- Search Menu

Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Acquisition
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Religion
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business Strategy
- Business History
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Systems
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Politics and Law
- Politics of Development
- Public Policy
- Public Administration
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

A newer edition of this book is available.
- < Previous chapter
11 Conclusion and overview
- Published: September 2013
- Cite Icon Cite
- Permissions Icon Permissions
Substance addiction is a chronic relapsing disorder. Individuals abuse substances for different reasons. There may be personal and mitigating circumstances that lead people to substance abuse (e.g. stress or unhappiness). People may also be at increased risk of initiating substance abuse due to their age. The commencement of adolescence, for example, is a unique period of neurobiological development. Compared to children and adults, adolescents exhibit a number of psychological traits, such as risky and reward-seeking behaviour. The emergence of these traits may reflect the relatively early functional development of brain limbic affective and reward systems compared to the prefrontal cortex. As such, the period of adolescence may confer a vulnerability to the onset of drug misuse and addiction due to developmental changes in neurobiology, which seem to encourage reward-centred and risky decision-making behaviour.
Additionally, there are genetic risks for substance abuse. Twin registry and adoption studies, for example, have shown that the heritability of alcoholism may be as high as 50–60%. Whatever the cause, substance abuse and dependence confers significant social, mental, and medical impairment in those individuals afflicted, together with huge economic costs to society.
Signed in as
Institutional accounts.
- Google Scholar Indexing
- GoogleCrawler [DO NOT DELETE]
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Pathways of Addiction: Opportunities in Drug Abuse Research (1996)
Chapter: 1. introduction, 1 introduction.
Drug abuse research became a subject of sustained scientific interest by a small number of investigators in the late nineteenth and early twentieth centuries. Despite their creative efforts to understand drug abuse in terms of general advances in biomedical science, the medical literature of the early twentieth century is littered with now-discarded theories of drug dependence, such as autointoxication and antibody toxins, and with failed approaches to treatment. Eventually, escalating social concern about the use of addictive drugs and the emergence of the biobehavioral sciences during the post-World War II era led to a substantial investment in drug abuse research by the federal government (see Appendix B ). That investment has yielded substantial advances in scientific understanding about all facets of drug abuse and has also resulted in important discoveries in basic neurobiology, psychiatry, pain research, and other related fields of inquiry. In light of how little was understood about drug abuse such a short time ago, the advances of the past 25 years represent a remarkable scientific accomplishment. Yet there remains a disconnect between what is now known scientifically about drug abuse and addiction, the public's understanding of and beliefs about abuse and addiction, and the extent to which what is known is actually applied in public health settings.
During its brief history, drug abuse research has been supported mainly by the federal government, with occasional investments by major private foundations. At the federal level, the lead agency for drug abuse research is the National Institute on Drug Abuse (NIDA), which supports
85 percent of the world's research on drug abuse and addiction. Other sponsoring agencies include the National Institute of Mental Health (NIMH), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and the Substance Abuse and Mental Health Services Administration (SAMHSA), all in the Department of Health and Human Services; as well as the Office of Justice Programs (OJP) in the Department of Justice. Throughout the federal government, the FY 1995 investment in drug abuse research and development was $542.2 million, which represents 4 percent of the $13.3 billion spent by the federal government on drug abuse (ONDCP, 1996). By comparison, $8.5 billion (64 percent of the FY 1995 budget) was spent on criminal justice programs, 1 $2.7 billion (20 percent) on treatment of drug abuse, and $1.6 billion (12 percent) on prevention efforts.
In 1992, the General Accounting Office (GAO) released a report Drug Abuse Research: Federal Funding and Future Needs, which recommended that Congress review the place of research in drug control policy and its modest 4 percent share of the drug control budget. The report questioned whether the federal commitment to research was adequate, given the enormity of research needs (GAO, 1992), and whether adequate evaluation research was being conducted to determine the efficacy of various drug control programs. In FY 1995, drug abuse research was still little more than 4 percent of the entire drug control budget.
In January 1995, NIDA requested the Institute of Medicine (IOM) to examine accomplishments in drug abuse research and provide guidance for future research opportunities. This report by the IOM Committee on Opportunities in Drug Abuse Research focuses broadly on opportunities and priorities for future scientific research in drug abuse. After a brief review of major accomplishments in drug abuse research, the remainder of this chapter discusses the vocabulary and basic concepts used in the report, highlights the importance of the nation's investment in drug abuse research, and explores some of the factors that could improve the yield from that investment.
MAJOR ACHIEVEMENTS IN DRUG ABUSE RESEARCH
There have been remarkable achievements in drug abuse research over the past quarter of a century as researchers have learned more about the biological and psychosocial aspects of drug use, abuse, and dependence. Behavioral researchers have developed animal and human mod-
els of drug-seeking behavior, that have, for example, yielded objective measures of initiation and repeated administration of drugs, thereby providing the scientific foundation for assessments of "abuse liability" (i.e., the potential for abuse) of specific drugs (see Chapter 2 ). This information is an essential predicate for informed regulatory decisions under the Food, Drug and Cosmetic Act and the Controlled Substances Act. Taking advantage of technological advances in molecular biology, neuroscientists have identified receptors or receptor types in the brain for opioids, cocaine, benzodiazepines, and marijuana and have described the ways in which the brain adapts to, and changes after, exposure to drugs. Those alterations, which may persist long after the termination of drug use, appear to involve changes in gene expression. They may explain enhanced susceptibility to future drug exposure, thereby shedding light on the enigmas of withdrawal and relapse at the molecular level (see Chapter 3 ). Epidemiologists have designed and implemented epidemiological surveillance systems that enable policymakers to monitor patterns of drug use in the population ( Chapter 4 ) and that enable researchers to investigate the causes and consequences of drug use and abuse (Chapters 5 and 7 , respectively). Paralleling broader trends in health promotion and disease prevention in the past 20 years, the field of drug abuse prevention has made significant progress in evaluating the effectiveness of interventions implemented in a range of settings including communities, schools, and families (see Chapter 6 ).
Marked gains have also been made in treatment research, including improvements in diagnostic criteria; development of a wide range of treatment interventions and sophisticated methods to assess treatment outcome; and development and approval of Leo-alpha-acetylmethadol (LAAM), a medication for the treatment of opioid dependence. Pharmacological and psychosocial treatments, alone or in combination, have been shown to be effective for drug dependencies, and treatment has been shown to reduce drug use, HIV (human immunodeficiency virus) infection rates, health care costs, and criminal activity (see Chapter 8 ).
Drug abuse researchers have also made major contributions to knowledge in adjacent fields of scientific inquiry. For example, NIDA-sponsored research was the driving force in the identification of morphine-like substances that serve as neurotransmitters in specific neurons located throughout the central and peripheral nervous systems (Orson et al., 1994). Identification of these substances represents a dramatic breakthrough in understanding the mechanisms of pain, reinforcement, and stress. Additionally, the discovery of opioid peptides as neurotransmitters played a key role in the identification of numerous other peptide neurotransmitters (Cooper et al., 1991; Goldstein, 1994; Hokfelt et al., 1995). These discoveries have broadened the understanding of brain function and now
form the basis of many current strategies in the design of new drug treatments for neuropsychiatric disorders. Additionally, drug abuse research has contributed to the development of brain imaging techniques.
Drug abuse research has also provided a major impetus for neuropharmacological research in psychiatry since the late 1950s, when it was discovered that LSD (lysergic acid diethylamide; a hallucinogen that produces psychotic symptoms) affected the brain's serotonin systems (Cooper et al., 1991). That seminal discovery stimulated decades of research in the neuropharmacological basis of behavior and psychiatric disorders. The impact on antipsychotic research has been dramatic. In addition, stimulants (e.g., cocaine and amphetamine) were found to produce a state of paranoid psychosis, resembling schizophrenia, in some people. The actions of stimulants on the brain's dopamine pathways continue to inform researchers of the potential role of those pathways in the treatment, and perhaps the pathophysiology, of schizophrenia (Kahn and Davis, 1995). Drug abuse research also has had an impact on antidepressant research (e.g., the actions of drugs of abuse on the brain's serotonin systems have provided useful models with which to investigate the role of those systems in depression and mania). Depression is a risk factor for treatment failure in smoking cessation (Glassman et al., 1993) and depression-like symptoms are dominant during cocaine withdrawal (DiGregorio, 1990). Consequently, treatment of depression in nicotine and cocaine-dependent individuals has been an area of interest for drug abuse research.
Some drugs that are abused, most notably the opioid analgesics, have essential medical uses. Since its founding, NIDA has been the major supporter of research into brain mechanisms of pain and analgesia, analgesic tolerance, and analgesic pharmacology. The resulting discoveries have led to an understanding of which brain circuits are required to generate pain and pain relief (Wall and Melzack, 1994), have revolutionized the treatment of postoperative and cancer pain (Folly and Interesse, 1986; Car et al., 1992; Jacob et al., 1994), and have led to improved treatments for many other conditions that result in chronic pain (see Chapter 3 ).
VOCABULARY OF DRUG ABUSE
Ordinarily, scientific vocabulary evolves toward greater clarity and precision in response to new empirical discoveries and reconceptualizations. That creative process is evident within each of the disciplines of drug abuse research covered in various chapters of this report. Interestingly, however, the words describing the field as a whole, and connecting each chapter to the next, seem to defy the search for clarity and precision. Does "drug" include alcohol and tobacco? What is "abuse"? Are use and
abuse mutually exclusive categories? Are abuse and dependence mutually exclusive categories? Does use of illicit drugs per se amount to abuse? Does abuse include underage use of nicotine? Is addiction synonymous with dependence?
These ambiguities have persisted for decades because the vocabulary of drug abuse is inevitably influenced by peoples' attitudes and values. If the task were solely a scientific one, precise terminology would have emerged long before now. However, because the choice of words in this field always carries a nonscientific message, scientists themselves cannot always agree on a common vocabulary.
Consider the case of nicotine; from a pharmacological standpoint, nicotine is functionally similar to other psychoactive drugs. However, many researchers and policymakers choose to exclude nicotine from the category of drug. The same is true of alcohol; for example, other terms, such as ''chemical dependency" or "substance abuse," are often used as generic terms encompassing the abuse of nicotine and alcohol as well as abuse of illicit drugs. This semantic strategy is chosen to signify the difference in legal status among alcohol, nicotine, and illicit drugs. In recent years, however, a growing number of researchers have adopted a more inclusive use of the term drug. In the case of nicotine, this move tends to reflect a policy judgment that nicotine should be classified as a drug under the federal Food, Drug and Cosmetic Act.
In the committee's view, the term drug should be understood, in its generic sense, to encompass alcohol and nicotine as well as illicit drugs. It is very important for the general public to recognize that alcohol and nicotine constitute, by far, the nation's two largest drug problems, whether measured in terms of morbidity, mortality, or social cost. Abuse of and dependence on those drugs have serious individual and societal consequences. Continued separation of alcohol, nicotine, and illicit drugs in everyday speech is an impediment to public education, prevention, and therapeutic progress.
Although the committee uses the term drug, in its generic sense, to encompass alcohol and nicotine, the report focuses, at NIDA's request, on research opportunities relating to illicit drugs; research on alcohol and nicotine is discussed only when the scientific inquiries are intertwined. Because the report sometimes ranges more broadly than illicit drugs, however, the committee has adopted several semantic conventions to promote clarity and avoid redundancy. First, the term drug, unmodified, refers to all psychoactive drugs, including alcohol and nicotine. When reference is intended solely to illicit drugs such as heroin, cocaine, and other drugs regulated by the Controlled Substances Act, the committee says so explicitly. Occasionally, to ensure that the intended meaning is clear, the report refers to "illicit drugs and nicotine" or to "illicit drugs
and alcohol," as the case may be. Additionally, the words opiate and opioid are used interchangeably, although opiates are derivative of morphine and opioids are all compounds with morphine-like properties (they may be synthetic and not resemble morphine chemically).
The report employs the standard three-stage conceptualization of drug-taking behavior that applies to all psychoactive drugs, whether licit or illicit. Each stage—use, abuse, dependence—is marked by higher levels of use and increasingly serious consequences. Thus, when the report refers to the "use" of drugs, the term is usually employed in a narrow sense to distinguish it from intensified patterns of use. Conversely, the term "abuse" is used to refer to any harmful use, irrespective of whether the behavior constitutes a "disorder'' in the DSM-IV diagnostic nomenclature (see Appendix C ). When the intent is to emphasize the clinical categories of abuse and dependence, that is made clear.
The committee also draws a clear distinction between patterns of drug-taking behavior, however described, and the harmful consequences of that behavior for the individual and for society. These consequences include the direct, acute effects of drug taking such as a drug-induced toxic psychosis or impaired driving, the effects of repeated drug taking on the user's health and social functioning, and the effects of drug-seeking behavior on the individual and society. It bears emphasizing that adverse consequences can be associated with patterns of drug use that do not amount to abuse or dependence in a clinical sense, although the focus of this report and the committee's recommendations is on the more intensified patterns of use (i.e., abuse and dependence) since they cause the majority of the serious consequences.
DEFINITIONS AND BASIC CONCEPTS
Drug use may be defined as occasional use strongly influenced by environmental factors. Drug use is not a medical disorder and is not listed as such in either of the two most important diagnostic manuals—the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSMIV; APA, 1994); or the International Classification of Diseases (ICD-10; WHO, 1992). (See Appendix C for DSM-IV and ICD-10 diagnostic criteria.) Drug use implies intake for nonmedical purposes; it may or may not be accompanied by clinically significant impairment or distress on a given occasion.
Drug abuse is characterized in DSM-IV as including regular, sporadic, or intensive use of higher doses of drugs leading to social, legal, or interpersonal problems. Like DSM-IV, ICD-10 identifies a nondependent but problematic syndrome of drug use but calls it "harmful use" instead
of abuse. This syndrome is defined by ICD-10 as use resulting in actual physical or psychological harm.
Drug dependence (or addiction) is characterized in both DSM-IV and ICD-10 as drug-seeking behavior involving compulsive use of high doses of one or more drugs, either licit or illicit, for no clear medical indication, resulting in substantial impairment of health and social functioning. Dependence is usually accompanied by tolerance and withdrawal 2 and (like abuse) is generally associated with a wide range of social, legal, psychiatric, and medical problems. Unlike patients with chronic pain or persistent anxiety, who take medication over long periods of time to obtain relief from a specific medical or psychiatric disorder (often with resulting tolerance and withdrawal), persons with dependence seek out the drug and take it compulsively for nonmedical effects.
Tolerance occurs when certain medications are taken repeatedly. With opiates for example, it can be detected after only a few days of use for medical purposes such as the treatment of pain. If the patient suddenly stops taking the drug, a withdrawal syndrome may ensue. Physicians often confuse this phenomenon, referred to as physical dependence, with true addiction. That can lead to withholding adequate medication for the treatment of pain because of the very small risk that addiction with drug-seeking behavior may occur.
As a consequence of its compulsive nature involving the loss of control over drug use, dependence (or addiction) is typically a chronically relapsing disorder (IOM, 1990, 1995; Meter, 1996; O'Brien and McLennan, 1996; McLennan et al., in press). Although individuals with drug dependence can often complete detoxification and achieve temporary abstinence, they find it very difficult to sustain that condition and avoid relapse over time. Most persons who achieve sustained remission do so only after a number of cycles of detoxification and relapse (Dally and Marital, 1992). Relapse is caused by a constellation of biological, family, social, psychological, and treatment factors and is demonstrated by the fact that at least half of former cigarette smokers quit three or more times before they successfully achieve stable remission from nicotine addiction (Schilling, 1992). Similarly, within one year of treatment, relapse occurs in 30-50 percent of those treated for drug dependence, although the level
of drug use may not be as high as before treatment (Daley and Marlatt, 1992; McLellan et al., in press). Unlike those who use (or even abuse) drugs, individuals with addiction have a substantially diminished ability to control drug consumption, a factor that contributes to their tendency to relapse.
Another terminological issue arises in relation to the terms addiction and dependence. For some scientists, the proper terms for compulsive drug seeking is addiction, rather than dependence. In their view, addiction more clearly signifies the essential behavioral differences between compulsive use of drugs for their nonmedical effects and the syndrome of "physical dependence" that can develop in connection with repeated medical use. In response, many scientists argue that dependence has been defined in both ICD-10 and DSM-IV to encompass the behavioral features of the disorder and has become the generally accepted term in the diagnostic nomenclature. Moreover, some scientists object to the term addiction on the grounds that it is associated with stigmatizing social images and that a less pejorative term would help to promote public understanding of the medical nature of the condition. The committee has not attempted to resolve this controversy. For purposes of this report, the terms addiction and dependence are used interchangeably.
An inherent aspect of drug addiction is the propensity to relapse. Relapse should not be viewed as treatment failure; addiction itself should be considered a brain disease similar to other chronic and relapsing conditions such as hypertension, diabetes, and asthma (IOM, 1995; O'Brien and McLellan, 1996). In the latter, significant improvement is considered successful treatment even though complete remission or cure is not achieved. In the area of drug abuse, however, many individuals (both lay and professional) expect treatment programs to perform like vaccine programs, where one episode of treatment offers lifetime immunity. Not surprisingly, because of that expectation, people are inevitably disappointed in the relatively high relapse rates associated with most treatments. If, however, addiction is understood as a chronically relapsing brain disease, then—for any one treatment episode—evidence of treatment efficacy would include reduced consumption, longer abstention periods, reduced psychiatric symptoms, improved health, continued employment, and improved family relations. Most of those results are demonstrated regularly in treatment outcome studies.
The idea that drug addiction is a chronic relapsing condition, requiring long-term attention, has been resisted in the United States and in some other countries (Brewley, 1995). Many lay people view drug addiction as a character defect requiring punishment or incarceration. Proponents of the medical model, however, point to the fact that addiction is a distinct morbid process that has characteristics and identifiable signs and
symptoms that affect organ systems (Miller, 1991; Meter, 1996). Characterization of addiction as a brain disease is bolstered by evidence of genetic vulnerability to addiction, physical correlates of its clinical course, physiological changes as a result of repeated drug use, and fundamental changes in brain chemistry as evidenced by brain imaging (Volkow et al., 1993). This is not to say that behavioral, social, and environmental factors are immaterial—they all play a role in onset and outcome, just as they do in heart disease, kidney disease, tuberculosis, or other infectious diseases. Thus, the contemporary understanding of disease fully incorporates the voluntary behavioral elements that lead many people to be skeptical about the applicability of the medical model to drug addiction. In any case, the committee embraces the disease concept, not because it is indisputable but because this paradigm facilitates scientific investigation in many important areas of knowledge, without inhibiting or distorting scientific inquiry in other parts of the field.
IMPORTANCE OF DRUG ABUSE RESEARCH
The widespread prevalence of illicit drug use in the United States is well documented in surveys of households, students, and prison and jail inmates ( Chapter 4 ). Based on the National Household Survey on Drug Abuse (NHSDA), an annual survey presently sponsored by SAMHSA, it was estimated that in 1994, 12.6 million people had used illicit drugs (primarily marijuana) in the past month (SAMHSA, 1995). That figure represents 6 percent of the population 12 years of age or older. 3 The number of heavy drug users, using drugs at least once a week, is difficult to determine. It has been estimated that in 1993 there were 2.1 million heavy cocaine users and 444,000-600,000 heavy heroin users (Rhodes et al., 1995). This population represents a significant burden to society, not only in terms of federal expenditures but also in terms of costs related to the multiple consequences of drug abuse (see Chapter 7 ).
