How to Write a Reflective Essay?
07 August, 2020
17 minutes read
Author: Elizabeth Brown
A reflective essay is a personal perspective on an issue or topic. This article will look at how to write an excellent reflexive account of your experience, provide you with reflexive essay framework to help you plan and organize your essay and give you a good grounding of what good reflective writing looks like.

What is a Reflective Essay?
A reflective essay requires the writer to examine his experiences and explore how these experiences have helped him develop and shaped him as a person. It is essentially an analysis of your own experience focusing on what you’ve learned.
Don’t confuse reflexive analysis with the rhetorical one. If you need assistance figuring out how to write a rhetorical analysis , give our guide a read!
Based on the reflective essay definition, this paper will follow a logical and thought-through plan . It will be a discussion that centers around a topic or issue. The essay should strive to achieve a balance between description and personal feelings.
It requires a clear line of thought, evidence, and examples to help you discuss your reflections. Moreover, a proper paper requires an analytical approach . There are three main types of a reflective essay: theory-based, a case study or an essay based on one’s personal experience.
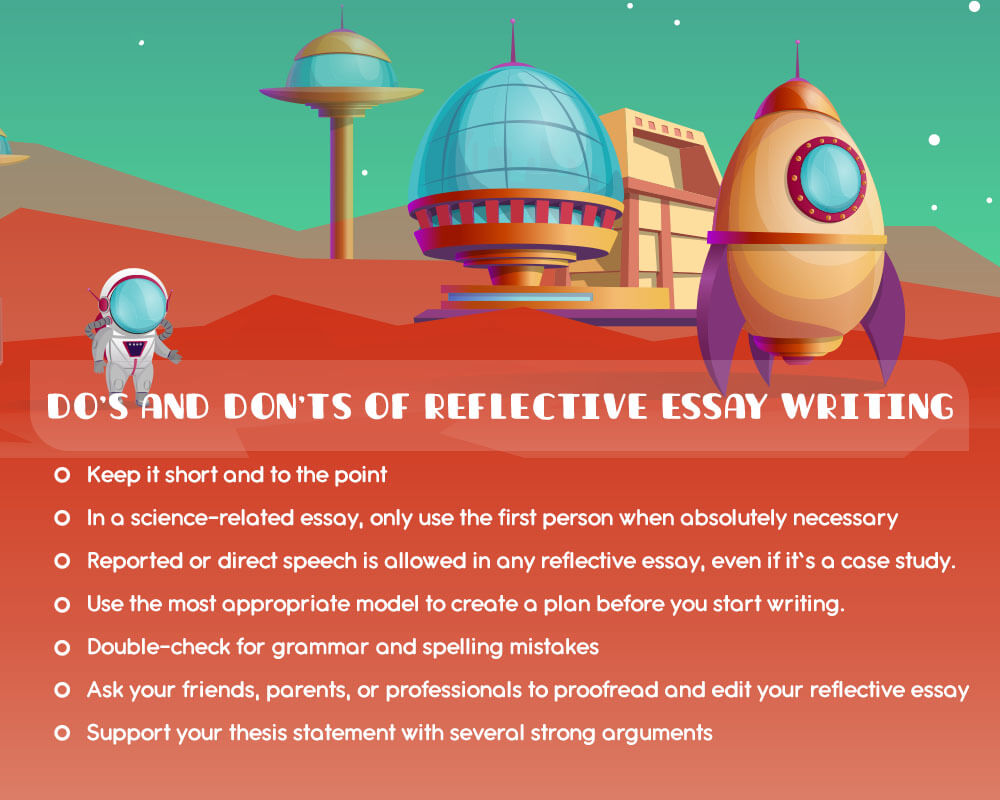
Unlike most academic forms of writing, this writing is based on personal experiences and thoughts. As such, first-person writing position where the writer can refer to his own thoughts and feelings is essential. If the writer talks about psychology or medicine, it is best to use the first-person reference as little as possible to keep the tone objective and science-backed.
To write this paper, you need to recollect and share personal experience . However, there is still a chance that you’ll be asked to talk about a more complex topic.
By the way, if you are looking for good ideas on how to choose a good argumentative essay topic , check out our latest guide to help you out!
The Criteria for a Good Reflective Essay
The convention of an academic reflective essay writing will vary slightly depending on your area of study. A good reflective essay will be written geared towards its intended audience. These are the general criteria that form the core of a well-written piece:
- A developed perspective and line of reasoning on the subject.
- A well-informed discussion that is based on literature and sources relevant to your reflection.
- An understanding of the complex nuance of situations and the tributary effects that prevent them from being simple and clear-cut.
- Ability to stand back and analyze your own decision-making process to see if there is a better solution to the problem.
- A clear understanding of h ow the experience has influenced you.
- A good understanding of the principles and theories of your subject area.
- Ability to frame a problem before implementing a solution.
These seven criteria form the principles of writing an excellent reflective essay.
Still need help with your essay? Handmade Writing is here to assist you!
What is the Purpose of Writing a Reflective Essay?
The purpose of a reflective essay is for a writer to reflect upon experience and learn from it . Reflection is a useful process that helps you make sense of things and gain valuable lessons from your experience. Reflective essay writing allows you to demonstrate that you can think critically about your own skills or practice strategies implementations to learn and improve without outside guidance.
Another purpose is to analyze the event or topic you are describing and emphasize how you’ll apply what you’ve learned.
How to Create a Reflective Essay Outline
- Analyze the task you’ve received
- Read through and understand the marking criteria
- Keep a reflective journal during the experience
- Use a reflective framework (Schon, Driscoll, Gibbs, and Kolb) to help you analyze the experience
- Create a referencing system to keep institutions and people anonymous to avoid breaking their confidentiality
- Set the scene by using the five W’s (What, Where, When, Who and Why) to describe it
- Choose the events or the experiences you’re going to reflect on
- Identify the issues of the event or experience you want to focus on
- Use literature and documents to help you discuss these issues in a wider context
- Reflect on how these issues changed your position regarding the issue
- Compare and contrast theory with practice
- Identify and discuss your learning needs both professionally and personally
Don’t forget to adjust the formatting of your essay. There are four main format styles of any academic piece. Discover all of them from our essay format guide!
Related Posts: Essay outline | Essay format Guide
Using Reflective Frameworks
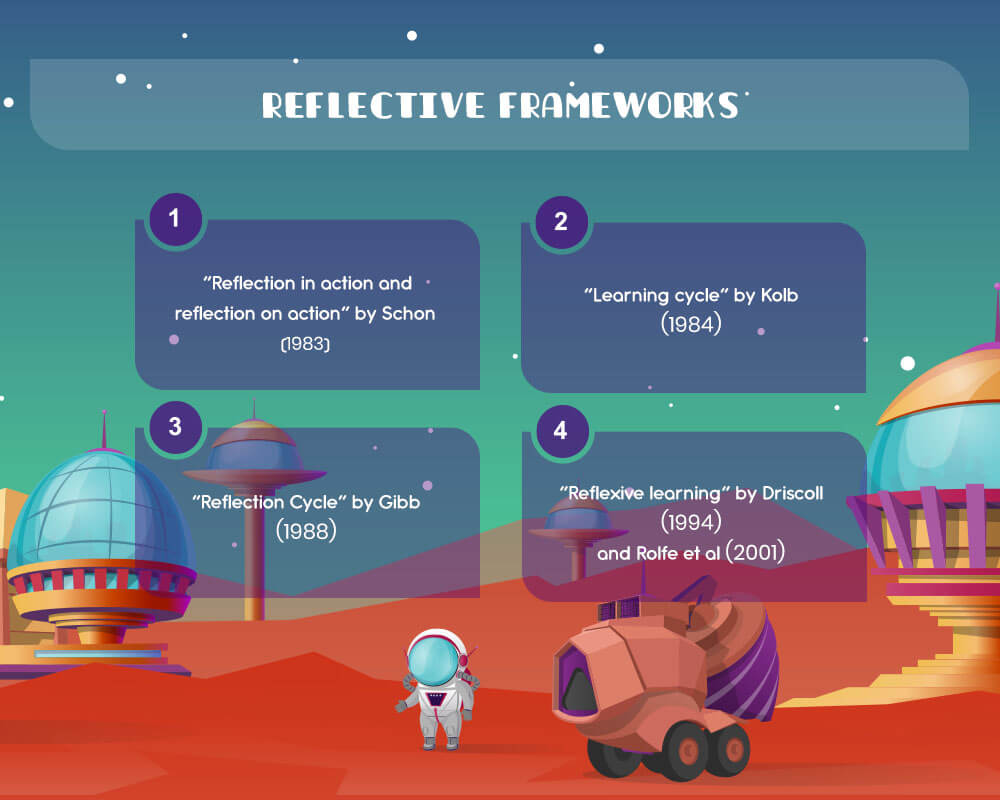
A good way to develop a reflective essay plan is by using a framework that exists. A framework will let help you break the experience down logical and make the answer easier to organize. Popular frameworks include: Schon’s (1983) Reflection in action and reflection on action .
Schon wrote ‘The Reflective Practitioner’ in 1983 in which he describes reflection-in-action and reflection-on-action as tools for learning how to meet challenges that do not conform to formulas learned in school through improvisation. He mentioned two types of reflection : one during and one after. By being aware of these processes while on a work-experience trail or clinical assignment you have to write a reflective account for, you get to understand the process better. So good questions to ask in a reflective journal could be:
<td “200”>Reflection-pre-action <td “200”>Reflection-in-action <td “200”>Reflection-on-Action<td “200”>What might happen? <td “200”>What is happening in the situation? <td “200”>What were your insights after?<td “200”>What possible challenges will you face? <td “200”>Is it working out as you expected? <td “200”>How did it go in retrospect?<td “200”>How will you prepare for the situation? <td “200”>What are the challenges you are dealing with? <td “200”>What did you value and why?<td “200”> <td “200”>What can you do to make the experience a successful one? <td “200”>What would you do differently before or during a similar situation?<td “200”> <td “200”>What are you learning? <td “200”>What have you learned?
This will give you a good frame for your paper and help you analyze your experience.
Kolb’s (1984) Learning Cycle
Kolb’s reflective framework works in four stages:
- Concrete experience. This is an event or experience
- Reflective observation. This is reflecting upon the experience. What you did and why.
- Abstract conceptualization. This is the process of drawing conclusions from the experience. Did it confirm a theory or falsify something? And if so, what can you conclude from that?
- Active experimentation. Planning and trying out the thing you have learned from this interaction.
Gibb’s (1988) Reflection Cycle
Gibbs model is an extension of Kolb’s. Gibb’s reflection cycle is a popular model used in reflective writing. There are six stages in the cycle.
- Description. What happened? Describe the experience you are reflecting on and who is involved.
- Feelings. What were you thinking and feeling at the time? What were your thoughts and feelings afterward?
- Evaluation. What was good and bad about the experience? How did you react to the situation? How did other people react? Was the situation resolved? Why and how was it resolved or why wasn’t it resolved? Could the resolution have been better?
- Analysis. What sense can you make of the situation? What helped or hindered during the event? How does this compare to the literature on the subject?
- Conclusion. What else could you have done? What have you learned from the experience? Could you have responded differently? How would improve or repeat success? How can you avoid failure?
- Action plan. If it arose again what would you do? How can you better prepare yourself for next time?
Driscoll’s Method (1994) and Rolfe et al (2001) Reflexive Learning
The Driscoll Method break the process down into three questions. What (Description), So What (Analysis) and Now What (Proposed action). Rolf et al 2001 extended the model further by giving more in-depth and reflexive questions.
- What is the problem/ difficulty/reason for being stuck/reason for feeling bad?
- What was my role in the situation?
- What was I trying to achieve?
- What actions did I take?
- What was the response of others?
- What were the consequences for the patient / for myself / for others?
- What feeling did it evoke in the patient / in myself / in others?
- What was good and bad about the experience?
- So, what were your feelings at the time?
- So, what are your feelings now? Are there any differences? Why?
- So, what were the effects of what you did or did not do?
- So, what good emerged from the situation for yourself and others? Does anything trouble you about the experience or event?
- So, what were your experiences like in comparison to colleagues, patients, visitors, and others?
- So, what are the main reasons for feeling differently from your colleagues?
- Now, what are the implications for you, your colleagues and the patients?
- Now, what needs to happen to alter the situation?
- Now, what are you going to do about the situation?
- Now, what happens if you decide not to alter anything?
- Now, what will you do differently if faced with a similar situation?
- Now, what information would you need to deal with the situation again?
- Now, what methods would you use to go about getting that information?
This model is mostly used for clinical experiences in degrees related to medicine such as nursing or genetic counseling. It helps to get students comfortable thinking over each experience and adapting to situations.
This is just a selection of basic models of this type of writing. And there are more in-depth models out there if you’re writing a very advanced reflective essay. These models are good for beginner level essays. Each model has its strengths and weaknesses. So, it is best to use one that allows you to answer the set question fully.
This written piece can follow many different structures depending on the subject area . So, check your assignment to make sure you don’t have a specifically assigned structural breakdown. For example, an essay that follows Gibbs plan directly with six labeled paragraphs is typical in nursing assignments. A more typical piece will follow a standard structure of an introduction, main body, and conclusion. Now, let’s look into details on how to craft each of these essay parts.
How to Write an Introduction?
There are several good ways to start a reflective essay . Remember that an introduction to a reflective essay differs depending on upon what kind of reflection is involved. A science-based introduction should be brief and direct introducing the issue you plan on discussing and its context.
Related post: How to write an Essay Introduction
For example, a nursing student might want to discuss the overreliance on medical journals in the industry and why peer-reviewed journals led to mistaken information. In this case, one good way how to start a reflective essay introduction is by introducing a thesis statement. Help the reader see the real value of your work.
Do you need help with your thesis statement? Take a look at our recent guide explaining what is a thesis statement .
Let’s look at some reflective essay examples.
‘During my first month working at Hospital X, I became aware just how many doctors treated peer-views journal articles as a gospel act. This is a dangerous practice that because of (a), (b) and (c) could impact patients negatively.’
The reflective essay on English class would begin differently. In fact, it should be more personal and sound less bookish .
How to Write the Main Body Paragraphs?
The main body of the essay should focus on specific examples of the issue in question. A short description should be used for the opener. Each paragraph of this piece should begin with an argument supporting the thesis statement.
The most part of each paragraph should be a reflexive analysis of the situation and evaluation . Each paragraph should end with a concluding sentence that caps the argument. In a science-based essay, it is important to use theories, other studies from journals and source-based material to argue and support your position in an objective manner.
How to Write the Conclusion?
A conclusion should provide a summary of the issues explored, remind the reader of the purpose of the essay and suggest an appropriate course of action in relation to the needs identified in the body of the essay.
This is mostly an action plan for the future. However, if appropriate a writer can call readers to action or ask questions. Make sure that the conclusion is powerful enough for readers to remember it. In most cases, an introduction and a conclusion is the only thing your audience will remember.
Reflective Essay Topics
Here are some good topics for a reflective essay. We’ve decided to categorize them to help you find good titles for reflective essays that fit your requirement.
Medicine-related topics:
- Write a reflective essay on leadership in nursing
- How did a disease of your loved ones (or your own) change you?
- Write a reflection essay on infection control
- How dealing with peer-reviewed journals interrupts medical procedures?
- Write a reflection essay about community service
- Write a reflective essay on leadership and management in nursing
Topics on teamwork:
- Write a reflective essay on the group presentation
- What makes you a good team player and what stays in the way of improvement?
- Write a reflective essay on the presentation
- Write about the last lesson you learned from working in a team
- A reflective essay on career development: How teamwork can help you succeed in your career?
Topics on personal experiences:
- Write a reflective essay on the pursuit of happiness: what it means to you and how you’re pursuing it?
- Write a reflective essay on human sexuality: it is overrated today? And are you a victim of stereotypes in this area?
- Write a reflective essay on growing up
- Reflective essay on death: How did losing a loved one change your world?
- Write a reflective essay about a choice you regret
- Write a reflective essay on the counseling session
Academic topics:
- A reflective essay on the writing process: How does writing help you process your emotions and learn from experiences?
- Write a reflective essay on language learning: How learning a new language changes your worldview
- A reflective essay about a choice I regret
Related Posts: Research Paper topics | Compare&Contrast Essay topics
Reflective Essay Example
Tips on writing a good reflective essay.
Some good general tips include the following:
As long as you use tips by HandMade Writing, you’ll end up having a great piece. Just stick to our recommendations. And should you need the help of a pro essay writer service, remember that we’re here to help!

