

कोविड-19 के दौरान स्वास्थ्य और कुशलता
मौजूदा गतिरोध के दरमियान, हम सब के लिए स्वस्थ जीवनशैली कायम रखना बहुत मुश्किल हो गया है। वित्तीय मामलों, बच्चों की देख-भाल, बुजुर्ग माता-पिता, नौकरी की सुरक्षा पर आए संकट आदि से जुड़ी अनिश्चितता और चिंताओं ने हमारी जीवनचर्या, जीवनशैली और मानसिक स्वास्थ्य सभी को अस्त-व्यस्त कर दिया है। भविष्य की अनिश्चितता, अनवरत चल रही न्यूज कवरेज और सोशल मीडिया पर लगातार आते संदेशों की बाढ़ से हमारी चिंता का बढ़ जाना स्वभाविक है। ऐसी स्थितियों में तनाव होना सामान्य है। तनाव से हमारे सोने और खाने-पीने की आदत बदल जाती है, इससे चिड़चिड़ापन या भावनात्मक ज्वार आता है, मानसिक संबल घट जाता है और लोग शराब या दूसरी लत में पड़ने लगते हैं। अगर आप ऐसा कुछ महसूस कर रहे हैं तो मदद हासिल करने से हिचकिचाएं नहीं।* स्वस्थ जीवनशैली अपनाए रखना और अपनी पुरानी जीवनचर्या में लौट आना भी बहुत महत्वपूर्ण है।
तनाव से निपटने और अपने मानसिक, शारीरिक व सामाजिक स्वास्थ्य को कायम रखने के कुछ नुस्खे-
*भारत – राष्ट्रीय मानसिक स्वास्थ्य और तंत्रिका विज्ञान संस्थान (निमहांस) ने स्वास्थ्य और परिवार कल्याण मंत्रालय के साथ साझेदारी में यह मानसिक-सामाजिक टोल-फ्री हेल्पलाइन नंबर 08046110007 शुरू किया है।

मानसिक स्वास्थ्य

शारीरिक स्वास्थ्य

सामाजिक स्वास्थ्य
- connect with us
- 1800-572-9877
- [email protected]
- We’re on your favourite socials!

Frequently Search
Couldn’t find the answer? Post your query here
- अन्य आर्टिकल्स
कोरोना वायरस पर निबंध (Essay on Coronavirus in Hindi) - Covid-19 महामारी पर हिंदी में निबंध
Updated On: January 09, 2024 05:14 pm IST
- कोरोना वायरस पर निबंध (Essay on Coronavirus in Hindi) 100, …
- कोरोना वायरस पर निबंध (Essay on Coronavirus in Hindi) 100 …
- कोरोना वायरस पर निबंध (Essay on Coronavirus in Hindi) 200 …
- कोरोना वायरस पर निबंध (Essay on Coronavirus in Hindi) 500 …
- कोरोना वायरस पर निबंध 10 लाइन हिंदी में (Essay on …

कोरोना वायरस पर निबंध (Essay on Coronavirus in Hindi) 100, 200 और 500 शब्दों में
कोरोना वायरस पर निबंध (essay on coronavirus in hindi) 100 शब्दों में , कोरोना वायरस पर निबंध (essay on coronavirus in hindi) 200 शब्दों में, कोरोना वायरस पर निबंध (essay on coronavirus in hindi) 500 शब्दों में, covid-19 पर निबंध - प्रस्तावना , कोरोना वायरस की उत्पत्ति, कोरोना वायरस से बचाव के उपाय.
- अपने हाथों को बार-बार धोएं। हाथ धोने से कोरोना वायरस के फैलने का जोखिम कम हो जाता है। हाथों को कम से कम 20 सेकंड तक साबुन और पानी से धोना चाहिए। यदि साबुन और पानी उपलब्ध नहीं हैं, तो अल्कोहल-आधारित हैंड सैनिटाइज़र का उपयोग किया जा सकता है।
- संक्रमित व्यक्ति से दूर रहें। कोरोना वायरस संक्रमित व्यक्ति के खांसने या छींकने से निकलने वाले महीन बूंदों के माध्यम से फैलता है। यदि आप किसी ऐसे व्यक्ति के संपर्क में हैं जो संक्रमित है, तो अपने लक्षणों पर ध्यान दें और यदि आपके कोई लक्षण दिखाई दें तो तुरंत चिकित्सा सहायता लें।
- सार्वजनिक स्थानों पर मास्क पहनें। मास्क पहनने से कोरोना वायरस के फैलने से बचाव में मदद मिल सकती है।
- अपने चेहरे को छूने से बचें। अपने चेहरे को छूने से कोरोना वायरस आपके शरीर में प्रवेश कर सकता है।
- स्वस्थ आहार खाएं, पर्याप्त नींद लें और नियमित रूप से व्यायाम करें।
- भीड़-भाड़ वाले स्थानों पर जाने से बचें।
- सार्वजनिक परिवहन का उपयोग करने से बचें।
COVID-19 पर निबंध - निष्कर्ष
कोरोना वायरस पर निबंध 10 लाइन हिंदी में (essay on coronavirus in 10 lines in hindi) .
- कोरोना वायरस उन वायरस के समूह से है जो बहुत तेजी से संक्रमित करते हैं।
- कोरोना वायरस की शुरुआत चीन के वुहान शहर से हुई जहां इसे इंसानों ने बनाया।
- भारत में कोरोना वायरस का पहला मामला जनवरी 2020 में सामने आया था।
- कोरोना वायरस खांसने और छींकने से फैलता है और खांसते और छींकते समय हमें अपना मुंह और नाक ढक लेना चाहिए।
- हमें अपनी सुरक्षा के लिए मास्क पहनना चाहिए और अपने हाथों को नियमित रूप से साफ करना चाहिए।
- हमारी सुरक्षा के लिए, सरकार ने इस वायरस के प्रसार को रोकने के लिए पूरे देश को बंद कर दिया था।
- कोरोना वायरस के कारण स्कूल को ऑनलाइन कर दिया गया था और छात्र घर से पढ़ाई करते थे।
- कोरोना वायरस के कारण लॉकडाउन में सभी लोग घर पर थे।
- इस दौरान बहुत से लोगों ने अपने परिवार के सदस्यों के साथ खूब समय बिताया।
- खुद को सुरक्षित रखने के लिए नियमित रूप से हाथ धोना और चेहरे पर मास्क पहनना बहुत जरूरी है।
Are you feeling lost and unsure about what career path to take after completing 12th standard?
Say goodbye to confusion and hello to a bright future!
क्या यह लेख सहायक था ?
सबसे पहले जाने.
लेटेस्ट अपडेट प्राप्त करें
क्या आपके कोई सवाल हैं? हमसे पूछें.
24-48 घंटों के बीच सामान्य प्रतिक्रिया
व्यक्तिगत प्रतिक्रिया प्राप्त करें
बिना किसी मूल्य के
समुदाय तक पहुंचे
समरूप आर्टिकल्स
- मदर्स डे पर निबंध (Mothers Day Essay in Hindi): मातृ दिवस पर हिंदी में निबंध
- शिक्षक दिवस पर निबंध (Teachers Day Essay in Hindi) - टीचर्स डे पर 200, 500 शब्दों में हिंदी में निबंध देखें
- दिल्ली विश्वविद्यालय (डीयू) में साउथ कैंपस कॉलेजों की लिस्ट (List of South Campus Colleges in DU): चेक करें टॉप 10 रैंकिंग
- लेक्चरर बनने के लिए करियर पथ (Career Path to Become a Lecturer): योग्यता, प्रवेश परीक्षा और पैटर्न
- KVS एडमिशन लिस्ट 2024-25 (प्रथम, द्वितीय, तृतीय) की जांच कैसे चेक करें (How to Check KVS Admission List 2024-25How to Check KVS Admission List 2024-25 (1st, 2nd, 3rd): डायरेक्ट लिंक, लेटेस्ट अपडेट, क्लास 1 उच्च कक्षा के लिए स्टेप्स
- 2024 के लिए भारत में फर्जी विश्वविद्यालयों की नई लिस्ट (Fake Universities in India): कहीं भी एडमिशन से पहले देख लें ये सूची
नवीनतम आर्टिकल्स
- 100% जॉब प्लेसमेंट वाले टॉप इंस्टिट्यूट (Top Institutes With 100% Job Placements): हाई पैकेज, टॉप रिक्रूटर यहां दखें
- हरियाणा पॉलिटेक्निक परीक्षा 2024 (Haryana Polytechnic Exam 2024): यहां चेक करें संबंधित तारीखें, परीक्षा पैटर्न और काउंसलिंग प्रोसेस
- यूपी पुलिस सिलेबस 2024 (UP Police Syllabus 2024 in Hindi) - सिपाही, हेड कांस्टेबल भर्ती पाठ्यक्रम हिंदी में देखें
- 10वीं के बाद डिप्लोमा कोर्स (Diploma Courses After 10th): मैट्रिक के बाद बेस्ट डिप्लोमा कोर्स, एडमिशन, फीस और कॉलेज की लिस्ट देखें
- पर्यावरण दिवस पर निबंध (Essay on Environment Day in Hindi) - विश्व पर्यावरण दिवस पर हिंदी में निबंध कैसे लिखें
- भारत में पुलिस रैंक (Police Ranks in India): बैज, स्टार और वेतन वाले पुलिस पद जानें
- जेएनवीएसटी रिजल्ट 2024 (JNVST Result 2024): नवोदय विद्यालय कक्षा 6वीं और 9वीं का रिजल्ट
- 10वीं के बाद सरकारी नौकरियां (Government Jobs After 10th) - जॉब लिस्ट, योग्यता, भर्ती और चयन प्रक्रिया की जांच करें
- 10वीं के बाद आईटीआई कोर्स (ITI Courses After 10th in India) - एडमिशन प्रोसेस, टॉप कॉलेज, फीस, जॉब स्कोप जानें
- यूपीएससी सीएसई मेन्स पासिंग मार्क्स 2024 (UPSC CSE Mains Passing Marks 2024)
नवीनतम समाचार
- CBSE 12th टॉपर्स 2024 लिस्ट: राज्य और स्ट्रीम-वार टॉपर के नाम, मार्क्स प्रतिशत देखें
- CBSE 12th रिजल्ट 2024 लिंक एक्टिव: आसानी से डाउनलोड करें इंटर की मार्कशीट
- MP Board 10th Toppers 2024 List Available: MPBSE 10वीं के डिस्ट्रिक्ट वाइज टॉपर्स की लिस्ट देखें
ट्रेंडिंग न्यूज़

Subscribe to CollegeDekho News
- Select Stream Engineering Management Medical Commerce and Banking Information Technology Arts and Humanities Design Hotel Management Physical Education Science Media and Mass Communication Vocational Law Others Education Paramedical Agriculture Nursing Pharmacy Dental Performing Arts
कॉलेजदेखो के विशेषज्ञ आपकी सभी शंकाओं में आपकी मदद कर सकते हैं
- Enter a Valid Name
- Enter a Valid Mobile
- Enter a Valid Email
- By proceeding ahead you expressly agree to the CollegeDekho terms of use and privacy policy
शामिल हों और विशेष शिक्षा अपडेट प्राप्त करें !
Details Saved

Your College Admissions journey has just begun !
Try our AI-powered College Finder. Feed in your preferences, let the AI match them against millions of data points & voila! you get what you are looking for, saving you hours of research & also earn rewards
For every question answered, you get a REWARD POINT that can be used as a DISCOUNT in your CAF fee. Isn’t that great?
1 Reward Point = 1 Rupee
Basis your Preference we have build your recommendation.

Vikram Patel: India’s Mental Health, Before and During COVID-19
Oct 21, 2020 | Announcements , Faculty , India , News

Around the world, the COVID-19 pandemic has hit communities hard, with many people suffering from the virus itself, facing unemployment, or unable to interact with family and friends. As time goes on, the effects of the pandemic are not limited to just our physical health, but have impacted our mental health, as well.
We spoke with Vikram Patel, the Pershing Square Professor of Global Health in the Department of Global Health and Social Medicine at Harvard Medical School, to learn more about the status of mental health in India and South Asia at large, both before and during the pandemic.
Professor Patel will take part in an upcoming seminar on November 9, “The Impact of COVID-19 on Mental Health in China, India, and the United States,” alongside other panelists from Harvard University, Shanghai Jiao Tong University, and Central South University, to compare the current state of mental health across countries.

Can you tell us a little about what you are currently researching?
My main focus has been on scaling-up approaches that we have demonstrated are effective in improving access to quality mental health care — principally, the delivery of psychosocial interventions by frontline providers, such as community health workers, for the prevention and treatment of mental health problems. Much of my work is centered on translating the robust implementation science findings into real-world impact.
In general, how would you summarize the status of mental health in India? What is the prevalence of mental health issues in the region?
Even before the pandemic, we had very good data to inform our understanding of the burden of mental health problems in India, mainly from the Government of India’s National Health Survey conducted about 3 years ago with a large representative sample of over 30,000 participants from around the country.
The survey showed that about 10% of India’s adult population met clinical criteria for a mental health disorder. That would translate to anywhere from 70-100 million people at the time of the survey. The survey also showed that the most common problems were mood and anxiety disorders, and that very high proportions of persons affected had neither received nor sought any kind of care in the previous twelve months, approaching nearly 90% for the mood and anxiety disorders.
What are the challenges in addressing mental health disorders in India? Are there differences in the approach to mental healthcare across countries of South Asia?
I think there are a lot of similarities in the challenges and opportunities for addressing mental health problems in the different countries of South Asia. The countries share a similar social, historical, and cultural context. Of course, there are also some differences too, but I think the similarities are far greater. From my first-hand experience in India, the barriers to addressing mental health disorders can be categorized in two buckets. The first are supply-side barriers, notably the inadequate number of healthcare workers skilled to provide mental health care. The fact that there are more psychiatrists of Indian origin working in the US than in India itself gives us a sense of the enormous shortage of mental health practitioners. Even these few practitioners are located in urban areas and in the private sector, which negatively affects access to mental healthcare by rural and low-income communities.
There is also the demand-side barrier: communities are reluctant to access mental healthcare, which has been historically organized in a way that is heavily influenced by biomedical framing of “diagnoses, doctors, and drugs.” For the general population, such a framing is foreign to their understanding of mental health issues. Furthermore, most psychiatric beds are located in mental hospitals, built during the colonial era and associated with coercion, removal from society, and sedative medication. This history and imagery has contributed to the stigma about seeking mental healthcare.
Have you observed differences or similarities in how mental health issues impact low-, middle-, and high-income countries?
My main research into mental health focuses on African and South Asian contexts. Based on this experience and my clinical practice in four countries, I have observed that the core phenomena that characterize broad categories of mental health disorders are remarkably similar across contexts and cultures — and, besides, there are similarities in how people respond to interventions. Thus, mental health disorders are universal health experiences with similar “core” features and responses to interventions.
That said, culture and context greatly influence the way mental health disorders are experienced, understood, and responded to, and thus mental healthcare must embrace a diversity of perspectives, experiences, and providers.
How can South Asia’s governments and communities improve efforts toward addressing mental health?
We must move away from the narrow binary biomedical approach to mental health. Each and every one of us must value our own mental health, which is best understood as a dimension, as opposed to only being concerned about suffering from a mental health disorder.
The binary approach of diagnoses and disorders works well for infectious diseases, but not for mental health. If we approach our thinking about mental health across a dimension, we see that there is a range of actions each of us can engage in, from promotion and prevention to care and recovery. The need of the hour is to scale up what works.
There is robust evidence on the effective delivery of psychosocial intervention by frontline workers in community and primary care settings. For people with serious mental illnesses, like schizophrenia, healthcare workers need to think more about ways for social inclusion, and work must be done toward the elimination of coercion and involuntary treatment. And, of course, we must invest in prevention by targeting adverse environments, especially in childhood and adolescence.
You have an upcoming event in November that will delve into the impact of COVID-19 in China, the US, and India. How would you summarize the impact of COVID-19 on mental health in India?
COVID has helped bring the issue of mental health out of the shadows, which is a very welcome development. Much of this attention has been focused on mood and anxiety problems, triggered by the uncertainty and a growing sense of frustration in the face of the pandemic.
The truth is that uncertainty is affecting everyone, but its impact is disproportionate across populations. Low-income or disadvantaged communities have been much worse hit, for example, due to the potential loss of income and work. This has led to significant adverse mental health consequences, and I fear that this will lead to a steep increase in mental health problems throughout the vulnerable communities of India.
Additionally, during lockdown, many routine healthcare services shut down. People with serious mental illnesses rely on routine care. The shutdown spells disaster for people who need such continuing care. Though the impact has not yet been documented, I fear a steep increase of relapses in this vulnerable group of persons.
Have there been changes in India regarding the approach to mental health since the onset of COVID-19?
It’s been a bit of a mixed picture. On one hand, there is a lot of community action that is being led by frontline workers, civil society organizations, and NGOs — India’s greatest assets. These groups are working across the country, and they are sometimes the only source of support for marginalized communities.
On the other hand, it has been a sorry tale of disregard for the disproportionate impact of lockdown and the pandemic on rural, marginalized, and low-income populations. When the definitive history of the pandemic response around the world and in India is written, what will stand out is this disregard by the privileged, from politicians and bureaucrats to the wealthy and even some scientists, to the devastating impact of lockdown on the millions who are voiceless.
What are your top recommendations to care for one’s own mental health during the pandemic? What are your main concerns?
I think uncertainty is the main stressor that has been affecting people everywhere — including here in the US. Uncertainty is part of the human condition, and from an evolutionary perspective, humans are geared to respond to uncertainty in ways that protect ourselves. In times like these, however, when uncertainty is chronic, pervasive, unanticipated, there is no sense of when it will end, and when every day seems to bring more bad news, combined with concerns about upcoming elections, political polarization, and climate change, these uncertainties significantly affect mental health.
So, how do we mitigate the adverse effects of these uncertainties on our mental health? We can’t simply wish it away. There are certain things that can be done to help: maintain a routine and structure in your day and minimize the time reading or watching news — as the media deals with so many negatives. Be as aware of your mental health as you are of your physical health, and acknowledge distress and speak to a trusted person when you are distressed. Focus on the present; there is little to be gained by worrying about the future. Meditate, exercise, and do things that are meaningful to yourself and others around you. Right now, it’s a great time to get into community action; it’s something that is desperately needed and can build and enhance your well-being.
In the coming weeks and months, what is needed to avert a mental health crisis in South Asia or even around the world?
I’m extremely concerned about the global mental health crisis that we will face. Even before the pandemic, there was significant, robust data that showed worsening mental health, especially in young people, around the world, and in the US suicide mortality has increased 50% in last decade in this demographic.
The pandemic with its uncertainties and the economic recessions will likely cause this burden of mental health problems to worsen. Even before the pandemic, mental healthcare was not fit for purpose. We now have a historic and urgent opportunity to reimagine the future of mental healthcare. There is always the call for more investment, but that must be guided by the best science on what is cost effective in mental healthcare. We must also pay attention to a human rights perspective, which necessitates us to deliver healthcare in a way that always respects and protects a person’s dignity. ☆
———
Join us on Monday, November 9 at 8:15 PM EST to listen to Vikram Patel and others discuss the impact of COVID-19 on mental health in China, India, and the United States.
Register via zoom : https://harvard.zoom.us/webinar/register/wn_cldc-z0uqsuno0ykyonf5g.
☆ All opinions expressed by our interview subjects are their own and do not reflect the views of the Mittal Institute and its staff.
Recent Posts
- A Look Back on Mittal Institute’s Spring Flagship Events: May 2-3, 2024
- Aisha Kokan ’26 Studied Mental Health in India through LMSAI Grant
- Storykit Program Inspires Academic Excellence in Pakistan Schools
- Annual Symposium Preview: Genetics and Medicine
- Annual Symposium Preview: Understanding Climate in South Asia
Yearly Archive
- Afghanistan
- Announcements
- Arts at LMSAI
- India Seminar Series
- Arts at SAI
- Graduate Student Associates
- South Asia in the News
- Research Affiliates
- Social Enterprise
- Name * First Last
- Affiliation Please List your Professional Affiliation
- Current Harvard Student
- Harvard Alumni
BRIEF RESEARCH REPORT article
The effect of covid-19 and related lockdown phases on young peoples' worries and emotions: novel data from india.

