disorder ( 54 , 59 , 61 , 62 , 67 ). Furthermore, we found a limited literature on polydrug use, although it is common and linked to poorer treatment outcomes, social maladjustment, and overdose lethality ( 93–95 ). Future studies should investigate more carefully the different categories of drug use disorders, polydrug use, and links with novel psychoactive substances. Third, it is not possible to meta-analyze studies of selected populations because the effects of mediators cannot be modeled. Therefore, our findings are not necessarily risk estimates in specific subpopulations, such as prisoners or individuals who are participating in treatment programs. For example, our estimates might be overestimates given that we excluded studies of individuals under drug treatment, which could decrease risk of violence ( 96 , 97 ). Fourth, we found links between hallucinogen use and violence in the general population, but there appears to be heterogeneity in their associations by population. For example, in criminal justice populations, recent work has found decreased associations between hallucinogen use and repeated offending in substance-involved offenders under community corrections supervision ( 48 ), which is also reported among intimate partner violence perpetrators ( 47 , 98 ). Among individuals with schizophrenia, there is an increased risk ( 99 ). Finally, due to lack of data, we identified only a few factors that might explain heterogeneity between studies. For example, we were not able to examine whether some factors moderate the link between drug use disorders and violence, such as being subjected to violence, comorbidity of other substance use disorders (including alcohol) and mental health conditions, time between onset of drug use and violent outcome, and other social determinants (including poverty and access to services). In addition, the heterogeneity analyses were based on different drug categories and limited by variations in primary study settings. The results should therefore be interpreted with caution and read in the context of implications for future research rather than clinical practice.
Moreover, some factors could be associated with, could mediate, or could modify links between drug misuse and violence. For instance, an umbrella review of 22 meta-analyses based on over 120,000 individuals has shown that a range of neuropsychiatric disorders—including schizophrenia, personality disorders, and bipolar disorders—and perpetration, being a witness, or being a victim of violence during childhood are linked to increased risk of violence ( 72 ), suggesting that all of these comorbidities can be confounders. In addition, individuals who are victims of violence might use drugs as a coping mechanism, and victimization itself might in turn lead to later violence ( 35–39 ). Therefore, more research accounting for these factors is necessary.
Conclusions
This systematic review has synthesized evidence on associations between individual categories of drug use disorder and violent outcomes. The findings suggest that all categories of drug use disorder have an elevated risk of violence, and that study design and type of violent outcome partly explain variation in risk estimates between studies.
Author affiliations: Department of Psychiatry, National Clinical Research Center for Mental Disorders, Second Xiangya Hospital of Central South University, Changsha, China (Shaoling Zhong); and Department of Psychiatry, University of Oxford, Oxford, United Kingdom (Rongqin Yu, Seena Fazel).
This work was funded by the China Scholarship Council (grant 201806370093 to S.Z) and the Wellcome Trust Senior Research Fellowship (grant 202836/Z/16/Z to S.F.).
Conflict of interest: none declared.
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017 . Lancet . 2018 ; 392 ( 10159 ): 1789 – 1858 .
Degenhardt L , Whiteford HA , Ferrari AJ , et al. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010 . Lancet . 2013 ; 382 ( 9904 ): 1564 – 1574 .
Google Scholar
McGinty EE , Choksy S , Wintemute GJ . The relationship between controlled substances and violence . Epidemiol Rev . 2016 ; 38 ( 1 ): 5 – 31 .
Degenhardt L , Hall W . Extent of illicit drug use and dependence, and their contribution to the global burden of disease . Lancet . 2012 ; 379 ( 9810 ): 55 – 70 .
Nutt DJ , King LA , Phillips LD . Drug harms in the UK: a multicriteria decision analysis . Lancet . 2010 ; 376 ( 9752 ): 1558 – 1565 .
Grann M , Fazel S . Substance misuse and violent crime: Swedish population study . BMJ . 2004 ; 328 ( 7450 ): 1233 – 1234 .
Hoaken PN , Stewart SH . Drugs of abuse and the elicitation of human aggressive behavior . Addict Behav . 2003 ; 28 ( 9 ): 1533 – 1554 .
Atkinson A , Anderson Z , Hughes K , et al. Interpersonal Violence and Illicit Drugs . Liverpool, UK : Centre for Public Health, Liverpool John Moores University ; 2009 .
Google Preview
Duke AA , Smith KM , Oberleitner L , et al. Alcohol, drugs, and violence: a meta-meta-analysis . Psychol Violence . 2018 ; 8 ( 2 ):238.
Fazel S , Yoon P , Haye AJ . Substance use disorders in prisoners: an updated systematic review and meta-regression analysis in recently incarcerated men and women . Addiction . 2017 ; 112 ( 10 ): 1725 – 1739 .
Ritchie H , Roser M . Substance Use. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Results . Seattle, WA : Institute for Health Metrics and Evaluation; http://ghdx.healthdata.org/gbd-results-tool . Accessed September 8, 2019 .
Degenhardt L , Charlson F , Ferrari A , et al. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016 . Lancet Psychiatry . 2018 ; 5 ( 12 ): 987 – 1012 .
Pedersen W , Skardhamar T . Cannabis and crime: findings from a longitudinal study . Addiction . 2010 ; 105 ( 1 ): 109 – 118 .
Huas C , Hassler C , Choquet M . Has occasional cannabis use among adolescents also to be considered as a risk marker? Eur J Public Health . 2008 ; 18 ( 6 ): 626 – 629 .
Schoeler T , Theobald D , Pingault JB , et al. Continuity of cannabis use and violent offending over the life course . Psychol Med . 2016 ; 46 ( 8 ): 1663 – 1677 .
Swartout KM , White JW . The relationship between drug use and sexual aggression in men across time . J Interpers Violence . 2010 ; 25 ( 9 ): 1716 – 1735 .
Green KM , Doherty EE , Stuart EA , et al. Does heavy adolescent marijuana use lead to criminal involvement in adulthood? Evidence from a multiwave longitudinal study of urban African Americans . Drug Alcohol Depend . 2010 ; 112 ( 1–2 ): 117 – 125 .
Farabee D , Joshi V , Anglin MD . Addiction careers and criminal specialization . Crime Delinquency . 2001 ; 47 ( 2 ): 196 – 220 .
Narvaez JC , Jansen K , Pinheiro RT , et al. Violent and sexual behaviors and lifetime use of crack cocaine: a population-based study in Brazil . Soc Psychiatry Psychiatr Epidemiol . 2014 ; 49 ( 8 ): 1249 – 1255 .
El-Bassel N , Gilbert L , Wu E , et al. Perpetration of intimate partner violence among men in methadone treatment programs in New York City . Am J Public Health . 2007 ; 97 ( 7 ): 1230 – 1232 .
Chermack ST , Grogan-Kaylor A , Perron BE , et al. Violence among men and women in substance use disorder treatment: a multi-level event-based analysis . Drug Alcohol Depend . 2010 ; 112 ( 3 ): 194 – 200 .
Moore TM , Stuart GL , Meehan JC , et al. Drug abuse and aggression between intimate partners: a meta-analytic review . Clin Psychol Rev . 2008 ; 28 ( 2 ): 247 – 274 .
Bennett T , Holloway K , Farrington D . The statistical association between drug misuse and crime: a meta-analysis . Aggress Violent Behav . 2008 ; 13 ( 2 ): 107 – 118 .
Boles SM , Miotto K . Substance abuse and violence: a review of the literature . Aggress Violent Behav . 2003 ; 8 ( 2 ): 155 – 174 .
Collins RE . The effect of gender on violent and nonviolent recidivism: a meta-analysis . J Crim Just . 2010 ; 38 ( 4 ): 675 – 684 .
Fazel S , Långström N , Hjern A , et al. Schizophrenia, substance abuse, and violent crime . JAMA . 2009 ; 301 ( 19 ): 2016 – 2023 .
Fazel S , Lichtenstein P , Grann M , et al. Bipolar disorder and violent crime: new evidence from population-based longitudinal studies and systematic review . Arch Gen Psychiatry . 2010 ; 67 ( 9 ): 931 – 938 .
Yu R , Geddes JR , Fazel S . Personality disorders, violence, and antisocial behavior: a systematic review and meta-regression analysis . J Pers Disord . 2012 ; 26 ( 5 ): 775 – 792 .
Large MM , Nielssen O . Violence in first-episode psychosis: a systematic review and meta-analysis . Schizophr Res . 2011 ; 125 ( 2–3 ): 209 – 220 .
Stith SM , Smith DB , Penn CE , et al. Intimate partner physical abuse perpetration and victimization risk factors: a meta-analytic review . Aggress Violent Behav . 2004 ; 10 ( 1 ): 65 – 98 .
Clark CB , Zyambo CM , Li Y , et al. The impact of non-concordant self-report of substance use in clinical trials research . Addict Behav . 2016 ; 58 : 74 – 79 .
Denis CM , Gelernter J , Hart AB , et al. Inter-observer reliability of DSM-5 substance use disorders . Drug Alcohol Depend . 2015 ; 153 : 229 – 235 .
Hasin DS , O’Brien CP , Auriacombe M , et al. DSM-5 criteria for substance use disorders: recommendations and rationale . Am J Psychiatry . 2013 ; 170 ( 8 ): 834 – 851 .
Bushman BJ . Human aggression while under the influence of alcohol and other drugs: an integrative research review . Curr Dir Psychol Sci . 1993 ; 2 ( 5 ): 148 – 151 .
Afifi TO , Henriksen CA , Asmundson GJ , et al. Childhood maltreatment and substance use disorders among men and women in a nationally representative sample . Can J Psychiatry . 2012 ; 57 ( 11 ): 677 – 686 .
Asberg K , Renk K . Substance use coping as a mediator of the relationship between trauma symptoms and substance use consequences among incarcerated females with childhood sexual abuse histories . Subst Use Misuse . 2012 ; 47 ( 7 ): 799 – 808 .
Duke NN , Pettingell SL , McMorris BJ , et al. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences . Pediatrics . 2010 ; 125 ( 4 ): e778 – e786 .
Dardis CM , Dixon KJ , Edwards KM , et al. An examination of the factors related to dating violence perpetration among young men and women and associated theoretical explanations: a review of the literature . Trauma, Violence, and Abuse . 2015 ; 16 ( 2 ): 136 – 152 .