The ultimate aim of the nation's investment in drug abuse research is to enable society to take effective measures to prevent drug use, abuse, and dependence, and thereby reduce its adverse individual and social consequences and associated costs. The adverse consequences of drug abuse are numerous and profound and affect the individual's physical health and psychological and social functioning. Consequences of drug abuse include increased rates of HIV infection and tuberculosis (TB); education and vocational impairment; developmental harms to children of
drug-using parents associated with fetal exposure or maltreatment and neglect; and increased violence (see Chapter 7 ). It now appears that injection drug use is the leading risk factor for new HIV infection in the United States (Holmberg, 1996). Most (80 percent) HIV-infected heterosexual men and women who do not use injection drugs have been infected through sexual contact with HIV-infected injection drug users (IUDs). Thus, it is not surprising that the geographic distribution of heterosexual AIDS cases has been essentially the same as the distribution of male injection drug users' AIDS cases (Holmberg, 1996) Further, the IUDs-associated HIV epidemic in men is reflected in the heterosexual epidemic in women, which is reflected in HIV infection in children (CDC, 1995). Nearly all children who acquire HIV infection do so prenatal (see Chapter 7 ).
The extent of the impact of drug use and abuse on society is evidenced by its enormous economic burden. In 1990, illicit drug abuse is estimated to have cost the United States more than $66 billion. When the cost of illicit drug use and abuse is tallied with that of alcohol and nicotine ( Table 1.1 ), the collective cost of drug use and abuse exceeds the estimated annual $117 billion cost of heart disease and the estimated annual $104 billion cost of cancer (AHA, 1992; ACS, 1993; D. Rice, University of California at San Francisco, personal communication, 1995).
As noted above, the federal government accounts for a large segment of the societal expenditure on illicit drug abuse control—spending more than $13.3 billion in FY 1995 (ONDCP, 1996). About two-thirds was devoted to interdiction, intelligence, incarceration, and other law enforcement activities. Research, however, accounts for only 4 percent of federal outlays, a percentage that has remained virtually unchanged since 1981 (ONDCP, 1996) ( Figure 1.1 ). Given the social costs of illicit drug abuse and the enormity of the federal investment in prevention and control, research into the causes, consequences, treatment, and prevention of drug abuse should have a higher priority. Enhanced support for drug abuse research would be a socially sound investment, because scientific research can be expected to generate new and improved treatments, as well as prevention and control strategies that can help reduce the enormous social burden associated with drug abuse.
THE CONTEXT OF DRUG ABUSE RESEARCH
In the chapters that follow, the committee identifies research initiatives that seem most promising and most likely to lead to successful efforts to reduce drug abuse and its associated social costs. Although the yield from these initiatives will depend largely on the creativity and skill of scientists, the many contextual factors that will also have a major bear-
TABLE 1.1 Estimated Economic Costs (million dollars) of Drug Abuse, 1990
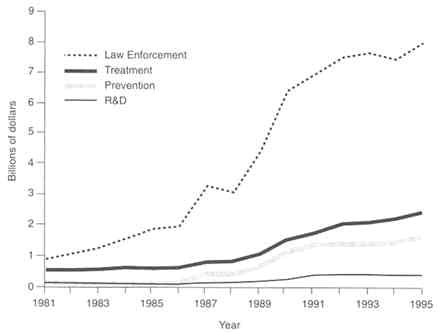
FIGURE 1.1 Federal drug control budget trends (1981-1995). NOTE: Figures are in current dollars. SOURCE: ONDCP (1996).
ing on the payoff from scientific inquiry cannot be ignored. The committee has identified six major factors that, if successfully addressed, could optimize the gains made in each area of drug abuse research: stable funding; use of a comprehensive public health framework; wider acceptance of a medical model of drug dependence; better translation of research findings into practice; raising the status of drug abuse research; and facilitating interdisciplinary research.
Stable Funding
A stable level of funding in any area of biomedical research is needed to sustain and build on research accomplishments, to retain a cadre of experts in a field, and to attract young investigators. Drug abuse research, in comparison with many other research venues, has not enjoyed consistent federal support (IOM, 1990, 1995; see also Appendix B ). The field has suffered from difficulties in recruiting and retaining young researchers and clinicians and in maintaining a stable research infrastructure (IOM, 1995). Society's capacity to contain and manage drug abuse
depends upon a stable, long-term investment in research. The vicissitudes in federal research funding often reflect changing currents in public opinion toward drugs and drug users ( Appendix B ). However, drug abuse will not disappear; it is an endemic social and public health problem. The nation must commit itself to a sustained effort. The social investment in research is an investment in "human capital" that must be sustained over the long term in order to reap the expected gains. An investment in this field is squandered if researchers who have been recruited and trained in drug abuse research are drawn to other fields because of uncertainty about the stability of future funding.
Adoption of a Comprehensive Public Health Framework
The social impact of drug abuse research can be enhanced significantly by conceptualizing goals and priorities within a comprehensive public health framework (Goldstein, 1994). All too often, public discourse about drug abuse is characterized by such unnecessary and fruitless disputes as whether drug abuse should be viewed as a social and moral problem or a health problem, whether the drug problem can best be solved by law enforcement or by medicine, whether priority should be placed on reducing supply or reducing demand, and so on. The truth is that these dichotomies oversimplify a brain disease impacted by a complex set of behaviors and a diverse array of potentially useful social responses. Forced choices of this nature also tend to inhibit or foreclose potentially useful research strategies. Confusion about social goals can lead to confusion about research priorities and can obscure the links between investigations viewing the subject through different lenses.
Some issues tend to recur. A prominent dispute centers on whether preventing drug use is important in itself or whether society should be more concerned with abuse or with the harmful consequences of use. The answer, of course, is that such a forced choice obscures, rather than clarifies, the issues. From a public health standpoint, drug use is a risk factor; the significance of use (whether of alcohol, nicotine, or illicit drugs) lies in the risk of harm associated with it (e.g., fires from smoking, impaired driving from alcohol or illicit drugs, or developmental setbacks) and in the risk that use will intensify, escalating to abuse or dependence. Those risks vary widely in relation to drug, user characteristics, social context, etc. Attention to the consequences of use and to the risk of escalation helps to set priorities (for research and policy) and provides a framework for assessing the impact of different interventions.
From a public policy standpoint, arguments about goals and priorities are fraught with controversy. From the standpoint of research strategy, however, the key lies in asking the right questions (e.g., What influ-
ences the pathways from use, to abuse, to dependence? What are the effects of needle exchange programs on illicit drug use and on HIV disease?) and in generating the knowledge required to facilitate informed policy debate. The main virtues of a comprehensive public health approach are that it helps to disentangle scientific questions from policy questions and that it encompasses all of the pertinent empirical questions, including the causes and consequences of use, abuse, and dependence, as well as the efficacy and cost of all types of interventions. In sum, the social payoff from drug abuse research can be enhanced substantially by integrating diverse strands of inquiry within a public health framework.
Acceptance of a Medical Model of Drug Dependence
Drug dependence is a chronic, relapsing brain disease that, like other diseases, can be evaluated and treated with the standard tools of medicine, including efforts in prevention, diagnosis, and treatment with medications and behavioral or psychosocial therapies. Unfortunately, the medical model of dependence is not universally accepted by health professionals and others in the treatment community; it is widely rejected within the law enforcement community and often by the public at large, which tends to view the complex and varied patterns of use, abuse, and dependence as an undifferentiated behavior rather than a medical problem.
Resistance to the medical model takes many forms. One is resistance to pharmacotherapies, such as methadone, that are seen as substituting licit drugs for illicit drugs without changing drug-taking behavior. Conversely, treatment approaches that adopt a rigid drug-free strategy preclude the use of medications for patients with other psychiatric disorders that are easily treated by pharmacotherapeutic approaches. On a subtler level, resistance to the use of pharmacotherapies is evidenced by the routine use of inadequate doses of methadone (D'Aunno and Vaughn, 1992). Finally, for others, all forms of drug abuse signify a failure of willpower or a moral weakness requiring punishment, incarceration, or moral education rather than treatment (Anglin and Hser, 1992).
Resistance to the medical model of drug dependence presents numerous barriers to research. Clinical researchers experience difficulty in soliciting participation by both treatment program administrators and patients, who are sometimes mistrustful of researchers' motives. If research involves a medication that is itself prone to abuse, there are additional regulatory requirements for drug scheduling, storage, and record keeping that act to discourage investigation (see Chapter 10 ; IOM, 1995). The ever-present threat of inappropriate intrusion by law enforcement agents has a chilling effect on treatment research (McDuff et al., 1993). All barri-
ers to inquiry, irrespective of whether they are legal or social in origin, raise the cost of research and discourage researchers from entering the field. Additionally, those barriers diminish the likelihood that a pharmaceutical company will invest in the development of antiaddiction medications (IOM, 1995). 4 Broader acceptance of the medical model of drug dependence would provide an incentive for researchers and clinicians to enter this field of research. Over time, a developing consensus in support of the medical model could facilitate common discourse, help to shape a shared research agenda within a public health framework, and diminish tensions between the research and treatment communities and the criminal justice system.
Better Translation of Research Findings into Practice and Policy
To benefit society, new research findings must be disseminated adequately to treatment providers, educators, law enforcement officials, and community leaders. In the case of prevention practices, it is often difficult for communities to change entrenched policies, particularly when combined with political imperatives for action to counteract drug abuse. In the case of treatment, technology transfer is impeded by the heterogeneity of providers and their marginalization at the outskirts of the medical community (see IOM, 1990, 1995; see also Chapter 8 ). Physicians and psychiatrists are seldom employed by specialized drug treatment facilities (approximately one-quarter employ medical doctors), and treatment is delivered by counselors whose training and supervision vary greatly and who have little access to and understanding of research results (Ball and Ross, 1991; Batten et al., 1993). These factors not only impede the transfer of research findings to the field but also impede communication from the field to the laboratory so that research designs can be modified in response to clinical realities (Pentz, 1994). Thus, there is a real need for bidirectional communication, from bench to bedside and back to the basic scientist (IOM, 1994).
The committee is aware, however, of recent technology transfer efforts in the field such as the Treatment Improvement Protocol Series, an initiative to establish guidelines for drug abuse treatment with an emphasis on incorporating research findings (SAMHSA, 1993), and the Prevention Enhancement Protocol System, a process implemented by the Center
for Substance Abuse Prevention in which scientists and practitioners develop protocols to identify and evaluate the strength of evidence on topics related to prevention interventions. Similar efforts will be invaluable for communicating and integrating research results to the treatment community.
Research frequently results in product development leading to changes in operations and an overall enhancement of the value of the enterprise. For example, in the pharmaceutical industry research often leads to the development of new medications or devices. In the public sector, however, research is often divorced from the implementation of findings and development. Research is often more basic than applied, and the fruits of research are not realized by the government, but by the private sector. Although that approach may be appropriate, it is unfortunately not always the most productive strategy for advancing research, knowledge, and product development. That is particularly true in the development of medications for opiate and cocaine addictions, where there is a great need for commitment from the private sector. However, many obstacles prevent active involvement of the pharmaceutical industry in this area of research and development (IOM, 1995).
A similar problem arises in relation to policymaking. Because debates about drug policy tend to be so highly polarized and politicized, research findings are often distorted, or selectively deployed, for rhetorical purposes. Researchers cannot prevent this practice, which is a common feature of political debate in a democratic society. However, researchers and their sponsors should not be indifferent to the disconnect between policy discourse and science. Researchers should establish and support institutional mechanisms for communicating an important message to policymakers and to the general public. Scientific research has produced a solid, and growing, body of knowledge about drug abuse and about the efficacy of various interventions that aim to prevent and control it. As long as drug abuse remains a poorly understood social problem, policy will be based mainly on wish and supposition; steps should be taken to educate policymakers about the scientific and technological advances in addiction research. Only then will it be possible for policymaking to support legislation that adequately funds new research and applies research findings. To some extent, persisting failure to reap the fruits of drug abuse research is attributable to the low visibility of the field—a problem to which the discussion now turns.
Raising the Status of Drug Abuse Research
Drug abuse research is often an undervalued area of inquiry, and most scientists and clinicians choose other disciplines in which to develop
their careers. Compared with other fields of research, investigators in drug abuse are often paid less, have less prestige among their peers, and must contend with the unique complexities of performing research in this area (e.g., regulations on controlled substances) (see IOM, 1995). The overall result is an insufficient number of basic and clinical researchers. IOM has recently begun a study, funded by the W. M. Keck Foundation of Los Angeles, to develop strategies to raise the status of drug abuse research. 5
Weak public support for this field of study is evident in unstable federal funding (see above), a lack of pharmaceutical industry investment in the development of antiaddiction medications (IOM, 1995), and inadequate funding for research training (IOM, 1995). NIDA's FY 1994 training budget, which is crucial to the flow of young researchers into the field, was about 2 percent of its extramural research budget, a percentage substantially lower than the overall National Institutes of Health (NIH) training budget, which averages 4.8 percent of its extramural research budget.
Beyond funding problems, investigators face a host of barriers to research: research subjects may pose health risks (e.g., TB, HIV/AIDS, and other infectious diseases), may be noncompliant, may deny their drug abuse problems, and may be involved in the criminal justice system. Even when research is successful and points to improvements in service delivery, the positive outcome may not be translated into practice or policy. For example, more than a year after the Food and Drug Administration's (FDA's) approval of levo-alpha-acetylmethadol (LAAM) as the first new medication for the treatment of opiate dependence in over 20 years, fewer than 1,000 patients nationwide actually had received the medication (IOM, 1995). More recently, scientific evidence regarding the beneficial effects of needle exchange programs (NRC, 1995) has received inadequate attention. Continuing indifference to scientific progress in drug abuse research inevitably depresses the status of the field, leading in turn to difficulties in recruiting new investigators.
Increasing Interdisciplinary Research
The breadth of expertise needed in drug abuse research spans many disciplines, including the behavioral sciences, pharmacology, medicine, and the neurosciences, and many fields of inquiry, including etiology, epidemiology, prevention, treatment, and health services research. Aspects of research relating to drug use tend to draw on developmental perspectives and to focus on general population samples in community settings, especially schools. Aspects of research relating to abuse and de-
pendence tend to be more clinical in nature, drawing on psychopathological perspectives. Additionally, a full account of any aspect of drug-taking behavior must also reflect an understanding of social context. The rich interplay between neuroscience and behavioral research and between basic and clinical research poses distinct challenges and opportunities.
Unfortunately, research tends to be fragmented within disciplinary boundaries. The difficulties in conducting successful interdisciplinary research are well known. Funds for research come from many separate agencies, such as the NIDA, NIMH, and SAMHSA. These agencies all have different programmatic emphases as they attempt to shape the direction of research in their respective fields. In times of funding constraints, agencies may be less inclined to fund projects at the periphery of their interests.
Additionally, NIH study sections, which rank grant proposals, are discipline specific, making it difficult for interdisciplinary proposals to ''qualify" (i.e., receive a high rank) for funding. Another problem is that the most advanced scientific literature tends to be compartmentalized within discipline or subject matter categories, making it difficult for scientists to see the whole field. The problem is exacerbated by what Tonry (1990) has called "fugitive literatures," studies carried out by private sector research firms or independent research agencies and available only in reports submitted to the sponsoring agency.
In light of lost opportunities for collaboration and interdisciplinary research, IOM (1995) previously recommended the creation and expansion of comprehensive drug abuse centers to coordinate all aspects of drug abuse research, training, and treatment. The field of drug abuse research presents a real opportunity to bridge the intellectual divide between the behavioral and neuroscience communities and to overcome the logistical impediments to interdisciplinary research.
INVESTING WISELY IN DRUG ABUSE RESEARCH
This report sets forth drug abuse research initiatives for the next decade based on a thorough assessment of what is now known and a calculated judgment about what initiatives are most likely to advance our knowledge in useful ways. This report is not meant to be a road map or tactical battle plan, but is best regarded as a strategic outline. Within each discipline of drug abuse research, the committee has highlighted priorities for future research. However, the committee did not make any attempt to prioritize recommendations across varied disciplines and fields of research. Prudent research planning must respond to newly emerging opportunities and needs while maintaining a steady commitment to the
achievement of long-term objectives. The ability to respond to new goals and needs may be the real challenge for the field of drug abuse research.
Drug abuse research is an important public investment. The ultimate aim of that investment is to reduce the enormous social costs attributable to drug abuse and dependence. Of course, drug abuse research must also compete for funding with research in other fields of public health, research in other scientific domains, and other pressing public needs. Recognizing the scarcity of resources, the committee has also considered ways in which the research effort can be harnessed most effectively to increase the yield per dollar invested. These include stable funding, use of a comprehensive public health framework, wider acceptance of a medical model of drug dependence, better translation of research findings into practice and policy, raising the status of drug abuse research, and facilitating interdisciplinary research.
The committee notes that there have been major accomplishments in drug abuse research over the past 25 years and commends NIDA for leading that effort. The committee is convinced that the field is on the threshold of significant advances, and that a sustained research effort will strengthen society's capacity to reduce drug abuse and to ameliorate its adverse consequences.
ORGANIZATION OF THE REPORT
This report sets forth a series of initiatives in drug abuse research. 6 Each chapter of the report covers a segment of the field, describes selected accomplishments, and highlights areas that seem ripe for future research. As noted, the committee has not prioritized areas for future research but, instead, has identified those areas that most warrant further exploration.
Chapter 2 describes behavioral models of drug abuse and demonstrates how the use of behavioral procedures has given researchers the ability to measure drug-taking objectively and to study the development, maintenance, and consequences of that behavior. Chapter 3 discusses drug abuse within the context of neurotransmission; it describes neurobiological advances in drug abuse research and provides the foundation for the current understanding of addiction as a brain disease. The epidemiological information systems designed to gather information on drug use in the United States are identified in Chapter 4 . The data collected from the systems provide an essential foundation for systematic study of
the etiology and consequences of drug abuse, which are addressed, respectively, in Chapters 5 and 7 . Chapter 6 addresses the efficacy of interventions designed to prevent drug abuse. The effectiveness of drug abuse treatment and the difficulties in treating special populations of drug users are discussed in Chapter 8 , while the impact of managed care on access, costs, utilization, and outcomes of treatment is addressed in Chapter 9 . Finally, Chapter 10 discusses the effects of drug control on public health and identifies areas for policy-relevant research.
Specific recommendations appear in each chapter. Although these recommendations reflect the committee's best judgment regarding priorities within the specific domains of research, the committee did not identify priorities or rank recommendations for the entire field of drug abuse research. Opportunities for advancing knowledge exist in all domains. It would be a mistake to invest too narrowly in a few fields of inquiry. At the present time, soundly conceived research should be pursued in all domains along the lines outlined in this report.
ACS (American Cancer Society). 1993. Cancer Facts and Figures, 1993 . Washington, DC: ACS.
AHA (American Heart Association). 1992. 1993 Heart and Stroke Fact Statistics . Dallas, TX: AHA.
Anglin MD, Hser Y. 1992. Treatment of drug abuse. In: Watson RR, ed. Drug Abuse Treatment. Vol. 3, Drug and Alcohol Abuse Reviews . New York: Humana Press.
APA (American Psychiatric Association). 1994. Diagnostic and Statistical Manual of Mental Disorders . 4th ed. Washington, DC: APA.
Ball JC, Ross A. 1991. The Effectiveness of Methadone Maintenance Treatment . New York: Springer-Verlag.
Batten H, Horgan CM, Prottas J, Simon LJ, Larson MJ, Elliott EA, Bowden ML, Lee M. 1993. Drug Services Research Survey Final Report: Phase I . Contract number 271-90-8319/1. Submitted to the National Institute of Drug Abuse. Waltham, MA: Bigel Institute for Health Policy, Brandeis University.
Brewley T. 1995. Conversation with Thomas Brewley. Addiction 90:883-892.
Carr DB, Jacox AK, Chapman CR, et al. 1992. Acute Pain Management: Operative or Medical Procedures and Trauma. Clinical Practice Guidelines . AHCPR Publication No. 92-0032. Rockville, MD: U.S. Public Health Service, Agency for Health Care Policy and Research.