- 1 Department of Psychology, Magadh University, Bodh Gaya, India
- 2 Department of Psychology, Banaras Hindu University, Varanasi, India
- 3 Department of Psychology, Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, United Kingdom
- 4 Division of Psychology, Department of Life Sciences, and Center for Cognitive Neuroscience, College of Health, Medicine and Life Sciences, Brunel University, London, United Kingdom
The COVID-19 pandemic has posed unprecedented stress to young people. Despite recent speculative suggestions of poorer mental health in young people in India since the start of the pandemic, there have been no systematic efforts to measure these. Here we report on the content of worries of Indian adolescents and identify groups of young people who may be particularly vulnerable to negative emotions along with reporting on the impact of coronavirus on their lives. Three-hundred-and-ten young people from North India (51% male, 12–18 years) reported on their personal experiences of being infected by the coronavirus, the impact of the pandemic and its' restrictions across life domains, their top worries, social restrictions, and levels of negative affect and anhedonia. Findings showed that most participants had no personal experience (97.41%) or knew anyone (82.58%) with COVID-19, yet endorsed moderate-to-severe impact of COVID-19 on their academics, social life, and work. These impacts in turn associated with negative affect. Participants' top worries focused on academic attainments, social and recreational activities, and physical health. More females than males worried about academic attainment and physical health while more males worried about social and recreational activities. Thus, Indian adolescents report significant impact of the pandemic on various aspects of their life and are particularly worried about academic attainments, social and recreational activities and physical health. These findings call for a need to ensure provisions and access to digital education and medical care.
Introduction
The COVID-19 pandemic has had far-reaching consequences on the physical and mental health of individuals as well as the health of economies across the globe. While young people may be less susceptible to severe forms of the illness, suffering milder symptoms, lower morbidity, and better prognosis compared to adults ( 1 , 2 ) they have experienced an upsurge in stress ( 3 , 4 ) precipitating loneliness, anxiety and depression in many ( 5 – 8 ). As emotional symptoms in adolescence can become associated with many serious mental health outcomes including suicide, long-term physical health consequences, and significant healthcare burden ( 9 – 11 ), the effect of COVID-19 on young people's mental health could be more damaging in the longer run than the infection itself ( 12 ). Measuring early signs of mental health challenges such as worries and negative emotions in young people is thus an urgent priority for researchers ( 13 , 14 ) as well as policy-makers, including identifying those most vulnerable to mental health difficulties. While this information is crucial for both high- and low-income countries, countries with lower resources dedicated to mental health may benefit more from early forecasts of these needs.
India has one of the highest COVID-19 infection rates in the world with over 2.5 million confirmed cases and the death toll on the rise ( 15 , 16 ). The first case of COVID-19 was identified on January 30, 2020 in Kerala ( 17 ) in a student who had returned from Wuhan, China ( 18 ). However, since March 2020, there has been an upsurge in the spread of the infection. In response, the Government imposed a nationwide lockdown to prevent community transmission of the infection. Despite some regional differences in the extent of lockdown restrictions, based on total COVID-19 cases in that region ( 18 ), everyone in India has experienced closure of educational and training institutions; hotels and restaurants; malls, cinemas, gyms, sports centers; and places of worship. A recent correspondence article by Patra and Patro ( 19 ) speculated that school closures in particular may have been especially damaging for young people and highlighted the urgent need to address mental health issues in Indian adolescents. Yet there have been no such systematic efforts to our knowledge. Here, we report new data from a small cohort of young people from India. We describe their experiences of the COVID-19 pandemic and the impact of COVID-19 pandemic on their daily life. We describe the content of the most common worries reported by young people alongside quantitative measures of current negative and (absence of) positive emotions—symptom-markers of common mental health difficulties such as anxiety and depression. We then assess which young people (in terms of gender, age, and socioeconomic status) are particularly susceptible to reporting more negative emotions and fewer positive emotions. In India, before the pandemic started, public awareness around mental health in young people had been increasing along with the recognition that such problems can be economically costly ( 20 ). Our data can thus signpost emerging, potentially costly mental health problems post-pandemic.
Participants and General Procedures
This study received approval from the Institutional Ethics Committee, Institute of Medical Sciences, Banaras Hindu University (Ref No.: Dean/2020/EC/1975) and King's College London Research Ethics Committee (Ref: HR-19/20-18250). Participants were recruited between June 5, 2020 and July 12, 2020. Prospective participants from different states of North India (Uttar Pradesh, Bihar, New Delhi, West Bengal, Madhya Pradesh, Gujrat) and their parents were identified by circulating information about the study including eligibility criteria (aged 12–18 years; currently residing in India) through social media sites, such as Facebook and WhatsApp. Interested and eligible individuals were sent bilingual (Hindi and English) information sheets (one for young people, one for the parents if the participant was aged 12–17 years). Those who agreed to participate after reading the information sheet received the survey link for both the English and Hindi versions and were requested to complete one based on their language preference. The survey link began with a question about the participants' age. If the participant was 18 years, they viewed and completed a consent form with an electronic signature and their contact details for follow-up assessments. Any participant aged 12–17 years was presented with an assent form with a parental/guardian consent form. To verify that parent/guardian consents were authentic, follow-up phone contact was made with the parent/guardian using the provided contact details. Survey questions were not presented further for incomplete consent/assent forms.
The online survey was developed using Qualtrics software (Qualtrics, Provo, UT). The first third of the survey comprised questions around demographics, personal experiences and knowledge of others who had been infected by the coronavirus, extent of social restrictions and social contact, and the impact of the viral outbreak on various life domains. The second third of the survey included measures of poor mental health such as negative affect, anhedonia (absence of positive affect), and the content of worries. The final third included measures of well-being (positive aspects of mental health), more specific negative emotional experiences (loneliness, boredom) and a cognitive measure (positive and negative future imagery) (presented elsewhere). All Hindi translations used the translation-back-translation method. MS completed the first set of translations, which were back translated by TS. JL checked the back-translations. Where there were definitional discrepancies with the original scale, these were discussed with RP and VK and re-translations were done by MS. The average time taken by the participant to complete the survey was 20 min.
Demographics
Participants submitted information on their age, sex assigned at birth, family monthly income level, and number of family members.
Personal Experiences of and Knowledge of Close Others With COVID-19
Five items (with yes/no responses) measured the extent to which participants had experienced the infection: have you ever been affected or suspected of having the coronavirus infection at any time, do you currently have a confirmed diagnosis of coronavirus infection, are you currently suspected of having a diagnosis of coronavirus infection, have you had a past confirmed diagnosis of coronavirus infection but have now recovered, have you had a past suspected diagnosis of coronavirus infection but have now recovered. Five items (with yes/no responses) assessed whether participants knew others who had experienced the infection, including: a family member, friend, other acquaintance (e.g., classmate), other individual known indirectly (e.g., acquaintance of a family member/friend/acquaintance), know no one with the illness. If the participants endorsed one of the first 4 items, they were asked whether the individual affected had recovered, were still recovering, were hospitalized or had passed away.
Social Restrictions Associated With COVID-19
To describe the extent of reduced social contact, participants indicated the total number of days spent in self-isolation (i.e., not leaving the house), days in which they spent 15 min or more outside the house, days in which they had face-to-face contact with another person for 15 min or more, days in which they had a phone or video call with another person for 15 min or more.
Impact of COVID-19
Participants rated the impact of the outbreak (including associated lockdown measures) on work, study, finances, social life (including leisure activities), relationship with family, physical health, emotions, and caring responsibilities (for children/siblings or elderly/fragile family members) over the last 2 weeks on a 5-point scale (0 = not applicable/none, 1 = very mildly, 2 = mildly, 3 = moderately, 4 = severely). Responses were summed across items to create a total impact score. In the current sample, the internal consistency reliability for the impact items was 0.706.
Content of Worries
Participants were asked to write down their top 3 worries using free text boxes. All free text responses were reviewed by two researchers (MS, TS), who then independently derived “worry categories” based on these responses. The categories proposed by MS and TS were then reviewed by RP, VK, and JL. Where common categories were identified by both researchers these were used in the final worry categories. Where there were differences, these were resolved through discussions, using the life domains listed in the COVID-19 impact questions to help guide the identification of conceptually distinct areas. The final 12 categories along with their descriptions are shown in Table 4 . Using this coding scheme and definitions, all responses were coded by both MS and TS independently to assess inter-rater agreement (Cohen's Kappa reliability). This was 0.98 for Worry 1, 0.90 for Worry 2, and 0.91 for Worry 3.
Negative Affect
The 10 negative affect items from the Positive and Negative Affect Schedule ( 21 ) were used to assess negative emotions. Respondents used a 5- point Likert scale ranging from 1 (very slightly or not at all) to 5 (extremely) to indicate the extent to which they experienced the given mood states during the last 2 weeks. A total negative affect score, ranging from 10 to 50, was created by summing across the scores of individual items. Cronbach's alpha was 0.878.
Nine items (nos. 1, 3, 4, 5, 7, 9, 10, 13, and 14) from the 14-item Snaith-Hamilton Pleasure Scale ( 22 ) were used to index anhedonia, the inability to experience pleasure; the remaining 7 items were deemed unlikely to apply during lockdown phases. Four response options were given for each item (strongly disagree, disagree, agree, or strongly agree), where strongly disagree and disagree were scored 1 and agree and strongly agree, scored 0. A summed score across items therefore ranged from 0 to 14, where higher scores indicated greater absence of positive affect. Cronbach's alpha was 0.723.
Statistical Analyses
After presenting the demographic characteristics of the sample, gender differences in age and income were analyzed using independent sample t -tests. Descriptives of young peoples' personal experiences of the infection, knowledge of others with the infection, the effect of lockdown on social isolation and contact with others and impact across other life domains were presented next. Before conducting any statistical analysis, the data were checked for fulfilling the assumptions for normality ( 23 ). The data did not show serious deviations from normality based on the histogram plots, except a slight positive skew for anhedonia. The skewness and kurtosis values of the data were also within the recommended limit of ±2 ( 24 , 25 ), most being < 1 (except for anhedonia which was >1). Thus, we employed parametric analyses for all the variables except for anhedonia which was explored using non-parametric tests. We investigated the degree to which the overall impact of COVID-19 across life domains varied as a function of gender (using independent samples t -test) and age and family income levels (using bivariate correlations). For the worry data, the percentage of individuals endorsing each worry category was calculated for each of the top 3 worries (first, second, third). However, in the final analysis, we collapsed across the top 3 worries to generate an overall percentage across participants of endorsing that worry among one of their top 3 worries. This meant, for instance, that any participant who rated the same worry across all 3 of their top worries was only represented once. The final percentage of young people endorsing the worry categories was compared across gender and for interpretability, by categorical age groups (Younger adolescents = 12–15 years; Older adolescents = 16–18 years) using chi-square tests. Finally, we presented data on negative affect and absence of positive affect (anhedonia); we investigated how these variables varied across gender, age, and per capita monthly income using multiple linear regression models; we further assessed whether inclusion of interaction terms significantly added to variance explained. Given a slight positive skew for anhedonia, we log-transformed this variable when conducting the regression analysis. To complement the multiple regression analysis of demographic predictors and their interactions, we also ran a series of parametric and non-parametric t -tests and correlations for negative affect and anhedonia, respectively, to assess the extent to which gender, age and family income levels individually associated with these variables. Correlations also assessed the extent to which the overall impact of COVID-19 associated with negative affect and anhedonia.
Demographic Characteristics
The final sample comprised 310 Asian-Indian adolescents (Mean age = 15.69 years; SD = 1.92) of whom 159 were males (Mean age = 15.60 years; SD = 1.98) and 151 were females (Mean age = 15.78 years; SD = 1.87). Males and females did not differ significantly in age, t (308) = −0.84, p = 0.40, d = 0.05. Furthermore, the Levene's test of equality of variances indicated an equal spread of scores in males and females ( F = 0.89, p = 0.34). Only 192 participants provided data for monthly per capita family income, which ranged from 125 to 150,000 Rupees (Mean = 9698.20; SD = 18315.22) with no significant mean or variance differences in the monthly per capita income between males and females [Male Mean = 8343.61; SD = 15065.95; Female Mean = 11439.82; SD = 21768.30; t (190) = −1.16, p = 0.25], d = 0.16, Levene's test of equality of variances: F = 2.63, p = 0.10.
Experiences of COVID-19
Item-level data for personal experiences and knowledge of close others with COVID-19 infections are presented in Table 1 for all participants; and males and females separately. Most young people had not personally experienced or known someone with the coronavirus infection. Of those who did report knowing someone infected with COVID-19, just under half (49.09%) reported that the affected person they knew had recovered from the infection, 12.73% reported that the person was still recovering, 14.54% reported that the known person was hospitalized, while 25.45% participants reported that the affected person passed away.
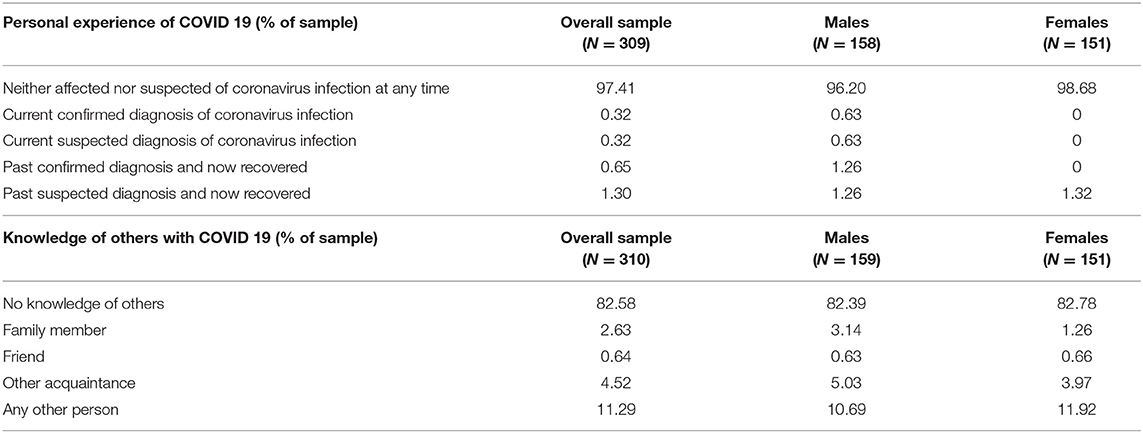
Table 1 . Personal experience of and knowledge of others with COVID-19 (Of note, while the first set of questions about personal experiences of COVID-19 reflects mutually exclusive response options (therefore adding up to 100%), the set of questions around knowledge of others are not all mutually exclusive. For instance, a participant reporting a family member as well as an acquaintance infected with the virus would be included twice, once when calculating the percentage of participants reporting an infected family member and once when calculating the percentage of participants having an infected acquaintance. Therefore, participants having knowledge of others with COVID-19 do not add up to 100%).
Social Restrictions and Impact of COVID-19
Item-level data for questions around social restrictions and reduced social contact are presented in Table 2 for all participants, for male and females separately; and correlations with age and monthly per capita family income. Compared to males, female participants spent significantly more days in self-isolation and more days engaging in phone or video call for 15 min or more. Participants with lower monthly per capita income spent more days in which they were out for 15 min or more, but fewer days engaging in phone or video calls. Age did not correlate with perceived social restrictions.
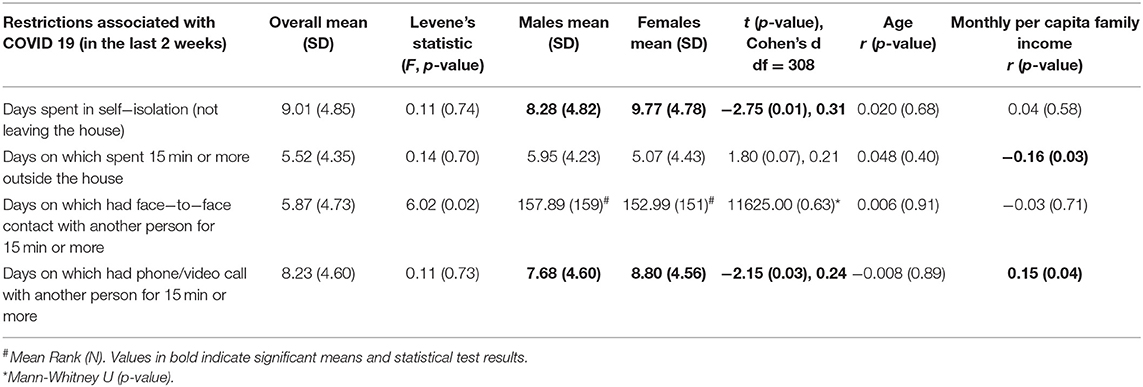
Table 2 . Restrictions associated with COVID−19.
Mean ratings of the impact of COVID-19 on various life domains are presented in Table 3 . Looking at how many young people endorsed moderate-to-severe impact for each domain, 43.6% reported this on their work, 56.8% on their studies, and 48.4% on their social life and recreational activities. Just under half of young people reported moderate-to-severe impact of the pandemic on their family relationships (48.4%), on their caring responsibilities (49.4%) and on their physical health (42.6%). However, 52% reported this for their emotions. For finances, moderate-to-severe impact was reported by 26.8% of young people. Sex, age, and per capita monthly income effects were examined on each domain-specific impact score and the total score, summed across mean ratings for each domain ( Table 3 ). No significant associations emerged between age and impact across any domain ( Table 3 ). Males reported higher mean impact scores for relationships with family members and physical health. Participants with lower per capita income experienced more impact of COVID-19 across life domains (indicated by total impact score) than those with higher monthly per capita income.
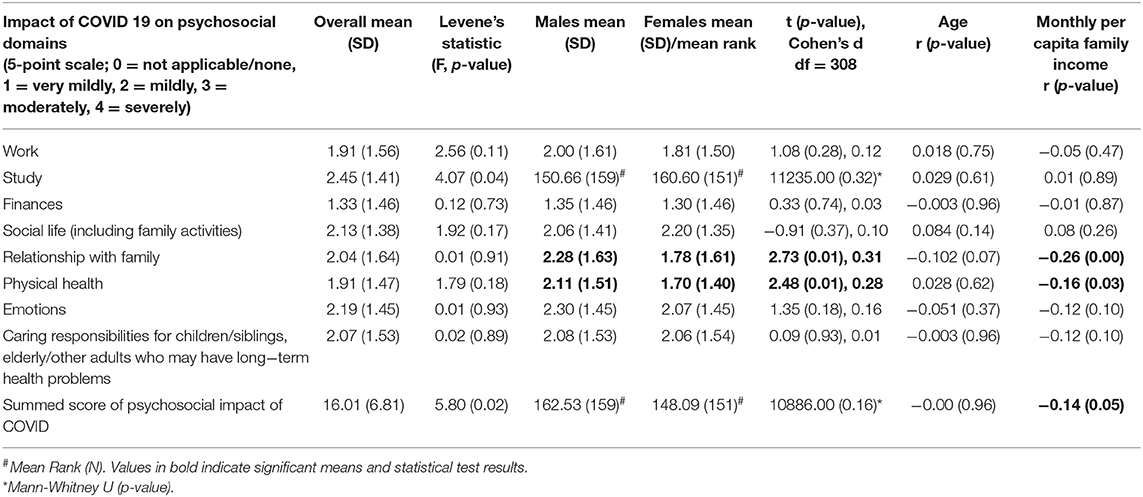
Table 3 . Impact of COVID-19 on psychosocial domains.
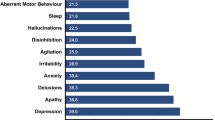
The percentages of young people endorsing each worry category for each of their top 3 worries are presented in the first three columns of Table 4 . These were used to derive the overall percentages of young people endorsing each worry category as one of their top 3 worries presented in Column 4. Using this fourth column, we noted that most participants reported education and studies (Academic) as one of their top worries. The second most common worry of participants centered around “Physical health, fitness, and safety.” Worries about “Social and recreational activities” also emerged as a major concern for several participants, followed by “Finances.” Some participants also listed “Global and societal concerns.” More females reported concerns about “Academic,” and “Physical health, fitness, and safety,” compared to males ( Table 4 ) while male participants reported more worries around “Social and recreational activities” activities than female participants. Comparison of worries across the adolescent groups revealed that while a higher percentage of older adolescents reported each of the worries as one of their top three worries compared to younger adolescents (except for “Unclear” category), the differences were statistically significant only for “Academic,” “Physical health, fitness, and safety,” “Global and societal concerns,” and “Other” categories ( Table 4 ).
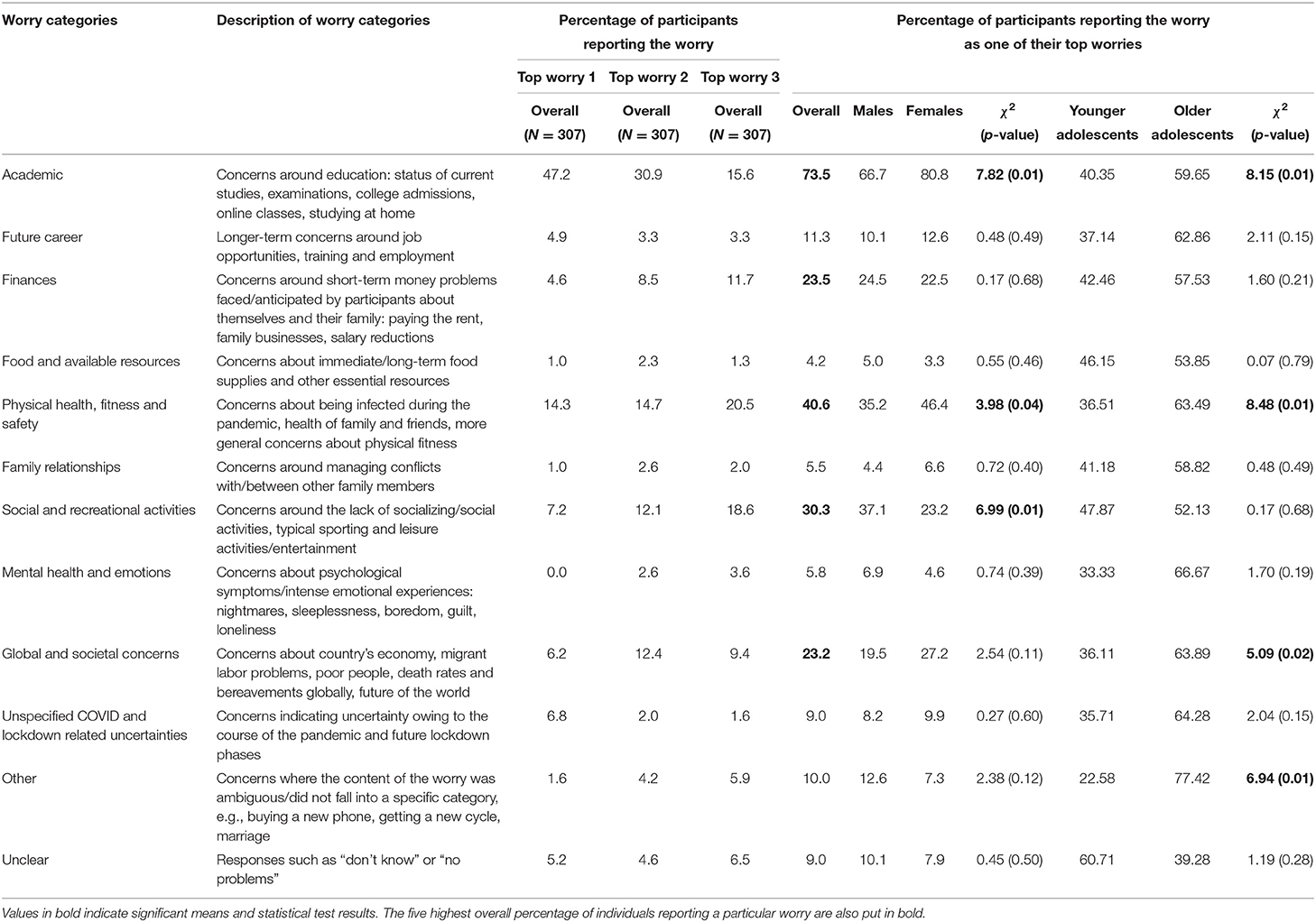
Table 4 . Participants' reported content of top three worries over the last 2 weeks.
A stepwise multiple regression was conducted with negative affect as the dependent variable and age, gender, and per capita monthly income as predictors in step 1 and their interaction terms (i.e., age x gender, age x per capita monthly income, gender x per capita monthly income, and age x gender x per capita monthly income) entered in step 2. Results indicated that the model predicted by the demographic variables was non-significant, F (3,187) = 2.11, p = 0.10 (Adjusted R 2 = 0.017). Nor did the inclusion of interaction terms significantly increase variance explained, R 2 change = 0.004, p = 0.36, F (4,186) = 1.79, p = 0.13 (Adjusted R 2 = 0.016). These findings suggested that males and females did not differ on total negative affect, t (305) = −0.90, p = 0.37, d = 0.10 [Male mean = 21.67 (SD = 8.78), Female mean = 22.51 (SD = 7.85)], Levene's test of equality of variances: F = 0.46, p = 0.50. Nor were there significant correlations with age ( r = 0.09, p = 0.10) and per capita monthly income ( r = −0.11, p = 0.13). However, significant correlations emerged between negative affect and reported impact of COVID-19 across life domains ( r = 0.26, p < 0.001). Negative affect correlated (mostly) weakly but significantly with impact of COVID-19 on social life ( r = 0.13, p = 0.02), relationship with family ( r = 0.14, p = 0.01), physical health ( r = 0.20, p < 0.001), emotions ( r = 0.23, p < 0.001), and caring responsibilities ( r = 0.18, p < 0.001), but not with work ( r = 0.11, p = 0.06), study ( r = 0.07, p = 0.22), and finances ( r = 0.11, p = 0.06).
A stepwise multiple regression, similar to that conducted for “negative affect” was conducted for anhedonia but with the log-transformed scores since the anhedonia scores were slightly positively skewed. Results showed that the model with all demographic predictors was non-significant, Model 1: F (3,156) = 1.44, p = 0.23 (Adjusted R 2 = 0.008). Inclusion of interaction terms did not significantly increase the variance explained, R 2 change = 0.000, p = 0.85, F (4,155) = 1.08, p = 0.37 (Adjusted R 2 = 0.002). Assessment of the individual demographic predictors showed that males (Mean Rank = 165.43) reported higher levels of anhedonia than females (Mean Rank = 141.09); Mann–Whitney U = 9838.50, N1 = 156, N2 = 150, p = 0.01. Participants belonging to families with higher monthly per capita income experienced lower levels of anhedonia ( r s = −0.17, p = 0.02). However, there were no significant correlations between reported impact summed across life domains and anhedonia ( r s = −0.02, p = 0.74). While anhedonia correlated positively but weakly with impact of COVID-19 on physical health ( r s = 0.13, p = 0.02), it showed a significant but weak negative relationship with impact of COVID-19 on study ( r s = −0.20, p < 0.001) and social life ( r s = −0.11, p < 0.05). Anhedonia did not correlate significantly with the impact of COVID-19 on work ( r s = 0.01, p = 0.93), finances ( r s = −0.02, p = 0.70), relationship with family ( r s = 0.09, p = 0.13), emotions ( r s = −0.04, p = 0.45), and caring responsibilities ( r s = −0.02, p = 0.73).
This paper describes baseline data for a cohort of Indian adolescents recruited to a study aiming to assess the longitudinal impact of COVID-19 on negative emotions, worries and strategies used to manage these emotions. Participants were recruited at a time when the total number of coronavirus-infected people in India stood at 236,184 and ended when the total number of infections was 879,466, showing a consistent rise during the period of (baseline) data collection ( 16 ). Yet, even during this period of rising infections, personal experiences and knowledge of others who had been exposed to the coronavirus infection were uncommon for most of our participants. Nonetheless, participants reported moderate-to-severe impact of COVID-19. The impact data together with qualitative data on their top worries, underscored academic studies as a salient area of concern for most young people in this cohort, a likely outcome of social distancing measures preventing school attendance and educational progress. Other salient worries for young people were concerns over the health and safety of self and loved ones and the absence of age-typical social and recreational activities, again expected worries emerging due to the pandemic itself and associated lockdown measures. Interestingly, young people commonly reported worries for their own finances as well as the Indian and global economy, and society more generally. Significantly higher percentage of older adolescents (16–18 years) than younger ones (12–15 years) were worried about their academics, physical health and safety, global and societal concerns and other kinds of worries, which can be expected since with increasing age, the academic work and curriculum gets more difficult and late adolescence is also the crucial time for career explorations ( 26 ). Adolescence is a time of emerging independence (taking on more responsibilities for their own future) but also of interdependence, where self-construal becomes linked to roles and commitments to other groups in society ( 27 ). Identifying the content of these stressors and worries can help governments decide where to propose subsequent policy changes and facilitate society-wide measures. Beyond the need for dedicated mental health services (helplines, centers) called for in earlier papers [e.g., ( 28 )], our data specifically underscore the need for investment of resources into the safe opening of schools, changes to the curriculum and/or the provision of digital education to all young people. Reassurance over access to quality medical care is also a priority.
Within these impacts and worries, there were some gender differences. More females than males reported Academic as a top worry (though this gender difference was not replicated in quantitative impact ratings), which is likely since Indian adolescent females have been reported “more sincere” toward studies than Indian adolescent males, potentially meaning they are more committed and motivated to academic achievement ( 29 ). Males reported a greater impact of COVID-19 on physical health in quantitative ratings; in the Indian context male adolescents are more likely to engage in outdoor sports ( 30 ) and experience fewer sociocultural barriers to outdoor physical activity ( 31 ) than female adolescents. This difference between genders where males spent more time out of the house than females, may also have emerged because males identified social and recreational activities as a top concern; females by contrast, followed restrictions associated with COVID reporting more days in social isolation and on phone/video calls. Perhaps relatedly, more females expressed worries over physical health, fitness, and safety from contracting the virus than male participants. Sedentary lifestyles resulting from the lockdown ( 32 ) may not only affect childhood obesity but can also significantly affect mental health of adolescents. Some interesting trends were also noted in relation to socio-economic status (SES) of the participants, as indexed by the per capita monthly income of their families. Lower SES was associated with a higher impact of COVID across life domains but particularly with impacts on physical health and family. Lower SES was associated with more days participants spent outside of the home, which could explain the reported impact on physical health. Adolescents belonging to lower SES may be residing in crowded living situations, which together with parental stress due to the economic crisis ( 33 ), may mean them having to navigate more complicated family dynamics. Higher SES was associated with more days spent on phone/video calls, probably because participants belonging to higher SES have greater access to laptops, smartphones, and/or tablets than those from lower SES.
In terms of negative and (absence of) positive emotions, means reported in our sample using translated versions of standardized questionnaires were commensurate with those reported in general youth population samples in the west ( 34 ). Self-reported negative affect did not correlate with age, SES and did not vary between males and females but was greater in those reporting more impact of COVID-19 across life domains. Males and those from lower SES reported more anhedonia. These findings pursued longitudinally in time can help us to identify those who show propensity for anxiety/depression across time allowing us to signpost need for mental health resources. Although anhedonia was negatively linked with the impact of COVID-19 on study and social life of the participants, these associations were weak.
There are several study limitations. First, the sample has been obtained using convenience sampling methods (using social media) and responders were only from a few North Indian states. Hence it is difficult to say how representative it is of 12–18 year old Indian adolescents. Moreover, given the study survey requirements, only participants who had access to the Internet and had a registered phone number (to verify parental consent) could be recruited, biasing the study sample composition. However, SES classes seemed to be adequately represented since using the Modified BG Prasad Socio-economic Classification 2019 ( 35 ), (although there was some missing data) the sample reflected the entire continuum of SES classes in India. Second, as data was collected online, qualitative responses were unprobed and very often single word answers had to be coded, affecting the reliability of these data. Nonetheless, inter-rater reliability using this coding scheme was high. Third, participants did not report on whether they lived in rural or urban areas of their respective cities, and therefore our data cannot speak to rural-urban differences in adolescents' worries, negative and positive emotions. Future studies should measure and compare the impact of rural and urban populations on these indices of poor mental health. Finally, many of the scales used were not standardized. However, as internal consistencies were acceptable, this study adds potential new measures for future studies of young people in the Indian context.
Conclusions
Our study showed that even though a handful of participants had personal experiences of or knew someone who had been infected by COVID-19, all our participants reported considerable impact of the pandemic on various aspects of their life, which was linked to higher negative affectivity. Adolescents also expressed worries about their studies, physical health and safety as well as social and recreational activities, with some gender differences. While our findings are unable to demonstrate causality between the impact of these COVID-19 related changes and worries, negative affect and anhedonia, nonetheless, the findings highlight the urgent need for government policy makers to take concrete steps to mitigate potential adverse effects of the pandemic on the mental health of Indian adolescents.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Ethics Committee, Institute of Medical Sciences, Banaras Hindu University (Ref No.: Dean/2020/EC/1975); King's College London Research Ethics Committee (Ref: HR-19/20-18250). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
JL, MS, VK, RP, TH, LR, and TS contributed to the conception and design of the study. RP, TS, JL, VK, and MS contributed to the development of study materials, contributed to analysis, and interpretation of study data. MS and TS contributed to acquisition of study data. MS and JL wrote first draft of the paper. VK, RP, TS, TH, and LR critiqued the output for important intellectual content. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Ludvigsson JF. Systematic review of COVID 19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. (2020) 109:1088–95. doi: 10.1111/apa.15270
CrossRef Full Text | Google Scholar
2. Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Carducci FIC, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. (2020) 4:653–61. doi: 10.1016/S2352-4642(20)30177-2
3. Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canad J Behav Sci. (2020) 52:177. doi: 10.1037/cbs0000215
4. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cadernos Saúde Públ. (2020) 36:e00054020. doi: 10.1590/0102-311x00054020
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res . (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
6. Chen F, Zheng D, Liu J, Gong Y, Guan Z, Lou D. Depression and anxiety among adolescents during COVID-19: a cross-sectional study. Brain Behav Immun. (2020) 88:36–8. doi: 10.1016/j.bbi.2020.05.061
7. Zhou SJ, Zhang LG, Wang LL, Guo ZC, Wang JQ, Chen JC, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. (2020) 29:749–58. doi: 10.1007/s00787-020-01541-4
8. UK Youth. The Impact of COVID-19 on Young People & The Youth Sector . (2020). Available online at: www.ukyouth.org/wp-content/uploads/2020/04/UK-Youth-Covid-19-Impact-Report-External-Final-08.04.20.pdf (accessed July 22, 2020).
9. Rivenbark JG, Odgers CL, Caspi A, Harrington H, Hogan S, Houts RM, et al. The high societal costs of childhood conduct problems: evidence from administrative records up to age 38 in a longitudinal birth cohort. J Child Psychol Psychiatry. (2018) 59:703–10. doi: 10.1111/jcpp.12850
10. Ewest F, Reinhold T, Vloet TD, Wenning V, Bachmann CJ. Health insurance expenses caused by adolescents with a diagnosis of conduct disorder. Kindheit Entwicklung. (2013) 22:41–7. doi: 10.1026/0942-5403/a000097
CrossRef Full Text
11. Bernfort L, Nordfeldt S, Persson J. ADHD from a socio-economic perspective. Acta Paediatr. (2008) 97:239–45. doi: 10.1111/j.1651-2227.2007.00611.x
12. Depoux A, Martin S, Karafillakis E, Preet R, Wilder-Smith A, Larson H. The pandemic of social media panic travels faster than the COVID-19 outbreak. J Travel Med. (2020) 27:taaa031. doi: 10.1093/jtm/taaa031
13. O'Connor DB, Aggleton JP, Chakrabarti B, Cooper CL, Creswell C, Dunsmuir S, et al. Research priorities for the COVID-19 pandemic and beyond: a call to action for psychological science. Br J Psychol. (2020) 111:603–29. doi: 10.1111/bjop.12468
14. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:P547–60. doi: 10.1016/S2215-0366(20)30168-1
15. Gupta A, Banerjee S, Das S. Significance of geographical factors to the COVID-19 outbreak in India. Model Earth Syst Environ. (2020) 6:2645–53. doi: 10.1007/s40808-020-00838-2
16. Worldometers (2020). Available online at: http://www.worldometers.info/coronavirus/india/
17. PIB Delhi. Update on Novel Coronavirus: One Positive Case Reported in Kerala . (2020). Available online at: https://pib.gov.in/pressreleaseiframepage.aspx?prid=1601095 (accessed July 22, 2020).
18. Kaushik S, Kaushik S, Sharma Y, Kumar R, Yadav JP. The Indian perspective of COVID-19 outbreak. VirusDisease . (2020) 31:1–8. doi: 10.1007/s13337-020-00587-x
19. Patra S, Patro BK. COVID-19 and adolescent mental health in India. Psychiatry Res. (2020) 293:113429. doi: 10.1016/j.psychres.2020.113429
20. Gururaj G, Varghese M, Benegal V, Rao GN, Pathak K, Singh LK, et al. National Mental Health Survey of India, 2015-16: Summary Report . Bengaluru: National Institute of Mental Health and Neurosciences (2016).
21. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. (1988) 54:1063–70. doi: 10.1037/0022-3514.54.6.1063
22. Snaith RP, Hamilton M, Morley S, Humayan A, Hargreaves D, Trigwell P. A scale for the assessment of hedonic tone the Snaith–Hamilton pleasure scale. Br J Psychiatry. (1995) 167:99–103. doi: 10.1192/bjp.167.1.99
23. Field A. Discovering Statistics Using SPSS (3rd ed.). London: Sage Publications Ltd. (2009).
Google Scholar
24. Trochim WM, Donnelly JP. The Research Methods Knowledge Base 3rd ed. Cincinnati: Atomic Dog (2006).
25. Gravetter F, Wallnau L. Essentials of Statistics for the Behavioral Sciences 8th ed. Belmont: Wadsworth (2014).
26. Tiedeman DV, O'Hara RP. Career Development: Choice and Adjustment . New York, NY: College Entrance Examination Board (1963).
27. Markus HR, Kitayama S. Culture and the self: Implications for cognition, emotion, and motivation. Psychol Rev. (1991) 98:224–53. doi: 10.1037/0033-295X.98.2.224
28. Das S. Mental health and psychosocial aspects of COVID-19 in India: the challenges and responses. J Health Manag. (2020) 22:197–205. doi: 10.1177/0972063420935544
29. Dhull I, Kumari S. Academic stress among adolescent in relation to gender. Int J Appl Res. (2015) 1:394–6. Available online at: https://www.allresearchjournal.com/archives/?year=2015&vol=1&issue=11&part=F&ArticleId=931
30. Swaminathan S, Selvam S, Thomas T, Kurpad AV, Vaz M. Longitudinal trends in physical activity patterns in selected urban south Indian school children. Ind J Med Res. (2011) 134:174–80.
PubMed Abstract | Google Scholar
31. Satija A, Khandpur N, Satija S, Mathur Gaiha S, Prabhakaran D, Reddy KS, et al. Physical activity among adolescents in India: a qualitative study of barriers and enablers. Health Educ Behav. (2018) 45:926–34. doi: 10.1177/1090198118778332
32. Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19–related school closings and risk of weight gain among children. Obesity. (2020) 28:1008–9. doi: 10.1002/oby.22813
33. Cluver L, Lachman JM, Sherr L, Wessels I, Krug E, Rakotomalala S, et al. Parenting in a time of COVID-19. Lancet. (2020) 395:E64. doi: 10.1016/S0140-6736(20)30736-4
34. Leventhal AM, Unger JB, Audrain-McGovern J, Sussman S, Volk HE, Strong DR. Measuring anhedonia in adolescents: a psychometric analysis. J Pers Assess. (2015) 97:506–14. doi: 10.1080/00223891.2015.1029072
35. Pandey VK, Aggarwal P, Kakkar R. Modified BG prasad socio-economic classification, update-2019. Ind J Commun Health. (2019) 31:123–5. Available online at: https://www.iapsmupuk.org/journal/index.php/IJCH/article/view/1055
Keywords: COVID-19, young people, India, worries, emotions
Citation: Shukla M, Pandey R, Singh T, Riddleston L, Hutchinson T, Kumari V and Lau JYF (2021) The Effect of COVID-19 and Related Lockdown Phases on Young Peoples' Worries and Emotions: Novel Data From India. Front. Public Health 9:645183. doi: 10.3389/fpubh.2021.645183
Received: 11 January 2021; Accepted: 26 April 2021; Published: 20 May 2021.
Reviewed by:
Copyright © 2021 Shukla, Pandey, Singh, Riddleston, Hutchinson, Kumari and Lau. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer Y. F. Lau, jennifer.lau@kcl.ac.uk ; Tushar Singh, tusharsinghalld@gmail.com
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 03 October 2022
How COVID-19 shaped mental health: from infection to pandemic effects
- Brenda W. J. H. Penninx ORCID: orcid.org/0000-0001-7779-9672 1 , 2 ,
- Michael E. Benros ORCID: orcid.org/0000-0003-4939-9465 3 , 4 ,
- Robyn S. Klein 5 &
- Christiaan H. Vinkers ORCID: orcid.org/0000-0003-3698-0744 1 , 2
Nature Medicine volume 28 , pages 2027–2037 ( 2022 ) Cite this article
40k Accesses
127 Citations
488 Altmetric
Metrics details
- Epidemiology
- Infectious diseases
- Neurological manifestations
- Psychiatric disorders
The Coronavirus Disease 2019 (COVID-19) pandemic has threatened global mental health, both indirectly via disruptive societal changes and directly via neuropsychiatric sequelae after SARS-CoV-2 infection. Despite a small increase in self-reported mental health problems, this has (so far) not translated into objectively measurable increased rates of mental disorders, self-harm or suicide rates at the population level. This could suggest effective resilience and adaptation, but there is substantial heterogeneity among subgroups, and time-lag effects may also exist. With regard to COVID-19 itself, both acute and post-acute neuropsychiatric sequelae have become apparent, with high prevalence of fatigue, cognitive impairments and anxiety and depressive symptoms, even months after infection. To understand how COVID-19 continues to shape mental health in the longer term, fine-grained, well-controlled longitudinal data at the (neuro)biological, individual and societal levels remain essential. For future pandemics, policymakers and clinicians should prioritize mental health from the outset to identify and protect those at risk and promote long-term resilience.
Similar content being viewed by others

