
Breech presentation
Sep 09, 2012
950 likes | 4.78k Views
Breech presentation . Breech presentation or podalic :-. when buttock of fetal occupies the lower segment of uterus, it is called breech presentation. Breech presentation occurs in 3-4% of all deliveries . Types of breech :- 1. Full/Complete Breech (cannonball position) (5-10%)
Share Presentation
- localization
- shoulder arrest
- sacro posterior
- inferior angle
- ill define outline
- delay progress

Presentation Transcript
Breech presentation or podalic:- when buttock of fetal occupies the lower segment of uterus, it is called breech presentation. Breech presentation occurs in 3-4% of all deliveries • Types of breech:- • 1. Full/Complete Breech (cannonball position) (5-10%) • 2. Incomplete Breech • 3. Frank Breech (pike position) (50-70%) • 4. Footling Breech (10-30%)
Types of breech:- • 1. Full/Complete Breech:- arms & legs flexed • 2. Incomplete Breech • 3. Frank Breech:- arms flexed but legs extended straight up over head • 4. Footling Breech:- one or both feet extended downward and may exit the birth canal first.
Lie:- • Longitudinal • Presentation:- • Breech • Denominator:- • Sacrum
The positions are:- • Left sacro-anterior(LSA) – commonest • Right sacro-anterior (RSA) • Left sacro- posterior(LAP) • Right sacro-posterior (RSP)
Etiology: • Prematurity(due to rotation) commonest • Factor preventing spontaneous version: -- - Breech with extended legs - Twin - Oligohydramnios - Congenital malformation of uterus; septate uterus, Bicornuate uterus - Short cord - Contacted pelvis
Favorable adaptation: - Placenta praevia - Contracted pelvis • Undue mobility of fetus - Hydrocephalus - Multipara with lax abdomen
Recurrent breech:- Recurrent breech means more than 3 consecutive breech pregnancy. Causes:- • Congenital malformed uterus • Contracted pelvis • Cornual attachment of placenta
DIAGNOSIS: • History:- -Previous breech presentation. • Abdominal examination:- - Fundal grip:-hard, round ballottable head. - Lateral grip:- fetal back on one side palpable as smooth curve structure whereas limbs on other side felt small irregular structure. - Pelvic grip: broader, softer and irregular mass with ill define outline. - Fetal heart sounds: above the umbilicus - before engagement , below the umbilicus after engagement.
P/V examination:- -During pregnancy:- soft and irregular part are felt. -During labour:- palpation of ischial tuberocities, sacrum and its spine, sole of foot, genitalias and anus. • Investigations:- - USG:- confirmatory.
VAGINAL EXAMINATION Presenting parts: Complete breech presentations: palpation of ischial tuberocities, sacrum and its spine, sole of foot, genitalias and anus.
Frank breech presentation: palpation of ischial tuberocities, sacrum and its spine, genitalias and anus.
Footling presentations palpation of sole of foot
USG: • Confirm the diagnosis • Detect the gestational age and weight of baby • Detect the fetal congenital abnormalities • Detect the uterine anomalies • Localization of placenta • Liquor • Attitude of the fetus X-ray abdomen
Management of breech • Antenatal management • Management at term • Management during labour
A. Antenatal management:- • Identification of the complicating factors. • External cephalic version- if not contraindicated, at 32-34 wks. • If fails, repeat version after 1 wk.
B. Management at term:- • Planning the method of delivery. • Elective caesarean section when indicated • Vaginal breech delivery when indicated.
Criteria/indication for vaginal breech delivery or caesarean section
C. Management during labour:- First stage:- • Bed rest in left lateral position to prevent early rupture of membrane and cord prolapse. • If normal progress:- liquid diet • If delay progress/cs:- nothing per oral. • Adequate parenteral nutrition • Vaginal examination should be perform only when the membrane ruptures to exclude cord prolapse. • Adequate sedation and analgesia to prevent premature bear down.
Second stage:- Three types of vaginal breech deliveries are described, as follows: 1. Spontaneous breech delivery: 2. Assisted breech delivery: 3. Breech extraction:
Spontaneous breech:- • The expulsion of fetus occurs with very little assistance other than support of the fetus. • This method should not be encourage.
2. Assisted breech delivery:- • The delivery of the foetus is by assistance from the beginning to the end. • The patients buttocks are brought to the edge of table and legs on lithotomy position. She is catheterized by sterile plastic catheter. • Liberal medio-lateral episiotomy is done at crowning of buttocks under 1%xylocaine analgesia. • Baby is allowed to delivered by its own up to umbilicus. • Subsequently the shoulder is crowned on contraction and released posterior arm followed by anterior arm.
3. Breech extraction:- • When the entire body of foetus is extracted by the obstetrician with minimal aid from the mother in an emergency situation such as foetal distress.
Delivery of after coming head in vaginal breech delivery The following are common methods in use:- • Burn- Marshall method • Forceps delivery • Jaw flexion and shoulder traction (Mauriceau - Smellie - Veit technique)
Burn- Marshall method:- • Baby’s trunk is allowed to hang by its own for a while (never for more than 1 minute). • When the nape of the neck is visible under the pubic arch, baby’s trunk is gradually lifted up and swing up towards mother’s abdomen by holding baby’s legs above the ankles, thus head is delivered. • Meanwhile, the left hand to guard the perineum.
Forceps delivery:- • Forceps can be used as a routine and considered as best method if there is skilled person. • Baby is lifted up by the assistance by grasping baby’s ankles. • Forceps is applied from below the trunk off baby on baby’s head at level of biparietal diameters. • Head is gently delivered with mouth appearing at vulva when mouth is aspirated by mucus sucker.
Jaw flexion & shoulder traction (Mauriceau - Smellie - Veit technique) • Head lying above the pelvic outlet. • The baby is placed on the supinated left forearm with the limbs hanging on either side. • The middle and index finger of the left hand are placed over the malar bones on either side. This maintains flexion of the head. • The ring and little fingers of the pronated right hand are placed on the baby’s right shoulder, the index finger is placed on the left shoulder and the middle finger is placed on the sub-occipital region.
5. Traction is now given in downward and backward direction till the nape of neck is visible under the pubic arch. The assistance gives supra pubic pressure during the period to maintain flexion. 6. There after, the baby is carried in upward and forward direction towards the mother’s abdomen releasing the face, brow and lastly, the trunk is depressed to release the occiput and vertex. 7. The method should be employed preferably under general anesthesia.
Management of complicated breech delivery
Problems which may arise during breech delivery:- • Arrest of buttock • Shoulder arrest • After coming head arrest
Arrest of the buttock :- Causes:- 1 . Weak uterine contraction/uterine inertia:- mx. Is oxytocin injection 2 . Rigid perineum:- mx. Is liberal episiotomy 3. Breech with extended legs:- mx. is Pinard’s manoeuvre
Pinard’s maneuver:- • pt. should be under GA. • The palmer surface of obstetrician is to be introduce facing the ventral surface of foetus. • Breech is pushed up at least to the level of symphysis pubis. • Middle and index fingers should apply pressure in popliteal fossa and abduction of the fossa done, which causes partial flexion of leg. • Head is flexed by other hand abdominally i.e externally. • The foot is brought down by grasping at the ankle by internal fingers. • Other leg is brought down in the same manner.
Shoulder arrest:- Cause :- • Extended arms:- mx. is Lovset’smanoeuvre.
Lovset’s maneuver:- • The maneuver should start only when the inferior angle of scapula is visible underneath the pubic arch. • The baby is grasped using both hands by femoropelvic grip keeping the thumbs parallel to the vertebral column. • The baby is lifted up slightly to cause lateral flexion. The trunk is rotate through 1800 keeping the back anterior and maintaining downward traction. This will bring posterior arm to emerge under the pubic arch which is then hooked out. • The trunk is then rotate in the reverse direction keeping the back anterior to deliver the anterior shoulder under the symphysis pubis.
After coming head arrest :- Causes:- • Deflexed head :- Jaw flexion & shoulder traction • Contracted pelvis:- em. c/s • High up head:- forceps delivery • Hydrocephalus:- craniotomy
COMPLICATIONS: FETAL: • Birth asphyxia: due to - cord compression - delay delivery of head - retraction of the placenta - premature attempt for respiration while the head is still inside. 2. Intracranial haemorrhage:- due to sudden decompression of the un-moulded head. If it is delivered suddenly causing tear to the tentorium cerebelli and haemorrhage in the subarachnoid space.
Cont…………. • Haematoma in sterno-mastoid muscle • Fractures & dislocation of cervical spines, femur, humerus, hip joint. • Visceral injuries:- rupture of liver, kidney due to pressure or faulty handling, prolapsed cord. • Nerve injuries:- stretching of the brachial plexus causes Erb’s and klumpke’s palsy. • All these leads to an Increase perinatal morbidity and mortality.
Maternal: • Increased operative delivery • Rupture of the uterus • Lacerations and tear of the cervix, vaginal. • Extensions of the episiotomy and deep perineal tears. • Anesthesia: cause uterine atony; postpartum hemorrhage • Maternal infection • Puerperal sepsis.
Prevention of the fetal and maternal complication: • External cephalic version, if no contraindication • If version is fail or contraindicated, delivery is done by elective CS. • Vaginal breech delivery or manipulation should be done by a skilled obstetricians.
- More by User

Vaginal or caesarean delivery: How research has turned breech birth around
Introduction:. Breech presentation occurs in 3-4% of singleton pregnancies at term (RCOG,2006)Over the last fifty years there has been a phenomenal shift in clinical practice from vaginal breech birth to caesarean sectionWorldwide the vast majority of breech babies are now delivered by planned cae
701 views • 29 slides
ABNORMAL PRESENTATION BREECH
Malpositions
883 views • 25 slides
The Preterm Breech Vaginal Versus. Abdominal Delivery
Introduction. The literature on this subject shows varied conflicting data. On one side, there are reports stating that vaginal delivery does not increase morbidity/mortality for preterm breech. On the other hand, there are many investigators reporting that the method of choice for delivering these
706 views • 24 slides
Moxibustion for Correction of Breech Presentation: A Randomized Controlled Trial JAMA 1998 280: 1580-1584
556 views • 23 slides
Breech Presentation
Breech Presentation. By Gabriel Eydt and Jennifer Kasbary.
2.34k views • 31 slides
Presentation Title Presentation Subtitle
National Society of Black Engineers. Presentation Title Presentation Subtitle. Agenda. Your own sub headline. This is an example text. Go ahead and replace it. 1. This is an example text. Go ahead and replace it. 2. ✓. This is an example text. Go ahead and replace it. 3. 4.