Park S , Kim S-H . Who are the victims and who are the perpetrators in dating violence? Sharing the role of victim and perpetrator . Trauma, Violence, and Abuse . 2019 ; 20 ( 5 ): 732 – 741 .
Funk M , Drew N , Knapp M . Mental health, poverty and development . J Public Ment Health . 2012 ; 11 ( 4 ): 166 – 185 .
Hall W , Degenhardt L . Adverse health effects of non-medical cannabis use . Lancet . 2009 ; 374 ( 9698 ): 1383 – 1391 .
Degenhardt L , Glantz M , Evans-Lacko S , et al. Estimating treatment coverage for people with substance use disorders: an analysis of data from the World Mental Health Surveys . World Psychiatry . 2017 ; 16 ( 3 ): 299 – 307 .
Krupski A , Graves MC , Bumgardner K , et al. Comparison of homeless and non-homeless problem drug users recruited from primary care safety-net clinics . J Subst Abuse Treat . 2015 ; 58 : 84 – 89 .
Goldstein PJ . The drugs/violence nexus: a tripartite conceptual framework . J Drug Issues . 1985 ; 15 ( 4 ): 493 – 506 .
Stroup DF , Berlin JA , Morton SC , et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting . JAMA . 2000 ; 283 ( 15 ): 2008 – 2012 .
Moher D , Liberati A , Tetzlaff J , et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement . PLoS Med . 2009 ; 6 ( 7 ):e1000097.
Thiessen MS , Walsh Z , Bird BM , et al. Psychedelic use and intimate partner violence: the role of emotion regulation . J Psychopharmacol . 2018 ; 32 ( 7 ): 749 – 755 .
Hendricks PS , Clark CB , Johnson MW , et al. Hallucinogen use predicts reduced recidivism among substance-involved offenders under community corrections supervision . J Psychopharmacol . 2014 ; 28 ( 1 ): 62 – 66 .
Peterson J , Welch V , Losos M , et al. The Newcastle-Ottawa scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses . Ottawa, Canada : Ottawa Hospital Research Institute ; 2011 .
Higgins J , Altman D , Sterne J . Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0 . Chichester, UK : The Cochrane Collaboration ; 2011 .
Borenstein M , Hedges LV , Higgins JP , et al. A basic introduction to fixed-effect and random-effects models for meta-analysis . Res Synth Methods . 2010 ; 1 ( 2 ): 97 – 111 .
Borenstein M , Hedges LV , Higgins JP , et al. Introduction to Meta-Analysis . West Sussex, UK : John Wiley & Sons ; 2009 .
Harford TC , Chen CM , Grant BF . Other-and self-directed forms of violence and their relationship with number of substance use disorder criteria among youth ages 12–17: results from the National Survey on Drug Use and Health . J Stud Alcohol Drugs . 2016 ; 77 ( 2 ): 277 – 286 .
Harford TC , H-Y Y , Chen CM , et al. Substance use disorders and self-and other-directed violence among adults: results from the National Survey on Drug Use and Health . J Affect Disord . 2018 ; 225 : 365 – 373 .
Egger M , Smith GD , Schneider M , et al. Bias in meta-analysis detected by a simple, graphical test . BMJ . 1997 ; 315 ( 7109 ): 629 – 634 .
Swanson JW , Holzer CE III , Ganju VK , et al. Violence and psychiatric disorder in the community: evidence from the Epidemiologic Catchment Area surveys . Psychiatr Serv . 1990 ; 41 ( 7 ): 761 – 770 .
Friedman AS , Kramer S , Kreisher C , et al. The relationships of substance abuse to illegal and violent behavior, in a community sample of young adult African American men and women (gender differences) . J Subst Abuse . 1996 ; 8 ( 4 ): 379 – 402 .
Payer DE , Lieberman MD , London ED . Neural correlates of affect processing and aggression in methamphetamine dependence . Arch Gen Psychiatry . 2011 ; 68 ( 3 ): 271 – 282 .
Feingold A , Kerr DC , Capaldi DM . Associations of substance use problems with intimate partner violence for at-risk men in long-term relationships . J Fam Psychol . 2008 ; 22 ( 3 ): 429 – 438 .
Van Dorn R , Volavka J , Johnson N . Mental disorder and violence: is there a relationship beyond substance use? Soc Psychiatry Psychiatr Epidemiol . 2012 ; 47 ( 3 ): 487 – 503 .
Smith PH . Intimate Partner Violence Among Adults: the Role of Illicit Drug Use [thesis] . Buffalo, NY : State University of New York ; 2014 .
Feingold A , Capaldi DM . Associations of women's substance dependency symptoms with intimate partner violence . Partn Abus . 2014 ; 5 ( 2 ): 152 – 167 .
McCauley HL , Breslau JA , Saito N , et al. Psychiatric disorders prior to dating initiation and physical dating violence before age 21: findings from the National Comorbidity Survey Replication (NCS-R) . Soc Psychiatry Psychiatr Epidemiol . 2015 ; 50 ( 9 ): 1357 – 1365 .
White HR , Buckman J , Pardini D , et al. The association of alcohol and drug use with persistence of violent offending in young adulthood . J Dev Life Course Criminol . 2015 ; 1 ( 3 ): 289 – 303 .
Trauffer N , Widom CS . Child abuse and neglect, and psychiatric disorders in nonviolent and violent female offenders . Violence Gend . 2017 ; 4 ( 4 ): 137 – 143 .
Corrigan PW , Watson AC . Findings from the National Comorbidity Survey on the frequency of violent behavior in individuals with psychiatric disorders . Psychiatry Res . 2005 ; 136 ( 2–3 ): 153 – 162 .
Harford TC , Chen CM , Kerridge BT , et al. Self-and other-directed forms of violence and their relationship with lifetime DSM-5 psychiatric disorders: results from the National Epidemiologic Survey on Alcohol Related Conditions–III (NESARC-III) . Psychiatry Res . 2018 ; 262 : 384 – 392 .
Arseneault L , Moffitt TE , Caspi A , et al. Mental disorders and violence in a total birth cohort: results from the Dunedin study . Arch Gen Psychiatry . 2000 ; 57 ( 10 ): 979 – 986 .
Christoffersen MN , Francis B , Soothill K . An upbringing to violence? Identifying the likelihood of violent crime among the 1966 birth cohort in Denmark . J Forensic Psychiatry Psychol . 2003 ; 14 ( 2 ): 367 – 381 .
ten Have M , de Graaf R , van Weeghel J , et al. The association between common mental disorders and violence: to what extent is it influenced by prior victimization, negative life events and low levels of social support? Psychol Med . 2014 ; 44 ( 7 ): 1485 – 1498 .
Altintas M , Inanc L , Hunca AN , et al. Theory of mind, aggression and impulsivity in patients with synthetic cannabinoid use disorders: a case-control study . Anadolu Psikiyatr De . 2019 ; 20 ( 1 ): 5 – 12 .
Fazel S , Smith EN , Chang Z , et al. Risk factors for interpersonal violence: an umbrella review of meta-analyses . Br J Psychiatry . 2018 ; 213 ( 4 ): 609 – 614 .
Pulay AJ , Dawson DA , Hasin DS , et al. Violent behavior and DSM-IV psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions . J Clin Psychiatry . 2008 ; 69 ( 1 ): 12 – 22 .
McLellan AT , Lewis DC , O'Brien CP , et al. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation . JAMA . 2000 ; 284 ( 13 ): 1689 – 1695 .
Koehn JD , Bach P , Hayashi K , et al. Impact of incarceration on rates of methadone use in a community recruited cohort of injection drug users . Addict Behav . 2015 ; 46 : 1 – 4 .
Bukten A , Skurtveit S , Gossop M , et al. Engagement with opioid maintenance treatment and reductions in crime: a longitudinal national cohort study . Addiction . 2012 ; 107 ( 2 ): 393 – 399 .
Vorma H , Sokero P , Aaltonen M , et al. Participation in opioid substitution treatment reduces the rate of criminal convictions: evidence from a community study . Addict Behav . 2013 ; 38 ( 7 ): 2313 – 2316 .
Bahji A , Carlone D , Altomare J . Acceptability and efficacy of naltrexone for criminal justice-involved individuals with opioid use disorder: a systematic review and meta-analysis . Addiction . 2020 ; 115 ( 8 ): 1413 – 1425 .
Maremmani I , Rolland B , Somaini L , et al. Buprenorphine dosing choices in specific populations: review of expert opinion . Expert Opin Pharmacother . 2016 ; 17 ( 13 ): 1727 – 1731 .
Mitchell O , Wilson DB , MacKenzie DL . The effectiveness of incarceration-based drug treatment on criminal behavior: a systematic review . Campbell Syst Rev . 2012 ; 8 ( 1 ): i – 76 .
Perry A , Woodhouse R , Neilson M , et al. Are non-pharmacological interventions effective in reducing drug use and criminality? A systematic and meta-analytical review with an economic appraisal of these interventions . Int J Environ Res Public Health . 2016 ; 13 ( 10 ): 966 .
Shaffer DK . Looking inside the black box of drug courts: a meta-analytic review . Justice Quarterly . 2011 ; 28 ( 3 ): 493 – 521 .
Mitchell O , Wilson DB , Eggers A , et al. Drug courts' effects on criminal offending for juveniles and adults . Campbell Syst Rev . 2012 ; 8 ( 1 ): i – 87 .
de Andrade D , Ritchie J , Rowlands M , et al. Substance use and recidivism outcomes for prison-based drug and alcohol interventions . Epidemiol Rev . 2018 ; 40 ( 1 ): 121 – 133 .
Mitchell O , Wilson DB , MacKenzie DL . Does incarceration-based drug treatment reduce recidivism? A meta-analytic synthesis of the research . J Exp Criminol . 2007 ; 3 ( 4 ): 353 – 375 .
Chang Z , Lichtenstein P , Långström N , et al. Association between prescription of major psychotropic medications and violent reoffending after prison release . JAMA . 2016 ; 316 ( 17 ): 1798 – 1807 .
Grant BF , Saha TD , Ruan WJ , et al. Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions–III . JAMA. Psychiat . 2016 ; 73 ( 1 ): 39 – 47 .
Merline AC , Schulenberg JE , O'Malley PM , et al. Substance use in marital dyads: premarital assortment and change over time . J Stud Alcohol Drugs . 2008 ; 69 ( 3 ): 352 – 361 .
