

Which program are you applying to?
Get accepted speak with an admissions expert today.
- Grad School
- Sample Essays
- The Public Health Student
What if people lived healthier lives, practiced preventive medicine, and took precautions against illness and disease? My days in the physical therapy department often made me think about the prevention of injuries as well as the injuries themselves. I was already doubting my future career choice as a physical therapist. Although I loved the science of it and helping people, the lack of variety within the field and its limited options for growth bothered me. I needed a career that helped a large number of people, emphasized prevention and primary care rather than tertiary care, and would continually challenge and motivate me to improve. Knowing that I really did not want to pursue physical therapy as I had originally planned, my thoughts wandered to the area of public health, particularly health management.
My first true introduction to the public health arena came in a class offered through the Big U School of Public Health. As I listened to experts speak about contemporary health issues, I was intrigued. The world of "capitation," "rationing of care," and Medicaid fascinated me as I saw the range of problems that public health professionals were trying to solve in innovative ways. This one semester class provided me with a basic but thorough understanding of the issues faced in health care today. In the last two years I have continued to learn about public health both through coursework and work in the field.
Because field experience is such a valuable learning tool, I searched for a research assistant position that would allow me to view public health at a different level. I worked on a project at a county health clinic in Englewood, a low-income, minority community. The program attempted to increase treatment compliance rates for adolescents diagnosed with tuberculosis who must complete a six-month medical program. Working for the county exposed me to a different side of health care that I had previously seen. Service and organization were not assets of the county and yet its role in the public health "ecosystem" was and is critical. Its job of immunizing thousands and interacting with all members of the community is often forgotten, but is important for keeping an entire community healthy.
My work at the county health clinic as well as my knowledge of some areas of public health led me to accept an internship in Washington D.C. this past summer. The internship provided me with a greater understanding of a federal public health agency’s operations and allowed me to contribute in a variety of ways to the XYZ Department in which I worked. Most importantly I worked on "policy issues" which involved identifying and summarizing problems that were out of the ordinary as well as documenting resolved issues in order to establish protocols to increase the department’s efficiency. In addition I served on a scientific review panel which was responsible for editing a seventy-page proposed regulation before its submission.
Along with my duties at XYZ, I attended seminars and met with public health leaders at different functions and events. All these activities confirmed my growing interest in preventive medicine, outcomes and effectiveness, and quality of care, particularly within the private/managed care sector. These are my strongest interests because I believe they are fundamental to our nation’s health. We must achieve efficiency and access without sacrificing quality.
The University of ____ would help me achieve my goals of furthering my public health education through the specialized coursework offered as part of its health administration program. [The client provides specifics here about the program’s specific appeal and strengths]
Since rejecting physical therapy as a career possibility my interest in public health has only grown. I welcome the challenge of serving a large community and participating in such a dynamic and challenging field. What if an aspirin a day could prevent heart attacks? What if abandoning unnecessary procedures saved thousands of dollars, which then allowed a hospital to treat other patients needing care? What if every person was guaranteed care and that care was good? I would like to find answers for these questions during my career as a public health graduate student and professional.

Other Sample Essays
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Institute of Medicine (US) Committee on Assuring the Health of the Public in the 21st Century. The Future of the Public's Health in the 21st Century. Washington (DC): National Academies Press (US); 2002.