429 views • 22 slides
Presentation Presentation
Presentation Presentation. How to Present Your Ideas. Organization . Media is all organized. No technicalities occur during presentation. . Voice. Strong voice. Audible throughout the room. Confident in that which is being said. . Visuals. Generous color.
671 views • 6 slides
Presentation on Presentation
Presentation on Presentation. IMMERSE 2014 4-30-14. Outline. Technical presentations versus other Using PowerPoint Slides Backgrounds, colors, fonts, sizes Organization Too much/too little information Content Enough background information for your audience
562 views • 22 slides

Vaginal Breech Delivery
Vaginal Breech Delivery. Objectives Incidence and Significance Selection Management Intrapartum Delivery. Definition longitudinal lie breech or lower extremity presenting cephalic pole in the uterine fundus Types frank - flexed hips, extended knees
1.55k views • 25 slides
Alhadi Araibi Alkhadra Hospital. Breech Presentation. What you need to know about Breech Presentation. What is Breech Presentation? Types of Breech Presentation Importance of Breech Presentation Causes of Breech Presentation Diagnosis of Breech Presentation Management Options.
5.77k views • 24 slides

PRESENTATION TITLE PRESENTATION TITLE PRESENTATION TITLE
September 10-13, 2012 Orlando, Florida. PRESENTATION TITLE PRESENTATION TITLE PRESENTATION TITLE. Speaker Name(s) Speaker Name(s). Learning Points. List 1-3 key points that attendees will take away from your session. Return on Investment.
375 views • 6 slides
Mechanism of labor abnormal presentation and breech
DR. AHMED ABDULWAHAB Assistant Professor, Consultant OBGYN Department. Mechanism of labor abnormal presentation and breech. محاضره مهمه جدا – بالنظري وبالاوسكي.
1.06k views • 40 slides
Presentation title Presentation title
Presentation title Presentation title. Speaker details Speaker details. Test title. Slide content Slide content Slide content Slide content.
153 views • 2 slides

Breech Presentation. Aida Owlia and Christina Sun. Objectives. 10588 List strategies for management of abnormal fetal presentations, As well as the relative timing of each intervention. Case.
4.29k views • 27 slides

Student Conference: Breech Presentation
Student Conference: Breech Presentation. Michael Hale Chris Hong James Ross. The Case. A 32 yo G3T2P0A0L2 woman presents for routine prenatal care at 37 weeks. Her pregnancy is complicated by the following: Rh-negative status Depression
936 views • 22 slides
Breech presentation. By Dr. Khattab KAEO Prof & Head of Obstetrics and Gynaecology Department Faculty of Medicine, Al-Azhar University , Damietta. The fetal buttocks enter the pelvis first. Incidence: 3-4% (1:30) at term. 15% at 29-32 weeks' gestation.
603 views • 14 slides

Presentation Name Presentation Date
A collaborative approach to experiential learning across the province. Presentation Name Presentation Date. Today’s Presenters. Name , Position Name , Position Name , Position. Vision. The premier on-line connection for employers to register their interest in experiential learning.
458 views • 22 slides
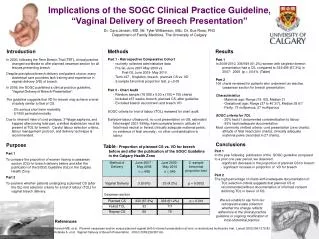
Implications of the SOGC Clinical Practice Guideline, “Vaginal Delivery of Breech Presentation”
Implications of the SOGC Clinical Practice Guideline, “Vaginal Delivery of Breech Presentation” Dr. Cara Janzen, MD, Mr. Tyler Williamson, BSc. Dr. Sue Ross, PhD Department of Family Medicine, The University of Calgary. Introduction. Methods. Results.
478 views • 1 slides
Obstetric emergencies Prolapsed cord Shoulder dystocia Breech delivery Twin delivery
Obstetric emergencies Prolapsed cord Shoulder dystocia Breech delivery Twin delivery. Aims. To recognise the above emergencies To practise the skills needed to manage them To achieve competence in those skills. Prolapsed cord.
446 views • 34 slides
Breech presentation. Breech presentation or podalic :-. when buttock of fetal occupies the lower segment of uterus, it is called breech presentation. Breech presentation occurs in 3-4% of all deliveries. Types of breech :- 1. Full/Complete Breech (cannonball position) (5-10%)
911 views • 44 slides

519 views • 25 slides
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Breech?
When a fetus is delivered buttocks or feet first
- Types of Presentation
Risk Factors
Complications.
Breech concerns the position of the fetus before labor . Typically, the fetus comes out headfirst, but in a breech delivery, the buttocks or feet come out first. This type of delivery is risky for both the pregnant person and the fetus.
This article discusses the different types of breech presentations, risk factors that might make a breech presentation more likely, treatment options, and complications associated with a breech delivery.
Verywell / Jessica Olah
Types of Breech Presentation
During the last few weeks of pregnancy, a fetus usually rotates so that the head is positioned downward to come out of the vagina first. This is called the vertex position.
In a breech presentation, the fetus does not turn to lie in the correct position. Instead, the fetus’s buttocks or feet are positioned to come out of the vagina first.
At 28 weeks of gestation, approximately 20% of fetuses are in a breech position. However, the majority of these rotate to the proper vertex position. At full term, around 3%–4% of births are breech.
The different types of breech presentations include:
- Complete : The fetus’s knees are bent, and the buttocks are presenting first.
- Frank : The fetus’s legs are stretched upward toward the head, and the buttocks are presenting first.
- Footling : The fetus’s foot is showing first.
Signs of Breech
There are no specific symptoms associated with a breech presentation.
Diagnosing breech before the last few weeks of pregnancy is not helpful, since the fetus is likely to turn to the proper vertex position before 35 weeks gestation.
A healthcare provider may be able to tell which direction the fetus is facing by touching a pregnant person’s abdomen. However, an ultrasound examination is the best way to determine how the fetus is lying in the uterus.
Most breech presentations are not related to any specific risk factor. However, certain circumstances can increase the risk for breech presentation.
These can include:
- Previous pregnancies
- Multiple fetuses in the uterus
- An abnormally shaped uterus
- Uterine fibroids , which are noncancerous growths of the uterus that usually appear during the childbearing years
- Placenta previa, a condition in which the placenta covers the opening to the uterus
- Preterm labor or prematurity of the fetus
- Too much or too little amniotic fluid (the liquid that surrounds the fetus during pregnancy)
- Fetal congenital abnormalities
Most fetuses that are breech are born by cesarean delivery (cesarean section or C-section), a surgical procedure in which the baby is born through an incision in the pregnant person’s abdomen.
In rare instances, a healthcare provider may plan a vaginal birth of a breech fetus. However, there are more risks associated with this type of delivery than there are with cesarean delivery.
Before cesarean delivery, a healthcare provider might utilize the external cephalic version (ECV) procedure to turn the fetus so that the head is down and in the vertex position. This procedure involves pushing on the pregnant person’s belly to turn the fetus while viewing the maneuvers on an ultrasound. This can be an uncomfortable procedure, and it is usually done around 37 weeks gestation.
ECV reduces the risks associated with having a cesarean delivery. It is successful approximately 40%–60% of the time. The procedure cannot be done once a pregnant person is in active labor.
Complications related to ECV are low and include the placenta tearing away from the uterine lining, changes in the fetus’s heart rate, and preterm labor.
ECV is usually not recommended if the:
- Pregnant person is carrying more than one fetus
- Placenta is in the wrong place
- Healthcare provider has concerns about the health of the fetus
- Pregnant person has specific abnormalities of the reproductive system
Recommendations for Previous C-Sections
The American College of Obstetricians and Gynecologists (ACOG) says that ECV can be considered if a person has had a previous cesarean delivery.
During a breech delivery, the umbilical cord might come out first and be pinched by the exiting fetus. This is called cord prolapse and puts the fetus at risk for decreased oxygen and blood flow. There’s also a risk that the fetus’s head or shoulders will get stuck inside the mother’s pelvis, leading to suffocation.
Complications associated with cesarean delivery include infection, bleeding, injury to other internal organs, and problems with future pregnancies.
A healthcare provider needs to weigh the risks and benefits of ECV, delivering a breech fetus vaginally, and cesarean delivery.
In a breech delivery, the fetus comes out buttocks or feet first rather than headfirst (vertex), the preferred and usual method. This type of delivery can be more dangerous than a vertex delivery and lead to complications. If your baby is in breech, your healthcare provider will likely recommend a C-section.
A Word From Verywell
Knowing that your baby is in the wrong position and that you may be facing a breech delivery can be extremely stressful. However, most fetuses turn to have their head down before a person goes into labor. It is not a cause for concern if your fetus is breech before 36 weeks. It is common for the fetus to move around in many different positions before that time.
At the end of your pregnancy, if your fetus is in a breech position, your healthcare provider can perform maneuvers to turn the fetus around. If these maneuvers are unsuccessful or not appropriate for your situation, cesarean delivery is most often recommended. Discussing all of these options in advance can help you feel prepared should you be faced with a breech delivery.
American College of Obstetricians and Gynecologists. If your baby is breech .
TeachMeObGyn. Breech presentation .
MedlinePlus. Breech birth .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term . Cochrane Database Syst Rev . 2015 Apr 1;2015(4):CD000083. doi:10.1002/14651858.CD000083.pub3
By Christine Zink, MD Dr. Zink is a board-certified emergency medicine physician with expertise in the wilderness and global medicine.
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Labor & Delivery
What Causes Breech Presentation?
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered.
What Is Breech Presentation?
Types of breech presentation, what causes a breech baby, can you turn a breech baby, how are breech babies delivered.
FatCamera/Getty Images
Toward the end of pregnancy, your baby will start to get into position for delivery, with their head pointed down toward the vagina. This is otherwise known as vertex presentation. However, some babies turn inside the womb so that their feet or buttocks are poised to be delivered first, which is commonly referred to as breech presentation, or a breech baby.
As you near the end of your pregnancy journey, an OB-GYN or health care provider will check your baby's positioning. You might find yourself wondering: What causes breech presentation? Are there risks involved? And how are breech babies delivered? We turned to experts and research to answer some of the most common questions surrounding breech presentation, along with what causes this positioning in the first place.