A life lesson in Romeo and Juliet taught by death
Due to human nature, we draw conclusions only when life gives us a lesson since the experience of others is not so effective and powerful. Therefore, when analyzing and sorting out common problems we face, we may trace a parallel with well-known book characters or real historical figures. Moreover, we often compare our situations with […]

Ethical Research Paper Topics
Writing a research paper on ethics is not an easy task, especially if you do not possess excellent writing skills and do not like to contemplate controversial questions. But an ethics course is obligatory in all higher education institutions, and students have to look for a way out and be creative. When you find an […]

Art Research Paper Topics
Students obtaining degrees in fine art and art & design programs most commonly need to write a paper on art topics. However, this subject is becoming more popular in educational institutions for expanding students’ horizons. Thus, both groups of receivers of education: those who are into arts and those who only get acquainted with art […]

To grade or not to grade: assessing written reflection

Just over a year ago, while I was a fourth year medical student (SL), I was required to write a reflective essay entitled, “When a patient became a person.” This piece of work contrasted starkly with the “scientific,” evidence-based approach that I had grown accustomed to. I relished this opportunity to think holistically about a patient encounter. Committing my thoughts to paper allowed me to revisit clinical experiences, and to reflect on my personal and professional progress. I have found reflection particularly useful in patient encounters that are challenging or emotionally loaded. Reflecting on these situations has enabled me to learn from good practice I have observed and to be better equipped to communicate with and support patients. The Medical Schools Council and the General Medical Council recently released guidance on reflection specifically for medical students , emphasising the importance of reflective practice and suggesting ways for students to develop skills as “reflective practitioners”, both independently and through medical school assignments. [1]
At UCL Medical School (UCLMS) reflective writing forms part of the formative medical student portfolio. Students in their first clinical year submit two 1000-word reflective pieces as part of the clinical and professional practice (CPP) curriculum. This reflective work is marked and graded by trained tutors. Grading of our reflective essays has always stirred significant debate among my peers. There is also discussion about the emphasis on written work as the mainstay of reflection.
Much has been written on reflection , including by medical students and junior doctors . [2,3] As a medical student representative, I wanted to investigate my peers’ opinions regarding our reflective writing assignments. I therefore compiled an anonymous, voluntary questionnaire, which I and other student representatives distributed to students who had completed these assignments. Students were asked to rate their views on reflective writing, its grading and to suggest possible changes.
Through this questionnaire I learned that views on reflective writing were polarised. Many students valued reflective writing, acknowledging reflection to be a key skill in becoming a doctor. Many of my peers also appreciated grading of reflective work and found it gratifying to receive a high grade for their assignments. Bespoke feedback from tutors was largely well received and deemed to be valuable. I personally found receiving tailored support and guidance from a senior on subjects that can be sensitive or difficult to communicate to be a real strength of the curriculum.
However, many of us also feel that reflection is personal, subjective and does not lend itself to grading. Receiving a low grade can be demoralising and can imply that the student has reflected “incorrectly,” which many students find inappropriate. I can also see how fulfilling specific grading criteria may encourage contrived writing at the expense of genuine reflection.
When students were asked to comment on possible changes to reflective writing, some suggested greater standardisation of marking and feedback, while others proposed removing set titles or the grading system altogether. Some expressed anxiety about the confidentiality of written reflection in the wake of the Bawa-Garba case , in which the contents of a junior doctor’s reflective portfolio may have “fed into” court proceedings. [4] There were also comments about alternative methods for reflection, with many preferring face to face or verbal reflection.
Some students like myself, had participated in Balint groups or Schwartz Rounds, both of which are confidential formats for group discussion and reflection around clinical experiences . [5,6] Poetry, music and art were also suggested as formats for reflection. These are all important creative outlets, but may not be practical for medical school reflective practice. In addition, they may not provide the same function or the same benefits as written reflection. Reflective writing requires deliberate, considered thought around an experience, to allow for learning and potential changes to future practice; other media for reflection may not deliver this.
When I reported these findings to faculty (FG, JY), it resulted in a change to the reflective curriculum. A more detailed online guide to reflective writing for students has been introduced outlining the purpose of reflective practice, relevance to our future careers, different reflective opportunities available within our curriculum and useful models for reflection. In addition, welcome tips on composing the assignment have been provided. Additional essay titles, some suggested by the student body, have been included to widen the choices available. It was gratifying to see these changes implemented.
As someone who has participated in reflective practice at every opportunity during my undergraduate career, being able to co-create and contribute to the reflective curriculum has been invaluable. I appreciate the difficulties in incorporating reflective, unexamined aspects into a full medical education, and feel fortunate to be part of a medical school which can be responsive to the needs of its students.

Jenan Younis is a Colorectal Surgeon and Clinical Teaching Fellow at UCL Medical School Competing interests: None declared

Faye Gishen is a consultant physician and the associate head of the MBBS at UCL Medical School. Competing interests: None declared
References:
- General Medical Council. The reflective practitioner – a guide for medical students. 2019. https://www.gmc-uk.org/education/standards-guidance-and-curricula/guidance/reflective-practice/the-reflective-practitioner—a-guide-for-medical-students (accessed 3 September 2019)
- Macaulay CP, Winyard PJW. Reflection: tick box exercise or learning for all?. BMJ. 2012;345:e7468.
- Furmedge D. Written Reflection is Dead in the Water. BMJ . 2016;353:i3250.
- Dyer C, Cohen D. How should doctors use e-portfolios in the wake of the Bawa-Garba case? BMJ . 2018;360:k572.
- Roberts M. Balint groups: A tool for personal and professional resilience. Can Fam Physician. 2012;58(3):245-7.
- Gishen F, Whitman S, Gill D, Barker R, Walker S. Schwartz Centre Rounds: a new initiative in the undergraduate curriculum—what do medical students think?. BMC Med Educ. 2016, 16:246 https://doi.org/10.1186/s12909-016-0762-6
Information for Authors
BMJ Opinion provides comment and opinion written by The BMJ's international community of readers, authors, and editors.
We welcome submissions for consideration. Your article should be clear, compelling, and appeal to our international readership of doctors and other health professionals. The best pieces make a single topical point. They are well argued with new insights.
For more information on how to submit, please see our instructions for authors.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
Reflective writing
- Related content
- Peer review
- Helen C Richardson , consultant in ENT and senior clinical lecturer
- James Cook University Hospital, Middlesbrough Helen.Richardson{at}stees.nhs.uk
Increasingly, at all stages of medical education, we are asked to keep a learning portfolio, which usually includes some reflective writing. While those fresh from medical school will be familiar with this learning tool, it may be unfamiliar and difficult for others.
Reflective writing is said to encourage a writer to learn from an event, as it necessitates focused and analytical thinking. The lessons learnt can be identified and recorded, as can learning needs for future attention.
Description
Use the word “I” frequently.
Start with a description of an event. Be as objective and detailed as you can. Avoid judgments or interpretations.
Perceptions
Be clear that you have moved from description to interpretation. Make this difference explicit for readers (whether for yourself at a later date, a tutor, or an educational supervisor).
Describe the way you perceived the event. Why do you think things happened the way they did? Don't assume something was inevitable after what has happened previously.
Feelings and emotions
This is the most difficult step for many, but is a valuable source of self learning. Be as honest as you can about the emotions and feelings that the event triggered. What in particular precipitated the emotions you describe?
Avoid assuming that your response is just the way anyone would react. Consider possible alternatives—are there patterns in your emotional response to events?
It can help to try to see things from others' viewpoints.
Your own role
Why did you act as you did? • How else could you have acted?
Which parts went well or badly? Why? • What have you learnt? • What will you do differently next time? • What learning needs have you identified? ■
- Open access
- Published: 09 January 2023
A systematic scoping review of reflective writing in medical education
- Jia Yin Lim 1 , 2 ,
- Simon Yew Kuang Ong 3 , 4 , 5 ,
- Chester Yan Hao Ng 1 , 2 ,
- Karis Li En Chan 1 , 2 ,
- Song Yi Elizabeth Anne Wu 1 , 2 ,
- Wei Zheng So 1 , 2 ,
- Glenn Jin Chong Tey 1 , 2 ,
- Yun Xiu Lam 1 , 2 ,
- Nicholas Lu Xin Gao 1 , 2 ,
- Yun Xue Lim 1 , 2 ,
- Ryan Yong Kiat Tay 1 , 2 ,
- Ian Tze Yong Leong 1 , 2 ,
- Nur Diana Abdul Rahman 4 ,
- Min Chiam 4 ,
- Crystal Lim 6 ,
- Gillian Li Gek Phua 2 , 5 , 7 ,
- Vengadasalam Murugam 2 , 5 ,
- Eng Koon Ong 2 , 4 , 5 , 8 &
- Lalit Kumar Radha Krishna 1 , 2 , 4 , 5 , 9 , 10
BMC Medical Education volume 23 , Article number: 12 ( 2023 ) Cite this article
6749 Accesses
19 Citations
2 Altmetric
Metrics details
Reflective writing (RW) allows physicians to step back, review their thoughts, goals and actions and recognise how their perspectives, motives and emotions impact their conduct. RW also helps physicians consolidate their learning and boosts their professional and personal development. In the absence of a consistent approach and amidst growing threats to RW’s place in medical training, a review of theories of RW in medical education and a review to map regnant practices, programs and assessment methods are proposed.
A Systematic Evidence-Based Approach guided Systematic Scoping Review (SSR in SEBA) was adopted to guide and structure the two concurrent reviews. Independent searches were carried out on publications featured between 1st January 2000 and 30th June 2022 in PubMed, Embase, PsychINFO, CINAHL, ERIC, ASSIA, Scopus, Google Scholar, OpenGrey, GreyLit and ProQuest. The Split Approach saw the included articles analysed separately using thematic and content analysis. Like pieces of a jigsaw puzzle, the Jigsaw Perspective combined the themes and categories identified from both reviews. The Funnelling Process saw the themes/categories created compared with the tabulated summaries. The final domains which emerged structured the discussion that followed.
A total of 33,076 abstracts were reviewed, 1826 full-text articles were appraised and 199 articles were included and analysed. The domains identified were theories and models, current methods, benefits and shortcomings, and recommendations.
Conclusions
This SSR in SEBA suggests that a structured approach to RW shapes the physician’s belief system, guides their practice and nurtures their professional identity formation. In advancing a theoretical concept of RW, this SSR in SEBA proffers new insight into the process of RW, and the need for longitudinal, personalised feedback and support.
Peer Review reports
Introduction
Reflective practice in medicine allows physicians to step back, review their actions and recognise how their thoughts, feelings and emotions affect their decision-making, clinical reasoning and professionalism [ 1 ]. This approach builds on Dewey [ 2 ], Schon [ 3 , 4 ], Kolb [ 5 ], Boud et al. [ 6 ] and Mezirow [ 7 ]’s concepts of critical self-examination. It sees new insights drawn from the physician’s experiences and considers how assumptions may integrate into their current values, beliefs and principles (henceforth belief system) [ 8 , 9 ].
Teo et al. [ 10 ] build on this concept of reflective practice. The authors suggest that the physician’s belief system informs and is informed by their self-concepts of identity which are in turn rooted in their self-concepts of personhood - how they conceive what makes them who they are [ 11 ]. This posit not only ties reflective practice to the shaping of the physician’s moral and ethical compass but also offers evidence of it's role in their professional identity formation (PIF) [ 8 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 ]. With PIF [ 8 , 24 ] occupying a central role in medical education, these ties underscore the critical importance placed on integrating reflective practice in medical training.
Perhaps the most common form of reflective practice in medical education is reflective writing (RW) [ 25 ]. Identified as one of the distinct approaches used to achieve integrated learning, education, curriculum and teaching [ 26 ], RW already occupies a central role in guiding and supporting longitudinal professional development [ 27 , 28 , 29 ]. Its ability to enhance self-monitoring and self-regulation of decisional paradigms and conduct has earned RW a key role in competency-based medical practice and continuing professional development [ 30 , 31 , 32 , 33 , 34 , 35 , 36 ].
However, the absence of consistent guiding principles, dissonant practices, variable structuring and inadequate assessments have raised concerns as to RW’s efficacy and place in medical training [ 25 , 37 , 38 , 39 ]. A Systematic Scoping Review is proposed to map current understanding of RW programs. It is hoped that this SSR will also identify gaps in knowledge and regnant practices, programs and assessment methods to guide the design of RW programs.
Methodology
A Systematic Scoping Review (SSR) is employed to map the employ, structuring and assessment of RW in medical education. An SSR-based review is especially useful in attending to qualitative data that does not lend itself to statistical pooling [ 40 , 41 , 42 ] whilst its broad flexible approach allows the identification of patterns, relationships and disagreements [ 43 ] across a wide range of study formats and settings [ 44 , 45 ].
To synthesise a coherent narrative from the multiple accounts of reflective writing, we adopt Krishna’s Systematic Evidence-Based Approach (SEBA) [ 10 , 15 , 21 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 ]. A SEBA-guided Systematic Scoping Review (SSR in SEBA) [ 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 50 , 53 , 54 , 55 ] facilitates reproducible, accountable and transparent analysis of patterns, relationships and disagreements from multiple angles [ 56 ].
The SEBA process (Fig. 1 ) comprises the following elements: 1) Systematic Approach, 2) Split Approach, 3) Jigsaw Perspective, 4) Funnelling Process, 5) Analysis of data and non-data driven literature, and 6) Synthesis of SSR in SEBA [ 10 , 15 , 21 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 57 , 58 , 59 , 60 ] . Every stage was overseen by a team of experts that included medical librarians from the Yong Loo Lin School of Medicine (YLLSoM) at the National University of Singapore, and local educational experts and clinicians at YLLSoM, Duke-NUS Medical School, Assisi Hospice, Singapore General Hospital, National Cancer Centre Singapore and Palliative Care Institute Liverpool.

