The Person-Centered Care in Nursing Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment

Introduction
Person-centered care, holistic nursing, and cultural humility.
Health care workers should possess numerous competencies in order to provide their patients with high-quality care. However, the current landscape of health care is characterized by the changing power dynamic between medical professionals and patients that challenges their traditional roles within the system. Thus, the person-centered care approach, which allows patients to become active participants in their own treatment, is currently predominant in health care. This post is dedicated to person-centered care and the role and application of principles of holistic nursing, cultural humility, and self-reflection in nursing practice.
A person-centered strategy in nursing concerns patients being actively involved in the health care process. Person-centered care can be defined as an approach that takes into consideration “a person’s context and individual expression, preferences, and beliefs” (Santana et al., 2018, p. 430). Furthermore, it involves other stakeholders in the patient’s health in the decision-making process, for example, their family, friends, and caregivers participating in the patient care (Byrne et al., 2020). Thus, the person-centered care approach urges nurses to partner with their patients to design a more comprehensive and individualized care plan that translates into the patients receiving high-quality medical care and experiencing better health outcomes. Overall, it can be argued that, at its core, person-centered care is the approach that shows respect and consideration to the patients. It means viewing clients as persons with their own views and desires towards their health that should be taken into account when delivering care.
In my future role as a nursing practitioner, I will try to apply the principles of holistic nursing, cultural humility, and self-reflection in order to enhance the experience of patients assigned to me. Person-centered care can be viewed as a holistic approach to nursing as it takes account of different dimensions relating to the whole well-being of a person (Santana et al., 2018). Thus, holistic practice is not restricted to the aspects of physical and psychological health and well-being of a patient but considers the impact of cultural and religious beliefs and social environment on them. In my practice, I aim to include details on patients’ beliefs, socio-economic backgrounds, and social environment into their medical history to improve their health care experience and promote their health and well-being.
Furthermore, to provide patients with holistic health care, it is crucial for nursing practitioners to have cultural humility and self-reflection skills. Cultural humility in nursing is an ability of a nurse to enter a relationship with a patient “with the intention of honoring their beliefs, customs, and values” (Stubbe, 2020, p. 49). Thus, cultural humility involves a nurse’s understanding that patients know more about the nuances of their beliefs and customs. Therefore, their opinion should be the leading one regarding spiritual and cultural practices relating to health care. In my future practice, I will ask patients about the aspects of their beliefs, customs, and traditions that I am unfamiliar with to avoid stereotyping. I will also ensure that other medical professionals on the team are aware of these nuances. In addition, cultural humility demands continuous self-evaluation and self-reflection from nursing practitioners (Masters et al., 2019). Self-reflection allows nurses to examine their professional practices relating to clinical actions and person-centered care, allowing them to grow and develop further. I will strive to reflect on my encounters with patients to deliver better care and grow as a professional.
In summary, person-centered care is an integral approach in contemporary health care. It ensures that patients are put in the center of the health care process, and medical professionals account for their culture, personal beliefs, and preferences. Such competencies as the holistic approach to nursing, cultural humility, and self-reflection allow nursing practitioners to ensure the opinions and desires of the patients are considered and to provide them with high-quality care.
Byrne, A., Baldwin, A., & Harvey, C. (2020). Whose centre is it anyway? Defining person-centred care in nursing: An integrative review. PLOS ONE , 15 (3), 1–21. Web.
Masters, C., Robinson, D., Faulkner, S., Patterson, E., McIlraith, T., & Ansari, A. (2019). Addressing biases in patient care with the 5Rs of cultural humility, a clinician coaching tool. Journal of General Internal Medicine , 34 (4), 627–630. Web.
Santana, M. J., Manalili, K., Jolley, R. J., Zelinsky, S., Quan, H., & Lu, M. (2018). How to practice person-centred care: A conceptual framework. Health Expectations , 21 (2), 429–440. Web.
Stubbe, D. E. (2020). Practicing cultural competence and cultural humility in the care of diverse patients. Focus , 18 (1), 49–51. Web.
- Person-centered Approach vs. Cognitive-Behavioral Approach
- Psychology. Existential and Person-Centered Theories
- The Person-Centered Theory by Carl Rogers
- The Merging of Departments for Cost Containment
- The Future of Nursing Workforce in 50 Years
- Doctor of Nursing Practice Essentials in Psychiatry
- Middle-Range Theories and Conceptual Models
- Nursing Theory Discussion Board
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, June 6). The Person-Centered Care in Nursing. https://ivypanda.com/essays/the-person-centered-care-in-nursing/
"The Person-Centered Care in Nursing." IvyPanda , 6 June 2023, ivypanda.com/essays/the-person-centered-care-in-nursing/.
IvyPanda . (2023) 'The Person-Centered Care in Nursing'. 6 June.
IvyPanda . 2023. "The Person-Centered Care in Nursing." June 6, 2023. https://ivypanda.com/essays/the-person-centered-care-in-nursing/.
1. IvyPanda . "The Person-Centered Care in Nursing." June 6, 2023. https://ivypanda.com/essays/the-person-centered-care-in-nursing/.
Bibliography
IvyPanda . "The Person-Centered Care in Nursing." June 6, 2023. https://ivypanda.com/essays/the-person-centered-care-in-nursing/.
Academic Support for Nursing Students
No notifications.
Disclaimer: This essay has been written by a student and not our expert nursing writers. View professional sample essays here.
View full disclaimer
Any opinions, findings, conclusions, or recommendations expressed in this essay are those of the author and do not necessarily reflect the views of NursingAnswers.net. This essay should not be treated as an authoritative source of information when forming medical opinions as information may be inaccurate or out-of-date.
Person-centred Care Essay
Info: 2359 words (9 pages) Nursing Essay Published: 11th Feb 2020
Reference this
Introduction: Reflective essay on person centred care
If you need assistance with writing your nursing essay, our professional nursing essay writing service is here to help!
Our nursing and healthcare experts are ready and waiting to assist with any writing project you may have, from simple essay plans, through to full nursing dissertations.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services

- Nursing Essay Writing Service

- Nursing Dissertation Service

- Reflective Writing Service
DMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on the NursingAnswers.net website then please:
Our academic writing and marking services can help you!
- Marking Service
- Samples of our Work
- Full Service Portfolio
Related Lectures
Study for free with our range of nursing lectures!
- Drug Classification
- Emergency Care
- Health Observation
- Palliative Care
- Professional Values

Write for Us
Do you have a 2:1 degree or higher in nursing or healthcare?
Study Resources
Free resources to assist you with your nursing studies!
- APA Citation Tool
- Example Nursing Essays
- Example Nursing Assignments
- Example Nursing Case Studies
- Reflective Nursing Essays
- Nursing Literature Reviews
- Free Resources
- Reflective Model Guides
- Nursing and Healthcare Pay 2021
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Whose centre is it anyway? Defining person-centred care in nursing: An integrative review
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Central Queensland University School of Nursing, Midwifery and Social Science, Townsville, Queensland, Australia
Roles Conceptualization, Methodology, Supervision, Validation, Visualization, Writing – review & editing
Roles Conceptualization, Investigation, Methodology, Supervision, Validation, Writing – review & editing
- Amy-Louise Byrne,
- Adele Baldwin,
- Clare Harvey