CDC (Centers for Disease Control and Prevention). 1995. HIV/AIDS Surveillance Report 7(2).
Cooper JR, Bloom FE, Roth RH. 1991. The Biochemical Basis of Neuropharmacology . 6th ed. New York: Oxford University Press.
Daley DC, Marlatt GA. 1992. Relapse prevention: Cognitive and behavioral interventions. In: Lowinson JH, Ruiz P, Millman RB, Langrod JG, eds. Substance Abuse: A Comprehensive Textbook . Baltimore: Williams and Wilkins.
D'Aunno T, Vaughn TE. 1992. Variation in methadone treatment practices. Journal of the American Medical Association 267:253-258.
DiGregorio GJ. 1990. Cocaine update: Abuse and therapy. American Family Physician 41(1):247-250.
Foley KM, Inturrisi CE, eds. 1986. Opioid Analgesics in the Management of Clinical Pain. Advances in Pain Research and Therapy. Vol. 8. New York: Raven Press.
GAO (General Accounting Office). 1992. Drug Abuse Research: Federal Funding and Future Needs . GAO/PEMD-92-5. Washington, DC: GAO.
Glassman AH, Covey LS, Dalack GW, Stetner F, Rivelli SK, Fleiss J, Cooper TB. 1993. Smoking cessation, clonidine, and vulnerability to nicotine among dependent smokers. Clinical Pharmacology and Therapeutics 54(6):670-679.
Goldstein A. 1994. Addiction: From Biology to Drug Policy . New York: W.H. Freeman.
Hokfelt TGM, Castel MN, Morino P, Zhang X, Dagerlind A. 1995. General overview of neuropeptides. In: Bloom FE, Kupfer DJ, eds. Psychopharmacology: Fourth Generation of Progress . New York: Raven Press. Pp. 483-492.
Holmberg SD. 1996 . The estimated prevalence and incidence of HIV in 96 large U.S. metropolitan areas . American Journal of Public Health 86(5):642-654.
IOM (Institute of Medicine). 1990. Treating Drug Problems . Washington, DC: National Academy Press.
IOM (Institute of Medicine). 1994. AIDS and Behavior: An Integrated Approach . Washington, DC: National Academy Press.
IOM (Institute of Medicine). 1995. The Development of Medications for the Treatment of Opiate and Cocaine Addictions. Washington, DC: National Academy Press.
Jacox A, Carr DB, Payne R, et al. 1994. Management of Cancer Pain. Clinical Practice Guideline . AHCPR Publication No. 94-0592. Rockville, MD: U.S. Public Health Service, Agency for Health Care Policy and Research.
Kahn RS, Davis KL. 1995. New developments in dopamine and schizophrenia. In: Bloom FE, Kupfer DJ, eds. Psychopharmacology: Fourth Generation of Progress . New York: Raven Press. Pp. 1193-1204.
McDuff DR, Schwartz RP, Tommasello A, Tiegel S, Donovan T, Johnson JL. 1993. Outpatient benzodiazepine detoxification procedure for methadone patients. Journal of Substance Abuse Treatment 10:297-302.
McLellan AT, Metzger DS, Alterman Al, Woody GE, Durell J, O'Brien CP. In press. Is addiction treatment "worth it"? Public health expectations, policy-based comparisons. Milbank Quarterly .
Meyer R. 1996. The disease called addiction: Emerging evidence in a 200-year debate. Lancet 347:162-166.
Miller NS. 1991. Drug and alcohol addiction as a disease. In: Miller NS, ed. Comprehensive Handbook of Drug and Alcohol Addiction . New York: Marcel Dekker.
MMWR (Morbidity and Mortality Weekly Report). 1994. Medical care expenditures attributable to cigarette smoking, United States, 1993. Morbidity and Mortality Weekly Report 43(26):469-472.
NRC (National Research Council). 1995. Preventing HIV Transmission: The Role of Sterile Needles and Bleach . Washington, DC: National Academy Press.
O'Brien CP, McLellan AT. 1996. Myths about the treatment of addiction. Lancet 347:237-240.
Olson GA, Olson RD, Kastin AJ. 1994. Endogenous opiates, 1993. Peptides 15:1513-1556.
ONDCP (Office of National Drug Control Policy). 1996. National Drug Control Strategy . Washington, DC: ONDCP.
Pentz M. 1994. Directions for future research in drug abuse prevention. Preventive Medicine 23:646-652.
Rhodes W, Scheiman P, Pittayathikhun T, Collins L, Tsarfaty V. 1995. What America's Users Spend on Illegal Drugs, 1988-1993 . Prepared for the Office of National Drug Control Policy, Washington, DC.
Rice DP, Kelman S, Miller LS, Dunmeyer S. 1990. The Economic Costs of Alcohol and Drug Abuse and Mental Illness: 1985 . DHHS Publication No. (ADM) 90-1694. San Francisco: University of California, Institute for Health and Aging.
Rice DP, Max W, Novotny T, Shultz J, Hodgson T. 1992. The Cost of Smoking Revisited: Preliminary Estimates . Paper presented at the American Public Health Association Annual Meeting, November 23, 1992. Washington, DC.
SAMHSA (Substance Abuse and Mental Health Services Administration). 1993. Improving Treatment for Drug-Exposed Infants: Treatment Improvement Protocol (TIP) Series . Washington, DC: U.S. Department of Health and Human Services.
SAMHSA (Substance Abuse and Mental Health Services Administration). 1995. National Household Survey on Drug Abuse: Population Estimates 1994 . Washington, DC: U.S. Department of Health and Human Services.
Schelling TC. 1992 . Addictive drugs: The cigarette experience. Science 255:431-433.
Tonry M. 1990. Research on drugs and crime. In: Morris N, Tonry M, eds. Drugs and Crime . Vol. 13 . Chicago: University of Chicago Press.
Volkow ND, Fowler JS, Wang G-J, Hitzemann R, Logan J, Schlyer DJ, Dewey SI, Wolf AD. 1993. Decreased dopamine D2 receptor availability is associated with reduced frontal metabolism in cocaine abusers. Synapse 14:169-177.
Wall PD, Melzack R. 1994. Textbook of Pain . 3rd ed. Edinburg: Churchill-Livingstone.
WHO (World Health Organization). 1992. International Statistical Classification of Diseases and Related Health Problems . Tenth Revision. Geneva: WHO.
Drug abuse persists as one of the most costly and contentious problems on the nation's agenda. Pathways of Addiction meets the need for a clear and thoughtful national research agenda that will yield the greatest benefit from today's limited resources.
The committee makes its recommendations within the public health framework and incorporates diverse fields of inquiry and a range of policy positions. It examines both the demand and supply aspects of drug abuse.
Pathways of Addiction offers a fact-filled, highly readable examination of drug abuse issues in the United States, describing findings and outlining research needs in the areas of behavioral and neurobiological foundations of drug abuse. The book covers the epidemiology and etiology of drug abuse and discusses several of its most troubling health and social consequences, including HIV, violence, and harm to children.
Pathways of Addiction looks at the efficacy of different prevention interventions and the many advances that have been made in treatment research in the past 20 years. The book also examines drug treatment in the criminal justice setting and the effectiveness of drug treatment under managed care.
The committee advocates systematic study of the laws by which the nation attempts to control drug use and identifies the research questions most germane to public policy. Pathways of Addiction provides a strategic outline for wise investment of the nation's research resources in drug abuse. This comprehensive and accessible volume will have widespread relevance—to policymakers, researchers, research administrators, foundation decisionmakers, healthcare professionals, faculty and students, and concerned individuals.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
- First Online: 24 June 2017
Cite this chapter

- John Joshua 2
557 Accesses
The use of illicit drugs and the quality of life is intended to provide a rational for a change in some of the present drug policies. After all, the use and the abuse of drugs is largely a health issue and cannot be solved without adequately considering the causes of drug abuse, including the medical, psychiatric, psychological, and sociological factors. Criminal law can only be part of the solution; it has to effectively work with psychologically and medically trained personnel. To use solely the criminal law in regard to drug abuse may treat the symptoms, but it is not a cure. It has been argued that the legalization of the use of illegal drugs but within a regulated market might be more suitable.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Johnson, C. M., & Meier, K. J. (1990). The wages of sin: Taxing America’s legal vices. Western Political Quarterly, 43 (3), 577–595.
Article Google Scholar
Download references
Author information
Authors and affiliations.
Deakin University, Melbourne, Victoria, Australia
John Joshua
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to John Joshua .
Rights and permissions
Reprints and permissions
Copyright information
© 2017 The Author(s)
About this chapter
Joshua, J. (2017). Conclusion. In: The Economics of Addictive Behaviours Volume III. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-319-59138-4_8
Download citation
DOI : https://doi.org/10.1007/978-3-319-59138-4_8
Published : 24 June 2017
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-319-59137-7
Online ISBN : 978-3-319-59138-4
eBook Packages : Economics and Finance Economics and Finance (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 22 February 2021
Addiction as a brain disease revised: why it still matters, and the need for consilience
- Markus Heilig 1 ,
- James MacKillop ORCID: orcid.org/0000-0003-4118-9500 2 , 3 ,
- Diana Martinez 4 ,
- Jürgen Rehm ORCID: orcid.org/0000-0001-5665-0385 5 , 6 , 7 , 8 ,
- Lorenzo Leggio ORCID: orcid.org/0000-0001-7284-8754 9 &
- Louk J. M. J. Vanderschuren ORCID: orcid.org/0000-0002-5379-0363 10
Neuropsychopharmacology volume 46 , pages 1715–1723 ( 2021 ) Cite this article
89k Accesses
103 Citations
326 Altmetric
Metrics details
A Correspondence to this article was published on 03 May 2021
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that the brain disease view is deterministic, fails to account for heterogeneity in remission and recovery, places too much emphasis on a compulsive dimension of addiction, and that a specific neural signature of addiction has not been identified. We acknowledge that some of these criticisms have merit, but assert that the foundational premise that addiction has a neurobiological basis is fundamentally sound. We also emphasize that denying that addiction is a brain disease is a harmful standpoint since it contributes to reducing access to healthcare and treatment, the consequences of which are catastrophic. Here, we therefore address these criticisms, and in doing so provide a contemporary update of the brain disease view of addiction. We provide arguments to support this view, discuss why apparently spontaneous remission does not negate it, and how seemingly compulsive behaviors can co-exist with the sensitivity to alternative reinforcement in addiction. Most importantly, we argue that the brain is the biological substrate from which both addiction and the capacity for behavior change arise, arguing for an intensified neuroscientific study of recovery. More broadly, we propose that these disagreements reveal the need for multidisciplinary research that integrates neuroscientific, behavioral, clinical, and sociocultural perspectives.
Similar content being viewed by others
Subtypes in addiction and their neurobehavioral profiles across three functional domains

Drug addiction: from bench to bedside
The neurobiology of drug addiction: cross-species insights into the dysfunction and recovery of the prefrontal cortex
Introduction.
Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that “addiction is a brain disease”, articulated a set of implications of this position, and outlined an agenda for realizing its promise [ 1 ]. The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the efforts of researchers, and resource allocation by funding agencies. A subsequent 2000 paper by McLellan et al. [ 2 ] examined whether data justify distinguishing addiction from other conditions for which a disease label is rarely questioned, such as diabetes, hypertension or asthma. It concluded that neither genetic risk, the role of personal choices, nor the influence of environmental factors differentiated addiction in a manner that would warrant viewing it differently; neither did relapse rates, nor compliance with treatment. The authors outlined an agenda closely related to that put forward by Leshner, but with a more clinical focus. Their conclusion was that addiction should be insured, treated, and evaluated like other diseases. This paper, too, has been exceptionally influential by academic standards, as witnessed by its ~3000 citations to date. What may be less appreciated among scientists is that its impact in the real world of addiction treatment has remained more limited, with large numbers of patients still not receiving evidence-based treatments.
In recent years, the conceptualization of addiction as a brain disease has come under increasing criticism. When first put forward, the brain disease view was mainly an attempt to articulate an effective response to prevailing nonscientific, moralizing, and stigmatizing attitudes to addiction. According to these attitudes, addiction was simply the result of a person’s moral failing or weakness of character, rather than a “real” disease [ 3 ]. These attitudes created barriers for people with substance use problems to access evidence-based treatments, both those available at the time, such as opioid agonist maintenance, cognitive behavioral therapy-based relapse prevention, community reinforcement or contingency management, and those that could result from research. To promote patient access to treatments, scientists needed to argue that there is a biological basis beneath the challenging behaviors of individuals suffering from addiction. This argument was particularly targeted to the public, policymakers and health care professionals, many of whom held that since addiction was a misery people brought upon themselves, it fell beyond the scope of medicine, and was neither amenable to treatment, nor warranted the use of taxpayer money.
Present-day criticism directed at the conceptualization of addiction as a brain disease is of a very different nature. It originates from within the scientific community itself, and asserts that this conceptualization is neither supported by data, nor helpful for people with substance use problems [ 4 , 5 , 6 , 7 , 8 ]. Addressing these critiques requires a very different perspective, and is the objective of our paper. We readily acknowledge that in some cases, recent critiques of the notion of addiction as a brain disease as postulated originally have merit, and that those critiques require the postulates to be re-assessed and refined. In other cases, we believe the arguments have less validity, but still provide an opportunity to update the position of addiction as a brain disease. Our overarching concern is that questionable arguments against the notion of addiction as a brain disease may harm patients, by impeding access to care, and slowing development of novel treatments.
A premise of our argument is that any useful conceptualization of addiction requires an understanding both of the brains involved, and of environmental factors that interact with those brains [ 9 ]. These environmental factors critically include availability of drugs, but also of healthy alternative rewards and opportunities. As we will show, stating that brain mechanisms are critical for understanding and treating addiction in no way negates the role of psychological, social and socioeconomic processes as both causes and consequences of substance use. To reflect this complex nature of addiction, we have assembled a team with expertise that spans from molecular neuroscience, through animal models of addiction, human brain imaging, clinical addiction medicine, to epidemiology. What brings us together is a passionate commitment to improving the lives of people with substance use problems through science and science-based treatments, with empirical evidence as the guiding principle.
To achieve this goal, we first discuss the nature of the disease concept itself, and why we believe it is important for the science and treatment of addiction. This is followed by a discussion of the main points raised when the notion of addiction as a brain disease has come under criticism. Key among those are claims that spontaneous remission rates are high; that a specific brain pathology is lacking; and that people suffering from addiction, rather than behaving “compulsively”, in fact show a preserved ability to make informed and advantageous choices. In the process of discussing these issues, we also address the common criticism that viewing addiction as a brain disease is a fully deterministic theory of addiction. For our argument, we use the term “addiction” as originally used by Leshner [ 1 ]; in Box 1 , we map out and discuss how this construct may relate to the current diagnostic categories, such as Substance Use Disorder (SUD) and its different levels of severity (Fig. 1) .
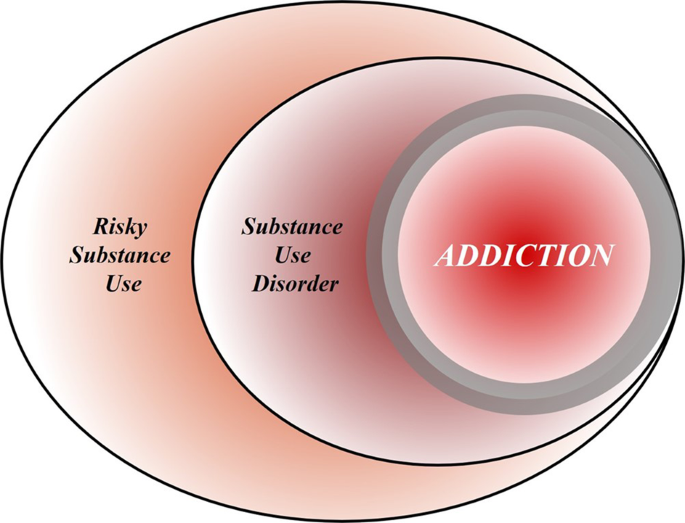
Risky (hazardous) substance use refers to quantity/frequency indicators of consumption; SUD refers to individuals who meet criteria for a DSM-5 diagnosis (mild, moderate, or severe); and addiction refers to individuals who exhibit persistent difficulties with self-regulation of drug consumption. Among high-risk individuals, a subgroup will meet criteria for SUD and, among those who have an SUD, a further subgroup would be considered to be addicted to the drug. However, the boundary for addiction is intentionally blurred to reflect that the dividing line for defining addiction within the category of SUD remains an open empirical question.
Box 1 What’s in a name? Differentiating hazardous use, substance use disorder, and addiction
Although our principal focus is on the brain disease model of addiction, the definition of addiction itself is a source of ambiguity. Here, we provide a perspective on the major forms of terminology in the field.
Hazardous Substance Use
Hazardous (risky) substance use refers to quantitative levels of consumption that increase an individual’s risk for adverse health consequences. In practice, this pertains to alcohol use [ 110 , 111 ]. Clinically, alcohol consumption that exceeds guidelines for moderate drinking has been used to prompt brief interventions or referral for specialist care [ 112 ]. More recently, a reduction in these quantitative levels has been validated as treatment endpoints [ 113 ].
Substance Use Disorder
SUD refers to the DSM-5 diagnosis category that encompasses significant impairment or distress resulting from specific categories of psychoactive drug use. The diagnosis of SUD is operationalized as 2 or more of 11 symptoms over the past year. As a result, the diagnosis is heterogenous, with more than 1100 symptom permutations possible. The diagnosis in DSM-5 is the result of combining two diagnoses from the DSM-IV, abuse and dependence, which proved to be less valid than a single dimensional approach [ 114 ]. Critically, SUD includes three levels of severity: mild (2–3 symptoms), moderate (4–5 symptoms), and severe (6+ symptoms). The International Classification of Diseases (ICD) system retains two diagnoses, harmful use (lower severity) and substance dependence (higher severity).
Addiction is a natural language concept, etymologically meaning enslavement, with the contemporary meaning traceable to the Middle and Late Roman Republic periods [ 115 ]. As a scientific construct, drug addiction can be defined as a state in which an individual exhibits an inability to self-regulate consumption of a substance, although it does not have an operational definition. Regarding clinical diagnosis, as it is typically used in scientific and clinical parlance, addiction is not synonymous with the simple presence of SUD. Nowhere in DSM-5 is it articulated that the diagnostic threshold (or any specific number/type of symptoms) should be interpreted as reflecting addiction, which inherently connotes a high degree of severity. Indeed, concerns were raised about setting the diagnostic standard too low because of the issue of potentially conflating a low-severity SUD with addiction [ 116 ]. In scientific and clinical usage, addiction typically refers to individuals at a moderate or high severity of SUD. This is consistent with the fact that moderate-to-severe SUD has the closest correspondence with the more severe diagnosis in ICD [ 117 , 118 , 119 ]. Nonetheless, akin to the undefined overlap between hazardous use and SUD, the field has not identified the exact thresholds of SUD symptoms above which addiction would be definitively present.
Integration
The ambiguous relationships among these terms contribute to misunderstandings and disagreements. Figure 1 provides a simple working model of how these terms overlap. Fundamentally, we consider that these terms represent successive dimensions of severity, clinical “nesting dolls”. Not all individuals consuming substances at hazardous levels have an SUD, but a subgroup do. Not all individuals with a SUD are addicted to the drug in question, but a subgroup are. At the severe end of the spectrum, these domains converge (heavy consumption, numerous symptoms, the unambiguous presence of addiction), but at low severity, the overlap is more modest. The exact mapping of addiction onto SUD is an open empirical question, warranting systematic study among scientists, clinicians, and patients with lived experience. No less important will be future research situating our definition of SUD using more objective indicators (e.g., [ 55 , 120 ]), brain-based and otherwise, and more precisely in relation to clinical needs [ 121 ]. Finally, such work should ultimately be codified in both the DSM and ICD systems to demarcate clearly where the attribution of addiction belongs within the clinical nosology, and to foster greater clarity and specificity in scientific discourse.
