Best Obstetrics and Gynecology Programs
Ranked in 2023, part of Best Medical Schools
Practitioners in this field focus on women's health
Practitioners in this field focus on women's health care. Most OB-GYNs are generalists, though some have subspecialties such as reproductive endocrinology. These are the top medical programs for obstetrics and gynecology. Read the methodology »
For full rankings, MCAT scores and student debt data, sign up for the U.S. News Medical School Compass .

Here are the Best Obstetrics and Gynecology Programs
Harvard university, johns hopkins university, university of michigan--ann arbor, duke university, university of california--san francisco, new york university (grossman), university of pennsylvania (perelman), columbia university, northwestern university (feinberg).
SEE THE FULL RANKINGS
- Clear Filters

- # 1 in Obstetrics and Gynecology
- # 1 in Best Medical Schools: Research
- # 22 in Best Medical Schools: Primary Care (tie)
$66,284 (full-time) TUITION AND FEES
699 ENROLLMENT (FULL-TIME)
Its tuition is full-time: $66,284. The faculty-student ratio at Harvard University is 14.6:1. The Medical School has... Read More »
Medical school
Tuition and fees.
$66,284 (full-time)
ENROLLMENT (FULL-TIME)
Mcat total score.

Baltimore , MD
- # 2 in Obstetrics and Gynecology
- # 2 in Best Medical Schools: Research
- # 92 in Best Medical Schools: Primary Care (tie)
$59,700 (full-time) TUITION AND FEES
470 ENROLLMENT (FULL-TIME)
The School of Medicine at Johns Hopkins University has an application deadline of Oct. 15. The application fee at Johns... Read More »
$59,700 (full-time)

Ann Arbor , MI
- # 3 in Obstetrics and Gynecology
- # 13 in Best Medical Schools: Research (tie)
- # 26 in Best Medical Schools: Primary Care (tie)
$50,265 (in-state, full-time) TUITION AND FEES
$69,714 (out-of-state, full-time) TUITION AND FEES
667 ENROLLMENT (FULL-TIME)
The Medical School at University of Michigan--Ann Arbor has an application deadline of Oct. 15. The application fee at... Read More »
$50,265 (in-state, full-time)
$69,714 (out-of-state, full-time)

Durham , NC
- # 4 in Obstetrics and Gynecology (tie)
- # 5 in Best Medical Schools: Research (tie)
- # 111 in Best Medical Schools: Primary Care
$63,310 (full-time) TUITION AND FEES
507 ENROLLMENT (FULL-TIME)
The School of Medicine at Duke University has an application deadline of Oct. 15. The application fee at Duke... Read More »
$63,310 (full-time)
San Francisco , CA
- # 5 in Best Medical Schools: Primary Care
$38,073 (in-state, full-time) TUITION AND FEES
$50,318 (out-of-state, full-time) TUITION AND FEES
680 ENROLLMENT (FULL-TIME)
The School of Medicine at University of California--San Francisco has an application deadline of Oct. 15. The... Read More »
$38,073 (in-state, full-time)
$50,318 (out-of-state, full-time)

New York , NY
- # 6 in Obstetrics and Gynecology
- # 10 in Best Medical Schools: Research (tie)
- # 67 in Best Medical Schools: Primary Care (tie)
N/A TUITION AND FEES
N/A ENROLLMENT (FULL-TIME)
The faculty-student ratio at New York University (Grossman) is 2.5:1. Read More »

Philadelphia , PA
- # 7 in Obstetrics and Gynecology
- # 3 in Best Medical Schools: Research
- # 34 in Best Medical Schools: Primary Care (tie)
$61,586 (full-time) TUITION AND FEES
626 ENROLLMENT (FULL-TIME)
The Perelman School of Medicine at University of Pennsylvania (Perelman) has an application deadline of Oct. 15. The... Read More »
$61,586 (full-time)

- # 8 in Obstetrics and Gynecology (tie)
- # 4 in Best Medical Schools: Research
$66,816 (full-time) TUITION AND FEES
577 ENROLLMENT (FULL-TIME)
The College of Physicians and Surgeons at Columbia University has an application deadline of Oct. 15. The application... Read More »
$66,816 (full-time)

Chicago , IL
- # 71 in Best Medical Schools: Primary Care (tie)
$67,880 (full-time) TUITION AND FEES
632 ENROLLMENT (FULL-TIME)
The Feinberg School of Medicine at Northwestern University (Feinberg) has an application deadline of Nov. 1. The... Read More »
$67,880 (full-time)

University of California--Los Angeles (Geffen)
Los Angeles , CA
- # 10 in Obstetrics and Gynecology (tie)
- # 18 in Best Medical Schools: Research (tie)
- # 10 in Best Medical Schools: Primary Care
$40,562 (in-state, full-time) TUITION AND FEES
$52,807 (out-of-state, full-time) TUITION AND FEES
743 ENROLLMENT (FULL-TIME)
The David Geffen School of Medicine at University of California--Los Angeles (Geffen) has an application deadline of... Read More »
$40,562 (in-state, full-time)
$52,807 (out-of-state, full-time)

University of Pittsburgh
Pittsburgh , PA
- # 11 in Best Medical Schools: Primary Care (tie)
$61,194 (in-state, full-time) TUITION AND FEES
$63,576 (out-of-state, full-time) TUITION AND FEES
602 ENROLLMENT (FULL-TIME)
The School of Medicine at University of Pittsburgh has an application deadline of Oct. 15. The application fee at... Read More »
$61,194 (in-state, full-time)
$63,576 (out-of-state, full-time)

Washington University in St. Louis
St. Louis , MO
- # 82 in Best Medical Schools: Primary Care (tie)
$65,001 (full-time) TUITION AND FEES
448 ENROLLMENT (FULL-TIME)
The School of Medicine at Washington University in St. Louis has an application deadline of Nov. 30. The application... Read More »
$65,001 (full-time)
See all 31 Ranked Schools
Get the U.S. News Grad Schools School Compass and start finding the grad schools school that's right for you. You'll have access to expanded data including GMAT scores, financial aid information, graduate salary and employment statistics and more!
More Schools in this List (Alphabetical)

Emory University
Atlanta , GA
- in Obstetrics and Gynecology
- # 23 in Best Medical Schools: Research
- # 64 in Best Medical Schools: Primary Care (tie)
$53,000 (full-time) TUITION AND FEES
592 ENROLLMENT (FULL-TIME)
The School of Medicine at Emory University has an application deadline of Oct. 15. The application fee at Emory... Read More »
$53,000 (full-time)
Icahn School of Medicine at Mount Sinai
- # 98 in Best Medical Schools: Primary Care (tie)
$58,685 (full-time) TUITION AND FEES
531 ENROLLMENT (FULL-TIME)
The medical school at Icahn School of Medicine at Mount Sinai has an application deadline of Oct. 1. The application... Read More »
$58,685 (full-time)

Oregon Health and Science University
Portland , OR
- # 30 in Best Medical Schools: Research (tie)
- # 3 in Best Medical Schools: Primary Care
$46,148 (in-state, full-time) TUITION AND FEES
$70,936 (out-of-state, full-time) TUITION AND FEES
572 ENROLLMENT (FULL-TIME)
The School of Medicine at Oregon Health and Science University has an application deadline of Oct. 15. The application... Read More »
$46,148 (in-state, full-time)
$70,936 (out-of-state, full-time)

University of Alabama--Birmingham
Birmingham , AL
- # 35 in Best Medical Schools: Research (tie)
- # 24 in Best Medical Schools: Primary Care (tie)
$31,198 (in-state, full-time) TUITION AND FEES
$62,714 (out-of-state, full-time) TUITION AND FEES
806 ENROLLMENT (FULL-TIME)
The School of Medicine at University of Alabama--Birmingham has an application deadline of Nov. 1. The application fee... Read More »
$31,198 (in-state, full-time)
$62,714 (out-of-state, full-time)
Wayne State University
School of medicine, obgyn obstetrics & gynecology, phd in physiology (concentration in reproductive science).
This is an integrated Ph.D. program incorporating the teaching, research and physical resources of two departments, Physiology and Obstetrics & Gynecology, at Wayne State University's School of Medicine and offers interdisciplinary doctoral training in the Reproductive Sciences with the degree earned through the Department of Physiology. The program's integration into the Department of Obstetrics & Gynecology allows students the unique opportunity to obtain a Ph.D degree in a clinical environment. This close association of basic science and clinical medicine affords students a better comprehension of translational research opportunities directed toward ultimately benefiting reproductive medicine and health.
The curriculum represents an academic focus directed toward graduate education and research training in reproduction and development including genomics, proteomics, molecular biology and bioinformatics. Dissertation research is typically performed in basic science laboratories located at the C.S. Mott Center for Human Growth and Development under the mentorship of Ob/Gyn graduate teaching faculty.
- Mentored Faculty
- Current Grants
- Honors and Recognition
- Yale WRHR Scholars & Mentors
- Yale WRHR Advisory Committee
- Yale WRHR Application
Postdoctoral Information
- Discovery to Cure Internships
- Secondary Faculty
- YURS Biobank
INFORMATION FOR
- Residents & Fellows
- Researchers
Postdoctoral Appointments
Postdoctoral Associates/Fellows interested in conducting research in reproductive health and sciences should directly contact a Principal Investigator in the Division of Reproductive Sciences to inquire about opportunities for an appointment in the Department of Obstetrics, Gynecology & Reproductive Sciences.
Postdoctoral appointments enable recent PhD (and equivalent advanced degree) recipients to extend their education and professional training. The opportunity to carry out postdoctoral studies in a research environment such as provided at Yale University can significantly broaden an individual’s expertise, provide a period of more independent scholarship, and help define future career paths. The breadth of the academic community, together with the physical resources in the libraries and laboratories, make Yale University a particularly rich environment for postdoctoral training. In addition to deriving individual benefits, postdoctoral appointees make important contributions to the research mission of Yale University.
There are two categories of appointees: Postdoctoral Fellows and Postdoctoral Associates. The difference arises from the requirements of the funding source. Appointees funded from Yale-administered research grants, contracts, or other University sources in order to provide services related to the supported research are classified as Postdoctoral Associates; they are employees of the University even though they are considered trainees. Postdoctoral Fellows are also trainees, but they are not Yale employees. They may be funded either from training grants to the University or from funding awarded to the trainee from an outside source. Postdoctoral associates and fellows have different benefits .
All incoming postdoctoral associates and fellows must attend a Postdoctoral Orientation that will highlight the most important things you need to know as you start your postdoctoral training. This is provided by the Office of Postdoctoral Affairs . As part of your professional training at Yale, you are also required to submit an Individual Development Plan to the Office once a year. The other major organization on campus that advocates for postdoctoral scholars is the Yale Postdoctoral Association that offers regular professional development workshops, mentorship training and social events for the postdoctoral community.
Postdoctoral Orientation
Postdoctoral training.
A successful postdoctoral experience requires not only progress in your research endeavors but also the development of your career plans. Yale’s Office for Postdoctoral Affairs offers many resources, including: Career Services, Teaching, Grant Writing, Scientific Writing, Responsible Conduct of Research, the Business of Bioscience, Online Career Resources and Job Postings, Post doc Fellowship Websites.
- Education Home
- Medical Education Technology Support
- Graduate Medical Education
- Medical Scientist Training Program
- Public Health Sciences Program
- Continuing Medical Education
- Clinical Performance Education Center
- Center for Excellence in Education
- Research Home
- Biochemistry & Molecular Genetics
- Biomedical Engineering
- Cell Biology
- Microbiology, Immunology, & Cancer Biology (MIC)
- Molecular Physiology & Biological Physics
- Neuroscience
- Pharmacology
- Public Health Sciences
- Office for Research
- Clinical Research
- Clinical Trials Office
- Funding Opportunities
- Grants & Contracts
- Research Faculty Directory
- Cancer Center
- Cardiovascular Research Center
- Carter Immunology Center
- Center for Behavioral Health & Technology
- Center for Brain Immunology & Glia
- Center for Diabetes Technology
- Center for Immunity, Inflammation & Regenerative Medicine
- Center for Public Health Genomics
- Center for Membrane & Cell Physiology
- Center for Research in Reproduction
- Myles H. Thaler Center for AIDS & Human Retrovirus Research
- Child Health Research Center (Pediatrics)
- Division of Perceptual Studies
- Research News: The Making of Medicine
- Core Facilities
- Virginia Research Resources Consortium
- Center for Advanced Vision Science
- Charles O. Strickler Transplant Center
- Keck Center for Cellular Imaging
- Institute of Law, Psychiatry & Public Policy
- Translational Health Research Institute of Virginia
- Clinical Home
- Anesthesiology
- Dermatology
- Emergency Medicine
- Family Medicine
- Neurosurgery
- Obstetrics & Gynecology
- Ophthalmology
- Orthopaedic Surgery
- Otolaryngology
- Physical Medicine & Rehabilitation
- Plastic Surgery, Maxillofacial, & Oral Health
- Psychiatry & Neurobehavioral Sciences
- Radiation Oncology
- Radiology & Medical Imaging
- UVA Health: Patient Care
- Diversity Home
- Diversity Overview
- Student Resources
- GME Trainee Resources
- Faculty Resources
- Community Resources
Obstetrics and Gynecology
Our mission in the Department of Obstetrics and Gynecology at the University of Virginia is to provide excellence, innovation and superior quality in the care of patients, in the training and mentoring of health professionals, and in the creation and sharing of knowledge in patient health. Our Department has a long history of success in these areas as a result of our teamwork, collaboration and mutual support among our members.
- Patient Information
Welcome from the Chair

Paola Gehrig, MD Chair, Department of Obstetrics & Gynecology
Commitment to Excellence
The University of Virginia Medical Center has once again been recognized by Newsweek on its Best Maternity Hospitals 2023 list, receiving the highest possible rating of five ribbons. This recognition marks four years in a row that our maternity care has ranked among the best nationally. This is the result of all the hard work from our physicians, nurses, midwives and all of our team members who provide the best possible patient care.
Thank you for your interest in the Department of Obstetrics and Gynecology at the University of Virginia Health System. On behalf of the faculty, fellows, residents and staff, we welcome you.
Quality Improvement and Teamwork in Gynecologic Surgery
Meet Dr. Laura Homewood, MD, a minimally invasive gynecologic surgeon at UVA Health, and an Assistant Professor in the Department of Obstetrics and Gynecology. In this video Dr. Homewood addresses the excellent care provided at UVA Health, and the importance of teamwork. “UVA Health is at the leading edge of this quality improvement initiative in gynecologic surgery,” says Dr. Homewood. As part of her leadership efforts to improve surgical care, Dr. Homewood assembled The Gynecologic Surgical Quality Improvement Collaborative, comprising 25 sites including hospitals across the United States and Canada. According to Dr. Homewood, "In the medical research world, female health isn’t getting the same level of attention or funding dollars as men’s health. We’re trying to get better funding, better research, and higher quality data to promote women's health. This is a field that deserves more attention." To learn more about the Gynecologic Surgical Quality Improvement Collaborative, click the Learn More button below to read the UVA Health feature article: "UVA Health Leads Effort to Improve Women’s Healthcare Research & Practices."
Latest News All News »
UVA Health Named One of the Best Maternity Hospitals in the U.S.