- Published: March 10, 2020
- https://doi.org/10.1371/journal.pone.0229923
- Peer Review
- Reader Comments
The aims of this literature review were to better understand the current literature about person-centred care (PCC) and identify a clear definition of the term PCC relevant to nursing practice.
Method/Data sources
An integrative literature review was undertaken using The Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, Scopus and Pubmed databases. The limitations were English language, full text articles published between 1998 and 2018 within Australian, New Zealand, Canada, USA, Europe, Ireland and UK were included. The international context off PCC is then specifically related to the Australian context.
Review methods
The review adopted a thematic analysis to categorise and summarise themes with reference to the concept of PCC. The review process also adhered to the Preferred Reporting System for Meta-Analysis (PRISMA) and applied the Critical Appraisal Skills Programme (CASP) tools to ensure the quality of the papers included for deeper analysis.
While definitions of PCC do exist, there is no universally used definition within the nursing profession. This review has found three core themes which contribute to how PCC is understood and practiced, these are People , Practice and Power . This review uncovered a malalignment between the concept of PCC and the operationalisation of the term; this misalignment was discovered at both the practice level, and at the micro, meso and micro levels of the healthcare service.
The concept of PCC is well known to nurses, yet ill-defined and operationalised into practice. PCC is potentially hindered by its apparent rhetorical nature, and further investigation of how PCC is valued and operationalised through its measurement and reported outcomes is needed. Investigation of the literature found many definitions of PCC, but no one universally accepted and used definition. Subsequently, PCC remains conceptional in nature, leading to disparity between how it is interpreted and operationalised within the healthcare system and within nursing services.
Citation: Byrne A-L, Baldwin A, Harvey C (2020) Whose centre is it anyway? Defining person-centred care in nursing: An integrative review. PLoS ONE 15(3): e0229923. https://doi.org/10.1371/journal.pone.0229923
Editor: Janhavi Ajit Vaingankar, Institute of Mental Health, SINGAPORE
Received: September 17, 2019; Accepted: February 18, 2020; Published: March 10, 2020
Copyright: © 2020 Byrne et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: The author(s) received no specific funding for this work. The publication is funded under the first authors Research Higher Degree (PhD) budget.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Healthcare is changing, for both providers and recipients of care, with ongoing challenges to traditional roles and power balances. The causative factors of changes to the way healthcare is provided are complex, but one contributing factor is easier access to healthcare information and better-informed populations [ 1 ] whereby people as healthcare consumers have access to healthcare information through multiple media. On the surface, consumers are no longer seen as passive recipients of care, but rather as valuable and active members of the healthcare team. The concept of Person-Centred Care (PCC) is used to describe a certain model for the role of the patient within the healthcare system and the way in which care is provided to the patient [ 2 , 3 ]. Globally, there is continued advocacy for person-centred, individualised care [ 4 ], with the contemporary term for PCC being frequently presented in healthcare discourse, and frequently associated with the safety and quality of healthcare service provision [ 5 , 6 ]. Indeed, partnering with consumers within a person-centred framework is now a fundamental requirement for Australian healthcare services, meaning that they cannot achieve accreditation without demonstration of PCC [ 7 ]. Hence, PCC is now seen in healthcare service strategy and models of care, designed to support the voice of the patient and the role of the healthcare service in engaging with patients [ 6 ]. PCC also forms part of the Australian nursing professional standards [ 8 ] yet is paradoxically described as an ‘extra’ to nursing practice [ 9 ], taking a back seat to nursing tasks and errands that make up the day to day regime of the nurse.
Despite the discourse around PCC, and the requirements of PCC within healthcare, there appears to be no universally accepted definition of the term. This leaves the concept open to interpretation and potential confusion, particularly when personnel, in this case nurses, attempt to operationalise it. This review investigated the meaning of PCC with reference to nurses across different practice settings and specialities. To further facilitate the understanding [ 10 ] and theory development of the concept of PCC, this review adopted an integrative review methodology [ 11 ].
In the late 1950’s and 60’s, PCC, and care for the entire self was first described in the context of psychiatry, such as in Rogers’ ‘On becoming a person’ [ 12 ]. Patient-centred medicine was a term first coined by psychoanalyst Michael Balint. Balint was instrumental in the education of general practitioners around psychodynamic factors of patients and challenged the traditional illness-orientated model [ 13 ]. Balint’s challenge extended beyond the traditional healthcare model to include both the physical and psychosocial as part of the practitioner’s role. Balint explained; “Here , in additional to trying to discover a localized illness or illnesses , the doctor also has to examine the whole person in order to form what we call an ‘overall diagnosis . ’ The patient , in fact , has to be understood as a unique human-being . ” [ 13 p269].
The idea of caring for the whole person, and the divide between traditional medical practice and the psychosocial needs of the patient was discussed by Engle in 1977. He wrote; “The dominant model of disease today is biomedical…It assumes disease to be fully accounted for by deviations from the norm of measurable biological (somatic) variables . It leaves no room within its framework for the social , psychological , and behavioural dimensions of illness . ” [ 14 p379]. The biopsychosocial model proposed provided a new basis for care which included care of the mind and body. Over the succeeding years, this model of care and the notion of patient centre care continued to evolve, with many iterations of the term moving with the changing climate of healthcare systems.
PCC gained significant traction through the Institute of Medicines (IOM) 2001 report ‘Crossing the Quality Chasm: A New Health System in the 21 st Century’ [ 15 ] as a key element of quality healthcare. The IOM provided one of the first contemporary definitions, stating that PCC “encompasses qualities of compassion , empathy and responsiveness to the needs , values and expressed preferences of the individual patient” [ 15 p48]. The World Health Organization continues to advocate for integrated care that is in tune with the patient’s wants and needs through the framework on Integrated People-Centred Care. This includes the vision that “all people have equal access to quality health services that are co-produced in a way that meets their life course needs” . [ 5 ] This framework aims to improve engagement of people and communities, strengthen governance and accountability, reorientate the model of healthcare, and coordinate services across sectors [ 5 ], seeing people as important contributors and decision makers over their own care.
More recently, the Australian Commission on Safety and Quality in Health Care (ACSQHC) defines PCC as an “innovative approach to the planning , delivery , and evaluation of health care … [involving] mutually beneficial partnerships among health care providers , patients , and families . ” [ 2 p13]. Thus, PCC has become an integral element of care from a quality, planning and practice level, and therefore appears prominently in Australian healthcare service discourse and associated models of care, often presented as an underpinning philosophy for the way in which nursing care is provided [ 3 ]. The concept of PCC continues to evolve, notably in the change to ‘person’ rather than ‘patient’ in recognition of the whole person, not simply the disease process. Other variables such as Family-centred care are used more in the context of aged care and paediatrics [ 16 , 17 ].
As the term has become more common in healthcare discourse, frameworks have emerged to allow the term to be operationalised into practice. There are several person-centred nursing frameworks including the Senses [ 18 ], VIP [ 19 ], 6 C’s [ 20 ], The Burford Model [ 21 ] and McCormack and McCance’s framework [ 22 ]. These frameworks describe elements such as attributes of staff, methods of interactions, coordination of care and services, the care environment and consideration of outcomes of care. These examples provide insight into attempts to operationalise PCC, into individual practice and healthcare service provision.
Nurses are the healthcare professionals who spend the most time with people and are therefore in a position to act as their advocates, with nursing staff managing the continuity of care [ 23 ]. This review seeks to investigate the meaning of person-centred nursing practice, and acts as a starting point for a wider study into the concept of PCC for people with long term conditions. Consumers of healthcare navigate a complex and fragmented system, with fragmentation leading to patients feeling lost, and a decrease in the quality of services offered [ 24 ]. This places even greater importance on a partnership between provider and receiver, particularly in the face of increasing chronicity/complexity of care. Within this fragmented and complex system, the patient must always remain at the centre of their care. Hence, there is a need for a robust definition to ensure PCC is more clearly operationalised and care delivered is designed around the needs of the patient, rather than trying to make the patient fit within the system.
This review uses the term person rather than patient in recognition of the person as a whole. Where clarity is required, the term healthcare consumer is used; a term frequently used in Australia.
The aim of this literature review was to understand better from the literature how nurses operationalise the definition of PCC.
Search questions
This literature review sought to answer the following questions:
- Is there a commonly/generally accepted definition for PCC that is used by nurses?
- How do nurses operationalise PCC in practice?
Search strategy
An integrative literature review was conducted using the terms Person Cent* Care OR Patient Cent* Care AND Nurs* AND Definition OR Meaning OR understanding OR Concept. The search was expanded to include similar terms and concepts such as patient/person-centredness and personalisation. A major subject heading of ‘patient centred care’ was used within the searches. This review is positioned within the nursing discipline; therefore, articles were included if they were specific to nursing or if they included nursing texts in the review. English language, full text articles published between 1998 and 2018 were included. Publications from Australia and New Zealand, Canada, USA, Europe, UK and Ireland were included to gain an understanding of PCC in the western context. The Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, Scopus and Pubmed databases were searched. This search is registered with PROSPERO (ID number 148778) and was completed in March 2019. While the search strategy includes international literature, this will be related back to the Australian context, in order to understand how PCC operates within Australia.
Data extraction
The framework, from Whittemore and Knafl [ 11 ], describes a comprehensive review, identifying the maximum number of eligible primary sources and requires the researcher to explicitly justify decisions made in the sampling. Using this framework, a total of 1817 articles met the search terms, highlighting the volume of literature available on the concept of PCC. Table 1 provides the scope of inclusions and exclusions. From this, 255 articles were selected for review.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0229923.t001
After removal of duplicates, 203 articles were subjected to full review. A further refined strategy excluded Key Performance Indicators (KPI), service measures, assessment tools and validations as the goal was defining the term, rather than to assess how it is measured; these represented a large proportion of the articles within the search. A total of 44 articles were subjected to quality review. To ensure adequate rigour, reliability and relevance, all articles were evaluated against the Critical Appraisal Skills Programme (CASP) systematic and qualitative review checklists [ 25 , 26 ] by the lead author and reviewed by a senior researcher on the team. The relevance of the papers and the quality of the reviews/articles themselves was appraised. All articles were appraised against the aims of this review. Following this, a total of 17 articles were included in the final review. Fig 1 provides the summary for the search process while S1 File provides the PRISMA checklist.
https://doi.org/10.1371/journal.pone.0229923.g001
Using the previously identified framework that allowed for data from diverse methods and approaches to be analysed and compared, a constant comparison method was used to convert data from different categories into patterns, themes and relationships. The data is thus displayed below in Table 2 to encompass the full depth of the concept and to provide new understanding, and its implications to practice [ 11 ]. Table 2 demonstrates the characteristics of the articles reviewed including their design methods, populations and findings.
https://doi.org/10.1371/journal.pone.0229923.t002
This review set out to investigate if a universal definition of PCC for nursing exists and is used; what was uncovered was a deeper understanding of the concept and operationalisation of PCC, highlighting a malalignment between concept and reality. Three (3) core themes were identified in the review process, each of which is comprised of two (2) sub-themes. These three core themes of People , Practice , and Power , with the respective sub-themes are discussed are summarised in Table 3 .
https://doi.org/10.1371/journal.pone.0229923.t003
Theme 1: People
Unsurprisingly, the most common threads in the literature about PCC relate to people and, consistent with the philosophy of PCC, is described as basic, human kindness and respectful behaviour [ 22 , 27 , 28 , 29 ]. The core theme of People comprises two sub-themes: Recognising uniqueness and Partnerships .
Recognising uniqueness.
PCC, as the name suggests, is care that is considered and based on the individual person, who is the recipient of care. Prominent in the literature are the concepts of personhood, individuality and uniqueness [ 16 , 28 , 30 ]. Individuality, and the sense of self, understands that each person has their own unique wants, needs and desires [ 16 , 29 ] Personhood reinforces and values the complete person, with an understanding that illness affects the entire person [ 31 ]; an holistic consideration of the person that extends to family interventions and involvement [ 27 , 32 ] described as developing and maintaining trust within the family unit [ 33 , 34 ]. Uniqueness is central to this subtheme as recognition of the person as a unique being leads to unique and tailored care, based on the needs of the whole person [ 16 , 29 ].
Partnership.
The literature discusses the need for a relationship between healthcare provider and healthcare receiver as a way of facilitating information, knowledge and decision making. The term ‘relationship’ is prominent in the literature including the terms therapeutic relationship [ 16 ], clinical relationship [ 35 ] and partnership [ 29 , 36 , 37 ]. This is described in the contexts of cohesive, cooperative teams [ 29 , 32 ], mutuality between provider and receiver [ 38 ], and the balance of power and the sharing of knowledge [ 16 ]. These themes are further developed through the practice of the nurse and are thus carried forward to the next theme, Practice.
Theme 2: Practice
PCC is a product of person-centred practice, particularly in the context of nursing. However, the ability to practice PCC is influenced by professional and system factors. The core theme of Practice is comprised of the sub-themes Doing and Space .
‘Doing’ refers to the complex interplay of professional attributes, behaviours and tasks that makes up the daily remit of the nurse; that is, the ‘doing’ of nursing is a combination of these things within the care environment. Personal attributes of nursing staff emerge as a common element in the literature related to PCC. The literature describes attributes such as communication, respect, values, empathy, compassion and non-judgemental behaviour [ 9 , 29 ]. Lusk and Fater [ 7 ] further describe such attributes as caring, faith and hope, trust, relationships, teaching, learning and listening. In describing a framework to facilitate the practice of person-centred care, McCormack and McCance [ 22 ] discussed professional competence, interpersonal skill, job commitment and professional insight. Others have extended this to include understanding vulnerability, fear, the patient identity [ 30 ] and highlight the need to recognise the person as competent to make decisions [ 31 ]. This view, centred on dignity and privacy and the moral and ethical behaviours of the nurse [ 16 , 28 ], facilitates the relationship and balance of power with the person. Delivering whole person care includes elements such as respect for the individual [ 16 ], and planning care that is based on individual needs [ 25 ]. In practice, this is described as the person being valued for their lived experience, life stories [ 9 , 16 ] and the continuation of self [ 34 ]. Kitson et al. [ 35 ] describe this as addressing both the physical and emotional needs of the person and alleviating anxiety.
The existing literature alludes to the idea of opening a space to practice PCC. The literature describes this as being flexible within the care, offering choice [ 9 , 31 ], and creating opportunities for people to engage [ 34 ]. Practicing PCC involves freely giving information to the person [ 36 ] and finding the time to listen and engage with them [ 36 , 39 ], which implies that PCC is a proactive way of delivering nursing care. Gachoud et al. [ 32 ] found that nurses see themselves as most important in delivering PCC, with Doctors playing a lesser role in PCC practice. This understanding creates a concept whereby nurses are pivotal in creating an environment in which the person can truly engage.
While PCC is an individual practice method, the environment within which nurses’ practice must be considerate and supportive of the delivery of PCC as a significant priority; a view supported by McCormack and McCance [ 22 ] in their description of organisational systems and leadership within PCC. Despite competing priorities and the associated tasks of daily practice, nurses must find and open a space to practice PCC as an essential element of the profession. Interestingly, PCC within the literature is often discussed as an addition to nursing tasks. Edvardsson et al. state that promoting PCC in aged care includes doing ‘little extras’ [ 9 p50], such as understanding the patient’s life story, making eye contact and using the person’s name. Marshall et al. found that nurses describe PCC as ‘making the effort’ and ‘going the extra mile’ [ 37 p2667], being helpful and timely with care and attention. Others describe making choices available [ 16 ], ascertaining priorities [ 27 ] and doing the ‘right’ thing [ 31 ].
Theme 3: Power
PCC as a concept is about balancing power between the provider and receiver of care. The notion of PCC is imbued with connotation of power, discussed in relation to all elements of the care and is intertwined in some way with all themes within this review. The sub-themes of Power are the Power over one’s care and the Power to practice PCC .
Power over one’s care.
The idea of power balance is discussed in the literature and includes the sharing of knowledge [ 29 ], respect for decision making and individualised care based on these decisions [ 28 , 17 ]. Further to this is the notion of the person having ‘active’ involvement in the care process [ 22 , 35 ]. This is described through identification of the person’s strengths and reinforcing this through the care continuum [ 16 , 38 ]. In addition to this, the literature describes empowerment, promoting the sense of self efficacy [ 31 , 33 , 37 ], supporting the person to be as self-managing as possible [ 36 ] or to have a level of autonomy in their care. Here, the person holds the power in care planning and decision making throughout the care journey and there is a responsibility of knowledge transference and the maintenance of personal autonomy [ 35 ]. This is apparent in the literature through concepts such as control, rights, patient involvement and participation [ 27 , 33 , 35 ]. PCC, however, places importance on a marriage between provider and receiver as a process of sharing knowledge, rather being entirely self-governing, in which the provider (as the custodian of knowledge) has an obligation to impart knowledge.
The power to practice PCC.
The need for care systems to be innovative and make a commitment to PCC comes through in the literature [ 22 ], as well as the need for the environment to allow for flexibility and to factor time and space to practice PCC [ 9 , 36 ]. This is a significant shift from the traditional biomedical model, whereby emphasis on personal choice [ 33 ] and partnerships [ 17 ] must be considered within all layers of the healthcare system. Barriers and enablers including workplace culture, leadership [ 22 ], policy and practice, organisational systems, environment [ 28 , 35 ], workload, and ward culture [ 37 ] were identified. The literature also included topics around cost [ 28 ], care coordination [ 28 , 33 ] and of course, outcomes of clinical care provided [ 27 , 29 , 30 ].
Jakimowicz et al. [ 30 ] noted the conflict between system standards, benchmarking and the provision of PCC in a time poor environment. Consistently, the literature discussed the idea of measuring PCC as a method of quantifying this important element of nursing practice amongst the myriad of measurable tasks nursing time is allocated to. The need and ability to measure PCC is cited as crucial for quality improvement of care [ 31 , 38 ]. This review excluded articles related to the measurement of PCC as the primary aim was to find how PCC was defined, however this was still very much a part of the discussion around the meaning and practice of PCC. Morgan and Yoder [ 31 ] discussed several measurement tools, finding them to align more with the effect of care rather than the care directly. Lawrence & Kinn [ 27 ] found that outcome measures used where often in line with the needs and requirements of clinicians, auditors and researchers, or hospital clinical outcomes [ 33 ], rather than with the goals of the patient. Outcomes vary from self-care, patient satisfaction, well-being and improved quality of care [ 28 , 31 , 38 ] to improved adherence and decreased hospitalisation [ 29 ]. This highlights competing priorities within the nursing profession and demonstrates that nursing time is conflicted between what they ‘should’ do and what they ‘must’ do, hence highlighting a nurses limited power to practice PCC in the context of the system standards.
The review demonstrates that the concept of PCC is indeed a method of providing care, or the way in which nurses deliver care. To be person-centred, the nurse must recognise the person as unique, form meaningful partnerships, open a space within the doing of their day to involve and engage with the person, allowing the person control and power of their care.
It is interesting to note that while the existing literature covers a wide variety of clinical areas, and patient and staff perspectives, there were indeed core common themes of PCC. Despite the core concepts associated with PCC taking on more importance within certain clinical areas; for example, continuation of self in aged care [ 9 , 34 ], patient advocacy for intensive care [ 30 ], or communication in stroke care [ 27 ], they are consistent across specialities with the themes building on one another. Perhaps the reason why PCC has been so widely accepted is that the characteristics are simple, kind, human interactions, valuing both the person and the care provider. While definitions of PCC exist, there is no one universally used definition of PCC in nursing practice, potentially compounding a degree of separation between practice and healthcare systems. The findings demonstrate a tension between the theory and the conceptualisation of PCC, and as a result, the operationalisation of the term at both the practice level and a wider healthcare service level.
At the practice level, the theory/practice gap for PCC was evident. The theory/practice gap includes elements of practice failing to reflect theory, perceptions of theory being irrelevant to practice, and ritualistic nursing practice. Consequences of the theory/practice gap can greatly influence nursing practice and collaboration [ 40 ]. In the context of PCC, the theory/practice gap is apparent in the challenge of translating the ideas of PCC into a concrete concept. It is of significance that PCC is seen as ‘extra’ or additional to nursing tasks when these professional behaviours are in line with the Australian Nursing Professional Standards [ 8 ], which requires that they are an intrinsic element of the nursing profession. In fact, to be a registered nurse in Australia one must demonstrate respect for the person as the expert, respect autonomy and “ share knowledge and practice that supports person-centred care” [ 8 ]. This highlights an important matter for consideration; why are core elements of PCC being viewed as ‘going the extra mile’ rather than a core competency for nurses? Certainly, from the perspective of the professional standards, PCC should not be the road less travelled, but rather the daily standard practice of nursing. One answer to this may be the task orientation of the contemporary nursing culture that sees nurses required to meet organisational time allocations for care [ 41 ]. Sharp, McAllister and Broadbent [ 42 ] uncovered a tension between PCC and nursing culture, finding that nurses were increasingly bogged down with tasks and processes, taking them away from the people that they provide nursing care for. These authors found that this led to a feeling of frustration and helplessness in nurses who appear to have accepted the culture of auditable, measurable activities and processes, particularly within the climate of organisational accreditation requirements. This activity-based nursing environment manifests in missed nursing care largely related to patient centred elements, e.g. discharge planning, communication within the healthcare team, absence of adequate patient education on key factors of care such as medication guidance, functional assessment and so on [ 43 , 44 ].
Further, it is apparent that the concept of PCC cannot be isolated from other philosophies of nursing practice and in fact, is embedded in other approaches to nursing care. For example, as outlined by Kim [ 45 ], nursing is defined by dimensions, rather than characteristics. If PCC is considered as a dimension, a complex, interwoven mix of characteristics, then it is possible to gain some concrete understanding of PCC in the context of all clinical areas. The five dimensions proposed by Kim reflect the ‘human’ side of nursing practice, and like the general interpretation of PCC, shows how human interactions, values and knowledge combine to provide care. Kim goes on to say that these dimensions vary with individual nurses and changing clinical situations; which seems to fit with the current confusion about PCC giving choice and decision-making power to patients. As found in this review, PCC attempts to balance the power between providers of care and receivers, giving choice and decision-making power. Yet the focus on nursing tasks and prioritisation of these tasks is evident, demonstrating the malalignment between concept and practice, where research has identified that the current task-oriented system of nursing does fail to meet the care needs of patients [ 46 ].
Nursing practice, however, is only one element of delivering PCC within the healthcare system. This disparity extends between the concept of PCC and its ability to exist within the current healthcare system itself, where time to care is explicitly rationed through budgets that do not allow for individualised person-centred care [ 47 ].
The notion of PCC is one centred on mutuality and a balance of power; a distinct move from the paternalistic biomedical model to a biopsychosocial model that is guided by the person, rather than the disease process. However, in current healthcare services, care is often system centred. That is, care is organised, funded and coordinated in a way that meets the needs of the system or service [ 28 , 33 ]. System fragmentation is understood to have significant influence on people accessing care, whereby people with long-term and complex conditions are most vulnerable to the negative impact from the lack of care coordination and cohesion [ 48 ].
In Australia, complex funding models are central to the concept of system fragmentation which begins at the Commonwealth and State funding levels [ 48 ], making it difficult for patients to navigate the system. System silos remain a significant issue for healthcare services and for the delivery of care, with Medicare models remaining fragmented for specialist services [ 49 ]. The States are the healthcare system managers, yet the federal government holds the responsibility of leading primary healthcare. This presents a challenge in provided collaborative and integrated services, particularly for those with long-term conditions [ 50 ]. The OECD highlight the importance of reducing system fragmentation in order to ‘Improve the co-ordination of patient care .’ [ 50 p1].
Indeed, system fragmentation leads to an increased ‘treatment burden’, whereby poor treatment coordination, ineffective communication and confusion about treatments can contribute to poor health outcomes and greater levels of cost, time, travel and medications for the person [ 51 ] Sav et al. [ 51 ] discuss the need for individualised and coordinated services across specialities as a requirement for reducing treatment burden. In addition to this, the Australian Charter of Healthcare Rights prescribes the rights of those seeking care in any Australian service and includes the right to access, respect, communication and participation [ 52 ]. Accreditation of healthcare services is conditional to evidence of multi-level partnerships with consumers of health. Positive partnerships (PCC) are clearly linked to improved access to care, which in turn leads to reports of positive experiences and better-quality healthcare. Of critical importance at an organisational and government level, the standards also describe this partnership as a mechanism for reducing hospital costs through improved rates of preventable hospitalisation and reducing hospital length of stay [ 7 ].
Potentially Preventable Hospitalisations (PPH) place considerable economic and resource burden on the healthcare system, with approximately 47% of PPH being attributed to long-term conditions [ 53 ]. Thus, reducing preventable hospitalisation is a measurable target for healthcare services under the National Healthcare Agreement as a way of controlling the escalating costs of care and maintaining sound fiscal management of public services [ 54 ]. In line with the ACSQHC standard Partnering with Consumers , PCC has been introduced to some services as a mechanism for improving communication between services and those with long term conditions. What is less clear, is how care tailored to the individuals wants and needs of the patient (PCC), exists within a system predominately focused on reducing variation and the associated costs of care. While the philosophy of PCC naturally fits within the care environment, understanding how effective it is, how the person is included and how outcomes important to the person are captured, take a lower precedent to the measure of reduced hospital costs, self-efficacy and reduced hospitalisation. Capturing what is important for the individual presents a difficult task for services providing population-based care.
These system wide constraints provide a considerable challenge to nurses in their attempts to operationalise the concept of PCC. Nursing, it seems, has become task orientated, a sentiment supported by Foe & Kitson who found that nurses are constrained by a ‘checklist’ mentality, whereby completing and documenting tasks is seen as more important than engaging with the person [ 55 p100]. These tasks and checklists align with the requirements of the National Standards for hospital accreditation. An example of this is the need to collect data on the use of invasive devices or the allocated time intervals in which screening (such as skin inspection and falls risk) must occur; for example within eight (8) hours of admission [ 7 ]. Indeed, policy and procedure for nursing practice reflect that of the need of accreditation and national policy requirements as opposed to the needs of individual people. While partnering with consumers is an important element of the standards [ 7 ], quantifying the way in which healthcare services and indeed nurses engage with patients is less clear. Kitson states ‘ Nursing theory , it would seem , has been limited by the profession’s ability to systematically document the complexity and richness of what happens when nurses and patients (and their careers) interact’ [ 35 p99], an issue it seems stemming from the fact that nursing interventions promoting person-centred, compassionate care are poorly described, with little to no consensus on the term, and interventions that do exist are poorly evaluated [ 56 ]. On top of this, nurses are generally not encouraged, nor enabled to reflect on practice in order to generate new insights and nursing practice [ 35 ]. Molina-Mula et al. [ 23 ], discuss the nursing profession as being the key to professional teamwork models, meeting the needs of patients and thereby increasing their personal decision-making capacity. However, it is possible that PCC is hindered by the level of professional autonomy, time and space afforded to nurses [ 57 ]. Indeed, the malalignment discussed herein, demonstrates that nurses may be hindered at higher levels of system compliance or difficulties in coordinating care services, which permeates nursing culture and ultimately nursing practice, limiting their ability to provide PCC that is individualised to the people seeking care.
Finally, while this review excluded articles related to the measurement and indicators of PCC, this is undoubtedly linked to its perceived meaning and how it is operationalised. This review demonstrates that the understanding of PCC is made up of how and where PCC appears in healthcare discourse and shows that PCC is potentially skewed by how it is(n’t) measured and the outcomes that are(n’t) reported as a product of PCC. This finding presents a framework within which further investigation of the concept of PCC (Meaning, Practice, Measures, Outcomes) within healthcare services could be undertaken. This proposed framework will be applied by the author to conduct further research into the role of PCC within nurse-led service for people with long-term conditions.
Implications for practice
This review highlights the dominant discourse around the concept of PCC yet uncovered the idea of malalignment between the rhetoric and the reality of the concept. Further exploration of the alignment between healthcare services and the goal of PCC may prove beneficial in ensuring the practice of PCC is fostered from all levels of the healthcare service. The above provides a rationale for why the definition of PCC should be provided, given that the concept is currently somewhat nebulous in nature. A consistent definition, with reference to all levels of the healthcare service including practice, will ensure that the concept stays true to the philosophy of compassionate and balanced care. Any definition provided should carefully consider how PCC is measured and prioritised within the healthcare system, which has the potential to move the concept from its current rhetorical nature, to a genuine commitment and priority of nurses and services. Lastly, the review provides a basis for the importance of nursing education and workforce development of the concept and the practice of PCC, given the apparent barriers that nurses may face in delivering PCC.
Limitations
This integrated review was limited to articles relating to the nursing profession and hence has excluded reviews on PCC in relation to other disciplines. Practice related elements such as procedure, service measures and outcomes of PCC were excluded from this review as the aim was to find a generalised way of defining the term. Furthermore, only one framework met the criteria of the search strategy and was included, there are however, several frameworks for PCC in nursing and hence some elements of PCC and their definitions may have been excluded.
This review was performed with published literature only, with no investigation of grey literature undertaken. PCC is often discussed in healthcare service literature, including procedure, service profiles and service strategy. This information will undoubtedly have an impact on how nurses understand and practice PCC within their own area and within their service. This review was designed to investigate a universal definition of PCC as described in the literature and hence chose to limit this to an academic search. The practice of PCC from a policy to practice perspective perpetuates meaning and will be the subject of further research for the author.
This review was conducted as a starting point for the author’s research higher degree (PhD) studies, and hence the search strategy and quality processes were completed by one person. All elements of the review were discussed at length with academic supervisors to ensure adequate rigor and accuracy throughout the search, review and integrative process.
The concept of PCC is well known to nurses, yet ill-defined and operationalised into practice. Healthcare service policy and care provisions, and indeed nursing services, need a clear definition of PCC in order to work toward embedding it into practice and into models of care in a meaningful and genuine way. However, PCC is potentially hindered by its apparent rhetorical nature, and further investigation of how PCC is valued and operationalised through its measurement and reported outcomes will serve the philosophy of PCC well. Investigation of the literature found many definitions of PCC, but no one universally accepted and used definition. Subsequently, PCC remains conceptional in nature, leading to disparity between how it is(n’t)operationalised within the healthcare system and within nursing services. In light of the malalignment discovered within this review, a universal definition of PCC is not provided herein; instead, this review highlights the need for further investigation of PCC between the levels of the healthcare service (at the micro, meso and macro levels) and how this influences the critical work that nurses do in supporting people through their healthcare journey.
Supporting information
S1 file. prisma checklist..
https://doi.org/10.1371/journal.pone.0229923.s001
- View Article
- Google Scholar
- 2. Australian Commission on Safety and Quality in Healthcare. Patient-centred care: Improving quality and safety by focusing care on patients and consumers. [Internet]. Sydney: ACSQHC; 2010. https://www.safetyandquality.gov.au/wp-content/uploads/2012/01/PCCC-DiscussPaper.pdf (2010).
- PubMed/NCBI
- 4. Health Consumers Queensland. Consumer and Community Engagement Framework for Health Organisations and Consumers. Brisbane: HCQ; 2017. http://www.hcq.org.au/wp-content/uploads/2017/03/HCQ-CCE-Framework-2017.pdf
- 5. World Health Organization. WHO framework on integrated people-centred health Services [Internet]. Geneva: WHO; 2016. http://www.who.int/servicedeliverysafety/areas/people-centred-care/ipchs- what/en/
- 6. Australian Commission on Safety and Quality in Healthcare. Person-centred healthcare organisations. Sydney: ACSQHC; 2018. https://www.safetyandquality.gov.au/our-work/patient-and-consumer-centred-care/person-centred-organisations/
- 7. Australian Commission on Safety and Quality in Healthcare. National Quality and Safety Health Service Standards Second edition. Sydney: ACSQHC; 2017. https://www.safetyandquality.gov.au/wp-content/uploads/2017/12/National-Safety-and-Quality-Health-Service-Standards-second-edition.pdf .
- 8. Nursing and Midwifery Board of Australia. Registered Nurse Standards of Practice. Sydney: NMBA; 2016. https://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Professional-standards/registered-nurse-standards-for-practice.aspx
- 10. Broome ME Integrative literature reviews for the development of concepts. In Rodgers BL, Knafl KA, editors. Concepts Development in Nursing. 2nd ed. Philadelphia: WB Saunders Co; 1993. p.231–250.
- 12. Rogers RR. On becoming a person. New York: Houghton Mifflin; 1995.
- 15. Institute of Medicine. Crossing the Quality Chasm: A new health system for the 21st Century. Washington: IOM; 2001. https://www.med.unc.edu/pediatrics/quality/documents/crossing-the-quality-chasm .
- 18. Nolan MR, Brown J, Davies S, Nolan J, Keady J. The Senses Framework: improving care or older people through relationship-centred approach: Getting research into practice [Internet]. Sheffield: 2006. http://shura.shu.ac.uk/280/1/PDF_Senses_Framework_Report.pdf
- 19. Brooker D. Person-Centred Dementia Care: Making Services Better. London: Jessica Kingsley Publishers; 2007.
- 20. National Health Service (NHS). The 6 Cs. London: NHS; 2016. https://www.england.nhs.uk/leadingchange/about/the-6cs/
- 21. Johns C. The Burford NDU model: Caring in practice. Cambridge: Oxford; 1994.
- 25. Critical Appraisal Skills Programme. Systematic Review. Oxford: CASP; 2018. https://casp-uk.net/wp-content/uploads/2018/03/CASP-Systematic-Review-Checklist-2018_fillable-form.pdf
- 26. Critical Appraisal Skills Programme. Qualitative research. Oxford: CASP; 2018. https://casp-uk.net/wp-content/uploads/2018/03/CASP-Qualitative-Checklist-2018_fillable_form.pdf
- 45. Kim HS. Five Dimensions of Nursing Practice. In: Kim HS. The Essence of Nursing Practice: Philosophy and Perspective. New York: Springer publishing company; 2015. p. 81–102
- 49. Calder R, Dunkin R, Rochford C, Nichols T. Australian Health Services: too complex to navigate. A review of the national reviews of Australia’s health service arrangements. Melbourne: Australian Health Policy Collaboration; 2019. https://www.vu.edu.au/sites/default/files/australian-health-services-too-complex-to-navigate.pdf
- 50. Organisation of Economic Cooperation and Development. Heath Policy Overview Health Policy Australia. Paris: OECD; 2015. http://www.oecd.org/australia/Health-Policy-in-Australia-December-2015.pdf
- 52. Australian Commission on Safety and Quality in Healthcare. Australian Charter of Healthcare Rights. Sydney: ACSQHC; 2008. https://www.safetyandquality.gov.au/australian-charter-healthcare-rights
- 53. Australian Institute of Health and Welfare. Potentially preventable hospitalisations in Australia by small geographic area. Canberra: AIHW; 2019. https://www.aihw.gov.au/reports/primary-health-care/potentially-preventable-hospitalisations/contents/overview
- 54. Australian Institute of Health and Welfare. National Healthcare Agreement. Canberra: AIHW; 2019. https://meteor.aihw.gov.au/content/download.phtml?customDownloadType=mrIndicatorSetAdvanced&itemIds%5B%5D=698954&shortNames=long&includeRMA=0&userFriendly=userFriendly&form=long&media=pdf
Domain 2: Person-Centered Care
Descriptor: Person-centered care focuses on the individual within multiple complicated contexts, including family and/or important others. Person-centered care is holistic, individualized, just, respectful, compassionate, coordinated, evidence-based, and developmentally appropriate. Person-centered care builds on a scientific body of knowledge that guides nursing practice regardless of specialty or functional area.
Contextual Statement: Person-centered care is the core purpose of nursing as a discipline. This purpose intertwines with any functional area of nursing practice, from the point of care where the hands of those that give and receive care meet, to the point of systems-level nursing leadership. Foundational to person-centered care is respect for diversity, differences, preferences, values, needs, resources, and the determinants of health unique to the individual. The person is a full partner and the source of control in team-based care. Person-centered care requires the intentional presence of the nurse seeking to know the totality of the individual’s lived experiences and connections to others (family, important others, community). As a scientific and practice discipline, nurses employ a relational lens that fosters mutuality, active participation, and individual empowerment. This focus is foundational to educational preparation from entry to advanced levels irrespective of practice areas.
With an emphasis on diversity, equity, and inclusion, person-centered care is based on best evidence and clinical judgment in the planning and delivery of care across time, spheres of care, and developmental levels. Contributing to or making diagnoses is one essential aspect of nursing practice and critical to an informed plan of care and improving outcomes of care (Olson et al., 2019). Diagnoses at the system-level are equally as relevant, affecting operations that impact care for individuals. Person-centered care results in shared meaning with the healthcare team, recipient of care, and the healthcare system, thus creating humanization of wellness and healing from birth to death.
Search for Resources
Entry-Level Domain 2 Competencies
2.1 Engage with the Individual in establishing a caring relationship.
2.1a Demonstrate qualities of empathy.
2.1b Demonstrate compassionate care.
2.1c Establish mutual respect with the individual and family.
2.2 Communicate effectively with individuals.
2.2a Demonstrate relationship-centered care.
2.2b Consider individual beliefs, values, and personalized information in communications.
2.2c Use a variety of communication modes appropriate for the context.
2.2d Demonstrate the ability to conduct sensitive or difficult conversations.
2.2e Use evidence-based patient teaching materials, considering health literacy, vision, hearing, and cultural sensitivity.
2.2f Demonstrate emotional intelligence in communications.
2.3 Integrate assessment skills in practice.
2.3a Create an environment during assessment that promotes a dynamic interactive experience.
2.3b Obtain a complete and accurate history in a systematic manner.
2.3c Perform a clinically relevant, holistic health assessment.
2.3d Perform point of care screening/diagnostic testing (e.g. blood glucose, PO2, EKG).
2.3e Distinguish between normal and abnormal health findings.
2.3f Apply nursing knowledge to gain a holistic perspective of the person, family, community, and population.
2.3g Communicate findings of a comprehensive assessment.
2.4 Diagnose actual or potential health problems and needs.
2.4a Synthesize assessment data in the context of the individual’s current preferences, situation, and experience.
2.4b Create a list of problems/health concerns.
2.4c Prioritize problems/health concerns.
2.4d Understand and apply the results of social screening, psychological testing, laboratory data, imaging studies, and other diagnostic tests in actions and plans of care.
2.4e Contribute as a team member to the formation and improvement of diagnoses.
2.5 Develop a plan of care.
2.5a Engage the individual and the team in plan development.
2.5b Organize care based on mutual health goals.
2.5c Prioritize care based on best evidence.
2.5d Incorporate evidence-based intervention to improve outcomes and safety.
2.5e Anticipate outcomes of care (expected, unexpected, and potentially adverse).
2.5f Demonstrate rationale for plan.
2.5g Address individuals’ experiences and perspectives in designing plans of care.
2.6 Demonstrate accountability for care delivery.
2.6a Implement individualized plan of care using established protocols.
2.6b Communicate care delivery through multiple modalities.
2.6c Delegate appropriately to team members.
2.6d Monitor the implementation of the plan of care.
2.7 Evaluate outcomes of care.
2.7a Reassess the individual to evaluate health outcomes/goals.
2.7b Modify plan of care as needed.
2.7c Recognize the need for modifications to standard practice.
2.8 Promote self-care management.
2.8a Assist the individual to engage in self-care management.
2.8b Employ individualized educational strategies based on learning theories, methodologies, and health literacy.
2.8c Educate individuals and families regarding self-care for health promotion, illness prevention, and illness management.
2.8d Respect individuals and families’ self-determination in their healthcare decisions.
2.8e Identify personal, system, and community resources available to support self-care management.
2.9 Provide care coordination.
2.9a Facilitate continuity of care based on assessment of assets and needs.
2.9b Communicate with relevant stakeholders across health systems.
2.9c Promote collaboration by clarifying responsibilities among individual, family, and team members.
2.9d Recognize when additional expertise and knowledge is needed to manage the patient.
2.9e Provide coordination of care of individuals and families in collaboration with care team.
Advanced-Level Domain 2 Competencies
2.1d Promote caring relationships to effect positive outcomes.
2.1e Foster caring relationships.
2.2g Demonstrate advanced communication skills and techniques using a variety of modalities with diverse audiences.
2.2h Design evidence-based, person-centered engagement materials.
2.2i Apply individualized information, such as genetic/genomic, pharmacogenetic, and environmental exposure information in the delivery of personalized health care.
2.2j Facilitate difficult conversations and disclosure of sensitive information.
2.3h Demonstrate that one’s practice is informed by a comprehensive assessment appropriate to the functional area of advanced nursing practice.
2.4f Employ context driven, advanced reasoning to the diagnostic and decision-making process.
2.4g Integrate advanced scientific knowledge to guide decision making.
2.5h Lead and collaborate with an interprofessional team to develop a comprehensive plan of care.
2.5i Prioritize risk mitigation strategies to prevent or reduce adverse outcomes.
2.5j Develop evidence-based interventions to improve outcomes and safety.
2.5k Incorporate innovations into practice when evidence is not available.
2.6e Model best care practices to the team.
2.6f Monitor aggregate metrics to assure accountability for care outcomes.
2.6g Promote delivery of care that supports practice at the full scope of education.
2.6h Contribute to the development of policies and processes that promote transparency and accountability.
2.6i Apply current and emerging evidence to the development of care guidelines/tools.
2.6j Ensure accountability throughout transitions of care across the health continuum.
2.7d Analyze data to identify gaps and inequities in care and monitor trends in outcomes.
2.7e Monitor epidemiological and system-level aggregate data to determine healthcare outcomes and trends.
2.7f Synthesize outcome data to inform evidence-based practice, guidelines, and policies.
2.8f Develop strategies that promote self-care management.
2.8g Incorporate the use of current and emerging technologies to support self-care management.
2.8h Employ counseling techniques, including motivational interviewing, to advance wellness and self-care management.
2.8i Evaluate adequacy of resources available to support self-care management.
2.8j Foster partnerships with community organizations to support self-care management.
2.9f Evaluate communication pathways among providers and others across settings, systems, and communities.
2.9g Develop strategies to optimize care coordination and transitions of care.
2.9h Guide the coordination of care across health systems.
2.9i Analyze system-level and public policy influence on care coordination.
2.9j Participate in system-level change to improve care coordination across settings.
The Person-Centred Nursing Framework
- First Online: 27 April 2021
Cite this chapter