What is a disease?
In his classic 1960 book “The Disease Concept of Alcoholism”, Jellinek noted that in the alcohol field, the debate over the disease concept was plagued by too many definitions of “alcoholism” and too few definitions of “disease” [ 10 ]. He suggested that the addiction field needed to follow the rest of medicine in moving away from viewing disease as an “entity”, i.e., something that has “its own independent existence, apart from other things” [ 11 ]. To modern medicine, he pointed out, a disease is simply a label that is agreed upon to describe a cluster of substantial, deteriorating changes in the structure or function of the human body, and the accompanying deterioration in biopsychosocial functioning. Thus, he concluded that alcoholism can simply be defined as changes in structure or function of the body due to drinking that cause disability or death. A disease label is useful to identify groups of people with commonly co-occurring constellations of problems—syndromes—that significantly impair function, and that lead to clinically significant distress, harm, or both. This convention allows a systematic study of the condition, and of whether group members benefit from a specific intervention.
It is not trivial to delineate the exact category of harmful substance use for which a label such as addiction is warranted (See Box 1 ). Challenges to diagnostic categorization are not unique to addiction, however. Throughout clinical medicine, diagnostic cut-offs are set by consensus, commonly based on an evolving understanding of thresholds above which people tend to benefit from available interventions. Because assessing benefits in large patient groups over time is difficult, diagnostic thresholds are always subject to debate and adjustments. It can be debated whether diagnostic thresholds “merely” capture the extreme of a single underlying population, or actually identify a subpopulation that is at some level distinct. Resolving this issue remains challenging in addiction, but once again, this is not different from other areas of medicine [see e.g., [ 12 ] for type 2 diabetes]. Longitudinal studies that track patient trajectories over time may have a better ability to identify subpopulations than cross-sectional assessments [ 13 ].
By this pragmatic, clinical understanding of the disease concept, it is difficult to argue that “addiction” is unjustified as a disease label. Among people who use drugs or alcohol, some progress to using with a quantity and frequency that results in impaired function and often death, making substance use a major cause of global disease burden [ 14 ]. In these people, use occurs with a pattern that in milder forms may be challenging to capture by current diagnostic criteria (See Box 1 ), but is readily recognized by patients, their families and treatment providers when it reaches a severity that is clinically significant [see [ 15 ] for a classical discussion]. In some cases, such as opioid addiction, those who receive the diagnosis stand to obtain some of the greatest benefits from medical treatments in all of clinical medicine [ 16 , 17 ]. Although effect sizes of available treatments are more modest in nicotine [ 18 ] and alcohol addiction [ 19 ], the evidence supporting their efficacy is also indisputable. A view of addiction as a disease is justified, because it is beneficial: a failure to diagnose addiction drastically increases the risk of a failure to treat it [ 20 ].
Of course, establishing a diagnosis is not a requirement for interventions to be meaningful. People with hazardous or harmful substance use who have not (yet) developed addiction should also be identified, and interventions should be initiated to address their substance-related risks. This is particularly relevant for alcohol, where even in the absence of addiction, use is frequently associated with risks or harm to self, e.g., through cardiovascular disease, liver disease or cancer, and to others, e.g., through accidents or violence [ 21 ]. Interventions to reduce hazardous or harmful substance use in people who have not developed addiction are in fact particularly appealing. In these individuals, limited interventions are able to achieve robust and meaningful benefits [ 22 ], presumably because patterns of misuse have not yet become entrenched.
Thus, as originally pointed out by McLellan and colleagues, most of the criticisms of addiction as a disease could equally be applied to other medical conditions [ 2 ]. This type of criticism could also be applied to other psychiatric disorders, and that has indeed been the case historically [ 23 , 24 ]. Today, there is broad consensus that those criticisms were misguided. Few, if any healthcare professionals continue to maintain that schizophrenia, rather than being a disease, is a normal response to societal conditions. Why, then, do people continue to question if addiction is a disease, but not whether schizophrenia, major depressive disorder or post-traumatic stress disorder are diseases? This is particularly troubling given the decades of data showing high co-morbidity of addiction with these conditions [ 25 , 26 ]. We argue that it comes down to stigma. Dysregulated substance use continues to be perceived as a self-inflicted condition characterized by a lack of willpower, thus falling outside the scope of medicine and into that of morality [ 3 ].

Chronic and relapsing, developmentally-limited, or spontaneously remitting?
Much of the critique targeted at the conceptualization of addiction as a brain disease focuses on its original assertion that addiction is a chronic and relapsing condition. Epidemiological data are cited in support of the notion that large proportions of individuals achieve remission [ 27 ], frequently without any formal treatment [ 28 , 29 ] and in some cases resuming low risk substance use [ 30 ]. For instance, based on data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study [ 27 ], it has been pointed out that a significant proportion of people with an addictive disorder quit each year, and that most afflicted individuals ultimately remit. These spontaneous remission rates are argued to invalidate the concept of a chronic, relapsing disease [ 4 ].
Interpreting these and similar data is complicated by several methodological and conceptual issues. First, people may appear to remit spontaneously because they actually do, but also because of limited test–retest reliability of the diagnosis [ 31 ]. For instance, using a validated diagnostic interview and trained interviewers, the Collaborative Studies on Genetics of Alcoholism examined the likelihood that an individual diagnosed with a lifetime history of substance dependence would retain this classification after 5 years. This is obviously a diagnosis that, once met, by definition cannot truly remit. Lifetime alcohol dependence was indeed stable in individuals recruited from addiction treatment units, ~90% for women, and 95% for men. In contrast, in a community-based sample similar to that used in the NESARC [ 27 ], stability was only ~30% and 65% for women and men, respectively. The most important characteristic that determined diagnostic stability was severity. Diagnosis was stable in severe, treatment-seeking cases, but not in general population cases of alcohol dependence.
These data suggest that commonly used diagnostic criteria alone are simply over-inclusive for a reliable, clinically meaningful diagnosis of addiction. They do identify a core group of treatment seeking individuals with a reliable diagnosis, but, if applied to nonclinical populations, also flag as “cases” a considerable halo of individuals for whom the diagnostic categorization is unreliable. Any meaningful discussion of remission rates needs to take this into account, and specify which of these two populations that is being discussed. Unfortunately, the DSM-5 has not made this task easier. With only 2 out of 11 symptoms being sufficient for a diagnosis of SUD, it captures under a single diagnostic label individuals in a “mild” category, whose diagnosis is likely to have very low test–retest reliability, and who are unlikely to exhibit a chronic relapsing course, together with people at the severe end of the spectrum, whose diagnosis is reliable, many of whom do show a chronic relapsing course.
The NESARC data nevertheless show that close to 10% of people in the general population who are diagnosed with alcohol addiction (here equated with DSM-IV “dependence” used in the NESARC study) never remitted throughout their participation in the survey. The base life-time prevalence of alcohol dependence in NESARC was 12.5% [ 32 ]. Thus, the data cited against the concept of addiction as a chronic relapsing disease in fact indicate that over 1% of the US population develops an alcohol-related condition that is associated with high morbidity and mortality, and whose chronic and/or relapsing nature cannot be disputed, since it does not remit.
Secondly, the analysis of NESARC data [ 4 , 27 ] omits opioid addiction, which, together with alcohol and tobacco, is the largest addiction-related public health problem in the US [ 33 ]. This is probably the addictive condition where an analysis of cumulative evidence most strikingly supports the notion of a chronic disorder with frequent relapses in a large proportion of people affected [ 34 ]. Of course, a large number of people with opioid addiction are unable to express the chronic, relapsing course of their disease, because over the long term, their mortality rate is about 15 times greater than that of the general population [ 35 ]. However, even among those who remain alive, the prevalence of stable abstinence from opioid use after 10–30 years of observation is <30%. Remission may not always require abstinence, for instance in the case of alcohol addiction, but is a reasonable proxy for remission with opioids, where return to controlled use is rare. Embedded in these data is a message of literally vital importance: when opioid addiction is diagnosed and treated as a chronic relapsing disease, outcomes are markedly improved, and retention in treatment is associated with a greater likelihood of abstinence.
The fact that significant numbers of individuals exhibit a chronic relapsing course does not negate that even larger numbers of individuals with SUD according to current diagnostic criteria do not. For instance, in many countries, the highest prevalence of substance use problems is found among young adults, aged 18–25 [ 36 ], and a majority of these ‘age out’ of excessive substance use [ 37 ]. It is also well documented that many individuals with SUD achieve longstanding remission, in many cases without any formal treatment (see e.g., [ 27 , 30 , 38 ]).
Collectively, the data show that the course of SUD, as defined by current diagnostic criteria, is highly heterogeneous. Accordingly, we do not maintain that a chronic relapsing course is a defining feature of SUD. When present in a patient, however, such as course is of clinical significance, because it identifies a need for long-term disease management [ 2 ], rather than expectations of a recovery that may not be within the individual’s reach [ 39 ]. From a conceptual standpoint, however, a chronic relapsing course is neither necessary nor implied in a view that addiction is a brain disease. This view also does not mean that it is irreversible and hopeless. Human neuroscience documents restoration of functioning after abstinence [ 40 , 41 ] and reveals predictors of clinical success [ 42 ]. If anything, this evidence suggests a need to increase efforts devoted to neuroscientific research on addiction recovery [ 40 , 43 ].
Lessons from genetics
For alcohol addiction, meta-analysis of twin and adoption studies has estimated heritability at ~50%, while estimates for opioid addiction are even higher [ 44 , 45 ]. Genetic risk factors are to a large extent shared across substances [ 46 ]. It has been argued that a genetic contribution cannot support a disease view of a behavior, because most behavioral traits, including religious and political inclinations, have a genetic contribution [ 4 ]. This statement, while correct in pointing out broad heritability of behavioral traits, misses a fundamental point. Genetic architecture is much like organ structure. The fact that normal anatomy shapes healthy organ function does not negate that an altered structure can contribute to pathophysiology of disease. The structure of the genetic landscape is no different. Critics further state that a “genetic predisposition is not a recipe for compulsion”, but no neuroscientist or geneticist would claim that genetic risk is “a recipe for compulsion”. Genetic risk is probabilistic, not deterministic. However, as we will see below, in the case of addiction, it contributes to large, consistent probability shifts towards maladaptive behavior.
In dismissing the relevance of genetic risk for addiction, Hall writes that “a large number of alleles are involved in the genetic susceptibility to addiction and individually these alleles might very weakly predict a risk of addiction”. He goes on to conclude that “generally, genetic prediction of the risk of disease (even with whole-genome sequencing data) is unlikely to be informative for most people who have a so-called average risk of developing an addiction disorder” [ 7 ]. This reflects a fundamental misunderstanding of polygenic risk. It is true that a large number of risk alleles are involved, and that the explanatory power of currently available polygenic risk scores for addictive disorders lags behind those for e.g., schizophrenia or major depression [ 47 , 48 ]. The only implication of this, however, is that low average effect sizes of risk alleles in addiction necessitate larger study samples to construct polygenic scores that account for a large proportion of the known heritability.
However, a heritability of addiction of ~50% indicates that DNA sequence variation accounts for 50% of the risk for this condition. Once whole genome sequencing is readily available, it is likely that it will be possible to identify most of that DNA variation. For clinical purposes, those polygenic scores will of course not replace an understanding of the intricate web of biological and social factors that promote or prevent expression of addiction in an individual case; rather, they will add to it [ 49 ]. Meanwhile, however, genome-wide association studies in addiction have already provided important information. For instance, they have established that the genetic underpinnings of alcohol addiction only partially overlap with those for alcohol consumption, underscoring the genetic distinction between pathological and nonpathological drinking behaviors [ 50 ].
It thus seems that, rather than negating a rationale for a disease view of addiction, the important implication of the polygenic nature of addiction risk is a very different one. Genome-wide association studies of complex traits have largely confirmed the century old “infinitisemal model” in which Fisher reconciled Mendelian and polygenic traits [ 51 ]. A key implication of this model is that genetic susceptibility for a complex, polygenic trait is continuously distributed in the population. This may seem antithetical to a view of addiction as a distinct disease category, but the contradiction is only apparent, and one that has long been familiar to quantitative genetics. Viewing addiction susceptibility as a polygenic quantitative trait, and addiction as a disease category is entirely in line with Falconer’s theorem, according to which, in a given set of environmental conditions, a certain level of genetic susceptibility will determine a threshold above which disease will arise.
A brain disease? Then show me the brain lesion!
The notion of addiction as a brain disease is commonly criticized with the argument that a specific pathognomonic brain lesion has not been identified. Indeed, brain imaging findings in addiction (perhaps with the exception of extensive neurotoxic gray matter loss in advanced alcohol addiction) are nowhere near the level of specificity and sensitivity required of clinical diagnostic tests. However, this criticism neglects the fact that neuroimaging is not used to diagnose many neurologic and psychiatric disorders, including epilepsy, ALS, migraine, Huntington’s disease, bipolar disorder, or schizophrenia. Even among conditions where signs of disease can be detected using brain imaging, such as Alzheimer’s and Parkinson’s disease, a scan is best used in conjunction with clinical acumen when making the diagnosis. Thus, the requirement that addiction be detectable with a brain scan in order to be classified as a disease does not recognize the role of neuroimaging in the clinic.
For the foreseeable future, the main objective of imaging in addiction research is not to diagnose addiction, but rather to improve our understanding of mechanisms that underlie it. The hope is that mechanistic insights will help bring forward new treatments, by identifying candidate targets for them, by pointing to treatment-responsive biomarkers, or both [ 52 ]. Developing innovative treatments is essential to address unmet treatment needs, in particular in stimulant and cannabis addiction, where no approved medications are currently available. Although the task to develop novel treatments is challenging, promising candidates await evaluation [ 53 ]. A particular opportunity for imaging-based research is related to the complex and heterogeneous nature of addictive disorders. Imaging-based biomarkers hold the promise of allowing this complexity to be deconstructed into specific functional domains, as proposed by the RDoC initiative [ 54 ] and its application to addiction [ 55 , 56 ]. This can ultimately guide the development of personalized medicine strategies to addiction treatment.
Countless imaging studies have reported differences in brain structure and function between people with addictive disorders and those without them. Meta-analyses of structural data show that alcohol addiction is associated with gray matter losses in the prefrontal cortex, dorsal striatum, insula, and posterior cingulate cortex [ 57 ], and similar results have been obtained in stimulant-addicted individuals [ 58 ]. Meta-analysis of functional imaging studies has demonstrated common alterations in dorsal striatal, and frontal circuits engaged in reward and salience processing, habit formation, and executive control, across different substances and task-paradigms [ 59 ]. Molecular imaging studies have shown that large and fast increases in dopamine are associated with the reinforcing effects of drugs of abuse, but that after chronic drug use and during withdrawal, brain dopamine function is markedly decreased and that these decreases are associated with dysfunction of prefrontal regions [ 60 ]. Collectively, these findings have given rise to a widely held view of addiction as a disorder of fronto-striatal circuitry that mediates top-down regulation of behavior [ 61 ].
Critics reply that none of the brain imaging findings are sufficiently specific to distinguish between addiction and its absence, and that they are typically obtained in cross-sectional studies that can at best establish correlative rather than causal links. In this, they are largely right, and an updated version of a conceptualization of addiction as a brain disease needs to acknowledge this. Many of the structural brain findings reported are not specific for addiction, but rather shared across psychiatric disorders [ 62 ]. Also, for now, the most sophisticated tools of human brain imaging remain crude in face of complex neural circuit function. Importantly however, a vast literature from animal studies also documents functional changes in fronto-striatal circuits, as well their limbic and midbrain inputs, associated with addictive behaviors [ 63 , 64 , 65 , 66 , 67 , 68 ]. These are circuits akin to those identified by neuroimaging studies in humans, implicated in positive and negative emotions, learning processes and executive functions, altered function of which is thought to underlie addiction. These animal studies, by virtue of their cellular and molecular level resolution, and their ability to establish causality under experimental control, are therefore an important complement to human neuroimaging work.
Nevertheless, factors that seem remote from the activity of brain circuits, such as policies, substance availability and cost, as well as socioeconomic factors, also are critically important determinants of substance use. In this complex landscape, is the brain really a defensible focal point for research and treatment? The answer is “yes”. As powerfully articulated by Francis Crick [ 69 ], “You, your joys and your sorrows, your memories and your ambitions, your sense of personal identity and free will, are in fact no more than the behavior of a vast assembly of nerve cells and their associated molecules”. Social and interpersonal factors are critically important in addiction, but they can only exert their influences by impacting neural processes. They must be encoded as sensory data, represented together with memories of the past and predictions about the future, and combined with representations of interoceptive and other influences to provide inputs to the valuation machinery of the brain. Collectively, these inputs drive action selection and execution of behavior—say, to drink or not to drink, and then, within an episode, to stop drinking or keep drinking. Stating that the pathophysiology of addiction is largely about the brain does not ignore the role of other influences. It is just the opposite: it is attempting to understand how those important influences contribute to drug seeking and taking in the context of the brain, and vice versa.
But if the criticism is one of emphasis rather than of principle—i.e., too much brain, too little social and environmental factors – then neuroscientists need to acknowledge that they are in part guilty as charged. Brain-centric accounts of addiction have for a long time failed to pay enough attention to the inputs that social factors provide to neural processing behind drug seeking and taking [ 9 ]. This landscape is, however, rapidly changing. For instance, using animal models, scientists are finding that lack of social play early in life increases the motivation to take addictive substances in adulthood [ 70 ]. Others find that the opportunity to interact with a fellow rat is protective against addiction-like behaviors [ 71 ]. In humans, a relationship has been found between perceived social support, socioeconomic status, and the availability of dopamine D2 receptors [ 72 , 73 ], a biological marker of addiction vulnerability. Those findings in turn provided translation of data from nonhuman primates, which showed that D2 receptor availability can be altered by changes in social hierarchy, and that these changes are associated with the motivation to obtain cocaine [ 74 ].
Epidemiologically, it is well established that social determinants of health, including major racial and ethnic disparities, play a significant role in the risk for addiction [ 75 , 76 ]. Contemporary neuroscience is illuminating how those factors penetrate the brain [ 77 ] and, in some cases, reveals pathways of resilience [ 78 ] and how evidence-based prevention can interrupt those adverse consequences [ 79 , 80 ]. In other words, from our perspective, viewing addiction as a brain disease in no way negates the importance of social determinants of health or societal inequalities as critical influences. In fact, as shown by the studies correlating dopamine receptors with social experience, imaging is capable of capturing the impact of the social environment on brain function. This provides a platform for understanding how those influences become embedded in the biology of the brain, which provides a biological roadmap for prevention and intervention.
We therefore argue that a contemporary view of addiction as a brain disease does not deny the influence of social, environmental, developmental, or socioeconomic processes, but rather proposes that the brain is the underlying material substrate upon which those factors impinge and from which the responses originate. Because of this, neurobiology is a critical level of analysis for understanding addiction, although certainly not the only one. It is recognized throughout modern medicine that a host of biological and non-biological factors give rise to disease; understanding the biological pathophysiology is critical for understanding etiology and informing treatment.
Is a view of addiction as a brain disease deterministic?
A common criticism of the notion that addiction is a brain disease is that it is reductionist and in the end therefore deterministic [ 81 , 82 ]. This is a fundamental misrepresentation. As indicated above, viewing addiction as a brain disease simply states that neurobiology is an undeniable component of addiction. A reason for deterministic interpretations may be that modern neuroscience emphasizes an understanding of proximal causality within research designs (e.g., whether an observed link between biological processes is mediated by a specific mechanism). That does not in any way reflect a superordinate assumption that neuroscience will achieve global causality. On the contrary, since we realize that addiction involves interactions between biology, environment and society, ultimate (complete) prediction of behavior based on an understanding of neural processes alone is neither expected, nor a goal.