During your pregnancy, your baby constantly moves around the uterus. Indeed, most babies do somersaults up until the 36th week of pregnancy , when they pick their final position in the womb, says Laura Riley , MD, an OB-GYN in New York City. Approximately 3-4% of babies end up “upside-down” in breech presentation, with their feet or buttocks near the cervix.
Breech presentation is typically diagnosed during a visit to an OB-GYN, midwife, or health care provider. Your physician can feel the position of your baby's head through your abdominal wall—or they can conduct a vaginal exam if your cervix is open. A suspected breech presentation should ultimately be confirmed via an ultrasound, after which you and your provider would have a discussion about delivery options, potential issues, and risks.
There are three types of breech babies: frank, footling, and complete. Learn about the differences between these breech presentations.
Frank Breech
With frank breech presentation, your baby’s bottom faces the cervix and their legs are straight up. This is the most common type of breech presentation.
Footling Breech
Like its name suggests, a footling breech is when one (single footling) or both (double footling) of the baby's feet are in the birth canal, where they’re positioned to be delivered first .
Complete Breech
In a complete breech presentation, baby’s bottom faces the cervix. Their legs are bent at the knees, and their feet are near their bottom. A complete breech is the least common type of breech presentation.
Other Types of Mal Presentations
The baby can also be in a transverse position, meaning that they're sideways in the uterus. Another type is called oblique presentation, which means they're pointing toward one of the pregnant person’s hips.
Typically, your baby's positioning is determined by the fetus itself and the shape of your uterus. Because you can't can’t control either of these factors, breech presentation typically isn’t considered preventable. And while the cause often isn't known, there are certain risk factors that may increase your risk of a breech baby, including the following:
- The fetus may have abnormalities involving the muscular or central nervous system
- The uterus may have abnormal growths or fibroids
- There might be insufficient amniotic fluid in the uterus (too much or too little)
- This isn’t your first pregnancy
- You have a history of premature delivery
- You have placenta previa (the placenta partially or fully covers the cervix)
- You’re pregnant with multiples
- You’ve had a previous breech baby
In some cases, your health care provider may attempt to help turn a baby in breech presentation through a procedure known as external cephalic version (ECV). This is when a health care professional applies gentle pressure on your lower abdomen to try and coax your baby into a head-down position. During the entire procedure, the fetus's health will be monitored, and an ECV is often performed near a delivery room, in the event of any potential issues or complications.
However, it's important to note that ECVs aren't for everyone. If you're carrying multiples, there's health concerns about you or the baby, or you've experienced certain complications with your placenta or based on placental location, a health care provider will not attempt an ECV.
The majority of breech babies are born through C-sections . These are usually scheduled between 38 and 39 weeks of pregnancy, before labor can begin naturally. However, with a health care provider experienced in delivering breech babies vaginally, a natural delivery might be a safe option for some people. In fact, a 2017 study showed similar complication and success rates with vaginal and C-section deliveries of breech babies.
That said, there are certain known risks and complications that can arise with an attempt to deliver a breech baby vaginally, many of which relate to problems with the umbilical cord. If you and your medical team decide on a vaginal delivery, your baby will be monitored closely for any potential signs of distress.
Ultimately, it's important to know that most breech babies are born healthy. Your provider will consider your specific medical condition and the position of your baby to determine which type of delivery will be the safest option for a healthy and successful birth.
ACOG. If Your Baby Is Breech .
American Pregnancy Association. Breech Presentation .
Gray CJ, Shanahan MM. Breech Presentation . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Mount Sinai. Breech Babies .
Takeda J, Ishikawa G, Takeda S. Clinical Tips of Cesarean Section in Case of Breech, Transverse Presentation, and Incarcerated Uterus . Surg J (N Y). 2020 Mar 18;6(Suppl 2):S81-S91. doi: 10.1055/s-0040-1702985. PMID: 32760790; PMCID: PMC7396468.
Shanahan MM, Gray CJ. External Cephalic Version . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Fonseca A, Silva R, Rato I, Neves AR, Peixoto C, Ferraz Z, Ramalho I, Carocha A, Félix N, Valdoleiros S, Galvão A, Gonçalves D, Curado J, Palma MJ, Antunes IL, Clode N, Graça LM. Breech Presentation: Vaginal Versus Cesarean Delivery, Which Intervention Leads to the Best Outcomes? Acta Med Port. 2017 Jun 30;30(6):479-484. doi: 10.20344/amp.7920. Epub 2017 Jun 30. PMID: 28898615.
Related Articles
- Help & Feedback
- About epocrates
Breech presentation
Highlights & basics, diagnostic approach, risk factors, history & exam, differential diagnosis.
- Tx Approach
Emerging Tx
Complications.
PATIENT RESOURCES
Patient Instructions
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head.
Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence decreases as pregnancy progresses and by term occurs in 3% to 4% of singleton term pregnancies.
Treatment options include external cephalic version to increase the likelihood of vaginal birth or a planned cesarean section, the optimal gestation being 37 and 39 weeks, respectively.
Planned cesarean section is considered the safest form of delivery for infants with a persisting breech presentation at term.
Quick Reference
Key Factors
buttocks or feet as the presenting part
Fetal head under costal margin, fetal heartbeat above the maternal umbilicus.
Other Factors
subcostal tenderness
Pelvic or bladder pain.
Diagnostics Tests
1st Tests to Order
transabdominal/transvaginal ultrasound
Treatment options.
presumptive
<37 weeks' gestation
specialist evaluation
corticosteroid
magnesium sulfate
≥37 weeks' gestation not in labor
unsuccessful ECV with persistent breech
Classifications
Types of breech presentation
Baby's buttocks lead the way into the birth canal
Hips are flexed, knees are extended, and the feet are in close proximity to the head
65% to 70% of breech babies are in this position.
Baby presents with buttocks first
Both the hips and the knees are flexed; the baby may be sitting cross-legged.
One or both of the baby's feet lie below the breech so that the foot or knee is lowermost in the birth canal
This is rare at term but relatively common with premature fetuses.
Common Vignette
Other Presentations
Epidemiology
33% of births less than 28 weeks' gestation
14% of births at 29 to 32 weeks' gestation
9% of births at 33 to 36 weeks' gestation
6% of births at 37 to 40 weeks' gestation.
Pathophysiology
- Natasha Nassar, PhD
- Christine L. Roberts, MBBS, FAFPHM, DrPH
- Jonathan Morris, MBChB, FRANZCOG, PhD
- John W. Bachman, MD
- Rhona Hughes, MBChB
- Brian Peat, MD
- Lelia Duley, MBChB
- Justus Hofmeyr, MD

Clinical exam
Palpation of the abdomen to determine the position of the baby's head
Palpation of the abdomen to confirm the position of the fetal spine on one side and fetal extremities on the other
Palpation of the area above the symphysis pubis to locate the fetal presenting part
Palpation of the presenting part to confirm presentation, to determine how far the fetus has descended and whether the fetus is engaged.

Ultrasound examination
Premature fetus.
Prematurity is consistently associated with breech presentation. [ 6 ] [ 9 ] This may be due to the smaller size of preterm infants, who are more likely to change their in utero position.
Increasing duration of pregnancy may allow breech-presenting fetuses time to grow, turn spontaneously or by external cephalic version, and remain cephalic-presenting.
Larger fetuses may be forced into a cephalic presentation in late pregnancy due to space or alignment constraints within the uterus.
small for gestational age fetus
Low birth-weight is a risk factor for breech presentation. [ 9 ] [ 11 ] [ 12 ] [ 13 ] [ 14 ] Term breech births are associated with a smaller fetal size for gestational age, highlighting the association with low birth-weight rather than prematurity. [ 6 ]
nulliparity
Women having a first birth have increased rates of breech presentation, probably due to the increased likelihood of smaller fetal size. [ 6 ] [ 9 ]
Relaxation of the uterine wall in multiparous women may reduce the odds of breech birth and contribute to a higher spontaneous or external cephalic version rate. [ 10 ]
fetal congenital anomalies
Congenital anomalies in the fetus may result in a small fetal size or inappropriate fetal growth. [ 9 ] [ 12 ] [ 14 ] [ 15 ]
Anencephaly, hydrocephaly, Down syndrome, and fetal neuromuscular dysfunction are associated with breech presentation, the latter due to its effect on the quality of fetal movements. [ 9 ] [ 14 ]
previous breech delivery
The risk of recurrent breech delivery is 8%, the risk increasing from 4% after one breech delivery to 28% after three. [ 16 ]
The effects of recurrence may be due to recurring specific causal factors, either genetic or environmental in origin.
uterine abnormalities
Women with uterine abnormalities have a high incidence of breech presentation. [ 14 ] [ 17 ] [ 18 ] [ 19 ]
female fetus
Fifty-four percent of breech-presenting fetuses are female. [ 14 ]
abnormal amniotic fluid volume
Both oligohydramnios and polyhydramnios are associated with breech presentation. [ 1 ] [ 12 ] [ 14 ]
Low amniotic fluid volume decreases the likelihood of a fetus turning to a cephalic position; an increased amniotic fluid volume may facilitate frequent change in position.
placental abnormalities
An association between placental implantation in the cornual-fundal region and breech presentation has been reported, although some studies have not found it a risk factor. [ 8 ] [ 20 ] [ 21 ] [ 22 ] [ 10 ] [ 14 ]
The association with placenta previa is also inconsistent. [ 8 ] [ 9 ] [ 22 ] Placenta previa is associated with preterm birth and may be an indirect risk factor.
Pelvic or vaginal examination reveals the buttocks and/or feet, felt as a yielding, irregular mass, as the presenting part. [ 26 ] In cephalic presentation, a hard, round, regular fetal head can be palpated. [ 26 ]
The Leopold maneuver on examination suggests breech position by palpation of the fetal head under the costal margin. [ 26 ]
The baby's heartbeat should be auscultated using a Pinard stethoscope or a hand-held Doppler to indicate the position of the fetus. The fetal heartbeat lies above the maternal umbilicus in breech presentation. [ 1 ]
Tenderness under one or other costal margin as a result of pressure by the harder fetal head.
Pain due to fetal kicks in the maternal pelvis or bladder.
breech position
Visualizes the fetus and reveals its position.
Used to confirm a clinically suspected breech presentation. [ 28 ]
Should be performed by practitioners with appropriate skills in obstetric ultrasound.
Establishes the type of breech presentation by imaging the fetal femurs and their relationship to the distal bones.
Transverse lie
Differentiating Signs/Symptoms
Fetus lies horizontally across the uterus with the shoulder as the presenting part.
