An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


Biological, Psychological, and Social Determinants of Depression: A Review of Recent Literature
Olivia remes.
1 Institute for Manufacturing, University of Cambridge, Cambridge CB3 0FS, UK
João Francisco Mendes
2 NOVA Medical School, Universidade NOVA de Lisboa, 1099-085 Lisbon, Portugal; ku.ca.mac@94cfj
Peter Templeton
3 IfM Engage Limited, Institute for Manufacturing, University of Cambridge, Cambridge CB3 0FS, UK; ku.ca.mac@32twp
4 The William Templeton Foundation for Young People’s Mental Health (YPMH), Cambridge CB2 0AH, UK
Associated Data
Depression is one of the leading causes of disability, and, if left unmanaged, it can increase the risk for suicide. The evidence base on the determinants of depression is fragmented, which makes the interpretation of the results across studies difficult. The objective of this study is to conduct a thorough synthesis of the literature assessing the biological, psychological, and social determinants of depression in order to piece together the puzzle of the key factors that are related to this condition. Titles and abstracts published between 2017 and 2020 were identified in PubMed, as well as Medline, Scopus, and PsycInfo. Key words relating to biological, social, and psychological determinants as well as depression were applied to the databases, and the screening and data charting of the documents took place. We included 470 documents in this literature review. The findings showed that there are a plethora of risk and protective factors (relating to biological, psychological, and social determinants) that are related to depression; these determinants are interlinked and influence depression outcomes through a web of causation. In this paper, we describe and present the vast, fragmented, and complex literature related to this topic. This review may be used to guide practice, public health efforts, policy, and research related to mental health and, specifically, depression.
1. Introduction
Depression is one of the most common mental health issues, with an estimated prevalence of 5% among adults [ 1 , 2 ]. Symptoms may include anhedonia, feelings of worthlessness, concentration and sleep difficulties, and suicidal ideation. According to the World Health Organization, depression is a leading cause of disability; research shows that it is a burdensome condition with a negative impact on educational trajectories, work performance, and other areas of life [ 1 , 3 ]. Depression can start early in the lifecourse and, if it remains unmanaged, may increase the risk for substance abuse, chronic conditions, such as cardiovascular disease, and premature mortality [ 4 , 5 , 6 , 7 , 8 ].
Treatment for depression exists, such as pharmacotherapy, cognitive behavioural therapy, and other modalities. A meta-analysis of randomized, placebo-controlled trials of patients shows that 56–60% of people respond well to active treatment with antidepressants (selective serotonin reuptake inhibitors, tricyclic antidepressants) [ 9 ]. However, pharmacotherapy may be associated with problems, such as side-effects, relapse issues, a potential duration of weeks until the medication starts working, and possible limited efficacy in mild cases [ 10 , 11 , 12 , 13 , 14 ]. Psychotherapy is also available, but access barriers can make it difficult for a number of people to get the necessary help.
Studies on depression have increased significantly over the past few decades. However, the literature remains fragmented and the interpretation of heterogeneous findings across studies and between fields is difficult. The cross-pollination of ideas between disciplines, such as genetics, neurology, immunology, and psychology, is limited. Reviews on the determinants of depression have been conducted, but they either focus exclusively on a particular set of determinants (ex. genetic risk factors [ 15 ]) or population sub-group (ex. children and adolescents [ 16 ]) or focus on characteristics measured predominantly at the individual level (ex. focus on social support, history of depression [ 17 ]) without taking the wider context (ex. area-level variables) into account. An integrated approach paying attention to key determinants from the biological, psychological, and social spheres, as well as key themes, such as the lifecourse perspective, enables clinicians and public health authorities to develop tailored, person-centred approaches.
The primary aim of this literature review: to address the aforementioned challenges, we have synthesized recent research on the biological, psychological, and social determinants of depression and we have reviewed research from fields including genetics, immunology, neurology, psychology, public health, and epidemiology, among others.
The subsidiary aim: we have paid special attention to important themes, including the lifecourse perspective and interactions between determinants, to guide further efforts by public health and medical professionals.
This literature review can be used as an evidence base by those in public health and the clinical setting and can be used to inform targeted interventions.
2. Materials and Methods
We conducted a review of the literature on the biological, psychological, and social determinants of depression in the last 4 years. We decided to focus on these determinants after discussions with academics (from the Manchester Metropolitan University, University of Cardiff, University of Colorado, Boulder, University of Cork, University of Leuven, University of Texas), charity representatives, and people with lived experience at workshops held by the University of Cambridge in 2020. In several aspects, we attempted to conduct this review according to PRISMA guidelines [ 18 ].
The inclusion and exclusion criteria are the following:
- - We included documents, such as primary studies, literature reviews, systematic reviews, meta-analyses, reports, and commentaries on the determinants of depression. The determinants refer to variables that appear to be linked to the development of depression, such as physiological factors (e.g., the nervous system, genetics), but also factors that are further away or more distal to the condition. Determinants may be risk or protective factors, and individual- or wider-area-level variables.
- - We focused on major depressive disorder, treatment-resistant depression, dysthymia, depressive symptoms, poststroke depression, perinatal depression, as well as depressive-like behaviour (common in animal studies), among others.
- - We included papers regardless of the measurement methods of depression.
- - We included papers that focused on human and/or rodent research.
- - This review focused on articles written in the English language.
- - Documents published between 2017–2020 were captured to provide an understanding of the latest research on this topic.
- - Studies that assessed depression as a comorbidity or secondary to another disorder.
- - Studies that did not focus on rodent and/or human research.
- - Studies that focused on the treatment of depression. We made this decision, because this is an in-depth topic that would warrant a separate stand-alone review.
- Next, we searched PubMed (2017–2020) using keywords related to depression and determinants. Appendix A contains the search strategy used. We also conducted focused searches in Medline, Scopus, and PsycInfo (2017–2020).
- Once the documents were identified through the databases, the inclusion and exclusion criteria were applied to the titles and abstracts. Screening of documents was conducted by O.R., and a subsample was screened by J.M.; any discrepancies were resolved through a communication process.
- The full texts of documents were retrieved, and the inclusion and exclusion criteria were again applied. A subsample of documents underwent double screening by two authors (O.R., J.M.); again, any discrepancies were resolved through communication.
- a. A data charting form was created to capture the data elements of interest, including the authors, titles, determinants (biological, psychological, social), and the type of depression assessed by the research (e.g., major depression, depressive symptoms, depressive behaviour).
- b. The data charting form was piloted on a subset of documents, and refinements to it were made. The data charting form was created with the data elements described above and tested in 20 studies to determine whether refinements in the wording or language were needed.
- c. Data charting was conducted on the documents.
- d. Narrative analysis was conducted on the data charting table to identify key themes. When a particular finding was noted more than once, it was logged as a potential theme, with a review of these notes yielding key themes that appeared on multiple occasions. When key themes were identified, one researcher (O.R.) reviewed each document pertaining to that theme and derived concepts (key determinants and related outcomes). This process (a subsample) was verified by a second author (J.M.), and the two authors resolved any discrepancies through communication. Key themes were also checked as to whether they were of major significance to public mental health and at the forefront of public health discourse according to consultations we held with stakeholders from the Manchester Metropolitan University, University of Cardiff, University of Colorado, Boulder, University of Cork, University of Leuven, University of Texas, charity representatives, and people with lived experience at workshops held by the University of Cambridge in 2020.
We condensed the extensive information gleaned through our review into short summaries (with key points boxes for ease of understanding and interpretation of the data).
Through the searches, 6335 documents, such as primary studies, literature reviews, systematic reviews, meta-analyses, reports, and commentaries, were identified. After applying the inclusion and exclusion criteria, 470 papers were included in this review ( Supplementary Table S1 ). We focused on aspects related to biological, psychological, and social determinants of depression (examples of determinants and related outcomes are provided under each of the following sections.
3.1. Biological Factors
The following aspects will be discussed in this section: physical health conditions; then specific biological factors, including genetics; the microbiome; inflammatory factors; stress and hypothalamic–pituitary–adrenal (HPA) axis dysfunction, and the kynurenine pathway. Finally, aspects related to cognition will also be discussed in the context of depression.
3.1.1. Physical Health Conditions
Studies on physical health conditions—key points:
- The presence of a physical health condition can increase the risk for depression
- Psychological evaluation in physically sick populations is needed
- There is large heterogeneity in study design and measurement; this makes the comparison of findings between and across studies difficult
A number of studies examined the links between the outcome of depression and physical health-related factors, such as bladder outlet obstruction, cerebral atrophy, cataract, stroke, epilepsy, body mass index and obesity, diabetes, urinary tract infection, forms of cancer, inflammatory bowel disorder, glaucoma, acne, urea accumulation, cerebral small vessel disease, traumatic brain injury, and disability in multiple sclerosis [ 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 ]. For example, bladder outlet obstruction has been linked to inflammation and depressive behaviour in rodent research [ 24 ]. The presence of head and neck cancer also seemed to be related to an increased risk for depressive disorder [ 45 ]. Gestational diabetes mellitus has been linked to depressive symptoms in the postpartum period (but no association has been found with depression in the third pregnancy trimester) [ 50 ], and a plethora of other such examples of relationships between depression and physical conditions exist. As such, the assessment of psychopathology and the provision of support are necessary in individuals of ill health [ 45 ]. Despite the large evidence base on physical health-related factors, differences in study methodology and design, the lack of standardization when it comes to the measurement of various physical health conditions and depression, and heterogeneity in the study populations makes it difficult to compare studies [ 50 ].
The next subsections discuss specific biological factors, including genetics; the microbiome; inflammatory factors; stress and hypothalamic–pituitary–adrenal (HPA) axis dysfunction, and the kynurenine pathway; and aspects related to cognition.
3.1.2. Genetics
Studies on genetics—key points:
There were associations between genetic factors and depression; for example:
- The brain-derived neurotrophic factor (BDNF) plays an important role in depression
- Links exist between major histocompatibility complex region genes, as well as various gene polymorphisms and depression
- Single nucleotide polymorphisms (SNPs) of genes involved in the tryptophan catabolites pathway are of interest in relation to depression
A number of genetic-related factors, genomic regions, polymorphisms, and other related aspects have been examined with respect to depression [ 61 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 ]. The influence of BDNF in relation to depression has been amply studied [ 117 , 118 , 141 , 142 , 143 ]. Research has shown associations between depression and BDNF (as well as candidate SNPs of the BDNF gene, polymorphisms of the BDNF gene, and the interaction of these polymorphisms with other determinants, such as stress) [ 129 , 144 , 145 ]. Specific findings have been reported: for example, a study reported a link between the BDNF rs6265 allele (A) and major depressive disorder [ 117 ].
Other research focused on major histocompatibility complex region genes, endocannabinoid receptor gene polymorphisms, as well as tissue-specific genes and gene co-expression networks and their links to depression [ 99 , 110 , 112 ]. The SNPs of genes involved in the tryptophan catabolites pathway have also been of interest when studying the pathogenesis of depression.
The results from genetics studies are compelling; however, the findings remain mixed. One study indicated no support for depression candidate gene findings [ 122 ]. Another study found no association between specific polymorphisms and major depressive disorder [ 132 ]. As such, further research using larger samples is needed to corroborate the statistically significant associations reported in the literature.
3.1.3. Microbiome
Studies on the microbiome—key points:
- The gut bacteria and the brain communicate via both direct and indirect pathways called the gut-microbiota-brain axis (the bidirectional communication networks between the central nervous system and the gastrointestinal tract; this axis plays an important role in maintaining homeostasis).
- A disordered microbiome can lead to inflammation, which can then lead to depression
- There are possible links between the gut microbiome, host liver metabolism, brain inflammation, and depression
The common themes of this review have focused on the microbiome/microbiota or gut metabolome [ 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 ], the microbiota-gut-brain axis, and related factors [ 152 , 162 , 163 , 164 , 165 , 166 , 167 ]. When there is an imbalance in the intestinal bacteria, this can interfere with emotional regulation and contribute to harmful inflammatory processes and mood disorders [ 148 , 151 , 153 , 155 , 157 ]. Rodent research has shown that there may be a bidirectional association between the gut microbiota and depression: a disordered gut microbiota can play a role in the onset of this mental health problem, but, at the same time, the existence of stress and depression may also lead to a lower level of richness and diversity in the microbiome [ 158 ].
Research has also attempted to disentangle the links between the gut microbiome, host liver metabolism, brain inflammation, and depression, as well as the role of the ratio of lactobacillus to clostridium [ 152 ]. The literature has also examined the links between medication, such as antibiotics, and mood and behaviour, with the findings showing that antibiotics may be related to depression [ 159 , 168 ]. The links between the microbiome and depression are complex, and further studies are needed to determine the underpinning causal mechanisms.
3.1.4. Inflammation
Studies on inflammation—key points:
- Pro-inflammatory cytokines are linked to depression
- Pro-inflammatory cytokines, such as the tumour necrosis factor (TNF)-alpha, may play an important role
- Different methods of measurement are used, making the comparison of findings across studies difficult
Inflammation has been a theme in this literature review [ 60 , 161 , 164 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 ]. The findings show that raised levels of inflammation (because of factors such as pro-inflammatory cytokines) have been associated with depression [ 60 , 161 , 174 , 175 , 178 ]. For example, pro-inflammatory cytokines, such as tumour necrosis factor (TNF)-alpha, have been linked to depression [ 185 ]. Various determinants, such as early life stress, have also been linked to systemic inflammation, and this can increase the risk for depression [ 186 ].
Nevertheless, not everyone with elevated inflammation develops depression; therefore, this is just one route out of many linked to pathogenesis. Despite the compelling evidence reported with respect to inflammation, it is difficult to compare the findings across studies because of different methods used to assess depression and its risk factors.
3.1.5. Stress and HPA Axis Dysfunction
Studies on stress and HPA axis dysfunction—key points:
- Stress is linked to the release of proinflammatory factors
- The dysregulation of the HPA axis is linked to depression
- Determinants are interlinked in a complex web of causation
Stress was studied in various forms in rodent populations and humans [ 144 , 145 , 155 , 174 , 176 , 180 , 185 , 186 , 187 , 188 , 189 , 190 , 191 , 192 , 193 , 194 , 195 , 196 , 197 , 198 , 199 , 200 , 201 , 202 , 203 , 204 , 205 , 206 , 207 , 208 , 209 , 210 , 211 ].
Although this section has some overlap with others (as is to be expected because all of these determinants and body systems are interlinked), a number of studies have focused on the impact of stress on mental health. Stress has been mentioned in the literature as a risk factor of poor mental health and has emerged as an important determinant of depression. The effects of this variable are wide-ranging, and a short discussion is warranted.
Stress has been linked to the release of inflammatory factors, as well as the development of depression [ 204 ]. When the stress is high or lasts for a long period of time, this may negatively impact the brain. Chronic stress can impact the dendrites and synapses of various neurons, and may be implicated in the pathway leading to major depressive disorder [ 114 ]. As a review by Uchida et al. indicates, stress may be associated with the “dysregulation of neuronal and synaptic plasticity” [ 114 ]. Even in rodent studies, stress has a negative impact: chronic and unpredictable stress (and other forms of tension or stress) have been linked to unusual behaviour and depression symptoms [ 114 ].
The depression process and related brain changes, however, have also been linked to the hyperactivity or dysregulation of the HPA axis [ 127 , 130 , 131 , 182 , 212 ]. One review indicates that a potential underpinning mechanism of depression relates to “HPA axis abnormalities involved in chronic stress” [ 213 ]. There is a complex relationship between the HPA axis, glucocorticoid receptors, epigenetic mechanisms, and psychiatric sequelae [ 130 , 212 ].
In terms of the relationship between the HPA axis and stress and their influence on depression, the diathesis–stress model offers an explanation: it could be that early stress plays a role in the hyperactivation of the HPA axis, thus creating a predisposition “towards a maladaptive reaction to stress”. When this predisposition then meets an acute stressor, depression may ensue; thus, in line with the diathesis–stress model, a pre-existing vulnerability and stressor can create fertile ground for a mood disorder [ 213 ]. An integrated review by Dean and Keshavan [ 213 ] suggests that HPA axis hyperactivity is, in turn, related to other determinants, such as early deprivation and insecure early attachment; this again shows the complex web of causation between the different determinants.
3.1.6. Kynurenine Pathway
Studies on the kynurenine pathway—key points:
- The kynurenine pathway is linked to depression
- Indolamine 2,3-dioxegenase (IDO) polymorphisms are linked to postpartum depression
The kynurenine pathway was another theme that emerged in this review [ 120 , 178 , 181 , 184 , 214 , 215 , 216 , 217 , 218 , 219 , 220 , 221 ]. The kynurenine pathway has been implicated not only in general depressed mood (inflammation-induced depression) [ 184 , 214 , 219 ] but also postpartum depression [ 120 ]. When the kynurenine metabolism pathway is activated, this results in metabolites, which are neurotoxic.
A review by Jeon et al. notes a link between the impairment of the kynurenine pathway and inflammation-induced depression (triggered by treatment for various physical diseases, such as malignancy). The authors note that this could represent an important opportunity for immunopharmacology [ 214 ]. Another review by Danzer et al. suggests links between the inflammation-induced activation of indolamine 2,3-dioxegenase (the enzyme that converts tryptophan to kynurenine), the kynurenine metabolism pathway, and depression, and also remarks about the “opportunities for treatment of inflammation-induced depression” [ 184 ].
3.1.7. Cognition
Studies on cognition and the brain—key points:
- Cognitive decline and cognitive deficits are linked to increased depression risk
- Cognitive reserve is important in the disability/depression relationship
- Family history of cognitive impairment is linked to depression
A number of studies have focused on the theme of cognition and the brain. The results show that factors, such as low cognitive ability/function, cognitive vulnerability, cognitive impairment or deficits, subjective cognitive decline, regression of dendritic branching and hippocampal atrophy/death of hippocampal cells, impaired neuroplasticity, and neurogenesis-related aspects, have been linked to depression [ 131 , 212 , 222 , 223 , 224 , 225 , 226 , 227 , 228 , 229 , 230 , 231 , 232 , 233 , 234 , 235 , 236 , 237 , 238 , 239 ]. The cognitive reserve appears to act as a moderator and can magnify the impact of certain determinants on poor mental health. For example, in a study in which participants with multiple sclerosis also had low cognitive reserve, disability was shown to increase the risk for depression [ 63 ]. Cognitive deficits can be both causal and resultant in depression. A study on individuals attending outpatient stroke clinics showed that lower scores in cognition were related to depression; thus, cognitive impairment appears to be associated with depressive symptomatology [ 226 ]. Further, Halahakoon et al. [ 222 ] note a meta-analysis [ 240 ] that shows that a family history of cognitive impairment (in first degree relatives) is also linked to depression.
In addition to cognitive deficits, low-level cognitive ability [ 231 ] and cognitive vulnerability [ 232 ] have also been linked to depression. While cognitive impairment may be implicated in the pathogenesis of depressive symptoms [ 222 ], negative information processing biases are also important; according to the ‘cognitive neuropsychological’ model of depression, negative affective biases play a central part in the development of depression [ 222 , 241 ]. Nevertheless, the evidence on this topic is mixed and further work is needed to determine the underpinning mechanisms between these states.
3.2. Psychological Factors
Studies on psychological factors—key points:
- There are many affective risk factors linked to depression
- Determinants of depression include negative self-concept, sensitivity to rejection, neuroticism, rumination, negative emotionality, and others
A number of studies have been undertaken on the psychological factors linked to depression (including mastery, self-esteem, optimism, negative self-image, current or past mental health conditions, and various other aspects, including neuroticism, brooding, conflict, negative thinking, insight, cognitive fusion, emotional clarity, rumination, dysfunctional attitudes, interpretation bias, and attachment style) [ 66 , 128 , 140 , 205 , 210 , 228 , 235 , 242 , 243 , 244 , 245 , 246 , 247 , 248 , 249 , 250 , 251 , 252 , 253 , 254 , 255 , 256 , 257 , 258 , 259 , 260 , 261 , 262 , 263 , 264 , 265 , 266 , 267 , 268 , 269 , 270 , 271 , 272 , 273 , 274 , 275 , 276 , 277 , 278 , 279 , 280 , 281 , 282 , 283 , 284 , 285 , 286 , 287 , 288 , 289 , 290 ]. Determinants related to this condition include low self-esteem and shame, among other factors [ 269 , 270 , 275 , 278 ]. Several emotional states and traits, such as neuroticism [ 235 , 260 , 271 , 278 ], negative self-concept (with self-perceptions of worthlessness and uselessness), and negative interpretation or attention biases have been linked to depression [ 261 , 271 , 282 , 283 , 286 ]. Moreover, low emotional clarity has been associated with depression [ 267 ]. When it comes to the severity of the disorder, it appears that meta-emotions (“emotions that occur in response to other emotions (e.g., guilt about anger)” [ 268 ]) have a role to play in depression [ 268 ].
A determinant that has received much attention in mental health research concerns rumination. Rumination has been presented as a mediator but also as a risk factor for depression [ 57 , 210 , 259 ]. When studied as a risk factor, it appears that the relationship of rumination with depression is mediated by variables that include limited problem-solving ability and insufficient social support [ 259 ]. However, rumination also appears to act as a mediator: for example, this variable (particularly brooding rumination) lies on the causal pathway between poor attention control and depression [ 265 ]. This shows that determinants may present in several forms: as moderators or mediators, risk factors or outcomes, and this is why disentangling the relationships between the various factors linked to depression is a complex task.
The psychological determinants are commonly researched variables in the mental health literature. A wide range of factors have been linked to depression, such as the aforementioned determinants, but also: (low) optimism levels, maladaptive coping (such as avoidance), body image issues, and maladaptive perfectionism, among others [ 269 , 270 , 272 , 273 , 275 , 276 , 279 , 285 , 286 ]. Various mechanisms have been proposed to explain the way these determinants increase the risk for depression. One of the underpinning mechanisms linking the determinants and depression concerns coping. For example, positive fantasy engagement, cognitive biases, or personality dispositions may lead to emotion-focused coping, such as brooding, and subsequently increase the risk for depression [ 272 , 284 , 287 ]. Knowing the causal mechanisms linking the determinants to outcomes provides insight for the development of targeted interventions.
3.3. Social Determinants
Studies on social determinants—key points:
- Social determinants are the conditions in the environments where people are born, live, learn, work, play, etc.; these influence (mental) health [ 291 ]
- There are many social determinants linked to depression, such as sociodemographics, social support, adverse childhood experiences
- Determinants can be at the individual, social network, community, and societal levels
Studies also focused on the social determinants of (mental) health; these are the conditions in which people are born, live, learn, work, play, and age, and have a significant influence on wellbeing [ 291 ]. Factors such as age, social or socioeconomic status, social support, financial strain and deprivation, food insecurity, education, employment status, living arrangements, marital status, race, childhood conflict and bullying, violent crime exposure, abuse, discrimination, (self)-stigma, ethnicity and migrant status, working conditions, adverse or significant life events, illiteracy or health literacy, environmental events, job strain, and the built environment have been linked to depression, among others [ 52 , 133 , 235 , 236 , 239 , 252 , 269 , 280 , 292 , 293 , 294 , 295 , 296 , 297 , 298 , 299 , 300 , 301 , 302 , 303 , 304 , 305 , 306 , 307 , 308 , 309 , 310 , 311 , 312 , 313 , 314 , 315 , 316 , 317 , 318 , 319 , 320 , 321 , 322 , 323 , 324 , 325 , 326 , 327 , 328 , 329 , 330 , 331 , 332 , 333 , 334 , 335 , 336 , 337 , 338 , 339 , 340 , 341 , 342 , 343 , 344 , 345 , 346 , 347 , 348 , 349 , 350 , 351 , 352 , 353 , 354 , 355 , 356 , 357 , 358 , 359 , 360 , 361 , 362 , 363 , 364 , 365 , 366 , 367 , 368 , 369 , 370 , 371 ]. Social support and cohesion, as well as structural social capital, have also been identified as determinants [ 140 , 228 , 239 , 269 , 293 , 372 , 373 , 374 , 375 , 376 , 377 , 378 , 379 ]. In a study, part of the findings showed that low levels of education have been shown to be linked to post-stroke depression (but not severe or clinical depression outcomes) [ 299 ]. A study within a systematic review indicated that having only primary education was associated with a higher risk of depression compared to having secondary or higher education (although another study contrasted this finding) [ 296 ]. Various studies on socioeconomic status-related factors have been undertaken [ 239 , 297 ]; the research has shown that a low level of education is linked to depression [ 297 ]. Low income is also related to depressive disorders [ 312 ]. By contrast, high levels of education and income are protective [ 335 ].