A fairer representation of a contemporary neuroscience view is that it believes insights from neurobiology allow useful probabilistic models to be developed of the inherently stochastic processes involved in behavior [see [ 83 ] for an elegant recent example]. Changes in brain function and structure in addiction exert a powerful probabilistic influence over a person’s behavior, but one that is highly multifactorial, variable, and thus stochastic. Philosophically, this is best understood as being aligned with indeterminism, a perspective that has a deep history in philosophy and psychology [ 84 ]. In modern neuroscience, it refers to the position that the dynamic complexity of the brain, given the probabilistic threshold-gated nature of its biology (e.g., action potential depolarization, ion channel gating), means that behavior cannot be definitively predicted in any individual instance [ 85 , 86 ].
Driven by compulsion, or free to choose?
A major criticism of the brain disease view of addiction, and one that is related to the issue of determinism vs indeterminism, centers around the term “compulsivity” [ 6 , 87 , 88 , 89 , 90 ] and the different meanings it is given. Prominent addiction theories state that addiction is characterized by a transition from controlled to “compulsive” drug seeking and taking [ 91 , 92 , 93 , 94 , 95 ], but allocate somewhat different meanings to “compulsivity”. By some accounts, compulsive substance use is habitual and insensitive to its outcomes [ 92 , 94 , 96 ]. Others refer to compulsive use as a result of increasing incentive value of drug associated cues [ 97 ], while others view it as driven by a recruitment of systems that encode negative affective states [ 95 , 98 ].
The prototype for compulsive behavior is provided by obsessive-compulsive disorder (OCD), where compulsion refers to repeatedly and stereotypically carrying out actions that in themselves may be meaningful, but lose their purpose and become harmful when performed in excess, such as persistent handwashing until skin injuries result. Crucially, this happens despite a conscious desire to do otherwise. Attempts to resist these compulsions result in increasing and ultimately intractable anxiety [ 99 ]. This is in important ways different from the meaning of compulsivity as commonly used in addiction theories. In the addiction field, compulsive drug use typically refers to inflexible, drug-centered behavior in which substance use is insensitive to adverse consequences [ 100 ]. Although this phenomenon is not necessarily present in every patient, it reflects important symptoms of clinical addiction, and is captured by several DSM-5 criteria for SUD [ 101 ]. Examples are needle-sharing despite knowledge of a risk to contract HIV or Hepatitis C, drinking despite a knowledge of having liver cirrhosis, but also the neglect of social and professional activities that previously were more important than substance use. While these behaviors do show similarities with the compulsions of OCD, there are also important differences. For example, “compulsive” substance use is not necessarily accompanied by a conscious desire to withhold the behavior, nor is addictive behavior consistently impervious to change.
Critics question the existence of compulsivity in addiction altogether [ 5 , 6 , 7 , 89 ], typically using a literal interpretation, i.e., that a person who uses alcohol or drugs simply can not do otherwise. Were that the intended meaning in theories of addiction—which it is not—it would clearly be invalidated by observations of preserved sensitivity of behavior to contingencies in addiction. Indeed, substance use is influenced both by the availability of alternative reinforcers, and the state of the organism. The roots of this insight date back to 1940, when Spragg found that chimpanzees would normally choose a banana over morphine. However, when physically dependent and in a state of withdrawal, their choice preference would reverse [ 102 ]. The critical role of alternative reinforcers was elegantly brought into modern neuroscience by Ahmed et al., who showed that rats extensively trained to self-administer cocaine would readily forego the drug if offered a sweet solution as an alternative [ 103 ]. This was later also found to be the case for heroin [ 103 ], methamphetamine [ 104 ] and alcohol [ 105 ]. Early residential laboratory studies on alcohol use disorder indeed revealed orderly operant control over alcohol consumption [ 106 ]. Furthermore, efficacy of treatment approaches such as contingency management, which provides systematic incentives for abstinence [ 107 ], supports the notion that behavioral choices in patients with addictions remain sensitive to reward contingencies.
Evidence that a capacity for choosing advantageously is preserved in addiction provides a valid argument against a narrow concept of “compulsivity” as rigid, immutable behavior that applies to all patients. It does not, however, provide an argument against addiction as a brain disease. If not from the brain, from where do the healthy and unhealthy choices people make originate? The critical question is whether addictive behaviors—for the most part—result from healthy brains responding normally to externally determined contingencies; or rather from a pathology of brain circuits that, through probabilistic shifts, promotes the likelihood of maladaptive choices even when reward contingencies are within a normal range. To resolve this question, it is critical to understand that the ability to choose advantageously is not an all-or-nothing phenomenon, but rather is about probabilities and their shifts, multiple faculties within human cognition, and their interaction. Yes, it is clear that most people whom we would consider to suffer from addiction remain able to choose advantageously much, if not most, of the time. However, it is also clear that the probability of them choosing to their own disadvantage, even when more salutary options are available and sometimes at the expense of losing their life, is systematically and quantifiably increased. There is a freedom of choice, yet there is a shift of prevailing choices that nevertheless can kill.
Synthesized, the notion of addiction as a disease of choice and addiction as a brain disease can be understood as two sides of the same coin. Both of these perspectives are informative, and they are complementary. Viewed this way, addiction is a brain disease in which a person’s choice faculties become profoundly compromised. To articulate it more specifically, embedded in and principally executed by the central nervous system, addiction can be understood as a disorder of choice preferences, preferences that overvalue immediate reinforcement (both positive and negative), preferences for drug-reinforcement in spite of costs, and preferences that are unstable ( “I’ll never drink like that again;” “this will be my last cigarette” ), prone to reversals in the form of lapses and relapse. From a contemporary neuroscience perspective, pre-existing vulnerabilities and persistent drug use lead to a vicious circle of substantive disruptions in the brain that impair and undermine choice capacities for adaptive behavior, but do not annihilate them. Evidence of generally intact decision making does not fundamentally contradict addiction as a brain disease.
Conclusions
The present paper is a response to the increasing number of criticisms of the view that addiction is a chronic relapsing brain disease. In many cases, we show that those criticisms target tenets that are neither needed nor held by a contemporary version of this view. Common themes are that viewing addiction as a brain disease is criticized for being both too narrow (addiction is only a brain disease; no other perspectives or factors are important) or too far reaching (it purports to discover the final causes of addiction). With regard to disease course, we propose that viewing addiction as a chronic relapsing disease is appropriate for some populations, and much less so for others, simply necessitating better ways of delineating the populations being discussed. We argue that when considering addiction as a disease, the lens of neurobiology is valuable to use. It is not the only lens, and it does not have supremacy over other scientific approaches. We agree that critiques of neuroscience are warranted [ 108 ] and that critical thinking is essential to avoid deterministic language and scientific overreach.
Beyond making the case for a view of addiction as a brain disease, perhaps the more important question is when a specific level of analysis is most useful. For understanding the biology of addiction and designing biological interventions, a neurobiological view is almost certainly the most appropriate level of analysis, in particular when informed by an understanding of the behavioral manifestations. In contrast, for understanding the psychology of addiction and designing psychological interventions, behavioral science is the natural realm, but one that can often benefit from an understanding of the underlying neurobiology. For designing policies, such as taxation and regulation of access, economics and public administration provide the most pertinent perspectives, but these also benefit from biological and behavioral science insights.
Finally, we argue that progress would come from integration of these scientific perspectives and traditions. E.O. Wilson has argued more broadly for greater consilience [ 109 ], unity of knowledge, in science. We believe that addiction is among the areas where consilience is most needed. A plurality of disciplines brings important and trenchant insights to bear on this condition; it is the exclusive remit of no single perspective or field. Addiction inherently and necessarily requires multidisciplinary examination. Moreover, those who suffer from addiction will benefit most from the application of the full armamentarium of scientific perspectives.
Funding and disclosures
Supported by the Swedish Research Council grants 2013-07434, 2019-01138 (MH); Netherlands Organisation for Health Research and Development (ZonMw) under project number 912.14.093 (LJMJV); NIDA and NIAAA intramural research programs (LL; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health); the Peter Boris Chair in Addictions Research, Homewood Research Institute, and the National Institute on Alcohol Abuse and Alcoholism grants AA025911, AA024930, AA025849, AA027679 (JM; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health).
MH has received consulting fees, research support or other compensation from Indivior, Camurus, BrainsWay, Aelis Farma, and Janssen Pharmaceuticals. JM is a Principal and Senior Scientist at BEAM Diagnostics, Inc. DM, JR, LL, and LJMJV declare no conflict of interest.
Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278:45–7.
Article CAS PubMed Google Scholar
McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–95.
Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol Alcohol. 2011;46:105–12.
Heyman GM. Addiction and choice: theory and new data. Front Psychiatry. 2013;4:31.
Article PubMed PubMed Central Google Scholar
Heather N, Best D, Kawalek A, Field M, Lewis M, Rotgers F, et al. Challenging the brain disease model of addiction: European launch of the addiction theory network. Addict Res Theory. 2018;26:249–55.
Article Google Scholar
Pickard H, Ahmed SH, Foddy B. Alternative models of addiction. Front Psychiatr.y 2015;6:20.
Google Scholar
Hall W, Carter A, Forlini C. The brain disease model of addiction: is it supported by the evidence and has it delivered on its promises? Lancet Psychiatr. 2015;2:105–10.
Hart CL. Viewing addiction as a brain disease promotes social injustice. Nat Hum Behav. 2017;1:0055.
Heilig M, Epstein DH, Nader MA, Shaham Y. Time to connect: bringing social context into addiction neuroscience. Nat Rev Neurosc.i 2016;17:592–9.
Article CAS Google Scholar
Jellinek EM. The disease concept of alcoholism. Hillhouse Press on behalf of the Christopher J. Smithers Foundation: New Haven, CT; 1960.
Stevenson A. Oxford dictionary of English. 3 ed. New York, NY: Oxford University Press; 2010.
Fan J, May SJ, Zhou Y, Barrett-Connor E. Bimodality of 2-h plasma glucose distributions in whites: the Rancho Bernardo study. Diabetes Care 2005;28:1451–6.
King AC, Vena A, Hasin D, De Wit D, O’Connor CJ, Cao D. Subjective responses to alcohol in the development and maintenance of alcohol use disorder (AUD). Am J Psychiatry. 2021. https://doi.org/10.1176/appi.ajp.2020.20030247 .
GBD. 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5:987–1012.
Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. Br Med J. 1976;1:1058–61.
Article CAS PubMed PubMed Central Google Scholar
Epstein DH, Heilig M, Shaham Y. Science-based actions can help address the opioid crisis. Trends Pharm Sci. 2018;39:911–16.
Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abus Treat. 2005;28:321–9.
Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Datab System Rev. 2013;5:CD009329.
Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings a systematic review and meta-analysis. JAMA. 2014;311:1889–900.
Article PubMed CAS Google Scholar
Mark TL, Kranzler HR, Song X. Understanding US addiction physicians’ low rate of naltrexone prescription. Drug Alcohol Depend. 2003;71:219–28.
Article PubMed Google Scholar
Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376:1558–65.
Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12:274–83.
Laing RD. The divided self; a study of sanity and madness. London: Tavistock Publications; 1960.
Foucault M, Khalfa J. History of madness. New York: Routledge; 2006.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL. et al.Comorbidity of mental disorders with alcohol and other drug abuse. Results Epidemiologic Catchment Area (ECA) study.JAMA. 1990;264:2511–8.
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–16.
Lopez-Quintero C, Hasin DS, de Los Cobos JP, Pines A, Wang S, Grant BF, et al. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011;106:657–69.
Humphreys K. Addiction treatment professionals are not the gatekeepers of recovery. Subst Use Misuse. 2015;50:1024–7.
Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86:214–21.
Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72.
Culverhouse R, Bucholz KK, Crowe RR, Hesselbrock V, Nurnberger JI Jr, Porjesz B, et al. Long-term stability of alcohol and other substance dependence diagnoses and habitual smoking: an evaluation after 5 years. Arch Gen Psychiatry. 2005;62:753–60.
Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42.
Skolnick P. The opioid epidemic: crisis and solutions. Annu Rev Pharm Toxicol. 2018;58:143–59.
Hser YI, Evans E, Grella C, Ling W, Anglin D. Long-term course of opioid addiction. Harv Rev Psychiatry. 2015;23:76–89.
Mathers BM, Degenhardt L, Bucello C, Lemon J, Wiessing L, Hickman M. Mortality among people who inject drugs: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:102–23.
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–66.
Article PubMed PubMed Central CAS Google Scholar
Lee MR, Sher KJ. “Maturing Out” of binge and problem drinking. Alcohol Res: Curr Rev. 2018;39:31–42.
Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–92.
Berridge V. The rise, fall, and revival of recovery in drug policy. Lancet. 2012;379:22–23.
Parvaz MA, Moeller SJ, d’Oleire Uquillas F, Pflumm A, Maloney T, Alia-Klein N, et al. Prefrontal gray matter volume recovery in treatment-seeking cocaine-addicted individuals: a longitudinal study. Addict Biol. 2017;22:1391–401.
Korponay C, Kosson DS, Decety J, Kiehl KA, Koenigs M. Brain volume correlates with duration of abstinence from substance abuse in a region-specific and substance-specific manner. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2:626–35.
PubMed PubMed Central Google Scholar
Janes AC, Datko M, Roy A, Barton B, Druker S, Neal C, et al. Quitting starts in the brain: a randomized controlled trial of app-based mindfulness shows decreases in neural responses to smoking cues that predict reductions in smoking. Neuropsychopharmacology. 2019;44:1631–38.
Humphreys K, Bickel WK. Toward a neuroscience of long-term recovery from addiction. JAMA Psychiatry. 2018;75:875–76.
Verhulst B, Neale MC, Kendler KS. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychol Med. 2015;45:1061–72.
Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nat Rev Genet. 2005;6:521–32.
Kendler KS, Jacobson KC, Prescott CA, Neale MC. Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. AJ Psychiatry. 2003;160:687–95.
Schizophrenia Working Group of the Psychiatric Genomics C. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7.
Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet. 2018;50:668–81.
Wray NR, Lin T, Austin J, McGrath JJ, Hickie IB, Murray GK, et al. From basic science to clinical application of polygenic risk scores: a primer. JAMA Psychiatry. 2021;78:101–9.
Walters RK, Polimanti R, Johnson EC, McClintick JN, Adams MJ, Adkins AE, et al. Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders. Nat Neurosci. 2018;21:1656–69.
Visscher PM, Wray NR. Concepts and misconceptions about the polygenic additive model applied to disease. Hum Hered. 2015;80:165–70.
Heilig M, Leggio L. What the alcohol doctor ordered from the neuroscientist: theragnostic biomarkers for personalized treatments. Prog Brain Res. 2016;224:401–18.
Rasmussen K, White DA, Acri JB. NIDA’s medication development priorities in response to the Opioid Crisis: ten most wanted. Neuropsychopharmacology. 2019;44:657–59.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. AJ Psychiatry. 2010;167:748–51.
Kwako LE, Schwandt ML, Ramchandani VA, Diazgranados N, Koob GF, Volkow ND, et al. Neurofunctional domains derived from deep behavioral phenotyping in alcohol use disorder. AJ Psychiatry. 2019;176:744–53.
Kwako LE, Bickel WK, Goldman D. Addiction biomarkers: dimensional approaches to understanding addiction. Trends Mol Med. 2018;24:121–28.
Xiao P, Dai Z, Zhong J, Zhu Y, Shi H, Pan P. Regional gray matter deficits in alcohol dependence: a meta-analysis of voxel-based morphometry studies. Drug Alcohol Depend. 2015;153:22–8.
Ersche KD, Williams GB, Robbins TW, Bullmore ET. Meta-analysis of structural brain abnormalities associated with stimulant drug dependence and neuroimaging of addiction vulnerability and resilience. Curr Opin Neurobiol. 2013;23:615–24.
Klugah-Brown B, Di X, Zweerings J, Mathiak K, Becker B, Biswal B. Common and separable neural alterations in substance use disorders: a coordinate-based meta-analyses of functional neuroimaging studies in humans. Hum Brain Mapp. 2020;41:4459–77.
Volkow ND, Fowler JS, Wang GJ. The addicted human brain: insights from imaging studies. J Clin Investig. 2003;111:1444–51.
Goldstein RZ, Volkow ND. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci. 2011;12:652–69.
Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry. 2015;72:305–15.
Scofield MD, Heinsbroek JA, Gipson CD, Kupchik YM, Spencer S, Smith AC, et al. The nucleus accumbens: mechanisms of addiction across drug classes reflect the importance of glutamate homeostasis. Pharm Rev. 2016;68:816–71.
Korpi ER, den Hollander B, Farooq U, Vashchinkina E, Rajkumar R, Nutt DJ, et al. Mechanisms of action and persistent neuroplasticity by drugs of abuse. Pharm Rev. 2015;67:872–1004.
Luscher C, Malenka RC. Drug-evoked synaptic plasticity in addiction: from molecular changes to circuit remodeling. Neuron. 2011;69:650–63.
Everitt BJ. Neural and psychological mechanisms underlying compulsive drug seeking habits and drug memories–indications for novel treatments of addiction. Eur J Neurosci. 2014;40:2163–82.
Lesscher HM, Vanderschuren LJ. Compulsive drug use and its neural substrates. Rev Neurosci. 2012;23:731–45.
Cruz FC, Koya E, Guez-Barber DH, Bossert JM, Lupica CR, Shaham Y, et al. New technologies for examining the role of neuronal ensembles in drug addiction and fear. Nat Rev Neurosci. 2013;14:743–54.
Crick F. The astonishing hypothesis: the scientific search for the soul. Scribner; Maxwell Macmillan International: New York, NY; 1994.
Vanderschuren LJ, Achterberg EJ, Trezza V. The neurobiology of social play and its rewarding value in rats. Neurosci Biobehav Rev. 2016;70:86–105.
Venniro M, Zhang M, Caprioli D, Hoots JK, Golden SA, Heins C, et al. Volitional social interaction prevents drug addiction in rat models. Nat Neurosci. 2018;21:1520–29.
Martinez D, Orlowska D, Narendran R, Slifstein M, Liu F, Kumar D, et al. Dopamine type 2/3 receptor availability in the striatum and social status in human volunteers. Biol Psychiatry. 2010;67:275–8.
Wiers CE, Shokri-Kojori E, Cabrera E, Cunningham S, Wong C, Tomasi D, et al. Socioeconomic status is associated with striatal dopamine D2/D3 receptors in healthy volunteers but not in cocaine abusers. Neurosci Lett. 2016;617:27–31.
Morgan D, Grant KA, Gage HD, Mach RH, Kaplan JR, Prioleau O, et al. Social dominance in monkeys: dopamine D2 receptors and cocaine self-administration. Nat Neurosci. 2002;5:169–74.
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e356–e66.
Gilbert PA, Zemore SE. Discrimination and drinking: a systematic review of the evidence. Soc Sci Med 2016;161:178–94.
Oshri A, Gray JC, Owens MM, Liu S, Duprey EB, Sweet LH, et al. Adverse childhood experiences and amygdalar reduction: high-resolution segmentation reveals associations with subnuclei and psychiatric outcomes. Child Maltreat. 2019;24:400–10.
Holmes CJ, Barton AW, MacKillop J, Galván A, Owens MM, McCormick MJ, et al. Parenting and salience network connectivity among African Americans: a protective pathway for health-risk behaviors. Biol Psychiatry. 2018;84:365–71.
Brody GH, Gray JC, Yu T, Barton AW, Beach SR, Galván A, et al. Protective prevention effects on the association of poverty with brain development. JAMA Pediatr. 2017;171:46–52.