A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle-aged and older adults from the Canadian Longitudinal Study on Aging
Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis
The effects of the COVID-19 pandemic on neuropsychiatric symptoms in dementia and carer mental health: an international multicentre study
In 2019, the COVID-19 outbreak was declared a pandemic by the World Health Organization (WHO), with 590 million confirmed cases and 6.4 million deaths worldwide as of August 2022 (ref. 1 ). To contain the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) across the globe, many national and local governments implemented often drastic restrictions as preventive health measures. Consequently, the pandemic has not only led to potential SARS-CoV-2 exposure, infection and disease but also to a wide range of policies consisting of mask requirements, quarantines, lockdowns, physical distancing and closure of non-essential services, with unprecedented societal and economic consequences.
As the world is slowly gaining control over COVID-19, it is timely and essential to ask how the pandemic has affected global mental health. Indirect effects include stress-evoking and disruptive societal changes, which may detrimentally affect mental health in the general population. Direct effects include SARS-CoV-2-mediated acute and long-lasting neuropsychiatric sequelae in affected individuals that occur during primary infection or as part of post-acute COVID syndrome (PACS) 2 —defined as symptoms lasting beyond 3–4 weeks that can involve multiple organs, including the brain. Several terminologies exist for characterizing the effects of COVID-19. PACS also includes late sequalae that constitute a clinical diagnosis of ‘long COVID’ where persistent symptoms are still present 12 weeks after initial infection and cannot be attributed to other conditions 3 .
Here we review both the direct and indirect effects of COVID-19 on mental health. First, we summarize empirical findings on how the COVID-19 pandemic has impacted population mental health, through mental health symptom reports, mental disorder prevalence and suicide rates. Second, we describe mental health sequalae of SARS-CoV-2 virus infection and COVID-19 disease (for example, cognitive impairment, fatigue and affective symptoms). For this, we use the term PACS for neuropsychiatric consequences beyond the acute period, and will also describe the underlying neurobiological impact on brain structure and function. We conclude with a discussion of the lessons learned and knowledge gaps that need to be further addressed.
Impact of the COVID-19 pandemic on population mental health
Independent of the pandemic, mental disorders are known to be prevalent globally and cause a very high disease burden 4 , 5 , 6 . For most common mental disorders (including major depressive disorder, anxiety disorders and alcohol use disorder), environmental stressors play a major etiological role. Disruptive and unpredictable pandemic circumstances may increase distress levels in many individuals, at least temporarily. However, it should be noted that the pandemic not only resulted in negative stressors but also in positive and potentially buffering changes for some, including a better work–life balance, improved family dynamics and enhanced feelings of closeness 7 .
Awareness of the potential mental health impact of the COVID-19 pandemic is reflected in the more than 35,000 papers published on this topic. However, this rapid research output comes with a cost: conclusions from many papers are limited due to small sample sizes, convenience sampling with unclear generalizability implications and lack of a pre-COVID-19 comparison. More reliable estimates of the pandemic mental health impact come from studies with longitudinal or time-series designs that include a pre-pandemic comparison. In our description of the evidence, we, therefore, explicitly focused on findings from meta-analyses that include longitudinal studies with data before the pandemic, as recently identified through a systematic literature search by the WHO 8 .
Self-reported mental health problems
Most studies examining the pandemic impact on mental health used online data collection methods to measure self-reported common indicators, such as mood, anxiety or general psychological distress. Pooled prevalence estimates of clinically relevant high levels of depression and anxiety symptoms during the COVID-19 pandemic range widely—between 20% and 35% 9 , 10 , 11 , 12 —but are difficult to interpret due to large methodological and sample heterogeneity. It also is important to note that high levels of self-reported mental health problems identify increased vulnerability and signal an increased risk for mental disorders, but they do not equal clinical caseness levels, which are generally much lower.
Three meta-analyses, pooling data from between 11 and 61 studies and involving ~50,000 individuals or more 13 , 14 , 15 , compared levels of self-reported mental health problems during the COVID-19 pandemic with those before the pandemic. Meta-analyses report on pooled effect sizes—that is, weighted averages of study-level effect sizes; these are generally considered small when they are ~0.2, moderate when ~0.5 and large when ~0.8. As shown in Table 1 , meta-analyses on mental health impact of the COVID-19 pandemic reach consistent conclusions and indicate that there has been a heterogeneous, statistically significant but small increase in self-reported mental health problems, with pooled effect sizes ranging from 0.07 to 0.27. The largest symptom increase was found when using specific mental health outcome measures assessing depression or anxiety symptoms. In addition, loneliness—a strong correlate of depression and anxiety—showed a small but significant increase during the pandemic (Table 1 ; effect size = 0.27) 16 . In contrast, self-reported general mental health and well-being indicators did not show significant change, and psychotic symptoms seemed to have decreased slightly 13 . In Europe, alcohol purchase decreased, but high-level drinking patterns solidified among those with pre-pandemic high drinking levels 17 . When compared to pre-COVID levels, no change in self-reported alcohol use (effect size = −0.01) was observed in a recent meta-analysis summarizing 128 studies from 58 (predominantly European and North American) countries 18 .
What is the time trajectory of self-reported mental health problems during the pandemic? Although findings are not uniform, various large-scale studies confirmed that the increase in mental health problems was highest during the first peak months of the pandemic and smaller—but not fully gone—in subsequent months when infection rates declined and social restrictions eased 13 , 19 , 20 . Psychological distress reports in the United Kingdom increased again during the second lockdown period 15 . Direct associations between anxiety and depression symptom levels and the average number of daily COVID-19 cases were confirmed in the US Centers for Disease Control and Prevention (CDC) data 21 . Studies that examined longer-term trajectories of symptoms during the first or even second year of the COVID-19 pandemic are more sparse but revealed stability of symptoms without clear evidence of recovery 15 , 22 . The exception appears to be for loneliness, as some studies confirmed further increasing trends throughout the first COVID-19 pandemic year 22 , 23 . As most published population-based studies were conducted in the early time period in which absolute numbers of SARS-CoV2-infected individuals were still low, the mental health impacts described in such studies are most likely due to indirect rather than direct effects of SARS-CoV-2 infection. However, it is possible that, in longer-term or later studies, these direct and indirect effects may be more intertwined.
The extent to which governmental policies and communication have impacted on population mental health is a relevant question. In cross-country comparisons, the extent of social restrictions showed a dose–response relationship with mental health problems 24 , 25 . In a review of 33 studies worldwide, it was concluded that governments that enacted stringent measures to contain the spread of COVID-19 benefitted not only the physical but also the mental health of their population during the pandemic 26 , even though more stringent policies may lead to more short-term mental distress 25 . It has been suggested that effective communication of risks, choices and policy measures may reduce polarization and conspiracy theories and mitigate the mental health impact of such measures 25 , 27 , 28 .
In sum, the general pattern of results is that of an increase in mental health symptoms in the population, especially during the first pandemic months, that remained elevated throughout 2020 and early 2021. It should be emphasized that this increase has a small effect size. However, even a small upward shift in mental health problems warrants attention as it has not yet shown to be returned to pre-pandemic levels, and it may have meaningful cumulative consequences at the population level. In addition, even a small effect size may mask a substantial heterogeneity in mental health impact, which may have affected vulnerable groups disproportionally (see below).