The Future of the Public's Health in the 21st Century.
- Hardcopy Version at National Academies Press
3 The Governmental Public Health Infrastructure
The success or failure of any government in the final analysis must be measured by the well-being of its citizens. Nothing can be more important to a state than its public health; the state's paramount concern should be the health of its people.
Franklin Delano Roosevelt
(quoted in Gostin, 2000)
An effective public health system that can assure the nation's health requires the collaborative efforts of a complex network of people and organizations in the public and private sectors, as well as an alignment of policy and practice of governmental public health agencies at the national, state, and local levels. In the United States, governments at all levels (federal, state, and local) have a specific responsibility to strive to create the conditions in which people can be as healthy as possible. For governments to play their role within the public health system, policy makers must provide the political and financial support needed for strong and effective governmental public health agencies.
Weaknesses in the nation's governmental public health infrastructure were clearly demonstrated in the fall of 2001, when the once-hypothetical threat of bioterrorism became all too real with the discovery that many people had been exposed to anthrax from letters sent through the mail. Communication among federal, state, and local health officials and with political leaders, public safety personnel, and the public was often cumbersome, uncoordinated, incomplete, and sometimes inaccurate. Laboratories were overwhelmed with testing of samples, both real and false. Many of these systemic weaknesses were well known to public health professionals, but resources to address them had been insufficient. A strong and effective governmental public health infrastructure is essential not only to respond to crises such as these but also to address ongoing challenges such as preventing or managing chronic illnesses, controlling infectious diseases, and monitoring the safety of food and water.
The fragmentation of the governmental public health infrastructure is in part a direct result of the way in which governmental roles and responsibilities at the federal, state, and local levels have evolved over U.S. history. This history also explains why the nation lacks a comprehensive national health policy that could be used to align health-sector investment, governmental public health agency structure and function, and incentives for the private sector to work more effectively as part of a broader public health system. In this chapter, the committee reviews the organization of governmental public health agencies in the United States. The chapter then examines some of the most critical shortcomings in the public health infrastructure at the federal, state, and local levels: the preparation of the public health workforce, inadequate information systems and public health laboratories, and organizational impediments to effective management of public health activities. The committee recommends steps that must be taken to respond to these challenges so that governmental public health agencies can meet their obligations within the public health system to protect and improve the population's health.
The committee believes that the federal and state governments share a responsibility for assuring the public's health. From a historical and constitutional perspective, public health is largely a local and state function. The role of the states and localities is a primary and important one. The federal government, however, has the resources, expertise, and the obligation to assess the health of the nation and to make recommendations for its improvement. Ensuring a sound public health infrastructure is an urgent matter, and the committee urges the federal government to engage in planning for national and regional funding to accomplish this.
- PRIOR ASSESSMENTS OF THE PUBLIC HEALTH INFRASTRUCTURE
In 1988, The Future of Public Health (IOM, 1988) reported that the American public health system, particularly its governmental components, was in disarray. In that report, the responsible committee sought to clarify the nature and scope of public health activities and to focus specifically on the roles and responsibilities of governmental agencies. Aiming to provide a set of directions for public health that could attract the support of the broader society, the committee produced findings and made recommendations dealing with three basic issues:
The mission of public health
The government's role in fulfilling this mission and
The responsibilities unique to each level of government
The mission of public health was specified as “fulfilling society's interest in assuring conditions in which people can be healthy” (IOM, 1988: 7). The government's role in fulfilling this mission was described in terms of three core functions of public health practice: assessment of health status and health needs, policy development, and assurance that necessary services are provided. States were considered to have primary public responsibility for health, but it was considered essential that residents of every community have access to public health protections through a local component of the public health system. The public health obligations of the federal government included informing the nation about public health policy issues, aiding states and localities in carrying out their public health functions in a coordinated manner, and setting national health goals and standards. The report also contained recommendations for a review of the statutory basis for public health, the establishment of the governmental public health infrastructure as the clear organizational hub for public health activities, better linkages to other government agencies with health-related responsibilities, and strategies to strengthen the capacities of public health agencies to perform the core functions. A complete listing of the recommendations from that report can be found in Appendix C .
Responding to Disarray
The Future of Public Health provided the public health community with a common language and a focus for reform, and progress has been made. In Washington, Illinois, and Michigan, for example, revisions of the state public health codes resulted in the inclusion of mandatory provisions for funding and the distribution of services to all communities “no matter how small or remote,” as recommended by the Institute of Medicine (IOM) (1988). In 1994, the Public Health Functions Working Group, a committee convened by the Department of Health and Human Services (DHHS) with representatives from all major public health constituencies, agreed on a list of the essential services of public health. This list of services translates the three core functions into a more concrete set of activities, called the 10 Essential Public Health Services (see Box 3–1 ). These essential services provide the foundation for the nation's public health strategy, including the Healthy People 2010 objectives concerning the public health infrastructure (DHHS, 2000) (see Appendix D ) and the development of National Public Health Performance Standards (CDC, 1998) for state and local public health systems.
BOX 3–1
The 10 Essential Public Health Services. Assessment Monitor health status to identify community health problems
At least four subsequent National Academies reports have made a strong case for sustained federal action both domestically and internationally to strengthen the public health infrastructure (IOM, 1992, 1997a, 1997b; NRC, 2002). The federal government has yet to take the initiative to develop a comprehensive, long-term plan to build and sustain the financing for this infrastructure at the state and local levels to ensure the availability of the essential health services to all people, and this is a critical concern. The federal government has, however, developed and funded various new programs and organizational units, which, if effectively coordinated, could serve as important components of a more systematic program. The Centers for Disease Control and Prevention (CDC) established (in 1989) the Public Health Practice Program Office and strengthened university-based Centers for Prevention Research (initiated in 1983). CDC also developed Public Health Leadership Institutes (initiated in 1992) at the national and regional levels and the National Public Health Training Network (initiated in 1993). Both programs respond to recommendations to improve the overall leadership competencies of public health practitioners. In 1993, CDC began discussions of a modern and uniform approach to public health surveillance, and it has moved forward with the development of a National Electronic Disease Surveillance Network. More recently, CDC has worked with states to establish the Health Alert Network (initiated in 1999) to improve information and communication systems for both routine and emergency use and the Centers for Public Health Preparedness (launched in 2000) to improve linkages between local health agencies and academic centers. These programs provided important services in the aftermath of September 11, 2001.
Many units within CDC have contributed to strengthening the public health infrastructure. The National Center for Chronic Disease Prevention and Health Promotion, for example, has led the effort to develop statewide population-based cancer registries, a tracking system for cardiovascular disease, and a program for the early detection of breast and cervical cancer (CDC, 2002). The National Center for Environmental Health also contributed to the improvement of public health monitoring and assessment functions when it developed a biomonitoring program to measure people's exposures to 27 different chemicals by analyzing human blood and urine samples. This program offers the first national assessment of people's exposure to 24 chemicals for which exposures were not previously assessed and 3 for which exposures were previously assessed. In 2002, the center began developing a nationwide environmental public health tracking network in response to a Pew Environmental Health Commission report entitled America's Environmental Health Gap: Why the Country Needs A National Health Tracking Network (Pew Environmental Health Commission, 2000; www.cdc.gov/nceh/tracking/background.htm ). Among CDC initiatives are the development of immunization registries and a guide to community preventive services ( www.cdc.gov ).
Limited Progress
Despite this progress, the committee found that in many important ways, the public health system that was in disarray in 1988 remains in disarray today. Many of the recommendations from The Future of Public Health have not been put into action. There has been no fundamental reform of the statutory framework for public health in most of the nation. Funding for the public health infrastructure has recently increased to support the infrastructure that relates to bioterrorism and emergency preparedness but may still be insufficient. Furthermore, governmental and nongovernmental support (both political and financial) and advocacy for the report's recommendations have been limited. Progress is mixed in strengthening public health agencies' capacities to address environmental health problems, in building linkages with the mental health field, and in meeting the health care needs of the medically indigent. In addition, new information and technological challenges face the system today. In a recent review of the nation's public health infrastructure for the U.S. Senate Appropriations Committee, CDC (2001d) pointed to the need for further efforts to address gaps in workforce capacity and competency, information and data systems, and the organizational capacities of state and local health departments and laboratories.
Finding continued disarray in the public health system is especially disturbing because the nation faces increasingly diverse threats and challenges. The early detection of and the response to these threats will depend on capacity and expertise within the public health system at every level. The gaps in the system warrant urgent remediation. Many of these basic reforms also require actions from agencies that are outside the direct control of governmental public health agencies but whose policies and programs can have important health consequences, such as the Environmental Protection Agency (EPA) (environment) and the Departments of Agriculture (nutrition and food safety), Labor (working conditions), and Treasury (economic development). This support has not been forthcoming from elected or appointed government officials (including those in control of budgets), and stakeholders in the broader public health system—who should have been partners in the vision of creating a healthier nation—have yet to be effectively mobilized in this effort.
In the next section, the committee provides an overview of the special role of governmental public health agencies (at the federal, tribal, state, and local levels). The section addresses the legal framework for governmental responsibility and its authorities for protecting the health of the people as well as the organization of the governmental public health infrastructure.
- THE ROLE OF GOVERNMENTS IN PUBLIC HEALTH: AN OVERVIEW AND LEGAL FRAMEWORK
Governments at every level—federal, tribal, state, and local—play important roles in protecting, preserving, and promoting the public's health and safety (Gostin, 2000, 2002). In the United States, the government's responsibility for the health of its citizens stems, in part, from the nature of democracy itself. Health officials are either directly elected or appointed by democratically elected officials. To the extent, therefore, that citizens place a high priority on health, these elected officials are held accountable to ensure that the government is able to monitor the population's health and intervene when necessary through laws, policies, regulations, and expenditure of the resources necessary for the health and safety of the public.
The U.S. Constitution provides for a national government, with power divided among the legislative, executive, and judicial branches, each with distinct authority. The states have adopted similar schemes of governance. In health matters, the legislative branch creates health policy and allocates the resources to implement it. In the executive branch, health departments and other agencies must act within the scope of legislative authority by implementing legislation and establishing health regulations to enforce health policy. The judiciary's task is to interpret laws and resolve legal disputes. Increasingly, the courts have exerted substantial control over public health policy by determining the boundaries of government power (Gostin, 2000). The separation of powers provides a system of checks and balances to ensure that no single branch of government can act without some degree of oversight and control by another.
Modern public health agencies wield considerable power to make rules to control private behavior, interpret statutes and regulations, and adjudicate disputes about whether an individual or a company has conformed to health and safety standards. In the area of health and safety (which is highly complex and technical), public health agencies are expected to have the expertise and long-range perspective necessary to assemble the facts about health risks and to devise solutions.
Role of State and Local Governments in Assuring Population Health
States and their local subdivisions retain the primary responsibility for health under the U.S. Constitution. 1 To fulfill this responsibility, state and local public health authorities engage in a variety of activities, including monitoring the burden of injury and disease in the population through surveillance systems; identifying individuals and groups that have conditions of public health importance with testing, reporting, and partner notification; providing a broad array of prevention services such as counseling and education; and helping assure access to high-quality health care services for poor and vulnerable populations. State and local governments also engage in a broad array of regulatory activities. They seek to ensure that businesses conduct themselves in ways that are safe and sanitary (through the institution of measures such as inspections, licenses, and nuisance abatements) and that individuals do not engage in unduly risky behavior or pose a danger to others (through the provision of services such as vaccinations, directly observed therapy, and isolation), and they oversee the quality of health care provided in the public and private sectors.
Role of Tribal Governments in Assuring Population Health
Although their legal status varies, tribal governments have a unique sovereignty and right to self-determination that is often based on treaties with the federal government. Under these treaties, the federal government has an obligation to provide tribes with certain services, including health-related services. In addition, American Indians and Alaska Natives are eligible as individual citizens to participate in state health programs. However, in some instances, tribal–state relations are strained, and there are often misunderstandings about the relative responsibilities of states and tribes for the financing of health care and population-based public health services. Until the mid-1970s, the federal government directly provided health care services to American Indians living on reservations and to Alaska Natives living in villages through the Indian Health Service (IHS), an agency within DHHS. In 1975, the Indian Self-Determination and Education Assistance Act (P.L. 93–638) established two other options for obtaining these services: (1) tribal governments can contract with IHS to provide the services or (2) administrative control, operation, and funding for the services can be transferred to a tribal government (IHS, 2001c). In the mid-1970s, legislation also authorized funding health services for American Indians living in urban areas. 2 The operation of IHS programs depends on annual discretionary appropriations, which are generally considered inadequate (Noren et al., 1998; IHS, 2001a). Some tribes are able to supplement IHS funding, but many cannot. Many tribes have health directors and operate extensive public health programs that include environmental safety and community health education, as well as direct curative and preventive services.
Role of the Federal Government in Assuring Population Health
The federal government acts in six main areas related to population health: (1) policy making, (2) financing, (3) public health protection, (4) collecting and disseminating information about U.S. health and health care delivery systems, (5) capacity building for population health, and (6) direct management of services (Boufford and Lee, 2001). For most of its history, the U.S. Supreme Court has granted the federal government broad powers under the Constitution to protect the public's health and safety. Under the power to “regulate Commerce . . . among several states” and other constitutional powers, the federal government acts in areas such as environmental protection, occupational health and safety, and food and drug purity (Gostin, 2000). The federal government may set conditions on the expenditure of federal funds (e.g., require adoption of a minimum age of 21 for legal consumption of alcoholic beverages to receive Federal-Aid Highway Funds), tax commodities whose use results in risky behavior (e.g., cigarettes), reduce taxes for socially desirable behaviors (e.g., for voluntary employer provision of health care), and regulate persons and businesses whose activities may affect interstate commerce (e.g., manufacturers of pharmaceuticals and vaccines so that they are safe and effective).
The judicial branch also can shape federal health policy in many ways. It can interpret public health statutes and determine whether agencies are acting within the scope of their legislative authority. The courts can also decide whether public health statutes and regulations are constitutionally permissible. The Supreme Court has made many decisions of fundamental importance to the public's health. The court has upheld the government's power to protect the public's health (e.g., require vaccinations), set conditions on the receipt of public funds (e.g., set a minimum drinking age), and affirmed a woman's right to reproductive privacy (e.g., a right to contraception and abortion). Gostin (2000) notes that although the courts generally have been permissive on matters of public health, stricter scrutiny has come when there is any appearance of discrimination against a suspect class or invasion of a fundamental right, such as bodily integrity.
Public Health Law: The Need for State Reforms
Because primary responsibility for protection of the public's health rests with the states, their laws and regulations concerning public health matters are critical in determining the appropriateness and effectiveness of the governmental public health infrastructure. At present, however, the law relating to public health is scattered across countless statutes and regulations at the state and local levels and is highly fragmented among the states and territories. Furthermore, public health law is beset by problems of antiquity, inconsistency, redundancy, and ambiguity that make it ineffective, or even counterproductive, in advancing the population's health.
The most striking characteristic of state public health law, and the one that underlies many of its defects, is its overall antiquity. Much of public health law contains elements that are 40 to 100 years old, and old public health statutes are often outmoded in ways that directly reduce their effectiveness and their conformity with modern legal norms in matters such as protection of individual rights. 3 These laws often do not reflect contemporary scientific understandings of health risks or the prevention and treatment of health problems. For example, laws aimed at preventing casual transmission of airborne diseases such as influenza and measles have little relevance for control of the sexually transmitted and blood-borne pathogens that are major concerns of health authorities today (Gostin et al., 1999). When many of these statutes were written, the science of public health, in fields such as epidemiology and biostatistics, and of behavior and behavioral interventions, such as client-centered counseling, was in its infancy.
Related to the problem of antiquity is the problem of multiple layers of law. The law in most states consists of successive layers of statutes and amendments, built up over more than 100 years in some cases, in response to changing perceptions of health threats. This is particularly troublesome in the area of infectious diseases, which forms a substantial part of state health codes. Colorado's disease control statute, for example, has separate sections for venereal diseases, tuberculosis, and HIV. All three sections authorize compulsory control measures, but they vary significantly in the procedures required and the public health philosophy expressed. Whereas the venereal disease statute simply empowers compulsory examination whenever health officials deem it necessary, the HIV section sets out a list of increasingly intrusive options (requiring use of the least restrictive) and places the burden of proof on the health department to show a danger to public health (Gostin et al., 1999).
Because health codes in each state and territory have evolved independently, they show profound variations in their structures, substance, and procedures for detecting, controlling, and preventing injury and disease. In fact, statutes and regulations among American jurisdictions vary so significantly in definitions, methods, age, and scope that they defy orderly categorization. There is, however, good reason for greater uniformity among the states in matters of public health. Health threats are rarely confined to single jurisdictions, instead posing risks across regions or the entire nation.
State laws do not have to be identical. There is often a justification for the differences in approaches among the states if there are divergent needs or circumstances. There is also a case for states' acting as laboratories to determine the best approach. Nevertheless, a certain amount of consistency is vital in public health. Infectious diseases and other health threats do not confine themselves to state boundaries but pose regional or even national challenges. States must be able to engage in surveillance and respond to health threats in a predictable and consistent fashion, using similar legal structures. Consistent public health statutes would help facilitate surveillance and data sharing, communication, and coordinated responses to health threats among the states. Consider the coordination that would be necessary if a biological attack were to occur in the tristate area of New York, New Jersey, and Connecticut. Laws that complicate or hinder data communication among states and responsible agencies would impede a thorough investigation and response to such a public health emergency.
To remedy the problems of antiquity, inconsistency, redundancy, and ambiguity, the Robert Wood Johnson and W. K. Kellogg Foundations' Turning Point initiative launched a Public Health Statute Modernization Collaborative in 2000 “to transform and strengthen the legal framework for the public health system through a collaborative process to develop a model public health law” (Gostin, 2002). The model public health law focuses on the organization, delivery, and funding of essential public health services, as well as the mission and powers of public health agencies. It is scheduled for completion by October 2003, and current drafts are available on the Turning Point website, at http://www.turningpointprogram.org .
The process of law reform took on new urgency after the events of September 11, 2001, and the subsequent intentional dispersal of anthrax through the postal system. In response, the Center for Law and the Public's Health at Georgetown University and Johns Hopkins University drafted the Model State Emergency Health Powers Act (MSEHPA) at the request of CDC ( www.publichealthlaw.net ). DHHS recommends that each state review its legislative and regulatory needs and requirements for public health preparedness. MSEHPA offers a guide or checklist for governors and legislatures to review their current laws. As of September 2002, three-quarters of the states had introduced a version of MSEHPA, and 19 states had adopted all or part of the act (Gostin et al., 2002). The model act, under review by federal and state officials, defines the purpose of the legislation as giving the governor and other state and local authorities the powers and ability to prevent, detect, manage, and contain emergency health threats without unduly interfering with civil rights and liberties. The legislation would address matters including reporting requirements, information sharing, access to contaminated facilities, medical examination and testing, and procedures for isolation and quarantine (Center for Law and the Public's Health, 2001).
CDC is facilitating the law reform process through its internal Public Health Law Collaborative. Efforts are in place to improve scientific understanding of the interaction between law and public health and to strengthen the legal foundation for public health practice. Through the Public Health Law Collaborative, CDC is joined in its work in public health law by a growing number of partners. These include public health practice associations, academic institutions and researchers, and public policy organizations ( www.phppo.cdc.gov/PhLawNet ).
The committee finds that the problems of antiquity, inconsistency, redundancy, and ambiguity render many public health laws ineffective or even counterproductive in improving population health. A set of standards and procedures would add needed clarity and coherence to legal regulation. Therefore, the committee recommends that the Secretary of the Department of Health and Human Services, in consultation with states, appoint a national commission to develop a framework and recommendations for state public health law reform. In particular, the national commission would review all existing public health law as well as the Turning Point 4 Model State Public Health Act and the Model State Emergency Health Powers Act 5 ; provide guidance and technical assistance to help states reform their laws to meet modern scientific and legal standards; and help foster greater consistency within and among states, especially in their approach to different health threats. It is essential that any reform of public health legislation address the powers needed to deal effectively with bioterrorism and other public health emergencies that pose significant threats across state boundaries. Each state could adapt the commission's recommendations to its unique legal structures and particular needs for public health preparedness. Public health is traditionally a state function, so the commission would provide guidance to the states rather than impose standards.
The following section provides a description of the federal, state, and local governmental agencies that are responsible for protecting the health of the public. Later in the chapter, the committee examines certain aspects of the state and local public health infrastructures that are of special concern.
The State and Local Governmental Public Health Infrastructure
Although the states carry the primary constitutional responsibility and authority for public health activities in the United States, public health administration first began in cities in the late eighteenth century (Rosen, 1993). The burgeoning social problems of industrial cities convinced legislatures to form more elaborate and professional public health administrations within municipal governments (Duffy, 1990). City boards of health were established to obtain effective agency supervision and control of health threats facing the population. Only after the Civil War did states form boards of health. County and rural health departments emerged in the early twentieth century (Ferrell and Mead, 1936). Today, there are more than 3,000 local public health agencies, 3,000 local boards of health, and 60 state, territorial, and tribal health departments (CDC, 2001b).
Structure and Governance of State and Local Public Health Agencies
The organization and authority granted to state and local public health agencies vary substantially across the country. Every state has an agency with responsibility for public health activities. That agency may be an independent department or a component of a department with broader responsibilities, such as human services programs. In 31 states, the state health officer is also the head of the larger health and human services agency (Turnock, 2000). Physicians and nurses often lead state public health agencies. At the local level, however, general managers with business training rather than formal training in public health or medicine may lead public health agencies.
States differ in terms of the relationship between the state agency and the agencies serving localities within the state. In some states (e.g., Arkansas, Florida, Georgia, and Missouri), the state public health infrastructure is centralized, meaning that the state agency has direct control and authority for supervision of local public health agencies. In other states (e.g., California, Illinois, and Ohio), local public health agencies developed independently from the state agency, in that they are run by counties or townships (rather than the state) and report directly to local boards of health or health commissioners or are governed by cooperative agreements. Still other states (e.g., Iowa and North Dakota) have no local public health agencies and the state public health agency is preeminent (Fraser, 1998).
In a recent report on the local public health agency infrastructure, the National Association of County and City Health Officials (NACCHO) (2001d) identified five types of local public health agencies (see Figure 3–1 ).
FIGURE 3–1
Types of local public health agencies (LPHAs) across the United States.
The most common arrangement is a local public health agency (LPHA) serving a single county, ranging from small rural counties (e.g., Issaquena County, Mississippi, with a population less than 1,000) to large metropolitan counties (e.g., Los Angeles County, with a population approaching 10 million). LPHAs may also serve single cities of various sizes (e.g., Kansas City, Missouri, and New York City). A combined city–county local public health agency is also found (e.g., Seattle-King County, Washington). Township local public health agencies are common in states with strong “home-rule” political systems 6 (e.g., Connecticut, Massachusetts, and New Jersey). City or township health agencies may operate within counties that are also served by county health agencies.
Multicounty local public health agencies often span large geographic areas in the western United States. For example, the Northeast Colorado Health District serves six counties, an area roughly equivalent in size to that of the state of Vermont. In these local public health agencies, health directors may be accountable to multiple county boards of health or to a combined board of health whose membership represents the counties or other units covered by the local public health agency. The multicounty local public health agency category also includes state health department regional offices that act as local public health agencies, an arrangement found in several states (e.g., Alabama, New Mexico, Tennessee, and Vermont).
The governance of state and local public health agencies generally fits one of three models. In a cabinet model, the head of the agency is appointed by and answers to the governor, mayor, or other executive authority. Under a board-of-health model, the state or local health director reports to an appointed board representing constituencies served by the department. In many cases, however, a board of health functions in a strictly advisory capacity, with no oversight authority. Under an “umbrella” model, the public health agency is part of a larger agency, and the health director either heads the agency or reports to its head. There are considerable variations within these three models.
Even with this great variability in governance at both the state and local levels, there are no data to suggest what an “ideal” state and local agency governance structure might be. Thus, it would be important for state agencies to examine their present governance structures and evaluate mechanisms to make these structures more effective. Doing so should serve to build and strengthen relationships with local public health agencies, coordinate efforts for the delivery of the essential public health services and crisis response services, integrate essential health information, and respond to the changing health needs of the population.
Scope of Agency Responsibilities and Activities
At both the state and local levels, there are differences among public health agencies in terms of the scope of their authority, responsibilities, and activities. At the state level, activities such as immunization, infectious disease control and reporting, health education, and health statistics are common to most public health agencies. States are also responsible for licensing and regulating the institutional and individual providers that deliver health care services. However, states differ in whether the public health agency has responsibility for programs such as mental health and substance abuse, environmental health, and Medicaid. These organizational differences make it more complicated to frame and pursue a coherent national agenda concerning changes and improvements in the governmental public health infrastructure.
A recent NACCHO (2001e) survey of local public health agency infrastructures has helped document the variation in services provided at the local level. Among county health departments, for example, 98 percent provided childhood immunizations (directly or through contract services), 76 percent were responsible for restaurant inspections and licensing, and 31 percent provided dental services. City and township local public health agencies were often less likely to offer services that other types of local public health agencies provided. The most common services provided by local public health agencies include those most associated with traditional public health practice: adult and childhood immunizations, communicable disease control, community assessment, community outreach and education, environmental health services, epidemiology and surveillance, food safety, health education, restaurant inspections, and tuberculosis testing. Services provided by a smaller percentage of local public health agencies included treatment for chronic disease, behavioral and mental health services, programs for the homeless, substance abuse services, and veterinary public health (NACCHO, 2001d).
One widespread change in the scope of local public health agency activities is a reduction in the direct delivery of health care services, especially to Medicaid participants. This is consistent with a national effort to have governmental public health agencies return their attention to the more population-based public health services that had been weakened by the pressing need to provide safety-net services to uninsured individuals. Although some have been unable to do so, many state and local public health agencies now have contracts with managed care organizations and other private providers to serve those populations. A substantial transfer of service delivery from health departments to private providers has also occurred for childhood immunizations under federal and state programs for the purchase and distribution of vaccines (IOM, 2000a). Some researchers have found the partnership between managed care and local public health agencies to be positively associated with the overall scope and perceived effectiveness of local public health activities in terms of their ability to meet population-based community needs (Mays et al., 2001). (See Chapter 5 for additional discussion of the role of health care services providers in the public health system.) However, some local public health agencies have found it difficult to compensate for the loss of revenue that had previously come from the delivery of health care services that have now been transferred to managed care organizations (Wall, 1998; Keane et al., 2001).
- THE FEDERAL PUBLIC HEALTH INFRASTRUCTURE
In contrast to state and local public health agencies, the federal government has a limited role in the direct delivery of essential public health services. Nevertheless, it plays a crucial role in protecting and improving the health of the population by providing leadership in setting health goals, policies, and standards, especially through its regulatory powers. It also contributes operational and financial resources: to assure financing of health care for vulnerable populations through Medicare, Medicaid, Community and Migrant Health Centers, and IHS programs; to finance research and higher education; and to support development of the scientific and technological tools needed to improve the effectiveness of the public health infrastructure at all levels.
Organization of the Federal Public Health Infrastructure
At the federal level, the lead entity responsible for public health activities is DHHS. Several key agencies in DHHS comprise the U.S. Public Health Service (PHS): the Agency for Healthcare Research and Quality, CDC, the Agency for Toxic Substances and Disease Registry (ATSDR), the Food and Drug Administration (FDA), the Health Resources and Services Administration (HRSA), IHS, the National Institutes of Health (NIH), and the Substance Abuse and Mental Health Services Administration (SAMHSA). In addition, various White House agencies such as the Office of Science and Technology Policy and the Office of National Drug Control Policy, 14 cabinet-level departments and agencies (e.g., Department of Agriculture, Department of Transportation, EPA, Department of Veterans Affairs [VA], and Department of Defense [DOD]), and more than 10 public corporations and commissions and subcabinet agencies are responsible for certain health programs.
The U.S. Congress oversees the activities of federal agencies through committees that review the authorization of programs and the appropriation of funds. Multiple committees in both the House of Representatives and the Senate have jurisdiction over DHHS programs and health-related activities in other departments. These multiple authorities and congressional jurisdictions are an important reason for the “disarray” noted in previous IOM reports.
Scope of DHHS Responsibilities and Activities
Although activities and responsibilities related to public health are spread throughout the federal government, the committee focused its attention on DHHS and its agencies as the principal federal component of the nation's governmental public health infrastructure and as the principal point of contact for other federal agencies with health or health-related programs and for state and local public health agencies. Reviewed briefly here are DHHS activities related to the previously noted functions of policy making, financing of public health activities, public health protection, collection and dissemination of information about U.S. health and health care delivery systems, capacity building for population health, and direct management of services. Some of these activities are considered in more detail later in this chapter, in conjunction with the discussion of specific concerns regarding weaknesses in the nation's governmental public health infrastructure.
Policy Making
Policy making is a critical function for DHHS and involves the initiation, shaping, and ultimately, implementation of congressional and presidential decisions. It involves the creation and use of an evidence base, informed by social values, so that public decision makers can shape legislation, regulations, and programs. The annual budget cycle is routinely the time when lawmakers present new legislation and renew legislation for existing programs and when DHHS defends proposed program budgets to Congress. Policy making also occurs through program initiatives that do not require legislative action. One of the leading examples in public health is the Healthy People initiative, which establishes national goals and objectives for health promotion and disease prevention. The Healthy People initiative is led by the DHHS Office of Disease Prevention and Health Promotion and now involves all DHHS operating divisions, other federal departments, and partnerships with state and local public health officials, as well as more than 350 national membership organizations, nongovernmental organizations, and corporate sponsors. Although the effort is voluntary, the activity and regular widespread public consultation involved in the initiative have perhaps proved to be the department's most effective nonlegislative policy vehicle for promoting action on population health at the national, state, and local levels (Boufford and Lee, 2001).
Financing of Public Health Activities
Through a variety of mechanisms—grants, contracts, and reimbursements through publicly funded health insurance programs—DHHS is an important financial contributor to the activities of state and local governmental public health agencies, primarily by financing personal health care services through mandatory spending for the entitlement programs of Medicaid. The fiscal year (FY) 2002 budget for Medicaid amounted to $142 billion (OMB, 2001b); in sharp contrast, the DHHS discretionary budget for PHS agencies in FY 2002 was about $41 billion, of which $23.2 billion was designated for NIH. Very little of this discretionary money goes directly to states for governmental public health agency infrastructure.
Public Health Protection
Public health protection is perhaps the most classic public health function of the federal government. In this regard, the federal government uses its surveillance capacity to assess health risks and its standard-setting and regulatory powers to protect the public from health risks: unfair treatment; low-quality services; and unsafe foods, medicines, biologics such as blood and medical devices, as well as environmental and occupational health hazards. In addition to certain regulatory responsibilities, DHHS also develops and maintains a research base that produces the scientific evidence needed to support the regulations in health-related areas that other federal agencies use. The principal regulatory agencies of DHHS are FDA for drugs and biologics, medical devices, and certain foods and the Centers for Medicare and Medicaid Services (CMS) for health care providers. Both CMS and FDA are responsible for regulatory oversight of laboratories (Boufford and Lee, 2001). Other departments and agencies outside DHHS are also responsible for regulations that protect health. 7
Collection and Dissemination of Information
Timely and reliable data are an essential component of public health assessment, policy development, and assurance at all levels of government. DHHS, particularly the PHS agencies, sponsors a variety of public health and health care data systems and activities. These include national vital and health statistics, household surveys on health and nutrition, health care delivery cost and utilization information, and reporting requirements for programs funded by federal grants or assistance. The National Center for Health Statistics within CDC is the primary agency collecting and reporting health information for the federal government. CMS collects administrative data on the Medicare and Medicaid programs and conducts beneficiary surveys. The Administration for Children and Families and the Administration on Aging also collect data on human services. Other agencies (e.g., the Census Bureau, the Department of Agriculture, and the Department of Labor) also collect data that are important for public health purposes. In addition, the collection and dissemination of research findings can be considered part of this activity.
Capacity Building for Population Health
The capacity-building function of the federal government centers on ensuring the ability of its own agencies to effectively discharge their responsibilities. It also centers on ensuring that state and local levels of government have the resources—human, financial, and organizational—they need to carry out the responsibilities delegated to them by the federal government or for which they are responsible by law as they work to assure and promote the health of the communities that they serve. In terms of the public health infrastructure, this includes striving for effective collaboration within DHHS, between DHHS and other cabinet departments for domestic and international health policy, and between DHHS and state and local public health departments. With more than 200 categorical public health programs in DHHS and a variety of health-related programs in other federal agencies, the alignment of policies and strategies is challenging. This also makes it difficult to devise an approach to the systematic and accountable long-term investment of federal funding in governmental public health agencies at the state and local levels.
Direct Management of Services
Federal funding supports the delivery of medical care through a variety of categorical grant programs (e.g., for community health centers and maternal and child health services) and insurance programs (e.g., Medicaid and Medicare). However, the direct management of clinical or other services delivered to individuals is a small part of DHHS's role. Under DHHS, direct medical care and public health services are provided primarily by IHS, which serves members of federally recognized American Indian tribes. As tribal governments assume greater responsibility for managing these services, the role of IHS could evolve into that of a payer or purchaser rather than a provider of services. In addition, DOD and VA play larger direct management roles in the provision of health care services for their particular constituencies.
The next section highlights the current status of certain critical components of the public health infrastructure that support the public health system in carrying out essential public health functions. These components include the public health workforce, information and data systems, and public health laboratories. The section also reviews how these components of the infrastructure are critical to emergency preparedness and response activities.
- CRITICAL COMPONENTS OF THE PUBLIC HEALTH INFRASTRUCTURE
The Public Health Workforce
The governmental public health infrastructure at the federal, state, and local levels consists of physical resources (e.g., laboratories), information networks, and human resources (the public health workforce). An adequately sized and appropriately trained workforce performing competently is an essential element of the public health infrastructure. The public health workforce at the federal, state, and local levels must be prepared to respond to an array of needs, such as the assurance of health-related environmental safety, the interpretation of scientific data that can influence health outcomes, or the clarification of vast amounts of highly technical information after a community emergency. In addition to meeting the scientific and technical requirements of public health practice, state and local public health officials are often expected to provide community leadership, manage community reactions, and communicate about risk, protection, and prevention.
Current estimates indicate that approximately 450,000 individuals are working in salaried public health positions, with many more contributing to this mission through nongovernmental organizations or on a voluntary basis (HRSA, 2000). Public health practitioners have training in a variety of disciplines, including the biological and health sciences, psychology, education, nutrition, ethics, sociology, epidemiology, biostatistics, business, computer science, political science, law, public affairs, and urban planning.
Recent studies have shown, however, that the current public health workforce is unevenly prepared to meet the challenges that accompany the practice of public health today. An estimated 80 percent of the current workforce lacks formal training in public health (CDC-ATSDR, 2001). Moreover, the major changes in technology, biomedical knowledge, informatics, and community expectations will continue to challenge and redefine the practice of public health, requiring that current public health practitioners receive the additional, ongoing training and support they need to update their existing skills (Pew Health Professions Commission, 1998).
Training and Education for the Public Health Workforce
Competency-based training.
Given that early public health efforts in the United States were aimed at improving sanitation, controlling infectious diseases, assuring the safety of food and water supplies, and immunizing children, it is hardly surprising that public health workers at that time were predominantly graduates of schools of medicine, nursing, and the biological sciences. Today, however, the public health workforce has broader responsibilities and must be much more diverse. For example, as part of the performance of essential services, members of the public health workforce must be prepared to engage the community in effective actions to promote mental, physical, environmental, and social health. Advances in biomedical and genomics research and technologies have the potential to change the way public health practitioners think about population-level disease risk and how disease prevention and health promotion activities might be practiced. Moreover, rapidly evolving computer and information technologies and the use of mass media and social marketing have the potential to revolutionize health departments' access to up-to-date surveillance information, disease databases, and communications networks as well as to enhance worker productivity.
The need to strengthen the public health workforce was recognized by IOM in 1988 and has been the focus of a variety of efforts since then. Some of these activities will be discussed in the chapter on the role of academia in the public health system ( Chapter 8 ). A few key efforts focusing on the current workforce (rather than training new workers) are also covered here. In particular, the report The Public Health Workforce: An Agenda for the 21st Century (USPHS, 1997) called for greater leadership on workforce issues from national, state, and local public health agencies; use of a standard taxonomy to better assess and monitor workforce composition; competency-based curriculum development; and greater use of new technologies for distance learning. The Taskforce for Public Health Workforce Development, established in 1999 by CDC and ATSDR, recommended six broad strategies for a national public health workforce development agenda (CDC, 2000e):
Monitor current workforce composition and project future needs.
Identify competencies and develop curricula.
Design integrated learning systems.
Use incentives to promote public health practice competencies.
Conduct and support evaluation and research.
Assure financial support for a lifelong learning system in public health.
An almost universal priority for workforce development is ensuring that all public health practitioners have mastery over a basic set of competencies involving generalizable knowledge, skills, and abilities that allow them to effectively and efficiently function as part of their public health organizations or systems (CDC-ATSDR, 2000; DHHS, 2000; CDC, 2001d) (see Appendix E for an extended list of competencies for public health workers). Many experienced public health professionals require a variety of cross-cutting competencies to help them meet the routine and emergent challenges of public health, as well as specialized skills and abilities in areas such as maternal and child health, community health, and genomics. In addition, a recent survey of the local public health infrastructure found that several specific public health occupations are projected to be the most needed in the coming 5 years (NACCHO, 2001e). These occupations included public health nurses, epidemiologists, and environmental specialists (NACCHO, 2001e) (see Figure 3–2 ).
FIGURE 3–2
Public health occupations most needed in 5 years.
The Council on Linkages between Academia and Public Health Practice 8 has developed a list of 68 core public health competencies in eight domains (see Box 3–2 ), with different levels of competency expectations for frontline public health workers, senior professional staff, program specialists, and leaders (Council on Linkages between Academia and Public Health Practice, 2001). An expert panel convened by CDC, ATSDR, and HRSA has recommended adoption of this list as the basis for competency-based training of the public health workforce (CDC, 2000e). Use of this list as the basis for training and continuing education for the public health workforce was recommended, regardless of the programmatic or categorical focus of the training (CDC, 2000e). Efforts are under way in the various public health training networks to establish models that will contribute to a systematic approach to competency-based training that is linked to the essential services framework and grounded in prior competency validation efforts (CDC, 2000e).
BOX 3–2
The Core Public Health Competencies. Analysis and assessment Policy development and program planning
Meeting the Needs for Workforce Development
The issue of workforce training and competency is central to the success of any public health system. Governmental public health agencies have a responsibility to identify the public health workforce needs within their jurisdictions and to implement policies and programs to fill those needs. In addition, an assessment of current competency levels and needs is essential to develop and deliver the appropriate competency-based training, as well as to evaluate the impact of that training in practice settings. Workforce training and education efforts may be conducted in partnership with academia and other relevant and appropriate community partners, and ideally, a percentage of public health employees should be targeted annually for continuing education (DHHS, 2000). These and other issues are discussed in the 2003 IOM report Who Will Keep the Public Healthy: Educating Public Health Professionals for the 21st Century .
Training resources for the public health workforce are expanding, spurred by modest funding by HRSA for Public Health Training Centers and by CDC for Public Health Preparedness Centers. By mid-2002, there were 14 Training Centers and 15 Preparedness Centers, which form the backbone of a national public health training network. Both types of centers promote a variety of general workforce development strategies, although the CDC-funded centers place a heavier emphasis on bioterrorism preparedness.
Given the importance of the workforce in carrying out the mission of public health, the committee finds that education and development of the current workforce must continue to be a fundamental priority within the broader efforts to improve the state and local public health infrastructure. Therefore, the committee recommends that all federal, state, and local governmental public health agencies develop strategies to ensure that public health workers who are involved in the provision of essential public health services demonstrate mastery of the core public health competencies appropriate to their jobs. The Council on Linkages between Academia and Public Health Practice should also encourage the competency development of public health professionals working in public health system roles in for-profit and nongovernmental entities.
To facilitate ongoing workforce development, the committee encourages public health agencies to engage in training partnerships with academia to ensure the availability of coordinated, continuous, and accessible systems of education. These systems should be capable of addressing a variety of workforce training needs, ranging from education on the basic competencies to continuing education for individuals in the specialized professional disciplines of public health science.
Furthermore, the committee recommends that Congress designate funds for CDC and HRSA to periodically assess the preparedness of the public health workforce, to document the training necessary to meet basic competency expectations, and to advise on the funding necessary to provide such training.
Preparing Public Health Leaders
Senior public health officials must have the preparation not only to manage a government agency but also to provide guidance to the workforce with regard to health goals or priorities, interact with stakeholders and constituency groups, provide policy direction to a governing board, and interact with other agencies at all levels of government whose actions and decisions affect the population whose health they are trying to assure (Turnock, 2000). These tasks require a unique and demanding set of talents: professional expertise in the specific subject area; substantive expertise in the content and values of public health; and competencies in the core skills of leadership. Those who have mastery of the skills to mobilize, coordinate, and direct broad collaborative actions within the complex public health system must lead in implementing the actions outlined in this report. They require the skills for vision, communication, and implementation. Although many of these skills are innate for most professionals and other leaders, they need constant refinement and honing.
CDC has pioneered the development and funding of a national Public Health Leadership Institute, and in the intervening dozen years, more than 500 leaders in public health have been exposed to leadership training and skill building (described in more detail in the Academia chapter). Furthermore, a similar network of State and Regional Public Health Leadership Institutes has been funded and, over time, has developed the capacity to work collaboratively through a national network, which permits institutes to benchmark and share best practices and continue the process of learning needed to help with state-of-the art curriculum and educational training efforts. Equally notable has been the development of the Management Academy for Public Health, a joint effort of the major public health philanthropies. Although effort is still at an early stage, this academy has already generated graduates who work hand in glove with senior leadership in public health organizations. Furthermore, the Turning Point Initiative devotes efforts to increasing collaborative leadership across all sectors and at all levels (Larson et al., 2002)
Another key to leadership is continuity in office long enough to exert the leadership and to provide the institutional memory to defend public health agencies and the public health sector from the political winds of the moment. Yet, the committee finds there has been great difficulty in recruiting, developing, and retaining the leaders so vital to the job.
A state health official's term, if that official is a political appointee, is tied to the governor's term. Health officials must work with legislators who operate on 2-year terms. Given that the average tenure of a state health officer is relatively short (an average of 3.9 years and a median of 2.9 years) (ASTHO, 2002), many state health officials find it difficult to create longer-term plans for achieving health goals on shorter-term time frames (Meit, 2001). Additionally, because state health officers report to many governing bodies, they generally have less direct access to policy makers, and state health officials must prioritize the issues that they think deserve the most attention (Meit, 2001). Political factors at the state level can also have a significant impact on the abilities of public health leadership to influence policy. To address the specific issues of discontinuity occasioned by the rapid turnover, particularly of state health officials, the Robert Wood Johnson Foundation has funded a unique State Health Leadership Initiative administered by the National Governors Association to immerse newly appointed officials in a curriculum for political leadership and provide a network of resources and mentors.
Governmental public health leadership is a critical component of the infrastructure that must be strengthened, supported, and held accountable by all of the partners of the public health system and the community at large. For this reason, the committee recommends that leadership training, support, and development be a high priority for governmental public health agencies and other organizations in the public health system and for schools of public health that supply the public health infrastructure with its professionals and leaders.
Considering Credentialing as a Tool for Workforce Development
Credentialing is a mechanism that is used to certify specific levels of professional preparation. There are many different forms of credentials, including academic degrees, professional certifications, and licenses. For example, medical credentials include medical degrees to certify successful completion of course work, professional testing (e.g., through medical board exams) to provide evidence of qualification to practice medicine, and medical licensing to establish compliance with state standards for medical practice. An individual credentialed as a Certified Health Education Specialist (CHES) has successfully completed a course of study and passed a competency-based test.
Although some public health workers are credentialed as physicians, nurses, health educators, or environmental health practitioners, few are credentialed within those professions specifically for public health practice. Most physicians working in public health lack board certification in preventive medicine or public health; most nurses working in public health lack credentials in community public health nursing; and most individuals working as health educators lack the CHES credential. Furthermore, no single credentialing or certification process has been established to test the various competencies required for the interdisciplinary field of public health; thus, the majority of the public health workforce (80 percent) lacks credentials (HRSA, 2000).
Given the importance of establishing and maintaining a competent public health workforce, CDC and other public health agencies and organizations, including NACCHO, the Association of State and Territorial Health Officials (ASTHO), the Association of Schools of Public Health, and the American Public Health Association (APHA), are examining the feasibility of creating a credentialing system for public health workers based on competencies linked to the essential public health services framework. CDC (2001d) has recommended the use of credentialing. Such a process would complement efforts to establish national public health performance standards for state and local public health systems based on the essential public health services framework and the related objectives of Healthy People 2010 (Objective 23–11) (DHHS, 2000). Although this national effort focuses on experienced public health leaders, support is growing for the concept of credentialing at a basic level all public health workers and at an intermediate level the experienced professionals from many disciplines who share the need for higher-level, cross-cutting competencies in the areas of public health practice, community health assessment, policy development, communication, and program development and evaluation.
Certification or credentialing would help establish that public health practitioners have a demonstrated level of accomplishment in and mastery of the principles of public health practice. In terms of building the capacity of the public health workforce, the credentialing process could help document the knowledge, skills, and performance of experienced workers who may not have formal academic training and could encourage other workers to seek additional training to meeting credentialing requirements. An especially important component of this process is that it could play a key role in shaping the training and preparation of future public health practitioners and leaders.
The key challenge is whether and how public health organizations can begin to integrate competency-based credentialing in their hiring, promotion, performance appraisal, and salary structures. Although the idea of credentialing has considerable support at the federal level, states and particularly localities have voiced concerns that workforce credentialing mandates may become too closely tied to federal funding mechanisms. In these situations, the fiscal impact could be grave for public health departments that do not or cannot meet credentialing requirements (community informants, personal communications to the committee, 2001).
The committee finds that in the ongoing debate about public health workforce credentialing, what is most needed is a national dialogue that can address the full range of issues and concerns. Therefore, the committee recommends that a formal national dialogue be initiated to address the issue of public health workforce credentialing. The Secretary of DHHS should appoint a national commission on public health workforce credentialing to lead this dialogue. The commission should be charged with determining if a credentialing system would further the goal of creating a competent workforce and, if applicable, the manner and time frame for implementation by governmental public health agencies at all levels. The dialogue should include representatives from federal, state, and local public health agencies, academia, and public health professional organizations who can represent and discuss the various perspectives on the workforce credentialing debate.
Special Need for Communication Skills
The role of communication in public health practice cannot be underestimated. It is crucial for the successful performance of public health's core functions and essential services. Governmental public health agencies must communicate effectively internally as well as externally with other governmental agencies and nongovernmental stakeholders and partners. Informing and advising the public about health promotion and disease prevention are standard duties of both state and local public health agencies, and listening to community voices is also critical for programs to be effective. In emergency situations, public health professionals must have the ability to communicate clearly and effectively—being aggressive and credible enough to command attention—with both the public and other officials about the nature of the health hazards and the steps necessary to minimize health risks.
The response to the discovery of anthrax exposures in the fall of 2001 brought into sharp focus the importance of effective communication in the face of serious health risks. According to New York Times medical reporter Dr. Lawrence Altman, lapses and delays in communication with the public and with public health and health care professionals could have made the situation worse had the anthrax exposures been more widespread (Altman, 2001). Altman found that the delay was attributed in part to Federal Emergency Response Act restrictions about disclosing information and to the Federal Bureau of Investigation's (FBI's) criminal investigation. Altman suggested, however, that CDC could have issued information as a part of the parallel public health investigation that was already under way. The initial paucity of information on anthrax and the investigations in the Morbidity and Mortality Weekly Report ( MMWR ), one of CDC's most valuable means of quickly informing public health and health care professionals about communicable diseases, was also noted (Altman, 2001). MMWR 's editor reported being “out of the [information] loop” for some time (Altman, 2001). It should be noted that CDC used the Health Alert Network many times after September 11, 2001, to alert public health officials and to disseminate information.
The federal government's handling of the anthrax attacks also prompted criticism of DHHS for uncoordinated communication as well as a convoluted and inadequate public communication strategy (Connolly, 2001). For example, as reported by the press, the department's initial decisions to direct all media requests through the Secretary's press office effectively silenced CDC, FDA, and NIH, the agencies with the most relevant expertise (Connolly, 2001). The lack of information from DHHS was also frustrating to other federal, state, and local leaders and governmental public health officials, some of whom learned about new cases and contamination in their states though network and cable television newscasts (Connolly, 2001). The lesson from these and other communication breakdowns is evident: clear and effective communication, both internal and external, is a critical service of the governmental public health infrastructure.
Under more normal circumstances, public health communication is important for gathering information from the community about their health concerns as well as delivering and even “marketing” health information to the public. Because the responsibilities of public health agencies cover all aspects of health, public health officials are in a unique position to provide timely, accurate health-related information to the public on a wide variety of topics, ranging from depression and other mental health issues to obesity and physical activity, environmental health and safety, emergency preparedness, and policies that affect health or health outcomes.
However, few public health agencies have staff members who are trained to interact effectively with the public and to work effectively with the news media. In fact, the most recent examination of the public health workforce indicated that 575 individuals in the public health workforce have the expertise to be classified in the category of “Public Relations/ Media Specialist” (HRSA, 2000). Of these 575 people, most are working in DHHS and other federal health agencies. Of the others, 115 are working in state and territorial public health agencies and 12 are working in voluntary agencies (HRSA, 2000).
Given the tremendous potential of the mass media and evolving information technologies, such as the Internet, to influence the knowledge, normative beliefs, and behavior patterns of individuals and groups, governmental public health agencies must be prepared to use these communication tools. The public health workforce must have sufficient expertise in communications to be able to engage diverse audiences with public health information and messages and to work with the media to ensure the accuracy of the health-related information they convey to the public. For example, public health officials can develop relationships with journalists and assist them in accurately representing health risks and interpreting the significance of new research findings so that reporting on public health issues is accurate and members of the public can make informed decisions about protecting their health.
For these reasons, the committee finds that communication skills and competencies are crucial to the effective performance of the 10 essential public health services and the practice of public health at the federal, state, and local levels. Therefore, the committee recommends that all partners within the public health system place special emphasis on communication as a critical core competency of public health practice. Governmental public health agencies at all levels should use existing and emerging tools (including information technologies) for effective management of public health information and for internal and external communication. To be effective, such communication must be culturally appropriate and suitable to the literacy levels of the individuals in the communities they serve. To build this capacity in the public health workforce, communications skills and competencies should be included in the curricula of all workforce development programs. Communication competencies should include training in risk communication, interpersonal and group methods for gathering and transmitting information, and interfacing with the public about public health information and issues, as well as the interpretation of health-related news. This is addressed in greater detail in a companion report, Who Will Keep the Public Healthy: Educating Public Health Professionals for the 21st Century (IOM, 2003).
Information Networks
Information and the systems through which it is produced are critical tools that enable public health agencies to meet their responsibilities for monitoring health status and for identifying health hazards and risks to the populations they serve. Public health agencies also rely on information and information systems to assess communities' resources and their capacity to respond to health needs and problems. Such assessments inform the interventions and policies designed to address the community's health needs (Keppel and Freedman, 1995). It is essential that the governmental public health infrastructure have a system that is capable of supporting the collection, analysis, and application of myriad forms of health-related data and information.
Without adequate surveillance, local, state, and federal officials cannot know the true scope of existing health problems and may not recognize new diseases until many people have been affected.
Bernice Steinhard
General Accounting Office
The committee uses the term “information” in its most general form, referring to three distinct terms in information science: data, information, and knowledge. Data are the essential elements of information; that is, data are the measurements and facts about an individual, an environment, or a community. Information is what is generated when data are placed in context via the tool of analysis. When rules are applied to the information, knowledge is generated (Lumpkin, 2001). All of these elements—data, information, and knowledge—are critical products of public health information networks.
Of particular concern for the public health infrastructure are interrelated weaknesses in the nation's disease surveillance systems and inadequate access to information systems and communication tools. The committee emphasizes the need for an integrated information infrastructure to overcome many of these problems.
Surveillance Efforts and Reporting Systems
For communicable diseases, effective epidemiological surveillance can make the difference between the rapid identification and treatment of a few cases of disease and an outbreak that debilitates an entire community. Responsibility for surveillance, one of the most important functions of the public health infrastructure, is shared among federal, state, and local public health agencies. States and localities collect and report data; and federal agencies, especially CDC, in the case of infectious and chronic diseases, provide valuable technical support, training, and grant funding (GAO, 1999a).
The rapid development of new information technology offers the potential for a greatly improved surveillance capacity. For example, it is now possible to engage in real-time data collection via the Internet and through linkages to electronic patient records. New technologies also offer the potential for automated data analyses, such as pattern recognition software that would be able to detect unusual disease patterns. Moreover, new technologies offer new options for disseminating the information produced by surveillance efforts (Baxter et al., 2000). However, the nation's surveillance capacity is weakened by fragmentation and gaps.
Fragmentation of Surveillance Systems
Fragmentation has developed in surveillance systems in part because legal authority for surveillance rests with states and localities and they have not developed uniform standards for data elements, collection procedures, storage, and transmission. The lack of uniformity has made it difficult for states and localities to work collaboratively among themselves or with the private sector to develop more effective surveillance systems. Although The Future of Public Health recommended the development of a uniform national health data set (IOM, 1988), progress has been limited.
Requirements under the Health Insurance Portability and Accountability Act (HIPAA; P.L. 104–191) for the development and use of comprehensive new standards for the electronic transmission of health information may result in greater consistency of certain types of data. However, there is uncertainty about the scope of the rules under HIPAA, and state and local health departments must determine what portion of their electronic health information might be subject to the requirements established by HIPAA (ASTHO, 2001a, 2001b).
Another key factor shaping the development of surveillance systems is that, historically, investment in these systems has been largely categorical, resulting in fragmentation of surveillance efforts across the spectrum of infectious disease threats and other programs for other specific diseases and populations. An inventory of public health data projects and systems identified more than 200 separate DHHS data systems in seven broad programmatic areas (Boufford and Lee, 2001). The multiplicity of surveillance systems for food-borne illnesses illustrates the problem (see Box 3–3 ).
BOX 3–3
An Example of Fragmentation in Disease Surveillance Systems. A recent study—based on a survey of public health officials in all 50 states, the District of Columbia, and New York City—of the Centers for Disease Control and Prevention's (more...)
A lack of integration in federal data systems helps drive fragmentation at the state and local levels. Data collected in accordance with the specifications of separate federal programs often cannot be accessed at the local level because of differences in formats, definitions, classification systems, personal identifiers, or sampling strategies (Lumpkin et al., 1995). The fragmentation means that state and local public health agencies inevitably must spend time on duplicative data-reporting activities that drain already scarce staff resources (GAO, 1999a). The current combination of system incompatibility and lack of integration hinders the ability of program managers to know what information exists and how to access that information and hinders the ability of local health agencies to provide integrated care to their communities (Lumpkin et al., 1995). CDC's National Electronic Disease Surveillance System (NEDSS) is working to electronically integrate a number of surveillance activities; details can be found in the discussion of information systems later in this chapter.
Gaps in Surveillance
Existing surveillance activities contain notable gaps. In particular, little information is routinely collected on chronic diseases and conditions, such as asthma and diabetes, even though chronic diseases account for four of every five deaths in the United States and annually cost the nation approximately $325 billion in health care and lost worker productivity (Pew Environmental Health Commission, 2000). Similarly, environmental pollutants and toxins are monitored primarily for the purposes of environmental protection and regulation, but no surveillance and tracking system monitors the health outcomes, such as birth defects and developmental disorders, that are potentially linked to toxic exposures. With an improved awareness of these health risks and a more comprehensive understanding of the health status of the population, public health agencies from the federal to the local level would be able to design better interventions and prevention efforts.
The Pew Environmental Health Commission (1999, 2000) has called for the development of a national health-tracking network to monitor the prevalence of chronic conditions such as asthma and for the development of national birth defects registries. Ideally, these comprehensive disease registries and surveillance networks would be accessible to and used by state and local public health agencies to better understand and monitor the health status of the communities they serve. Additionally, these registries would have the potential to be linked with registries from private health care delivery organizations (such as hospitals and managed care organizations) so that more comprehensive disease prevalence estimates could be easily and readily obtained. The Pew Environmental Health Commission reports and recommendations have been endorsed by major public health organizations, including APHA, ASTHO, the Association of Public Health Laboratories, the Council of State and Territorial Epidemiologists (CSTE), NACCHO, and the Public Health Foundation (PHF). The committee strongly supports this recommendation and applauds the U.S. Congress for providing $17.5 million for the development and implementation of a nationwide environmental health-tracking network and capacity development in environmental health in state and local health departments (Conference Report Accompanying H.R. 3061, 2002).
Another gap in the current disease surveillance system is syndrome surveillance, which captures data on the basis of clinical signs and symptoms of illness (e.g., a fever or rash), not just formal diagnoses of specific diseases. Related indicators for such surveillance might be sales of prescription and nonprescription medications. Interest in syndrome surveillance has grown because of its potential value for early detection of disease outbreaks, including those that might result from a bioterrorist act. Such a system depends on the rapid aggregation and assessment of data to permit detection of clinical and geographic patterns.
Although no national syndrome surveillance network is in operation, some state and local public health agencies are beginning to test and implement such systems. For example, New York City has had an active syndrome surveillance system since the 1990s (LLGIS, 2001), and systems are also operating in the Seattle–King County Department of Public Health (Duchin, 2002) and the Idaho Department of Health and Welfare (1999). Syndrome surveillance systems played an important role during the anthrax outbreaks in New York City and in the Washington, D.C., area.
These systems generally require partnerships with practicing physicians, hospital emergency rooms and outpatient departments, community-based clinics, and sometimes neighboring state and county health departments. A system conceived at Sandia National Laboratories (2002), 9 the Rapid Syndrome Validation Project (RSVP), is being developed and tested in a collaborative effort with the New Mexico Health Department, Los Alamos National Laboratory, and the University of New Mexico Health Sciences Center, Department of Emergency Medicine. RSVP incorporates a realtime medical database and allows electronic data linkages with all local health departments throughout the state, the four district offices and their satellites, and the state offices.
At the federal level, CDC's Enhanced Surveillance Project (ESP) is working with state and local health departments and information systems contractors to develop real-time syndrome surveillance and analytical methods (CDC, 2001d). During special events, ESP sites monitor data on emergency department visits at sentinel hospitals. These data are analyzed at CDC and reported back to the health departments for confirmation and appropriate follow-up. ESP has been tested at events such as the Republican and Democratic National Conventions in 2000 and the 2002 Olympic Games in Utah (CDC, 2001d). DOD (2002), through its Global Emerging Infections Surveillance and Response System, is evaluating a system for the rapid identification of disease-related syndromes in patients at military health care facilities in the Washington, D.C., area.
The committee notes that although these syndrome surveillance programs show promise, their widespread effectiveness is still being evaluated and no syndrome surveillance system has identified a potential biological emergency. A forthcoming report (2003) by the IOM Committee on Emerging Microbial Threats to Health in the 21st Century addresses syndrome surveillance in more detail.
Information Systems and Communications Tools
New systems and technologies.
Several initiatives have emerged to try to resolve the problems of fragmentation and incompatibility in the nation's disease surveillance systems and to gain the benefits of integrated health data networks and communications systems. A key 1995 report, Integrating Public Health Information and Surveillance Systems , documented the problems and recommended a framework for leadership on the issue as well as specific steps for achieving the long-term vision of integration of public health information and surveillance systems (CDC, 1995). After publication of that report, CDC established the Integrated Health Information and Surveillance Systems Board to formulate and enact policy for integrating public health information and surveillance systems, yet it is not clear that it has played this role. If adequately supported, the board could provide an ongoing coordinating mechanism for CDC and ATSDR to lead the integration of public health information systems.
In 1992, CDC developed the Information Network for Public Health Officials (INPHO) in collaboration with state health departments. INPHO was established to foster communication between public and private partners, to make information more accessible, and to allow the rapid and secure exchange of data (GAO, 1999a). By 1997, 14 states had begun INPHO projects, some combining their INPHO resources with other CDC grant funds to build statewide networks linking state and local public health departments. Some states' networks include links to private laboratories. The system has produced measurable benefits in some states. For example, in Washington State, electronic information-sharing systems reduced the passive reporting time from 35 days to 1 day and gave both local authorities and the School of Public Health at the University of Washington access to health data for analysis (Davies and Jernigan, 1998; P. Wahl, personal communication, February 2, 2002).
The recommendations of the 1995 report have also led CDC to develop NEDSS (CDC, 2000b). Although the system is now in the early stages of development, one of its objectives is to electronically integrate a variety of surveillance activities, including the National Electronic Telecommunications System for Surveillance and the reporting systems for HIV/AIDS, tuberculosis, vaccine-preventable diseases, and infectious diseases. It is also intended to facilitate more accurate and timely disease reporting to CDC and state and local public health departments. NEDSS will incorporate data standards, an Internet-based communication infrastructure that is designed according to industry and public policy standards on data access and sharing, confidentiality protection, and burden reduction (CDC, 2000b).
CDC has also developed the Epidemic Information Exchange (Epi-X). This system, which became operational in November 2000, enables secure, web-based communication among federal, state, and local epidemiologists, laboratories, and other members of the public health community and allows them to instantly notify others about urgent public health events and search the Epi-X database for information on outbreaks and unusual health events.
Another initiative, the Health Alert Network, emphasizes the communication capabilities that are necessary for more integrated information systems. It was designed as a system for electronic communication between health departments and CDC, with the Internet used as its backbone (CDC, 2000c). It also supports distance-learning activities and provides health departments at all levels with the capacity to broadcast and receive health alerts (CDC, 2000c). Although parts of this system are still in development, CDC used the Health Alert Network at noon on September 11, 2001, to advise public health officials to begin heightened disease surveillance (NACCHO, 2001b).
In support of these various activities, CDC is adopting information technology standards and procedures to establish a secure data network (SDN). Network development focuses on the technical requirements for maintaining the confidentiality of data and providing a secure method for encrypting and transferring files from state health departments to a CDC program application via the Internet. The SDN not only gives CDC several ways of obtaining data from states, but it also provides a consistent method for authenticating the transmission source and ensuring data integrity (CDC, 2000c). A public health information network is under consideration at CDC to serve as a vehicle, with an effective governance mechanism, to ensure the integration of existing public health information systems within CDC and coordinated development of future ones with state and local public health agencies.
Although the committee applauds the development of these important systems and coordination efforts, it is concerned about the apparent lack of an effective mechanism to ensure their integration or their coordination with future efforts to create a fully developed national health information infrastructure, which we strongly support.
Continuing Problems
Despite these efforts, the public health information infrastructure is not yet fully capable of handling situations for which rapid, clear communication and information transfer are essential. Because the integration of public health data and information networks has not yet been accomplished, state and local public health agencies are still obliged to operate the more than 100 disparate data systems whose lack of integration slows the flow of information in times of crisis. Data and information network integration must also take into account the new data and information systems under development. Many of these new systems have not been fully implemented across the nation or, in the case of Epi-X, have been implemented only at the state level, leaving localities with read-only terminals and other tools that prevent interactive access to information or, even worse, leaving them out of the information loop entirely (Brewin, 2001). Furthermore, many local public health agencies, especially those in small and remote communities, do not have the resources or technical capacity to handle the implementation of new information technology, which requires expensive and complicated hardware and software. These disparities result in some states and localities having easy access to updated or urgent information, whereas others must continue to rely on the now-antiquated methods of paper-based reports, telephone connections, and the U.S. Postal Service as their primary means of retrieving and reporting information.
Early detection and response is critical, and it all hinges on communications and information technology.
Dr. Paul Wiesner
DeKalb County,
Georgia, Board of Health
These weaknesses were demonstrated clearly during the bioterrorism events of October 2001. Despite the years of warning about the potential for such attacks, only half of the nation's state, local, and territorial public health departments had full-time Internet connectivity when the first anthrax case was reported on October 4. Another 20 percent of state, local, and territorial health agencies lacked e-mail and, therefore, were unable to receive electronic updates regarding the anthrax events (Brewin, 2001). Given that robust and smoothly functioning information and communications networks are the key to defending against a bioterrorist attack, many of the nation's public health agencies were left unprepared.
Since September 11, 2001, public health agencies and officials have repeatedly urged the U.S. Congress to increase the levels of funding devoted to improving the nation's public health information infrastructure. The recommendations in CDC's review of this infrastructure specifically emphasized the need to ensure that health departments at all levels have access to modern means of rapid electronic data exchange and communication (CDC, 2001c). Although the current bioterrorism preparedness appropriations ($40 million) are directed toward the Health Alert Network and Epi-X (CSTE, 2001), these are just two of the systems necessary for enhanced, comprehensive disease surveillance (NACCHO, 2001e). It is possible that additional appropriations for bioterrorism or emergency preparedness may be able to provide more resources for the improvement of the other components of the nation's surveillance and information networks.
Moving Toward a National Health Information Infrastructure
Through the Telecommunications Act of 1993, the nation embarked on an effort to develop a National Information Infrastructure (NII), sometimes called the Information Super Highway (Boufford and Lee, 2001). The National Health Information Infrastructure (NHII) is the health component of this effort. Whereas some parts of the federal government, such as the Department of Commerce and the National Aeronautics and Space Administration, have moved ahead quickly on their NII agendas, the areas of public health, human services related to health, and community health are the least developed aspects of NII.
The National Committee on Vital and Health Statistics (NCVHS), the key external advisory body on data activities to the Secretary of DHHS, has outlined a vision and a process for building NHII. The report Information for Health: A Strategy for Building the National Health Information Infrastructure (NCVHS, 2002) presents the core of the vision as the pulling together of many separate initiatives and systems into an integrated data system that will give health officials and others optimal access to the information and knowledge they need to make the best possible health decisions for communities. The report's recommendations are comprehensive, stressing the importance of information flow to the public and across sectors of the public health system and attaching equal importance to consumer, clinical, and population health dimensions (NCVHS, 2002). To ensure that NHII supports all facets of individual health, health care, and community health, it must be developed in a manner that takes into account human factors (e.g., values and relationships), institutional requirements (e.g., practices, laws, and standards), and technological components (e.g., systems and applications).
NHII, when implemented, could have a profound impact on the effectiveness, efficiency, and overall quality of health and health care in the United States. It would allow the public health system and others to address concerns such as public health emergencies, medical errors, and health disparities in a more timely and comprehensive fashion (NCVHS, 2002). The links to data from the health care delivery system are critical to state public health agency efforts to monitor the quality of health care. The community aspects of population health are ripe for development as part of NHII because of the emerging scientific insight into the nature of health and its determinants (see Chapter 2 ). Better access to information on communities and their subpopulations will help health professionals and others identify various health threats, problems related to social or environmental conditions, and the unique needs of vulnerable populations. More powerful information tools will help identify patterns and trends from isolated events, and the rapid communication afforded by the network will aid in informing and educating individuals and the community at large about critical health issues.
The committee agrees with NCVHS that the nation's public health interest is served by the development of a standardized approach to an information infrastructure and that the development of a comprehensive, integrated system is a federal responsibility. Therefore, the committee recommends that the Secretary of DHHS provide leadership to facilitate the development and implementation of the National Health Information In frastructure (NHII). Implementation of NHII should take into account, where possible, the findings and recommendations of the National Committee on Vital and Health Statistics (NCVHS) working group on NHII. Congress should consider options for funding the development and deployment of NHII (e.g., in support of clinical care, health information for the public, and public health practice and research) through payment changes, tax credits, subsidized loans, or grants.
In carrying out this responsibility, CDC should ensure that this system is easily accessible and can be used and maintained by public health agencies at the federal, state, and local levels. This system should include the establishment of standards for consistent data collection and transmission practices, the assurance of privacy protections, the capacity for transmission of urgent health alerts across all levels of the public health system, and the implementation of data systems that facilitate reporting, analysis, and dissemination. CDC should work with its public health partners to ensure adequate and ongoing training in the effective use of the techniques that comprise this system. Although this system is critical for the fulfillment of the essential services of public health, it should also be both respectful of the need for privacy protections and mindful of the need for efficient data exchange.
The exact cost of a comprehensive NHII needs to be determined. Estimates by Lee and colleagues (2001) indicate a total need of about $14 billion over 10 years. This would be a combination of federal, state, local, and private-sector funds ramping up to a peak investment of $1.7 billion per year in 2007 and flattening out for the remaining years; the amounts needed to sustain the system after that period were not estimated.
Public Health Laboratories
Public health laboratories are a critical component of the disease surveillance resources of the public health infrastructure, providing essential capacity to detect, identify, and monitor the presence of infectious or toxic agents in populations and the environments in which those populations live. Investigations in these laboratories resulted in the identification of the organisms that cause diphtheria, cholera, tuberculosis, Hansen's disease (leprosy), and typhoid fever, paving the way for the development of vaccines and treatments to prevent and control those diseases (Valdiserri, 1993). Public health laboratories are also described as the safety net between the local water plant and the kitchen tap in many communities (APHL, 2000); they provide laboratory support for epidemiological studies and perform diagnostic tests (such as cytology testing and neonatal screening) that may influence the treatment of individual patients. Moreover, public health laboratories provide leadership to set laboratory regulations and serve as the standard of excellence for local and private laboratory performance (APHL, 2002a).
In 1999, the General Accounting Office (GAO) (1999a) reported that the nation had 158,000 clinical laboratories, of which 90,000 were in physicians' offices. About 10,000 laboratories were in hospitals or were privately operated. Every state public health department operates at least one laboratory, and some local health departments have laboratory facilities. Federal laboratories, such as those operated by CDC, provide testing services and consultation not available at the state level and training in testing methods (GAO, 1999b). CDC's Division of Laboratory Systems supports extramural and intramural research and oversees a laboratory standards program that describes laboratory practices and services and that assesses parameters for measuring and testing quality (CDC, 2001c). Highest priority is given to research on testing of diseases that are of the greatest public health importance (e.g., HIV and tuberculosis) and research to enhance the standards under the Clinical Laboratory Improvement Amendments (CLIA) (e.g., genetic testing and cervical cytology). 10
GAO (1999a) also recommended that the CDC director lead an effort by federal, state, and local public health officials to establish a consensus on the core laboratory capacities needed at each level of government. This information will aid policy makers in assessing whether existing resources are adequate and evaluating where investments are most needed.
With regard to the financing of state public health laboratories, unpublished survey data from the Association of Public Health Laboratories (APHL) show that in FY 2001, public health laboratories received a median of 50 percent of their funding from states, with a median of 33 percent from fee-for-service funding and about 15 percent from the federal government (S. Becker, Executive Director of APHL, personal communication, June 13, 2002). Although these percentages reflect the funding data obtained by APHL for both FY 1999 and FY 2001, the trend is that state funding for public health laboratories has been decreasing and fee-for-service funding has been increasing, potentially encouraging laboratories to increase their levels of fee-for-service activities. Although federal funding has remained relatively constant, the recent increases in federal funding for bioterrorism and emergency preparedness and response are likely to increase the federal contribution to public health laboratories.
GAO (2001b) reported that the nation's laboratories and other parts of the infectious disease surveillance system were not well prepared to detect or respond to a bioterrorist attack because of reductions in laboratory staffing and training that have affected the ability of state and local authorities to identify biological agents. The limitations of existing laboratory capacity were clearly demonstrated by the 1999 outbreak of West Nile virus in New York State. Even with a relatively small outbreak in an area served by one of the nation's largest local public health agencies, the investigations taxed federal, state, and local laboratory resources (GAO, 2001b). Both New York State and CDC laboratories were inundated with requests for testing, and CDC had to process the bulk of the testing because of the limited capacity of the New York State laboratories. Federal officials indicated that if another outbreak had occurred simultaneously, CDC would not have been able to respond (GAO, 2001b).
Many public health laboratories are unable to keep pace with the monitoring and tracking of infectious agents that are already known in communities. Some states do not routinely test for important infectious diseases. For example, although most states conducted surveillance for tuberculosis, Escherichia coli O157:H7, pertussis, and cryptosporidiosis, fewer than half of state laboratories tested for penicillin-resistant Streptococcus pneumoniae and hepatitis C (GAO, 1999a). Nearly half of the state public health laboratories lacked access to advanced molecular detection systems and other technologies for identifying specific strains of pathogens, information that is valuable to epidemiological investigations to trace the sources of disease outbreaks.
Many state public health directors and epidemiologists report that inadequate staffing and information-sharing problems hinder their ability to generate and use laboratory data for surveillance (GAO, 1999a). A recent study conducted by APHL (2002b) raised concerns about the public health laboratory workforce. The study found that the country is facing an imminent shortage of qualified public health laboratory directors. APHL anticipates 13 vacancies over the next 5 years in state public health laboratory directorships, with a replacement pool that current laboratory directors describe as either inadequate or marginally adequate in size to meet future demands (APHL, 2002b). Moreover, inadequate laboratory staffing is a problem. Although there is great variability in laboratory staffing among the states, states devoted a median of 8 staff per 1 million population to laboratory testing of infectious diseases 11 (GAO, 1999b). Additionally, according to the American Society for Clinical Pathology, the United States faces a serious shortage of medical laboratory personnel (ASCP, 2000). In state or local laboratories that have few personnel trained to handle the complexity and volume of work associated with bioterrorism scares (e.g., anthrax), there is little capacity to sustain states of “alert” for days or weeks (APHL, 2002b).
Efforts are under way to modernize the manner in which laboratory information is recorded and communicated; these efforts emphasize the use of automated, electronic systems (CDC, 1999). A 1997 meeting of CDC, CSTE, and APHL to design strategies for implementing effective electronic laboratory-based reporting produced a recommendation to base such strategies on the use of Health Level 7 (HL–7), a national standard for communicating clinical health information (CDC, 1997). Other issues discussed at a 1999 meeting included modes of data transmission, data privacy, software development, data quality, data flow, and recommendations concerning leadership and coordination, software tools and technical support, policy development, training and education, and public–private collaborations (CDC, 1999).
In 2001, the Center for Infectious Disease Research and Policy (CIDRAP) and the Working Group on Bioterrorism Preparedness 12 estimated that approximately $200 million was needed as an initial investment to improve state and local preparedness with regard to laboratory capacity. This funding would support
- Further development and implementation of the Laboratory Response Network, which is a multilevel laboratory network composed of federal, state, county, and city public health laboratories designed to receive and analyze specimens from a range of sources;
- Full implementation of the National Laboratory System, which is a communications system designed to rapidly share laboratory information among public health, hospital, and commercial laboratories;
- Integration of chemical terrorism preparedness into laboratory improvements; and
- Improved diagnostic testing and identification of potential agents of bioterrorism by animal and wildlife laboratories and improved communications among human, animal, and wildlife laboratories.
CDC has initiated a program to develop a cohesive national laboratory system to ensure disease surveillance and the capacity for effective response (CDC, 2001c). Under this initiative, the proposed National System for Laboratory Testing for Public Health seeks to ensure the availability of a consistent public health laboratory capacity (CDC, 2001c). A report on the FY 2002 bioterrorism-related appropriations provided for infrastructure improvements. In FY 2000, CDC awarded approximately $11 million to 48 states and four major urban health departments to improve and upgrade their surveillance and epidemiological capabilities (GAO, 2001b). More recently (2002), bioterrorism-related federal funds ($1 billion) designated to help prepare state infrastructures for bioterrorism and other emergencies have begun to flow to states ( http://www.hhs.gov/news/press/2002pres/20020131b.html ). The bulk of funds designated for laboratory capacity building (about $40 million) will go to enhance CDC's intramural laboratory capacity.
State public health laboratories, assisted by CDC, are working to deploy more sophisticated laboratory equipment that can help identify suspected bioterrorism attacks quickly and precisely. In addition, CDC is working to validate the use of molecular DNA and antibody tests in potential cases of bioterrorism; setting uniform guidelines for the use of faster, more sensitive instruments; and planning to supply state public health laboratories with identical kits of biological reagents necessary to identify bioterrorism agents. The efforts aim to improve confidence in test results and guarantee that the results can be verified quickly at other laboratories (Hamilton, 2001).
Given the important role of public health laboratories in assuring the health of the population and in protecting the nation's security, the committee believes that federal, state, and local public health agencies should have access to a strong, state-of-the-art public health laboratory system. Furthermore, the committee believes that these public health laboratories are an essential part of a robust and stable surveillance capability necessary to identify emerging threats, natural or intentional, to the health of the public and to track the effectiveness of interventions at multiple levels.
In addition to the overall assessment of the public health system, the committee recommends that DHHS evaluate the status of the nation's public health laboratory system, including an assessment of the impact of recent increased funding. The evaluation should identify remaining gaps, and funding should be allocated to close them. Working with the states, DHHS should agree on a base funding level that will maintain the enhanced laboratory system and allow the rapid deployment of newly developed technologies.
Special Role of the Governmental Public Health Infrastructure in Emergency Preparedness and Response
In the wake of the events of September 11, 2001, federal, state, and local public health agencies—and indeed, the nation as a whole—have been grappling with the crucial question of whether the public health system is prepared to cope with future terrorist attacks. Even before the events of 2001, the threat of chemical terrorism had grown more real in the United States because of developments in the mid-1990s such as the discovery of the Iraqi biological weapons program and the release of sarin nerve gas in the Tokyo subway by the Aum Shinrikyo cult (Henderson, 1998). Resources put into the improvement of the public health system's ability to respond to bioterrorism will yield benefits that go far beyond that specific concern, but only if adequate funds are made available to strengthen the public health infrastructure's ability to detect and combat natural disease outbreaks, such as E. coli and other food-borne pathogens, and to work with other vital partners in the public health system to provide the protection necessary for the assurance of public health.
With our public health infrastructure in its current shape, trying to detect and respond to a bioterrorism attack is comparable to running O'Hare Airport's air traffic control system with tin cans and string.
Dr. Michael Osterholm
University of Minnesota
Readiness of Local Public Health Agencies
Until recently, the degree to which public health departments were actually prepared for bioterrorist attacks or other emergencies was unknown. Determining the level of state and local health departments' emergency preparedness and response capacities is crucial because public health officials are among those, along with firefighters, emergency medical personnel, and local law enforcement personnel, who serve on “rapid response” teams when large-scale emergency situations arise. These health department officials must work closely with federal public health agencies such as CDC and, occasionally, law enforcement agencies (e.g., the FBI and the Department of Justice) to investigate and resolve the various threats to the community's health, regardless of whether the threat is natural in origin (e.g., floods, tornadoes, and earthquakes) or intentional (e.g., bioterrorist attacks).
Two weeks following the attacks on September 11, 2001, NACCHO (2001a) conducted a brief survey to understand the impacts of the events on local health departments and to assess how well those health departments would be able to respond in the event of this and other types of emergencies such as biological or chemical threats. Of the 999 NACCHO members contacted, 530 responded within a week. Survey results indicated that local public health officials played a variety of roles in response to the September 11 terrorist events, including communicating with various community-level partners; working with response partners to develop, update, and review emergency response protocols and plans; and providing information to the media and the concerned public. Of the inquiries received by local health officials, most concerned vaccination and the availability of medicines. Other inquiries focused on the degree to which the local community was prepared and what the local public health agency was doing to prepare the community.
The public health system is the vital link in our ability to preserve and protect human life when disaster strikes.
ASTHO (2001c)
An alarming finding was the extent to which the local public health agencies themselves were unprepared for bioterrorist attacks. Of those who responded, only 20 percent indicated that their agency had a comprehensive response plan. Most of the respondents, 56 percent, indicated that their agency's response plan was still under development, and 24 percent indicated that their agency had no plan at all (NACCHO, 2001a). Health officials themselves were also unprepared. When asked how prepared they felt to respond to concerned citizens' inquiries, only 38 percent of health officials stated that they were “pretty well prepared” to respond, whereas another 50 percent of respondents indicated that they were only “somewhat prepared.” The remaining respondents (12 percent) felt that they were “not prepared at all” (NACCHO, 2001a).
Survey respondents also reported on the frustrations that they encountered during that time of crisis. For example, the main frustration voiced was the lack or malfunctioning of resources and equipment, including necessary communications tools such as pagers, cell phones, e-mail, and faxes. The second most common frustration was the partial or total lack of communication from federal and state agencies, which was often interpreted as a sign of poor leadership. In fact, some health officials indicated that they had to rely on the news media rather than on local disaster response agencies, state public health departments, or federal agencies to be alerted to and receive updates about the September 11 crisis (NACCHO, 2001a). Other state and local public health officials noted that during the subsequent anthrax outbreaks, staff attention to other public health activities was diverted to responding to the public's concerns and questions, not to mention the investigation of false anthrax reports (California Bay Area Health Officials, personal communication, 2001).
Improving Preparedness
The data from the NACCHO survey paint a disquieting picture of the preparedness of the nation's local health departments and thus the heightened vulnerability of communities. This is hardly surprising news, however, given that state and local public health agencies have been underfunded and understaffed for decades and have less “surge capacity or potential” (i.e., the ability to respond to a sudden influx of demand) than hospitals (Center for Civilian Biodefense Studies, 2001). Several efforts to improve readiness are under way.
In 1999, DHHS created the Bioterrorism Preparedness and Response Initiative, which is aimed at upgrading the nation's public health capacity to respond to bioterrorism and to establish a formal Bioterrorism Preparedness and Response Program. 13 So far the accomplishments that have been under this initiative include creation of a National Pharmaceutical Stockpile Program and operationalization of the Rapid Response and Advanced Technology Laboratory, which is able to identify rapidly biological and chemical agents rarely seen in the United States (CDC, 2001a).
The development of a nationwide, integrated information, communication, and training network (of which the Health Alert Network, NEDSS, and Epi-X should be a part), as recommended by the National Committee on Vital and Health Statistics, will also help strengthen the ability of federal, state, and local public health agencies to share information (CDC, 2001a). External communications systems also must be strengthened to ensure the rapid and effective transfer of information and communication between public health agencies and other frontline emergency responders, including health care providers, law enforcement and emergency response personnel, and government officials (CDC, 2000a). The importance of effective communication in times of crisis cannot be overstated (ASTHO, 2001c).
The Columbia University School of Nursing Center for Health Policy is a CDC-supported project that has specified the competencies in emergency response needed by all public health workers (Columbia Center for Health Policy, 2001). These individual competencies are complementary to the organizational capacities for bioterrorism response developed by CDC (2001b), the standards for state and local public health performance (CDC, 2001b), and procedures for state and local public health department leaders to notify CDC in the event of a bioterrorist attack (CDC, 2001a).
It is also vital that health care providers and facilities acknowledge their important role as part of the larger system that assures population health, both in general and in times of crisis. Because frontline health care providers (i.e., those in urgent care and emergency room facilities) are often the first to see unusual illnesses or injuries, they must constantly be vigilant to notice trends that seem out of the ordinary and must report these trends to local public health departments (ASTHO, 1999; CDC, 2000a). Once such observations are reported, public health investigators can provide appropriate follow-up through epidemiological investigations.
Investing in Infrastructure Improvements
If the United States is going to be appropriately prepared for a terrorist attack (biological, chemical, or otherwise), one of the top priorities must be to strengthen the public health infrastructure at all levels so that it is strong enough, flexible enough, and capable enough to respond to emergency situations of this nature (CDC, 2000a).
An estimated initial investment of approximately $400 million is needed to improve state and local preparedness with regard to personnel, training, epidemiology, and surveillance capacity (Center for Infectious Disease Research and Policy and Workgroup on Bioterrorism Preparedness, 2001). This level of investment would cover the integration of bioterrorism preparedness activities into existing communicable disease prevention and control programs such as CDC's emerging infections program, the training of public health practitioners, and the hiring of designated public health veterinarians for states that do not have one. An estimated additional $200 million was also recommended to begin to improve state and local preparedness with regard to information and communication systems (e.g., Health Alert Network, NEDSS, Epi-X, and rapid communication systems). It was also noted that additional funds would be needed to sustain these systems effectively over time.
Progress toward these estimated needs has been addressed by some of the new resources for infrastructure improvement made available through bioterrorism-related appropriations. A report on the FY 2002 appropriations makes reference to infrastructure improvements such as those authorized by the Public Health Improvement Act of 2000 (P.L. 106–505). Furthermore, in 2002, Congress authorized a variety of bioterrorism-related activities in the Public Health Security and Bioterrorism Preparedness and Response Act of 2002 (OMB, 2002) (see Table 3–1 ).
TABLE 3–1
FY 2002 DHHS Bioterrorism Funding.
Following the passage of the Public Health Threats and Emergency Act of 2000, there were plans to develop two separate grant programs—one for basic public health infrastructure and the other for bioterrorism preparedness. These were subsequently combined with a stronger emphasis on specific preparation for bioterrorism and other such emergencies.
CDC staff (Office of Terrorism Preparedness and Emergency Response) provided information on funding for the state and local public health infrastructure from FY 1999 to FY 2002 as a subset of total appropriations for bioterrorism. Of total appropriations of $124 million (FY 1999), $156 million (FY 2000), and $182 million (FY 2001), $55 million, $57.6 million, and $67.8 million, respectively, were allocated to state and local capacity building prior to the FY 2002 DHHS bioterrorism funding. The bulk of the funding was for the Health Alert Network; and smaller amounts were allocated for public health laboratory infrastructure and other needs, such as staff development and epidemiology and detection systems. For FY 2002, and prior to September 11, 2001, states were to receive $75 million; however, this amount was supplemented with $915 million. The following seven “capacity areas” (along with the estimated funding levels), deemed necessary for bioterrorism preparedness, were identified for allocation of these funds:
Preparedness planning and readiness assessment ($183 million, including $65 million for the pharmaceutical stockpile)
Surveillance and epidemiology capacity ($183 million)
Laboratory capacity, biological agents ($118.9 million)
Laboratory capacity, chemical agents ($0)
Health Alert Network/communication and information technology ($109.8 million)
Communicating health risks and health information dissemination ($46.7 million)
Education and training ($91.5 million)
The total represents about 42 percent of CDC's total appropriations for bioterrorism and emergency preparedness.
Although the overall resources for the improvement of state and local public health department capacities have increased substantially because of these allocations, it should be noted that the local public health infrastructure provides other important functions that are not covered by the improvements made as a result of these appropriations (e.g., conducting active syndrome surveillance, performing on-the-spot epidemiological investigation, developing local-level bioterrorism preparedness plans, and administering mass vaccinations) (NACCHO, 2001c). For these reasons, it is important to ensure that the improvements that will be made to state and local infrastructures are based on comprehensive data about what is needed to ensure the delivery of the 10 essential public health services at the community level. Furthermore, it is important to ensure that funding levels are sustained over time to maintain these improvements. Most importantly, however, the improvement of public health preparedness capabilities will require the sustained involvement and commitment of policy makers at all levels of government, with ample attention being given to ensuring appropriate accountability (Salinsky, 2002). Doing so is crucial in assuring the safety and preparedness of all of the nation's communities.
Can an appropriate balance be struck between responding to the threat of bioterrorism and ensuring an effective public health response to the health problems facing the nation on a daily basis, such as HIV/AIDS and heart disease?
Eileen Salinsky
National Health Policy Forum
- FINANCING THE PUBLIC HEALTH INFRASTRUCTURE
State and local governments traditionally have had financial responsibility for basic governmental public health services, such as workforce training, the development of information systems and the organizational capacity to conduct disease surveillance and prevention programs, the management of public health laboratories, the implementation of population-based prevention and health education programs, and other protections such as water and air quality management, waste disposal, and pest control. Yet the federal government also has a financial responsibility for assuring the capacity of the public health infrastructure at the state and local levels. Unlike the areas of medical care and biomedical research, however, the federal government has never made a similar level of investment in the public health infrastructure, such as the clinical laboratories, surveillance systems, or environmental monitoring systems needed to monitor health and health threats at the state and community levels. In the past, in response to perceptions of great national need, substantial federal investments played a crucial role in the development of the hospital industry and of the biomedical research capacity as well as the expansions of medical schools. What a national government pays for is a critical statement about priorities.
Assessing Infrastructure Costs and the Need for Federal Investment
As the committee has noted, there are vast differences across the country in the scope of activities, the resources available, and the organization of the governmental public health infrastructure at the state and local levels and in the sizes of the populations served. This complicates the task of assessing the cost of public health services and the appropriate investment in the governmental infrastructure that delivers these services or ensures that they are provided. In 1997, the DHHS Office of the Assistant Secretary for Planning and Evaluation commissioned the Lewin Group 14 to develop a comprehensive data strategy to characterize the state of the nation's public health infrastructure. The report urged a collective effort with ASTHO, NACCHO, and PHF to study the status of the public health infrastructure and respond with a sustained investment plan to address the needs identified (The Lewin Group, 1997).
Assessing the funds and expenditures for the public health infrastructure at the local level is complex. Data from NACCHO (2001d) illustrate some of this complexity. The average annual expenditure of the 630 local public health agencies reporting was $4.5 million (1999 dollars), but 50 percent of these agencies had expenditures of $621,000 or less. By contrast, 25 percent of the agencies serving large populations of 500,000 or more had annual expenditures of more than $46 million. On average, local public health agencies reported receiving 44 percent of their funding from local government, 30 percent from state government (including funds passed through federal programs), 19 percent from reimbursements for services, 3 percent from the federal government, and 4 percent from other sources.
ASTHO, NACCHO, the National Association of Local Boards of Health (NALBOH), and PHF, in various collaborative efforts supported by DHHS, have been exploring ways to measure actual expenditures at the state and local levels for each of the 10 essential public health services (Barry et al., 1998; Public Health Foundation, 2000). Feasibility studies show promise, but no systematic accounting of this sort is being done on a regular basis.
Almost no data are available on how much would be needed to adequately build and sustain the necessary public health infrastructure to support the nationwide provision of the essential public health services at the local level. One jurisdiction—Bergen County, New Jersey—conducted a detailed analysis of the funding needed for the public health infrastructure to be able to meet new state public health practice standards. Its estimate of $5.1 million per year translates into about $6.61 per capita and represents the county's best current judgment of the total, ongoing investment in infrastructure required to support the provision of the 10 essential public health services throughout the county (National Partnership for Social Enterprise, 2002). Various IOM reports (IOM, 1988, 1992, 1997a, 1997b, 2000a) have made a case for sustained action, both domestically and internationally, to strengthen the public health infrastructure. A detailed examination of infrastructure needs specifically in support of the nation's immunization system produced a recommendation for annual federal funding of $200 million for the next 5 years, along with an overall increase in funding from state governments of $100 million (IOM, 2000b). That report also emphasized the importance of stability in infrastructure funding, documenting the adverse impact at the state and local levels of rapid increases followed by rapid decreases in federal funding during the 1990s.
As policy makers and the public health community contemplate substantial increases in funding to improve the ability of the public health system to respond to threats of bioterrorism, the committee urges them to consider the lessons that the experience of the immunization program offers. Congress responded to the national measles outbreak in 1989–1991, in part, by increasing funding for state immunization infrastructure grants from $37 million in 1990 to $261 million in 1995, but the appropriations were reduced by about $80 million in 1996 and had fallen to $111 million by 1999. A variety of barriers (e.g., the requirements of state budget cycles and the administrative constraints of a 1-year grant period) had made it difficult for states to absorb the initial influx of grant funds, but funding was cut just as states had begun to build program capacity (IOM, 2000b). Moreover, the influx of federal funding had led state legislatures to cut state funding for infrastructure activities (Freed et al., 2000). Both stable and sustained funding is needed for the effective performance of the public health infrastructure.
On the basis of available data, the committee was unable to conclude what level of federal funding may be warranted as an ongoing, governmental investment in the development and maintenance of the public health infrastructure to ensure that it can provide the essential public health services to all Americans. It is expected that funding for the Public Health Improvement Act of 2000 will enhance the public health infrastructure, but it is unclear to what extent these additional investments would further improve the ability of the public health infrastructure to meet its broad day-to-day responsibilities for protecting and improving the health of the population. A commitment for sustained public health infrastructure financing (unrelated to bioterrorism-related activities) is clearly needed.
Prior efforts at systematic nationwide studies of financing for public health have failed because of their exclusive focus on the budgets of state and local governmental public health agencies rather than the funding of the public health system, thus preventing appropriate benchmarking for communities that have various approaches to the allocation of roles and responsibilities within the system. For example, in the late 1960s, Congress became increasingly aware of the need for accountability pertaining to state expenditures and performance as the amount of funding allocated to state health departments was increasing under Section 314(d) of the Public Health Service Act. As a result, the PHS agencies allocated funds to create the National Public Health Program Reporting System (NPHPRS). Started in 1970 and operated by the Public Health Foundation, all states routinely participated in this voluntary reporting system. Data were collected and verified for items such as federal and nonfederal expenditures by program areas, the organizational structures of health departments, and revenue amounts and sources. This was the only data source of this type in the nation. While discussions were occurring around health care reform in the early 1990s, PHF worked with state and local public health agencies to improve NPHPRS, using the Healthy People 2000 objectives as the basis for performance measures and the 10 essential services as the framework for collecting expenditure data. In 1995, PHS discontinued funding because NPHPRS could not provide program management data for federal agencies. Nearly a decade later, no reporting system exists and no data on state public health expenditures and programs are available. Although different methods of categorizing and cataloging expenditures have been studied, the research indicates that use of the 10 essential public health services for collection of expenditure data is feasible, reliable, and beneficial to the public health community. In addition, the National Public Health Performance Standards Program's Local Public Health System Performance Assessment Instrument appears to be effective in assessing the capabilities of local public health agencies to provide essential public health services.
There is still a great need for an expenditure reporting system for public health agencies based on the framework of the essential public health services and consistent with the newly implemented National Public Health Performance Standards Program to produce a needs assessment and expenditures data as a basis for estimating the investments needed. To begin this process, the committee recommends that DHHS be accountable for assessing the state of the nation's governmental public health infrastructure and its capacity to provide the essential public health services to every community and for reporting that assessment annually to Congress and the nation. The assessment should include a thorough evaluation of federal, state, and local funding for the nation's governmental public health infrastructure and should be conducted in collaboration with state and local officials. The assessment should identify strengths and gaps and serve as the basis for plans to develop a funding and technical assistance plan to assure sustainability. The public availability of these reports will enable state and local public health agencies to use them for continual self-assessment and evaluation.
Organizational Impact of Federal Grant Funding
The ways in which funds are transmitted have an impact on program effectiveness. At present, most discretionary funding distributed by DHHS to states and some local entities is allocated through block grants, formula grants, and categorical programs. According to the White House's Blueprint for New Beginnings accompanying the FY 2002 budget, DHHS manages hundreds of discrete public health activities. For these activities, states receive about $4 billion in formula grants and about $3 billion through block grants. The Blueprint for New Beginnings (White House, 2001) notes that potential reform of formula and block grant programs is a priority of the administration. The administration is considering increasing state flexibility to address public health needs through expanded transfer authorities and other mechanisms to remove barriers to effective targeting of public health resources at the state and local levels. The Blueprint does not address the need to increase the flexibility of categorical grants.
Formula grants are characterized by the allocation of funds to states in accordance with a distribution formula prescribed by law or administrative regulation. Two examples of formula grants can be found under Title I and Title II of the Ryan White CARE Act. Formula-driven grants have been difficult to modify on the basis of new variables influencing a particular issue or changes in the demographics of affected populations. The political process often prevents formula revisions that would negatively affect significant numbers of states, even if the expressed purposes of funding would be better realized by shifts to more needy populations or to other geographic areas.
Block grant programs are a subset of formula allocation programs in which the recipient has broad discretion in the application of funds received in support of broad program areas (e.g., Prevention and Treatment of Substance Abuse and Preventive Health and Health Services Block Grants). Block grant programs have various reporting requirements.
One of the questions that has been long asked is about the effectiveness of the block grant mechanism in targeting funding to a particular purpose or need. Michael Rich (1993) conducted highly regarded studies of this issue, in the area of funding for the poor. After significant empirical analysis of the distribution of Community Development Block Grants, he drew several broad conclusions about this funding vehicle:
- State and local officials play an important role in determining the degree to which federal grants are used to balance income and resources in resource-poor areas.
- The capacity and will of governments to target federal grant funds to the poor vary widely. Government officials tend to spread benefits widely as opposed to concentrating them where the need is the greatest.
- Strong coalitions are more effective in influencing federal program decisions, including targeting areas of greatest need. However, local coalitions need a strong federal partner to make explicit targeting more acceptable locally.
A literature review of different models for federal funding conducted by the DHHS Office of the Inspector General in 1994 noted that states report that block grants increased administrative efficiency and integration and did not replace state funds.
Categorical grants provide states and other recipients with funding for specific programs. CDC provides a significant amount of funding to state government departments of health through categorical grants (e.g., for HIV/ AIDS prevention, sexually transmitted disease control, tuberculosis control, and chronic disease). They are highly restrictive in terms of how the recipients may use the funding, may add administrative costs and complexities, and may worsen fragmented program management and service delivery, as federal prohibitions against mixing funds create programmatic “stove-pipes.” The result can be separation and gaps in services, because even related program areas become insulated and isolated from each other and lack the flexibility to respond to changes at the recipient level. Furthermore, measuring their real effectiveness has been difficult at times because of the large number of individual grants and the lack of resources for effective performance monitoring (Boufford and Lee, 2001).
The DHHS Performance Partnership initiative and the Oregon Option are examples of efforts to use a more performance-oriented approach to categorical funding by integrating multiple categorical programs under larger umbrella categories. Under the Performance Partnership initiative, DHHS and its partners worked together to reach consensus on the results to be achieved by the program and develop performance measures to monitor progress toward the stated results. The Oregon Option tested the proposition that multiple levels of government can align their efforts to achieve results that matter to people. Both initiatives involved signing memoranda of understanding (MOU) that committed them to work cooperatively to both determine the results to be achieved and to get the job done. The question of creating linkages of funding to benefit coalitions demands another role for governments in partnering with key local stakeholders.
This situation should be remedied. Expanded transfer authorities and other mechanisms to remove barriers and facilitate, rather than hinder, the alignment of resources and policy for the actualization of national health objectives should be considered. Thus, the committee recommends that the federal government and states renew efforts to experiment with clustering or consolidation of categorical grants for the purpose of increasing local flexibility to address priority health concerns and enhance the efficient use of limited resources.
Financial Implications of a Changing Mission for Governmental Public Health Agencies in Providing Health Care Services
Essential public health service number 7 (see Box 3–1 ) charges state and local governmental public health agencies to “link people to needed personal health services and assure the provision of health care when otherwise unavailable” (Public Health Functions Steering Committee, 1994). Thus, state and local governmental public health agencies are responsible for providing a safety net to guarantee that personal health care services are available to all members of the communities they serve. As noted earlier, since 1988, state and local governments have turned increasingly to the private sector, particularly managed care organizations, to provide health care services for Medicaid beneficiaries and others, many of whom were once served directly by local public health departments. In addition, an increasing number of employees (approximately 85 percent) (Kuttner, 1999) are covered by private health insurance, reducing their need for services from public health departments. These changes seemed to provide great promise that local public health agencies would be able to shift their focus from the provision of personal health care services to previously neglected population-based public health functions (IOM, 1996). In some states and communities, however, services to Medicaid patients had offered an important revenue stream that subsidized the population health programs of governmental public health agencies (Keane et al., 2001).
Thus, these agencies find themselves in a difficult relationship with managed care plans: on the one hand, encouraging their active partnership in the public health system, while, on the other, competing with them for revenues for some of these services (Lumpkin et al., 1998). A study of state public health agencies found that 16 of 47 states had some kind of collaboration between their public health departments and managed care groups (DHHS, 1999). In most cases, the managed care organizations were contracted to provide direct patient care (e.g., primary care and clinical preventive services). Other studies of this collaboration reported similar findings.
Although there is great potential benefit from collaborations between public health agencies and managed care plans, current economic trends for managed care programs are not optimistic. In 1997, 67 percent of managed care plans sponsored by safety-net providers lost money, and only 8 percent indicated that they broke even (Gray and Rowe, 2000). In recent years, managed care organizations have been withdrawing from collaborative contracts with governmental public health agencies, once again leaving these agencies with the pressure of having to deliver personal health care services including primary care services to the uninsured or vulnerable populations rejected by the medical care system. This instability in service delivery is also contributing to the disruption of individuals' continuity and availability of care (IOM, 2000a).
Of potential assistance to safety-net providers is the reemerging interest in federal support for “a doubling” of community health centers, operated either by traditional governmental public health agencies or by nongovernmental organizations. Congress recently awarded DHHS with funding to add 1,200 new and expanded health center sites over a 5-year period. At the end of 2002, DHHS will have invested $165 million in 260 new and expanded health centers capable of serving an additional 1.25 million people (HRSA, 2002). As these centers redevelop, the lessons of the past must be kept in mind. The allocation of federal and state resources to communities for these facilities and other health-related programs should be coordinated in a process that ensures the involvement and approval (or at least acknowledgment) of local public health agencies. Moreover, coordination with state and local public health authorities and other community resources is essential (IOM, 1988).
The committee finds that, as in 1988, the continued lack of a nationwide strategy to ensure adequate financing of personal medical, preventive, and health promotion services will continue to place undue burdens on the public health system and to fragment the provision of personal health care services to those most in need of comprehensive integrated approaches. Also, if the number of uninsured continues to increase, the diversion of resources urgently needed for population health efforts to the health care assurance component of the governmental public health system may be required.
The recent downturn in in-state revenues due to the national economic slump will exacerbate problems of sustaining the state share of Medicaid funding and lessen the likelihood of increased or, perhaps, even sustained state funding for the governmental public health infrastructure.
Improving the Operation and Management of the Governmental Public Health Infrastructure
Successfully implementing health policy based on multiple determinants of health and their impact on the health of communities and populations will depend on the effective performance of public health agencies at all levels of government. The committee has discussed the need to strengthen specific aspects of the governmental public health infrastructure at the federal, state, and local levels—the competency of the workforce, the integration and enhancement of information and communication networks, and the improvement of the laboratory and organizational capacities to ensure that the essential public health functions are available to all Americans. Another important priority is to improve the management and coordination of the work of public health agencies as they support this goal of protecting and improving the health of the population.
Public Health Performance Standards and the Accreditation of State and Local Health Departments
Performance measurement has become an essential tool for guiding quality improvement efforts and for holding organizations in the public and private sectors accountable for meeting specified responsibilities. The National Public Health Performance Standards Program (NPHPSP), initiated in 1998, is an effort to use the ideas of performance measurement to promote the organization of state and local public health practice around delivery of the essential public health services (see Box 3–4 ).
BOX 3–4
The National Public Health Performance Standards Program. Started in 1998, the National Public Health Performance Standards Program (NPHPSP) is a collaborative effort between the Centers for Disease Control and Prevention (CDC) and a variety of national (more...)
In a national partnership, CDC, ASTHO, NACCHO, NALBOH, APHA, and PHF are working together to establish measurable performance standards for state and local public health systems, to develop tools to assess performance against these standards, and to create incentives for states and localities to use such tools. Some of these measures could be used in a “report card” or as standards in a national program that accredits public health agencies.
The performance standards effort is seen as one way to help move the state and local components of the nation's public health system closer to the system envisioned in The Future of Public Health (IOM, 1988). Separate sets of tools for governance have been developed and tested. The instruments are available via CDC's NPHPSP website ( www.phppo.cdc.gov/nphpsp ), the ASTHO website for the state instrument ( www.astho.org/phiip/performance.ht-ml ) (ASTHO, 2001d), the NACCHO website for the local instrument ( www.naccho.org/project48.cfm ) (NACCHO, 2001f), and the NALBOH website for the governance instrument ( www.nalboh.org/perfstds/perfstds.htm ) (NALBOH, 2001). Although the program is aimed at assessing the performance of the public health system as a whole, it recognizes that governmental public health agencies have key responsibilities for leading, coordinating, and supporting the efforts of various contributors.
The interest in measuring the performance of the public health system extends to the possibility of establishing a formal process of accreditation to certify that governmental public health agencies are meeting specified levels of performance. Several states have developed or are developing state-specific performance requirements for local governmental public health agencies, but interest has also emerged in the development of nationally standardized, systematic performance evaluations for state and local public health agencies.
No agreement has been reached on the appropriate criteria or process for accreditation. One of the key challenges is to create a system that is flexible enough to accommodate the wide variety of public health department structures and circumstances across states. Given the resource constraints that state and local governmental public health agencies currently face, it is unclear how performance standards can be met or accreditation can be achieved when the resources to provide even the most basic services are often lacking. Linking federal funding to accreditation based on public health performance standards has been proposed, but there may not be adequate incentives for states and localities that do not receive significant portions of their overall funding from federal agencies. The promise of a long-term federal investment at the state and local levels linked to such a system could change the situation considerably.
To address these and other concerns, NACCHO has convened the Voluntary Accreditation Committee, which consists of eight local health officers who are charged with maintaining an ongoing discussion of the advantages and disadvantages of voluntary accreditation of local health departments. They are currently researching lessons that might be learned from other voluntary accreditation efforts, such as those for hospitals, managed care organizations, and law enforcement agencies. The Voluntary Accreditation Committee is also taking into account the work of states such as Florida, Illinois, Michigan, Missouri, Ohio, and Washington that are already active in the development of state-specific accreditation or performance standards for their local public health agencies.
Despite the controversies concerning accreditation, the committee believes that greater accountability is needed on the part of state and local public health agencies with regard to the performance of the core public health functions of assessment, assurance, and policy development and the essential public health services. Furthermore, the committee believes that development of a uniform set of national standards leading to public health agency accreditation could provide such a mechanism, but only if adherence to such standards is linked to a commitment of sustained federal investment in the state and local public health infrastructure to assure that resources are available. Moreover, such a mechanism could serve to increase levels of accountability among state and local elected officials in whose jurisdictions these agencies operate. The breakthrough concepts of NPHPSP provide a way to conceptualize the system as the unit of accreditation and, from there, to evaluate the role of the agencies in facilitating the work of the system.
Accreditation is a useful tool for improving the quality of services provided to the public by setting standards and evaluating performance against those standards. Accreditation mechanisms have helped to ensure the robustness of the health care delivery system (hospitals, clinics, programs) and medical and other educational programs. Accreditation processes also provide information to the public about the quality of the services they receive (e.g., National Committee for Quality Assurance report cards on health plans) (IOM, 2001). Governmental public health agencies currently have no such framework, and the communities they serve have little information on the quality of the services they receive. An accreditation process could provide a structure for establishing quality assurance and improvements in governmental public health agencies. Therefore, the committee recommends that the Secretary of DHHS appoint a national commission to consider if an accreditation system would be useful for improving and building state and local public health agency capacities. If such a system is deemed useful, the commission should make recommendations on how it would be governed and develop mechanisms (e.g., incentives) to gain state and local government participation in the accreditation effort. Membership on this commission should include representatives from CDC, ASTHO, NACCHO, and nongovernmental organizations.
This commission should focus on the development of a system that will further the efforts of NPHPSP. The work of this commission should be closely linked to that of the commission whose creation the committee has recommended to examine issues related to the credentialing of public health workers, because it is conceivable that these mechanisms could be linked. In both efforts, the relationship of the official public health agency to its role in the larger public health system will be key to accreditation.
Special Concerns About the Capacity to Meet Local Public Health Needs
In The Future of Public Health (1988), the IOM committee concluded that “no community, no matter how small or remote, should be without identifiable and realistic access to the benefits of public health protection, which is possible only through a local component of the public health delivery system” (IOM, 1988: 144). The rationale behind this finding is clear: If a community is going to be able to meet its own health needs, it must have access to an identifiable public health infrastructure to provide the essential public health services. Today, concerns remain about the availability of an adequate local public health infrastructure, particularly in terms of staffing and communications systems, to provide these services.
Despite the presence of some 3,000 local public health agencies throughout the country, these agencies are not equally distributed across states or across rural and urban areas. For example, Bergen County, New Jersey, with a population of approximately 884,000 and an area of 234 square miles (Census Bureau, 2001a), is served by a strong county health department, 55 local boards of health, and 22 independent public health agencies that serve different and occasionally overlapping communities (T. Milne, NACCHO, personal communication, October 31, 2001). By contrast, the state of Maine, with a population of about 1.3 million distributed over 30,862 square miles (Census Bureau, 2001b), has two local public health agencies (T. Milne, NACCHO, personal communication, October 31, 2001). Challenges come from both an abundance of local public health agencies and their scarcity. When multiple public health departments serve the same geographic area, they may experience difficulties coordinating activities and aligning priorities. However, rural areas, with little or no local public health presence, may suffer from inadequate public health capacity or resources to address local needs and a paucity of educational and training support (Johnson and Morris, 2000).
Either we are all protected or we are all at risk.
Dr. Jeffrey Koplan,
Formerly, Centers for Disease Control and Prevention
Data from NACCHO (2001e) also point to substantial differences in the workforce available to local public health agencies. NACCHO's 1999– 2000 survey found that 50 percent of all local public health agencies responding had 17 or fewer full-time employees or contract staff, but for those serving metropolitan areas, 50 percent had at least 28 full-time employees or contract staff. Some local public health agencies, however, currently have only one half-time employee as their entire public health agency staff. Staffing levels have shown little change over the past decade. A 1997 survey found that the median number of full-time employees was 16 (NACCHO, 1998), and in 1992–1993, NACCHO (2001e) reported that 42 percent of local public health agencies had less than 10 full-time staff members. Given the many responsibilities and wide-ranging duties inherent in the assurance of population health, the committee is concerned that these low numbers do not bode well for the core capacity of some local public health agencies to provide the 10 essential public health services to their communities.
Simply increasing the size of the local public health agency workforce appears problematic, however. The committee is concerned about reports by 68 percent of local public health agencies that budget restrictions prevent them from hiring needed staff, including public health nurses, environmental specialists, health educators, epidemiologists, and administrative personnel (NACCHO, 2001d). In addition, local public health agencies in smaller, nonmetropolitan jurisdictions indicated that they could not hire the necessary staff because of a lack of qualified candidates in their areas and difficulty attracting other candidates to their locations. Only 19 percent of the local public health agencies indicated that they needed new staff because of projected expansions of their programs and services (NACCHO, 2001d).
Many local public health departments also lack even the most basic tools necessary for rapid communication and access to information (GAO, 1999b). For example, a 1999 survey of 1,200 local public health departments found that 19 percent did not have the capacity to send and receive e-mail via the Internet (Fraser, 1999). The most common barriers cited by the departments without Internet access were prohibitive costs (64 percent), the need for hardware (64 percent), and the need for staff training (63 percent). Additionally, only 48 percent of the health departments surveyed indicated that the director had continuous, high-speed Internet access at work, and only 44 percent indicated that the department had broadcast fax capabilities (Fraser, 1999). In all cases, public health agencies in smaller and more remote jurisdictions had the least access to information and communications technologies, even though these agencies may actually have the greatest need for such technologies.
Given the evidence concerning the local public health workforce and communication capacity as well as related observations made throughout this chapter, the committee finds that too little has been done to support and strengthen the local public health infrastructure. Over the past 14 years, governmental public health agencies have made great efforts in response to the recommendations concerning local public health agencies in The Future of Public Health (1988) (see Appendix C ). Unfortunately, until recently, progress has been slow because of the lack of political and financial support that was needed long ago to fully realize the vision of the 1988 report. Recent increases in infrastructure support in connection with bioterrorism preparedness are somewhat encouraging, but there is concern that such efforts may reinforce the complex problems created by prior categorical funding if excellent specific services (e.g., surveillance are informatics) are built on the foundation of a crumbling infrastructure. For these reasons, the committee believes that every community, no matter how small or remote, should have identifiable and realistic access to the essential public health services, and that it is the responsibility of the states to ensure that such services are available. However, for states to meet this obligation, the committee recommends that DHHS develop a comprehensive investment plan for a strong governmental national public health infrastructure with a timetable, clear performance measures, and regular progress reports to the public. State and local governments should also provide adequate, consistent, and sustainable funding for the governmental public health infrastructure. This investment is crucial to assure the preparedness of public health departments and the protection of communities, regardless of their size or location.
Some communities provided comments to the committee noting that a more precise description of an essential minimum level of local official agency capacity would aid their efforts to obtain public health services. In an effort to be responsive to these requests, the committee struggled with the challenge to be more explicit with regard to the level of public health capacity that should be present in these small and remote communities. Not surprisingly, some familiar problems were encountered. For example, there are questions involving the proper definition of a “community” for this purpose and the appropriate response if a community has too small an economic base to sustain a formal public health agency with the necessary presence and capacity to provide public health protections.
The most robust approach to assessing need seems to be the use of a functional analysis based on the ability to provide the essential public health services, as recommended above. The committee recognizes the potential value of a recommendation regarding the development of a formula to determine the “critical mass” of services and population (e.g., a ratio of one of each of the critical professions per 50,000 or 100,000 population), the geographic accessibility of services, and the workforce capacity necessary for the effective development of local public health agencies to serve small or remote communities. Before such a recommendation can be made, however, solid, practice-oriented research must be conducted to provide the evidence on which to base a formula or other criteria.
The committee had hoped to be able to provide specific guidance to assist the nation in its efforts to rebuild and finance its public health infrastructure. However, a comprehensive search of the published literature and extensive information gathering yielded very little firm, generalizable evidence on which to structure public health practice recommendations like those noted. To remedy this situation, the committee recommends that CDC, in collaboration with the Council on Linkages between Academia and Public Health Practice and other public health system partners, develop a research agenda and estimate the funding needed to build the evidence base that will guide policy making for public health practice.
Strengthening the Management Capacity of DHHS
From 1993 to 1997, DHHS, like all federal government departments, conducted a reinvention exercise to determine what work it should do and how it could do that work more effectively and responsively. A recent monograph on DHHS and the impact of departmental reinvention efforts in the late 1990s identified two issues of particular significance: (1) the effect of the balance between centralization and decentralization on the management of departmental activities and (2) the relationship of the department with other agencies (Boufford and Lee, 2001).
Centralization versus Decentralization: Models for Managing DHHS
The committee's discussion of key federal functions—policy making, financing, infrastructure development, and the like—illustrate how the problems of fragmentation in federal public health activities affect the functioning of state and local public agencies. Such problems are related to historical patterns and political interests that have shaped federal health structures, but they are not being addressed by the present management structure for health activities in DHHS. The reinvention exercise led to a decision to have each of the PHS agencies report directly to the Secretary of DHHS rather than to the Assistant Secretary for Health. Potential advantages were seen in bringing the agency heads closer to the Secretary and having more than a single voice for health at the decision-making table. Boufford and Lee (2001) found that without a formal mechanism for joint priority setting and routine decision-making across the department, operations became even more decentralized, with staff identifying more with their own agencies or programs than with the department as a whole. The leadership of operating divisions generally prefers to report directly to the Secretary, but division leaders would also welcome a clearly defined structure to formalize coordination, collaboration, and communication among departmental units. Creating a formal mechanism for regular meetings of the heads of operating divisions, as well as meetings with the Secretary, would permit more substantive and forward-looking discussion of priorities and policies and would address the operational challenges of coordination and communication within the department. Such a forum could also provide better oversight and interaction with cross-departmental groups created to address issues identified by the Secretary, such as the Data Council, the Children's Council, and the Environmental Health Policy Committee. A defined charter, staff, and timetable for selected cross-cutting activities would strengthen collaboration across units and produce specific recommendations for action.
Recent decisions by DHHS leadership to recentralize public and legislative affairs functions do not address the fundamental issue of policy and program coordination. There is also tension within DHHS about the role of the regional offices (Boufford and Lee, 2001). Advocates for strong regional offices see them as effective vehicles for communicating DHHS priorities, learning about local needs and circumstances, and developing appropriate responses through the department or by other means. The regional offices are also seen as aids in convening state leadership in health and human services in those regions and in convening local leaders to help them find ways to increase their access to federal programs or to collaborate with others in the public and private sectors to make DHHS programs effective. Although others prefer that DHHS agencies work directly with state and local governments and grantees, such agency-by-agency linkages can add to the fragmentation of efforts to address population health.
If regional offices are to become an integral and valuable part of DHHS, they will require managerial attention and resources for significant staff development or redeployment to obtain the expertise needed in certain program areas (Boufford and Lee, 2001).
Interagency Collaboration
Interagency collaboration at the federal level can be difficult because of the specialized nature of agency structures. Every agency has its traditional role and expectations for performance, its legislative champions, and its special-interest advocates. According to Bardach (1998), barriers to collaboration across agency lines are the fact that collaboration tends to blur an agency's mission and the fact that the agency is politically accountable for pursuing that mission. This historical reality has led to the increasing isolation of cabinet departments and the agencies within those departments from each other and has created real barriers to the programs within agencies that seek to collaborate. This is understandable historically but is clearly dysfunctional in an increasingly complex world where no single agency can do its important work in isolation.
This lack of integration is especially evident in the area of health, where health-related programs are already fragmented within DHHS and are widely distributed across cabinet and subcabinet departments outside DHHS. For example, when EPA became an independent agency, it assumed the regulatory functions of environmental protection, yet the key expertise in the human health effects of environmental hazards remains at DHHS in the National Center for Environmental Health at CDC, ATSDR, the National Institute of Environmental Health Sciences at NIH, and some parts of FDA.
Many agencies not traditionally associated with health issues make policy and manage programs with potential implications for health (see Chapter 2 ). Greater policy coordination with the Departments of Education, Energy, Treasury, and Labor, to name a few, could enhance the potential to create the societal conditions needed for people to be as healthy as possible. Another area for greater collaboration and coordination is with nongovernmental entities. This can be particularly challenging in the area of health care delivery because of the government's role as regulator and payer. The same holds true at the state level.
The need for effective coordinating structures is very important because most experienced government officials agree that major organizational restructuring is rarely worth the time and political trouble involved (even if it could be achieved), so although it may seem advisable to reunite DHHS and EPA or create a food safety agency independent from portions of FDA, the Department of Agriculture, and EPA, the obstacles are formidable. Bardach (1998) found, however, that various administrative mechanisms could enhance the effectiveness of cross-agency collaboration. These may include formal agreements at the executive level; assignment of personnel, budget, equipment, and space to a collaborative task; delegation and accountability for the relationships relating to the task; and the provision of administrative services to support the work. The success of efforts such as the Presidential Task Force on Food Safety, the Task Force on Environmental Health Risks and Safety Risks to Children, and the multiagency task force on bioterrorism demonstrate the benefits of cross-agency collaboration.
The committee particularly noted that the lack of coordination between DHHS and other agencies with health-related responsibilities often creates major obstacles to the effective use of federal regulatory and standard-setting powers in health. Inconsistencies between DHHS agencies and other science-based regulatory agencies—for example, between DHHS and EPA—lead to standards on the levels of particular chemicals or toxins hazardous to the health of humans that are different from the levels hazardous to the health of animals and vegetation (Boufford and Lee, 2001). These issues are usually addressed on a case-by-case basis through work groups or crisis management activities. During the Reagan administration, for example, cabinet councils chaired by a designated secretary were used to coordinate efforts across departments. They worked when they were well staffed and participation at the deputy or assistant secretary level was consistent, with secretaries available as needed (Edward Brandt, personal communication, 2001).
A final challenge is the integration of federal standard setting and regulation with the equally varied jurisdictions of state and local health departments or other health-related agencies. Again, creative and sustained mechanisms to develop collaborative relationships and to harmonize regulations within DHHS, across federal agencies, and among federal, state, and local governments are critical to effective action for protecting the population's health.
In June 2001, the Secretary of DHHS established the Advisory Committee on Regulatory Reform. The committee is charged with conducting a department-wide initiative to reduce regulatory burdens in health care and to respond faster to the concerns of health care providers, state and local governments, and individual Americans who are affected by DHHS rules. The Advisory Committee conducted six data-gathering meetings across the country. The committee was expected to present a final report and recommendations in the fall of 2002 for changes in four areas: health care delivery, health systems operations, biomedical and health research, and the development of pharmaceuticals and other products. A review of the report shows that much attention was directed to implementing changes in the health care delivery component of the public health system, with little attention paid to the regulatory inconsistencies, burdens, and inefficiencies in the governmental public health component of the system.
Given these organizational and management findings, the committee recommends that the Secretary of DHHS review the regulatory authorities of DHHS agencies with health-related responsibilities to reduce overlap and inconsistencies, ensure that the department's management structure is best suited to coordinate the efforts among agencies within DHHS with health-related responsibilities, and, to the extent possible, simplify relationships with state and local governmental public health agencies. Similar efforts should be made to improve coordination with other federal cabinet agencies performing important public health services, such as the Department of Agriculture and the Environmental Protection Agency.
The committee also notes that the division of authority in the federal government hinders the development of a coherent international health policy. With increasing cross-border flows of people, pharmaceuticals, and food, countries cannot adequately protect their populations through unilateral domestic or foreign policy action; they must collaborate with other countries and within the frameworks of international agreements. This is especially true in matters of health and environment. The World Health Organization (WHO) is a forum for standard setting on issues such as international travel health standards, the quality of pharmaceuticals, and food quality and safety. A lack of funding for research on diseases that disproportionately affect the developing world (the “10/90” gap) (Davey, 2000), the weakness of the research infrastructure in these countries, and the need to address matters of intellectual property involved in making basic drugs available to nations without their own production capacities are only a few of the issues that can benefit from high levels of involvement from developed countries such as the United States, with its wealth and scientific expertise.
At present, the Department of State is the lead U.S. agency on international affairs and pays dues to international agencies like WHO. Because of the importance of health and science to its work, it has recently appointed a deputy assistant secretary for health and science. The funding for U.S. development assistance in health comes through congressional funding to the U.S. Agency for International Development, which funds much of its international health work by contract with DHHS, largely CDC. DHHS has only limited authority from Congress to spend money on international health activities. Coordination across all these agencies is critical to assuring a coordinated strategy for international health. During the Clinton administration, a senior public health officer served on the National Security Council (NSC) as health liaison to the various agencies. In a consultation conducted by IOM, among representatives from the major departments that address international health issues (and others involved in international health policy, from EPA to the Departments of Agriculture and Commerce), all agreed that there was a problem in coordination and clear leadership on international health that prevented effective long-term planning. They agreed that NSC leadership could provide a focal point for such coordination, absent an executive decision to appoint a lead agency (IOM, 1999). The NSC health liaison position was phased out during the early days of the Bush administration.
In America's Vital Interest in Global Health, IOM (1997a) called for better coordination of global health policy within the U.S. government through the use of a Task Force on Global Health. That report also recommended legislative changes to expand international authorities and funding to DHHS “because of its unique scientific and technical expertise” to lead such an effort across the government and to serve as a focal point for links to nongovernmental organizations and academia. This committee concurs with the need for an effective mechanism for coordination of international health policy making and urges the administration and Congress to consider steps to this end such as the appointment of a permanent NSC liaison for international health, the designation of a lead agency for international health or the formation of a formal cross-cabinet body, and the review of Public Health Service Act authorities for DHHS funding of international health initiatives.
Federalism and a National Public Health Policy
The relationships among various levels of government have always been complex and hotly contested. In most spheres of public health (e.g., injury prevention, clean air and water, and infectious disease surveillance and control), federal, state, and local governments all have a presence. As in all essential government endeavors, good communication and cooperation among the various levels of government are vital. Federalism functions as a sorting device for determining which government, federal or state, may legitimately respond to a public health threat. Often, the national and state governments exercise public health powers concurrently, but the Supremacy Clause gives Congress the authority to preempt state public health regulation, even if the state is acting squarely within its police powers ( Gade v. National Solid Waste Management Association , 505 U.S. 88, 98 [1992]). Federal preemption occurs in many areas of public health regulation, including labeling and advertising of cigarettes, self-insured health care plans, and occupational health and safety.
Although there may be debates over the constitutional roles of the federal and state governments, a more fundamental concern is that each level of government operates effectively in assuring the conditions for the public's health. First, strong public health leadership is essential. This means that where the various levels of government are operating at the same time, clear understanding of who is in charge and who has responsibility for which tasks must exist. During the anthrax outbreak, for example, it was often unclear which level of authority was in charge: the Secretary of DHHS, the local public health commissioners in Florida, New York, and Washington, D.C., or the Department of Justice (FBI). Second, no significant gaps in public health protection should exist. This means that at least one level of government should be actively involved in dealing with important health problems.
Because the major interactions of the federal and state governments in recent years have related to issues of health care financing through the Medicaid program (or through welfare programs), they have tended to focus on arguments over money and degrees of freedom to spend it. States have often been reduced to being just another interest group. If a mechanism could be developed to engage the states as potential partners in a larger national strategy such as the health agenda that clearly depends on collaborative action for success, it could change these relationships.
Direct relationships between the federal government and local governments constitute a complicated issue. In the American system, local governments are the creatures of state governments, from which they get their authority and resources (or the authority to raise revenues). There are more than 90,000 units of local government in the United States; 90 percent have populations of less than 10,000 and 80 percent have populations of less than 5,000 (Cigler, 1998). Their policy-making and managerial capacities are highly variable, as are their capacities and resources in health. It is clear that some units of local government look to the federal government to correct the inequities that they experience at the hands of state governments; others are in tense relations with their state counterparts, and direct federal connections may exacerbate tensions. Ways to manage relationships that engage local governments but that respect the rights of the state governments in terms of their relationships to local governments must be considered in any long-term partnership-building process.
The committee believes that a more comprehensive and coordinated approach to health policy is necessary to improve the alignment of federal, state, and local governmental authorities and financial resources to support effective action in improving population health. This kind of coordination is critical to creating a true public health system from the multiple, often disconnected, and somewhat competitive organizations that must work together to promote and protect the health of the public. As one step toward better coordination, DHHS should be looking to new ways to collaborate more effectively with governmental public health agencies at the state and local levels.
This is not a new problem for DHHS. In 1960, then Surgeon General Leroy Edgar Burney convened an external expert group to “study the present and future mission of the public health service and design the best possible structure to deal with its multiple new functions.” It found that PHS needed to develop mechanisms to allow it to work “with, rather than through state agencies” (Study Group on the Mission and Organization of the Public Health Service, 1960). During the Nixon administration, there was similar recognition of the importance of improving relationships between federal, state, and community organizations to serve the populations in greatest need. This led to strengthening of the regional offices of DHHS and establishing an office on intergovernmental affairs. As discussed earlier, the department's policy and structures for dealing with state and local governments have varied over the years, but the mechanisms within the department are weak at present.
One way to achieve better communication is through formal links with the national organizations representing state and local health officials, ASTHO and NACCHO, which often collaborate with the department in activities such as the Healthy People (2010) initiative and the development of National Public Health Performance Standards. The department could also enhance its efforts to seek state and local perspectives on public health policy through the National Governors Association and the U.S. Conference of Mayors, which have staff who work on health issues.
The committee believes that a more formal entity could facilitate the link between the Secretary of DHHS and state public health officers for the purpose of improving communication, coordination, and collaborative action on a national health agenda. In considering the form of such an effort, it is important to recognize that the U.S. health care system is highly devolved, and as noted earlier, historically, the major responsibility for the essential public health services has rested with state governments, but with that responsibility subject to federal regulations and with the public health services partially supported by federal revenues (more revenues are provided for health care delivery than for the public health infrastructure). Because governments have a unique role in assuring the conditions for health of the population and because health is a public good, the high level of interdependence of federal and state governments in achieving national health goals such as those articulated in Healthy People 2010 (DHHS, 2000) requires effective communication and collaboration.
In a 1997 report on the principles of state–federal relations, the National Governors Association, while noting the importance of state autonomy and the preservation of the ability of the states to address local circumstances, agreed that there was a need for a federal role in certain domestic issues—when issues are national in scope and the national interest is at risk and to help states meet the needs of special populations. It also reaffirmed its support for a federal role in assuring equality of access, addressing the issues beyond the capacities of individual states, and ensuring that all states have the fiscal capacity to meet the requirements of federal goals. It further cites the critical importance of close working relationships with “our federal partners” (NGA, 1997). Although this discussion did not specifically address collaboration in public health, the principles would seem to apply and call for direct interaction between the governmental public health leadership of states and the DHHS rather than through annual meetings of representative organizations or interest groups.
Therefore, the committee recommends that Congress mandate the establishment of a National Public Health Council. This National Public Health Council would bring together the Secretary of DHHS and state health commissioners at least annually to
- Provide a forum for communication and collaboration on action to achieve national health goals as articulated in Healthy People 2010 ;
- Advise the Secretary of DHHS on public health issues;
- Advise the Secretary of DHHS on financing and regulations that affect the governmental public health capacity at the state and local levels;
- Provide a forum for overseeing the development of an incentive-based federal–state-funded system to sustain a governmental public health infrastructure that can assure the availability of essential public health services to every American community and can monitor progress toward this goal (e.g., through report cards);
- Review and evaluate the domestic policies of other cabinet agencies for their impacts on national health outcomes (e.g., through health impact reports) and for their impacts on the reduction and elimination of health disparities; and
- Submit an annual report on their deliberations and recommendations to Congress.
The Council should be chaired by the Secretary of DHHS and cochaired by a state public health director on a rotating basis. An appropriately resourced secretariat should be established in the Office of the Secretary to ensure that the council has access to the information and expertise of all DHHS agencies during its deliberations.
The committee believes that public health exists within a sphere of political and policy-making activity, from which it cannot and should not be separated. Thus, public health must operate within the boundaries of democracy and must take place in a rational, evidence-based political process. Therefore, the proposed Council may change with changes in administration.
- CONCLUDING OBSERVATIONS
To most effectively protect and promote the health of the population, the nation's entire governmental public health infrastructure—its human resources, information systems, and organizational capacity—must be revitalized and strengthened. Doing so will require federal, state, and local governmental collaboration to assess the needs in each community and to identify national and local strategies to meet those needs. Furthermore, federal, state, and local governments will need to create innovative financing mechanisms that can add new resources (including those from the private sector) to those already committed by all levels of government to infrastructure development and capacity building and ensure that these investments are sustainable over time. Most importantly, it is the responsibility of the federal government to ensure that these actions at the federal, state, and local levels contribute to the creation and maintenance of a comprehensive, intersectoral public health system that serves to protect and promote the health of Americans.
- Altman LK. 2001. CDC team tackles anthrax . New York Times , October 16.
- APHL (Association of Public Health Laboratories). 2000. On the front line: protecting the nation's health . Available online at http://www .phppo.cdc .gov/dls/aphl-ofl.asp . Accessed March 12, 2002.
- APHL. 2002. a. Advancing the National Electronic Disease Surveillance System: An Essential Role for Public Health Laboratories . Report of the Association of Public Health Laboratories. Washington, DC: APHL.
- APHL. 2002. b. Who Will Run America's Public Health Labs? Educating Future Laboratory Directors . Report prepared by Schoenfeld E, Banfield-Capers SY, and Mays G for the Association of Public Health Laboratories. February. Washington, DC: APHL.
- ASCP (American Society for Clinical Pathologists). 2000. Laboratory workforce shortage stresses need for health professions funding (last updated on April 6, 2000) . Available online at http://www .ascp.org . Accessed March 18, 2002.
- ASTHO (Association of State and Territorial Health Officials). 1999. Bioterrorism preparedness: medical first response . Testimony of David R. Johnson, MD, MPH, Deputy Director for Public Health and Chief Medical Executive, Michigan Department of Community Health, on behalf of the Association of State and Territorial Health Officials, to the U.S. House of Representatives Subcommittee on National Security, Veterans Affairs, and International Relations, September 22. Available online at http://www .aphl.org/Advocacy /Testimony/index.cfm . Accessed March 12, 2002.
- ASTHO. 2001. a. HIPAA Issue Brief No. 1 , February 1. Covered entities under HIPAA. Available online at http://www .astho.org/phiip/documents .html . Accessed March 12, 2002.
- ASTHO. 2001. b. HIPAA policy brief , March 28 . Available online at http://www .astho.org/phiip/documents .html . Accessed March 12, 2002.
- ASTHO. 2001. c. Bioterrorism preparedness . Testimony submitted to the U.S. Senate Committee on Appropriations, Subcommittee on Labor, Health and Human Services, and Education , October 3. Washington, DC: ASTHO.
- ASTHO. 2001. d. Performance assessment and standards, state tool . Available online at http://www .astho.org/phiip/performance .html . Accessed March 12, 2002.
- ASTHO. 2002. 2002 salary survey of state and territorial health officials . Available online at http://www .astho.org/about/salary.html . Accessed March 12, 2002.
- Bardach, E. 1998. Getting Agencies to Work Together . Washington, DC: Brookings Institution.
- Barry MA, Centra L, Pratt E, Brown CK, Giordano L. 1998. Where do the dollars go? Measuring local public health expenditures . Submitted to the Office of Disease Prevention and Health Promotion, Department of Health and Human Services, by NACCHO, NALBOH, and PHF. Available online at www .phf.org . Accessed March 12, 2002.
- Baxter R, Rubin R, Steinberg C, Carroll C, Shapiro J, Yang A (for The Lewin Group). 2000. Assessing Core Capacity for Infectious Diseases Surveillance . Final report. Department of Health and Human Services.
- Beaulieu J, Scutchfield FD. 2002. Assessment of the validity of the National Public Health Performance Standards: the local public health performance assessment instrument . Public Health Reports 117(1):28–36. [ PMC free article : PMC1497412 ] [ PubMed : 12297679 ]
- Boufford JI, Lee P. 2001. Health Policies for the 21st Century: Challenges and Recommendations for the U.S. Department of Health and Human Services . New York: Milbank Memorial Fund.
- Brewin B. 2001. Anthrax threat exposes IT ills . Computerworld , October 22.
- Bureau of the Census. 2001. a. State and county quick facts: Bergen County, New Jersey (year 2000 data) . Available online at http://quickfacts .census .gov/qfd/states/34/34003.html . Accessed March 12, 2002.
- Bureau of the Census. 2001. b. State and county quick facts: Maine (year 2000 data) . Available online at http://quickfacts.census.gov/ qfd/states/23000.html . Accessed March 12, 2002.
- CDC (Centers for Disease Control and Prevention). 1995. Integrating public health information and surveillance systems: report and recommendations, Spring 1995 . Available online at www .cdc.gov/od/hissb/docs/katz-0.htm . Accessed March 12, 2002.
- CDC. 1997. Electronic reporting of laboratory data for public health . Report and recommendations from the March 24–25 meeting sponsored by the Council of State and Territorial Epidemiologists, Association of State and Territorial Public Health Laboratory Directors, and CDC. Available online at http://www .cdc.gov/od/hissb/act_elr.htm . Accessed March 12, 2002.
- CDC. 1998. National Public Health Performance Standards Program . Available online at http://www .phppo.cdc .gov/nphpsp/index.asp . Accessed June 2, 2002.
- CDC. 1999. Electronic reporting of laboratory information for public health . Report and recommendations from the January 7–8, 1999, meeting sponsored by the Centers for Disease Control and Prevention, Association of Public Health Laboratories, Council of State and Territorial Epidemiologists, and Association of State and Territorial Health Officials. Available online at http://www .cdc.gov/od/hissb/act_elr.htm . Accessed June 2, 2002.
- CDC. 2000. a. Biological and chemical terrorism: strategic plan for preparedness and response. Recommendations of the CDC Strategic Planning Workgroup . Morbidity and Mortality Weekly Report 49(RR–4):1–14. [ PubMed : 10803503 ]
- CDC. 2000. b. Integration project: National Electronic Disease Surveillance System . Available online at www .cdc.gov/od/hissb/act_int.htm . February 29. Accessed June 2, 2002.
- CDC. 2000. c. Supporting public health surveillance through the National Electronic Disease Surveillance System (NEDSS) . Available online at www .cdc.gov/od/hissb/docs.htm . Accessed June 3, 2002.
- CDC. 2000. d. Proceedings from the Public Health Workforce Expert Panel Workshop, Pine Mountain, GA, November 1–2 . Atlanta, GA: CDC.
- CDC. 2001. a. Bioterrorism: program in brief , January . Available online at www .cdc.gov/programs . Accessed June 2, 2002.
- CDC. 2001. b. Public health's infrastructure: a status report. Prepared for the Appropriations Committee of the U.S. Senate , March . Available online at www .phppo.cdc.gov . Accessed June 2, 2002.
- CDC. 2001. c. Innovations in public health: 2001 program review . Available online at http://www .phppo.cdc .gov/documents/ProgramReview2001.pdf . Accessed June 2, 2002.
- CDC. 2001. d. Enhanced surveillance project (ESP) . Available online at http://www.bt.cdc.gov/ episurv/esp.asp . Accessed June 2, 2002.
- CDC. 2001. e. A Global Life-Long Learning System: Building a Stronger Frontline Against Health Threats . January 5. Atlanta, GA: CDC.
- CDC. 2001. f. Genomics workforce competencies 2001 . Available online at www .cdc.gov/genetics /training/competencies/comps.htm . Accessed June 2, 2002.
- CDC. 2002. Programs in brief: chronic disease prevention . Available online at www.cdc.gov/ programs/chronic . Accessed March 19, 2003.
- CDC and Agency for Toxic Substances Disease Registry (ATSDR). 2001. A Global and National Implementation Plan for Public Health Workforce Development . Draft dated January 5. Atlanta, GA: CDC.
- Center for Civilian Biodefense Studies. 2001. Hearing on FEMA's role in managing bioterrorist attacks and the impact of public health concerns on bioterrorism preparedness . Testimony of Tara O'Toole, MD, MPH, Senior Fellow, Center for Civilian Biodefense Studies, the Johns Hopkins University Schools of Public Health and Medicine, to the U.S. Senate Government Affairs Subcommittee on International Security, Proliferation and Federal Services, July 23. Available online at http://www .hopkins-biodefense .org/pages/library/ fema.html. Accessed March 12, 2002.
- Center for Infectious Disease Research and Policy and Workgroup on Bioterrorism Preparedness. 2001. Preparing a framework for public health action and bioterrorism preparedness: recommendations for federal funding of public health activities . Available online at www .asmusa.org/pasrc/fundingforbwc.htm . Accessed March 12, 2002.
- Center for Law and the Public's Health. 2001. The Model State Emergency Health Powers Act: legislative specifications table . December 21 . Available online at: http://www. publichealthlaw.net . Accessed March 12, 2002.
- Cigler BA. 1998. Emerging trends in state and local relations . In Hanson RL, editor. (Ed.). Governing Partners: State–Local Relations in the United States . Boulder, CO: Westview Press.
- Columbia Center for Health Policy. 2001. Local public health competency for emergency response . Columbia University School of Nursing, Center for Health Policy, April 2001 . Available online at http://cpmcnet.columbia.edu/dept/nursing/institute-centers/chphsr/ ERMain.html . Accessed July 18, 2002.
- Connolly C. 2001. U.S. officials reorganize strategy on bioterrorism . Washington Post , November 8, p. A01.
- Council on Linkages between Academia and Public Health Practice. 2001. Core competencies for public health practice . Available online at http://www.trainingfinder.org/competencies/ list.htm . Accessed July 18, 2002.
- CSTE (Council of State and Territorial Epidemiologists). 2001. The CSTE Washington Report, Vol. 5 (No. 20) , October 24.
- Davey S. 2000. The 10/90 Report on Health Research 2000 . Geneva: Global Forum for Health Research.
- Davies J, Jernigan DB. 1998. Development and evaluation of electronic laboratory-based reporting for infectious diseases surveillance . Paper presented at the International Conference for Emerging Infectious Diseases, Atlanta, GA, March 8–11.
- Department of Defense. 2002. Syndromic surveillance: a new way to track emerging infectious diseases . Available online at http://www .geis.ha.osd .mil/getpage.asp?page =Syndromic-Surveillance .htm&action =7&click=KeyPrograms . Accessed March 19, 2002.
- DHHS (Department of Health and Human and Services). 1994. Federal Approaches to Funding Public Health Programs: A Literature Review . Document No. OEI-01-94-00/60, August. Washington, DC: DHHS.
- DHHS. 2000. Public health infrastructure . In Healthy People 2010 . Available online at http://www.health.gov/healthypeople/document/tableofcontents. htm#volume2 . Accessed March 19, 2002.
- Duchin JS. 2002. Syndromic surveillance for bioterrorism and naturally-occurring communicable disease outbreaks . Presentation slides. Presented at the Asia Pacific Economic Cooperation Forum Network of Networks meeting, Seattle, WA, January 28–30. Available online at www .apec.org/infectious/NoN/Duchin.pdf . Accessed March 18, 2002.
- Duffy J. 1990. The Sanitarians: A History of American Public Health . Urbana, IL: University of Chicago Press. [ PubMed : 17750114 ]
- Ferrell JA, Mead PA. 1936. History of county health organizations in the United States 1908– 1933 . Washington, DC: Government Printing Office.
- Forquera R. 2001. Urban Indian health . Issue brief prepared for the Henry J. Kaiser Family Foundation, November . Available online at http://www .kff.org/content/2001/6006/ . Accessed March 18, 2002.
- Fraser M. 1998. State and Local Health Department Structures Implications for Systems Change . Transformations for Public Health (The Turning Point Newsletter) 1(4).
- Fraser MR. 1999. Information technology and local health departments . Presentation to the NACCHO Board Annual Meeting, Dearborn, MI, July 1 . Available online at www. naccho.org/GENERAL156.cfm . Accessed March 18, 2002.
- Freed GL, Clark SJ, Cowan AE. 2000. State-level perspectives on immunization policies, practices, and program financing in the 1990s . American Journal of Preventive Medicine 19(3 Suppl.):32–44. [ PubMed : 11024329 ]
- GAO (General Accounting Office). 1999. a. Emerging infectious diseases: consensus on needed laboratory capacity could strengthen surveillance . Report to the Chairman, U.S. Senate Subcommittee on Public Health, Committee on Health, Education, Labor, and Pensions, February. Document No. GAO/HEHS-99-26. Available online at www .gao.gov . Accessed March 18, 2002.
- GAO. 1999. b. Emerging infectious diseases: national surveillance system could be strengthened . Testimony of Bernice Steinhardt, Director of Health Services Quality and Public Health Issues, Health, Education, and Human Services Division, U.S. General Accounting Office, to the U.S. Senate Subcommittee on Public Health, Committee on Health, Education, Labor, and Pensions, February 25. Document No. GAO/T-HEHS-99-62. Available online at www .gao.gov . Accessed March 18, 2002.
- GAO. 2001. a. Food safety: CDC is working to address limitations in several of its foodborne disease surveillance systems . Report to the Chairman, U.S. Senate Committee on Agriculture, Nutrition, and Forestry, September. Document No. GAO-01-973. Available online at www .gao.gov . Accessed March 18, 2002.
- GAO. 2001. b. Bioterrorism: coordination and preparedness . Testimony of Janet Heinrich, Director, Health Care—Public Health Issues, U.S. General Accounting Office, to the Subcommittee on Government Efficiency, Financial Management, and Intergovernmental Relations, Committee on Government Reform, U.S. House of Representatives, October 5. Document No. GAO-02-129T. Available online at www .gao.gov . Accessed March 18, 2002.
- Gostin LO. 2000. Public Health Law: Power, Duty, Restraint . Berkeley: University of California Press.
- Gostin LO. 2002. Public Health Law and Ethics . Berkeley, New York: University of California Press; and Milbank Memorial Fund.
- Gostin LO, Burris S, Lazzarini Z. 1999. The law and the public's health: a study of infectious disease law in the United States . Columbia Law Review 59(1999):35. [ PubMed : 10558403 ]
- Gostin LO, Sapsin JW, Teret S, Burris S, Mair JS, Hodge JG Jr, Vernick JS. 2002. The model state emergency health powers act: planning and response to bioterrorism and naturally occurring infectious diseases . Journal of the American Medical Association 288(5):622– 628. [ PubMed : 12150674 ]
- Gray BH, Rowe C. 2000. Safety-net health plans: a status report . Health Affairs 19(1):185– 193. [ PubMed : 10645086 ]
- Halverson PK, Nicola RM, Baker EL. 1998. Performance measurement and accreditation of public health organizations: a call to action . Journal of Public Health Management and Practice 4(4):5–7. [ PubMed : 10186760 ]
- Hamilton DP. 2001. Public health labs aim to deploy better tests to identify bioagents . Wall Street Journal , October 11, p. A12.
- Health Insurance Portability and Accountability Act of 1996. P.L. 104–191; 110 Statute 1936-2103 . Available online at http://aspe .hhs.gov/admnsimp/pl104191 .htm . Accessed March 12, 2002.
- Henderson DA. 1998. Bioterrorism as a public health threat . Emerging Infectious Diseases 4(3) . Available online at www .cdc.gov/ncidod/EID /vol4no3/henderson.htm . Accessed March 12, 2002.
- HRSA (Health Resources and Services Administration). 2000. The Public Health Workforce: Enumeration 2000 . Prepared for HRSA by Kristine Gebbie, Center for Health Policy, Columbia University School of Nursing, December. Washington, DC: HRSA.
- HRSA. 2002. HRSA awards 27 community health center grants to improve access to services: president asks for $114 million increase in program for fiscal year 2003 . HRSA press release, March 7 , 2002. Available online at http://newsroom .hrsa .gov/releases/2002releases /chcgrants030702.htm . Accessed November 3, 2002.
- Idaho Department of Health and Welfare. 1999. Public health in the new millennium: progress, new threats, new partners . Idaho Disease Bulletin 6(6) . Available online at http://www2 .state.id .us/dhw/cdp/bulletin/db12-99htm . Accessed March 12, 2002.
- IHS (Indian Health Service). 2001. a. Eligibility . February . Available online at http:// info.ihs.gov/TreatiesLaws/Treaties_INDEX.asp . Accessed March 12, 2002.
- IHS. 2001. b. Indians in urban areas . February . Available online at http://info.ihs.gov/People/ People_INDEX.asp . Accessed March 12, 2002.
- IHS. 2001. c. Tribal self-determination . February . Available online at http://info.ihs.gov/ TreatiesLaws/Treaties_INDEX.asp . Accessed March 12, 2002.
- IOM (Institute of Medicine). 1988. The Future of Public Health . Washington DC: National Academy Press. [ PubMed : 25032306 ]
- IOM. 1992. Emerging Infections: Microbial Threats to Health . In Lederberg J, editor; , Shope RE, editor; , Oaks SC, Jr, editor. . (Eds.). Washington DC: National Academy Press. [ PubMed : 25121245 ]
- IOM. 1996. Healthy Communities: New Partnerships for the Future of Public Health . Washington, DC: National Academy Press.
- IOM. 1997. a. America's Vital Interest in Global Health . Washington, DC: National Academy Press.
- IOM. 1997. b. In Durch JS, editor; , Bailey LA, editor; , Stoto MA, editor. (Eds.). Improving Health in the Community: A Role for Performance Monitoring . Washington DC: National Academy Press. [ PubMed : 25121202 ]
- IOM. 1999. Creating a High Profile for Global Health . Highlights from an Institute of Medicine conference , February 28, 1999. Washington, DC: National Academy Press.
- IOM. 2000. a. America's Health Care Safety Net: Intact but Endangered . Washington, DC: National Academy Press. [ PubMed : 25077222 ]
- IOM. 2000. b. Calling the Shots: Immunization Finance Policies and Practices . Washington, DC: National Academy Press. [ PubMed : 25077270 ]
- IOM. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century . Washington, DC: National Academy Press. [ PubMed : 25057539 ]
- IOM. 2003. Who Will Keep the Public Healthy? Educating Public Health Professionals in the 21st Century . Washington, DC: The National Academies Press.
- Johnson R, Morris TF. 2000. Stabilizing the rural public health infrastructure . Publication for the National Advisory Committee on Rural Health, February . Available online at http: //www.nal.usda.gov/orhp/nac_rep.htm . Accessed March 12, 2002.
- Keane C, Marx J, Ricci E. 2001. Privatization and the scope of public health: a national survey of local health department directors . American Journal of Public Health 91(4): 611–617. [ PMC free article : PMC1446649 ] [ PubMed : 11291374 ]
- Keppel KG, Freedman MA. 1995. What is assessment? Journal of Public Health Management and Practice 1(2):1–7. [ PubMed : 10186603 ]
- Kuttner R. 1999. The American health care system—employer-sponsored health coverage . New England Journal of Medicine 340(3):248–252. [ PubMed : 9895408 ]
- Larson C, Sweeney C, Christian A, Olson L. 2002. Collaborative Leadership and Health: A Review of the Literature . Seattle, WA: Turning Point National Program Office.
- Lee PB, Abramovice BG, Lee PR. 2001. Written supplement to the testimony of Dr. Philip R. Lee to supplement a presentation to the Workgroup on Health Statistics for the 21st Century and the Workgroup on National Health Information Infrastructure of the National Committee on Vital and Health Statistics . Available online at http://ncvhs.hhs.gov/ 001030h7.htm . Accessed September 23, 2002.
- The Lewin Group. 1997. Strategies for obtaining public health infrastructure data at the federal, state and local levels . Prepared for DHHS. Available online at http:// aspe.hhs.gov/PIC/pdf/6179.PDF . Accessed November 3, 2002.
- LLGIS (Local Leaders for Geographic Information Systems) Consortium. 2001. Bioterrorism in New York . Available online at http://www .llgis.org/pages/news/index .htm . Accessed March 12, 2002.
- Lumpkin JR. 2001. Air, water, places, and data—public health in the information age . Journal of Public Health Management and Practice 7(6):22–30. [ PubMed : 11710166 ]
- Lumpkin JR, Atkinson D, Biery R, Cundiff D, McGlothlin M, Novick LF. 1995. The development of integrated public health information systems: a statement by the Joint Council of Governmental Public Health Agencies . Journal of Public Health Management and Practice 1(4):55–59. [ PubMed : 10186643 ]
- Lumpkin JR, Landrum LB, Oldfield A, Kimel P, Jones MC, Moody CM, Turnock BJ. 1998. Impact of Medicaid resources on core public health responsibilities of local health departments in Illinois . Journal of Public Health Management and Practice 4(6):69–78. [ PubMed : 10187080 ]
- Mays GP, Halverson PK, Stevens R. 2001. The contributions of managed care plans to public health practice: evidence from the nation's largest local health departments . Public Health Reports 116(Suppl. I):50–67. [ PMC free article : PMC1913663 ] [ PubMed : 11889275 ]
- Meit MB. 2001. I'm OK, but I'm not too sure about you: public health at the state and local levels . Journal of Public Health Management and Practice 7(1):vii–viii. [ PubMed : 11141630 ]
- NACCHO (National Association of County and City Health Officials). 1998. Preliminary results from the 1997 Profile of U.S. Local Health Departments . NACCHO Research Brief No. 1., September. Washington, D.C.: NACCHO.
- NACCHO. 2001. a. Assessment of local bioterrorism and emergency preparedness . NACCHO Research Brief No. 5, October . Available online at www .naccho.org/project48.cfm . Accessed March 12, 2002.
- NACCHO. 2001. b. Testimony of Rex Archer, director, Kansas City Health Department, Kansas City, Missouri, on behalf of NACCHO before the U.S. Senate Subcommittee on Labor, Health and Human Services, Education and Related Agencies, Committee on Appropriations , October . Available online at http://www.naccho.org/advocacydoc424. cfm . Accessed March 12, 2002.
- NACCHO. 2001. c. NACCHO statement to the press regarding the administration's bioterrorism emergency funding request , October 18 . Available online at www.naccho. org/press40.cfm . Accessed March 12, 2002.
- NACCHO. 2001. d. Local public health agency infrastructure: a chartbook , October . Available online at www .naccho.org/prod111.cfm . Accessed March 12, 2002.
- NACCHO. 2001. e. Letter to the president regarding bioterrorism funding , October 18 . Available online at www .naccho.org/advocacydoc430.cfm . Accessed September 13, 2002.
- NACCHO. 2001. f. National Public Health Performance Standards Program (NPHPSP), local instrument . Available online at www .naccho.org/project48.cfm . Accessed March 12, 2002.
- NALBOH (National Association of Local Boards of Health). 2001. National Public Health Performance Standards program, governance instrument . Available online at http://www .nalboh.org /perfstds/instrument.htm . Accessed March 12, 2002.
- National Partnership for Social Enterprise. 2002. A Business Plan for the Implementation of Practice Standards in Bergen County: A Demonstration Project of the New Jersey Department of Health and Senior Services , December 29, 2001. Bergen County, NJ: Bergen County, Department of Health Services.
- NCVHS (National Committee on Vital and Health Statistics). 2002. Information for Health: A Strategy for Building the National Health Information Infrastructure . Report and recommendations from the Work Group on the National Health Information Infrastructure , Washington, DC, November 15, 2001 . Available online at http://ncvhs .hhs.gov . Accessed March 12, 2002.
- NGA (National Governors Association). 1997. Policy positions . Washington, DC: National Governors Association.
- Noren J, Kindig D, Sprenger A. 1998. Challenges to Native American health care . Public Health Reports 113(1):22–33. [ PMC free article : PMC1308364 ] [ PubMed : 9885525 ]
- NRC (National Research Council). 2002. Making the Nation Safer: The Role of Science and Technology in Countering Terrorism . Washington, DC: The National Academies Press.
- OMB (Office of Management and Budget). 2001. Budget summary, FY 2002 . Available online at http://www .whitehouse .gov/omb/budget/fy2002/budiv_3.html . Accessed September 18, 2002.
- OMB. 2002. Budget of the United States Government, Fiscal Year 2003 . Washington, DC: OMB.
- Osterholm MT, Schwartz J. 2000. Living Terrors: What America Needs to Know to Survive a Bioterrorist Catastrophe . New York: Delacorte Press.
- Pew Environmental Health Commission. 1999. Healthy from the Start: Why America Needs a Better System to Track and Understand Birth Defects and the Environment . Report sponsored by the Pew Environmental Health Commission at the Johns Hopkins School of Hygiene and Public Health, November . Available online at http://pewenvirohealth. jhsph.edu . Accessed September 18, 2002.
- Pew Environmental Health Commission. 2000. America's Environmental Health Gap: Why the Country Needs a Nationwide Tracking Network . Report sponsored by the Pew Environmental Health Commission at the Johns Hopkins School of Hygiene and Public Health, November . Available online at http: //pewenvirohealth.jhsph.edu . Accessed September 18, 2002.
- Pew Health Professions Commission. 1998. Recreating Health Professional Practice for a New Century . San Francisco: Pew Health Professions Commission.
- Public Health Foundation. 2000. Statewide public health expenditures: a pilot study in Maryland , March 2000 . Available online at http://www .phf.org/Reports.htm . Accessed March 12, 2002.
- Public Health Functions Steering Committee. 1994. Public health in America, fall 1994 . Available online at www .health.gov/phfunctions/public.htm . Accessed March 12, 2002.
- Rich M. 1993. Federal policymaking and the poor: national goals, local choices, and distributional outcomes . Princeton, NJ: Princeton University Press.
- Rosen G. A History of Public Health . 1993. Baltimore, MD: Johns Hopkins University Press.
- Salinsky E. 2002. Will the nation be ready for the next bioterrorism attack? Mending gaps in the public health infrastructure . National Health Policy Issue Brief No. 776, June 12 . Available online at http://www .nhpf.org/ibonline.cfm . Accessed September 18, 2002. [ PubMed : 12083160 ]
- Sandia National Laboratories. 2002. Rapid Syndromic Validation Project (RSVP) . Available online at http://www .cmc.sandia.gov/bio/rsvp . Accessed September 18, 2002.
- Study Group on the Mission and Organization of the Public Health Service. 1960. The Hundley Report .
- Turnock B. 2000. Public Health: What It Is and How It Works , 2nd ed. Gaithersburg, MD: Aspen Publishers.
- U.S. House of Representatives. 2002. House Report 107-350 - Making Appropriations for the Department of Defense for the Fiscal Year Ending September 30, 2002, and for Other Purposes . Available online at: http://thomas .loc.gov . Accessed October 21, 2002.
- USPHS (U.S. Public Health Service). 1997. The Public Health Workforce: An Agenda for the 21st Century . Washington, DC: Department of Health and Human Services.
- Valdiserri R. 1993. Temples of the future: an historical overview of the laboratory's role in public health practice . Annual Review of Public Health 14:635–648. [ PubMed : 8323605 ]
- Wall S. 1998. Transformations in public health systems . Health Affairs 17(3):64–80. [ PubMed : 9637967 ]
- White House. 2001. A Blueprint For New Beginnings: A Responsible Budget for America's Priorities . Washington, DC: U.S. Government Printing Office. Available online at: http:/ /www.whitehouse.gov/news/usbudget/ blueprint/budtoc.html . Accessed March 18, 2002.
The 10th Amendment enunciates the plenary power retained by the states: “The powers not delegated to the United States by the Constitution, nor prohibited by it to the States, are reserved to the States respectively, or to the people.”
According to 1990 Census Bureau data, about 56 percent of the American Indian and Alaska Native population lived in urban areas (IHS, 2001b). Census data for 2000 show a similar pattern, with 57 percent of individuals who identify themselves solely as Native American or Alaska Native living in metropolitan areas (Forquera, 2001).
For example, a South Dakota statute passed in the late 1800s and last amended in 1977 makes it a misdemeanor for a person infected with a “contagious disease” to “intentionally [expose] himself . . . in any public place or thoroughfare” (S.D. Codified Laws § 34–22–5). Similarly, an 1895 New Jersey statute forbids common carriers to “accept for transportation within this state any person affected with a communicable disease or any article of clothing, bedding, or other property so infected” without a license from the local board of health (N.J. Stat. Ann. § 26:4–11 9). This might have made some sense in a time when diseases such as influenza, diphtheria, and measles were significant sources of serious illness and death, but it serves little purpose today. Although it may be impolite for people with the flu to walk around in public, it is not a major health threat. Furthermore, efforts to isolate people who do not pose a significant health risk would often violate modern disability discrimination law (it was held that the threat of disease did not justify excessively stringent quarantine of a blind plaintiff's guide dog) (see Crowder v. Kitagawa , 81 F.3d 1480, 1481, 9th Circuit, 1996).
Turning Point, a program funded by the Robert Wood Johnson and W. K. Kellogg Foundations, works to strengthen the public health infrastructure at the state and local levels across the United States and spearheads the Turning Point National Collaborative on Public Health Statute Modernization.
The Model State Emergency Health Powers Act (MSEHPA) provides states with the powers needed “to detect and contain bioterrorism or a naturally occurring disease outbreak. Legislative bills based on MSEHPA have been introduced in 34 states” (Gostin et al., 2002).
Home-rule statutes (in constitutions or by statute) give localities (e.g., cities or counties) powers of self-government. In such cases, localities can exercise police powers independently from the state.
Federal agencies have developed numerous regulatory techniques and decision-making processes to identify and respond to health and safety risks (Gostin, 2000). Agencies can control entry into a field by requiring a license or permit to undertake specified activities; set health and safety standards, conduct inspections to ensure compliance, adjudicate violations, and impose penalties; abate nuisances that threaten the public; dispense grants, subsidies, or other incentives; and influence conduct through a wide variety of informal methods (Gostin, 2000). For example, the Department of Agriculture regulates the safety of meat, poultry, and eggs. EPA regulates air and water pollution, pesticides, and toxic wastes. The Department of Energy oversees radiation-related environmental management, environmental safety and health, and civilian radioactive waste management. The Department of Labor regulates occupational health and safety and self-insured employee benefit plans. The Department of Transportation sets and monitors standards for highway safety. The Bureau of Alcohol, Tobacco, and Firearms in the Department of the Treasury, the Consumer Product Safety Commission, the Federal Trade Commission, and the Occupational Safety and Health Administration also issue regulations that protect the public against health risks (Boufford and Lee, 2001).
The Council on Linkages between Academia and Public Health Practice is composed of leaders from national organizations representing the public health practice and academic communities. The council grew out of the Public Health Faculty/Agency Forum, which developed recommendations for improving the relevance of public health education to the demands of public health in the practice sector. The council and its partners have focused attention on the need for a public health practice research agenda.
Sandia is a multiprogram engineering and science laboratory operated by Sandia Corporation, a Lockheed Martin Company, for the Department of Energy's National Nuclear Security Administration.
CLIA, enacted by Congress in 1988, mandated a broad and wide-ranging change in the regulation of laboratories that perform testing for medical diagnoses. CLIA expanded federal regulatory authority to approximately 170,000 laboratories, most of which were previously unregulated laboratories in physicians' offices. In 1997, these laboratories performed an estimated 8 billion tests at a cost of approximately $30 billion. In June 1991, the Secretary of DHHS delegated responsibility for development and implementation of the scientific and technical aspects of the regulations to CDC. Within CDC, the Division of Laboratory Systems, Public Health Practice Program Office, carries out the responsibility of standards development and laboratory improvement, whereas CMS administers the program (CDC, 2001c).
Individual states reported a range from 1.4 to 89 staff per 1 million population.
CIDRAP was established in September 2001 with the mission of (1) supporting the development of and refining public policies relating to the prevention, control, and treatment of infectious diseases to ensure that they reflect the most current biomedical knowledge, and (2) promoting practices among both health care professionals and the public that aim to reduce illness and death from infectious diseases through provision of accurate, up-to-date information and education.
At the time that this report was drafted, legislation for a Department of Homeland Security was under debate. The legislation proposes a “single focal point” for managing and overseeing security functions across Congress, federal departments and agencies, state governments, and local governments. Such a department undoubtedly will have direct and indirect implications for governmental public health agencies. However, the evolving nature of this process led the committee not to include a discussion of this work in progress.
The Lewin Group is a health and human services consulting firm whose activities include advising public, private, and nonprofit sectors to improve policy, manage and evaluate programs, and maximize performance as well as other issues.
- Cite this Page Institute of Medicine (US) Committee on Assuring the Health of the Public in the 21st Century. The Future of the Public's Health in the 21st Century. Washington (DC): National Academies Press (US); 2002. 3, The Governmental Public Health Infrastructure.
- PDF version of this title (7.3M)