Dr. Duska & Dr. Ring: Improve Cancer Prevention and Clinical Trial Access Across U.S.
Mother Baby Unit Has Expanded

At-Home Menopause Tests – Pros & Cons

Shark Tank Research Competition

New Guide on Menopause
Obstetrics & Gynecology

Deborah Anderson, PhD
Professor of Obstetrics/Gynecology and Virology, Immunology & Microbiology

Philip Connors
Assistant Professor of Obstetrics and Gynecology

Lillian Sosa
Assistant Program Director, Genetic Counseling Assistant Professor, Obstetrics and Gynecology Licensed Genetic Counselor

Susan White
Director, Physician Assistant Program

Virginia D. Winn, MD, PhD
Associate professor of obstetrics and gynecology (reproductive and stem cell biology).
- Print Profile
- Email Profile
Virginia D. Winn, MD, PhD, is an Associate Professor of Obstetrics and Gynecology at Stanford University, the Director of Reproductive, Stem Cell and Perinatal Biology at Stanford School of Medicine's, and the Program Director for the Women’s Reproductive Health Research (K12) at Stanford Program. Dr. Winn received both her PhD training and medical education from the University of Rochester School of Medicine and Dentistry (in 1994 and 1996 respectively.) She completed her OBGYN residency and MFM fellowship at UCSF. She received research training through the NIH-funded Reproductive Scientist Development Program (RSDP). Dr. Winn was on faculty at University of Colorado and from 2006 to 2014 leading a basic and translational NIH-funded research program. She then moved to Stanford in 2014. She is Board Certified in Obstetrics and Gynecology and Maternal and Fetal Medicine from the American Board of Obstetrics and Gynecology. As a physician scientist, Dr. Winn’s ultimate goal is to examine human placental biology and translate findings to improved clinical care resulting in healthier mothers and babies. Her lab uses a combination of molecular, cellular, tissue and translational studies in their research. Dr. Winn is a member of the Dunlevie Maternal-Fetal Medicine Center for Discovery, Innovation and Clinical Impact, the Maternal and Child Health Research Institute (MCHRI), the Stanford Cardiovascular Institute, BioX. She is a recipient the MCHRI Arline & Pete Harman Faculty Scholar award, and is currently a H&H Evergreen Scholar.
Clinical Focus
- Maternal and Fetal Medicine
Academic Appointments
- Associate Professor - University Medical Line, Obstetrics & Gynecology - Reproductive Biology
- Member, Bio-X
- Member, Cardiovascular Institute
- Member, Maternal & Child Health Research Institute (MCHRI)
Administrative Appointments
- Director of Reproductive, Stem Cell and Perinatal Biology Division, Stanford University School of Medicine (2014 - Present)
- Leadership Council, Society of Reproductive Investigation (2020 - 2023)
- Basic Science Domain Lead, Dunlevie MFM Center for Discovery, Innovation and Clinical Impact (2021 - Present)
- Research Director, NIH K12 Women's Reproductive Health Research (2020 - 2025)
- Executive Committee, Stanford Maternal and Child Health Research Institute (MCHRI) (2016 - Present)
- Evaluation Committee, Reproductive Scientist Development Program (RSDP) (2018 - Present)
Boards, Advisory Committees, Professional Organizations
- Fellow, American Board of Obstetric and Gynecology (2005 - Present)
- Member, American College of Obstetrics and Gynecology (2000 - Present)
- Full Member, Society of Maternal Fetal Medicine (2003 - Present)
- Full Member, Society of Reproductive Investigation (SRI, formerly SGI) (1997 - Present)
- Member, AIUM (2018 - Present)
- Advisory Board, AAP Perinatal Medicine (2011 - 2014)
Determining the link between preeclampsia and later cardiovascular disease using a life course approach and multi-omics.
Collaborators
- Mark Hlatky , Professor of Medicine , Stanford University
- David Stevenson , Stanford
- Gary Shaw , Professor of Pediatrics , Stanford
- Marcia Stefanick , Professor (Research) of Medicine (Stanford Prevention Research Center), of Obstetrics and Gynecology and, by courtesy, of Health Research and Policy (Epidemiology) , Stanford
- Brice Gaudilliere , Associate Professor , Stanford
- Nima Aghaeepour , Stanford
- Mark Snyder , Professor and Chair Department of Genetics , Stanford
- Seda Tierney , Stanford
Professional Education
- Board Certification: American Board of Obstetrics and Gynecology, Maternal and Fetal Medicine (2009)
- Board Certification: American Board of Obstetrics and Gynecology, Obstetrics and Gynecology (2005)
- Fellowship: UCSF (2003) CA
- Residency: UCSF (2000) CA
- Medical Education: University of Rochester School of Medicine (1996) NY
- PhD Training: University of Rochester School of Medicine (1994)
- Clinical (Primary) This is the primary clinic for this clinical provider. For additional clinical locations and information, please visit the link(s) listed below in the 'Additional Clinical Info' section. Perinatal Diagnostic Center 725 Welch Rd West Bldg Palo Alto CA 94304 Tel: (650) 725-7030 Fax: (650) 725-2878
- Stanford Health Care
- Stanford Medicine Children's Health
- Dunlevie Maternal Fetal Medicine Center
- Maternal and Child Health Research Institute
- EPOCH Study
- NatPro Study
- SUNBEAM study
Current Research and Scholarly Interests
The Winn Laboratory seeks to understand the unique biological mechanisms of human placentation. While the placenta itself is one of the key characteristics for defining mammals, the human placenta is different from most available animal models: it is one of the most invasive placentas, and results in the formation of an organ comprised of cells from both the fetus and the mother. In addition to this fascinating chimerism, fetal cells are deeply involved in the remodeling of the maternal vasculature in order to redirect large volumes of maternal blood to the placenta to support the developing fetus. As such, the investigation of this human organ covers a large array of biological processes, and deals not only with understanding its endocrine function, but the physiologic process of immune tolerance, vascular remodeling, and cellular invasion.
2023-24 Courses
- Directed Reading in Obstetrics and Gynecology OBGYN 299 (Win, Spr)
- Early Clinical Experience in Obstetrics and Gynecology OBGYN 280 (Win, Spr)
- Graduate Research in Reproductive Biology OBGYN 399 (Win, Spr)
- Honors HUMBIO 194 (Spr)
- Medical Scholars Research OBGYN 370 (Win, Spr)
- Research in Human Biology HUMBIO 193 (Aut, Win)
- Undergraduate Research in Reproductive Biology OBGYN 199 (Aut, Win, Spr)
Stanford Advisees
- Postdoctoral Faculty Sponsor Shilpi Sehgal
- Doctoral Dissertation Co-Advisor (NonAC) Kenisha Puckett
- Doctoral Dissertation Reader (NonAC) Alea Delmastro
- Postdoctoral Research Mentor Shilpi Sehgal
Graduate and Fellowship Programs
- Neonatal-Perinatal Medicine (Fellowship Program)
- Stem Cell Biology and Regenerative Medicine (Phd Program)
All Publications
Publications (72).
- All Publications (72)
- Featured Publications (18)
- Journal Articles (70)
- Conference Proceedings (2)
Publication Topics For This Person
- Amino Acid Sequence
- Antigens, CD
- Antigens, Differentiation, Myelomonocytic
- Case-Control Studies
- Cells, Cultured
- Chorionic Villi
- Cohort Studies
- Cross-Sectional Studies
- Enzyme-Linked Immunosorbent Assay
- Fibroblasts
- Gene Expression
- Gene Expression Regulation, Developmental
- Gestational Age
- Infant, Newborn
- Influenza A Virus, H1N1 Subtype
- Influenza Vaccines
- Influenza, Human
- Maternal-Fetal Exchange
- Molecular Sequence Data
- Pre-Eclampsia
- Prostaglandin-Endoperoxide Synthases
- RNA, Messenger
- Reverse Transcriptase Polymerase Chain Reaction
- Transcription, Genetic
- Trophoblasts
- Ultrasonography, Prenatal
- Young Adult
- Student/Faculty Portal
- Learning Hub (Brightspace)
- Continuous Professional Development

Obstetrics and Gynecology
Explore residency and fellowship programs in obstetrics and gynecology at Mayo Clinic School of Graduate Medical Education
About the department
Mayo Clinic has one of the largest obstetrics and gynecology practices in the world. The Department of Obstetrics and Gynecology includes more than 55 specialists who have expertise in gynecologic oncology, minimally invasive gynecologic surgery, urogynecology, reproductive endocrinology and infertility, and obstetrics and maternal fetal medicine. The Department of Obstetrics and Gynecology cares for more than 28,000 women and performs nearly 6,000 total surgeries annually across Mayo's three campuses.
adult obstetrics & gynecology hospital (U.S. News, 2023-2024)
or more women cared for annually by the Department of Obstetrics and Gynecology
total surgeries performed annually across Mayo's three campuses
About the programs
Mayo Clinic School of Graduate Medical Education offers exceptional obstetrics and gynecology (OBGYN) residencies and fellowships at Mayo Clinic's campuses in Arizona, Florida, and Minnesota.
Candidates may apply to only one program at a time. You may apply to the same program at more than one campus, if available. Learn more about our obstetrics and gynecology GME training programs:
Residency programs
Fellowship programs, explore other programs.
Mayo Clinic School of Graduate Medical Education
See full program list
Search all programs
- Skip to main content

- All countries /
- North America /
- All study levels /
- Postgraduate /
- Health and Medicine /
6 Universities in the USA offering Postgraduate Gynecology degrees and courses
More Information
Are you looking for Postgraduate courses in Gynecology? Here you can find course providers offering full-time, part-time, online or distance learning options.
You've reached your limit of 10 Favourites
Colorado State University
THE World Ranking: 401
Black Hills State University
Drexel university online.

Midwestern University - Drowners Grove Campus

Johns Hopkins University
THE World Ranking: 15

Northwestern University
THE World Ranking: 28
There are more Gynecology courses available in North America
- Colorado (inc. Denver)
- Illinois (inc. Springfield)
- Maryland (inc. Annapolis)
- Pennsylvania (inc. Harrisburg)
- South Dakota (inc. Pierre)
- Study level:
- Postgraduate
- Masters Degrees
- Doctoral Degrees
- Study mode:
- Online/Distance
Filter your results
Tell us about you.
- Nationality Select country Select country
- My current qualification is from Select country Yes No Select country Select country
- Current qualification {0} is not applicable for the study level you selected below. Qualification Qualification
- Grade type (only one grade type for your qualification) Grade type Grade type
- My score (current or expected) Please select Please select Please select Please select Please select Please select
Tell us your preferences
- Subject Gynecology
- Qualification Postgraduate
- Destination USA
- Study options
- Annual tuition fees
Subject areas
Qualification, destination.
- The UConn School of Business has grown to become one of the most comprehensive business schools in the country.
- NEW: Want to study in your home country for a foreign qualification? Find out more about cross-border study!

Division of Reproductive Sciences
MISSION : Engage in innovative research that leads to impactful discoveries in all aspects of human reproduction, while fostering a team-centric, inclusive mentoring environment.
VISION : Be a leading research hub that accelerates knowledge to improve human reproductive health.
- skip to Cookie Notice
- skip to Main Navigation
- skip to Main Content
- skip to Footer
- Find a Doctor
- Find a Location
- Appointments & Referrals
- Patient Gateway
- Español
- Leadership Team
- Quality & Safety
- Equity & Inclusion
- Community Health
- Education & Training
- Centers & Departments
- Browse Treatments
- Browse Conditions A-Z
- View All Centers & Departments
- Clinical Trials
- Cancer Clinical Trials
- Cancer Center
- Digestive Healthcare Center
- Heart Center
- Mass General for Children
- Neuroscience
- Orthopaedic Surgery
- Information for Visitors
- Maps & Directions
- Parking & Shuttles
- Services & Amenities
- Accessibility
- Visiting Boston
- International Patients
- Medical Records
- Billing, Insurance & Financial Assistance
- Privacy & Security
- Patient Experience
- Explore Our Laboratories
- Industry Collaborations
- Research & Innovation News
- About the Research Institute
- Innovation Programs
- Education & Community Outreach
- Support Our Research
- Find a Researcher
- News & Events
- Ways to Give
- Patient Rights & Advocacy
- Website Terms of Use
- Apollo (Intranet)
Obstetrics & Gynecology
- Like us on Facebook
- Follow us on Twitter
- See us on LinkedIn
- Print this page
International Gynecologic Oncology Observerships
- Global OB/GYN
Contact Information
OB/GYN Global Health
Yawkey Center for Outpatient Care, Suite 9E 55 Fruit Street Boston , MA 02114
Email: [email protected]
Explore These Observerships
The Division of Gynecologic Oncology at Massachusetts General Hospital (MGH) offers two different gynecologic oncology observership programs:
Virtual International Gynecologic Oncology Observership
In-person international gynecologic oncology observership.
Under the direction of Annekathryn Goodman, MD , a specialist in the Center for Gynecologic Oncology at Massachusetts General Hospital and professor of Obstetrics, Gynecology and Reproductive Biology at Harvard Medical School, the gynecologic oncology observerships provide physicians from around the world the opportunity to expand their knowledge and deepen their expertise in caring for women with gynecologic cancers.
These programs are intended for practicing physicians with prior experience caring for women with gynecologic cancers. There is no tuition cost. Upon successful completion of the program, participants will receive a certificate of attendance.