- Brendan McCormack 4 &
- Tanya McCance 5
9258 Accesses
9 Citations
In this chapter, the Person-centred Nursing Framework developed by McCormack and McCance [1, 2] will be described, and an updated framework will be presented. This will be placed in the context of the origins of the framework, which are founded on the concepts of caring and person-centredness. The evolution of the framework will be discussed, highlighting the changes over time that have characterised its development. The position of the Person-centred Nursing Framework as a middle-range theory will be explored and placed in the context of nursing theory development as a basis for practice. Finally, we will illustrate the centrally of the framework to knowledge generation that demonstrates a strong relationship between the theory, practice and research of person-centred practice.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or Ebook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Person-Centered Nursing and Other Health Professions
Person-Centred Care, Theory, Operationalisation and Effects

The Concept of Individualised Care
McCormack B, McCance TV. Development of a framework for person-centred nursing. J Adv Nurs. 2006;56(5):1–8.
Article Google Scholar
McCormack B, McCance T. Person-centred nursing: theory and practice. Oxford: Wiley Blackwell; 2010.
Book Google Scholar
Gadamar HG. Truth and method. New York: Crossroad; 1989.
Google Scholar
McCormack B. Negotiating partnerships with older people—a person-centred approach. Basingstoke: Ashgate; 2001.
McCormack B. A conceptual framework for person-centred practice with older people. Int J Nurs Pract. 2003;9:202–9.
Heidegger M. Being and time. Oxford: Blackwell; 2005.
McCance TV. Caring in nursing practice: the development of a conceptual framework. Res Theory Nurs Pract. 2003;17(2):101–16.
McCormack B, McCance T, Slater P, McCormick J, McArdle C, Dewing J. Person-centred outcomes and cultural change. In: Manley K, McCormack B, Wilson V, editors. International practice development in nursing and healthcare. Oxford: Blackwell; 2008. p. 189–214.
Fawcett J. Analysis and evaluation of conceptual models of nursing. 3rd ed. Philadelphia: F. A. Davis; 1995.
Lynch B, McCance T, McCormack B, Brown D. The development of the person-centred situational leadership framework: revealing the being of person-centredness in nursing homes. J Clin Nurs. 2018;27:427–40.
McCance T, Gribben B, McCormack B, Laird E. Promoting person-centred practice within acute care: the impact of culture and context on a facilitated practice development programme. Int Pract Dev J. 2013;3(1):2.
Buckley C, McCormack B, Ryan A. Valuing narrative in the care of older people. J Clin Nurs. 2014;23(17–18):565–2577.
McCormack B, McCance T. United Kingdom: the person-centred nursing model. In: Fitzpatrick JJ, Whall AL, editors. Conceptual models of nursing: global perspectives. New Jersey: Pearson Education; 2016.
McCormack B, McCance T. Person-centred nursing and health care—theory and practice. Oxford: Wiley Publishing; 2017.
Slater P, McCance T, McCormack B. Exploring person-centred practice within acute hospital settings. Int Pract Dev J. 2015. http://www.fons.org/library/journal/volume5-person-centredness-suppl/article9 .
McCormack B, Dewing J, McCance T. Developing person-centred care: addressing contextual challenges through practice development. Online J Issues Nurs. 2011;16(2):3.
PubMed Google Scholar
McCormack B, Dewing J, Breslin L, Tobin C, Manning M, Coyne-Nevin A, et al. The implementation of a model of person-centred practice in older person settings: final report. Dublin: Office of the Nursing Services Director, Health Services Executive; 2010.
Gadow S. Existential advocacy: philosophical foundations of nursing. In: Spicker SF, Gadow S, editors. Nursing: images and ideals—opening dialogue with the humanities. New York: Springer; 1980.
Brown D, McCormack B. Exploring psychological safety as a component of facilitation within the Promoting Action Research in Health Services (PARiHS) framework through the lens of pain management practices with older people. J Adv Nurs. 2016;25:2921–32. https://onlinelibrary.wiley.com/doi/epdf/10.1111/jocn.13348 .
Carmona M. Place value: place quality and its impact on health, social, economic and environmental outcomes. J Urban Des. 2019;24(1):1–48. https://doi.org/10.1080/13574809.2018.1472523 .
Seedhouse D. Health: the foundations for achievement. London: Wiley; 1986.
Titchen A, McCormack B, with Tyagi V. Dancing the mandalas of critical creativity in nursing and healthcare . Centre for Person-centred Practice Research, Queen Margaret University Edinburgh; 2020. https://www.cpcpr.org/critical-creativity .
Mekki TE, Øye C, Kristensen BM, Dahl H, Haaland A, Aas Nordin K, Strandos MR, Terum TM, Ydstebø AE, McCormack B. The inter-play between facilitation and context in the Promoting Action on Research Implementation in Health Services framework: a qualitative exploratory implementation study embedded in a cluster randomised controlled trial to reduce restraint in nursing homes. J Adv Nurs. 2017;73(11):2622–32.
Laird L, McCance T, McCormack B, Gribben B. Patients’ experiences of in-hospital care when nursing staff were engaged in a practice development programme to promote person-centredness: a narrative analysis study. Int J Nurs Stud. 2015;52(9):1454–62. https://doi.org/10.1016/j.ijnurstu.2015.05.002 .
Article PubMed Google Scholar
New South Wales Health 2012 Essentials of care program in NSW, Australia. https://www.health.nsw.gov.au/nursing/culture/Documents/essentials-of-care-program-overview.pdf . Accessed Aug 2020.
Slater P, Bunting B, McCormack B. The development and pilot testing of an instrument to measure nurses’ working environment: the nursing context index. Worldviews Evid-Based Nurs. 2009;6(3):173–82.
McCormack B, McCarthy G, Wright J, Slater P, Coffey A. Development and testing of the context assessment index. Worldviews Evid Based Nurs. 2009;6(1):27–35.
Slater P, McCance TV, McCormack B. The development and testing of the Person-centred Practice Inventory—Staff (PCPI-S). Int J Qual Health Care. 2017;29(4):541–7. https://doi.org/10.1093/intqhc/mzx066 .
Wilson V, Dewing J, Cardiff S, Mekki TE, Øye C, McCance T. A person-centred observational tool: devising the Workplace Culture Critical Analysis Tool®. Int Pract Dev J. 2020;10:1. https://doi.org/10.19043/ipdj.101.003 .
Article CAS Google Scholar
McCance TV, Telford L, Wilson J, MacLeod O, Dowd A. Identifying key performance indicators for nursing and midwifery care using a consensus approach. J Clin Nurs. 2012;21(7&8):1145–54.
McCance T, Hastings J, Dowler H. Evaluating the use of key performance indicators to evidence the patient experience. J Clin Nurs. 2015;24:3084–94.
McCance T, Wilson V. Using person-centred key performance indicators to improve paediatric services: an international venture. Int Pract Dev J. 2015;5:8. https://www.fons.org/library/journal/volume5-person-centredness-suppl/article8 .
McCance T, Wilson V, Korman K. Paediatric International Nursing Study: using person-centred key performance indicators to benchmark children’s services. J Clin Nurs. 2016;25(13–14):2018–27.
Knowles M. The adult learner: a neglected species. 3rd ed. Houston: Gulf Publishing; 1984.
O’Donnell D, McCormack B, McCance T, McIlfatrick S. A meta-synthesis of person-centredness in nursing curricula. Int Pract Dev J. 2020;10(2)(special issue). https://doi.org/10.19043/ipdj.10Suppl2.002 .
McCormack B, Dewing J. International Community of Practice for Person-centred Practice: position statement on person-centredness in health and social care Curricula. Int Pract Dev J. 2019;9(1):3. https://doi.org/10.19043/ipdj.91.003 .
Haraldsdottir E, Donaldson K, Lloyd A, McCormack B. Reaching for the rainbow: person-centred practice in palliative care. Int Pract Dev J. 2020;10(1):5. https://www.fons.org/Resources/Documents/Journal/Vol10No1/IPDJ_10_01_05.pdf.
McCormack B, Dickson C, Smith T, Ford H, Ludwig S, Moyes R, Lee L, Adam E, Paton T, Lydon B, Spiller J. ‘It’s a nice place, a nice place to be’. The story of a practice development programme to further develop person-centred cultures in palliative and end-of-life care. Int Pract Dev J. 2018;8(1):2. https://doi.org/10.19043/ipdj81.002 .
Download references
Author information
Authors and affiliations.
Division of Nursing, School of Health Science, Queen Margaret University, Musselburgh, UK
Brendan McCormack
School of Nursing, Ulster University, Newtownabbey, Northern Ireland
Tanya McCance
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Brendan McCormack .
Editor information
Editors and affiliations.
Division of Nursing - School of Health Science, Queen Margaret University, Musselburgh, UK
School of Nursing, University of Ulster, Newtownabbey, UK
Rights and permissions
Reprints and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
McCormack, B., McCance, T. (2021). The Person-Centred Nursing Framework. In: Dewing, J., McCormack, B., McCance, T. (eds) Person-centred Nursing Research: Methodology, Methods and Outcomes. Springer, Cham. https://doi.org/10.1007/978-3-030-27868-7_2
Download citation
DOI : https://doi.org/10.1007/978-3-030-27868-7_2
Published : 27 April 2021
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-27867-0
Online ISBN : 978-3-030-27868-7
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Open access
- Published: 03 September 2021
A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward
- Abukari Kwame 1 &
- Pammla M. Petrucka 2
BMC Nursing volume 20 , Article number: 158 ( 2021 ) Cite this article
399k Accesses
179 Citations
97 Altmetric
Metrics details
Providing healthcare services that respect and meet patients’ and caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns, beliefs, and contextual variables. Achieving patient-centered care and communication in nurse-patient clinical interactions is complex as there are always institutional, communication, environmental, and personal/behavioural related barriers. To promote patient-centered care, healthcare professionals must identify these barriers and facitators of both patient-centered care and communication, given their interconnections in clinical interactions. A person-centered care and communication continuum (PC4 Model) is thus proposed to orient healthcare professionals to care practices, discourse contexts, and communication contents and forms that can enhance or impede the acheivement of patient-centered care in clinical practice.
Peer Review reports
Providing healthcare services that respect and meet patients’ and their caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thus constituting patient-centered care. Care is “a feeling of concern for, or an interest in, a person or object which necessitates looking after them/it” [ 1 ]. The Institute of Medicine (IOM) noted that to provide patient-centered care means respecting and responding to individual patient’s care needs, preferences, and values in all clinical decisions [ 2 ]. In nursing care, patient-centered care or person-centered care must acknowledge patients’ experiences, stories, and knowledge and provide care that focuses on and respects patients’ values, preferences, and needs by engaging the patient more in the care process [ 3 ]. Healthcare providers and professionals are thus required to fully engage patients and their families in the care process in meaningful ways. The IOM, in its 2003 report on Health Professions Education , recognized the values of patient-centered care and emphasized that providing patient-centered care is the first core competency that health professionals’ education must focus on [ 4 ]. This emphasis underscored the value of delivering healthcare services according to patients’ needs and preferences.
Research has shown that effective communication between patients and healthcare providers is essential for the provision of patient care and recovery [ 5 , 6 , 7 , 8 ]. Madula et al. [ 6 ], in a study on maternal care in Malawi, noted that patients reported being happy when the nurses and midwives communicated well and treated them with warmth, empathy, and respect. However, other patients said poor communication by nurses and midwives, including verbal abuse, disrespect, or denial from asking questions, affected their perceptions of the services offered [ 6 ]. Similarly, Joolaee et al. [ 9 ] explored patients’ experiences of caring relationships in an Iranian hospital where they found that good communication between nurses and patients was regarded as “more significant than physical care” among patients.
According to Boykins [ 10 ], effective communication is a two-way dialogue between patients and care providers. In that dialogue, both parties speak and are listened to without interrupting; they ask questions for clarity, express their opinions, exchange information, and grasp entirely and understand what the others mean. Also, Henly [ 11 ] argued that effective communication is imperative in clinical interactions. He observed that health and illness affect the quality of life, thereby making health communication critical and that the “intimate and sometimes overwhelming nature of health concerns can make communicating with nurses and other healthcare providers very challenging” [ 11 ]. Furthermore, Henly [ 11 ] added that patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns. Given the prevalence of face-to-face and device-mediated communications and interactions in healthcare settings, we must explore and clarify who, what, where, when, why, and how interactions with individuals, families, and communities are receiving care and health services [ 11 ].
The value of effective communication in nurse-patient clinical interactions cannot be overemphasized, as “research has shown that communication processes are essential to more accurate patient reporting and disclosure” [ 12 ]. Respectful communication between nurses and patients can reduce uncertainty, enhance greater patient engagement in decision making, improve patient adherence to medication and treatment plans, increase social support, safety, and patient satisfaction in care [ 12 , 13 ]. Thus, effective nurse-patient clinical communication is essential to enhancing patient-centered care and positive care outcomes.
Patient-centered communication, also known as person-centered communication or client-centered communication, is defined as a process that invites and encourages patients and their families to actively participate and negotiate in decision-making about their care needs, as cited in [ 7 ]. Patient-centered communication is crucial in promoting patient-centered care and requires that patients and their caregivers engage in the care process. As McLean [ 14 ] observed, patient-centered care can be enhanced through patient-centered communication by valuing patients’ dignity and rights. Through open communication and collaboration, where information and care plans are shared among care providers, patients, and their families, care provision becomes patient-centered [ 14 ].
Given the interconnected nature of patient-centered care and communication, we must identify the barriers and enablers of patient-centered care and communication and proposed efficient ways to enhance that because patient-centered communication is essential in achieving patient-centered care. Our aim in this paper is to identify the barriers and facilitators of patient-centered care and communication and propose and present a patient-centered care and communication continuum (PC4) Model to explain how patient-centered care can be enhanced in nurse-patient clinical interactions. As Grant and Booth argued, critical reviews are often used to present, analyse, and synthesized research evidence from diverse sources, the outcome of which is a hypothesis or a model as an interpretation of existing data to enhance evidence-based practice [ 15 ]. Thus, this critical literature review study explores the questions: what are the barriers and facilitators of patient-centered care and how can patient-centered care be enhanced through effective clinical communication?
An earlier version of this study was submitted as part of author AK’s doctoral comprehensive exams in February 2021. An interdisciplinary doctoral committee recommended many of the included literature and the questions explored in this study based on the current discourse of patient-centered care advocated for in many healthcare facilities and in recognition of the universal healthcare access objective of the health sustainable development goal. Additional searches for literature were conducted between September and November 2020 using keywords such as barriers and facilitators of nurse-patient interaction, patient-centered care, patient-centered communication , and nurse-patient communication . Databases searched included CINAHL, PubMed, Medline, and Google Scholar. Included studies in this critical review were empirical research on nurse-patient interactions in different care settings published in English and open access. All relevant articles were read, and their main findings relevant to our review questions were identified and organized into themes and subthemes discussed in this paper. Other published studies were read, and together with those that addressed the review question, a model was developed regarding how to enhance patient-centered care through effective communication.
Barriers to Patient-Centered Care and Communication
Nurses constitute a significant workforce of care providers whose practices can severely impact care outcomes (both positive and negative). Nurses spend much time with patients and their caregivers. As a result, positive nurse-patient and caregiver relationships are therapeutic and constitute a core component of care [ 9 , 13 ]. In many instances, nurses serve as translators or patients’ advocates, in addition to performing their primary care duties. Although good nurse-patient relationships positively impact nurse-patient communication and interaction, studies have shown that several factors impede these relationships with significant consequences on care outcomes and quality [ 6 , 16 , 17 ]. Thus, these barriers limit nurses’ and other care providers’ efforts to provide healthcare that meets patients’ and caregivers’ needs. We categorize the barriers to patient-centered care and communication into four kinds: institutional and healthcare system-related, communication-related, environment-related, and personal and behaviour-related barriers. Although these barriers are discussed in separate subheadings, they are interlinked in complex ways during clinical practice.
Institutional and Healthcare System Related Barriers
Many barriers to providing patient-centered care and communication during nurse-patient interactions emanate from healthcare institutional practices or the healthcare system itself. Some of these factors are implicated in healthcare policy or through management styles and strategies.
Shortage of nursing staff, high workload, burnout, and limited-time constituted one complex institutional and healthcare system-level barrier to effective care delivery [ 18 , 19 ]. For instance, Loghmani et al. [ 20 ] found that staffing shortages prevented nurses from having adequate time with patients and their caregivers in an Iranian intensive care unit. Limitations in nursing staff, coupled with a high workload, led to fewer interactions between nurses, patients, and caregivers. Similarly, Anoosheh et al. [ 16 ] found that heavy nursing workload was ranked highest as a limiting factor to therapeutic communication in nurse-patient interactions in Iran.
In a study on communication barriers in two hospitals affiliated with Alborz University of Medical Sciences, Norouzinia et al. [ 21 ] found that shortage of nurses, work overload, and insufficient time to interact with patients were significant barriers to effective nurse-patient interactions. Similar factors are identified as barriers to nurse-patient communication and interactions in other studies [ 13 , 16 , 18 ]. For instance, Amoah et al. [ 16 ] reported that nursing staff shortage and high workload were barriers to patient-centered care and therapeutic communication among Ghanaian nurses and patients. Amoah and colleagues reported a patient’s statement that:
[B]ecause there are few nurses at the ward, sometimes you would want a nurse to attend to you, but he or she might be working on another patient, so in such case, the nurse cannot divide him or herself into two to attend to you both [ 16 ].
Nurses and patients and their caregivers have noted that limited time affects nurse-patient interactions, communication, and care quality. Besides, Yoo et al. [ 22 ] reported that limited visiting hours affected communications between caregivers and nurses in a tertiary hospital in Seoul, Korea. Since the caregivers had limited time to spend with patients, they had little knowledge about the intensive care unit and distrusted the nurses.
Although nursing staff shortage is a significant barrier to patient-centered care and communication that healthcare institutions and managers must know, some healthcare scholars have critique nurses’ complaints of time limitation. For instance, McCabe [ 7 ] argued that the quality of nurse-patient interactions is what matters and not the quantity of time spent with patients and their caregivers. McCabe maintained that “spending long periods with patients does not always result in positive nurse-patient relationships” [ 7 ]. He argued that implementing patient-centered care does not require additional time; hence, nurses’ perceptions of being too busy cannot excuse poor therapeutic communication during clinical interactions. Instead, nurses are encouraged to develop self-awareness, self-reflection, and a commitment to ensuring that patients receive the needed care.
Another institution-related barrier to patient-centered care and communication is the healthcare system’s emphasis on task-centered care. Care providers are more focused on completing care procedures than satisfying patients’ and caregivers’ needs and preferences. This barrier to patient-centered care and communication is acknowledged in several studies [ 7 , 14 , 20 , 22 , 23 ]. For example, McLean [ 14 ] studied dementia care in nursing homes in the United States. She found that patient-centered care and communication in one nursing home (Snow I) were severely affected when nurses, physicians, and care managers focused on completing tasks or observing care and institutional routines to the detriment of satisfying patients’ care needs. However, in the other care home (Snow II), patient-centered care was enhanced as nurses, physicians, and the care home managers focused on addressing patients’ needs and values rather than completing care routines and tasks.
Similarly, Yoo and colleagues [ 22 ] observed that nurse-patient communication was affected when the ICU nurses placed urgency on completing tasks linked directly to patients’ health (e.g., stabilizing vital signs) than communicating to addressed patients’ specific needs. This evidence shows that when nurses are more task-focused, patients and caregivers are treated as bodies and objects, on which medical and care practices must be performed to restore health. Research has shown that when nurses focus on task-oriented care, it becomes hard to provide holistic care to patients or teach and communicate with patients even when nurses are less busy [ 20 ].
Nursing managers and their management styles can affect patient-centered care and communication. Studies have revealed that the management styles that nursing managers implement can either facilitate or impede patient-centered care [ 14 , 22 ]. When nurse managers orient their nursing staff towards task-centered care practices, it affects nurse-patient interaction and communication. Moreover, when nurse managers fail to address their staff’s mental health needs and personal challenges, it influences how nurses attend to patients’ care needs. For example, nurses have indicated that nurse-patient communication is affected when nurse managers are unsupportive or unresponsive to their needs [ 20 ].
In a study exploring nursing and midwifery managers’ perspectives on obstacles to compassion giving and therapeutic care across 17 countries, Papadopoulos et al. [ 24 ] discovered that nurses and midwifery managers’ characteristics and experiences could facilitate or impede compassion and therapeutic interactions in nursing care. Negative personal attitudes, including selfishness, arrogance, self-centeredness, rudeness, lack of leadership skills, the desire for power, and feelings of superiority among nurses and midwifery managers, were obstacles to compassion building. The study further showed that managers who emphasize rules, tasks, and results do not prioritize relationship-building and see their staff as workers rather than team members [ 24 ]. Therefore, nurse managers and care administrators must monitor nurse-patient interaction and communication to address nurses’ concerns and support them, especially in resource-constrained and high patient turnover contexts [ 25 , 26 ].
Communication-Related Barriers
Effective communication is essential to providing patient-centered care. Studies have shown that poor communication between care providers and patients and their caregivers affects care outcomes and perceptions of care quality [ 7 , 16 , 27 , 28 ]. A consistent communication-related barrier in nurse-patient interaction is miscommunication, which often leads to misunderstandings between nurses, patients, and their families [ 20 ]. Other communication-related barriers include language differences between patients and healthcare providers [ 6 , 16 , 27 ], poor communication skills, and patients’ inability to communicate due to their health state, especially in ICU, dementia, or end-of-life care contexts [ 13 , 22 ]. For instance, in their maternity care study, Madula et al. [ 6 ] noted that language barriers significantly affected effective communication between nurses/midwives and expectant mothers. A patient in their study indicated that although many nurses were polite and communicated well, some nurses had challenges communicating with patients in the Chitumbuka language, which affected those nurses’ ability to interact effectively with patients [ 6 ].
Furthermore, Norouzinia et al. [ 21 ] asserted that effective communication could not be established when nurses and patients have a language difference. Moreover, the meanings of certain non-verbal communication acts (e.g., head nodding, eye gaze, touch) can invoke different interpretations across different cultures, which could impede the interactions between patients and nurses. Even in healthcare contexts where nurses and patients speak the same language, “differences in vocabulary, rate of speaking, age, background, familiarity with medical technology, education, physical capability, and experience can create a huge cultural and communication chasm” between nurses and patients [ 12 ]. In ICU and other similar care settings, nurses find it difficult to effectively communicate with patients because the mechanical ventilators made it hard for patients to talk [ 22 ].
To overcome the communication-related barriers, healthcare institutions must make it a responsibility to engage translators and interpreters to facilitate nurse-patient interactions where a language barrier exists. Moreover, nurses working in ICU and other similar settings should learn and employ alternative forms of communication to interact with patients.
Environment-Related Barriers
The environment of the care setting can impact nurse-patient communication and the resulting care. Thus, “good health care experiences start with a welcoming environment” [ 29 ]. Mastors believed that even though good medicine and the hands working to provide care and healing to the sick and wounded are essential, we must not “forget the small things: a warm smile, an ice chip, a warm blanket, a cool washcloth. A pillow flipped to the other side and a boost in bed” [ 29 ]. The environment-related barriers are obstacles within the care setting that inhibit nurse-patient interaction and communication and may include a noisy surrounding, unkept wards, and beds, difficulties in locating places, and navigating care services. Noisy surroundings, lack of privacy, improper ventilation, heating, cooling, and lighting in specific healthcare units can affect nurse-patient communication. These can prevent patients from genuinely expressing their healthcare needs to nurses, which can subsequently affect patient disclosure or make nursing diagnoses less accurate [ 13 , 18 , 21 ]. For instance, Amoah et al. [ 16 ] revealed that an unconducive care environment, including noisy surroundings and poor ward conditions, affected patients’ psychological states, impeding nurse-patient relationships and communication. Moreover, when care services are not well-coordinated, new patients and their caregivers find it hard to navigate the care system (e.g., locating offices for medical tests and consultations), which can constrain patient-centered care and communication.
Reducing the environment-related barriers will require making the care setting tidy/clean, less noisy, and coordinating care services in ways that make it easy for patients and caregivers to access. Coordinating and integrating care services, making care services accessible, and promoting physical comfort are crucial in promoting patient-centered care, according to Picker’s Eight Principles of Patient-Centered Care [ 30 ].
Personal and Behaviour Related Barriers
The kind of nurse-patient relationships established between nurses and patients and their caregivers will affect how they communicate. Since nurses and patients may have different demographic characteristics, cultural and linguistic backgrounds, beliefs, and worldviews about health and illnesses, nurses’, patients’, and caregivers’ attitudes can affect nurse-patient communication and care outcomes. For instance, differences in nurses’ and patients’ cultural backgrounds and belief systems have been identified as barriers to therapeutic communication and care [ 12 , 13 , 21 ]. Research shows that patients’ beliefs and cultural backgrounds affected their communication with nurses in Ghana [ 16 ]. These scholars found that some patients refused a blood transfusion, and Muslim patients refused female nurses to attend to them because of their religious beliefs [ 16 ]. Further, when nurses, patients, or their caregivers have misconceptions about one another due to past experiences, dissatisfaction about the care provided, or patients’ relatives and caregivers unduly interfere in the care process, nurse-patient communication and patient-centered care were affected [ 16 , 21 ].
Similarly, nurse-patient communication was affected when patients or caregivers failed to observe nurses’ recommendations or abuse nurses due to misunderstanding [ 20 ], while patients’ bad attitudes or disrespectful behaviours towards nurses can inhibit nurses’ ability to provide person-centered care [ 31 ]. The above-reviewed studies provided evidence on how patients’ and caregivers’ behaviours can affect nurses’ ability to communicate and deliver patient-centered care.
On the other hand, nurses’ behaviours can also profoundly affect communication and care outcomes in the nurse-patient dyad. When nurses disrespect, verbally abuse (e.g., shouting at or scolding), and discriminate against patients based on their social status, it affects nurse-patient communication, care outcomes, and patient disclosure [ 6 , 32 ]. For instance, Al-Kalaldeh et al. [ 18 ] believe that nurse-patient communication is challenged when nurses become reluctant to hear patients’ feelings and expressions of anxiety. When nurses ignore patients’ rights to share ideas and participate in their care planning, such denials may induce stress, discomfort, lack of trust in nurses, thereby leading to less satisfaction of care [ 18 ].
Furthermore, when nurses fail to listen to patients’ and caregivers’ concerns, coerce patients to obey their rules and instructions [ 16 , 17 , 20 ], or fail to provide patients with the needed information, nurse-patient communication and patient-centered care practices suffer. To illustrate, in Ddumba-Nyanzia et al.‘s study on communication between HIV care providers and patients, a patient remarked that: “I realized no matter how much I talked to the counselor, she was not listening. She was only hearing her point of view and nothing else, [and] I was very upset” [ 17 ]. This quote indicates how care provider attitudes can constrain care outcomes. Due to high workload, limited time, poor remunerations, and shortage of personnel, some nurses can develop feelings of despair, emotional detachment, and apathy towards their job, which can lead to low self-esteem or poor self-image, with negative consequences on nurse-patient interactions [ 13 , 18 ].
Given the significance of effective communication on care, overcoming the above personal and behaviour related barriers to patient-centered care and communication is crucial. Nurses, patients, and caregivers need to reflect on the consequences of their behaviours on the care process. Thus, overcoming these barriers begins with embracing the facilitators of patient-centered care and communication, which we turn to in the next section.
Facilitators of patient-centered care and communication
Patient-centered care and communication can be facilitated in several ways, including building solid nurse-patient relationships.