Hanson JL, Gillmore AD, Yu T, Holmes CJ, Hallowell ES, Barton AW, et al. A family focused intervention influences hippocampal-prefrontal connectivity through gains in self-regulation. Child Dev. 2019;90:1389–401.
Borsboom D, Cramer A, Kalis A. Brain disorders? Not really… why network structures block reductionism in psychopathology research. Behav Brain Sci. 2018;42:1–54.
Field M, Heather N, Wiers RW. Indeed, not really a brain disorder: Implications for reductionist accounts of addiction. Behav Brain Sci. 2019;42:e9.
Pascoli V, Hiver A, Van Zessen R, Loureiro M, Achargui R, Harada M, et al. Stochastic synaptic plasticity underlying compulsion in a model of addiction. Nature. 2018;564:366–71.
James W. The dilemma of determinism. Whitefish, MT: Kessinger Publishing; 2005.
Gessell B. Indeterminism in the brain. Biol Philos. 2017;32:1205–23.
Jedlicka P. Revisiting the quantum brain hypothesis: toward quantum (neuro)biology? Front Mol Neurosci. 2017;10:366.
Heyman GM. Addiction: a disorder of choice. Cambridge, MA: Harvard University Press; 2010.
Heather NQ. Is addiction a brain disease or a moral failing? A: Neither. Neuroethics. 2017;10:115–24.
Ahmed SH, Lenoir M, Guillem K. Neurobiology of addiction versus drug use driven by lack of choice. Curr Opin Neurobiol. 2013;23:581–7.
Hogarth L, Lam-Cassettari C, Pacitti H, Currah T, Mahlberg J, Hartley L, et al. Intact goal-directed control in treatment-seeking drug users indexed by outcome-devaluation and Pavlovian to instrumental transfer: critique of habit theory. Eur J Neurosci. 2019;50:2513–25.
Mathis V, Kenny PJ. From controlled to compulsive drug-taking: the role of the habenula in addiction. Neurosci Biobehav Rev. 2019;106:102–11.
Luscher C, Robbins TW, Everitt BJ. The transition to compulsion in addiction. Nat Rev Neurosci. 2020;21:247–63.
Robinson TE, Berridge KC. Addiction. Annu Rev Psychol. 2003;54:25–53.
Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8:1481–89.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38.
Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychol Rev. 1990;97:147–68.
Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Rev. 1993;18:247–91.
Koob GF, Le Moal M. Plasticity of reward neurocircuitry and the ‘dark side’ of drug addiction. Nat Neurosci. 2005;8:1442–4.
Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive-compulsive disorder. Nat Rev Dis Prim. 2019;5:52.
Vanderschuren LJ, Everitt BJ. Drug seeking becomes compulsive after prolonged cocaine self-administration. Science 2004;305:1017–9.
American_Psychiatric_Association. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc; 2013.
Book Google Scholar
Spragg SDS. Morphine addiction in chimpanzees. Comp Psychol Monogr. 1940;15:132–32.
Lenoir M, Cantin L, Vanhille N, Serre F, Ahmed SH. Extended heroin access increases heroin choices over a potent nondrug alternative. Neuropsychopharmacology. 2013;38:1209–20.
Caprioli D, Venniro M, Zeric T, Li X, Adhikary S, Madangopal R, et al. Effect of the novel positive allosteric modulator of metabotropic glutamate receptor 2 AZD8529 on incubation of methamphetamine craving after prolonged voluntary abstinence in a rat model. Biol Psychiatry. 2015;78:463–73.
Augier E, Barbier E, Dulman RS, Licheri V, Augier G, Domi E, et al. A molecular mechanism for choosing alcohol over an alternative reward. Science. 2018;360:1321–26.
Bigelow GE. An operant behavioral perspective on alcohol abuse and dependence. In: Heather N, Peters TJ, Stockwell T, editors. International handbook of alcohol dependence and problems. John Wiley & Sons Ltd; 2001. p. 299–315.
Higgins ST, Heil SH, Lussier JP. Clinical implications of reinforcement as a determinant of substance use disorders. Annu Rev Psychol. 2004;55:431–61.
Satel S, Lilienfeld SO. Brainwashed: the seductive appeal of mindless neuroscience. New York, NY: Basic Books; 2015.
Wilson EO. Consilience: the unity of knowledge. New York, NY: Vintage Books; 1999.
Saunders JB, Degenhardt L, Reed GM, Poznyak V. Alcohol use disorders in ICD-11: past, present, and future. Alcohol Clin Exp Res 2019;43:1617–31.
Organization. WH. ICD-11 for mortality and morbidity statistics. 2018. https://icd.who.int/browse11/l-m/en . Accessed 21 Oct 2020.
Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst Abus. 2007;28:7–30.
Witkiewitz K, Hallgren KA, Kranzler HR, Mann KF, Hasin DS, Falk DE, et al. Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the World Health Organization risk drinking levels. Alcohol Clin Exp Res 2017;41:179–86.
Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. AJ Psychiatry. 2013;170:834–51.
Rosenthal RJ, Faris SB. The etymology and early history of ‘addiction’. Addict Res Theory. 2019;27:437–49.
Martin CS, Steinley DL, Verges A, Sher KJ. The proposed 2/11 symptom algorithm for DSM-5 substance-use disorders is too lenient. Psychol Med. 2011;41:2008–10.
Degenhardt L, Bharat C, Bruno R, Glantz MD, Sampson NA, Lago L, et al. Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: analysis of data from the WHO’s World Mental Health Surveys. Addiction. 2019;114:534–52.
PubMed Google Scholar
Lago L, Bruno R, Degenhardt L. Concordance of ICD-11 and DSM-5 definitions of alcohol and cannabis use disorders: a population survey. Lancet Psychiatry. 2016;3:673–84.
Lundin A, Hallgren M, Forsman M, Forsell Y. Comparison of DSM-5 classifications of alcohol use disorders with those of DSM-IV, DSM-III-R, and ICD-10 in a general population sample in Sweden. J Stud Alcohol Drugs. 2015;76:773–80.
Kwako LE, Momenan R, Litten RZ, Koob GF, Goldman D. Addictions neuroclinical assessment: a neuroscience-based framework for addictive disorders. Biol Psychiatry. 2016;80:179–89.
Rehm J, Heilig M, Gual A. ICD-11 for alcohol use disorders: not a convincing answer to the challenges. Alcohol Clin Exp Res. 2019;43:2296–300.
Download references
Acknowledgements
The authors want to acknowledge comments by Drs. David Epstein, Kenneth Kendler and Naomi Wray.
Author information
Authors and affiliations.
Center for Social and Affective Neuroscience, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Markus Heilig
Peter Boris Centre for Addictions Research, McMaster University and St. Joseph’s Healthcare Hamilton, Hamilton, ON, Canada
- James MacKillop
Homewood Research Institute, Guelph, ON, Canada
New York State Psychiatric Institute and Columbia University Irving Medical Center, New York, NY, USA
Diana Martinez
Institute for Mental Health Policy Research & Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health (CAMH), Toronto, ON, Canada
Jürgen Rehm
Dalla Lana School of Public Health and Department of Psychiatry, University of Toronto (UofT), Toronto, ON, Canada
Klinische Psychologie & Psychotherapie, Technische Universität Dresden, Dresden, Germany
Department of International Health Projects, Institute for Leadership and Health Management, I.M. Sechenov First Moscow State Medical University, Moscow, Russia
Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, Translational Addiction Medicine Branch, National Institute on Drug Abuse Intramural Research Program and National Institute on Alcohol Abuse and Alcoholism Division of Intramural Clinical and Biological Research, National Institutes of Health, Baltimore and Bethesda, MD, USA
Lorenzo Leggio
Department of Population Health Sciences, Unit Animals in Science and Society, Faculty of Veterinary Medicine, Utrecht University, Utrecht, the Netherlands
Louk J. M. J. Vanderschuren
You can also search for this author in PubMed Google Scholar
Contributions
All authors jointly drafted the paper.
Corresponding author
Correspondence to Markus Heilig .
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Heilig, M., MacKillop, J., Martinez, D. et al. Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacol. 46 , 1715–1723 (2021). https://doi.org/10.1038/s41386-020-00950-y
Download citation
Received : 10 November 2020
Revised : 11 December 2020
Accepted : 14 December 2020
Published : 22 February 2021
Issue Date : September 2021
DOI : https://doi.org/10.1038/s41386-020-00950-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The importance of choice and agency in animal models of addiction.
- Serge H. Ahmed
Journal of Neural Transmission (2024)
Neuromarkers in addiction: definitions, development strategies, and recent advances
- Nicholas R. Harp
- Tor D. Wager
What Do We Know About Informal Caregiving in the Field of Addiction?: A Scoping Review
- Mélissa Côté
- Eve-Emmanuelle Morency
- Nadine Blanchette-Martin
International Journal of Mental Health and Addiction (2024)
Persistent impacts of smoking on resting-state EEG in male chronic smokers and past-smokers with 20 years of abstinence
- Yoonji Jeon
- Dongil Chung
Scientific Reports (2023)
A contextualized reinforcer pathology approach to addiction
- Samuel F. Acuff
- James G. Murphy
Nature Reviews Psychology (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Heroin Research Report Overview
Heroin is a highly addictive opioid drug, and its use has repercussions that extend far beyond the individual user. The medical and social consequences of drug use—such as hepatitis, HIV/AIDS, fetal effects, crime, violence, and disruptions in family, workplace, and educational environments—have a devastating impact on society and cost billions of dollars each year.
Although heroin use in the general population is rather low, the numbers of people starting to use heroin have been steadily rising since 2007. 1 This may be due in part to a shift from misuse of prescription pain relievers to heroin as a readily available, cheaper alternative 2-5 and the misperception that pure heroin is safer than less pure forms because it does not need to be injected.
Like many other chronic diseases, substance use disorders can be treated. Medications are available to treat heroin use disorder while reducing drug cravings and withdrawal symptoms, thus improving the odds of achieving abstinence. There are now a variety of medications that can be tailored to a person’s recovery needs while taking into account co-occurring health conditions. Medication combined with behavioral therapy is particularly effective, offering hope to individuals who suffer from substance use disorders and for those around them.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Research Council (US) and Institute of Medicine (US) Committee on Drug Use in the Workplace; Normand J, Lempert RO, O'Brien CP, editors. Under the Influence? Drugs and the American Work Force. Washington (DC): National Academies Press (US); 1994.

Under the Influence? Drugs and the American Work Force.
- Hardcopy Version at National Academies Press
Summary: Conclusions and Recommendations
This report is concerned with the implications of drug use for workplace safety and productivity. It examines the prevalence of alcohol and other drug use by the U.S. work force, the impact of such use on job-related behavior, and the effectiveness of workplace drug intervention programs. This emphasis on workplace productivity rather than social consequences affects the purpose, methods, and evaluation criteria used in this report, just as it often affects researchers investigating these issues.
- The Committee's Charge
The committee was charged with: (1) analyzing the available research knowledge on the prevalence and etiology of drug consumption by the work force; (2) studying the impact of drug behavior on work performance, productivity, safety, and health; and (3) evaluating the effectiveness, costs, and benefits of organizational drug intervention programs at the work site.
- Definition Of Terms
Three key terms in the committee's charge require clarification, because their definitions have a significant bearing on the committee's interpretation of the scope of its work.
Drug : The committee defines the term drug to include any psychotropic substance that, if consumed, will affect a person's psychological status or physiological state or behavior. We consider only substances whose use is problematic enough to represent a meaningful threat to the welfare of individual users or others and whose prevalence is high enough among the work force to have the potential to affect business productivity. The report focuses its attention on general drug class categories, includes alcohol within its scope, and briefly addresses issues surrounding tobacco.
Use, Abuse, and Dependence : Drug taking can be classified into one of three categories: (1) use, (2) abuse, and (3) dependence. Use is defined as the limited, controlled consumption of a drug (in terms of frequency and quantity) without significant toxic, adverse physical, or psychological consequences to the user (Glantz, 1992). Regular use of prescribed medications, legal drugs such as nicotine, caffeine, and alcohol, and certain illegal drugs can lead to physiological dependence. This simply means that the abrupt cessation of drug taking produces a set of symptoms called a withdrawal syndrome. The presence of physiological dependence does not necessarily imply abuse or dependence in the behavioral sense. Abuse is defined as a level of drug use that typically leads to adverse consequences (physical or psychological). Drug use at this level is not necessarily associated with any particular frequency but is associated with use in quantities sufficient to result in some toxicity to the user, and the patterns of use usually have some characteristics of psychopathological behavior. Dependence in the behavioral sense is defined as a level of drug use that has significant adverse physical and psychological consequences. This level of use is characterized by the consumption of toxic doses of the drug that impair the user's ability to function and is also characterized by a compulsive desire to use a drug repeatedly.
Work Force : Although one might confine the question of alcohol and other drug use by the work force to the use of those substances by employees while at work, the committee believes its charge requires a more encompassing definition. By work force we mean to include any active member of the labor force, including those seeking or available for employment. Work force alcohol and other drug use is the use of those substances by any work force member, whether the use occurs on or off the job, so long as the use has potential workplace effects. Consequently, issues concerning hangover or residual effects of alcohol and other drugs taken when not at work, as well as correlates of individual alcohol and other drug use and work force participation, are all relevant.
- Conclusions And Recommendations
Part I: Scope of Alcohol and Other Drug Use
Chapter 2 etiology of alcohol and other drug use: an overview of potential causes.
- The most vulnerable age and primary risk factors associated with drug use initiation typically precede an individual's entry into the work force. This fact has important implications for work-related prevention interventions designed to prevent the onset of drug use. This means that workplace interventions may have only limited effects on preventing initiation into most categories of drug use.
- Most alcohol and other drug users do not develop patterns of clinically defined abuse or dependence. The progression from use to abuse and dependence varies with drug type as well as with factors that are specific to individuals and their environments. It is not possible, however, to predict with great accuracy which alcohol and other drug users will become abusers or will eventually need treatment.
- If use and abuse have different causes, it follows that they are likely to benefit from different types of interventions, so it is important to further explore the hypothesis that any type of drug use at the work site in fact reflects abuse.
- Among illicit drug users, polydrug use, most often including the use of alcohol and tobacco, is the norm rather than the exception.
Recommendation: In evaluating the impact of alcohol and other drug use on behavior, specific attention should be paid to the actions of drugs in combination.
• Based on the sparse empirical evidence accumulated to date, alcohol and other drug use by the work force appears to be more a function of the personal qualities of individuals than of their work environments. However, most studies of why workers use alcohol and other drugs have serious methodological flaws. Hence, the work environment cannot be ruled out as a contributing or interactive factor in generating use among workers or protecting them from it.
Recommendation: Research is still needed to sort out the relative impact of the work environment and individual traits on workers' alcohol and other drug use. This research should test realistic theories involving such potential critical variables as drug availability, local norms, work stress and attending to such complexities as interaction effects and reverse causation.
Chapter 3 Epidemiological Evidence: The Dimensions of the Problem
Data sources ranging from self-report questionnaires to urinalysis testing to emergency room visits provide important insights about the use of alcohol and other drugs among members of the general population and the work force. Taken together, the data indicate that, since the late 1970s:
The prevalence of illicit drug use among members of the general population and the work force has been decreasing, but continues to affect a sizable proportion of the population, especially young adults.
Illicit drug use may be decreasing among occasional users, but it may be stable or even increasing among hard-core users who are generally not well represented in surveys.
Heavy alcohol use has been relatively stable over the past several years; rates of heavy drinking have been notably high among young adult men, especially those in the military and among workers in such industries as construction, transportation, and wholesale goods.
Cigarette smoking has been declining during the past decade for those 18 and older, but has been relatively stable for youths ages 12 to 17.
Illicit drug use is more common among unemployed than employed persons, and weekly alcohol use is highest among young employed workers.
Illicit drug use is relatively high among male workers in certain industries such as construction and relatively low among professionals.
- Given these long-term trends, we must be cautious in attributing short-term changes in alcohol and other drug use in either society or in the work force to specific national efforts to stem the use of drugs.
- Few epidemiological studies are targeted directly at the work force, leaving researchers to rely on data sources designed for other uses.
Recommendation: More focused epidemiological studies, including longitudinal studies, are needed to assess the magnitude and severity of alcohol and other drug use among the work force. As a first step, the National Household Surveys on Drug Abuse should be modified to provide specific information about job characteristics, job-related behaviors, and alcohol and other drug use at work. Ultimately a national panel survey devoted to this topic should be instituted. In addition, other studies are needed that provide better information about: (1) employment patterns among persons who use alcohol and other drugs; (2) patterns of alcohol and other drug use among workers; (3) patterns of use in heavily using populations to better understand the employment history and work experience of these individuals; and (4) the impact of illicit drug use and heavy alcohol use on work activity.
Although the workplace offers a unique opportunity to obtain leverage on the alcohol and other drug problems of some users, there are many serious alcohol and other drug abusers who are not regularly employed, if they are employed at all. In 1990, approximately 7 percent of workers reported having used an illicit drug and approximately 6 percent reported having drunk heavily in the past month, compared with 14 percent and 6 percent, respectively, for the unemployed.
- Given the relative low base rate of alcohol and other drug abusers in the employed segment of the work force compared with other selected populations, postemployment workplace alcohol and other drug interventions may help a limited number of abusers, but workplace-oriented interventions cannot solve society's problems with alcohol and other drugs.
- Alcohol and tobacco are the drugs most widely abused by members of the U.S. work force. The adverse health consequences of these drugs are well known. In terms of prevalence rates of work force use and perceived effects of use on performance, alcohol is more likely to have adverse consequences.
Recommendation: Any program that addresses drug use by the work force should include alcohol, the drug most associated with perceived detrimental job performance, as a priority.
Rates of self-reported alcohol and other drug use on the job vary according to occupation, age, gender, and ethnicity. Excluding tobacco and caffeine, most surveys find that fewer than 10 percent of workers report having used alcohol or other drugs while on the job during the prior year. Some studies, however, report significantly higher usage rates. Much of the difference in the reported rates appears attributable to differences in the samples surveyed and the questions asked.
Recommendation: It is important to investigate alcohol and other drug use in different well-specified samples and to develop benchmark measures to allow findings that are comparable across studies.
Part II: Effects of Use
Chapter 4 impact of alcohol and other drug use: laboratory studies.
• Laboratory studies of the effects of alcohol and other drugs on behavior have shown inconsistent results. These differences may be due, in part, to differences in the populations tested, the measurements used, and the range of drug doses administered.
Recommendation: Benchmark measures should be included in laboratory studies to permit generalization across studies. Funding agencies should consider holding conferences to establish such benchmarks.
Laboratory studies show small performance-enhancing effects of commonly used doses of cocaine and other stimulants. Commonly used doses of marijuana produce variable decrements in performance. Alcohol and prescribed sedatives produce decreases in performance depending on the dose, time of consumption, and the time-course of circulating concentrations of the drug's active metabolites, relative to the work schedule. All drug effects are influenced by dose and prior experience. The age of individuals and the presence of other drugs may also mediate the influence of particular drugs.
• The use of alcohol and other drugs away from the work site, including prescription drugs and over-the-counter medication, may have detrimental effects during work, especially for those in safety-sensitive positions. Thus, a long-acting drug taken the night before work or alcohol taken at lunch away from the job may have on-the-job effects like those of drugs taken at the work site. In addition, cessation of drug use may produce either withdrawal or hangover effects that affect work site performance. To date there has been little research directed toward any of these issues.
Recommendation: Researchers and funding agencies should devote more attention to the ways in which prescription and over-the-counter medications affect job performance, especially for safety-sensitive positions.
Recommendation: Studies of work site alcohol and other drug use should encompass off-site use that may have on-the-job effects. Hangover and withdrawal effects should also be considered in assessing the workplace implications of alcohol and other drug use.