The SEBA Process
STAGE 1 of SEBA: Systematic Approach
Determining the title and background of the review.
Ensuring a systematic approach, the expert team and the research team agreed upon the overall goals of the review. Two separate searches were performed, one to look at the theories of reflection in medical education, and another to review regnant practices, programs, and assessment methods used in reflective writing in medical education. The PICOs is featured in Table 1 .
Identifying the research question
Guided by the Population Concept, Context (PCC) elements of the inclusion criteria and through discussions with the expert team, the research question was determined to be: “ How is reflective writing structured, assessed and supported in medical education? ” The secondary research question was “ How might a reflective writing program in medical education be structured? ”
Inclusion criteria
All study designs including grey literature published between 1st January 2000 to 30th June 2022 were included [ 61 , 62 ]. We also consider data on medical students and physicians from all levels of training (henceforth broadly termed as physicians).
Ten members of the research team carried out independent searches using seven bibliographic databases (PubMed, Embase, PsychINFO, CINAHL, ERIC, ASSIA, Scopus) and four grey literature databases (Google Scholar, OpenGrey, GreyLit, ProQuest). Variations of the terms “reflective writing”, “physicians and medical students”, and “medical education” were applied.
Extracting and charting
Titles and abstracts were independently reviewed by the research team to identify relevant articles that met the inclusion criteria set out in Table 1 . Full-text articles were then filtered and proposed. These lists were discussed at online reviewer meetings and Sandelowski and Barroso [ 63 ]’s approach to ‘negotiated consensual validation’ was used to achieve consensus on the final list of articles to be included.
Stage 2 of SEBA: Split Approach
The Split Approach was employed to enhance the trustworthiness of the SSR in SEBA [ 64 , 65 ]. Data from both searches were analysed by three independent groups of study team members.
The first group used Braun and Clarke [ 66 ]’s approach to thematic analysis. Phase 1 consisted of ‘actively’ reading the included articles to find meaning and patterns in the data. The analysis then moved to Phase 2 where codes were constructed. These codes were collated into a codebook and analysed using an iterative step-by-step process. As new codes emerge, previous codes and concepts were incorporated. In Phase 3, codes and subthemes were organised into themes that best represented the dataset. An inductive approach allowed themes to be “defined from the raw data without any predetermined classification” [ 67 ]. In Phase 4, these themes were then further refined to best depict the whole dataset. In Phase 5, the research team discussed the results and consensus was reached, giving rise to the final themes.
The second group employed Hsieh and Shannon [ 68 ]’s approach to directed content analysis. Categories were drawn from Mann et al. [ 9 ]’s article, “Reflection and Reflective Practice in Health Professions Education: A Systematic Review” and Wald and Reis [ 69 ]’s article “Beyond the Margins: Reflective Writing and Development of Reflective Capacity in Medical Education”.
The third group created tabulated summaries in keeping with recommendations drawn from Wong et al. [ 56 ]’s "RAMESES Publication Standards: Meta-narrative Reviews" and Popay et al. [ 70 ]’s “Guidance on the C onduct of N arrative Synthesis in Systematic Reviews”. The tabulated summaries served to ensure that key aspects of included articles were not lost.
Stage 3 of SEBA: Jigsaw Perspective
The Jigsaw Perspective [ 71 , 72 ] saw the findings of both searches combined. Here, overlaps and similarities between the themes and categories from the two searches were combined to create themes/categories. The themes and subthemes were compared with the categories and subcategories identified, and similarities were verified by comparing the codes contained within them. Individual subthemes and subcategories were combined if they were complementary in nature.
Stage 4 of SEBA: Funnelling Process
The Funnelling Process saw the themes/categories compared with the tabulated summaries to determine the consistency of the domains created, forming the basis of the discussion.
Stage 5: Analysis of data and non-data driven literature
Amidst concerns that data from grey literature which were neither peer-reviewed nor necessarily evidence-based may bias the synthesis of the discussion, the research team separately thematically analysed the included grey literature. These themes were compared with themes from data-driven or research-based peer-reviewed data and were found to be the same and thus unlikely to have influenced the analysis.
Stage 6: Synthesis of SSR in SEBA
The Best Evidence Medical Education (BEME) Collaboration Guide and the Structured approach to the Reporting In healthcare education of Evidence Synthesis (STORIES) were used to guide the discussion.
A total of 33,076 abstracts were reviewed from the two separate searches on theories of reflection in medical education, and on regnant practices, programs and assessments of RW programs in medical education. A total of 1826 full-text articles were appraised from the separate searches, and 199 articles were included and analysed. The PRISMA Flow Chart may be found in Fig. 2 a and b. The domains identified when combining the findings of the two separate searches were 1) Theories and Models, 2) Current Methods, 3) Benefits and Shortcomings and 4) Recommendations.
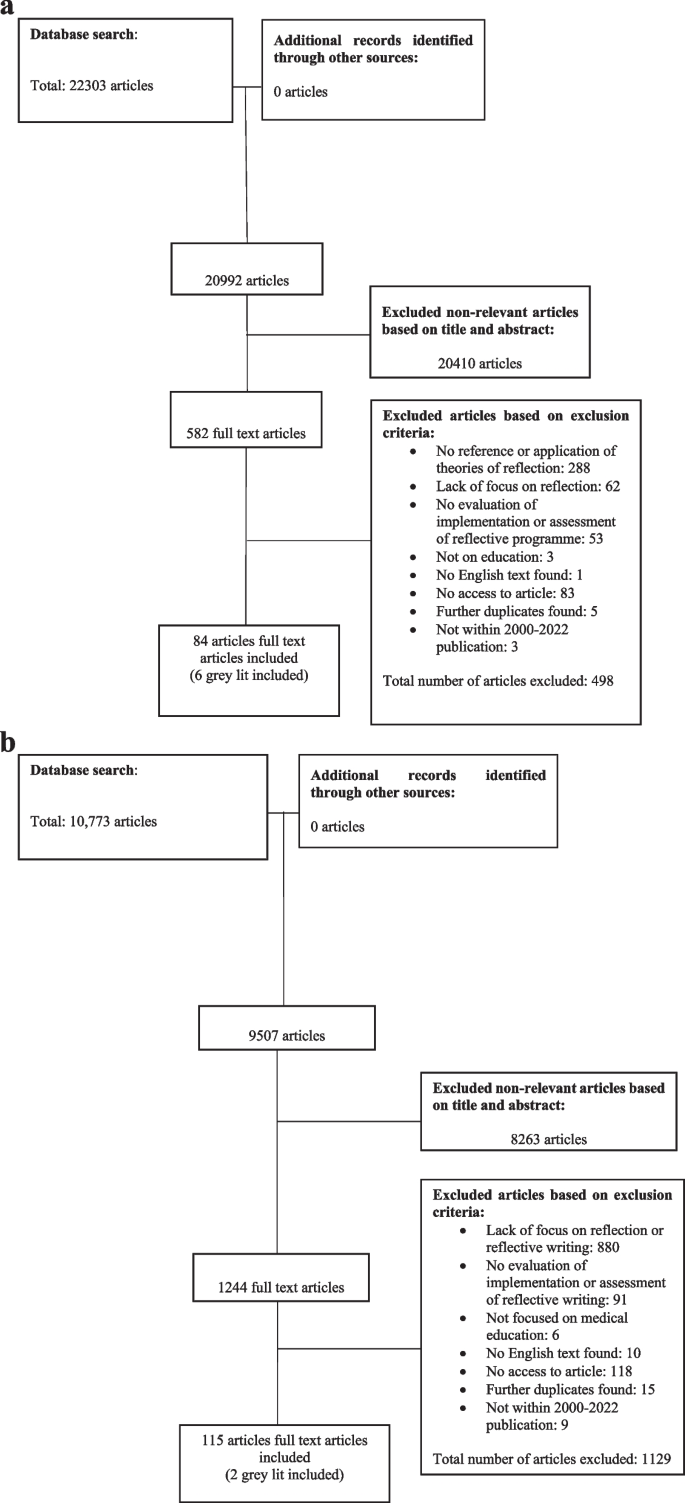
a PRISMA Flow Chart (Search Strat #1: Theories of Reflection in Medical Education). b PRISMA Flow Chart (Search Strat #2: Reflective Writing in Medical Education)
Domain 1: Theories and Models
Many current theories and models surrounding RW in medical education are inspired by Kolb’s Learning Cycle [ 5 ] (Table 2 ). These theories focus on descriptions of areas of reflection; evaluations of experiences and emotions; how events may be related to previous experiences; knowledge critiques of their impact on thinking and practice; integration of learning points; and the physician’s willingness to apply lessons learnt [ 6 , 73 , 74 , 75 ]. In addition, some of these theories also consider the physician’s self-awareness, ability and willingness to reflect [ 76 ], contextual factors related to the area of reflection [ 4 , 77 ] and the opportunity to reflect effectively within a supportive environment [ 78 , 79 ]. Ash and Clayton's DEAL Model recommends inclusion of information from all five senses [ 80 , 81 , 82 , 83 ]. Johns's Model of Structured Reflection [ 84 ] advocates giving due consideration to internal and external influences upon the event being evaluated. Rodgers [ 39 ] underlines the need for appraisal of the suppositions and assumptions that precipitate and accompany the effects and responses that may have followed the studied event. Griffiths and Tann [ 75 ], Mezirow [ 77 ], Kim [ 85 ], Roskos et al. [ 86 ], Burnham et al. [ 87 ], Korthagen and Vasalos [ 78 ] and Koole et al. [ 74 ] build on Dewey [ 2 ] and Kolb [ 5 ]’s notion of creating and experimenting with a ‘working hypothesis’. These models also propose that the lessons learnt from experimentations should be critiqued as part of a reiterative process within the reflective cycle. Underlining the notion of the reflective cycle and the long-term effects of RW, Pearson and Smith [ 88 ] suggest that reflections should be carried out regularly to encourage longitudinal and holistic reflections on all aspects of the physician’s personal and professional life.
Regnant theories shape assessments of RW (Table 3 ). This extends beyond Thorpe [ 96 ]’s study which categorises reflective efforts into ‘non-reflectors’, ‘reflectors’, ‘critical reflectors’, and focuses on their process, structure, depth and content. van Manen [ 97 ], Plack et al. [ 98 ], Rogers et al. [ 99 ] and Makarem et al. [ 100 ] begin with evaluating the details of the events. Kim’s Critical Reflective Inquiry Model [ 85 ] and Bain’s 5Rs Reflective Framework [ 101 ] also consider characterisations of emotions involved. Other models appraise the intentions behind actions and thoughts [ 85 ], the factors precipitating the event [ 101 ] and meaning-making [ 85 ]. Other theories consider links with previous experiences [ 100 ], the integration of thoughts, justifications and perspectives [ 99 ], and the hypothesising of future strategies [ 98 ].