A group of determinants touched upon by several studies included adverse childhood or early life experiences: ex. conflict with parents, early exposure to traumatic life events, bullying and childhood trauma were found to increase the risk of depression (ex. through pathways, such as inflammation, interaction effects, or cognitive biases) [ 161 , 182 , 258 , 358 , 362 , 380 ].
Gender-related factors were also found to play an important role with respect to mental health [ 235 , 381 , 382 , 383 , 384 , 385 ]. Gender inequalities can start early on in the lifecourse, and women were found to be twice as likely to have depression as men. Gender-related factors were linked to cognitive biases, resilience and vulnerabilities [ 362 , 384 ].
Determinants can impact mental health outcomes through underpinning mechanisms. For example, harmful determinants can influence the uptake of risk behaviours. Risk behaviours, such as sedentary behaviour, substance abuse and smoking/nicotine exposure, have been linked to depression [ 226 , 335 , 355 , 385 , 386 , 387 , 388 , 389 , 390 , 391 , 392 , 393 , 394 , 395 , 396 , 397 , 398 , 399 , 400 , 401 ]. Harmful determinants can also have an impact on diet. Indeed, dietary aspects and diet components (ex. vitamin D, folate, selenium intake, iron, vitamin B12, vitamin K, fiber intake, zinc) as well as diet-related inflammatory potential have been linked to depression outcomes [ 161 , 208 , 236 , 312 , 396 , 402 , 403 , 404 , 405 , 406 , 407 , 408 , 409 , 410 , 411 , 412 , 413 , 414 , 415 , 416 , 417 , 418 , 419 , 420 , 421 , 422 , 423 , 424 , 425 , 426 , 427 , 428 ]. A poor diet has been linked to depression through mechanisms such as inflammation [ 428 ].
Again, it is difficult to constrict diet to the ‘social determinants of health’ category as it also relates to inflammation (biological determinants) and could even stand alone as its own category. Nevertheless, all of these factors are interlinked and influence one another in a complex web of causation, as mentioned elsewhere in the paper.
Supplementary Figure S1 contains a representation of key determinants acting at various levels: the individual, social network, community, and societal levels. The determinants have an influence on risk behaviours, and this, in turn, can affect the mood (i.e., depression), body processes (ex. can increase inflammation), and may negatively influence brain structure and function.
3.4. Others
Studies on ‘other’ determinants—key points:
- A number of factors are related to depression
- These may not be as easily categorized as the other determinants in this paper
A number of factors arose in this review that were related to depression; it was difficult to place these under a specific heading above, so this ‘other’ category was created. A number of these could be sorted under the ‘social determinants of depression’ category. For example, being exposed to deprivation, hardship, or adversity may increase the risk for air pollution exposure and nighttime shift work, among others, and the latter determinants have been found to increase the risk for depression. Air pollution could also be regarded as an ecologic-level (environmental) determinant of mental health.
Nevertheless, we have decided to leave these factors in a separate category (because their categorization may not be as immediately clear-cut as others), and these factors include: low-level light [ 429 ], weight cycling [ 430 ], water contaminants [ 431 ], trade [ 432 ], air pollution [ 433 , 434 ], program-level variables (ex. feedback and learning experience) [ 435 ], TV viewing [ 436 ], falls [ 437 ], various other biological factors [ 116 , 136 , 141 , 151 , 164 , 182 , 363 , 364 , 438 , 439 , 440 , 441 , 442 , 443 , 444 , 445 , 446 , 447 , 448 , 449 , 450 , 451 , 452 , 453 , 454 , 455 , 456 , 457 , 458 , 459 , 460 , 461 , 462 , 463 , 464 , 465 , 466 , 467 , 468 , 469 ], mobile phone use [ 470 ], ultrasound chronic exposure [ 471 ], nighttime shift work [ 472 ], work accidents [ 473 ], therapy enrollment [ 226 ], and exposure to light at night [ 474 ].
4. Cross-Cutting Themes
4.1. lifecourse perspective.
Studies on the lifecourse perspective—key points:
- Early life has an importance on mental health
- Stress has been linked to depression
- In old age, the decline in social capital is important
Trajectories and life events are important when it comes to the lifecourse perspective. Research has touched on the influence of prenatal or early life stress on an individual’s mental health trajectory [ 164 , 199 , 475 ]. Severe stress that occurs in the form of early-life trauma has also been associated with depressive symptoms [ 362 , 380 ]. It may be that some individuals exposed to trauma develop thoughts of personal failure, which then serve as a catalyst of depression [ 380 ].
At the other end of the life trajectory—old age—specific determinants have been linked to an increased risk for depression. Older people are at a heightened risk of losing their social networks, and structural social capital has been identified as important in relation to depression in old age [ 293 ].
4.2. Gene–Environment Interactions
Studies on gene–environment interactions—key points:
- The environment and genetics interact to increase the risk of depression
- The etiology of depression is multifactorial
- Adolescence is a time of vulnerability
A number of studies have touched on gene–environment interactions [ 72 , 77 , 82 , 119 , 381 , 476 , 477 , 478 , 479 , 480 , 481 ]. The interactions between genetic factors and determinants, such as negative life events (ex. relationship and social difficulties, serious illness, unemployment and financial crises) and stressors (ex. death of spouse, minor violations of law, neighbourhood socioeconomic status) have been studied in relation to depression [ 82 , 135 , 298 , 449 , 481 ]. A study reported an interaction of significant life events with functional variation in the serotonin-transporter-linked polymorphic region (5-HTTLPR) allele type (in the context of multiple sclerosis) and linked this to depression [ 361 ], while another reported an interaction between stress and 5-HTTLPR in relation to depression [ 480 ]. Other research reported that the genetic variation of HPA-axis genes has moderating effects on the relationship between stressors and depression [ 198 ]. Another study showed that early-life stress interacts with gene variants to increase the risk for depression [ 77 ].
Adolescence is a time of vulnerability [ 111 , 480 ]. Perceived parental support has been found to interact with genes (GABRR1, GABRR2), and this appears to be associated with depressive symptoms in adolescence [ 480 ]. It is important to pay special attention to critical periods in the lifecourse so that adequate support is provided to those who are most vulnerable.
The etiology of depression is multifactorial, and it is worthwhile to examine the interaction between multiple factors, such as epigenetic, genetic, and environmental factors, in order to truly understand this mental health condition. Finally, taking into account critical periods of life when assessing gene–environment interactions is important for developing targeted interventions.
5. Discussion
Depression is one of the most common mental health conditions, and, if left untreated, it can increase the risk for substance abuse, anxiety disorders, and suicide. In the past 20 years, a large number of studies on the risk and protective factors of depression have been undertaken in various fields, such as genetics, neurology, immunology, and epidemiology. However, there are limitations associated with the extant evidence base. The previous syntheses on depression are limited in scope and focus exclusively on social or biological factors, population sub-groups, or examine depression as a comorbidity (rather than an independent disorder). The research on the determinants and causal pathways of depression is fragmentated and heterogeneous, and this has not helped to stimulate progress when it comes to the prevention and intervention of this condition—specifically unravelling the complexity of the determinants related to this condition and thus refining the prevention and intervention methods.
The scope of this paper was to bring together the heterogeneous, vast, and fragmented literature on depression and paint a picture of the key factors that contribute to this condition. The findings from this review show that there are important themes when it comes to the determinants of depression, such as: the microbiome, dysregulation of the HPA axis, inflammatory reactions, the kynurenine pathway, as well as psychological and social factors. It may be that physical factors are proximal determinants of depression, which, in turn, are acted on by more distal social factors, such as deprivation, environmental events, and social capital.
The Marmot Report [ 291 ], the World Health Organization [ 482 ], and Compton et al. [ 483 ] highlight that the most disadvantaged segments of society are suffering (the socioeconomic context is important), and this inequality in resources has translated to inequality in mental health outcomes [ 483 ]. To tackle the issue of egalitarianism and restore equality in the health between the groups, the social determinants need to be addressed [ 483 ]. A wide range of determinants of mental health have been identified in the literature: age, gender, ethnicity, family upbringing and early attachment patterns, social support, access to food, water and proper nutrition, and community factors. People spiral downwards because of individual- and societal-level circumstances; therefore, these circumstances along with the interactions between the determinants need to be considered.
Another important theme in the mental health literature is the lifecourse perspective. This shows that the timing of events has significance when it comes to mental health. Early life is a critical period during the lifespan at which cognitive processes develop. Exposure to harmful determinants, such as stress, during this period can place an individual on a trajectory of depression in adulthood or later life. When an individual is exposed to harmful determinants during critical periods and is also genetically predisposed to depression, the risk for the disorder can be compounded. This is why aspects such as the lifecourse perspective and gene–environment interactions need to be taken into account. Insight into this can also help to refine targeted interventions.
A number of interventions for depression have been developed or recommended, addressing, for example, the physical factors described here and lifestyle modifications. Interventions targeting various factors, such as education and socioeconomic status, are needed to help prevent and reduce the burden of depression. Further research on the efficacy of various interventions is needed. Additional studies are also needed on each of the themes described in this paper, for example: the biological factors related to postpartum depression [ 134 ], and further work is needed on depression outcomes, such as chronic, recurrent depression [ 452 ]. Previous literature has shown that chronic stress (associated with depression) is also linked to glucocorticoid receptor resistance, as well as problems with the regulation of the inflammatory response [ 484 ]. Further work is needed on this and the underpinning mechanisms between the determinants and outcomes. This review highlighted the myriad ways of measuring depression and its determinants [ 66 , 85 , 281 , 298 , 451 , 485 ]. Thus, the standardization of the measurements of the outcomes (ex. a gold standard for measuring depression) and determinants is essential; this can facilitate comparisons of findings across studies.
5.1. Strengths
This paper has important strengths. It brings together the wide literature on depression and helps to bridge disciplines in relation to one of the most common mental health problems. We identified, selected, and extracted data from studies, and provided concise summaries.
5.2. Limitations
The limitations of the review include missing potentially important studies; however, this is a weakness that cannot be avoided by literature reviews. Nevertheless, the aim of the review was not to identify each study that has been conducted on the risk and protective factors of depression (which a single review is unable to capture) but rather to gain insight into the breadth of literature on this topic, highlight key biological, psychological, and social determinants, and shed light on important themes, such as the lifecourse perspective and gene–environment interactions.
6. Conclusions
We have reviewed the determinants of depression and recognize that there are a multitude of risk and protective factors at the individual and wider ecologic levels. These determinants are interlinked and influence one another. We have attempted to describe the wide literature on this topic, and we have brought to light major factors that are of public mental health significance. This review may be used as an evidence base by those in public health, clinical practice, and research.
This paper discusses key areas in depression research; however, an exhaustive discussion of all the risk factors and determinants linked to depression and their mechanisms is not possible in one journal article—which, by its very nature, a single paper cannot do. We have brought to light overarching factors linked to depression and a workable conceptual framework that may guide clinical and public health practice; however, we encourage other researchers to continue to expand on this timely and relevant work—particularly as depression is a top priority on the policy agenda now.
Acknowledgments
Thank you to Isla Kuhn for the help with the Medline, Scopus, and PsycInfo database searches.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/brainsci11121633/s1 , Figure S1: Conceptual framework: Determinants of depression, Table S1: Data charting—A selection of determinants from the literature.
Appendix A.1. Search Strategy
Search: ((((((((((((((((“Gene-Environment Interaction”[Majr]) OR (“Genetics”[Mesh])) OR (“Genome-Wide Association Study”[Majr])) OR (“Microbiota”[Mesh] OR “Gastrointestinal Microbiome”[Mesh])) OR (“Neurogenic Inflammation”[Mesh])) OR (“genetic determinant”)) OR (“gut-brain-axis”)) OR (“Kynurenine”[Majr])) OR (“Cognition”[Mesh])) OR (“Neuronal Plasticity”[Majr])) OR (“Neurogenesis”[Mesh])) OR (“Genes”[Mesh])) OR (“Neurology”[Majr])) OR (“Social Determinants of Health”[Majr])) OR (“Glucocorticoids”[Mesh])) OR (“Tryptophan”[Mesh])) AND (“Depression”[Mesh] OR “Depressive Disorder”[Mesh]) Filters: from 2017—2020.
Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R)
- exp *Depression/
- exp *Depressive Disorder/
- exp *”Social Determinants of Health”/
- exp *Tryptophan/
- exp *Glucocorticoids/
- exp *Neurology/
- exp *Genes/
- exp *Neurogenesis/
- exp *Neuronal Plasticity/
- exp *Kynurenine/
- exp *Genetics/
- exp *Neurogenic Inflammation/
- exp *Gastrointestinal Microbiome/
- exp *Genome-Wide Association Study/
- exp *Gene-Environment Interaction/
- exp *Depression/et [Etiology]
- exp *Depressive Disorder/et
- or/4-16 637368
- limit 22 to yr = “2017–Current”
- “cause* of depression”.mp.
- “cause* of depression”.ti.
- (cause adj3 (depression or depressive)).ti.
- (caus* adj3 (depression or depressive)).ti.
Appendix A.2. PsycInfo
(TITLE ( depression OR “ Depressive Disorder ”) AND TITLE (“ Social Determinants of Health ” OR tryptophan OR glucocorticoids OR neurology OR genes OR neurogenesis OR “ Neuronal Plasticity ” OR kynurenine OR genetics OR “ Neurogenic Inflammation ” OR “ Gastrointestinal Microbiome ” OR “ Genome-Wide Association Study ” OR “ Gene-Environment Interaction ” OR aetiology OR etiology )) OR TITLE ( cause* W/3 ( depression OR depressive )).
Author Contributions
O.R. was responsible for the design of the study and methodology undertaken. Despite P.T.’s involvement in YPMH, he had no role in the design of the study; P.T. was responsible for the conceptualization of the study. Validation was conducted by O.R. and J.F.M. Formal analysis (data charting) was undertaken by O.R. O.R. and P.T. were involved in the investigation, resource acquisition, and data presentation. The original draft preparation was undertaken by O.R. The writing was conducted by O.R., with review and editing by P.T. and J.F.M. Funding acquisition was undertaken by O.R. and P.T. All authors have read and agreed to the published version of the manuscript.
This research was funded by The William Templeton Foundation for Young People’s Mental Health, Cambridge Philosophical Society, and the Aviva Foundation.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Advertisement
Major Depressive Disorder: Advances in Neuroscience Research and Translational Applications
- Open access
- Published: 13 February 2021
- Volume 37 , pages 863–880, ( 2021 )
Cite this article
You have full access to this open access article

- Zezhi Li 1 , 2 ,
- Meihua Ruan 3 ,
- Jun Chen 1 , 5 &
- Yiru Fang ORCID: orcid.org/0000-0002-8748-9085 1 , 4 , 5
47k Accesses
112 Citations
16 Altmetric
Explore all metrics
A Correction to this article was published on 17 May 2021
This article has been updated
Major depressive disorder (MDD), also referred to as depression, is one of the most common psychiatric disorders with a high economic burden. The etiology of depression is still not clear, but it is generally believed that MDD is a multifactorial disease caused by the interaction of social, psychological, and biological aspects. Therefore, there is no exact pathological theory that can independently explain its pathogenesis, involving genetics, neurobiology, and neuroimaging. At present, there are many treatment measures for patients with depression, including drug therapy, psychotherapy, and neuromodulation technology. In recent years, great progress has been made in the development of new antidepressants, some of which have been applied in the clinic. This article mainly reviews the research progress, pathogenesis, and treatment of MDD.
Similar content being viewed by others

Dopamine: Functions, Signaling, and Association with Neurological Diseases

Molecular Mechanisms of Psilocybin and Implications for the Treatment of Depression
Lavender oil preparation Silexan is effective in mild-to-moderate major depression: a randomized, placebo- and reference-controlled trial
Avoid common mistakes on your manuscript.
Major depressive disorder (MDD) also referred to as depression, is one of the most severe and common psychiatric disorders across the world. It is characterized by persistent sadness, loss of interest or pleasure, low energy, worse appetite and sleep, and even suicide, disrupting daily activities and psychosocial functions. Depression has an extreme global economic burden and has been listed as the third largest cause of disease burden by the World Health Organization since 2008, and is expected to rank the first by 2030 [ 1 , 2 ]. In 2016, the Global Burden of Diseases, Injuries, and Risk Factors Study demonstrated that depression caused 34.1 million of the total years lived with disability (YLDs), ranking as the fifth largest cause of YLD [ 3 ]. Therefore, the research progress and the clinical application of new discoveries or new technologies are imminent. In this review, we mainly discuss the current situation of research, developments in pathogenesis, and the management of depression.
Current Situation of Research on Depression
Analysis of published papers.
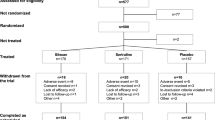
In the past decade, the total number of papers on depression published worldwide has increased year by year as shown in Fig. 1 A. Searching the Web of Science database, we found a total of 43,863 papers published in the field of depression from 2009 to 2019 (search strategy: TI = (depression$) or ts = ("major depressive disorder$")) and py = (2009 – 2019), Articles). The top 10 countries that published papers on the topic of depression are shown in Fig. 1 B. Among them, researchers in the USA published the most papers, followed by China. Compared with the USA, the gap in the total number of papers published in China is gradually narrowing (Fig. 1 C), but the quality gap reflected by the index (the total number of citations and the number of citations per paper) is still large, and is lower than the global average (Fig. 1 D). As shown in Fig. 1 E, the hot research topics in depression are as follows: depression management in primary care, interventions to prevent depression, the pathogenesis of depression, comorbidity of depression and other diseases, the risks of depression, neuroimaging studies of depression, and antidepressant treatment.
Analysis of published papers around the world from 2009 to 2019 in depressive disorder. A The total number of papers [from a search of the Web of Science database (search strategy: TI = (depression$) or ts = ("major depressive disorder$")) and py = (2009 – 2019), Articles)]. B The top 10 countries publishing on the topic. C Comparison of papers in China and the USA. D Citations for the top 10 countries and comparison with the global average. E Hot topics.
Analysis of Patented Technology Application
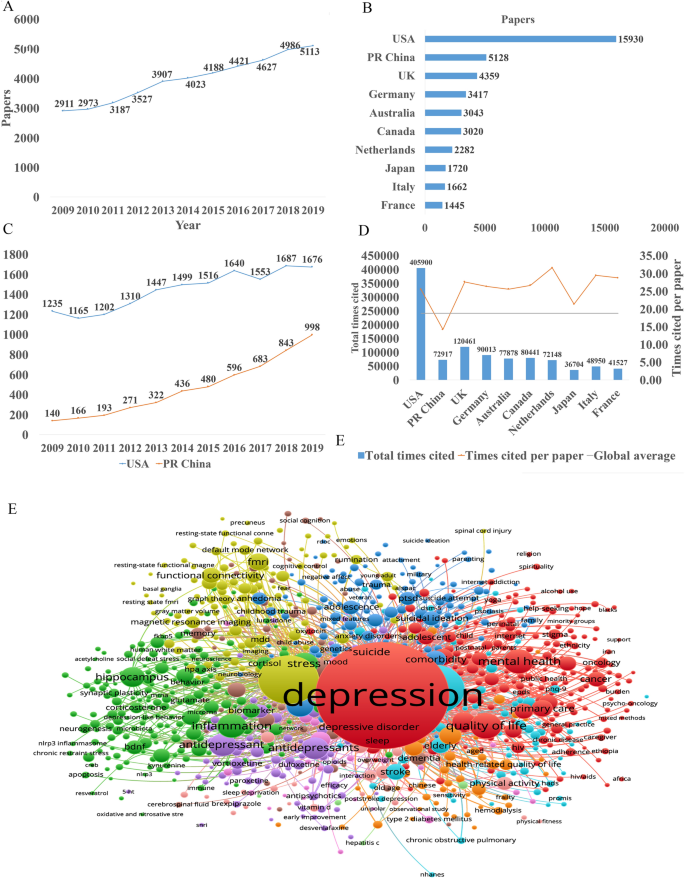
There were 16,228 patent applications in the field of depression between 2009 and 2019, according to the Derwent Innovation Patent database. The annual number and trend of these patents are shown in Fig. 2 A. The top 10 countries applying for patents related to depression are shown in Fig. 2 B. The USA ranks first in the number of depression-related patent applications, followed by China. The largest number of patents related to depression is the development of antidepressants, and drugs for neurodegenerative diseases such as dementia comorbid with depression. The top 10 technological areas of patents related to depression are shown in Fig. 2 C, and the trend in these areas have been stable over the past decade (Fig. 2 D).
Analysis of patented technology applications from 2009 to 2019 in the field of depressive disorder. A Annual numbers and trends of patents (the Derwent Innovation patent database). B The top 10 countries/regions applying for patents. C The top 10 technological areas of patents. D The trend of patent assignees. E Global hot topic areas of patents.
Analysis of technical hotspots based on keyword clustering was conducted from the Derwent Innovation database using the "ThemeScape" tool. This demonstrated that the hot topic areas are as follows (Fig. 2 E): (1) improvement for formulation and the efficiency of hydrobromide, as well as optimization of the dosage; intervention for depression comorbid with AD, diabetes, and others; (3) development of alkyl drugs; (4) development of pharmaceutical acceptable salts as antidepressants; (5) innovation of the preparation of antidepressants; (6) development of novel antidepressants based on neurotransmitters; (7) development of compositions based on nicotinic acetylcholine receptors; and (8) intervention for depression with traditional Chinese medicine.
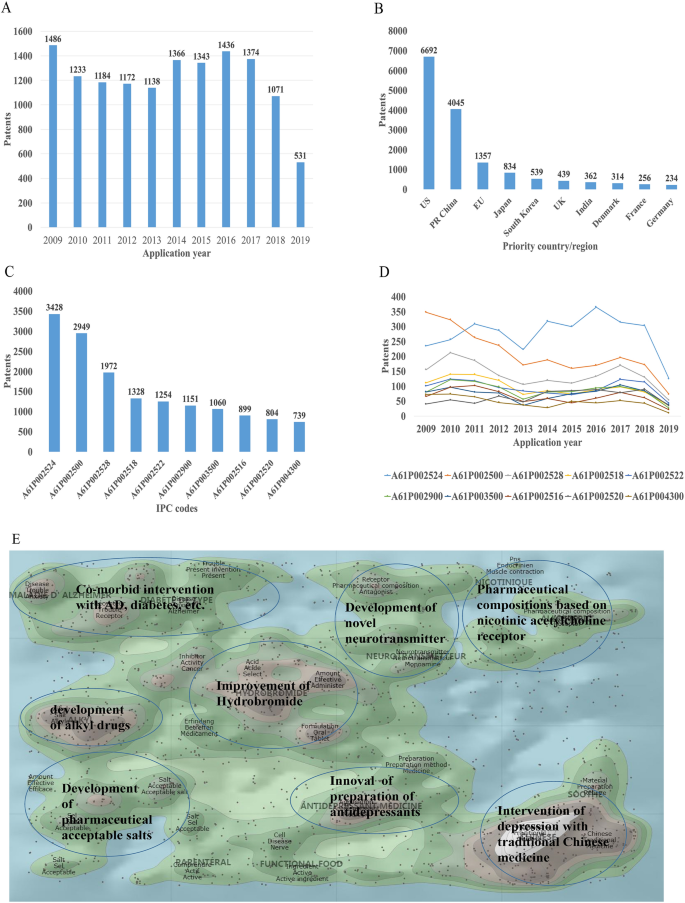
Analysis of Clinical Trial
There are 6,516 clinical trials in the field of depression in the ClinicalTrials.gov database, and among them, 1,737 valid trials include the ongoing recruitment of subjects, upcoming recruitment of subjects, and ongoing clinical trials. These clinical trials are mainly distributed in the USA (802 trials), Canada (155), China (114), France (93), Germany (66), UK (62), Spain (58), Denmark (41), Sweden (39), and Switzerland (23). The indications for clinical trials include various types of depression, such as minor depression, depression, severe depression, perinatal depression, postpartum depression, and depression comorbid with other psychiatric disorders or physical diseases, such as schizophrenia, epilepsy, stroke, cancer, diabetes, cardiovascular disease, and Parkinson's disease.
