

Enter a Search Term
Fda approves first-of-its-kind glaucoma treatment.
- Research News
Reviewed by Preeti Subramanian, PhD
The U.S. Food and Drug Administration has approved a new treatment for glaucoma, iDose® TR (travoprost intracameral implant, 75 mcg). iDose TR is a first-of-its kind treatment that is designed to provide up to three years of 24/7, continuous drug therapy directly inside the eye, helping people with glaucoma take control over the elevated eye pressure associated with this vision disease.
It is the first eye implant to deliver medication 24/7 for an extended period of time. Another FDA-approved implant, Durysta, is biodegradable and dissolves after six months.
Glaucoma is a group of diseases that cause damage to the optic nerve, a bundle of more than one million nerve fibers that carry visual information from the eye to the brain. The most common form of glaucoma, open angle glaucoma, is caused by increased pressure in the eye.
If left untreated, glaucoma can cause permanent damage to the eye, which means vision loss cannot be reversed. Prescription eye drops are the most common treatment for glaucoma, but they can be difficult to administer correctly and can cause uncomfortable or irritating side effects. High rates of non-compliance and non-adherence to prescription medications contribute to disease progression.
iDose TR treats glaucoma by automatically releasing the same type of medication used for decades in the most commonly prescribed eye drops. After 12 months of a clinical study, 81% of people were able to eliminate the burden of taking daily eye drops.
“BrightFocus welcomes the approval of iDose as a new option for people with glaucoma to take control of their treatment,” said BrightFocus President and CEO Stacy Pagos Haller. “By potentially reducing the need for daily eye drops, this new treatment offers an improved treatment for the three million Americans living with glaucoma.”
The manufacturer, Glaukos, expects iDose TR to be available in the first quarter of 2024. View the full press release for more details.
iDose delivers a class of drugs called prostaglandin analogs, which reduce pressure in the eye by increasing the outward flow of fluid from the eye. In 2004, BrightFocus' National Glaucoma Research program funded research exploring the mechanism behind how prostaglandin analogs reduce eye pressure, improving scientists' ability to understand how this class of drugs works.
BrightFocus has invested nearly $100 million in vision research worldwide on the causes and potential prevention and treatment of glaucoma and macular degeneration. BrightFocus Foundation’s National Glaucoma Research program has funded breakthrough studies that have led to a better understanding of the disease and novel treatments. Learn more.
Explore more:
Glaucoma Treatment Guide
Listen: New Frontiers in Glaucoma Surgeries
Glaucoma in the African American and Hispanic Communities
About BrightFocus
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Through its flagship research programs — Alzheimer’s Disease Research, National Glaucoma Research, and Macular Degeneration Research — the Foundation has awarded nearly $290 million in groundbreaking research funding over the past 50 years and shares the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org .
The information provided in this section is a public service of BrightFocus Foundation, should not in any way substitute for the advice of a qualified healthcare professional, and is not intended to constitute medical advice. Although we make efforts to keep the medical information on our website updated, we cannot guarantee that the information on our website reflects the most up-to-date research.
Please consult your physician for personalized medical advice; all medications and supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical product or therapy.
Don’t miss out.
Receive glaucoma breakthrough news, research updates, and inspiring stories.
A new treatment for glaucoma?
- Feinberg School of Medicine
- Global Health
A Northwestern Medicine study in mice has identified new treatment targets for glaucoma, including preventing a severe pediatric form of glaucoma, as well as uncovering a possible new class of therapy for the most common form of glaucoma in adults.
In people with high pressure glaucoma, fluid in the eye doesn’t properly drain and builds up pressure on the optic nerve, leading to vision loss. It affects 60 million people worldwide and is the most common cause of blindness in people over 60 years old.
While there are a few treatments available for open angle glaucoma, the most common form of glaucoma in adults (eye drops, oral medication, laser treatments), there are no cures, and a severe form of glaucoma in children between birth and three years old known as primary congenital glaucoma can only be treated with surgery.
“Although primary congenital glaucoma is much rarer than open angle glaucoma , it is devastating for children,” said corresponding author Dr. Susan Quaggin , chief of nephrology and hypertension in the Department of Medicine at Northwestern University Feinberg School of Medicine. “New treatments and new classes of treatments are urgently needed to slow vision loss in both forms.
Using gene editing, the scientists in the study developed new models of glaucoma in mice that resembled primary congenital glaucoma. By injecting a new, long-lasting and non-toxic protein treatment (Hepta-ANGPT1) into mice, the scientists were able to replace the function of genes that, when mutated, cause glaucoma. With this injectable treatment, the scientists also successfully prevented glaucoma from ever forming in one model. This same therapy, when injected into the eyes of healthy adult mice, reduced pressure in the eyes, supporting it as a possible new class of therapy for the most common cause of glaucoma in adults (high intraocular pressure open angle glaucoma).
The study, “Cellular crosstalk regulates the aqueous humor outflow pathway and provides new targets for glaucoma therapies,” was published Oct. 18 in the journal Nature Communications.
60 million people worldwide are affected by glaucoma
The next step is to develop the appropriate delivery system for the successful new protein treatment in patients and bring it to production, Quaggin said.
Additionally, the scientists used bioinformatics and single cell RNA sequence data to understand and identify glaucoma pathways that can be explored in the future for additional therapeutic targets for the disease, such as ones that regulate communication with a specialized blood vessel in the eye (Schlemm’s canal) that is important for draining fluid and maintaining normal eye pressure.
“Having a treatment that can promote remodeling and/or growth of a defective Schlemm’s canal to treat glaucoma would be fantastic,” Quaggin said. “These studies are the first step to that goal.
“Our hope is that this study leads to the first targeted therapy that effectively promotes (aqueous humor) fluid outflow from the front of an eye, reversing the underlying biologic defect in patients with glaucoma.”
Other Northwestern co-authors are Ben Thompson (first), Dr. Jing Jin , Pan Liu and medical student Raj Purohit. This study builds on major teamwork and an ongoing collaboration with University of Madison-Wisconsin co-authors Terri Young and Stuart Thomson.
Funding for the study was provided by the National Eye Institute (grant numbers R01 EY025799, P30 EY016665 and R01 EY014685), the National Heart, Lung and Blood Institute (grant number R01 HL124120), the National Institutes of Health Office of the Director (grant number 1S10OD025120), the National Institute of Diabetes and Digestive and Kidney Diseases (grant number P30 DK114857), the National Cancer Institute (grant number CCSG P30 CA060553), and Research to Prevent Blindness.
Editor’s Picks

This algorithm makes robots perform better
‘the night watchman’ named next one book selection, six northwestern faculty elected to american academy of arts and sciences, related stories.

Less than one in five youth received mental health services they needed 16 years after detention
Ready for this summer’s cicada noise, tech can’t replace human coaches in obesity treatment.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

Had a bad experience meditating? You’re not alone.

Families may remove brain-injured patients from life support too soon

What to do about mental health crisis among Black males
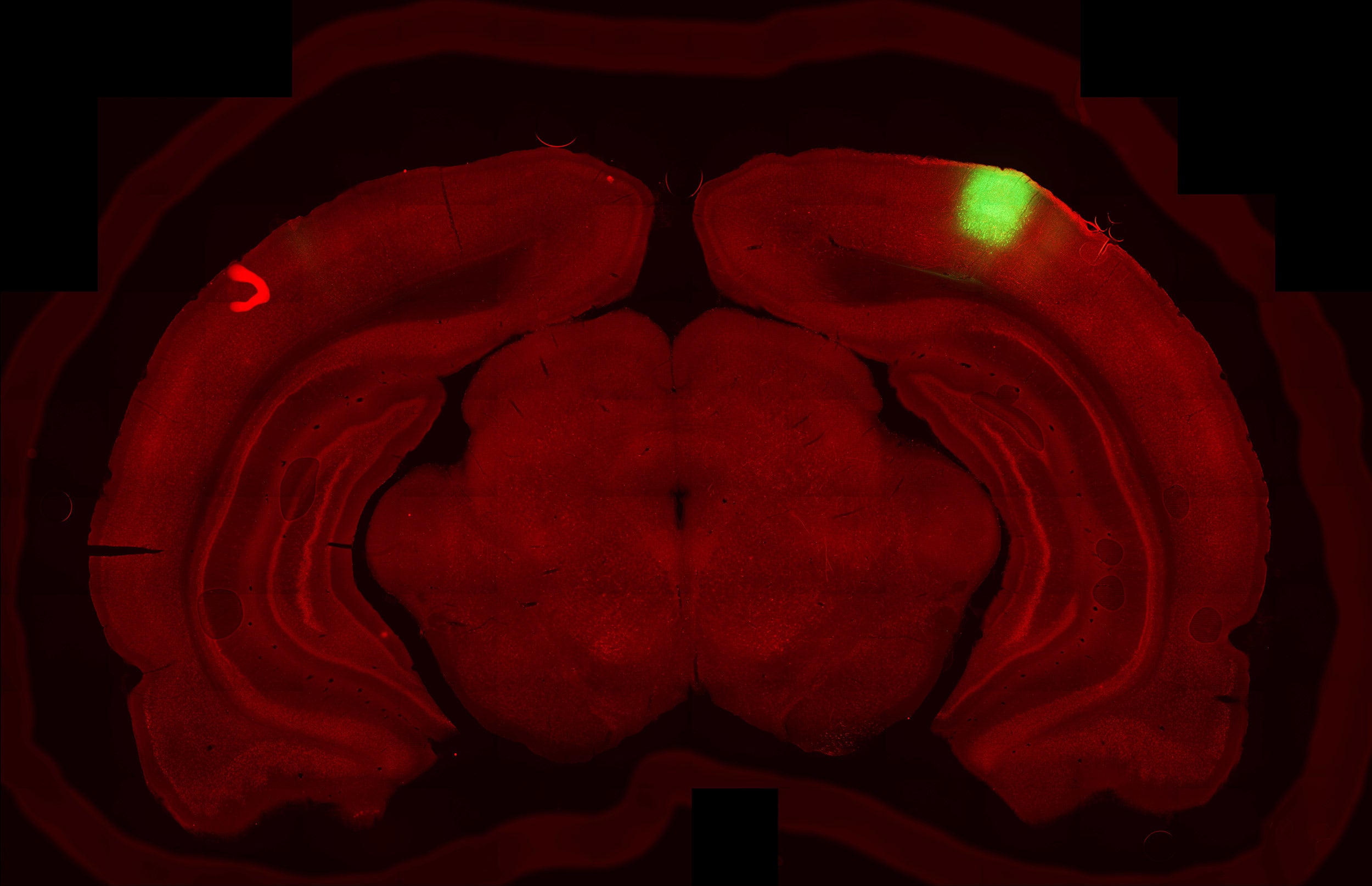
Researchers at HMS have successfully restored vision loss and reversed glaucoma-induced damage in mice.
Credit: Sinclair Lab/Harvard Medical School
Seeing clearly again
Ryan Jaslow
MEEI Communications
Harvard Medical School scientists reverse age-related vision loss, eye damage from glaucoma in mice
Harvard Medical School scientists report they have successfully restored vision in mice by turning back the clock on aged eye cells in the retina to recapture youthful gene function.
The team’s work, described Dec. 2 in the publication Nature, represents the first demonstration that it may be possible to safely reprogram complex tissues, such as the nerve cells of the eye, to an earlier age.
In addition to resetting the cells’ aging clock, the researchers successfully reversed vision loss in animals with a condition mimicking human glaucoma, a leading cause of blindness around the world.
The achievement represents the first successful attempt to reverse glaucoma-induced vision loss, rather than merely stem its progression, the team said.
If replicated through further studies, the approach could pave the way for therapies to promote tissue repair across various organs and reverse aging and age-related diseases in humans.
“Our study demonstrates that it’s possible to safely reverse the age of complex tissues such as the retina and restore its youthful biological function,” said senior author David Sinclair, professor of genetics in the Blavatnik Institute at Harvard Medical School, co-director of the Paul F. Glenn Center for Biology of Aging Research at HMS and an expert on aging.
Sinclair and colleagues caution that the findings remain to be replicated in further studies, including in different animal models, before any human experiments. Nonetheless, they add, the results offer a proof of concept and a pathway to designing treatments for a range of age-related human diseases.
“If affirmed through further studies, these findings could be transformative for the care of age-related vision diseases like glaucoma and to the fields of biology and medical therapeutics for disease at large,” Sinclair said.
“At the beginning of this project, many of our colleagues said our approach would fail or would be too dangerous to ever be used. Our results suggest this method is safe and could potentially revolutionize the treatment of the eye and many other organs affected by aging.” Yuancheng Lu, lead study author
For their work, the team used an adeno-associated virus (AAV) as a vehicle to deliver into the retinas of mice three youth-restoring genes — Oct4, Sox2, and Klf4 — that are normally switched on during embryonic development. The three genes, together with a fourth one, which was not used in this work, are collectively known as Yamanaka factors.
The treatment had multiple beneficial effects on the eye. First, it promoted nerve regeneration following optic-nerve injury in mice with damaged optic nerves. Second, it reversed vision loss in animals with a condition mimicking human glaucoma. And third, it reversed vision loss in aging animals without glaucoma.
The team’s approach is based on a new theory about why we age. Most cells in the body contain the same DNA molecules but have widely diverse functions. To achieve this degree of specialization, these cells must read only genes specific to their type. This regulatory function is the purview of the epigenome, a system of turning genes on and off in specific patterns without altering the basic underlying DNA sequence of the gene.
This theory postulates that changes to the epigenome over time cause cells to read the wrong genes and malfunction — giving rise to diseases of aging. One of the most important changes to the epigenome is DNA methylation, a process by which methyl groups are tacked onto DNA. Patterns of DNA methylation are laid down during embryonic development to produce the various cell types. Over time, youthful patterns of DNA methylation are lost, and genes inside cells that should be switched on get turned off and vice versa, resulting in impaired cellular function. Some of these DNA methylation changes are predictable and have been used to determine the biologic age of a cell or tissue.
Yet, whether DNA methylation drives age-related changes inside cells has remained unclear. In the current study, the researchers hypothesized that if DNA methylation does, indeed, control aging, then erasing some of its footprints might reverse the age of cells inside living organisms and restore them to their earlier, more youthful state.
Past work had achieved this feat in cells grown in laboratory dishes but fell short of demonstrating the effect in living organisms.
The new findings demonstrate that the approach could be used in animals as well.
Overcoming an important hurdle
Lead study author, Yuancheng Lu , research fellow in genetics at HMS and a former doctoral student in Sinclair’s lab, developed a gene therapy that could safely reverse the age of cells in a living animal.
Lu’s work builds on the Nobel Prize winning discovery of Shinya Yamanaka, who identified the four transcription factors, Oct4, Sox2, Klf4, c-Myc, that could erase epigenetics markers on cells and return these cells to their primitive embryonic state from which they can develop into any other type of cell.
Subsequent studies, however, showed two important setbacks. First, when used in adult mice, the four Yamanaka factors could also induce tumor growth, rendering the approach unsafe. Second, the factors could reset the cellular state to the most primitive cell state, thus completely erasing a cell’s identity.
Lu and colleagues circumvented these hurdles by slightly modifying the approach. They dropped the gene c-Myc and delivered only the remaining three Yamanaka genes, Oct4, Sox2, and Klf4. The modified approach successfully reversed cellular aging without fueling tumor growth or losing their identity.
Gene therapy applied to optic nerve regeneration
In the current study, the researchers targeted cells in the central nervous system because it is the first part of the body affected by aging. After birth, the ability of the central nervous system to regenerate declines rapidly.
To test whether the regenerative capacity of young animals could be imparted to adult mice, the researchers delivered the modified three-gene combination via an AAV into retinal ganglion cells of adult mice with optic nerve injury.
For the work, Lu and Sinclair partnered with Zhigang He , HMS professor of neurology and of ophthalmology at Boston Children’s Hospital, who studies optic nerve and spinal cord neuro-regeneration.
The treatment resulted in a two-fold increase in the number of surviving retinal ganglion cells after the injury and a five-fold increase in nerve regrowth.
“At the beginning of this project, many of our colleagues said our approach would fail or would be too dangerous to ever be used,” said Lu. “Our results suggest this method is safe and could potentially revolutionize the treatment of the eye and many other organs affected by aging.”
Reversal of glaucoma and age-related vision loss
More like this.