Domain 2: Current methods of structuring RW programs
Current programs focus on supporting the physician throughout the reflective process. Whilst due consideration is given to the physician’s motivations, insight, experiences, capacity and capabilities [ 25 , 96 , 112 , 113 , 114 , 115 , 116 ], programs also endeavour to ensure appropriate selection and training of physicians intending to participate in RW. Efforts are also made to align expectations, and guide and structure the RW process [ 37 , 116 , 117 , 118 , 119 , 120 , 121 , 122 ]. Physicians are provided with frameworks [ 76 , 79 , 105 , 123 , 124 ], rubrics [ 99 , 123 , 125 , 126 ], examples of the expected quality and form of reflection [ 96 , 115 , 116 ], and how to include emotional and contextual information in their responses [ 121 , 127 , 128 , 129 ].
Other considerations are enclosed in Table 4 including frequency, modality and the manner in which RW is assessed.
Domain 3: Benefits and Shortcomings
The benefits of RW are rarely described in detail and may be divided into personal and professional benefits as summarised in Table 5 for ease of review. From a professional perspective, RW improves learning [ 96 , 112 , 119 , 147 , 157 , 170 , 179 , 185 , 186 , 187 , 188 , 189 , 190 , 191 , 192 ], facilitates continuing medical education [ 119 , 128 , 173 , 174 , 193 , 194 , 195 ], inculcates moral, ethical, professional and social standards and expectations [ 118 , 156 , 160 ], improves patient care [ 29 , 120 , 129 , 131 , 135 , 142 , 194 , 196 , 197 , 198 , 199 ] and nurtures PIF [ 150 , 157 , 172 , 191 , 200 ].
From a personal perspective, RW increases self-awareness [ 114 , 127 , 137 , 161 , 166 , 179 , 185 , 202 , 216 ], self-advancement [ 9 , 131 , 134 , 150 , 168 , 174 , 195 , 205 , 217 , 229 ], facilitates understanding of individual strengths, weaknesses and learning needs [ 112 , 119 , 150 , 152 , 170 , 218 , 219 ], promotes a culture of self-monitoring, self-improvement [ 130 , 172 , 173 , 185 , 193 , 198 , 201 , 210 , 211 ], developing critical perspectives of self [ 193 , 223 ] and nurtures resilience and better coping [ 154 , 160 , 206 ]. RW also guides shifts in thinking and perspectives [ 148 , 149 , 156 , 203 , 207 , 208 ] and focuses on a more holistic appreciation of decision-making [ 37 , 118 , 126 , 174 , 177 , 194 , 196 , 199 , 200 , 224 , 225 , 226 ] and their ramifications [ 37 , 112 , 116 , 130 , 131 , 141 , 154 , 179 , 193 , 194 , 196 , 204 , 207 , 218 , 230 ].
Table 6 combines current lists of the shortcomings of RW. These limitations may be characterised by individual, structural and assessment styles.
It is suggested that RW does not cater to the different learning styles [ 220 , 232 ], cultures [ 190 ], roles, values, processes and expectations of RW [ 114 , 129 , 135 , 138 , 142 , 209 , 227 , 234 ], and physicians' differing levels of self-awareness [ 29 , 79 , 119 , 176 , 188 , 226 , 231 , 236 ], motivations [ 29 , 119 , 136 , 138 , 157 , 161 , 167 , 168 , 169 , 176 , 181 , 193 , 196 , 226 , 232 , 233 ] and willingness to engage in RW [ 37 , 114 , 136 , 149 , 160 , 183 ]. RW is also limited by poorly prepared physicians and misaligned expectations whilst a lack of privacy and a safe setting may precipitate physician anxiety at having their private thoughts shared [ 129 , 149 , 209 , 231 ]. RW is also compromised by a lack of faculty training [ 143 , 145 , 239 ], mentoring support [ 37 , 50 , 119 , 133 , 196 ] and personalised feedback [ 50 , 114 , 136 , 167 , 229 ] which may lead to self-censorship [ 37 , 114 , 136 , 149 , 160 , 183 ] and an unwillingness to address negative emotions arising from reflecting on difficult events [ 114 , 168 , 176 , 193 , 230 ], circumventing the reflective process [ 118 , 142 , 165 , 196 ] .
Variations in assessment styles [ 9 , 115 , 157 , 161 , 166 , 193 , 209 ], depth [ 29 , 105 , 118 , 126 , 177 , 207 ] and content [ 37 , 114 , 136 , 149 , 169 , 183 , 196 ], and pressures to comply with graded assessments [ 114 , 115 , 118 , 129 , 138 , 143 , 149 , 155 , 157 , 209 , 232 , 237 , 238 ] also undermine efforts of RW.
Domain 4. Recommendations
In the face of practice variations and challenges, there have been several recommendations on improving practice.
Boosting awareness of RW
Acknowledging the importance of a physician’s motivations, willingness and judgement [ 37 ], an RW program must acquaint physicians with information on RW’s role [ 128 ], program expectations, the form, frequency and assessments of RW and the support available to them [ 130 , 132 , 150 , 154 , 242 ] and its benefits to their professional and personal development [ 96 , 227 ] early in their training programs [ 115 , 220 , 242 , 243 ]. Physicians should also be trained on the knowledge and skills required to meet these expectations [ 1 , 37 , 135 , 151 , 160 , 215 , 244 , 245 ].
A structured program and environment
Recognising that effective RW requires a structured program. Recommendations focus on three aspects of the program design [ 132 ]. One is the need for trained faculty [ 9 , 115 , 219 , 220 , 230 , 233 , 242 , 246 ], accessible communications, protected time for RW and debriefs [ 125 ], consistent mentoring support [ 190 ] and assessment processes [ 247 ]. This will facilitate trusting relationships between physicians and faculty [ 30 , 114 , 168 , 196 , 231 , 233 ]. Two, the need to nurture an open and trusting environment where physicians will be comfortable with sharing their reflections [ 96 , 128 ], discussing their emotions, plans [ 127 , 248 ] and receiving feedback [ 9 , 37 , 79 , 114 , 119 , 128 , 135 , 173 , 176 , 179 , 190 , 237 ]. This may be possible in a decentralised classroom setting [ 163 , 190 ]. Three, RW should be part of the formal curriculum and afforded designated time. RW should be initiated early and longitudinally along the training trajectory [ 116 , 122 ].
Adjuncts to RW programs
Several approaches have been suggested to support RW programs. These include collaborative reflection, in-person discussion groups to share written reflections [ 128 , 131 , 138 , 196 , 199 , 231 , 249 ] and reflective dialogue to exchange feedback [ 119 ], use of social media [ 149 , 160 , 169 , 194 , 204 , 230 ], video-recorded observations and interactions for users to review and reflect on later [ 133 ]. Others include autobiographical reflective avenues in addition to practice-oriented reflection [ 137 ], support groups to help meditate stress or emotions triggered by reflections [ 249 ] and mixing of reflective approaches to meet different learning styles [ 169 , 250 ].
In answering the primary research question, “How is reflective writing structured, assessed and supported in medical education?” , this SSR in SEBA highlights several key insights. To begin, RW involves integrating the insights of an experience or point of reflection (henceforth ‘event’) into the physician’s currently held values, beliefs and principles (henceforth belief system). Recognising that an ‘event’ has occurred and that it needs deeper consideration highlights the physician’s sensitivity . Recognising the presence of an ‘event’ triggers an evaluation as to the urgency in which it needs to be addressed, where it stands amongst other ‘events’ to be addressed and whether the physician has the appropriate skills, support and time to address the ‘event’. This reflects the physician’s judgement . The physician must then determine whether they are willing to proceed and the ramifications involved. These include ethical, medical, clinical, administrative, organisational, sociocultural, legal and professional considerations. This is then followed by contextualising them to their own personal, psychosocial, clinical, professional, research, academic, and situational setting. Weighing these amidst competing ‘events’ underlines the import of the physician’s ability to ‘balance’ considerations. Creating and experimenting on their ‘working hypothesis’ highlights their ‘ability’, whilst how they evaluate the effects of their experimentation and how they adapt their practice underscores their ‘ responsiveness ’ [ 2 , 5 , 74 , 75 , 77 , 78 , 85 , 86 , 87 , 90 ].
The concepts of ‘ sensitivity’, ‘judgement’, ‘willingness’, ‘balance’, ‘ability’ and ‘responsiveness’ spotlight environmental and physician-related factors. These include the physician’s motivations, knowledge, skills, attitudes, competencies, working style, needs, availabilities, timelines, and their various medical, clinical, administrative, organisational, sociocultural, legal, professional, personal, psychosocial, clinical, research, academic and situational experiences. It also underlines the role played by the physician’s beliefs, moral values, ethical principles, familial mores, cultural norms, attitudes, thoughts, decisional preferences, roles and responsibilities. The environmental-related factors include the influence of the curriculum, the culture, structure, format, assessment and feedback of the RW process and the program it is situated in. Together, the physician and their environmental factors not only frame RW as a sociocultural construct necessitating holistic review but also underscore the need for longitudinal examination of its effects. This need for holistic and longitudinal appraisal of RW is foregrounded by the experimentations surrounding the ‘working hypothesis’ [ 2 , 5 , 72 , 74 , 77 , 84 , 85 , 86 , 90 ]. In turn, experimentations and their effects affirm the notion of regular use of RW and reiterate the need for longitudinal reflective relationships that provide guidance, mentoring and feedback [ 87 , 90 ]. These considerations set the stage for the proffering of a new conceptual model of RW.
To begin, the Krishna Model of Reflective Writing (Fig. 3 ) builds on the Krishna-Pisupati Model [ 10 ] used to describe evaluations of professional identity formation (PIF) [ 8 , 10 , 24 , 251 ]. Evidenced in studies of how physicians cope with death and dying patients, moral distress and dignity-centered care [ 46 , 54 ], the Krishna-Pisupati Model suggests that the physician’s belief system is informed by their self-concepts of personhood and identity. This is effectively characterised by the Ring Theory of Personhood (RToP) [ 11 ].
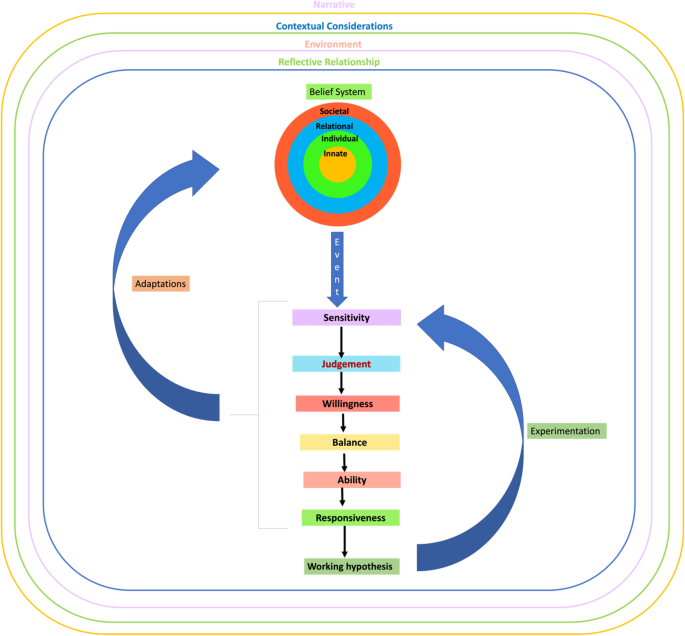
Krishna Model of Reflective Writing
The Krishna Model of RW posits that the RToP is able to encapsulate various aspects of the physician’s belief system. The Innate Ring which represents the innermost ring of the four concentric rings depicting the RToP is derived from currently held spiritual, religious, theist, moral and ethical values, beliefs and principles [ 13 , 51 , 53 , 252 ]. Encapsulating the Innate Ring is the Individual Ring. The Individual Ring’s belief system is derived from the physician’s thoughts, conduct, biases, narratives, personality, decision-making processes and other facets of conscious function which together inform the physician’s Individual Identity [ 13 , 51 , 53 , 252 ]. The Relational Ring is shaped by the values, beliefs and principles governing the physician’s personal and important relationships [ 13 , 51 , 53 , 252 ]. The Societal Ring, the outermost ring of the RToP is shaped by regnant societal, religious, professional and legal expectations, values, beliefs and principles which inform their interactions with colleagues and acquaintances [ 13 , 51 , 53 , 252 ]. Adoption of the RToP to depict this belief system not only acknowledges the varied aspects and influences that shape the physician’s identity but that the belief system evolves as the physician’s environment, narrative, context and relationships change.
The environmental factors influencing the belief system include the support structures used to facilitate reflections such as appropriate protected time, a consistent format for RW, a structured assessment program, a safe environment, longitudinal support, timely feedback and trained faculty. The Krishna Model of RW also recognises the importance of the relationships which advocate for the physician and proffer the physician with coaching, role modelling, supervision, networking opportunities, teaching, tutoring, career advice, sponsorship and feedback upon the RW process. Of particular importance is the relationship between physician and faculty (henceforth reflective relationship). The reflective relationship facilitates the provision of personalised, appropriate, holistic, and frank communications and support. This allows the reflective relationship to support the physician as they deploy and experiment with their ‘working hypothesis’. As a result, the Krishna Model of RW focuses on the dyadic reflective relationship and acknowledges that there are wider influences beyond this dyad that shape the RW process. This includes the wider curriculum, clinical, organisational, social, professional and legal considerations within specific practice settings and other faculty and program-related factors. Important to note, is that when an ‘event’ triggers ‘ sensitivity’, ‘judgement’, ‘willingness’, ‘balance’, ‘ability’ and ‘responsiveness’, the process of creating and experimenting with a ‘working hypothesis' and adapting one's belief system is also shaped by the physician’s narratives, context, environment and relationships.
In answering its secondary question, “ How might a reflective writing program in medical education be structured? ”, the data suggests that an RW program ought to be designed with due focus on the various factors influencing the physician's belief system, their ‘sensitivity’, ‘judgement’, ‘willingness’, ‘balance’, ‘ability’ and ‘responsiveness’, and their creation and experimentation with their ‘working hypothesis’. These will be termed the ‘physician's reactions’ . The design of the RW program ought to consider the following factors:
Belief system
Recognising that the physician’s notion of ‘ sensitivity’, ‘judgement’, ‘willingness’, ‘balance’, ‘ability’ and ‘responsiveness’ is influenced by their experience, skills, knowledge, attitude and motivations, physicians recruited to the RW program should be carefully evaluated
To align expectations, the physician should be introduced to the benefits and role of RW in their personal and professional development
The ethos, frequency, goals and format of the reflection and assessment methods should be clearly articulated to the physician [ 253 ]
The physician should be provided with the knowledge, skills and mentoring support necessary to meet expectations [ 76 , 79 , 105 , 123 , 124 , 254 , 255 ]
Training and support must also be personalised
Contextual considerations
Recognising that the physician’s academic, personal, research, administrative, clinical, professional, sociocultural and practice context will change, the structure, approach, assessment and support provided must be flexible and responsive
The communications platform should be easily accessible and robust to attend to the individual needs of the physician in a timely and appropriate manner
The program must support diversity [ 207 ]
Environment
The reflective relationship is shaped by the culture and structure of the environment in which the program is hosted in
The RW programs must be hosted within a formal structured curriculum, supported and overseen by a host organisation which is able to integrate the program into regnant educational and assessment processes [ 9 , 115 , 219 , 220 , 230 , 233 , 242 , 246 ]
Reflective relationship
The faculty must be trained and provided access to counselling, mindfulness meditation and stress management programs [ 249 ]
The faculty must support the development of the physician’s metacognitive skills [ 256 , 257 , 258 , 259 ], and should create a platform that facilitates community-centered learning [ 173 , 176 ], structured, timely, personalised open feedback [ 119 , 135 , 179 , 237 ] and support [ 128 , 131 , 138 , 196 , 199 , 231 , 249 ]
The faculty must be responsive to changes and provide appropriate personal, educational and professional support and adaptations to the assessment process when required [ 207 ]
To facilitate the development of effective reflective relationships, a consistent faculty member should work with the physician and build a longitudinal trusting, open and supportive reflective relationship
Physician’s reactions
The evolving nature of the various structures and influences upon the RW process underscores the need for longitudinal assessment and support
The physician must be provided with timely, appropriate and personalised training and feedback
The program’s structure and oversight must also be flexible and responsive
There must be accessible longitudinal mentoring support
The format and assessment of RW must account for growing experience and competencies as well as changing motivations and priorities
Whilst social media may be employed to widen sharing [ 149 , 155 , 160 , 169 , 194 ], privacy must be maintained [ 120 , 189 ]
On assessment
Assessment rubrics should be used to guide the training of faculty, education of physicians and guidance of reflections [ 37 , 116 , 117 , 118 , 119 , 120 , 121 , 122 ]
Assessments ought to take a longitudinal perspective to track the physician's progress [ 116 , 122 ]
Based on the results from this SSR in SEBA, we forward a guide catering to novice reflective practitioners (Additional file 1 ).
Limitations
This SSR in SEBA suggests that, amidst the dearth of rigorous quantitative and qualitative studies in RW and in the presence of diverse practices, approaches and settings, conclusions may not be easily drawn. Extrapolations of findings are also hindered by evidence that appraisals of RW remain largely reliant upon single time point self-reported outcomes and satisfaction surveys.
This SSR in SEBA highlights a new model for RW that requires clinical validation. However, whilst still not clinically proven, the model sketches a picture of RW’s role in PIF and the impact of reflective processes on PIF demands further study. As we look forward to engaging in this area of study, we believe further research into the longer-term effects of RW and its potential place in portfolios to guide and assess the development of physicians must be forthcoming.
Availability of data and materials
All data generated or analysed during this review are included in this published article and its supplementary files.
Abbreviations
Reflective Writing
Professional Identity Formation
Ring Theory of Personhood
Best Evidence Medical Education
Structured approach to the Reporting In healthcare education of Evidence Synthesis
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Systematic Scoping Review
Systematic Evidence-Based Approach
Yong Loo Lin School of Medicine
Population, Intervention, Comparison, Outcome, Study Design
Realist And Meta-narrative Evidence Syntheses - Evolving Standards
Wang Y-H, Liao H-C. Construction and validation of an analytic reflective writing scoring rubric for healthcare students and providers. 醫學教育. 2020;24(2):53–72.
Google Scholar
Dewey J. How we think: a restatement of the relation of reflective thinking to the educative process. Am J Psychol. 1933;46:528.
Schon DA. The reflective practitioner: how professionals think in action. New York: Basic Books; 1983.
Schon DA. Educating the reflective practitioner: towards a new design for teaching and learning in the profession. San Francisco: Jossey-Bass; 1987.
Kolb DA. Experiential learning: experience as the source of learning and development. Englewood Cliffs: Prentice Hall; 1984.
Boud D, Keogh R, Walker D. Reflection: turning experience into learning. London: Kogan Page; 1985.
Mezirow J. Fostering critical reflection in adulthood: a guide to transformative and emancipatory learning. San Francisco: Jossey-Bass; 1990.
Sarraf-Yazdi S, Teo YN, How AEH, Teo YH, Goh S, Kow CS, et al. A scoping review of professional identity formation in undergraduate medical education. J Gen Intern Med. 2021;36(11):3511–21.
Article Google Scholar
Mann K, Gordon J, MacLeod A. Reflection and reflective practice in health professions education: a systematic review. Adv Health Sci Educ. 2009;14(4):595–621.
Teo KJH, Teo MYK, Pisupati A, Ong RSR, Goh CK, Seah CHX, et al. Assessing professional identity formation (PIF) amongst medical students in Oncology and Palliative Medicine postings: a SEBA guided scoping review. BMC Palliat Care. 2022;21(1):200.
Radha Krishna LK, Alsuwaigh R. Understanding the fluid nature of personhood - the ring theory of personhood. Bioethics. 2015;29(3):171–81.
Ryan M, Ryan M. Theorising a model for teaching and assessing reflective learning in higher education. High Educ Res Dev. 2013;32(2):244–57.
Huang H, Toh RQE, Chiang CLL, Thenpandiyan AA, Vig PS, Lee RWL, et al. Impact of dying neonates on doctors’ and nurses’ personhood: a systematic scoping review. J Pain Symptom Manag. 2022;63(1):e59–74.
Vig PS, Lim JY, Lee RW, Huang H, Tan XH, Lim WQ, et al. Parental bereavement–impact of death of neonates and children under 12 years on personhood of parents: a systematic scoping review. BMC Palliat Care. 2021;20(1):1–7.
Chan NPX, Chia JL, Ho CY, Ngiam LXL, Kuek JTY, Ahmad Kamal NHB, et al. Extending the ring theory of personhood to the care of dying patients in intensive care units. Asian Bioeth Rev. 2022;14(1):71–86.
Tay J, Compton S, Phua G, Zhuang Q, Neo S, Lee G, et al. Perceptions of healthcare professionals towards palliative care in internal medicine wards: a cross-sectional survey. BMC Palliat Care. 2021;20(1):101.
Teo YH, Peh TY, Abdurrahman A, Lee ASI, Chiam M, Fong W, et al. A modified Delphi approach to enhance nurturing of professionalism in postgraduate medical education in Singapore. Singap Med J. 2021. https://doi.org/10.11622/smedj.2021224 .
Chiam M, Ho CY, Quah E, Chua KZY, Ng CWH, Lim EG, et al. Changing self-concept in the time of COVID-19: a close look at physician reflections on social media. Philos Ethics Humanit Med. 2022;17(1):1.
Zhou JX, Goh C, Chiam M, Krishna LKR. Painting and Poetry From a Bereaved Family and the Caring Physician. J Pain Symptom Manage. 2022;S0885-3924(22):00476-6.
Cheong CWS, Quah ELY, Chua KZY, Lim WQ, Toh RQE, Chiang CLL, et al. Post graduate remediation programs in medicine: a scoping review. BMC Med Educ. 2022;22(1):294.
Goh S, Wong RSM, Quah ELY, Chua KZY, Lim WQ, Ng ADR, et al. Mentoring in palliative medicine in the time of covid-19: a systematic scoping review. BMC Med Educ. 2022;22(1):359.
Venktaramana V, Loh EKY, Wong CJW, Yeo JW, Teo AYT, Chiam CSY, et al. A systematic scoping review of communication skills training in medical schools between 2000 and 2020. Med Teach. 2022;44(9):997-1006.
Chia EW, Huang H, Goh S, Peries MT, Lee CC, Tan LH, et al. A systematic scoping review of teaching and evaluating communications in the intensive care unit. Asia Pac Schol. 2021;6(1):3–29.
Toh RQE, Koh KK, Lua JK, Wong RSM, Quah ELY, Panda A, et al. The role of mentoring, supervision, coaching, teaching and instruction on professional identity formation: a systematic scoping review. BMC Med Educ. 2022;22(1):531.
Charon R, Hermann N. Commentary: a sense of story, or why teach reflective writing? Acad Med. 2012;87(1):5–7.
Matinho D, Pietrandrea M, Echeverria C, Helderman R, Masters M, Regan D, et al. A systematic review of integrated learning definitions, frameworks, and practices in recent health professions education literature. Educ Sci. 2022;12(3):165.
Saltman DC, Tavabie A, Kidd MR. The use of reflective and reasoned portfolios by doctors. J Eval Clin Pract. 2012;18(1):182–5.
Kinsella EA. Technical rationality in Schön’s reflective practice: dichotomous or non-dualistic epistemological position. Nurs Philos. 2007;8(2):102–13.
Tsingos C, Bosnic-Anticevich S, Smith L. Reflective practice and its implications for pharmacy education. Am J Pharm Educ. 2014;78(1):18.
Arntfield S, Parlett B, Meston CN, Apramian T, Lingard L. A model of engagement in reflective writing-based portfolios: interactions between points of vulnerability and acts of adaptability. Med Teach. 2016;38(2):196–205.
Edgar L, et al. ACGME: the milestones guidebook. 2020. Available from: https://www.acgme.org/globalassets/milestonesguidebook.pdf .
Council GM. Tomorrow’s doctors. 2009. Available from: http://www.ub.edu/medicina_unitateducaciomedica/documentos/TomorrowsDoctors_2009.pdf .
Council GM. The reflective practitioner - guidance for doctors and medical students. Available from: https://www.gmc-uk.org/education/standards-guidance-and-curricula/guidance/reflective-practice/the-reflective-practitioner-guidance-for-doctors-and-medical-students . Accessed 3 Aug 2022.
England RCoSo. Good surgical practice. Available from: https://www.rcseng.ac.uk/standards-and-research/gsp/ . Accessed 3 Aug 2022.
Physicians TRACo. The Royal Australasian College of Physicians basic training curriculum standards: competencies. 2017. Available from: https://www.racp.edu.au/docs/default-source/default-document-library/competencies-for-basic-trainees-in-adult-internal-medicine-and-paediatrics-child-health.pdf?sfvrsn=6fdc0d1a_4 .
Surgeons RACo. RACS competencies. Available from: https://www.surgeons.org/en/Trainees/the-set-program/racs-competencies . Accessed 3 Aug 2022.
Murdoch-Eaton D, Sandars J. Reflection: moving from a mandatory ritual to meaningful professional development. Arch Dis Child. 2014;99(3):279–83.
Thompson N, Pascal J. Developing critically reflective practice. Reflective Pract. 2012;13(2):311–25.
Rodgers C. Defining reflection: another look at John Dewey and reflective thinking. Teach Coll Rec. 2002;104:842–66.
Hinchcliff R, Greenfield D, Moldovan M, Westbrook JI, Pawsey M, Mumford V, et al. Narrative synthesis of health service accreditation literature. BMJ Qual Saf. 2012;21(12):979–91.
Boden C, Ascher MT, Eldredge JD. Learning while doing: program evaluation of the medical library association systematic review project. J Med Libr Assoc. 2018;106(3):284.
Mays N, Roberts E, Popay J. Synthesising research evidence. Studying the organisation and delivery of health services: research methods; 2001. p. 220.
Davey S, Davey A, Singh J. Metanarrative review: current status and opportunities for public health research. Int J Health Syst Disaster Manag. 2013;1(2):59–63.
Greenhalgh T, Wong G. Training materials for meta-narrative reviews. UK: Global Health Innovation and Policy Unit Centre for Primary Care and Public Health Blizard Institute, Queen Mary University of London; 2013.
Osama T, Brindley D, Majeed A, Murray KA, Shah H, Toumazos M, et al. Teaching the relationship between health and climate change: a systematic scoping review protocol. BMJ Open. 2018;8(5):e020330.
Chua KZY, Quah ELY, Lim YX, Goh CK, Lim J, Wan DWJ, et al. A systematic scoping review on patients’ perceptions of dignity. BMC Palliat Care. 2022;21(1):118.
Hong DZ, Lim AJS, Tan R, Ong YT, Pisupati A, Chong EJX, et al. A systematic scoping review on portfolios of medical educators. J Med Educ Curric Dev. 2021;8:23821205211000356.
Tay KT, Ng S, Hee JM, Chia EWY, Vythilingam D, Ong YT, et al. Assessing professionalism in medicine - a scoping review of assessment tools from 1990 to 2018. J Med Educ Curric Dev. 2020;7:2382120520955159.
Lim C, Zhou JX, Woong NL, Chiam M, Krishna LKR. Addressing the needs of migrant workers in ICUs in Singapore. J Med Educ Curric Dev. 2020;7:2382120520977190.
Ong YT, Quek CWN, Pisupati A, Loh EKY, Venktaramana V, Chiam M, et al. Mentoring future mentors in undergraduate medical education. PLoS One. 2022;17(9):e0273358.
Kuek JTY, Ngiam LXL, Kamal NHA, Chia JL, Chan NPX, Abdurrahman ABHM, et al. The impact of caring for dying patients in intensive care units on a physician’s personhood: a systematic scoping review. Philos Ethics Humanit Med. 2020;15(1):12.
Ngiam L, Ong YT, Ng JX, Kuek J, Chia JL, Chan N, et al. Impact of caring for terminally ill children on physicians: a systematic scoping review. Am J Hosp Palliat Care. 2021;38(4):396–418.
Ho CY, Lim N-A, Ong YT, Lee ASI, Chiam M, Gek GPL, et al. The impact of death and dying on the personhood of senior nurses at the National Cancer Centre Singapore (NCCS): a qualitative study. BMC Palliat Care. 2022;21(1):1–10.
Quah ELY, Chua KZY, Lua JK, Wan DWJ, Chong CS, Lim YX, et al. A systematic review of stakeholder perspectives of dignity and assisted dying. J Pain Symptom Manag. 2022. https://doi.org/10.1016/j.jpainsymman.2022.10.004 .
Quek CWN, Ong RRS, Wong RSM, Chan SWK, Chok AK-L, Shen GS, et al. Systematic scoping review on moral distress among physicians. BMJ Open. 2022;12(9):e064029.
Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: meta-narrative reviews. BMC Med. 2013;11(1):20.
Pring R. The ‘false dualism’of educational research. J Philos Educ. 2000;34(2):247–60.
Crotty M. The foundations of social research: meaning and perspective in the research process. Thousand Oaks: SAGE; 1998.
Ford K. Taking a narrative turn: possibilities, challenges and potential outcomes. OnCUE J. 2012;6(1):23-36.
Schick-Makaroff K, MacDonald M, Plummer M, Burgess J, Neander W. What synthesis methodology should I use? A review and analysis of approaches to research synthesis. AIMS Public Health. 2016;3:172–215.
Peters M, Godfrey C, McInerney P, Soares C, Khalil H, Parker D. The Joanna Briggs Institute reviewers’ manual 2015: methodology for JBI scoping reviews2015 April 29, 2019. Available from: http://joannabriggs.org/assets/docs/sumari/Reviewers-Manual_Methodology-for-JBI-Scoping-Reviews_2015_v1.pdf .
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6.
Sandelowski M, Barroso J. Handbook for synthesizing qualitative research. New York: Springer; 2007.
Chua WJ, Cheong CWS, Lee FQH, Koh EYH, Toh YP, Mason S, et al. Structuring mentoring in medicine and surgery. A systematic scoping review of mentoring programs between 2000 and 2019. J Contin Educ Health Prof. 2020;40(3):158–68.
Ng YX, Koh ZYK, Yap HW, Tay KT, Tan XH, Ong YT, et al. Assessing mentoring: a scoping review of mentoring assessment tools in internal medicine between 1990 and 2019. PLoS One. 2020;15(5):e0232511.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Cassol H, Pétré B, Degrange S, Martial C, Charland-Verville V, Lallier F, et al. Qualitative thematic analysis of the phenomenology of near-death experiences. PLoS One. 2018;13(2):e0193001.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Wald H, Reis S. Beyond the margins: fostering reflective capacity through reflective writing in medical education. J Gen Int Med. 2010;25:746–9.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme version, vol. 1; 2006. p. b92.
France EF, Wells M, Lang H, Williams B. Why, when and how to update a meta-ethnography qualitative synthesis. Syst Rev. 2016;5:44.
Noblit GW, Hare RD, Hare RD. Meta-ethnography: synthesizing qualitative studies. Newbury Park: Sage Publications; 1988.
Book Google Scholar
Gibbs G. Learning by doing: a guide to teaching and learning methods. Thousand Oaks: FEU; 1988.
Koole S, Dornan T, Aper L, Scherpbier A, Valcke M, Cohen-Schotanus J, et al. Factors confounding the assessment of reflection: a critical review. BMC Med Educ. 2011;11(1):104.
Day C. Reflection: A Necessary but Not Sufficient Condition for Professional Development. British Educational Research Journal. 1993;19(1):83–93.
Sweet L, Bass J, Sidebotham M, Fenwick J, Graham K. Developing reflective capacities in midwifery students: enhancing learning through reflective writing. Women Birth. 2019;32(2):119–26.
Mezirow J. Understanding transformation theory. Adult Educ Q. 1994;44(4):222–32.
Korthagen F, Vasalos A. Levels in reflection: core reflection as a means to enhance professional growth. Teach Teach. 2005;11(1):47–71.
McLeod N. Reflecting on reflection: improving teachers’ readiness to facilitate participatory learning with young children. Prof Dev Educ. 2015;41(2):254–72.
Ash SL, Clayton PH. The articulated learning: an approach to guided reflection and assessment. Innov High Educ. 2004;29(2):137–54.
Ash S, Clayton P. Generating, deepening, and documenting learning: the power of critical reflection in applied learning. J Appl Learn High Educ. 2009;1:25–48.
Lay K, McGuire L. Teaching students to deconstruct life experience with addictions: a structured reflection exercise. J Teach Addict. 2008;7(2):145–63.