Based on the database of the Chinese Clinical Trial Registry website, a total of 143 clinical trials for depression have been carried out in China. According to the type of research, they are mainly interventional and observational studies, as well as a small number of related factor studies, epidemiological studies, and diagnostic trials. The research content involves postpartum, perinatal, senile, and other age groups with clinical diagnosis (imaging diagnosis) and intervention studies (drugs, acupuncture, electrical stimulation, transcranial magnetic stimulation). It also includes intervention studies on depression comorbid with coronary heart disease, diabetes, and heart failure.
New Medicine Development
According to the Cortellis database, 828 antidepressants were under development by the end of 2019, but only 292 of these are effective and active (Fig. 3 A). Large number of them have been discontinued or made no progress, indicating that the development of new drugs in the field of depression is extremely urgent.
New medicine development from 2009 to 2019 in depressive disorder. A Development status of new candidate drugs. B Top target-based actions.
From the perspective of target-based actions, the most common new drugs are NMDA receptor antagonists, followed by 5-HT targets, as well as dopamine receptor agonists, opioid receptor antagonists and agonists, AMPA receptor modulators, glucocorticoid receptor antagonists, NK1 receptor antagonists, and serotonin transporter inhibitors (Fig. 3 B).
Epidemiology of Depression
The prevalence of depression varies greatly across cultures and countries. Previous surveys have demonstrated that the 12-month prevalence of depression was 0.3% in the Czech Republic, 10% in the USA, 4.5% in Mexico, and 5.2% in West Germany, and the lifetime prevalence of depression was 1.0% in the Czech Republic, 16.9% in the USA, 8.3% in Canada, and 9.0% in Chile [ 4 , 5 ]. A recent meta-analysis including 30 Countries showed that lifetime and 12-month prevalence depression were 10.8% and 7.2%, respectively [ 6 ]. In China, the lifetime prevalence of depression ranged from 1.6% to 5.5% [ 7 , 8 , 9 ]. An epidemiological study demonstrated that depression was the most common mood disorder with a life prevalence of 3.4% and a 12-month prevalence of 2.1% in China [ 10 ].
Some studies have also reported the prevalence in specific populations. The National Comorbidity Survey-Adolescent Supplement (NCS-A) survey in the USA showed that the lifetime and 12-month prevalence of depression in adolescents aged 13 to 18 were 11.0% and 7.5%, respectively [ 11 ]. A recent meta-analysis demonstrated that lifetime prevalence and 12-month prevalence were 2.8% and 2.3%, respectively, among the elderly population in China [ 12 ].
Neurobiological Pathogenesis of Depressive Disorder
The early hypothesis of monoamines in the pathophysiology of depression has been accepted by the scientific community. The evidence that monoamine oxidase inhibitors and tricyclic antidepressants promote monoamine neurotransmission supports this theory of depression [ 13 ]. So far, selective serotonin reuptake inhibitors and norepinephrine reuptake inhibitors are still the first-line antidepressants. However, there remain 1/3 to 2/3 of depressed patients who do not respond satisfactorily to initial antidepressant treatment, and even as many as 15%–40% do not respond to several pharmacological medicines [ 14 , 15 ]. Therefore, the underlying pathogenesis of depression is far beyond the simple monoamine mechanism.
Other hypotheses of depression have gradually received increasing attention because of biomarkers for depression and the effects pharmacological treatments, such as the stress-responsive hypothalamic pituitary adrenal (HPA) axis, neuroendocrine systems, the neurotrophic family of growth factors, and neuroinflammation.
Stress-Responsive HPA Axis
Stress is causative or a contributing factor to depression. Particularly, long-term or chronic stress can lead to dysfunction of the HPA axis and promote the secretion of hormones, including cortisol, adrenocorticotropic hormone, corticotropin-releasing hormone, arginine vasopressin, and vasopressin. About 40%–60% of patients with depression display a disturbed HPA axis, including hypercortisolemia, decreased rhythmicity, and elevated cortisol levels [ 16 , 17 ]. Mounting evidence has shown that stress-induced abnormality of the HPA axis is associated with depression and cognitive impairment, which is due to the increased secretion of cortisol and the insufficient inhibition of glucocorticoid receptor regulatory feedback [ 18 , 19 ]. In addition, it has been reported that the increase in cortisol levels is related to the severity of depression, especially in melancholic depression [ 20 , 21 ]. Further, patients with depression whose HPA axis was not normalized after treatment had a worse clinical response and prognosis [ 22 , 23 ]. Despite the above promising insights, unfortunately previous studies have shown that treatments regulating the HPA axis, such as glucocorticoid receptor antagonists, do not attenuate the symptoms of depressed patients [ 24 , 25 ].
Glutamate Signaling Pathway
Glutamate is the main excitatory neurotransmitter released by synapses in the brain; it is involved in synaptic plasticity, cognitive processes, and reward and emotional processes. Stress can induce presynaptic glutamate secretion by neurons and glutamate strongly binds to ionotropic glutamate receptors (iGluRs) including N-methyl-D-aspartate receptors (NMDARs) and α-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid receptors (AMPARs) [ 26 ] on the postsynaptic membrane to activate downstream signal pathways [ 27 ]. Accumulating evidence has suggested that the glutamate system is associated with the incidence of depression. Early studies have shown increased levels of glutamate in the peripheral blood, cerebrospinal fluid, and brain of depressed patients [ 28 , 29 ], as well as NMDAR subunit disturbance in the brain [ 30 , 31 ]. Blocking the function of NMDARs has an antidepressant effect and protects hippocampal neurons from morphological abnormalities induced by stress, while antidepressants reduce glutamate secretion and NMDARs [ 32 ]. Most importantly, NMDAR antagonists such as ketamine have been reported to have profound and rapid antidepressant effects on both animal models and the core symptoms of depressive patients [ 33 ]. On the other hand, ketamine can also increase the AMPAR pathway in hippocampal neurons by up-regulating the AMPA glutamate receptor 1 subunit [ 34 ]. Further, the AMPAR pathway may be involved in the mechanism of antidepressant effects. For example, preclinical studies have indicated that AMPAR antagonists might attenuate lithium-induced depressive behavior by increasing the levels of glutamate receptors 1 and 2 in the mouse hippocampus [ 35 ].
Gamma-Aminobutyric Acid (GABA)
Contrary to glutamate, GABA is the main inhibitory neurotransmitter. Although GABA neurons account for only a small proportion compared to glutamate, inhibitory neurotransmission is essential for brain function by balancing excitatory transmission [ 36 ]. Number of studies have shown that patients with depression have neurotransmission or functional defects of GABA [ 37 , 38 ]. Schür et al ., conducted a meta-analysis of magnetic resonance spectroscopy studies, which showed that the brain GABA level in depressive patients was lower than that in healthy controls, but no difference was found in depressive patients in remission [ 39 ]. Several postmortem studies have shown decreased levels of the GABA synthase glutamic acid decarboxylase in the prefrontal cortex of patients with depression [ 40 , 41 ]. It has been suggested that a functional imbalance of the GABA and glutamate systems contributes to the pathophysiology of depression, and activation of the GABA system might induce antidepressant activity, by which GABA A receptor mediators α2/α3 are considered potential antidepressant candidates [ 42 , 43 ]. Genetic mouse models, such as the GABA A receptor mutant mouse and conditional the Gad1-knockout mouse (GABA in hippocampus and cerebral cortex decreased by 50%) and optogenetic methods have verified that depression-like behavior is induced by changing the level of GABA [ 44 , 45 ].
Neurotrophin Family
The neurotrophin family plays a key role in neuroplasticity and neurogenesis. The neurotrophic hypothesis of depression postulates that a deficit of neurotrophic support leads to neuronal atrophy, the reduction of neurogenesis, and the destruction of glia support, while antidepressants attenuate or reverse these pathophysiological processes [ 46 ]. Among them, the most widely accepted hypothesis involves brain-derived neurotrophic factor (BDNF). This was initially triggered by evidence that stress reduces the BDNF levels in the animal brain, while antidepressants rescue or attenuate this reduction [ 47 , 48 ], and agents involved in the BDNF system have been reported to exert antidepressant-like effects [ 49 , 50 ]. In addition, mounting studies have reported that the BDNF level is decreased in the peripheral blood and at post-mortem in depressive patients, and some have reported that antidepressant treatment normalizes it [ 51 , 52 ]. Furthermore, some evidence also showed that the interaction of BDNF and its receptor gene is associated with treatment-resistant depression [ 15 ].
Recent studies reported that depressed patients have a lower level of the pro-domain of BDNF (BDNF pro-peptide) than controls. This is located presynaptically and promotes long-term depression in the hippocampus, suggesting that it is a promising synaptic regulator [ 53 ].
Neuroinflammation
The immune-inflammation hypothesis has attracted much attention, suggesting that the interactions between inflammatory pathways and neural circuits and neurotransmitters are involved in the pathogenesis and pathophysiological processes of depression. Early evidence found that patients with autoimmune or infectious diseases are more likely to develop depression than the general population [ 54 ]. In addition, individuals without depression may display depressive symptoms after treatment with cytokines or cytokine inducers, while antidepressants relieve these symptoms [ 55 , 56 ]. There is a complex interaction between the peripheral and central immune systems. Previous evidence suggested that peripheral inflammation/infection may spread to the central nervous system in some way and cause a neuroimmune response [ 55 , 57 ]: (1) Some cytokines produced in the peripheral immune response, such as IL-6 and IL-1 β, can leak into the brain through the blood-brain barrier (BBB). (2) Cytokines entering the central nervous system act directly on astrocytes, small stromal cells, and neurons. (3) Some peripheral immune cells can cross the BBB through specific transporters, such as monocytes. (4) Cytokines and chemokines in the circulation activate the central nervous system by regulating the surface receptors of astrocytes and endothelial cells at the BBB. (5) As an intermediary pathway, the immune inflammatory response transmits peripheral danger signals to the center, amplifies the signals, and shows the external phenotype of depressive behavior associated with stress/trauma/infection. (6) Cytokines and chemokines may act directly on neurons, change their plasticity and promote depression-like behavior.
Patients with depression show the core feature of the immune-inflammatory response, that is, increased concentrations of pro-inflammatory cytokines and their receptors, chemokines, and soluble adhesion molecules in peripheral blood and cerebrospinal fluid [ 58 , 59 , 60 ]. Peripheral immune-inflammatory response markers not only change the immune activation state in the brain that affects explicit behavior, but also can be used as an evaluation index or biological index of antidepressant therapy [ 61 , 62 ]. Li et al . showed that the level of TNF-α in patients with depression prior to treatment was higher than that in healthy controls. After treatment with venlafaxine, the level of TNF-α in patients with depression decreased significantly, and the level of TNF-α in the effective group decreased more [ 63 ]. A recent meta-analysis of 1,517 patients found that antidepressants significantly reduced peripheral IL-6, TNF-α, IL-10, and CCL-2, suggesting that antidepressants reduce markers of peripheral inflammatory factors [ 64 ]. Recently, Syed et al . also confirmed that untreated patients with depression had higher levels of inflammatory markers and increased levels of anti-inflammatory cytokines after antidepressant treatment, while increased levels of pro-inflammatory cytokines were found in non-responders [ 62 ]. Clinical studies have also found that anti-inflammatory cytokines, such as monoclonal antibodies and other cytokine inhibitors, may play an antidepressant role by blocking cytokines. The imbalance of pro-inflammatory and anti-inflammatory cytokines may be involved in the pathophysiological process of depression.
In addition, a recent study showed that microglia contribute to neuronal plasticity and neuroimmune interaction that are involved in the pathophysiology of depression [ 65 ]. When activated microglia promote inflammation, especially the excessive production of pro-inflammatory factors and cytotoxins in the central nervous system, depression-like behavior can gradually develop [ 65 , 66 ]. However, microglia change polarization as two types under different inflammatory states, regulating the balance of pro- and anti-inflammatory factors. These two types are M1 and M2 microglia; the former produces large number of pro-inflammatory cytokines after activation, and the latter produces anti-inflammatory cytokines. An imbalance of M1/M2 polarization of microglia may contribute to the pathophysiology of depression [ 67 ].
Microbiome-Gut-Brain Axis
The microbiota-gut-brain axis has recently gained more attention because of its ability to regulate brain activity. Many studies have shown that the microbiota-gut-brain axis plays an important role in regulating mood, behavior, and neuronal transmission in the brain [ 68 , 69 ]. It is well established that comorbidity of depression and gastrointestinal diseases is common [ 70 , 71 ]. Some antidepressants can attenuate the symptoms of patients with irritable bowel syndrome and eating disorders [ 72 ]. It has been reported that gut microbiome alterations are associated with depressive-like behaviors [ 73 , 74 ], and brain function [ 75 ]. Early animal studies have shown that stress can lead to long-term changes in the diversity and composition of intestinal microflora, and is accompanied by depressive behavior [ 76 , 77 ]. Interestingly, some evidence indicates that rodents exhibit depressive behavior after fecal transplants from patients with depression [ 74 ]. On the other hand, some probiotics attenuated depressive-like behavior in animal studies, [ 78 ] and had antidepressant effects on patients with depression in several double-blind, placebo-controlled clinical trials [ 79 , 80 ].
The potential mechanism may be that gut microbiota can interact with the brain through a variety of pathways or systems, including the HPA axis, and the neuroendocrine, autonomic, and neuroimmune systems [ 81 ]. For example, recent evidence demonstrated that gut microbiota can affect the levels of neurotransmitters in the gut and brain, including serotonin, dopamine, noradrenalin, glutamate, and GABA [ 82 ]. In addition, recent studies showed that changes in gut microbiota can also impair the gut barrier and promote higher levels of peripheral inflammatory cytokines [ 83 , 84 ]. Although recent research in this area has made significant progress, more clinical trials are needed to determine whether probiotics have any effect on the treatment of depression and what the potential underlying mechanisms are.
Other Systems and Pathways
There is no doubt that several other systems or pathways are also involved in the pathophysiology of depression, such as oxidant-antioxidant imbalance [ 85 ], mitochondrial dysfunction [ 86 , 87 ], and circadian rhythm-related genes [ 88 ], especially their critical interactions ( e.g. interaction between the HPA and mitochondrial metabolism [ 89 , 90 ], and the reciprocal interaction between oxidative stress and inflammation [ 2 , 85 ]). The pathogenesis of depression is complex and all the hypotheses should be integrated to consider the many interactions between various systems and pathways.
Advances in Various Kinds of Research on Depressive Disorder
Genetic, molecular, and neuroimaging studies continue to increase our understanding of the neurobiological basis of depression. However, it is still not clear to what extent the results of neurobiological studies can help improve the clinical and functional prognosis of patients. Therefore, over the past 10 years, the neurobiological study of depression has become an important measure to understand the pathophysiological mechanism and guide the treatment of depression.
Genetic Studies
Previous twin and adoption studies have indicated that depression has relatively low rate of heritability at 37% [ 91 ]. In addition, environmental factors such as stressful events are also involved in the pathogenesis of depression. Furthermore, complex psychiatric disorders, especially depression, are considered to be polygenic effects that interact with environmental factors [ 13 ]. Therefore, reliable identification of single causative genes for depression has proved to be challenging. The first genome-wide association studies (GWAS) for depression was published in 2009, and included 1,738 patients and 1,802 controls [ 92 , 93 ]. Although many subsequent GWASs have determined susceptible genes in the past decade, the impact of individual genes is so small that few results can be replicated [ 94 , 95 ]. So far, it is widely accepted that specific single genetic mutations may play minor and marginal roles in complex polygenic depression. Another major recognition in GWASs over the past decade is that prevalent candidate genes are usually not associated with depression. Further, the inconsistent results may also be due to the heterogeneity and polygenic nature of genetic and non-genetic risk factors for depression as well as the heterogeneity of depression subtypes [ 95 , 96 ]. Therefore, to date, the quality of research has been improved in two aspects: (1) the sample size has been maximized by combining the data of different evaluation models; and (2) more homogenous subtypes of depression have been selected to reduce phenotypic heterogeneity [ 97 ]. Levinson et al . pointed out that more than 75,000 to 100,000 cases should be considered to detect multiple depression associations [ 95 ]. Subsequently, several recent GWASs with larger sample sizes have been conducted. For example, Okbay et al . identified two loci associated with depression and replicated them in separate depression samples [ 98 ]. Wray et al . also found 44 risk loci associated with depression based on 135,458 cases and 344,901 controls [ 99 ]. A recent GWAS of 807,553 individuals with depression reported that 102 independent variants were associated with depression; these were involved in synaptic structure and neural transmission, and were verified in a further 1,507,153 individuals [ 100 ]. However, even with enough samples, GWASs still face severe challenges. A GWAS only marks the region of the genome and is not directly related to the potential biological function. In addition, a genetic association with the indicative phenotype of depression may only be part of many pathogenic pathways, or due to the indirect influence of intermediate traits in the causal pathway on the final result [ 101 ].
Given the diversity of findings, epigenetic factors are now being investigated. Recent studies indicated that epigenetic mechanisms may be the potential causes of "loss of heritability" in GWASs of depression. Over the past decade, a promising discovery has been that the effects of genetic information can be directly influenced by environment factors, and several specific genes are activated by environmental aspects. This process is described as interactions between genes and the environment, which is identified by the epigenetic mechanism. Environmental stressors cause alterations in gene expression in the brain, which may cause abnormal neuronal plasticity in areas related to the pathogenesis of the disease. Epigenetic events alter the structure of chromatin, thereby regulating gene expression involved in neuronal plasticity, stress behavior, depressive behavior, and antidepressant responses, including DNA methylation, histone acetylation, and the role of non-coding RNA. These new mechanisms of trans-generational transmission of epigenetic markers are considered a supplement to orthodox genetic heredity, providing the possibility for the discovery of new treatments for depression [ 102 , 103 ]. Recent studies imply that life experiences, including stress and enrichment, may affect cellular and molecular signaling pathways in sperm and influence the behavioral and physiological phenotypes of offspring in gender-specific patterns, which may also play an important role in the development of depression [ 103 ].
Brain Imaging and Neuroimaging Studies
Neuroimaging, including magnetic resonance imaging (MRI) and molecular imaging, provides a non-invasive technique for determining the underlying etiology and individualized treatment for depression. MRI can provide important data on brain structure, function, networks, and metabolism in patients with depression; it includes structural MRI (sMRI), functional MRI (fMRI), diffusion tensor imaging, and magnetic resonance spectroscopy.
Previous sMRI studies have found damaged gray matter in depression-associated brain areas, including the frontal lobe, anterior cingulate gyrus, hippocampus, putamen, thalamus, and amygdala. sMRI focuses on the thickness of gray matter and brain morphology [ 104 , 105 ]. A recent meta-analysis of 2,702 elderly patients with depression and 11,165 controls demonstrated that the volumes of the whole brain and hippocampus of patients with depression were lower than those of the control group [ 106 ]. Some evidence also showed that the hippocampal volume in depressive patients was lower than that of controls, and increased after treatment with antidepressants [ 107 ] and electroconvulsive therapy (ECT) [ 108 ], suggesting that the hippocampal volume plays a critical role in the development, treatment response, and clinical prognosis of depression. A recent study also reported that ECT increased the volume of the right hippocampus, amygdala, and putamen in patients with treatment-resistant depression [ 109 ]. In addition, postmortem research supported the MRI study showing that dentate gyrus volume was decreased in drug-naive patients with depression compared to healthy controls, and was potentially reversed by treatment with antidepressants [ 110 ].
Diffusion tensor imaging detects the microstructure of the white matter, which has been reported impaired in patients with depression [ 111 ]. A recent meta-analysis that included first-episode and drug-naïve depressive patients showed that the decrease in fractional anisotropy was negatively associated with illness duration and clinical severity [ 112 ].
fMRI, including resting-state and task-based fMRI, can divide the brain into self-related regions, such as the anterior cingulate cortex, posterior cingulate cortex, medial prefrontal cortex, precuneus, and dorsomedial thalamus. Many previous studies have shown the disturbance of several brain areas and intrinsic neural networks in patients with depression which could be rescued by antidepressants [ 113 , 114 , 115 , 116 ]. Further, some evidence also showed an association between brain network dysfunction and the clinical correlates of patients with depression, including clinical symptoms [ 117 ] and the response to antidepressants [ 118 , 119 ], ECT [ 120 , 121 ], and repetitive transcranial magnetic stimulation [ 122 ].
It is worth noting that brain imaging provides new insights into the large-scale brain circuits that underlie the pathophysiology of depressive disorder. In such studies, large-scale circuits are often referred to as “networks”. There is evidence that a variety of circuits are involved in the mechanisms of depressive disorder, including disruption of the default mode, salience, affective, reward, attention, and cognitive control circuits [ 123 ]. Over the past decade, the study of intra-circuit and inter-circuit connectivity dysfunctions in depression has escalated, in part due to advances in precision imaging and analysis techniques [ 124 ]. Circuit dysfunction is a potential biomarker to guide psychopharmacological treatment. For example, Williams et al . found that hyper-activation of the amygdala is associated with a negative phenotype that can predict the response to antidepressants [ 125 ]. Hou et al . showed that the baseline characteristics of the reward circuit predict early antidepressant responses [ 126 ].
Molecular imaging studies, including single photon emission computed tomography and positron emission tomography, focus on metabolic aspects such as amino-acids, neurotransmitters, glucose, and lipids at the cellular level in patients with depression. A recent meta-analysis examined glucose metabolism and found that glucose uptake dysfunction in different brain regions predicts the treatment response [ 127 ].
The most important and promising studies were conducted by the ENIGMA (Enhancing NeuroImaging Genetics through Meta Analysis) Consortium, which investigated the human brain across 43 countries. The ENIGMA-MDD Working Group was launched in 2012 to detect the structural and functional changes associated with MDD reliably and replicate them in various samples around the world [ 128 ]. So far, the ENIGMA-MDD Working Group has collected data from 4,372 MDD patients and 9,788 healthy controls across 14 countries, including 45 cohorts [ 128 ]. Their findings to date are shown in Table 1 [ 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 ].
Objective Index for Diagnosis of MDD
To date, the clinical diagnosis of depression is subjectively based on interviews according to diagnostic criteria ( e.g. International Classification of Diseases and Diagnostic and Statistical Manual diagnostic systems) and the severity of clinical symptoms are assessed by questionnaires, although patients may experience considerable differences in symptoms and subtypes [ 138 ]. Meanwhile, biomarkers including genetics, epigenetics, peripheral gene and protein expression, and neuroimaging markers may provide a promising supplement for the development of the objective diagnosis of MDD, [ 139 , 140 , 141 ]. However, the development of reliable diagnosis for MDD using biomarkers is still difficult and elusive, and all methods based on a single marker are insufficiently specific and sensitive for clinical use [ 142 ]. Papakostas et al . showed that a multi-assay, serum-based test including nine peripheral biomarkers (soluble tumor necrosis factor alpha receptor type II, resistin, prolactin, myeloperoxidase, epidermal growth factor, BDNF, alpha1 antitrypsin, apolipoprotein CIII, brain-derived neurotrophic factor, and cortisol) yielded a specificity of 81.3% and a sensitivity of 91.7% [ 142 ]. However, the sample size was relatively small and no other studies have yet validated their results. Therefore, further studies are needed to identify biomarker models that integrate all biological variables and clinical features to improve the specificity and sensitivity of diagnosis for MDD.
Management of Depression
The treatment strategies for depression consist of pharmacological treatment and non-pharmacological treatments including psychotherapy, ECT [ 98 ], and transcranial magnetic stimulation. As psychotherapy has been shown to have effects on depression including attenuating depressive symptoms and improving the quality of life [ 143 , 144 ]; several practice guidelines are increasingly recommending psychotherapy as a monotherapy or in combination with antidepressants [ 145 , 146 ].