In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- The Governmental Public Health Infrastructure - The Future of the Public's Healt... The Governmental Public Health Infrastructure - The Future of the Public's Health in the 21st Century
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Breaking down the MPA/MPP personal statement, personal essay, and supplemental essay
Essays for graduate study cover a myriad of topics. Here at SPIA, we hope our essays help reflect and speak to our culture, our community, and our values—the stuff we care about. We require a variety of essays and short answer written responses, and each serves a slightly different purpose toward helping us to understand the academic and professional trajectory of each person as well as the motivation for graduate study at Princeton. No one thing is determinative in our process or application; we read each file individually and holistically, and admissions decisions are based on the totality of information in the file.
The personal statement should answer the prompt and include an explanation of one’s commitment to a career in public service. We are interested in a clear description of the policy areas of interest to you and why you care about them as well as how your previous academic, personal, and professional experiences have shaped your career goals. We want to know why you want to enroll at SPIA, what you hope to gain from our program, as well as your career plans in terms of policy issues and agencies or organizations you wish to work with and why. We are looking to understand Why Princeton. Why now. And what’s next.
SPIA’s supplemental essay has long been the part of our application where we ask you to go beyond the other dimensions of the file and where we seek to get to know you on a more personal and individual basis. We all come from somewhere and it shapes us – both in who we become and what we value. We’re interested in your story and what shaped you. What do you value? This essay often helps us to further understand the person behind the paper.
This year, the Graduate School introduced the personal essay . The announcement of this essay reaffirms Princeton’s strong commitment to welcoming students from diverse backgrounds and experiences. It provides applicants an additional space to describe how their academic interests and life experiences will help them contribute to Princeton’s scholarly community. We hope to further understand how you will contribute to our tight-knit and vibrant campus community.
We understand there may be some similarities and overlap in how you interpret and write each essay. Our hope, of course, is that each essay will reveal something new and that each provides space and opportunity to translate through as rich and as full a description of your background, goals, and aspirations as possible.
Through each of them, we are looking for you to tell us your story in the way that only you can.
Writing Guide
Writing serves as a useful skill for anyone in the field of public health — students and professionals alike. Public health students must enroll in writing-intensive courses that require essays and research papers. Once students graduate, they put their skills to use writing reports on community health. They may compose presentations, research studies, or press releases, depending on their jobs. Those who stay in academia continue to write research papers throughout their careers.
Students should begin cultivating a clear and concise writing style long before they graduate.
They should also learn how to use standardized citations. Understanding how to properly cite sources will help students as they conduct research and publish their findings. Citations also help students and researchers avoid plagiarism.
This guide explains how to write a public health report, a research paper, and an exam essay. The page also advises students on how to conduct research online and find trustworthy sources. Students can review citation style guides and public health writing samples.
Featured Online Programs
Types of writing public health students will do in school, personal statements.
When applying to a public health program, schools often require students to submit personal statements. Schools may either ask students to write a general personal essay answer a certain prompt. Usually, prompts center around applicants’ interest in public health or about the public health field in general. Students might come across a prompt similar to this one: “Identify a public health issue in the U.S., and how you would work to rectify it as a public health professional.” Alternately, students may encounter this common topic: “What drove you to pursue a career in public health?”
Schools look for essays that are honest, well-written, and well-organized. Students should get the reader’s attention with an anecdote illustrating their commitment to public health. Was it an experience with adversity or discrimination that prompted you to pursue this career? Did you learn about the importance of public health while volunteering or traveling? Include those details in the story.
Students should also demonstrate their current knowledge of public health. They may write about their career goals as well. However, students should avoid writing exaggerations, falsehoods, or superlatives. People who read admissions essays can typically sense when applicants are stretching the truth. If the school makes the personal statement optional, students should still consider writing one. A personal statement demonstrates commitment and hard work, and may help make up for flawed or weak admissions materials.
In some public health courses, professors require students to answer essay questions during exams. This can be intimidating since students do not usually know the prompt until they actually start the exam. Students have a limited amount of time to write the essay, typically one or two hours. Students should allot their time accordingly. Some students do not plan their work before they begin writing; this can lead to sloppy essays with weak supporting points, disorganized information, and tangents unrelated to the prompt.
For a 60-minute time frame, students may give themselves 10 minutes to brainstorm, plan, and outline.
During the brainstorming process, students should write their thesis statement.
Then they should jot down three points that support the thesis. These ideas will serve as the three body paragraphs. Students may give themselves five minutes to write the introduction, 30 minutes to write the body, and then five minutes to write the conclusion. They then have 10 minutes to proofread. Students often inadvertently miss this step, but proofreading may make or break the essay.
Students should begin planning long before the day of the essay. Students ought to review the material well enough to be prepared for any prompt. They should carefully look over their lecture notes to determine which points the professor emphasized during classes. These points will likely prove significant when it comes time for the exam. Students should also make sure that they actually answer the prompt instead of rushing and jumping to assumptions.
Research Papers
In a research paper, students examine the existing research, theories, case studies, and ideas about a particular topic. Students have several weeks to write research papers, which may seem like a huge amount of time. However, research papers demand a lot of work, so students should start early. Professors rarely assign strict, narrow prompts for research papers. Instead, they usually give students a topic or range of topics, and students choose their focus. Public health topics may include how poverty or race affects access to healthcare; opioid abuse; the social consequences of HIV/AIDS; childhood obesity; or maternal mortality in third world countries.
Students should start by brainstorming a list of points and ideas they will investigate. Then comes the most time-intensive and significant part of a research paper: the research itself. Students ought to use multiple different resources to help them craft their arguments. Options include online databases, academic journals, and their college library. Make sure you keep track of citations and sources as you go.
Students should also make sure their essays are well-structured. A well-written thesis unites the main points of the paper. Unlike essays, research papers usually include more than five paragraphs. Students may break down their arguments into different sections. A research paper must include a works cited or bibliography that credits all sources. The exact length of the paper and number of sources depends on the professor’s expectations.
Over the course of their academic careers, public health students write many kinds of essays. Professors often assign persuasive essays, in which the student must make a convincing argument; expository essays, in which the student explores and explains an idea; narrative essays, in which the student tells a story; comparative essays, in which the students analyzes two different viewpoints; and cause and effect essays, in which the student must explain the logic behind why certain events or phenomena occur.
- Narrative: In a narrative essay, the author tells a meaningful story. Studying public health, you probably won’t write many narratives. However, narrative essays can support an argument or prove a point. For instance, if you argue that every community should have a free clinic, you might tell a personal story about your experience growing up in a low-income neighborhood with no access to healthcare. Make sure your essay demonstrates a clear plot, follows an organized structure, and includes many details.
- Expository: When professors assign expository essays, they expect students to explain or describe a concept. These essays help professors evaluate whether students have a firm grasp on a topic. Expository essay often include five paragraphs: an introduction with a thesis statement, three main points backing that thesis statement, and a conclusion. Students should do plenty of planning and research before writing to ensure they adequately address the prompt and include enough evidence.
- Persuasive: Persuasive essays appear commonly in academic assignments. Students first develop an argument as a thesis statement. Then, they generate a cogent defense of that argument by researching supporting evidence. Students should be able to anticipate arguments against their thesis statement and include counterpoints. In persuasive essays, students not only demonstrate their knowledge of the course material, but also prove their critical thinking skills by developing their case.
- Comparative: A comparative essay requires students to compare and contrast two ideas, viewpoints, or things. For example, public health students may compare two texts, theories, public health systems, or positions on an issue. First of all, students should create a list of similarities and differences between the two items. After that, they can develop a thesis statement on whether the similarities outweigh the differences or vice versa. Finally, they should organize the essay. They can either defend their thesis statement by listing each point of comparison, or they can split the essay in half by discussing subject one and then subject two.
- Cause and Effect: These essays require students to explain how one event or theory leads to a specific consequence. For instance, a public health student might argue that abstinence-only education in public schools leads to a higher rate of teenage pregnancies. Students should remember that just because one event follows another, those two events do not necessarily influence one another. In other words, correlation does not equal causation. In the analysis portion of the essay, students must explain specific reasons why they think the two events are connected using data and other evidence.
Citations Guide for Public Health Students
In public health writing, just as any other discipline, students must cite their sources. If students use ideas, theories, or research without crediting the original source — even unintentionally — then they have plagiarised. An accusation of plagiarism could follow the student throughout their education and professional career. Professors may fail students who plagiarise, sinking their GPA. Plagiarism accusations can also ruin a student’s credibility. Fortunately, students can avoid plagiarism by properly giving credit for their data and ideas. Common citation styles include those listed below.
American Psychological Association (APA) Style
Students in the social sciences use APA style when writing their essays and research papers. Business and nursing students also commonly use APA style. APA prefers active voice over passive voice, as well as concise language over flowery words. Research papers written in APA style should include a title page, abstract, and a reference page. In-text citations list the author’s name, year of publication, and page number if applicable. Below is an example of how to cite a source using APA style.
In-text citation:
In Milwaukee, poor neighbourhoods were segregated by design (Desmond, 2017, p. 249).
On the works cited page:
Desmond, M. (2017). Evicted: Poverty and profit in the American city . London: Penguin Books.
Chicago Manual of Style (CMS)
History students and students of the natural sciences typically use Chicago, or Turabian, style in their research. Papers written in Chicago style include three sections: the title page, the main body, and a references page. This style also uses footnotes to source information and provide more context. In-text citations list the author’s name, the date of publication, and the page where the student found the data. Unlike APA style, though, the in-text citation does not use a “p.” before the page number. See the example below:
In Milwaukee, poor neighbourhoods were segregated by design (Desmond 2017, 249).
Desmond, Matthew. Evicted: Poverty and Profit in the American City . London: Penguin Books, 2017.
Modern Language Association (MLA) Format
Students of the humanities — including literature, foreign languages, and cultural studies — use MLA style in their research papers. Unlike APA and Chicago style, MLA style does not require students to add a title page. MLA papers also do not include an abstract. Students only need to include the paper itself and a works cited page that corresponds with in-text citations. When adding citations in the body of the text, MLA includes the author’s last name and the page number in parentheses. This style does not list the publication year. You can find an example of MLA citation below:
In Milwaukee, poor neighbourhoods were segregated by design (Desmond 249).
Associated Press (AP) Style
Journalists use Associated Press, or AP style, in their work. AP style standardizes grammar and spelling usage across news media and mass communications. Students rarely use AP style, unless they are writing an article in their subject area for a newspaper or magazine. AP style prioritizes brevity and conciseness above all else. Therefore, it includes several rules that differ from other writing styles. For instance, AP style eliminates the last comma in a list of items (for example: “She dressed in capris, a tank top and sandals”). Since students and professors do not use AP style for academic papers, AP style does not include a reference page like other style guides. Instead, AP style simply uses non-parenthetical in-text citations.
“People who live in low-income communities lack opportunities to exercise,” said Lydia Homerton, professor of public health at Hero College.
The Best Writing Style for Public Health Majors
Professionals in the public health field use APA, the most common style in the social sciences. Professors expect students to use APA style as well. Public health research follows a standardized system of citing sources, making it easier for students and professionals in the field to conduct further research. Students should add a title page and abstract before the essay, as well as a list of references in the back.
Common Writing Mistakes Students Make
Active vs. passive voice.
When writing essays and research papers, students should use active voice and avoid passive voice. Learning the difference between passive and active constructions can be tricky. First of all, students should be able to identify the subject in a sentence. The subject is the noun performing an action. Take this sentence: “The woman catches the keys.” In this case, the woman is the subject of the sentence because she is the one performing the action, catching. The sentence “The woman catches the keys” is active because it focuses on the subject and the action. You can identify an active sentence by checking if the first noun is a subject performing an action.
By contrast, examine this sentence: “The keys were caught by the woman.” The first noun, “keys,” is not performing an action. Instead, it is being acted upon. The subject performing the action — the woman — is at the end of the sentence and not the beginning. This sentence uses passive voice instead of active voice. Some passive sentences do not include a subject at all. For example, “The keys were caught.”
Active voice makes writing more concise and easy to understand. Active sentences often include more information, especially about the subject performing an action. In research papers, students should use active voice whenever possible. However, sometimes it is clear that the author is the one performing the action, so active voice is not necessary. For instance, a researcher might write “the experiment was conducted Friday” instead of “I conducted the experiment Friday.”
Punctuation
Incorrect punctuation confuses readers. The wrong punctuation can change or obfuscate the meaning of a sentence, paragraph, or the entire essay. Publishers, professors, and other researchers often look down on papers with incorrect grammar, even if the content includes important or accurate research. Consequently, students should always use proper grammar in their essays.
The wrong punctuation can change or obfuscate the meaning of a sentence, paragraph, or the entire essay.
While students make many different errors with punctuation, most common errors revolve around colons and commas. Understand the difference between colons and semicolons. Both punctuation marks separate two parts of a sentence. Students should use colons when introducing a list. (“He ate lots of meat: pork, chicken, steak, veal, and duck.”) Colons can also introduce an appositive or new idea. (“She finally gave him the gift: a new computer.”) Semicolons, on the other hand, connect two complete, independent sentences. These sentences should be separate but related. (“He ate a lot of meat; he was ravenous.”)
Students should also take care to avoid comma splices. A comma splice occurs when writers connect two independent sentences using a comma. The following sentence includes a comma splice: “She danced with her boyfriend, he was very clumsy.” Instead, students could add an “and” to connect the two sentences. (“She danced with her boyfriend, and he was very clumsy.”) Alternately, writers could connect the sentences with a semicolon. (“She danced with her boyfriend; he was very clumsy.”) Lastly, writers could separate the two sentences with a period.
Proper grammar helps readers understand your essays. Proper grammar also gives your essay credibility. If you have a perfectly-argued essay, but your paper includes multiple grammar mistakes, the reader will likely be skeptical of the entire argument.
Understand the difference between there/their/they’re. “There” refers to a place. (“The dog is over there.”) Their shows possession. (“This is their house.”) “They’re” is a contraction for “they are.” (“They’re eating at the diner.”)
Also learn the difference between it’s and its. “It’s” is the contraction for “it is.” (“It’s hot outside.”) “Its” shows possession. (“The bird eats in its cage.”)
Make sure your sentences include proper subject-verb agreement. In other words, if the subject of a sentence is plural, the verb should also be plural. For example, use “The boy and his sisters are eating breakfast” instead of “The boy and his sisters is eating breakfast.”
Writing Resources for Public Health Students
- Guide to Improving Scientific Writing in Public Health : This guide from the World Health Organization and the Pan American Health Organization teaches students how to write about complicated scientific material in a way that’s easy for readers to understand. The guide includes tips on vocabulary and format.
- Argument, Structure, and Credibility in Public Health Writing : Written by a professor at Harvard’s School of Public Health, this essay breaks down how to make effective arguments in public health writing. The page includes flow charts and figures to help illustrate exactly how public health essays should be organized.
- Purdue Online Writing Lab APA Style Guide : Purdue’s Online Writing Lab includes style guides for all writing and citation styles, including APA. The style guides help students understand how to format papers, use in-text citations, and create reference pages.
- Award-Winning Health Articles : One of the best ways to improve your writing is to read good examples. This page lists nine award-winning public health writing samples.
- The Women’s and Children’s Health Policy Center Writing Skills Guide : This website links to several modules on writing public health documents. Lessons include policy briefs and memos.
Take the next step toward your future with online learning.
Discover schools with the programs and courses you’re interested in, and start learning today.