Lay K, McGuire L. Building a lens for critical reflection and reflexivity in social work education. Soc Work Educ. 2010;29(5):539–50.
Johns C. Nuances of reflection. J Clin Nurs. 1994;3(2):71–4.
Kim HS. Critical reflective inquiry for knowledge development in nursing practice. J Adv Nurs. 1999;29(5):1205–12.
Roskos K, Vukelich C, Risko V. Reflection and learning to teach reading: a critical review of literacy and general teacher education studies. J Lit Res. 2001;33:595–635.
Burnham J. Developments in Social GGRRAAACCEEESSS: visible-invisible, voiced-unvoiced. In I. Krause (Ed.), Cultural Reflexivity. London: Karnac.
Pearson M, Smith D. In: Boud D, Keogh R, Walker D, editors. Debriefing in experience-based learning, reflection: turning experience into learning. London: Kogan Page; 1985.
Argyris C, Schön DA. Organizational learning: A theory of action perspective, Reading, Mass: Addison Wesley. 1978.
Mamede S, Schmidt HG. The structure of reflective practice in medicine. Med Educ. 2004;38(12):1302–8.
Ryan M. Improving reflective writing in higher education: a social semiotic perspective. Teach High Educ. 2011;16(1):99–111.
Beauchamp C. Understanding reflection in teaching: a framework for analyzing the literature; 2006.
Atkins S, Murphy K. Reflection: a review of the literature. J Adv Nurs. 1993;18(8):1188–92.
Carver CS, Scheier MF. On the self-regulation of behavior, vol. xx. New York: Cambridge University Press; 1998. p. 439–xx.
Grant A. The impact of life coaching on goal attainment, metacognition and mental health. Soc Behav Personal Int J. 2003;31:253–63.
Thorpe K. Reflective learning journals: from concept to practice. Reflective Pract. 2004;5(3):327–43.
van Manen M. The tact of teaching: the meaning of pedagogical thoughtfulness. NY: SUNY Press; 1991a.
Plack MM, Driscoll M, Marquez M, Cuppernull L, Maring J, Greenberg L. Assessing reflective writing on a pediatric clerkship by using a modified Bloom’s taxonomy. Ambul Pediatr. 2007;7(4):285–91.
Rogers J, Peecksen S, Douglas M, Simmons M. Validation of a reflection rubric for higher education. Reflective Pract. 2019;20(6):761–76.
Makarem NN, Saab BR, Maalouf G, Musharafieh U, Naji F, Rahme D, et al. Grading reflective essays: the reliability of a newly developed tool- GRE-9. BMC Med Educ. 2020;20(1):331.
Bain J, Ballantyne R, Mills C, Lester N. Reflecting on practice: student teachers’ perspectives; 2002.
Kember D, Leung DYP, Jones A, Loke AY, McKay J, Sinclair K, et al. Development of a questionnaire to measure the level of reflective thinking. Assess Eval High Educ. 2000;25(4):381–95.
Hatton N, Smith D. Reflection in teacher education: towards definition and implementation. Teach Teach Educ. 1995;11(1):33–49.
Moon JA. Reflection in learning and professional development: theory and practice; 1999.
Wald HS, Borkan JM, Taylor JS, Anthony D, Reis SP. Fostering and evaluating reflective capacity in medical education: developing the REFLECT rubric for assessing reflective writing. Acad Med. 2012;87(1):41–50.
Stein D. Teaching critical reflection. Myths and realities no. 7. Undefined; 2000. p. 1–4.
Morrow E. Teaching critical reflection. Teach High Educ. 2011;16:211–23.
Plack MM, Driscoll M, Blissett S, McKenna R, Plack TP. A method for assessing reflective journal writing. J Allied Health. 2005;34(4):199–208.
Aukes LC, Geertsma J, Cohen-Schotanus J, Zwierstra RP, Slaets JP. The development of a scale to measure personal reflection in medical practice and education. Med Teach. 2007;29(2–3):177–82.
Bradley J. A model for evaluating student learning in academically based service. In: Connecting cognition and action: evaluation of student performance in service learning courses; 1995. p. 13–26.
Lee H-J. Understanding and assessing preservice teachers’ reflective thinking. Teach Teach Educ. 2005;21(6):699–715.
Kanthan R, Senger JL. An appraisal of students’ awareness of “self-reflection” in a first-year pathology course of undergraduate medical/dental education. BMC Med Educ. 2011;11:67.
Kassab SE, Bidmos M, Nomikos M, Daher-Nashif S, Kane T, Sarangi S, et al. Construct validity of an instrument for assessment of reflective writing-based portfolios of medical students. Adv Med Educ Pract. 2020;11:397–404.
Pavlovich K. The development of reflective practice through student journals. High Educ Res Dev. 2007;26(3):281–95.
Sukhato K, Sumrithe S, Wongrathanandha C, Hathirat S, Leelapattana W, Dellow A. To be or not to be a facilitator of reflective learning for medical students? A case study of medical teachers’ perceptions of introducing a reflective writing exercise to an undergraduate curriculum. BMC Med Educ. 2016;16:102.
Tuncer H, Özkan Y. A case study on assessing reflectivity levels of pre-service language teachers through journals. Novitas-ROYAL Res Youth Lang. 2018;12(2):173–86.
Albanese MA. Crafting the reflective lifelong learner: why, what and how. Med Educ. 2006;40(4):288–90.
Ament Giuliani Franco C, Franco RS, Cecilio-Fernandes D, Severo M, Ferreira MA, de Carvalho-Filho MA. Added value of assessing medical students’ reflective writings in communication skills training: a longitudinal study in four academic centres. BMJ Open. 2020;10(11):e038898.
Embo MP, Driessen E, Valcke M, Van Der Vleuten CP. Scaffolding reflective learning in clinical practice: a comparison of two types of reflective activities. Med Teach. 2014;36(7):602–7.
Kasman DL. “Doctor, are you listening?” A writing and reflection workshop. Fam Med. 2004;36(8):549–52.
Locher M, Koenig R, Meier J. A genre analysis of reflective writing texts by English medical students. In: Narrative matters in medical contexts across disciplines. Amsterdam: John Benjamins; 2015. p. 141–64.
Miller Juve AK, Kirsch JR. Does participation in written guided reflective practice exercises affect readiness for self-directed learning in a sample of US anesthesiology residents? J Educ Perioper Med. 2019;21(2):E622.
Krueger RB, Sweetman MM, Martin M, Cappaert TA. Self-reflection as a support to evidence-based practice: a grounded theory exploration. Occup Ther Health Care. 2020;34(4):320–50.
Wegner C, Remmert K, Ohlberger S. Evaluation of a wiki for lesson reflection in the project “Kolumbus-Kids” at Bielefeld University. Electron J Sci Educ. 2017;21(4):1–40.
Too WK. Facilitating the development of pre-service teachers as reflective learners: a Malaysian experience. Lang Learn J. 2013;41(2):161–74.
Tsingos C, Bosnic-Anticevich S, Lonie JM, Smith L. A model for assessing reflective practices in pharmacy education. Am J Pharm Educ. 2015;79(8):124.
Eriksen M. Facilitating authentic becoming. J Manag Educ. 2012;36(5):698–736.
Henderson E, Berlin A, Freeman G, Fuller J. Twelve tips for promoting significant event analysis to enhance reflection in undergraduate medical students; 2002. p. 121–4.
Rosenbaum ME, Lobas J, Ferguson K. Using reflection activities to enhance teaching about end-of-life care. J Palliat Med. 2005;8(6):1186–95.
Bernard AW, Gorgas D, Greenberger S, Jacques A, Khandelwal S. The use of reflection in emergency medicine education. Acad Emerg Med. 2012;19(8):978–82.
Nagano H, Obara H, Takayama Y. A brief home-based palliative care learning experience for medical students and resident doctors in Okinawa, Japan. PLoS One. 2019;14(6):e0218780.
Zhu X. Student teachers’ reflection during practicum: plenty on action, few in action. Reflective Pract. 2011;12(6):763–75.
Jamil FM, Hamre BK. Teacher reflection in the context of an online professional development course: applying principles of cognitive science to promote teacher learning. Action Teach Educ. 2018;40(2):220–36.
Larsen DP, London DA, Emke AR. Using reflection to influence practice: student perceptions of daily reflection in clinical education. Perspect Med Educ. 2016;5(5):285–91.
Naeger DM, Hua EW, Ahearn B, Webb EM. Reflective writing: a potential tool to improve interprofessional teamwork with radiologists. Acad Radiol. 2015;22(10):1221–5.
Raut AV, Gupta SS. Reflection and peer feedback for augmenting emotional intelligence among undergraduate students: a quasi-experimental study from a rural medical college in central India. Educ Health (Abingdon). 2019;32(1):3–10.
Spector-Mersel G. Life story reflection in social work education: a practical model. J Soc Work Educ. 2017;53(2):286–99.
Martin M. Reflection in teacher education: how can it be supported? Educ Action Res. 2005;13(4):525–42.
Thomas PA, Goldberg H. Tracking reflective practice-based learning by medical students during an ambulatory clerkship. J Gen Intern Med. 2007;22(11):1583–6.
Kitchen M. Junior doctors’ guide to portfolio learning and building. Clin Teach. 2012;9(5):308–11.
Shoffner M. Informal reflection in pre-service teacher education. Reflective Pract. 2008;9(2):123–34.
Adams CL, Nestel D, Wolf P. Reflection: a critical proficiency essential to the effective development of a high competence in communication. J Vet Med Educ. 2006;33(1):58–64.
Moniz T, Arntfield S, Miller K, Lingard L, Watling C, Regehr G. Considerations in the use of reflective writing for student assessment: issues of reliability and validity. Med Educ. 2015;49(9):901-8.
Ottenberg AL, Pasalic D, Bui GT, Pawlina W. An analysis of reflective writing early in the medical curriculum: the relationship between reflective capacity and academic achievement. Med Teach. 2016;38(7):724–9.
Miller-Kuhlmann R, O'Sullivan PS, Aronson L. Essential steps in developing best practices to assess reflective skill: A comparison of two rubrics. Med Teach. 2016;38(1):75-81.
Khanna R, Singh RK, Singhal R. Reflective learning for behavioral guidance in pediatric dentistry. J Indian Soc Pedod Prev Dent. 2020;38(3):293–303.
Abdullah M. Promoting reflective thinking skills by using web 2.0 application. Online Submission. 2015:1–15.
Ballon BC, Skinner W. “Attitude is a little thing that makes a big difference”: reflection techniques for addiction psychiatry training. Acad Psychiatry. 2008;32(3):218–24.
Brown A, Jauregui J, Ilgen JS, Riddell J, Schaad D, Strote J, et al. Does the medium matter? Evaluating the depth of reflective writing by medical students on social media compared to the traditional private essay using the REFLECT rubric. West J Emerg Med. 2020;21(1):18–25.
Chuang LL, Liu HW, Lin YC, Wang YW, Chu SY. Using structured narrative to help a medical student reflect on an unexpected clinical situation. Tzu Chi Med J. 2013;25(1):68–70.
Goldman JDG, Grimbeek P. Pre-service primary school teachers’ self-reflective competencies in their own teaching. Eur J Psychol Educ. 2015;30(2):189–207.
Liu GZ, Jawitz OK, Zheng D, Gusberg RJ, Kim AW. Reflective writing for medical students on the surgical clerkship: oxymoron or antidote? J Surg Educ. 2016;73(2):296–304.
Sellheim D, Weddle M. Using a collaborative course reflection process to enhance faculty and curriculum development. Coll Teach. 2015;63(2):52–61.
Shiozawa T, Glauben M, Banzhaf M, Griewatz J, Hirt B, Zipfel S, et al. An insight into professional identity formation: qualitative analyses of two reflection interventions during the dissection course. Anat Sci Educ. 2020;13(3):320–32.
Shaughnessy AF, Allen L, Duggan A. Attention without intention: explicit processing and implicit goal-setting in family medicine residents’ written reflections. Educ Prim Care. 2017;28(3):150–6.
Vicini A, Shaughnessy AF, Duggan AP. Cultivating the inner life of a physician through written reflection. Ann Fam Med. 2017;15(4):379–81.
Bruno A, Dell'Aversana G. Reflective practice for psychology students: the use of reflective journal feedback in higher education. Psychol Learn Teach. 2017;16(2):248–60.
DasGupta S, Charon R. Personal illness narratives: using reflective writing to teach empathy. Acad Med. 2004;79(4):351–6.
Etscheidt S, Curran CM, Sawyer CM. Promoting reflection in teacher preparation programs: a multilevel model. Teach Educ Spec Educ. 2012;35(1):7–26.
Eutsler L, Curcio R. Private blog reflections connecting course content with field experiences: preservice teachers grapple with teacher identity. Reflective Pract. 2019;20(2):250–65.
Freeman M. Reflective logs: an aid to clinical teaching and learning. Int J Lang Commun Disord. 2001;36(Suppl):411–6.
Wetmore AO, Boyd LD, Bowen DM, Pattillo RE. Reflective blogs in clinical education to promote critical thinking in dental hygiene students. J Dent Educ. 2010;74(12):1337–50.
Young MR. Reflection fosters deep learning: the ‘reflection page & relevant to you’ intervention. J Instr Pedagog. 2018;20:1–17.
Zoellner BP, Chant RH, Lee K. Do we do Dewey? Using a dispositional framework to examine reflection within internship professional development plans. Teach Educ. 2017;52(3):203–21.
Peterkin A, Roberts M, Kavanagh L, Havey T. Narrative means to professional ends: new strategies for teaching CanMEDS roles in Canadian medical schools. Can Fam Physician. 2012;58(10):e563–9.
Pavlovich K, Collins E, Jones G. Developing students’ skills in reflective practice: design and assessment. J Manag Educ. 2009;33(1):37–58.
Janson C, Filibert S. Discursive digital reflection: a method for enhancing supervision and training. References. 2018;2:200–12.
Glassburn S, McGuire LE, Lay K. Reflection as self-care: models for facilitative supervision. Reflective Pract. 2019;20(6):692–704.
Fischer MA, Haley HL, Saarinen CL, Chretien KC. Comparison of blogged and written reflections in two medicine clerkships. Med Educ. 2011;45(2):166–75.
Grant A, Kinnersley P, Metcalf E, Pill R, Houston H. Students’ views of reflective learning techniques: an efficacy study at a UK medical school. Med Educ. 2006;40(4):379–88.
Hargreaves K. Reflection in medical education. J Univ Teach Learn Pract. 2016;13(2):1–21.
Wald HS, Reis SP, Monroe AD, Borkan JM. ‘The loss of my elderly patient:’ interactive reflective writing to support medical students’ rites of passage. Med Teach. 2010;32(4):e178–84.
Hulsman RL, Harmsen AB, Fabriek M. Reflective teaching of medical communication skills with DiViDU: assessing the level of student reflection on recorded consultations with simulated patients. Patient Educ Couns. 2009;74(2):142–9.
Karnieli-Miller O, Palombo M, Meitar D. See, reflect, learn more: qualitative analysis of breaking bad news reflective narratives. Med Educ. 2018;52(5):497–512.
Stephens MB, Reamy BV, Anderson D, Olsen C, Hemmer PA, Durning SJ, et al. Writing, self-reflection, and medical school performance: the human context of health care. Mil Med. 2012;177(9 Suppl):26–30.
Biggerstaff MA. Social work ethics online: reflective learning. J Technol Hum Serv. 2005;23(3–4):245–57.
Campbell BH, Treat R, Johnson B, Derse AR. Creating reflective space for reflective and “unreflective” medical students: exploring seminal moments in a large-group writing session. Acad Med. 2020;95(6):882–7.
Coulehan J, Granek IA. Commentary: “I hope I’ll continue to grow”: rubrics and reflective writing in medical education. Acad Med. 2012;87(1):8–10.
McGuire L, Lay K, Peters J. Pedagogy of reflective writing in professional education. J Scholarsh Teach Learn. 2009;9(1):93–107.
Nurulhuda MH, Siti Norazlina J, Harmy MY, Norwati D, Hassan Basri M. Enhancing reflective writing through e-learning in undergraduate medical education; 2017.
Herrick-Reynolds K, Sewanan LR, Zheng DJ, Wang P, Encandela J, Shahu A, et al. A novel near-peer reflective writing workshop. Clin Teach. 2019;16(4):339–44.
Devi V, Abraham RR, Kamath U. Teaching and assessing reflecting skills among undergraduate medical students experiencing research. J Clin Diagn Res. 2017;11(1):Jc01–jc5.
Vivekananda-Schmidt P, Marshall M, Stark P, McKendree J, Sandars J, Smithson S. Lessons from medical students’ perceptions of learning reflective skills: a multi-institutional study. Med Teach. 2011;33(10):846–50.
Grierson L, Winemaker S, Taniguchi A, Howard M, Marshall D, Zazulak J. The reliability characteristics of the REFLECT rubric for assessing reflective capacity through expressive writing assignments: a replication study. Perspect Med Educ. 2020;9(5):281–5.
Charon R, Hermann N, Devlin MJ. Close reading and creative writing in clinical education: teaching attention, representation, and affiliation. Acad Med. 2016;91(3):345–50.
Coward M. Does the use of reflective models restrict critical thinking and therefore learning in nurse education? What have we done? Nurse Educ Today. 2011;31(8):883–6.
Dyke M. The role of the “other” in reflection, knowledge formation and action in a late modernity. Int J Lifelong Educ. 2006;25(2):105–23.
Nguyen QD, Fernandez N, Karsenti T, Charlin B. What is reflection? A conceptual analysis of major definitions and a proposal of a five-component model. Med Educ. 2014;48(12):1176–89.
Shaw R. A model of the transformative journey into reflexivity: an exploration into students’ experiences of critical reflection. Reflective Pract. 2013;14(3):319–35.
Xiao Q, Zhu P, Hsu MK, Zhuang W, Peltier J. Reflective learning in a Chinese MBA Programme: scale assessment and future recommendations. J Furth High Educ. 2016;40(1):1–22.
Yakov G, Riskin A, Flugelman AA. Mechanisms involved in the formation of professional identity by medical students. Med Teach. 2021;43(4):428–38.
Tan XH, Foo MA, Lim SLH, Lim MBXY, Chin AMC, Zhou J, et al. Teaching and assessing communication skills in the postgraduate medical setting: a systematic scoping review. BMC Med Educ. 2021;21(1):483.
Baldwin K, Lucas B. Promoting reflective practice skills for postgraduate GPs: do journals aid journeys? Educ Prim Care. 2012;23(3):213–6.
Chretien KC, Chheda SG, Torre D, Papp KK. Reflective writing in the internal medicine clerkship: a national survey of clerkship directors in internal medicine. Teach Learn Med. 2012;24(1):42–8.
McGlinn EP, Chung KC. A pause for reflection: incorporating reflection into surgical training. Ann Plast Surg. 2014;73(2):117–20.
Bjerkvik LK, Hilli Y. Reflective writing in undergraduate clinical nursing education: a literature review. Nurse Educ Pract. 2019;35:32–41.
Olex AL, DiazGranados D, McInnes BT, Goldberg S. Local topic mining for reflective medical writing. AMIA Summits Transl Sci Proc. 2020;2020:459.
Winkel AF, Yingling S, Jones AA, Nicholson J. Reflection as a learning tool in graduate medical education: a systematic review. J Grad Med Educ. 2017;9(4):430–9.
Carr S, Carmody D. Experiential learning in women’s health: medical student reflections. Med Educ. 2006;40(8):768–74.
Shapiro J, Kasman D, Shafer A. Words and wards: a model of reflective writing and its uses in medical education. J Med Humanit. 2006;27(4):231–44.
Dreyer A, Mlambo M, Mapukata-Sondzaba N. Medical students using the technique of 55-word stories to reflect on a 6-week rotation during the integrated primary care block. Afr J Health Prof Educ. 2021;13(2):135–9.
Malau-Aduli BS, Jones K, Smith AM, Sen Gupta T, Hays RB. Understanding medical students’ transformative experiences of early preclinical international rural placement over a 20-year period. BMC Med Educ. 2022;22(1):652.
Liao K-C, Peng C-H, Snell L, Wang X, Huang C-D, Saroyan A. Understanding the lived experiences of medical learners in a narrative medicine course: a phenomenological study. BMC Med Educ. 2021;21(1):321.
Bracken RC, Major A, Paul A, Ostherr K. Reflective writing about near-peer blogs: a novel method for introducing the medical humanities in premedical education. J Med Humanit. 2021;42(4):535–69.
Kind T, Everett VR, Ottolini M. Learning to connect: students’ reflections on doctor-patient interactions. Patient Educ Couns. 2009;75(2):149–54.
Piumatti G, Guttormsen S, Zurbuchen B, Abbiati M, Gerbase MW, Baroffio A. Trajectories of learning approaches during a full medical curriculum: impact on clinical learning outcomes. BMC Med Educ. 2021;21(1):370.
Smith E. Teaching critical reflection. Teach High Educ. 2011;16(2):211–23.
Talarico S, Zubairi M, Daneman D, Punnett A, Martimianakis MAT. Fostering transformative learning in a social pediatrics research summer studentship. Acad Med. 2019;94(5):692–6.
Cox E. Adult learners learning from experience: using a reflective practice model to support work-based learning. Reflective Pract. 2005;6(4):459–72.
Yaylaci S, Ulman YI, Vatansever K, Senyurek G, Turkmen S, Aldinc H, et al. Integrating patient management, reflective practice, and ethical decision-making in an emergency medicine intern boot camp. BMC Med Educ. 2021;21(1):536.
Williams E, Jarrell JA, Rubenstein J. A week in the life: pediatric palliative care through the eyes of a medical student. Children (Basel). 2021;8(11):971.
Dhaliwal U, Singh S, Singh N. Reflective student narratives: honing professionalism and empathy. Indian J Med Ethics. 2018;3(1):9–15.
Janssen F, de Hullu E, Tigelaar D. Using a domain-specific model to improve student teachers’ reflections on positive teaching experiences. Action Teach Educ. 2009;31(2):86–98.
Curtis P, Gorolay S, Curtis A, Harris M. What do general practitioners think of written reflection? A focus group study. Educ Prim Care. 2016;27(4):292–8.
Dalsgaard C. Reflective mediation: toward a sociocultural conception of situated reflection. Frontline Learn Res. 2020;8(1):1–13.
Sheikh F, Gathecha E, Arbaje AI, Christmas C. Internal medicine residents’ views about care transitions: results of an educational intervention. J Med Educ Curric Dev. 2021;8:2382120520988590.
Tashiro J, Shimpuku Y, Naruse K, Maftuhah, Matsutani M. Concept analysis of reflection in nursing professional development. Jpn. J Nurs Sci. 2013;10(2):170–9.
Vettraino E, Linds W, Downie H. Embodied reflexivity: discerning ethical practice through the six-part story method. Reflective Pract. 2019;20(2):218–33.
Standal Ø, Rugseth G. Practicum in adapted physical activity: a Dewey-inspired action research project. Adapt Phys Act Q. 2014;31(3):219–39.
Ekebergh M. Lifeworld-based reflection and learning: a contribution to the reflective practice in nursing and nursing education. Reflective Pract. 2007;8(3):331–43.
Farrell TSC. Reflecting on reflective practice: (re)visiting Dewey and Schon. TESOL J. 2012;3(1):7–16.
Curtis P, Taylor G, Riley R, Pelly T, Harris M. Written reflection in assessment and appraisal: GP and GP trainee views. Educ Prim Care. 2017;28(3):141–9.
Cunningham H, Taylor DS, Desai UA, Ender KL, Glickstein J, Krishnan US, et al. Reading the self: medical students’ experience of reflecting on their writing over time. Acad Med. 2021;96(8):1168–74.
Asselin ME. Reflective narrative: a tool for learning through practice. J Nurses Staff Dev. 2011;27(1):2–6.
Smith J. Sailing through social LA GRRAACCEESS: tool for deconstructing and facilitating reflective and reflexive practice. Reflective Pract. 2016;17(5):570–82.
Hudson JN, Rienits H, Corrin L, Olmos M. An innovative OSCE clinical log station: a quantitative study of its influence on Log use by medical students. BMC Med Educ. 2012;12:111.
Song P, Stewart R. Reflective writing in medical education. Med Teach. 2012;34(11):955–6.
Jackson P. Understanding the experience of experience: a practical model of reflective practice for Coaching. International Journal of Evidence Based Coaching and Mentoring. 2004;2(1):57–67.
Meilijson S, Katzenberger I. A clinical education program for speech-language pathologists applying reflective practice, evidence-based practice and case-based learning. Folia Phoniatr Logop. 2017;66(4–5):158–63.
Shaughnessy AF, Duggan AP. Family medicine residents’ reactions to introducing a reflective exercise into training. Educ Health (Abingdon). 2013;26(3):141–6.
Boudreau JD, Liben S, Fuks A. A faculty development workshop in narrative-based reflective writing. Perspect Med Educ. 2012;1(3):143–54.
Rees CE, Shepherd M, Chamberlain S. The utility of reflective portfolios as a method of assessing first year medical students’ personal and professional development. Reflective Pract. 2005;6(1):3–14.
Glod SA, Richard D, Gordon P, Fecile ML, Kees-Folts D, Kreher M, et al. A curriculum for clerkship students to foster professionalism through reflective practice and identity formation. MedEdPORTAL. 2016;12:10416.
Pieters J, Verstegen DML, Dolmans DHJM, Warmenhoven FC, van den Beuken-van Everdingen MHJ. Design and evaluation of a learning assignment in the undergraduate medical curricula on the four dimensions of care: a mixed method study. BMC Med Educ. 2021;21(1):309.
Driessen EW, van Tartwijk J, Overeem K, Vermunt JD, van der Vleuten CP. Conditions for successful reflective use of portfolios in undergraduate medical education. Med Educ. 2005;39(12):1230–5.
Prosser M, Stephenson T, Mathur J, Enayati H, Kadie A, Abdi MM, et al. Reflective practice and transcultural psychiatry peer e-learning between Somaliland and the UK: a qualitative evaluation. BMC Med Educ. 2021;21(1):58.
Hayton A, Kang I, Wong R, Loo LK. Teaching medical students to reflect more deeply. Teach Learn Med. 2015;27(4):410–6.
Roberts P. Reflection: a renewed and practical focus for an existing problem in teacher education. Aust J Teach Educ. 2016;41(7):19–35.
Soemantri D, Mustika R, Greviana N. Inter-rater reliability of reflective-writing assessment in an undergraduate professionalism course in medical education. Educ Med J. 2022;14(1).
Reynolds M. Reflective practice: origins and interpretations, Action Learning: Research and Practice. 2011;8(1):5–13.
Warner R, Picard M. What do Master’s students’ structured reflections say about the learning processes involved in commencing a research project? J Univ Teach Learn Pract. 2020;17(1):7.
Collin S, Karsenti T, Komis V. Reflective practice in initial teacher training: critiques and perspectives. Reflective Pract. 2013;14(1):104–17.
Rajhans V, Eichler R, Sztrigler Cohen O, Gordon-Shaag A. A novel method of enhancing students’ involvement in reflective writing. Clin Teach. 2021;18(2):174–9.
Goodyear HM, Bindal T, Wall D. How useful are structured electronic portfolio templates to encourage reflective practice? Med Teach. 2013;35(1):71–3.
Tawanwongsri W, Phenwan T. Reflective and feedback performances on Thai medical students’ patient history-taking skills. BMC Med Educ. 2019;19(1):141.
Mohammadi E, Mirzazadeh A, Shahsavari H, Sohrabpour AA. Clinical teachers’ perceptions of role modeling: a qualitative study. BMC Med Educ. 2021;21(1):261.
Hastami Y, Claramita M, Suryadi E. Reflective writing skills of undergraduate medical students. eJournal Kedokteran Indonesia. 2018;6(2):97-104.
Swan Sein A, Rashid H, Meka J, Amiel J, Pluta W. Twelve tips for embedding assessment for and as learning practices in a programmatic assessment system. Med Teach. 2021;43(3):300–6.
Sternlieb JL. A guide to introducing and integrating reflective practices in medical education. Int J Psychiatry Med. 2015;49(1):95–105.
Sieben JM, Heeneman S, Verheggen MM, Driessen EW. Can concept mapping support the quality of reflections made by undergraduate medical students? A mixed method study. Med Teach. 2021;43(4):388–96.
Tan R, Qi Ting JJ, Zhihao Hong D, Sing Lim AJ, Ong YT, Pisupati A, et al. Medical student portfolios: a systematic scoping review. J Med Educ Curric Dev. 2022;9:23821205221076022.
Ong RSR, Wong RSM, Chee RCH, Quek CWN, Burla N, Loh CYL, et al. A systematic scoping review moral distress amongst medical students. BMC Med Educ. 2022;22(1):466.
Schaepkens SPC, Veen M, de la Croix A. Is reflection like soap? a critical narrative umbrella review of approaches to reflection in medical education research. Adv Health Sci Educ Theory Pract. 2022;27(2):537–51.
Merlo G, Ryu H, Harris TB, Coverdale J. MPRO: a professionalism curriculum to enhance the professional identity formation of university premedical students. Med Educ Online. 2021;26(1):1886224.
Whipp JL. Scaffolding critical reflection in online discussions: helping prospective teachers think deeply about field experiences in urban schools. J Teach Educ. 2003;54(4):321–33.
Artioli G, Deiana L, De Vincenzo F, Raucci M, Amaducci G, Bassi MC, et al. Health professionals and students’ experiences of reflective writing in learning: a qualitative meta-synthesis. BMC Med Educ. 2021;21(1):394.
Sagin A, Ellman MS, Shariff RR, Jones CA, Tindall K, Siropaides CH. A multicenter qualitative analysis of medical student narratives after a palliative care elective. Am J Hosp Palliat Care. 2021;38(9):1126–34.
Park KH, Kam BS, Yune SJ, Lee SY, Im SJ. Changes in self-reflective thinking level in writing and educational needs of medical students: a longitudinal study. PLoS One. 2022;17(1):e0262250.
Rozental L, Meitar D, Karnieli-Miller O. Medical students’ experiences and needs from written reflective journal feedback. Med Educ. 2021;55(4):505–17.
Download references
Acknowledgements
The authors would like to dedicate this paper to the late Dr. S Radha Krishna and A/Prof Cynthia Goh whose advice and ideas were integral to the success of this review and Thondy and Maia Olivia whose lives continue to inspire us.
The authors would also like to thank the anonymous reviewers, Dr. Ruaraidh Hill and Dr. Stephen Mason for their helpful comments which greatly enhanced this manuscript.
No funding was received for this review.
Author information
Authors and affiliations.
Yong Loo Lin School of Medicine, National University of Singapore, NUHS Tower Block, 1E Kent Ridge Road, Level 11, Singapore, 119228, Singapore
Jia Yin Lim, Chester Yan Hao Ng, Karis Li En Chan, Song Yi Elizabeth Anne Wu, Wei Zheng So, Glenn Jin Chong Tey, Yun Xiu Lam, Nicholas Lu Xin Gao, Yun Xue Lim, Ryan Yong Kiat Tay, Ian Tze Yong Leong & Lalit Kumar Radha Krishna
Division of Supportive and Palliative Care, National Cancer Centre Singapore, 11 Hospital Crescent, Singapore, 169610, Singapore
Jia Yin Lim, Chester Yan Hao Ng, Karis Li En Chan, Song Yi Elizabeth Anne Wu, Wei Zheng So, Glenn Jin Chong Tey, Yun Xiu Lam, Nicholas Lu Xin Gao, Yun Xue Lim, Ryan Yong Kiat Tay, Ian Tze Yong Leong, Gillian Li Gek Phua, Vengadasalam Murugam, Eng Koon Ong & Lalit Kumar Radha Krishna
Division of Medical Oncology, National Cancer Centre Singapore, 11 Hospital Crescent, Singapore, 169610, Singapore
Simon Yew Kuang Ong
Division of Cancer Education, National Cancer Centre Singapore, 11 Hospital Crescent, Singapore, 169610, Singapore
Simon Yew Kuang Ong, Nur Diana Abdul Rahman, Min Chiam, Eng Koon Ong & Lalit Kumar Radha Krishna
Duke-NUS Medical School, National University of Singapore, 8 College Rd, Singapore, 169857, Singapore
Simon Yew Kuang Ong, Gillian Li Gek Phua, Vengadasalam Murugam, Eng Koon Ong & Lalit Kumar Radha Krishna
Medical Social Services, Singapore General Hospital, Outram Rd, Singapore, 169608, Singapore
Crystal Lim
Lien Centre for Palliative Care, Duke-NUS Medical School, National University of Singapore, 8 College Rd, Singapore, 169857, Singapore
Gillian Li Gek Phua
Assisi Hospice, 832 Thomson Rd, Singapore, 574627, Singapore
Eng Koon Ong
Palliative Care Institute Liverpool, Academic Palliative & End of Life Care Centre, Cancer Research Centre, University of Liverpool, 200 London Road, Liverpool, L3 9TA, UK
Lalit Kumar Radha Krishna
PalC, The Palliative Care Centre for Excellence in Research and Education, PalC c/o Dover Park Hospice, 10 Jalan Tan Tock Seng, Singapore, 308436, Singapore
You can also search for this author in PubMed Google Scholar
Contributions
All authors were involved in data curation, formal analysis, investigation, preparing the original draft of the manuscript as well as reviewing and editing the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Lalit Kumar Radha Krishna .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
All authors have no competing interests for this review.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Guide to Reflective Writing.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lim, J.Y., Ong, S.Y.K., Ng, C.Y.H. et al. A systematic scoping review of reflective writing in medical education. BMC Med Educ 23 , 12 (2023). https://doi.org/10.1186/s12909-022-03924-4
Download citation
Received : 10 August 2022
Accepted : 25 November 2022
Published : 09 January 2023
DOI : https://doi.org/10.1186/s12909-022-03924-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Reflective writing
- Medical education
- Professional identity formation
- Undergraduate medical education
- Postgraduate medical education
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Guide on How to Write a Reflection Paper with Free Tips and Example