Focusing on the fovea
Linking sight and movement
Making sense of how the blind ‘see’ color
Following the encouraging findings in mice with optic nerve injuries, the team partnered with colleagues at Schepens Eye Research Institute of Massachusetts Eye and Ear Bruce Ksander , HMS associate professor of ophthalmology, and Meredith Gregory-Ksander , HMS assistant professor of ophthalmology. They planned two sets of experiments: one to test whether the three-gene cocktail could restore vision loss due to glaucoma and another to see whether the approach could reverse vision loss stemming from normal aging.
In a mouse model of glaucoma, the treatment led to increased nerve cell electrical activity and a notable increase in visual acuity, as measured by the animals’ ability to see moving vertical lines on a screen. Remarkably, it did so after the glaucoma-induced vision loss had already occurred.
“Regaining visual function after the injury occurred has rarely been demonstrated by scientists,” Ksander said. “This new approach, which successfully reverses multiple causes of vision loss in mice without the need for a retinal transplant, represents a new treatment modality in regenerative medicine.”
The treatment worked similarly well in elderly, 12-month-old mice with diminishing vision due to normal aging. Following treatment of the elderly mice, the gene expression patterns and electrical signals of the optic nerve cells were similar to young mice, and vision was restored. When the researchers analyzed molecular changes in treated cells, they found reversed patterns of DNA methylation — an observation suggesting that DNA methylation is not a mere marker or a bystander in the aging process, but rather an active agent driving it.
“What this tells us is the clock doesn’t just represent time — it is time,” said Sinclair. “If you wind the hands of the clock back, time also goes backward.”
The researchers said that if their findings are confirmed in further animal work, they could initiate clinical trials within two years to test the efficacy of the approach in people with glaucoma. Thus far, the findings are encouraging, researchers said. In the current study, a one-year, whole-body treatment of mice with the three-gene approach showed no negative side effects.
Other authors on the paper include Benedikt Brommer, Xiao Tian, Anitha Krishnan, Margarita Meer, Chen Wang, Daniel Vera, Qiurui Zeng, Doudou Yu, Michael Bonkowski, Jae-Hyun Yang, Songlin Zhou, Emma Hoffmann, Margarete Karg, Michael Schultz, Alice Kane, Noah Davidsohn, Ekaterina Korobkina, Karolina Chwalek, Luis Rajman, George Church, Konrad Hochedlinger, Vadim Gladyshev, Steve Horvath, and Morgan Levine.
This work was supported in part by a Harvard Medical School Epigenetics Seed Grant and Development Grant, The Glenn Foundation for Medical Research, Edward Schulak, the National Institutes of Health (grants R01AG019719,R37AG028730, R01EY026939, R01EY021526, R01AG067782, R01GM065204, R01AG065403, R01EY025794, R24EY028767 and R21EY030276), and the St. Vincent de Paul Foundation.
Share this article
You might like.
Altered states of consciousness through yoga, mindfulness more common than thought and mostly beneficial, study finds — though clinicians ill-equipped to help those who struggle

Of the survivors within one study group, more than 40% recovered at least some independence.

Symposium examines thorny, multifaceted dilemma from systemic racism in policing, healthcare to stigma attached to psychotherapy in community
Six receive honorary degrees
Harvard recognizes educator, conductor, theoretical physicist, advocate for elderly, writer, and Nobel laureate
Five alumni elected to the Board of Overseers
Six others join Alumni Association board
Everything counts!
New study finds step-count and time are equally valid in reducing health risks
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Mayo Clin Proc Innov Qual Outcomes
- v.6(6); 2022 Dec
Updates on the Diagnosis and Management of Glaucoma
Glaucoma is the leading cause of blindness throughout the world (after cataracts); therefore, general physicians should be familiar with the diagnosis and management of affected patients. Glaucomas are usually categorized by the anatomy of the anterior chamber angle (open vs narrow/closed), rapidity of onset (acute vs chronic), and major etiology (primary vs secondary). Most glaucomas are primary (ie, without a contributing comorbidity); however, several coexisting ophthalmic conditions may serve as the underlying etiologies of secondary glaucomas. Chronic glaucoma occurs most commonly; thus, regular eye examinations should be performed in at-risk patients to prevent the insidious loss of vision that can develop before diagnosis. Glaucoma damages the optic nerve and retinal nerve fiber layer, leading to peripheral and central visual field defects. Elevated intraocular pressure (IOP), a crucial determinant of disease progression, remains the only modifiable risk factor; thus, all current treatments (medications, lasers, and operations) aim to reduce the IOP. Pharmacotherapy is the usual first-line therapy, but noncompliance, undesirable adverse effects, and cost limit effectiveness. Laser and surgical treatments may lower IOP significantly over long periods and may be more cost effective than pharmacotherapy, but they are plagued by greater procedural risks and frequent treatment failures. Traditional incisional procedures have recently been replaced by several novel, minimally invasive glaucoma surgeries with improved safety profiles and only minimal decreases in efficacy. Minimally invasive glaucoma surgeries have dramatically transformed the surgical management of glaucoma; nevertheless, large, randomized trials are required to assess their long-term efficacy.
Article Highlights
- • Glaucoma, a leading cause of blindness throughout the world, presents with an open or closed anterior chamber angle, structural damage to the optic nerve (seen in all stages), and visual field defects (seen in later stages). Glaucoma may be asymptomatic until the late stages, thereby emphasizing the need for general physicians to understand important diagnostic criteria and management options.
- • The progression of glaucoma is mitigated by lowering the intraocular pressure, which is done with topical medications, laser procedures, or incisional operations.
- • Minimally invasive glaucoma surgery, with a favorable safety profile and efficacy that rivals traditional incisional procedures, has transformed glaucoma care.
Glaucoma can be defined as a progressive optic neuropathy that induces optic disc cupping and retinal ganglion cell apoptosis. 1 As the world’s leading cause of irreversible blindness, the disease currently affects 3.5% of individuals aged between 40 and 80 years. The incidence of glaucoma is increasing, together with life expectancies, in resource-limited countries, and nearly 112 million people are expected to be affected by 2040. 1 , 2 Early detection can slow disease progression, but because visual field loss may be asymptomatic until the late stages, a timely diagnosis is frequently delayed. 3 Common risk factors for glaucoma include advancing age, a positive family history, race (non-Caucasian), and elevated intraocular pressure (IOP). 4 , 5 Once diagnosed with glaucoma, most patients require lifelong care.
Aqueous humor is produced by the ciliary body, and after percolating through the posterior chamber, around the lens, and through the pupil, it exits the eye through the semiporous trabecular meshwork (TM) in the iridocorneal angle of the anterior chamber. Aqueous humor then flows into the circumferential vascular collection duct (Schlemm canal) and leaves the eye through the distal collector channels that drain into the episcleral venous system. 6 , 7 , 8 A detailed anatomical view of the anterior eye segment and the aqueous outflow pathway is displayed in Figure 1 . The pathogenesis of glaucoma includes inadequate drainage of aqueous humor because of increased resistance through the meshwork 7 or occlusion of the angle, 9 both of which elevate the IOP. Elevated IOP contributes to an irreversible, progressive ocular neuropathy characterized by retinal ganglion cell apoptosis. 1 Patients with elevated IOP without other signs of glaucoma are said to have ocular hypertension, and those with optic disc enlargement but normal IOP and no other signs of glaucoma are classified as glaucoma suspects.

Ultrasound biomicroscopy (UBM) of the anterior eye segment. A, UBM shows the ciliary zonules (CZ), ciliary body (CB), sclera (S), cornea (C), anterior chamber (AC), posterior chamber (PC), and lens (L). The anterior chamber angle (ACA) is indicated by the arrow. B, Magnified UBM of the ACA shows the trabecular meshwork (TM), Schlemm canal (SC), and collector channels (CCs).
The risk factors and pathogenesis that underly glaucoma have been well described in the literature; however, the biological basis of the disease remains incompletely understood. The biomechanical and vascular theories of glaucoma propose that elevated IOP compromises axonal integrity at the optic nerve head (ONH), which leads to ganglion cell apoptosis. 5 The biomechanical theory posits that abnormally narrow scleral fenestrations at the ONH limit axoplasmic flow, 5 , 7 , 10 whereas the vascular theory states that decreased perfusion pressure leads to hypoxia and ischemic damage of the ONH. 5 , 7 , 11 Both theories include IOP as a risk factor; however, one-third of patients with glaucoma have normal IOPs (normal tension glaucoma). 5 Glaucoma has been associated with Alzheimer disease 12 and a loss of cognitive function, 13 which suggests that neurodegeneration may contribute to the pathogenesis. 5 However, despite the different pathogenetic theories, elevated IOP consistently contributes to disease progression and remains the only treatable risk factor. 5 , 7
The goal of glaucoma treatment is to lower IOP with medications, laser procedures, and/or operation. First-line therapy is usually pharmacotherapy, with laser and surgical procedures added for further IOP reduction in eyes with inadequate initial responses. Incisional operations consist of filtration procedures (eg, trabeculectomy) or tube shunt implantation, both of which reroute aqueous humor flow past the damaged angle into the subconjunctival space forming a filtration bleb. 14
Traditional incisional operations lower the IOP effectively; however, complication rates, including scar tissue proliferation, endophthalmitis, and conjunctival hemorrhage, are high. The IOP-lowering effect often decreases over time, which results in high 5-year reoperation rates (trabeculectomy, 15.1%; tube shunt implantation, 14.0%; EX-PRESS shunt, 18.3%). 15 , 16 , 17 These high reoperation rates speak to the need for procedures that increase conventional aqueous outflow while protecting the conjunctiva from surgical manipulation. This has led to the development of several conjunctival sparing, minimally invasive glaucoma surgeries (MIGSs) for the treatment of primary open-angle glaucoma (POAG). Minimally invasive glaucoma surgeries do not reduce IOP as well as traditional filtering procedures, but they have excellent safety profiles. 18
We believe that because of the expanding treatment options and increasing worldwide prevalence of glaucoma, an updated commentary on glaucoma and its treatment options is important for medical physicians. In this article, we provide a comprehensive updated review of the diagnosis and management of adult glaucoma through 2022.
A broad literature search with no time frame was carried out in PubMed with the following key words: “glaucoma prevalence,” “glaucoma risk factors,” “glaucoma diagnosis,” “glaucoma management,” “open-angle glaucoma,” angle-closure glaucoma,” “secondary glaucoma,” “tonometry,” “glaucoma medication,” “conventional aqueous outflow,” “unconventional aqueous outflow,” “glaucoma laser procedures,” “trabeculectomy,” “glaucoma tube shunt surgery,” and “minimally invasive glaucoma surgery.” Identified articles and their references were scrutinized, and those relevant to the subject matter were selected.
Diagnosis of Glaucoma
Types of glaucoma.
Glaucoma may be broadly categorized as open-angle glaucoma (OAG) and angle-closure glaucoma (ACG). Primary OAG and primary ACG are seen most frequently; however, several ocular conditions cause secondary glaucomas ( Table 1 ).
Table 1
Common Glaucoma Types are Listed According to Whether the Anterior Chamber Angle is Open or Closed a
Most eyes with glaucoma have diminished conventional aqueous outflow despite a normal gonioscopic appearance of the iridocorneal angle. These OAGs are slowly progressive optic neuropathies in which ONH cupping gradual increases and peripheral visual field loss develops. 15 , 19 The most common type of glaucoma—the POAG—affects 74% of patients with glaucoma. 20 Outflow resistance may be modulated by hydrodynamic pore-substrate interactions within the inner wall of the Schlemm canal, and patients with POAG have been found to have reduced pore density. 21
Several types of secondary OAG occur much less frequently than POAG. Pigmentary glaucoma occurs when friction between the lens zonules and iris pigment epithelium releases pigment granules that lodge in the TM and increase outflow resistance. 22 , 23 Exfoliative glaucoma, the most common form of secondary OAG, occurs when microscopic clumps of protein fibers are synthesized within the eye and clog the TM. 24 Exfoliation material has also been found in the heart, kidney, liver, and lungs. 24 , 25 Other forms of secondary OAG include uveitic and traumatic glaucomas, 26 , 27 , 28 use of ocular or systemic corticosteroids, 29 and antineoplastic drugs. 30 Increased episcleral venous pressure due to conditions such as carotid-cavernous sinus fistulas may cause OAG. 31
Angle-closure glaucomas are rapidly progressive ocular neuropathies characterized by the occlusion of at least 270° of the iridocorneal angle. 3 Angle-closure glaucomas are only one-third as common as OAGs; however, they are responsible for approximately 50% of all glaucoma-induced blindness. Primary ACG, which arises from pupillary block (appositional closure of the iridocorneal angle that results from an increasing pressure differential between the anterior and posterior chambers of the eye 32 ) or plateau iris (an anteriorly positioned ciliary body that causes contact between the iris and TM with resultant angle crowding 33 ), has a global prevalence of 0.6%. 3 , 34 , 35 Primary ACG occurs most frequently in women, Asians, people with hypermetropic (short) eyes and people with shallow anterior chambers. 34 Affected patients require urgent treatment (usually laser iridotomy) to reverse obstruction of the angle. 34
Several secondary types of ACG are seen. Neovascular glaucoma, new blood vessels that occlude the angle, may develop from central retinal vein occlusion or diabetic retinopathy and generally carries a poor visual prognosis. 1 , 36 Phacomorphic glaucoma involves angle-closure because of lens intumescence (advanced cataract), and cataract removal typically leads to good visual recovery. 37 Angle-closure may be caused by corneal endothelium abnormalities (eg, iridocorneal endothelium syndromes) 38 or large iris or ciliary body masses. 39 Several medications, including anticholinergics, may precipitate ACG in eyes with preexisting narrow angles. 1 , 40
Differentiating between OAG and ACG is usually done via gonioscopic examination with slit lamp viewing. 41 Gonioscopy has long been the gold standard for visualizing the anterior chamber angle (ACA); however, challenges, including lens-eye contact, lack of objective measurements, a steep learning curve, and inconsistent interpretations between physicians, exist. 41 , 42 Advanced ACA imaging techniques including swept-source optical coherence tomography (OCT), goniophotography systems, and deep learning algorithms have been developed to overcome the limitations of gonioscopy. 43
Examination
Approximately 50% of individuals in the resource-limited countries are unaware that they have glaucoma, underscoring the importance of patient awareness education in diagnosis and management. 3 , 44 , 45 The diagnosis of glaucoma involves risk assessment, measurement of visual acuity, IOP, and corneal thickness, OCT imaging of the retinal nerve fiber layer (RNFL) and ONH, and visual field testing. Because most patients with glaucoma are asymptomatic for years, it is recommended that those with risk factors (advanced age, family history, non-White race, high IOP, and steroid use) be referred to an eye care provider for a glaucoma assessment. 3 , 4 , 5
Intraocular pressure needs to be monitored regularly in patients at a high risk of developing glaucoma. It is commonly measured using rebound tonometry (iCare ic100; iCare) or the “gold standard” Goldmann applanation tonometry. The iCare tonometer measures IOP-dependent rebound velocity after brief corneal contact, whereas Goldmann applanation tonometry measures the force required to flatten a 3.06-mm diameter segment of the cornea. 46 Agreement in measurements is good between the 2 devices; however, the reliability of the iCare decreases at higher IOPs and with thicker central corneas. 47 , 48 , 49 Normal IOP ranges from 11 to 21 mm Hg 50 ; however, IOP should be evaluated with consideration of optic nerve defects and/or high central cornea values. 51 Up to 50% of glaucomatous eyes have normal IOP measurements, 3 , 52 which emphasizes the importance of performing additional diagnostic imaging when indicated.
Making the diagnosis of glaucoma, particularly at an early stage, can be difficult because there is no uniform standard for diagnosis. 3 Structural changes of early glaucoma can be seen with OCT imaging of the optic nerve and macula, and functional changes in advanced glaucoma can be detected with visual field testing. Normal appearances of the ONH, RNFL, and visual field are shown in Figure 2 A, C, and E, respectively. All glaucomas are defined by ONH degeneration with disc excavation ( Figure 2 B) and RNFL thinning ( Figure 2 D). 53 Optic nerve head damage is characterized by thinning of the neuroretinal rim, usually in the superior and inferior quadrants, although the remainder of the ONH may remain pink with a normal neuroretinal rim. 3 , 53 Glaucomatous damage leads to retinal ganglion cell apoptosis, which can be seen as thinning between the internal limiting membrane and ganglion cell layer on OCT. 53 As glaucoma progresses, ONH and RNFL abnormalities cause visual field defects ( Figure 2 F). Visual field defects are often not observed in the early stages of glaucoma because peripheral vision and Snellen visual acuity are preserved until RNFL damage reaches an advanced stage. 51