First, an essential facilitator of patient-centered care and communication is overcoming practical communication barriers in the nurse-patient dyad. Given the importance of communication in healthcare delivery, nurses, patients, caregivers, nursing managers, and healthcare administrators need to ensure that effective therapeutic communication is realized in the care process and becomes part of the care itself. Studies have shown that active listening among care providers is essential to addressing many barriers to patient-centered care and communication [ 7 , 13 ]. Although handling medical tasks promptly in the care process is crucial, the power of active listening is critical, meaningful, and therapeutic [ 22 ]. By listening to patients’ concerns, nurses can identify patients’ care needs and preferences and address their fears and frustrations.
Another facilitator of patient-centered care is by understanding patients and their unique needs [ 25 ], showing empathy and attending attitudes [ 7 , 13 ], expressing warmth and respect [ 22 ], and treating patients and caregivers with dignity and compassion as humans. For instance, McCabe [ 7 ] noted that attending, which obligates nurses to demonstrate that they are accessible and ready to listen to patients, is a patient-centered care process; a fundamental requirement for nurses to show genuineness and empathy, despite the high workload. Showing empathy, active listening, respect, and treating patients with dignity are core to nursing and care, and recognized in the Code of Ethics for Nurses [ 33 ], and further emphasized in the ongoing revision of the Code of Ethics for nurses [ 34 ].
Besides, engaging patients and caregivers in the care process through sharing information, inviting their opinion, and collaborating with them constitutes another facilitator of patient-centered care and communication. When patients and caregivers are engaged in the care process, misunderstandings and misconceptions are minimized. When information is shared, patients and caregivers learn more about their health conditions and the care needed. As McLean [ 14 ] argued, ensuring open communication between care providers and patients and their families is essential to enhancing patient-centered care. Conflicts ensue when patients or their families are denied information or involvement in the care process. As a result, the Harvard Medical School [ 30 ] identified patient engagement, information sharing, and nurse-patient collaboration during care as essential patient-centered care principles.
Finally, health policy must be oriented towards healthcare practices and management to facilitate patient-centered care and communication. These policies, at a minimum, can involve changes in management styles within healthcare institutions, where nurse managers and healthcare administrators reflect on nursing and care practices to ensure that the Code of Ethics of Nurses and patients’ rights are fully implemented. Resource constraints, staff shortages, and ethical dilemmas mainly affect care practices and decision-making. Nonetheless, if patients are placed at the center of care and treated with dignity and respect, most of the challenges and barriers of patient-centered care will diminish. Empowering practicing nurses, equipping them with interpersonal communication skills through regular in-service training, supporting them to overcome their emotional challenges, and setting boundaries during nurse-patient interactions will enhance patient-centered care practices.
In line with the above discussion, Camara et al. [ 25 ] identify three core dimensions that nurses, patients, and caregivers must observe to enhance patient-centered care: treating the patient as a person and seeing the care provider as a person and a confidant. Regarding the first dimension, care providers must welcome patients, listen to them, share information with them, seek their consent, and show them respect when providing care. The second dimension requires that the healthcare provider be seen and respected as a person, and negative perceptions about care providers must be demystified. According to Camara et al. [ 25 ], care providers must not overemphasize their identities as experts but rather establish good relationships with patients to understand patients’ personal needs and problems. Lastly, patients and caregivers must regard care providers as confidants who build and maintain patients’ trust and encourage patients’ participation in care conversations. With this dimension, patients and caregivers must know that nurses and other care providers have the patient at heart and work to meet their care needs and recovery process.
Camara et al.‘s [ 25 ] three dimensions are essential and position patients, their caregivers, and nurses as partners who must engage in dialogic communication to promote patient-centered care. As a result, effective communication, education, and increased health literacy among patients and caregivers will be crucial in that direction.
Enhancing Patient-Centered Care and Communication: A Proposed Model
Nursing care practices that promote patient-centered communication will directly enhance patient-centered care, as patients and their caregivers will actively engage in the care process. To enhance patient-centered communication, we propose person-centered care and communication continuum (PC4) as a guiding model to understand patient-centered communication, its pathways, and what communication and care practices healthcare professionals must implement to achieve person-centered care. In this PC4 Model, we emphasize the person instead of the patient because they are a person before becoming a patient. Moreover, the PC4 Model is supposed to apply to all persons associated with patient care; thus, respect for the dignity of their personhood is crucial.
Although much is written about patient-centered communication in the healthcare literature, there is a gap regarding its trajectory and what communication content enhances patient-centered communication. Also, little is known about how different clinical discourse spaces influence communication and its content during nurse-patient clinical interactions. Using evidence from Johnsson et al. [ 3 ], Murira et al. [ 23 ], and Liu et al. [ 35 ], among other studies, we outline the components of the PC4 Model and how different discourse spaces in the clinical setting and the content of communication impact patient-centered care and communication.
The proposed PC4 Model in this paper has three unbounded components based on the purpose of and how communication is performed among care providers, patients, and their caregivers. Figure 1 illustrates the PC4 Model, its features, and trajectory.
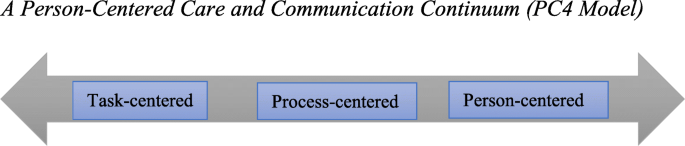
A Person-Centered Care and Communication Continuum (PC4 Model)
Task-Centered Communication
At the lowest end of the PC4 Model is task-centered communication. Here, the care provider’s role is to complete medical tasks as fast as possible with little or no communication with the patient and their caregivers. Patients and caregivers are treated as bodies or objects whose disease symptoms need to be studied, identified, recorded, treated, or cured. As Johnsson et al. [ 3 ] observed, communication content at this stage is mainly biomedically oriented, where nurses and other healthcare professionals focus on the precise medical information (e.g., history taking, medical examination, test results, medication, etc.) about the patient. With a task-centered orientation, nurses make journal entries about their patients’ disease state and ensure that treatment plans, diagnostic tests, and medical prescriptions are completed. Communication at this stage is often impersonal or rigid (see [ 23 ] for details). Care providers may address patients and their caregivers by using informal attributes (e.g., bed 12, the woman in the red shirt, card 8, etc.), thereby ignoring patients’ and caregivers’ personal and unique identities. Patients’ and caregivers’ nonverbal communication signs are mostly overlooked.
Motivations for task-centered communication can be attributed to time limitation, high workload, and staff shortage, thereby pushing nurses and other care providers to reach as many patients as possible. Moreover, the healthcare system’s orientation towards and preference for biomedically-focused care seems to favour task-centered communication [ 7 , 14 ].
Depending on the clinical discourse space under which patient-provider interactions occur, different forms of communication are employed. Clinical discourse spaces can be public (e.g., in the ward, patient bedside), private (e.g., consulting rooms, medical test labs, nurse staff station, etc.), or semi-private (e.g., along the corridor) [ 35 ]. In these clinical discourse spaces, nurse-patient communication can be uninformed (patients or caregivers are not informed about patients’ care conditions or why specific data and routines are performed). It can be non-private (others can hear what the nurse and patient are talking about) or authoritative (care providers demonstrate power and control and position themselves as experts) [ 23 ]. Finally, in task-centered communication, healthcare providers often use medical jargon or terminologies [ 3 ] since the goal of communication is not to engage the patient in the process. Usually, patients or their caregivers are not allowed to ask questions, or their questions get ignored or receive superficial, incomprehensible responses.
Process-Centered Communication
Process-centered communication is an intermediate stage on the continuum, which could slip back into the task-centered or leap forward into person-centered communication. Through process-centered communication, care providers make an effort to know patients and their caregivers as they perform care routines. Care providers ask patients or their caregivers questions to understand the care conditions but may not encourage patients or caregivers to express their thoughts about their care needs. Patients and caregivers are recognized as persons with uniques care needs but may not have the agency to influence the care process. Care providers may chit-chat with patients or their caregivers to pass the time as they record patients’ medical records or provide care. Unlike task-centered communication, there is informative and less authoritative communication between nurses and patients and their caregivers. The goal of process-centered communication could be a mixture of instrumental and relational, with less display of power and control by nurses.
Person-Centered Communication
This is the highest point of the PC4 Model, where patient-centered care is actualized. At this stage of the communication continuum, patients and caregivers are treated as unique persons with specific care needs and are seen as collaborators in the care process. As McLean [ 14 ] observed, caregiving becomes a transactional relationship between the care provider and receiver at the person-centered stage of the continuum. The care itself becomes intersubjective, a mutual relational practice, and an ongoing negotiation for care providers and receivers [ 14 ].
The content of communication at this stage of the continuum is both “personal” and “explanatory” [ 3 ]. Nurses and other healthcare providers create meaningful relationships with patients and their caregivers, understand patients’ concerns, needs, and problems, use open-ended questions to encourage patients or caregivers to express their thoughts and feelings about the care situation. Nurses and other healthcare professionals explain care routines, patients’ health conditions, and management plans in lay language to patients and caregivers through person-centered communication. Accomplishing this level includes employing alternative forms of communication to meet the needs of intensive care unit patients, deaf patients, and ventilated and intubated patients. For instance, it has been shown that “deaf people […] frequently do not have access to clear and efficient communication in the healthcare system, which deprives them of critical health information and qualified health care” [ 36 ]. Empathetic communication practices, including active listening, showing genuine interest in patients’ care, and respect and warmth, become a significant part of nursing care [ 3 , 7 , 14 , 22 ].
Different communication strategies are employed based on the care situation and context. Chit-chatting, as a form of personal communication [ 3 ], use of humor as a communication strategy [ 7 , 8 ], and even maintaining silence [ 28 ] are essential in enhancing person-centered care and communication. Both care providers and patients or their caregivers use relationship-building and -protecting humor (see [ 28 ] for details) to address difficult situations in the care process.
Implications of the PC4 Model for Nursing Practice
Given the values of effective communication in nurse-patient interactions and care outcomes, nurses and other healthcare providers must ensure that they develop therapeutic relationships with patients, their families, and caregivers to promote person-centered care and communication. Achieving that begins with knowing and reflecting on the barriers of therapeutic communication and ways to minimize them. The PC4 Model draws nurses and all healthcare providers’ attention to patient-centered care pathways and how effective communication is necessary. Healthcare professionals, including nurses, must be aware of how their communication orientation–––either oriented toward completing tasks, following care processes or toward addressing patients’ and their caregivers’ needs––can impact patient-centered care. Healthcare providers must observe the care context, patients’ unique situations, their non-verbal language and action, and whether they belong to historically marginalized groups or cultures.
Mastors [ 29 ] has offered healthcare providers some guidance to reflect on as they communicate and interact with patients and caregivers. Thus, (a) instead of asking patients, “What’s the matter?“ care providers must consider asking them, “What’s important to you?“ With this question, the patient is given a voice and empowered to contribute to their own care needs. Care providers should (b) check with patients in the waiting room to update patients whose waiting time has been longer than usual, based on the care context. They should also (c) try to remember their conversations with patients to build on them during subsequent interactions. This continuity can be enhanced by nurse managers reexamining how they deploy care providers to patients. The same nurse can be assigned to the same patients for the duration of the patient’s stay to help patients feel valued and visible [ 29 ].
Knowledge of cultural competence, sensitivity, humility, and interpersonal communication skills will help achieve and implement the PC4 Model. As Cuellar [ 37 ] argues, “[h]umility is about understanding and caring for all people [and] being empathetic.“ Cultural competence is a “dynamic process of acquiring the ability to provide effective, safe, and quality care to the patients through considering their different cultural aspects” [ 38 ]. The concept of cultural competence entails “cultural openness, awareness, desire, knowledge and sensitivity” during care [ 39 ]. It demands that care providers respect and tailor care to align with patients’ and caregivers’ values, needs, practices, and expectations, based on care and moral ethics and understanding [ 39 ]. Active listening and showing compassion as therapeutic relationship-building skills are essential, and continuous education and mentorship will be crucial to developing these skills among healthcare providers.
We invite qualitative and quantitative studies, especially on language use and communication strategies, to explore and evaluate the PC4 Model. Providing in-depth and experiential data on ways to increase its effectiveness as a tool to guide healthcare providers is highly desired. More knowledge can support healthcare providers in offering evidence-based patient-centered care in different healthcare settings and units.
Conclusions
Effective communication is an essential factor in nurse-patient interactions and a core component of nursing care. When communication in the nurse-patient dyad is patient-centered, it becomes therapeutic. It allows for trust and mutual respect in the care process, thereby promoting care practices that address patients’ and caregivers’ needs, concerns, and preferences. We have identified the barriers and facilitators of patient-centered care and communication and proposed a person-centered care and communication continuum (PC4 Model) to demonstrate how patient-centered communication intersects with patient-centered care.
Availability of data and materials
Not applicable.
Abbreviations
Intensive Care Unit
Institution of Medicine
Person-Centered Care and Communication Continuum
Etheredge HR. “Hey sister! Where’s my kidney?“ Exploring ethics and communication in organ transplantation in Gauteng, South Africa, Ph.D. dissertation, Johannesburg. University of the Witwatersrand; 2015.
Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. National Academy Press; 2001.
Johnsson A, Wagman P, Boman A, Pennbrant S. What are they talking about? Content of the communication exchanges between nurses, patients and relatives in a department of medicine for older people: An ethnographic study. J Clin Nurs. 2018 Apr;27(7–9):e1651-9. doi: https://doi.org/10.1111/jocn.14315 .
Long KA. The Institute of Medicine report on health professions education: A bridge to quality. Policy Polit Nurs Pract. 2003 Nov;4(4):259–62. doi: https://doi.org/10.1177/1527154403258304 .
Crawford T, Candlin S, Roger P. (2017). New perspectives on understanding cultural diversity in nurse-patient communication. Collegian, 2017 Feb 1;24(1):63 – 9. https://doi.org/10.1016/j.colegn.2015.09.001 .
Madula P, Kalembo WF, Yu H, Kaminga CA. Healthcare provider-patient communication: A qualitative study of women’s perceptions during childbirth. Reprod Health. 2018 Dec;15(135):1–10. https://doi.org/10.1186/s12978-018-0580-x .
McCabe C. Nurse-patient communication: An exploration of patients’ experiences. J Clin Nurs. 2004 Jan;13(1):41–9.
Schöpf AC, Martin GS, Keating MA. Humor as a communication strategy in provider-patient communication in a chronic care setting. Qual Health Res. 2017 Feb;27(3):374–90. doi: https://doi.org/10.1177/1049732315620773 .
Joolaee S, Joolaei A, Tschudin V, Bahrani N, Nikbakht NA. Caring relationship: the core component of patients’ rights practice as experienced by patients and their companions. J Med Ethics Hist Med. 2010;3(4):1–7.
Google Scholar
Boykins AD. Core communication competences in patient-centered care. The ABNF J. 2014 Apr 1;25(2):40 – 5.
Henly SJ. Health communication research for nursing science and practice. Nurs Res [Editorial] 2016:257–8. doi: https://doi.org/10.1097/NNR.0000000000000171 .
Ruben BD. Communication theory and health communication practice: The more things change, the more they stay the same. Health Commun. 2016 Jan 2;31(1):1–11. doi: https://doi.org/10.1080/10410236.2014.923086 .
Bello P. Effective communication in nursing practice: A literature review. BSc Nursing Thesis. Arcada; 2017. Available at https://core.ac.uk/download/pdf/84798372.pdf Accessed 20 Jan 2021.
McLean A. The person in dementia: A study of nursing home care in the US. Toronto, University of Toronto Press; 2007.
Grant MJ, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info Libraries J. 2009;26:91–108. Doi: https://doi.org/10.1111/j.1471-1842.2009.00848.x .
Article Google Scholar
Amoah KMV, Anokye R, Boakye SD, Acheampong E, Budu-Ainooson A, Okyere E, Kumi-Boateng G, Yeboah C, Afriyie OJ. A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nurs. 2019 Dec;18(4)1–8. https://doi.org/10.1186/s12912-019-0328-0 .
Ddumba-Nyanzia I, Kaawa-Mafigiria D, Johannessen H. Barriers to communication between HIV care providers (HCPs) and women living with HIV about childbearing: A qualitative study. Patient Educ Couns. 2016 May 1:99(5):754–9. https://doi.org/10.1016/j.pec.2015.11.023 .
Al-Kalaldeh M, Amro N, Qtait M. Barriers to effective nurse-patient communication in the emergency department. Emerg Nurse. 2021 Mar 2;29(2). doi: https://doi.org/10.7748/en.2020.e1969 .
Sethi D, Rani MK. Communication barrier in health care setting as perceived by nurses and patient. Int J Nurs Educ 2017 Oct. 2016;9(4):30. doi: https://doi.org/10.5958/j.2320-8651.2.1.001 .
Loghmani L, Borhani F, Abbaszadeh A. Factors affecting the nurse-patients’ family communication in intensive care unit of Kerman: A qualitative study. J Caring Sci. 2014 Mar;3(1):67–2. doi: https://doi.org/10.5681/jcs.2014.008 .
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci. 2016 Jun;8(6):65–4. https://doi.org/10.5539/gjhs.v8n6p65 .
Yoo HJ, Lim OB, Shim JL. Critical care nurses’ communication experiences with patients and families in an intensive care unit: A qualitative study. PLoS One. 2020 Jul 9;15(7):e0235694. https://doi.org/10.1371/journal.pone.0235694 .
Murira N, Lützen K, Lindmark G, Christensson K. Communication patterns between healthcare providers and their clients at an antenatal clinic in Zimbabwe. Health Care Women Int. 2003 Feb 1;24(2):83 – 2. https://doi.org/10.1080/07399330390170060 .
Papadopoulos I, Lazzarino R, Koulouglioti C, Aagard M, Akman O, Alpers L-M, Apostolara P, Araneda Bernal J, Biglete-Pangilinan S, Eldar-Regev O, Gonzalez-Gil MT, Kouta C, Zorba A. Obstacles to compassion-giving among nursing and midwifery managers: An international study. Int Nurs Rev. 2020 Aug;11:1–13.
Camara BS, Belaid L, Manet H, Kolie D, Guilard E, Bigirimana T, Delamou A. What do we know about patient-provider interactions in sub-Saharan Africa? A scoping review. Pan Afr Med J. 2020;88(88):1–13. doi: https://doi.org/10.11604/pamj.2020.37.88.24009 .
Kwame A, Petrucka PM. Communication in nurse-patient interaction in healthcare settings in sub-Saharan Africa: A scoping review. Int J Afr Nurs Sci. 2020 Jan 1;12:100198. https://doi.org/10.1016/j.ijans.2020.100198 .
Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. Int Nurs Rev. 2009 Jun;56(2):243–9.
Vuković M, Gvozdenović BS, Stamatović-Gajić B, Ilić M, Gajić T. Development and evaluation of the nurse quality of communication with patient questionnaire. Srp Arh Celok Lek. 2010;138(1–2):79–4. doi: https://doi.org/10.2298/SARH1002079V .
Article PubMed Google Scholar
Mastors P. (2018). What do patients want, need, and have the right to expect? Nurs Adm Q. 2018 Jul 1;42(3):192-8. doi: https://doi.org/10.1097/NAQ.0000000000000297 .
Harvard Medical School. The Eight Principles of Patient Centered Care; 2015 Nov 18. Available from OneView: https://www.oneviewhealthcare.com/the-eight-principles-of-patient-centered-care/ Accessed 28 Dec 2020.
White J, Phakoe M, Rispel LC. ‘Practice what you preach’: Nurses’ perspectives on the Code of Ethics and Service Pledge in five South African hospitals. Glob Health Action. 2015 Dec 1;8(1):26341. https://doi.org/10.3402/gha.v8.26341 .
Kruger L-M, Schoombee C. The other side of caring: abuse in a South African maternity ward. J Reprod Infant Psychol. 2010 Feb 1;28(1):84–101. doi: https://doi.org/10.1080/02646830903294979 .
International Council of Nurses. ICN Code of Ethics for Nurses; 2012. Available from www.icn.ch/images/stories/documents/about/icncode_english.pdf . Accessed 20 Dec 2020.
Stievano A, Tschudin V. The ICN code of ethics for nurses: A time for revision. Nurs Health Policy Perspect. 2019 Jun;66(2):154–6.
Liu W, Manias E, Gerdtz M. Medication communication during ward rounds on medical wards: Power relations and spatial practices. Health 2012 Mar. 2012;17(2):113–34. doi: https://doi.org/10.1177/1363459312447257 .
Hoglind TA. Healthcare language barriers affect deaf people, too. 2018 Oct 11. Retrieved from Boston University [BU] School of Public Health: Available from https://www.bu.edu/sph/news/articles/2018/healthcare-language-barriers-affect-deaf-people-too/ Accessed 15 Jan 2021.
Cuellar NG. Humility. A concept in cultural sensitivity. JTranscult Nurs [Editorial]. 2018 Apr 26; 29(4):317. https://doi.org/10.1177/1043659618772384 .
Sharifi N, Adib-Hajbaghery M, Najafi M. Cultural competence in nursing: A concept analysis. Int J Nurs Stud. 2019 Nov 1;99(103386):1–8. https://doi.org/10.1016/j.ijnurstu.2019.103386 .
Henderson S, Horne M, Hills R, Kendall E. Cultural competence in healthcare in the community: A concept analysis. Health Soc Care Community. 2018 Jul;26(4):590–603. doi: https://doi.org/10.1111/hsc.12556 .
Download references
Acknowledgments
We express our gratitude to the first author’s doctoral committee members for their valuable comments, suggestions, and critique of an earlier version of this paper. We are also grateful to the anonymous reviewers for the insightful comments and suggestions that have helped us improve the study’s quality.
Authors' information
Abukari Kwame is a Ph.D. candidate in Interdisciplinary Studies in the College of Graduate and Postdoctoral Studies, University of Saskatchewan, interested in patients' rights in nurse-patient clinical communications and interactions in the hospital setting. He holds two Master of Philosophy degrees in Indigenous Studies and English Linguistics. Abukari's research interests include language use in social interaction, health communication, First/Second language acquisition, African traditional medical knowledge, and Indigenous and qualitative research methodologies.
Pammla M. Petrucka is a professor in Nursing and has international research experience with many of her graduate students from Africa, Asia, and the Caribbean. Pammla has published extensively in the field of nursing. Her research interests are vast, including child and maternal health, Indigenous peoples' health, global health, and vulnerable populations, with extensive experiences in qualitative research and indigenous research methodologies. Pammla is co-editor of the BMC Nursing journal and a reviewer for many other academic journals.
The authors have not received any funding for the conduct, preparation, and publication of this paper.
Author information
Authors and affiliations.
College of Graduate and Postdoctoral Studies, University of Saskatchewan, Saskatoon, Canada
Abukari Kwame
College of Nursing, University of Saskatchewan, Regina Campus, Regina, Canada
Pammla M. Petrucka
You can also search for this author in PubMed Google Scholar
Contributions
Both authors conceived the topic. PMP recommended the literature, AK searched and added more sources, and drafted the paper. PMP reviewed the paper for intellectual content. Both AK and PMP read and approved the final version.
Corresponding author
Correspondence to Abukari Kwame .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kwame, A., Petrucka, P.M. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs 20 , 158 (2021). https://doi.org/10.1186/s12912-021-00684-2
Download citation
Received : 05 May 2021
Accepted : 18 August 2021
Published : 03 September 2021
DOI : https://doi.org/10.1186/s12912-021-00684-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient-centered care
- Therapeutic communication
- Nurse-patient interactions
- Clinical discourse space
- Patient-centered care and communication continuum
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Supplements
- BMJ Journals
You are here
- Volume 5, Issue 12
- The empirical evidence underpinning the concept and practice of person-centred care for serious illness: a systematic review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-2667-1665 Alessandra Giusti 1 , 2 ,
- http://orcid.org/0000-0002-2991-8160 Kennedy Nkhoma 1 ,
- Ruwayda Petrus 3 ,
- Inge Petersen 3 ,
- Liz Gwyther 4 ,
- Lindsay Farrant 4 ,
- http://orcid.org/0000-0003-3076-0783 Sridhar Venkatapuram 2 ,
- http://orcid.org/0000-0001-9653-8689 Richard Harding 1
- 1 Cicely Saunders Institute of Palliative Care, Policy and Rehabilitation , King's College London , London , UK
- 2 King's Global Health Institute , King's College London , London , UK
- 3 School of Applied Human Sciences , University of KwaZulu-Natal College of Humanities , Durban , South Africa
- 4 School of Public Health and Family Medicine , University of Cape Town Faculty of Health Sciences , Cape Town , Western Cape , South Africa
- Correspondence to Alessandra Giusti; alessandra.giusti{at}kcl.ac.uk
Introduction Person-centred care has become internationally recognised as a critical attribute of high-quality healthcare. However, the concept has been criticised for being poorly theorised and operationalised. Serious illness is especially aligned with the need for person-centredness, usually necessitating involvement of significant others, management of clinical uncertainty, high-quality communication and joint decision-making to deliver care concordant with patient preferences. This review aimed to identify and appraise the empirical evidence underpinning conceptualisations of ‘person-centredness’ for serious illness.
Methods Search strategy conducted in May 2020. Databases: CINAHL, Embase, PubMed, Ovid Global Health, MEDLINE and PsycINFO. Free text search terms related to (1) person-centredness, (2) serious illness and (3) concept/practice. Tabulation, textual description and narrative synthesis were performed, and quality appraisal conducted using QualSyst tools. Santana et al ’s person-centred care model (2018) was used to structure analysis.
Results PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow data: n=12,446 studies screened by title/abstract, n=144 full articles assessed for eligibility, n=18 studies retained. All studies (n=18) are from high-income countries, and are largely of high quality (median score 0.82). The findings suggest that person-centred care encompasses the patient and family being respected, given complete information, involved in decision-making and supported in their physical, psychological, social and existential needs. The studies highlight the importance of involving and supporting family/friends, promoting continuation of normality and self-identity, and structuring service organisation to enable care continuity.
Conclusion Person-centred healthcare must value the social network of patients, promote quality of life and reform structurally to improve patients’ experience interacting with the healthcare system. Staff must be supported to flexibly adapt skills, communication, routines or environments for individual patients. There remains a need for primary data investigating the meaning and practice of PCC in a greater diversity of diagnostic groups and settings, and a need to ground potential components of PCC within broader universal values and ethical theory.
- systematic review
- health services research
- health systems
- health policy
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/bmjgh-2020-003330
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Key questions
What is already known.
Person-centred care has become internationally recognised as a dimension of high-quality healthcare, promoted as a core competency of health workers, a key component of primary care and essential to achieving the Universal Health Coverage goals.
Ongoing conceptual debates are attempting to determine what constitutes ‘person-centredness’ and how this concept can be understood and implemented in a variety of settings.
Serious illness is especially aligned with the need for PCC; the complex clinical scenarios surrounding serious illness usually necessitate the involvement of significant others and depend on high-quality communication and joint decision-making to deliver care concordant with patient preferences, with recognition and management of clinical uncertainty.
What are the new findings?
Included studies largely support the Santana et al model of PCC and suggest that additional domains should be given visibility: family and friend involvement and support; promoting continuation of normality and self-identity; structuring service organisation to enable continuity of care and patient navigation.
The empirical data stresses the importance of patients and families being respected, listened to, understood, given honest, complete and comprehendible information and being engaged in all decisions that affect their daily life, care and treatment. Patients must be supported in their physical, psychological, social and spiritual needs.
All retained studies were conducted in high-income, Western countries.
Empirical studies present invaluable data on the meaning and practice of PCC, however none develop this evidence into a theorised framework for implementation of PCC for serious illnesses.
What do the new findings imply?
Person-centred healthcare must value the social network of each patient, promote quality of life and personal goals not only health status improvement, and implement structural reforms to improve patients’ experience of interacting with the healthcare system.
Health systems must be structured to enable sufficient availability and accessibility of health workers, and support staff to be able and willing to flexibly adapt skills, communication, routines or environments for individual patients.
There is a need for primary data investigating the meaning and practice of PCC in a greater diversity of diagnostic groups and settings, particularly non-Western, low- and middle-income settings.
There is a need to consider the theoretical underpinnings of PCC and to ground potential components within broader universal values and ethical theory.