Annekathryn Goodman, MD, MS, MPH
- Director of Strength and Serenity MGH Global Initiative to End Gender- Based Violence
- Codirector MGH Women's Global Health
- Professor Obstetrics, Gynecology, Reproductive Biology Harvard Medical School
The MGH Department of Obstetrics & Gynecology offers a three-week virtual observership in gynecologic oncology.
Program Length:
This is a three-week observership. When completing the application form, please indicate two preferred months to observe.
The curriculum for the virtual observership includes remote attendance at daily morning didactics, including:
- Tumor Boards
- Pathology Conferences
- Gynecologic Oncology Journal Club
- Palliative Care Rounds
- Obstetrics and Gynecology Grand Rounds
- Teaching Conferences
- Global Health Conferences, Journal Club Meetings and Grand Rounds
In addition, participants will engage in regular study sessions with Dr. Goodman.
At the completion of the observership, each participant is expected to develop a written research project on a topic related to gynecologic oncology.
Requirements
One three-week rotation will take place each month, with no more than one physician invited per rotation. When completing your application, please indicate your preferred month to observe.
Each applicant must be a practicing physician or physician-in-training who takes care of women with cancer, is on staff at an institution, and is fluent in English.
Please note that each applicant must be able to commit to attending all the didactic sessions listed below (Eastern Time), plus two additional hours/week of independent study.
- 7:00 - 8:00 am – Gyn Oncology Fellow Journal Club (weekly)
- 7:00 - 8:00 am – Gyn Oncology Didactics (weekly)
- 8:00 - 9:00 am – Global Health Grand Rounds (monthly)
- 9:00 - 10:00 am – Global Health Community Meeting (monthly)
- 12:00 - 1:00 pm – Global Health Journal Club (monthly)
- 7:00 - 8:00 am – Gyn Oncology Tumor Board (weekly)
- 8:00 - 9:00 am – Palliative Care Grand Rounds (weekly)
- 7:00 - 8:00 am – OB/GYN Resident Didactics (weekly)
- 8:00 - 9:00 am – OB/GYN Grand Rounds (weekly)
- 12:00 - 1:00 pm – Cancer Center Grand Rounds (weekly)
- 5:00 - 6:00 pm – Ethics Committee (monthly)
- 7:00 - 8:00 am – Independent Study (weekly)
How to Apply
To apply, please provide the following:
- Completed online application form (click “submit” at bottom of form)
- Completed gynecology oncology assessment (click “submit” at bottom of form)
- A letter of professional reference from director-level supervisor on hospital or institution letterhead. This letter should include:
- Applicant and supervisor's positions at the home institution
- That the applicant works full-time and is in good standing at the institution
- Why the applicant is an excellent candidate for this observership
- What skills and interests the applicant will bring to the observership
- How the applicant’s participation in the observership will benefit the home institution
- A copy of your curriculum vitae (CV)
- A copy of your medical diploma
- A copy of your medical license
- A 500-word essay (in English) describing your current experience in taking care of women with cancer, your personal goals for the observership, and your vision for gynecologic oncology at your home institution
Please email items 3-7 to [email protected] ; alternatively, mail to: International Gynecologic Oncology Observership Program, Massachusetts General Hospital, Yawkey 9E, 55 Fruit Street, Boston, MA 02114.
If you have any questions, please send them to [email protected] .
The MGH Department of Obstetrics & Gynecology offers a two-month in-person observership in gynecologic oncology.
Program Length This is a two-month observership, with no more than one physician invited for each rotation. There are six available rotations per year:
- January-February
- March-April
- July-August
- September-October
- November-December
The curriculum for the in-person observership includes attendance at daily didactic lectures, observation in clinics or the operating room, and work in our simulation center to hone operative skills. Please be advised that, in an observership program, visitors will not physically engage with any patients or advise on any cases; visitors will strictly be observing/shadowing our professional staff.
At the completion of the observership, each participant is expected to prepare and present to the faculty, students, residents, and fellows at MGH a lecture on a topic related to gynecologic oncology. MGH does not award medical education credits for observerships; upon successful completion of an observership program, visitors receive a certificate of attendance.
Each applicant must be a practicing clinician on staff at an institution and fluent in English. The observership program is not suitable for students or individuals seeking residency opportunities at MGH or other United States institutions. Participation in our observership program does not have any bearing on any pending or future residency or fellowship applications. The MGH observership program is not affiliated with any Harvard Medical School programs. This position is unfunded. The visiting physician is expected to find their own funding for travel and living expenses and is responsible for making housing arrangements in Boston.
Learn more about living in Boston .
Massachusetts law and the federal Patient Protection and Affordable Care Act of 2010 require that observers obtain health insurance during their time at Massachusetts General Hospital. The United States government does not provide health care; observers are responsible for purchasing private health insurance.
The following information should be submitted at least 3 months prior to your chosen rotation:
- Completed gynecology oncology assessment (click “submit” at bottom of form)
- Current copy of your curriculum vitae (CV)
- Two letters of professional reference (from director-level supervisors) on hospital/institution letterhead. These letters should include, but are not limited to, the following:
- Your position at your home institution
- That you work full time and are in good standing at your institution
- Why you are an excellent candidate for this observership
- What skills/interests you will bring to the observership
- How your participation in the observership will benefit your home institution
- A 500-word essay describing your current experience with taking care of women with cancer, your personal goals for the two months of study and training at MGH, and your vision for gynecologic oncology at your home institution.
Please note that, during the application process, you will also need to provide a copy of your visa to the United States and a copy of your government-issued ID.
#1 Research Hospital in America
Mass General is recognized as a top hospital on the U.S. News Best Hospitals Honor Roll for 2023-2024.
Department of Obstetrics & Gynecology
The Department of Obstetrics and Gynecology at Mass General has advanced the science and the quality of care for patients since 1891.
Graduate Medical Education at Mass General
Learn from residents, fellows and program leaders about the exceptional learning experiences offered at Mass General.
OB/GYN Research
The state-of-the-art research conducted in the OB/GYN Department is focused on improving obstetric and gynecologic care for women across the lifespan.
OB/GYN Innovation
OB/GYN Advances is an update for health care professionals from specialists at Massachusetts General Hospital on research and clinical advances in obstetrics and gynecology.

Obstetrics and Gynecology
Training the next generation of OB-GYN physicians and improving women's health in Indiana
The mission of the Department of Obstetrics and Gynecology at Indiana University School of Medicine is to advance the health care of women in the State of Indiana and further impact the quality of women's health care both nationally and abroad. With a steady commitment to recruiting and retaining a diverse faculty, fellow and resident population to better serve the community, the department is educating the next generation of OB-GYN physicians and improving women’s health in Indiana.
The department has a long history of outstanding education, clinical care, quality improvement, and basic, clinical and translational research. The IU School of Medicine OB-GYN teaching faculty and appointed clinical faculty at all nine campuses throughout Indiana are eager to teach and have medical students as part of their teams.
IU School of Medicine Department of Obstetrics and Gynecology
Learn about what makes our department unique. Watch more Department of Obstetrics and Gynecology videos .

Clinical Care

2022 Department Annual Report
Read about the recent successes points of pride for the Department of Obstetrics and Gynecology at Indiana University School of Medicine.
Diverse and Collaborative Work Environment
Ob-gyn residency program.
Stipends and Benefits
Residency Track in Global Health

Nicole P. Scott, MD
Assistant Professor of Clinical Obstetrics & Gynecology
Read Bio Nicole P. Scott, MD

Jeffrey F. Peipert, MD, PhD
Chair, Department of Obstetrics & Gynecology
Read Bio Jeffrey F. Peipert, MD, PhD
Online giving is simple and secure. Thank you for supporting the Department of Obstetrics and Gynecology in research and education efforts.
- Skip to main menu
- Skip to user menu


The Complete Guide To Becoming An Obstetrics and Gynaecology Doctor
- Specialty Guides
The Role Of An Obstetrician & Gynaecologist
Torn between medicine and surgery? Fascinated by the intricacies of pregnancy and the female reproductive system?
If this sounds familiar, working within obstetrics and gynaecology may be what you are looking for. This article provides an insight into obstetrics and gynaecology and a guide to becoming a consultant in the specialty.
An obstetrics and gynaecology doctor provides care to pregnant women, their unborn child and manages diseases specific to women. More precisely, gynaecology revolves around the well-being of the female reproductive system and spans paediatric problems through to later years; it includes endocrinology, female urology and pelvic malignancy.
Obstetrics is primarily concerned with healthy and fit pregnant women, but also deals with acute or chronic conditions which may complicate their pregnancy. Most consultants work within both obstetrics and gynaecology (1).
Some common procedures and interventions performed by obstetricians and gynaecologists include:
Assisted delivery using instruments including forceps or ventouse (vacuum-assisted delivery)
Caesarean sections (planned or emergency)
Surgical interventions following miscarriage
Treating abnormal bleeding or polyps
Major surgery for gynaecological cancers
Minimal access surgery (e.g. in endometriosis)
Fertility treatment (assisted reproduction)
Obstetrics and gynaecology is an incredibly diverse specialty and balances intellectual stimulation and hands-on work. Your schedule is likely to mix ward rounds, seeing both inpatients and outpatients, performing scans, working in theatre, and attending specialist clinics.
Obstetricians and gynaecologists work within a diverse multidisciplinary team consisting of midwives, neonatologists, paediatricians, oncologists, urologists, and nurses to name a few; this is particularly important in the labour ward, which is a major component of this specialty.
In an average clinic, an obstetrician and gynaecologist may see 12 patients in one session, but this may vary depending on the complexity of cases. It is also possible to work in the community which offers a significant public health aspect to your work (1).
Apart from the necessary skills employed by all doctors, aspiring obstetricians and gynaecologists should demonstrate certain qualities and traits. Sensitivity, listening skills, as well as a sense of humour are of utmost importance as consultations often involve relating to patients and their families.
Excellent team-working skills and leadership ability are vital to effectively work in this specialty. The surgical component necessitates manual dexterity. As an acute specialty, obstetrics and gynaecology can be unpredictable and busy, requiring stamina and emotional resilience (1).
The specialty has evolved tremendously over the past few decades and continues to do so; it has also become female-dominated. A vast range of new cutting-edge technologies have emerged, and many initially incurable conditions have become curable, including gynaecological cancers.
Thus, obstetrics and gynaecology offers immense research opportunities, both at a clinical and molecular level (1).
A Typical Week
There is no such thing as a typical week or day for an obstetrician or gynaecologists due to the wealth of possible duties; your schedule highly depends on whether you are working as an obstetrician, gynaecologist, or both, and whether it includes a special interest related to a specific clinical skill e.g. ultrasounds, laparoscopy, prenatal screenings, or emergency gynaecology.
Consultant roles offer flexibility so you may develop new expertise and modify your clinical practice accordingly throughout your career (1,2).
Most trainees - and an increasing number of consultants - work on a shift pattern and start the day by attending wards, seeing inpatients and new admissions, and arranging any required investigations. Other direct clinical care duties include theatre sessions, antenatal clinics, labour wards, and a special interest (1,2).
Most consultants work during daytime and are regularly on-call out-of-hours on weekdays and weekends. Obstetrics and gynaecology has a substantial predictable on-call commitment, which mainly includes gynaecology ward and labour ward rounds, as well as telephone rounds.
Those on a gynaecology on-call rota must have a minimum of two day-time inpatient operating lists per month to maintain surgical skills for emergencies that may arise on-call.
The amount of unpredictable on-call commitment and emergency call-ins, eg attending the labour ward within 30 minutes, varies but is increasing. Some time must be allocated to teaching, audits, departmental meetings, and clinical governance.
The Route To Becoming An Obstetrician & Gynaecologist
Interested undergraduate medical students can join the medical society at their university and attend conferences for an opportunity to explore the specialty and network with potential future colleagues. Undertake student-selected modules and/or electives in obstetrics and gynaecology.
You may also want to consider registering with associated societies, institutes or professional bodies such as the Royal College of Obstetrics and Gynaecology (RCOG) and the British Medical Association (BMA) (1).
During your foundation years, aim to complete a rotation in obstetrics and gynaecology. If that is not possible, contact the obstetrics and gynaecology department at your hospital and ask how you can get involved. Furthermore, familiarise yourself with the person specification for specialty training and use this as a guide to develop your skills and abilities (1,3).
After completion of your foundation programme, you do not have to complete core medical training (CMT) or equivalent, but instead commence specialty training beginning at ST1 and running through to ST7; this means you do not need to go through an ST3 application once accepted for ST1 (1). In 2019, there were 2.02 applications per place for an ST1 post (4).
You need to demonstrate enthusiasm and commitment to the specialty for the recruitment process. To be eligible for specialty training, you will need to have acquired the Advanced Life Support Certificate from the Resuscitation Council UK. By the intended date of appointment, you will also need 18 months’ or less experience in obstetrics and gynaecology (not including foundation placements).
Additionally, academic and research achievements may aid in the selection process (1,3). Be ready to move to a different location as certain hospitals – such as the Southend University Hospital in Essex – are renowned for their excellence in this specialty and would prove beneficial to your career prospects (5).
By the end of ST2, you would normally complete Part One examinations of the RCOG, and Part Two at the end of ST5 and prior to ST6 to obtain full membership (MRCOG). A higher academic qualification, eg PhD (three-to-four years) or MD (two-to-three years), is desirable but not essential for a career in obstetrics and gynaecology. At the end of training, you will be awarded the certificate of completion of training (CCT) to go on to work as a consultant (1).
Subspecialties
While many consultant obstetricians and gynaecologists develop special interests, only a small proportion work as subspecialists. These are obstetricians and gynaecologists who have undertaken additional training and are recognised to have subspecialty expertise in their field. There are four recognised subspecialties in obstetrics and gynaecology: gynaecological oncology, maternal and foetal medicine, reproductive medicine, and urogynaecology.
You can complete subspecialty training any time after passing the Part two MRCOG. Training comprises two years of clinical training and one year of research; if you already have a higher academic degree or produced a relevant publication, it may count towards the research component (3).
NHS consultant salaries are the same for all specialties but vary between Scotland (highest), England, Northern Ireland, and Wales (lowest) and increase with service (up to 19 years). In 2020 the salary bands range from £77,779 to £109,849. Salaries can be further enhanced with NHS excellence awards.
Consultant obstetricians and gynaecologists may also wish to run private practices to supplement their salary; a purely private consultant is rare in the UK. On average, they can make a profit of an additional 49% of their NHS salary by working in the private sector (6).
In 2018, private obstetricians and gynaecologists made a profit of £74,000on average; this is higher than many specialties e.g. general surgery (£72,000) or Anaesthetics (£57,000), but lower than some others, such as urology (£92,000) or oncology (£102,000) (7).
For more information on salaries within the NHS, please feel free to review The Complete Guide to NHS Pay .
If you are interested in deepening your knowledge in obstetrics and gynaecology, you may find it useful to consult relevant journals, such as the ones listed below:
Human Reproduction
BJOG: An International Journal of Obstetrics and Gynaecology
Best Practice and Research in Obstetrics and Gynaecology
Journal of Perinatology
BMC Pregnancy and Childbirth
The following societies and institutes offer a wealth of information on conferences, symposiums, careers days, awards/competitions, podcasts, and learning resources to help you stand out when applying for obstetrics and gynaecology:
RCOG: Royal College of Obstetrics and Gynaecology
BUSOG: British Undergraduate Society of Obstetrics and Gynaecology
ESGO: European Society of Gynaecology and Obstetrics
Related Job Sources With BMJ Careers
- Hospital Jobs
- Psychiatry Jobs
- Public Health Jobs
- Research Jobs
- NHS Jobs in England
- NHS Jobs in Northern Ireland
- NHS Jobs in Scotland
- NHS Jobs in Wales
Other Complete Guides By BMJ Careers
- How To Become A Clinical Scientist
- How To Become A Diabetologist or Endocrinologist
- How To Become A Gastroenterologist
- How To Become A Neurophysiologist
- How To Become An Immunologist
1. Obstetrics and Gynaecology [Internet]. Healthcareer | NHS. [cited 2020 Jun 5]. Available from: https://www.healthcareers.nhs.uk/explore-roles/doctors/roles-doctors/obstetrics-and-gynaecology
2. Model Job Plans by Specialty [Internet]. British Medical Association. [cited 2020 Jun 5]. Available from: https://www.bma.org.uk/pay-and-contracts/job-planning/job-plans-by-specialty/model-job-plans-by-specialty
3. Careers Prospectus [Internet]. Royal College of Obstetricians and Gynaecologists. [cited 2020 Jun 5]. Available from: https://www.rcog.org.uk/en/careers-training/considering-a-career-in-og/careers-prospectus/
4. Specialty Recruitment Competition Ratios [Internet]. Specialty Training | NHS. 2019. Available from: https://specialtytraining.hee.nhs.uk/Portals/1/Competition Ratios 2019_1.pdf
5. Obstetrics and gynaecology training at Southend is top in the UK [Internet]. Southend University Hospital. 2018 [cited 2020 Jun 5]. Available from: http://www.southend.nhs.uk/about-us/media-centre/1week/obstetrics-and-gynaecology-training-at-southend-is-top-in-uk/
6. Morris S, Elliott B, Ma A, McConnachie A, Rice N, Skåtun D, et al. Analysis of consultants’ NHS and private incomes in England in 2003/4. J R Soc Med [Internet]. 2008 Jul;101(7):372–80. Available from: http://journals.sagepub.com/doi/10.1258/jrsm.2008.080004
7. No Title [Internet]. Independent Practitioner Today. [cited 2020 Jun 5]. Available from: https://www.independent-practitioner-today.co.uk
Share this article
Related articles