A reflection paper is a very common type of paper among college students. Almost any subject you enroll in requires you to express your opinion on certain matters. In this article, we will explain how to write a reflection paper and provide examples and useful tips to make the essay writing process easier.
Reflection papers should have an academic tone yet be personal and subjective. In this paper, you should analyze and reflect upon how an experience, academic task, article, or lecture shaped your perception and thoughts on a subject.
Here is what you need to know about writing an effective critical reflection paper. Stick around until the end of our guide to get some useful writing tips from the writing team at EssayPro — a research paper writing service
What Is a Reflection Paper
A reflection paper is a type of paper that requires you to write your opinion on a topic, supporting it with your observations and personal experiences. As opposed to presenting your reader with the views of other academics and writers, in this essay, you get an opportunity to write your point of view—and the best part is that there is no wrong answer. It is YOUR opinion, and it is your job to express your thoughts in a manner that will be understandable and clear for all readers that will read your paper. The topic range is endless. Here are some examples: whether or not you think aliens exist, your favorite TV show, or your opinion on the outcome of WWII. You can write about pretty much anything.
There are three types of reflection paper; depending on which one you end up with, the tone you write with can be slightly different. The first type is the educational reflective paper. Here your job is to write feedback about a book, movie, or seminar you attended—in a manner that teaches the reader about it. The second is the professional paper. Usually, it is written by people who study or work in education or psychology. For example, it can be a reflection of someone’s behavior. And the last is the personal type, which explores your thoughts and feelings about an individual subject.
However, reflection paper writing will stop eventually with one very important final paper to write - your resume. This is where you will need to reflect on your entire life leading up to that moment. To learn how to list education on resume perfectly, follow the link on our dissertation writing services .
Unlock the potential of your thoughts with EssayPro . Order a reflection paper and explore a range of other academic services tailored to your needs. Dive deep into your experiences, analyze them with expert guidance, and turn your insights into an impactful reflection paper.