Introduction
Person-centred care has become internationally recognised as a dimension of high-quality healthcare. 1 The Institute of Medicine describes quality care as that which is: “safe, effective, patient-centred, efficient, timely and equitable”. 2 WHO policy on people‐centred healthcare highlights person‐centredness as a core competency of health workers, a key component of primary care, and essential to achieving the Universal Health Coverage goals. 3–6
A variety of terms have been used to denote person-centred approaches. ‘ Patient -centredness’ was first to gain prominence and aimed to challenge the reductionism of the biomedical model and stress the importance of psychosocial factors. 2 3 Many moved towards use of the term ‘ person -centredness’, suggesting this better articulates the holism of the ‘whole person’ and a broader conception of well-being. 7 8 In recent years, the term ‘ people -centredness’ has also gained prominence, emphasising a focus on “the whole person in their specific familial and community contexts”. 9 Person-centred, patient-centred and people-centred care (PCC) all embody an approach that consciously adopts the perspectives of individuals, families and communities, respects and responds to their needs, values and preferences and sees them as participants in their own healthcare rather than just beneficiaries. 2 10
Conceptual clarity is critical to the design, delivery and replication of successful innovations in care. 11 Despite the global prominence of PCC as a goal of health systems, the approach suffers from a lack of clarity. Ongoing conceptual debates are attempting to determine what constitutes ‘person-centredness’ and how this concept can be understood and applied in a variety of contexts. 7 12–14 While numerous conceptualisations of PCC are presented in existing literature, 8 15–21 most do not appear to offer empirical origins or practical guidance on the implementation of PCC. The WHO Global strategy on people-centred and integrated health services recognises that there is not a single model of PCC to be proposed, but rather that it should be context-specific and that each country should generate its own evidence to enable appropriate, acceptable, feasible practice of PCC. 10 It is currently unclear what evidence is available to model contextually-appropriate and culturally-appropriate PCC.
The need for a person-centred approach is particularly important in the context of serious illness. The complex clinical scenarios surrounding serious illness usually necessitate the involvement of significant others, high-quality communication and joint decision-making to deliver care concordant with patient preferences, with recognition and management of clinical uncertainty. 22–24 As populations age, as infectious disease is better managed, and multimorbidity becomes more prevalent, serious health-related suffering associated with conditions such as cancer, chronic lung disease and dementia is rising fastest in low- and middle-income countries (LMICs). 25 Serious illness is also a context in which delivering PCC can be more complex and may require more dimensions to a greater degree than for non-serious illness. Focussing specifically on serious illness is therefore a means of ‘stress testing’ generalist PCC theory and ensuring it captures ‘what matters’ in all diagnostic cases. A better understanding of PCC in the context of serious illness would have health-system-wide relevance for other less complex clinical scenarios.
This systematic review aims to aggregate and appraise the empirical evidence underpinning the concept and practice of PCC in the context of serious illness. Specifically, the objectives of the review are to answer the following questions:
What is the primary data underpinning conceptualisations and practice-based frameworks of ‘person-centredness’ in the context of serious illness?
What is the quality of this data?
What are the key constructs of PCC according to this data?
This systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations. 26 The review protocol was registered prospectively with PROSPERO: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=139259 (registration number 139259).
Definition of terms
To structure this review, literature was considered in line with two frequently cited definitions of PCC, one policy-led (using the term ‘ people -centredness’) and one patient-led (using the term ‘ patient -centredness’):
“An approach to care that consciously adopts the perspectives of individuals, families and communities and sees them as participants as well as beneficiaries of trusted health systems that respond to their needs and preferences in humane and holistic ways.” (WHO, 2015) 10
“Care that is focussed and organised around people, rather than disease. Within this approach disease prevention and management are important but not enough to address the needs of person, family and community.” (International Alliance of Patients Organisations, 2007) 27
These definitions informed the broad review search strategy.
Numerous terms exist relating to person-centred care, including patient-centred, people-centred, patient-directed and so forth. We acknowledge that these various terms have differences in their origins and connotations. 28 However, as they overlap significantly and are often used interchangeably we chose to include all terms in the search strategy and analysis. When referring to this approach we chose to use the term ‘person-centred’. In agreement with Ekman et al 8 and The Health Foundation, 29 we take that view that the word ‘person’ avoids reducing the individual to a mere recipient of services and better highlights the whole human being with reason, preferences, needs and a social and cultural background.
The review focuses on serious illnesses in line with the following definition: “Serious illness carries a high risk of mortality, negatively impacts quality of life and daily function, and/or is burdensome in symptoms, treatments or caregiver stress. This includes conditions not advanced or high dependency/low function that carry a degree of clinical uncertainty” (Kelley et al , 2016). 30
According to Kelley et al ’s broadest definition of serious illness, serious medical conditions include: cancer (metastatic or hematological), renal failure, dementia, advanced liver disease or cirrhosis, diabetes with severe complications, amyotrophic lateral sclerosis, acquired immune deficiency syndrome, hip fracture, chronic obstructive pulmonary disease or interstitial lung disease if using home oxygen or hospitalised, and congestive heart failure if hospitalised for the condition. 30
Search strategy
The full search strategy is reported in online supplemental appendix A . The following databases were searched on 18 May 2020 with no date restrictions: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, MEDLINE, Ovid Global Health, PsycINFO and PubMed. Forward and backward reference chaining of included articles was performed.
Supplemental material
We included free text search terms (title, abstract and keyword search) related to (1) person-centred care/patient-centred care, (2) serious illness and (3) concept or practice (the meaning of PCC or way in which PCC is enacted). Search terms were adapted to each database subject headings and ‘exploded’ terms. The specific serious conditions included were those listed by Kelley et al 30 within their broad, operationalised definition of serious illness. Please see online supplemental appendix A for full list of search terms and example search strategy.
Data collection and extraction
All potential references identified were exported to EndNote reference manager and deduplicated. The primary reviewer (AG) assessed the titles and abstracts against the inclusion and exclusion criteria (detailed in online supplemental appendix A ). The full texts of remaining references were then similarly screened. Any reference for which inclusion was unclear was agreed through discussion with the secondary reviewer (KN) or adjudicated by a third reviewer (RH) if consensus was not reached. The following variables were extracted from retained studies into a common table: authors, year of publication, country, setting, aim and objectives, study design and methods, sample and main findings.
Quality assessment
We applied Kmet et al ’s Standard Quality Criteria 31 to the primary data. The checklists (quantitative data n=14-items, qualitative data 10-items) score each criterion ‘yes’=2, ‘partial’=1 and ‘no’=0. Items deemed not applicable are excluded from the summary score, which ranges from 1 (highest) to 0 (lowest). Online supplemental appendix A further details the method to calculate scores. We did not exclude studies based on quality score. The primary reviewer (AG) assessed the quality of each study. The secondary reviewer (KN) also assessed the quality of n=5 of the studies and met with the primary reviewer thereafter to compare assessments, resolve any discrepancies and enable reflections to be applied to all other studies’ quality assessments.
For quantitative studies, Kmet et al propose a cut-off score of 0.75 as the threshold for including a paper in a review. 31 As our goal was to assess data quality rather than exclude data failing to meet a quality threshold, we used Lee et al ’s 32 definitions for Kmet et al ’s quality scores; strong (summary score of >0.80), good (summary score of 0.71 to 0.79), adequate (summary score of 0.50 to 0.70) and limited (summary score of <0.50). For qualitative studies, Kmet et al use a threshold of 0.55 for inclusion of a study into their systematic review, 31 therefore we defined qualitative papers with scores of ≥0.55 as ‘adequate quality’ and ≤0.54 as ‘low quality’.
Data analysis
Retained studies were analysed using narrative synthesis in line with Guidance on the Conduct of Narrative Synthesis in Systematic reviews. 33 The preliminary synthesis was performed by tabulation, grouping and clustering.
To synthesise the extracted data the authors adopted a PCC model developed by Santana and colleagues 34 (hereafter referred to as Santana model). The Santana model was selected to structure the analysis of retained studies as it provides comprehensive, practical guidance for implementation of PCC, explicitly linking this guidance to the Donabedian model for assessing healthcare quality. 35 Santana et al ’s model was generated through a narrative review and synthesis of evidence, recommendations and best practice from implementation case studies, as well as existing frameworks. However, besides the consultation of a patient representative, there is limited voice of patients and families informing the model. The model’s authors suggest validation of the framework with additional diverse patient perspectives and to identify any necessary revisions or additions. 34
The components of the Santana model were used to construct an a priori coding frame for deductive analysis of the study findings retained in this systematic review (see online supplemental figure 1 for a priori coding frame). Findings that did not fit into the a priori frame were inductively coded into new codes. The primary reviewer (AG) coded the data using NVivo V.12 software, coding data that did not fit into the a priori frame into additional ‘Other’ nodes. The primary reviewer reviewed the contents of these ‘Other’ nodes throughout the analysis, generating new inductive codes where new themes appeared and revising or adding to these as more data was coded. New inductive codes were reviewed by the second and third reviewers (KN and RH), and discussed until consensus on new code meanings and labels was reached.
Patient and public involvement
Patient and public involvement was not conducted as part of this review.
The search summary flowchart following PRISMA guidelines is presented in figure 1 . The search yielded 12,446 references following deduplication, and 18 studies/n=19 papers 36–54 were retained and synthesised in this review. The characteristics of included studies are summarised in box 1 . Further detailed characteristics of each included study are presented in online supplemental table 1 , with Kmet et al ’s 31 data quality score.
Characteristics of included studies
Countries and settings.
All retained studies (n=18/18) reported data from high-income, Western countries.
The Netherlands (n=5/18) 36–40
Canada (n=3/18) 41–43
Australia (n=3/18) 44 45 49
USA (n=2/18) 46 50
UK (n=1/18) 47
Ireland (n=1/18) 53
Norway (n=1/18) 48
Sweden (n=1/18) 54
Germany (n=1/18 study reported in n=2/18 papers) 51 52
Healthcare settings
Hospital wards (n=5/18) 37 38 41 47 48
Residential aged care facilities (n=3/18) 44 45 54
Outpatient clinics (n=2/18) 36 50
Nursing homes (n=1/18) 53
Cancer centre (n=1/18) 42
Academic cancer institution (n=1/18) 43
Unknown/combination (n=5/18 studies reported in n=6/19 papers) 39 40 46 49 51 52
Diagnostic groups and healthcare professionals
Cancer (n=10/18 studies reported in n=11/17 papers) 36 38 39 41–43 48–52
Dementia (n=4/18) 44 45 53 54
End-stage renal disease (n=1/18) 37
Palliative or end-of-life care (n=2/18) 40 46
Mixed diagnostic groups experiencing acute care (n=1/18) 47
Participant groups included
Healthcare professionals (n=14/18 studies reported in n=15/18 papers) 37 39–47 49 51–54
Patients (n=10/18) 36–39 42 44 48–50 54
Caregivers (n=3/18) studies included 42 44 49
Volunteers working in palliative care (n=1/18) 40
Study designs
Qualitative designs (n=13/18):
Semi-structured interviews (n=11/18 studies reported in n=12/19 papers) 36 38 43–49 51–53
Focus groups (n=2/18) 43 47 50
Case studies (interview and observation) (n=1/18) 41
Mixed qualitative methods (posters and interviews, n=1/18) 42 interviews and focus groups, (n=1/18) 49
Quantitative design (n=1/18):
Survey (n=1/18) 54
Mixed-methodology designs (n=4/18):
Q methodology (n=2/18) 37 40
Questionnaire (n=1/18) 38
Delphi method (n=1/18) 39
Term used to refer to the PCC approach
Patient-centred care (n=8/18) 36–40 48–50
Person-centred care (n=7/18) 42 44 45 47 49 53 54
Patient-centred and family-centred care (n=1/18) 43
Client-centred care (n=1/18) 46
Individualised integrative care (n=1/18 reported in n=2/18 papers) 51 52
Interprofessional patient-centred care (n=1/18) 41
Kmet Data Quality Scores
Range=0.35 to 0.95 (possible range: 0 to 1)
Median=0.82
Qualitative studies and qualitative component of mixed-methods studies (n=17/18):
n=17 scored ≥0.55 (adequate quality)
n=1 scored ≤0.54 (low quality).
Quantitative studies and quantitative component of mixed-methods studies (n=5/18):
n=4 scored >0.80 (strong)
n=1 scored 0.71–0.79 (good)
Summary of aims and research questions of studies retained in this review
n=8/18 studies included an objective to investigate what is understood by the term PCC or what PCC should consist of in practice. 37 40 42 44–48
n=3/18 studies focused on patients’ experiences and expectations of care in relation to predetermined ideas of PCC components. 36 49 50
n=2/18 studies aimed to develop PCC indicators. 38 39
n=2/18 studies (reported in n=3/17 papers) aimed to investigate how teams that identify as providing PCC practice their care. 41 51 52
n=2/18 studies aimed to investigate clinicians’ knowledge and attitudes towards PCC. 43 53
n=1/18 study aimed to identify the organisational, environmental, resident and staff variables associated with aged care units with higher perceived levels of PCC. 54
- Download figure
- Open in new tab
- Download powerpoint
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2009 flow diagram.
Synthesis of included studies’ findings
Patient-family-provider relationship.
Overall, the findings suggest that PCC encompasses empowerment of both the patient and their family by being respected, 40 41 48 50 53 listened to, 36 37 47 48 understood, 47 given honest, complete and comprehendible information 36 37 39–41 43 48 49 and by being engaged in treatment decisions and all decisions that affect their daily life and care. 36 37 42 46 48 50 51 This requires collaborative, trusting relationships to be developed between patients, families and clinicians, 40 47 49–51 which rely on clinicians’ communication skills, 39 43 49 attitude 41 and demonstrable compassion, 42 for example, by comforting nervous patients. 36 The studies highlighted specific patient information needs, for example, using diagrams or drawings to aid comprehension, using accessible language, providing information about the possible course of the disease and information about the treatment option of ‘no active therapy’. 38 49 It was also raised that patients should be given the necessary information, education and support to enable self-management. 39
A further dominant theme was the importance of involving and supporting the patient’s family, friends or significant others, 36 44 46 47 49 although some patients may deem this a lesser priority. 37 40
In addition to physical symptom control, the studies suggest patients must also be supported in their psychological, social and spiritual needs, 39 40 45 49 51 52 with great attention to all needs and aspects of care that are important to the person. 36 42 46 47 Sufficient time 51 52 and availability of staff 41 was identified as crucial to address these needs. 54 This also requires flexibility and willingness to adapt skills, routines or environments for individual patients. 44 46
Several studies’ findings placed weight on promoting autonomy, continuation of self and normality and enabling patients to participate in life. 44 45 52 53 This was particularly highlighted in studies focussed on dementia patients and nursing homes, 44 53 where a dementia-friendly physical environment was also deemed important. 54
Organisational level requirements
On an organisational level, PCC was reported to demand a shared philosophy of care, 54 satisfactory leadership, support from colleagues and continuing education and mentorship of staff. 54 PCC was seen as requiring interdisciplinary collaboration, 51 54 and consistency and regularity in collaboration of all members of a care team. 41 Furthermore, all staff (not only front-line) were deemed responsible for providing person-centred care. 42 Included studies highlighted the importance of the coordination and continuity of patient care 44 49 and of streamlining care delivery, 43 for example, by having nursing staff provide additional teaching following the physician visit, 43 or appointing each patient a care coordinator. 37 39 49 Studies also indicated the importance of enhancing accessibility of healthcare services and considering logistical barriers, such as lack of transport or financial resources. 49
Complementary findings across participant groups, across countries and across PCC terms
There were no clear discrepancies between the findings of studies incorporating patient participants, caregiver participants or healthcare professional participants. The heterogeneity of studies did not permit analysis to determine difference between countries or regions. However, the study conducted with indigenous Australian populations reported study-specific findings such as the high financial burden of accessing care and the importance of feeling ‘culturally safe’ within the healthcare system. 49 There was also no evidence of consistent differences between findings from studies using different terms within the PCC consortium, that is, patient-centred care, patient-centred and family-centred care, client-centred care and so on. Based on the WHO definition of ‘people-centredness’, we hypothesised that this term has conceptual differences to person-centredness and patient-centredness and wished to investigate what these may be. However, as none of the retained empirical studies used this term we did not have the opportunity to investigate this.
Domains of Santana model supported by included studies’ data
The data from included studies largely supported the Santana model components ( online supplemental table 2 ), providing more detail about the specific meanings of subdomains, and suggesting relationships between concepts. This is particularly the case for many of the model’s Process dimensions which saw numerous corresponding data codes, for example, Being responsive to preferences, needs and values; Sensitivity to emotional or psychosocial needs; Sharing information; Shared decision-making .
Understanding patient within his or her unique psychosocial or cultural context is an example of a Santana model domain that is better specified through the included studies’ findings. Findings related to this domain suggest that clinicians should show interest in the person as a whole and gain an understanding of their psychological and emotional health, spiritual and existential issues, living conditions, financial situation, social support system, culture, personal identity and daily routines and activities. This knowledge should then be translated into tailored care, perhaps providing emotional support from nurses, referring to appropriate specialists, considering patient convenience and resource availability when ordering investigations and initiating conversations and activities that may be meaningful to a particular patient. 36 38 39 42–47 49 51 52
Domains of Santana model left unpopulated by included studies’ data
Table 1 presents domains of the Santana model for which no corresponding study data was found. Predominantly, the Structure components of the Santana model were unpopulated by findings from the 16 studies. This includes domains such as “S3. Co-designing the development and implementation of health promotion and prevention programs”, and “Spiritual and religious spaces”. “P2b. Providing resources” was the only Process domain to be left unpopulated by the data. Outcome dimensions “O2b Patient-Reported Experiences (PREMs)” and “O2c. Patient-Reported Adverse Outcomes (PRAOs)” were left with no corresponding findings from included studies.
- View inline
Santana model domains with no assigned codes from included studies:
Model adaptation: evidence additional to Santana model domains
Additional units of meaning arose from the included studies that are currently lacking in the Santana model: Family and friend involvement and support, Promoting continuation of normality and self-identity and Structuring service organisation to enable continuity of care and patient navigation . Table 2 presents these inductively-identified additional themes with examples of corresponding codes from supporting studies. Table 3 presents an adapted version of the Santana framework incorporating these additional themes.
Inductively-identified themes additional to Santana model with corresponding codes(see online supplemental table 2 for full table of studies’ findings deductively mapped onto Santana model and inductively mapped onto additional themes)
Adapted Santana framework incorporating additional themes from the empirical evidence (presented in bold text)
Specifically, Family and friend involvement and support was described as: inviting the patient to bring someone to appointments, 39 establishing conversation with family/friends; 42 involving family/friends in information-sharing and decisions regarding the patient’s care; 37 providing family/friends with opportunities to ask specialists and nurses questions; 38 respecting the opinions and worries of friends/family; 36 acknowledging family/friends in their role as carer for the patient; 37 44 and involving family/friends at all stages including long-term care, treatment and follow-up. 38 Being involved was deemed to avoid feelings of anxiety among family 44 49 and aid the patient emotionally, practically and in understanding and reflecting on information provided by clinicians. 49 51 This domain of PCC also requires healthcare professionals to pay attention to the needs of family/friends of the patient, 37 46 49 including providing accommodations in or near the hospital during treatment if possible, 37 49 and gathering information on the emotional health of family/friends and referring to specialists as appropriate. 39 It is worth noting that some patients and professionals may place this need as a low priority compared with other PCC domains. 37 40
Promoting continuation of normality and self-identity was discussed as requiring encouragement and enablement of persons with serious illness to participate in life despite the disease, and to regain a sense of control and self-efficacy. 51 52 This requires the clinician to consider a patient’s life goals and self-identity when discussing care and treatment options. 51 For long-term inpatients, particularly those with dementia, arranging and enabling meaningful activities was also viewed as a critical part of PCC. Creating individually targeted activities were described not only as providing a meaningful content to the day, but also as a means in reaffirming the residents as individual persons who were able to do the things they enjoyed. 44
Structuring service organisation to enable continuity of care and patient navigation encapsulates a collection of studies’ findings highlighting the importance of streamlining and easing patient navigation, ensuring continuity of care and simplifying the process of multi-specialist care. Suggestions for enabling this included appointing each patient a care coordinator or liaison officer, 37 41 49 ensuring patients see the same professionals over time 36 41 44 using multidisciplinary clinics to decrease wait times and patient anxiety between specialist referrals, 43 and arranging for nursing staff to provide additional information or education following a physician visit. 43
This review has revealed that a number of different constructs underpin the meaning and practice of PCC in the research evidence. These include patient and family empowerment and autonomy through respectful communication, appropriate information sharing and shared decision-making, addressing psychological, social, spiritual and cultural needs and enhancing coordination and continuity of care. The findings of this review indicate that person-centred healthcare must value the social network of each patient, and should promote quality of life and personal goals, not only health status improvement. This implies that person-centred health systems should be structured with flexible health workforce capacity and support staff to adapt skills, communication, routines or environments for individual patients and their families.
The studies’ findings largely validate the domains of the Santana framework of PCC, supporting their importance and providing more detail about specific meanings and subcomponents. The empirical findings of included studies also highlight new PCC themes additional to the Santana model. In focussing on serious illness, this review provides insights into the meaning of PCC that other, less severe conditions may not draw attention to.
The additional theme from included studies’ findings : Family and friend involvement and support , is in line with several other prominent conceptualisations of PCC. 2 16 55 It particularly aligns with conceptualisations that focus on ‘ people -centred’ care, such as that by the WHO, bringing attention to the health of people within their full social circles and communities. 56 57 The vast majority of everyday care is often undertaken by patient’s families and social networks. Enabling families and friends to be active participants in a patient’s healthcare should therefore rightly be a key goal of person-centred health systems reform.
Included studies also indicate PCC as enabling patients to continue to participate in daily life and meaningful activities, promoting continuation of self, personal identity and normality. This finding emphasises that patients’ highly value quality of life and continuation of their normal lives, not only health status improvement. This supports the idea that PCC involves striving to avoid damage to personal identities that the person values, 58 and ties into findings from research with frail populations showing patients value care that supports ‘getting back to normal’ or ‘finding a new normal’. 59 This finding also overlaps with a dimension of Mead and Bower’s patient-centredness framework: the ‘patient-as-person’, which places focus on the individual’s experience of illness and the impact of illness on the individual’s life or sense of self. 15
The third additional theme : Structuring service organisation to enable continuity of care and patient navigation, places particular weight on the organisational and structural reforms that are needed to enable person-centred, care-continuity processes. It highlights that PCC requires not only aspects of the clinician–patient interaction to reform, but also the experience the patient has in interacting with the wider healthcare system. Continuity of care has been presented within other prominent conceptualisations of PCC 17 17 18 55 55 however the specific structural features needed to enable this are rarely discussed. This review’s findings point towards some practical steps for achieving this, such as appointing each patient a care coordinator or arranging for nursing staff to provide additional teaching following a physician visit.
Strengths and limitations
The literature search conducted was comprehensive, considered numerous synonyms for PCC and involved no country or year of publication restrictions. This review also benefitted from interdisciplinary, multinational co-authors, allowing a range of perspectives and cultural viewpoints to inform the analysis and discussion. However, the review does suffer some limitations. First, only peer-reviewed studies published in English were included. Second, the review research questions and search strategy relating to ‘practice’ may have contributed to the lack of supporting data for structure and outcome domains of the Santana model. Third, only publications that included the term ‘person-centred’ (or synonym) were included. Research has certainly been conducted in non-Western LMICs that could inform models of PCC, for example, studies investigating ‘good communication skills’ or ‘empathetic care’. However, searching terms related to, in addition to near synonyms of, PCC would have deemed this review unfeasible. Our aim was to understand PCC as it is currently described.
Conclusions; implications for PCC research, policy and practice
This review indicates that there is a stark absence of theoretical models of PCC for serious illness that are grounded in empirical data. Future research should aim to generate theoretically-underpinned empirical frameworks for clinicians and policy makers on how to implement PCC through relevant, appropriate healthcare delivery.
It would also be insightful for future studies to further investigate the aforementioned PCC domains additional to the Satana model to validate whether these domains should constitute PCC components, and if so, what the specific, operationalisable actions within those components should be. One particular additional theme, Involving and supporting the patient’s family and friends , unsurprisingly surfaced most clearly in studies that included caregivers as participants (n=3). This highlights the importance of including this participant group in further empirical studies.
The included studies add depth and detail to existing Santana model domains, such as: Understanding patient within his or her unique psychosocial or cultural context . The findings related to this domain recognise that much of health is determined outside the clinic by social situations beyond the patient–clinician interaction, such as education, employment, income, housing, social support and gender. 60 Acknowledging and addressing these social determinants of health are critical to delivering PCC. Healthcare professionals must be given the support, tools and structures to actively engage with these social determinants of a person’s health and illness. However, this finding also raises the wider question of where the responsibility of PCC lies and how much of this rests with the individual clinic and clinician. Certain socially determined aspects of patient health can be positively influenced by a healthcare professional, others cannot. Consideration is needed about how and when clinicians should go beyond the clinic, and how to involve any external actors in contributing towards better patient health outcomes. 61 We must reflect on how a practice-based theory of PCC should sit within the broader socio-economic and cultural environment in which a health system operates.
Included studies also strongly support Santana model domains revolving around information sharing, shared decision-making and clinicians taking the time to properly understand each patient’s needs. This reaffirms the importance of in-depth holistic assessment of the patient and the need to empower patients and families through health literacy, equipping them with the knowledge to make informed decisions. 62
Several Outcome and Structure components of the Santana model were left unsupported by findings from the studies. This is not to say that those subdomains are unimportant, but that evidence to support them is lacking, and that patients, caregivers and professionals are most immediately exposed to, and concerned with, discussing processes. Future primary research with healthcare managers or policy makers should specify important structural and outcome domains. However, we could also perhaps infer that patients and caregivers facing serious illness are as, or even more, concerned with the quality of processes than with the outcomes which are most often the focus of healthcare improvement efforts. This suggests we should value process improvements as we value outcome improvements and should value the processes of person-centred care in and of themselves rather than just as a means to a series of outcomes. This supports ethical arguments that we should recognise the intrinsic, not just instrumental, value of PCC, and should pursue it as a valued quality and ethical domain in its own right. 13 58
The lack of study findings corresponding to some Structure components of the Santana model may also be a result of the lack of diversity in settings and diagnostic groups of included studies. The components left unpopulated by the studies’ findings appear to be those less relevant among the diagnostic groups and high-income settings of included studies. For example, Facility that prioritises the safety and security of its patients and staff is less likely to be voiced as a concern in high-income settings with lower rates of violent crime and civil unrest. Health promotion is an element of PCC that seems less poignant in cases of patients with end-of-life cancer and dementia; this topic may be of greater relevance in other serious conditions that are more responsive to lifestyle factors, such as chronic obstructive pulmonary disease. More empirical work is needed to confirm whether these components are of importance, what these components consist of and how they should be operationalised in day-to-day practice. This empirical investigation would be most insightful if conducted in a diverse range of contexts within which these components are likely to be more relevant.
PCC is an approach that evolved from high-income countries, and African theorists have questioned the relevance of Eurocentric conceptualisations and noted the absence of data to understand the meaning, feasibility and acceptability of PCC in non-Western LMICs. 63 This is unsurprising given existing biasses in healthcare research towards high-income countries, and limited resources and platforms for LMICs to conduct and promote this research. In the context of fewer resources, PCC may also be mistakenly perceived as a ‘nice-to-have luxury’ rather than a ‘need-to-have necessity’ and may be challenging to promote in settings with a history of disease-specific, vertical programmes. However, the lack of diversity in study countries raises questions about how both Santana model domains and additional themes could be conceptualised and operationalised globally, in a diversity of settings. Successful enactment of person-centred care would require a multitude of contextual and cultural factors to be considered and accommodated. For example, as Markus and Kitayama 64 discuss, the dominant construal of self differs between Western and other contexts. Western notions of the ‘self’ are that of an individual independent agent, while in most non-Western societies the ‘individual’ is more integrated with significant others. A patient with more interdependent views of self may be highly concerned with harmonising relationships and views. This has very real implications for the clinician–patient interaction and how to best practice involvement and support of a patient’s family and wider social network. Data from more individualistic cultures, such as that from the included Galekop et al study, 40 may suggest that ‘ there are some meetings involving the whole family, but ultimately, it is the patient who decides and not the family ’ . In a more collectivist culture, however, great importance may be placed on collective decision-making and the impacts of illness on a person’s network, 65 and thus, person-centred care would need to enable this. We must carefully consider the underlying values and determinants of culture in order to ensure cultural sensitivity in PCC theory. 58 66 A global theory of PCC and resulting policy would need to accommodate different beliefs and worldviews and centre around a common set of human values.
- Britten N ,
- Lydahl D , et al
- Institute of Medicine Committee on Quality of Health Care in A
- World Health Organization
- Chronic Diseases and Health Promotion Department
- Veillette AM , et al
- World Health Organization and International Bank for Reconstruction and Development/The World Bank
- Mezzich JE ,
- Appleyard J ,
- Botbol M , et al
- Swedberg K ,
- Taft C , et al
- Fenwick KM ,
- Barr N , et al
- Epstein RM ,
- Harding E ,
- Lawrence M ,
- Härter M , et al
- Naldemirci Öncel , et al
- Marshall A ,
- Bassett K , et al
- Jayadevappa R ,
- Haggerty J , et al
- McCormick KM
- Sleeman KE ,
- de Brito M ,
- Etkind S , et al
- Liberati A ,
- Tetzlaff J , et al
- International Alliance of Patients’ Organisations
- The Health Foundation
- Kelley AS ,
- Covinsky KE ,
- Gorges RJ , et al
- Packer TL ,
- Tang SH , et al
- Roberts H ,
- Sowden A , et al
- Santana MJ ,
- Manalili K ,
- Jolley RJ , et al
- Donabedian A
- Bisschop JAS ,
- Kloosterman FR ,
- van Leijen-Zeelenberg JE , et al
- Leensvaart L ,
- Berghout M , et al
- Hermens R ,
- Hulscher M , et al
- Uphoff EPMM ,
- Wennekes L ,
- Punt CJA , et al
- Galekop MMJ ,
- van Dijk HM ,
- van Exel J , et al
- Bilodeau K ,
- Vendette A , et al
- Nguyen TK ,
- Bauman GS ,
- Watling CJ , et al
- Edvardsson D ,
- Fetherstonhaugh D ,
- Oppert ML ,
- O'Keeffe VJ ,
- Anderson K ,
- Griffiths K , et al
- Chhatre S ,
- Wittink M , et al
- Kienle GS ,
- Mussler M ,
- Fuchs D , et al
- Colomer J ,
- Sjögren K ,
- Lindkvist M ,
- Sandman P-O , et al
- World Health Organization,
- Maeseneer J ,
- Weel Cvan ,
- Daeren L , et al
- Entwistle VA ,
- Etkind SN ,
- Nicholson CJ , et al
- Venkatapuram S
- Lowther K ,
- Harding R ,
- Simms V , et al
- Markus HR ,
- Stanford J ,
- Sandberg DM ,
- Gwyther L , et al
- Setlhare V ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
Handling editor Seye Abimbola
Twitter @KennedyNkhoma6, @sridhartweet
Contributors AG planned, conducted, reported and submitted this systematic review, and is responsible for the overall content as guarantor. KN assessed the quality of a subselection of included studies and compared assessments with AG. KN and RH reviewed the work as required. RP, IP, LG, LF and SV contributed to design and interpretation. KN, RH, SV, RP, IP, LG and LF approved the manuscript.
Funding This research was partly funded by the National Institute of Health Research (NIHR) Global Health Research Unit on Health System Strengthening in sub-Saharan Africa, King’s College London (GHRU 16/136/54) using UK aid from the UK Government to support global health research.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement All data relevant to the study are included in the article or uploaded as supplementary information. This paper is a systematic review and does not report novel primary data.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Login / FREE TRIAL