Chapter 5 Impact of Alcohol and Other Drug Use: Observational/Field Studies
- Field studies have consistently linked alcohol and other drug use to higher rates of absenteeism; they also provide evidence of an association between alcohol (and perhaps other drug) use and increased rates of accidents, particularly in the transportation industry. Less consistent evidence exists linking alcohol and other drug use to other negative work behaviors, although the current research base is insufficient to support firm conclusions. When associations between alcohol and other drug use and counterproductive workplace behavior are found, relationships are most often of moderate or low strength even when they are statistically significant.
- The empirical relationships found between alcohol and other drug use and job performance are complex and need not imply causation. Relationships may exist for some job performance outcomes like absenteeism but not for others. Alcohol and other drug use may be just one among many characteristics of a more deviant lifestyle, and associations between use and degraded job performance may be due not to drug-related impairment but to general deviance or other factors.
Recommendation: To intervene more effectively in improving job performance, we must develop a better research base from which to assess how alcohol and other drug use and other factors act alone and in combination to degrade job performance.
• Widely cited cost estimates of the effects of alcohol and other drug use on U.S. productivity are based on questionable assumptions and weak measures. Moreover, these cost-of-drug-use studies do not provide estimates of potential savings associated with implementing particular public policies toward alcohol and other drugs.
Recommendation: Further research is needed to develop refined, defensible estimates of how much alcohol and other drug use costs specific organizations and society at large. Business decision makers and policy makers should be cautious in making decisions on the basis of the evidence currently available.
Part III: Effectiveness of Workplace Interventions
Chapter 6 detecting and assessing alcohol and other drug use.
• Methods approved by the National Institute on Drug Abuse (NIDA) for detecting drugs and their metabolites in urine are sensitive and accurate.
Urine collections systems are a critical component of the drug-testing process, but they are the most vulnerable to interference or tampering. Positive results, at concentrations greater than or equal to NIDA-specified thresholds, reliably indicate prior drug use. There is, however, room for further improvement along the lines of the recommendations emanating from the 1989 Consensus Report on Employee Drug Testing and the 1992 On-Site Drug Testing Study. Moreover, more could be learned about laboratory strengths and problems if data already collected in the Department of Defense and NIDA blind quality control and proficiency test programs were properly evaluated.
Recommendation: To obtain accurate test results, all work-related urine tests, including applicant tests, should be conducted using procedural safeguards and quality control standards similar to those put forth by NIDA. All laboratories, including on-site workplace testing facilities, should be required to meet these standards of practice, whether or not they are certified under HHS-NIDA guidelines.
Recommendation: The extensive data on the reliability of laboratory drug-testing results that have been accumulated by the DoD and NIDA blind performance testing programs should be analyzed by independent investigators and the findings of their analyses published in the scientific literature.
• Government standards have improved the quality of laboratory practices; however, the inflexibility and the difficulty of making prompt changes to established government regulations may inhibit the development of new analytical techniques and better experimental-based procedures. Strict regulation of drug-testing procedures and the National Laboratory Certification Programs are nonetheless justified. High-volume, production-oriented drugtesting laboratory operations require the vigilant forensic quality control of routine repetitive procedures, rather than innovative experimental science. Strict regulation need not, however, mean bureaucratic inflexibility that pointlessly increases costs or retards progress, nor should it interfere with research designed to improve current urine testing procedures or efforts to develop reliable tests using specimens other than urine.
Recommendation: Within a regime of strict quality control, allowances should be made for variations in procedures so long as they do not compromise standards and they do reflect professional judgments of laboratory directors and forensic toxicologists about what is required to meet individual program needs. No laboratory should be penalized for any practice that is clearly an improvement on or beyond what is required by the HHS-NIDA guidelines. When such innovations are attempted, data on their performance should be systematically collected and shared with NIDA. NIDA should take the lead in disseminating to all laboratories information about such improvements and should provide advice promptly as problems, research results, and new data become available.
• At present, urine remains the best-understood specimen for evaluation of drug use, and it is the easiest to analyze. Thus, it must for the moment remain the specimen of choice in employee drug-testing programs. However, other specimens have potential advantages over urine in that they involve less intrusive collection procedures or have a longer detection period.
Recommendation: Researchers should be encouraged to evaluate the utility of using specimens other than urine, such as head hair and saliva, for the detection of drugs and their metabolites.
• There has been an unnecessary proliferation of drugs included in the urine test battery. Testing for LSD and sedative drugs, for example, is not always justified.
Recommendation: Additional drugs should not be added to the drug-testing panel without some justification based on epidemiological data for the industry and region. The analytical methods used to identify additional drugs should meet existing NIDA technical criteria.
• Preemployment drug testing may have serious consequences for job applicants. Applicants, unlike most employees, often do not enjoy safeguards commensurate with these consequences. A particular danger of unfairness arises because screening test data are often reported to companies despite the known possibility of false positive classification errors.
Recommendation: No positive drug test result should be reported for a job applicant until a positive screening test has been confirmed by GC/MS technology. If a positive test result is reported by the laboratory, the applicant should be properly informed and should have an opportunity to challenge such results, including access to a medical review officer or other qualified individual to assist in the interpretation of positive results, before the information is given to those who will make the hiring decision.
• Drug-testing results may reveal drugs taken legally for medical treatment that do not seriously affect an employee's job performance. These drugs may, however, be associated with conditions that the employee for good reasons wishes to keep private.
Recommendation: In the absence of a strong detrimental link to job performance, legally prescribed or over-the-counter medications detected by drug testing should not be reported to employers. Furthermore, such results should not be made part of any employment record, except confidential health records with the employee's permission.
• Alcohol and other drug use by work force members cannot be reliably inferred from performance assessments, since performance decrements may have many antecedents. Conversely, performance decrements are often not obvious despite alcohol and other drug use. More direct measures of the likely quality of worker performance hold promise for determining workers' fitness to perform specific jobs at specific times, regardless of the potential cause of impairment. Efforts to identify such measures, however, are still in their infancy.
Recommendation: If an organization's goal is to avoid work decrement (e.g., accidents, injuries, performance level) due to impairment, then research should be conducted on the utility of performance tests prior to starting work as an alternative to alcohol and other drug tests.
• Integrity testing and personality profiles do not provide accurate measures of individual alcohol and other drug use and have not been adequately evaluated as predictors or proxy measures of use. Using these tests to aid in employment decisions involves a significant risk of falsely identifying some individuals as users and missing others who actually use drugs. The accuracy of these tests is affected not only by their validity but also by the characteristics of the population being tested. Urine tests, by contrast, can be quite accurate in detecting recent drug use.
Recommendation: If an organization treats alcohol and other drug use as a hiring criterion, it should rely on urinalysis testing that conforms with NIDA guidelines to detect use rather than on personality profiles or paper-and-pencil tests.
Chapter 7 Impact of Drug-Testing Programs on Productivity
- The empirical evidence pertaining to the efficacy of preemployment drug testing indicates that such programs may be useful to employers in choosing wisely among job applicants. However, regardless of the magnitude of the correlations between drug use and dysfunctional job behavior measures, the practical effectiveness of any drug-testing program depends on other parameters, such as the prevalence of drug use in the population tested. The presence of significant relationships between drug use and workplace performance measures does not necessarily mean that an effective drug-testing program will substantially improve work force performance, and a program that substantially improves performance with some employees or in some job settings may do little to improve performance with other employees or in other job settings.
- Despite beliefs to the contrary, the preventive effects of drug-testing programs have never been adequately demonstrated. Although, there are some suggestive data (e.g., see the military data in Chapter 3 ) that allude to the deterrent effect of employment drug-testing programs, there is as yet no conclusive scientific evidence from properly controlled studies that employment drug-testing programs widely discourage drug use or encourage rehabilitation.
Recommendation: Longitudinal research should be conducted to determine whether drug-testing programs have deterrent effects.
- Many studies of alcohol and other drug use by the work force have been flawed in their designs and implementation. Organizations that conduct their own drug studies can, by encouraging their researchers to publish in professional journals, enhance quality control and contribute to a knowledge base that will enable them to deal more effectively with future alcohol and other drug problems.
- Different objectives have been suggested for work site drug testing and diverse alcohol and other drug intervention programs. These include improving workers' performance, preventing accidents, saving on health costs, and working toward a drug-free society by deterring drug use. The effectiveness of alcohol and other drug intervention programs cannot be adequately evaluated unless the goals of such programs are clear.
Recommendation: Organizations should clearly articulate their objectives prior to initiating alcohol and other drug intervention programs and should regularly evaluate their programs in light of these objectives.
Among job applicants and workers, testing for drugs other than alcohol is already common and generally accepted. Of young men in a 1991 general population survey of high school graduates, 33 percent reported that they had been tested, 61 percent reported that they approved of preemployment testing, and 60 percent reported that they approved of postemployment testing. Approval rates were even higher among those who had been tested.
• Very little is known about what happens to job applicants who are not hired or to employees who are fired as a consequence of a positive drug test.
Recommendation: Research should be conducted on the impact of drug-testing programs with attention to those who remain within the organization as well as to those who are not hired or are dismissed. In particular, more information is needed about the impact of drug-testing programs on the health and productivity of the work force.
Recommendation: In light of the relatively low rates of alcohol and other drug abuse among the work force (see Chapter 3 ), the moderate predictive validity of testing programs (see Chapter 7 ), and the fact that many factors other than drug use may cause performance deficiencies seen in drug users (see Chapter 5 ), drug-testing programs should not be viewed as a panacea for curing workplace performance problems. Nonetheless, drug testing for safety-sensitive positions may still be justified in the interest of public safety.
Chapter 8 Employee Assistance Programs
• Recovery from alcoholism and other drug use disorders is a process that can take months or years of continuing care. The continuing abuse of alcohol or other drugs is a chronic disorder, and the evidence suggests that the ameliorative effects of brief treatments without follow-up are seldom sustained over the long run. Employee assistance programs (EAPs) are well situated to oversee that follow-up, which is essential to a long-term recovery.
Recommendation: Because of high dropout rates in substance abuse treatment programs, EAPs should monitor treatment participation and provide for long-term follow-up.
• EAPs are not generic across work sites. EAPs should and do vary across work sites and over time. Thus, it is misguided to ask whether the generic EAP is an effective program.
Recommendation: EAPs should be evaluated in terms of the amount and quality (including process evaluation) of the services they provide and not just by patient count. Researchers should seek to understand how EAPs contribute to a range of different outcomes in a range of different settings. This requires more high-quality critical case studies of EAPs, perhaps with some common criteria of programmatic effectiveness. Care must be taken to secure adequate control groups, and, rather than attempting to evaluate the overall effectiveness of supposedly static programs, attention should be paid to the effects of particular EAP services and their dynamic nature.
• Given the measurement limitations of drug test results in assessing drug abuse or dependence (see Chapter 6 ), not all individuals testing positive require or are likely to benefit from treatment, counseling, or other administrative actions that might be triggered by a positive drug test result. Blanket rules referring all positive-testing employees to treatment can be costly to employers without providing commensurate benefits to them or their employees. Care is required to determine the appropriate course of action in the event of a positive test.
Recommendation: Persons reviewing test results should be required to demonstrate expertise with respect to toxicology, pharmacology, and occupational medicine. Standards should be set and continuing education and certification should be required. Such individuals should be involved in the interpretation of the results of drug-testing programs, and in the case of positive postemployment tests, should assist other professional staff in interpreting the seriousness of revealed drug use and provide guidance in determining the best course of action for coping with any drug problems (e.g., evaluation referral to proper medical specialist if needed).
Appendix A Methodological Issues
• The most powerful methodology for evaluating the effectiveness of workplace alcohol and other drug intervention programs is the randomized field experiment. The implementation of new work site alcohol and other drug intervention programs or significant changes in existing programs provide propitious occasions for experimental assessment.
Recommendation: To enhance scientific knowledge, organizations instituting new work site alcohol and other drug intervention programs should proceed experimentally if possible. Funding agencies should make field experiments a priority and should consider providing start-up aid to private companies that are willing to institute programs experimentally and subject them to independent evaluation.
- Glantz, M.D. 1992. A developmental psychopathology model of drug abuse vulnerability . Pp. 389-418 in M. Glantz, editor; and R. Pickens, editor. , eds., Vulnerability of Drug Abuse . Washington, D.C.: American Psychological Association.
- Cite this Page National Research Council (US) and Institute of Medicine (US) Committee on Drug Use in the Workplace; Normand J, Lempert RO, O'Brien CP, editors. Under the Influence? Drugs and the American Work Force. Washington (DC): National Academies Press (US); 1994. Summary:, Conclusions and Recommendations.
- PDF version of this title (2.6M)
In this Page
Recent activity.
- Conclusions and Recommendations - Under the Influence? Conclusions and Recommendations - Under the Influence?
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
The Origin and Impact of Crack Cocaine in the United States
This essay about crack cocaine’s rise in the 1980s examines its devastating impact on American society. It explores the origins of cocaine, the creation of crack, and its widespread appeal, especially in economically disadvantaged communities. The social consequences, including addiction, crime, and the racial bias in law enforcement responses, are highlighted. The essay emphasizes the ongoing legacy of the crack epidemic and advocates for a compassionate, comprehensive approach to addressing drug addiction.
How it works
In the turbulent realm of American drug culture, few substances have left as significant and destructive a legacy as crack cocaine. Its rise in the 1980s signaled a new era of addiction, crime, and social decay, leaving behind a path of destruction that still echoes through U.S. communities today.
To understand the origins of crack cocaine, one must first consider the broader context of cocaine itself. Sourced from the coca plant native to South America, cocaine has long been used by indigenous peoples for its stimulating effects.
However, it wasn’t until the late 19th century that it became popular in the Western world, praised as a wonder drug with medicinal benefits and even used in early versions of Coca-Cola.
Throughout the 20th century, cocaine remained present in various forms, from powder to paste. However, the landscape began to shift in the 1970s with increased cocaine trafficking from South America to the United States. This surge led to a burgeoning cocaine market, especially in urban areas like Miami and Los Angeles, where the drug became popular among wealthy individuals and celebrities.
The development of crack cocaine in the early 1980s profoundly altered America’s drug landscape. Crack, a smokable and crystalline form of cocaine, provided a cheaper, more potent alternative to powdered cocaine. Its creation was made possible by using baking soda to “freebase” cocaine, a process that made it more accessible to a wider audience.
The impact of crack cocaine on American society was immediate and devastating. Its low price and intense high made it particularly attractive to economically disadvantaged communities, resulting in widespread addiction. Crack houses, where the drug was bought, sold, and consumed, became symbols of the urban decay that afflicted many inner-city neighborhoods.
The social consequences of crack addiction were severe. Families were torn apart as parents fell into addiction, leaving children to fend for themselves or enter the foster care system. Crime rates surged as addicts turned to theft, robbery, and other illicit activities to support their habits. The crack epidemic worsened existing socioeconomic disparities, disproportionately affecting communities of color and perpetuating cycles of poverty and disenfranchisement.
The response to the crack epidemic was marked by severe law enforcement measures, most notably the Anti-Drug Abuse Act of 1986. This legislation imposed harsh mandatory minimum sentences for crack-related offenses, leading to mass incarceration, especially among African American and Latino populations. The sentencing disparity between crack and powdered cocaine offenses, with the former carrying significantly harsher penalties, underscored the racial bias in the criminal justice system.
Although the crack epidemic subsided by the mid-1990s, its legacy continues to profoundly shape American society. The scars of addiction, violence, and incarceration from those dark years persist, contributing to ongoing issues of poverty, crime, and racial inequality. Additionally, the stigmatization of crack addiction continues, further marginalizing those struggling with substance abuse and hindering efforts at rehabilitation and recovery.
In recent years, there has been a growing recognition of the need for a more compassionate and comprehensive approach to addressing drug addiction. Efforts to shift the focus from punitive measures to treatment and harm reduction have gained momentum, with initiatives such as drug courts and needle exchange programs aimed at reducing the societal impact of substance abuse.
However, the specter of crack cocaine remains a cautionary tale about the dangers of unchecked drug proliferation and the consequences of punitive drug policies. Its legacy serves as a stark reminder of the need for vigilance in addressing the complex interplay of social, economic, and political factors underlying substance abuse and addiction in America. Only through a holistic approach that tackles root causes and prioritizes compassion and equity can we hope to break the cycle of addiction and build a healthier, more resilient society for future generations.
Cite this page
The Origin and Impact of Crack Cocaine in the United States. (2024, May 28). Retrieved from https://papersowl.com/examples/the-origin-and-impact-of-crack-cocaine-in-the-united-states/
"The Origin and Impact of Crack Cocaine in the United States." PapersOwl.com , 28 May 2024, https://papersowl.com/examples/the-origin-and-impact-of-crack-cocaine-in-the-united-states/
PapersOwl.com. (2024). The Origin and Impact of Crack Cocaine in the United States . [Online]. Available at: https://papersowl.com/examples/the-origin-and-impact-of-crack-cocaine-in-the-united-states/ [Accessed: 30 May. 2024]
"The Origin and Impact of Crack Cocaine in the United States." PapersOwl.com, May 28, 2024. Accessed May 30, 2024. https://papersowl.com/examples/the-origin-and-impact-of-crack-cocaine-in-the-united-states/
"The Origin and Impact of Crack Cocaine in the United States," PapersOwl.com , 28-May-2024. [Online]. Available: https://papersowl.com/examples/the-origin-and-impact-of-crack-cocaine-in-the-united-states/. [Accessed: 30-May-2024]
PapersOwl.com. (2024). The Origin and Impact of Crack Cocaine in the United States . [Online]. Available at: https://papersowl.com/examples/the-origin-and-impact-of-crack-cocaine-in-the-united-states/ [Accessed: 30-May-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
Substance Abuse, Social Problems, and Racial Disparities Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Drug-related disorders are dangerous and widespread in the United States: they increase the possibility of mental issues and criminal activity and lead to addiction. The underserved and less protected social classes, such as ethnic and racial minorities, are much more vulnerable to these problems. They have more chances of arrest for the usage and limited access to social protection, treatment, and support. In addition, as they live in poorer conditions, they are susceptible to violence and probably have many psychological traumas, which increase the probability of drugs being used to ease the pain temporarily. In that way, underserved minorities have increased chances of suffering from substance abuse and its consequences, such as crimes and mental problems. I think we should focus on helping them rather than punishing them.
Substance Use and Abuse
There is a controversy about what should be considered substance abuse and what is normal usage. Students often describe their experience with substances, including alcohol and marijuana, as something normal (Willis et al., 2019). The number of substance users in the U.S. remains high, with more than 130 million Americans drinking alcohol and more than 35 million smoking weed regularly, as one can see in Figure 1 (SAMHSA, 2022). According to Figure 2, those suffering from drug misuse rarely seek any help, even if they need and want it. More secure social classes can use substances and feel well with them, knowing they will not be arrested and can obtain aid when necessary. Conversely, underserved people are much more susceptible to risks and sufferings associated with substances (Wallace & Muroff, 2002). Therefore, substance use and abuse are not directly connected; generally, the lower one’s life conditions are, the larger the abuse risk.