Free Reflection Paper Example
Now that we went over all of the essentials about a reflection paper and how to approach it, we would like to show you some examples that will definitely help you with getting started on your paper.
Reflection Paper Format
Reflection papers typically do not follow any specific format. Since it is your opinion, professors usually let you handle them in any comfortable way. It is best to write your thoughts freely, without guideline constraints. If a personal reflection paper was assigned to you, the format of your paper might depend on the criteria set by your professor. College reflection papers (also known as reflection essays) can typically range from about 400-800 words in length.
Here’s how we can suggest you format your reflection paper:

How to Start a Reflection Paper
The first thing to do when beginning to work on a reflection essay is to read your article thoroughly while taking notes. Whether you are reflecting on, for example, an activity, book/newspaper, or academic essay, you want to highlight key ideas and concepts.
You can start writing your reflection paper by summarizing the main concept of your notes to see if your essay includes all the information needed for your readers. It is helpful to add charts, diagrams, and lists to deliver your ideas to the audience in a better fashion.
After you have finished reading your article, it’s time to brainstorm. We’ve got a simple brainstorming technique for writing reflection papers. Just answer some of the basic questions below:
- How did the article affect you?
- How does this article catch the reader’s attention (or does it all)?
- Has the article changed your mind about something? If so, explain how.
- Has the article left you with any questions?
- Were there any unaddressed critical issues that didn’t appear in the article?
- Does the article relate to anything from your past reading experiences?
- Does the article agree with any of your past reading experiences?
Here are some reflection paper topic examples for you to keep in mind before preparing to write your own:
- How my views on rap music have changed over time
- My reflection and interpretation of Moby Dick by Herman Melville
- Why my theory about the size of the universe has changed over time
- How my observations for clinical psychological studies have developed in the last year
The result of your brainstorming should be a written outline of the contents of your future paper. Do not skip this step, as it will ensure that your essay will have a proper flow and appropriate organization.
Another good way to organize your ideas is to write them down in a 3-column chart or table.

Do you want your task look awesome?
If you would like your reflection paper to look professional, feel free to check out one of our articles on how to format MLA, APA or Chicago style
Writing a Reflection Paper Outline
Reflection paper should contain few key elements:
Introduction
Your introduction should specify what you’re reflecting upon. Make sure that your thesis informs your reader about your general position, or opinion, toward your subject.
- State what you are analyzing: a passage, a lecture, an academic article, an experience, etc...)
- Briefly summarize the work.
- Write a thesis statement stating how your subject has affected you.
One way you can start your thesis is to write:
Example: “After reading/experiencing (your chosen topic), I gained the knowledge of…”
Body Paragraphs
The body paragraphs should examine your ideas and experiences in context to your topic. Make sure each new body paragraph starts with a topic sentence.
Your reflection may include quotes and passages if you are writing about a book or an academic paper. They give your reader a point of reference to fully understand your feedback. Feel free to describe what you saw, what you heard, and how you felt.
Example: “I saw many people participating in our weight experiment. The atmosphere felt nervous yet inspiring. I was amazed by the excitement of the event.”
As with any conclusion, you should summarize what you’ve learned from the experience. Next, tell the reader how your newfound knowledge has affected your understanding of the subject in general. Finally, describe the feeling and overall lesson you had from the reading or experience.
There are a few good ways to conclude a reflection paper:
- Tie all the ideas from your body paragraphs together, and generalize the major insights you’ve experienced.
- Restate your thesis and summarize the content of your paper.
We have a separate blog post dedicated to writing a great conclusion. Be sure to check it out for an in-depth look at how to make a good final impression on your reader.
Need a hand? Get help from our writers. Edit, proofread or buy essay .
How to Write a Reflection Paper: Step-by-Step Guide
Step 1: create a main theme.
After you choose your topic, write a short summary about what you have learned about your experience with that topic. Then, let readers know how you feel about your case — and be honest. Chances are that your readers will likely be able to relate to your opinion or at least the way you form your perspective, which will help them better understand your reflection.
For example: After watching a TEDx episode on Wim Hof, I was able to reevaluate my preconceived notions about the negative effects of cold exposure.
Step 2: Brainstorm Ideas and Experiences You’ve Had Related to Your Topic
You can write down specific quotes, predispositions you have, things that influenced you, or anything memorable. Be personal and explain, in simple words, how you felt.
For example: • A lot of people think that even a small amount of carbohydrates will make people gain weight • A specific moment when I struggled with an excess weight where I avoided carbohydrates entirely • The consequences of my actions that gave rise to my research • The evidence and studies of nutritional science that claim carbohydrates alone are to blame for making people obese • My new experience with having a healthy diet with a well-balanced intake of nutrients • The influence of other people’s perceptions on the harm of carbohydrates, and the role their influence has had on me • New ideas I’ve created as a result of my shift in perspective
Step 3: Analyze How and Why These Ideas and Experiences Have Affected Your Interpretation of Your Theme
Pick an idea or experience you had from the last step, and analyze it further. Then, write your reasoning for agreeing or disagreeing with it.
For example, Idea: I was raised to think that carbohydrates make people gain weight.
Analysis: Most people think that if they eat any carbohydrates, such as bread, cereal, and sugar, they will gain weight. I believe in this misconception to such a great extent that I avoided carbohydrates entirely. As a result, my blood glucose levels were very low. I needed to do a lot of research to overcome my beliefs finally. Afterward, I adopted the philosophy of “everything in moderation” as a key to a healthy lifestyle.
For example: Idea: I was brought up to think that carbohydrates make people gain weight. Analysis: Most people think that if they eat any carbohydrates, such as bread, cereal, and sugar, they will gain weight. I believe in this misconception to such a great extent that I avoided carbohydrates entirely. As a result, my blood glucose levels were very low. I needed to do a lot of my own research to finally overcome my beliefs. After, I adopted the philosophy of “everything in moderation” as a key for having a healthy lifestyle.
Step 4: Make Connections Between Your Observations, Experiences, and Opinions
Try to connect your ideas and insights to form a cohesive picture for your theme. You can also try to recognize and break down your assumptions, which you may challenge in the future.
There are some subjects for reflection papers that are most commonly written about. They include:
- Book – Start by writing some information about the author’s biography and summarize the plot—without revealing the ending to keep your readers interested. Make sure to include the names of the characters, the main themes, and any issues mentioned in the book. Finally, express your thoughts and reflect on the book itself.
- Course – Including the course name and description is a good place to start. Then, you can write about the course flow, explain why you took this course, and tell readers what you learned from it. Since it is a reflection paper, express your opinion, supporting it with examples from the course.
- Project – The structure for a reflection paper about a project has identical guidelines to that of a course. One of the things you might want to add would be the pros and cons of the course. Also, mention some changes you might want to see, and evaluate how relevant the skills you acquired are to real life.
- Interview – First, introduce the person and briefly mention the discussion. Touch on the main points, controversies, and your opinion of that person.
Writing Tips
Everyone has their style of writing a reflective essay – and that's the beauty of it; you have plenty of leeway with this type of paper – but there are still a few tips everyone should incorporate.
Before you start your piece, read some examples of other papers; they will likely help you better understand what they are and how to approach yours. When picking your subject, try to write about something unusual and memorable — it is more likely to capture your readers' attention. Never write the whole essay at once. Space out the time slots when you work on your reflection paper to at least a day apart. This will allow your brain to generate new thoughts and reflections.
- Short and Sweet – Most reflection papers are between 250 and 750 words. Don't go off on tangents. Only include relevant information.
- Clear and Concise – Make your paper as clear and concise as possible. Use a strong thesis statement so your essay can follow it with the same strength.
- Maintain the Right Tone – Use a professional and academic tone—even though the writing is personal.
- Cite Your Sources – Try to cite authoritative sources and experts to back up your personal opinions.
- Proofreading – Not only should you proofread for spelling and grammatical errors, but you should proofread to focus on your organization as well. Answer the question presented in the introduction.
'If only someone could write my essay !' you may think. Ask for help our professional writers in case you need it.
Do You Need a Well-Written Reflection Paper?
Then send us your assignment requirements and we'll get it done in no time.
How To Write A Reflection Paper?
How to start a reflection paper, how long should a reflection paper be, related articles.
.webp)
On Bringing Your Whole Self to Medicine with Dr. Suzanne Koven The Physician’s Journey
Suzanne Koven is a primary care physician and the inaugural writer-in-residence at Massachusetts General Hospital. Her writing has appeared in the New England Journal of Medicine, Boston Globe, and other publications. She is also a faculty member at Harvard Medical School. In 2017, Dr. Koven published an essay describing the challenges faced by female physicians, including her struggle with imposter syndrome. Over the years her essay became the book "Letter to a Young Female Physician" which provides a deeply felt reflection on her career in medicine. In this episode, we explore pivotal moments in Suzanne´s career and how she has integrated the different parts of her self to become a better doctor.
- Episode Website
- More Episodes
- Copyright 2024 All rights reserved.
Top Podcasts In Education
Reflective Practice in Health Care Essay
Introduction, the description/ event, evaluation and analysis, recommendation and action plan.
Reflection refers to an approach used to comprehend the personal practice process nature, which results in escalated knowledge as well as proper application in healthcare work, which eradicates the chances for medical errors (Walker, 1996). Reflection allows a person to think about an action and through this way, engage in a continuous learning process (Hendricks, Mooney and Berry, 1996: 100). Therefore, reflective practice is the most key source of personal improvement and professional development. As a result, the concept has become popular globally (Price, 2004: 470).
An evidence-based tool of practice applies the best care a patient can afford. The principal goal of evidence-based practice is clinical expert opinion or expertise, caregiver/ patient/ client perspectives (Pattinson, 2011). For the purpose of this assignment, the Gibbs reflective model is vital. A summarized model will offer reflection guidance as structured in the six stages. The stages are; event or description, feeling or thoughts, evaluation, analysis, conclusion, and the action plan. This paper presents a case scenario where the practitioners involved in the care of the patient did not have effective communication, which impacted negatively on the patient. It also emphasizes the need for proper communication in health care.
Several years ago, as a senior anesthesia technician was just about to release an ODA for the lunch break, a boy who was approximately 5 years old and a pediatric cardiac patient was undergoing a dental clearance. After the dentist was thorough, the inhalation agent got terminated so as to allow the patient to recover prior to the removal of the endotracheal tube. The long extension set for intravenous use had already been closed as the short procedure was taking place. The boy began breathing again and tried to open his eyes. The reverse drugs were about to be given when the anesthetist requested the ODA to flush the intravenous line using 5ml of normal saline. However, the patient stopped breathing suddenly because of the boule that forced the residual muscle relaxant back into the patient. Consequently, the anesthetist began ventilating the patient, and it took approximately thirty minutes for the patient to recover. The patient did not experience considerable harm.
The shock was one of the feelings that overcame me first. The anesthetist was impatient in treating the patient and seemed to be in a hurry (Boud et al, 1985). He ought to have waited before flushing the intravenous line so as to avoid the formation of a boule, which forced the residual muscle relaxant back into the patient. Maybe he wanted to have finished all his duties before releasing the ODA for lunch. Moreover, there seemed to be miscommunication between the ODA and the anesthetist. Both of them should have deep knowledge of the process and, therefore, there should be no errors as was the case (Rolfe, Freshwater and Jasper, 2001). It was extremely sad to see the suffering young boy lying down. I was torn between many negative emotions; sorrow, pity, empathy, and blame on the healthcare professionals (Davies, 2012).
As mandated by healthcare policies and standards, I strongly feel that healthcare professionals should adhere to them to prevent adverse effects on patients (Pattinson, 2011). Professionals ought to realize that there are countless areas where there can be a resultant detrimental impact on the well-being of the patient if there is miscommunication or inadequate communication between providers (Walker, 1996).
In the mentioned occasion, the patient should have taken the residual muscle relaxant out first before flushing the intravenous vein with normal saline (Molyneux, 2001). The anesthetist seemed not to be patient enough. Moreover, the anesthetist went beyond his obligation’s limit by authorizing the ODP to flush without thinking of the repercussions (Schon, 1991). In essence, the anesthetist failed to adhere to the protocol expected during patient management (Mac Suibhne, 2009: 434). Regardless of how long healthcare professionals have been in practice, they should always realize that they are dealing with human life and, therefore, be extremely keen (Mann and Gordon, 2009: 617).
In my reflection, I realized that there are numerous issues that are preventable if there is proper and effective communication within the settings (Schon, 1991). These include drug reactions and interactions, increased care cost and hospitalization time, untimely medications and procedures, and inappropriate treatment. All these can be prevented if professionals adhere to the protocols of effective communication (Asper, 2003: 45). If the anesthetist and ODP were communicating effectively and were aware of the proper guidelines to follow, the patient would have recovered normally from the procedure done.
It is imperative for the anesthetist to be aware of his vital role in the patient’s life. Hence, he should have adhered to the set protocol, guidelines, and standards, and ensured effective and timely communication between himself and the ODP. Flushing the IV after muscle relaxation ensures the patient recovers normally (Mann and Gordon, 2009: 617). Healthcare research indicates that approximately eighty percent of all grave medical errors are a result of miscommunication (Price, 2004: 47). It has been noted that when handing over patients to other professionals for specialized procedures, there is always incomplete information handover (Schön, 1991). Moreover, healthcare professionals lack adequate time to discuss the patients’ issues in detail, which results in negative impacts on the patient (Brown et al, 2003: 40).
In my opinion, the anesthetist was not sufficiently accountable and responsible. A medical practitioner who is responsible and accountable enough has a keen interest in a patient’s outcome. In this case, the anesthetist was impatient, which almost led to detrimental effects on the patient. He ought to have been accountable and waited for the muscles to relax before administering the drug. On the same note, the anesthetist and ODP ought to have ensured that proper medication is given to the patient. Price (2004: 40) asserts that this is because giving a patient the wrong medication is unethical and can result in detrimental patient effects.
It is worth noting that ineffective communication goes with other human factors. For instance, there might be differences among the various departments (Molyneux, 2001: 30). When professionals from these departments meet for a procedure, grudges they hold against each other may result in the patient suffering. This is ethically unacceptable and contrary to the patient’s rights (Bolton, 2010). Moreover, it is imperative that professionals go through the guidelines of the procedures they are to perform. This reduces the chances of errors. According to Schön (1991), another ethical measure is to seek the client’s consent.
It is worth noting that many patients suffer as a result of the failure of healthcare professionals to adhere to effective communication. Mostly, healthcare professionals do not dedicate adequate and quality time to patients (Larrivee, 2000: 293). They perform most of the procedures in a hurry, which affects patients negatively (Mann & Gordon, 2009: 620). If the anesthetist was not in a hurry and dedicated to the patient’s result, he would have allowed adequate time before flushing the IV. This would have ensured that the patient responded successfully after the procedure.
Ineffective and inadequate communication has been reported to be the vital contributing factor to inadvertent patient harm and medical errors (Welsh Assembly Government, 2008). It does not only result in emotional and physical inconveniences to all those concerned but also adverse happenings, which are extremely costly. For instance, the resulting cost from medical errors in Victoria’s hospitals is approximately a billion dollars every year (Boud, Keogh & Walker, 1985: 34). It is worth noting that today, healthcare is extremely diverse and complex, and improving communication amidst professionals in healthcare would considerably support safe patient care delivery (Asper, 2003). It is extremely vital that managements in hospitals stimulate action and discussion, as well as raise awareness in regard to the units, divisions, and organizations where more teamwork and improved communication is essential (Brown et al, 2003). Mostly, ineffective communication is particularly the known cause that leads to sentinel events. Ineffective communication which is ambiguous, incomplete, inaccurate, untimely, and where the recipient does not comprehend clearly, increases the results and errors, for poor patient safety (Welsh Assembly Government, 2008).
There exists immense evidence linking poor and ineffective communication between teams in healthcare (Mac Suibhne, 2009: 430). The stated results are extremely negative patient impacts (Brown et al, 2003: 96). For instance, according to America’s Joint Commission, the key cause of more than seventy percent of sentinel occurrences is a communication failure. Moreover, America’s Veterans Affairs Department National Centre for Patient Safety acknowledges that failed communication in healthcare is the chief root foundation of seventy-five percent negative patient impacts (Leitch and Day, 2000: 157).
When the patient sees too many patients, miscommunication may result (Brown et al, 2003: 103). Usually, patients make efforts to ensure the best treatment choices (Larrivee, 2000: 293). However, the treating doctor may be unconcerned about other experts caring for the patient. In most cases, physicians are usually unaware that their patients are being treated for disease complications (Hendricks, Mooney & Berry, 1996: 100). The spectrum of poor communication included services and medication being duplicated, the patient being given more medication than is necessary, and wrong surgery sites (Asper, 2003).
The negative drug interaction is another potential danger. This is mostly because the patient is ignorant of the medication being given and may not identify cases of over medication. Such a situation threatens life and should be prevented at all costs (Boud, Keogh & Walker, 1985: 91). Patients also have a role to play in their health care. They have the right to ask questions and confirm procedures (Davies, 2012: 7).
In order to ensure such a case never repeats among ODPs and anesthetists, the case will be reported to the head of the department. Discussing it will ensure that all professionals handle their patients with extra keenness and that they follow procedures and guidelines well (Ministry of Justice, 2006). Consequently, it will be discussed during the monthly meeting of the department. During the meeting, all health care professionals will be present, including the ODP and anesthetist in mention. Both will be requested to elaborate on what and why it happened. This will be aimed at reviewing their role in every procedure (Leitch and Day, 2000: 154). Moreover, the anesthetist will have to apologize to the family and elaborate on the issue to them. This will ensure accountability. These grave measures will be geared towards ensuring that all patients receive adequate, timely, and proper treatment (McSherry, Pearce and Tingle, 2011).
According to Davies (2012, 10), the main reason for writing and addressing the incident in detail is to prevent and avoid such an occurrence again. It is vital that the ODA enquires and double checks every detail with the anesthetist. Moreover, all drugs and syringes should be labeled to avoid using the wrong ones on the patient. The anesthetist should be the only one who handles them to avoid confusion.
An incident like this happens often in the UK. According to the Health and Care Professions Council (HCPC), such a case happens 109 times annually (Brown et al, 2003: 96). There is, therefore, a need to address issues surrounding it so as to reduce its incidence and prevalence.
In my opinion, failure to dedicate adequate time for patient care and miscommunication are the key causes of this incident. Following the HPC guidelines would have prevented the incident from occurring (Ministry of Justice, 2006). In the mentioned case, an efficient leader who could adhere to the use of a checklist and the structured plan was absent. This would guarantee patient safety before conducting the anesthesia as recommended by WHO.
In the light of this discussion, health care professionals should be trained adequately to ensure their effective communication and accountable participation (McSherry, Pearce and Tingle, 2011). I recommend that a structured documentation checklist, good teamwork, effective communication be made the key targets for a quality improvement plan which ensures patient safety in all departments (Asper, 2003). The majority of hospitals’ managements are unaware of the miscommunication pervasiveness that exists (Davies, 2012: 11). Moreover, miscommunication goes unnoticed in many healthcare settings. Factors that affect the quality of communication are usually ignored, which results in detrimental health impacts on patients (Schön, 1983).
In order to ensure effective communication between healthcare teams, there is the need to consider intercultural communication between staff, the circumstances and content of communication, various discourse modes, presence of resources and opportunities for creating a common body of understanding, and linguistic and cultural distances (Welsh Assembly Government, 2008). The management should ensure strategies where all these are incorporated towards effective communication (Asper, 2003: 34).
Asper, M 2003, Beginning Reflective Practice (Foundations in Nursing and Health Care) , Nelson Thomas Ltd., Cheltenham.
Bolton, G 2010, Reflective Practice, Writing and Professional Development (3rd edn), Sage Publications, California.
Boud, D, Keogh, R & Walker, D 1985, Reflection, Turning Experience into Learning , Routledge, New York.
Brown, G et al, eds., 2003, Becoming an Advanced Health Practitioner, Butterworth Heinemann, Edinburgh.
Davies, S 2012, “Embracing reflective practice”, Education for Primary Care, vol. 23, pp. 9–12.
Hendricks, J, Mooney, D & Berry, C 1996, “A practical strategy approach to the use of the reflective practice in critical care nursing”, Intensive & critical care nursing, vol. 12 no. 2, pp. 97–101.
Larrivee, B 2000, “Transforming Teaching Practice: Becoming the critically reflective teacher”, Reflective Practice, vol. 1 no. 3, pp. 293.
Leitch, R & Day, C 2000, “Action research and reflective practice: towards a holistic view”, Educational Action Research , vol. 8, pp. 179.
Mac Suibhne, S 2009, “’Wrestle to be the man philosophy wished to make you’: Marcus Aurelius, reflective practitioner”, Reflective Practice, vol. 10 no. 4, pp. 429–436.
Mann, K & Gordon, M 2009, “Reflection and reflective practice in health professions education: a systematic review”, Adv in Health Sci Educ, vol. 14, pp. 595–621.
McSherry, R, Pearce, P & Tingle, J 2011, Clinical governance: a guide to implementation for healthcare professionals (3rd ed.), Wiley-Blackwell, Oxford.
Ministry of Justice 2006, Making sense of human rights: a short introduction. Web.
Molyneux, J 2001, “Interprofessional teamworking: what makes teams work well”, Journal of Interprofessional Care , vol. 15 no.1, pp. 29-35.
Pattinson, S 2011, Medical law and ethics ( 3rd ed ) , Sweet & Maxwell/Thomson Reuters, London.
Price, 2004, “Encouraging reflection and critical thinking in practice”, Nursing Standard, vol. 18, pp. 47.
Rolfe, G, Freshwater, D & Jasper, M 2001, Critical Reflection for Nursing and the Helping Professions , Palgrave, Basingstoke, U.K.
Schön, D. A 1983, The Reflective Practitioner, How Professionals Think In Action , Basic Books, London. Schon, D. A 1991, The reflective practitioner: how professionals think in action , Arena, London.
Walker, S 1996, “Reflective practice in the accident and emergency setting”, Accident and emergency nursing, vol. 4 no.1, pp. 27–30.
Welsh Assembly Government 2008, Reference guide for consent to examination or treatment. Cardiff: Welsh Assembly Government. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, May 9). Reflective Practice in Health Care. https://ivypanda.com/essays/reflective-practice-in-health-care/
"Reflective Practice in Health Care." IvyPanda , 9 May 2022, ivypanda.com/essays/reflective-practice-in-health-care/.
IvyPanda . (2022) 'Reflective Practice in Health Care'. 9 May.
IvyPanda . 2022. "Reflective Practice in Health Care." May 9, 2022. https://ivypanda.com/essays/reflective-practice-in-health-care/.
1. IvyPanda . "Reflective Practice in Health Care." May 9, 2022. https://ivypanda.com/essays/reflective-practice-in-health-care/.
Bibliography
IvyPanda . "Reflective Practice in Health Care." May 9, 2022. https://ivypanda.com/essays/reflective-practice-in-health-care/.
- Nurse Anaesthetist’s History and Role: Local Anesthesia and Complex Procedures
- Medieval and Early Modern Japan: Oda Nobunaga, Toyotomi Hideyoshi and Tokugawa Ieyasu
- Advanced Practice Nurse: Roles, Pros and Cons
- Health Workforce in Australia
- Higher Quality of Healthcare
- Centralization of Laboratory Information
- Major Health Policy Themes in Canada
- Conducting CODCD Building in Sydney University Project
Wayne State University
School of information sciences, school of information sciences current students, instructions for writing reflective essays.
Instructions
In the reflective essay, the student will discuss how s/he has developed as an information professional during the School. The student will discuss each of the four MLIS student learning outcomes, and demonstrate how they have become proficient in these learning outcomes.
The essay should following standard writing practice, with introduction, subheadings, and conclusion piece, free of grammar and typo mistakes. References are required.
For each MLIS learning outcome, the student uses 300-350 words to demonstrate their understanding of the learning outcome, and then uses an appropriate artifact to support their competency in the learning outcome.
Since multiple components are included in each learning outcome, the student can address one or two components for each learning outcome. Please use several sentences to justify your focus on those components.
For example : for LO#3, “Demonstrate professional competency, including critical thinking, research, communication, cultural competence, technology development, digital literacy, leadership, lifelong learning, and adherence to professional ethics”, students might address only “technology development” and “lifelong learning” components in their reflections.
As a concluding piece of the essay, the student will include their stance or philosophy of the information profession. The student will gird the philosophy piece using readings of the research, professional literature, personal experiences, and the learning outcomes. Students can address questions like: What is an information professional? What are the characteristics, qualities and knowledge that will be most important to you as an information professional?
Use of writing in the first person is encouraged. Essay Submission
The final product will be a 1400-1700 word reflective essay, with suitable and ethical citation practices followed (final word count excludes bibliography). Please note that this is not a personal history or review of courses taken during the School. Instead, it is an articulation of your growth as an information professional and your adoption of a personal professional philosophy.
You may submit the reflective essay in .doc, .docx, or pdf formats. Please do not submit the essay in .zip or .rar format.
Make sure your reflective essay has the following elements:
Introduction
Discussion of each MLIS learning outcome
Discussion of appropriate artifacts in relation to each MLIS learning outcome
Professional philosophy
Conclusion
References