The Complete Guide To NHS Pay For Doctors

The Complete Guide To Becoming an Aviation and Space Medicine Doctor

The Complete Guide To Becoming A Paediatrician
Latest articles, the ultimate guide to the simulated consultation assessment (sca) for gp trainees, “i didn’t want it to be a dirty secret" – how sharing a cancer and depression diagnosis taught a doctor to heal..
Advancing and Transforming Health
- See us on instagram
- See us on twitter

Residency Training Program
Our vision is to train and mentor the future local and global leaders, advancing and transforming women’s health across the lifespan.
Our Residency Mission
The mission of the Stanford ObGyn Residency Program is to train competent, compassionate and inquisitive obstetrician-gynecologists that will become leaders in clinical care, education and research in Ob/Gyn and its subspecialties.
Letter from Residency Team
Teaching Faculty
Division of gynecology & gynecologic specialties.
- Diana Atashroo, MD
- ^ Stephanie Cizek, MD
- ^ Paula Hillard, MD
- Justin Junn, MD, MBA
- Michelle Khan, MD, MPH
- Deirdre Lum, MD
- Juno Obedin-Maliver, MD
- Leah Millheiser, MD
- Kathryn Sanserino, MD
- Rachel Chan Seay, MD
- Leslee Subak, MD
- ^ Nichole Tyson, MD
- John Wachtel, MD
Complex Family Planning Specialty
- Paul Blumenthal, MD, MPH
- Kate Shaw, MD, MS - Chief and Fellowship Director
- Erica Cahill, MD - Fellowship Associate Director
- Andrea Henkel, MD
- Michele Hugin, MD
- Jade Shorter, MD, MPH
- Amy Voedisch, MD, MS
Family Planning Fellows
- Stephanie Amaya, MD
- Serena Liu, MD
Female Pelvic Medicine & Reconstructive Surgery/Urogynecology
- Bertha Chen, MD
- Eric Sokol, MD
- Lisa Rogo-Gupta, MD
- Kavita Mishra, MD
Urogyn Fellows
- Shayan Khorsandi, MD
- Clair Burton, MD
Division of Gynecologic Oncology
- Amer Karam, MD
- Jonathan Berek, MD, MMS
- Stephanie Chow, MD
- Emily Clair McClung, MD
- Oliver Dorigo, MD, PhD - Chief
- Babak Litkouhi, MD - Fellowship Director
- Malte Renz, MD, PhD
- Valerie Sugiyama, MD
- Nelson Teng, MD, PhD
- Erinn Rankin, PhD
- GynOnc Fellows
- Ashley Moon, MD
- Susan Lang, MD
- Sahana Somasegar, MD
- Elizabeth "Evie" Adams, MD
Division of Reproductive Endocrinology & Infertility
- Lusine Aghajanova, MD
- Ruben Alvero, MD - Chief
- Brindha Bavan, MD
- Ruth Lathi, MD - Fellowship Director
- Amin Milki, MD
- Steven Nakajima, MD
- Liesl Nel-Theemat, PhD, HCLD, MBA
- Anna Sokalska, MD, PhD
REI Fellows
- Brent Monseur, MD, ScM
- Mike Strug, DO, PhD
- Ed Nguyen, MD, PhD
- Esther Chung, MD
- Anu Rambhatla, MD
- Arian Khorshid, MD
Division of Maternal-Fetal Medicine and Obstetrics
- Natali Aziz, MD
- Katherine Bianco, MD
- Yair Blumenfeld, MD
- Mark Boddy, MD
- Jane Chueh, MD
- Charlotte Conturie, MD
- Maurice Druzin, MD
- * Deirdre Lyell, MD - Associate Chief
- Yasser El-Sayed, MD - Chief and Vice Chair of Ob/Gyn
- Luis Garcia, MD
- Ronald Gibbs, MD
- Tiffany Herrero, MD - Fellowship Associate Director
- Iro Igbinosa, MD
- Amy Judy, MD, MPH
- Scarlett Karakash, MD
- Stephanie Leonard, PhD
- Elliot Main, MD
- Danielle Panelli, MD
- Priya Prasad, MD
- Martha Rode, MD
- Meryl Sperling, MD
- Sanaa Suharwardy, MD
- Erica Wu, MD - Fellowship Director
MFM Fellows
- Kathleen Minor, MD
- Christina Johnson, MD
- Anne Waldrop, MD
- Hayley Miller, MD
- Nicola Perlman, MD
- Noor Joudi, MD
- Cecilia Bonaduce Leggett, MD
- Xixi Du Plummer, MD, PhD
General Obstetrics
- Sylvie Blumstein, MD
- Caroline Bowker, MD
- Laura Brodzinsky, MD
- Susan Crowe, MD
- Kay Daniels, MD
- Cynthia DeTata, MD
- Jeffrey Faig, MD
- Joanne Nino, DO
Midwifery Care
- Colleen Moreno, DNP, APRN, CNM
- Lynn Chiarello, CNM
Division of Reproductive, Stem Cell and Perinatal Biology
- Virginia D. Winn, MD, PhD
- Roger Pedersen, PhD
- Vittorio Sebastiano, PhD
^Pediatric and Adolescent Gynecology

Why Stanford?
Jaclyn Estes, MD , explains "for me it was all about the people. I wanted to train at a program where I felt supported and could build life long relationships."
View additional testimonials
Dr. Estes elaborates "almost everyone in the program showed up to the delivery of my second child (not to mention taking care of me during the pregnancy!) and they have already become some of my closest friends. I'm looking forward to continuing to build these bonds over the next 3 years."
Our cookies
We use cookies for three reasons: to give you the best experience on PGS, to make sure the PGS ads you see on other sites are relevant , and to measure website usage. Some of these cookies are necessary to help the site work properly and can’t be switched off. Cookies also support us to provide our services for free, and by click on “Accept” below, you are agreeing to our use of cookies .You can manage your preferences now or at any time.
Privacy overview
We use cookies, which are small text files placed on your computer, to allow the site to work for you, improve your user experience, to provide us with information about how our site is used, and to deliver personalised ads which help fund our work and deliver our service to you for free.
The information does not usually directly identify you, but it can give you a more personalised web experience.
You can accept all, or else manage cookies individually. However, blocking some types of cookies may affect your experience of the site and the services we are able to offer.
You can change your cookies preference at any time by visiting our Cookies Notice page. Please remember to clear your browsing data and cookies when you change your cookies preferences. This will remove all cookies previously placed on your browser.
For more detailed information about the cookies we use, or how to clear your browser cookies data see our Cookies Notice
Manage consent preferences
Strictly necessary cookies
These cookies are necessary for the website to function and cannot be switched off in our systems.
They are essential for you to browse the website and use its features.
You can set your browser to block or alert you about these cookies, but some parts of the site will not then work. We can’t identify you from these cookies.
Functional cookies
These help us personalise our sites for you by remembering your preferences and settings. They may be set by us or by third party providers, whose services we have added to our pages. If you do not allow these cookies, then these services may not function properly.
Performance cookies
These cookies allow us to count visits and see where our traffic comes from, so we can measure and improve the performance of our site. They help us to know which pages are popular and see how visitors move around the site. The cookies cannot directly identify any individual users.
If you do not allow these cookies we will not know when you have visited our site and will not be able to improve its performance for you.
Marketing cookies
These cookies may be set through our site by social media services or our advertising partners. Social media cookies enable you to share our content with your friends and networks. They can track your browser across other sites and build up a profile of your interests. If you do not allow these cookies you may not be able to see or use the content sharing tools.
Advertising cookies may be used to build a profile of your interests and show you relevant adverts on other sites. They do not store directly personal information, but work by uniquely identifying your browser and internet device. If you do not allow these cookies, you will still see ads, but they won’t be tailored to your interests.
PhD in Obstetrics and Gynaecology
University of cambridge, different course options.
- Key information
Course Summary
Tuition fees, entry requirements, similar courses at different universities, key information data source : idp connect, qualification type.
PhD/DPhil - Doctor of Philosophy
Subject areas
Obstetrics Gynecology
Course type
The Department of Obstetrics and Gynaecology has two broad areas of research activity. The first covers the use of large population databases to identify key predictive features associated with human pregnancy. Research is also focused on perinatal control of maternal and fetal smooth muscle contractility, clinical research interest in predicting pregnancy complications such as intra-uterine growth restriction, preterm labour and perinatal death.
The second major area focuses on the cellular and molecular aspects of the growth of the placenta and its interaction with the endometrium. This includes a detailed investigation of the immune dialogue occurring between the fetal and maternal compartments. Genetic and epigenetic modulation of placental function is also a key area within this field. Modern genomic methods are utilised in both human and genetically manipulated animal models.
An additional aspect of this work focuses on the development of blood vessels in all tissues but focusing on those in the endometrium and placenta, in healthy tissue and in ectopic endometrium and cancer. This interdisciplinary work involves complex teams of molecular and cellular biologists, anatomists, mathematicians, bioinformaticians, statisticians and clinician-scientists.
The aim of the PhD is to carry out a research project which contributes new knowledge to the field.
Learning Outcomes
During the course of this study, programme students will be expected to:
- read and assimilate relevant background information;
- formulate a clear and well-defined hypothesis;
- design an experimental strategy to address the hypothesis;
- acquire the necessary skills and carry out laboratory work;
- interpret experimental data appropriately and draw sound conclusions; and
- write a suitably detailed and formatted thesis.
UK fees Course fees for UK students
For this course (per year)
International fees Course fees for EU and international students
Applicants for this course should have achieved a UK 2.1 Honours Degree.
Reproductive Genetics and Fetal Medicine MSc
Ucl (university college london), mch surgery (obstetrics and gynaecology), canterbury christ church university, phd/mphil maternal and child health/midwifery, city, university of london, global maternal health msc, child health, obstetrics, and gynaecology phd, university of nottingham.