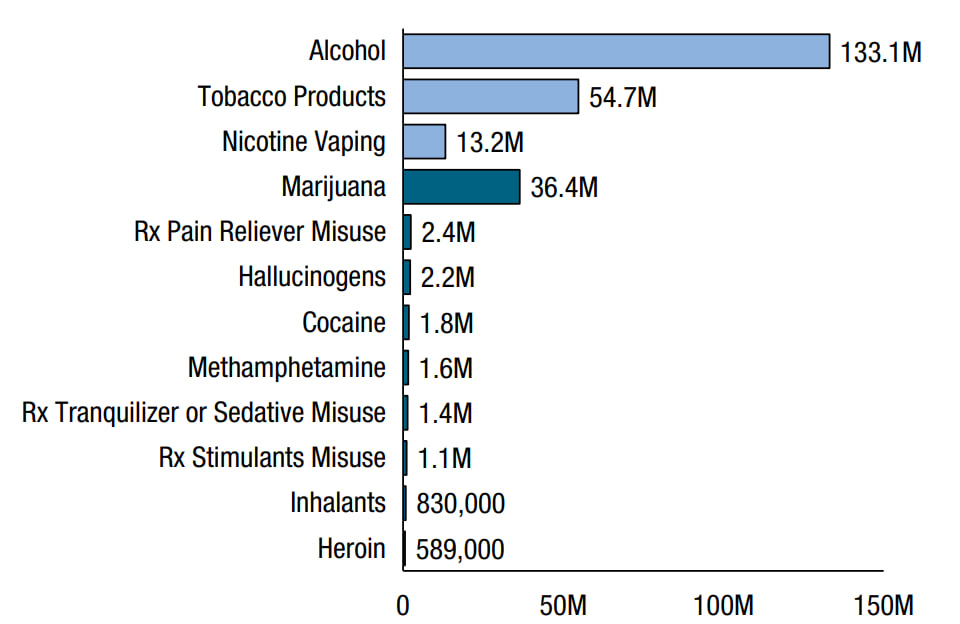
Personal Opinion
I believe that substance use and abuse are different things, despite being interconnected. However, while it is possible to use substances without becoming addicted, it is easy to ignore the risks (Willis et al., 2019). Therefore, to ensure that substance usage will not lead to wrong consequences, one needs to be familiar with the mechanism of drug action and have unrestricted access to treatment and support. As this article will show, people use drugs mostly from being in a desperate state and poor living conditions; underserved social groups, such as many African Americans, are especially vulnerable. It is especially true for alcohol and hard drugs like crack cocaine and opioids. On the other hand, people living in better conditions suffer much less from substance usage (Wallace & Muroff, 2002). If we work firstly to improve the living conditions of all people, regardless of their race or social class, it will be much more efficient in solving these problems than severe punishments.
Societal Costs of Substance Use Disorders: Crime and Mental Issues
Criminal activity and mental issues are the main negative consequences of drug abuse. Both are interconnected and present among underserved people to a much greater extent. As mentioned, altered states of consciousness caused by drugs lead to risky behavior, such as promiscuity, conflicts, and fights (Willis et al., 2019). Along with that, the criminalization of drug users often increases the violence and sufferings connected with addiction (Dee & Pyne, 2022). People who need help are often arrested, sued, and punished instead of receiving it, leading to an increased chance of being involved in criminal activity (Bourgois, 2003). Underserved social groups, such as racial minorities, are especially vulnerable due to poor living conditions and dangerous environments.
Problems with mental health and drug addiction strengthen each other. Depression, anxiety, and pain syndromes increase the chances of using drugs, including illegal ones, to feel temporal relief (SAMHSA, 2022). Criminal activity, poor conditions, and a dangerous environment are also deeply interconnected with drug usage and mental health problems, as they can cause psychological traumas (Kim et al., 2019). They can cause even more destructive and self-destructive behavior if one does not cope with them. All these factors are especially common among underserved populations, including African American youths (Shervington & Bland, 2004). Thus, crime, mental issues, and substance abuse are three interconnected social problems that we should study together. I believe that, along with punishing actual criminals, underserved people should obtain social support. It will provide them and their children the chance to live in better conditions.
Drug Epidemics and Disparities
Underreporting and racial disparities.
People often tend to hide that they have any drug-related disorder, fearing social stigmatization and criminal consequences, especially when taking illicit drugs. As drug users have more chances of encountering a police officer, who will arrest them than someone who will help, they can hide their problems and even refuse to have treatment (Dee & Pyne, 2022). As figure 2 shows, almost 97% of Americans with problems feel that they need no treatment, and another 2% refused to get it, according to the official estimate. Racial disparities are present among the U.S. population: it is connected with the poorer life quality of African and Latin Americans compared to Caucasians (Shervington & Bland, 2004). African American youth often live in conditions where violence is usual. They often cannot obtain help with their psychological traumas, remaining in the vicious cycle of crime, drugs, and mental problems.
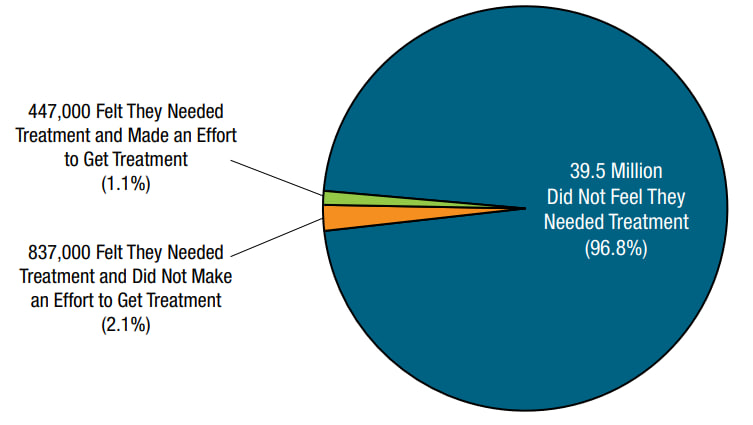
African Americans: Crack Epidemic
Crack is a cocaine-based drug used by smoking: in the 1980s and 1990s, crack usage was exceptionally high. Figure 3 shows the number of articles related to crack abuse in popular newspapers, and the time of the epidemic can be seen by peaks (Hartman & Golub, 1999). Crack usage is associated with African American, especially in the context of crimes and other social problems that are widespread among them (Wallace & Muroff, 2002). However, the actual usage by Black Americans is roughly the same as by Caucasians and even slightly lower.
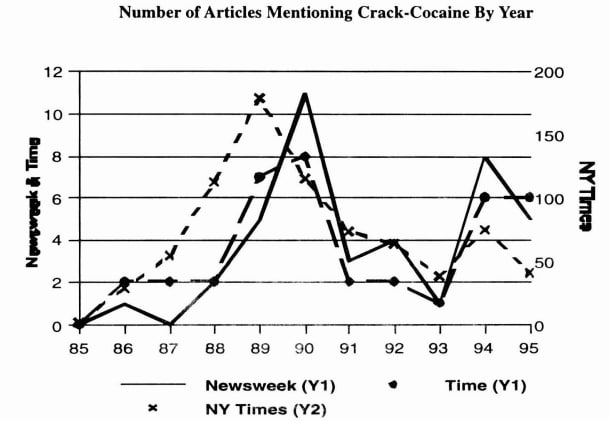
Caucasians: Opioid Epidemic
Similarly, the opioid epidemic defines a widespread usage of opioid drugs, which continues to rise now. Opioids are used to relieve pain, but they are extremely addictive, have severe withdrawal syndrome, and increase the chance of death. While the usage of heroin, one of the most common opioid drugs, is much lower than many others, as Figure 1 shows, its danger is much higher (SAMHSA, 2022). Unlike the crack epidemic, the opioid one tends to be associated mostly with Caucasians, as there is a much larger percentage of them being reported as opioid users, as one can see in Figure 4 (Alexander et al., 2018). However, rates are highly underreported in states with large Black populations, which shows that they actually suffer from the opioid epidemic, too. The problem is even worse for them due to poorer living conditions and limited access to support and treatment.
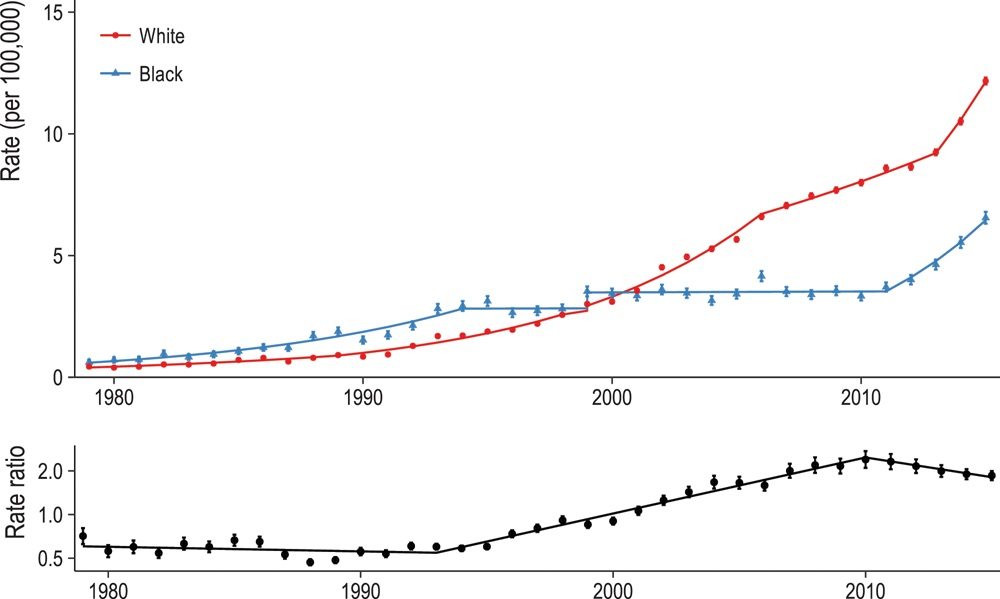
Thus, social problems are primarily caused not by the usage itself but by the poor living conditions and dangerous environment. African Americans are generally poorer than other racial groups and, therefore, subjected to social problems such as domestic violence and lack of health services (Shervington & Bland, 2004). In the 1980s, during the peak of the crack epidemic, police used brute force and incarceration to fight drug spread and usage, but despite the limited public support, it only worsened the situation (Murch, 2015). Overcrowded prisons were full of violence, and living conditions worsened; therefore, crime and mental issues rose. Today, opioid epidemic is mostly associated with Caucasians, but many Black Americans suffer from it, remaining unnoticed and with much less medical support. Stereotypes about African Americans who are all criminals and addicts show the social stigmatization problem (Shervington & Bland, 2004). It is extremely dangerous, as it prevents us from solving social problems and, instead, expands the hate and animosity between races and social groups.
Drug misuse is a large social and personal issue associated with criminal activity and mental issues. Crack cocaine and opioids, especially heroin, are the most dangerous drugs, causing severe addiction and increasing risky behavior, mental problems, and chances of sudden death. Underserved populations, such as racial and ethnic minorities, are the most vulnerable to all three issues. Even if we limit their drug access, without providing medical and psychological support, they will still be engaged in criminality and other destructive activities. Therefore, we should apply a complex approach to solve drug abuse issues. Along with punishing criminals, we should increase people’s literacy about drugs, especially among underserved populations, and provide them with medical and psychological support.
Alexander, M. J., Kiang, M. V., & Barbieri, M. (2018). Trends in Black and White opioid mortality in the United States, 1979–2015 . Epidemiology , 29 (5), 707–715. Web.
Bourgois, P. (2003). Crack and the political economy of social suffering . Addiction Research & Theory , 11 (1), 31–37. Web.
Dee, T. S., & Pyne, J. (2022). A community response approach to mental health and substance abuse crises reduced crime . Science Advances , 8 (23). Web.
Hartman, D. M., & Golub, A. (1999). The social construction of the crack epidemic in the print media . Journal of Psychoactive Drugs , 31 (4), 423–433. Web.
Kim, B. K. E., Gilman, A. B., Kosterman, R., & Hill, K. G. (2019). Longitudinal associations among depression, substance abuse, and crime: A test of competing hypotheses for driving mechanisms . Journal of Criminal Justice , 62 , 50–57. Web.
Murch, D. (2015). Crack in Los Angeles: Crisis, militarization, and black response to the late twentieth-century war on drugs . Journal of American History , 102 (1), 162–173. Web.
SAMHSA. (2022). Key substance use and mental health indicators in the United States: Results from the 2021 national survey on drug use and health . In Substance Abuse and Mental Health Services Administration . Web.
Shervington, D. O., & Bland, I. J. (2004). A study of psychosocial determinants of the crack cocaine epidemic in African American males . Addictive Disorders & Their Treatment , 3 (2), 51–57. Web.
Wallace, J. M., & Muroff, J. R. (2002). Preventing substance abuse among African American children and youth: Race differences in risk factor exposure and vulnerability . The Journal of Primary Prevention , 22 (3), 235–261. Web.
Willis, E., Adams, R., & Keene, J. (2019). If everyone is doing it, it must be safe: College students’ development of attitudes toward poly-substance use . Substance Use & Misuse , 54 (11), 1886–1893. Web.
- The Crack Epidemic of the 1980s
- The Opioid Pandemic Problem and Solutions
- Stigma Effects on Mental Health Treatment in Minorities
- Substance Abuse: Case Study Analysis
- The Impact of Alcohol on the Health of the Addict
- Diagnostic Impressions of Whip Whitaker from the Flight Film
- Music Therapy to Reduce Substance Abuse Among Children
- Marijuana Addiction: Benefits and Negative Sides
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, May 27). Substance Abuse, Social Problems, and Racial Disparities. https://ivypanda.com/essays/substance-abuse-social-problems-and-racial-disparities/
"Substance Abuse, Social Problems, and Racial Disparities." IvyPanda , 27 May 2024, ivypanda.com/essays/substance-abuse-social-problems-and-racial-disparities/.
IvyPanda . (2024) 'Substance Abuse, Social Problems, and Racial Disparities'. 27 May.
IvyPanda . 2024. "Substance Abuse, Social Problems, and Racial Disparities." May 27, 2024. https://ivypanda.com/essays/substance-abuse-social-problems-and-racial-disparities/.
1. IvyPanda . "Substance Abuse, Social Problems, and Racial Disparities." May 27, 2024. https://ivypanda.com/essays/substance-abuse-social-problems-and-racial-disparities/.
Bibliography
IvyPanda . "Substance Abuse, Social Problems, and Racial Disparities." May 27, 2024. https://ivypanda.com/essays/substance-abuse-social-problems-and-racial-disparities/.

COMMENTS
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
In Addiction: A disorder of choice, Gene Heyman surveys a broad array of evidence—historical, anthropological, survey, clinical, and laboratory-based to build an argument about the role of basic choice processes in the phenomena that comprise drug addiction. He makes a compelling, multifaceted argument that conceptualizing drug addiction as a chronic disease (like schizophrenia or diabetes ...
The current paper highlights the causes of drug abuse, and describes the treatment and prevention of drug abuse and addiction for proper management of the problem. Discover the world's research 25 ...
Both prevention and treatment of substance abuse are pertinent to public health, as the two approaches need to employ a multilevel perspective to conceptualize and solve fallout generated from drug trafficking, misuse and harm [ 11, 12 ]. This points to the need to investigate human hereditary, biological, and psychological needs, cognitive and ...
Introduction. Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that "addiction is a brain disease", articulated a set of implications of this position, and outlined an agenda for realizing its promise [].The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the ...
Many people who use addictive substances or who show potentially addictive behaviours are not heavy users. Many people try out such behaviours: some stop after first use, others go on to use occasionally, and others will use moderately or heavily over time. But patterns of use do not just go in one direction: people cease or reduce their behaviours, and they may change in different directions ...
Recent research, however, is beginning to reveal that non-drug or behavioural addictions, especially gambling, show strong neural similarities to substance addiction. Therefore, research examining the brains of both substance and behavioural addiction populations will likely elucidate what the effects of substances of abuse are on the brain as ...
Drug abuse research also has had an impact on antidepressant research (e.g., the actions of drugs of abuse on the brain's serotonin systems have provided useful models with which to investigate the role of those systems in depression and mania). Depression is a risk factor for treatment failure in smoking cessation (Glassman et al., 1993) and ...
opiates to addiction patients and all proprietors of opium products needed to be registered with the federal government, creating the ancestor to the modern PDMP database. One reason cited as a motivation for the Harrison Act was "the careless prescribing of these drugs by physicians" (Terry, 1915). In an effort to
In the vast issue of substance abuse on a global scale, ongoing initiatives and strategic directions are continuously taken. In alignment with the United Nations Sustainable Development Goals, governments have committed to enhancing the prevention and treatment of substance abuse [].Worldwide, drug use remains prevalent and the estimated number of drug users grew from 240 million in 2011 to ...
Substance abuse during adolescence. The use of substances by youth is described primarily as intermittent or intensive (binge) drinking and characterized by experimentation and expediency (Degenhardt et al., Citation 2016; Morojele & Ramsoomar, Citation 2016; Romo-Avilés et al., Citation 2016).Intermittent or intensive substance use is linked to the adolescent's need for activities that ...
Abstract. The use of illicit drugs and the quality of life is intended to provide a rational for a change in some of the present drug policies. After all, the use and the abuse of drugs is largely a health issue and cannot be solved without adequately considering the causes of drug abuse, including the medical, psychiatric, psychological, and ...
Drug addiction is a chronic disease characterized by drug seeking and use that is compulsive, or difficult to control, despite harmful consequences. Brain changes that occur over time with drug use challenge an addicted person's self-control and interfere with their ability to resist intense urges to take drugs.
Addiction is an SSA journal publishing peer-reviewed research reports on pharmalogical and behavioural addictions spanning many different disciplines. Abstract Aims The aim of this study was to characterize the circumstances of drug overdose deaths and determine whether naloxone administration differed by overdose decedent race and ethnicity ...
INTRODUCTION. Substance abuse is a common phenomenon in the world and has invaded the human society as the most important social damage.[1,2] Substance abuse is a nonadaptive model of drug use, which results in adverse problems and consequences, and includes a set of cognitive, behavioral, and psychological symptoms.[]Iran also, due to its specific human and geographic features, has a ...
smoking of cigarettes and gradually drowns the person into the trap of drug abuse. Stress, anxiety, peer pressure, poverty are some of the main causes of drug abuse.As is well said -"it is ...
More specific advice for writing abstract conclusions. Addiction publishes abstracts that are clear, accurate and succinct. Each abstract conclusion must provide the main generalisable statement resulting from the study. In other words, abstract conclusions should function as stand-alone statements that report the study's main findings in ...
The research problem of the study was to examine whether why drug adductors relapsing in the rehabilitation process 3. Objectives of the Research The main objective of this research is to study Drug Addiction & the Rehabilitation Process in Sri Lanka. Basically this study attempted to study drug offenders from Psycho-social aspect
The present research paper explored the impact of drug addiction on mental health. Method:The present study consists of 60 subjects randomly selected among which 30 were adolescents (15 males and ...
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that ...
Heroin Research ReportOverview. Overview. Heroin is a highly addictive opioid drug, and its use has repercussions that extend far beyond the individual user. The medical and social consequences of drug use—such as hepatitis, HIV/AIDS, fetal effects, crime, violence, and disruptions in family, workplace, and educational environments—have a ...
Summary: Conclusions and Recommendations. This report is concerned with the implications of drug use for workplace safety and productivity. It examines the prevalence of alcohol and other drug use by the U.S. work force, the impact of such use on job-related behavior, and the effectiveness of workplace drug intervention programs.
This narrative review attempts to discuss the major drug laws, policies, and national programs of the Government of India (GoI). Methods: A thorough search was conducted to look for policies, programs, acts, and notifications related to substance use/ drug use on various websites of different ministries of the GoI.
Essay Example: In the turbulent realm of American drug culture, few substances have left as significant and destructive a legacy as crack cocaine. Its rise in the 1980s signaled a new era of addiction, crime, and social decay, leaving behind a path of destruction that still echoes through U
Conclusion: Problem of drug addiction in youth in Pakistan is rising at a worrying trend. Numerous familial as well socio-cultural factors in the etiology of drug abuse and addiction have been ...
Conclusion. Drug misuse is a large social and personal issue associated with criminal activity and mental issues. Crack cocaine and opioids, especially heroin, are the most dangerous drugs, causing severe addiction and increasing risky behavior, mental problems, and chances of sudden death. ... Addiction Research & Theory, 11(1), 31-37. Web ...