Master of Public Health
A thesis is a substantive and original body of work that allows the student to synthesize and integrate knowledge from their public health course work and practicum experiences, apply it to a particular topic area, and communicate their ideas and findings through a scholarly written product. The thesis represents the culmination of the student’s educational experience in the Vanderbilt MPH Program.
The thesis may take on different formats, depending on the student’s track focus and interests. Regardless of the format chosen, the student must apply critical thought, systematic analysis, and clear presentation.
Each student is responsible for identifying a topic and appropriate format for their thesis with the assistance and guidance of faculty advisers and faculty thesis readers.
The practicum product must be distinct from the thesis. Although the practicum and thesis can be related, the student must be able to articulate how the two projects are independent from one another. The practicum is a practice experience that allows students to apply and develop skills in public health concepts. The thesis is the synthesis and integration of knowledge acquired in coursework and through the practicum and results in an original scholarly work.
View selection of published theses
Additionally, students have the option to pursue publishing their thesis products in scholarly journals.
2024 Thesis Topics
2023 thesis topics, 2022 thesis topics, 2021 thesis topics, 2020 thesis topics, 2019 thesis topics, 2018 thesis topics, 2017 thesis topics, 2016 thesis topics, 2015 thesis topics, 2014 thesis topics, 2013 thesis topics, 2012 thesis topics.
- About the School
- Quick Facts
- Administration
- Basic Sciences
- A-Z Directory
- Contact Information
- Campus Maps & Parking
- Current Students
- Basic Sciences Faculty Affairs
- Clinical Faculty Affairs
- Eskind Biomedical Library
- People Finder
Trainings and tools
- Home: Trainings and tools
- Public health and QI toolbox
- Resource library for advancing health equity
- Public health nursing tools and resources
- CHS administration handbook
- All publications and handbooks
- Related: TA and workforce development
- Return to the Center for Public Health Practice
Contact Info
Table of Contents Next Chapter
Introduction: Public health in Minnesota
What is public health? What does public health do?
Minnesota's public health system functions as a partnership between state and local governments, and is designed to ensure that the public's health and safety are protected statewide while providing local governments with the flexibility needed to identify and address local needs.
In a time of constrained resources, community health boards need to continue to build capacity to address increasingly complex public health issues. Many regions use similar approaches to maximize resources, including cross-jurisdictional sharing to achieve economies of scale, increasing efficiency, focusing on quality improvement, developing the public health workforce and leadership, and emphasizing the importance of a strong public health infrastructure.
What is public health?
Public health focuses on the health needs of the population as a whole, and gives priority to preventing problems over the early detection and treatment of problems. By focusing on the greatest good for the greatest number of people, public health organizes community resources to meet health needs and takes positive action to address community health issues.
Public health is based on an understanding of the causes of health problems; a person's health outcomes can be impacted by everything from genetics, to environmental factors, to living conditions, to cultural norms, and to individual choices. It is generally accepted that overall population health is determined by the four factors below, approximately weighted according to their impact.
One theory that breaks down the factors that influence health follows:
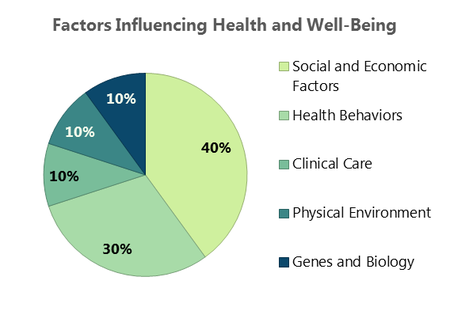
Public health is closely intertwined with many other issues that affect public health—called social determinants of health. For example, poor health habits like smoking or excess alcohol use can lead to chronic diseases and increased hospital costs. Youth violence can result in increased costs for court time and correctional facilities. It can be difficult to visualize the broad factors that influence health, which can make public health difficult to describe in concrete terms.
The Centers for Disease Control and Prevention (better known as the CDC) compiled the following Ten great health achievements -- United States, 2001-2010 :
- Vaccine-Preventable Diseases
- Prevention and Control of Infectious Diseases
- Tobacco Control
- Maternal and Infant Health
- Motor Vehicle Safety
- Cardiovascular Disease Prevention
- Occupational Safety
- Cancer Prevention
- Childhood Lead Poisoning Prevention
- Public Health Preparedness and Response
This list is based on the opportunity for prevention, and the impact on death, illness, and disability in the United States.
What does public health do?
According to the Institute of Medicine's well-known 1988 study, The future of public health , the core functions described below are carried out primarily by government and constitute the most critical foundations of an effective public health system.