Study at Cambridge
About the university, research at cambridge.
- Undergraduate courses
- Events and open days
- Fees and finance
- Postgraduate courses
- How to apply
- Postgraduate events
- Fees and funding
- International students
- Continuing education
- Executive and professional education
- Courses in education
- How the University and Colleges work
- Term dates and calendars
- Visiting the University
- Annual reports
- Equality and diversity
- A global university
- Public engagement
- Give to Cambridge
- For Cambridge students
- For our researchers
- Business and enterprise
- Colleges & departments
- Email & phone search
- Museums & collections
- Course Directory
PhD in Obstetrics and Gynaecology
Postgraduate Study
- Why Cambridge overview
- Chat with our students
- Cambridge explained overview
- The supervision system
- Student life overview
- In and around Cambridge
- Leisure activities
- Student unions
- Music awards
- Student support overview
- Mental health and wellbeing
- Disabled students
- Accommodation
- Language tuition
- Skills training
- Support for refugees
- Courses overview
- Department directory
- Qualification types
- Funded studentships
- Part-time study
- Research degrees
- Visiting students
- Finance overview
- Fees overview
- What is my fee status?
- Part-time fees
- Application fee
- Living costs
- Funding overview
- Funding search
- How to apply for funding
- University funding overview
- Research Councils (UKRI)
- External funding and loans overview
- Funding searches
- External scholarships
- Charities and the voluntary sector
- Funding for disabled students
- Widening participation in funding
- Colleges overview
- What is a College?
- Choosing a College
- Terms of Residence
- Applying overview
- Before you apply
- Entry requirements
- Application deadlines
- How do I apply? overview
- Application fee overview
- Application fee waiver
- Life Science courses
- Terms and conditions
- Continuing students
- Disabled applicants
- Supporting documents overview
- Academic documents
- Finance documents
- Evidence of competence in English
- AI and postgraduate applications
- Terms and Conditions
- Applicant portal and self-service
- After you apply overview
- Confirmation of admission
- Student registry
- Previous criminal convictions
- Deferring an application
- Updating your personal details
- Appeals and Complaints
- Widening participation
- Postgraduate admissions fraud
- International overview
- Immigration overview
- ATAS overview
- Applying for an ATAS certificate
- Current Cambridge students
- International qualifications
- Competence in English overview
- What tests are accepted?
- International events
- International student views overview
- Akhila’s story
- Alex’s story
- Huijie’s story
- Kelsey’s story
- Nilesh’s story
- Get in touch!
- Events overview
- Upcoming events
- Postgraduate Open Days overview
- Discover Cambridge: Master’s and PhD Study webinars
- Virtual tour
- Research Internships
- How we use participant data
- Postgraduate Newsletter
Primary tabs
- Overview (active tab)
- Requirements
- How To Apply
The Department of Obstetrics and Gynaecology has two broad areas of research activity. The first covers the use of large population databases to identify key predictive features associated with human pregnancy, such as intrauterine growth restriction, preterm labour and perinatal death.
The second major area focuses on the cellular and molecular aspects of the growth of the placenta and its interaction with the endometrium. This includes a detailed investigation of the immune dialogue occurring between the fetal and maternal compartments. Genetic and epigenetic modulation of placental function is also a key area within this field. Modern genomic methods are utilised in both human and genetically manipulated animal models.
An additional aspect of this work focuses on the development of blood vessels in all tissues but focusing on those in the endometrium and placenta. This interdisciplinary work involves complex teams of molecular and cellular biologists, anatomists, mathematicians, bioinformaticians, statisticians and clinician-scientists.
The aim of the PhD is to carry out a research project which contributes new knowledge to the field.
The course introduces students to research skills and specialist knowledge. Its main aims are:
- to give students with relevant experience at first-degree level the opportunity to carry out focused research in the discipline under close supervision; and
- to give students the opportunity to acquire or develop skills and expertise relevant to their research interests.
Learning Outcomes
During the course of this study, programme students will be expected to:
- read and assimilate relevant background information;
- formulate a clear and well-defined hypothesis;
- design an experimental strategy to address the hypothesis;
- acquire the necessary skills and carry out laboratory work;
- interpret experimental data appropriately and draw sound conclusions; and
- write a suitably detailed and formatted thesis.
Applicants currently taking the MPhil in Medical Science (Obstetrics and Gynaecology) and applying to continue to a PhD will be required to pass the MPhil satisfactorily and in a timely manner.
Those who wish to progress to a PhD after completing an MPhil will be required to satisfy their potential supervisor, Head of Department and the Faculty Degree Committee that they have the skills and ability to achieve the higher degree.
The Postgraduate Virtual Open Day usually takes place at the end of October. It’s a great opportunity to ask questions to admissions staff and academics, explore the Colleges virtually, and to find out more about courses, the application process and funding opportunities. Visit the Postgraduate Open Day page for more details.
See further the Postgraduate Admissions Events pages for other events relating to Postgraduate study, including study fairs, visits and international events.
Key Information
3-4 years full-time, 4-7 years part-time, study mode : research, doctor of philosophy, department of obstetrics & gynaecology, course - related enquiries, application - related enquiries, course on department website, dates and deadlines:, lent 2024 (closed).
Some courses can close early. See the Deadlines page for guidance on when to apply.
Easter 2024 (Closed)
Michaelmas 2024 (closed), easter 2025, funding deadlines.
These deadlines apply to applications for courses starting in Michaelmas 2024, Lent 2025 and Easter 2025.
Similar Courses
- Medical Science (Obstetrics and Gynaecology) MPhil
- MD (Doctor of Medicine) MD
- Biological Sciences (Infection Biology and Molecular Immunology) by advanced study MPhil
- Medical Science (Oncology) MPhil
- Oncology PhD
Postgraduate Admissions Office
- Admissions Statistics
- Start an Application
- Applicant Self-Service
At a glance
- Bringing a family
- Current Postgraduates
- Cambridge Students' Union (SU)
University Policy and Guidelines
Privacy Policy
Information compliance
Equality and Diversity
Terms of Study
About this site
About our website
Privacy policy
© 2024 University of Cambridge
- Contact the University
- Accessibility
- Freedom of information
- Privacy policy and cookies
- Statement on Modern Slavery
- University A-Z
- Undergraduate
- Postgraduate
- Research news
- About research at Cambridge
- Spotlight on...
You are using an outdated browser. Please upgrade your browser to improve your experience.

Closing gaps in women’s health research
Walstrom Family creates endowed fund to foster next generation of women’s health leaders

There is a gender gap in medicine.
Not just when it comes to symptoms—which present differently in women than they do in men—or to the prevalence of certain diseases and conditions but also with regard to diagnosis and treatment.
According to the National Institutes of Health Office of Research on Women’s Health, women account for nearly 78% of patients with autoimmune disease and are more likely to have chronic pain. The time between symptom onset and eventual diagnosis can be much longer for women than it is for men.
To close the gap between women’s health research and other scientific disciplines, Ward and Mari Margaret Walstrom of Harbor Springs have made a $1 million gift to bolster education and research in the MSU College of Human Medicine’s Department of Obstetrics, Gynecology and Reproductive Biology.
Ward, a graduate of MSU, and Mari Margaret Walstrom, have long been engaged with MSU and its programs. But their gift stems from firsthand experience with the harm gaps in women’s health care knowledge can cause, as their daughter suffered years of undiagnosed health issues.
“Maybe this is just one little puzzle piece, to help solve the problem thousands of women across the world are experiencing: years of horrible pain with no answers or relief,” said Mari Margaret Walstrom. “We see this as a starting point to spare others from suffering...we have to start somewhere, to give women hope.”
The Walstrom Family Endowed Women’s Health Research Fund is creating an early-career training program to increase the number of scientists and clinicians pursuing a lifelong career focused on women’s health care and research.
“We are grateful for the support of Ward and Mari Margaret Walstrom, which will inspire the next generation of medical clinicians and researchers in women’s health,” said MSU President Kevin M. Guskiewicz, Ph.D. “Their gift will provide greater access to resources and opportunities and will hasten the pace of bringing health innovation to improve women’s lives.”
The program pairs medical and graduate students with research teams and will support independent research projects. Four College of Human Medicine early-career graduate students, including one third-year medical student, were recently selected and awarded the funds; each will utilize the Walstroms’ financial support to push forward current research projects, which would not have been possible otherwise.
“It is our desire to support MSU’s research in women’s health, including causes and cures for pelvic pain, and potential relationships and effects of drugs suppressing the immune system,” Ward Walstrom added.
To help further engage the West Michigan and MSU communities in critical women’s health issues and challenges, the fund will also sponsor lectureships, symposia and presentations featuring national and international leaders in women’s health research.
“One in ten women are facing inflammatory pain and other uterine challenges, and the Walstroms’ commitment provides a path of inspiration for others to make a difference at the college,” said College of Human Medicine Dean Aron Sousa. “Our shared hope is that their generosity leads to new science and new scientists who make the world better for women everywhere who are suffering.”
The Department of Obstetrics, Gynecology and Reproductive Biology was ranked number one in funding from the National Institutes of Health (NIH) in 2023, according to a recent Blue Ridge Institute for Medical Research Report.
Among 67 universities, the department has been in the top five of its peer institutions for many years and moved to the top spot last year.
One reason for the high ranking, College of Human Medicine Dean Aron Sousa said, is the college’s partnership with Henry Ford Health, whose researchers collaborate with the college’s scientists and are included as MSU faculty.
MEET THE CHANGE-MAKERS

The impact the Walstrom’s gift will have on women’s health was the topic of a recent MSU Today podcast with Professor and Chair of the Dept. of Obstetrics, Gynecology and Reproductive Health Dr. Richard Leach and two of the four inaugural Walstrom research fund recipients.
Shannon Harkins is a genetics and genome sciences Ph.D. candidate who will use the funding in her research exploring the role of a gene in endometrial cancer. She previously worked at the Dana Farber Cancer Institute and Massachusetts General Hospital and became committed to working to understand the increase in aggressive cancers and disparities in outcomes for minority populations.
Roksolana Sudyk, a future Spartan M.D., is using the funding in a research project to understand the benefits and risks in the use of acetaminophen, such as over the counter Tylenol, in treating chronic pain during pregnancy. She talks about how her career has been influence by her own experiences with chronic pain from endometriosis.
LISTEN to the full podcast
LEARN MORE about support for the College of Human Medicine by contacting Senior Director of Development Karen Weber at [email protected] or by calling (616) 234-2827.
Research, Women
Human Medicine
WHERE YOU MAKE A DIFFERENCE