‘We have been left with the worst of both worlds on nurse recruitment’
STEVE FORD, EDITOR
- You are here: Nurse educators
Theory in practice
Nursing theories 1: person-centred care
23 October, 2017

This article is a bite-size summary of the concept of person-centred care. It is the first article in a six-part series on nursing theories and their implications for practice
Citation: Chapman H (2017) Nursing theories 1: person-centred care. Nursing Times [online]; 113: 10, 59.
Author: Hazel Chapman is postgraduate tutor, University of Chester.
- Scroll down to read the article or download a print-friendly PDF here
- Click here to see other articles in this series
Introduction
The underpinning theory that guides nursing practice can sometimes be forgotten in busy clinical environments. This article, the first in a six-part series providing a snapshot of nursing theories and their implications for practice, discusses person-centred care.
What is person-centred care?
Person-centred care involves knowledge of the individual as whole person, involving them – and where appropriate their family and friends – in helping to assess their own needs and plan their own care. The opposite of this is a task-focused approach, where Maslow’s hierarchy of needs is used to prioritise physical tasks over social care (Rollin, 2011).
Where does it come from?
The origins of person-centred care are in humanistic psychotherapy. Carl Rogers (1951) suggested we develop a view of ourselves in childhood based on our interactions with important others. If we are loved, valued and respected, we feel worthy of love, value and respect. Rogers called this unconditional positive regard.
If we are only valued for behaving in a certain way, we learn to hide some thoughts and behaviours. This conditional positive regard leads to a lack of congruence. Congruence is when the person we see ourselves as, and our ideal self, are similar. If we think we are a failure, we are afraid to ‘be ourselves’, preventing personal growth.
Rogers (1951) believed we need to learn throughout our lives and are capable of achieving personal growth through unconditional positive regard within trusting, genuine and open relationships, whatever our age. If this growth is prevented through feelings of insecurity, we become unhappy and even mentally ill.
In person-centred therapy, a trusting relationship requires the therapist to be genuine with their clients, to empathise with them (understand the service user’s world from their own perspective), and to value them without judging them. Over time, clients develop a sense of congruence, where the self and the ideal self meet.
This process of self-actualisation enables clients to gain confidence and self-esteem, making them open to new feelings and experiences, focusing on life as a process rather than a goal and valuing deep relationships with others (Rogers, 1959).
What does this mean for nurses?
In person-centred care, caring is central to nursing practice, and nurses’ relationships with the service user are fundamental to that individual’s experiences of care. The service user’s role is one of partnership, rather than a passive receiver of care. A person-centred relationship promotes self-esteem (positive self-regard) and self-efficacy (a feeling of being able to achieve one’s goals). Box 1 outlines the implications for practice.
Choice and education are central to person-centred care, which is also related to increased service user satisfaction. However, this move from a dependent, passive service user to an empowered partner in care requires a trusting relationship in which nurses do not react negatively to missed appointments or perceived ‘non-compliance’. Instead, nurses support the person to express their fears and concerns, to develop a trusting relationship that will promote self-caring behaviour. These humanistic concepts of “respect for persons, individual right to self-determination, mutual respect, and understanding” (McCormack et al, 2011) underpin person-centred care.
Box 1. Implications for practice
When interacting with service users:
- Treat them as individuals, and take cues from them regarding their interests, concerns and wishes
- Try to see their situation as they understand it and do not dismiss their views or fears – if they feel pain or are worried about their health, carry out relevant assessments and explain your actions
- Use every care episode to develop a trusting relationship with the service user, and ensure you give them the knowledge they need, empowering them to make decisions
- Include the person in the care planning process, focusing on communicating to understand and meet their views of their care needs
- Focusing on task completion
- A paternalistic approach of ’nurse knows best’
Also in this series
- Nursing theories 2: clinical supervision
- Nursing theories 3: nursing models
- Nursing theories 4: adherence and concordance
- Nursing theories 5: gender theory
- Nursing theories 6: social class
Related files
171025 nursing theories 1 person centred care.
- Add to Bookmarks
Related articles

Launch your nursing career – study at the University of Nottingham
Why study nursing at the University of Nottingham? We believe in the nursing profession and remain passionate about the care people receive.

Monitor, contribute, inform: a process to guide nursing associates
This article introduces a framework to support the integration and understanding of the role across care environments.