The assessment function of public health can be viewed as "knowing what needs to be done." This encompasses activities such as epidemiological surveillance, data collection and analysis, monitoring and forecasting, root cause analysis, and other research practices. The assessment function is often used to facilitate decision making by collecting the best evidence with which to weigh competing options and consider the allocation of limited resources.
Policy development
The policy development function of public health can be viewed as "being part of the solution." This includes being involved in the crafting of legislation, rules, policies, practices, and budgets. In its policy development capacity, a public health entity may plan for and set priorities, provide leadership and advocacy, convene and negotiate with stakeholders, mobilize resources, provide training, or encourage private action. In policy development, the process is often just as important as the product—it will ideally be fair, inclusive, and far-sighted.
Assurance can also be thought of as "making sure it happens." The government can ensure public health services are delivered by mandating them, providing services directly, or incenting other sectors to take action. This often requires implementation of legislative language, regulation, reporting on progress, and holding stakeholders accountable. Exercising this authority comes with great responsibility and entails a strong level of commitment to the welfare of the community. In its assurance capacity, the government is challenged to strike the appropriate balance between free market interests and social equity or the greater good.
Next : Government's responsibility for public health
- public health practice
Home — Application Essay — National Universities — Why I Chose Public Health
Why I Chose Public Health
- University: Harvard University
About this sample