Current Antidepressant Treatment
Antidepressants approved by the US Food and Drug Administration (FDA) are shown in Table 2 . Due to the relatively limited understanding of the etiology and pathophysiology of depression, almost all the previous antidepressants were discovered by accident a few decades ago. Although most antidepressants are usually safe and effective, there are still some limitations, including delayed efficacy (usually 2 weeks) and side-effects that affect the treatment compliance [ 147 ]. In addition, <50% of all patients with depression show complete remission through optimized treatment, including trials of multiple drugs with and without simultaneous psychotherapy. In the past few decades, most antidepressant discoveries focused on finding faster, safer, and more selective serotonin or norepinephrine receptor targets. In addition, there is an urgent need to develop new approaches to obtain more effective, safer, and faster antidepressants. In 2019, the FDA approved two new antidepressants: Esketamine for refractory depression and Bresanolone for postpartum depression. Esmolamine, a derivative of the anesthetic drug ketamine, was approved by the FDA for the treatment of refractory depression, based on a large number of preliminary clinical studies [ 148 ]. For example, several randomized controlled trials and meta-analysis studies showed the efficacy and safety of Esketamine in depression or treatment-resistant depression [ 26 , 149 , 150 ]. Although both are groundbreaking new interventions for these debilitating diseases and both are approved for use only under medical supervision, there are still concerns about potential misuse and problems in the evaluation of mental disorders [ 151 ].
To date, although several potential drugs have not yet been approved by the FDA, they are key milestones in the development of antidepressants that may be modified and used clinically in the future, such as compounds containing dextromethorphan (a non-selective NMDAR antago–nist), sarcosine (N-methylglycine, a glycine reuptake inhibitor), AMPAR modulators, and mGluR modulators [ 152 ].
Neuromodulation Therapy
Neuromodulation therapy acts through magnetic pulse, micro-current, or neural feedback technology within the treatment dose, acting on the central or peripheral nervous system to regulate the excitatory/inhibitory activity to reduce or attenuate the symptoms of the disease.
ECT is one of most effective treatments for depression, with the implementation of safer equipment and advancement of techniques such as modified ECT [ 153 ]. Mounting evidence from randomized controlled trial (RCT) and meta-analysis studies has shown that rTMS can treat depressive patients with safety [ 154 ]. Other promising treatments for depression have emerged, such as transcranial direct current stimulation (tDCS) [ 155 ], transcranial alternating current stimulation (tACS)[ 156 ], vagal nerve stimulation [ 157 ], deep brain stimulation [ 158 ] , and light therapy [ 159 ], but some of them are still experimental to some extent and have not been widely used. For example, compared to tDCS, tACS displays less sensory experience and adverse reactions with weak electrical current in a sine-wave pattern, but the evidence for the efficacy of tACS in the treatment of depression is still limited [ 160 ]. Alexander et al . recently demonstrated that there was no difference in efficacy among different treatments (sham, 10-Hz and 40-Hz tACS). However, only the 10-Hz tACS group had more responders than the sham and 40-Hz tACS groups at week 2 [ 156 ]. Further RCT studies are needed to verify the efficacy of tACS. In addition, the mechanism of the effect of neuromodulation therapy on depression needs to be further investigated.
Precision Medicine for Depression
Optimizing the treatment strategy is an effective way to improve the therapeutic effect on depression. However, each individual with depression may react very differently to different treatments. Therefore, this raises the question of personalized treatment, that is, which patients are suitable for which treatment. Over the past decade, psychiatrists and psychologists have focused on individual biomarkers and clinical characteristics to predict the efficiency of antidepressants and psychotherapies, including genetics, peripheral protein expression, electrophysiology, neuroimaging, neurocognitive performance, developmental trauma, and personality [ 161 ]. For example, Bradley et al . recently conducted a 12-week RCT, which demonstrated that the response rate and remission rates of the pharmacogenetic guidance group were significantly higher than those of the non-pharmacogenetic guidance group [ 162 ].
Subsequently, Greden et al . conducted an 8-week RCT of Genomics Used to Improve Depression Decisions (GUIDED) on 1,167 MDD patients and demonstrated that although there was no difference in symptom improvement between the pharmacogenomics-guided and non- pharmacogenomics-guided groups, the response rate and remission rate of the pharmacogenomics-guided group increased significantly [ 163 ].
A recent meta-analysis has shown that the baseline default mode network connectivity in patients with depression can predict the clinical responses to treatments including cognitive behavioral therapy, pharmacotherapy, ECT, rTMS, and transcutaneous vagus nerve stimulation [ 164 ]. However, so far, the biomarkers that predict treatment response at the individual level have not been well applied in the clinic, and there is still a lot of work to be conducted in the future.
Future Perspectives
Although considerable progress has been made in the study of depression during a past decade, the heterogeneity of the disease, the effectiveness of treatment, and the gap in translational medicine are critical challenges. The main dilemma is that our understanding of the etiology and pathophysiology of depression is inadequate, so our understanding of depression is not deep enough to develop more effective treatment. Animal models still cannot fully simulate this heterogeneous and complex mental disorder. Therefore, how to effectively match the indicators measured in animals with those measured in genetic research or the development of new antidepressants is another important challenge.
Change history
17 may 2021.
A Correction to this paper has been published: https://doi.org/10.1007/s12264-021-00694-9
Dadi AF, Miller ER, Bisetegn TA, Mwanri L. Global burden of antenatal depression and its association with adverse birth outcomes: an umbrella review. BMC Public Health 2020, 20: 173
Article PubMed PubMed Central Google Scholar
Zhu S, Zhao L, Fan Y, Lv Q, Wu K, Lang X. Interaction between TNF-alpha and oxidative stress status in first-episode drug-naive schizophrenia. Psychoneuroendocrinology 2020, 114: 104595
Article CAS PubMed Google Scholar
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390: 1211–1259
Article Google Scholar
Andrade L, Caraveo-Anduaga JJ, Berglund P, Bijl RV, De Graaf R, Vollebergh W, et al. The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int J Methods Psychiatr Res 2003, 12: 3–21
Article PubMed Google Scholar
Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health 2013, 34: 119–138
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep 2018, 8: 2861
Liu J, Yan F, Ma X, Guo HL, Tang YL, Rakofsky JJ, et al. Prevalence of major depressive disorder and socio-demographic correlates: Results of a representative household epidemiological survey in Beijing, China. J Affect Disord 2015, 179: 74–81
Zhang YS, Rao WW, Cui LJ, Li JF, Li L, Ng CH, et al. Prevalence of major depressive disorder and its socio-demographic correlates in the general adult population in Hebei province, China. J Affect Disord 2019, 252: 92–98
Ma X, Xiang YT, Cai ZJ, Li SR, Xiang YQ, Guo HL, et al. Prevalence and socio-demographic correlates of major depressive episode in rural and urban areas of Beijing, China. J Affect Disord 2009, 115: 323–330
Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry 2019, 6: 211–224
Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry 2015, 54(37–44): e32
Google Scholar
Wang F, Zhang QE, Zhang L, Ng CH, Ungvari GS, Yuan Z, et al. Prevalence of major depressive disorder in older adults in China: A systematic review and meta-analysis. J Affect Disord 2018, 241: 297–304
Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature 2008, 455: 894–902
Article CAS PubMed PubMed Central Google Scholar
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry 2006, 163: 1905–1917
Li Z, Zhang Y, Wang Z, Chen J, Fan J, Guan Y, et al. The role of BDNF, NTRK2 gene and their interaction in development of treatment-resistant depression: data from multicenter, prospective, longitudinal clinic practice. J Psychiatr Res 2013, 47: 8–14
Murphy BE. Steroids and depression. J Steroid Biochem Mol Biol 1991, 38: 537–559
Pariante CM, Lightman SL. The HPA axis in major depression: classical theories and new developments. Trends Neurosci 2008, 31: 464–468
Keller J, Gomez R, Williams G, Lembke A, Lazzeroni L, Murphy GM Jr, et al. HPA axis in major depression: cortisol, clinical symptomatology and genetic variation predict cognition. Mol Psychiatry 2017, 22: 527–536
Gomez RG, Fleming SH, Keller J, Flores B, Kenna H, DeBattista C, et al. The neuropsychological profile of psychotic major depression and its relation to cortisol. Biol Psychiatry 2006, 60: 472–478
Lamers F, Vogelzangs N, Merikangas KR, de Jonge P, Beekman AT, Penninx BW. Evidence for a differential role of HPA-axis function, inflammation and metabolic syndrome in melancholic versus atypical depression. Mol Psychiatry 2013, 18: 692–699
Nandam LS, Brazel M, Zhou M, Jhaveri DJ. Cortisol and major depressive disorder-translating findings from humans to animal models and back. Front Psychiatry 2019, 10: 974
Owashi T, Otsubo T, Oshima A, Nakagome K, Higuchi T, Kamijima K. Longitudinal neuroendocrine changes assessed by dexamethasone/CRH and growth hormone releasing hormone tests in psychotic depression. Psychoneuroendocrinology 2008, 33: 152–161
Mickey BJ, Ginsburg Y, Sitzmann AF, Grayhack C, Sen S, Kirschbaum C, et al. Cortisol trajectory, melancholia, and response to electroconvulsive therapy. J Psychiatr Res 2018, 103: 46–53
Stetler C, Miller GE. Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. Psychosom Med 2011, 73: 114–126
Aubry JM. CRF system and mood disorders. J Chem Neuroanat 2013, 54: 20–24
Correia-Melo FS, Leal GC, Vieira F, Jesus-Nunes AP, Mello RP, Magnavita G, et al. Efficacy and safety of adjunctive therapy using esketamine or racemic ketamine for adult treatment-resistant depression: A randomized, double-blind, non-inferiority study. J Affect Disord 2020, 264: 527–534
Duman RS, Voleti B. Signaling pathways underlying the pathophysiology and treatment of depression: novel mechanisms for rapid-acting agents. Trends Neurosci 2012, 35: 47–56
Sanacora G, Zarate CA, Krystal JH, Manji HK. Targeting the glutamatergic system to develop novel, improved therapeutics for mood disorders. Nat Rev Drug Discov 2008, 7: 426–437
Hashimoto K. The role of glutamate on the action of antidepressants. Prog Neuropsychopharmacol Biol Psychiatry 2011, 35: 1558–1568
Gray AL, Hyde TM, Deep-Soboslay A, Kleinman JE, Sodhi MS. Sex differences in glutamate receptor gene expression in major depression and suicide. Mol Psychiatry 2015, 20: 1057–1068
Chandley MJ, Szebeni A, Szebeni K, Crawford JD, Stockmeier CA, Turecki G, et al. Elevated gene expression of glutamate receptors in noradrenergic neurons from the locus coeruleus in major depression. Int J Neuropsychopharmacol 2014, 17: 1569–1578
Musazzi L, Treccani G, Mallei A, Popoli M. The action of antidepressants on the glutamate system: regulation of glutamate release and glutamate receptors. Biol Psychiatry 2013, 73: 1180–1188
Kadriu B, Musazzi L, Henter ID, Graves M, Popoli M, Zarate CA Jr. Glutamatergic Neurotransmission: Pathway to Developing Novel Rapid-Acting Antidepressant Treatments. Int J Neuropsychopharmacol 2019, 22: 119–135
Beurel E, Grieco SF, Amadei C, Downey K, Jope RS. Ketamine-induced inhibition of glycogen synthase kinase-3 contributes to the augmentation of alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid (AMPA) receptor signaling. Bipolar Disord 2016, 18: 473–480
Gould TD, O’Donnell KC, Dow ER, Du J, Chen G, Manji HK. Involvement of AMPA receptors in the antidepressant-like effects of lithium in the mouse tail suspension test and forced swim test. Neuropharmacology 2008, 54: 577–587
Duman RS, Sanacora G, Krystal JH. Altered Connectivity in Depression: GABA and Glutamate Neurotransmitter Deficits and Reversal by Novel Treatments. Neuron 2019, 102: 75–90
Ghosal S, Hare B, Duman RS. Prefrontal Cortex GABAergic Deficits and Circuit Dysfunction in the Pathophysiology and Treatment of Chronic Stress and Depression. Curr Opin Behav Sci 2017, 14: 1–8
Fee C, Banasr M, Sibille E. Somatostatin-positive gamma-aminobutyric acid interneuron deficits in depression: Cortical microcircuit and therapeutic perspectives. Biol Psychiatry 2017, 82: 549–559
Schur RR, Draisma LW, Wijnen JP, Boks MP, Koevoets MG, Joels M, et al. Brain GABA levels across psychiatric disorders: A systematic literature review and meta-analysis of (1) H-MRS studies. Hum Brain Mapp 2016, 37: 3337–3352
Guilloux JP, Douillard-Guilloux G, Kota R, Wang X, Gardier AM, Martinowich K, et al. Molecular evidence for BDNF- and GABA-related dysfunctions in the amygdala of female subjects with major depression. Mol Psychiatry 2012, 17: 1130–1142
Karolewicz B, Maciag D, O’Dwyer G, Stockmeier CA, Feyissa AM, Rajkowska G. Reduced level of glutamic acid decarboxylase-67 kDa in the prefrontal cortex in major depression. Int J Neuropsychopharmacol 2010, 13: 411–420
Lener MS, Niciu MJ, Ballard ED, Park M, Park LT, Nugent AC, et al. Glutamate and gamma-aminobutyric acid systems in the pathophysiology of major depression and antidepressant response to ketamine. Biol Psychiatry 2017, 81: 886–897
Chen X, van Gerven J, Cohen A, Jacobs G. Human pharmacology of positive GABA-A subtype-selective receptor modulators for the treatment of anxiety. Acta Pharmacol Sin 2019, 40: 571–582
Ren Z, Pribiag H, Jefferson SJ, Shorey M, Fuchs T, Stellwagen D, et al. Bidirectional homeostatic regulation of a depression-related brain state by gamma-aminobutyric acidergic deficits and ketamine treatment. Biol Psychiatry 2016, 80: 457–468
Kolata SM, Nakao K, Jeevakumar V, Farmer-Alroth EL, Fujita Y, Bartley AF, et al. Neuropsychiatric phenotypes produced by GABA reduction in mouse cortex and hippocampus. Neuropsychopharmacology 2018, 43: 1445–1456
Duman RS, Li N. A neurotrophic hypothesis of depression: role of synaptogenesis in the actions of NMDA receptor antagonists. Philos Trans R Soc Lond B Biol Sci 2012, 367: 2475–2484
Albert PR, Benkelfat C, Descarries L. The neurobiology of depression—revisiting the serotonin hypothesis. I. Cellular and molecular mechanisms. Philos Trans R Soc Lond B Biol Sci 2012, 367: 2378–2381
Li K, Shen S, Ji YT, Li XY, Zhang LS, Wang XD. Melatonin augments the effects of fluoxetine on depression-like behavior and hippocampal BDNF-TrkB signaling. Neurosci Bull 2018, 34: 303–311
Zhang JJ, Gao TT, Wang Y, Wang JL, Guan W, Wang YJ, et al. Andrographolide exerts significant antidepressant-like effects involving the hippocampal BDNF system in mice. Int J Neuropsychopharmacol 2019, 22: 585–600
Wang JQ, Mao L. The ERK pathway: Molecular mechanisms and treatment of depression. Mol Neurobiol 2019, 56: 6197–6205
Chiou YJ, Huang TL. Serum brain-derived neurotrophic factors in taiwanese patients with drug-naive first-episode major depressive disorder: Effects of antidepressants. Int J Neuropsychopharmacol 2017, 20: 213–218
CAS PubMed Google Scholar
Youssef MM, Underwood MD, Huang YY, Hsiung SC, Liu Y, Simpson NR, et al. Association of BDNF Val66Met polymorphism and brain BDNF levels with major depression and suicide. Int J Neuropsychopharmacol 2018, 21: 528–538
Kojima M, Matsui K, Mizui T. BDNF pro-peptide: physiological mechanisms and implications for depression. Cell Tissue Res 2019, 377: 73–79
Jeon SW, Kim YK. Inflammation-induced depression: Its pathophysiology and therapeutic implications. J Neuroimmunol 2017, 313: 92–98
Miller AH, Raison CL. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol 2016, 16: 22–34
Zhao G, Liu X. Neuroimmune advance in depressive disorder. Adv Exp Med Biol 2019, 1180: 85–98
Li Z, Wang Z, Zhang C, Chen J, Su Y, Huang J, et al. Reduced ENA78 levels as novel biomarker for major depressive disorder and venlafaxine efficiency: Result from a prospective longitudinal study. Psychoneuroendocrinology 2017, 81: 113–121
Ambrosio G, Kaufmann FN, Manosso L, Platt N, Ghisleni G, Rodrigues ALS, et al. Depression and peripheral inflammatory profile of patients with obesity. Psychoneuroendocrinology 2018, 91: 132–141
Mao R, Zhang C, Chen J, Zhao G, Zhou R, Wang F, et al. Different levels of pro- and anti-inflammatory cytokines in patients with unipolar and bipolar depression. J Affect Disord 2018, 237: 65–72
Enache D, Pariante CM, Mondelli V. Markers of central inflammation in major depressive disorder: A systematic review and meta-analysis of studies examining cerebrospinal fluid, positron emission tomography and post-mortem brain tissue. Brain Behav Immun 2019, 81: 24–40
Haroon E, Daguanno AW, Woolwine BJ, Goldsmith DR, Baer WM, Wommack EC, et al. Antidepressant treatment resistance is associated with increased inflammatory markers in patients with major depressive disorder. Psychoneuroendocrinology 2018, 95: 43–49
Syed SA, Beurel E, Loewenstein DA, Lowell JA, Craighead WE, Dunlop BW, et al. Defective inflammatory pathways in never-treated depressed patients are associated with poor treatment response. Neuron 2018, 99(914–924): e913
Li Z, Qi D, Chen J, Zhang C, Yi Z, Yuan C, et al. Venlafaxine inhibits the upregulation of plasma tumor necrosis factor-alpha (TNF-alpha) in the Chinese patients with major depressive disorder: a prospective longitudinal study. Psychoneuroendocrinology 2013, 38: 107–114
Kohler CA, Freitas TH, Stubbs B, Maes M, Solmi M, Veronese N, et al. Peripheral alterations in cytokine and chemokine levels after antidepressant drug treatment for major depressive disorder: systematic review and meta-analysis. Mol Neurobiol 2018, 55: 4195–4206
Innes S, Pariante CM, Borsini A. Microglial-driven changes in synaptic plasticity: A possible role in major depressive disorder. Psychoneuroendocrinology 2019, 102: 236–247
Sochocka M, Diniz BS, Leszek J. Inflammatory response in the CNS: Friend or foe? Mol Neurobiol 2017, 54: 8071–8089
Zhang L, Zhang J, You Z. Switching of the microglial activation phenotype is a possible treatment for depression disorder. Front Cell Neurosci 2018, 12: 306
Sandhu KV, Sherwin E, Schellekens H, Stanton C, Dinan TG, Cryan JF. Feeding the microbiota-gut-brain axis: diet, microbiome, and neuropsychiatry. Transl Res 2017, 179: 223–244
Gonzalez-Arancibia C, Urrutia-Pinones J, Illanes-Gonzalez J, Martinez-Pinto J, Sotomayor-Zarate R, Julio-Pieper M, et al. Do your gut microbes affect your brain dopamine? Psychopharmacology (Berl) 2019, 236: 1611–1622
Article CAS Google Scholar
Kennedy PJ, Cryan JF, Dinan TG, Clarke G. Irritable bowel syndrome: a microbiome-gut-brain axis disorder? World J Gastroenterol 2014, 20: 14105–14125
Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology 2002, 122: 1140–1156
Ruepert L, Quartero AO, de Wit NJ, van der Heijden GJ, Rubin G, Muris JW. Bulking agents, antispasmodics and antidepressants for the treatment of irritable bowel syndrome. Cochrane Database Syst Rev 2011: CD003460.
Marin IA, Goertz JE, Ren T, Rich SS, Onengut-Gumuscu S, Farber E, et al. Microbiota alteration is associated with the development of stress-induced despair behavior. Sci Rep 2017, 7: 43859
Zheng P, Zeng B, Zhou C, Liu M, Fang Z, Xu X, et al. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s metabolism. Mol Psychiatry 2016, 21: 786–796
Curtis K, Stewart CJ, Robinson M, Molfese DL, Gosnell SN, Kosten TR, et al. Insular resting state functional connectivity is associated with gut microbiota diversity. Eur J Neurosci 2019, 50: 2446–2452
O’Mahony SM, Marchesi JR, Scully P, Codling C, Ceolho AM, Quigley EM, et al. Early life stress alters behavior, immunity, and microbiota in rats: implications for irritable bowel syndrome and psychiatric illnesses. Biol Psychiatry 2009, 65: 263–267
Garcia-Rodenas CL, Bergonzelli GE, Nutten S, Schumann A, Cherbut C, Turini M, et al. Nutritional approach to restore impaired intestinal barrier function and growth after neonatal stress in rats. J Pediatr Gastroenterol Nutr 2006, 43: 16–24
Hao Z, Wang W, Guo R, Liu H. Faecalibacterium prausnitzii (ATCC 27766) has preventive and therapeutic effects on chronic unpredictable mild stress-induced depression-like and anxiety-like behavior in rats. Psychoneuroendocrinology 2019, 104: 132–142
Messaoudi M, Violle N, Bisson JF, Desor D, Javelot H, Rougeot C. Beneficial psychological effects of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in healthy human volunteers. Gut Microbes 2011, 2: 256–261
Rudzki L, Ostrowska L, Pawlak D, Malus A, Pawlak K, Waszkiewicz N, et al. Probiotic Lactobacillus Plantarum 299v decreases kynurenine concentration and improves cognitive functions in patients with major depression: A double-blind, randomized, placebo controlled study. Psychoneuroendocrinology 2019, 100: 213–222
Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci 2013, 36: 305–312
Mittal R, Debs LH, Patel AP, Nguyen D, Patel K, O’Connor G, et al. Neurotransmitters: The critical modulators regulating gut-brain axis. J Cell Physiol 2017, 232: 2359–2372
Diviccaro S, Giatti S, Borgo F, Barcella M, Borghi E, Trejo JL, et al. Treatment of male rats with finasteride, an inhibitor of 5alpha-reductase enzyme, induces long-lasting effects on depressive-like behavior, hippocampal neurogenesis, neuroinflammation and gut microbiota composition. Psychoneuroendocrinology 2019, 99: 206–215
Kiecolt-Glaser JK, Wilson SJ, Bailey ML, Andridge R, Peng J, Jaremka LM, et al. Marital distress, depression, and a leaky gut: Translocation of bacterial endotoxin as a pathway to inflammation. Psychoneuroendocrinology 2018, 98: 52–60
Lindqvist D, Dhabhar FS, James SJ, Hough CM, Jain FA, Bersani FS, et al. Oxidative stress, inflammation and treatment response in major depression. Psychoneuroendocrinology 2017, 76: 197–205
Czarny P, Wigner P, Galecki P, Sliwinski T. The interplay between inflammation, oxidative stress, DNA damage, DNA repair and mitochondrial dysfunction in depression. Prog Neuropsychopharmacol Biol Psychiatry 2018, 80: 309–321
Xie X, Yu C, Zhou J, Xiao Q, Shen Q, Xiong Z, et al. Nicotinamide mononucleotide ameliorates the depression-like behaviors and is associated with attenuating the disruption of mitochondrial bioenergetics in depressed mice. J Affect Disord 2020, 263: 166–174
Wang XL, Yuan K, Zhang W, Li SX, Gao GF, Lu L. Regulation of circadian genes by the MAPK pathway: Implications for rapid antidepressant action. Neurosci Bull 2020, 36: 66–76
Xie X, Shen Q, Yu C, Xiao Q, Zhou J, Xiong Z, et al. Depression-like behaviors are accompanied by disrupted mitochondrial energy metabolism in chronic corticosterone-induced mice. J Steroid Biochem Mol Biol 2020, 200: 105607
Zhang LF, Shi L, Liu H, Meng FT, Liu YJ, Wu HM, et al. Increased hippocampal tau phosphorylation and axonal mitochondrial transport in a mouse model of chronic stress. Int J Neuropsychopharmacol 2012, 15: 337–348
Flint J, Kendler KS. The genetics of major depression. Neuron 2014, 81: 1214
Sullivan PF, de Geus EJ, Willemsen G, James MR, Smit JH, Zandbelt T, et al. Genome-wide association for major depressive disorder: a possible role for the presynaptic protein piccolo. Mol Psychiatry 2009, 14: 359–375
Dunn EC, Brown RC, Dai Y, Rosand J, Nugent NR, Amstadter AB, et al. Genetic determinants of depression: recent findings and future directions. Harv Rev Psychiatry 2015, 23: 1–18
Major Depressive Disorder Working Group of the Psychiatric GC, Ripke S, Wray NR, Lewis CM, Hamilton SP, Weissman MM, et al. A mega-analysis of genome-wide association studies for major depressive disorder. Mol Psychiatry 2013, 18: 497–511.