Creative health: challenging student nurses to learn from the arts
An arts-based practice learning placement helped nursing students develop an understanding of the value of social prescribing

Supporting student nurses to demonstrate professional values
Professional values form part of the student nurse journey while on placement. Staff and educators can help nursing students meet these.
Have your say
Sign in or Register a new account to join the discussion.
- Latest hearings
Person-centred care
- Caring with Confidence: The Code in Action
- Accountability
- Professional judgement
- Speaking up
- Being inclusive and challenging discrimination
- Social media
- End-of-life care
- Professionalism

In this animation we look at person-centred care .
Kindness and respect mean different things to different people. That’s why it matters to be person-centred. Being person-centred means thinking about what makes each person unique, and doing everything you can to put their needs first.
This animation supports nurses, midwives and nursing associates to understand why being person-centred leads to even better care.
Did you find this video useful?
We want to know if this video resource was helpful to you. Let us know
In the next video, we’ll talk about end-of-life care.
Related pages
- Last updated: 17/12/2020
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMJ Glob Health
- v.5(12); 2020

The empirical evidence underpinning the concept and practice of person-centred care for serious illness: a systematic review
Alessandra giusti.
1 Cicely Saunders Institute of Palliative Care, Policy and Rehabilitation, King's College London, London, UK
2 King's Global Health Institute, King's College London, London, UK
Kennedy Nkhoma
Ruwayda petrus.
3 School of Applied Human Sciences, University of KwaZulu-Natal College of Humanities, Durban, South Africa
Inge Petersen
Liz gwyther.
4 School of Public Health and Family Medicine, University of Cape Town Faculty of Health Sciences, Cape Town, Western Cape, South Africa
Lindsay Farrant
Sridhar venkatapuram, richard harding, associated data.
bmjgh-2020-003330supp001.pdf
bmjgh-2020-003330supp002.pdf
bmjgh-2020-003330supp003.pdf
Introduction
Person-centred care has become internationally recognised as a critical attribute of high-quality healthcare. However, the concept has been criticised for being poorly theorised and operationalised. Serious illness is especially aligned with the need for person-centredness, usually necessitating involvement of significant others, management of clinical uncertainty, high-quality communication and joint decision-making to deliver care concordant with patient preferences. This review aimed to identify and appraise the empirical evidence underpinning conceptualisations of ‘person-centredness’ for serious illness.
Search strategy conducted in May 2020. Databases: CINAHL, Embase, PubMed, Ovid Global Health, MEDLINE and PsycINFO. Free text search terms related to (1) person-centredness, (2) serious illness and (3) concept/practice. Tabulation, textual description and narrative synthesis were performed, and quality appraisal conducted using QualSyst tools. Santana et al ’s person-centred care model (2018) was used to structure analysis.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow data: n=12,446 studies screened by title/abstract, n=144 full articles assessed for eligibility, n=18 studies retained. All studies (n=18) are from high-income countries, and are largely of high quality (median score 0.82). The findings suggest that person-centred care encompasses the patient and family being respected, given complete information, involved in decision-making and supported in their physical, psychological, social and existential needs. The studies highlight the importance of involving and supporting family/friends, promoting continuation of normality and self-identity, and structuring service organisation to enable care continuity.
Person-centred healthcare must value the social network of patients, promote quality of life and reform structurally to improve patients’ experience interacting with the healthcare system. Staff must be supported to flexibly adapt skills, communication, routines or environments for individual patients. There remains a need for primary data investigating the meaning and practice of PCC in a greater diversity of diagnostic groups and settings, and a need to ground potential components of PCC within broader universal values and ethical theory.
Key questions
What is already known.
- Person-centred care has become internationally recognised as a dimension of high-quality healthcare, promoted as a core competency of health workers, a key component of primary care and essential to achieving the Universal Health Coverage goals.
- Ongoing conceptual debates are attempting to determine what constitutes ‘person-centredness’ and how this concept can be understood and implemented in a variety of settings.
- Serious illness is especially aligned with the need for PCC; the complex clinical scenarios surrounding serious illness usually necessitate the involvement of significant others and depend on high-quality communication and joint decision-making to deliver care concordant with patient preferences, with recognition and management of clinical uncertainty.
What are the new findings?
- Included studies largely support the Santana et al model of PCC and suggest that additional domains should be given visibility: family and friend involvement and support; promoting continuation of normality and self-identity; structuring service organisation to enable continuity of care and patient navigation.
- The empirical data stresses the importance of patients and families being respected, listened to, understood, given honest, complete and comprehendible information and being engaged in all decisions that affect their daily life, care and treatment. Patients must be supported in their physical, psychological, social and spiritual needs.
- All retained studies were conducted in high-income, Western countries.
- Empirical studies present invaluable data on the meaning and practice of PCC, however none develop this evidence into a theorised framework for implementation of PCC for serious illnesses.
What do the new findings imply?
- Person-centred healthcare must value the social network of each patient, promote quality of life and personal goals not only health status improvement, and implement structural reforms to improve patients’ experience of interacting with the healthcare system.
- Health systems must be structured to enable sufficient availability and accessibility of health workers, and support staff to be able and willing to flexibly adapt skills, communication, routines or environments for individual patients.
- There is a need for primary data investigating the meaning and practice of PCC in a greater diversity of diagnostic groups and settings, particularly non-Western, low- and middle-income settings.
- There is a need to consider the theoretical underpinnings of PCC and to ground potential components within broader universal values and ethical theory.
Person-centred care has become internationally recognised as a dimension of high-quality healthcare. 1 The Institute of Medicine describes quality care as that which is: “safe, effective, patient-centred, efficient, timely and equitable”. 2 WHO policy on people‐centred healthcare highlights person‐centredness as a core competency of health workers, a key component of primary care, and essential to achieving the Universal Health Coverage goals. 3–6
A variety of terms have been used to denote person-centred approaches. ‘ Patient -centredness’ was first to gain prominence and aimed to challenge the reductionism of the biomedical model and stress the importance of psychosocial factors. 2 3 Many moved towards use of the term ‘ person -centredness’, suggesting this better articulates the holism of the ‘whole person’ and a broader conception of well-being. 7 8 In recent years, the term ‘ people -centredness’ has also gained prominence, emphasising a focus on “the whole person in their specific familial and community contexts”. 9 Person-centred, patient-centred and people-centred care (PCC) all embody an approach that consciously adopts the perspectives of individuals, families and communities, respects and responds to their needs, values and preferences and sees them as participants in their own healthcare rather than just beneficiaries. 2 10
Conceptual clarity is critical to the design, delivery and replication of successful innovations in care. 11 Despite the global prominence of PCC as a goal of health systems, the approach suffers from a lack of clarity. Ongoing conceptual debates are attempting to determine what constitutes ‘person-centredness’ and how this concept can be understood and applied in a variety of contexts. 7 12–14 While numerous conceptualisations of PCC are presented in existing literature, 8 15–21 most do not appear to offer empirical origins or practical guidance on the implementation of PCC. The WHO Global strategy on people-centred and integrated health services recognises that there is not a single model of PCC to be proposed, but rather that it should be context-specific and that each country should generate its own evidence to enable appropriate, acceptable, feasible practice of PCC. 10 It is currently unclear what evidence is available to model contextually-appropriate and culturally-appropriate PCC.
The need for a person-centred approach is particularly important in the context of serious illness. The complex clinical scenarios surrounding serious illness usually necessitate the involvement of significant others, high-quality communication and joint decision-making to deliver care concordant with patient preferences, with recognition and management of clinical uncertainty. 22–24 As populations age, as infectious disease is better managed, and multimorbidity becomes more prevalent, serious health-related suffering associated with conditions such as cancer, chronic lung disease and dementia is rising fastest in low- and middle-income countries (LMICs). 25 Serious illness is also a context in which delivering PCC can be more complex and may require more dimensions to a greater degree than for non-serious illness. Focussing specifically on serious illness is therefore a means of ‘stress testing’ generalist PCC theory and ensuring it captures ‘what matters’ in all diagnostic cases. A better understanding of PCC in the context of serious illness would have health-system-wide relevance for other less complex clinical scenarios.
This systematic review aims to aggregate and appraise the empirical evidence underpinning the concept and practice of PCC in the context of serious illness. Specifically, the objectives of the review are to answer the following questions:
- What is the primary data underpinning conceptualisations and practice-based frameworks of ‘person-centredness’ in the context of serious illness?
- What is the quality of this data?
- What are the key constructs of PCC according to this data?
This systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations. 26 The review protocol was registered prospectively with PROSPERO: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=139259 (registration number 139259).
Definition of terms
To structure this review, literature was considered in line with two frequently cited definitions of PCC, one policy-led (using the term ‘ people -centredness’) and one patient-led (using the term ‘ patient -centredness’):
- “An approach to care that consciously adopts the perspectives of individuals, families and communities and sees them as participants as well as beneficiaries of trusted health systems that respond to their needs and preferences in humane and holistic ways.” (WHO, 2015) 10
- “Care that is focussed and organised around people, rather than disease. Within this approach disease prevention and management are important but not enough to address the needs of person, family and community.” (International Alliance of Patients Organisations, 2007) 27
These definitions informed the broad review search strategy.
Numerous terms exist relating to person-centred care, including patient-centred, people-centred, patient-directed and so forth. We acknowledge that these various terms have differences in their origins and connotations. 28 However, as they overlap significantly and are often used interchangeably we chose to include all terms in the search strategy and analysis. When referring to this approach we chose to use the term ‘person-centred’. In agreement with Ekman et al 8 and The Health Foundation, 29 we take that view that the word ‘person’ avoids reducing the individual to a mere recipient of services and better highlights the whole human being with reason, preferences, needs and a social and cultural background.
The review focuses on serious illnesses in line with the following definition: “Serious illness carries a high risk of mortality, negatively impacts quality of life and daily function, and/or is burdensome in symptoms, treatments or caregiver stress. This includes conditions not advanced or high dependency/low function that carry a degree of clinical uncertainty” (Kelley et al , 2016). 30
According to Kelley et al ’s broadest definition of serious illness, serious medical conditions include: cancer (metastatic or hematological), renal failure, dementia, advanced liver disease or cirrhosis, diabetes with severe complications, amyotrophic lateral sclerosis, acquired immune deficiency syndrome, hip fracture, chronic obstructive pulmonary disease or interstitial lung disease if using home oxygen or hospitalised, and congestive heart failure if hospitalised for the condition. 30
Search strategy
The full search strategy is reported in online supplemental appendix A . The following databases were searched on 18 May 2020 with no date restrictions: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, MEDLINE, Ovid Global Health, PsycINFO and PubMed. Forward and backward reference chaining of included articles was performed.
Supplementary data
We included free text search terms (title, abstract and keyword search) related to (1) person-centred care/patient-centred care, (2) serious illness and (3) concept or practice (the meaning of PCC or way in which PCC is enacted). Search terms were adapted to each database subject headings and ‘exploded’ terms. The specific serious conditions included were those listed by Kelley et al 30 within their broad, operationalised definition of serious illness. Please see online supplemental appendix A for full list of search terms and example search strategy.
Data collection and extraction
All potential references identified were exported to EndNote reference manager and deduplicated. The primary reviewer (AG) assessed the titles and abstracts against the inclusion and exclusion criteria (detailed in online supplemental appendix A ). The full texts of remaining references were then similarly screened. Any reference for which inclusion was unclear was agreed through discussion with the secondary reviewer (KN) or adjudicated by a third reviewer (RH) if consensus was not reached. The following variables were extracted from retained studies into a common table: authors, year of publication, country, setting, aim and objectives, study design and methods, sample and main findings.
Quality assessment
We applied Kmet et al ’s Standard Quality Criteria 31 to the primary data. The checklists (quantitative data n=14-items, qualitative data 10-items) score each criterion ‘yes’=2, ‘partial’=1 and ‘no’=0. Items deemed not applicable are excluded from the summary score, which ranges from 1 (highest) to 0 (lowest). Online supplemental appendix A further details the method to calculate scores. We did not exclude studies based on quality score. The primary reviewer (AG) assessed the quality of each study. The secondary reviewer (KN) also assessed the quality of n=5 of the studies and met with the primary reviewer thereafter to compare assessments, resolve any discrepancies and enable reflections to be applied to all other studies’ quality assessments.
For quantitative studies, Kmet et al propose a cut-off score of 0.75 as the threshold for including a paper in a review. 31 As our goal was to assess data quality rather than exclude data failing to meet a quality threshold, we used Lee et al ’s 32 definitions for Kmet et al ’s quality scores; strong (summary score of >0.80), good (summary score of 0.71 to 0.79), adequate (summary score of 0.50 to 0.70) and limited (summary score of <0.50). For qualitative studies, Kmet et al use a threshold of 0.55 for inclusion of a study into their systematic review, 31 therefore we defined qualitative papers with scores of ≥0.55 as ‘adequate quality’ and ≤0.54 as ‘low quality’.
Data analysis
Retained studies were analysed using narrative synthesis in line with Guidance on the Conduct of Narrative Synthesis in Systematic reviews. 33 The preliminary synthesis was performed by tabulation, grouping and clustering.
To synthesise the extracted data the authors adopted a PCC model developed by Santana and colleagues 34 (hereafter referred to as Santana model). The Santana model was selected to structure the analysis of retained studies as it provides comprehensive, practical guidance for implementation of PCC, explicitly linking this guidance to the Donabedian model for assessing healthcare quality. 35 Santana et al ’s model was generated through a narrative review and synthesis of evidence, recommendations and best practice from implementation case studies, as well as existing frameworks. However, besides the consultation of a patient representative, there is limited voice of patients and families informing the model. The model’s authors suggest validation of the framework with additional diverse patient perspectives and to identify any necessary revisions or additions. 34
The components of the Santana model were used to construct an a priori coding frame for deductive analysis of the study findings retained in this systematic review (see online supplemental figure 1 for a priori coding frame). Findings that did not fit into the a priori frame were inductively coded into new codes. The primary reviewer (AG) coded the data using NVivo V.12 software, coding data that did not fit into the a priori frame into additional ‘Other’ nodes. The primary reviewer reviewed the contents of these ‘Other’ nodes throughout the analysis, generating new inductive codes where new themes appeared and revising or adding to these as more data was coded. New inductive codes were reviewed by the second and third reviewers (KN and RH), and discussed until consensus on new code meanings and labels was reached.
Patient and public involvement
Patient and public involvement was not conducted as part of this review.
The search summary flowchart following PRISMA guidelines is presented in figure 1 . The search yielded 12,446 references following deduplication, and 18 studies/n=19 papers 36–54 were retained and synthesised in this review. The characteristics of included studies are summarised in box 1 . Further detailed characteristics of each included study are presented in online supplemental table 1 , with Kmet et al ’s 31 data quality score.
Characteristics of included studies
Countries and settings.
All retained studies (n=18/18) reported data from high-income, Western countries.
- The Netherlands (n=5/18) 36–40
- Canada (n=3/18) 41–43
- Australia (n=3/18) 44 45 49
- USA (n=2/18) 46 50
- UK (n=1/18) 47
- Ireland (n=1/18) 53
- Norway (n=1/18) 48
- Sweden (n=1/18) 54
- Germany (n=1/18 study reported in n=2/18 papers) 51 52
Healthcare settings
- Hospital wards (n=5/18) 37 38 41 47 48
- Residential aged care facilities (n=3/18) 44 45 54
- Outpatient clinics (n=2/18) 36 50
- Nursing homes (n=1/18) 53
- Cancer centre (n=1/18) 42
- Academic cancer institution (n=1/18) 43
- Unknown/combination (n=5/18 studies reported in n=6/19 papers) 39 40 46 49 51 52
Diagnostic groups and healthcare professionals
- Cancer (n=10/18 studies reported in n=11/17 papers) 36 38 39 41–43 48–52
- Dementia (n=4/18) 44 45 53 54
- End-stage renal disease (n=1/18) 37
- Palliative or end-of-life care (n=2/18) 40 46
- Mixed diagnostic groups experiencing acute care (n=1/18) 47
Participant groups included
- Healthcare professionals (n=14/18 studies reported in n=15/18 papers) 37 39–47 49 51–54
- Patients (n=10/18) 36–39 42 44 48–50 54
- Caregivers (n=3/18) studies included 42 44 49
- Volunteers working in palliative care (n=1/18) 40
Study designs
Qualitative designs (n=13/18):
- Semi-structured interviews (n=11/18 studies reported in n=12/19 papers) 36 38 43–49 51–53
- Focus groups (n=2/18) 43 47 50
- Case studies (interview and observation) (n=1/18) 41
- Mixed qualitative methods (posters and interviews, n=1/18) 42 interviews and focus groups, (n=1/18) 49
Quantitative design (n=1/18):
- Survey (n=1/18) 54
Mixed-methodology designs (n=4/18):
- Q methodology (n=2/18) 37 40
- Questionnaire (n=1/18) 38
- Delphi method (n=1/18) 39
Term used to refer to the PCC approach
- Patient-centred care (n=8/18) 36–40 48–50
- Person-centred care (n=7/18) 42 44 45 47 49 53 54
- Patient-centred and family-centred care (n=1/18) 43
- Client-centred care (n=1/18) 46
- Individualised integrative care (n=1/18 reported in n=2/18 papers) 51 52
- Interprofessional patient-centred care (n=1/18) 41
Kmet Data Quality Scores
Range=0.35 to 0.95 (possible range: 0 to 1)
Median=0.82
Qualitative studies and qualitative component of mixed-methods studies (n=17/18):
- n=17 scored ≥0.55 (adequate quality)
- n=1 scored ≤0.54 (low quality).
Quantitative studies and quantitative component of mixed-methods studies (n=5/18):
- n=4 scored >0.80 (strong)
- n=1 scored 0.71–0.79 (good)
Summary of aims and research questions of studies retained in this review
- n=8/18 studies included an objective to investigate what is understood by the term PCC or what PCC should consist of in practice. 37 40 42 44–48
- n=3/18 studies focused on patients’ experiences and expectations of care in relation to predetermined ideas of PCC components. 36 49 50
- n=2/18 studies aimed to develop PCC indicators. 38 39
- n=2/18 studies (reported in n=3/17 papers) aimed to investigate how teams that identify as providing PCC practice their care. 41 51 52
- n=2/18 studies aimed to investigate clinicians’ knowledge and attitudes towards PCC. 43 53
- n=1/18 study aimed to identify the organisational, environmental, resident and staff variables associated with aged care units with higher perceived levels of PCC. 54

PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2009 flow diagram.
Synthesis of included studies’ findings
Patient-family-provider relationship.
Overall, the findings suggest that PCC encompasses empowerment of both the patient and their family by being respected, 40 41 48 50 53 listened to, 36 37 47 48 understood, 47 given honest, complete and comprehendible information 36 37 39–41 43 48 49 and by being engaged in treatment decisions and all decisions that affect their daily life and care. 36 37 42 46 48 50 51 This requires collaborative, trusting relationships to be developed between patients, families and clinicians, 40 47 49–51 which rely on clinicians’ communication skills, 39 43 49 attitude 41 and demonstrable compassion, 42 for example, by comforting nervous patients. 36 The studies highlighted specific patient information needs, for example, using diagrams or drawings to aid comprehension, using accessible language, providing information about the possible course of the disease and information about the treatment option of ‘no active therapy’. 38 49 It was also raised that patients should be given the necessary information, education and support to enable self-management. 39
A further dominant theme was the importance of involving and supporting the patient’s family, friends or significant others, 36 44 46 47 49 although some patients may deem this a lesser priority. 37 40
In addition to physical symptom control, the studies suggest patients must also be supported in their psychological, social and spiritual needs, 39 40 45 49 51 52 with great attention to all needs and aspects of care that are important to the person. 36 42 46 47 Sufficient time 51 52 and availability of staff 41 was identified as crucial to address these needs. 54 This also requires flexibility and willingness to adapt skills, routines or environments for individual patients. 44 46
Several studies’ findings placed weight on promoting autonomy, continuation of self and normality and enabling patients to participate in life. 44 45 52 53 This was particularly highlighted in studies focussed on dementia patients and nursing homes, 44 53 where a dementia-friendly physical environment was also deemed important. 54
Organisational level requirements
On an organisational level, PCC was reported to demand a shared philosophy of care, 54 satisfactory leadership, support from colleagues and continuing education and mentorship of staff. 54 PCC was seen as requiring interdisciplinary collaboration, 51 54 and consistency and regularity in collaboration of all members of a care team. 41 Furthermore, all staff (not only front-line) were deemed responsible for providing person-centred care. 42 Included studies highlighted the importance of the coordination and continuity of patient care 44 49 and of streamlining care delivery, 43 for example, by having nursing staff provide additional teaching following the physician visit, 43 or appointing each patient a care coordinator. 37 39 49 Studies also indicated the importance of enhancing accessibility of healthcare services and considering logistical barriers, such as lack of transport or financial resources. 49
Complementary findings across participant groups, across countries and across PCC terms
There were no clear discrepancies between the findings of studies incorporating patient participants, caregiver participants or healthcare professional participants. The heterogeneity of studies did not permit analysis to determine difference between countries or regions. However, the study conducted with indigenous Australian populations reported study-specific findings such as the high financial burden of accessing care and the importance of feeling ‘culturally safe’ within the healthcare system. 49 There was also no evidence of consistent differences between findings from studies using different terms within the PCC consortium, that is, patient-centred care, patient-centred and family-centred care, client-centred care and so on. Based on the WHO definition of ‘people-centredness’, we hypothesised that this term has conceptual differences to person-centredness and patient-centredness and wished to investigate what these may be. However, as none of the retained empirical studies used this term we did not have the opportunity to investigate this.
Domains of Santana model supported by included studies’ data
The data from included studies largely supported the Santana model components ( online supplemental table 2 ), providing more detail about the specific meanings of subdomains, and suggesting relationships between concepts. This is particularly the case for many of the model’s Process dimensions which saw numerous corresponding data codes, for example, Being responsive to preferences, needs and values; Sensitivity to emotional or psychosocial needs; Sharing information; Shared decision-making .
Understanding patient within his or her unique psychosocial or cultural context is an example of a Santana model domain that is better specified through the included studies’ findings. Findings related to this domain suggest that clinicians should show interest in the person as a whole and gain an understanding of their psychological and emotional health, spiritual and existential issues, living conditions, financial situation, social support system, culture, personal identity and daily routines and activities. This knowledge should then be translated into tailored care, perhaps providing emotional support from nurses, referring to appropriate specialists, considering patient convenience and resource availability when ordering investigations and initiating conversations and activities that may be meaningful to a particular patient. 36 38 39 42–47 49 51 52
Domains of Santana model left unpopulated by included studies’ data
Table 1 presents domains of the Santana model for which no corresponding study data was found. Predominantly, the Structure components of the Santana model were unpopulated by findings from the 16 studies. This includes domains such as “S3. Co-designing the development and implementation of health promotion and prevention programs”, and “Spiritual and religious spaces”. “P2b. Providing resources” was the only Process domain to be left unpopulated by the data. Outcome dimensions “O2b Patient-Reported Experiences (PREMs)” and “O2c. Patient-Reported Adverse Outcomes (PRAOs)” were left with no corresponding findings from included studies.
Santana model domains with no assigned codes from included studies:
| Structure | “S1a. Core values and Philosophy of the organisation” subdomains: “S1b. Establishing operational definition of PCC” subdomains: “S2. Co-designing the development and implementation of educational programs” subdomains: “S3. Co-designing the development and implementation of health promotion and prevention programs” and all sub-domains “S4a. Ensure resources for staff to practice PCC” and subdomain: “S5. Providing a supportive and accommodating PCC environment” subdomains: “S6. Developing and integrating structures to support health information technology” and all subdomains “S7. Creating structures to measure and monitor PCC” and subdomain: “Co-design and develop framework for measurement, monitoring and evaluation” |
| Process | “P2b. Providing resources” |
| Outcome | “O2b Patient-Reported Experiences (PREMs)” and subdomain: “Recommendation or rating of hospital, healthcare provider” “O2c. Patient-Reported Adverse Outcomes (PRAOs)” and subdomains: |
Model adaptation: evidence additional to Santana model domains
Additional units of meaning arose from the included studies that are currently lacking in the Santana model: Family and friend involvement and support, Promoting continuation of normality and self-identity and Structuring service organisation to enable continuity of care and patient navigation . Table 2 presents these inductively-identified additional themes with examples of corresponding codes from supporting studies. Table 3 presents an adapted version of the Santana framework incorporating these additional themes.
Inductively-identified themes additional to Santana model with corresponding codes(see online supplemental table 2 for full table of studies’ findings deductively mapped onto Santana model and inductively mapped onto additional themes)
| Inductively-identified themes additional to Santana model | Number of supporting studies | Examples of corresponding codes from supporting studies |
| Family and friend involvement and support | 11 | ). (Ross et al, 2015, p1228; Quality score 0.8) . (Edvardsson et al, 2010, p2614; Quality score 0.8) ). (Galekop et al, 2019, p4; Quality score 0.95 (qualitative), 0.85 (quantitative)) . (Bisschop et al, 2017, p2250; Quality score 0.85) . (Ouwens et al, 2010, p126; Quality score 0.65 (qualitative), 0.78 (quantitative)) . (One of final set of approved quality indicators), (Uphoff et al, 2011, p35; Quality score 0.8 (qualitative), 0.88 (quantitative)) ). (Green et al, 2018, p8; Quality score 0.85) |
| Promoting continuation of normality and self-identity | 8 | . (Kienle et al, 2016, p483, Quality score 0.9) (Kienle et al, 2018, p128; Quality score 0.9) (Kienle et al, 2016, p482, Quality score 0.9) . (Edvardsson et al, 2010, p2615; Quality score 0.8) . Pizzi, 2015, p446; Quality score 0.65) |
| Structuring service organisation to enable continuity of care and patient navigation | 10 | . (Physician identified patient- and family-centred strategy pertaining to streamlining care delivery.) (Nguyen et al, 2017 (online supplemental table 2); Quality score 0.65) ) (Bilodeau et al, 2015, p109; Quality score 0.7) ) Bisschop et al, 2017, p2250; Quality score 0.85) (Edvardsson et al, 2010, p2616; Quality score 0.8) ). (Kienle et al, 2016, p488, Quality score 0.9) |
Adapted Santana framework incorporating additional themes from the empirical evidence (presented in bold text)
| Structure | Process | Outcome |
| S1. Creating a PCC culture subdomain S1a. Core values and philosophy of the organisation S1b. Establishing operational definition of PCC S2. Co- designing the development and implementation of educational programs Standardised PCC training in all healthcare professional programs S3. Co- designing the development and implementation of health promotion and prevention programs S3a. Collaboration and empowerment of patients, communities and organisations in design of programs S4. Supporting a workforce committed to PCC S4a. Ensure resources for staff to practice PCC S5. Providing a supportive and accommodating PCC environment S5a. Designing healthcare facilities and services promoting PCC S5b. Integrating organisation-wide services promoting PCC S6. Developing and integrating structures to support health information technology Common e-health platform for health information exchange across providers and patients S7. Creating structures to measure and monitor PCC performance Co-design and develop framework for measurement, monitoring and evaluation . | P1. Cultivating communication P1a. Listening to patients P1b. Sharing information P1c. Discussing care plans with patients P2. Respectful and compassionate care P2a. Being responsive to preferences, needs and values P2b. Providing supportive care P3. Engaging patients in managing their care Co-designing care plans with patients P4. Integration of care Communication and information sharing for coordination and continuity of care across the continuum of care | O1. Access to care O1a. Timely access to care Components O1b. Care availability O1c. Financial burden O2. Patient-Reported Outcomes (PROs) O2a. Patient-Reported Outcomes Measures (PROMs) O2b. Patient-Reported Experiences (PREMs) O2c. Patient-Reported Adverse Outcomes (PRAOs) |
Specifically, Family and friend involvement and support was described as: inviting the patient to bring someone to appointments, 39 establishing conversation with family/friends; 42 involving family/friends in information-sharing and decisions regarding the patient’s care; 37 providing family/friends with opportunities to ask specialists and nurses questions; 38 respecting the opinions and worries of friends/family; 36 acknowledging family/friends in their role as carer for the patient; 37 44 and involving family/friends at all stages including long-term care, treatment and follow-up. 38 Being involved was deemed to avoid feelings of anxiety among family 44 49 and aid the patient emotionally, practically and in understanding and reflecting on information provided by clinicians. 49 51 This domain of PCC also requires healthcare professionals to pay attention to the needs of family/friends of the patient, 37 46 49 including providing accommodations in or near the hospital during treatment if possible, 37 49 and gathering information on the emotional health of family/friends and referring to specialists as appropriate. 39 It is worth noting that some patients and professionals may place this need as a low priority compared with other PCC domains. 37 40
Promoting continuation of normality and self-identity was discussed as requiring encouragement and enablement of persons with serious illness to participate in life despite the disease, and to regain a sense of control and self-efficacy. 51 52 This requires the clinician to consider a patient’s life goals and self-identity when discussing care and treatment options. 51 For long-term inpatients, particularly those with dementia, arranging and enabling meaningful activities was also viewed as a critical part of PCC. Creating individually targeted activities were described not only as providing a meaningful content to the day, but also as a means in reaffirming the residents as individual persons who were able to do the things they enjoyed. 44
Structuring service organisation to enable continuity of care and patient navigation encapsulates a collection of studies’ findings highlighting the importance of streamlining and easing patient navigation, ensuring continuity of care and simplifying the process of multi-specialist care. Suggestions for enabling this included appointing each patient a care coordinator or liaison officer, 37 41 49 ensuring patients see the same professionals over time 36 41 44 using multidisciplinary clinics to decrease wait times and patient anxiety between specialist referrals, 43 and arranging for nursing staff to provide additional information or education following a physician visit. 43
This review has revealed that a number of different constructs underpin the meaning and practice of PCC in the research evidence. These include patient and family empowerment and autonomy through respectful communication, appropriate information sharing and shared decision-making, addressing psychological, social, spiritual and cultural needs and enhancing coordination and continuity of care. The findings of this review indicate that person-centred healthcare must value the social network of each patient, and should promote quality of life and personal goals, not only health status improvement. This implies that person-centred health systems should be structured with flexible health workforce capacity and support staff to adapt skills, communication, routines or environments for individual patients and their families.
The studies’ findings largely validate the domains of the Santana framework of PCC, supporting their importance and providing more detail about specific meanings and subcomponents. The empirical findings of included studies also highlight new PCC themes additional to the Santana model. In focussing on serious illness, this review provides insights into the meaning of PCC that other, less severe conditions may not draw attention to.
The additional theme from included studies’ findings : Family and friend involvement and support , is in line with several other prominent conceptualisations of PCC. 2 16 55 It particularly aligns with conceptualisations that focus on ‘ people -centred’ care, such as that by the WHO, bringing attention to the health of people within their full social circles and communities. 56 57 The vast majority of everyday care is often undertaken by patient’s families and social networks. Enabling families and friends to be active participants in a patient’s healthcare should therefore rightly be a key goal of person-centred health systems reform.
Included studies also indicate PCC as enabling patients to continue to participate in daily life and meaningful activities, promoting continuation of self, personal identity and normality. This finding emphasises that patients’ highly value quality of life and continuation of their normal lives, not only health status improvement. This supports the idea that PCC involves striving to avoid damage to personal identities that the person values, 58 and ties into findings from research with frail populations showing patients value care that supports ‘getting back to normal’ or ‘finding a new normal’. 59 This finding also overlaps with a dimension of Mead and Bower’s patient-centredness framework: the ‘patient-as-person’, which places focus on the individual’s experience of illness and the impact of illness on the individual’s life or sense of self. 15
The third additional theme : Structuring service organisation to enable continuity of care and patient navigation, places particular weight on the organisational and structural reforms that are needed to enable person-centred, care-continuity processes. It highlights that PCC requires not only aspects of the clinician–patient interaction to reform, but also the experience the patient has in interacting with the wider healthcare system. Continuity of care has been presented within other prominent conceptualisations of PCC 17 17 18 55 55 however the specific structural features needed to enable this are rarely discussed. This review’s findings point towards some practical steps for achieving this, such as appointing each patient a care coordinator or arranging for nursing staff to provide additional teaching following a physician visit.
Strengths and limitations
The literature search conducted was comprehensive, considered numerous synonyms for PCC and involved no country or year of publication restrictions. This review also benefitted from interdisciplinary, multinational co-authors, allowing a range of perspectives and cultural viewpoints to inform the analysis and discussion. However, the review does suffer some limitations. First, only peer-reviewed studies published in English were included. Second, the review research questions and search strategy relating to ‘practice’ may have contributed to the lack of supporting data for structure and outcome domains of the Santana model. Third, only publications that included the term ‘person-centred’ (or synonym) were included. Research has certainly been conducted in non-Western LMICs that could inform models of PCC, for example, studies investigating ‘good communication skills’ or ‘empathetic care’. However, searching terms related to, in addition to near synonyms of, PCC would have deemed this review unfeasible. Our aim was to understand PCC as it is currently described.
Conclusions; implications for PCC research, policy and practice
This review indicates that there is a stark absence of theoretical models of PCC for serious illness that are grounded in empirical data. Future research should aim to generate theoretically-underpinned empirical frameworks for clinicians and policy makers on how to implement PCC through relevant, appropriate healthcare delivery.
It would also be insightful for future studies to further investigate the aforementioned PCC domains additional to the Satana model to validate whether these domains should constitute PCC components, and if so, what the specific, operationalisable actions within those components should be. One particular additional theme, Involving and supporting the patient’s family and friends , unsurprisingly surfaced most clearly in studies that included caregivers as participants (n=3). This highlights the importance of including this participant group in further empirical studies.
The included studies add depth and detail to existing Santana model domains, such as: Understanding patient within his or her unique psychosocial or cultural context . The findings related to this domain recognise that much of health is determined outside the clinic by social situations beyond the patient–clinician interaction, such as education, employment, income, housing, social support and gender. 60 Acknowledging and addressing these social determinants of health are critical to delivering PCC. Healthcare professionals must be given the support, tools and structures to actively engage with these social determinants of a person’s health and illness. However, this finding also raises the wider question of where the responsibility of PCC lies and how much of this rests with the individual clinic and clinician. Certain socially determined aspects of patient health can be positively influenced by a healthcare professional, others cannot. Consideration is needed about how and when clinicians should go beyond the clinic, and how to involve any external actors in contributing towards better patient health outcomes. 61 We must reflect on how a practice-based theory of PCC should sit within the broader socio-economic and cultural environment in which a health system operates.
Included studies also strongly support Santana model domains revolving around information sharing, shared decision-making and clinicians taking the time to properly understand each patient’s needs. This reaffirms the importance of in-depth holistic assessment of the patient and the need to empower patients and families through health literacy, equipping them with the knowledge to make informed decisions. 62
Several Outcome and Structure components of the Santana model were left unsupported by findings from the studies. This is not to say that those subdomains are unimportant, but that evidence to support them is lacking, and that patients, caregivers and professionals are most immediately exposed to, and concerned with, discussing processes. Future primary research with healthcare managers or policy makers should specify important structural and outcome domains. However, we could also perhaps infer that patients and caregivers facing serious illness are as, or even more, concerned with the quality of processes than with the outcomes which are most often the focus of healthcare improvement efforts. This suggests we should value process improvements as we value outcome improvements and should value the processes of person-centred care in and of themselves rather than just as a means to a series of outcomes. This supports ethical arguments that we should recognise the intrinsic, not just instrumental, value of PCC, and should pursue it as a valued quality and ethical domain in its own right. 13 58
The lack of study findings corresponding to some Structure components of the Santana model may also be a result of the lack of diversity in settings and diagnostic groups of included studies. The components left unpopulated by the studies’ findings appear to be those less relevant among the diagnostic groups and high-income settings of included studies. For example, Facility that prioritises the safety and security of its patients and staff is less likely to be voiced as a concern in high-income settings with lower rates of violent crime and civil unrest. Health promotion is an element of PCC that seems less poignant in cases of patients with end-of-life cancer and dementia; this topic may be of greater relevance in other serious conditions that are more responsive to lifestyle factors, such as chronic obstructive pulmonary disease. More empirical work is needed to confirm whether these components are of importance, what these components consist of and how they should be operationalised in day-to-day practice. This empirical investigation would be most insightful if conducted in a diverse range of contexts within which these components are likely to be more relevant.
PCC is an approach that evolved from high-income countries, and African theorists have questioned the relevance of Eurocentric conceptualisations and noted the absence of data to understand the meaning, feasibility and acceptability of PCC in non-Western LMICs. 63 This is unsurprising given existing biasses in healthcare research towards high-income countries, and limited resources and platforms for LMICs to conduct and promote this research. In the context of fewer resources, PCC may also be mistakenly perceived as a ‘nice-to-have luxury’ rather than a ‘need-to-have necessity’ and may be challenging to promote in settings with a history of disease-specific, vertical programmes. However, the lack of diversity in study countries raises questions about how both Santana model domains and additional themes could be conceptualised and operationalised globally, in a diversity of settings. Successful enactment of person-centred care would require a multitude of contextual and cultural factors to be considered and accommodated. For example, as Markus and Kitayama 64 discuss, the dominant construal of self differs between Western and other contexts. Western notions of the ‘self’ are that of an individual independent agent, while in most non-Western societies the ‘individual’ is more integrated with significant others. A patient with more interdependent views of self may be highly concerned with harmonising relationships and views. This has very real implications for the clinician–patient interaction and how to best practice involvement and support of a patient’s family and wider social network. Data from more individualistic cultures, such as that from the included Galekop et al study, 40 may suggest that ‘ there are some meetings involving the whole family, but ultimately, it is the patient who decides and not the family ’ . In a more collectivist culture, however, great importance may be placed on collective decision-making and the impacts of illness on a person’s network, 65 and thus, person-centred care would need to enable this. We must carefully consider the underlying values and determinants of culture in order to ensure cultural sensitivity in PCC theory. 58 66 A global theory of PCC and resulting policy would need to accommodate different beliefs and worldviews and centre around a common set of human values.
Handling editor: Seye Abimbola
Twitter: @KennedyNkhoma6, @sridhartweet
Contributors: AG planned, conducted, reported and submitted this systematic review, and is responsible for the overall content as guarantor. KN assessed the quality of a subselection of included studies and compared assessments with AG. KN and RH reviewed the work as required. RP, IP, LG, LF and SV contributed to design and interpretation. KN, RH, SV, RP, IP, LG and LF approved the manuscript.
Funding: This research was partly funded by the National Institute of Health Research (NIHR) Global Health Research Unit on Health System Strengthening in sub-Saharan Africa, King’s College London (GHRU 16/136/54) using UK aid from the UK Government to support global health research.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information. This paper is a systematic review and does not report novel primary data.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
- Find My Rep
You are here
Sage online ordering services are currently unavailable due to a service outage. We are working to restore service as soon as possible. In the meantime, our books are still available widely via retailers and online. Inspection copies can be requested direct from Vitalsource and Kortext . if you need further assistance please visit our Contact us page for further information. Thank you for your patience and we apologise for the inconvenience.
Understanding Person-Centred Care for Nursing Associates
- Myles Harris
- Description
Understanding how to deliver effective, person-centred care is vital for a future career as a Nursing Associate. In this book, trainee nursing associates are introduced to the principles of person-centred care, with case studies from a variety of healthcare settings and guidance on caring for different patient groups, from acute care to long-term and palliative care. This allows TNAs to see how the theory can be directly applied to their daily practice, regardless of where they work. The book also covers key issues in relation to providing care, such as inclusivity, ethics, legal issues, and health inequalities. Key features:
- Fully mapped to the new NMC standards of proficiency for nursing associates (2018)
- Case studies, activities and other learning features help TNAs understand the theory and apply it to practice
- Designed around a Nursing Associate course, this book demonstrates how person-centred care feeds into each core module
ABOUT THE SERIES: The Understanding Nursing Associate Practice series (UNAP) is a new collection of books uniquely designed to support trainee Nursing Associates throughout their training and into a professional career.
I am thrilled to see this text written specifically for Nursing Associates. Aligning to the NMC Standards of Proficiency and with reference to a wide variety of patient/client considerations across the lifespan, this is an invaluable read for any Nursing Associate student embarking on their educational journey.
Developing the Nursing Associate Programme at the moment and looking at all resources to support the modules.
Excellent book. Pity the e-version is only available through a hefty subscription.
This book presents a comprehensive, culturally appropriate view of person centred care. It is easy to understand and written at a level that is relevant to the learning needs of Nursing Associate students. The examples used are applicable to practice and correlated to the NMC Code of Conduct. A very useful book for students to use for their essay and for classroom discussion. One of the biggest selling point of the book is, it can be easily understood by readers who are not native English speakers.
Clear language that students will understand. Linked well to NMC standards and gives context with case studies
Students from a range of backgrounds can relate to this text and the practical scenarios within
Good basic information, however use of Mind Tools as a reference source has undermined adoption; we discourage apprentices from using on-line sources that may not be academically robust. Liked the mapping to the NMC standards for Nursing Associate but would have been enhanced by also mapping the apprenticeship standard (Ofsted requires integration into curriculum)..
Preview this book
For instructors.
Please select a format:
Select a Purchasing Option
- Electronic Order Options VitalSource Amazon Kindle Google Play eBooks.com Kobo

Related Products


COMMENTS
A person-centered strategy in nursing concerns patients being actively involved in the health care process. Person-centered care can be defined as an approach that takes into consideration "a person's context and individual expression, preferences, and beliefs" (Santana et al., 2018, p. 430). Furthermore, it involves other stakeholders in ...
The relevance of the papers and the quality of the reviews/articles themselves was appraised. All articles were appraised against the aims of this review. Following this, a total of 17 articles were included in the final review. ... Defining Person-Centred Care in Nursing; An Integrative Review. The valuable feedback has been considered and ...
Introduction: Reflective essay on person centred care. Modern day Healthcare has increasingly embraced concepts of client-centred practice and empowerment. However, Taylor (2003) posits that existing literature on the subject does not give clear and unambiguous descriptions of the ways by which nurses can empower clients.
Person-centred care means treating patients as individuals and as equal partners in the business of healing; it is personalised, coordinated and enabling. 1 It is not a medical model and should be regarded as multidisciplinary, recognising that a person may need more than one professional to support them. Working in this way means recognising ...
A person-centered care philosophy is uniquely supported by Jean Watson's definition of nursing and the ten carative factors that she identified in her theory of nursing. Watson defined nursing as, "a human science of persons and human health-illness experiences mediated by professional, personal, scientific, esthetic and ethical human ...
Access to care (O1) is defined as the system's capacity to provide care efficiently after a need is recognized, as well as costs associated with receiving care. 97 A person‐centred access model acknowledges the structures that may result in physical or financial barriers, as well as or other determinants of health‐care access; 97 it can ...
Aim The aims of this literature review were to better understand the current literature about person-centred care (PCC) and identify a clear definition of the term PCC relevant to nursing practice. Method/Data sources An integrative literature review was undertaken using The Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, Scopus and Pubmed databases. The limitations ...
The notion of patient-centeredness has been in the literature since the mid-20th century or earlier. For example, in 1960, the patient-centered approach was considered "a trend in modern nursing practice . . . gradually replacing the procedure-centered approach . . . as the prime concern of the nurse" (Hofling & Leininger, 1960, pp. 4-5).). Madeleine Leininger, a prominent nurse theorist ...
Person-centered care is holistic, individualized, just, respectful, compassionate, coordinated, evidence-based, and developmentally appropriate. Person-centered care builds on a scientific body of knowledge that guides nursing practice regardless of specialty or functional area. Contextual Statement: Person-centered care is the core purpose of ...
Introduction: Reflective essay on person centred care. Modern day Healthcare has increasingly embraced concepts of client-centred practice and empowerment. However, Taylor (2003) posits that existing literature on the subject does not give clear and unambiguous descriptions of the ways by which nurses can empower clients.
The Person-centred Nursing Framework was derived from two original doctoral studies. McCormack's study aimed to explore the meaning of autonomy for older people in hospital settings and used a qualitative research approach guided by the hermeneutic philosophy described by Gadamer [].This resulted in a conceptual framework for person-centred practice with older people referred to by McCormack ...
The term 'person-centred care' is used frequently in healthcare policy and practice. However, the ways in which the concept is translated into everyday nursing care continue to present a challenge. Person-centred care has been explored extensively within the care of older people, people with dementia and people with a learning disability.
A patient journey (PJ) is the ensemble of care events organized by time across all diagnoses and providers to improve or maintain health for one patient. The PJ is the HCS core product [ 4 ]. There are three roles in every PJ: the patient, the professional (s) and a governance/payer, hereafter 'the PJ partners.'.
A person-centered care and communication continuum (PC4 Model) is thus proposed to orient healthcare professionals to care practices, discourse contexts, and communication contents and forms that can enhance or impede the acheivement of patient-centered care in clinical practice. ... In nursing care, patient-centered care or person-centered ...
Introduction Person-centred care has become internationally recognised as a critical attribute of high-quality healthcare. However, the concept has been criticised for being poorly theorised and operationalised. Serious illness is especially aligned with the need for person-centredness, usually necessitating involvement of significant others, management of clinical uncertainty, high-quality ...
This article discusses the important concept of person-centred care and how this can be achieved. Following an introduction defining what is meant by this term and contrasting it with the term patient-centred care, the relevant and pertinent parts of the Nursing and Midwifery Council code will then be identified and discussed. The four principles of person-centred care will then be presented ...
This article is a bite-size summary of the concept of person-centred care. It is the first article in a six-part series on nursing theoriesand their implications for practice. Citation:Chapman H(2017) Nursing theories 1: person-centred care. Nursing Times[online]; 113: 10, 59. Author:Hazel Chapman is postgraduate tutor, University of Chester.
Development of Person Centred Nursing Care. The aim of this essay is to describe the history of person-centred care, explain why person-centred approach is important in healthcare environment and how it is achieved. This essay will also explain the concept of a person-centeredness, the concepts of a person and personhood and the issues arising ...
Video. In this animation we look at person-centred care. Kindness and respect mean different things to different people. That's why it matters to be person-centred. Being person-centred means thinking about what makes each person unique, and doing everything you can to put their needs first. This animation supports nurses, midwives and ...
a detailed person centered care approach essay within your reflection describe the episode of care and how you assessed, planned, delivered and evaluated care. Skip to document. ... Introduction to Adult Nursing (4NH009) 45 Documents. Students shared 45 documents in this course. University University of Wolverhampton. Academic year: 2021/2022 ...
Evaluation of person‐centred and relationship‐centred care interventions focus on both the measurement of person/patient outcomes, as well as those for the nurse, wider team and family. Evaluations of specific interventions are often framed within a disease or condition specific setting (for example, dementia).
1 INTRODUCTION. Since the early 2000s, emphasis on patient- and family-centred care (PFCC) has been increasing in a variety of health care settings, spinning from paediatric to health care facilities for adults and older adults. 1, 2 Supported by literature that PFCC improves patient and family experiences, this approach has been broadly embraced by health care institutions. 3 Aligned with ...
Person-centred care has become internationally recognised as a dimension of high-quality healthcare. 1 The Institute of Medicine describes quality care as that which is: "safe, effective, patient-centred, efficient, timely and equitable". 2 WHO policy on people‐centred healthcare highlights person‐centredness as a core competency of ...
First edition. Understanding how to deliver effective, person-centred care is vital for a future career as a Nursing Associate. In this book, trainee nursing associates are introduced to the principles of person-centred care, with case studies from a variety of healthcare settings and guidance on caring for different patient groups, from acute ...