Comparison of optic nerve head (ONH), retinal nerve fiber layer (RNFL), and visual fields in normal and glaucomatous eyes. A, Normal ONH with round, elevated ONH and a small central cup. B, Glaucomatous ONH with excavation and thinning of neuroretinal rim. C, Optical coherence tomography (OCT) examination shows normal RNFL thickness. D, OCT examination shows RNFL thinning in glaucomatous eyes. E, A full field in both eyes is shown. F, Abnormal visual field results in glaucomatous eyes are shown. The right eye field shows a superior altitudinal defect, moderate inferior arcuate defects, and a nasal step. The left eye field shows a superior paracentral defect with nasal step that splits fixation, an early inferior arcuate scotoma, and nasal step.
A general correlation between OCT imaging and visual field examination can be observed; however, there is no widely accepted method for comparing the two, 54 and diagnosing glaucoma is ultimately up to the discretion of the physician. Once glaucoma has been diagnosed, its severity must be categorized—typically as mild, moderate, or severe. Because all glaucoma types present with structural damage, most classification systems grade severity on the basis of functional visual field abnormalities. Most recently (2015), the International Classification of Diseases, Tenth Revision, released a grading system that associates mild glaucoma with a general absence of visual field defects, moderate glaucoma with visual field abnormalities in 1 hemifield (but outside 5° of fixation), and severe glaucoma with abnormalities in both hemifields and visual field loss within 5° of fixation. 55
Management of Glaucoma
Medical therapy.
Guidelines from the American Academy of Ophthalmology Preferred Practice Pattern (2020) state that an initial IOP reduction of 20%-30% is a suitable goal to slow disease progression, even in eyes with normal tension glaucoma. 56 The IOP must be carefully monitored during each follow-up visit, and the IOP control goal should be lowered further if progression continues. 56
Intraocular pressure–lowering medications have been the first-line therapy for most patients with glaucoma for several decades ( Table 2 ). Pharmacotherapy for glaucoma has evolved significantly over the past several decades with the introduction of topical carbonic anhydrase inhibitors (CAIs), beta blockers, prostaglandin analogs, and alpha agonists. 57 These medications have greater effectiveness and more favorable safety profiles than the older topical (pilocarpine) and systemic (oral CAIs) treatments. 57 In accordance with the generally accepted pharmacotherapy principles, the desired IOP range should be achieved with the fewest medications and least adverse effects. 3 Because of their tendency to induce glaucoma, ocular and systemic corticosteroids should be administered with caution in at-risk patients. 29
Table 2
US Food and Drug Administration–Approved Medications Used for the Treatment of Glaucoma
Prostaglandin analogs (PGAs) are the most commonly used medications for the treatment of OAG and ocular hypertension. Prostaglandin analogs compensate for decreased TM outflow by increasing outflow through the uveoscleral pathway, 58 where aqueous humor moves through the ciliary muscle into the supraciliary and suprachoroidal spaces. 59 Prostaglandin analogs are administered once daily, are well tolerated, and have limited systemic adverse effects. 3 , 58 The main ocular adverse effects are eyelash growth, iris pigmentation, and uveitis. 56 Because most PGAs do not target the primary outflow pathway (TM), concerns have been raised about their long-term efficacy. 57 The recently approved latanoprostene bunod 0.024% may target the TM rather than the uveoscleral pathway, 57 , 60 and compared with timolol 0.5% over 3 months of follow-up, it has superior IOP-lowering efficacy and a comparable safety profile. 57 , 61 , 62 Prostaglandin analogs are a significant improvement over cholinergic agonists (such as pilocarpine), which induce miosis and increase conventional outflow by decreasing outflow resistance. 63 Pilocarpine, a mainstay of glaucoma treatment in the 1970s and 1980s, needed to be administered 4 times per day, a difficult regimen to maintain, which contributed to its being supplanted by beta blockers and PGAs. 3
Both CAIs and beta blockers lower the IOP by targeting the aqueous humor production in the ciliary body. After topical administration, CAIs penetrate the cornea and reach the ciliary body epithelium, where they reduce the production of bicarbonate ions. 64 The CAIs (dorzolamide 2% and brinzolamide 1%) are administered 2 or 3 times daily, 64 but they are generally less effective than PGAs and beta blockers, which limits their use as first-line therapy. Systemic CAIs (methazolamide and acetazolamide) are highly effective, which makes them useful in the treatment of ACG; however, their use is limited by their high incidence of adverse effects that cause 50% of patients to become intolerant after 1 month.
Beta adrenergic antagonists (beta blockers) block the sympathetic nerve endings in the ciliary body epithelium, which decreases the production of aqueous. 65 Beta blockers may be nonselective or cardioselective (β1 selective), the latter of which is well tolerated in patients with asthma and chronic obstructive pulmonary disease. 65 The advantages of beta blockers include their relatively low cost and once-daily administration. 3 , 5 Topically administered beta blockers enter the venous circulation but escape the first-pass metabolism in the liver, which predisposes the patient to pulmonary (bronchial constriction) and cardiac (arrythmias) disturbances. 5 , 66 Systemic absorption can be lessened by eyelid closure or gentle punctal occlusion for 2 minutes after topical administration. 3
Topical alpha-adrenergic agonists (brimonidine and iopidine) reduce the IOP by decreasing the aqueous humor production and increasing the outflow. 3 They are administered 2 or 3 times daily and are usually used as second-line agents in combination with other drugs. A retrospective study found that combination treatment (CAI+PGA) was more prevalent in everyday practice than alpha-2 agonists + PGA, suggesting that the administration of alpha-2 agonists may be accompanied by more adverse effects. 67
Rho kinase inhibitors are a recently introduced medication class that uses a combined mechanism of increasing the conventional outflow and decreasing the episcleral venous pressure. 68 Netarsudil 0.02%, a rho kinase inhibitor approved by the US Food and Drug Administration in 2017, has IOP-lowering efficacy comparable with that of timolol 0.5%, but with more frequent adverse effects. 59 , 69 , 70
Pharmacotherapy is an effective short-term treatment strategy; however, limitations to long-term use include cost, adverse effects, and failure to reach the target IOP. Nonadherence to the administration schedule is another significant issue because fewer than half of the patients with glaucoma regularly use antiglaucoma medications as prescribed after 1 year. 5 , 71
Laser Therapy
When pharmacotherapy fails to achieve the target IOP and prevent vision loss, laser and surgical procedures are indicated. Laser procedures effectively lower the IOP and minimize the long-term costs that are associated with the long-term use of multiple pressure-lowering medications. 5 A variety of laser procedures can be performed in glaucomatous eyes, with the procedure of choice depending on the etiology of the disease ( Table 3 ).
Table 3
Laser Procedures for the Treatment of Glaucoma
IOP, intraocular pressure; LPI, laser peripheral iridotomy; TM, trabecular meshwork.
Laser trabeculoplasty and ab-interno excimer trabeculostomy (Glautec AG) are both indicated for OAG that is refractory to pharmacotherapy. Laser trabeculoplasty—multiple spots of thermal laser applied directly to the TM—induces favorable structural changes that increase the aqueous humor outflow. 72 Argon laser trabeculoplasty, developed in 1979, uses a with a blue-green continuous-wave laser (488 and 514 nm) to disrupt the TM, whereas selective laser trabeculoplasty (SLT), developed in 1995, uses low energy, brief duration, large spots from a green, frequency-doubled laser to target melanin-containing cells and spare the TM tissue. 73 Selective laser trabeculoplasty has largely supplanted argon laser trabeculoplasty because of its favorable safety profile, comparable IOP-lowering efficacy, and ability for repeated treatment applications. 74 More recently introduced laser trabeculoplasty procedures include titanium-sapphire laser trabeculoplasty and pattern scanning trabeculoplasty. Limited short-term data suggest that both the procedures have efficacy and safety profiles similar to that of SLT. 74 Laser trabeculoplasty procedures are generally preferred over operations because they are less invasive and possess better safety profiles. 3 , 74 Ab-interno excimer trabeculostomy is a MIGS similar to laser trabeculoplasty that uses a 308-nm XeCl excimer laser to create microperforations in the TM and inner wall of the Schlemm canal. 75 Excimer trabeculostomy has a comparable safety profile and IOP-lowering efficacy similar to SLT over 2 years. 75
Patients with ACG require different laser procedures from those with OAG. A laser peripheral iridotomy creates a hole in the peripheral iris and is often performed to eliminate pupillary block, 76 whereas a laser peripheral iridoplasty uses low-power laser burns to relieve appositional angle closure (by shrinking the peripheral iris) in cases where laser peripheral iridotomy is ineffective. 77 When combined, both treatments have been shown to be safe and effective in lowering the IOP in eyes with acute primary ACG refractory to pharmacotherapy. 78 For eyes refractory to all other medical, surgical, and laser therapies, a series of cyclodestructive procedures that damage the ciliary body epithelium and decrease the IOP by reducing the aqueous humor secretion may be the final treatment option. 79 These procedures consist of endoscopic cytophotocoagulation (Endo Optiks), continuous-wave diode laser (IRIDEX Corp), or the newest alternative, MicroPulse transscleral laser therapy (IRIDEX Corp), which selectively targets the pigmented tissue of the ciliary body epithelium. 79 Cyclodestructive procedures are also useful for the secondary forms of glaucoma, such as uveitic, traumatic, or neovascular glaucoma; however, these procedures come have considerable risks and are particularly difficult to titrate. 79
Surgical Treatment
Operations are usually performed when medical and laser treatments have failed to achieve adequate IOP reduction. Surgical options consist of the traditional, bleb-based IOP-lowering operations (trabeculectomy and tube shunt implantation) and the newer, conjunctiva-sparing MIGSs ( Table 4 ). Bleb-based operations can effectively lower IOP; however, they may develop bleb-related complications and may have high reoperation rates. As a result, the current role of traditional procedures in the era of evolving MIGSs is unclear. Surgeons’ perspectives are changing 80 ; a recent practice preferences survey from the American Glaucoma Society (2017) found that trabeculectomy has fallen out of favor, with tube shunt implantation reported as the preferred incisional surgical treatment in 7 of 8 surgical centers. 81 When prospective MIGS trials are completed, the pendulum may swing in favor of MIGSs. 80
Table 4
Surgical Procedures for the Treatment of Glaucoma a
Trabecular Outflow Resistance
The juxtacanalicular tissue within the TM is the primary source of outflow resistance in eyes with POAG, with the inner wall of the Schlemm canal serving as an additional line of resistance. 82 , 83 , 84 To improve the aqueous outflow and lower the IOP, surgeons bypass the TM by directing the aqueous flow directly into the Schlemm canal or by rerouting the fluid from the anterior chamber into the subconjunctival space.
Traditional Incisional Operations
Trabeculectomy—the “gold standard” surgical glaucoma procedure for several decades—is the creation of a partial thickness scleral flap with excision of a segment of TM to create an alternate drainage route from the anterior chamber to the subconjunctival space. 85 , 86 Trabeculectomy can produce outstanding IOP control, particularly in eyes where an IOP near the low teens is targeted to slow glaucoma progression. 87 , 88 Trabeculectomy may be performed together with cataract extraction (CE) and/or administration of mitomycin C (MMC) on the surface of the sclera to prevent postoperative conjunctival fibrosis. 89 Trab-MMC alone, trab-MMC+CE, and trab-MMC in pseudophakic eyes were found to produce comparable IOP reductions and success rates after 5 years 90 ; however, other studies have found lower success rates with trab-MMC in pseudophakic eyes, probably because of postoperative inflammation after CE. 80 , 91
Tube shunt implantation, an alternative to trabeculectomy, has gained popularity in recent years. The implantation of tube shunts, often referred to as glaucoma drainage devices (GDDs), creates a permanent sclerostomy to drain the aqueous humor into the subconjunctival space. 92 The advantages of GDDs over trabeculectomy include decreased conjunctival scarring (by diverting aqueous drainage to the equatorial region of the eye and away from the limbus) and the formation of a permanent bleb (plate tube). 92 Most GDD designs are modeled after the early Molteno implant 93 and may be valved (promotes unidirectional flow) or nonvalved (passive-acting). 92 The Ahmed Baerveldt Comparison and Ahmed Versus Baerveldt studies compared the safety and efficacy of the valveless Baerveldt 350-mm 2 GDD (Johnson & Johnson) to that of the valved Ahmed-FP7 GDD (New World Medical Inc). Both devices were effective in reducing the IOP and the need for IOP-lowering medications, although a favorable IOP decrease, medication burden reduction, and safety profile (but with a higher incidence of hypotony) were seen with the valveless Baerveldt 350-mm 2 GDD at 5 years. 94 Recent advancements in valveless GDD operation include the development of the Ahmed ClearPath GDD (New World Medical Inc) and PAUL glaucoma implant (PGI; Advanced Ophthalmic Innovations). The Ahmed ClearPath GDD has several unique design features, such as a flexible, low-lying plate with anterior suture points to increase the ease of implantation, and a prethreaded 4-0 polypropylene ripcord to mitigate the risk of hypotony that has been reported in other GDD studies. 95 The PGI GDD has a smaller plate that occupies less space in the ACA and a relatively large endplate surface area through which the aqueous humor can be absorbed. 96 Early outcome data with the Ahmed ClearPath GDD and PGI found mean IOP reductions of 43% 97 and 51.6%, 96 at 6 months, respectively.
Both trabeculectomy and GDD implantation are effective treatment options for refractory glaucoma—eyes with poor results after both pharmacotherapy and laser. A 5-year comparison of trabeculectomy and tube shunt operation found that both techniques effectively lower the IOP (trabeculectomy: 49.5%; tube: 41.4%), with the tube group having a better safety profile. 97 In surgically naïve eyes with refractory glaucoma, the Primary Tube vs Trabeculectomy study found trabeculectomy to be superior, 98 whereas the Tube vs Trabeculectomy study reported similar outcomes in both groups at 5 years postoperatively in eyes that were not surgically naïve; however, eyes in the tube group had lower failure and reoperation rates. 17 , 97 Frequent complications within the early postoperative period included choroidal effusion (Tube, 14%; Trab, 13%) and shallow anterior chamber (Tube, 10%; Trab, 10%), and late postoperative complications included persistent corneal edema (Tube, 16%; Trab, 9%) and bleb encapsulation (Tube, 2%; Trab, 6%). 17 Many of the eyes needed postoperative interventions (Tube: 25%, Trab: 70%). 17 Craven et al 16 estimated that 25% of patients treated with trabeculectomy or a tube shunt needed additional interventions to address surgical failure.
Minimally Invasive Glaucoma Surgeries
The potential complications and surgical failures seen with traditional incisional operations speak to the need for better procedures for mild-to-moderate glaucoma that are minimally invasive yet durable. This has led to the introduction of MIGSs, which have revolutionized glaucoma care over the past decade. This group of novel procedures may sufficiently lower the IOP to delay or minimize the need for traditional incisional procedures, 82 and they are more suitable for patients with mild-to-moderate glaucoma. Minimally invasive glaucoma surgeries can be performed together with cataract operation, which makes them a valuable option for glaucomatous eyes with advanced cataracts (from aging, phacomorphic glaucoma, traumatic glaucoma, etc). Unlike the traditional filtration procedures, MIGSs are relatively simple to perform because they require surgical skills similar to those required for modern-day cataract surgery, 99 and they can be performed by cataract surgeons who are not glaucoma fellowship trained. Minimally invasive glaucoma surgeries have favorable safety profiles and are less invasive than traditional incisional operations. 100
One of the management challenges with performing MIGSs lies in whether to bypass or enhance the conventional aqueous outflow 101 because the currently available MIGS devices target 1 of the 3 pressure-lowering mechanisms: (1) the trabecular outflow pathway, referring to “angle-based” MIGSs that reroute the aqueous flow toward the Schlemm canal; (2) the subconjunctival space, referring to MIGSs that create a drainage pathway, diverting the aqueous humor to the subconjunctival space; (3) the suprachoroidal space, referring to MIGSs that increase the uveoscleral pathway outflow and divert the aqueous flow toward the suprachoroidal space. 100
MIGSs Targeting the Trabecular Outflow Pathway
Approximately 50%-75% of the outflow resistance lies within the TM and the inner wall of the Schlemm canal, whereas the remainder resides within the Schlemm canal and its distal collector channels. 102 , 103 , 104 , 105 This identifies the conventional outflow pathway as an attractive first target for the treatment of glaucoma. Angle-based MIGSs take advantage of the lower resistance within the Schlemm canal and divert the aqueous flow to the canal, thereby bypassing most of the outflow resistance. Despite this, however, a significant proportion of outflow resistance remains, thereby making these procedures unsuitable for patients with severe glaucoma who require significant IOP reduction. 80 Minimally invasive glaucoma surgeries that target the trabecular outflow pathway fall within the categories of trabecular bypass implant, ab-interno canaloplasty, ab-interno trabeculotomy (AIT), goniotomy, and the more recently introduced combined goniotomy/viscodilation and trabeculotomy/viscodilation procedures.
The iStent (Glaukos Corporation), the first trabecular bypass implant, has produced excellent results when implanted into glaucomatous eyes that are well-controlled on 1 IOP-lowering medication. 80 Additional IOP lowering is observed when placing more than 1 stent, which led to the development of the iStent inject and iStent inject W. 100 A study comparing the early outcomes of the iStent and iStent inject reported favorable IOP (iStent, 4.3%; iStent inject, 19.1%) and medication reduction results (iStent, 72.2%; iStent inject, 94.1%) in the iStent inject group at 12 months, with a similar safety profile observed in both the groups. 106 Ab-interno canaloplasty is typically performed with the iTrack microcatheter (Nova Eye Medical), and a retrospective comparison with ab-externo canaloplasty (iTrack with a 9-0 prolene tensioning suture) found comparable safety and efficacy. 107 Ab-interno trabeculotomy and goniotomy procedures bring the anterior chamber, Schlemm canal, and distal collector channels into direct communication through the disruption or partial excision of the TM. 108 The Trabectome (Neomedix), a long-standing AIT procedure, uses electrocauterization to ablate the TM and has been documented to safely and effectively reduce the IOP. 108 Recent advancements in excisional goniotomy include the Kahook Dual Blade (KDB; New World Medical) and KDB Glide (New World Medical) devices. Although limited data on KDB Glide exist within the literature, several studies of KDB have shown that it has a favorable safety profile and similar effectiveness to AIT procedures. 109 , 110
Angle-based MIGS procedures are easy to perform and have favorable safety profiles, but compared with traditional trabeculectomy, they have more limited abilities to lower IOP. 101 , 111 Distal outflow (collector channels and episcleral veins), which is often overlooked in the treatment of glaucoma, may play a pivotal role in IOP control and is unaffected by canalicular-based MIGS procedures. Studies with bovine and monkey eyes have found that collector channels may alter the pressure distribution within the Schlemm canal, suggesting that the aqueous outflow may depend on the location of these distal elements. 84 , 102 , 112 Resistance within the Schlemm canal and the collector channels appears to limit the outflow increase of trabecular bypass procedures to 13%-26% and IOP reduction to the mid-teens, but a greater pressure decrease is expected if a moderate dilation of the Schlemm canal and the collector channels is achieved. 84 , 113 , 114 Goniotomy and trabeculotomy may be performed concurrently with the implantation of an ophthalmic viscosurgical device (STREAMLINE Surgical Systems, New World Medical; OMNI360 Surgical Systems, Sight Sciences) to the Schlemm canal to reduce the distal outflow resistance and promote further IOP reduction. Interim analyses of the STREAMLINE and OMNI trials have shown effective, sustained IOP reductions and meaningful medication reductions at 6 and 12 months, respectively. 115 , 116
MIGSs Targeting the Subconjunctival Space
Minimally invasive glaucoma surgeries devices within this category work similarly to trabeculectomy by diverting the aqueous humor flow directly into the subconjunctival space. 100 The main disadvantage of this strategy is the potential for subconjunctival fibrosis, which for trabeculectomy may be prevented by the intraoperative application of MMC. 100 Subconjunctival MIGS devices, which are designed based on the Hagen-Poiseuille equation, include the ab-internally implanted XEN45 gel stent (Allergan) and the ab-externally implanted PRESERFLO microshunt (Santen). Both devices produce comparable safety profiles, IOP reductions, and overall surgical success at 2 years. 117 The analysis of both implantation approaches with an experimental microfluidic system found higher outflow resistance and less predictable bleb formation with ab-interno implantation. This may affect the long-term IOP control and could direct the development of future subconjunctival-based MIGS devices. 118
MIGSs Targeting the Suprachoroidal Space
The third category of MIGSs aims to increase the uveoscleral outflow. 100 The uveoscleral pathway is not limited by the pressure “floor” formed by episcleral venous pressure; thus, diverting the aqueous humor into the suprachoroidal space could have a greater lower IOP capacity. 119 Unfortunately, current studies have yet to realize such results. After the recall of CyPass (Alcon) in 2018 because of corneal endothelial cell loss from malpositioned devices, most suprachoroidal MIGSs are still under investigation. 119 A review of recent studies indicates favorable safety profiles and effective short-term IOP reductions to the mid-teens with the iStent SUPRA (Glaukos Corporation), STARflo (iSTAR Medical), and gold implant (SOLX, Inc). Longer follow-ups and more robust trial designs are still required for the US Food and Drug Administration approval of suprachoroidal MIGSs, 120 and long-term efficacy may be limited by fibroblast migration and proliferation. 121
The pathogenesis of glaucoma is multifactorial and incompletely understood, and diagnosis methods and management strategies are constantly being improved. Treatment outcomes, safety profiles, and recovery times have improved with the introduction of MIGSs. Future work should aim to develop MIGS devices with greater IOP-lowering capabilities than traditional incisional operations.
Potential Competing Interests
The authors report no competing interests.
Acknowledgments
The authors acknowledge Jason S. Calhoun, COA, for the ultrasound biomicroscopy image ( Figure 1 ).
At a glance: Glaucoma
Loss of side (peripheral) vision, blind spots, blindness
Dilated eye exam with visual field testing
Medicine (usually eye drops), laser treatment, surgery
What is glaucoma?
Glaucoma is a group of eye diseases that can cause vision loss and blindness by damaging a nerve in the back of your eye called the optic nerve.
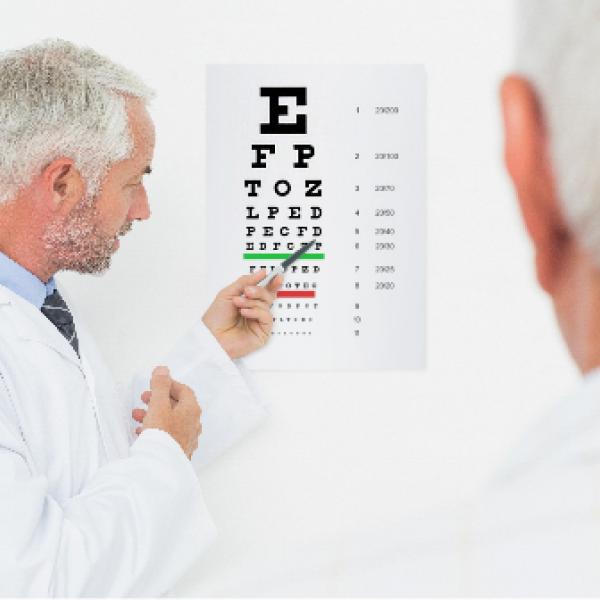
The symptoms can start so slowly that you may not notice them. The only way to find out if you have glaucoma is to get a comprehensive dilated eye exam.
There’s no cure for glaucoma, but early treatment can often stop the damage and protect your vision.
What are the types of glaucoma?
There are many different types of glaucoma, but the most common type in the United States is called open-angle glaucoma — that’s what most people mean when they talk about glaucoma. Other types are less common, like angle-closure glaucoma and congenital glaucoma.
What are the symptoms of glaucoma?
At first, glaucoma doesn’t usually have any symptoms. That’s why half of people with glaucoma don’t even know they have it.
Over time, you may slowly lose vision, usually starting with your side (peripheral) vision — especially the part of your vision that’s closest to your nose. Because it happens so slowly, many people can’t tell that their vision is changing at first.
But as the disease gets worse, you may start to notice that you can’t see things off to the side anymore. Without treatment, glaucoma can eventually cause blindness.
Am I at risk for glaucoma?
Anyone can get glaucoma, but some people are at higher risk. You’re at higher risk if you:
- Are over age 60, especially if you’re Hispanic/Latino
- Are African American and over age 40
- Have a family history of glaucoma
Talk with your doctor about your risk for glaucoma, and ask how often you need to get checked. If you’re at higher risk, you need to get a comprehensive dilated eye exam every 1 to 2 years.