Words: 674 |
Published: Feb 15, 2024
Words: 674 | Pages: 1 | 4 min read
I have been driven by a passion for improving the well-being and quality of life for individuals and communities. This desire has led me to pursue a career in public health. In this essay, I will outline the reasons why I chose public health as my field of study and how I believe it aligns with my values and aspirations.
Say no to plagiarism.
Get a tailor-made essay on
'Why Violent Video Games Shouldn't Be Banned'?
One of the primary reasons I chose public health is its inherent focus on social justice. Public health recognizes that health disparities exist due to various social determinants, including socioeconomic status, race, and access to healthcare. By addressing these underlying factors, public health strives to create a more equitable society where everyone has the opportunity to lead a healthy life.
I firmly believe that health is a fundamental human right, and it should not be determined by one's background or circumstances. Public health offers me the platform and tools to challenge the status quo, advocate for marginalized groups, and work towards eliminating health disparities.
Another aspect that attracted me to public health is its interdisciplinary nature. Public health encompasses a wide range of disciplines, including epidemiology, biostatistics, environmental health, health policy, and social and behavioral sciences. This multidisciplinary approach allows me to explore and understand health issues from various angles.
I find great value in the intersectionality of different disciplines, as it enables a comprehensive understanding of complex health challenges. By collaborating with professionals from diverse backgrounds, I can leverage their expertise and perspectives to develop innovative and effective solutions for public health issues. This interdisciplinary nature of public health ensures that I am constantly learning, adapting, and broadening my knowledge base.
Choosing public health also stems from my desire to make a tangible impact on individuals and communities. Public health interventions have the power to save lives, prevent diseases, and improve overall well-being on a large scale. It is not merely about providing immediate treatment but rather focusing on prevention and health promotion.
By working in public health, I can contribute to the development and implementation of evidence-based strategies that address the root causes of health issues. Whether it is designing preventive programs, conducting research on emerging diseases, or advocating for policy changes, public health allows me to translate my passion into concrete actions that positively influence the lives of others.
Public health also offers a global perspective, which resonates deeply with my personal experiences and aspirations. The interconnectedness of health transcends national boundaries, making it crucial to consider global health issues with a holistic approach.
I have witnessed firsthand the impact of health disparities in developing countries during volunteer experiences abroad. These experiences have motivated me to address global health inequities and work towards empowering communities to achieve better health outcomes.
Public health equips me with the skills and knowledge to address challenges in both local and global contexts. It allows me to engage in meaningful work that transcends borders and contribute to the well-being of diverse populations.
Lastly, I chose public health because it is a field that is constantly evolving and adapting to new challenges and discoveries. The emergence of new diseases, advancements in technology, and changing societal dynamics necessitate ongoing innovation in public health.
I am drawn to the dynamic nature of public health, as it requires continuous learning and staying up-to-date with the latest research and best practices. This ever-evolving landscape presents exciting opportunities for me to contribute to emerging fields such as digital health, genomics, and health informatics.
By choosing public health, I am embarking on a journey of lifelong learning and growth, where I can actively contribute to the generation of new knowledge and drive positive change.
Keep in mind: This is only a sample.
Get a custom paper now from our expert writers.
In summary, I chose public health because it aligns with my values of social justice and equity, offers interdisciplinary collaboration, provides opportunities for tangible impact, presents a global perspective, and embraces the constant evolution of the field. Public health offers me the platform to address pressing health issues and work towards creating a healthier, more equitable society. I am eager to harness my passion, skills, and knowledge in public health to make a lasting difference in the lives of individuals and communities.
Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Karlyna PhD
Verified writer
- Expert in: National Universities