Similar predisposing factors such as placenta previa, abnormal amniotic fluid volume, and uterine anomalies, although more common in multiparity. [ 1 ] [ 2 ] [ 29 ]
Differentiating Tests
Clinical examination and fetal auscultation may be indicative.
Ultrasound confirms presentation.
Treatment Approach
Breech presentation <37 weeks' gestation.
The UK Royal College of Obstetricians and Gynaecologists (RCOG) recommends that corticosteroids should be offered to women between 24 and 34+6 weeks' gestation, in whom imminent preterm birth is anticipated. Corticosteroids should only be considered after discussion of risks/benefits at 35 to 36+6 weeks. Given within 7 days of preterm birth, corticosteroids may reduce perinatal and neonatal death and respiratory distress syndrome. [ 32 ] The American College of Obstetricians and Gynecologists (ACOG) recommends a single course of corticosteroids for pregnant women between 24 and 33+6 weeks' gestation who are at risk of preterm delivery within 7 days, including those with ruptured membranes and multiple gestations. It may also be considered for pregnant women starting at 23 weeks' gestation who are at risk of preterm delivery within 7 days. A single course of betamethasone is recommended for pregnant women between 34 and 36+6 weeks' gestation at risk of preterm birth within 7 days, and who have not received a previous course of prenatal corticosteroids. Regularly scheduled repeat courses or serial courses (more than two) are not currently recommended. A single repeat course of prenatal corticosteroids should be considered in women who are less than 34 weeks' gestation, who are at risk of preterm delivery within 7 days, and whose prior course of prenatal corticosteroids was administered more than 14 days previously. Rescue course corticosteroids could be provided as early as 7 days from the prior dose, if indicated by the clinical scenario. [ 33 ]
Magnesium sulfate given before anticipated early preterm birth reduces the risk of cerebral palsy in surviving infants. Physicians electing to use magnesium sulfate for fetal neuroprotection should develop specific guidelines regarding inclusion criteria, treatment regimens, and concurrent tocolysis. [ 34 ]
Breech presentation from 37 weeks' gestation, before labor
ECV is the initial treatment for a breech presentation at term when the patient is not in labor. It involves turning a fetus presenting by the breech to a cephalic (head-down) presentation to increase the likelihood of vaginal birth. [ 35 ] [ 36 ] Where available, it should be offered to all women in late pregnancy, by an experienced clinician, in hospitals with facilities for emergency delivery, and no contraindications to the procedure. [ 35 ] There is no upper time limit on the appropriate gestation for ECV, with success reported at 42 weeks.
There is no general consensus on contraindications to ECV. Contraindications include multiple pregnancy (except after delivery of a first twin), ruptured membranes, current or recent (<1 week) vaginal bleeding, rhesus isoimmunization, other indications for cesarean section (e.g., placenta previa or uterine malformation), or abnormal electronic fetal monitoring. [ 35 ] One systematic review of relative contraindications for ECV highlighted that most contraindications do not have clear empirical evidence. Exceptions include placental abruption, severe preeclampsia/HELLP syndrome, or signs of fetal distress (abnormal cardiotocography and/or Doppler flow). [ 36 ]
The procedure involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
The overall ECV success rate varies but, in a large series, 47% of women following an ECV attempt had a cephalic presentation at birth. [ 35 ] [ 38 ] Various factors influence the success rate. One systematic review found ECV success rates to be 68% overall, with the rate significantly higher for women from African countries (89%) compared with women from non-African countries (62%), and higher among multiparous (78%) than nulliparous women (48%). [ 39 ] Overall, the ECV success rates for nulliparous and multiparous non-African women were 43% and 73%, respectively, while for nulliparous and multiparous African women rates were 79% and 91%, respectively. Another study reported no difference in success rate or rate of cesarean section among women with previous cesarean section undergoing ECV compared with women with previous vaginal birth. However, numbers were small and further studies in this regard are required. [ 40 ]
Women's preference for vaginal delivery is a major contributing factor in their decision for ECV. However, studies suggest women with a breech presentation at term may not receive complete and/or evidence-based information about the benefits and risks of ECV. [ 41 ] [ 42 ] Although up to 60% of women reported ECV to be painful, the majority highlighted the benefits outweigh the risks (71%) and would recommend ECV to their friends or be willing to repeat for themselves (84%). [ 41 ] [ 42 ]
Cardiotocography and ultrasound should be performed before and after the procedure. Tocolysis should be used to facilitate the maneuver, and Rho(D) immune globulin should be administered to women who are Rhesus negative. [ 35 ] Tocolytic agents include adrenergic beta-2 receptor stimulants such as albuterol, terbutaline, or ritodrine (widely used with ECV in some countries, but not yet available in the US). One Cochrane review of tocolytic beta stimulants demonstrates that these are less likely to be associated with failed ECV, and are effective in increasing cephalic presentation and reducing cesarean section. [ 43 ] There is no current evidence to recommend one beta-2 adrenergic receptor agonist over another. Until these data are available, adherence to a local protocol for tocolysis is recommended. The Food and Drug Administration has issued a warning against using injectable terbutaline beyond 48 to 72 hours, or acute or prolonged treatment with oral terbutaline, in pregnant women for the prevention or prolonged treatment of preterm labor, due to potential serious maternal cardiac adverse effects and death. [ 44 ] Whether this warning applies to the subcutaneous administration of terbutaline in ECV is still unclear; however, studies currently support this use. The European Medicines Agency (EMA) recommends that injectable beta agonists should be used for up to 48 hours between the 22nd and 37th week of pregnancy only. They should be used under specialist supervision with continuous monitoring of the mother and unborn baby owing to the risk of adverse cardiovascular effects in both the mother and baby. The EMA no longer recommends oral or rectal formulations for obstetric indications. [ 45 ]
If ECV is successful, pregnancy care should continue as usual for any cephalic presentation. One systematic review assessing the mode of delivery after a successful ECV found that these women were at increased risk for cesarean section and instrumental vaginal delivery compared with women with spontaneous cephalic pregnancies. However, they still had a lower rate of cesarean section following ECV (i.e., 47%) compared with the cesarean section rate for those with a persisting breech (i.e., 85%). With a number needed to treat of three, ECV is still considered to be an effective means of preventing the need for cesarean section. [ 46 ]
Planned cesarean section should be offered as the safest mode of delivery for the baby, even though it carries a small increase in serious immediate maternal complications compared with vaginal birth. [ 24 ] [ 25 ] [ 31 ] In the US, most unsuccessful ECV with persistent breech will be delivered via cesarean section.
A vaginal mode of delivery may be considered by some clinicians as an option, particularly when maternal request is provided, senior and experienced staff are available, there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
Breech presentation from 37 weeks' gestation, during labor
The first option should be a planned cesarean section.
There is a small increase in the risk of serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
The long-term risks include potential compromise of future obstetric performance, increased risk of repeat cesarean section, infertility, uterine rupture, placenta accreta, placental abruption, and emergency hysterectomy. [ 60 ] [ 61 ] [ 62 ] [ 63 ]
Planned cesarean section is safer for babies, but is associated with increased neonatal respiratory distress. The risk is reduced when the section is performed at 39 weeks' gestation. [ 64 ] [ 65 ] [ 66 ] For women undergoing a planned cesarean section, RCOG recommends an informed discussion about the potential risks and benefits of a course of prenatal corticosteroids between 37 and 38+6 weeks' gestation. Although prenatal corticosteroids may reduce admission to the neonatal unit for respiratory morbidity, it is uncertain if there is any reduction in respiratory distress syndrome, transient tachypnea of the newborn, or neonatal unit admission overall. In addition, prenatal corticosteroids may result in harm to the neonate, including hypoglycemia and potential developmental delay. [ 32 ] ACOG does not recommend corticosteroids in women >37 weeks' gestation. [ 33 ]
Undiagnosed breech in labor generally results in cesarean section after the onset of labor, higher rates of emergency cesarean section associated with the least favorable maternal outcomes, a greater likelihood of cord prolapse, and other poor infant outcomes. [ 23 ] [ 67 ] [ 49 ] [ 68 ] [ 69 ] [ 70 ] [ 71 ]
This mode of delivery may be considered by some clinicians as an option for women who are in labor, particularly when delivery is imminent. Vaginal breech delivery may also be considered, where suitable, when delivery is not imminent, maternal request is provided, senior and experienced staff are available, there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
Findings from one systematic review of 27 observational studies revealed that the absolute risks of perinatal mortality, fetal neurologic morbidity, birth trauma, 5-minute Apgar score <7, and neonatal asphyxia in the planned vaginal delivery group were low at 0.3%, 0.7%, 0.7%, 2.4%, and 3.3%, respectively. However, the relative risks of perinatal mortality and morbidity were 2- to 5-fold higher in the planned vaginal than in the planned cesarean delivery group. Authors recommend ongoing judicious decision-making for vaginal breech delivery for selected singleton, term breech babies. [ 72 ]
ECV may also be considered an option for women with breech presentation in early labor, when delivery is not imminent, provided that the membranes are intact.
A woman presenting with a breech presentation <37 weeks is an area of clinical controversy. Optimal mode of delivery for preterm breech has not been fully evaluated in clinical trials, and the relative risks for the preterm infant and mother remain unclear. In the absence of good evidence, if diagnosis of breech presentation prior to 37 weeks' gestation is made, prematurity and clinical circumstances should determine management and mode of delivery.