When to get help right away
Angle-closure glaucoma can cause these sudden symptoms:
- Intense eye pain
- Upset stomach (nausea)
- Blurry vision
If you have any of these symptoms, go to your doctor or an emergency room now.
What causes glaucoma?
Scientists aren’t sure what causes the most common types of glaucoma, but many people with glaucoma have high eye pressure — and treatments that lower eye pressure help to slow the disease.
There’s no way to prevent glaucoma. That’s why eye exams are so important — so you and your doctor can find it before it affects your vision.
How will my eye doctor check for glaucoma?
Eye doctors can check for glaucoma as part of a comprehensive dilated eye exam. The exam is simple and painless — your doctor will give you some eye drops to dilate (widen) your pupil and then check your eyes for glaucoma and other eye problems. The exam includes a visual field test to check your side vision.

Did you know?
Glaucoma can happen in 1 eye or both eyes
Some people with high eye pressure don’t get glaucoma — and there’s a type of glaucoma that happens in people with normal eye pressure
Normal eye pressure varies by person — what’s normal for 1 person could be high for another
What’s the treatment for glaucoma?
Doctors use different types of treatment for glaucoma, including medicines (usually eye drops), laser treatment, and surgery.
If you have glaucoma, it’s important to start treatment right away. Treatment won’t undo any damage to your vision, but it can stop it from getting worse.
Medicines. Prescription eye drops are the most common treatment. They lower the pressure in your eye and prevent damage to your optic nerve.
Learn more about glaucoma medicines
Laser treatment. To lower your eye pressure, doctors can use lasers to help the fluid drain out of your eye. It’s a simple procedure that your doctor can do in the office.
Learn more about laser treatment for glaucoma
Surgery. If medicines and laser treatment don’t work, your doctor might suggest surgery. There are several different types of surgery that can help the fluid drain out of your eye.
Learn more about glaucoma surgery
Talk over your options with your doctor. While glaucoma is a serious disease, treatment works well. Remember these tips:
- If your doctor prescribes medicine, be sure to take it every day
- Tell your doctor if your treatment causes side effects
- See your doctor for regular check-ups
- If you’re having trouble with everyday activities because of your vision loss, ask your doctor about vision rehabilitation services or devices that could help
- Encourage family members to get checked for glaucoma, since it can run in families

Featured Resource: Talk With Your Doctor About Glaucoma
Do you have glaucoma? This guide makes it easy to talk with your doctor about your condition. It includes:
- Information about glaucoma
- Questions for the doctor
- A symptom tracker

What is the latest research on glaucoma?
Scientists are studying what causes glaucoma and how we can find it earlier and treat it better. NEI also funds research on new treatment options.