+ 129 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online

Are you interested in getting a customized paper?
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on National Universities
I had thought of living in simplicity and happiness before, but I never understood its significance until I heard this sentence. “I will not allow you to come to my house. I am poor.” I stared and looked at him as my eyes filled [...]
Personal Statement I have sworn on my biology textbook instead of the Bible since my sophomore year because I have an obsession with truth. After reading The Sound and the Fury a month ago I thought that I had the truth of [...]
Growing up, I was always fascinated by the world of sports. From watching my favorite basketball teams on TV to playing soccer with friends at the local park, sports have always been an integral part of my life. As I grew older, [...]
“It is your turn to speak, Hyun Jung.” This was the moment that I had feared the most when I was first accepted to an international school. My English skills were terribly poor, which often led me to avoid difficult interactions [...]
Though my high school does not have a Creed, I feel that if it did the Colorado Creed would fit perfectly. Henry M. Gunn High School breeds a caliber of student that is both intellectually hungry and incredibly compassionate. [...]
97%. That is the survival rate for thyroid cancer. It’s the first thing I looked up after my diagnosis. I felt like something inside me shattered. I told myself I could live with that because, statistically speaking, I would be [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

- USF Research
- USF Libraries
Digital Commons @ USF > College of Public Health > Public Health Practice > Theses and Dissertations
Public Health Theses and Dissertations
Theses/dissertations from 2023 2023.
Needs Assessment for a Web-Based Support Resource for Patients with a Pathogenic Variant in LMNA , Dylan M. Allen
Evaluation of a Story-telling Approach to Educate Minority Populations About Inherited Cancer , Celestyn B. Angot
Using the Genetic Counseling Skills Checklist to Characterize Prenatal Genetic Counseling , David A. Cline
Reframing Resistance, Resilience, and Racial Equity in Maternal Health: A Mixed Methods Exploration of Paternal Involvement and the Racial Disparity in Severe Maternal Morbidity , Marshara G. Fross
Student Perceptions of the Nonmedical Use of Prescription Stimulants and Preferences for Health Education , Ana Gutierrez
Relationships between Leading and Trailing Indicators at Construction Sites in Yanbu Industrial City, Saudi Arabia , Anas H. Halloul
Variability of Air Sampling Results Using Air-O-Cell Cassettes , Christina M. Haworth
Use of Silica Dust and Lunar Simulants for Assessing Lunar Regolith Exposure , Layzamarie Irizarry-Colon
The Aging Workforce: How it Relates to Incident Rates within a Distribution Warehouse and a Chemical Manufacturing Building , Elisabeth V. Jones
Fuzzy KC Clustering Imputation for Missing Not At Random Data , Markku A. Malmi Jr.
Piloting a Spanish-language Web-based Tool for Hereditary Cancer Genetic Testing , Gretter Manso
Development of a ddPCR Multiplex to Measure the Immune Response to Borrelia burgdorferi. , Kailey Marie McCain
A Healthcare Claims Investigation of Parasomnia Epidemiology, Associations with Attention Deficit/Hyperactivity Disorder, and REM Sleep Behavior Disorder Correlates , Anh Thy Ha Nguyen
Diet and Salivary Microbiome on Cardiovascular Risk and Glycemic Control in Participants with and without Type 1 Diabetes: The CACTI Study , Tiantian Pang
Evaluation of Two Methods to Estimate Wet Bulb Globe Temperature from Heat Index , Stephi Pofanl
Intimate Conversations: A Mixed-Methods Study of African American Father-Adolescent Sexual Risk Communication , Shanda A. Vereen
Assessment of ISO Heart Rate Method to Estimate Metabolic Rate , Karl Williams
Theses/Dissertations from 2022 2022
Outcomes of a Periodic Exposure Assessment of Workers at a University Campus , Logan M. Armagast
Evaluating the Effect of Public Health Governance Structure and Public Opinion on COVID-19 Disease Control Interventions , Daniel Chacreton
Alpha Synuclein: A therapeutic target and biomarker for Parkinson’s Disease , Max Chase
A Study of Noise Exposures for Amusement Park Employees by Positions and Ride Categories , Danielle M. Dao
Bayesian Network-based Diagnostic Support Tool with Limited Point-of-Care Ultrasound for Work-related Elbow Injuries , Cristina Maria Franceschini Sánchez
Host-Pathogen Coevolution Between Tasmanian Devils (Sarcophilus harrisii) and Devil Facial Tumor Disease , Dylan Garret Gallinson
Measurements of Generalizability and Adjustment for Bias in Clinical Trials , Yuanyuan Lu
Examining the Relationship between Racial Respect among Black Early Childhood Professionals and their Perceptions of Black Children , Kayla Nembhard
Etiology of sterile intra-amniotic inflammation: An exploratory study , Zoe M. Taylor
Evaluating and Improving a Novel Toolkit for Implementation and Optimization of Lynch Syndrome Universal Tumor Screening , Tara M. Wolfinger
Theses/Dissertations from 2021 2021
Exploring Adult Attachment in Intimate Relationships among Women who Were Exposed to Intimate Partner Violence in Childhood: A Convergent Mixed Methods Approach , Ngozichukwuka C. Agu
Comparison of the Effectiveness of Disinfectant-Impregnated Wipes Versus Detergent Wipes for Surface Decontamination , Jacob Amadin
Limited Point of Care Ultrasound Clinical Decision Support Model for Work-related Injuries of the Shoulder Utilizing Bayesian Network , Gwen Marie Ayers
Synthesis of a Multimodal Ecological Model for Scalable, High-Resolution Arboviral Risk Prediction in Florida , Sean P. Beeman
Feasibility of a Virtual Group Nutrition Intervention for Adolescents with Autism Spectrum Disorder , Acadia W. Buro
Defining Codes Based on the Consolidated Framework for Implementation Research in the Context of the Implementing Universal Lynch Syndrome Screening , Jasmine A. Burton-Akright
Americans’ Familiarity, Interest, and Actions with Direct-to-Consumer Genetic Testing , Riley L. Carroll
Does Better A1C Control Worsen Osteoarthritis? An Electronic Health Record Cross-Sectional Study , Sarah C. Cattaneo
Analysis of Post-traumatic Stress Disorder Gene Expression Profiles in a Prospective, Community-based Cohort , Jan Dahrendorff
Differential Privacy for Regression Modeling in Health: An Evaluation of Algorithms , Joseph Ficek
Does Time-Weighted Averaging for WBGT and Metabolic Rate Work for Work-Recovery Cycles? , John W. Flach
Screening of Pregnant Women with Opioid Use Disorder: Identifying Factors Impacting Implementation of Screening Recommendations Using the Theoretical Domains Framework , Tara R. Foti
Epigenetic Potential in an Introduced Passerine , Haley E. Hanson
Face Mask Use to Protect Against COVID-19; Importance of Substrate, Fit, and User Tendencies , Evelyn Kassel
Novel Educational Material for Patients with a Variant of Uncertain Significance (VUS) in a Cancer Risk Gene , Meghan E. Kelley
Mechanisms and Mitigation: Effects of Light Pollution on West Nile Virus Dynamics , Meredith E. Kernbach
Seasonality in Competence to Transmit West Nile Virus for a Widespread Reservoir , Kyle L. Koller
Mealtimes in Early Childhood Education Centers During COVID-19: A Mixed-Methods Assessment of Responsibilities, Interactions, and Best Practices , Joanna Mackie
Development and Validation of an Isothermal Amplification Assay for Eastern Equine Encephalitis Virus , Mikayla D. Maddison
Evaluating the Development and Implementation of Campus-based Sexual and Interpersonal Violence Prevention Programming , Robyn Manning-Samuels
Bait-and-Kill: Targeting a Novel Heme Biochemical Pathway in Hundreds of Cancers , Christopher G. Marinescu
Acclimatization Protocols and Their Outcomes , Ayub M. Odera
Promoting HPV vaccination with vaccine-hesitant parents using social media: a formative research mixed-method study , Silvia Sommariva
Sleep Diagnoses and Low Back Pain in U.S. Military Veterans , Kenneth A. Taylor
Theses/Dissertations from 2020 2020
Journey Mapping the Minority Student’s Path Toward Genetic Counseling: A Holistic Picture , Tatiana E. Alvarado-Wing
Using Observations from the UAW-Ford Ergonomic Assessment Tool to Predict Distal Upper Extremity Musculoskeletal Disorders , Zachariah T. Brandes-Powell
Do Similar Exposure Groups (SEG) differ from Air Force base to Air Force base? A Combat Arms Training and Maintenance (CATM) noise exposure comparison of Moody AFB and MacDill AFB. , Miriam F. Escobar
Predictors of Premature Discontinuation from Behavioral Health Services: A Mixed Methods Study Guided by the Andersen & Newman Model of Health Care Utilization , Shawna M. Green
Non-invasive Sex Determination and Genotyping of Transgenic Brugia malayi Larvae , Santiago E. Hernandez Bojorge
Does Gestational Diabetes Mellitus Increases the Risk of Preeclampsia Among Primigravid Women? , Astha Kakkad
Evaluating Effects of Cancer Genetic Counseling on Several Brief Patient Impact Measures , Alyson Kneusel
Impact of Heat-Related Illness and Natural Environments on Behavioral Health Related Emergency and Hospital Utilization in Florida , Natasha Kurji
The Quantification of Heavy Metals in Infant Formulas Offered by the Florida WIC Program , Naya Martin
Differences in Knowledge Acquisition, Perceived Engagement and Self-Efficacy in Latino Promotores Delivering the Heart Disease Prevention Program Su Corazόn, Su Vida , Samuel Matos-Bastidas
Spatial and Temporal Determinants Associated with Eastern Equine Encephalitis Virus Activity in Florida , Kristi M. Miley
Using Observations from the UAW-Ford Ergonomic Assessment Tool to Predict Low Back Musculoskeletal Disorders , Colins Nwafor
On the Importance of Context: Examining the Applicability of Infertility Insurance Mandates in the United States Using a Mixed-Methods Study Design , Nathanael B. Stanley
Exploration of Factors Associated with Perceptions of Community Safety among Youth in Hillsborough County, Florida: A Convergent Parallel Mixed-Methods Approach , Yingwei Yang
Theses/Dissertations from 2019 2019
The Ability of the U.S. Military’s WBGT-based Flag System to Recommend Safe Heat Stress Exposures , David R. Almario
The Relationship between Continuous Glucose Monitor (CGM) Derived Metrics and Indices of Glycemic Control , Ryan Bailey
“Man plans but ultimately, God decides”: A Phenomenological Investigation of the Contextual Family Planning Beliefs of Recently Resettled Congolese Refugee Women in West Central Florida. , Linda Bomboka Wilson
‘If He Hits Me, Is That Love? I Don’t Think So’: An Ethnographic Investigation of the Multi-Level Influences Shaping Indigenous Women’s Decision-Making Around Intimate Partner Violence in the Rural Peruvian Andes , Isabella Li Chan
An Assessment of the Role of Florida Pharmacists in the Administration of Inactivated Influenza Vaccine to Pregnant Women , Oluyemisi O. Falope
Epidemiological Analysis of Malaria Decrease in El Salvador from 1955 until 2017 , Tatiana I. Gardellini Guevara
Self-Collected Sampling Methods for Chlamydia and Gonorrhea Screening Among College Women: Exploring Patient-Centered Intervention Characteristics , Stacey B. Griner
The Relationship Between Hand and Wrist Musculoskeletal Disorders and Hand Activity and Posture , Warren M. Henry
Speeding Diagnosis and Saving Money Using Point of Care Ultrasound Rather Than MRI for Work-related MSK Injuries , Jared A. Jeffries
Mitigating Barriers to Chronic Disease Risk Factor Prevention and Management in Disadvantaged Communities , Krys M. Johnson
Comparing Family Sharing Behaviors in BRCA Carriers with PALB2 Carriers , Joy E. Kechik
Investigating Air Pollution and Equity Impacts of a Proposed Transportation Improvement Program for Tampa , Talha Kemal Kocak
Exploring Young Women’s Choice to Initiate Use of Long-acting Reversible Contraception: A Mixed Methods Approach , Helen Mahony
Evaluation of Clinical Practices and Needs about Variants of Uncertain Significance Results in Inherited Cardiac Arrhythmia and Inherited Cardiomyopathy Genes , Reka D. Muller
Effects of Medications with Anticholinergic Properties and Opioids on Cognitive Function and Neural Volumetric Changes in Elderly Australians , Malinee Neelamegam
Sundaas Story: A Mixed-Methods Study of Household Sanitation Provisioning in Urban Informal Housing in India , Sarita Vijay Panchang
A Retrospective Study of the Opioid Epidemic and Fentanyl Related Overdose Fatality Cases in a Florida West Coast Medical Examiner District Population , Anne Terese Powell
Using Predicted Heat Strain to Evaluate Sustainable Exposures , Samantha L. Thacker
Isokinetic Sampling Efficiency Differences for Blunt Edge vs Sharp Edge Sampling Probes , Cory A. Treloar
Using the Consolidated Framework for Implementation Research to Investigate Daily Pre-exposure Prophylaxis (emtricitabine/tenofovir DF) Implementation via Community-based HIV Testing Sites in Florida , Deanne E. Turner
“We can learn some things from them, but they can learn some things from us too”: Intergenerational Perceptions of Shared Infant Feeding Information , Alexis L. Woods Barr
Theses/Dissertations from 2018 2018
Comparison of Modeled and Measured Pesticide Concentrations in Air , Trenell Davis Boggans
Effectiveness of Biocide Substitution and Management Plan Implementation for the Control of , Adelmarie Bones
Design, Construction, and Characterization of the University of South Florida Wind Tunnel , Jason S. Garcia
Characterization of Scanning Mobility Particle Sizers For Use With Nanoaerosols , Michael R. Henderson
Validation of the Thermal Work Limit (TWL) Against Known Heat Stress Exposures , Danielle L. Kapanowski
Validation of a New Concept for Measuring Respirable Dusts , Xiao Liu
Occupational Noise Exposure Evaluation of Airline Ramp Workers , Adekunle Ogunyemi
Reduction in Needlestick Injuries Using a Novel Package of Interventions , Kamal Thakor Patel
Ability of the ISO Predicted Heat Strain Method to Predict a Limiting Heat Stress Exposure , Edgar Prieto
Developing the Evidence Base for Mental Health Policy and Services: Inquiries into Epidemiology, Cost-Benefits, and Utilization , Joseph L. Smith
Occupational Sharps Injuries in Medical Trainees at the University of South Florida: A Follow-up Study , Kourtni L. Starkey
Particles in Welding Fumes , Rebecca T. Williams
Theses/Dissertations from 2017 2017
The Effects of Maternal Folate on Fetal Brain and Body Size among Smoking Mothers , Korede K. Adegoke
The Influence of Tropical Forests and Climate Change on the Fates of Select Organic Pollutants in a Jamaican Watershed , Kayon Barrett
Advanced Search
- Email Notifications and RSS
- All Collections
- USF Faculty Publications
- Open Access Journals
- Conferences and Events
- Theses and Dissertations
- Textbooks Collection
Useful Links
- Rights Information
- SelectedWorks
- Submit Research
Home | About | Help | My Account | Accessibility Statement | Language and Diversity Statements
Privacy Copyright
Public Health/Health Administration Program
During the latter quarter of the 1800s and the first quarter of the 1900s, scientific development, especially in microbiology steered in a novel aspect for the field of public health. This bacteriologic phase of the public health movement was led by the discoveries of Louis Pasteur and Robert Koch and the subsequent ‘germ theory of disease. In his learning, Pasteur revealed aerobic and anaerobic organisms and started to reflect on the likelihood of a causal connection between germs and disease. Koch, a country physician, revealed the bacillus accountable for anthrax and was able to exhibit that the disease was transmissible. This newly discovered germ theory opened the door for new opportunities to control infectious diseases, including developed diagnosis, comprehending the states of carriers, and insight into the importance of vectors for transmission of diseases.
The bacteriologic discoveries of Pasteur and Koch formed a transition between the old and the new public health. The relation between bacteria and disease causation drew attention away from the sanitary problems of water supply, housing, street cleaning as well as living conditions of the poor. In the process, a disease-focused approach to public health became significant for the health officers as well as local health agencies. Due to this growth in the field, I am interested in joining the field and working with health officers to assist the community. Public health may be described as controlling diseases, ensuring a healthy and enhanced life through environmental hygiene as well as enlightening the community on the importance of personal cleanliness and identification of illnesses early enough before they become fatal. Ideally, this is what has attracted me in advancing my studies in public health administration.
My father has been diagnosed with a rare kind of “adenocarcinoma of the stomach” and is likely to undergo an operation soon; doctors say the cause of the disease is unknown. In this context, my nerve has switched to take a master’s in public health to work on the causes of such a rare type of illness. “Hope” and “Miracle” are the 2 words remaining in front of me in this scenario. Hence I am determined to take up a study in public health to determine the environmental causes for such rare disorders.
Academically, I possess a doctorate in Ph.D. Environmental Science and Engineering (Indian Institute of Technology, Bombay) and two master’s degrees in M.Phil. Environmental Science (Bharathiar University) and M.Sc. Environmental Science (P.S.G.College of Arts and Science). I have also volunteered in various organizations and events which have enhanced my leadership skills. These include director in Young Students Movement, eye camps in rotary club, Center for Environmental Education, cultural committee during SPICMACAY convention 2006, and Washington Hospital Health Care Center, Fremont, CA.
As a research scholar, my notable accomplishments include, publication of 4 peer-reviewed research papers in highly reputed international journals, co-authorship in 3 book chapters in the Environmental Engineering bio-series, a lead role in drafting Environmental Status Report for the State of Chattisgarh, India, and contribution to a research proposal for the Department of Biotechnology, Government of India. My research papers also bagged awards for their technical excellence at different conferences held at the national level. I am a life member of the Indian Association of Separation Scientists and Technologists, the Indian Environmental Association, and the Indian Association of Environmental Engineers. In addition, I have experience in teaching, having been a lecturer at Erode Arts College in the department of Microbiology during the years 1999 to 2000 and at Bharathiar University in the Department of Environmental Science during the years 2001 to 2002.
I Chose to intern with the country environmental laboratory to gain experience in the environmental sampling and analysis of priority pollutants (air/water) affecting health and the environment. Development and application of activated carbon from locally available materials (straw, fruit peel) to reduce the concentration of toxic metals (Pb, Cu, Zn & Hg) and priority pollutants (TOC, COD & BOD) in dyeing wastewater was the objective of the project. A team of scientists tested columns with activated carbon on a pilot scale and recommended setting up activated carbon columns for the final polishing of dye effluent in the common effluent treatment plant (CETP) in our country.
With society continuing to grow, there is a need for more public health professionals who can work with the public and communities to address the wide range of community-identified public health problems. Thus there is the steady growth of career in the field of public health which has attracted me to join the field. This career is directed to serve the health and the environment. This will expound my knowledge in the environmental studies that I have undergone, as well as go along with satisfying my soul once I become a public health professional. I have also been attracted by the fact that this field connects science and policy spheres, hence one can holistic ideas about health, environment as well as the laws governing them. The other point of attraction is that the field is diverse and thus will give me the opportunity to communicate to specialists from the science, management, and policy spheres. I am determined to protect health and the environment just as the field is focused on and definite goals for the protection of health and the environment.
My experience in public health administration will help me in pursuing my goals in this program. I am focused, organized, and able to communicate ideas clearly to the people as I have a background in environmental research and knowledge of treatment and handling of priority environmental pollutants. In addition, I can manage multitasking, making me be effective in handling scientific and management issues. Moreover, my administrative ability and experience to serve as the head of the department of microbiology will be helpful in handling teaching and administrative tasks. Nevertheless, I am enthusiastic and looking forward to attaining my dream of becoming a public health professional in your institution.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, April 1). Public Health/Health Administration Program. https://studycorgi.com/public-health-health-administration-program/
"Public Health/Health Administration Program." StudyCorgi , 1 Apr. 2022, studycorgi.com/public-health-health-administration-program/.
StudyCorgi . (2022) 'Public Health/Health Administration Program'. 1 April.
1. StudyCorgi . "Public Health/Health Administration Program." April 1, 2022. https://studycorgi.com/public-health-health-administration-program/.
Bibliography
StudyCorgi . "Public Health/Health Administration Program." April 1, 2022. https://studycorgi.com/public-health-health-administration-program/.
StudyCorgi . 2022. "Public Health/Health Administration Program." April 1, 2022. https://studycorgi.com/public-health-health-administration-program/.
This paper, “Public Health/Health Administration Program”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: April 1, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
SPHHS to Launch Online Master of Health Administration Degree Program in Fall 2025

The University of Massachusetts Amherst School of Public Health and Health Sciences has recently been approved by the UMass Board of Trustees and the Massachusetts Board of Higher Education to offer a new Master of Health Administration program that will be available to students in fall 2025.
In their April 2024 meeting, the trustees approved a Master of Health Administration (MHA), an online degree program in the Department of Health Promotion and Policy. The part-time, online MHA program will be one of the few of its kind offered by a Massachusetts public university.
The curriculum is comprised of 40 credits including core courses in public health (health policy and management), management, strategic management, leadership, graduate seminars and a capstone experience that involves a service-learning case study with the student’s current or prospective place of employment.
Lawrence Pellegrini , director of the Online MPH in Public Health Practice Program and senior lecturer in health policy and management, says the program is designed to be completed in three years for individuals who want to further their education part-time while continuing to work.
“The degree is designed for working professionals looking to acquire needed skillsets to gain leadership positions within the healthcare field,” Pellegrini says. “The program is fully online and asynchronous which offers a great deal of flexibility for students to complete the degree while balancing other responsibilities.”
The program differs from a business school master’s program in health care administration or master’s in business administration because it is within the SPHHS and is public health focused.
“We’re a school of public health,” Pellegrini says. “A lot of the values that we're going to be installing in the context of our program are going to be very much public health-oriented, so there would be a lot of population-based approaches to healthcare innovation.”
Graduates would be prepared for roles as healthcare administrators across industry sectors in businesses, educational institutions, government agencies, non-profit groups, community wellness programs, residential healthcare facilities, hospitals and clinical settings.
Global footer
- ©2024 University of Massachusetts Amherst
- Site policies
- Non-discrimination notice
- Accessibility
- Terms of use
- Share full article
Advertisement
Supported by
Guest Essay
Doctors Need a Better Way to Treat Patients Without Their Consent