Primary Options
12 mg intramuscularly every 24 hours for 2 doses
6 mg intramuscularly every 12 hours for 4 doses
The UK Royal College of Obstetricians and Gynaecologists recommends that corticosteroids should be offered to women between 24 and 34+6 weeks' gestation, in whom imminent preterm birth is anticipated. Corticosteroids should only be considered after discussion of risks/benefits at 35 to 36+6 weeks. Given within 7 days of preterm birth, corticosteroids may reduce perinatal and neonatal death and respiratory distress syndrome. [ 32 ]
The American College of Obstetricians and Gynecologists recommends a single course of corticosteroids for pregnant women between 24 and 33+6 weeks' gestation who are at risk of preterm delivery within 7 days, including those with ruptured membranes and multiple gestations. It may also be considered for pregnant women starting at 23 weeks' gestation who are at risk of preterm delivery within 7 days. A single course of betamethasone is recommended for pregnant women between 34 and 36+6 weeks' gestation at risk of preterm birth within 7 days, and who have not received a previous course of prenatal corticosteroids. Regularly scheduled repeat courses or serial courses (more than two) are not currently recommended. A single repeat course of prenatal corticosteroids should be considered in women who are less than 34 weeks' gestation, who are at risk of preterm delivery within 7 days, and whose prior course of prenatal corticosteroids was administered more than 14 days previously. Rescue course corticosteroids could be provided as early as 7 days from the prior dose, if indicated by the clinical scenario. [ 33 ]
consult specialist for guidance on dose
external cephalic version (ECV)
There is no upper time limit on the appropriate gestation for ECV; it should be offered to all women in late pregnancy by an experienced clinician in hospitals with facilities for emergency delivery and no contraindications to the procedure. [ 35 ] [ 36 ]
ECV involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
There is no general consensus on contraindications to ECV. Contraindications include multiple pregnancy (except after delivery of a first twin), ruptured membranes, current or recent (<1 week) vaginal bleeding, rhesus isoimmunization, other indications for cesarean section (e.g., placenta previa or uterine malformation), or abnormal electronic fetal monitoring. [ 35 ] One systematic review of relative contraindications for ECV highlighted that most contraindications do not have clear empirical evidence. Exceptions include placental abruption, severe preeclampsia/HELLP syndrome, or signs of fetal distress (abnormal cardiotocography and/or Doppler flow). [ 36 ]
Cardiotocography and ultrasound should be performed before and after the procedure.
If ECV is successful, pregnancy care should continue as usual for any cephalic presentation. A systematic review assessing the mode of delivery after a successful ECV found that these women were at increased risk for cesarean section and instrumental vaginal delivery compared with women with spontaneous cephalic pregnancies. However, they still had a lower rate of cesarean section following ECV (i.e., 47%) compared with the cesarean section rate for those with a persisting breech (i.e., 85%). With a number needed to treat of 3, ECV is still considered to be an effective means of preventing the need for cesarean section. [ 46 ]
tocolytic agents
see local specialist protocol for dosing guidelines
Tocolytic agents include adrenergic beta-2 receptor stimulants such as albuterol, terbutaline, or ritodrine (widely used with external cephalic version [ECV] in some countries, but not yet available in the US). They are used to delay or inhibit labor and increase the success rate of ECV. There is no current evidence to recommend one beta-2 adrenergic receptor agonist over another. Until these data are available, adherence to a local protocol for tocolysis is recommended.
The Food and Drug Administration has issued a warning against using injectable terbutaline beyond 48-72 hours, or acute or prolonged treatment with oral terbutaline, in pregnant women for the prevention or prolonged treatment of preterm labor, due to potential serious maternal cardiac adverse effects and death. [ 44 ] Whether this warning applies to the subcutaneous administration of terbutaline in ECV is still unclear; however, studies currently support this use. The European Medicines Agency (EMA) recommends that injectable beta agonists should be used for up to 48 hours between the 22nd and 37th week of pregnancy only. They should be used under specialist supervision with continuous monitoring of the mother and unborn baby owing to the risk of adverse cardiovascular effects in both the mother and baby. The EMA no longer recommends oral or rectal formulations for obstetric indications. [ 45 ]
A systematic review found there was no evidence to support the use of nifedipine for tocolysis. [ 73 ]
There is insufficient evidence to evaluate other interventions to help ECV, such as fetal acoustic stimulation in midline fetal spine positions, or epidural or spinal analgesia. [ 43 ]
Rho(D) immune globulin
300 micrograms intramuscularly as a single dose
Nonsensitized Rh-negative women should receive Rho(D) immune globulin. [ 35 ]
The indication for its administration is to prevent rhesus isoimmunization, which may affect subsequent pregnancy outcomes.
Rho(D) immune globulin needs to be given at the time of external cephalic version and should be given again postpartum to those women who give birth to an Rh-positive baby. [ 74 ]
It is best administered as soon as possible after the procedure, usually within 72 hours.
Dose depends on brand used. Dose given below pertains to most commonly used brands. Consult specialist for further guidance on dose.
elective cesarean section/vaginal breech delivery
Mode of delivery (cesarean section or vaginal breech delivery) should be based on the experience of the attending clinician, hospital policies, maternal request, and the presence or absence of complicating factors. In the US, most unsuccessful external cephalic version (ECV) with persistent breech will be delivered via cesarean section.
Cesarean section, at 39 weeks or greater, has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ] Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, bleeding, infection, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
Vaginal delivery may be considered by some clinicians as an option, particularly when maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
For women undergoing a planned cesarean section, the UK Royal College of Obstetricians and Gynaecologists recommends an informed discussion about the potential risks and benefits of a course of prenatal corticosteroids between 37 and 38+6 weeks' gestation. Although prenatal corticosteroids may reduce admission to the neonatal unit for respiratory morbidity, it is uncertain if there is any reduction in respiratory distress syndrome, transient tachypnea of the newborn, or neonatal unit admission overall. In addition, prenatal corticosteroids may result in harm to the neonate, including hypoglycemia and potential developmental delay. [ 32 ] The American College of Obstetricians and Gynecologists does not recommend corticosteroids in women >37 weeks' gestation. [ 33 ]
It is best administered as soon as possible after delivery, usually within 72 hours.
Administration of postpartum Rho (D) immune globulin should not be affected by previous routine prenatal prophylaxis or previous administration for a potentially sensitizing event. [ 74 ]
≥37 weeks' gestation in labor: no imminent delivery
planned cesarean section
For women with breech presentation in labor, planned cesarean section at 39 weeks or greater has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ]
Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
Continuous cardiotocography monitoring should continue until delivery. [ 24 ] [ 25 ]
vaginal breech delivery
Mode of delivery (cesarean section or vaginal breech delivery) should be based on the experience of the attending clinician, hospital policies, maternal request, and the presence or absence of complicating factors.
This mode of delivery may be considered by some clinicians as an option, particularly when maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
For women with persisting breech presentation, planned cesarean section has, however, been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ]
ECV may also be considered an option for women with breech presentation in early labor, provided that the membranes are intact.
There is no upper time limit on the appropriate gestation for ECV. [ 35 ]
Involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
Relative contraindications include placental abruption, severe preeclampsia/HELLP syndrome, and signs of fetal distress (abnormal cardiotocography and/or abnormal Doppler flow). [ 35 ] [ 36 ]
Rho(D) immune globulin needs to be given at the time of ECV and should be given again postpartum to those women who give birth to an Rh-positive baby. [ 74 ]
≥37 weeks' gestation in labor: imminent delivery
cesarean section
For women with persistent breech presentation, planned cesarean section has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ] Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
This mode of delivery may be considered by some clinicians as an option, particularly when delivery is imminent, maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
It is best administered as soon as possible after the delivery, usually within 72 hours.
External cephalic version before term
Moxibustion, postural management, follow-up overview, perinatal complications.
Compared with cephalic presentation, persistent breech presentation has increased frequency of cord prolapse, abruptio placentae, prelabor rupture of membranes, perinatal mortality, fetal distress (heart rate <100 bpm), preterm delivery, lower fetal weight. [ 10 ] [ 11 ] [ 67 ]
complications of cesarean section
There is a small increase in the risk of serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ]
The long-term risks include potential compromise of future obstetric performance, increased risk of repeat cesarean section, infertility, uterine rupture, placenta accreta, placental abruption, and emergency hysterectomy. [ 60 ] [ 61 ] [ 62 ] [ 63 ] The evidence suggests that using sutures, rather than staples, for wound closure after cesarean section reduces the incidence of wound dehiscence. [ 59 ]
Emergency cesarean section, compared with planned cesarean section, has demonstrated a higher risk of severe obstetric morbidity, intra-operative complications, postoperative complications, infection, blood loss >1500 mL, fever, pain, tiredness, and breast-feeding problems. [ 23 ] [ 48 ] [ 50 ] [ 70 ] [ 81 ]
Key Articles
Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. March 2017 [internet publication]. [Full Text]
Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
Referenced Articles
1. Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997.
2. Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002.
3. Scheer K, Nubar J. Variation of fetal presentation with gestational age. Am J Obstet Gynecol. 1976 May 15;125(2):269-70. [Abstract]
4. Nassar N, Roberts CL, Cameron CA, et al. Diagnostic accuracy of clinical examination for detection of non-cephalic presentation in late pregnancy: cross sectional analytic study. BMJ. 2006 Sep 16;333(7568):578-80. [Abstract] [Full Text]
5. Roberts CL, Peat B, Algert CS, et al. Term breech birth in New South Wales, 1990-1997. Aust N Z J Obstet Gynaecol. 2000 Feb;40(1):23-9. [Abstract]
6. Roberts CL, Algert CS, Peat B, et al. Small fetal size: a risk factor for breech birth at term. Int J Gynaecol Obstet. 1999 Oct;67(1):1-8. [Abstract]
7. Brar HS, Platt LD, DeVore GR, et al. Fetal umbilical velocimetry for the surveillance of pregnancies complicated by placenta previa. J Reprod Med. 1988 Sep;33(9):741-4. [Abstract]
8. Kian L. The role of the placental site in the aetiology of breech presentation. J Obstet Gynaecol Br Commonw. 1963 Oct;70:795-7. [Abstract]
9. Rayl J, Gibson PJ, Hickok DE. A population-based case-control study of risk factors for breech presentation. Am J Obstet Gynecol. 1996 Jan;174(1 Pt 1):28-32. [Abstract]
10. Westgren M, Edvall H, Nordstrom L, et al. Spontaneous cephalic version of breech presentation in the last trimester. Br J Obstet Gynaecol. 1985 Jan;92(1):19-22. [Abstract]
11. Brenner WE, Bruce RD, Hendricks CH. The characteristics and perils of breech presentation. Am J Obstet Gynecol. 1974 Mar 1;118(5):700-12. [Abstract]
12. Hall JE, Kohl S. Breech presentation. Am J Obstet Gynecol. 1956 Nov;72(5):977-90. [Abstract]
13. Morgan HS, Kane SH. An analysis of 16,327 breech births. JAMA. 1964 Jan 25;187:262-4. [Abstract]
14. Luterkort M, Persson P, Weldner B. Maternal and fetal factors in breech presentation. Obstet Gynecol. 1984 Jul;64(1):55-9. [Abstract]
15. Braun FH, Jones KL, Smith DW. Breech presentation as an indicator of fetal abnormality. J Pediatr. 1975 Mar;86(3):419-21. [Abstract]
16. Albrechtsen S, Rasmussen S, Dalaker K, et al. Reproductive career after breech presentation: subsequent pregnancy rates, interpregnancy interval, and recurrence. Obstet Gynecol. 1998 Sep;92(3):345-50. [Abstract]
17. Zlopasa G, Skrablin S, Kalafatić D, et al. Uterine anomalies and pregnancy outcome following resectoscope metroplasty. Int J Gynaecol Obstet. 2007 Aug;98(2):129-33. [Abstract]
18. Acién P. Breech presentation in Spain, 1992: a collaborative study. Eur J Obstet Gynecol Reprod Biol. 1995 Sep;62(1):19-24. [Abstract]
19. Michalas SP. Outcome of pregnancy in women with uterine malformation: evaluation of 62 cases. Int J Gynaecol Obstet. 1991 Jul;35(3):215-9. [Abstract]
20. Fianu S, Vaclavinkova V. The site of placental attachment as a factor in the aetiology of breech presentation. Acta Obstet Gynecol Scand. 1978;57(4):371-2. [Abstract]
21. Haruyama Y. Placental implantation as the cause of breech presentation [in Japanese]. Nihon Sanka Fujinka Gakkai Zasshi. 1987 Jan;39(1):92-8. [Abstract]
22. Filipov E, Borisov I, Kolarov G. Placental location and its influence on the position of the fetus in the uterus [in Bulgarian]. Akush Ginekol (Sofiia). 2000;40(4):11-2. [Abstract]
23. Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control study. BMJ. 2001 May 5;322(7294):1089-93. [Abstract] [Full Text]
24. Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
25. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. ACOG committee opinion no. 745: mode of term singleton breech delivery. Obstet Gynecol. 2018 Aug;132(2):e60-3. [Abstract] [Full Text]
26. Beischer NA, Mackay EV, Colditz P, eds. Obstetrics and the newborn: an illustrated textbook. 3rd ed. London: W.B. Saunders; 1997.