Glaucoma Resources
Last updated: November 15, 2023

Nature vs. Nurture: Exploring the role of genetics and environmental factors in Glaucoma risk
G laucoma, a leading cause of irreversible blindness worldwide, poses a significant public health challenge with approximately 80 million individuals affected globally. Alarmingly, half of these cases often go undiagnosed, exacerbating the risk of vision loss. In India alone, nearly 12 million people grapple with this condition, with a staggering 40-50 percent of cases evading detection. With projections indicating a rise in global blindness attributed to glaucoma, it becomes imperative to delve into its intricate mechanisms and risk factors.
While glaucoma manifests as a gradual loss of retinal ganglion cells (RGCs), its etiology remains elusive despite extensive research efforts. Age serves as a prominent risk factor, with individuals over 40 facing heightened susceptibility. Research also indicates a strong genetic predisposition, particularly evident in cases of juvenile-onset and early adult-onset glaucoma linked to specific gene mutations. The pathophysiology of glaucoma is multifaceted, involving an interplay of genetic predisposition, environmental influences, and stochastic factors. This complexity underscores the importance of exploring the delicate balance between nature and nurture in shaping glaucoma risk.
Exploring the Genetic Basis of Glaucoma
In recent years, there has been a notable shift in uncovering the genetic origins of glaucoma, marking a pivotal moment in enhancing our comprehension of this complex condition.
Primary open-angle glaucoma (POAG)
Primary open-angle glaucoma (POAG) is the most common type, characterized by no apparent eye abnormalities. While mutations in genes like myocilin, optineurin, and CYP1B1 contribute to some cases, recent genetic studies found more prevalent risk factors. These include alterations in DNA sequences near genes like CAV1/CAV2, CDKN2B antisense RNA, TMCO1, SIX1/SIX6, and LRP12/ZFPM2, as well as DNA loss in TBK1 and GALC, shedding light on various genetic elements associated with POAG.
Primary angle-closure glaucoma (PACG)
Primary angle-closure glaucoma (PACG) ranks as the second most prevalent type globally, impacting over 16 million individuals. It occurs when the drainage angle closes, hindering fluid outflow and elevating intraocular pressure. A recent extensive genetic investigation pinpointed genetic variations linked to PACG, particularly in or near PLEKHA7, PCMTD1/ST18, and COL11A1 genes. However, the exact role of these genes in PACG remains unclear.
READ ALSO: The connection between clogged eyes and glaucoma
Exfoliation glaucoma (XFG)
Exfoliation glaucoma (XFG), also known as pseudoexfoliation glaucoma, impacts millions globally and stands as the most prevalent identifiable type of open-angle glaucoma. It arises from exfoliation syndrome, a condition marked by the accumulation of white protein-like material on the lens and within the eye's drainage system, as well as other body tissues. Genetic variations in the LOXL1 and CNTNAP2 genes have been linked to XFG. Ongoing research aims to elucidate how these genes influence the formation of protein deposits and their role in glaucoma development.
Understanding Environmental Factors in Glaucoma Risk
Environmental factors play a crucial role in influencing primary open-angle glaucoma (POAG), impacting both intraocular pressure (IOP) and the rate of retinal ganglion cell apoptosis. While few environmental contributors to POAG are currently identified, certain activities like playing wind instruments, drinking coffee, specific yoga poses, tight necktie wear, and weightlifting can elevate IOP, while general physical exercise tends to lower it. Additionally, nutritional choices like dietary fat and antioxidant intake, along with lifestyle habits such as smoking and postmenopausal hormone use, may influence POAG development. Further research is needed to fully understand their impact on glaucoma onset. Notably, there's evidence of a gene-environment interaction between hormone replacement therapy and NOS3, a gene associated with nitric oxide synthase 3, as a POAG risk factor.
READ ALSO: Eyes itching? Watch before you take that drop, say docs
Residence in northern latitudes emerges as a significant risk factor for exfoliation syndrome (ES) and its related condition, exfoliation glaucoma. ES involves extracellular deposits and stands as the primary cause of secondary open-angle glaucoma. A retrospective study of over 3,300 incident ES cases in northern U.S. residents found an increased risk of ES development, while residing in southern latitudes correlated with reduced ES risk. Furthermore, adjustments for environmental effects revealed associations between climatic factors like high July temperatures and decreased ES risk, alongside increased risk with greater sunshine exposure. These findings suggest that factors like ambient temperature and sunlight exposure serve as environmental triggers for ES, although other elements of northern latitude living, such as altered vitamin D metabolism, could also contribute.
In conclusion, while genetic predispositions play a significant role in glaucoma, environmental factors also exert considerable influence on the risk and progression of the disease. Understanding these environmental risk factors is crucial for developing preventive strategies and personalized treatment approaches. Further research into the interplay between genetics and the environment will deepen our understanding of glaucoma's complex pathogenesis and pave the way for more effective management and ultimately, improved outcomes for patients. By addressing both genetic and environmental aspects comprehensively, we can move closer to reducing the burden of glaucoma and preserving vision for millions worldwide.
(Written By: Dr. P Sathyan, Director of Sathyan Eye Care Hospital & Coimbatore Glaucoma Foundation, Coimbatore)
For more news like this visit TOI . Get all the Latest News , City News , India News , Business News , and Sports News . For Entertainment News , TV News , and Lifestyle Tips visit Etimes

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 06 May 2024
Medications for attention deficit hyperactivity disorder associated with increased risk of developing glaucoma
- Rami Darwich ORCID: orcid.org/0000-0001-7125-230X 1 ,
- Mahyar Etminan 2 ,
- Bonnie He 1 &
- Brennan D. Eadie 1
Eye ( 2024 ) Cite this article
253 Accesses
1 Citations
50 Altmetric
Metrics details
- Risk factors
Attention deficit hyperactivity disorder (ADHD) therapies including atomoxetine, methylphenidate, and amphetamines are some of the most prescribed medications in North America. Due to their sympathomimetic action, these drugs are contraindicated in patients with a history of angle closure glaucoma (ACG). This study aims to determine the risk of ACG and open angle glaucoma (OAG) among users of these treatments.
This is a retrospective cohort study with a case control analysis using the PharMetrics Plus Database (IQVIA, USA). We created a cohort of new users of atomoxetine, methylphenidate, and amphetamines and they were followed to the first diagnosis of (1) ACG or OAG; or (2) end of follow up. For each case, four age-matched controls were selected. A conditional logistic regression model was used to adjust for confounders and to calculate adjusted incidence-rate-ratios (aIRRs).
A total of 240,257 new users of the ADHD medications were identified. The mean age was 45.0 ± 19.4 years and 55% of the cohort was female. Regular users of atomoxetine and amphetamines had a higher aIRR for developing ACG compared with non-users (aIRR = 2.55 95% CI [1.20–5.43] and 2.27 95% CI [1.42–3.63], respectively); while users of methylphenidate had a higher aIRR for developing OAG (aIRR = 1.23 95% CI [1.05–1.59]).
Conclusions
Use of amphetamines and atomoxetine had a higher risk for ACG, while use of methylphenidate was associated with a higher risk for OAG. Given the prevalence of ADHD medication use (medically and recreationally), our current data on their associated risk of glaucoma have profound public health implications.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
251,40 € per year
only 13,97 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Alzheimer’s disease risk reduction in clinical practice: a priority in the emerging field of preventive neurology