Mental disorders, self-harm and suicide
Whether the observed increase in mental health problems during the COVID-19 pandemic has translated into more mental disorders or even suicide mortality is not easy to answer. Mental disorders, characterized by more severe, disabling and persistent symptoms than self-reported mental health problems, are usually diagnosed by a clinician based on the International Classification of Diseases, 10th Revision (ICD-10) or the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) criteria or with validated semi-structured clinical interviews. However, during the COVID-19 pandemic, research systematically examining the population prevalence of mental disorders has been sparse. Unfortunately, we can also not strongly rely on healthcare use studies as the pandemic impacted on healthcare provision more broadly, thereby making figures of patient admissions difficult to interpret.
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic has led to a 28% (95% uncertainty interval (UI): 25–30) increase in major depressive disorders and a 26% (95% UI: 23–28) increase in anxiety disorders. It should be noted that these estimations come with high uncertainty as the assumption that transient pandemic-related increases in mental symptoms extrapolate into incident mental disorders remains disputable. So far, only four longitudinal population-based studies have measured and compared current mental (that is, depressive and anxiety) disorder prevalence—defined using psychiatric diagnostic criteria—before and during the pandemic. Of these, two found no change 30 , 31 , one found a decrease 32 and one found an increase in prevalence of these disorders 33 . These studies were local, limited to high-income countries, often small-scale and used different modes of assessment (for example, online versus in-person) before and during the pandemic. This renders these observational results uncertain as well, but their contrast to the GBD calculations 29 is striking.
Time-series analysis of monthly suicide trends in 21 middle-income to high-income countries across the globe yielded no evidence for an increase in suicide rates in the first 4 months of the pandemic, and there was evidence of a fall in rates in 12 countries 34 . Also in the United States, there was a significant decrease in suicide mortality in the first pandemic months but a slight increase in mortality due to drug overdose and homicide 35 . A living systematic review 36 also concluded that, throughout 2020, there was no observed increase in suicide rates in 20 studies conducted in North America, Europe and Asia. Analyses of electronic health record data in the primary care setting showed reduced rates of self-harm during the first COVID-19 pandemic year 37 . In contrast, emergency department visits for self-harm behavior were unchanged 38 or increased 39 . Such inconsistent findings across healthcare settings may reflect a reluctance in healthcare-seeking behavior for mental healthcare issues. In the living systematic review, eight of 11 studies that examined service use data found a significant decrease in reported self-harm/suicide attempts after COVID lockdown, which returned to pre-lockdown levels in some studies with longer follow-up (5 months) 36 .
In sum, although calculations based on survey data predict a global increase of mental disorder prevalence, objective and consistent evidence for an increased mental disorder, self-harm or suicide prevalence or incidence during the first pandemic year remains absent. This observation, coupled with the only small increase in mental health symptom levels in the overall population, may suggest that most of the general population has demonstrated remarkable resilience and adaptation. However, alternative interpretations are possible. First, there is a large degree of heterogeneity in the mental health impact of COVID-19, and increased mental health in one group (for example, due to better work–family balance and work flexibility) may have masked mental health problems in others. Various societal responses seen in many countries, such as community support activities and bolstering mental health and crisis services, may have had mitigating effects on the mental health burden. Also, the relationship between mental health symptom increases during stressful periods and its subsequent effects on the incidence of mental disorders may be non-linear or could be less visible due to resulting alternative outcomes, such as drug overdose or homicide. Finally, we cannot rule out a lag-time effect, where disorders may take more time to develop or be picked up, especially because some of the personal financial or social consequences of the COVID pandemic may only become apparent later. It should be noted that data from low-income countries and longer-term studies beyond the first pandemic year are largely absent.
Which individuals are most affected by the COVID-19 pandemic?
There is substantial heterogeneity across studies that evaluated how the COVID pandemic impacted on mental health 13 , 14 , 15 . Although our society as a whole may have the ability to adequately bounce back from pandemic effects, there are vulnerable people who have been affected more than others.
First, women have consistently reported larger increases in mental health problems in response to the COVID-19 pandemic than men 13 , 15 , 29 , 40 , with meta-analytic effect sizes being 44% 15 to 75% 13 higher. This could reflect both higher stress vulnerability or larger daily life disruptions due to, for example, increased childcare responsibilities, exposure to home violence or greater economic impact due to employment disruptions that all disproportionately fell to women 41 , thereby exacerbating the already existing pre-pandemic gender inequalities in depression and anxiety levels. In addition, adolescents and young adults have been disproportionately affected compared to younger children and older adults 12 , 15 , 29 , 40 . This may be the result of unfavorable behavioral and social changes (for example, school closure periods 42 ) during a crucial development phase where social interactions outside the family context are pivotal. Alarmingly, even though suicide rates did not seem to increase at the population level, studies in China 43 and Japan 44 indicated significant increases in suicide rates in children and adolescents.
Existing socio-cultural disparities in mental health may have further widened during the COVID pandemic. Whether the impact is larger for individuals with low socio-economic status remains unclear, with contrasting meta-analyses pointing toward this group being protected 15 or at increased risk 40 . Earlier meta-analyses did not find that the mental health impact of COVID-19 differed across Europe, North America, Asia and Oceania 13 , 14 , but data are lacking from Africa and South America. Nevertheless, a large-scale within-country comparison in the United States found that the mental health of Black, Hispanic and Asian respondents worsened relatively more during the pandemic compared to White respondents. Moreover, White respondents were more likely to receive professional mental healthcare during the pandemic, and, conversely, Black, Hispanic, and Asian respondents demonstrated higher levels of unmet mental healthcare needs during this time 45 .
People with pre-existing somatic conditions represent another vulnerable group in which the pandemic had a greater impact (pooled effect size of 0.25) 13 . This includes people with conditions such as epilepsy, multiple sclerosis or cardiometabolic disease as well as those with multiple comorbidities. The disproportionate impact may reflect this groupʼs elevated COVID-19 risk and, consequently, more perceived stress and fear of infection, but it could also reflect disruptions of regular healthcare services.
Healthcare workers faced increased workload, rapidly changing and challenging work environments and exposure to infections and death, accompanied by fear of infecting themselves and their families. High prevalences of (subthreshold) depression (13% 46 ), depressive symptoms (31% 47 ), (subthreshold) anxiety (16% 46 ), anxiety symptoms (23% 47 ) and post-traumatic stress disorder (~22% 46 , 47 ) have been reported in healthcare workers. However, a meta-analysis did not find a larger mental health impact of the pandemic as compared to the general population 40 , and another meta-analysis (of 206 studies) found that the mental health status of healthcare workers was similar to or even better than that of the general population during the first COVID year 48 . However, it is important to note that these meta-analyses could not differentiate between frontline and non-frontline healthcare workers.
Finally, individuals with pre-existing mental disorders may be at increased risk for exacerbation of mental ill-health during the pandemic, possibly due to disease history—illustrating a higher genetic and/or environmental vulnerability—but also due to discontinuity of mental healthcare. Already before the pandemic, mental health systems were under-resourced and disorganized in most countries 6 , 49 , but a third of all WHO member states reported disruptions to mental and substance use services during the first 18 months of the pandemic 50 , with reduced, shortened or postponed appointments and limited capacity for acute inpatient admissions 51 , 52 . Despite this, there is no clear evidence that individuals with pre-existing mental disorders are disproportionately affected by pandemic-related societal disruptions; the effect size for pandemic impact on self-reported mental health problems was similar in psychiatric patients and the general population 13 . In the United States, emergency visits for ten different mental disorders were generally stable during the pandemic compared to earlier periods 53 . In a large Dutch study 22 , 54 with multiple pre-pandemic and during-pandemic assessments, there was no difference in symptom increase among patients relative to controls (see Fig. 1 for illustration). In absolute terms, however, it is important to note that psychiatric patients show much higher symptom levels of depression, anxiety, loneliness and COVID-fear than healthy controls. Again, variation in mental health changes during the pandemic is large: next to psychiatric patients who showed symptom decrease due to, for example, experiencing relief from social pressures, there certainly have been many patients with symptom increases and relapses during the pandemic.
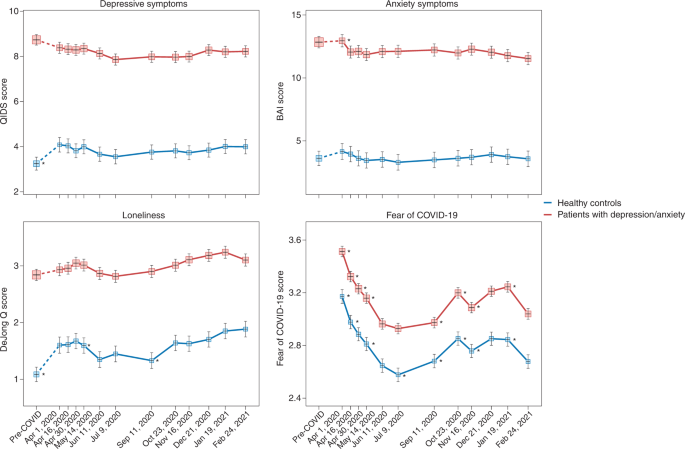
Trajectories of mean depressive symptoms (QIDS score), anxiety symptoms (BAI score), loneliness (De Jong questionnaire score) and Fear of COVID-19 score before and during the first year of the COVID-19 pandemic in healthy controls (blue line, n = 378) and in patients with depressive and/or anxiety disorders (red line, n = 908). The x -axis indicates time with one pre-COVID assessment (averaged over up to five earlier assessments conducted between 2006 and 2019) and 11 online assessments during April 2020 through February 2021. Symbols indicate the mean score during the assessment with 95% CIs. As compared to pre-COVID assessment scores, the figure shows a statistically significant increase of depression and loneliness symptoms during the first pandemic peak (April 2020) in healthy controls but not in patients (for more details, see refs. 22 , 54 ). Asterisks indicate where subsequent wave scores differ from the prior wave scores ( P < 0.05). The figure also illustrates the stability of depressive and anxiety symptoms during the first COVID year, a significant increase in loneliness during this period and fluctuations of Fear of COVID-19 score that positively correlate with infection rates in the Netherlands. Raw data are from the Netherlands Study of Depression and Anxiety (NESDA), which were re-analyzed for the current plots to illustrate differences between two groups (healthy controls versus patients). BAI, Beck Anxiety Inventory; QIDS, Quick Inventory of Depressive Symptoms.
Impact of COVID-19 infection and disease on mental health and the brain
Not only the pandemic but also COVID-19 itself can have severe impact on the mental health of affected individuals and, thus, of the population at large. Below we describe acute and post-acute neuropsychiatric sequelae seen in patients with COVID-19 and link these to neurobiological mechanisms.
Neuropsychiatric sequelae in individuals with COVID-19
Common symptoms associated with acute SARS-CoV-2 infection include headache, anosmia (loss of sense of smell) and dysgeusia (loss of sense of taste). The broader neuropsychiatric impact is dependent on infection severity and is very heterogeneous (Table 2 ). It ranges from no neuropsychiatric symptoms among the large group of asymptomatic COVID-19 cases to milder transient neuropsychiatric symptoms, such as fatigue, sleep disturbance and cognitive impairment, predominantly occurring among symptomatic patients with COVID-19 (ref. 55 ). Cognitive impairment consists of sustained memory impairments and executive dysfunction, including short-term memory loss, concentration problems, word-finding problems and impaired daily problem-solving, colloquially termed ‘brain fog’ by patients and clinicians. A small number of infected individuals become severely ill and require hospitalization. During hospital admission, the predominant neuropsychiatric outcome is delirium 56 . Delirium occurs among one-third of hospitalized patients with COVID-19 and among over half of patients with COVID-19 who require intensive care unit (ICU) treatment. These delirium rates seem similar to those observed among individuals with severe illness hospitalized for other general medical conditions 57 . Delirium is associated with neuropsychiatric sequalae after hospitalization, as part of post-intensive care syndrome 58 , in which sepsis and inflammation are associated with cognitive dysfunction and an increased risk of a broad range of psychiatric symptoms, from anxiety to depression and psychotic symptoms with hallucinations 59 , 60 .
A subset of patients with COVID-19 develop PACS 61 , which can include neuropsychiatric symptoms. A large meta-analysis summarizes 51 studies involving 18,917 patients with a mean follow-up of 77 days (range, 14–182 days) 62 . The most prevalent neuropsychiatric symptom associated with COVID-19 was sleep disturbance, with a pooled prevalence of 27.4%, followed by fatigue (24.4%), cognitive impairment (20.2%), anxiety symptoms (19.1%), post-traumatic stress symptoms (15.7%) and depression symptoms (12.9%) (Table 2 ). Another meta-analysis that assessed patients 12 weeks or more after confirmed COVID-19 diagnosis found that 32% experienced fatigue, and 22% experienced cognitive impairment 63 . To what extent neuropsychiatric symptoms are truly unique for patients with COVID remains unclear from these meta-analyses, as hardly any study included well-matched controls with other types of respiratory infections or inflammatory conditions.
Studies based on electronic health records have examined whether higher levels of neuropsychiatric symptoms truly translate into a higher incidence of clinically overt mental disorders 64 , 65 . In a 1-year follow-up using the US Veterans Affairs database, 153,848 survivors of SARS-CoV-2 infection exhibited an increased incidence of any mental disorder with a relative risk of 1.46 and, specifically, 1.35 for anxiety disorders, 1.39 for depressive disorders and 1.38 for stress and adjustment disorders, compared to a contemporary group and a historical control group ( n = 5,859,251) 65 . In absolute numbers, the incident risk difference attributable to SARS-CoV-2 for mental disorders was 64 per 1,000 individuals. Taquet et al. 64 analyzed electronic health records from the US-based TriNetX network with over 81 million patients and 236,379 COVID-19 survivors followed for 6 months. In absolute numbers, 6-month incidence of hospital contacts related to diagnoses of anxiety, affective disorder or psychotic disorder was 7.0%, 4.5% and 0.4%, respectively. Risks of incident neurological or psychiatric diagnoses were directly correlated with COVID-19 severity and increased by 78% when compared to influenza and by 32% when compared to other respiratory tract infections. In contrast, a medical record study involving 8.3 million adults confirmed that neuropsychiatric disorders were significantly elevated among COVID-19 hospitalized individuals but to a similar extent as in hospitalized patients with other severe respiratory disease 66 . In line with this, a study using language processing of clinical notes in electronic health records did not find an increase in fatigue, mood and anxiety symptoms among COVID-19 hospitalized individuals when compared to hospitalized patients for other indications and adjusted for sociodemographic features and hospital course 67 . It is important to note that research based only on hospital records might be influenced by increased health-seeking behavior that could be differential across care settings or by increased follow-up by hospitals of patients with COVID-19 (compared to patients with other conditions).
Consequently, whether PACS symptoms form a unique pattern due to specific infection with SARS-CoV-2 remains debatable. Prospective case–control studies that do not rely on hospital records but measure the incidence of neuropsychiatric symptoms and diagnoses after COVID-19 are still scarce, but they are critical for distinguishing causation and confounding when characterizing PACS and the uniqueness of neuropsychiatric sequalae after COVID-19 (ref. 68 ). Recent studies with well-matched control groups illustrate that long-term consequences may not be so unique, as they were similar to those observed in patients with other diseases of similar severity, such as after acute myocardial infarction or in ICU patients 56 , 66 . A first prospective follow-up study of COVID-19 survivors and control patients matched on disease severity, age, sex and ICU admission found similar neuropsychiatric outcomes, regarding both new-onset psychiatric diagnosis (19% versus 20%) and neuropsychiatric symptoms (81% versus 93%). However, moderate but significantly worse cognitive outcomes 6 months after symptom onset were found among survivors of COVID-19 (ref. 69 ). In line with this, a longitudinal study of 785 participants from the UK Biobank showed small but significant cognitive impairment among individuals infected with SARS-CoV-2 compared to matched controls 70 .
Numerous psychosocial mechanisms can lead to neuropsychiatric sequalae of COVID-19, including functional impairment; psychological impact due to, for example, fear of dying; stress of being infected with a novel pandemic disease; isolation as part of quarantine and lack of social support; fear/guilt of spreading COVID-19 to family or community; and socioeconomic distress by lost wages 71 . However, there is also ample evidence that neurobiological mechanisms play an important role, which is discussed below.
Neurobiological mechanisms underlying neuropsychiatric sequelae of COVID-19
Acute neuropsychiatric symptoms among patients with severe COVID-19 have been found to correlate with the level of serum inflammatory markers 72 and coincide with neuroimaging findings of immune activation, including leukoencephalopathy, acute disseminated encephalomyelitis, cytotoxic lesions of the corpus callosum or cranial nerve enhancement 73 . Rare presentations, including meningitis, encephalitis, inflammatory demyelination, cerebral infarction and acute hemorrhagic necrotizing encephalopathy, have also been reported 74 . Hospitalized patients with frank encephalopathies display impaired blood-brain barrier (BBB) integrity with leptomeningeal enhancement on brain magnetic resonance images 75 . Studies of postmortem specimens from patients who succumbed to acute COVID-19 reveal significant neuropathology with signs of hypoxic damage and neuroinflammation. These include evidence of BBB permeability with extravasation of fibrinogen, microglial activation, astrogliosis, leukocyte infiltration and microhemorrhages 76 , 77 . However, it is still unclear to what extent these findings differ from patients with similar illness severity due to acute non-COVID illness, as these brain effects might not be virus-specific effects but rather due to cytokine-mediated neuroinflammation and critical illness.
Post-acute neuroimaging studies in SARS-CoV-2-recovered patients, as compared to control patients without COVID-19, reveal numerous alterations in brain structure on a group level, although effect sizes are generally small. These include minor reduction in gray matter thickness in the various regions of the cortex and within the corpus collosum, diffuse edema, increases in markers of tissue damage in regions functionally connected to the olfactory cortex and reductions in overall brain size 70 , 78 . Neuroimaging studies of post-acute COVID-19 patients also report abnormalities consistent with micro-structural and functional alterations, specifically within the hippocampus 79 , 80 , a brain region critical for memory formation and regulating anxiety, mood and stress responses, but also within gray matter areas involving the olfactory system and cingulate cortex 80 . Overall, these findings are in line with ongoing anosmia, tremors, affect problems and cognitive impairment.
Interestingly, despite findings mentioned above, there is little evidence of SARS-CoV-2 neuroinvasion with productive replication, and viral material is rarely found in the central nervous system (CNS) of patients with COVID-19 (refs. 76 , 77 , 81 ). Thus, neurobiological mechanisms of SARS-CoV-2-mediated neuropsychiatric sequelae remain unclear, especially in patients who initially present with milder forms of COVID-19. Symptomatic SARS-CoV-2 infection is associated with hypoxia, cytokine release syndrome (CRS) and dysregulated innate and adaptive immune responses (reviewed in ref. 82 ). All these effects could contribute to neuroinflammation and endothelial cell activation (Fig. 2 ). Examination of cerebrospinal fluid in patients with neuroimaging findings revealed elevated levels of pro-inflammatory, BBB-destabilizing cytokines, including interleukin-6 (IL-6), IL-1, IL-8 and mononuclear cell chemoattractants 83 , 84 . Whether these cytokines arise from the periphery, due to COVID-19-mediated CRS, or from within the CNS, is unclear. As studies generally lack control patients with other severe illnesses, the specificity of such findings to SARS-CoV-2 also remains unclear. Systemic inflammatory processes, including cytokine release, have been linked to glial activation with expression of chemoattractants that recruit immune cells, leading to neuroinflammation and injury 85 . Cerebrospinal fluid concentrations of neurofilament light, a biomarker of neuronal damage, were reportedly elevated in patients hospitalized with COVID-19 regardless of whether they exhibited neurologic diseases 86 . Acute thromboembolic events leading to ischemic infarcts are also common in patients with COVID-19 due to a potentially increased pro-coagulant process secondary to CRS 87 .
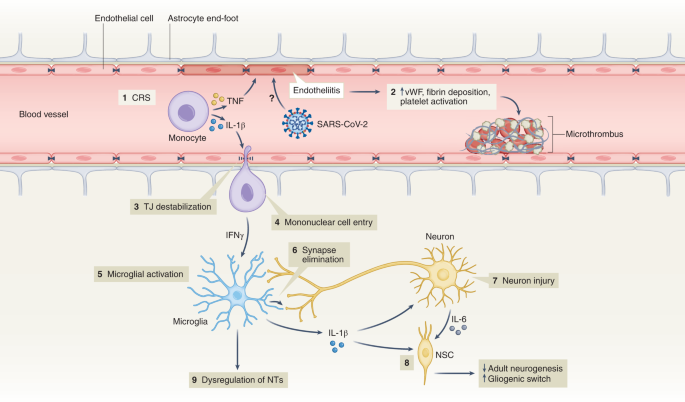
(1) Elevation of BBB-destabilizing cytokines (IL-1β and TNF) within the serum due to CRS or local interactions of mononuclear and endothelial cells. (2) Virus-induced endotheliitis increases susceptibility to microthrombus formation due to platelet activation, elevation of vWF and fibrin deposition. (3) Cytokine, mononuclear and endothelial cell interactions promote disruption of the BBB, which may allow entry of leukocytes expressing IFNg into the CNS (4), leading to microglial activation (5). (6) Activated microglia may eliminate synapses and/or express cytokines that promote neuronal injury. (7) Injured neurons express IL-6 which, together with IL-1β, promote a ‘gliogenic switch’ in NSCs (8), decreasing adult neurogenesis. (9) The combination of microglial (and possibly astrocyte) activation, neuronal injury and synapse loss may lead to dysregulation of NTs and neuronal circuitry. IFNg, interferon-g; NSC, neural stem cell; NT, neurotransmitter; TJ, tight junction; TNF, tumor necrosis factor; vWF, von Willebrand factor.
It is also unclear whether hospitalized patients with COVID-19 may develop brain abnormalities due to hypoxia or CRS rather than as a direct effect of SARS-CoV-2 infection. Hypoxia may cause neuronal dysfunction, cerebral edema, increased BBB permeability, cytokine expression and onset of neurodegenerative diseases 88 , 89 . CRS, with life-threatening levels of serum TNF-α and IL-1 (ref. 90 ) could also impact BBB function, as these cytokines destabilize microvasculature endothelial cell junctional proteins critical for BBB integrity 91 . In mild SARS-CoV-2 infection, circulating immune factors combined with mild hypoxia might impact BBB function and lead to neuroinflammation 92 , as observed during infection with other non-neuroinvasive respiratory pathogens 93 . However, multiple studies suggest that the SARS-CoV-2 spike protein itself may also induce venous and arterial endothelial cell activation and endotheliitis, disrupt BBB integrity or cross the BBB via adoptive transcytosis 94 , 95 , 96 .
Reducing neuropsychiatric sequelae of COVID-19
The increased risk of COVID-19-related neuropsychiatric sequalae was most pronounced during the first pandemic peak but reduced over the subsequent 2 years 64 , 97 . This may be due to reduced impact of newer SARS-CoV-2 strains (that is, Omicron) but also protective effects of vaccination, which limit SARS-CoV-2 spread and may, thus, prevent neuropsychiatric sequalae. Fully vaccinated individuals with breakthrough infections exhibit a 50% reduction in PACS 98 , even though vaccination does not improve PACS-related neuropsychiatric symptoms in patients with a prior history of COVID-19 (ref. 99 ). As patients with pre-existing mental disorders are at increased risk of SARS-CoV-2 infection, they deserve to be among the prioritization groups for vaccination efforts 100 .
Adequate treatment strategies for neuropsychiatric sequelae of COVID-19 are needed. As no specific evidence-based intervention yet exists, the best current treatment approach is that for neuropsychiatric sequelae arising after other severe medical conditions 101 . Stepped care—a staged approach of mental health services comprising a hierarchy of interventions, from least to most intensive, matched to the individual’s need—is efficacious with monitoring of mental health and cognitive problems. Milder symptoms likely benefit from counseling and holistic care, including physiotherapy, psychotherapy and rehabilitation. Individuals with moderate to severe symptoms fulfilling psychiatric diagnoses should receive guideline-concordant care for these disorders 61 . Patients with pre-existing mental disorders also deserve special attention when affected by COVID-19, as they have shown to have an increased risk of COVID-19-related hospitalization, complications and death 102 . This may involve interventions to address their general health, any unfavorable socioenvironmental factors, substance abuse or treatment adherence issues.
Lessons learned, knowledge gaps and future challenges
Ultimately, it is not only the millions of people who have died from COVID-19 worldwide that we remember but also the distress experienced during an unpredictable period with overstretched healthcare systems, lockdowns, school closures and changing work environments. In a world that is more and more globalized, connectivity puts us at risk for future pandemics. What can be learned from the last 2 years of the COVID-19 pandemic about how to handle future and longstanding challenges related to mental health?