27. Royal College of Obstetricians and Gynaecologists. Antepartum haemorrhage: green-top guideline no. 63. November 2011 [internet publication]. [Full Text]
28. American College of Obstetricians and Gynecologists. Practice bulletin no. 175: ultrasound in pregnancy. Obstet Gynecol. 2016 Dec;128(6):e241-56. [Abstract]
29. Enkin M, Keirse MJNC, Neilson J, et al. Guide to effective care in pregnancy and childbirth. 3rd ed. Oxford: Oxford University Press; 2000.
30. Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000083. [Abstract] [Full Text]
31. Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
32. Stock SJ, Thomson AJ, Papworth S, et al. Antenatal corticosteroids to reduce neonatal morbidity and mortality: Green-top Guideline No. 74. BJOG. 2022 Jul;129(8):e35-60. [Abstract] [Full Text]
33. American College of Obstetricians and Gynaecologists Committee on Obstetric Practice. Committee opinion no. 713: antenatal corticosteroid therapy for fetal maturation. August 2017 (reaffirmed 2020) [internet publication]. [Full Text]
34. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. Committee opinion no. 455: magnesium sulfate before anticipated preterm birth for neuroprotection. March 2010 (reaffirmed 2020) [internet publication]. [Full Text]
35. Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. March 2017 [internet publication]. [Full Text]
36. Rosman AN, Guijt A, Vlemmix F, et al. Contraindications for external cephalic version in breech position at term: a systematic review. Acta Obstet Gynecol Scand. 2013 Feb;92(2):137-42. [Abstract]
37. Hofmeyr GJ. Effect of external cephalic version in late pregnancy on breech presentation and caesarean section rate: a controlled trial. Br J Obstet Gynaecol. 1983 May;90(5):392-9. [Abstract]
38. Beuckens A, Rijnders M, Verburgt-Doeleman GH, et al. An observational study of the success and complications of 2546 external cephalic versions in low-risk pregnant women performed by trained midwives. BJOG. 2016 Feb;123(3):415-23. [Abstract]
39. Nassar N, Roberts CL, Barratt A, et al. Systematic review of adverse outcomes of external cephalic version and persisting breech presentation at term. Paediatr Perinat Epidemiol. 2006 Mar;20(2):163-71. [Abstract]
40. Sela HY, Fiegenberg T, Ben-Meir A, et al. Safety and efficacy of external cephalic version for women with a previous cesarean delivery. Eur J Obstet Gynecol Reprod Biol. 2009 Feb;142(2):111-4. [Abstract]
41. Pichon M, Guittier MJ, Irion O, et al. External cephalic version in case of persisting breech presentation at term: motivations and women's experience of the intervention [in French]. Gynecol Obstet Fertil. 2013 Jul-Aug;41(7-8):427-32. [Abstract]
42. Nassar N, Roberts CL, Raynes-Greenow CH, et al. Evaluation of a decision aid for women with breech presentation at term: a randomised controlled trial [ISRCTN14570598]. BJOG. 2007 Mar;114(3):325-33. [Abstract] [Full Text]
43. Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
44. US Food & Drug Administration. FDA Drug Safety Communication: new warnings against use of terbutaline to treat preterm labor. Feb 2011 [internet publication]. [Full Text]
45. European Medicines Agency. Restrictions on use of short-acting beta-agonists in obstetric indications - CMDh endorses PRAC recommendations. October 2013 [internet publication]. [Full Text]
46. de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
47. Lydon-Rochelle M, Holt VL, Martin DP, et al. Association between method of delivery and maternal rehospitalisation. JAMA. 2000 May 10;283(18):2411-6. [Abstract]
48. Yokoe DS, Christiansen CL, Johnson R, et al. Epidemiology of and surveillance for postpartum infections. Emerg Infect Dis. 2001 Sep-Oct;7(5):837-41. [Abstract]
49. van Ham MA, van Dongen PW, Mulder J. Maternal consequences of caesarean section. A retrospective study of intra-operative and postoperative maternal complications of caesarean section during a 10-year period. Eur J Obstet Gynecol Reprod Biol. 1997 Jul;74(1):1-6. [Abstract]
50. Murphy DJ, Liebling RE, Verity L, et al. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: a cohort study. Lancet. 2001 Oct 13;358(9289):1203-7. [Abstract]
51. Lydon-Rochelle MT, Holt VL, Martin DP. Delivery method and self-reported postpartum general health status among primiparous women. Paediatr Perinat Epidemiol. 2001 Jul;15(3):232-40. [Abstract]
52. Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. Br J Obstet Gynaecol. 1996 Feb;103(2):154-61. [Abstract]
53. Persson J, Wolner-Hanssen P, Rydhstroem H. Obstetric risk factors for stress urinary incontinence: a population-based study. Obstet Gynecol. 2000 Sep;96(3):440-5. [Abstract]
54. MacLennan AH, Taylor AW, Wilson DH, et al. The prevalence of pelvic disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000 Dec;107(12):1460-70. [Abstract]
55. Thompson JF, Roberts CL, Currie M, et al. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002 Jun;29(2):83-94. [Abstract]
56. Australian Institute of Health and Welfare. Australia's mothers and babies 2015 - in brief. October 2017 [internet publication]. [Full Text]
57. Mutryn CS. Psychosocial impact of cesarean section on the family: a literature review. Soc Sci Med. 1993 Nov;37(10):1271-81. [Abstract]
58. DiMatteo MR, Morton SC, Lepper HS, et al. Cesarean childbirth and psychosocial outcomes: a meta-analysis. Health Psychol. 1996 Jul;15(4):303-14. [Abstract]
59. National Institute for Health and Care Excellence. Caesarean birth. Mar 2021 [internet publication]. [Full Text]
60. Greene R, Gardeit F, Turner MJ. Long-term implications of cesarean section. Am J Obstet Gynecol. 1997 Jan;176(1 Pt 1):254-5. [Abstract]
61. Coughlan C, Kearney R, Turner MJ. What are the implications for the next delivery in primigravidae who have an elective caesarean section for breech presentation? BJOG. 2002 Jun;109(6):624-6. [Abstract]
62. Hemminki E, Merilainen J. Long-term effects of cesarean sections: ectopic pregnancies and placental problems. Am J Obstet Gynecol. 1996 May;174(5):1569-74. [Abstract]
63. Gilliam M, Rosenberg D, Davis F. The likelihood of placenta previa with greater number of cesarean deliveries and higher parity. Obstet Gynecol. 2002 Jun;99(6):976-80. [Abstract]
64. Morrison JJ, Rennie JM, Milton PJ. Neonatal respiratory morbidity and mode of delivery at term: influence of timing of elective caesarean section. Br J Obstet Gynaecol. 1995 Feb;102(2):101-6. [Abstract]
65. Annibale DJ, Hulsey TC, Wagner CL, et al. Comparative neonatal morbidity of abdominal and vaginal deliveries after uncomplicated pregnancies. Arch Pediatr Adolesc Med. 1995 Aug;149(8):862-7. [Abstract]
66. Hook B, Kiwi R, Amini SB, et al. Neonatal morbidity after elective repeat cesarean section and trial of labor. Pediatrics. 1997 Sep;100(3 Pt 1):348-53. [Abstract]
67. Nassar N, Roberts CL, Cameron CA, et al. Outcomes of external cephalic version and breech presentation at term: an audit of deliveries at a Sydney tertiary obstetric hospital, 1997-2004. Acta Obstet Gynecol Scand. 2006;85(10):1231-8. [Abstract]
68. Nwosu EC, Walkinshaw S, Chia P, et al. Undiagnosed breech. Br J Obstet Gynaecol. 1993 Jun;100(6):531-5. [Abstract]
69. Flamm BL, Ruffini RM. Undetected breech presentation: impact on external version and cesarean rates. Am J Perinatol. 1998 May;15(5):287-9. [Abstract]
70. Cockburn J, Foong C, Cockburn P. Undiagnosed breech. Br J Obstet Gynaecol. 1994 Jul;101(7):648-9. [Abstract]
71. Leung WC, Pun TC, Wong WM. Undiagnosed breech revisited. Br J Obstet Gynaecol. 1999 Jul;106(7):638-41. [Abstract]
72. Berhan Y, Haileamlak A. The risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: a meta-analysis including observational studies. BJOG. 2016 Jan;123(1):49-57. [Abstract] [Full Text]
73. Wilcox C, Nassar N, Roberts C. Effectiveness of nifedipine tocolysis to facilitate external cephalic version: a systematic review. BJOG. 2011 Mar;118(4):423-8. [Abstract]
74. Qureshi H, Massey E, Kirwan D, et al. BCSH guideline for the use of anti-D immunoglobulin for the prevention of haemolytic disease of the fetus and newborn. Transfus Med. 2014 Feb;24(1):8-20. [Abstract] [Full Text]
75. Hutton EK, Hofmeyr GJ, Dowswell T. External cephalic version for breech presentation before term. Cochrane Database Syst Rev. 2015 Jul 29;(7):CD000084. [Abstract] [Full Text]
76. Coyle ME, Smith CA, Peat B. Cephalic version by moxibustion for breech presentation. Cochrane Database Syst Rev. 2012 May 16;(5):CD003928. [Abstract] [Full Text]
77. Hofmeyr GJ, Kulier R. Cephalic version by postural management for breech presentation. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000051. [Abstract] [Full Text]
78. Hannah ME, Whyte H, Hannah WJ, et al. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):917-27. [Abstract]
79. Eide MG, Oyen N, Skjaerven R, et al. Breech delivery and Intelligence: a population-based study of 8,738 breech infants. Obstet Gynecol. 2005 Jan;105(1):4-11. [Abstract]
80. Whyte H, Hannah ME, Saigal S, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):864-71. [Abstract]
81. Brown S, Lumley J. Maternal health after childbirth: results of an Australian population based survey. Br J Obstet Gynaecol. 1998 Feb;105(2):156-61. [Abstract]
Published by
American College of Obstetricians and Gynecologists
2016 (reaffirmed 2022)
Royal College of Obstetricians and Gynaecologists (UK)
National Institute for Health and Care Excellence (UK)
Topic last updated: 2024-03-05
Natasha Nassar , PhD
Associate Professor
Menzies Centre for Health Policy
Sydney School of Public Health
University of Sydney
Christine L. Roberts , MBBS, FAFPHM, DrPH
Research Director
Clinical and Population Health Division
Perinatal Medicine Group
Kolling Institute of Medical Research
Jonathan Morris , MBChB, FRANZCOG, PhD
Professor of Obstetrics and Gynaecology and Head of Department
Peer Reviewers
John W. Bachman , MD
Consultant in Family Medicine
Department of Family Medicine
Mayo Clinic
Rhona Hughes , MBChB
Lead Obstetrician
Lothian Simpson Centre for Reproductive Health
The Royal Infirmary
Brian Peat , MD
Director of Obstetrics
Women's and Children's Hospital
North Adelaide
South Australia
Lelia Duley , MBChB
Professor of Obstetric Epidemiology
University of Leeds
Bradford Institute of Health Research
Temple Bank House
Bradford Royal Infirmary
Justus Hofmeyr , MD
Head of the Department of Obstetrics and Gynaecology
East London Private Hospital
East London
South Africa
When viewing this topic in a different language, you may notice some differences in the way the content is structured, but it still reflects the latest evidence-based guidance.