By Sandeep Jauhar
Dr. Jauhar is a cardiologist in New York who writes frequently about medical care and public health.
Not long ago, I took care of a middle-aged man at my hospital who had severe heart failure requiring life support. When he was disconnected from machines after a few days of treatment, he began to display psychotic symptoms, including delusional thinking, tangential speech and paranoia. He had a long history of untreated schizophrenia, I learned, which had estranged him from family members and friends, with whom he had virtually no contact.
My patient demanded to leave the hospital. However, sending him home was going to be a problem. He could not take care of himself. There was little chance he would take his medications, including a blood thinner to dissolve a clot in his heart before it caused a stroke. He was even less likely to take psychiatric drugs that he did not believe he needed.
My colleagues and I didn’t know what to do, so we called the treating psychiatrist. The psychiatrist immediately declared that our patient lacked the capacity to discharge himself from the hospital. The patient could not grasp the implications of this choice, for instance, or properly weigh its risks and benefits. The psychiatrist said the patient should remain in the hospital to receive psychiatric treatment, even against his will.
The psychiatrist’s opinion made sense to me. Patients with untreated schizophrenia have a higher rate of death than those who undergo treatment. Hopefully treatment would restore my patient’s judgment to the point where he would take his medications when he went home — or even decide not to take them, but to make that risky decision in the full appreciation of the likely consequences. (If autonomy means anything, it means that patients have the right to make bad decisions, too.) Treating him, even over his objections, seemed to be in his best interests.
However, according to New York law — and the law of other states — such involuntary treatment would require a court order. As doctors, we would have to plead our case before a judge. But was a judge without medical or psychiatric expertise the best person to decide this man’s fate?
In this case and also more generally, I think the answer is no. The law ought to be changed to keep such decisions in hospitals — in the hands of doctors, medical ethicists and other relevant experts.
Doctors don’t always have to resort to the courts to treat patients without their consent. There are some notable exceptions, such as during a life-threatening emergency (if a competent patient has not previously refused such treatment) or when there is a pressing societal interest (such as requiring patients with communicable tuberculosis to take antibiotics).
But judicial review has been the cornerstone of “treatment over objection,” as it’s known, for the past four decades or so. Appellate courts in the 1980s ruled that judicial hearings in such cases are needed to safeguard patients’ rights. For example, in 1983, in Rogers v. Commissioner of Department of Mental Health, the Massachusetts Supreme Judicial Court declared that a judge could override medical judgments favoring involuntary psychiatric treatment.
The underlying motivation behind judicial review was and remains laudable: to avoid the sort of paternalistic abuses that have characterized too much of medical history. Doctors often used to withhold bad news from patients, to cite just a small example. Involuntary treatment, even with benevolent intentions, reeks of such paternalism.
But though medical practice is by no means perfect, times have changed. The sort of abuse dramatized in the 1975 movie “One Flew Over the Cuckoo’s Nest,” with its harrowing depiction of forced electroconvulsive therapy, is far less common. Doctors today are trained in shared decision-making. Safeguards are now in place to prevent such maltreatment, including multidisciplinary teams in which nurses, social workers and bioethicists have a voice.
In addition to being less necessary to prevent abuse than they once were, courts are by nature poorly suited for making decisions about treatment over objection. For one thing, they are slow: Having to go to court often results in delays, sometimes up to a week or more, which can harm patients who need care urgently.
Moreover, judges have neither the experience nor the expertise to properly evaluate psychological states, assess decision-making capacity or determine whether a proposed treatment’s benefits outweigh its risks. It is no surprise that by some estimates 95 percent or more of requests for treatment over objection are approved by judges, who invariably haven’t met the patient and must rely on information provided by the treating medical team.
A better system for determining whether a patient should be treated over his or her objection would be a hospital hearing in which a committee of doctors, ethicists and other relevant experts — all of whom would be independent of the hospital and not involved in the care of the patient — engaged in conversation with the medical team and the patient and patient’s family. Having hearings on site would expedite decisions and minimize treatment delays. The committee would make the final decision.
Of course, such a committee would have to be granted immunity from legal liability (as with judges in our current system), so that experts would be willing to serve and speak candidly. Patients’ interests could be safeguarded by requiring the committee to publish its reasoning. Periodic audits by a regulatory body could ensure that the committee’s deliberations were meeting medical and ethical standards.
In the event that the committee could not reach a consensus on the best course of action (or if there were allegations of wrongdoing), then the parties involved could appeal to a judge. But that would be the exception rather than the rule.
In the case of my patient with heart failure, the decision ultimately didn’t have to go before a judge. Multiple discussions involving the patient, the hospital ethics and palliative care teams, social workers, nurses, psychiatrists and other doctors — discussions that in many respects served the function of a formal committee of the sort I’m proposing — yielded an agreement with the patient that his interests would be best served by sending him home with hospice care.
Capacity must be judged relative to the decision being made, and it became clear over the course of hospitalization that our patient understood the terminal nature of his condition and had the capacity to choose hospice care. Forced treatment was unlikely to significantly improve his psychiatric symptoms before the natural progression of heart failure caused his death.
So he was discharged home. It was the best decision under the circumstances, one reached by expert deliberation, not legal procedure. He passed away a few weeks later without, fortunately, ever setting foot in court.
Sandeep Jauhar ( @sjauhar ) is a doctor at Northwell Health in New York and the author, most recently, of “ My Father’s Brain : Life in the Shadow of Alzheimer’s.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Official websites use .mass.gov
Secure websites use HTTPS certificate
A lock icon ( ) or https:// means you’ve safely connected to the official website. Share sensitive information only on official, secure websites.
- search across the entire site
- search in Department of Public Health
- search in Executive Office of Health and Human Services
- This page, Healey-Driscoll administration awards $1 million to five organizations to address human trafficking, is offered by
- Department of Public Health
Press Release Healey-Driscoll administration awards $1 million to five organizations to address human trafficking
Media contact for healey-driscoll administration awards $1 million to five organizations to address human trafficking, katheleen conti, assistant director of media relations.
Boston — The Healey-Driscoll Administration has awarded $1 million to five organizations to support programs aimed at increasing awareness of human trafficking in Massachusetts and providing outreach and services to those most at risk for being victimized, and people who have experienced trafficking.
Chosen by the Massachusetts Department of Public Health in consultation with the Executive Office of Public Safety and Security, the organizations will implement strategies to raise public awareness about sex trafficking and labor trafficking in Massachusetts, how to recognize a trafficking situation, and how to respond appropriately. The organizations will also focus on connecting with groups at highest risk for trafficking and providing trauma-informed services to survivors.
Each organization will receive a one-time $200,000 grant, effective from July 2024 through December 2026, to support programs and services with demonstrated commitment to racial equity and informed or led by trafficking survivors. The funded organizations are: Children’s Advocacy Center of Suffolk County; RFK Community Alliance’s Legacy Mentoring program; Justice Resource Institute’s My Life My Choice program; RIA Inc.; and the Vietnamese American Civic Association, Inc.
“Human trafficking has a profound and long-lasting impact on those individuals and communities that are often targeted in these crimes of exploitation,” said Governor Maura Healey . “Combatting human trafficking is a priority of our administration, and this funding builds on our efforts to raise public awareness and to invest in programs that support survivors.”
“Whether behind closed doors or in plain sight, human trafficking is pervasive,” said Lieutenant Governor Kim Driscoll , who chairs the Governor’s Council to Address Sexual Assault, Domestic Violence, and Human Trafficking. “Investing in community-based organizations that provide a wide range of services to support survivors, identify victims, and educate the public will strengthen our efforts to combat human trafficking throughout Massachusetts.”
In Massachusetts, the impact of human trafficking has been concentrated on communities and populations that experience a higher burden related to structural racism and economic and social inequities. Traffickers commonly prey on individuals who have low or no income; undocumented immigrants; unaccompanied immigrant children and youth; people of color; homeless and runaway youth; people with limited English proficiency; people with disabilities; members of the LGBTQ+ community; people with substance use disorder; and children and youth who have been involved in the child welfare and/or juvenile justice systems.
“The stigma faced by victims of trafficking, especially sex trafficking, can play a significant role in whether they seek help and how well they can recover from the trauma they have experienced,” said Secretary of Health and Human Services Kate Walsh . “By focusing approaches on groups at higher risk of trafficking and helping connect them with appropriately tailored resources, these community-based supports will strengthen the short- and long-term health and well-being of survivors.”
“Across the nation and here in Massachusetts, human trafficking continues to be a serious public health issue that disproportionately impacts our most vulnerable populations, including those living in poverty, children, and undocumented immigrants,” said Robbie Goldstein, MD, PhD, Commissioner of the Department of Public Health . “Human trafficking is a profound violation of the most basic human rights, steeped in violence and coercion that pushes people into an oppressed existence. Public health can – and must – play a key role in identifying and addressing this complicated and multidimensional problem.”
“This grant funding supports the crucial work of community service providers in aiding survivors as they heal and rebuild their lives,” stated Secretary of Public Safety and Security Terrence Reidy . “Forming strong partnerships is key to combating this heinous crime and ensuring everyone’s right to live with dignity, respect, and without fear of abuse.”
In Massachusetts, sharing a border with five states and only a short drive to an international border is conducive for organized trafficking rings that move their victims frequently. Some industries that can lead to trafficking include construction, food, gaming, and commercial fishing. For some immigrants, a combination of factors can make them especially vulnerable to trafficking, including low or no English proficiency, low or no income, inability to work legally, and a lack of familiarity with public systems and benefits.
Data around the prevalence of sex and labor trafficking are known to be unreliable, as they depend on victims overcoming a climate of fear and self-identifying or being identified and assisted by someone in health care, law enforcement, or social services. One barometer is the National Human Trafficking Hotline , (888) 373-7888. In 2021 , the hotline received 339 reports from Massachusetts, 134 of which were from victims or survivors of human trafficking and resulting in the identification of 93 cases involving a total of 143 victims. Seventy-two of those cases involved sex trafficking.
Funding for this grant program was authorized by Chapter 268 of the Acts of 2022.
Last year, the Healey-Driscoll administration expanded the scope of what was formerly known as the Governor’s Council to Address Sexual Assault and Domestic Violence to include human trafficking, given the severity and prevalence of the crime in Massachusetts. The council is now called the Governor’s Council to Address Sexual Assault, Domestic Violence, and Human Trafficking.
Department of Public Health
Help us improve mass.gov with your feedback.
The feedback will only be used for improving the website. If you need assistance, please contact the Department of Public Health . Please limit your input to 500 characters.
Thank you for your website feedback! We will use this information to improve this page.
If you need assistance, please contact the Department of Public Health .
If you would like to continue helping us improve Mass.gov, join our user panel to test new features for the site.
About Us | Contact Us | Newsroom
Primary Care Office
The Primary Care Office (PCO) improves access to primary healthcare for medically underserved areas and populations. The office is funded through an annual grant from the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA) . Through outreach and partnerships, the PCO works to identify and reduce barriers to primary healthcare.
Services and Activities
- Health Professional Shortage Area (HPSA) Designation
- Healthcare Access Reports
- J-1 Visa Waiver Program
- Direct recruitment
- National Health Services Corps eligibility assistance
- Application assistance to federally qualified health center grants
- Consult on community planning resources for providers, county health departments and other groups
- Advocate for resources that promote access for medically underserved populations
- The Washington Association for Community Health is the state's primary care association. The association represents Washington's federally qualified health centers and works with the PCO to increase access to medical, dental and mental health.
- The Washington Healthcare Access Alliance (WHAA) works to strengthen the healthcare safety net in partnership with others. WHAA also functions as the state association for free clinics in Washington.
- The Area Health Education Center for Western Washington (AHECWW) in partnership with WHAA generate the Washington State Primary Care Needs Assessment (PCNA) , an overview of primary care capacity in Washington state.
Federally qualified health centers (FQHCs), also known as community health centers (CHCs), are facilities that receive funds from the HRSA Health Center Program to provide primary care services in underserved areas. These facilities are in both rural and urban settings and serve Washington residents regardless of their ability to pay.
A complete list of community health centers and FQHCs in the state along with a current map is on the Washington Association for Community Health website.
At the Department of Health, the Primary Care Office has a specific mission to support FQHCs and is able to provide technical assistance in a variety of areas.
For more information on Federally Qualified Health Centers, see What Is a Health Center ?
The Department of Health works in partnership with the U.S. Health Resources and Services Administration (HRSA) to identify geographic areas, populations and facilities experiencing a shortage of health care services. These designations are called Health Professional Shortage Areas (HPSA). HPSAs may be designated as having a shortage of primary medical care, dental or mental health providers. Each designation is assigned a HPSA score based on the analysis of survey data collected from providers and standardized national data sets. State and federal programs use these designations to determine eligibility for payment enhancements and workforce incentive programs. For more information, see What is a Shortage Designation ?
HPSA designations are available for three different disciplines of non-specialized health care:
- Primary medical care
- General dental care
- Mental health care
There are three general types of HPSAs designations:
Additional Resources
- Why are HPSAs important? See Which federal programs use HPSAs
- How does the HPSA application process work? See Reviewing shortage designation applications
- How are HPSA scores determined? See Scoring shortage designations
- Want to know if your location is in a shortage area? See Find shortage areas .
The Office of Community Health Systems manages the shortage designations for Washington state, under the Primary Care Office Agreement with HRSA. The Overview of Federal Health Professional Shortage Areas and Underserved Designations (PDF) discusses the program in more detail. We also maintain generalized mapping of our state's designated areas and produce high-level county Healthcare Access Reports that may be useful to those interested in healthcare access issues. For more information, see our Data, Maps and Other Resources page .
For more information about the HPSA designations, contact the Office of Community Health Systems .
Medically Underserved Areas/Populations (MUA/P) are geographic areas or populations designated by the Health Resources and Services Administration (HRSA) as having a lack of access to primary care services. These designations are a prerequisite to requesting grant awards to help establish health maintenance organizations or community health centers under section 330 of the Public Health Service Act. For more information, see What is a Medically Underserved Area/Population? :
- Which federal programs use MUA/Ps ?
- How do I request a new or update to an existing MUA/P ?
- How are MUA/P Scores calculated ?
- What to know if your location is in a MUA/P ?
The Office of Community Health Systems manages these designations for Washington state, under the Primary Care Office Agreement with HRSA. The Overview of Federal Health Professional Shortage Areas and Underserved Designations (PDF) discusses the program in more detail. We also maintain generalized mapping of our state's designated areas. For more information, see our Data, Maps and Other Resources page .
For information about MUA/P designations contact the Office of Community Health Systems .
Back to top
Contact and Connect
Contact our office | Subscribe to our topic to receive Rural Health updates .
- Care-a-Van Mobile Health Services
- Disability Organizations
- Drug User Health
- Food Safety
- Healthy Aging
- Healthy Home
- Illness and Disease
- Immunization
- Infants and Children
- Injury and Violence Prevention
- Men's Health
- Nutrition and Physical Activity
- Oral Health
- Poisoning and Drug Overdose
- Sexual and Reproductive Health
- Adolescents & Young Adults
- Women's Health
- Air Quality
- Climate and Health
- Contaminants
- Drinking Water
- Essentials for Childhood Initiative
- Health Equity
- Healthy Communities Washington
- Wastewater Management
- Water Recreation
- Worksite Wellness
- Facilities - New, Renew or Update
- File Complaint About Provider or Facility
- Healthcare Enforcement and Licensing Management System (HELMS)
- Healthcare Professional Credentialing Requirements
- Medical Commission
- Board of Nursing
- Professions - New, Renew or Update
- Provider Credential Search
- Veterans, Service Members and their Families
- Vital Records
- Data Guidelines
- Data Systems
- Data Topics A-Z
- Diseases and Chronic Conditions
- Environmental Health
- Health Behaviors
- Health Statistics
- Healthcare in Washington
- Injury Violence and Poisoning
- State Health Assessment
- Washington Tracking Network (WTN)
- Health and Safety Alerts
- Emergency Contacts and Numbers
- Bioterrorism and Terrorism
- Emergency Information for Specific Groups
- Get Ready for an Emergency
- Severe Weather and Natural Disasters
- Clinical Laboratory Reporting
- Emergency Medical Services (EMS) Systems
- Emergency Preparedness
- Healthcare Professions and Facilities
- Lactation and Infant Feeding-Friendly Environments
- Notifiable Conditions
- Public Health Laboratories
- Public Health System Resources and Services
- Rural Health
- Tribal Public Health and Relations
- Washington Health Alert Network
New Biden rule protects privacy for women who get abortions
- Medium Text

Sign up here.
Reporting by Ahmed Aboulenein; Editing by Andrea Ricci and Himani Sarkar
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab

Thomson Reuters
Washington-based correspondent covering U.S. healthcare and pharmaceutical policy with a focus on the Department of Health and Human Services and the agencies it oversees such as the Food and Drug Administration, previously based in Iraq and Egypt.

World Chevron

Police called in as protesters take building at University of California, Irvine
Pro-Palestinian protesters occupied a building at the University of California, Irvine, on Wednesday, leading university officials to call in multiple police agencies, cancel classes and advise people on campus to shelter in place, a university spokesperson said.

- Skip to main content
- Keyboard shortcuts for audio player
The clock is ticking to fix Social Security as retirees face automatic cut in 9 years

Scott Horsley

Social Security's finances have improved slightly in the last year. But benefits are still facing an automatic cut in less than a decade unless Congress takes steps to prop up the program. Kevin Dietsch/Getty Images hide caption
Social Security's finances have improved slightly in the last year. But benefits are still facing an automatic cut in less than a decade unless Congress takes steps to prop up the program.
Congress has less than a decade to fix Social Security before the popular program runs short of cash, threatening a sharp cut in benefits for nearly 60 million retirees and family members, according to a government report released Monday.
The report from Social Security trustees predicts the retirement program's trust fund will be exhausted in November of 2033. At that point, benefits would automatically be cut by 21%, unless lawmakers adopt changes before then.
There's some good news in the new forecast. Thanks to higher-than-expected worker productivity and a decline in expected disabilities, Social Security isn't burning through cash as fast as trustees predicted a year ago.

Many baby boomers own homes that are too big. Can they be enticed to sell them?
Still, the long-term demographic challenges haven't gone away. A growing number of baby boomers are collecting benefits, while there are fewer people in the workforce paying taxes for each retiree. Given today's low birthrates, that mismatch is not expected to change for decades, although a surge in immigration helps.
Proposed fixes
Congress could fix the problem by raising taxes that support Social Security, reducing retirement benefits, or some combination of the two. But a politically palatable solution has been elusive.
"When you see the two major candidates running for president tripping over themselves to promise what they won't do to fix the problem, you have to worry because those kinds of reforms really start at the top," says Maya MacGuineas, president of the Committee for a Responsible Federal Budget.
The Biden administration has pledged not to touch Social Security benefits.
"Seniors spent a lifetime working to earn the benefits they receive," Treasury Secretary Janet Yellen, who leads the trustees, said in a statement . "We are committed to steps that would protect and strengthen these programs that Americans rely on for a secure retirement."

Campus protests over the Gaza war
Top companies are on students' divest list. but does it really work.
Congressional Democrats have proposed higher taxes on the wealthy to support Social Security. Congressional Republicans have balked at that, instead calling for reducing the benefit formula and raising the retirement age for younger workers.
"Those who want to cut Social Security couch it in affordability," says Nancy Altman, who heads the advocacy group Social Security Works. "But of course, there's no question we can afford it. It's really a question of values. And as polarized as we are, we're not polarized over this."
Altman is confident that lawmakers will find a solution before automatic cuts take effect.
"If they didn't act, not only would they all be voted out of office," she says, "they couldn't even remain in Washington. They'd be chased down the street."
But the clock is ticking and delay has already been costly.

Fake Botox has sickened patients nationwide. Here's what to know — and what to avoid
"Every year the trustees warn us we have to make changes, and the sooner we make them, the better and easier it will be," says MacGuineas. "And every year we fail to make those changes."
Medicare and disability solvency
While Social Security's retirement program is in danger of running short of cash, a separate program that supports disabled people appears to be solvent for the long term, trustees said.
Medicare's finances have also improved somewhat in the last year, thanks to a strong economy and lower-than-expected spending. Still, the program, which provides health care for nearly 67 million people, is expected to face its own cash crunch in 2036.
- Social Security
- payroll taxes
- U.S. economy
83 Healthcare Administration Essay Topic Ideas & Examples
🏆 best healthcare administration topic ideas & essay examples, ✍️ healthcare administration essay topics for college, 📌 good essay topics on healthcare administration, 💡 simple & easy healthcare administration titles.
- Emergency Action Plan: Occupational Safety and Health Administration Company Name: Company Name. Company Contact: Name: Your Name Title: Position Telephone/Cell: Email: In the event of an emergency, employees are alerted by:
- Artificial Intelligence in Healthcare Administration The key stakeholders in addressing healthcare inefficiencies in the administrative processes include the government, hospital administrators and the direct-patient contact staff.
- Job Demands in Canadian Health Services Office Administration Currently, relevant job demands in the modern field of Canadian office administration of health services pose considerable challenges for newcomers to the industry.
- Gender and Leadership in Healthcare Administration The authors were studying the challenges that the female gender face in healthcare leadership. The authors concluded that gender inequality in management could not be affected by the type and size of the hospital.
- Administration Errors in a Mental Health Hospital The selection of a representative group from the population of interest is among the prerequisites for the production of reliable and generalizable results.
- Silica Exposure and Occupational Safety and Health Administration In this research, the main focus is to investigate whether the exposure rate on a worker at the Iron Foundry is above the set standard by the OSHA.
- Healthcare Administration: The Role of Information Technologies Sometimes people can use the OR and AND tools to calculate the probability. In addition to probability, Excel allows people to calculate measures of the central tendency.
- The Job of Health Care Administration or Executive Assistance In terms of the contributions of the course to the development of the professional experience for the position, such areas as decision-making and problem-solving were especially relevant.
- Career Development in Healthcare Administration The institution provides regular training to the members and updates the current trends that are witnessed in the healthcare sector. Second, The American Society for Healthcare Human Resources Administration is a website that helps in […]
- ACOs in Healthcare Administration As part of the Medicare and Medicaid program, the main goal of coordinated care is to optimize services by reducing duplication of services and improving care timeliness.
- Amazon’s Occupational Safety and Health Administration The story of one of the Amazon workers presents the company as a firm that does not value ethics in its strategic scheme. It is a matter of ethics to prioritize the employee’s well-being and […]
- Healthcare Administration: The Legal Aspects The essence of this study is to evaluate and assert the usefulness and the advantage of using case studies in teaching legal aspects in healthcare administration.
- Health Administration: Ethical and Legal Perspectives The HIPAA’s primary role was established in order to give people the authority to share their personal medical information, and again gain more accessibility of information about their health status healthcare.
- Legal Aspects of the US Health Care Administration Limiting or revoking the privileges of a medical practitioner is the extreme disciplinary step taken by the medical staff leaders of hospitals in USA.
- Aspects of Health Care Administration In most cases, the role of the administrator in a medical facility is to oversee and ensure the smooth sailing of the medical institution.
- U. S Public Health Administration The public health budget process is an important tool for governments in mobilizing resources that are needed for health, in the implementation of health-based policies and in the provision of quality health services that is […]
- US Public Health Administration While aspects of identification and curing of various kinds of diseases are surely within the agenda of public health, this is not its main task, which, in its broadest scope would embrace, preventive and protective […]
- US Public Health Public Health Administration If a catastrophic disaster occurs, public health staff are needed in terms of quantity and quality therefore, the US government has come up with initiatives to deal with the above.
- The Substance Abuse and Mental Health Services Administration’s Center Substance abuse and mental health services administration has a well-established principle of collaborating with public and private partners so as to provide the most effective services to the needy people within the society.
- Applications for Health Care Administration Finally, there is a need to build a simple but robust network infrastructure within the hospital that will not only allow the above three systems to operate collectively, but also prepare the hospital for future […]
- Finding a Job in the Healthcare Administration Field Following the recommendations, looking for new openings, and continuously working on skills and knowledge improvement can lead one to a good position in healthcare administration.
- Veterans Health Administration Integrative Care Model The purpose of the following study is to provide a thorough research on the influence of the practices conducted on mental health and to examine the overall effectiveness of the integrative care system in delivering […]
- Healthcare Organization’s Strategic Administration To cater to the needs of the population and react to the external and internal fluctuations of the environment, the company has to enhance the quality of the provided services and create a favorable environment […]
- Health and Human Services Administration Master’s Program In this section, I will discuss some of the reasons why I think I am best-placed in my career and the areas I need to sharpen my metrics.
- Health Administration Instructor’s Teaching Philosophy The US labor statistics show that health care is one of the most rapidly developing fields that accounts for the fact that it provides a huge variety of opportunities and options to build a career.
- Business Administration in the Healthcare Field Precise and states the objectives of the hospital, the market segment that it intends to serve, and how it intends to serve it.
- Health Administration Course and Lessons Learnt In this paper, I will present my reflections on the module assignments to identify the areas that I excelled in and those that I need to improve on.
- “Legal Aspects of Healthcare Administration” by George Pozgar In the context of healthcare, information management can be described as the maintenance of records containing the confidential data of patients and medical workers.
- Veteran Health Administration Program The hospital seems to offer quality care to patients, and one of the studies done showed that patients with diabetes got more care than in other health care systems.
- Occupational Safety and Health Administration In population, the mental state of people that arises from the need of space in excess of the available supply is referred to as crowding.
- Legal Aspects of US Healthcare System Administration Professional conduct within a health care setting is grounded in values that reflect the nature and the dynamics of the relationships between a provider and a patient.
- Veterans Health Administration in Northern California The organization mentors and monitors its employees using the best Performance Management System. The healthcare facility has hired the right supervisors and managers to monitor the system.
- Veteran Health Administration: Electronic Systems It is from such sessions that the staff will get a chance to learn from individuals who have prior significant experiences as well as knowledge in their areas of specialization.
- Veterans Health Administration System Development Lifecycle Evidence in support of this is identified in the GAO report which highlights the fact that despite spending large sums on money and time on the VA project implementation is yet to be done on […]
- Mental Health Administration With the increased number of cases, the government opted to have a policy that would see the proper administration of the condition; this lead to the formation of the Substance Abuse and Mental Health Services […]
- Healthcare Administration: Foreign Trade Commission The role of FTC is to ensure effective law enforcement on consumer interests by provision and sharing of its expertise with the federal state, international agencies and the legislative body in the US.
- Effects of Globalization in Health Care Administration In this regard, it fronts considerable challenges to the healthcare sector in the realms of administration and service provision. It is crucial to understand the provisions of globalization and how they affect the healthcare administration.
- Legal Aspects of Healthcare Administration This essay looks at the case of Terri Schiavo and the ethical issues that arose from it, the definitions used to judge cases similar to it from a bioethics perspective and it will attempt to […]
- Ethics in Health Administration The first group focuses on the issues that revolve around making of ethical decisions as well as the universal issues that have a bearing on ethics.
- Ethics in Health Administration: Four Principles of Autonomy For this reason, the role of the healthcare administrator will be to ensure that all the physicians in the organizations respect the choices made by the patients regarding treatment and other important factors pertaining the […]
- Business Administration in Healthcare Field The difference in the human perception of 3D and 2D images that calls for 3D image processing is the major focus of development in the field of informatics.
- The Evolution of Healthcare Administration
- The New Healthcare Administration: How They Drive Diversity?
- General Healthcare Administration Positions
- Global Human Resource Management in the Healthcare Administration
- Career Outlook of Health Administrators
- The Educational Requirements for Healthcare Administration
- International Finance for Healthcare Administration in the United States
- Analysis of the Professional Development Plan Healthcare Administration
- Ethical Diligence in Healthcare Administration
- Work Environment of Health Administrators
- Plans and Features of Healthcare Administration in the United State
- Useful Professional Associations in Healthcare Administration
- The Role of Stakeholders and Community Assessment in Health Nursing Collaboration between community health nurses and community stakeholders as well as community resource assessment can help nurses promote population health.
- Healthcare Management vs. Administration: Key Differences
- The Organizational Behavior of Healthcare Administration
- Changing From Legal Practice to Healthcare Administration
- Healthcare Administration for Patient Safety and Engagement
- System Planning and Control: Health Administration
- Dismissal of Healthcare Administration Employees
- How to Manage the Healthcare Administration in Real Life?
- Pros and Cons of the New Master’s Program in Healthcare Administration
- Queueing System Analysis of Healthcare Administration
- Marketing Strategies and Recommendations for Healthcare Administration
- Factors Affecting the Activities of Healthcare Administration
- Skills That Can Help Improve Work in Healthcare Administration
- The Current Corporate and Global Strategies of Healthcare Administration
- Past and Present in Healthcare Administration
- Law, Ethics, and Policy in Healthcare Administration
- Organizational Behavior and Culture Change at Healthcare Administration
- Sources of Income in the Healthcare Administration: How They Can Affect the Work of Employees
- Healthcare Administrators: Roles and Responsibilities
- Debunking Misconceptions About Healthcare Administration Roles
- The Future of Healthcare Administration
- The Realities of Healthcare Management: What Can Go Unnoticed?
- Healthcare Administration: A Combination of Theory and Practice
- What Is the Role of Information Technology in the Healthcare Administration?
- Stress and the Hospital Administrator: Sources and Solutions
- Technological Advancements in Healthcare Administration
- View of Hospital Administration as a Profession
- Success Factors and Leadership Strategies Healthcare Administration
- The Fundamentals of Healthcare Administration: Navigating Challenges and Coordinating Care
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 27). 83 Healthcare Administration Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/healthcare-administration-essay-topics/
"83 Healthcare Administration Essay Topic Ideas & Examples." IvyPanda , 27 Feb. 2024, ivypanda.com/essays/topic/healthcare-administration-essay-topics/.
IvyPanda . (2024) '83 Healthcare Administration Essay Topic Ideas & Examples'. 27 February.
IvyPanda . 2024. "83 Healthcare Administration Essay Topic Ideas & Examples." February 27, 2024. https://ivypanda.com/essays/topic/healthcare-administration-essay-topics/.
1. IvyPanda . "83 Healthcare Administration Essay Topic Ideas & Examples." February 27, 2024. https://ivypanda.com/essays/topic/healthcare-administration-essay-topics/.
Bibliography
IvyPanda . "83 Healthcare Administration Essay Topic Ideas & Examples." February 27, 2024. https://ivypanda.com/essays/topic/healthcare-administration-essay-topics/.
- Workplace Health Essay Topics
- Nursing Theory Questions
- Pharmacy Research Ideas
- The Help Paper Topics
- Genetics Research Ideas
- Heart Failure Titles
- Blood Pressure Ideas
- Career Ideas

IMAGES
VIDEO
COMMENTS
In this guide, we'll cover the nuts and bolts of how to write a standout personal statement for your MPH application. We'll help you understand what your personal statement should include and how to tackle the writing process. Plus, we'll show you a real-life example essay and break down why it works.
Sample Essays. The Public Health Student. What if people lived healthier lives, practiced preventive medicine, and took precautions against illness and disease? My days in the physical therapy department often made me think about the prevention of injuries as well as the injuries themselves. I was already doubting my future career choice as a ...
The public health budget process is an important tool for governments in mobilizing resources that are needed for health, in the implementation of health-based policies and in the provision of quality health services that is equitable and efficient. This essay explains why the budget process is complex and time-consuming, giving qualities of a ...
Public health administration is a career worth pursuing since it is challenging and exposes learners to various health issues including disease prevention, management and treatment. Secondly, it accommodates all other careers including law, education, management and research, therefore, making it a dynamic career that widens an individual's ...
clinical care: prevention, treatment, and management of illness and the preservation of mental and physical well-being through the services offered by medical and allied health professions; also known as health care. determinant: factor that contributes to the generation of a trait. epidemic or outbreak: occurrence in a community or region of ...
For example, the US Bureau of Labor Statistics (BLS) notes that the median annual salary for medical and health services managers - the job category under which public health administration falls - was $101,340 in 2021 [ 2 ]. Glassdoor, meanwhile, puts the average annual pay for public health administrators at $71,172 [ 3 ].
Responding to Disarray. The Future of Public Health provided the public health community with a common language and a focus for reform, and progress has been made. In Washington, Illinois, and Michigan, for example, revisions of the state public health codes resulted in the inclusion of mandatory provisions for funding and the distribution of services to all communities "no matter how small ...
Essays for graduate study cover a myriad of topics. Here at SPIA, we hope our essays help reflect and speak to our culture, our community, and our values—the stuff we care about. We require a variety of essays and short answer written responses, and each serves a slightly different purpose toward helping us to understand the academic and professional trajectory of each person as well as the ...
Writing serves as a useful skill for anyone in the field of public health — students and professionals alike. Public health students must enroll in writing-intensive courses that require essays and research papers. Once students graduate, they put their skills to use writing reports on community health. They may compose presentations, research studies, or press ...
Thesis. A thesis is a substantive and original body of work that allows the student to synthesize and integrate knowledge from their public health course work and practicum experiences, apply it to a particular topic area, and communicate their ideas and findings through a scholarly written product. The thesis represents the culmination of the student's educational experience...
ESSAYS ON PUBLIC HEALTH INSURANCE ABSTRACT Over the last ten years there have been dramatic changes in the health insurance environment in the United States, spurred on by broad reforms in the public health insurance sector. In 2006 the Medicare Prescription Drug, Improvement and Modernization Act went into
Sample Personal Statement. As I reflect back on my path to health administration, one word defines my journey: perseverance. Whether in my personal or professional life, I have been faced with situations that required a high level of focus, hard work, and maturity to see them through. These experiences first led me to healthcare administration ...
public health, the art and science of preventing disease, prolonging life, and promoting physical and mental health, sanitation, personal hygiene, control of infectious diseases, and organization of health services.From the normal human interactions involved in dealing with the many problems of social life, there has emerged a recognition of the importance of community action in the promotion ...
According to the Institute of Medicine's well-known 1988 study, The future of public health, the core functions described below are carried out primarily by government and constitute the most critical foundations of an effective public health system. Assessment. The assessment function of public health can be viewed as "knowing what needs to be done."
The CDC Foundation defines public health as "the science of protecting and improving the health of people and their communities." 1. When we think about the word "health," we typically associate it with medical matters, so the definition of public health can seem a little confusing. Unlike the practice of medicine in clinical settings ...
Get custom essay. In summary, I chose public health because it aligns with my values of social justice and equity, offers interdisciplinary collaboration, provides opportunities for tangible impact, presents a global perspective, and embraces the constant evolution of the field. Public health offers me the platform to address pressing health ...
Koop, C. (2004).Reducing the health consequences of smoking 25 years of progress: Report of the Surgeon General.Darby, PA: Diane Publishing. McLean, R. (2002) Financial management in Health care Organizations Boston, MA: Cengage Learning Morrinson, R. (1973) Inflation can be stopped: what is inflation, its history in the US, its various causes, incorrect beliefs about it, how it can be stopped ...
Theses/Dissertations from 2022. PDF. Outcomes of a Periodic Exposure Assessment of Workers at a University Campus, Logan M. Armagast. PDF. Evaluating the Effect of Public Health Governance Structure and Public Opinion on COVID-19 Disease Control Interventions, Daniel Chacreton.
Change management helps people to change their behaviors, attitudes, and/or work processes to achieve a desired business objective or outcome. • Change management as a discipline includes the processes, tools, and techniques used to manage the human elements of change which are applied at the individual, project, and organizational level ...
Health care administrators must not only concern themselves with the patients, but with their staff as well. Consider choosing a staff management or development topic for your doctoral dissertation. You might consider topics such as: The effect of tuition reimbursement policies on staff turnover/retention rates.
Ideally, this is what has attracted me in advancing my studies in public health administration. ... As a research scholar, my notable accomplishments include, publication of 4 peer-reviewed research papers in highly reputed international journals, co-authorship in 3 book chapters in the Environmental Engineering bio-series, a lead role in ...
The University of Massachusetts Amherst School of Public Health and Health Sciences has recently been approved by the UMass Board of Trustees and the Massachusetts Board of Higher Education to offer a new Master of Health Administration program that will be available to students in fall 2025.. In their April 2024 meeting, the trustees approved a Master of Health Administration (MHA), an online ...
Guest Essay. How to Treat a Patient Without His Consent. May 13, 2024. Video. ... Dr. Jauhar is a cardiologist in New York who writes frequently about medical care and public health.
Boston — The Healey-Driscoll Administration has awarded $1 million to five organizations to support programs aimed at increasing awareness of human trafficking in Massachusetts and providing outreach and services to those most at risk for being victimized, and people who have experienced trafficking.. Chosen by the Massachusetts Department of Public Health in consultation with the Executive ...
The final conclusion to this study. The controversy surrounding public-private collaborations or partnerships notwithstanding, it is believed that such partnerships are indispensable in current scenarios, where one party on its own, cannot take up major initiatives without the active technical, commercial and administrative support skills of other players.
The Primary Care Office (PCO) improves access to primary healthcare for medically underserved areas and populations. The office is funded through an annual grant from the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA). Through outreach and partnerships, the PCO works to identify and reduce barriers to primary healthcare.
U.S. President Joe Biden's administration issued a final rule on Monday aimed at strengthening privacy protections for women seeking abortions that bans the disclosure of protected health ...
Lykos sponsored the clinical trials of MDMA. The results are included in the company's application to the FDA seeking approval to market the drug for therapy-assisted PTSD treatment. Researchers ...
Congress has less than a decade to fix Social Security before the popular program runs short of cash, threatening a sharp cut in benefits for nearly 60 million retirees and family members ...
Artificial Intelligence in Healthcare Administration. The key stakeholders in addressing healthcare inefficiencies in the administrative processes include the government, hospital administrators and the direct-patient contact staff. We will write. a custom essay specifically for you by our professional experts.