Schulenberg JE , Patrick ME , Kloska DD , et al. Substance use disorder in early midlife: a national prospective study on health and well-being correlates and long-term predictors . Substance Abuse: Research and Treatment . 2015 ; 9 ( suppl 1 ): 41 – 57 .
Kassebaum NJ , Arora M , Barber RM , et al. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015 . Lancet . 2016 ; 388 ( 10053 ): 1603 – 1658 .
UNODC . World Drug Report 2018 . Vienna, Austria : United Nations Publications ; 2018 .
Chalk P . The Latin American Drug Trade: Scope, Dimensions, Impact, and Response . Santa Monica, CA : Rand Corporation ; 2011 .
Leri F , Bruneau J , Stewart J . Understanding polydrug use: review of heroin and cocaine co-use . Addiction . 2003 ; 98 ( 1 ): 7 – 22 .
Jones JD , Mogali S , Comer SD . Polydrug abuse: a review of opioid and benzodiazepine combination use . Drug Alcohol Depend . 2012 ; 125 ( 1–2 ): 8 – 18 .
Connor JP , Gullo MJ , White A , et al. Polysubstance use: diagnostic challenges, patterns of use and health . Curr Opin Psychiatry . 2014 ; 27 ( 4 ): 269 – 275 .
van der Pol TM , Henderson CE , Hendriks V , et al. Multidimensional family therapy reduces self-reported criminality among adolescents with a cannabis use disorder . Int J Offender Ther Comp Criminol . 2018 ; 62 ( 6 ): 1573 – 1588 .
Ward CL , Mertens JR , Bresick GF , et al. Screening and brief intervention for substance misuse: does it reduce aggression and HIV-related risk behaviours? Alcohol Alcohol . 2015 ; 50 ( 3 ): 302 – 309 .
Walsh Z , Hendricks PS , Smith S , et al. Hallucinogen use and intimate partner violence: prospective evidence consistent with protective effects among men with histories of problematic substance use . J Psychopharmacol . 2016 ; 30 ( 7 ): 601 – 607 .
Lamsma J , Cahn W , Fazel S . Use of illicit substances and violent behaviour in psychotic disorders: two nationwide case-control studies and meta-analyses . Psychol Med . 2020 ; 50 ( 12 ): 2028 – 2033 .
- heterogeneity
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1478-6729
- Copyright © 2024 Johns Hopkins Bloomberg School of Public Health
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Domestic Violence and Abuse: Theoretical Explanation and Perspectives
- First Online: 17 November 2019
Cite this chapter

- Parveen Ali 3 ,
- Julie McGarry 4 &
- Caroline Bradbury-Jones 5
2778 Accesses
3 Citations
Domestic violence and abuse (DVA) is a complex issue and it is important to understand how and why this happens. Such understanding can help find strategies to minimise DVA. Over past decades, many explanations have been proposed to explain DVA from various perspectives. This chapter aims to present an aggregated overview of that information to help healthcare professionals understand the phenomenon from a theoretical perspective. The chapter provides information about various perspectives including biological, psychological, sociological, and ecological frameworks.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Web Resource
https://www.who.int/violenceprevention/approach/ecology/en/
Afifi TO, Mota N, Sareen J, MacMillan HL (2017) The relationships between harsh physical punishment and child maltreatment in childhood and intimate partner violence in adulthood. BMC Public Health 17(1):493
PubMed PubMed Central Google Scholar
Ali PA, Naylor PB (2013a) Intimate partner violence: a narrative review of the biological and psychological explanations for its causation. Aggress Violent Behav 18(3):373–382
Google Scholar
Ali PA, Naylor PB (2013b) Intimate partner violence: a narrative review of the feminist, social and ecological explanations for its causation. Aggress Violent Behav 18(6):611–619
Atkinson MP, Greenstein TN, Lang MM (2005) For women, breadwinning can be dangerous: gendered resource theory and wife abuse. J Marriage Fam 67:1137–1148
Babcock JC, Graham K, Canady B, Ross JM (2011) A proximal change experiment testing two communication exercises with intimate partner violent men. Behav Ther 42(2):336–347. https://doi.org/10.1016/j.beth.2010.08.010
Article PubMed PubMed Central Google Scholar
Ball P, Wyman E (1978) Battered wives and powerlessness: what can counselors do? Victimology 2:545–557
Bandura A (1977) Social learning theory. General Learning Press, New York
Barnes JC, TenEyck M, Boutwell BB, Beaver KM (2013) Indicators of domestic/intimate partner violence are structured by genetic and nonshared environmental influences. J Psychiatr Res 47(3):371–376
CAS PubMed Google Scholar
Baron K, Smith T, Butner J, Nealey-Moore J, Hawkins M, Uchino B (2007) Hostility, anger, and marital adjustment: concurrent and prospective associations with psychosocial vulnerability. J Behav Med 30(1):1–10
PubMed Google Scholar
Baumrind D, Lazerle RE, Cowan PA (2002) Ordinary physical punishment: is it harmful? Comment on Gershoff. Psychol Bull 128:580–589
Berns SB, Jacobson NS, Gottman JM (1999) Demand/withdraw interaction patterns between different types of batterers and their spouses. J Marital Fam Ther 25(3):337–348
Bhandari M, Sprague S, Tornetta P 3rd, D’Aurora V, Schemitsch E, Shearer H et al (2008) (Mis)perceptions about intimate partner violence in women presenting for orthopaedic care: a survey of Canadian orthopaedic surgeons. J Bone Joint Surg Am 90(7):1590–1597
Black DS, Sussman S, Unger JB (2010) A further look at the intergenerational transmission of violence: witnessing interparental violence in emerging adulthood. J Interpers Violence 25(6):1022–1042
Blood RO, Wolfe DM (1960) Husbands and wives. Free Press, Glencoe
Bowlby J (1969) Attachment and loss: Vol I. Attachment. Basic Books, New York
Bowlby J (1973) Attachment and loss: Vol II. Separation. Basic Books, New York
Bowlby J (1988) A secure base: parent child attachment and healthy human development. Basic Books, New York
Bronfenbrenner U (1977) Toward an experimental ecology of human development. Am Psychol 32(7):513–531
Bronfenbrenner U (1979) The ecology of human development: experiments by nature and design. Harvard University Press, Cambridge
Bronfenbrenner U (1986) Ecology of the family as a context for human development: research perspectives. Dev Psychol 22(6):723–742
Cannon EA, Bonomi AE, Anderson ML, Rivara FP (2009) The intergenerational transmission of witnessing intimate partner violence. Arch Pediatr Adolesc Med 163(8):706–708
Carter J (2015) Patriarchy and violence against women and girls. Lancet 385(9978):e40–e41
Chester DS, DeWall CN (2018) The roots of intimate partner violence. Curr Opin Psychol 19:55–59. https://doi.org/10.1016/j.copsyc.2017.04.009
Article PubMed Google Scholar
Choenni V, Hammink A, van de Mheen D (2017) Association between substance use and the perpetration of family violence in industrialized countries: a systematic review. Trauma Violence Abuse 18(1):37–50. https://doi.org/10.1177/1524838015589253
Corvo K, Dutton D (2015) Neurotransmitter and neurochemical factors in domestic violence perpetration: implications for theory development. Partn Abus 6(3):351–364
Craven Z (2003) Battered woman syndrome. Australian domestic and family violence clearinghouse. http://www.austdvclearinghouse.unsw.edu.au/PDF%20files/battered%20_woman_syndrome.pdf
Delsol C, Margolin G (2004) The role of family-of-origin violence in men’s marital violence perpetration. Clin Psychol Rev 24(1):99–122
DeMaris A, Benson ML, Fox GL, Hill T, Wyk JV (2003) Distal and proximal factors in domestic violence: a test of an integrated model. J Marriage Fam 65:652–667
Dobash RP, Dobash RE (2004) Women’s violence to men in intimate relationships: working on a puzzle. Br J Criminol 44(3):324–349
Ehrensaft MK, Moffitt TE, Caspi A (2006) Is domestic violence followed by an increased risk of psychiatric disorders among women but not among men? A longitudinal cohort study. Am J Psychiatry 163(5):885–892. https://doi.org/10.1176/appi.ajp.163.5.885
Eirich GM, Robinson JH (2017) Does earning more than your spouse increase your financial satisfaction? A comparison of men and women in the United States, 1982 to 2012. J Fam Issues 38(17):2371–2399
Farrington K (1986) The application of stress theory to the study of family violence: principles, problems and prospects. J Fam Violence 1:131–149
Fehringer JA, Hindin MJ (2009) Like parent, like child: intergenerational transmission of partner violence in Cebu, the Philippines. J Adolesc Health 44(4):363–371
Fiebert MS (2008) References examining assaults by women on their spouses or male partners: an annotated bibliography. http://www.csulb.edu/~mfiebert/assault.htm
Fox GL, Benson ML, DeMaris AA, Wyk JV (2002) Economic distress and intimate violence: testing family stress and resources theories. J Marriage Fam 64(3):793–807
García-Moreno C, Jansen HAFM, Ellsberg M, Heise L, Watts C (2005) WHO multi-country study on women’s health and domestic violence against women: initial results onprevalence, health outcomes and women’s responses. World Health Organization, Geneva
Gershoff ET (2002) Corporal punishment by parents and associated child behaviors and experiences: a meta-analytic and theoretical review. Psychol Bull 128(4):539–579
Gormley B (2005) An adult attachment theoretical perspective of gender symmetry in intimate partner violence. Sex Roles 52:785–795
Haj-Yahia MM, Schiff M (2007) Definitions of and beliefs about wife abuse among undergraduate students of social work. Int J Offender Ther Comp Criminol 51(2):170–190. https://doi.org/10.1177/0306624x06291457
Hazan C, Shaver P (1987) Romantic love conceptualized as an attachment process. J Pers Soc Psychol 52(3):511–524
Hines DA, Saudino KJ (2002) Intergenerational transmission of intimate partner violence. Trauma Violence Abuse 3:210–225. https://doi.org/10.1177/15248380020033004
Article Google Scholar
Hines DA, Saudino KJ (2004) Genetic and environmental influences on intimate partner aggression: a preliminary study. Violence Vict 19:701–718
Holtzworth-Munroe A, Smutzler N, Stuart GL (1998) Demand and withdraw communication among couples experiencing husband violence. J Consult Clin Psychol 66(5):731–743
Homans GC (1974) Social behavior; its elementary forms (Revised ed.). Harcourt, Brace, Jovanovich, New York
Iverson KM, Jimenez S, Harrington KM, Resick PA (2011) The contribution of childhood family violence on later intimate partner violence among robbery victims. Violence Vict 26(1):73–87
Jasinski JL (2001) Theoretical explanations for violence against women. In: Renzetti CM, Edleson JL, Bergen RK (eds) The sourcebook on violence against women. Sage Publications, Thousand Oaks, pp 5–22
McPhail BA, Busch NB, Kulkarni S, Rice S (2007) An integrative feminist model: the evolving feminist perspective on intimate partner violence. Violence Against Women 13:817–841
Melzer SA (2002) Gender, work, and intimate violence: men’s occupational violence spillover and compensatory violence. J Marriage Fam 64(4):820–832
Mills S (1998) Postcolonial feminist theory. In: Jackson S, Jones J (eds) Contemporary feminist theories. Edinburgh University Press, Edinburgh
Milner JS, Thomsen CJ, Crouch JL, Rabenhorst MM, Martens PM, Dyslin CW et al (2010) Do trauma symptoms mediate the relationship between childhood physical abuse and adult child abuse risk? Child Abuse Negl 34(5):332–344
Mohanty CT (1991) Introduction. In: Mohanty CT, Russo A, Torres L (eds) In third world women and the politics of feminism. Indiana University Press, Bloomington
Mossière A, Maeder EM, Pica E (2018) Racial composition of couples in battered spouse syndrome cases: a look at juror perceptions and decisions. J Interpers Violence 33(18):2867–2890. https://doi.org/10.1177/0886260516632355
Narayan U (1997) Dislocating cultures: identities, traditions, and third-world feminism. Routledge, New York
Naved R, Azim S, Bhuiya A, Persson L (2006) Physical violence by husbands: magnitude, disclosure and help seeking behaviour of women in Bangladesh. Soc Sci Med 62:2917–2929
Norlander B, Eckhardt C (2005) Anger, hostility, and male perpetrators of intimate partner violence: a meta-analytic review. Clin Psychol Rev 25(2):119–152
O’Brien JE (1971) Violence in divorce prone families. J Marriage Fam 33(4):692–698.