Breech presentation
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head.
Associated with increased morbidity and mortality for the mother in terms of emergency caesarean section and placenta praevia; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence decreases as pregnancy progresses and by term occurs in 3% to 4% of singleton term pregnancies.
Treatment options include external cephalic version to increase the likelihood of vaginal birth or a planned caesarean section, the optimal gestation being 37 and 39 weeks, respectively.
Planned caesarean section is considered the safest form of delivery for infants with a persisting breech presentation at term.
Breech presentation in pregnancy occurs when a baby presents with the buttocks or feet rather than the head first (cephalic presentation) and is associated with increased morbidity and mortality for both the mother and the baby. [1] Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997. [2] Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002. There is good current evidence regarding effective management of breech presentation in late pregnancy using external cephalic version and/or planned caesarean section.
History and exam
Key diagnostic factors.
- presence of risk factors
- buttocks or feet as the presenting part
- fetal head under costal margin
- fetal heartbeat above the maternal umbilicus
Other diagnostic factors
- subcostal tenderness
- pelvic or bladder pain
Risk factors
- premature fetus
- small for gestational age fetus
- nulliparity
- fetal congenital anomalies
- previous breech delivery
- uterine abnormalities
- abnormal amniotic fluid volume
- placental abnormalities
- female fetus
Diagnostic investigations
1st investigations to order.
- transabdominal/transvaginal ultrasound
Treatment algorithm
<37 weeks' gestation and in labour, ≥37 weeks' gestation not in labour, ≥37 weeks' gestation in labour: no imminent delivery, ≥37 weeks' gestation in labour: imminent delivery, contributors, natasha nassar, phd.
Associate Professor
Menzies Centre for Health Policy
Sydney School of Public Health
University of Sydney
Disclosures
NN has received salary support from Australian National Health and a Medical Research Council Career Development Fellowship; she is an author of a number of references cited in this topic.
Christine L. Roberts, MBBS, FAFPHM, DrPH
Research Director
Clinical and Population Health Division
Perinatal Medicine Group
Kolling Institute of Medical Research
CLR declares that she has no competing interests.
Jonathan Morris, MBChB, FRANZCOG, PhD
Professor of Obstetrics and Gynaecology and Head of Department
JM declares that he has no competing interests.
Peer reviewers
John w. bachman, md.
Consultant in Family Medicine
Department of Family Medicine
Mayo Clinic
JWB declares that he has no competing interests.
Rhona Hughes, MBChB
Lead Obstetrician
Lothian Simpson Centre for Reproductive Health
The Royal Infirmary
RH declares that she has no competing interests.
Brian Peat, MD
Director of Obstetrics
Women's and Children's Hospital
North Adelaide
South Australia
BP declares that he has no competing interests.
Lelia Duley, MBChB
Professor of Obstetric Epidemiology
University of Leeds
Bradford Institute of Health Research
Temple Bank House
Bradford Royal Infirmary
LD declares that she has no competing interests.
Justus Hofmeyr, MD
Head of the Department of Obstetrics and Gynaecology
East London Private Hospital
East London
South Africa
JH is an author of a number of references cited in this topic.
Differentials
- Transverse lie
- Caesarean birth
- Mode of term singleton breech delivery
Use of this content is subject to our disclaimer
Help us improve BMJ Best Practice
Please complete all fields.
I have some feedback on:
We will respond to all feedback.
For any urgent enquiries please contact our customer services team who are ready to help with any problems.
Phone: +44 (0) 207 111 1105
Email: [email protected]
Your feedback has been submitted successfully.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Obstet Gynaecol India
- v.62(4); 2012 Aug

Delivery in Breech Presentation: The Decision Making
Department of Obstetrics and Gynaecology, Pt.J.N.M. Medical College and Dr. B.R.A.M Hospital, E-8, Shankar Nagar, Raipur, Chhattisgarh 492001 India
Nalini Mishra
Rajni dewangan.
To optimize the fetomaternal oucome using different modes of delivery in breech presentation.
Materials and Methods
265 women with different parity and gestational age having singleton breech were studied during Jan 2007 to Sep 2009 at Pt. J.N.M. Medical College and associated Dr. B.R.A.M. Hospital Raipur Chhattisgarh and were assigned to either planned or emergency cesarean section or trial of vaginal delivery after counseling. Fetomaternal outcome was compared in various modes of delivery.
Observations
Incidence of breech presentation was 2.1 %, prematurity was the most common cause. 113 (42.6 %) women delivered vaginally. 54 (20.4 %) were planned for cesarean section. Emergency cesarean section was done in 98 (37 %). Although perinatal morbidity and mortality was lower in caesarean section group as compared to vaginal delivery group, but the difference became statistically insignificant after adjustment for confounding factors. ( p = 0.14)
In view of insignificant difference in the fetomaternal outcome balanced decision about mode of delivery on a case by case basis will go a long way in improving both foetal and maternal outcome. Regular drill and conduct of vaginal breech delivery should be pursued in all maternity hospitals.
Introduction
About 3–4 % of all pregnancies have breech presentation at term. The management of term breech is highly controversial and varies among different institutions and even among different clinicians in the same institution. The decision to perform cesarean delivery is often based on personal experience or a fear of litigation.
From the historical perspective, vaginal delivery of the persistent breech presentation had been the tradition since the first century a . d . Intended vaginal delivery is the common practice in most developing countries. Probably, the obstetricians are also more conversant in the technique of assisted breech delivery. This protocol received a major setback in the year 2000 when Lancet published the results of the Term Breech Trial by Mary E Hannah, which clearly concluded that planned cesarean section is better than planned vaginal birth for the term fetus with breech presentation in terms of neonatal outcome [ 1 ]. Serious maternal complication was similar between the two groups. It evoked stinging criticism, itemizing the methodological errors and unsupportable conclusions [ 2 ]. There is an urgent need to evaluate it in context of the resource poor countries before accepting it as the “Last word.” An overall policy of planned cesarean section in all term breeches would prevent complications of vaginal delivery because there would be no vaginal breech delivery. This might result in shifting of the contemporary art of conducting such delivery to the shelves of medical history. On further analysis of the Term Breech Trial, an important interaction involved a country’s perinatal mortality rate. In the countries with a low perinatal mortality rate, planned cesarean section had much greater benefits for the infant, whereas in countries where the perinatal mortality rate is high, the same benefits were much lower than the entire group as a whole. As many as 39 additional cesareans might be needed to avoid one serious infant morbidity or death in comparison to as few as seven additional cesarean sections in countries with a low perinatal mortality rate. This important observation is much more pertinent in countries with limited facilities for cesarean section.
Unfortunately, the number of obstetricians able to conduct the vaginal breech delivery is declining quite fast. If the trend continues, what will happen when a woman with breech presentation at term gets admitted in advanced labor at a center where cesarean section cannot be performed urgently and the obstetrician present has never conducted a vaginal breech delivery? It will indeed be a very sad day for our specialty.
As the controversy continues, repeated evaluations and reviews of management in this subset of women are needed. The present study was conducted with an objective to optimize the perinatal outcome, while keeping the art of conducting and training vaginal breech deliveries alive.
A total of 265 women with singleton breech presentation with >28 weeks gestational age were included in the present study during the period from Jan 2007 to Sep. 2009 (33 months).
On admission, the demographic profile of the women, as well as a detailed menstrual and obstetric history, was noted. General, systemic, and obstetric examination was carried out. All women were subjected to a routine investigation and obstetric ultrasonography and afterward, they were assigned to either cesarean section (planned/emergency) or vaginal delivery on the basis of the obstetric examination (clinical and sonographical) and the presence of complicating factors. Women having standard indications of cesarean section in breech like fetopelvic disproportion, hyperextension of the head, footling presentation, and associated complications (medical or obstetric) were assigned to the planned cesarean section group, whereas the remaining women having term breech were given a trial of vaginal breech delivery. The plan of delivery for the both term and preterm breech was discussed with the women and their attendants because of limited beds in the intensive neonatal care unit as well as probable course and complication of vaginal delivery. A trial of vaginal delivery was given to those who consented to it.