Major depressive disorder: hypothesis, mechanism, prevention and treatment

Dimerization and antidepressant recognition at noradrenaline transporter
Data availability.
Data can be provided upon a reasonable request. The authors can share the complete data set creation plan and the analytic code upon request; please contact Dr. Mahyar Etminan. The data sets utilized in this study are accessible with permission from IQVIA. However, there are restrictions on the availability of this data, as it was used under license for this study and is not publicly accessible.
Ayyıldız D, Ayyıldız T. Ophthalmological findings in children and adolescents with attention deficit and hyperactivity disorder. Int Phys Med Rehabil J. 2019;4:276–9.
Guvenmez O, Cubuk M, Gunes S. The effects of medication on intraocular pressure in children with attention deficit hyperactivity disorder: a prospective study. J Popul Ther Clin Pharm. 2020;27:e45–50.
Google Scholar
Mechler K, Banaschewski T, Hohmann S, Häge A. Evidence-based pharmacological treatment options for ADHD in children and adolescents. Pharm Ther. 2021;23:107940.
Faraone SV. The pharmacology of amphetamine and methylphenidate: relevance to the neurobiology of attention-deficit/hyperactivity disorder and other psychiatric comorbidities. Neurosci Biobehav Rev. 2018;87:255–70.
Article CAS PubMed PubMed Central Google Scholar
Bradley C. The behavior of children receiving benzedrine. Am J Psychiatry. 1937;94:577–85.
Article Google Scholar
McCabe SE, Schulenberg JE, Wilens TE, Schepis TS, McCabe VV, Veliz PT. Prescription stimulant medical and nonmedical use among US secondary school students, 2005 to 2020. JAMA Netw Open. 2023;6:e238707–07.
Article PubMed PubMed Central Google Scholar
McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100:96–106.
Article PubMed Google Scholar
Chen LY, Crum RM, Strain EC, Alexander GC, Kaufmann C, Mojtabai R. Prescriptions, nonmedical use, and emergency department visits involving prescription stimulants. J Clin Psychiatry. 2016;77:e297–304.
Lu C-K, Kuang T-M, Chou JC-K. Methylphenidate (Ritalin)-associated cataract and glaucoma. J Chin Med Assoc. 2006;69:589–90.
Article CAS PubMed Google Scholar
Bartlik B, Harmon G, Kaplan P. Use of methylphenidate in a patient with glaucoma and attention-deficit hyperactivity disorder: a clinical dilemma. Arch Gen Psychiatry. 1997;54:188–89.
Julien RG, Vincendeau J. Fuchs heterochromy, glaucoma and sympathomimetics. Bulletin des societes d’ophtalmologie de France 1956:187-8.
Karabulut M, Karabulut S, Kocatürk T, Ozkan SB. Is the treatment of attention deficit hyperactivity disorder a new cause of cataract? Open J Ophthalmol 2018;8. https://doi.org/10.4236/ojoph.2018.81004
Bymaster FP, Katner JS, Nelson DL, Hemrick-Luecke SK, Threlkeld PG, Heiligenstein JH, et al. Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacology. 2002;27:699–711.
Upadhyaya HP, Desaiah D, Schuh KJ, Bymaster FP, Kallman MJ, Clarke DO, et al. A review of the abuse potential assessment of atomoxetine: a nonstimulant medication for attention-deficit/hyperactivity disorder. Psychopharmacology. 2013;226:189–200.
Eadie B, Etminan M, Mikelberg FS. Risk for uveitis with oral moxifloxacin: a comparative safety study. JAMA Ophthalmol. 2015;133:81–84.
Eadie BD, Etminan M, Carleton BC, Maberley DA, Mikelberg FS. Association of repeated intravitreous bevacizumab injections with risk for glaucoma surgery. JAMA Ophthalmol. 2017;135:363–68.
Hussein M, Wei W, Mastey V, Sanchez RJ, Wang D, Murdock DJ, et al. Real-world effectiveness of casirivimab and imdevimab among patients diagnosed with COVID-19 in the ambulatory setting: a retrospective cohort study using a large claims database. BMJ Open. 2022;12:e064953.
Essebag V, Genest J Jr, Suissa S, Pilote L. The nested case-control study in cardiology. Am Heart J. 2003;146:581–90.
İzci F, göde öğüten E. Methylphenidate induced increase in intraocular pressure, Dusunen Adam . J Psychiatry Neurol Sci. 2016;29. https://doi.org/10.5350/dajpn2016290413 .
Larrañaga-Fragoso P, Noval S, Rivero J, Boto-de-los-Bueis A. The effects of methylphenidate on refraction and anterior segment parameters in children with attention deficit hyperactivity disorder. J AAPOS . 2015;19. https://doi.org/10.1016/j.jaapos.2015.04.005
Duman NS, Duman R, Sarı Gökten E, Duman R. Lens opacities in children using methylphenidate hydrochloride. Cutan Ocul Toxicol. 2017;36:362–65.
Kong N, Bao Y, Zhao H, Kang X, Tai X, Shen Y. Methylphenidate causes cytotoxicity on photoreceptor cells via autophagy. Hum Exp Toxicol. 2020;40:71–80.
Corona JC. Role of oxidative stress and neuroinflammation in attention-deficit/hyperactivity disorder. Antioxidants. 2020;9:1039.
Corona JC, Carreón-Trujillo S, González-Pérez R, Gómez-Bautista D, Vázquez-González D, Salazar-García M. Atomoxetine produces oxidative stress and alters mitochondrial function in human neuron-like cells. Sci Rep. 2019;9:13011.
Izzotti A, Bagnis A, Saccà SC. The role of oxidative stress in glaucoma. Mutat Res. 2006;612:105–14.
de la Torre R, Farré M, Navarro M, Pacifici R, Zuccaro P, Pichini S. Clinical pharmacokinetics of amfetamine and related substances: monitoring in conventional and non-conventional matrices. Clin Pharmacokinet. 2004;43:157–85.
Kelly RP, Yeo KP, Teng C-H, Smith BP, Lowe S, Soon D, et al. Hemodynamic effects of acute administration of atomoxetine and methylphenidate. J Clin Pharmacol. 2005;45:851–55.
Lowe RF. Primary creeping angle-closure glaucoma. Br J Ophthalmol. 1964;48:544–50.
Enoch J, Jones L, Taylor DJ, Bronze C, Kirwan JF, Jones PR, et al. How do different lighting conditions affect the vision and quality of life of people with glaucoma? A systematic review. Eye. 2020;34:138–54.
D’Alli RE. Chapter 90 - Child And Adolescent Psychopharmacology. In: Carey WB, Crocker AC, Coleman WL, et al., eds. Developmental-Behavioral Pediatrics (Fourth Edition). Philadelphia: W.B. Saunders 2009:885-910.
Cui YM, Teng CH, Pan AX, Yuen E, Yeo KP, Zhou Y, et al. Atomoxetine pharmacokinetics in healthy Chinese subjects and effect of the CYP2D6*10 allele. Br J Clin Pharmacol. 2007;64:445–9.
Trzepacz PT, Williams DW, Feldman PD, Wrishko RE, Witcher JW, Buitelaar JK. CYP2D6 metabolizer status and atomoxetine dosing in children and adolescents with ADHD. Eur Neuropsychopharmacol. 2008;18:79–86.
Download references
Acknowledgements
This study was funded by the Glaucoma Research Society of Canada Project Grant.
Author information
Authors and affiliations.
Department of Ophthalmology and Visual Sciences, Dalhousie University, Halifax, NS, Canada
Rami Darwich, Bonnie He & Brennan D. Eadie
Department of Ophthalmology and Visual Sciences, University of British Columbia, Vancouver, BC, Canada
Mahyar Etminan
You can also search for this author in PubMed Google Scholar
Contributions
RD was responsible for designing the study, conducting the search, analysing, and interpreting results, and writing the report. BH contributed to the design of the research and provided feedback on the report. ME and BE supervised the design of the study, writing the report, extracting and analysing data, interpreting the results, and provided feedback on the report.
Corresponding author
Correspondence to Mahyar Etminan .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplemental table 1: icd-9 and icd-10 of the angle closure subtypes., supplemental table 2: icd-9 and icd-10 of the open angle subtypes., rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Darwich, R., Etminan, M., He, B. et al. Medications for attention deficit hyperactivity disorder associated with increased risk of developing glaucoma. Eye (2024). https://doi.org/10.1038/s41433-024-03100-6
Download citation
Received : 29 May 2023
Revised : 31 March 2024
Accepted : 18 April 2024
Published : 06 May 2024
DOI : https://doi.org/10.1038/s41433-024-03100-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Scientists uncover promising treatment target for resistant brain cancer
For many patients with a deadly type of brain cancer called glioblastoma, chemotherapy resistance is a big problem.
Current standard treatments, including surgery, radiation, and chemotherapy using the drug temozolomide, have limited effectiveness and have not significantly changed in the past five decades. Although temozolomide can initially slow tumor progression in some patients, typically the tumor cells rapidly become resistant to the drug.
But now, Virginia Tech researchers with the Fralin Biomedical Research Institute at VTC may have moved a step closer to a solution.
Working with glioblastoma cell cultures, including glioblastoma stem cells derived from patient specimens, and laboratory mouse models harboring human cancer cells, scientists have pinpointed an effective molecular signaling pathway that is thought to be crucial for cancer cell survival during temozolomide treatment. The findings are now online in iScience, an open-access journal of Cell Publishing.
"In the past 50 years, treatment options for glioblastoma have remained largely unchanged, relying on surgery, radiation, and temozolomide," said Zhi Sheng, senior author of the study and assistant professor at the Fralin Biomedical Research Institute. "However, temozolomide's effectiveness is limited, and resistance to the chemotherapy inevitably develops in patients. Since it's the only currently available approved chemotherapy that can effectively reach the brain, finding ways to restore its effectiveness is crucial in addressing the treatment failure in glioblastoma."
Researchers examined the Phosphoinositide 3 Kinase (PI3K) molecular signaling pathway, which is like a communication system inside cells. It tells cells how to grow, survive, and divide. When this pathway is activated, it can promote cancer growth, so scientists and clinicians generally thought blocking it could be a way to treat cancer.
Their results have not been successful.
In the new research, Fralin Biomedical Research Institute scientists found that in some brain cancer patients who didn't respond to treatment, levels were high of a specific form of the signaling protein called PI3K-beta that helps regulate cellular processes.
When they blocked just PI3K-beta in cell cultures and mouse models harboring cancer cells, the tumor cells became more sensitive to temozolomide treatment. In addition, using a drug that blocks PI3K-beta along with the usual treatment slowed down the cancer cells' growth.
Researchers are uncertain why PI3K, in its various forms, are very similar in structure yet do different things in the body.
"The reason previous treatments targeting the PI3K pathway failed is because they didn't distinguish between PI3K-beta and its related proteins," Sheng said. "This research shows that PI3K-beta is specific to glioblastoma, making it the crucial target for effective treatment."
Going forward, overcoming the blood-brain barrier remains a hurdle for delivering P13K-beta inhibitors into the brain, which will be crucial for translating the findings into the clinic to help patients.
"We will resolve these issues in our future studies," Sheng said.
Co-first authors of the study are Kevin Pridham, a former postdoctoral associate at the Fralin Biomedical Research Institute, and Kasen Hutchings and Patrick Beck, two former medical students at the Virginia Tech Carilion School of Medicine who are pursuing their medical careers in radiology in Las Vegas and pediatrics in Philadelphia, respectively.
Cell specimens were provided by Carilion Clinic. Study results are in part based on data generated by The Cancer Genome Atlas Research Network, the Dependency Map, the Genotype-Tissue Expression, or the Chinese Glioma Genome Atlas. The research was supported by the National Institutes of Health.
- Brain Tumor
- Colon Cancer
- Lung Cancer
- Brain-Computer Interfaces
- Multiple Sclerosis
- Alzheimer's
- Esophageal cancer
- Colorectal cancer
- Chemotherapy
- Diabetes mellitus type 2
- Spanish flu
Story Source:
Materials provided by Virginia Tech . Original written by John Pastor. Note: Content may be edited for style and length.
Journal Reference :
- Kevin J. Pridham, Kasen R. Hutchings, Patrick Beck, Min Liu, Eileen Xu, Erin Saechin, Vincent Bui, Chinkal Patel, Jamie Solis, Leah Huang, Allison Tegge, Deborah F. Kelly, Zhi Sheng. Selective regulation of chemosensitivity in glioblastoma by phosphatidylinositol 3-kinase beta . iScience , 2024; 27 (6): 109921 DOI: 10.1016/j.isci.2024.109921
Cite This Page :
Explore More
- Charge Your Laptop in a Minute?
- Caterpillars Detect Predators by Electricity
- 'Electronic Spider Silk' Printed On Human Skin
- Engineered Surfaces Made to Shed Heat
- Innovative Material for Sustainable Building
- Human Brain: New Gene Transcripts
- Epstein-Barr Virus and Resulting Diseases
- Origins of the Proton's Spin
- Symbiotic Bacteria Communicate With Plants
- Birdsong and Human Voice: Same Genetic Blueprint
Trending Topics
Strange & offbeat.
More From Forbes
Inflation is already soaking the rich 1%, new research shows.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
HUNGARY - JUNE 28: A Woman Lighting Her Cigarette With A Bill Of A Billion Pengos, As If It Was ... [+] Merely A Piece Of Paper, On June 28, 1946, While Hungary Was Going Through A Galloping Inflation. (Photo by Keystone-France/Gamma-Keystone via Getty Images)
The recent inflationary surge is squeezing households, but not likely in the way you think. It’s hitting the wealthy disproportionately, new research shows.
Inflation peaked at 9.1% in June 2022, and has recently dropped to 3.4% in April, according to data collated by TradingEconomics . However, the inflation rate is still way higher than it was in the five years through 2020 when the Consumer Price index grew at a rate that hovered around 2% and sometimes went negative.
In many ways that stability was good for the economy. But the jump in inflation after the pandemic has hit everyone in the wallet, experts say. However, it’s also true some groups got hit harder than others.
“Virtually all households are hurt by inflation,” states a recent working paper distributed by the National Bureau of Economic Research titled ‘ Inflation’s Impact on American Households .’ “But richer households typically face larger percentage losses thanks to their higher share of asset income relative to labor income.”
Put simply, wealthier people tend to get more from their dividends or interest on investments rather than from salaries. The impact of inflation on the former (dividends and interest) is far greater.
“Inflation’s net taxation is highly progressive with the richest 1 percent experiencing nearly 2.6 times the average percentage decline in lifetime spending as those in the bottom quintile,” the paper states. It was authored by David Altig, Alan J. Auerbach, Erin F. Eidschun, Laurence J. Kotlikoff, and Victor Yifan Ye.
The 83 Best Memorial Day Sales According To Our Deal Savvy Editors
The best beers in canada according to the canadian brewing awards, nyt ‘strands’ #84 hints, spangram and answers for sunday, may 26th.
The authors use an example of someone in the top quartile of income would see a drop in inflation-adjusted spending of 9.84% if inflation jumped from zero to 10% per annum. However, someone in the 75th percentile would see a drop of 4.83% in spending, on average, according to the paper’s analysis.
The downside for the economy is richer people invest far more money into the economy which helps creates growth and creates jobs. If the rich feel squeezed fiscally then, rightly or wrongly, the rest of us suffer. Investment is a key variable in determining growth and most economists believe that without foreign and domestic investing any economy will suffer.
Findings from the paper also suggest that the inflation-tax (its tax because it robs people of the spending power of their savings) turns out to be a progressive tax. That means that the rich are hurt far more than the poor by this un-legislated hit to their wealth.
“Even were inflation fully anticipated and, thus, financially neutral, it would have a major and quite progressive impact, via the fiscal system, on the average level and distribution of Americans’ lifetime spending,” the report states. Put another way, the poorer you are the less inflation hurts your net worth. And it works vice versa also.
That’s something that the White House administration may find desirable at the moment given its leftward political leaning. However, what will happen to the economy if nominal in tax rate increases are added to the mix? How bad will that be for the U.S.

- Editorial Standards
- Reprints & Permissions
Join The Conversation
One Community. Many Voices. Create a free account to share your thoughts.
Forbes Community Guidelines
Our community is about connecting people through open and thoughtful conversations. We want our readers to share their views and exchange ideas and facts in a safe space.
In order to do so, please follow the posting rules in our site's Terms of Service. We've summarized some of those key rules below. Simply put, keep it civil.
Your post will be rejected if we notice that it seems to contain:
- False or intentionally out-of-context or misleading information
- Insults, profanity, incoherent, obscene or inflammatory language or threats of any kind
- Attacks on the identity of other commenters or the article's author
- Content that otherwise violates our site's terms.
User accounts will be blocked if we notice or believe that users are engaged in:
- Continuous attempts to re-post comments that have been previously moderated/rejected
- Racist, sexist, homophobic or other discriminatory comments
- Attempts or tactics that put the site security at risk
- Actions that otherwise violate our site's terms.
So, how can you be a power user?
- Stay on topic and share your insights
- Feel free to be clear and thoughtful to get your point across
- ‘Like’ or ‘Dislike’ to show your point of view.
- Protect your community.
- Use the report tool to alert us when someone breaks the rules.
Thanks for reading our community guidelines. Please read the full list of posting rules found in our site's Terms of Service.
New research could help predict the next solar flare
When will we be able to see the northern lights again this study could help predict the exact phenomena that caused the bewitching phenomena in the first place..

Newly published research could help predict when there will be "powerful solar storms."
According to Northwestern's McCormick School of Engineering, an international team of researchers found that the sun’s magnetic field starts around 20,000 miles below its surface. Previously, the magnetic field was thought to have originated 130,000 miles below its surface.
According to NASA , the sun's magnetic field is created by a magnetic dynamo that is inside of it. This study aimed to prove that the dynamo actually begins near the sun's surface. Researchers hope that a better understanding of the sun's dynamo could help predict future solar flares.
“This work proposes a new hypothesis for how the sun’s magnetic field is generated that better matches solar observations, and, we hope, could be used to make better predictions of solar activity," said the study's co-author Daniel Lecoanet, an assistant professor of engineering sciences and applied mathematics, researcher at the McCormick School of Engineering and a member of the Center for Interdisciplinary Exploration and Research in Astrophysics .
It's an age-old question that astronomer Galileo Galilei tried to answer, but hundreds of years later, researchers say they found the answer and published the findings in the journal , Nature .
“Understanding the origin of the sun’s magnetic field has been an open question since Galileo and is important for predicting future solar activity, like flares that could hit the Earth,” Lecoanet said.
What is a solar flare?
A solar flare is an explosion of radiation that is produced by the sun and can result in solar storms
Recently, the same powerful solar storm that created the bewildering Northern Lights seen across North America , affected farmers' equipment at the height of planting season. Machines and tools that rely on GPS, like tractors, glitched and struggled with navigational issues.
The National Oceanic and Atmospheric Administration also warned that it could disrupt communications.
Pretty and damaging
While solar flares can cause phenomena such as the aurora borealis that captured attention at the beginning of May, they can cause a lot of damage, too. This is why it's important for researchers to be able to predict when they will hit.
"Although this month’s strong solar storms released beautiful, extended views of the Northern Lights, similar storms can cause intense destruction," said the school in a statement.
According to the university, solar flares can damage the following:
- Earth-orbiting satellites
- Electricity grids
- Radio communications.
How was it calculated?
For their study, researchers ran complex calculations on a NASA supercomputer to discover where the magnetic field is generated.
To figure out where these flares originated, researchers developed "state-of-the-art numerical simulations to model the sun’s magnetic field," states the school.
This new model now takes torsional oscillations into account. It correlates with magnetic activity and is a phenomenon in the sun "in which the solar rotation is periodically sped up or slowed down in certain zones of latitude while elsewhere the rotation remains essentially steady," states a different study .
The sun is super active
The sun is at its solar maximum, meaning it is reaching the height of its 11-year cycle and is at the highest rate of solar activity.
Folks can expect to see more solar flares and solar activity, including solar storms.
Contributing: Eric Lagatta , USA TODAY
Julia is a trending reporter for USA TODAY. She has covered various topics, from local businesses and government in her hometown, Miami, to tech and pop culture. You can connect with her on LinkedIn or follow her on X, formerly Twitter , Instagram and TikTok : @juliamariegz
Advertisement
Supported by
Ozempic Cuts Risk of Chronic Kidney Disease Complications, Study Finds
A major clinical trial showed such promising results that the drug’s maker halted it early.
- Share full article