Overmier JB, Seligman MEP (1967) Effects of inescapable shock upon subsequent escape and avoidance responding. J Comp Physiol Psychol 63:28–33
Papadakaki M, Tzamalouka GS, Chatzifotiou S, Chliaoutakis J (2009) Seeking for risk factors of intimate partner violence (IPV) in a Greek National Sample. J Interpers Violence:732–750. https://doi.org/10.1177/0886260508317181
Parks KA, Fals-Stewart W (2004) The temporal relationship between college women’s alcohol consumption and victimization experiences. Alcohol Clin Exp Res 28:625–629
Pease B (2000) Recreating men: post modern masculinity politics. Sage, London
Quinney R (1970) The social reality of crime. Little Brown, Boston
Ramos Salazar L (2015) The negative reciprocity process in marital relationships: a literature review. Aggress Violent Behav 24:113–119. https://doi.org/10.1016/j.avb.2015.05.008
Satyanarayana VA, Hebbani S, Hegde S, Krishnan S, Srinivasan K (2015) Two sides of a coin: perpetrators and survivors perspectives on the triad of alcohol, intimate partner violence and mental health in South India. Asian J Psychiatr 15:38–43. https://doi.org/10.1016/j.ajp.2015.04.014
Saudino K, Hines D (2007) Etiological similarities between psychological and physical aggression in intimate relationships: a behavioral genetic exploration. J Fam Violence 22(3):121–129
Seligman ME, Maier SF (1967) Failure to escape traumatic shock. J Exp Psychol 74:1–9
Simmons CA, Lehmann P, Cobb N (2008) Women arrested for partner violence and substance use: an exploration of discrepancies in the literature. J Interpers Violence 23:707–727
Stith SM, Smith DB, Penn CE, Ward DB, Tritt D (2004) Intimate partner physical abuse perpetration and victimization risk factors: a meta-analytic review. Aggress Violent Behav 10(1):65–98
Stuart GL, McGeary JE, Shorey RC, Knopik VS, Beaucage K, Temple JR (2014) Genetic associations with intimate partner violence in a sample of hazardous drinking men in batterer intervention programs. Violence Against Women 20(4):385–400
Sutton TE (2019) Review of attachment theory: familial predictors, continuity and change, and intrapersonal and relational outcomes. Marriage Fam Rev 55(1):1–22. https://doi.org/10.1080/01494929.2018.1458001
Testa M, Derrick JL (2014) A daily process examination of the temporal association between alcohol use and verbal and physical aggression in community couples. Psychol Addict Behav 28(1):127
Testa M, Kubiak A, Quigley BM, Houston RJ, Derrick JL, Levitt A et al (2012) Husband and wife alcohol use as independent or interactive predictors of intimate partner violence. J Stud Alcohol Drugs 73(2):268–276. https://doi.org/10.15288/jsad.2012.73.268
Thompson MP, Kingree JB (2006) The roles of victim and perpetrator alcohol use in intimate partner violence outcomes. J Interpers Violence 21:163–177. https://doi.org/10.1177/0886260505282283
Turk A (1977) Class, conflict, and criminalization. Sociol Focus 10:209–220
Waites EA (1978) Female masochism and the enforced restriction of choice. Victimology 2:535–544
Walker L (1977/1978) Battered women and learned helplessness. Victimology 2:525–534
Walker L (1979) The battered woman. Harper & Row, New York
Walker A (1993) In search of our mothers’ gardens: Womanist prose. Harcourt Brace Jovanovich, San Diego
Walker LA (2006) Battered woman syndrome: empirical findings. Ann N Y Acad Sci 1087:142–157
Walker L, Browne A (1985) Gender and victimization by intimates. J Pers 53:179–195
Waltz J, Babcock JC, Jacobson NS, Gottman JM (2000) Testing a typology of batterers. J Consult Clin Psychol 68(4):658
Wood RL, Liossi C, Wood L (2005) The impact of head injury neurobehavioural sequelae on personal relationships: preliminary findings. Brain Inj 19(10):845–851
Download references
Author information
Authors and affiliations.
School of Health Sciences, The University of Sheffield, Sheffield, UK
Parveen Ali
School of Health Sciences, The University of Nottingham, Queen’s Medical Centre, Nottingham, UK
Julie McGarry
University of Birmingham, Birmingham, UK
Caroline Bradbury-Jones
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Parveen Ali .
Editor information
Editors and affiliations.
School of Health Sciences, University of Sheffield, Sheffield, South Yorkshire, UK
Rights and permissions
Reprints and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Ali, P., McGarry, J., Bradbury-Jones, C. (2020). Domestic Violence and Abuse: Theoretical Explanation and Perspectives. In: Ali, P., McGarry, J. (eds) Domestic Violence in Health Contexts: A Guide for Healthcare Professions. Springer, Cham. https://doi.org/10.1007/978-3-030-29361-1_2
Download citation
DOI : https://doi.org/10.1007/978-3-030-29361-1_2
Published : 17 November 2019
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-29360-4
Online ISBN : 978-3-030-29361-1
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Open access
- Published: 09 August 2019
The psychological subtype of intimate partner violence and its effect on mental health: protocol for a systematic review and meta-analysis
- Sarah Dokkedahl ORCID: orcid.org/0000-0003-3090-4660 1 ,
- Robin Niels Kok 2 , 3 ,
- Siobhan Murphy 1 ,
- Trine Rønde Kristensen 4 ,
- Ditte Bech-Hansen 1 &
- Ask Elklit 1
Systematic Reviews volume 8 , Article number: 198 ( 2019 ) Cite this article
64k Accesses
50 Citations
48 Altmetric
Metrics details
Background/aim
Psychological violence is estimated to be the most common form of intimate partner violence (IPV). Despite this, research on the independent effect of psychological violence on mental health is scarce. Moreover, the lack of a clear and consistent definition of psychological violence has made results difficult to compare. The present study therefore aims to consolidate knowledge on psychological violence by conducting a systematic review and random-effects meta-analysis on the association between psychological violence and mental health problems, when controlling for other types of violence (e.g. physical and sexual) and taking into account severity, frequency, and duration of psychological violence.
The present study is registered in the International Prospective Register for Systematic Reviews (PROSPERO; #CRD42018116026) and the study design follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Additional file 1 ). A dual search will be conducted in the electronic databases PsycINFO, PubMed, EMBASE, and Web of Science. Data will be extracted using Endnote and Covidence and a meta-analysis will be conducted using Metafor-package in the programming language R. The Quality Assessment Tool for Quantitative Studies developed by the Effective Public Health Practice Project will be used to assess the quality of the included studies (i.e. weak, moderate and strong).
Results and discussion
The present review will help consolidate knowledge on psychological violence by evaluating whether frequency, severity or actual “type” of psychological violence produces the most harm. A thorough quality assessment will help overcome potential limitations regarding expected variations in terminology and assessment of psychological violence.
Systematic review registration
PROSPERO CRD42018116026 .
Peer Review reports
Intimate partner violence (IPV) is a global health problem characterized as any behaviour within an intimate relationship that causes physical, psychological or sexual harm [ 1 ]. At present, it is well-documented that IPV can cause extensive mental health consequences among its victims [ 2 , 3 , 4 , 5 ]. IPV can be characterized as an interpersonal trauma, and symptoms of posttraumatic stress disorder (PTSD) have been identified in 31–84.4% of women exposed to IPV [ 2 ]; along with other comorbid symptoms such as depression, anxiety, suicidality, substance abuse and sleep disturbances [ 2 , 5 , 6 ].
The subtype of psychological violence (compared to physical and sexual violence) is estimated to be the most common form of IPV in both the USA [ 7 ] and Europe [ 8 ], affecting between 35 and 49% of men and women. This has led legislators in some European countries to criminalize psychological violence as an independent offence, making it equally punishable as physical violence (e.g. Norway [ 9 ] and England [ 10 ]). Although some researchers have argued that psychological violence in itself cannot be classified as a trauma, as it does not meet the first criterion of diagnosing PTSD (i.e. threat to life or physical integrity [ 11 , 12 ]), a more recent review on IPV and mental health argues that psychological violence can independently cause PTSD, depression and anxiety [ 13 ].