Give mental health equal priority to physical health
The COVID-19 pandemic has demonstrated that our population seems quite resilient and adaptive. Nevertheless, even if society as a whole may bounce back, there is a large group of people whose mental health has been and will be disproportionately affected by this and future crises. Although various groups, such as the WHO 8 , the National Health Commission of China 103 , the Asia Pacific Disaster Mental Health Network 104 and a National Taskforce in India 105 , developed mental health policies early on, many countries were late in realizing that a mental health agenda deserves immediate attention in a rapidly evolving pandemic. Implementation of comprehensive and integrated mental health policies was generally inconsistent and suboptimal 106 and often in the shadow of policies directed at containing and reducing the spread of SARS-CoV-2. Leadership is needed to convey the message that mental health is as important as physical health and that we should focus specific attention and early interventions on those at the highest risk. This includes those vulnerable due to factors such as low socioeconomic status, specific developmental life phase (adolescents and young adults), pre-existing risk (poor physical or somatic health and early life trauma) or high exposure to pandemic-related (work) changes—for example, women and healthcare personnel. This means that not only should investment in youth and reducing health inequalities remain at the top of any policy agenda but also that mental health should be explicitly addressed from the start in any future global health crisis situation.
Communication and trust is crucial for mental health
Uncertainty and uncontrollability during the pandemic have challenged rational thinking. Negative news travels fast. Communication that is vague, one-sided and dishonest can negatively impact on mental health and amplify existing distress and anxiety 107 . Media reporting should not overemphasize negative mental health impact—for example, putative suicide rate increases or individual negative experiences—which could make situations worse than they actually are. Instead, communication during crises requires concrete and actionable advice that avoids polarization and strengthens vigilance, to foster resilience and help prevent escalation to severe mental health problems 108 , 109 .
Rapid research should be collaborative and high-quality
Within the scientific community, the topic of mental health during the pandemic led to a multitude of rapid studies that generally had limited methodological quality—for example, cross-sectional designs, small or selective sampling or study designs lacking valid comparison groups. These contributed rather little to our understanding of the mental health impact of the emerging crisis. In future events that have global mental health impact, where possible, collaborative and interdisciplinary efforts with well-powered and well-controlled prospective studies using standardized instruments will be crucial. Only with fine-grained determinants and outcomes can data reliably inform mental health policies and identify who is most at risk.
Do not neglect long-term mental health effects
So far, research has mainly focused on the acute and short-term effects of the pandemic on mental health, usually spanning pandemic effects over several months to 1 year. However, longer follow-up of how a pandemic impacts population mental health is essential. Can societal and economic disruptions after the pandemic increase risk of mental disorders at a later stage when the acute pandemic effects have subsided? Do increased self-reported mental health problems return to pre-pandemic levels, and which groups of individuals remain most affected in the long-term? We need to realize that certain pandemic consequences, particularly those affecting income and school/work careers, may become visible only over the course of several years. Consequently, we should maintain focus and continue to monitor and quantify the effects of the pandemic in the years to come—for example, by monitoring mental healthcare use and suicide. This should include specific at-risk populations (for example, adolescents) and understudied populations in low-income and middle-income countries.
Pay attention to mental health consequences of infectious diseases
Even though our knowledge on PACS is rapidly expanding, there are still many unanswered questions related to who is at risk, the long-term course trajectories and the best ways to intervene early. Consequently, we need to be aware of the neuropsychiatric sequelae of COVID-19 and, for that matter, of any infectious disease. Clinical attention and research should be directed toward alleviating potential neuropsychiatric ramifications of COVID-19. Next to clinical studies, studies using human tissues and appropriate animal models are pivotal to determine the CNS region-specific and neural-cell-specific effects of SARS-CoV-2 infection and the induced immune activation. Indeed, absence of SARS-CoV-2 neuroinvasion is an opportunity to learn and discover how peripheral neuroimmune mechanisms can contribute to neuropsychiatric sequelae in susceptible individuals. This emphasizes the importance of an interdisciplinary approach where somatic and mental health efforts are combined but also the need to integrate clinical parameters after infection with biological parameters (for example, serum, cerebrospinal fluid and/or neuroimaging) to predict who is at risk for PACS and deliver more targeted treatments.
Prepare mental healthcare infrastructure for pandemic times
If we take mental health seriously, we should not only monitor it but also develop the resources and infrastructure necessary for rapid early intervention, particularly for specific vulnerable groups. For adequate mental healthcare to be ready for pandemic times, primary care, community mental health and public mental health should be prepared. In many countries, health services were not able to meet the population’s mental health needs before the pandemic, which substantially worsened during the pandemic. We should ensure rapid access to mental health services but also address the underlying drivers of poor mental health, such as mitigating risks of unemployment, sexual violence and poverty. Collaboration in early stages across disciplines and expertise is essential. Anticipating disruption to face-to-face services, mental healthcare providers should be more prepared for consultations, therapy and follow-up by telephone, video-conferencing platforms and web applications 51 , 52 . The pandemic has shown that an inadequate infrastructure, pre-existing inequalities and low levels of technological literacy hindered the use and uptake of e-health, both in healthcare providers and in patients across different care settings. The necessary investments can ensure rapid upscaling of mental health services during future pandemics for those individuals with a high mental health need due to societal changes, government measures, fear of infection or infection itself.
Even though much attention has been paid to the physical health consequences of COVID-19, mental health has unjustly received less attention. There is an urgent need to prepare our research and healthcare infrastructures not only for adequate monitoring of the long-term mental health effects of the COVID-19 pandemic but also for future crises that will shape mental health. This will require collaboration to ensure interdisciplinary and sound research and to provide attention and care at an early stage for those individuals who are most vulnerable—giving mental health equal priority to physical health from the very start.
WHO Coronavirus (COVID-19) Dashboard (WHO, 2022; https://covid19.who.int/
Rando, H. M. et al. Challenges in defining long COVID: striking differences across literature, electronic health records, and patient-reported information. Preprint at https://www.medrxiv.org/content/10.1101/2021.03.20.21253896v1 (2021).
Nalbandian, A. et al. Post-acute COVID-19 syndrome. Nat. Med. 27 , 601–615 (2021).
Article CAS PubMed PubMed Central Google Scholar
Abbafati, C. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396 , 1204–1222 (2020).
Article Google Scholar
Penninx, B. W., Pine, D. S., Holmes, E. A. & Reif, A. Anxiety disorders. Lancet 397 , 914–927 (2021).
Article PubMed PubMed Central Google Scholar
Herrman, H. et al. Time for united action on depression: a Lancet –World Psychiatric Association Commission. Lancet 399 , 957–1022 (2022).
Article PubMed Google Scholar
Radka, K., Wyeth, E. H. & Derrett, S. A qualitative study of living through the first New Zealand COVID-19 lockdown: affordances, positive outcomes, and reflections. Prev. Med. Rep. 26 , 101725 (2022).
Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact (WHO, 2022).
Dragioti, E. et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 94 , 1935–1949 (2022).
Zhang, S. X. et al. Mental disorder symptoms during the COVID-19 pandemic in Latin America—a systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 31 , e23 (2022).
Zhang, S. X. et al. Meta-analytic evidence of depression and anxiety in Eastern Europe during the COVID-19 pandemic. Eur. J. Psychotraumatol . 13 , 2000132 (2022).
Racine, N. et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 175 , 1142–1150 (2021).
Robinson, E., Sutin, A. R., Daly, M. & Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 296 , 567–576 (2022).
Article CAS PubMed Google Scholar
Prati, G. & Mancini, A. D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 51 , 201–211 (2021).
Patel, K. et al. Psychological distress before and during the COVID-19 pandemic among adults in the United Kingdom based on coordinated analyses of 11 longitudinal studies. JAMA Netw. Open 5 , e227629 (2022).
Ernst, M. et al. Loneliness before and during the COVID-19 pandemic: a systematic review with meta-analysis. Am. Psychol . 77 , 660–677 (2022).
Kilian, C. et al. Changes in alcohol use during the COVID-19 pandemic in Europe: a meta-analysis of observational studies. Drug Alcohol Rev . 41 , 918–931 (2022).
Acuff, S. F., Strickland, J. C., Tucker, J. A. & Murphy, J. G. Changes in alcohol use during COVID-19 and associations with contextual and individual difference variables: a systematic review and meta-analysis. Psychol. Addict. Behav. 36 , 1–19 (2022).
Varga, T. V. et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg. Health Eur . 2 , 100020 (2021).
Fancourt, D., Steptoe, A. & Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry 8 , 141–149 (2021).
Jia, H. et al. National and state trends in anxiety and depression severity scores among adults during the COVID-19 pandemic—United States, 2020–2021. MMWR Morb. Mortal. Wkly. Rep. 70 , 1427–1432 (2021).
Kok, A. A. L. et al. Mental health and perceived impact during the first Covid-19 pandemic year: a longitudinal study in Dutch case–control cohorts of persons with and without depressive, anxiety, and obsessive-compulsive disorders. J. Affect. Disord. 305 , 85–93 (2022).
Su, Y. et al. Prevalence of loneliness and social isolation among older adults during the COVID-19 pandemic: a systematic review and meta-analysis. Int. Psychogeriatr. https://doi.org/10.1017/S1041610222000199 (2022).
Knox, L., Karantzas, G. C., Romano, D., Feeney, J. A. & Simpson, J. A. One year on: what we have learned about the psychological effects of COVID-19 social restrictions: a meta-analysis. Curr. Opin. Psychol. 46 , 101315 (2022).
Aknin, L. B. et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. Lancet Public Health 7 , e417–e426 (2022).
Lee, Y. et al. Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J. Affect. Disord. 290 , 364–377 (2021).
Wu, J. T. et al. Nowcasting epidemics of novel pathogens: lessons from COVID-19. Nat. Med. 27 , 388–395 (2021).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395 , 912–920 (2020).
Santomauro, D. F. et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 398 , 1700–1712 (2021).
Knudsen, A. K. S. et al. Prevalence of mental disorders, suicidal ideation and suicides in the general population before and during the COVID-19 pandemic in Norway: a population-based repeated cross-sectional analysis. Lancet Reg. Health Eur . 4 , 100071 (2021).
Ayuso-Mateos, J. L. et al. Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population. Epidemiol. Psychiatr. Sci . 30 , e49 (2021).
Vloo, A. et al. Gender differences in the mental health impact of the COVID-19 lockdown: longitudinal evidence from the Netherlands. SSM Popul. Health 15 , 100878 (2021).
Winkler, P. et al. Prevalence of current mental disorders before and during the second wave of COVID-19 pandemic: an analysis of repeated nationwide cross-sectional surveys. J. Psychiatr. Res. 139 , 167–171 (2021).
Pirkis, J. et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry 8 , 579–588 (2021).
Faust, J. S. et al. Mortality from drug overdoses, homicides, unintentional injuries, motor vehicle crashes, and suicides during the pandemic, March–August 2020. JAMA 326 , 84–86 (2021).
John, A. et al. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: update of living systematic review. F1000Res. 9 , 1097 (2020).
Steeg, S. et al. Temporal trends in primary care-recorded self-harm during and beyond the first year of the COVID-19 pandemic: time series analysis of electronic healthcare records for 2.8 million patients in the Greater Manchester Care Record. EClinicalMedicine 41 , 101175 (2021).
Rømer, T. B. et al. Psychiatric admissions, referrals, and suicidal behavior before and during the COVID-19 pandemic in Denmark: a time-trend study. Acta Psychiatr. Scand. 144 , 553–562 (2021).
Holland, K. M. et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry 78 , 372–379 (2021).
Kunzler, A. M. et al. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Global Health 17 , 34 (2021).
Flor, L. S. et al. Quantifying the effects of the COVID-19 pandemic on gender equality on health, social, and economic indicators: a comprehensive review of data from March, 2020, to September, 2021. Lancet 399 , 2381–2397 (2022).
Viner, R. et al. School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the first COVID-19 wave: a systematic review. JAMA Pediatr. 176 , 400–409 (2022).
Zheng, X. Y. et al. Trends of injury mortality during the COVID-19 period in Guangdong, China: a population-based retrospective analysis. BMJ Open 11 , e045317 (2021).
Tanaka, T. & Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 5 , 229–238 (2021).
Thomeer, M. B., Moody, M. D. & Yahirun, J. Racial and ethnic disparities in mental health and mental health care during the COVID-19 pandemic. J. Racial Ethn. Health Disparities https://doi.org/10.1007/s40615-021-01006-7 (2022).
Hill, J. E. et al. The prevalence of mental health conditions in healthcare workers during and after a pandemic: systematic review and meta-analysis. J. Adv. Nurs. 78 , 1551–1573 (2022).
Marvaldi, M., Mallet, J., Dubertret, C., Moro, M. R. & Guessoum, S. B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 126 , 252–264 (2021).
Phiri, P. et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine 34 , 100806 (2021).
Jorm, A. F., Patten, S. B., Brugha, T. S. & Mojtabai, R. Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries. World Psychiatry 16 , 90–99 (2017).
Third Round of the Global Pulse Survey on Continuity of Essential Health Services during the COVID-19 Pandemic (WHO, 2021).
Baumgart, J. G. et al. The early impacts of the COVID-19 pandemic on mental health facilities and psychiatric professionals. Int. J. Environ. Res. Public Health 18 , 8034 (2021).
Raphael, J., Winter, R. & Berry, K. Adapting practice in mental healthcare settings during the COVID-19 pandemic and other contagions: systematic review. BJPsych Open 7 , e62 (2021).
Anderson, K. N. et al. Changes and inequities in adult mental health-related emergency department visits during the COVID-19 pandemic in the US. JAMA Psychiatry 79 , 475–485 (2022).
Pan, K. Y. et al. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case–control cohorts. Lancet Psychiatry 8 , 121–129 (2021).
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W. & Kelley, K. W. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat. Rev. Neurosci. 9 , 46–56 (2008).
Nersesjan, V. et al. Central and peripheral nervous system complications of COVID-19: a prospective tertiary center cohort with 3-month follow-up. J. Neurol. 268 , 3086–3104 (2021).
Wilson, J. E. et al. Delirium. Nat. Rev. Dis. Prim . 6 , 90 (2020).
Rawal, G., Yadav, S. & Kumar, R. Post-intensive care syndrome: an overview. J. Transl. Intern. Med. 5 , 90–92 (2017).
Pandharipande, P. P. et al. Long-term cognitive impairment after critical illness. N. Engl. J. Med. 369 , 1306–1316 (2013).
Girard, T. D. et al. Long-term cognitive impairment after hospitalization for community-acquired pneumonia: a prospective cohort study. J. Gen. Intern. Med. 33 , 929–935 (2018).
Crook, H., Raza, S., Nowell, J., Young, M. & Edison, P. Long covid—mechanisms, risk factors, and management. BMJ 374 , n1648 (2021).
Badenoch, J. B. et al. Persistent neuropsychiatric symptoms after COVID-19: a systematic review and meta-analysis. Brain Commun . 4 , fcab297 (2021).
Ceban, F. et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav. Immun. 101 , 93–135 (2022).
Taquet, M., Geddes, J. R., Husain, M., Luciano, S. & Harrison, P. J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 8 , 416–427 (2021).
Xie, Y., Xu, E. & Al-Aly, Z. Risks of mental health outcomes in people with covid-19: cohort study. BMJ 376 , e068993 (2022).
Kieran Clift, A. et al. Neuropsychiatric ramifications of severe COVID-19 and other severe acute respiratory infections. JAMA Psychiatry 79 , 690–698 (2022).
Castro, V. M., Rosand, J., Giacino, J. T., McCoy, T. H. & Perlis, R. H. Case–control study of neuropsychiatric symptoms following COVID-19 hospitalization in 2 academic health systems. Mol. Psych. (in the press).
Amin-Chowdhury, Z. & Ladhani, S. N. Causation or confounding: why controls are critical for characterizing long COVID. Nat. Med. 27 , 1129–1130 (2021).
Nersesjan, V. et al. Neuropsychiatric and cognitive outcomes in patients 6 months after COVID-19 requiring hospitalization compared with matched control patients hospitalized for non-COVID-19 illness. JAMA Psychiatry 79 , 486–497 (2022).
Douaud, G. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604 , 697–707 (2022).
Zhang, H. et al. Psychological experience of COVID-19 patients: a systematic review and qualitative meta-synthesis. Am. J. Infect. Control 50 , 809–819 (2022).
Mazza, M. G. et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav. Immun. 89 , 594–600 (2020).
Moonis, G. et al. The spectrum of neuroimaging findings on CT and MRI in adults With COVID-19. AJR Am. J. Roentgenol. 217 , 959–974 (2021).
Asadi-Pooya, A. A. & Simani, L. Central nervous system manifestations of COVID-19: a systematic review. J. Neurol. Sci . 413 , 116832 (2020).
Lersy, F. et al. Cerebrospinal fluid features in patients with Coronavirus Disease 2019 and neurological manifestations: correlation with brain magnetic resonance imaging findings in 58 patients. J. Infect. Dis. 223 , 600–609 (2021).
Thakur, K. T. et al. COVID-19 neuropathology at Columbia University Irving Medical Center/New York Presbyterian Hospital. Brain 144 , 2696–2708 (2021).
Cosentino, G. et al. Neuropathological findings from COVID-19 patients with neurological symptoms argue against a direct brain invasion of SARS-CoV-2: a critical systematic review. Eur. J. Neurol. 28 , 3856–3865 (2021).
Tian, T. et al. Long-term follow-up of dynamic brain changes in patients recovered from COVID-19 without neurological manifestations. JCI Insight 7 , e155827 (2022).
Lu, Y. et al. Cerebral micro-structural changes in COVID-19 patients—an MRI-based 3-month follow-up study. EClinicalMedicine 25 , 100484 (2020).
Qin, Y. et al . Long-term microstructure and cerebral blood flow changes in patients recovered from COVID-19 without neurological manifestations. J. Clin. Invest . 131 , e147329 (2021).
Matschke, J. et al. Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol. 19 , 919–929 (2020).
Shivshankar, P. et al. SARS-CoV-2 infection: host response, immunity, and therapeutic targets. Inflammation 45 , 1430–1449 (2022).
Manganotti, P. et al. Cerebrospinal fluid and serum interleukins 6 and 8 during the acute and recovery phase in COVID-19 neuropathy patients. J. Med. Virol. 93 , 5432–5437 (2021).
Farhadian, S. et al. Acute encephalopathy with elevated CSF inflammatory markers as the initial presentation of COVID-19. BMC Neurol . 20 , 248 (2020).
Francistiová, L. et al. Cellular and molecular effects of SARS-CoV-2 linking lung infection to the brain. Front. Immunol . 12 , 730088 (2021).
Paterson, R. W. et al. Serum and cerebrospinal fluid biomarker profiles in acute SARS-CoV-2-associated neurological syndromes. Brain Commun . 3 , fcab099 (2021).
Cryer, M. J. et al. Prothrombotic milieu, thrombotic events and prophylactic anticoagulation in hospitalized COVID-19 positive patients: a review. Clin. Appl. Thromb. Hemost . 28 , 10760296221074353 (2022).
Nalivaeva, N. N. & Rybnikova, E. A. Editorial: Brain hypoxia and ischemia: new insights into neurodegeneration and neuroprotection. Front. Neurosci . 13 , 770 (2019).
Brownlee, N. N. M., Wilson, F. C., Curran, D. B., Lyttle, N. & McCann, J. P. Neurocognitive outcomes in adults following cerebral hypoxia: a systematic literature review. NeuroRehabilitation 47 , 83–97 (2020).
Del Valle, D. M. et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 26 , 1636–1643 (2020).
Daniels, B. P. et al. Viral pathogen-associated molecular patterns regulate blood–brain barrier integrity via competing innate cytokine signals. mBio 5 , e01476-14 (2014).
Reynolds, J. L. & Mahajan, S. D. SARS-COV2 alters blood brain barrier integrity contributing to neuro-inflammation. J. Neuroimmune Pharmacol. 16 , 4–6 (2021).
Bohmwald, K., Gálvez, N. M. S., Ríos, M. & Kalergis, A. M. Neurologic alterations due to respiratory virus infections. Front. Cell. Neurosci . 12 , 386 (2018).
Khaddaj-Mallat, R. et al. SARS-CoV-2 deregulates the vascular and immune functions of brain pericytes via spike protein. Neurobiol. Dis . 161 , 105561 (2021).
Qian, Y. et al. Direct activation of endothelial cells by SARS-CoV-2 nucleocapsid protein is blocked by simvastatin. J Virol. 95 , e0139621 (2021).
Rhea, E. M. et al. The S1 protein of SARS-CoV-2 crosses the blood–brain barrier in mice. Nat. Neurosci. 24 , 368–378 (2021).
Magnúsdóttir, I. et al. Acute COVID-19 severity and mental health morbidity trajectories in patient populations of six nations: an observational study. Lancet Public Health 7 , e406–e416 (2022).
Antonelli, M. et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case–control study. Lancet Infect. Dis. 22 , 43–55 (2022).
Wisnivesky, J. P. et al. Association of vaccination with the persistence of post-COVID symptoms. J. Gen. Intern. Med . 37 , 1748–1753 (2022).
De Picker, L. J. et al. Severe mental illness and European COVID-19 vaccination strategies. Lancet Psychiatry 8 , 356–359 (2021).
Cohen, G. H. et al. Comparison of simulated treatment and cost-effectiveness of a stepped care case-finding intervention vs usual care for posttraumatic stress disorder after a natural disaster. JAMA Psychiatry 74 , 1251–1258 (2017).
Vai, B. et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry 8 , 797–812 (2021).
Xiang, Y. T. et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7 , 228 (2020).
Newnham, E. A. et al. The Asia Pacific Disaster Mental Health Network: setting a mental health agenda for the region. Int. J. Environ. Res. Public Health 17 , 6144 (2020).
Article CAS PubMed Central Google Scholar
Dandona, R. & Sagar, R. COVID-19 offers an opportunity to reform mental health in India. Lancet Psychiatry 8 , 9–11 (2021).
Qiu, D. et al. Policies to improve the mental health of people influenced by COVID-19 in China: a scoping review. Front. Psychiatry 11 , 588137 (2020).
Su, Z. et al. Mental health consequences of COVID-19 media coverage: the need for effective crisis communication practices. Global Health 17 , 4 (2021).
Petersen, M. B. COVID lesson: trust the public with hard truths. Nature 598 , 237 (2021).
van der Bles, A. M., van der Linden, S., Freeman, A. L. J. & Spiegelhalter, D. J. The effects of communicating uncertainty on public trust in facts and numbers. Proc. Natl Acad. Sci. USA 117 , 7672–7683 (2020).
Titze-de-Almeida, R. et al. Persistent, new-onset symptoms and mental health complaints in Long COVID in a Brazilian cohort of non-hospitalized patients. BMC Infect. Dis. 22 , 133 (2022).
Carfì, A., Bernabei, R. & Landi, F. Persistent symptoms in patients after acute COVID-19. JAMA 324 , 603–605 (2020).
Bliddal, S. et al. Acute and persistent symptoms in non-hospitalized PCR-confirmed COVID-19 patients. Sci. Rep. 11 , 13153 (2021).
Kim, Y. et al. Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect. Dis . 22 , 93 (2022).
Download references
Acknowledgements
The authors thank E. Giltay for assistance on data analyses and production of Fig. 1 . B.W.J.H.P. discloses support for research and publication of this work from the European Union’s Horizon 2020 research and innovation programme-funded RESPOND project (grant no. 101016127).
Author information
Authors and affiliations.
Department of Psychiatry, Amsterdam UMC, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands
Brenda W. J. H. Penninx & Christiaan H. Vinkers
Amsterdam Public Health, Mental Health Program and Amsterdam Neuroscience, Mood, Anxiety, Psychosis, Sleep & Stress Program, Amsterdam, The Netherlands
Biological and Precision Psychiatry, Copenhagen Research Center for Mental Health, Mental Health Center Copenhagen, Copenhagen University Hospital, Copenhagen, Denmark
Michael E. Benros
Department of Immunology and Microbiology, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark
Departments of Medicine, Pathology & Immunology and Neuroscience, Center for Neuroimmunology & Neuroinfectious Diseases, Washington University School of Medicine, St. Louis, MO, USA
Robyn S. Klein
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Brenda W. J. H. Penninx .
Ethics declarations
Competing interests.
The authors declare no conflicts of interest.
Peer review
Peer review information.
Nature Medicine thanks Jane Pirkis and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary handling editor: Karen O’Leary, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Penninx, B.W.J.H., Benros, M.E., Klein, R.S. et al. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med 28 , 2027–2037 (2022). https://doi.org/10.1038/s41591-022-02028-2
Download citation
Received : 06 June 2022
Accepted : 26 August 2022
Published : 03 October 2022
Issue Date : October 2022
DOI : https://doi.org/10.1038/s41591-022-02028-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Mental health disturbance in preclinical medical students and its association with screen time, sleep quality, and depression during the covid-19 pandemic.
- Tjhin Wiguna
- Valerie Josephine Dirjayanto
- Erik Kinzie
BMC Psychiatry (2024)
Protocol for a pilot cluster randomised controlled trial of a multicomponent sustainable return to work IGLOo intervention
- Oliver Davis
- Jeremy Dawson
- Fehmidah Munir
Pilot and Feasibility Studies (2024)
Impact of COVID-19 first wave on the mental health of healthcare workers in a Front-Line Spanish Tertiary Hospital: lessons learned
- Juan D. Molina
- Franco Amigo
- Gabriel Rubio
Scientific Reports (2024)
Long-term risk of psychiatric disorder and psychotropic prescription after SARS-CoV-2 infection among UK general population
- Daniel Prieto-Alhambra
Nature Human Behaviour (2024)
Changes in alcohol consumption and alcohol problems before and after the COVID-19 pandemic: a prospective study in heavy drinking young adults