IMAGES
VIDEO
COMMENTS
It integrates theoretical learning & clinical practice. It prepares medics for dealing with messy, ill -defined issues. It is part of student-centred learning, action research & experiential learning. It is an alternative to technical rationality, which forms the basis of traditional teaching.
Purpose . To investigate students' experience (over time) with meta-reflection writing exercises, called Signature Reflections. These exercises were used to strengthen reflective capacity, as part of a 4-year reflective writing portfolio curriculum that builds on a recognized strategy for reflection (narrative medicine) and employs longitudinal faculty-mentors.
Introduction. Reflective practice in medicine allows physicians to step back, review their actions and recognise how their thoughts, feelings and emotions affect their decision-making, clinical reasoning and professionalism [].This approach builds on Dewey [], Schon [3, 4], Kolb [], Boud et al. [] and Mezirow []'s concepts of critical self-examination.
positions also require a reflective essay. The reflective essay is the narrative story of the . impact and/or meaning. of the faculty member's accomplishments. It summarizes information provided about the . quantity. of accomplishments during the review period, enumerated on the Form on Progress and Excellence, and about the . quality. of those
4 A short guide to reflective writing Models of reflection There are frameworks that you can use to aid your reflective process. Alternatively, you may want to create your own. It needs to be a set of questions that you can ask yourself about an experience, plus a process by which you apply and learn from your reflection. Here are
1. Introduction. Reflection is proclaimed as a means to help physicians deal with medicine's inherent complexity, yet there is little agreement on the nature of reflection or how it should be taught and practiced (Schei et al., Citation 2019).While the importance of reflective thinking is emphasised by prominent scholars such as Dewey and Schön, a consensual definition of the term remains ...
There is a growing appreciation of the importance of reflection in medical education and professional practice. The Association of American Medical Colleges, the Accreditation Council on Graduate Medical Education, and credentialing organizations expect learners and practicing physicians to use reflection to continuously improve patient care. 1, 2 Reflection has been proposed as a means to ...
Set the scene by using the five W's (What, Where, When, Who and Why) to describe it. Choose the events or the experiences you're going to reflect on. Identify the issues of the event or experience you want to focus on. Use literature and documents to help you discuss these issues in a wider context.
The guidance on reflective practice for doctors and medical students has been developed jointly by Academy of Medical Royal Colleges, the UK Conference of Postgraduate Medical Deans (COPMeD), the General Medical Council (GMC) and the Medical Schools Counsel (MSC). The guidance considers why reflecting on experiences, both positive and negative ...
Examples of reflection. There is growing evidence from research that reflective practice improves the way people perform in their jobs. This is particularly important for medical practitioners to maintain and improve their standard of practice. Together with the Academy of Medical Royal Colleges, we're collecting a series of anonymised ...
Introduction. Reflective practice is something most people first formally encounter at university. This may be reflecting on a patient case, or an elective, or other experience. However, what you may not have considered is that you have been subconsciously reflecting your whole life: thinking about and learning from past experiences to avoid ...
To grade or not to grade: assessing written reflection. Just over a year ago, while I was a fourth year medical student (SL), I was required to write a reflective essay entitled, "When a patient became a person.". This piece of work contrasted starkly with the "scientific," evidence-based approach that I had grown accustomed to.
Reflection is something we do every day. It is an established part of medical education and a requirement for revalidation with the General Medical Council. 1 It is a focused learning process, which facilitates the development of insight and understanding, transforming the learner and guiding future practice. Reflection can take many forms: it ...
Action Plan. In future, I will aim to develop my assertive skills when working with colleagues, in order to ensure that the well-being of clients is maintained. In my next placement, I will make this a goal for my learning, and will discuss this with my mentor to work out strategies for how I can achieve this. *******************.
Writing requires attention and cognitive work, allowing exposure of abstract concepts (thoughts) in a more organized and symbolic way [14]. Writing inspires meaning-making to stimulate reflection [15]. Not all forms of writing are reflective, but the writing process itself comes close to self-analysis, which is essential for promoting reflection.
Reflective writing. Increasingly, at all stages of medical education, we are asked to keep a learning portfolio, which usually includes some reflective writing. While those fresh from medical school will be familiar with this learning tool, it may be unfamiliar and difficult for others. Reflective writing is said to encourage a writer to learn ...
MNHS: Reflective writing and critical incidents. Reflection on practice is an important aspect of your ongoing professional learning and development. In your course, this may take the form of a critical incident report. However, the focus is less on the event, incident or experience in itself. What is important is your reaction to it, and how ...
Here's a recap of the contents of this article, which also serves as a way to create a mind map: 1. Identify the topic you will be writing on. 2. Note down any ideas that are related to the topic and if you want to, try drawing a diagram to link together any topics, theories, and ideas. 3.
Reflective practice in medicine allows physicians to step back, review their actions and recognise how their thoughts, feelings and emotions affect their decision-making, clinical reasoning and professionalism [].This approach builds on Dewey [], Schon [3, 4], Kolb [], Boud et al. [] and Mezirow []'s concepts of critical self-examination.It sees new insights drawn from the physician's ...
Quick guide to reflective practice. What you need to know to be a reflective practitioner. Reflection is a core part of medical practice as well as an ethical duty, outlined in paragraph 13 of the GMC's 'Good medical practice' (2024). Formal reflective writing is an increasingly important aspect of medical training and professional development.
Never write the whole essay at once. Space out the time slots when you work on your reflection paper to at least a day apart. This will allow your brain to generate new thoughts and reflections. Short and Sweet - Most reflection papers are between 250 and 750 words. Don't go off on tangents.
She is also a faculty member at Harvard Medical School. In 2017, Dr. Koven published an essay describing the challenges faced by female physicians, including her struggle with imposter syndrome. Over the years her essay became the book "Letter to a Young Female Physician" which provides a deeply felt reflection on her career in medicine.
Introduction. Reflection refers to an approach used to comprehend the personal practice process nature, which results in escalated knowledge as well as proper application in healthcare work, which eradicates the chances for medical errors (Walker, 1996). Reflection allows a person to think about an action and through this way, engage in a ...
Use of writing in the first person is encouraged. Essay Submission The final product will be a 1400-1700 word reflective essay, with suitable and ethical citation practices followed (final word count excludes bibliography). Please note that this is not a personal history or review of courses taken during the School.