Regular drills of vaginal breech delivery are conducted in the department. During a trial of vaginal delivery, monitoring of fetal heart rate and progress of labor was done. Assisted breech delivery was the method of choice, maintaining a principle of noninterference till the delivery of the scapula. The delivery of the extended arms was accomplished by Lovset’s method, whereas the delivery of the aftercoming head was conducted by the Burns Marshall Method or Mauriceau Smellie Veit maneuver. After delivery, the baby was attended by the pediatrician and the Apgar Score at 1 and 5 min was noted and the baby was admitted to the neonatal intensive care unit if needed.
If fetal distress and arrest of progress in labor were suspected, the women were taken for emergency cesarean section. All the mothers and newborns were followed up for 7 days in the postnatal period. Data regarding the fetomaternal outcome were analyzed. Comparisons were made in terms of morbidity and mortality between groups of mothers and infants stratified by the mode of delivery.
The incidence of breech presentation in the present study was 2.1 %. It varies from 3 to 4 % in various studies [ 3 – 8 ]. A majority of the women were unbooked (55.5 %) and nulliparous (40.4 %). 77.3 % women were having term pregnancy (Table 1 ).
Table 1
Demographic profile ( n = 265)
Overall, 113 (42.6 %) women delivered vaginally, a majority of these were term. Planned cesarean section was done in 54 (20.4 %) for indications shown in Table 2 . Since this is the largest teaching hospital in the state with a greater number of referrals, a majority of unbooked women get admitted in labor and therefore could not be assigned the mode of delivery before hand. Emergency cesarean section had to be resorted to in 98 (37 %) women for various indications. A comparatively larger number of women in our study delivered vaginally as compared to the Term Breech Trial (33.2 %) [ 1 ], and the difference was alarming from the largest series containing 10,0730 women with only 4.9 % delivering vaginally [ 6 ]. As we have a very limited neonatal intensive care unit, we motivated women with low birth weight babies to deliver vaginally, but only after obtaining due consent for the same. A large number of vaginal births provided us with the opportunity to train our residents to conduct the vaginal breech delivery and to avoid cesarean section, thereby reducing operative burden upon the already over-worked obstetrics units. It also prevented uterine scar in a woman whose dwindling chances of hospital delivery in the next pregnancy could have compromised her obstetric future.
Table 2
Mode of delivery (N-265)
The incidence of overall neonatal morbidity was 3.4 % (Table 3 ), out of which 2.3 % was present in the vaginal delivery group, but this subgroup was constituted mainly by preterm babies (5 out of 9). Damage to soft tissue was sustained equally by the preterm infants of both the vaginal and cesarean groups (2 each). Such damage can be attributed to the fact that delivering the infants even by cesarean section is essentially the process of breech extraction. None of the injuries were life threatening.
Table 3
Neonatal morbidity in relation to different modes of delivery (N-265)
p value of preterm vaginal versus preterm cesarean section = 0.08 (nonsignificant)
Table 4 shows the overall incidence of perinatal mortality in the present study; it is 51 (19.2 %), out of which 40 (15.8 %) were found in the vaginal delivery group with only 13 (4.9 %) term and 27 (10.9 %) preterm deliveries. Only one (0.4 %) fatality was found in the planned cesarean section group in contrast to 10 (3.9 %) in the emergency cesarean section group. Perinatal mortality, neonatal mortality, and neonatal morbidity were significantly lower for the planned cesarean section group than for the planned vaginal birth group as reported by the Term Breech Trial and others [ 1 , 6 , 8 – 10 ]. In our study also, the perinatal mortality seems to be significantly higher in the vaginal delivery group, but since the primary objective of the study was to see the effect of mode of delivery on perinatal outcome, we have reassessed the perinatal mortality after excluding 24 cases of women admitted with intrauterine fetal demise (which also included 11 with congenital malformation). The adjusted number of 16 (6 %) is not significantly greater than the 11 (4.2 %) in the cesarean section group.
Table 4
Perinatal mortality in correlation with different modes of delivery ( n = 265)
p value (after excluding intrauterine demised) of vaginal versus cesarean section = 0.24 (nonsignificant)
Prematurity was the largest factor contributing to perinatal mortality. After excluding 31 (11.7 %) preterm births, the statistical difference between the term breech delivery in the vaginal delivery versus the cesarean section was not significant ( p = 0.14), although definitely higher for the vaginal group. The planned cesarean group at term pregnancy had a significantly better perinatal outcome ( p = 0.001), but the emergency cesarean section group did not prove to have the same advantage.
There was no maternal death in either group. Maternal morbidity in the cesarean section group was 3.4 % and in the vaginal group, it was 4.2 %. The difference was not significant statistically ( p = 0.5).
Table 5 depicts the comparable data of various studies after the Term Breech trial and shows a gradually increasing trend toward vaginal breech delivery, although almost universally concluding planned cesarean section to be better for the perinatal outcome. Our study is also in accordance with them, but the opportunity to plan the mode of delivery before labor is not provided to the obstetrician in a referral hospital like ours, and emergency cesarean section yielded comparable results in terms of perinatal outcome, a point also made by others [ 7 , 11 , 12 ]. We therefore recommend a very balanced decision regarding the mode of delivery in the tertiary centers of developing countries.
Table 5
Comparison of fetomaternal outcomes in different studies
When assisted vaginal breech delivery is accomplished after proper selection and counseling for women with breech presentation, cesarean section in preterm as well as term pregnancy can be avoided because the difference in terms of perinatal mortality and morbidity rates is not significant statistically between the vaginal and overall cesarean section groups after adjustment for confounding factors like prematurity and intrauterine fetal demise. Planned cesarean section is undoubtedly better. In countries where the majority of cesarean sections for breech presentation are done in emergency, a trial of vaginal delivery yields comparable results. Therefore, it is concluded that the balanced decision about the mode of delivery on a case by case basis as well as conduct, training, and regular drills of assisted breech delivery will go a long way to optimize the outcome of breech presentation in countries like ours.

COMMENTS
raj kumar. This document discusses breech presentation, including its definition, types, diagnosis, and management. Some key points: - Breech presentation is when the buttocks or lower limbs present first. It occurs in 3.5% of term deliveries and up to 25% of preterm deliveries. - Types include complete breech, frank breech, and footling breech.
Breech presentation - Download as a PDF or view online for free. ... Definition , Incidence , Risk factors , Complications ,Fetal complications , Maternal complications , Management, ... Dive into the intricate world of cells with our detailed Slideshare presentation. This educational resource is designed to provide a thorough understanding of ...
Breech presentation occurs when the fetus lies longitudinally with the pelvic or podalic pole presenting at the birth canal instead of the head. It has an incidence of 3-15% depending on gestational age. There are various types of breech including complete, frank, and footling. Breech delivery can be managed through external cephalic version ...
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the ...
Presentation Transcript. Breech presentation or podalic:- when buttock of fetal occupies the lower segment of uterus, it is called breech presentation. Breech presentation occurs in 3-4% of all deliveries • Types of breech:- • 1. Full/Complete Breech (cannonball position) (5-10%) • 2. Incomplete Breech • 3. Frank Breech (pike position ...
Summary. Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head. Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal ...
Breech presentations can be categorized into three main types based on the position of the baby's legs and butocks: Frank breech: The most common type, where the baby's butocks are positioned to come out first, with flexed hips and extended knees. Complete breech: In this type, both the baby's hips and knees are flexed, with the butocks ...
What Causes Breech Presentation? - Only about 15% of breech presentations have an identifiable etiology.5 - Established risks for breech presentation are: Previous breech presentation pregnancy,5,6,7,8 Late or lack of antenatal care,8,9 Prematurity (<37 weeks gestation),6,7,8 Comparatively lower birth weight,8,9 and Congenital anomalies.8,9,10
Introduction. Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman's and the baby's health. The aim of this review is to determine the most ...
Overview. Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. The percentage of breech deliveries decreases with advancing gestational age from 22-25% of births prior to 28 weeks' gestation to 7-15% of births at 32 weeks' gestation to 3-4% of ...
breech-presentation.ppt. The course is designed to assists student to acquire comprehensive knowledge of the normal functions of the organ systems of the human body to facilitate understanding of physiological basis of health, identify alteration in functions and provide the student with the necessary physiological knowledge to practice nursing.
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
Breech presentation: clinical practice guideline from the French College of Gynaecologists and Obstetricians [2020] ... The lack of a standard definition of a footling breech is problematic because the term is open to interpretation and will invariably lead to a higher rate of C/S for breech in this setting, further limiting birth mode options ...
A complete breech is the least common type of breech presentation. Other Types of Mal Presentations The baby can also be in a transverse position, meaning that they're sideways in the uterus.
Breech presentation is common in early pregnancy and decreases with advancing gestational age, as most babies turn spontaneously to a cephalic presentation before birth. [ 3] [ 4] The prevalence at term in singleton pregnancies is 3% to 4% of all births. [ 1] [ 2] The prevalence prior to term at various gestations is as follows: [ 3] 33% of ...
Breech presentation. This document provides information on breech births, including definitions, types, diagnosis, and management. It begins with an introduction defining breech birth as birth where the baby exits the pelvis feet or buttocks first instead of head first. It then describes the different types of breech presentations (complete ...
Women who have a breech presentation at term following an unsuccessful or declined offer of ECV should be counselled on the risks and benefits of planned vaginal breech delivery versus planned caesarean section. ... deliveries in 174 units in France and Belgium over a 12-month period. The strict criteria included 'normal' (definition ...
Definition Breech presentation is the presentation in which the fetus is in longitudinal lie and its buttock is the lower most part . 3. Incidence 28 weeks…25% Term 2-3% 1/3 are undiagnosed in labour
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head. Associated with increased morbidity and mortality for the mother in terms of emergency caesarean section and placenta praevia; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence of breech presentation was 2.1 %, prematurity was the most common cause. 113 (42.6 %) women delivered vaginally. 54 (20.4 %) were planned for cesarean section. Emergency cesarean section was done in 98 (37 %). Although perinatal morbidity and mortality was lower in caesarean section group as compared to vaginal delivery group, but the ...
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face ...
Breech Delivery The essence of the vaginal breech delivery is allowing as much spontaneous delivery by uterine action and maternal effort as possible Operator intervention should be limited to the manoeuvres. Nuchal arms are present in 0-5% of vaginal breech deliveries and in 9% of breech extractions.
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head. Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal siz...