By Dani Blum
Dani Blum has reported on Ozempic and similar drugs since 2022.
Semaglutide, the compound in the blockbuster drugs Ozempic and Wegovy , dramatically reduced the risk of kidney complications, heart issues and death in people with Type 2 diabetes and chronic kidney disease in a major clinical trial, the results of which were published on Friday. The findings could transform how doctors treat some of the sickest patients with chronic kidney disease, which affects more than one in seven adults in the United States but has no cure.
“Those of us who really care about kidney patients spent our whole careers wanting something better,” said Dr. Katherine Tuttle, a professor of medicine at the University of Washington School of Medicine and an author of the study. “And this is as good as it gets.” The research was presented at a European Renal Association meeting in Stockholm on Friday and simultaneously published in The New England Journal of Medicine .
The trial, funded by Ozempic maker Novo Nordisk, was so successful that the company stopped it early . Dr. Martin Holst Lange, Novo Nordisk’s executive vice president of development, said that the company would ask the Food and Drug Administration to update Ozempic’s label to say it can also be used to reduce the progression of chronic kidney disease or complications in people with Type 2 diabetes.
Diabetes is a leading cause of chronic kidney disease, which occurs when the kidneys don’t function as well as they should. In advanced stages, the kidneys are so damaged that they cannot properly filter blood. This can cause fluid and waste to build up in the blood, which can exacerbate high blood pressure and raise the risk of heart disease and stroke, said Dr. Subramaniam Pennathur, the chief of the nephrology division at Michigan Medicine.
The study included 3,533 people with kidney disease and Type 2 diabetes, about half of whom took a weekly injection of semaglutide, and half of whom took a weekly placebo shot.
Researchers followed up with participants after a median period of around three and a half years and found that those who took semaglutide had a 24 percent lower likelihood of having a major kidney disease event, like losing at least half of their kidney function, or needing dialysis or a kidney transplant. There were 331 such events among the semaglutide group, compared with 410 in the placebo group.
People who received semaglutide were much less likely to die from cardiovascular issues, or from any cause at all, and had slower rates of kidney decline.
Kidney damage often occurs gradually, and people typically do not show symptoms until the disease is in advanced stages. Doctors try to slow the decline of kidney function with existing medications and lifestyle modifications, said Dr. Melanie Hoenig, a nephrologist at Beth Israel Deaconess Medical Center who was not involved with the study. But even with treatment, the disease can progress to the point that patients need dialysis, a treatment that removes waste and excess fluids from the blood, or kidney transplants.
The participants in the study were extremely sick — the severe complications seen in some study participants are more likely to occur in people the later stages of chronic kidney disease, said Dr. George Bakris, a professor of medicine at the University of Chicago Medicine and an author of the study. Most participants in the trial were already taking medication for chronic kidney disease.
For people with advanced kidney disease, in particular, the findings are promising. “We can help people live longer,” said Dr. Vlado Perkovic, a nephrologist and renal researcher at the University of New South Wales, Sydney, and another author of the study.
While the data shows clear benefits, even the researchers studying drugs like Ozempic aren’t sure how, exactly, they help the kidneys. One leading theory is that semaglutide may reduce inflammation, which exacerbates kidney disease.
And the results come with several caveats: Roughly two-thirds of the participants were men and around two-thirds were white — a limitation of the study, the authors noted, because chronic kidney disease disproportionately affects Black and Indigenous patients. The trial participants taking semaglutide were more likely to stop the drug because of gastrointestinal issues, which are common side effects of Ozempic.
Doctors said they wanted to know whether the drug might benefit patients who have kidney disease but not diabetes, and some also had questions about the potential long-term risks of taking semaglutide.
Still, the results are the latest data to show that semaglutide can do more than treat diabetes or drive weight loss. In March, the F.D.A. authorized Wegovy for reducing the risk of cardiovascular issues in some patients. And scientists are examining semaglutide and tirzepatide, the compound in the rival drugs Mounjaro and Zepbound, for a range of other conditions , including sleep apnea and liver disease.
If the F.D.A. approves the new use, it could drive even more demand for Ozempic, which has faced recurrent shortages .
“I think it’s a game changer,” Dr. Hoenig said, “if I can get it for my patients.”
Dani Blum is a health reporter for The Times. More about Dani Blum
A Close Look at Weight-Loss Drugs
Supplement Stores: GNC and the Vitamin Shoppe are redesigning displays and taking other steps to appeal to people who are taking or are interested in drugs like Ozempic and Wegovy.
Senate Investigation: A Senate committee is investigating the prices that Novo Nordisk charges for Ozempic and Wegovy, which are highly effective at treating diabetes and obesity but carry steep price tags.
A Company Remakes Itself: Novo Nordisk’s factories work nonstop turning out Ozempic and Wegovy , but the Danish company has far bigger ambitions.
Transforming a Small Danish Town: In Kalundborg, population under 17,000, Novo Nordisk is making huge investments to increase production of Ozempic and Wegovy.
Ozempic’s Inescapable Jingle: The diabetes drug has become a phenomenon, and “Oh, oh, oh, Ozempic!” — a takeoff of the Pilot song “Magic” — has played a big part in its story.
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Is College Worth It?
2. public views on the value of a college degree, table of contents.
- Labor force trends and economic outcomes for young adults
- Economic outcomes for young men
- Economic outcomes for young women
- Wealth trends for households headed by a young adult
- The importance of a four-year college degree
- Getting a high-paying job without a college degree
- Do Americans think their education prepared them for the workplace?
- Is college worth the cost?
- Acknowledgments
- The American Trends Panel survey methodology
- Current Population Survey methodology
- Survey of Consumer Finances methodology
We asked Americans what they think about the value of a four-year college degree from a few different angles:
- Is a degree important in order for someone to get a well-paying job in today’s economy?
- Has the value of a degree changed in recent decades?
- Can someone without a degree get a well-paying job?
- How useful do people think their own education was in preparing them for a well-paying job?
- Is the cost of college worth it today?
Four-in-ten Americans say it is not too or not at all important to have a four-year college degree in order to get a well-paying job in today’s economy.
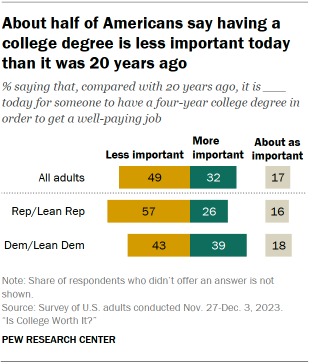
Only 25% say it’s extremely or very important to have a college degree, and 35% say it’s somewhat important.
We also asked the public about the importance of a college degree now versus 20 years ago.
About half of Americans (49%) say it’s less important today than it was in the past for someone to have a four-year degree in order to get a well-paying job. About a third (32%) say having a degree is more important now, and 17% say its importance hasn’t really changed.
Differences by party
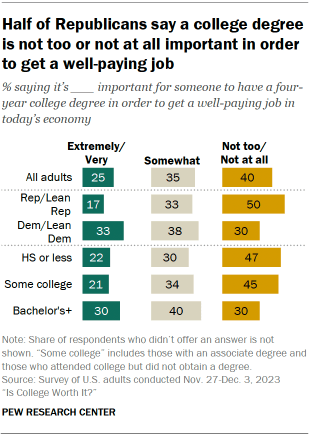
Half of Republicans and Republican-leaning independents – compared with 30% of Democrats and Democratic leaners – say it’s not too or not at all important to have a four-year college degree to get a well-paying job.
And a majority of Republicans (57%) say having a degree is less important today than it was 20 years ago; 43% of Democrats say the same.
These partisan gaps hold even after controlling for differences in the educational attainment of Republicans and Democrats.
Differences by education
College graduates are more likely than those with less education to say that having a college degree is extremely or very important (30% vs. 22%).
But views on whether having a college degree is more or less important today than it was 20 years ago don’t differ significantly by education. Roughly half of four-year college graduates (51%) and those with less education (48%) say it’s less important today for someone to have a college degree than it was in the past.
Adults with a postgraduate degree, however, have somewhat different views than those with a bachelor’s degree on both of these measures. Some 35% of postgraduates say it’s extremely or very important to have a four-year college degree in order to get a well-paying job, compared with 27% of those whose highest attainment is a bachelor’s degree.
And 39% of postgraduates – compared with 30% of those with a bachelor’s degree – say it’s more important to have a college degree today than it was 20 years ago.
Differences by age
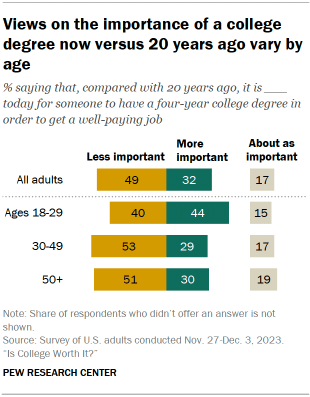
Young adults stand out in their views on the importance of a college degree today versus in the past.
Among those ages 18 to 29, 44% say having a degree is more important today in order to get a well-paying job than it was 20 years ago. By comparison, 29% of those 30 to 49 and 30% of those 50 and older say the same.
Americans also have mixed views when it comes to whether someone without a four-year college degree could get a well-paying job in today’s economy.
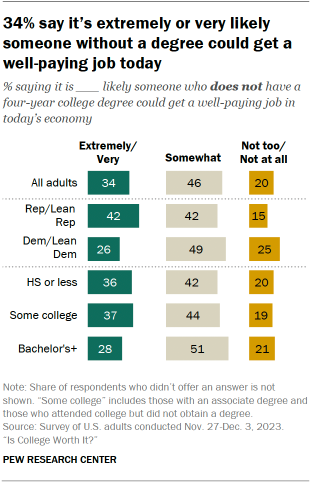
Only about a third (34%) say it’s extremely or very likely that someone withouta four-year degree could get this kind of job.
Nearly half say it’s somewhat likely that someone without a college degree could get a well-paying job, and 20% say it’s not too or not at all likely.
These views differ by:
- Partisanship: 42% of Republicans and 26% of Democrats say it’s extremely or very likely someone without a four-year degree could get a well-paying job. Among Democrats, 25% say it’s not too or not at all likely; just 15% of Republicans say the same.
- Education: 28% of adults with at least a bachelor’s degree say it’s extremely or very likely that someone without a college degree could get a well-paying job today. This compares with 37% of those with some college and 36% of those with a high school diploma or less education.
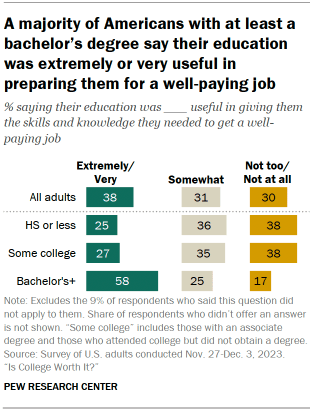
When thinking about how useful their own education was in giving them the skills and knowledge needed to get a well-paying job, a majority of those with a four-year college degree or more education (58%) say it was extremely or very useful. (This finding excludes the 9% of respondents who said this question did not apply to them.)
Adults with a postgraduate degree are especially likely to say their education was extremely or very useful: 72% say this, compared with 47% of those whose highest attainment is a bachelor’s.
By comparison, adults with less education have more mixed views. Among those who have not completed a bachelor’s degree, 38% say their education was not too or not at all useful in giving them the skills and knowledge needed to get a well-paying job; 35% say it was somewhat useful, and 26% say it was extremely or very useful.
These views don’t differ as substantially by age or by party.
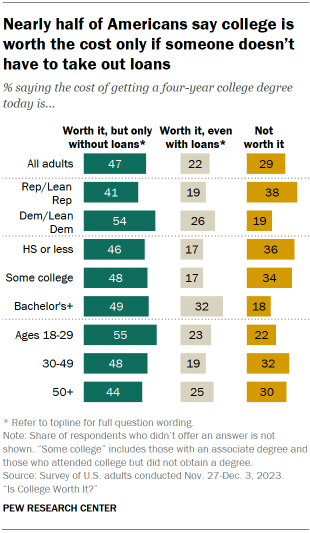
When asked about the cost of college these days, many Americans question whether it’s worth it if a student has to take on debt. Nearly half of adults (47%) say a four-year college degree is worth the cost, but only if someone doesn’t have to take out loans in order to attend.
Only 22% say college is worth the cost even if someone has to take out loans. And 29% say college isn’t worth the cost.
Meanwhile, data from the Federal Reserve shows that more than four-in-ten adults who attended college say they took out student loans for their education .
Views on the value of college differ by partisanship, education and age. But notably, in all groups except for Republicans, pluralities say the cost of college is worth it only if someone doesn’t have to take out loans.
A narrow majority of Democrats (54%) say the cost of getting a four-year college degree is worth it, but only if someone doesn’t have to take out loans. A smaller share of Republicans (41%) say the same.
About one-in-four Democrats (26%), compared with 19% of Republicans, say the cost is worth it even with loans.
Republicans are twice as likely as Democrats to say college is not worth the cost (38% vs. 19%).
Americans with at least a four-year college degree are much more likely than those with less education to say that college is worth the cost even if someone has to take out loans (32% vs. 17%).
Those with a postgraduate degree are among the most likely to express this view: 37% say college is worth the cost even after taking out loans. This compares with 29% among those with a bachelor’s but no postgraduate degree.
Even so, across all education levels, more say a four-year degree is worth the cost only if someone doesn’t take on debt than say it’s worth the cost with debt.
Those with some college or less education are about twice as likely as those with at least a bachelor’s degree to say the cost of getting a degree isn’t worth it at all (35% vs. 18%).
Young adults are more likely than their older counterparts to say the cost of a degree is worth it only if someone doesn’t take out loans: 55% of those ages 18 to 29 say this, compared with 48% of those 30 to 49 and 44% of those 50 and older.
And 18- to 29-year-olds are less likely to say the cost isn’t worth it at all (22% vs. roughly three-in-ten among older age groups).
Sign up for our weekly newsletter
Fresh data delivery Saturday mornings
Sign up for The Briefing
Weekly updates on the world of news & information
- Business & Workplace
- Economic Conditions
- Higher Education
- Income & Wages
- Recessions & Recoveries
- Student Loans
Half of Latinas Say Hispanic Women’s Situation Has Improved in the Past Decade and Expect More Gains
From businesses and banks to colleges and churches: americans’ views of u.s. institutions, fewer young men are in college, especially at 4-year schools, key facts about u.s. latinos with graduate degrees, private, selective colleges are most likely to use race, ethnicity as a factor in admissions decisions, most popular, report materials.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Language selection
- Français fr
Government of Canada invests in cutting-edge research and the next generation of scientists
From: Employment and Social Development Canada
News release
Today, while visiting the Kids Brain Health Network’ facility in Surrey, the Honourable Terry Beech, Minister of Citizens’ Services, on behalf of the Honourable François-Philippe Champagne, Minister of Innovation, Science and Industry, and the Honourable Mark Holland, Minister of Health, highlighted the government’s support for third-party science and research organizations through the Strategic Science Fund (SSF), including the investments in the work of the Kids Brain Health Network (KBHN) and the Community Circle on Scaling Business Innovation for Humanity.
More than $800 million in funding will go to 24 science and research organizations across Canada May 26, 2024 Surrey, British Columbia Employment and Social Development Canada Today, while visiting the Kids Brain Health Network’ facility in Surrey, the Honourable Terry Beech, Minister of Citizens’ Services, on behalf of the Honourable François-Philippe Champagne, Minister of Innovation, Science and Industry, and the Honourable Mark Holland, Minister of Health, highlighted the government’s support for third-party science and research organizations through the Strategic Science Fund (SSF), including the investments in the work of the Kids Brain Health Network (KBHN) and the Community Circle on Scaling Business Innovation for Humanity. As announced in December 2023, the SSF supports the work of 24 organizations, which were awarded through a new competitive, merit-based, and transparent process, informed by the advice of an independent expert review panel. These organizations span Canada’s science and research landscape and are making contributions in a range of crucial areas, including researching and developing health care solutions, supporting Indigenous inclusion and research, addressing climate change, supporting Arctic science and research, making advancements in emerging technologies such as quantum computing and artificial intelligence, promoting STEM education among young people, and facilitating learning and training opportunities for post-secondary students. Canada’s scientists and researchers are working to solve some of the world’s greatest challenges for the benefit of us all. Their innovations and discoveries are the foundation of Canadian economic growth and prosperity, as well as the health and well-being of people in Canada. That is why the Government of Canada has decided to invest $800 million in the SSF and will continue to make investments to boost research and innovation and ensure Canada remains a leader in innovation, research, and new technologies.
“Canada is renowned globally for its groundbreaking science and innovation. The Strategic Science Fund ensures Canada remains a leader in tackling some of the world's most challenging problems while also attracting the best talent and expertise. Our government embraces science, research, and evidence in policymaking, which leads to greater health outcomes and well-being for Canadians.” – The Honourable Terry Beech, Minister of Citizens’ Services
“Science and research are the cornerstones of Canada’s economic well-being and progress. Canada’s researchers work to expand our understanding of the world, and they generate new ideas to solve some of the biggest challenges of our time. With this investment through the Strategic Science Fund, the Government of Canada is continuing its support for world-class, cutting-edge research and for those who work to inspire and train the next generation.” – The Honourable François-Philippe Champagne, Minister of Innovation, Science and Industry
“By investing in health organizations through the Strategic Science Fund, we are advancing Canadian research and knowledge that will improve health outcomes across the country. This funding supports innovative medical treatments, advanced biotechnological applications, genomic science, regenerative medicine, and research into cancer and brain health. By deepening our understanding of health challenges and supporting science-based solutions, we are investing in the well-being of people in Canada.” – The Honourable Mark Holland, Minister of Health
Quick facts
The creation of the Strategic Science Fund (SSF) was announced in Budget 2019 as a way to make federal investments in third-party science and research more effective by assessing applicants using a framework of principles for allocating federal funding.
Since 2016, the government has provided more than $16 billion to support science and research.
In addition, Budget 2024 provides $825 million to increase support for master’s, doctoral and post-doctoral students, as well as $1.8 billion to the federal granting councils to increase core research grant funding and support Canadian researchers.
Budget 2024 also includes investments in modern, high-quality research facilities and infrastructure to help solve real-world problems, create economic opportunities, and attract and train the next generation of scientific talent.
The next call for applications to the SSF is scheduled to take place in 2026–2027. Funding from the current competition will be disbursed from April 2024 to March 2029, pending finalization of contribution agreements.
The Kids Brain Health Network (KBHN) is one of the 24 selected organizations. KBHN is a national research network focus on kids’ brain development and neurodevelopmental disabilities. KBHN can receive up to $17 million from the SSF.
Another selected organization is the Community Circle on Scaling Business Innovation for Humanity, which collaborates with Indigenous and rural communities to develop and implement innovative, sustainable solutions for water-health challenges through a unique, community-centric problem-solving methodology. The Circle is entitled to receiving up to $2.8 million in SSF funding.
Associated links
- List of recipients and funding amounts
Teodor Gaspar Press Secretary Office of the Minister of Citizens’ Services, Terry Beech [email protected] Media Relations Office Employment and Social Development Canada 819-994-5559 [email protected] Follow us on X (Twitter) Audrey Millette Press Secretary Office of the Minister of Innovation, Science and Industry [email protected] Media Relations Innovation, Science and Economic Development Canada [email protected] Christopher Aoun Press Secretary Office of the Minister of Health 613-291-4176 Media Relations Health Canada 613-957-2983 [email protected] Stay connected Find more services and information at Canada.ca/ISED . Follow Canadian Science on social media. X (Twitter): @CDNScience | Facebook: Canadian Science | Instagram: @cdnscience
Page details
Scientists Discover New Potential Glaucoma Treatment
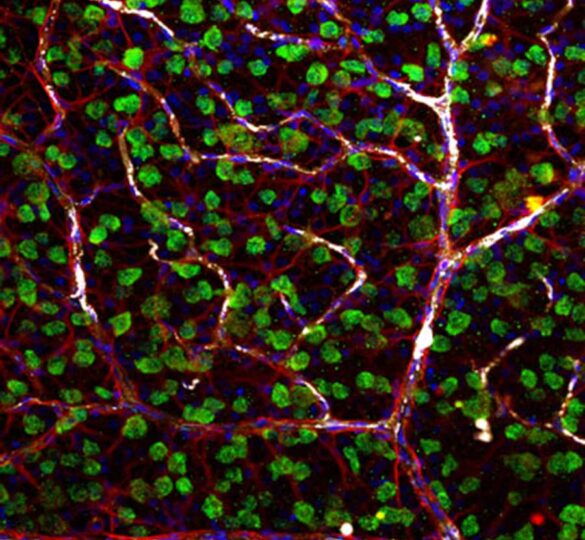
Vision scientists have discovered that naturally occurring molecules known as lipid mediators have the potential to halt the progression of glaucoma.
Vision scientists at UC Berkeley and the University of Toronto have discovered that naturally occurring molecules known as lipid mediators have the potential to halt the progression of glaucoma, the world’s second-leading cause of blindness.
Their findings, published in November 2017 in the online edition of the Journal of Clinical Investigation , mark an important step forward in the pursuit of a cure for glaucoma.
At present, there is no cure for glaucoma, which is estimated to affect 80 million people worldwide.
“Not only could this discovery lead to drugs to treat glaucoma, but the same mechanism, and options for prevention, may be applicable to other neurodegenerative diseases,” said study senior author Karsten Gronert, Professor of Optometry and Chair of Vision Science at UC Berkeley.
Using a model of glaucoma, Gronert and fellow researchers found that inflammation-regulating lipid mediators known as lipoxins secreted from star-shaped cells known as astrocytes stopped the degeneration of retinal ganglion cells. Ganglion cells are the neurons of the retina and optic nerve that receive information from photoreceptors.
“We’ve taken something everyone assumed was anti-inflammatory, and found that these same small molecules play a key role in neuroprotection, which is really exciting,” said study co-senior author John Flanagan, Dean and Professor of Optometry. Much of the study was conducted at UC Berkeley.
Specifically, researchers found that astrocytes, which help maintain brain function and form the nerve fiber layer of the retina and optic nerve, release therapeutic biological agents known as lipoxins A4 and B4, but only when the astrocytes are at rest and maintaining nerve function.
“It is commonly assumed that astrocytes activated by injuries release stress signals that kill off ganglion cells in the retina, causing optic nerve damage,” said Flanagan. “However, our research discovered that astrocytes that are triggered by injury actually turn off novel neuroprotective signals that prevent optic nerve damage.”
Researchers discovered secretions of lipoxins A4 and B4 in resting astrocytes in culture in the retina and optic nerve head. “This little-known lipid mediator has shown the potential to reverse cell death,” Gronert said. “We know of no drug that can do this.”
For decades, pharmaceutical companies have searched for neuroprotective drugs to treat glaucoma and other disorders marked by the death of nerve cells such as Alzheimer’s, Parkinson’s and ALS. Glaucoma is by far the most prevalent of these neurodegenerative diseases.
“At the same time, lipoxins have been explored as promising drug targets for treating inflammatory diseases, but nobody has been looking at them as being neuroprotective,” Gronert said. At present, the treatment option for glaucoma is to lower ocular pressure, but there are no effective treatments for preventing or stopping the neurodegeneration of glaucoma, which is irreversible and eventually can lead to blindness, Flanagan said.
The study authors are excited at the prospect of further investigations into the therapeutic benefits and mechanisms of lipoxins A4 and B4 and their potential to stop or reverse neural damage. They have jointly filed a patent application for use of lipoxins A4 and B4 to treat glaucoma and neurodegenerative diseases. Their eventual goal is to test the lipoxins as drugs in humans.
“These naturally occurring small lipids have great potential as therapies because they may play a fundamental role in preventing other neurodegenerative diseases. And that’s hugely significant, ” Flanagan said.
Source: UC Berkeley News
Pictured above: Laboratory photo of Retinal ganglion cells (green) connecting with astrocytes (red) and blood cells (white) in the inner retina. (Photo by Jeremy Sivak/University of Toronto)
First posted on December 18, 2017; Reviewed on May 13, 2022