Innovation Supercharged

Mott Foundation grants $25 million to MSU to expand public health initiatives in Flint
Ten Professors Given University Distinguished Honor
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
Interdisciplinary Graduate Program in Neuroscience
Banu gumusoglu, assistant professor, obstetrics and gynecology & assistant professor, psychiatry; neuroscience phd program alumna, featured in 2024 dare to discover.
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Preterm and Early-Term Birth, Heat Waves, and Our Changing Climate
- 1 Department of Environmental Health, Harvard T. H. Chan School of Public Health, Boston, Massachusetts
- 2 Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts
- 3 Department of Obstetrics & Gynecology, Massachusetts General Hospital, Boston
- 4 Division of Allergy and Inflammation, Department of Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts
- Original Investigation Preterm and Early-Term Delivery After Heat Waves Lyndsey A. Darrow, PhD; Mengjiao Huang, PhD; Joshua L. Warren, PhD; Matthew J. Strickland, PhD; Heather A. Holmes, PhD; Andrew J. Newman, PhD; Howard H. Chang, PhD JAMA Network Open
Heat waves pose an escalating threat to human health in general and the health of pregnant people and infants in particular. Darrow et al 1 used 2 large datasets—a natality database that includes 55 million recent US births and a 1-km 2 grid of historical daily temperatures—to demonstrate an association between heat waves and rates of preterm and early-term births. The authors identify important positive associations of preterm and early-term birth with hotter, longer heat waves among lower socioeconomic status subgroups, as well as among Hispanic and non-Hispanic Black mothers. While associations of extreme heat with hospitalizations, suicides, mortality, and other health outcomes among older adults and the general population are increasingly well understood, the association of extreme heat with time to conception, pregnancy loss, and general health of pregnant individuals and infants are less-often discussed. 2 , 3 Furthermore, prenatal exposure to extreme heat may also have effects across the lifespan, including early childhood development, pubertal transition, and reproductive function. The findings of Darrow et al 1 are consistent with other studies that have demonstrated positive associations between extreme heat and increased rates of stillbirths, premature births, and lower-birth-weight babies. Importantly, Darrow et al 1 address the heterogeneity of most prior studies that have varying definitions of excessive heat. Their definition of hot days that adjusted for the 97.5th percentile of the mean temperature adds a critical understanding that pregnancies in areas that are typically cool and dry will be affected as much as those that are in areas that are typically hot and humid.
This study represents an important step forward in our understanding of the perinatal risk associated with heat wave exposure and builds on a rapidly expanding literature on the association of extreme heat with pregnancy and birth outcomes. In addition to the association of heat with fetal development, heat has especially powerful effects on infants, particularly those who are born premature or early term, and can lead to disruptions in sleep, mental health, and behavioral health. In a 2020 systematic review, Bekkar et al 4 reviewed 68 studies comprising a total of more than 32 million births, finding that, of a subset of 10 studies investigating the impacts of heat, 9 identified associations between heat and adverse birth outcomes, such as preterm birth, low birth weight, and stillbirth. A review the following year identified 13 studies on links between heat exposure and congenital anomalies, principally with regard to heat exposure in the first trimester; while results included some null studies using self-recalled temperature, 10 of the studies found associations between heat exposure and congenital anomalies, including heart anomalies, neural tube defects, and facial and craniofacial abnormalities, as well as other conditions, including hypospadias. 5 Although the association of exposure to extreme heat with adverse pregnancy and fetal outcomes is increasingly clear, the immediate and lifelong effects of prematurity are typically excluded from assessments of the effects of heat from both a health and economic perspective. As the authors note, prematurity is a leading cause of mortality in the neonatal period and increases a child’s risk of respiratory disease, cognitive impairments, and behavioral challenges. By failing to include these implications of preterm and early-term births in public health assessments, we vastly underestimate the effects of heat on population health. The sample size of more than 55 million births in the study by Darrow et al 1 compares favorably with previous studies, providing validation of the outcomes they studied throughout major US metropolitan areas.
These results are part of a larger trend toward the use of large nationally representative health outcomes datasets in combination with spatially and temporally resolved information on historical exposures, such as heat, air quality, and other hazards. 6 These exposure datasets are being developed by both academic research groups and government agencies using combinations of historical weather station records, remote-sensing data, and interpolation and missing data smoothing techniques. Studies using such datasets represent a substantial step forward in terms of understanding individual environmental exposures across lengthy time spans and large geographic regions, and substantial opportunities exist to better understand the association between a variety of health outcomes and environmental hazards that are of increasing importance in the context of climate change.
Darrow et al 1 are timely in their engagement with heat, which is one of the principal physical threats that populations, particularly pregnant individuals and infants, who are especially sensitive to the effects of heat, will face because of global changes in the planet’s climate. In the US, the intensity of heat waves has increased by 24%, and the frequency of heat waves has more than doubled since the 1960s. 7 These changes are largely attributable to the effects of anthropogenic climate change; future heat waves are expected to be increasingly hazardous as global, regional, and local temperatures increase. 8
Mitigation of the intensity, frequency, and duration of heat waves, and ultimately the morbidity and mortality associated with future heat waves, depends on addressing the root causes of rising temperatures through rapid reductions in emissions of greenhouse gases around the world. Policies to limit warming on a global scale are expected to translate into less-dramatic increases in the health effects of future heat. Studies such as the one by Darrow et al, 1 which connect climate-responsive hazards with human effects that are easily understood and of wide public interest, such as preterm delivery, put a human face on the effects of climate change and can help policymakers and the public understand the scale of what is at risk and the importance of meaningful action.
Although solutions exist to address the root cause of warming and to adapt our systems and infrastructure to extreme heat, some amount of future warming and dangerous heat must be anticipated and planned for from the standpoint of national, regional, and metropolitan policy; public health surveillance and early warning; health care operations; and patient care. Understanding the scale of heat-related health harms and identifying which populations are at greatest risk through national studies that combine large datasets with high-resolution spatial and temporal exposure data provide an important path toward determining the hazards of greatest concern and the populations most in need of assistance or other forms of health protection, as well as tracking the effectiveness of policies and interventions to address these hazards and their effects.
Darrow et al 1 have provided a compelling set of results connecting heat waves with preterm and early-term delivery in the US. Their work has a variety of implications for different audiences. Physicians, nurses, and others working in direct patient care may choose to counsel pregnant patients and caregivers of infants on the risks associated with hot weather, drawing on this and other previous studies. In public health agencies, application of similar methods at local scales may provide opportunities to identify at-risk populations that can be prioritized to receive heat health protection interventions. For policymakers and members of the public, the increasingly clear connection between heat waves and harm to pregnant individuals and infants provides an important impetus to address root causes of our escalating exposure to heat waves and invest in adaptive strategies to reduce their effects at the scale of cities, neighborhoods, and individual homes. Opportunities abound for policymakers, businesses, and individuals to take action to address these distressing findings.
Published: May 24, 2024. doi:10.1001/jamanetworkopen.2024.12026
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Dresser C et al. JAMA Network Open .
Corresponding Author: Kari C. Nadeau, MD, PhD, Department of Environmental Health, Harvard T. H. Chan School of Public Health, 665 Huntington Ave, Bldg 1, Boston, MA 02115 ( [email protected] ).
Conflict of Interest Disclosures: Dr Dresser reported receiving grants from Biogen, Americares, and Climate Central outside the submitted work. Dr Nadeau reported receiving grants from the National Institute of Allergy and Infectious Diseases. the National Heart, Lung, and Blood Institute, the National Institute of Environmental Health Sciences, and Food Allergy Research & Education; being a National Scientific Committee member of the Immune Tolerance Network and a National Scientific Committee member of National Institutes of Health clinical research centers during the conduct of the study; being a cofounder of, consultant for, and holding stock options in IgGenix; holding stock options in Seed Health, ClostraBio, and Cour; being a cofounder of and holding stock options in Alladapt; serving as a consultant for Excellergy, Red Tree Ventures, and Regeneron; and being a cofounder of Latitude outside the submitted work; in addition, Dr Nadeau reported having a patent for Mixed Allergen Composition and Methods for Using the Same issued, a patent for Granulocyte-Based Methods for Detecting and Monitoring Immune System Disorders issued, and a patent for Methods and Assays for Detecting and Quantifying Pure Subpopulations of White Blood Cells in Immune System Disorders issued. No other disclosures were reported.
Additional Contributions: We thank Lindsey Burkhardt, MD, MPH, Center on the Developing Child, Harvard University, for her input on this commentary; she was not compensated for this contribution.
See More About
Dresser C , Mahalingaiah S , Nadeau KC. Preterm and Early-Term Birth, Heat Waves, and Our Changing Climate. JAMA Netw Open. 2024;7(5):e2412026. doi:10.1001/jamanetworkopen.2024.12026
Manage citations:
© 2024
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Open access
- Published: 23 May 2024
Integrating the social determinants of health into graduate medical education training: a scoping review
- Nehal Nour 1 ,
- David Onchonga 1 ,
- Siobhan Neville 1 ,
- Patrick O’Donnell 1 &
- Mohamed Elhassan Abdalla 1
BMC Medical Education volume 24 , Article number: 565 ( 2024 ) Cite this article
Metrics details
The social determinants of health (SDH) play a key role in the health of individuals, communities, and populations. Academic institutions and clinical licensing bodies increasingly recognize the need for healthcare professionals to understand the importance of considering the SDH to engage with patients and manage their care effectively. However, incorporating relevant skills, knowledge, and attitudes relating to the SDH into curricula must be more consistent. This scoping review explores the integration of the SDH into graduate medical education training programs.
A systematic search was performed of PubMed, Ovid MEDLINE, ERIC, and Scopus databases for articles published between January 2010 and March 2023. A scoping review methodology was employed, and articles related to training in medical or surgical specialties for registrars and residents were included. Pilot programs, non-SDH-related programs, and studies published in languages other than English were excluded.
The initial search produced 829 articles after removing duplicates. The total number of articles included in the review was 24. Most articles were from developed countries such as the USA (22), one from Canada, and only one from a low- and middle-income country, Kenya. The most highly represented discipline was pediatrics. Five papers explored the inclusion of SDH in internal medicine training, with the remaining articles covering family medicine, obstetrics, gynecology, or a combination of disciplines. Longitudinal programs are the most effective and frequently employed educational method regarding SDH in graduate training. Most programs utilize combined teaching methods and rely on participant surveys to evaluate their curriculum.
Applying standardized educational and evaluation strategies for SDH training programs can pose a challenge due to the diversity of the techniques reported in the literature. Exploring the most effective educational strategy in delivering these concepts and evaluating the downstream impacts on patient care, particularly in surgical and non-clinical specialties and low- and middle-income countries, can be essential in integrating and creating a sustainable healthcare force.
Peer Review reports
Introduction
The World Health Organization (WHO) defines the social determinants of health (SDH) as “the conditions in which people are born, grow, live, work, and age, that affect a wide range of health and quality of life outcomes.” These conditions are brought about by the nature in which resources, finances, and power are distributed locally, nationally, and globally and may include economic policies and systems, development agendas, social norms, social policies, and political systems [ 1 ]. SDH can have a significant impact on individual and population health. Studies have demonstrated that marginalized individuals and communities suffering discrimination have noticeably poorer health outcomes [ 2 ]..
There has been a clarion call to integrate SDH concepts for doctors seeking postgraduate training to equip future healthcare professionals with the appropriate competencies to tackle SDH-related factors at the patient and community level [ 3 , 4 , 5 ]. A critical understanding of the causes and impacts of SDH by doctors is needed to provide effective healthcare while offering adequate stewardship of limited resources and promoting health equity of the populations they serve [ 6 ]. Orienting medical training towards SDH is a significant step to equip physicians with the understanding, proficiencies, and attitudes needed to begin to address health inequalities [ 7 ].
Medical education regarding the SDH is crucial for future medical practitioners [ 8 ]. Besides potentially enhancing health outcomes for individual patients, physicians tackling these disparities will adopt the initiatives calling for changes to influence population and community health [ 9 , 10 , 11 ]. Thus, understanding social determinants of health requires a perspective shift for graduate learners, with the desired educational outcome being transformative learning [ 12 , 13 ].
Despite a growing understanding of the importance of integrating SDH into health professional curricula, the optimum approach to incorporating SDH teaching into undergraduate and graduate training curricula has yet to be clarified. A comprehensive guide for SDH teaching strategies would promote consistency in graduate training. A previous scoping review explored the inclusion of SDH in undergraduate medical curricula. The study highlighted the benefits of longitudinal curricula with community involvement in developing retainable knowledge and skills regarding SDH for medical students [ 14 ]. In 2019, a scoping review exploring the graduate curriculum interventions focused on SDH objectives concluded the insufficient physician training regarding SDH covers Canada only [ 15 ]..
This scoping review was performed to explore the extent of integration of SDH in graduate medical education curricula globally. The study objective was to explore the structure, content, training strategies, and evaluation methods used in incorporating SDH into training qualified doctors seeking higher medical training.
The scoping review was performed by searching four relevant databases – PubMed, Ovid MEDLINE, ERIC, and Scopus. The process was undertaken by standard scoping review methodology, including identifying the research question, identifying relevant studies, selecting studies, charting the data, and collating, summarizing, and reporting the results [ 16 ].
Formulation of the research question
All authors formulated the research question, guided by the WHO’s definition of social determinants of health [ 1 ]. The overall question: What has been published on the topic of the integration of SDH into graduate medical education curricula? Specifically, the research question focused on the content of the SDH teaching in the graduate medical curriculum, their presentation, teaching strategies, and program evaluation. It aimed to identify any gaps in the available literature to guide future research.
Identification of relevant studies, including the data sources and search strategy
Authors searched PubMed, Ovid MEDLINE, ERIC, and Scopus in March 2023. Individual search strategies were developed for each database, and searches were run for each database (Table 1 ). The search strategy was comprehensive to capture the diversity of the potential SDH integrated into the graduate medical education curricula. PRISMA-ScR guidelines [ 17 , 18 ] were followed, as illustrated in (Fig. 1 ). The study population consisted of medical professionals (doctors) in any discipline undertaking postgraduate training, including specialty trainees, residents, fellows, and registrars; the concept was the content of the curriculum used for teaching the SDH, with the context being graduate medical schools and training health facilities and institutes globally.