Levinson DF, Mostafavi S, Milaneschi Y, Rivera M, Ripke S, Wray NR, et al. Genetic studies of major depressive disorder: why are there no genome-wide association study findings and what can we do about it? Biol Psychiatry 2014, 76: 510–512
Sullivan PF, Agrawal A, Bulik CM, Andreassen OA, Borglum AD, Breen G, et al. Psychiatric genomics: An update and an agenda. Am J Psychiatry 2018, 175: 15–27
Schwabe I, Milaneschi Y, Gerring Z, Sullivan PF, Schulte E, Suppli NP, et al. Unraveling the genetic architecture of major depressive disorder: merits and pitfalls of the approaches used in genome-wide association studies. Psychol Med 2019, 49: 2646–2656
Okbay A, Baselmans BM, De Neve JE, Turley P, Nivard MG, Fontana MA, et al. Genetic variants associated with subjective well-being, depressive symptoms, and neuroticism identified through genome-wide analyses. Nat Genet 2016, 48: 624–633
Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet 2018, 50: 668–681
Howard DM, Adams MJ, Clarke TK, Hafferty JD, Gibson J, Shirali M, et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat Neurosci 2019, 22: 343–352
Ormel J, Hartman CA, Snieder H. The genetics of depression: successful genome-wide association studies introduce new challenges. Transl Psychiatry 2019, 9: 114
Uchida S, Yamagata H, Seki T, Watanabe Y. Epigenetic mechanisms of major depression: Targeting neuronal plasticity. Psychiatry Clin Neurosci 2018, 72: 212–227
Yeshurun S, Hannan AJ. Transgenerational epigenetic influences of paternal environmental exposures on brain function and predisposition to psychiatric disorders. Mol Psychiatry 2019, 24: 536–548
van Eijndhoven P, van Wingen G, Katzenbauer M, Groen W, Tepest R, Fernandez G, et al. Paralimbic cortical thickness in first-episode depression: evidence for trait-related differences in mood regulation. Am J Psychiatry 2013, 170: 1477–1486
Peng W, Chen Z, Yin L, Jia Z, Gong Q. Essential brain structural alterations in major depressive disorder: A voxel-wise meta-analysis on first episode, medication-naive patients. J Affect Disord 2016, 199: 114–123
Geerlings MI, Gerritsen L. Late-life depression, hippocampal volumes, and hypothalamic-pituitary-adrenal axis regulation: A systematic review and meta-analysis. Biol Psychiatry 2017, 82: 339–350
Maller JJ, Broadhouse K, Rush AJ, Gordon E, Koslow S, Grieve SM. Increased hippocampal tail volume predicts depression status and remission to anti-depressant medications in major depression. Mol Psychiatry 2018, 23: 1737–1744
Joshi SH, Espinoza RT, Pirnia T, Shi J, Wang Y, Ayers B, et al. Structural plasticity of the hippocampus and amygdala induced by electroconvulsive therapy in major depression. Biol Psychiatry 2016, 79: 282–292
Gryglewski G, Baldinger-Melich P, Seiger R, Godbersen GM, Michenthaler P, Klobl M, et al. Structural changes in amygdala nuclei, hippocampal subfields and cortical thickness following electroconvulsive therapy in treatment-resistant depression: longitudinal analysis. Br J Psychiatry 2019, 214: 159–167
Boldrini M, Santiago AN, Hen R, Dwork AJ, Rosoklija GB, Tamir H, et al. Hippocampal granule neuron number and dentate gyrus volume in antidepressant-treated and untreated major depression. Neuropsychopharmacology 2013, 38: 1068–1077
Liang S, Wang Q, Kong X, Deng W, Yang X, Li X, et al. White matter abnormalities in major depression biotypes identified by diffusion tensor imaging. Neurosci Bull 2019, 35: 867–876
Chen G, Guo Y, Zhu H, Kuang W, Bi F, Ai H, et al. Intrinsic disruption of white matter microarchitecture in first-episode, drug-naive major depressive disorder: A voxel-based meta-analysis of diffusion tensor imaging. Prog Neuropsychopharmacol Biol Psychiatry 2017, 76: 179–187
Brakowski J, Spinelli S, Dorig N, Bosch OG, Manoliu A, Holtforth MG, et al. Resting state brain network function in major depression - Depression symptomatology, antidepressant treatment effects, future research. J Psychiatr Res 2017, 92: 147–159
Dutta A, McKie S, Downey D, Thomas E, Juhasz G, Arnone D, et al. Regional default mode network connectivity in major depressive disorder: modulation by acute intravenous citalopram. Transl Psychiatry 2019, 9: 116
Meyer BM, Rabl U, Huemer J, Bartova L, Kalcher K, Provenzano J, et al. Prefrontal networks dynamically related to recovery from major depressive disorder: a longitudinal pharmacological fMRI study. Transl Psychiatry 2019, 9: 64
Muller VI, Cieslik EC, Serbanescu I, Laird AR, Fox PT, Eickhoff SB. Altered brain activity in unipolar depression revisited: Meta-analyses of neuroimaging studies. JAMA Psychiatry 2017, 74: 47–55
Connolly CG, Ho TC, Blom EH, LeWinn KZ, Sacchet MD, Tymofiyeva O, et al. Resting-state functional connectivity of the amygdala and longitudinal changes in depression severity in adolescent depression. J Affect Disord 2017, 207: 86–94
Godlewska BR, Browning M, Norbury R, Igoumenou A, Cowen PJ, Harmer CJ. Predicting treatment response in depression: The role of anterior cingulate cortex. Int J Neuropsychopharmacol 2018, 21: 988–996
Goldstein-Piekarski AN, Staveland BR, Ball TM, Yesavage J, Korgaonkar MS, Williams LM. Intrinsic functional connectivity predicts remission on antidepressants: a randomized controlled trial to identify clinically applicable imaging biomarkers. Transl Psychiatry 2018, 8: 57
Leaver AM, Vasavada M, Joshi SH, Wade B, Woods RP, Espinoza R, et al. Mechanisms of antidepressant response to electroconvulsive therapy studied with perfusion magnetic resonance imaging. Biol Psychiatry 2019, 85: 466–476
Miskowiak KW, Macoveanu J, Jorgensen MB, Stottrup MM, Ott CV, Jensen HM, et al. Neural response after a single ECT session during retrieval of emotional self-referent words in depression: A randomized, sham-controlled fMRI study. Int J Neuropsychopharmacol 2018, 21: 226–235
Du L, Liu H, Du W, Chao F, Zhang L, Wang K, et al. Stimulated left DLPFC-nucleus accumbens functional connectivity predicts the anti-depression and anti-anxiety effects of rTMS for depression. Transl Psychiatry 2018, 7: 3
Williams LM. Defining biotypes for depression and anxiety based on large-scale circuit dysfunction: a theoretical review of the evidence and future directions for clinical translation. Depress Anxiety 2017, 34: 9–24
Williams LM. Precision psychiatry: a neural circuit taxonomy for depression and anxiety. Lancet Psychiatry 2016, 3: 472–480
Williams LM, Korgaonkar MS, Song YC, Paton R, Eagles S, Goldstein-Piekarski A, et al. Amygdala reactivity to emotional faces in the prediction of general and medication-specific responses to antidepressant treatment in the randomized iSPOT-D trial. Neuropsychopharmacology 2015, 40: 2398–2408
Hou Z, Gong L, Zhi M, Yin Y, Zhang Y, Xie C, et al. Distinctive pretreatment features of bilateral nucleus accumbens networks predict early response to antidepressants in major depressive disorder. Brain Imaging Behav 2018, 12: 1042–1052
De Crescenzo F, Ciliberto M, Menghini D, Treglia G, Ebmeier KP, Janiri L. Is (18)F-FDG-PET suitable to predict clinical response to the treatment of geriatric depression? A systematic review of PET studies. Aging Ment Health 2017, 21: 889–894
Schmaal L, Pozzi E, T CH, van Velzen LS, Veer IM, Opel N, et al. ENIGMA MDD: seven years of global neuroimaging studies of major depression through worldwide data sharing. Transl Psychiatry 2020, 10: 172.
Schmaal L, Veltman DJ, van Erp TG, Samann PG, Frodl T, Jahanshad N, et al. Subcortical brain alterations in major depressive disorder: findings from the ENIGMA Major Depressive Disorder working group. Mol Psychiatry 2016, 21: 806–812
Schmaal L, Hibar DP, Samann PG, Hall GB, Baune BT, Jahanshad N, et al. Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA Major Depressive Disorder Working Group. Mol Psychiatry 2017, 22: 900–909
Frodl T, Janowitz D, Schmaal L, Tozzi L, Dobrowolny H, Stein DJ, et al. Childhood adversity impacts on brain subcortical structures relevant to depression. J Psychiatr Res 2017, 86: 58–65
Renteria ME, Schmaal L, Hibar DP, Couvy-Duchesne B, Strike LT, Mills NT, et al. Subcortical brain structure and suicidal behaviour in major depressive disorder: a meta-analysis from the ENIGMA-MDD working group. Transl Psychiatry 2017, 7: e1116
Tozzi L, Garczarek L, Janowitz D, Stein DJ, Wittfeld K, Dobrowolny H, et al. Interactive impact of childhood maltreatment, depression, and age on cortical brain structure: mega-analytic findings from a large multi-site cohort. Psychol Med 2020, 50: 1020–1031
de Kovel CGF, Aftanas L, Aleman A, Alexander-Bloch AF, Baune BT, Brack I, et al. No alterations of brain structural asymmetry in major depressive disorder: An ENIGMA consortium analysis. Am J Psychiatry 2019, 176: 1039–1049
Ho TC, Gutman B, Pozzi E, Grabe HJ, Hosten N, Wittfeld K, et al. Subcortical shape alterations in major depressive disorder: Findings from the ENIGMA major depressive disorder working group. Hum Brain Mapp 2020.
Han LKM, Dinga R, Hahn T, Ching CRK, Eyler LT, Aftanas L, et al. Brain aging in major depressive disorder: results from the ENIGMA major depressive disorder working group. Mol Psychiatry 2020.
van Velzen LS, Kelly S, Isaev D, Aleman A, Aftanas LI, Bauer J, et al. White matter disturbances in major depressive disorder: a coordinated analysis across 20 international cohorts in the ENIGMA MDD working group. Mol Psychiatry 2020, 25: 1511–1525
Lv X, Si T, Wang G, Wang H, Liu Q, Hu C, et al. The establishment of the objective diagnostic markers and personalized medical intervention in patients with major depressive disorder: rationale and protocol. BMC Psychiatry 2016, 16: 240
Fabbri C, Hosak L, Mossner R, Giegling I, Mandelli L, Bellivier F, et al. Consensus paper of the WFSBP Task Force on Genetics: Genetics, epigenetics and gene expression markers of major depressive disorder and antidepressant response. World J Biol Psychiatry 2017, 18: 5–28
Li Z, Zhang C, Fan J, Yuan C, Huang J, Chen J, et al. Brain-derived neurotrophic factor levels and bipolar disorder in patients in their first depressive episode: 3-year prospective longitudinal study. Br J Psychiatry 2014, 205: 29–35
Gong Q, He Y. Depression, neuroimaging and connectomics: a selective overview. Biol Psychiatry 2015, 77: 223–235
Papakostas GI, Shelton RC, Kinrys G, Henry ME, Bakow BR, Lipkin SH, et al. Assessment of a multi-assay, serum-based biological diagnostic test for major depressive disorder: a pilot and replication study. Mol Psychiatry 2013, 18: 332–339
Kolovos S, Kleiboer A, Cuijpers P. Effect of psychotherapy for depression on quality of life: meta-analysis. Br J Psychiatry 2016, 209: 460–468
Park LT, Zarate CA Jr. Depression in the primary care setting. N Engl J Med 2019, 380: 559–568
Health N C C F M . Depression: The treatment and management of depression in adults (updated edition) 2010.
Qaseem A, Barry MJ, Kansagara D. Clinical Guidelines Committee of the American College of P. Nonpharmacologic versus pharmacologic treatment of adult patients with major depressive disorder: A clinical practice guideline from the american college of physicians. Ann Intern Med 2016, 164: 350–359
Dodd S, Mitchell PB, Bauer M, Yatham L, Young AH, Kennedy SH, et al. Monitoring for antidepressant-associated adverse events in the treatment of patients with major depressive disorder: An international consensus statement. World J Biol Psychiatry 2018, 19: 330–348
Cristea IA, Naudet F. US Food and Drug Administration approval of esketamine and brexanolone. Lancet Psychiatry 2019, 6: 975–977
Zheng W, Cai DB, Xiang YQ, Zheng W, Jiang WL, Sim K, et al. Adjunctive intranasal esketamine for major depressive disorder: A systematic review of randomized double-blind controlled-placebo studies. J Affect Disord 2020, 265: 63–70
Popova V, Daly EJ, Trivedi M, Cooper K, Lane R, Lim P, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: A Randomized Double-Blind Active-Controlled Study. Am J Psychiatry 2019, 176: 428–438
Turner EH. Esketamine for treatment-resistant depression: seven concerns about efficacy and FDA approval. Lancet Psychiatry 2019, 6: 977–979
Murrough JW, Abdallah CG, Mathew SJ. Targeting glutamate signalling in depression: progress and prospects. Nat Rev Drug Discov 2017, 16: 472–486
Gill SP, Kellner CH. Clinical practice recommendations for continuation and maintenance electroconvulsive therapy for depression: Outcomes from a review of the evidence and a consensus workshop held in Australia in May 2017. J ECT 2019, 35: 14–20
McClintock SM, Reti IM, Carpenter LL, McDonald WM, Dubin M, Taylor SF, et al. Consensus recommendations for the clinical application of repetitive transcranial magnetic stimulation (rTMS) in the treatment of depression. J Clin Psychiatry 2018, 79.
Chase HW, Boudewyn MA, Carter CS, Phillips ML. Transcranial direct current stimulation: a roadmap for research, from mechanism of action to clinical implementation. Mol Psychiatry 2020, 25: 397–407
Alexander ML, Alagapan S, Lugo CE, Mellin JM, Lustenberger C, Rubinow DR, et al. Double-blind, randomized pilot clinical trial targeting alpha oscillations with transcranial alternating current stimulation (tACS) for the treatment of major depressive disorder (MDD). Transl Psychiatry 2019, 9: 106
Akhtar H, Bukhari F, Nazir M, Anwar MN, Shahzad A. Therapeutic efficacy of neurostimulation for depression: Techniques, current modalities, and future challenges. Neurosci Bull 2016, 32: 115–126
Zhou C, Zhang H, Qin Y, Tian T, Xu B, Chen J, et al. A systematic review and meta-analysis of deep brain stimulation in treatment-resistant depression. Prog Neuropsychopharmacol Biol Psychiatry 2018, 82: 224–232
Li X, Li X. The antidepressant effect of light therapy from retinal projections. Neurosci Bull 2018, 34: 359–368
Shekelle PG, Cook IA, Miake-Lye IM, Booth MS, Beroes JM, Mak S. Benefits and harms of cranial electrical stimulation for chronic painful conditions, depression, anxiety, and insomnia: A systematic review. Ann Intern Med 2018, 168: 414–421
Kessler RC. The potential of predictive analytics to provide clinical decision support in depression treatment planning. Curr Opin Psychiatry 2018, 31: 32–39
Bradley P, Shiekh M, Mehra V, Vrbicky K, Layle S, Olson MC, et al. Improved efficacy with targeted pharmacogenetic-guided treatment of patients with depression and anxiety: A randomized clinical trial demonstrating clinical utility. J Psychiatr Res 2018, 96: 100–107
Greden JF, Parikh SV, Rothschild AJ, Thase ME, Dunlop BW, DeBattista C, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: A large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res 2019, 111: 59–67
Long Z, Du L, Zhao J, Wu S, Zheng Q, Lei X. Prediction on treatment improvement in depression with resting state connectivity: A coordinate-based meta-analysis. J Affect Disord 2020, 276: 62–68
Download references
Acknowledgments
This review was supported by the National Basic Research Development Program of China (2016YFC1307100), the National Natural Science Foundation of China (81930033 and 81771465; 81401127), Shanghai Key Project of Science & Technology (2018SHZDZX05), Shanghai Jiao Tong University Medical Engineering Foundation (YG2016MS48), Shanghai Jiao Tong University School of Medicine (19XJ11006), the Sanming Project of Medicine in Shenzhen Municipality (SZSM201612006), the National Key Technologies R&D Program of China (2012BAI01B04), and the Innovative Research Team of High-level Local Universities in Shanghai.
Author information
Authors and affiliations.
Clinical Research Center and Division of Mood Disorders of Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, 200030, China
Zezhi Li, Jun Chen & Yiru Fang
Department of Neurology, Ren Ji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, 200127, China
Shanghai Institute of Nutrition and Health, Shanghai Information Center for Life Sciences, Chinese Academy of Science, Shanghai, 200031, China
Meihua Ruan
Center for Excellence in Brain Science and Intelligence Technology, Chinese Academy of Science, Shanghai, 200031, China
Shanghai Key Laboratory of Psychotic Disorders, Shanghai, 201108, China
Jun Chen & Yiru Fang
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Yiru Fang .
Ethics declarations
Conflicts of interest.
The authors declare no conflicts of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Li, Z., Ruan, M., Chen, J. et al. Major Depressive Disorder: Advances in Neuroscience Research and Translational Applications. Neurosci. Bull. 37 , 863–880 (2021). https://doi.org/10.1007/s12264-021-00638-3
Download citation
Received : 30 May 2020
Accepted : 30 September 2020
Published : 13 February 2021
Issue Date : June 2021
DOI : https://doi.org/10.1007/s12264-021-00638-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Major depressive disorder
- Pathogenesis
- Find a journal
- Publish with us
- Track your research
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Genetic Architectures of Adolescent Depression Trajectories in 2 Longitudinal Population Cohorts
- 1 Division of Psychiatry, Centre for Clinical Brain Sciences, University of Edinburgh, Edinburgh, United Kingdom
- 2 Department of Medical Epidemiology and Biostatistics, Karolinska Institute, Stockholm, Sweden
- 3 School of Health and Wellbeing, University of Glasgow, Glasgow, United Kingdom
- 4 School of Medical Sciences, Örebro University, Örebro, Sweden
- 5 Generation Scotland, Centre for Genomic and Experimental Medicine, Institute of Genetics and Molecular Medicine, University of Edinburgh, Edinburgh, United Kingdom
- 6 MRC Integrative Epidemiology Unit, University of Bristol, Bristol, United Kingdom
Question Could multitrait polygenic risk scores be used to strengthen genetic prediction of longitudinal depression across adolescence?
Findings In this longitudinal cohort replication study of 14 112 adolescents, stronger effect sizes of multitrait polygenic risk association with adverse depression trajectories were found compared with unitrait genetic risk.
Meaning Longitudinal depression has a robust genetic underpinning, and leveraging shared genetic information across multiple psychiatric traits may strengthen prediction models of depression in adolescence.
Importance Adolescent depression is characterized by diverse symptom trajectories over time and has a strong genetic influence. Research has determined genetic overlap between depression and other psychiatric conditions; investigating the shared genetic architecture of heterogeneous depression trajectories is crucial for understanding disease etiology, prediction, and early intervention.
Objective To investigate univariate and multivariate genetic risk for adolescent depression trajectories and assess generalizability across ancestries.
Design, Setting, and Participants This cohort study entailed longitudinal growth modeling followed by polygenic risk score (PRS) association testing for individual and multitrait genetic models. Two longitudinal cohorts from the US and UK were used: the Adolescent Brain and Cognitive Development (ABCD; N = 11 876) study and the Avon Longitudinal Study of Parents and Children (ALSPAC; N = 8787) study. Included were adolescents with genetic information and depression measures at up to 8 and 4 occasions, respectively. Study data were analyzed January to July 2023.
Main Outcomes and Measures Trajectories were derived from growth mixture modeling of longitudinal depression symptoms. PRSs were computed for depression, anxiety, neuroticism, bipolar disorder, schizophrenia, attention-deficit/hyperactivity disorder, and autism in European ancestry. Genomic structural equation modeling was used to build multitrait genetic models of psychopathology followed by multitrait PRS. Depression PRSs were computed in African, East Asian, and Hispanic ancestries in the ABCD cohort only. Association testing was performed between all PRSs and trajectories for both cohorts.
Results A total sample size of 14 112 adolescents (at baseline: mean [SD] age, 10.5 [0.5] years; 7269 male sex [52%]) from both cohorts were included in this analysis. Distinct depression trajectories (stable low, adolescent persistent, increasing, and decreasing) were replicated in the ALSPAC cohort (6096 participants; 3091 female [51%]) and ABCD cohort (8016 participants; 4274 male [53%]) between ages 10 and 17 years. Most univariate PRSs showed significant uniform associations with persistent trajectories, but fewer were significantly associated with intermediate (increasing and decreasing) trajectories. Multitrait PRSs—derived from a hierarchical factor model—showed the strongest associations for persistent trajectories (ABCD cohort: OR, 1.46; 95% CI, 1.26-1.68; ALSPAC cohort: OR, 1.34; 95% CI, 1.20-1.49), surpassing the effect size of univariate PRS in both cohorts. Multitrait PRSs were associated with intermediate trajectories but to a lesser extent (ABCD cohort: hierarchical increasing, OR, 1.27; 95% CI, 1.13-1.43; decreasing, OR, 1.23; 95% CI, 1.09-1.40; ALSPAC cohort: hierarchical increasing, OR, 1.16; 95% CI, 1.04-1.28; decreasing, OR, 1.32; 95% CI, 1.18-1.47). Transancestral genetic risk for depression showed no evidence for association with trajectories.
Conclusions and Relevance Results of this cohort study revealed a high multitrait genetic loading of persistent symptom trajectories, consistent across traits and cohorts. Variability in univariate genetic association with intermediate trajectories may stem from environmental factors. Multitrait genetics may strengthen depression prediction models, but more diverse data are needed for generalizability.