COMMENTS
The U.S. Food and Drug Administration has approved a new treatment for glaucoma, iDose® TR (travoprost intracameral implant, 75 mcg). iDose TR is a first-of-its kind treatment that is designed to provide up to three years of 24/7, continuous drug therapy directly inside the eye, helping people with glaucoma take control over the elevated eye pressure associated with this vision disease.
Using gene editing, the scientists in the study developed new models of glaucoma in mice that resembled primary congenital glaucoma. By injecting a new, long-lasting and non-toxic protein treatment (Hepta-ANGPT1) into mice, the scientists were able to replace the function of genes that, when mutated, cause glaucoma. ... and Research to Prevent ...
The most extensive genome-wide association study of glaucoma to date compared the genes of 34,179 people with the disease to 349,321 control participants. It enabled an international consortium of researchers to identify 44 new gene loci ("genetic street addresses" that denote a specific location on a gene). It confirmed 83 previously ...
Xen-DS: a novel technique of ab externo Xen implantation augmented with a modified deep sclerectomy for surgical treatment of glaucoma. A. Elbably. J. Richardson-May. A. Jacob. Research 21 May ...
The treatment had multiple beneficial effects on the eye. First, it promoted nerve regeneration following optic-nerve injury in mice with damaged optic nerves. Second, it reversed vision loss in animals with a condition mimicking human glaucoma. And third, it reversed vision loss in aging animals without glaucoma.
Glaucoma Research Foundation is dedicated to scientific research that deepens our understanding of glaucoma, generates new treatments, and will ultimately lead to a cure. Catalyst for a Cure (CFC) is Glaucoma Research Foundation's flagship research program. We are currently funding two CFC research teams.
Glaucoma Research Foundation is dedicated to scientific research that deepens our understanding of glaucoma, generates new treatments, and will ultimately lead to a cure. ... A New Path for Glaucoma Patients" was the topic of the 2022 Weston Family Lecture presented virtually on October 27, 2022. Neurodegeneration Explained
Indiana University School of Medicine researchers have identified a new therapeutic target that could lead to more effective treatment of glaucoma. Glaucoma is a neurodegenerative disease that ...
FULL STORY. A new, detailed genetic roadmap of glaucoma -- the world's leading cause of irreversible blindness -- will help researchers develop new drugs to combat the disease, by identifying ...
Glaucoma can be defined as a progressive optic neuropathy that induces optic disc cupping and retinal ganglion cell apoptosis. 1 As the world's leading cause of irreversible blindness, the disease currently affects 3.5% of individuals aged between 40 and 80 years. The incidence of glaucoma is increasing, together with life expectancies, in resource-limited countries, and nearly 112 million ...
Grantee. Researchers at Indiana University School of Medicine are using a novel approach to hopefully develop a new therapy for glaucoma, a complex disease that eventually leads to blindness, thanks to a new five-year, $2 million R01 grant from the National Eye Institute. The project, led by Tasneem Sharma, Ph.D. is called "Therapeutic ...
Dry eye and glaucoma may be the two most confounding conditions ophthalmologists face. Late last year, the US Food and Drug Administration (FDA) approved three new treatments for dry eye disease ...
Glaucoma is a group of eye diseases that can cause vision loss and blindness by damaging a nerve in the back of your eye called the optic nerve. The symptoms can start so slowly that you may not notice them. The only way to find out if you have glaucoma is to get a comprehensive dilated eye exam. There's no cure for glaucoma, but early ...
Most research to date on the connection between the vascular and nervous systems has been limited by technology that only allows scientists to take two-dimensional pictures. But Duan and Toma benefited from a new technique ... K08EY033030, and R01EY030138), NINDS (R35NS097305) and the Glaucoma Research Foundation. Topics. Biomedical Imaging;
The iris may block the drainage angle and cause a rapid buildup of eye pressure. Both types of glaucoma involve damage to the optic nerve, which can lead to vision loss and blindness. Around 10% ...
While glaucoma manifests as a gradual loss of retinal ganglion cells (RGCs), its etiology remains elusive despite extensive research efforts. Age serves as a prominent risk factor, with ...
This study aims to determine the risk of ACG and open angle glaucoma (OAG) among users of these treatments. This is a retrospective cohort study with a case control analysis using the PharMetrics ...
Glaucoma Research Foundation is dedicated to scientific research that deepens our understanding of glaucoma, generates new treatments, and will ultimately cure a disease that is the second leading cause of blindness. Research takes resources. That's why, for more than 40 years, we have rallied financial support for science with the potential ...
Results: In all groups, the AST, SC, and TM measurements were similar ( P >0.05). In the PXG group, SS lengths in the temporal area were shorter than those in the control and PXS groups ( P =0.012). There were significant correlations between TM length and AST in the PXG group ( P <0.05). The SS length exhibited moderately positive correlations ...
In the new research, Fralin Biomedical Research Institute scientists found that in some brain cancer patients who didn't respond to treatment, levels were high of a specific form of the signaling ...
It's hitting the wealthy disproportionately, new research shows. Inflation peaked at 9.1% in June 2022, and has recently dropped to 3.4% in April, according to data collated by TradingEconomics .
But a new study from Scripps Research is shedding light on the molecular drivers that could contribute to Alzheimer's progression. In the study, published in Advanced Science on May 21, 2024, the researchers used a new technique for studying single, living brain cells affected by Alzheimer's disease. By measuring the electrical activity of ...
Only 22% say the cost of getting a four-year college degree today is worth it even if someone has to take out loans. Some 47% say the cost is worth it only if someone doesn't have to take out loans. And 29% say the cost is not worth it. These findings come amid rising tuition costs and mounting student debt. Views on the cost of college ...
0:56. Newly published research could help predict when there will be "powerful solar storms." According to Northwestern's McCormick School of Engineering, an international team of researchers ...
May 24, 2024. Semaglutide, the compound in the blockbuster drugs Ozempic and Wegovy, dramatically reduced the risk of kidney complications, heart issues and death in people with Type 2 diabetes ...
Differences by age. Young adults stand out in their views on the importance of a college degree today versus in the past. Among those ages 18 to 29, 44% say having a degree is more important today in order to get a well-paying job than it was 20 years ago. By comparison, 29% of those 30 to 49 and 30% of those 50 and older say the same.
The creation of the Strategic Science Fund (SSF) was announced in Budget 2019 as a way to make federal investments in third-party science and research more effective by assessing applicants using a framework of principles for allocating federal funding.. Since 2016, the government has provided more than $16 billion to support science and research.
Vision scientists at UC Berkeley and the University of Toronto have discovered that naturally occurring molecules known as lipid mediators have the potential to halt the progression of glaucoma, the world's second-leading cause of blindness. Their findings, published in November 2017 in the online edition of the Journal of Clinical ...