Despite both legal recognition of psychological violence and documentation of its effect on mental health, the conceptualization of the phenomenon is ambiguous in both research and clinical practice. Acts of psychological violence are distributed along a continuum starting from what is commonly termed psychological aggression (e.g. yelling and insults) and ending with more severe abuse, often labelled coercion (e.g. threats and isolation). How we interpret psychological aggression and how we distinguish it from more severe abuse depends, among other things, on the context in which it occurs, when it occurred in a sequence, how it was interpreted and whether it was perceived as abusive [ 11 ].
Another challenge is that psychological violence is often characterized in different ways. For example, the conceptualization of “coercive control” can generally be understood in two ways: firstly, as an overall attempt to control one’s partner, in which IPV is a way of achieving control; secondly, as a subtype of IPV which is similar to—or a part of—the concept of psychological violence. The former is described in a structural perspective as more severe and gender-asymmetrical and is generally understood to be a representation of gender inequality [ 14 , 15 , 16 , 17 , 18 ]. The latter reflects a continuum of IPV from psychological aggression to more controlling behaviours constituting an assault [ 11 ]. Moreover, these are theoretical distinctions that have proven difficult for researchers and practitioners to conceptualize and apply.
The distinction between psychological violence and coercion is evident from the WHO, who define psychological violence (i.e. emotional or psychological abuse) such as “insults, belittling, constant humiliation, intimidation (e.g. destroying things), threats of harm, threats to take away children”, while controlling behaviour is defined as “isolating a person from family and friends; monitoring their movements; and restricting access to financial resources, employment, education or medical care” [ 1 ] (p. 1). The specific acts of violence separate these two definitions, while the overall psychological harm combines them. Likewise, the European Institute of Gender Equality (EIGE) states an overall definition of psychological violence, which can be understood from the perspective of caused harm: “Any act or behaviour which causes psychological harm to the partner or former partner. Psychological violence can take the form of, among others, coercion, defamation, a verbal insult or harassment” 19 (p. 45).
These variations in terminology are inevitably reflected in the psychometric instruments developed to assess psychological violence (Table 1 ; identified by the Centers for Disease Control and Prevention and the National Unit [ 20 ] against IPV in Denmark, LUV [ 21 ]). Indeed, the varying use of subscales (e.g. #7 and #9) and differing definitions of psychological violence make the findings from these studies difficult to compare and stresses the need to evaluate how the effect on mental health is influenced by such variations. For example, some instruments assess psychological aggression (e.g. #10), while others measure more severe controlling behaviours (e.g. #4). Furthermore, other instruments focus less on the act of violence and more on the effect on the victim (e.g. #12). When measuring the effect of psychological violence on mental health, the difference between acts and effects can be crucial. Evidence demonstrates that some acts defined as psychologically violent (i.e. threats to kill/harm) have been found to significantly load on a physical violence factor, most likely due to the aspect of physical threat, which makes the psychological and physical aspect hard to differentiate [ 11 ]. Furthermore, a majority of these assessment tools make use of frequency scores that do not differentiate between the severity of items. As such, items of psychological aggression (i.e. being called “ugly” and “worthless”) are equated to severe controlling behaviour and threats (i.e. threats to kill or take away children). This exemplifies how important these distinctions are if we wish to understand the independent effect of psychological violence on mental health. Examining mental health while evaluating the instruments used to measure the phenomenon will help us understand whether severity, frequency or actual “type” of psychological violence produces the most harm on the victim’s mental health [ 11 ].
In addition to problems with the conceptualization, a number of methodological challenges further characterize the field, e.g. sampling, design, scoring and gender bias [ 11 ]. Focusing on psychological aggression in lesbian, gay and bisexual individuals, Mason et al. [ 22 ] highlight the need for future research to clearly and consistently define psychological violence and separate it from other types of violence seeing that a more consistent definition will facilitate better comparisons across studies. The research group further stresses that scoring methods (e.g. frequency vs. dichotomous scoring) influence the magnitude of the effect size, which makes results difficult to compare. This challenge is further complicated by the use of self-administered questionnaires that may lack systematic development [ 22 ]. Moreover, Follingstad [ 11 ] emphasizes the need to differentiate between samples (i.e. dating relationships and marital or long-term cohabiting relationships), seeing that dating relationships are characterized by quantitatively and qualitatively less psychological violence. Finally, the majority of assessment tools are developed to specifically measure female victimization of psychological violence, despite male victimization being reported at equally high rates in some studies [ 7 ]. Although fewer studies have focused on the effects on mental health among male victims of psychological violence, studies indicate that they too present symptoms of anxiety, depression and sleep disturbances [ 13 , 23 ].
The aim of the present systematic review is to build on existing knowledge [ 13 ] concerning the effect of psychological violence on mental health, while evaluating the psychometric instruments used to assess psychological violence about how they conceptualize the phenomenon. To this day, most studies on IPV and mental health have pooled scores of physical, psychological and sexual IPV in their reporting [ 2 , 4 ], making a distinction of the individual effect of psychological violence difficult. When directly examining the effect of psychological violence, the lack of a clear and consistent definition of psychological violence has made results difficult to compare [ 13 , 22 ]. Consequently, important information is lost. The present study therefore aims to consolidate knowledge on psychological violence by evaluating whether frequency, severity or actual “type” of psychological aggression is associated with the most harm on mental health [ 11 ]. Methodological challenges will be considered by conducting quality assessments of all included studies, and results will control for the presence of physical and sexual violence (i.e. severity, duration and frequency). When possible, mediating and moderating factors will be evaluated, as well as potential gender differences. Based on the results, a discussion on assessment tools and methodological challenges will provide the grounds for recommendations concerning future research.
To sum up, the aim of this systematic review and meta-analysis is fourfold: (1) to estimate the individual effect of psychological violence on mental health (e.g. PTSD, depression and anxiety); (2) to estimate whether frequency, severity or actual “type” of violence is associated with the most harm; (3) to investigate gender, sampling and cultural differences through moderation analyses; and (4) to discuss the somewhat vague terminology and methodological challenges.
Methods and design
Methods of review.
The present protocol has been written in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines and is presented in accordance with the PRISMA-P checklist (Additional file 1 ). The protocol has further been registered in PROSPERO (#CRD42018116026).
The systematic review will be conducted as an individual and dual process by two researchers (SD + DBH) in regard to screening, eligibility and inclusion. Screening will be done on a title basis, followed by an abstract and full-text basis. A third researcher (RK) from the team will be consulted to resolve issues regarding disagreement of eligibility and inclusion on a full-text basis. If sufficient data can be extracted, a random-effects meta-analysis will be conducted on the extracted data.
It is expected that not all studies report the recorded data on psychological violence, but rather cluster subtypes of IPV (i.e. physical, sexual and psychological violence). In such cases, the corresponding authors will be contacted and invited to share the raw data.
Key definitions of the systematic review
Intimate partner violence.
As proposed in a statistical definition by EIGE, IPV is defined as “any act of physical, sexual, psychological or economic violence that occurs between former or current spouses or partners, whether or not the perpetrator shares or has shared the same residence with the victim” [ 19 ] (p. 44). This definition has been proposed to aid the EU member states to collect and compare administrative data on violence against women in a standardized manner [ 19 ].
- Psychological violence
A broad terminology for psychological violence is used in both scientific literature and in clinical practice (e.g. psychological violence, emotional abuse, coercion, psychological aggression). For clarity, this review will use the term psychological violence seeing that this definition links it directly to other types of IPV (e.g. physical or sexual violence), while emphasizing a core psychological aspect of harm in both the act of perpetration as well as the effect of victimization. The variation in terminology will shortly be addressed in the discussion.
In the current protocol, psychological violence will be defined by an overall definition combining that of both the WHO [ 1 ] (i.e. both emotional/psychological abuse and controlling behaviours) and the European Institute of Gender Equality [ 19 ]: “Any act or behaviour which causes psychological harm to the partner or former partner. Psychological violence can take the form of, among others, coercion, defamation, a verbal insult or harassment” [ 19 ] (p. 45), including belittling, constant humiliation, intimidation (e.g. destroying things), threats of harm, threats to take away children and/or isolating a person from family and friends; monitoring their movements; and restricting access to financial resources, employment, education or medical care [ 1 ] (p. 1). A broad definition will allow for studies using varying definitions to be included and will be assessed through subgroup analyses. The different definitions will be evaluated and discussed based on their effect on mental health.
Mental health in this context
As mentioned above, it has previously been argued that psychological violence alone cannot be characterized as a trauma [ 11 ]. However, recent studies have identified an association between psychological violence and PTSD [ 13 ]. Based on these findings, the authors consider psychological violence a potential traumatic event and wish to further examine the relationship between psychological violence and PTSD. Other mental health consequences identified are based on the National Institute for Health and Care Excellence (NICE) guidelines and comorbid mental health problems of PTSD [ 24 ], i.e. depression, anxiety, alcohol or drug abuse, suicidality, sexual problems, sleep problems, problems with concentration, somatization and functional problems (e.g. social, educational, or occupational) as well as feelings of shame and guilt.
Search method
A dual search will be conducted in the electronic databases PsycINFO, PubMed, EMBASE and Web of Science. Other methods used for identifying relevant research include reference checking and hand-searching of grey literature. Furthermore, the following scientific journals will be hand-searched: Journal of Interpersonal Violence and Journal of Violence and Victims .
Criteria for including studies
The review will include studies of psychological violence on mental health when controlling for other types of partner abuse. Hence, studies including an adult (≥ 18 years) population of victims of IPV (dating samples, national samples, clinical settings, etc.) that report on psychological violence specifically. Many studies are expected to include groups of comparison (e.g. non-abused or other types of abuse); however, comparisons are not required.
Furthermore, the review will only include peer-reviewed articles in English, German, Dutch or Scandinavian languages (i.e. Norwegian, Swedish or Danish).
Criteria for excluding studies
The review will exclude case studies, reviews, commentaries, editorials, letters to editorials, book chapters and other non-primary research articles.
Search string
See Table 2 for the PsycINFO search string.
Main outcome of interest
To investigate the independent effect of psychological violence on mental health. A meta-analysis will be performed to estimate the effect of psychological violence on PTSD, depression and anxiety. A narrative summary will present all related mental health problems as defined by the NICE guidelines [ 24 ].