Read More About
Grimes PZ , Adams MJ , Thng G, et al. Genetic Architectures of Adolescent Depression Trajectories in 2 Longitudinal Population Cohorts. JAMA Psychiatry. Published online May 15, 2024. doi:10.1001/jamapsychiatry.2024.0983
Manage citations:
© 2024
Artificial Intelligence Resource Center
Psychiatry in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 July 2021
Systematic review and meta-analysis of depression, anxiety, and suicidal ideation among Ph.D. students
- Emily N. Satinsky 1 ,
- Tomoki Kimura 2 ,
- Mathew V. Kiang 3 , 4 ,
- Rediet Abebe 5 , 6 ,
- Scott Cunningham 7 ,
- Hedwig Lee 8 ,
- Xiaofei Lin 9 ,
- Cindy H. Liu 10 , 11 ,
- Igor Rudan 12 ,
- Srijan Sen 13 ,
- Mark Tomlinson 14 , 15 ,
- Miranda Yaver 16 &
- Alexander C. Tsai 1 , 11 , 17
Scientific Reports volume 11 , Article number: 14370 ( 2021 ) Cite this article
88k Accesses
73 Citations
821 Altmetric
Metrics details
- Epidemiology
- Health policy
- Quality of life
University administrators and mental health clinicians have raised concerns about depression and anxiety among Ph.D. students, yet no study has systematically synthesized the available evidence in this area. After searching the literature for studies reporting on depression, anxiety, and/or suicidal ideation among Ph.D. students, we included 32 articles. Among 16 studies reporting the prevalence of clinically significant symptoms of depression across 23,469 Ph.D. students, the pooled estimate of the proportion of students with depression was 0.24 (95% confidence interval [CI], 0.18–0.31; I 2 = 98.75%). In a meta-analysis of the nine studies reporting the prevalence of clinically significant symptoms of anxiety across 15,626 students, the estimated proportion of students with anxiety was 0.17 (95% CI, 0.12–0.23; I 2 = 98.05%). We conclude that depression and anxiety are highly prevalent among Ph.D. students. Data limitations precluded our ability to obtain a pooled estimate of suicidal ideation prevalence. Programs that systematically monitor and promote the mental health of Ph.D. students are urgently needed.
Similar content being viewed by others
Prevalence of depression among Chinese university students: a systematic review and meta-analysis
A repeated cross-sectional analysis assessing mental health conditions of adults as per student status during key periods of the COVID-19 epidemic in France
Relationship between depression and quality of life among students: a systematic review and meta-analysis
Introduction.
Mental health problems among graduate students in doctoral degree programs have received increasing attention 1 , 2 , 3 , 4 . Ph.D. students (and students completing equivalent degrees, such as the Sc.D.) face training periods of unpredictable duration, financial insecurity and food insecurity, competitive markets for tenure-track positions, and unsparing publishing and funding models 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 —all of which may have greater adverse impacts on students from marginalized and underrepresented populations 13 , 14 , 15 . Ph.D. students’ mental health problems may negatively affect their physical health 16 , interpersonal relationships 17 , academic output, and work performance 18 , 19 , and may also contribute to program attrition 20 , 21 , 22 . As many as 30 to 50% of Ph.D. students drop out of their programs, depending on the country and discipline 23 , 24 , 25 , 26 , 27 . Further, while mental health problems among Ph.D. students raise concerns for the wellbeing of the individuals themselves and their personal networks, they also have broader repercussions for their institutions and academia as a whole 22 .
Despite the potential public health significance of this problem, most evidence syntheses on student mental health have focused on undergraduate students 28 , 29 or graduate students in professional degree programs (e.g., medical students) 30 . In non-systematic summaries, estimates of the prevalence of clinically significant depressive symptoms among Ph.D. students vary considerably 31 , 32 , 33 . Reliable estimates of depression and other mental health problems among Ph.D. students are needed to inform preventive, screening, or treatment efforts. To address this gap in the literature, we conducted a systematic review and meta-analysis to explore patterns of depression, anxiety, and suicidal ideation among Ph.D. students.
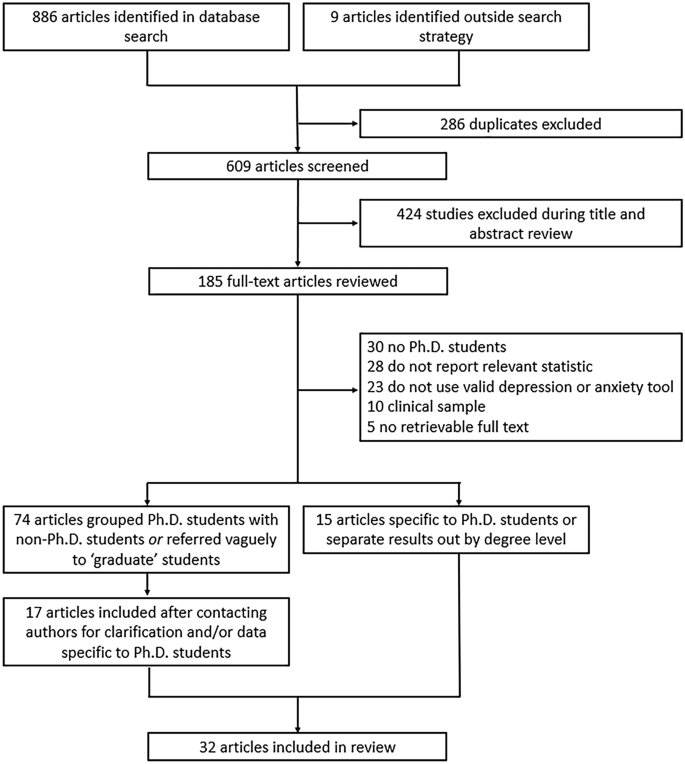
Flowchart of included articles.
The evidence search yielded 886 articles, of which 286 were excluded as duplicates (Fig. 1 ). An additional nine articles were identified through reference lists or grey literature reports published on university websites. Following a title/abstract review and subsequent full-text review, 520 additional articles were excluded.
Of the 89 remaining articles, 74 were unclear about their definition of graduate students or grouped Ph.D. and non-Ph.D. students without disaggregating the estimates by degree level. We obtained contact information for the authors of most of these articles (69 [93%]), requesting additional data. Three authors clarified that their study samples only included Ph.D. students 34 , 35 , 36 . Fourteen authors confirmed that their study samples included both Ph.D. and non-Ph.D. students but provided us with data on the subsample of Ph.D. students 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 . Where authors clarified that the sample was limited to graduate students in non-doctoral degree programs, did not provide additional data on the subsample of Ph.D. students, or did not reply to our information requests, we excluded the studies due to insufficient information (Supplementary Table S1 ).
Ultimately, 32 articles describing the findings of 29 unique studies were identified and included in the review 16 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 (Table 1 ). Overall, 26 studies measured depression, 19 studies measured anxiety, and six studies measured suicidal ideation. Three pairs of articles reported data on the same sample of Ph.D. students 33 , 38 , 45 , 51 , 53 , 56 and were therefore grouped in Table 1 and reported as three studies. Publication dates ranged from 1979 to 2019, but most articles (22/32 [69%]) were published after 2015. Most studies were conducted in the United States (20/29 [69%]), with additional studies conducted in Australia, Belgium, China, Iran, Mexico, and South Korea. Two studies were conducted in cross-national settings representing 48 additional countries. None were conducted in sub-Saharan Africa or South America. Most studies included students completing their degrees in a mix of disciplines (17/29 [59%]), while 12 studies were limited to students in a specific field (e.g., biomedicine, education). The median sample size was 172 students (interquartile range [IQR], 68–654; range, 6–6405). Seven studies focused on mental health outcomes in demographic subgroups, including ethnic or racialized minority students 37 , 41 , 43 , international students 47 , 50 , and sexual and gender minority students 42 , 54 .
In all, 16 studies reported the prevalence of depression among a total of 23,469 Ph.D. students (Fig. 2 ; range, 10–47%). Of these, the most widely used depression scales were the PHQ-9 (9 studies) and variants of the Center for Epidemiologic Studies-Depression scale (CES-D, 4 studies) 63 , and all studies assessed clinically significant symptoms of depression over the past one to two weeks. Three of these studies reported findings based on data from different survey years of the same parent study (the Healthy Minds Study) 40 , 42 , 43 , but due to overlap in the survey years reported across articles, these data were pooled. Most of these studies were based on data collected through online surveys (13/16 [81%]). Ten studies (63%) used random or systematic sampling, four studies (25%) used convenience sampling, and two studies (13%) used multiple sampling techniques.
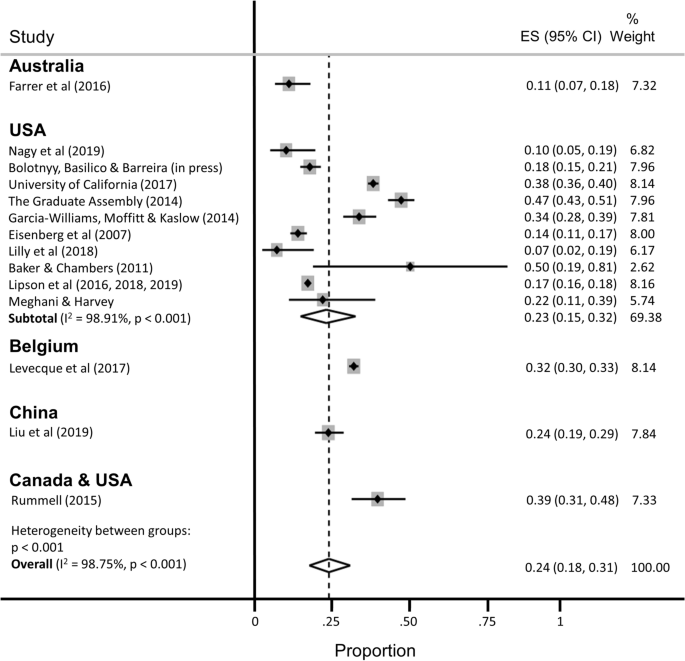
Pooled estimate of the proportion of Ph.D. students with clinically significant symptoms of depression.
The estimated proportion of Ph.D. students assessed as having clinically significant symptoms of depression was 0.24 (95% confidence interval [CI], 0.18–0.31; 95% predictive interval [PI], 0.04–0.54), with significant evidence of between-study heterogeneity (I 2 = 98.75%). A subgroup analysis restricted to the twelve studies conducted in the United States yielded similar findings (pooled estimate [ES] = 0.23; 95% CI, 0.15–0.32; 95% PI, 0.01–0.60), with no appreciable difference in heterogeneity (I 2 = 98.91%). A subgroup analysis restricted to the studies that used the PHQ-9 to assess depression yielded a slightly lower prevalence estimate and a slight reduction in heterogeneity (ES = 0.18; 95% CI, 0.14–0.22; 95% PI, 0.07–0.34; I 2 = 90.59%).
Nine studies reported the prevalence of clinically significant symptoms of anxiety among a total of 15,626 Ph.D. students (Fig. 3 ; range 4–49%). Of these, the most widely used anxiety scale was the 7-item Generalized Anxiety Disorder scale (GAD-7, 5 studies) 64 . Data from three of the Healthy Minds Study articles were pooled into two estimates, because the scale used to measure anxiety changed midway through the parent study (i.e., the Patient Health Questionnaire-Generalized Anxiety Disorder [PHQ-GAD] scale was used from 2007 to 2012 and then switched to the GAD-7 in 2013 40 ). Most studies (8/9 [89%]) assessed clinically significant symptoms of anxiety over the past two to four weeks, with the one remaining study measuring anxiety over the past year. Again, most of these studies were based on data collected through online surveys (7/9 [78%]). Five studies (56%) used random or systematic sampling, two studies (22%) used convenience sampling, and two studies (22%) used multiple sampling techniques.
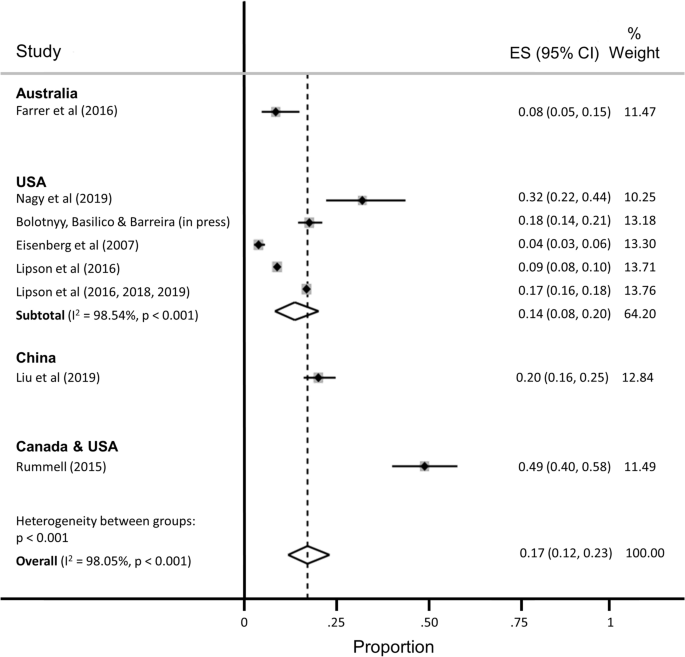
Pooled estimate of the proportion of Ph.D. students with clinically significant symptoms of anxiety.
The estimated proportion of Ph.D. students assessed as having anxiety was 0.17 (95% CI, 0.12–0.23; 95% PI, 0.02–0.41), with significant evidence of between-study heterogeneity (I 2 = 98.05%). The subgroup analysis restricted to the five studies conducted in the United States yielded a slightly lower proportion of students assessed as having anxiety (ES = 0.14; 95% CI, 0.08–0.20; 95% PI, 0.00–0.43), with no appreciable difference in heterogeneity (I 2 = 98.54%).
Six studies reported the prevalence of suicidal ideation (range, 2–12%), but the recall windows varied greatly (e.g., ideation within the past 2 weeks vs. past year), precluding pooled estimation.
Additional stratified pooled estimates could not be obtained. One study of Ph.D. students across 54 countries found that phase of study was a significant moderator of mental health, with students in the comprehensive examination and dissertation phases more likely to experience distress compared with students primarily engaged in coursework 59 . Other studies identified a higher prevalence of mental ill-health among women 54 ; lesbian, gay, bisexual, transgender, and queer (LGBTQ) students 42 , 54 , 60 ; and students with multiple intersecting identities 54 .
Several studies identified correlates of mental health problems including: project- and supervisor-related issues, stress about productivity, and self-doubt 53 , 62 ; uncertain career prospects, poor living conditions, financial stressors, lack of sleep, feeling devalued, social isolation, and advisor relationships 61 ; financial challenges 38 ; difficulties with work-life balance 58 ; and feelings of isolation and loneliness 52 . Despite these challenges, help-seeking appeared to be limited, with only about one-quarter of Ph.D. students reporting mental health problems also reporting that they were receiving treatment 40 , 52 .
Risk of bias
Twenty-one of 32 articles were assessed as having low risk of bias (Supplementary Table S2 ). Five articles received one point for all five categories on the risk of bias assessment (lowest risk of bias), and one article received no points (highest risk). The mean risk of bias score was 3.22 (standard deviation, 1.34; median, 4; IQR, 2–4). Restricting the estimation sample to 12 studies assessed as having low risk of bias, the estimated proportion of Ph.D. students with depression was 0.25 (95% CI, 0.18–0.33; 95% PI, 0.04–0.57; I 2 = 99.11%), nearly identical to the primary estimate, with no reduction in heterogeneity. The estimated proportion of Ph.D. students with anxiety, among the 7 studies assessed as having low risk of bias, was 0.12 (95% CI, 0.07–0.17; 95% PI, 0.01–0.34; I 2 = 98.17%), again with no appreciable reduction in heterogeneity.
In our meta-analysis of 16 studies representing 23,469 Ph.D. students, we estimated that the pooled prevalence of clinically significant symptoms of depression was 24%. This estimate is consistent with estimated prevalence rates in other high-stress biomedical trainee populations, including medical students (27%) 30 , resident physicians (29%) 65 , and postdoctoral research fellows (29%) 66 . In the sample of nine studies representing 15,626 Ph.D. students, we estimated that the pooled prevalence of clinically significant symptoms of anxiety was 17%. While validated screening instruments tend to over-identify cases of depression (relative to structured clinical interviews) by approximately a factor of two 67 , 68 , our findings nonetheless point to a major public health problem among Ph.D. students. Available data suggest that the prevalence of depressive and anxiety disorders in the general population ranges from 5 to 7% worldwide 69 , 70 . In contrast, prevalence estimates of major depressive disorder among young adults have ranged from 13% (for young adults between the ages of 18 and 29 years in the 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions III 71 ) to 15% (for young adults between the ages of 18 and 25 in the 2019 U.S. National Survey on Drug Use and Health 72 ). Likewise, the prevalence of generalized anxiety disorder was estimated at 4% among young adults between the ages of 18 and 29 in the 2001–03 U.S. National Comorbidity Survey Replication 73 . Thus, even accounting for potential upward bias inherent in these studies’ use of screening instruments, our estimates suggest that the rates of recent clinically significant symptoms of depression and anxiety are greater among Ph.D. students compared with young adults in the general population.
Further underscoring the importance of this public health issue, Ph.D. students face unique stressors and uncertainties that may put them at increased risk for mental health and substance use problems. Students grapple with competing responsibilities, including coursework, teaching, and research, while also managing interpersonal relationships, social isolation, caregiving, and financial insecurity 3 , 10 . Increasing enrollment in doctoral degree programs has not been matched with a commensurate increase in tenure-track academic job opportunities, intensifying competition and pressure to find employment post-graduation 5 . Advisor-student power relations rarely offer options for recourse if and when such relationships become strained, particularly in the setting of sexual harassment, unwanted sexual attention, sexual coercion, and rape 74 , 75 , 76 , 77 , 78 . All of these stressors may be magnified—and compounded by stressors unrelated to graduate school—for subgroups of students who are underrepresented in doctoral degree programs and among whom mental health problems are either more prevalent and/or undertreated compared with the general population, including Black, indigenous, and other people of color 13 , 79 , 80 ; women 81 , 82 ; first-generation students 14 , 15 ; people who identify as LGBTQ 83 , 84 , 85 ; people with disabilities; and people with multiple intersecting identities.
Structural- and individual-level interventions will be needed to reduce the burden of mental ill-health among Ph.D. students worldwide 31 , 86 . Despite the high prevalence of mental health and substance use problems 87 , Ph.D. students demonstrate low rates of help-seeking 40 , 52 , 88 . Common barriers to help-seeking include fears of harming one’s academic career, financial insecurity, lack of time, and lack of awareness 89 , 90 , 91 , as well as health care systems-related barriers, including insufficient numbers of culturally competent counseling staff, limited access to psychological services beyond time-limited psychotherapies, and lack of programs that address the specific needs either of Ph.D. students in general 92 or of Ph.D. students belonging to marginalized groups 93 , 94 . Structural interventions focused solely on enhancing student resilience might include programs aimed at reducing stigma, fostering social cohesion, and reducing social isolation, while changing norms around help-seeking behavior 95 , 96 . However, structural interventions focused on changing stressogenic aspects of the graduate student environment itself are also needed 97 , beyond any enhancements to Ph.D. student resilience, including: undercutting power differentials between graduate students and individual faculty advisors, e.g., by diffusing power among multiple faculty advisors; eliminating racist, sexist, and other discriminatory behaviors by faculty advisors 74 , 75 , 98 ; valuing mentorship and other aspects of “invisible work” that are often disproportionately borne by women faculty and faculty of color 99 , 100 ; and training faculty members to emphasize the dignity of, and adequately prepare Ph.D. students for, non-academic careers 101 , 102 .
Our findings should be interpreted with several limitations in mind. First, the pooled estimates are characterized by a high degree of heterogeneity, similar to meta-analyses of depression prevalence in other populations 30 , 65 , 103 , 104 , 105 . Second, we were only able to aggregate depression prevalence across 16 studies and anxiety prevalence across nine studies (the majority of which were conducted in the U.S.) – far fewer than the 183 studies included in a meta-analysis of depression prevalence among medical students 30 and the 54 studies included in a meta-analysis of resident physicians 65 . These differences underscore the need for more rigorous study in this critical area. Many articles were either excluded from the review or from the meta-analyses for not meeting inclusion criteria or not reporting relevant statistics. Future research in this area should ensure the systematic collection of high-quality, clinically relevant data from a comprehensive set of institutions, across disciplines and countries, and disaggregated by graduate student type. As part of conducting research and addressing student mental health and wellbeing, university deans, provosts, and chancellors should partner with national survey and program institutions (e.g., Graduate Student Experience in the Research University [gradSERU] 106 , the American College Health Association National College Health Assessment [ACHA-NCHA], and HealthyMinds). Furthermore, federal agencies that oversee health and higher education should provide resources for these efforts, and accreditation agencies should require monitoring of mental health and programmatic responses to stressors among Ph.D. students.
Third, heterogeneity in reporting precluded a meta-analysis of the suicidality outcomes among the few studies that reported such data. While reducing the burden of mental health problems among graduate students is an important public health aim in itself, more research into understanding non-suicidal self-injurious behavior, suicide attempts, and completed suicide among Ph.D. students is warranted. Fourth, it is possible that the grey literature reports included in our meta-analysis are more likely to be undertaken at research-intensive institutions 52 , 60 , 61 . However, the direction of bias is unpredictable: mental health problems among Ph.D. students in research-intensive environments may be more prevalent due to detection bias, but such institutions may also have more resources devoted to preventive, screening, or treatment efforts 92 . Fifth, inclusion in this meta-analysis and systematic review was limited to those based on community samples. Inclusion of clinic-based samples, or of studies conducted before or after specific milestones (e.g., the qualifying examination or dissertation prospectus defense), likely would have yielded even higher pooled prevalence estimates of mental health problems. And finally, few studies provided disaggregated data according to sociodemographic factors, stage of training (e.g., first year, pre-prospectus defense, all-but-dissertation), or discipline of study. These factors might be investigated further for differences in mental health outcomes.
Clinically significant symptoms of depression and anxiety are pervasive among graduate students in doctoral degree programs, but these are understudied relative to other trainee populations. Structural and clinical interventions to systematically monitor and promote the mental health and wellbeing of Ph.D. students are urgently needed.
This systematic review and meta-analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) approach (Supplementary Table S3 ) 107 . This study was based on data collected from publicly available bibliometric databases and did not require ethical approval from our institutional review boards.
Eligibility criteria
Studies were included if they provided data on either: (a) the number or proportion of Ph.D. students with clinically significant symptoms of depression or anxiety, ascertained using a validated scale; or (b) the mean depression or anxiety symptom severity score and its standard deviation among Ph.D. students. Suicidal ideation was examined as a secondary outcome.
We excluded studies that focused on graduate students in non-doctoral degree programs (e.g., Master of Public Health) or professional degree programs (e.g., Doctor of Medicine, Juris Doctor) because more is known about mental health problems in these populations 30 , 108 , 109 , 110 and because Ph.D. students face unique uncertainties. To minimize the potential for upward bias in our pooled prevalence estimates, we excluded studies that recruited students from campus counseling centers or other clinic-based settings. Studies that measured affective states, or state anxiety, before or after specific events (e.g., terrorist attacks, qualifying examinations) were also excluded.
If articles described the study sample in general terms (i.e., without clarifying the degree level of the participants), we contacted the authors by email for clarification. Similarly, if articles pooled results across graduate students in doctoral and non-doctoral degree programs (e.g., reporting a single estimate for a mixed sample of graduate students), we contacted the authors by email to request disaggregated data on the subsample of Ph.D. students. If authors did not reply after two contact attempts spaced over 2 months, or were unable to provide these data, we excluded these studies from further consideration.
Search strategy and data extraction
PubMed, Embase, PsycINFO, ERIC, and Business Source Complete were searched from inception of each database to November 5, 2019. The search strategy included terms related to mental health symptoms (e.g., depression, anxiety, suicide), the study population (e.g., graduate, doctoral), and measurement category (e.g., depression, Columbia-Suicide Severity Rating Scale) (Supplementary Table S4 ). In addition, we searched the reference lists and the grey literature.
After duplicates were removed, we screened the remaining titles and abstracts, followed by a full-text review. We excluded articles following the eligibility criteria listed above (i.e., those that were not focused on Ph.D. students; those that did not assess depression and/or anxiety using a validated screening tool; those that did not report relevant statistics of depression and/or anxiety; and those that recruited students from clinic-based settings). Reasons for exclusion were tracked at each stage. Following selection of included articles, two members of the research team extracted data and conducted risk of bias assessments. Discrepancies were discussed with a third member of the research team. Key extraction variables included: study design, geographic region, sample size, response rate, demographic characteristics of the sample, screening instrument(s) used for assessment, mean depression or anxiety symptom severity score (and its standard deviation), and the number (or proportion) of students experiencing clinically significant symptoms of depression or anxiety.