- Kasey G. Creswell
- Garrett C. Hisler
- Aidan G. C. Wright
Nature Mental Health (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 11 April 2023
Effects of the COVID-19 pandemic on mental health, anxiety, and depression
- Ida Kupcova 1 ,
- Lubos Danisovic 1 ,
- Martin Klein 2 &
- Stefan Harsanyi 1
BMC Psychology volume 11 , Article number: 108 ( 2023 ) Cite this article
8988 Accesses
12 Citations
38 Altmetric
Metrics details
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact. According to the World Health Organization (WHO), anxiety and depression prevalence increased by 25% globally. In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population.
A cross-sectional study using an anonymous online-based 45-question online survey was conducted at Comenius University in Bratislava. The questionnaire comprised five general questions and two assessment tools the Zung Self-Rating Anxiety Scale (SAS) and the Zung Self-Rating Depression Scale (SDS). The results of the Self-Rating Scales were statistically examined in association with sex, age, and level of education.
A total of 205 anonymous subjects participated in this study, and no responses were excluded. In the study group, 78 (38.05%) participants were male, and 127 (61.69%) were female. A higher tendency to anxiety was exhibited by female participants (p = 0.012) and the age group under 30 years of age (p = 0.042). The level of education has been identified as a significant factor for changes in mental state, as participants with higher levels of education tended to be in a worse mental state (p = 0.006).
Conclusions
Summarizing two years of the COVID-19 pandemic, the mental state of people with higher levels of education tended to feel worse, while females and younger adults felt more anxiety.
Peer Review reports
Introduction
The first mention of the novel coronavirus came in 2019, when this variant was discovered in the city of Wuhan, China, and became the first ever documented coronavirus pandemic [ 1 , 2 , 3 ]. At this time there was only a sliver of fear rising all over the globe. However, in March 2020, after the declaration of a global pandemic by the World Health Organization (WHO), the situation changed dramatically [ 4 ]. Answering this, yet an unknown threat thrust many countries into a psycho-socio-economic whirlwind [ 5 , 6 ]. Various measures taken by governments to control the spread of the virus presented the worldwide population with a series of new challenges to which it had to adjust [ 7 , 8 ]. Lockdowns, closed schools, losing employment or businesses, and rising deaths not only in nursing homes came to be a new reality [ 9 , 10 , 11 ]. Lack of scientific information on the novel coronavirus and its effects on the human body, its fast spread, the absence of effective causal treatment, and the restrictions which harmed people´s social life, financial situation and other areas of everyday life lead to long-term living conditions with increased stress levels and low predictability over which people had little control [ 12 ].
Risks of changes in the mental state of the population came mainly from external risk factors, including prolonged lockdowns, social isolation, inadequate or misinterpreted information, loss of income, and acute relationship with the rising death toll. According to the World Health Organization (WHO), since the outbreak of the COVID-19 pandemic, anxiety and depression prevalence increased by 25% globally [ 13 ]. Unemployment specifically has been proven to be also a predictor of suicidal behavior [ 14 , 15 , 16 , 17 , 18 ]. These risk factors then interact with individual psychological factors leading to psychopathologies such as threat appraisal, attentional bias to threat stimuli over neutral stimuli, avoidance, fear learning, impaired safety learning, impaired fear extinction due to habituation, intolerance of uncertainty, and psychological inflexibility. The threat responses are mediated by the limbic system and insula and mitigated by the pre-frontal cortex, which has also been reported in neuroimaging studies, with reduced insula thickness corresponding to more severe anxiety and amygdala volume correlated to anhedonia as a symptom of depression [ 19 , 20 , 21 , 22 , 23 ]. Speaking in psychological terms, the pandemic disturbed our core belief, that we are safe in our communities, cities, countries, or even the world. The lost sense of agency and confidence regarding our future diminished the sense of worth, identity, and meaningfulness of our lives and eroded security-enhancing relationships [ 24 ].
Slovakia introduced harsh public health measures in the first wave of the pandemic, but relaxed these measures during the summer, accompanied by a failure to develop effective find, test, trace, isolate and support systems. Due to this, the country experienced a steep growth in new COVID-19 cases in September 2020, which lead to the erosion of public´s trust in the government´s management of the situation [ 25 ]. As a means to control the second wave of the pandemic, the Slovak government decided to perform nationwide antigen testing over two weekends in November 2020, which was internationally perceived as a very controversial step, moreover, it failed to prevent further lockdowns [ 26 ]. In addition, there was a sharp rise in the unemployment rate since 2020, which continued until July 2020, when it gradually eased [ 27 ]. Pre-pandemic, every 9th citizen of Slovakia suffered from a mental health disorder, according to National Statistics Office in 2017, the majority being affective and anxiety disorders. A group of authors created a web questionnaire aimed at psychiatrists, psychologists, and their patients after the first wave of the COVID-19 pandemic in Slovakia. The results showed that 86.6% of respondents perceived the pathological effect of the pandemic on their mental status, 54.1% of whom were already treated for affective or anxiety disorders [ 28 ].
In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population. This study aimed to assess the symptoms of anxiety and depression in the general public of Slovakia. After the end of epidemiologic restrictive measures (from March to May 2022), we introduced an anonymous online questionnaire using adapted versions of Zung Self-Rating Anxiety Scale (SAS) and Zung Self-Rating Depression Scale (SDS) [ 29 , 30 ]. We focused on the general public because only a portion of people who experience psychological distress seek professional help. We sought to establish, whether during the pandemic the population showed a tendency to adapt to the situation or whether the anxiety and depression symptoms tended to be present even after months of better epidemiologic situation, vaccine availability, and studies putting its effects under review [ 31 , 32 , 33 , 34 ].
Materials and Methods
This study utilized a voluntary and anonymous online self-administered questionnaire, where the collected data cannot be linked to a specific respondent. This study did not process any personal data. The questionnaire consisted of 45 questions. The first three were open-ended questions about participants’ sex, age (date of birth was not recorded), and education. Followed by 2 questions aimed at mental health and changes in the will to live. Further 20 and 20 questions consisted of the Zung SAS and Zung SDS, respectively. Every question in SAS and SDS is scored from 1 to 4 points on a Likert-style scale. The scoring system is introduced in Fig. 1 . Questions were presented in the Slovak language, with emphasis on maintaining test integrity, so, if possible, literal translations were made from English to Slovak. The questionnaire was created and designed in Google Forms®. Data collection was carried out from March 2022 to May 2022. The study was aimed at the general population of Slovakia in times of difficult epidemiologic and social situations due to the high prevalence and incidence of COVID-19 cases during lockdowns and social distancing measures. Because of the character of this web-based study, the optimal distribution of respondents could not be achieved.
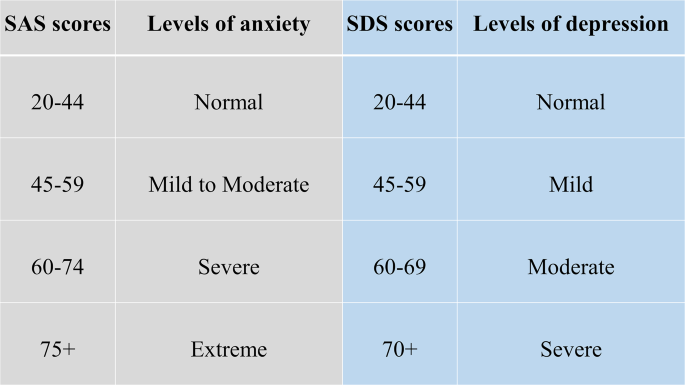
Categories of Zung SAS and SDS scores with clinical interpretation
During the course of this study, 205 respondents answered the anonymous questionnaire in full and were included in the study. All respondents were over 18 years of age. The data was later exported from Google Forms® as an Excel spreadsheet. Coding and analysis were carried out using IBM SPSS Statistics version 26 (IBM SPSS Statistics for Windows, Version 26.0, Armonk, NY, USA). Subject groups were created based on sex, age, and education level. First, sex due to differences in emotional expression. Second, age was a risk factor due to perceived stress and fear of the disease. Last, education due to different approaches to information. In these groups four factors were studied: (1) changes in mental state; (2) affected will to live, or frequent thoughts about death; (3) result of SAS; (4) result of SDS. For SAS, no subject in the study group scored anxiety levels of “severe” or “extreme”. Similarly for SDS, no subject depression levels reached “moderate” or “severe”. Pearson’s chi-squared test(χ2) was used to analyze the association between the subject groups and studied factors. The results were considered significant if the p-value was less than 0.05.
Ethical permission was obtained from the local ethics committee (Reference number: ULBGaKG-02/2022). This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines. Due to the anonymous design of the study and by the institutional requirements, written informed consent for participation was not required for this study.
In the study, out of 205 subjects in the study group, 127 (62%) were female and 78 (38%) were male. The average age in the study group was 35.78 years of age (range 19–71 years), with a median of 34 years. In the age group under 30 years of age were 34 (16.6%) subjects, while 162 (79%) were in the range from 31 to 49 and 9 (0.4%) were over 50 years old. 48 (23.4%) participants achieved an education level of lower or higher secondary and 157 (76.6%) finished university or higher. All answers of study participants were included in the study, nothing was excluded.
In Tables 1 and 2 , we can see the distribution of changes in mental state and will to live as stated in the questionnaire. In Table 1 we can see a disproportion in education level and mental state, where participants with higher education tended to feel worse much more than those with lower levels of education. Changes based on sex and age did not show any statistically significant results.
In Table 2 . we can see, that decreased will to live and frequent thoughts about death were only marginally present in the study group, which suggests that coping mechanisms play a huge role in adaptation to such events (e.g. the global pandemic). There is also a possibility that living in times of better epidemiologic situations makes people more likely to forget about the bad past.
Anxiety and depression levels as seen in Tables 3 and 4 were different, where female participants and the age group under 30 years of age tended to feel more anxiety than other groups. No significant changes in depression levels based on sex, age, and education were found.
Compared to the estimated global prevalence of depression in 2017 (3.44%), in 2021 it was approximately 7 times higher (25%) [ 14 ]. Our study did not prove an increase in depression, while anxiety levels and changes in the mental state did prove elevated. No significant changes in depression levels go in hand with the unaffected will to live and infrequent thoughts about death, which were important findings, that did not supplement our primary hypothesis that the fear of death caused by COVID-19 or accompanying infections would enhance personal distress and depression, leading to decreases in studied factors. These results are drawn from our limited sample size and uneven demographic distribution. Suicide ideations rose from 5% pre-pandemic to 10.81% during the pandemic [ 35 ]. In our study, 9.3% of participants experienced thoughts about death and since we did not specifically ask if they thought about suicide, our results only partially correlate with suicidal ideations. However, as these subjects exhibited only moderate levels of anxiety and mild levels of depression, the rise of suicide ideations seems unlikely. The rise in suicidal ideations seemed to be especially true for the general population with no pre-existing psychiatric conditions in the first months of the pandemic [ 36 ]. The policies implemented by countries to contain the pandemic also took a toll on the population´s mental health, as it was reported, that more stringent policies, mainly the social distancing and perceived government´s handling of the pandemic, were related to worse psychological outcomes [ 37 ]. The effects of lockdowns are far-fetched and the increases in mental health challenges, well-being, and quality of life will require a long time to be understood, as Onyeaka et al. conclude [ 10 ]. These effects are not unforeseen, as the global population suffered from life-altering changes in the structure and accessibility of education or healthcare, fluctuations in prices and food insecurity, as well as the inevitable depression of the global economy [ 38 ].
The loneliness associated with enforced social distancing leads to an increase in depression, anxiety, and posttraumatic stress in children in adolescents, with possible long-term sequelae [ 39 ]. The increase in adolescent self-injury was 27.6% during the pandemic [ 40 ]. Similar findings were described in the middle-aged and elderly population, in which both depression and anxiety prevalence rose at the beginning of the pandemic, during the pandemic, with depression persisting later in the pandemic, while the anxiety-related disorders tended to subside [ 41 ]. Medical professionals represented another specific at-risk group, with reported anxiety and depression rates of 24.94% and 24.83% respectively [ 42 ]. The dynamic of psychopathology related to the COVID-19 pandemic is not clear, with studies reporting a return to normal later in 2020, while others describe increased distress later in the pandemic [ 20 , 43 ].
Concerning the general population, authors from Spain reported that lockdowns and COVID-19 were associated with depression and anxiety [ 44 ]. In January 2022 Zhao et al., reported an elevation in hoarding behavior due to fear of COVID-19, while this process was moderated by education and income levels, however, less in the general population if compared to students [ 45 ]. Higher education levels and better access to information could improve persons’ fear of the unknown, however, this fact was not consistent with our expectations in this study, as participants with university education tended to feel worse than participants with lower education. A study on adolescents and their perceived stress in the Czech Republic concluded that girls are more affected by lockdowns. The strongest predictor was loneliness, while having someone to talk to, scored the lowest [ 46 ]. Garbóczy et al. reported elevated perceived stress levels and health anxiety in 1289 Hungarian and international students, also affected by disengagement from home and inadequate coping strategies [ 47 ]. Wathelet et al. conducted a study on French University students confined during the pandemic with alarming results of a high prevalence of mental health issues in the study group [ 48 ]. Our study indicated similar results, as participants in the age group under 30 years of age tended to feel more anxious than others.
In conclusion, we can say that this pandemic changed the lives of many. Many of us, our family members, friends, and colleagues, experienced life-altering events and complicated situations unseen for decades. Our decisions and actions fueled the progress in medicine, while they also continue to impact society on all levels. The long-term effects on adolescents are yet to be seen, while effects of pain, fear, and isolation on the general population are already presenting themselves.
The limitations of this study were numerous and as this was a web-based study, the optimal distribution of respondents could not be achieved, due to the snowball sampling strategy. The main limitation was the small sample size and uneven demographic distribution of respondents, which could impact the representativeness of the studied population and increase the margin of error. Similarly, the limited number of older participants could significantly impact the reported results, as age was an important risk factor and thus an important stressor. The questionnaire omitted the presence of COVID-19-unrelated life-changing events or stressors, and also did not account for any preexisting condition or risk factor that may have affected the outcome of the used assessment scales.
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to compliance with institutional guidelines but they are available from the corresponding author (SH) on a reasonable request.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.
Article PubMed PubMed Central Google Scholar
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727–33.
Liu Y-C, Kuo R-L, Shih S-R. COVID-19: the first documented coronavirus pandemic in history. Biomed J. 2020;43:328–33.
Advice for the public on COVID-19 – World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public . Accessed 13 Nov 2022.
Osterrieder A, Cuman G, Pan-Ngum W, Cheah PK, Cheah P-K, Peerawaranun P, et al. Economic and social impacts of COVID-19 and public health measures: results from an anonymous online survey in Thailand, Malaysia, the UK, Italy and Slovenia. BMJ Open. 2021;11:e046863.
Article PubMed Google Scholar
Mofijur M, Fattah IMR, Alam MA, Islam ABMS, Ong HC, Rahman SMA, et al. Impact of COVID-19 on the social, economic, environmental and energy domains: Lessons learnt from a global pandemic. Sustainable Prod Consum. 2021;26:343–59.
Article Google Scholar
Vlachos J, Hertegård E, Svaleryd B. The effects of school closures on SARS-CoV-2 among parents and teachers. Proc Natl Acad Sci U S A. 2021;118:e2020834118.
Ludvigsson JF, Engerström L, Nordenhäll C, Larsson E, Open Schools. Covid-19, and child and teacher morbidity in Sweden. N Engl J Med. 2021;384:669–71.
Miralles O, Sanchez-Rodriguez D, Marco E, Annweiler C, Baztan A, Betancor É, et al. Unmet needs, health policies, and actions during the COVID-19 pandemic: a report from six european countries. Eur Geriatr Med. 2021;12:193–204.
Onyeaka H, Anumudu CK, Al-Sharify ZT, Egele-Godswill E, Mbaegbu P. COVID-19 pandemic: a review of the global lockdown and its far-reaching effects. Sci Prog. 2021;104:368504211019854.
The Lancet null. India under COVID-19 lockdown. Lancet. 2020;395:1315.
Lo Coco G, Gentile A, Bosnar K, Milovanović I, Bianco A, Drid P, et al. A cross-country examination on the fear of COVID-19 and the sense of loneliness during the First Wave of COVID-19 outbreak. Int J Environ Res Public Health. 2021;18:2586.
COVID-19 pandemic. triggers 25% increase in prevalence of anxiety and depression worldwide. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide . Accessed 14 Nov 2022.
Bueno-Notivol J, Gracia-García P, Olaya B, Lasheras I, López-Antón R, Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int J Clin Health Psychol. 2021;21:100196.
Hajek A, Sabat I, Neumann-Böhme S, Schreyögg J, Barros PP, Stargardt T, et al. Prevalence and determinants of probable depression and anxiety during the COVID-19 pandemic in seven countries: longitudinal evidence from the european COvid Survey (ECOS). J Affect Disord. 2022;299:517–24.
Piumatti G, Levati S, Amati R, Crivelli L, Albanese E. Trajectories of depression, anxiety and stress among adults during the COVID-19 pandemic in Southern Switzerland: the Corona Immunitas Ticino cohort study. Public Health. 2022;206:63–9.
Korkmaz H, Güloğlu B. The role of uncertainty tolerance and meaning in life on depression and anxiety throughout Covid-19 pandemic. Pers Indiv Differ. 2021;179:110952.
McIntyre RS, Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020;290:113104.
Funkhouser CJ, Klemballa DM, Shankman SA. Using what we know about threat reactivity models to understand mental health during the COVID-19 pandemic. Behav Res Ther. 2022;153:104082.
Landi G, Pakenham KI, Crocetti E, Tossani E, Grandi S. The trajectories of anxiety and depression during the COVID-19 pandemic and the protective role of psychological flexibility: a four-wave longitudinal study. J Affect Disord. 2022;307:69–78.
Holt-Gosselin B, Tozzi L, Ramirez CA, Gotlib IH, Williams LM. Coping strategies, neural structure, and depression and anxiety during the COVID-19 pandemic: a longitudinal study in a naturalistic sample spanning clinical diagnoses and subclinical symptoms. Biol Psychiatry Global Open Sci. 2021;1:261–71.
McCracken LM, Badinlou F, Buhrman M, Brocki KC. The role of psychological flexibility in the context of COVID-19: Associations with depression, anxiety, and insomnia. J Context Behav Sci. 2021;19:28–35.
Talkovsky AM, Norton PJ. Negative affect and intolerance of uncertainty as potential mediators of change in comorbid depression in transdiagnostic CBT for anxiety. J Affect Disord. 2018;236:259–65.
Milman E, Lee SA, Neimeyer RA, Mathis AA, Jobe MC. Modeling pandemic depression and anxiety: the mediational role of core beliefs and meaning making. J Affect Disorders Rep. 2020;2:100023.
Sagan A, Bryndova L, Kowalska-Bobko I, Smatana M, Spranger A, Szerencses V, et al. A reversal of fortune: comparison of health system responses to COVID-19 in the Visegrad group during the early phases of the pandemic. Health Policy. 2022;126:446–55.
Holt E. COVID-19 testing in Slovakia. Lancet Infect Dis. 2021;21:32.
Stalmachova K, Strenitzerova M. Impact of the COVID-19 pandemic on employment in transport and telecommunications sectors. Transp Res Procedia. 2021;55:87–94.
Izakova L, Breznoscakova D, Jandova K, Valkucakova V, Bezakova G, Suvada J. What mental health experts in Slovakia are learning from COVID-19 pandemic? Indian J Psychiatry. 2020;62(Suppl 3):459–66.
Rabinčák M, Tkáčová Ľ, VYUŽÍVANIE PSYCHOMETRICKÝCH KONŠTRUKTOV PRE, HODNOTENIE PORÚCH NÁLADY V OŠETROVATEĽSKEJ PRAXI. Zdravotnícke Listy. 2019;7:7.
Google Scholar
Sekot M, Gürlich R, Maruna P, Páv M, Uhlíková P. Hodnocení úzkosti a deprese u pacientů se zhoubnými nádory trávicího traktu. Čes a slov Psychiat. 2005;101:252–7.
Lipsitch M, Krammer F, Regev-Yochay G, Lustig Y, Balicer RD. SARS-CoV-2 breakthrough infections in vaccinated individuals: measurement, causes and impact. Nat Rev Immunol. 2022;22:57–65.
Accorsi EK, Britton A, Fleming-Dutra KE, Smith ZR, Shang N, Derado G, et al. Association between 3 doses of mRNA COVID-19 vaccine and symptomatic infection caused by the SARS-CoV-2 Omicron and Delta Variants. JAMA. 2022;327:639–51.
Barda N, Dagan N, Cohen C, Hernán MA, Lipsitch M, Kohane IS, et al. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: an observational study. Lancet. 2021;398:2093–100.
Magen O, Waxman JG, Makov-Assif M, Vered R, Dicker D, Hernán MA, et al. Fourth dose of BNT162b2 mRNA Covid-19 vaccine in a nationwide setting. N Engl J Med. 2022;386:1603–14.
Dubé JP, Smith MM, Sherry SB, Hewitt PL, Stewart SH. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021;301:113998.
Kok AAL, Pan K-Y, Rius-Ottenheim N, Jörg F, Eikelenboom M, Horsfall M, et al. Mental health and perceived impact during the first Covid-19 pandemic year: a longitudinal study in dutch case-control cohorts of persons with and without depressive, anxiety, and obsessive-compulsive disorders. J Affect Disord. 2022;305:85–93.
Aknin LB, Andretti B, Goldszmidt R, Helliwell JF, Petherick A, De Neve J-E, et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. The Lancet Public Health. 2022;7:e417–26.
Prochazka J, Scheel T, Pirozek P, Kratochvil T, Civilotti C, Bollo M, et al. Data on work-related consequences of COVID-19 pandemic for employees across Europe. Data Brief. 2020;32:106174.
Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239e3.
Zetterqvist M, Jonsson LS, Landberg Ã, Svedin CG. A potential increase in adolescent nonsuicidal self-injury during covid-19: a comparison of data from three different time points during 2011–2021. Psychiatry Res. 2021;305:114208.
Mooldijk SS, Dommershuijsen LJ, de Feijter M, Luik AI. Trajectories of depression and anxiety during the COVID-19 pandemic in a population-based sample of middle-aged and older adults. J Psychiatr Res. 2022;149:274–80.
Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107:110247.
Stephenson E, O’Neill B, Kalia S, Ji C, Crampton N, Butt DA, et al. Effects of COVID-19 pandemic on anxiety and depression in primary care: a retrospective cohort study. J Affect Disord. 2022;303:216–22.
Goldberg X, Castaño-Vinyals G, Espinosa A, Carreras A, Liutsko L, Sicuri E et al. Mental health and COVID-19 in a general population cohort in Spain (COVICAT study).Soc Psychiatry Psychiatr Epidemiol. 2022;:1–12.
Zhao Y, Yu Y, Zhao R, Cai Y, Gao S, Liu Y, et al. Association between fear of COVID-19 and hoarding behavior during the outbreak of the COVID-19 pandemic: the mediating role of mental health status. Front Psychol. 2022;13:996486.
Furstova J, Kascakova N, Sigmundova D, Zidkova R, Tavel P, Badura P. Perceived stress of adolescents during the COVID-19 lockdown: bayesian multilevel modeling of the Czech HBSC lockdown survey. Front Psychol. 2022;13:964313.
Garbóczy S, Szemán-Nagy A, Ahmad MS, Harsányi S, Ocsenás D, Rekenyi V, et al. Health anxiety, perceived stress, and coping styles in the shadow of the COVID-19. BMC Psychol. 2021;9:53.
Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors Associated with Mental Health Disorders among University students in France Confined during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2025591.
Download references
Acknowledgements
We would like to provide our appreciation and thanks to all the respondents in this study.
This research project received no external funding.
Author information
Authors and affiliations.
Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Ida Kupcova, Lubos Danisovic & Stefan Harsanyi
Institute of Histology and Embryology, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Martin Klein
You can also search for this author in PubMed Google Scholar
Contributions
IK and SH have produced the study design. All authors contributed to the manuscript writing, revising, and editing. LD and MK have done data management and extraction, SH did the data analysis. Drafting and interpretation of the manuscript were made by all authors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Stefan Harsanyi .
Ethics declarations
Ethics approval and consent to participate.
Ethical permission was obtained from the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava (Reference number: ULBGaKG-02/2022). The need for informed consent was waived by the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava due to the anonymous design of the study. This study did not process any personal data and the dataset does not contain any direct or indirect identifiers of participants. This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kupcova, I., Danisovic, L., Klein, M. et al. Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol 11 , 108 (2023). https://doi.org/10.1186/s40359-023-01130-5
Download citation
Received : 14 November 2022
Accepted : 20 March 2023
Published : 11 April 2023
DOI : https://doi.org/10.1186/s40359-023-01130-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.
Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Discussions
- Certificates
- Collab Space
- Course Details
- Announcements