Secondary outcomes of interest include the following:
How does “type” of psychological violence affect mental health?
How does frequency and severity affect mental health outcomes? (e.g. high frequency and/or low severity or low frequency and/or high severity).
Are there potential gender differences in mental health consequences with regard to psychological violence?
Will controlling for previous trauma affect the association between psychological violence and mental health?
Does sample population differ in mental health consequences? (e.g. dating samples vs. treatment samples)
Finally, the systematic review aims to evaluate included psychometric tools measuring psychological violence and how potential variations in the conceptualization of psychological violence affects results.
Data extraction
Data will be extracted with help from Endnote and Covidence. Meta-analyses will be conducted using the programming language R. The authors will design a data extraction form. The form will include authors, year, sample size, population, country, age, gender, design, IPV assessment tool(s), mental health assessment, primary outcome (effect size), secondary outcome(s), timeframe of assessment (lifetime or specified), scoring method(s), previous trauma and previous mental health problems. Data will be extracted by one reviewer (SD), and independently cross-checked by another reviewer (DBH). Inconsistencies in data extraction will be resolved between the reviewers by referring to the source study until a consensus is reached.
Quality assessment
The “Quality Assessment Tool for Quantitative Studies” developed by the Effective Public Health Practice Project [ 25 ] will be used to assess the quality of the included studies. This is in line with previous research evaluating IPV psychometric tools [ 26 ]. Assessment will be based on six components: (1) selection bias, (2) study design, (3) confounders, (4) blinding, (5) data collection methods and (6) withdrawals and dropouts [ 24 , 25 ]. Two researchers (SD and DBH) will classify studies on three levels: weak, moderate and strong. If classifications are inconsistent a third researcher (RK) will be involved and classification will be discussed until consensus is reached. If possible, moderation analyses will compare studies of strong vs. weak quality.
Plan for data synthesis
As demonstrated above, studies on psychological violence are quite heterogeneous in regard to conceptualization, psychometrics, sampling, design, scoring, and so forth. Therefore, we will perform a random-effects meta-analysis, because we expect high heterogeneity in the included studies. The random-effects meta-analysis assumes variance in effect across studies due to real differences in effect as well as by chance. The meta-analysis will help estimate the common effect of psychological violence on mental health (i.e. PTSD, depression and anxiety) by synthesizing individual results. If possible, moderation analyses will compare studies according to quality assessment and varying samples. The I 2 statistic will be used to test for heterogeneity, and as suggested, an I 2 statistic above 75% implies considerable heterogeneity, while an I 2 statistic below 40% is not considered to be a concern [ 27 ].
The included studies are expected to report effect sizes of varying types (i.e. correlation, regression, mean differences and association of categorical variables, e.g. odds ratio). For data synthesis, the reported effect sizes will be recoded into the same type of effect size using the programming language R. For this meta-analysis, we expect to perform a stepwise analysis according to the outcome of interest. For the main outcome of interest, as well as subgroup analyses, the meta-analysis will be conducted with effect sizes based on correlations. Additionally, the impact of the duration and frequency of psychological violence will be estimated by using meta-regression. The Metafor-package for the programming language R will be applied to conduct the meta-analysis [ 28 ].
The present review will build on existing knowledge by statistically synthesizing results on the effect of psychological violence on mental health. The review will help consolidate knowledge on psychological violence by evaluating whether frequency, severity or actual “type” of psychological violence produces the most harm. This will strengthen our knowledge on psychological violence, and how best to assess and conceptualize the phenomenon.
While conducting the systematic review, we expect to encounter several limitations. The varying terminology and definitions of psychological violence will make results difficult to compare, just as the many and varying psychometrics tools will (Table 1 ). This is further complicated by the fact that many studies are likely to not even use validated instruments but instead base their results on a few self-constructed items. The review will aim to overcome these limitations by thorough quality assessment of the included studies with help from the Quality Assessment Tool for Quantitative Studies [ 25 ] and by performing relevant subgroup analyses. This does not only apply to psychological violence, but also mental health definitions and the psychometric instruments used to assess symptomatology. By critically examining the applied definitions and terminology as well as methodological challenges (e.g. sampling, design, scoring and gender bias) the review will serve as a status quo of the field and make grounds for future recommendations.
Finally, the systematic review is expected to have several clinical implications. We expect the meta-analysis to deepen our understanding of the different subtypes of psychological violence and how they independently interact with mental health outcomes. Likewise, we expect to give clarity on psychological violence and whether it should be understood as a traumatic event equal to other types of abuse (e.g. physical or sexual violence). Developing both preventive efforts and treatment programmes such information is important if we wish to directly target the needs of those affected by psychological violence and raise awareness to encourage both victims and perpetrators to seek help.
In research, this systematic review is expected to inspire researchers to clearly and consistently define psychological violence while carefully considering the psychometrics used to measure the phenomenon, as well as other methodological challenges. Moreover, we expect to get clarity on any potential gender bias.
On a final note, this work will hopefully inspire others to conduct similar research on children who grow up as either witnesses or victims of psychological violence.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
World Health Organization. Understanding and addressing violence against women: 2012. Retrieved from: http://apps.who.int/iris/bitstream/handle/10665/77432/WHO_RHR_12.36_eng.pdf?sequence=1 .
Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. J Fam Violence. 1999;14(2):99–132.
Article Google Scholar
Dutton MA, Green BL, Kaltman SI, Roesch DM, Zeffiro TA, Krause ED. Intimate partner violence, PTSD, and adverse health outcomes. J Interpers Violence. 2006;21(7):955–68.
Johnson DM, Zlotnick C, Perez S. The relative contribution of abuse severity and PTSD severity on the psychiatric and social morbidity of battered women in shelters. Behavior Therapy. 2008;39:232–41.
Devries KM, Mak JY, Bacchus LJ, Child JC, Falder G, Petzold M, et al. Intimate partner violence and incident depressive symptoms and suicide attempts: A systematic review of longitudinal studies. PLOS Med. 2013;10(5):e1001439.
Pigeon WR, Cerulli CJD, Richards HMS, He H, Perlis M, Caine E. Sleep disturbances and their association with mental health among women exposed to intimate partner violence. J Women’s Health. 2011;20(12):1923–9.
Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 summary report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and. Prevention. 2011; Retrieved from: https://www.cdc.gov/violenceprevention/pdf/nisvs_report2010-a.pdf .
European Union Agency for Fundamental Rights (EUAFR). Violence against women, an EU-wide survey: Main results. Vienna: European Union Agency for Fundamental Rights; 2014. Retrieved from https://fra.europa.eu/en/publication/2014/violence-against-women-eu-wide-survey-main-results-report .
Aas G, Andersen T. Mishandlingsbestemmelsen – En evaluering av loven mot mishandling I nære relasjoner jf. Strl. § 219 (§ 282/283). Politihøgskolen, Oslo; 2017. Retrieved from: https://phs.brage.unit.no/phs-xmlui/handle/11250/2427624 .
Home Office. Controlling or coercive behaviour in an intimate or family relationship – statutory guidance. framework. December, 2015; Retrieved from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/482528/Controlling_or_coercive_behaviour_-_statutory_guidance.pdf .
Follingstad DR. The impact of psychological aggression on women’s mental health and behavior – the status of the field. Trauma, Violence, Abuse. 2009;10(3):271–89.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM - IV - TR . Washington, DC: American Psychiatric Association; 2000.
Google Scholar
Lagdon S, Armour C. Stringer. Adult experiences of mental health outcomes as a result of intimate partner violence victimization: A systematic review. Eur J Psychotraumatol. 2014;5:24794.
Stark E. Coercive control. New York: Oxford University Press; 2007.
Stark E. Do violent acts equal abuse? Sex roles. 2010;62:201–11.
Johnson MP. Patriarchal terrorism and common couple violence. J Marriage Fam. 1995;57(2):283–94.
Johnson MP. A typology of domestic violence. Boston, MA: Northeastern University Press; 2008.
Walby S, Towers J. Untangling the concept of coercive control: Theorizing domestic violent crime. Criminology Criminal Justice. 2018;18(1):7–28.
EIGE. Glossary of definitions of rape, femicide, and intimate partner violence; 2017. Retrieved from: https://eige.europa.eu/rdc/eige-publications/glossary-definitions-rape-femicide-and-intimate-partner-violence
Thompson MP, Basile KC, Hertz MF, Sitterle D. Measuring intimate violence victimization and perpetration: A compendium of assessment tools. Atlanta (GA): Centers for Disease Control and Prevention, National Center Injury. Prev Control. 2006.
Oldrup, H., Andersen, S., Kjær. S., Nielsen, NH., von Rosen, CB. Psykiske, fysiske og sociale konsekvenser af psykisk vold i parforhold – kortlægning af forskning. Lev Uden Vold. København; 2018. Retrieved from: https://levudenvold.dk/wp-content/uploads/2018/08/rapport-konsekvenser-af-psykisk-vold-web.pdf
Mason TB, Lewis RJ, Milletich RJ, Kelley ML, Minifie JB, Derlega VJ. Psychological aggression in lesbian, gay, and bisexual individuals’ intimate relationships: A review of prevalence, correlates, and measurement issues. Aggress Violent Behav. 2014;19:219–34.
Próspero M. The effect of coercion in aggression and mental health among reciprocally violent couples. J Fam Violence. 2008;23:195–202.
National Collaborating Centre for Mental Health. Post-traumatic stress disorder – the management of ptsd in adults and children in primary and secondary care. National Clinical Practice Guidelines Number 26. The Royal College of Psychiatrists & The British Psychological Society. Gaskell and the British Psychological Society. Cromwell Press Limited, Trowbridge, Wiltshire; 2005. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK56494/pdf/Bookshelf_NBK56494.pd .
National Collaborating Centre for Methods of and Tools. Qualitative assessment tool for quantitative studies. Hamilton, ON: McMaster University; 2008. (Updated 03 October, 2017). Retrieved from: https://www.nccmt.ca/knowledge-repositories/search/14 .
Arkins B, Begley C, Higgins A. Measures for screening intimate partner violence: A systematic review. J Psychiatr Ment Health Nurs. 2016;23:217–35.
Article CAS Google Scholar
Cooper H. Research synthesis and meta-analysis. 5 th Ed. Duke University: Sage Publications, Inc.; 2017.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:3:1–48.