Risk of bias assessment
Following prior work 30 , 65 , the Newcastle–Ottawa Scale 111 was adapted and used to assess risk of bias in the included studies. Each study was assessed across 5 categories: sample representativeness, sample size, non-respondents, ascertainment of outcomes, and quality of descriptive statistics reporting (Supplementary Information S5 ). Studies were judged as having either low risk of bias (≥ 3 points) or high risk of bias (< 3 points).
Analysis and synthesis
Before pooling the estimated prevalence rates across studies, we first transformed the proportions using a variance-stabilizing double arcsine transformation 112 . We then computed pooled estimates of prevalence using a random effects model 113 . Study specific confidence intervals were estimated using the score method 114 , 115 . We estimated between-study heterogeneity using the I 2 statistic 116 . In an attempt to reduce the extent of heterogeneity, we re-estimated pooled prevalence restricting the analysis to studies conducted in the United States and to studies in which depression assessment was based on the 9-item Patient Health Questionnaire (PHQ-9) 117 . All analyses were conducted using Stata (version 16; StataCorp LP, College Station, Tex.). Where heterogeneity limited our ability to summarize the findings using meta-analysis, we synthesized the data using narrative review.
Woolston, C. Why mental health matters. Nature 557 , 129–131 (2018).
Article ADS CAS Google Scholar
Woolston, C. A love-hurt relationship. Nature 550 , 549–552 (2017).
Article Google Scholar
Woolston, C. PhD poll reveals fear and joy, contentment and anguish. Nature 575 , 403–406 (2019).
Article ADS CAS PubMed Google Scholar
Byrom, N. COVID-19 and the research community: The challenges of lockdown for early-career researchers. Elife 9 , e59634 (2020).
Article PubMed PubMed Central Google Scholar
Alberts, B., Kirschner, M. W., Tilghman, S. & Varmus, H. Rescuing US biomedical research from its systemic flaws. Proc. Natl. Acad. Sci. USA 111 , 5773–5777 (2014).
Article ADS CAS PubMed PubMed Central Google Scholar
McDowell, G. S. et al. Shaping the future of research: A perspective from junior scientists. F1000Res 3 , 291 (2014).
Article PubMed Google Scholar
Petersen, A. M., Riccaboni, M., Stanley, H. E. & Pammoli, F. Persistence and uncertainty in the academic career. Proc. Natl. Acad. Sci. USA 109 , 5213–5218 (2012).
Leshner, A. I. Rethinking graduate education. Science 349 , 349 (2015).
National Academies of Sciences Engineering and Medicine. Graduate STEM Education for the 21st Century (National Academies Press, 2018).
Google Scholar
Charles, S. T., Karnaze, M. M. & Leslie, F. M. Positive factors related to graduate student mental health. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1841207 (2021).
Riddle, E. S., Niles, M. T. & Nickerson, A. Prevalence and factors associated with food insecurity across an entire campus population. PLoS ONE 15 , e0237637 (2020).
Article CAS PubMed PubMed Central Google Scholar
Soldavini, J., Berner, M. & Da Silva, J. Rates of and characteristics associated with food insecurity differ among undergraduate and graduate students at a large public university in the Southeast United States. Prev. Med. Rep. 14 , 100836 (2019).
Clark, U. S. & Hurd, Y. L. Addressing racism and disparities in the biomedical sciences. Nat. Hum. Behav. 4 , 774–777 (2020).
Gardner, S. K. The challenges of first-generation doctoral students. New Dir. High. Educ. 2013 , 43–54 (2013).
Seay, S. E., Lifton, D. E., Wuensch, K. L., Bradshaw, L. K. & McDowelle, J. O. First-generation graduate students and attrition risks. J. Contin. High. Educ. 56 , 11–25 (2008).
Rummell, C. M. An exploratory study of psychology graduate student workload, health, and program satisfaction. Prof. Psychol. Res. Pract. 46 , 391–399 (2015).
Salzer, M. S. A comparative study of campus experiences of college students with mental illnesses versus a general college sample. J. Am. Coll. Health 60 , 1–7 (2012).
Hysenbegasi, A., Hass, S. & Rowland, C. The impact of depression on the academic productivity of university students. J. Ment. Health Policy Econ. 8 , 145–151 (2005).
PubMed Google Scholar
Harvey, S. et al. Depression and work performance: An ecological study using web-based screening. Occup. Med. (Lond.) 61 , 209–211 (2011).
Article CAS Google Scholar
Eisenberg, D., Golberstein, E. & Hunt, J. B. Mental health and academic success in college. BE J. Econ. Anal. Policy 9 , 40 (2009).
Lovitts, B. E. Who is responsible for graduate student attrition--the individual or the institution? Toward an explanation of the high and persistent rate of attrition. In: Annual Meeting of the American Education Research Association (New York, 1996). Available at: https://eric.ed.gov/?id=ED399878.
Gardner, S. K. Student and faculty attributions of attrition in high and low-completing doctoral programs in the United States. High. Educ. 58 , 97–112 (2009).
Lovitts, B. E. Leaving the Ivory Tower: The Causes and Consequences of Departure from Doctoral Study (Rowman & Littlefield Publishers, 2001).
Rigler Jr, K. L., Bowlin, L. K., Sweat, K., Watts, S. & Throne, R. Agency, socialization, and support: a critical review of doctoral student attrition. In: Proceedings of the Third International Conference on Doctoral Education: Organizational Leadership and Impact , University of Central Florida, Orlando, (2017).
Golde, C. M. The role of the department and discipline in doctoral student attrition: Lessons from four departments. J. High. Educ. 76 , 669–700 (2005).
Council of Graduate Schools. PhD Completion and Attrition: Analysis of Baseline Program Data from the PhD Completion Project (Council of Graduate Schools, 2008).
National Research Council. A Data-Based Assessment of Research-Doctorate Programs in the United States (The National Academies Press, 2011).
Akhtar, P. et al. Prevalence of depression among university students in low and middle income countries (LMICs): A systematic review and meta-analysis. J. Affect. Disord. 274 , 911–919 (2020).
Mortier, P. et al. The prevalence of suicidal thoughts and behaviours among college students: A meta-analysis. Psychol. Med. 48 , 554–565 (2018).
Article CAS PubMed Google Scholar
Rotenstein, L. S. et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: A systematic review and meta-analysis. JAMA 316 , 2214–2236 (2016).
Tsai, J. W. & Muindi, F. Towards sustaining a culture of mental health and wellness for trainees in the biosciences. Nat. Biotechnol. 34 , 353–355 (2016).
Levecque, K., Anseel, F., De Beuckelaer, A., Van der Heyden, J. & Gisle, L. Work organization and mental health problems in PhD students. Res. Policy 46 , 868–879 (2017).
Nagy, G. A. et al. Burnout and mental health problems in biomedical doctoral students. CBE Life Sci. Educ. 18 , 1–14 (2019).
Garcia-Williams, A., Moffitt, L. & Kaslow, N. J. Mental health and suicidal behavior among graduate students. Acad. Psychiatry 28 , 554–560 (2014).
Sheldon, K. M. Emotionality differences between artists and scientists. J. Res. Pers. 28 , 481–491 (1994).
Lightstone, S. N., Swencionis, C. & Cohen, H. W. The effect of bioterrorism messages on anxiety levels. Int. Q. Community Health Educ. 24 , 111–122 (2006).
Clark, C. R., Mercer, S. H., Zeigler-Hill, V. & Dufrene, B. A. Barriers to the success of ethnic minority students in school psychology graduate programs. School Psych. Rev. 41 , 176–192 (2012).
Eisenberg, D., Gollust, S. E., Golberstein, E. & Hefner, J. L. Prevalence and correlates of depression, anxiety, and suicidality among university students. Am. J. Orthopsychiatry 77 , 534–542 (2007).
Farrer, L. M., Gulliver, A., Bennett, K., Fassnacht, D. B. & Griffiths, K. M. Demographic and psychosocial predictors of major depression and generalised anxiety disorder in Australian university students. BMC Psychiatry 16 , 241 (2016).
Lipson, S. K., Zhou, S., Wagner, B. III., Beck, K. & Eisenberg, D. Major differences: Variations in undergraduate and graduate student mental health and treatment utilization across academic disciplines. J. Coll. Stud. Psychother. 30 , 23–41 (2016).
Lilly, F. R. W. et al. The influence of racial microaggressions and social rank on risk for depression among minority graduate and professional students. Coll. Stud. J. 52 , 86–104 (2018).
Lipson, S. K., Raifman, J., Abelson, S. & Reisner, S. L. Gender minority mental health in the U.S.: Results of a national survey on college campuses. Am. J. Prev. Med. 57 , 293–301 (2019).
Lipson, S. K., Kern, A., Eisenberg, D. & Breland-Noble, A. M. Mental health disparities among college students of color. J. Adolesc. Health 63 , 348–356 (2018).
Baker, A. J. L. & Chambers, J. Adult recall of childhood exposure to parental conflict: Unpacking the black box of parental alienation. J. Divorce Remarriage 52 , 55–76 (2011).
Golberstein, E., Eisenberg, D. & Gollust, S. E. Perceived stigma and mental health care seeking. Psychiatr. Serv. 59 , 392–399 (2008).
Hindman, R. K., Glass, C. R., Arnkoff, D. B. & Maron, D. D. A comparison of formal and informal mindfulness programs for stress reduction in university students. Mindfulness 6 , 873–884 (2015).
Hirai, R., Frazier, P. & Syed, M. Psychological and sociocultural adjustment of first-year international students: Trajectories and predictors. J. Couns. Psychol. 62 , 438–452 (2015).
Lee, J. S. & Jeong, B. Having mentors and campus social networks moderates the impact of worries and video gaming on depressive symptoms: A moderated mediation analysis. BMC Public Health 14 , 1–12 (2014).
Corral-Frias, N. S., Velardez Soto, S. N., Frias-Armenta, M., Corona-Espinosa, A. & Watson, D. Concurrent validity and reliability of two short forms of the mood and anxiety symptom questionnaire in a student sample from Northwest Mexico. J. Psychopathol. Behav. Assess. 41 , 304–316 (2019).
Meghani, D. T. & Harvey, E. A. Asian Indian international students’ trajectories of depression, acculturation, and enculturation. Asian Am. J. Psychol. 7 , 1–14 (2016).
Barry, K. M., Woods, M., Martin, A., Stirling, C. & Warnecke, E. A randomized controlled trial of the effects of mindfulness practice on doctoral candidate psychological status. J. Am. Coll. Health 67 , 299–307 (2019).
Bolotnyy, V., Basilico, M. & Barreira, P. Graduate student mental health: lessons from American economics departments. J. Econ. Lit. (in press).
Barry, K. M., Woods, M., Warnecke, E., Stirling, C. & Martin, A. Psychological health of doctoral candidates, study-related challenges and perceived performance. High. Educ. Res. Dev. 37 , 468–483 (2018).
Boyle, K. M. & McKinzie, A. E. The prevalence and psychological cost of interpersonal violence in graduate and law school. J. Interpers. Violence 36 , 6319-6350 (2021).
Heinrich, D. L. The causal influence of anxiety on academic achievement for students of differing intellectual ability. Appl. Psychol. Meas. 3 , 351–359 (1979).
Hish, A. J. et al. Applying the stress process model to stress-burnout and stress-depression relationships in biomedical doctoral students: A cross-sectional pilot study. CBE Life Sci. Educ. 18 , 1–11 (2019).
Jamshidi, F. et al. A cross-sectional study of psychiatric disorders in medical sciences students. Mater. Sociomed. 29 , 188–191 (2017).
Liu, C. et al. Prevalence and associated factors of depression and anxiety among doctoral students: The mediating effect of mentoring relationships on the association between research self-efficacy and depression/anxiety. Psychol. Res. Behav. Manag. 12 , 195–208 (2019).
Sverdlik, A. & Hall, N. C. Not just a phase: Exploring the role of program stage on well-being and motivation in doctoral students. J. Adult Contin. Educ. 26 , 1–28 (2019).
University of California Office of the President. The University of California Graduate student Well-Being Survey Report (University of California, 2017).
The Graduate Assembly. Graduate Student Happiness & Well-Being Report (University of California at Berkeley, 2014).
Richardson, C. M., Trusty, W. T. & George, K. A. Trainee wellness: Self-critical perfectionism, self-compassion, depression, and burnout among doctoral trainees in psychology. Couns. Psychol. Q. 33 , 187-198 (2020).
Radloff, L. S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1 , 385–401 (1977).
Spitzer, R. L., Kroenke, K., Williams, J. B. W. & Lowe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 166 , 1092–1097 (2006).
Mata, D. A. et al. Prevalence of depression and depressive symptoms among residents physicians: A systematic review and meta-analysis. JAMA 314 , 2373–2383 (2015).
Gloria, C. T. & Steinhardt, M. A. Flourishing, languishing, and depressed postdoctoral fellows: Differences in stress, anxiety, and depressive symptoms. J. Postdoct. Aff. 3 , 1–9 (2013).
Levis, B. et al. Patient Health Questionnaire-9 scores do not accurately estimate depression prevalence: Individual participant data meta-analysis. J. Clin. Epidemiol. 122 , 115-128.e111 (2020).
Tsai, A. C. Reliability and validity of depression assessment among persons with HIV in sub-Saharan Africa: Systematic review and meta-analysis. J. Acquir. Immune Defic. Syndr. 66 , 503–511 (2014).
Baxter, A. J., Scott, K. M., Vos, T. & Whiteford, H. A. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol. Med. 43 , 897–910 (2013).
Ferrari, A. et al. Global variation in the prevalence and incidence of major depressive disorder: A systematic review of the epidemiological literature. Psychol. Med. 43 , 471–481 (2013).
Hasin, D. S. et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry 75 , 336–346 (2018).
US Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2020).
Kessler, R. C. et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62 , 593–602 (2005).
Working Group report to the Advisory Committee to the NIH Director. Changing the Culture to End Sexual Harassment (U. S. National Institutes of Health, 2019).
National Academies of Sciences Engineering and Medicine. Sexual Harassment of Women: Climate, Culture, and Consequences in Academic Sciences, Engineering, and Medicine (The National Academies Press, 2018).
Wadman, M. A hidden history. Science 360 , 480–485 (2018).
Hockfield, S., Magley, V. & Yoshino, K. Report of the External Review Committee to Review Sexual Harassment at Harvard University (External Review Committee to Review Sexual Harassment at Harvard University, 2021).
Bartlett, T. & Gluckman, N. She left Harvard. He got to stay. Chronicle High. Educ. 64 , A14 (2021). Available at: https://www.chronicle.com/article/she-left-harvard-he-got-to-stay/.
Tseng, M. et al. Strategies and support for Black, Indigenous, and people of colour in ecology and evolutionary biology. Nat. Ecol. Evol. 4 , 1288–1290 (2020).
Williams, D. R. et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Arch. Gen. Psychiatry 64 , 305–315 (2007).
Wu, A. H. Gender bias in rumors among professionals: An identity-based interpretation. Rev. Econ. Stat. 102 , 867–880 (2020).
Kessler, R. C. Epidemiology of women and depression. J. Affect. Disord. 74 , 5–13 (2003).
Mattheis, A., Cruz-Ramirez De Arellano, D. & Yoder, J. B. A model of queer STEM identity in the workplace. J. Homosex 67 , 1839–1863 (2020).
Semlyen, J., King, M., Varney, J. & Hagger-Johnson, G. Sexual orientation and symptoms of common mental disorder or low wellbeing: Combined meta-analysis of 12 UK population health surveys. BMC Psychiatry 16 , 1–19 (2016).
Lark, J. S. & Croteau, J. M. Lesbian, gay, and bisexual doctoral students’ mentoring relationships with faculty in counseling psychology: A qualitative study. Couns. Psychol. 26 , 754–776 (1998).
Jaremka, L. M. et al. Common academic experiences no one talks about: Repeated rejection, imposter syndrome, and burnout. Perspect Psychol Sci 15 , 519–543 (2020).
Allen, H. K. et al. Substance use and mental health problems among graduate students: Individual and program-level correlates. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1725020 (2020).
Turner, A. & Berry, T. Counseling center contributions to student retention and graduation: A longitudinal assessment. J. Coll. Stud. Dev. 41 , 627–636 (2000).
Dyrbye, L. N., Thomas, M. R. & Shanafelt, T. D. Medical student distress: Causes, consequences, and proposed solutions. Mayo Clin. Proc. 80 , 1613–1622 (2005).
Tija, J., Givens, J. L. & Shea, J. A. Factors associated with undertreatment of medical student depression. J. Am. Coll. Health 53 , 219–224 (2005).
Dearing, R., Maddux, J. & Tangney, J. Predictors of psychological help seeking in clinical and counseling psychology graduate students. Prof. Psychol. Res. Pract. 36 , 323–329 (2005).
Langin, K. Amid concerns about grad student mental health, one university takes a novel approach. Science https://doi.org/10.1126/science.caredit.aay7113 (2019).
Guillory, D. Combating anti-blackness in the AI community. arXiv , arXiv:2006.16879 (2020).
Galán, C. A. et al. A call to action for an antiracist clinical science. J. Clin. Child Adolesc. Psychol 50 , 12-57 (2021).
Wyman, P. A. et al. Effect of the Wingman-Connect upstream suicide prevention program for air force personnel in training: A cluster randomized clinical trial. JAMA Netw Open 3 , e2022532 (2020).
Knox, K. L. et al. The US Air Force Suicide Prevention Program: Implications for public health policy. Am. J. Public Health 100 , 2457–2463 (2010).
Inclusive Climate Subcommittee of the Government Department Climate Change Committee. Government Department Climate Change: Final Report and Recommendations (Government Department, Harvard University, 2019).
Inclusive Climate Subcommittee of the Government Department Climate Change Committee. Government Department Climate Survey Report (Government Department, Harvard University, 2019).
Magoqwana, B., Maqabuka, Q. & Tshoaedi, M. “Forced to care” at the neoliberal university: Invisible labour as academic labour performed by Black women academics in the South African university. S. Afr. Rev. Sociol. 50 , 6–21 (2019).
Jones, H. A., Perrin, P. B., Heller, M. B., Hailu, S. & Barnett, C. Black psychology graduate students’ lives matter: Using informal mentoring to create an inclusive climate amidst national race-related events. Prof. Psychol. Res. Pract. 49 , 75–82 (2018).
Mathur, A., Meyers, F. J., Chalkley, R., O’Brien, T. C. & Fuhrmann, C. N. Transforming training to reflect the workforce. Sci. Transl. Med. 7 , 285 (2015).
Scharff, V. Advice: Prepare your Ph.D.s for diverse career paths. Chronicle High. Educ. 65 , 30 (2018).
Beattie, T. S., Smilenova, B., Krishnaratne, S. & Mazzuca, A. Mental health problems among female sex workers in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 17 , e1003297 (2020).
Ismail, Z. et al. Prevalence of depression in patients with mild cognitive impairment: A systematic review and meta-analysis. JAMA Psychiatry 74 , 58–67 (2017).
Lim, G. Y. et al. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 8 , 1–10 (2018).
Article ADS Google Scholar
Jones-White, D. R., Soria, K. M., Tower, E. K. B. & Horner, O. G. Factors associated with anxiety and depression among U.S. doctoral students: Evidence from the gradSERU survey. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1865975 (2021).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 151 , 264–269 (2009).
Helmers, K. F., Danoff, D., Steinert, Y., Leyton, M. & Young, S. N. Stress and depressed mood in medical students, law students, and graduate students at McGill University. Acad. Med. 72 , 708–714 (1997).
Rabkow, N. et al. Facing the truth: A report on the mental health situation of German law students. Int. J. Law Psychiatry 71 , 101599 (2020).
Bergin, A. & Pakenham, K. Law student stress: Relationships between academic demands, social isolation, career pressure, study/life imbalance and adjustment outcomes in law students. Psychiatr. Psychol. Law 22 , 388–406 (2015).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25 , 603–605 (2010).
Freeman, M. F. & Tukey, J. W. Transformations related to the angular and the square root. Ann. Math. Stat. 21 , 607–611 (1950).
Article MathSciNet MATH Google Scholar
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 7 , 177–188 (1986).
Wilson, E. B. Probable inference, the law of succession, and statistical inference. J. Am. Stat. Assoc. 22 , 209–212 (1927).
Newcombe, R. G. Two-sided confidence intervals for the single proportion: Comparison of seven methods. Stat. Med. 17 , 857–872 (1998).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21 , 1539–1558 (2002).
Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 16 , 606–613 (2001).
Download references
Acknowledgements
We thank the following investigators for generously sharing their time and/or data: Gordon J. G. Asmundson, Ph.D., Amy J. L. Baker, Ph.D., Hillel W. Cohen, Dr.P.H., Alcir L. Dafre, Ph.D., Deborah Danoff, M.D., Daniel Eisenberg, Ph.D., Lou Farrer, Ph.D., Christy B. Fraenza, Ph.D., Patricia A. Frazier, Ph.D., Nadia Corral-Frías, Ph.D., Hanga Galfalvy, Ph.D., Edward E. Goldenberg, Ph.D., Robert K. Hindman, Ph.D., Jürgen Hoyer, Ph.D., Ayako Isato, Ph.D., Azharul Islam, Ph.D., Shanna E. Smith Jaggars, Ph.D., Bumseok Jeong, M.D., Ph.D., Ju R. Joeng, Nadine J. Kaslow, Ph.D., Rukhsana Kausar, Ph.D., Flavius R. W. Lilly, Ph.D., Sarah K. Lipson, Ph.D., Frances Meeten, D.Phil., D.Clin.Psy., Dhara T. Meghani, Ph.D., Sterett H. Mercer, Ph.D., Masaki Mori, Ph.D., Arif Musa, M.D., Shizar Nahidi, M.D., Ph.D., Arthur M. Nezu, Ph.D., D.H.L., Angelo Picardi, M.D., Nicole E. Rossi, Ph.D., Denise M. Saint Arnault, Ph.D., Sagar Sharma, Ph.D., Bryony Sheaves, D.Clin.Psy., Kennon M. Sheldon, Ph.D., Daniel Shepherd, Ph.D., Keisuke Takano, Ph.D., Sara Tement, Ph.D., Sherri Turner, Ph.D., Shawn O. Utsey, Ph.D., Ron Valle, Ph.D., Caleb Wang, B.S., Pengju Wang, Katsuyuki Yamasaki, Ph.D.
A.C.T. acknowledges funding from the Sullivan Family Foundation. This paper does not reflect an official statement or opinion from the County of San Mateo.
Author information
Authors and affiliations.
Center for Global Health, Massachusetts General Hospital, Boston, MA, USA
Emily N. Satinsky & Alexander C. Tsai
San Mateo County Behavioral Health and Recovery Services, San Mateo, CA, USA
Tomoki Kimura
Department of Epidemiology and Population Health, Stanford University, Palo Alto, CA, USA
Mathew V. Kiang
Center for Population Health Sciences, Stanford University School of Medicine, Palo Alto, CA, USA
Harvard Society of Fellows, Harvard University, Cambridge, MA, USA
Rediet Abebe
Department of Electrical Engineering and Computer Science, University of California Berkeley, Berkeley, CA, USA
Department of Economics, Hankamer School of Business, Baylor University, Waco, TX, USA
Scott Cunningham
Department of Sociology, Washington University in St. Louis, St. Louis, MO, USA
Department of Microbiology, Immunology, and Molecular Genetics, Institute for Quantitative and Computational Biosciences, University of California Los Angeles, Los Angeles, CA, USA
Xiaofei Lin
Departments of Newborn Medicine and Psychiatry, Brigham and Women’s Hospital, Boston, MA, USA
Cindy H. Liu
Harvard Medical School, Boston, MA, USA
Cindy H. Liu & Alexander C. Tsai
Centre for Global Health, Edinburgh Medical School, Usher Institute, University of Edinburgh, Edinburgh, Scotland, UK
Department of Psychiatry, University of Michigan, Ann Arbor, MI, USA
Department of Global Health, Institute for Life Course Health Research, Stellenbosch University, Cape Town, South Africa
Mark Tomlinson
School of Nursing and Midwifery, Queens University, Belfast, UK
Fielding School of Public Health, Los Angeles Area Health Services Research Training Program, University of California Los Angeles, Los Angeles, CA, USA
Miranda Yaver
Mongan Institute, Massachusetts General Hospital, Boston, MA, USA
Alexander C. Tsai
You can also search for this author in PubMed Google Scholar
Contributions
A.C.T. conceptualized the study and provided supervision. T.K. conducted the search. E.N.S. contacted authors for additional information not reported in published articles. E.N.S. and T.K. extracted data and performed the quality assessment appraisal. E.N.S. and A.C.T. conducted the statistical analysis and drafted the manuscript. T.K., M.V.K., R.A., S.C., H.L., X.L., C.H.L., I.R., S.S., M.T. and M.Y. contributed to the interpretation of the results. All authors provided critical feedback on drafts and approved the final manuscript.