कोरोनावायरस वायरसों का एक बड़ा परिवार है जो सामान्य सर्दी-जुखाम से लेकर अधिक गंभीर बीमारियों जैसे मध्य पूर्व श्वसन सिंड्रोम(MERS)और गंभीर तीव्र श्वसन सिंड्रोम(SARS)का कारण बनता है।
एक नए कोरोनावायरस(COVID19)की पहचान चीन के वुहान में 2019 में हुई थी ।यह एक नया कोरोनावायरस है जो इससे पहले कभी मनुष्यों में नहीं पाया गया है ।
इस पाठ्यक्रम में भारतीय सांकेतिक भाषा के तीन वीडियो शामिल हैं ,जो कोविड-19 का परिचय प्रदान करते हैं और दिखाते हैं कि फाब्रिक मास्क और मेडिकल मास्क(कपड़े का मास्क और चिकित्सा मास्क) कैसे सुरक्षित रूप से पहनें ।
सामग्री निर्माण के बाद आधिकारिक रूप से बीमारी का नाम स्थापित किया गया था इसलिए nCov का कोई भी उल्लेख कोविड-19 के संबंध में ही है जो हाल ही में खोजे गए कोरोनावायरस के कारण होने वाला संक्रामक रोग है ।
Coronaviruses are a large family of viruses that are known to cause illness ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS).
A novel coronavirus (COVID-19) was identified in 2019 in Wuhan, China. This is a new coronavirus that has not been previously identified in humans.
This course consists of four videos in Indian Sign Language, which provide an introduction to COVID-19 and show how to safely wear fabric and medical masks.
It also includes a new module customised for children with disabilities and particularly for the ones who fall under neurodiverse group. It covers topics such as the details on how to wear a fabric/ medical mask, the hand wash rules, ways to dispose the used mask and about the importance of maintaining appropriate physical distance when in need.
As the official disease name was established after material creation, any mention of nCoV refers to COVID-19, the infectious disease caused by the most recently discovered coronavirus.
कृपया ध्यान दें: इन सामग्रियों को 03/03/2020 को लॉन्च किया गया था।
Course information
अवलोकन : इस पाठ्यक्रम में भारतीय सांकेतिक भाषा में तीन वीडियो शामिल हैं जो कोविड-19 का परिचय प्रदान करते हैं और दिखाते हैं कि फैब्रिक मास्क और मेडिकल मास्क(कपड़े का मास्क और चिकित्सा मास्क) कैसे सुरक्षित रूप से पहनें । चार जानने के लक्ष्य:
- कोविड-19 सहित सभी उभरते श्वसन वायरस के मूलभूत सिद्धांतों का विवरण इसमें है।
- फेब्रिक मास्क और मेडिकल मास्क (कपड़े का मास्क और चिकित्सा मास्क) को सुरक्षित रूप से पहनने का तरीका बताते हैं ।
पाठ्यक्रम की अवधि: लगभग 1 घंटे
प्रमाणपत्र: पाठ्यक्रम सामग्री का 100% पूरा करनेवाले प्रतिभागियों को एक प्रमाणपत्र दिया जाएगा।
चूंकि सामग्री निर्माण के बाद आधिकारिक रूप से बीमारी का नाम स्थापित किया गया था nCov का कोई भी उल्लेख कोविड-19 को संदर्भित करता है। यह हाल ही में खोजे गए कोरोनावायरस के कारण होनेवाली संक्रामक बीमारी है ।
कोविड-19 का कैसे पता लगाते हैं, रोकथाम कैसे है,पता लगने पर क्या करना है और नियंत्रण कैसे कर पाएँगे आदि की रीतिसहित उभरते श्वसन वायरस (2020), मेडिकल मास्क (चिकित्सा मास्क) कैसे पहनें *(2020) और फैब्रिक मास्क (कपड़े का मास्क)कैसे पहनें *(2020)आदि के संबंध में परिचयात्मक वीडियो से भारतीय सांकेतिक भाषा में अनूदित।
यह अनुवाद विश्व स्वास्थ्य संगठन(WHO) द्वारा सत्यापित नहीं है। यह संसाधन केवल अध्ययन की सहायता के लिए है।
Overview: This course consists of four videos in Indian Sign Language, which provide an introduction to COVID-19 and show how to safely wear fabric and medical masks. It also includes a module customised for children with disabilities with two text resources that cover the hygiene rules and precautions to prevent the spread of COVID-19.
Learning objectives:
- Describe the fundamental principles of emerging respiratory viruses, including COVID-19.
- Describe how to safely wear fabric and medical masks.
Course duration: Approximately 1 hour.
Certificates: A certificate is available to participants who complete 100% of the course material.
Translated into Indian Sign Language from the introductory video in Emerging Respiratory Viruses, including COVID-19, methods for detection, prevention, response and control (2020), How to wear a medical mask (2020) and How to wear a fabric mask (2020). WHO is not responsible for the content or accuracy of this translation. In the event of any inconsistency between the English and Indian Sign Language translation, the original English version shall be the binding and authentic version.
This translation is not verified by WHO. This resource is intended for learning support purposes only.
Course contents
मोड्यूल 1 : कोविड-19 का परिचय / module 1: introduction to covid-19 :, मोड्यूल 2 : मेडिकल मास्क(चिकित्सा मास्क) कैसे पहनें / module 2: how to wear a medical mask:, मोड्यूल 3 : फैब्रिक मास्क(कपड़े का मास्क) कैसे पहनें / module 3: how to wear a fabric mask:, module 4: materials for children with disabilities:, enroll me for this course, certificate requirements.
- Gain a Confirmation of Participation by completing at least 100% of the course material.