Identifying relevant studies
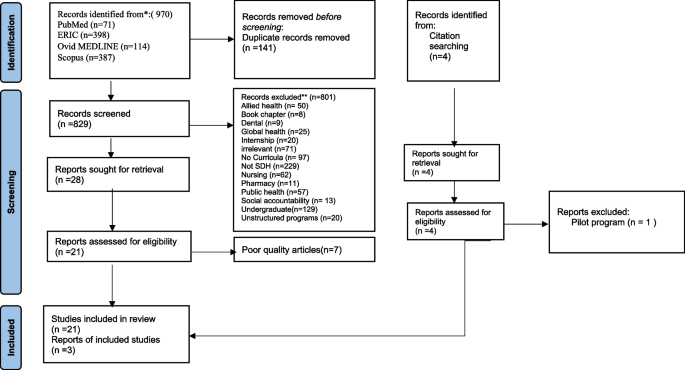
PRISMA flow diagram for the systematic scoping review of the SDH post-graduate training program
*Consider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers). **If automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: https://doi.org/10.1136/bmj.n71 . For more information, visit: (38)
Two authors (DO, NN) reviewed relevant articles after the initial removal of duplicates by exporting the references to Mendeley Reference Manager [ 19 ]; articles were analyzed using Rayyan [ 20 ], an online software that helps with a blinded screening of articles. Two authors (DO, NN) then independently screened the titles and abstracts without limiting the articles’ publication dates, population, and study locations. The remaining articles underwent full-text screening, and a third author was called to arbitrate where there were differences in screening outcomes.
Inclusion and exclusion criteria
Articles were deemed eligible for inclusion if they focused on graduate SDH curricula, including fellows, registrars, trainees, and residents. Studies had to contain structural curricula to qualify for inclusion. Articles published in English between January 2012 and March 2023 were included in the current study. If the program did not intend to integrate the SDH in graduate medical education or did not indicate a mechanism for evaluating the curriculum, they were excluded from this review. Also, the following exclusion criteria were applied: undergraduate programs, reports, systematic reviews, pilot programs, unstructured programs, programs not focusing on SDH teaching, programs not in English, internship studies, and studies that focused on allied health programs such as nursing, public health, global health, dentistry, and pharmacy.
Charting the data
The main characteristics of each graduate SDH medical curriculum were detailed, including the discipline integrating the program, the program title, length, educational methods, teaching concepts, and methods of curriculum evaluation. In this stage, data from the selected articles were extracted to a Microsoft Excel sheet, and key information about the authors and year of publication was included.
Quality assessment tool.
Two reviewers (DO, NN) performed an independent quality assessment for each article. The Medical Education Research Study Quality Instrument (MERSQI) [ 21 ] was selected for quality appraisal of the included articles. The appraisal tools assessed the articles over six domains – study design, sampling, type of data, validity of the evaluation, data synthesis, and outcome. All the included articles had a score of 9 and above, which is acceptable.
The original search yielded 970 articles. A total of 141 duplicates were removed. In the initial title and abstract screening step, 829 articles were examined. A further 801 articles were removed upon applying exclusion criteria. The exclusion criteria were: unrelated to SDH ( n = 229), associated with undergraduate curricula ( n = 129), not curriculum-based ( n = 97), irrelevant ( n = 71), nursing curricula ( n = 62), related to public health and disease prevention ( n = 57), allied health curricula ( n = 50), considered with global health and elimination of global issues ( n = 25), internship ( n = 20), unstructured programs ( n = 20), social accountability ( n = 13), pharmacy curricula ( n = 11), dentistry curricula ( n = 9) and book chapter ( n = 8).
Only 28 articles met the inclusion criteria. The next step was a full examination of the 28 articles that met the inclusion criteria and whose focus was oriented toward the contents of the SDH in graduate medical education. At this point, we removed seven articles as they did not meet the quality assessment criteria.
A total of 21 articles met the inclusion criteria and were included in the review. A hand search through the references of the included articles yielded another four studies; three were deemed eligible for inclusion, and one pilot program was excluded. The final number of articles included in the review was 24.
Summary of the graduate SDH training programs
Of the 24 programs included in the current scoping review, 22 were from graduate residency programs in the United States of America(USA), one from Canada, and one from a residency program in Kenya. Almost 50% ( n = 12) of the articles were based on pediatric graduate curricula, while nearly 21% ( n = 5) were from internal medicine programs, as indicated in Table 2 .
Structure and duration of the postgraduate SDH training
As Table 3 illustrates, of the 24 articles analyzed, the duration of the program relating to SDH varied. Twelve programs had longitudinal modules, spanning one to 3 years in the postgraduate medical residency [ 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 ], while five other programs spanned two to 9 months in the postgraduate medical residency [ 34 , 35 , 36 , 37 , 38 ]. Seven programs took between 2 weeks and 6 weeks [ 39 , 40 , 41 , 42 , 43 , 43 , 44 ], while the shortest program involved three online simulations; each simulation is 4 hours (one-half day) and completed during a module on advocacy [ 45 ].
The structure of the programs related to SDH varied across a range of thematic areas. A total of five courses had a focus on home visits and different community healthcare interventions [ 23 , 30 , 31 , 40 , 41 ], while another set of 10 programs was in the form of case-based workshops on a variety of topics such as prison healthcare, housing issues locating pharmacies and follow-up of patients after discharge [ 24 , 25 , 26 , 28 , 29 , 32 , 34 , 39 , 43 , 45 ] Lastly, nine programs focused on health advocacy topics, such as opportunities to integrate SDH at community health clinics, housing, education, and legal issues, integration of health disparities to clinical practices and equity, diversity, and inclusion [ 22 , 27 , 33 , 34 , 35 , 36 , 37 , 38 , 44 ].
Programs presentation methods
The approach to presenting the graduate SDH training and learning activities varied. All the programs used participatory learning, “where the learners are actively participating instead of being passive listeners,” as an educational strategy in combination with other teaching modalities. Eleven programs combined participatory learning with community placement and didactic teaching [ 23 , 24 , 25 , 28 , 31 , 33 , 34 , 36 , 40 , 41 , 42 ]. Another six programs relied on a participatory approach, with community placement and no formal lectures [ 27 , 35 , 36 , 43 , 44 , 45 ]. Three programs integrated didactic teaching and a participatory approach with no community engagement [ 29 , 37 , 38 ]. Another set of four programs included participatory learning only, requiring participant engagement, such as information gathering, group discussions, and activities [ 22 , 26 , 32 , 39 ].
Evaluation of the graduate SDH programs
All the reviewed programs ( n = 24) had an evaluation component in their curriculum. Six programs used pre- and post-learning evaluation surveys [ 24 , 25 , 30 , 32 , 35 , 38 ], while 11 programs used only post-learning evaluation surveys [ 22 , 27 , 28 , 31 , 36 , 37 , 39 , 40 , 41 , 44 , 45 ]. Three programs used thematic analysis of participants’ written reflections and interviews [ 26 , 34 , 44 ]. One program used both post-course interviews and participants’ reflections analysis [ 23 ]. One program combined pre and post-surveys with participants’ reflections [ 29 ]. Another program used pre-surveys and post-course reflections [ 43 ].Only one program evaluated the participants and the patient’s primary guardians’ views [ 33 ].
Five programs evaluated the participants’ affective learning, including their awareness, interest, and empathy combined with their level of knowledge regarding the SDH within the local context [ 23 , 29 , 31 , 42 , 44 ]. Another three programs used affective learning assessment solely [ 33 , 35 , 41 ]. One program adopted a comprehensive assessment on the three levels, including participants’ attitudes, knowledge, and performance [ 43 ]. Another program incorporated knowledge and performance as an evaluation tool [ 38 ], and one used the candidate’s performance as the main evaluation aspect [ 34 ]. Additionally, 13 programs only used the participants’ knowledge level as an evaluation indicator [ 22 , 24 , 25 , 26 , 27 , 28 , 30 , 32 , 37 , 39 , 40 , 41 , 45 ]..
This work details a scoping review of literature relating to incorporating the SDH in graduate medical training curricula. Notably, of a total of 24 included articles, 22 programs were implemented in the USA medical schools [ 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 45 ], with one program in Canada [ 44 ] and only one from a low- and middle-income country (Kenya) [ 22 ]. The evaluation of the programs varied on different levels; most programs performed post-learning evaluation only for the participants, and only one program added the patient’s perspective on the quality of service provided. The evaluation modules used need more clarity in reporting. The programs with extended training over the years reported a more favorable impact on the knowledge and the participant’s skills regarding SDH concepts. Participants favored training programs that blinded academic knowledge with community placement.
Paediatric training programs took the lead in training healthcare professionals in SDH. Other specialties, such as internal medicine, family medicine, and psychiatry, needed to be more proactive in integrating the SDH into their curriculum. Incorporating SDH concepts for all healthcare training is essential for weaving socially accountable healthcare into healthcare systems [ 46 ]..
Participants rated the SDH programs with a multi-year longitudinal structure highly. This finding agrees with other studies suggesting that spiral training programs improve trainees’ community integration, mentorship, confidence, knowledge in evidence-based medicine, patient-centred care, and reflective practice [ 47 , 48 , 49 , 50 ].. Our study found heterogeneity in each program’s content, as SDH factors can differ from one geographical location to another. The WHO study states that educators should apply a local context approach to tackle this issue [ 51 ]..
All the programs’ teaching strategies involved the participants in the teaching process, so-called “participatory learning.” The programs integrated academic knowledge with community placement and significantly impacted the comprehension of SDH concepts and their application in real-life situations. These findings correlate with studies emphasizing that combining theoretical learning with community engagement will enhance participants’ ability to cultivate an understanding of the core principles of the taught subject [ 52 , 53 , 54 , 55 , 56 , 57 ]..
Finally, most programs evaluated the participants’ knowledge level and confidence in recognizing SDH-related factors pre- and post, or post-program only. The reported evaluation outcomes included improved knowledge, awareness, and trust in dealing with diverse and underserved communities. Only one program interviewed the patients’ guardians and evaluated the care received by the trained physician [ 33 ]. This finding highlights a gap in program evaluation and the need to identify standardized criteria to monitor the success of SDH teaching in postgraduate curricula [ 58 ]..
Study limitations and strengths
The number of published articles demonstrating the implementation of SDH training in postgraduate programs is limited. This limitation is likely a significant under-representation of the innovation and scope of SDH integration into postgraduate curricula and again highlights the need for more high-quality literature assessing the effective incorporation, delivery, and assessment of SDH competencies. The scope of articles available in English primarily limited our study. The study focused on the programs including SDH teaching as a separate module not included with public health or global health. Our study is constrained by the unavailability of data from specific databases, which has restricted the scope of our research. Despite these limitations, our study has several strengths. Our study represents a pioneering effort in the field by conducting a comprehensive analysis of integrating SDH into graduate medical training programs. The significance of this research lies in its ability to shed light on the current state of these programs and identify critical areas for improvement. This study displays the heterogeneity of evaluation for such training programs and the deficiency in following the downstream impact of this training on patients’ health. These findings further support questions raised by medical education experts such as Sharma et al. (2018), who explained the importance of SDH teaching and the role of educators and training institutions yet criticized the focus on integration rather than evaluation [ 59 ]..
Implications for practice and future research
Our review has identified several future research implications; there needs to be more representation of the published literature about the topic in general and from low- and middle-income countries. The different expression of the SDH training programs by the developed countries’ training institutions may be because of the influence of The Accreditation Council for Graduate Medical Education (ACGME). The ACGME approves complete and independent medical education programs in the United States and Canada. The ACGME standards include addressing health equity and enhancing cultural competency through the taught curriculum of the accredited graduate program, which compels medical institutions to integrate SDH into their curricula [ 60 , 61 ]. This shows the critical influence accrediting bodies have on the content of medical curricula. As the United Nations (UN) stated in 2015, low- and middle-income countries face triple the burden of health issues and, therefore, creating a well-trained healthcare force and robust health system performance will decrease social disparities [ 62 , 63 ].
Integrating SDH into graduate medical education curricula is a dynamic and evolving area of research and practice. While the literature highlights the growing recognition of the importance of SDH education, it also reveals gaps in standardized curriculum development, assessment strategies, and long-term evaluation. Providing a multi-level structure approach for the methodology, implementation, and evaluation of SDH training programs will allow training bodies and institutions to integrate SDH concepts more effectively and produce a transparent blueprint for others to follow. Addressing these gaps will ensure that medical graduates are prepared to overcome complex SDH in healthcare.
Availability of data and materials
Data are available upon request by the corresponding author.
Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health . Accessed 16 Jan 2024.
Artiga S, Published EH. Beyond health care: the role of social determinants in promoting health and health equity. Kaiser Family Foundation; 2018. https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/ . Accessed 16 Jan 2024 .
Google Scholar
Matejic B, Vukovic D, Milicevic MS, Supic ZT, Vranes AJ, Djikanovic B, et al. Student-centerd medical education for the future physicians in the community: an experience from Serbia. HealthMED. 2012;6:517–24.
Vakani FS, Zahidie A. Teaching the social determinants of health in medical schools: challenges and strategies. J Coll Physicians Surg Pak. 2013;23:99–100.
Hudon C, Dumont-Samson O, Breton M, Bourgueil Y, Cohidon C, Falcoff H, et al. How to better integrate social determinants of health into primary healthcare: various stakeholders’ perspectives. Int J Environ Res Public Health. 2022;19.
Bell ML, Buelow JR. Teaching students to work with vulnerable populations through a patient advocacy course. Nurse Educ. 2014;39:236–40.
Article Google Scholar
Lewis JH, Lage OG, Grant BK, Rajasekaran SK, Gemeda M, Like RC, et al. Addressing the social determinants of health in undergraduate medical education curricula: a survey report. Adv Med Educ Pract. 2020;11:369–77.
Mahon KE, Henderson MK, Kirch DG. Selecting tomorrow’s physicians: the key to the future health care workforce. Acad Med. 2013;88:1806.
Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities — addressing social needs through medicare and medicaid. N Engl J Med. 2016;374:8–11.
Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;(129 Suppl 2 Suppl 2):19–31.
Gottlieb L, Colvin JD, Fleegler E, Hessler D, Garg A, Adler N. Evaluating the accountable health communities demonstration project. J Gen Intern Med. 2017;32:345–9.
Klein M, Beck AF. Social determinants of health education: a call to action. Acad Med. 2018;93:149–50.
Laven G, Newbury JW. Global health education for medical undergraduates. Rural Remote Health. 2011;11.
Nour N, Stuckler D, Ajayi O, Abdalla ME. Effectiveness of alternative approaches to integrating SDOH into medical education: a scoping review. BMC Med Educ. 2023;23.
Hunter K, Thomson B. A scoping review of social determinants of health curricula in post-graduate medical education. Can Med Educ J. 2019;10:e61–71.
Arksey H, O’malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid-Based Healthcare. 2015;13:141–6.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Mendeley Reference Manager | Mendeley. https://www.mendeley.com/reference-management/reference-manager . Accessed 16 Jan 2024.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
Cook DA, Reed DA. Appraising the quality of medical education research methods: the medical education research study quality instrument and the Newcastle-Ottawa scale-education. Acad Med. 2015;90:1067–76.
Nelligan IJ, Shabani J, Taché S, Mohamoud G, Mahoney M. An assessment of implementation of community oriented primary care in Kenyan family medicine postgraduate medical education programmes. Afr J Prim Health Care Fam Med. 2016;8:e1–4.
Goroncy A, Makaroff K, Trybula M, Regan S, Pallerla H, Goodnow K, et al. Home visits improve attitudes and self-efficacy: a longitudinal curriculum for residents. J Am Geriatr Soc. 2020;68:852–8.