Shepard MF, Campbell JA. The Abusive Behavior Inventory: A measure of psychological and physical abuse. J Interpers Violence. 1992; 7 :291–305.
Hegarty K, Sheehan M, Schonfeld C. A multidimensional definition of partner abuse: Development and preliminary validation of the Composite Abuse Scale. J Fam Violence. 1999;14:399–415.
Hegarty K, Bush R, Sheehan M. The Composite Abuse Scale: Further development and assessment of reliability and validity of a multidimensional partner abuse measure in clinical settings. Violence Victims. 2005;20:529–47.
Sullivan CM, Bybee DI. Reducing violence using community-based advocacy for women with abusive partners. J Consult Clin Psychol. 1999;67:43–53.
Sullivan CM, Parisian JA, Davidson WS. Index of psychological abuse: Development of a measure. Poster presentation at the annual conference of the American Psychological Association. San Francisco (CA; 1991.
O’Leary KD. Psychological abuse: A variable deserving critical attention in domestic violence. Violence Victims. 1999;14:3–23.
Rodenburg FA, Fantuzzo JW. The Measure of Wife Abuse: Steps toward the development of a comprehensive assessment technique. J Fam Violence. 1993;8:203–28.
Murphy CM, Hoover SA. Measuring emotional abuse in dating relationships as a multifactorial construct. Violence Victims. 1999;14:39–53.
Murphy C, Hoover S, Taft C. The Multidimensional Measure of Emotional Abuse: Factor structure and subscale validity. Toronto: Association for the Advancement of Behavior Therapy; 1999.
Hudson WW. The WALMYR assessment scales scoring manual. Tallahassee (FL): WALMYR Publishing Company; 1997.
Sackett LA, Saunders DG. The impact of different forms of psychological abuse on battered women. Violence and Victims. 1999;14:105–77.
Tolman RM. The development of a measure of psychological maltreatment of women by their male partners. Violence Victims. 1989;4:159–77.
Tolman RM. The validation of the Psychological Maltreatment of Women Inventory. Violence Victims. 1999;14:25–37.
Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scale (CTS2): development and preliminary psychometric data. J Fam Iss. 1996;17:283–316.
Straus MA, Hamby SL, Warren WL. The Conflict Tactics Scale handbook . Los Angeles (CA: Western Psychological Services; 2003.
Foshee VA, Linder GF, Bauman KE, et al. The Safe Dates project: Theoretical basis, evaluation design, and selected baseline findings. Am J of Prev Med. 1996;12:39–47.
Foshee VA, Bauman KE, Arriaga XB, Helms RW, Koch GG, Linder GF. An evaluation of Safe Dates, an adolescent dating violence program. Am J Public Health. 1998;88:45–50.
Smith PH, Earp JL, DeVellis R. Measuring battering: Development of the Women’s Experiences with Battering (WEB) Scale. Women’s. Womens Health. 1995;(1):273–88.
Smith PH, Smith JB, Earp JL. Beyond the measurement trap: A reconstructed conceptualized and measurement of woman battering. Psychology of Women Quarterly. 1999;23:177–93.
Smith PH, Thornton GE, DeVellis R, Earp J, Coker AL. A population-based study of the prevalence and distinctiveness of battering, physical assault, and sexual assault in intimate relationships. Violence Against Women. 2002;8:1208–32.
Sherin KM, Sinacore JM, Li XQ, Zitter RE, Shakil AHITS. A short domestic violence screening tool for use in a family practice setting. Fam Med. 1999;30(7):508–12.
Sherin KM, Sinacore JM, Li XQ, Zitter RE, Shakil A. HITS: a short domestic violence screening tool for use in a family practice setting. Fam Med. 1998;30(7):508-12.
Swahnberg IMK, Wijma B. The NorVold Abuse Abuse Questionnaire (NorAQ) – a validation of new measures of emotional, physical, and sexual abuse, and abuse in the health care system among women. Eur J Public Health. 2003;13:361–6.
Graham-Kevan N, Archer J. Physical aggression and control in heterosexual relationships: The effect of sampling. Violence Victims. 2003;18(2):181–96.
Follingstad DR, Coyne S, Gambone L. A representative measure of psychological aggression and its severity. Violence Victims. 2005;20(1):25–38.
Dutton, MA., Goodman, L., Schmidt, RJ. Development and validation of coercive control measure for intimate partner violence – final technical report. COSMOS Corporation: Bethesda, Maryland; 2005. Retrieved from: https://www.ncjrs.gov/pdffiles1/nij/grants/214438.pdf
Follingstad DR. A measure of psychological abuse normed on a nationally representative sample of adults. J Interpers Violence. 2010;26(6):1–21.
Rogers JM, Follingstad DR. Women’s experience to psychological abuse: Does that experience predict mental health outcomes? J Fam Violence. 2014;29(6):595–611.
Campbell DW, Campbell J, King C, Parker B, Ryan J. Violence Victims. 1994;9(3):259–74.
Campbell JC, Webster DW, Glass N. The danger assessment – validation of a lethality risk assessment instrument for intimate partner femicide. J Interpers Violence. 2009;24(4):653–74.
Download references
Acknowledgements
Not applicable.
These materials have received financial support from The Danish Victims Fund. The execution, content, and results of the materials are the sole responsibly of the authors. The analysis and viewpoints that have been made evident from the materials belong to the authors and do not necessarily reflect the views of The Council of The Danish Victims Fund. Funding was granted to Sarah Dokkedahl.
Author information
Authors and affiliations.
National Centre of Psychotraumatology, Department of Psychology at the University of Southern Denmark, 5230, Odense M, Denmark
Sarah Dokkedahl, Siobhan Murphy, Ditte Bech-Hansen & Ask Elklit
Department of Psychology at the University of Southern Denmark, Odense, Denmark
Robin Niels Kok
Centre for Innovative Medical Technology, Odense University Hospital, Odense, Denmark
Centre for persons subjected to violence, Frederiksberg Hospital, Frederiksberg, Denmark
Trine Rønde Kristensen
You can also search for this author in PubMed Google Scholar
Contributions
The present protocol has been prepared and written by the corresponding author Sarah Dokkedahl, with contributions from all the co-authors. All authors have contributed to the development of the search string and Robin Kok contributed in the development of the plan for data synthesis. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Sarah Dokkedahl .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
PRISMA-P 2015 Checklist (DOCX 30 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Dokkedahl, S., Kok, R.N., Murphy, S. et al. The psychological subtype of intimate partner violence and its effect on mental health: protocol for a systematic review and meta-analysis. Syst Rev 8 , 198 (2019). https://doi.org/10.1186/s13643-019-1118-1
Download citation
Received : 06 December 2018
Accepted : 26 July 2019
Published : 09 August 2019
DOI : https://doi.org/10.1186/s13643-019-1118-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emotional abuse, Intimate partner violence
- Mental health
- Psychometrics
- Abbreviations
- DSM Diagnostic and statistical manual of mental disorders
- EIGE European Institute of Gender Equality
- ICD International Classification of Diseases
- IPV Intimate Partner Violence
- NICE National Institute for Health and Care Excellence
- PMWI Psychological Maltreatment of Women Inventory
- PTSD Posttraumatic Stress Disorder
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

An official website of the United States government, Department of Justice.
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
NCJRS Virtual Library
Substance abuse and violence: a review of the literature, additional details, no download available, availability, related topics.
There are fresh calls to put more domestic violence offenders in prison. But mounting evidence suggests that 'jailing is failing'
Analysis There are fresh calls to put more domestic violence offenders in prison. But mounting evidence suggests that 'jailing is failing'
In the current firestorm of recriminations about the causes of domestic violence and how we might address it, there have been calls for the more frequent or more rapid jailing of violent men. But few are asking what happens then?
Perhaps, our jails being operated by departments of "corrections", we have assumed these men are leaving prison so corrected, and reformed of their impulse for violence.
If so, the assumption is dangerously wrong. The idea that by dispatching men, women and children to prison we're preventing them from committing further crime is deeply misguided. Instead, jail is too often a training ground for violence, populated by a ready network of future co-conspirators.
This is the finding of a series of eye-opening reports published in March by a research and policy institute called the Justice Reform Initiative (JRI). The organisation says we're doing criminal justice all wrong.
Lest anyone roll their eyes about bleeding heart academics, the JRI is stacked with the high priests of Australia's penal system, including four former high court justices, 10 former attorneys-general, three former police ministers and four former state premiers.
Their assessment is plain. Tougher sentences, and grimmer conditions inside prisons, do nothing to make the community safer; perversely, they may well do the opposite. The slogan adopted by the JRI's éminences grises: "Jailing is failing".
How do they know? The evidence, amassed over many years, is overwhelming.
A landmark paper published in The Prison Journal in 2011 found "there is little evidence that prisons reduce recidivism and at least some evidence to suggest that they have a criminogenic effect".
The study, which carries the subheading, "The High Cost of Ignoring Science", focused on soaring prison populations in the United States, and concluded "the use of custodial sanctions may have the unanticipated consequence of making society less safe".
The prison system's 'churn' pathway
The picture looks not much different back home.
Almost half of all people released from NSW prisons will return within just two years, and 57 per cent of people currently behind bars have been there before. In the Northern Territory, meanwhile, three-quarters of all people serving out a prison term in 2022 had previously done stretches inside .
In 2021, the Productivity Commission found Australia had one of the world's highest rates of recidivism. It is lumpy — South Australia in particular had a lower rate — but overall has been steadily rising for the past decade, and we compare poorly to other jurisdictions. The Commission reported that Norway's reoffending rate was 20 per cent, for example; in Austria it was 26 per cent.
The Commission said this: "High recidivism rates … suggest that many prisoners cycle in and out of prison, following a 'churn' pathway through the criminal justice system."
The majority of people in prison are serving relatively short sentences, many of which are too short to meet the eligibility requirements for rehabilitation schemes; and yet it is these men and women who most often reoffend. NSW Corrections' Violent Offender Therapeutic Program, for example, can take up to 12 months to complete.
The government has explicitly recognised that "due to the resource demands and length of their sentences, these individuals are … often released without adequate assessment or intervention".
To address this, it has introduced a range of "High Intensity Program Units" in NSW prisons targeting those on shorter sentences. The problem is, they don't seem to be working.