IMAGES
COMMENTS
Mental health & COVID-19 in Hindi: कोरोनावायरस महामारी (Coronavirus pandemic) ने विश्व भर के ...
Mythbusters: False information about COVID-19 with facts debunking these myths. Infographics and Resources: Infographics and reliable sources for information on COVID-19. Social Media Tips: How to use social media responsibly during COVID-19. Health & Well-being: Tips to manage stress and promote Physical, Mental and Social Well-being during ...
कोरोना वायरस पर निबंध (Essay on Coronavirus in Hindi) 100 शब्दों में कोरोना वायरस जिसे आमतौर पर COVID-19 के नाम से जाना जाता है, एक संक्रामक रोग है जो मनुष्यों में श्वसन प्रणाली ...
The major mental health issues reported were stress, anxiety, depression, insomnia, denial, anger and fear. Children and older people, frontline workers, people with existing mental health illnesses were among the vulnerable in this context. COVID-19 related suicides have also been increasingly common.
Around the world, the COVID-19 pandemic has hit communities hard, with many people suffering from the virus itself, facing unemployment, or unable to interact with family and friends. As time goes on, the effects of the pandemic are not limited to just our physical health, but have impacted our mental health, as well.
Introduction. Covid-19, commonly known as the novel Coronavirus is believed to have originated from a wet market in Wuhan, China, and has spread all over the world, resulting in a large number of hospitalizations and deaths (Wang et al. 2020).As of April 18, there were approximately 23,00,000 cases reported from across the globe (Worldometers 2020). ...
Mental health under COVID-19 by region An infographic from the World Health Organization showing statistics related to the impact of COVID-19 on mental health. COVID-19 lockdowns were first used in China and later worldwide by national and state governments. Most workplaces, schools, and public places were closed.
As emotional symptoms in adolescence can become associated with many serious mental health outcomes including suicide, long-term physical health consequences, and significant healthcare burden (9-11), the effect of COVID-19 on young people's mental health could be more damaging in the longer run than the infection itself .
There is no study to date that evaluated the mental health perspectives of people during the COVID-19 pandemic. It is important to study the mental health impacts in various populations (general populations, cases of COVID-19, close contacts of COVID-19 and healthcare workers) for planning effective intervention strategies for them.
कोविड-19 विश्वमारी. यह लेख एक वर्तमान बीमारी के प्रकोप का वर्णन करता है।. इस पृष्ठ पर दी गई जानकारी शीघ्र या कालान्तर (निकट या सुदूर ...
In 2019, the COVID-19 outbreak was declared a pandemic by the World Health Organization (WHO), with 590 million confirmed cases and 6.4 million deaths worldwide as of August 2022 (ref. 1).To ...
The COVID-19 pandemic has had a severe impact on the mental health and wellbeing of people around the world while also raising concerns of increased suicidal behaviour. In addition access to mental health services has been severely impeded. However, no comprehensive summary of the current data on these impacts has until now been made widely ...
Mental Health and COVID-19: Scientific brief -1- Introduction . The COVID-19 pandemic has had a severe impact on the mental health and wellbeing of people around the world (1). While many individuals have adapted (2), others have experienced mental health problems, in some cases a consequence of COVID-19 infection (3-5)
Mental health effects of COVID-19. A number of commentators in the popular media have noted that one potential silver-lining of this pandemic has been a mainstreaming of mental health within the broader considerations of the health impact of the pandemic. It is has been noted that mental health needs have never been as central to public discourse as during recent media discussions about the ...
Español. In the first year of the COVID-19 pandemic, global prevalence of anxiety and depression increased by a massive 25%, according to a scientific brief released by the World Health Organization (WHO) today. The brief also highlights who has been most affected and summarizes the effect of the pandemic on the availability of mental health ...
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020. Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19.
It has been recognized by the world that the traditional pre-COVID-19 models and policies for children and adolescents' mental health are no longer applicable during COVID 19 era. Hence, the need is felt for the transformation of policies that can take into account not only lock down duration but also times following the lockdown.
Overview: This course consists of four videos in Indian Sign Language, which provide an introduction to COVID-19 and show how to safely wear fabric and medical masks. It also includes a module customised for children with disabilities with two text resources that cover the hygiene rules and precautions to prevent the spread of COVID-19.
Physical distancing due to the COVID‐19 outbreak can have drastic negative effects on the mental health of the elderly and disabled individuals. Physical isolation at home among family members can put the elderly and disabled person at serious mental health risk. It can cause anxiety, distress, and induce a traumatic situation for them.
Investigating the Prevalence of COVID-19-Related Sleep Disorders Among Individuals Recovering from COVID-19: A Cross-Sectional Analytical Study, Jundishapur Journal of Health Sciences, 15, 4 ...
WHO and public health authorities around the world are acting to contain the COVID-19 outbreak. However, this time of crisis is generating stress throughout the population. The considerations presented in this document have been developed by the WHO Department of Mental Health and Substance Use as a series of messages that can be used in ...
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic has led to a 28% (95% uncertainty interval (UI): 25-30) increase in major depressive disorders and a 26% (95% UI: 23-28) increase in anxiety disorders.