Jacobs C, Seehaver A, Skiold-Hanlin S. A longitudinal underserved community curriculum for family medicine residents. Fam Med. 2019;51:48–54.
Ramadurai D, Sarcone EE, Kearns MT, Neumeier A. A case-based critical care curriculum for internal medicine residents addressing social determinants of health. MedEdPortal Publ. 2021;17:11128.
Knox KE, Lehmann W, Vogelgesang J, Simpson D. Community health, advocacy, and managing populations (CHAMP) longitudinal residency education and evaluation. J Patient-Cent Res Rev. 2018;5:45–54.
Christmas C, Dunning K, Hanyok LA, Ziegelstein RC, Rand CS, Record JD. Effects on physician practice after exposure to a patient-centered care curriculum during residency. J Grad Med Educ. 2020;12:705–9.
Morrison JM, Marsicek SM, Hopkins AM, Dudas RA, Collins KR. Using simulation to increase resident comfort discussing social determinants of health. BMC Med Educ. 2021;21:601.
Mullett TA, Rooholamini SN, Gilliam C, McPhillips H, Grow HM. Description of a novel curriculum on equity, diversity and inclusion for pediatric residents. J Natl Med Assoc. 2022;113:616–25.
Tschudy MM, Platt RE, Serwint JR. Extending the medical home into the community: a newborn home visitation program for pediatric residents. Acad Pediatr. 2013;13:443–50.
Lochner J, Lankton R, Rindfleisch K, Arndt B, Edgoose J. Transforming a family medicine residency into a community-oriented learning environment. Fam Med. 2018;50:518–25.
Lazow MA, Real FJ, Ollberding NJ, Davis D, Cruse B, Klein MD. Modernizing training on social determinants of health: a virtual neighborhood tour is noninferior to an in-person experience. Acad Pediatr. 2018;18:720–2.
Real FJ, Beck AF, Spaulding JR, Sucharew H, Klein MD. Impact of a neighborhood-based curriculum on the helpfulness of pediatric residents’ anticipatory guidance to impoverished families. Matern Child Health J. 2016;20:2261–7.
Daya S, Choi N, Harrison JD, Lai CJ. Advocacy in action: medical student reflections of an experiential curriculum. Clin Teach. 2021;18:168–73.
O’Toole JK, Burkhardt MC, Solan LG, Vaughn L, Klein MD. Resident confidence addressing social history: is it influenced by availability of social and legal resources? Clin Pediatr. 2012;51:625–31.
Gard LA, Cooper AJ, Youmans Q, Didwania A, Persell SD, Jean-Jacques M, et al. Identifying and addressing social determinants of health in outpatient practice: results of a program-wide survey of internal and family medicine residents. BMC Med Educ. 2020;20:18.
Traba C, Jain A, Pianucci K, Rosen-Valverde J, Chen S. Down to the last dollar: utilizing a virtual budgeting exercise to recognize implicit bias. MedEdPortal : J Teach Learn Resour. 2021;17:11199.
Lax Y, Braganza S, Patel M. Three-tiered advocacy: using a longitudinal curriculum to teach pediatric residents advocacy on an individual, community, and legislative level. J Med Educat Curri Develop. 2019;6:2382120519859300–2382120519859300.
Bradley J, Styren D, LaPlante A, Howe J, Craig SR, Cohen E. Healing through history: a qualitative evaluation of a social medicine consultation curriculum for internal medicine residents. BMC Med Educ. 2021;21:95.
Balighian E, Burke M, Davis A, Chinsky J, Tschudy MM, Perin J, et al. A posthospitalization home visit curriculum for pediatric patients. MedEdPortal Publ. 2020;16:10939.
Sufrin CB, Autry AM, Harris KL, Goldenson J, Steinauer JE. County jail as a novel site for obstetrics and gynecology resident education. J Grad Med Educ. 2012;4:346–50.
Real FJ, Michelson CD, Beck AF, Klein MD. Location, location, location: teaching about neighborhoods in pediatrics. Acad Pediatr. 2017;17:228–32.
Schmidt S, Higgins S, George M, Stone A, Bussey-Jone J, Dillard R. An experiential resident module for understanding social determinants of health at an academic safety-net hospital. MedEdPortal. 2017;13:10647.
Connors K, Rashid M, Chan M, Walton J, Islam B. Impact of social pediatrics rotation on residents’ understanding of social determinants of health. Med Educ Online. 2022;27.
Lazow MA, DeBlasio D, Ollberding NJ, Real FJ, Klein MD. Online simulated cases assess retention of virtual neighborhood tour curriculum. Matern Child Health J. 2019;23:1159–66.
Murray RB, Larkins S, Russell H, Ewen S, Prideaux D. Medical schools as agents of change : socially accountable medical education. Med J Aust. 2012;196:653.
Maryon-Davis A. How can we better embed the social determinants of health into postgraduate medical training? Clin Med J. 2011;11:61–3.
Bell SK, Krupat E, Fazio SB, Roberts DH, Schwartzstein RM. Longitudinal pedagogy: a successful response to the fragmentation of the third-year medical student clerkship experience. Acad Med. 2008;83:467–75.
Hoeppner MM, Olson DK, Larson SC. A longitudinal study of the impact of an emergency preparedness curriculum. Public Health Rep. 2010;125(Suppl 5 Suppl 5):24–32.
Hense H, Harst L, Küster D, Walther F, Schmitt J. Implementing longitudinal integrated curricula: systematic review of barriers and facilitators. Med Educ. 2021;55:558–73.
Committee on educating health professionals to address the social determinants of health, board on global health, institute of medicine, national academies of sciences, engineering, and medicine. A framework for educating health professionals to address the social determinants of health. Washington (DC): National Academies Press (US); 2016.
Book Google Scholar
Bélisle M, Lavoie P, Pepin J, Fernandez N, Boyer L, Lechasseur K, et al. A conceptual framework of student professionalization for health professional education and research. Int J Nurs Educ Scholarsh. 2021;18.
Hays R. Community-oriented medical education. Teach Teach Educ. 2007;23:286–93.
Lynch CD, Ash PJ, Chadwick BL, Hannigan A. Effect of community-based clinical teaching programs on student confidence: a view from the United Kingdom. J Dent Educ. 2010;74:510–6.
Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S. Commission on social determinants of health. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–9.
Nguemeni Tiako MJ, Johnson SF, Nkinsi NT, Landry A. Normalizing service learning in medical education to sustain medical student-led initiatives. Acad Med. 2021;96:1634.
Bamdas JAM, Averkiou P, Jacomino M. Service-learning programs and projects for medical students engaged with the community. Cureus. 2022;14:e26279.
Kreber C, Brook P. Impact evaluation of educational development programs. Int J Acad Dev. 2001;6:96–108.
Sharma M, Pinto AD, Kumagai AK. Teaching the social determinants of health: a path to equity or a road to nowhere? Acad Med. 2018;93:25–30.
ACGME Home. https://www.acgme.org/ . Accessed 7 Jun 2023.
New ACGME Equity Matters TM Initiative Aims to Increase Diversity, Equity, and Inclusion within Graduate Medical Education and Promote Health Equity. https://www.acgme.org/newsroom/2021/7/new-acgme-equity-matters-initiative-aims-to-increase-diversity-equity-and-inclusion-within-graduate-medical-education-and-promote-health-equity/ . Accessed 9 May 2023.
Mathers CD. History of global burden of disease assessment at the World Health Organization. Arch Public Health. 2020;78:77.
de Andrade LOM, Filho AP, Solar O, Rígoli F, de Salazar LM, Serrate PC-F, et al. Social determinants of health, universal health coverage, and sustainable development: case studies from Latin American countries. Lancet. 2015;385:1343–51.
Download references
Acknowledgements
The authors thank healthcare educators’ efforts to improve social inclusion in the healthcare section and the anonymous reviewers’ helpful comments that improved the manuscript.
No funding for this study
Author information
Authors and affiliations.
Faculty of Education & Health Services, School of Medicine, University of Limerick, Garraun, Castletroy, Co., Limerick, V94 T9PX, Ireland
Nehal Nour, David Onchonga, Siobhan Neville, Patrick O’Donnell & Mohamed Elhassan Abdalla
You can also search for this author in PubMed Google Scholar
Contributions
The author(s) read and approved the final manuscript. All authors conceived the manuscript, NN performed the search and analysis and wrote the first draft of the manuscript. SN and PO supported the manuscript’s interpretation and analysis and contributed to the writing and editing. DO contributed to the screening, second review, and data analysis. MEA supervised the research, including its conception, and contributed to revising the manuscript.
Corresponding authors
Correspondence to Nehal Nour or Siobhan Neville .
Ethics declarations
Ethical approval and consent to participate.
This research did not require ethical approval or consent for participation.
Consent to publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nour, N., Onchonga, D., Neville, S. et al. Integrating the social determinants of health into graduate medical education training: a scoping review. BMC Med Educ 24 , 565 (2024). https://doi.org/10.1186/s12909-024-05394-2
Download citation
Received : 27 June 2023
Accepted : 04 April 2024
Published : 23 May 2024
DOI : https://doi.org/10.1186/s12909-024-05394-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social determinants of health
- Graduate medical education
- Medical trainees
- Training program
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Fill out this form. Stanford Medicine's Department of Obstetrics and Gynecology research program lies at the nexus of what is current and what is possible for women's health, seeking to answer the most human of questions. Our basic scientists navigate the complexities of reproductive endocrinology, stem cell biology, and ovarian cancer.
Here are the Best Obstetrics and Gynecology Programs. Harvard University. Johns Hopkins University. University of Michigan--Ann Arbor. Duke University. University of California--San Francisco. New ...
This is an integrated Ph.D. program incorporating the teaching, research and physical resources of two departments, Physiology and Obstetrics & Gynecology, at Wayne State University's School of Medicine and offers interdisciplinary doctoral training in the Reproductive Sciences with the degree earned through the Department of Physiology.
Postdoctoral Appointments. Postdoctoral Associates/Fellows interested in conducting research in reproductive health and sciences should directly contact a Principal Investigator in the Division of Reproductive Sciences to inquire about opportunities for an appointment in the Department of Obstetrics, Gynecology & Reproductive Sciences.
25 Shattuck Street Boston, MA 02115 617-432-1000. Footer. MyHMS; Mission and Values; Privacy Policy; Digital Accessibility; Accessibility
Education and research are the foundation of our outstanding clinical care. Our mission in the Department of Obstetrics and Gynecology at NYU Langone Health is to improve the wellbeing of women through all stages of life. Our gynecologists, obstetricians, maternal-fetal medicine specialists, gynecologic oncologists, urogynecologists, and ...
Our mission in the Department of Obstetrics and Gynecology at the University of Virginia is to provide excellence, innovation and superior quality in the care of patients, in the training and mentoring of health professionals, and in the creation and sharing of knowledge in patient health. Our Department has a long history of success in these ...
Assistant Professor, Obstetrics and Gynecology Licensed Genetic Counselor. Susan White. Director, Physician Assistant Program. Related to Upcoming Thesis Deadline Boston University Chobanian & Avedisian School of Medicine: Graduate Medical Sciences 72 East Concord Street Boston, MA 02118 617-358-9518. Facebook; Twitter;
Stanford Medicine's Department of Obstetrics and Gynecology programs. The Women's Reproductive Health Research (WRHR) at Stanford Program. Funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (1K12HD103084), WRHR provides state-of-the-art, mentored, multidisciplinary research career development for outstanding junior clinician-scientists who will ...
Bio. Virginia D. Winn, MD, PhD, is an Associate Professor of Obstetrics and Gynecology at Stanford University, the Director of Reproductive, Stem Cell and Perinatal Biology at Stanford School of Medicine's, and the Program Director for the Women's Reproductive Health Research (K12) at Stanford Program. Dr.
Email the program administrator Helen Wong. Maternal-Fetal Medicine - Program Director, Erica Wu, MD. Email the program administrator Jacquie Laskey. Pediatric and Adolescent Gynecology - Program Director, Stephanie Cizek, MD. Email the program administrator Chiru Rwigi. Reproductive Endocrinology & Infertility - Program Director, Ruth Lathi, MD.
The Department of Obstetrics and Gynecology includes more than 55 specialists who have expertise in gynecologic oncology, minimally invasive gynecologic surgery, urogynecology, reproductive endocrinology and infertility, and obstetrics and maternal fetal medicine. The Department of Obstetrics and Gynecology cares for more than 28,000 women and ...
Obstetrics and Gynecology ©2021 Accreditation Council for Graduate Medical Education (AC GME) Page 3 of 59 ACGME Program Requirements for Graduate Medical Education in Obstetrics and Gynecology . Common Program Requirements (Residency) are in BOLD . Where applicable, text in italics describes the underlying philosophy of the requirements in that
Black Hills State University. USA. 115. Views. There are more Gynecology courses available in North America. VIEW ALL.
The Reproductive Sciences Division is led by Susan Murphy, PhD, Associate Professor in the Department Obstetrics and Gynecology and the Duke Nicholas School of the Environment, who was appointed Chief in December of 2017.. Dr. Murphy is an internationally recognized and highly accomplished reproductive scientist whose research has focused on the developmental origins on health and disease, in ...
This letter should include: Please email items 3-7 to [email protected]; alternatively, mail to: International Gynecologic Oncology Observership Program, Massachusetts General Hospital, Yawkey 9E, 55 Fruit Street, Boston, MA 02114. Contact Information.
The obstetrics and gynecology residency program at IU School of Medicine offers a broad spectrum of experience in a four-year program that is one of the largest residency programs in the country. Residents rotate through several hospitals and experience a diverse patient population. The OB-GYN Residency Program is an active partner with the IU Center for Global Health, which provides ...
Department: Obstetrics & Gynecology. Xuezhi Daniel Jiang, MD, PhD, is an associate professor in the Department of Obstetrics & Gynecology at Drexel University College of Medicine. * This physician's clinical practice is independent of Drexel University.
Department of Obstetrics and Gynecology. 227B Heritage Medical Research Centre. +1 (780) 492-2098. [email protected]. Sophia Ho. Graduate Program Administrator. Department of Obstetrics and Gynecology. 220 Heritage Medical Research Centre. +1 (780) 492-8560.
Available Fellowships Gynecologic Oncology Fellowship at Moffitt Cancer Center, Tampa, FL. The Accreditation Council for Graduate Medical Education (ACGME) has recently approved Moffitt Cancer Center to have an independent Gynecology Oncology Fellowship program to start academic year 2025-2026. For many years, under the accreditation of the American Board of Obstetrics and Gynecology (ABOG ...
Obstetrics and gynaecology is an incredibly diverse specialty and balances intellectual stimulation and hands-on work. Your schedule is likely to mix ward rounds, seeing both inpatients and outpatients, performing scans, working in theatre, and attending specialist clinics. Obstetricians and gynaecologists work within a diverse ...
Subak is chair of the Department of Obstetrics and Gynecology at Stanford University School of Medicine. She is also a Katharine Dexter McCormick and Stanley McCormick Memorial Professor, professor of obstetrics and gynecology and, by courtesy, of urology. Her clinical interests include female pelvic medicine, general gynecology, and LGBTQ+ health.
The Department of Obstetrics and Gynaecology has two broad areas of research activity. The first covers the use of large population databases to identify key predictive features associated with human pregnancy. Research is also focused on perinatal control of maternal and fetal smooth muscle contractility, clinical research interest in ...
PhD in Obstetrics and Gynaecology. The Department of Obstetrics and Gynaecology has two broad areas of research activity. The first covers the use of large population databases to identify key predictive features associated with human pregnancy, such as intrauterine growth restriction, preterm labour and perinatal death.
Dr. Gumusoglu, a 2020 graduate of the UI Interdisciplinary Graduate Program in Neuroscience, is currently a postdoctoral scholar in the laboratories of Mark Santillan, MD, PhD, associate professor of obstetrics and gynecology, and Donna Santillan, PhD, research associate professor of obstetrics and
Cesarean delivery rates are higher in the US than in other high-income countries. 1 Vaginal birth after cesarean (VBAC) is associated with reduced risk of maternal morbidity and future pregnancy complications vs cesarean delivery. 2 The VBAC rate increased in the US from 10.7% in 2010 to 16.2% in 2020, 3 but it is unknown whether racial, ethnic ...
LISTEN to the full podcast. LEARN MORE about support for the College of Human Medicine by contacting Senior Director of Development Karen Weber at [email protected] or by calling (616) 234-2827. To close the gap between women's health research and other scientific disciplines, Ward and Mari Margaret Walstrom have made a $1 million gift to MSU.
356 Medical Research Center Iowa City, IA 52242 (319) 335-9968 [email protected]
Heat waves pose an escalating threat to human health in general and the health of pregnant people and infants in particular. Darrow et al 1 used 2 large datasets—a natality database that includes 55 million recent US births and a 1-km 2 grid of historical daily temperatures—to demonstrate an association between heat waves and rates of preterm and early-term births.
This scoping review explores the integration of the SDH into graduate medical education training programs. A systematic search was performed of PubMed, Ovid MEDLINE, ERIC, and Scopus databases for articles published between January 2010 and March 2023. ... obstetrics, gynecology, or a combination of disciplines. Longitudinal programs are the ...