In 2022, the NSW Bureau of Crime Statistics and Research produced glum findings about the success of these HIPU programs, whose participants are filtered by eligibility requirements including signs of a "lack of motivation".
On the anti-violence program in particular, BOCSAR said, "we see little to no difference in reoffending rates between those who do not start a program at the HIPUs and those who start or finish a program".
Likewise, the "small differences in reimprisonment rates" did not rise to the level of statistical significance.
"Our analysis provides no evidence that receiving a program at a HIPU reduces the likelihood of any reoffending, violent reoffending or reimprisonment in the first year after release from custody. Any differences estimated in these outcomes are small and are confounded by the possibility that less risky individuals are more likely to receive a program."
It's also unclear whether programs like these are receiving the kind of financial and political capital needed for success. (The HIPU for persistently violent offenders, for example, was only being offered at one NSW prison as of last October .)
We're spending billions
The Justice Reform Initiative's March report says "there is no causal relationship between imprisonment rates and crime reduction". It cites recent research by Don Weatherburn, a renowned expert in this field and the former head of BOCSAR, who found "the available evidence paints a fairly dim picture of the effectiveness of prison in controlling crime".
Although crime would increase if incarceration was abolished altogether, Weatherburn found, "increasing the rate or risk of imprisonment above current levels would have no effect on the risk of re-offending and only a modest effect on overall rates of crime".
After decades at the coal-face of this issue, Weatherburn is unconcerned by this because there are other effective means by which to reduce the crime rate, and "more cost-effective ways of dealing with offenders other than imprisoning them".
The cost-efficiency picture is staggering.
In New South Wales alone taxpayers spend more than $2 billion a year on adult prisons, and another $201 million to incarcerate children. Each adult in prison costs almost $300 per day, and each child almost $2,800, or $1 million per year. Quite the price tag for a "corrections" program that seems to correct so few.
These concerns only grow more uncomfortable the deeper you delve. Pause to consider the typical cohort in jail (the mentally ill, the disadvantaged, the disproportionate number of First Nations people) or, indeed, the issue of drugs (one-in-three prisoners have a history of intravenous drug use) and the complexities only sharpen.
Eighty-five per cent of people in prison with a history of injecting drugs were under the influence at the time they committed the crime which landed them in jail. And 40 per cent say they were committing crimes only to fund their addiction.
"Traditional policing approaches to drug use-related crime do not reduce arrests or incarceration," the JRI says. To treat these people not as criminals but the unwell "will result in significant savings for the criminal justice system and improved outcomes for the whole community".
The missing magic ingredient
In fact, alternatives to incarceration have been shown to be radically more effective at reducing reoffending rates. Instead of one-in-two going back to jail, a recidivism rate of as low as 13.6 per cent has been achieved in Spain by emphasising and supporting healthy lifestyle choices, connections with family and emotional development.
The Productivity Commission recommended Australia pursue policies like those in Norway by paying more attention to "the underlying causes of offending" to achieve "better long-term recidivism outcomes" and lowering the cost of crime to the community. Doing so, it said, "would move Australian prison systems towards a stronger emphasis on rehabilitation and have the potential for better long-term outcomes".
Even the Institute of Public Affairs, the conservative think tank so often joined at the hip to the Liberal Party, has urged governments to embrace alternatives to prison.
However, it requires that magic ingredient missing from Australian politics for far too long: courage. Instead, "tough-on-crime" campaigns have been recycled over and again by politicians hungry for electoral success. Who among them might now admit their role in making society not more, but less safe?
- X (formerly Twitter)
Related Stories
Why law reform cannot be the only answer to australia's domestic violence crisis.
There is so much to be done to combat the gendered violence crisis. Here are a few places the government could start
Two out of five adult prisoners in New South Wales waiting 'in limbo' on remand
- Courts and Trials
- Crime Prevention
- Domestic Violence
- Prisons and Punishment

IMAGES
VIDEO
COMMENTS
Domestic violence is the use of intentional emotional, psychological, sexual, or physical force by one family member or intimate partner to control another. Violent acts include verbal, emotional, and physical intimidation; destruction of the victim's possessions; maiming or killing pets; threats; forced sex; and slapping, punching, kicking, choking, burning, stabbing, shooting, and killing ...
By investigating these factors, our study enhances the existing understanding of the complex dynamics of domestic violence within the unique context of the pandemic. The COVID-19 crisis has exacerbated various stressors and challenges within households, potentially intensifying the risk of violence. Understanding the interplay between these ...
Introduction. Historically, policymaking with respect to drugs, alcohol, and violence has focused on aggression in systems of drug distribution and supply (Executive Office of the President, 2016; Goldstein, 1985) and violence arising from intoxication in the night-time economy (Wickham, 2012).There is an increasing acknowledgment internationally, however, of the link between substance use and ...
Substance abuse and substance use disorder (SUD) are often used interchangeably to describe the misuse and abuse of substances. Changes to the way substance use disorder is diagnosed occurred in revisions to the Diagnostic and Statistical Manual of Mental Disorders with the release of the Fifth Edition (DSM-5).These changes made it easier for an individual to receive a substance use diagnosis ...
Substance abuse has been found to co-occur in 40-60% of IPV incidents across various studies. Several lines of evidence suggest that substance use/abuse plays a facilitative role in IPV by precipitating or exacerbating violence. ... Research has found that on days of heavy drug and/or alcohol use, physical violence was 11 times more likely ...
Introduction. The 2019 Domestic Abuse Bill proposes to establish a statutory definition of domestic abuse that includes 'controlling, coercive, threatening behaviour, violence or abuse' encompassing 'psychological, physical, sexual, economic and emotional forms of abuse' (HM Government, 2019: 5).It proposes to widen the scope of Domestic Abuse Protection Orders so that suspected ...
The authors conclude that there is a need for qualitative research to illuminate "how men ... with a particular interest in the health outcomes surrounding sexual violence, domestic abuse, and child sexual exploitation. She also has an interest in the development of integrated perpetrator interventions and evidence-based practice ...
Data were analyzed using binary logistic regression, and the. results showed that women in domestic are less influenced by substance abuse in their. completion of treatment programs. However, men are more affected by substance abuse. in completing treatment programs. Furthermore, employment significantly impacts.
Identifying these determinants is a vital step toward comprehending the complex nature of domestic violence. By synthesizing the findings from numerous studies, Table 1 presents a consolidated overview of the factors that have been consistently associated with domestic violence. This compilation serves as a valuable resource for researchers, practitioners, and policymakers seeking to address ...
1. Introduction. During the last twenty years, the idea of a 'toxic trio', or 'triad' (Fuller-Thomson, Sawyer, & Agbeyaka, 2019) has become deeply embedded in child protection policy and practice, especially perhaps in England.The first five items in the list of factors to be recorded in child in need assessments in England are drug misuse, alcohol misuse, domestic violence, mental health ...
Higher rates of substance misuse are found among domestic violence survivors than women who have not experienced abuse, suggesting that substance use coercion is more common than is recognized ...
Background Domestic violence and harmful alcohol consumption are considered major public health problems worldwide. These phenomena often co-occur, and they share several risk factors. Nevertheless, few in-depth studies have supported integrated interventions for both phenomena, in particular among Latin American women. This project will study the consumption of alcoholic beverages among women ...
Fifteen studies of hus-band to wife abuse published between 1974 and 1979 show that alcohol was present in 60-70 per cent of cases (Collins, 1981). A further overview of 52 studies (Hotaling and ...
Alcohol and Domestic Abuse/Violence. There is a strong evidence linking alcohol with domestic abuse or domestic violence (Gadd et al., 2019).A study conducted within the metropolitan area of Melbourne, Australia found that alcohol outlet density was significantly associated with domestic violence rates over time (Livingston, 2011).In Australia, alcohol-related domestic violence is twice more ...
DVA (also known as "domestic violence" or "DV" and "intimate partner violent" or "IPV") is defined as "any incident or pattern of incidents of controlling, coercive, threatening behaviour, violence or abuse between those aged 16 or over who are, or have been, intimate partners or family members regardless of gender or sexuality" (Home Office, 2018).
Although research has consistently found increased violence risk in drug use disorders, individual studies have shown that the magnitude of this increased risk varies depending on the drug category. For example, when compared with the general population, odds ratios of violence in cannabis use disorder have ranged from 1 to 7 ( 13-17 ), and ...
Domestic violence and abuse (DVA) is a complex issue and it is important to understand how and why this happens. Such understanding can help find strategies to minimise DVA. Over past decades, many explanations have been proposed to explain DVA from various perspectives. This chapter aims to present an aggregated overview of that information to ...
Background/aim Psychological violence is estimated to be the most common form of intimate partner violence (IPV). Despite this, research on the independent effect of psychological violence on mental health is scarce. Moreover, the lack of a clear and consistent definition of psychological violence has made results difficult to compare. The present study therefore aims to consolidate knowledge ...
It provides however, a new civil Domestic Abuse Protection Notice/ Order (DAPN/DAPO) and places the Domestic Violence Disclosure Scheme (DVDS) on a statutory footing. DAPNs are intended to give victim-survivors and children an additional protection measure immediately after a DA incident, providing breathing space or "space for action" ( 64 ).
On average, substance abuse programs operated with 2% times as many full-time employees as domestic violence programs (25 vs. 10) and with an average annual budget of over $1.8 million compared to the approximately $550,000 average budget observed for domestic violence programs.
The authors explain that substance abuse is related to violence is three ways. First, violence may be perpetrated while under the influence of drugs or alcohol; second, acts of violence may be perpetrated due to the nature of the drug trade and drug distribution; and third, violence may be perpetrated in order to obtain drugs.
1. Introduction. Substance use among college students is a significant public health issue in the United States. In a recent study, 23% of full-time college students reported illicit drug use, 63% reported using alcohol, 43% reported being drunk at least once in the past month, and 35% reported binge drinking (i.e., five or more consecutive drinks) in the last 2 weeks (Johnston, O'Malley ...
In the current firestorm of recriminations about the causes of domestic violence and how we might address it, there have been calls for the more frequent or more rapid jailing of violent men.
Domestic violence is one of the most negative experiences that can impact the temperament of teenagers, and the trauma it brings may accompany them for life. For a long time, news about domestic violence has frequently been reported. How to prevent and control domestic violence is a key issue in governance and public opinion.