Corresponding authors
Correspondence to Emily N. Satinsky or Alexander C. Tsai .

Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Satinsky, E.N., Kimura, T., Kiang, M.V. et al. Systematic review and meta-analysis of depression, anxiety, and suicidal ideation among Ph.D. students. Sci Rep 11 , 14370 (2021). https://doi.org/10.1038/s41598-021-93687-7
Download citation
Received : 31 March 2021
Accepted : 24 June 2021
Published : 13 July 2021
DOI : https://doi.org/10.1038/s41598-021-93687-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
How to improve academic well-being: an analysis of the leveraging factors based on the italian case.
- Alice Tontodimamma
- Emiliano del Gobbo
- Antonio Aquino
Quality & Quantity (2024)
Suicidal affective risk among female college students: the impact of life satisfaction
- Dawei Huang
- Xianbin Wang
Current Psychology (2024)
A single-center assessment of mental health and well-being in a biomedical sciences graduate program
- Sarah K. Jachim
- Bradley S. Bowles
- Autumn J. Schulze
Nature Biotechnology (2023)
Mental Health Problems Among Graduate Students in Turkey: a Cross-Sectional Study
- Cafer Kılıç
- Faika Şanal Karahan
International Journal for the Advancement of Counselling (2023)
A study in University of Ruhuna for investigating prevalence, risk factors and remedies for psychiatric illnesses among students
- Patikiri Arachchige Don Shehan Nilm Wijesekara
Scientific Reports (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
7 Depression Research Paper Topic Ideas
Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
In psychology classes, it's common for students to write a depression research paper. Researching depression may be beneficial if you have a personal interest in this topic and want to learn more, or if you're simply passionate about this mental health issue. However, since depression is a very complex subject, it offers many possible topics to focus on, which may leave you wondering where to begin.
If this is how you feel, here are a few research titles about depression to help inspire your topic choice. You can use these suggestions as actual research titles about depression, or you can use them to lead you to other more in-depth topics that you can look into further for your depression research paper.
What Is Depression?
Everyone experiences times when they feel a little bit blue or sad. This is a normal part of being human. Depression, however, is a medical condition that is quite different from everyday moodiness.
Your depression research paper may explore the basics, or it might delve deeper into the definition of clinical depression or the difference between clinical depression and sadness .
What Research Says About the Psychology of Depression
Studies suggest that there are biological, psychological, and social aspects to depression, giving you many different areas to consider for your research title about depression.
Types of Depression
There are several different types of depression that are dependent on how an individual's depression symptoms manifest themselves. Depression symptoms may vary in severity or in what is causing them. For instance, major depressive disorder (MDD) may have no identifiable cause, while postpartum depression is typically linked to pregnancy and childbirth.
Depressive symptoms may also be part of an illness called bipolar disorder. This includes fluctuations between depressive episodes and a state of extreme elation called mania. Bipolar disorder is a topic that offers many research opportunities, from its definition and its causes to associated risks, symptoms, and treatment.
Causes of Depression
The possible causes of depression are many and not yet well understood. However, it most likely results from an interplay of genetic vulnerability and environmental factors. Your depression research paper could explore one or more of these causes and reference the latest research on the topic.
For instance, how does an imbalance in brain chemistry or poor nutrition relate to depression? Is there a relationship between the stressful, busier lives of today's society and the rise of depression? How can grief or a major medical condition lead to overwhelming sadness and depression?
Who Is at Risk for Depression?
This is a good research question about depression as certain risk factors may make a person more prone to developing this mental health condition, such as a family history of depression, adverse childhood experiences, stress , illness, and gender . This is not a complete list of all risk factors, however, it's a good place to start.
The growing rate of depression in children, teenagers, and young adults is an interesting subtopic you can focus on as well. Whether you dive into the reasons behind the increase in rates of depression or discuss the treatment options that are safe for young people, there is a lot of research available in this area and many unanswered questions to consider.
Depression Signs and Symptoms
The signs of depression are those outward manifestations of the illness that a doctor can observe when they examine a patient. For example, a lack of emotional responsiveness is a visible sign. On the other hand, symptoms are subjective things about the illness that only the patient can observe, such as feelings of guilt or sadness.
An illness such as depression is often invisible to the outside observer. That is why it is very important for patients to make an accurate accounting of all of their symptoms so their doctor can diagnose them properly. In your depression research paper, you may explore these "invisible" symptoms of depression in adults or explore how depression symptoms can be different in children .
How Is Depression Diagnosed?
This is another good depression research topic because, in some ways, the diagnosis of depression is more of an art than a science. Doctors must generally rely upon the patient's set of symptoms and what they can observe about them during their examination to make a diagnosis.
While there are certain laboratory tests that can be performed to rule out other medical illnesses as a cause of depression, there is not yet a definitive test for depression itself.
If you'd like to pursue this topic, you may want to start with the Diagnostic and Statistical Manual of Mental Disorders (DSM). The fifth edition, known as DSM-5, offers a very detailed explanation that guides doctors to a diagnosis. You can also compare the current model of diagnosing depression to historical methods of diagnosis—how have these updates improved the way depression is treated?
Treatment Options for Depression
The first choice for depression treatment is generally an antidepressant medication. Selective serotonin reuptake inhibitors (SSRIs) are the most popular choice because they can be quite effective and tend to have fewer side effects than other types of antidepressants.
Psychotherapy, or talk therapy, is another effective and common choice. It is especially efficacious when combined with antidepressant therapy. Certain other treatments, such as electroconvulsive therapy (ECT) or vagus nerve stimulation (VNS), are most commonly used for patients who do not respond to more common forms of treatment.
Focusing on one of these treatments is an option for your depression research paper. Comparing and contrasting several different types of treatment can also make a good research title about depression.
A Word From Verywell
The topic of depression really can take you down many different roads. When making your final decision on which to pursue in your depression research paper, it's often helpful to start by listing a few areas that pique your interest.
From there, consider doing a little preliminary research. You may come across something that grabs your attention like a new study, a controversial topic you didn't know about, or something that hits a personal note. This will help you narrow your focus, giving you your final research title about depression.
Remes O, Mendes JF, Templeton P. Biological, psychological, and social determinants of depression: A review of recent literature . Brain Sci . 2021;11(12):1633. doi:10.3390/brainsci11121633
National Institute of Mental Health. Depression .
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition . American Psychiatric Association.
National Institute of Mental Health. Mental health medications .
Ferri, F. F. (2019). Ferri's Clinical Advisor 2020 E-Book: 5 Books in 1 . Netherlands: Elsevier Health Sciences.
By Nancy Schimelpfening Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
- Open access
- Published: 16 May 2024
Procrastination, depression and anxiety symptoms in university students: a three-wave longitudinal study on the mediating role of perceived stress
- Anna Jochmann 1 ,
- Burkhard Gusy 1 ,
- Tino Lesener 1 &
- Christine Wolter 1
BMC Psychology volume 12 , Article number: 276 ( 2024 ) Cite this article
719 Accesses
Metrics details
It is generally assumed that procrastination leads to negative consequences. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. Therefore, the aim of our study was to examine the harmful consequences of procrastination on students’ stress and mental health. We selected the procrastination-health model as our theoretical foundation and tried to evaluate the model’s assumption that trait procrastination leads to (chronic) disease via (chronic) stress in a temporal perspective. We chose depression and anxiety symptoms as indicators for (chronic) disease and hypothesized that procrastination leads to perceived stress over time, that perceived stress leads to depression and anxiety symptoms over time, and that procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress.
To examine these relationships properly, we collected longitudinal data from 392 university students at three occasions over a one-year period and analyzed the data using autoregressive time-lagged panel models.
Procrastination did lead to depression and anxiety symptoms over time. However, perceived stress was not a mediator of this effect. Procrastination did not lead to perceived stress over time, nor did perceived stress lead to depression and anxiety symptoms over time.
Conclusions
We could not confirm that trait procrastination leads to (chronic) disease via (chronic) stress, as assumed in the procrastination-health model. Nonetheless, our study demonstrated that procrastination can have a detrimental effect on mental health. Further health outcomes and possible mediators should be explored in future studies.
Peer Review reports
Introduction
“Due tomorrow? Do tomorrow.”, might be said by someone who has a tendency to postpone tasks until the last minute. But can we enjoy today knowing about the unfinished task and tomorrow’s deadline? Or do we feel guilty for postponing a task yet again? Do we get stressed out because we have little time left to complete it? Almost everyone has procrastinated at some point when it came to completing unpleasant tasks, such as mowing the lawn, doing the taxes, or preparing for exams. Some tend to procrastinate more frequently and in all areas of life, while others are less inclined to do so. Procrastination is common across a wide range of nationalities, as well as socioeconomic and educational backgrounds [ 1 ]. Over the last fifteen years, there has been a massive increase in research on procrastination [ 2 ]. Oftentimes, research focuses on better understanding the phenomenon of procrastination and finding out why someone procrastinates in order to be able to intervene. Similarly, the internet is filled with self-help guides that promise a way to overcome procrastination. But why do people seek help for their procrastination? Until now, not much research has been conducted on the negative consequences procrastination could have on health and well-being. Therefore, in the following article we examine the effect of procrastination on mental health over time and stress as a possible facilitator of this relationship on the basis of the procrastination-health model by Sirois et al. [ 3 ].
Procrastination and its negative consequences
Procrastination can be defined as the tendency to voluntarily and irrationally delay intended activities despite expecting negative consequences as a result of the delay [ 4 , 5 ]. It has been observed in a variety of groups across the lifespan, such as students, teachers, and workers [ 1 ]. For example, some students tend to regularly delay preparing for exams and writing essays until the last minute, even if this results in time pressure or lower grades. Procrastination must be distinguished from strategic delay [ 4 , 6 ]. Delaying a task is considered strategic when other tasks are more important or when more resources are needed before the task can be completed. While strategic delay is viewed as functional and adaptive, procrastination is classified as dysfunctional. Procrastination is predominantly viewed as the result of a self-regulatory failure [ 7 ]. It can be understood as a trait, that is, as a cross-situational and time-stable behavioral disposition [ 8 ]. Thus, it is assumed that procrastinators chronically delay tasks that they experience as unpleasant or difficult [ 9 ]. Approximately 20 to 30% of adults have been found to procrastinate chronically [ 10 , 11 , 12 ]. Prevalence estimates for students are similar [ 13 ]. It is believed that students do not procrastinate more often than other groups. However, it is easy to examine procrastination in students because working on study tasks requires a high degree of self-organization and time management [ 14 ].
It is generally assumed that procrastination leads to negative consequences [ 4 ]. Negative consequences are even part of the definition of procrastination. Research indicates that procrastination is linked to lower academic performance [ 15 ], health impairment (e.g., stress [ 16 ], physical symptoms [ 17 ], depression and anxiety symptoms [ 18 ]), and poor health-related behavior (e.g., heavier alcohol consumption [ 19 ]). However, most studies targeting consequences of procrastination are cross-sectional [ 4 ]. For that reason, it often remains unclear whether an examined outcome is a consequence or an antecedent of procrastination, or whether a reciprocal relationship between procrastination and the examined outcome can be assumed. Additionally, regarding negative consequences of procrastination on health, it is still largely unknown by which mechanisms they are mediated. Uncovering such mediators would be helpful in developing interventions that can prevent negative health consequences of procrastination.
The procrastination-health model
The first and only model that exclusively focuses on the effect of procrastination on health and the mediators of this effect is the procrastination-health model [ 3 , 9 , 17 ]. Sirois [ 9 ] postulates three pathways: An immediate effect of trait procrastination on (chronic) disease and two mediated pathways (see Fig. 1 ).
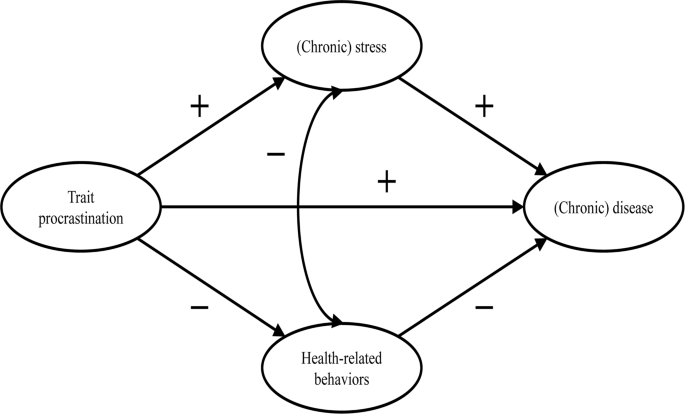
Adopted from the procrastination-health model by Sirois [ 9 ]
The immediate effect is not further explained. Research suggests that procrastination creates negative feelings, such as shame, guilt, regret, and anger [ 20 , 21 , 22 ]. The described feelings could have a detrimental effect on mental health [ 23 , 24 , 25 ].
The first mediated pathway leads from trait procrastination to (chronic) disease via (chronic) stress. Sirois [ 9 ] assumes that procrastination creates stress because procrastinators are constantly aware of the fact that they still have many tasks to complete. Stress activates the hypothalamic-pituitary-adrenocortical (HPA) system, increases autonomic nervous system arousal, and weakens the immune system, which in turn contributes to the development of diseases. Sirois [ 9 ] distinguishes between short-term and long-term effects of procrastination on health mediated by stress. She believes that, in the short term, single incidents of procrastination cause acute stress, which leads to acute health problems, such as infections or headaches. In the long term, chronic procrastination, as you would expect with trait procrastination, causes chronic stress, which leads to chronic diseases over time. There is some evidence in support of the stress-related pathway, particularly regarding short-term effects [ 3 , 17 , 26 , 27 , 28 ]. However, as we mentioned above, most of these studies are cross-sectional. Therefore, the causal direction of these effects remains unclear. To our knowledge, long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress have not yet been investigated.
The second mediated pathway leads from trait procrastination to (chronic) disease via poor health-related behavior. According to Sirois [ 9 ], procrastinators form lower intentions to carry out health-promoting behavior or to refrain from health-damaging behavior because they have a low self-efficacy of being able to care for their own health. In addition, they lack the far-sighted view that the effects of health-related behavior only become apparent in the long term. For the same reason, Sirois [ 9 ] believes that there are no short-term, but only long-term effects of procrastination on health mediated by poor health-related behavior. For example, an unhealthy diet leads to diabetes over time. The findings of studies examining the behavioral pathway are inconclusive [ 3 , 17 , 26 , 28 ]. Furthermore, since most of these studies are cross-sectional, they are not suitable for uncovering long-term effects of trait procrastination on (chronic) disease mediated by poor health-related behavior.
In summary, previous research on the two mediated pathways of the procrastination-health model mainly found support for the role of (chronic) stress in the relationship between trait procrastination and (chronic) disease. However, only short-term effects have been investigated so far. Moreover, longitudinal studies are needed to be able to assess the causal direction of the relationship between trait procrastination, (chronic) stress, and (chronic) disease. Consequently, our study is the first to examine long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, using a longitudinal design. (Chronic) disease could be measured by a variety of different indicators (e.g., physical symptoms, diabetes, or coronary heart disease). We choose depression and anxiety symptoms as indicators for (chronic) disease because they signal mental health complaints before they manifest as (chronic) diseases. Additionally, depression and anxiety symptoms are two of the most common mental health complaints among students [ 29 , 30 ] and procrastination has been shown to be a significant predictor of depression and anxiety symptoms [ 18 , 31 , 32 , 33 , 34 ]. Until now, the stress-related pathway of the procrastination-health model with depression and anxiety symptoms as the health outcome has only been analyzed in one cross-sectional study that confirmed the predictions of the model [ 35 ].
The aim of our study is to evaluate some of the key assumptions of the procrastination-health model, particularly the relationships between trait procrastination, (chronic) stress, and (chronic) disease over time, surveyed in the following analysis using depression and anxiety symptoms.
In line with the key assumptions of the procrastination-health model, we postulate (see Fig. 2 ):
Procrastination leads to perceived stress over time.
Perceived stress leads to depression and anxiety symptoms over time.
Procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress.
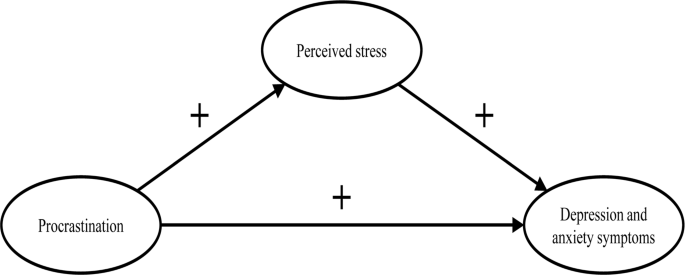
The section of the procrastination-health model we examined
Materials and methods
Our study was part of a health monitoring at a large German university Footnote 1 . Ethical approval for our study was granted by the Ethics Committee of the university’s Department of Education and Psychology. We collected the initial data in 2019. Two occasions followed, each at an interval of six months. In January 2019, we sent out 33,267 invitations to student e-mail addresses. Before beginning the survey, students provided their written informed consent to participate in our study. 3,420 students took part at the first occasion (T1; 10% response rate). Of these, 862 participated at the second (T2) and 392 at the third occasion (T3). In order to test whether dropout was selective, we compared sociodemographic and study specific characteristics (age, gender, academic semester, number of assessments/exams) as well as behavior and health-related variables (procrastination, perceived stress, depression and anxiety symptoms) between the participants of the first wave ( n = 3,420) and those who participated three times ( n = 392). Results from independent-samples t-tests and chi-square analysis showed no significant differences regarding sociodemographic and study specific characteristics (see Additional file 1: Table S1 and S2 ). Regarding behavior and health-related variables, independent-samples t-tests revealed a significant difference in procrastination between the two groups ( t (3,409) = 2.08, p < .05). The mean score of procrastination was lower in the group that participated in all three waves.
The mean age of the longitudinal respondents was 24.1 years ( SD = 5.5 years), the youngest participants were 17 years old, the oldest one was 59 years old. The majority of participants was female (74.0%), 7 participants identified neither as male nor as female (1.8%). The respondents were on average enrolled in the third year of studying ( M = 3.9; SD = 2.3). On average, the students worked about 31.2 h ( SD = 14.1) per week for their studies, and an additional 8.5 h ( SD = 8.5) for their (part-time) jobs. The average income was €851 ( SD = 406), and 4.9% of the students had at least one child. The students were mostly enrolled in philosophy and humanities (16.5%), education and psychology (15.8%), biology, chemistry, and pharmacy (12.5%), political and social sciences (10.6%), veterinary medicine (8.9%), and mathematics and computer science (7.7%).
We only used established and well evaluated instruments for our analyses.
- Procrastination
We adopted the short form of the Procrastination Questionnaire for Students (PFS-4) [ 36 ] to measure procrastination. The PFS-4 assesses procrastination at university as a largely stable behavioral disposition across situations, that is, as a trait. The questionnaire consists of four items (e.g., I put off starting tasks until the last moment.). Each item was rated on a 5-point scale ((almost) never = 1 to (almost) always = 5) for the last two weeks. All items were averaged, with higher scores indicating a greater tendency to procrastinate. The PFS-4 has been proven to be reliable and valid, showing very high correlations with other established trait procrastination scales, for example, with the German short form of the General Procrastination Scale [ 37 , 38 ]. We also proved the scale to be one-dimensional in a factor analysis, with a Cronbach’s alpha of 0.90.
Perceived stress
The Heidelberger Stress Index (HEI-STRESS) [ 39 ] is a three-item measure of current perceived stress due to studying as well as in life in general. For the first item, respondents enter a number between 0 (not stressed at all) and 100 (completely stressed) to indicate how stressed their studies have made them feel over the last four weeks. For the second and third item, respondents rate on a 5-point scale how often they feel “stressed and tense” and as how stressful they would describe their life at the moment. We transformed the second and third item to match the range of the first item before we averaged all items into a single score with higher values indicating greater perceived stress. We proved the scale to be one-dimensional and Cronbach’s alpha for our study was 0.86.
Depression and anxiety symptoms
We used the Patient Health Questionnaire-4 (PHQ-4) [ 40 ], a short form of the Patient Health Questionnaire [ 41 ] with four items, to measure depression and anxiety symptoms. The PHQ-4 contains two items from the Patient Health Questionnaire-2 (PHQ-2) [ 42 ] and the Generalized Anxiety Disorder Scale-2 (GAD-2) [ 43 ], respectively. It is a well-established screening scale designed to assess the core criteria of major depressive disorder (PHQ-2) and generalized anxiety disorder (GAD-2) according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). However, it was shown that the GAD-2 is also appropriate for screening other anxiety disorders. According to Kroenke et al. [ 40 ], the PHQ-4 can be used to assess a person’s symptom burden and impairment. We asked the participants to rate how often they have been bothered over the last two weeks by problems, such as “Little interest or pleasure in doing things”. Response options were 0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day. Calculated as the sum of the four items, the total scores range from 0 to 12 with higher scores indicating more frequent depression and anxiety symptoms. The total scores can be categorized as none-to-minimal (0–2), mild (3–5), moderate (6–8), and severe (9–12) depression and anxiety symptoms. The PHQ-4 was shown to be reliable and valid [ 40 , 44 , 45 ]. We also proved the scale to be one-dimensional in a factor analysis, with a Cronbach’s alpha of 0.86.
Data analysis
To test our hypotheses, we performed structural equation modelling (SEM) using R (Version 4.1.1) with the package lavaan. All items were standardized ( M = 0, SD = 1). Due to the non-normality of some study variables and a sufficiently large sample size of N near to 400 [ 46 ], we used robust maximum likelihood estimation (MLR) for all model estimations. As recommended by Hu and Bentler [ 47 ], we assessed the models’ goodness of fit by chi-square test statistic, root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), Tucker-Lewis index (TLI), and comparative fit index (CFI). A non-significant chi-square indicates good model fit. Since chi-square is sensitive to sample size, we also evaluated fit indices less sensitive to the number of observations. RMSEA and SRMR values of 0.05 or lower as well as TLI and CFI values of 0.97 or higher indicate good model fit. RMSEA values of 0.08 or lower, SRMR values of 0.10 or lower, as well as TLI and CFI values of 0.95 or higher indicate acceptable model fit [ 48 , 49 ]. First, we conducted confirmatory factor analysis for the first occasion, defining three factors that correspond to the measures of procrastination, perceived stress, and depression and anxiety symptoms. Next, we tested for measurements invariance over time and specified the measurement model, before testing our hypotheses.
Measurement invariance over time
To test for measurement invariance over time, we defined one latent variable for each of the three occasions, corresponding to the measures of procrastination, perceived stress, and depression and anxiety symptoms, respectively. As recommended by Geiser and colleagues [ 50 ], the links between indicators and factors (i.e., factor loadings and intercepts) should be equal over measurement occasions; therefore, we added indicator specific factors. A first and least stringent step of testing measurement invariance is configural invariance (M CI ). It was examined whether the included constructs (procrastination, perceived stress, depression and anxiety symptoms) have the same pattern of free and fixed loadings over time. This means that the assignment of the indicators to the three latent factors over time is supported by the underlying data. If configural invariance was supported, restrictions for the next step of testing measurement invariance (metric or weak invariance; M MI ) were added. This means that each item contributes to the latent construct to a similar degree over time. Metric invariance was tested by constraining the factor loadings of the constructs over time. The next step of testing measurement invariance (scalar or strong invariance; M SI ) consisted of checking whether mean differences in the latent construct capture all mean differences in the shared variance of the items. Scalar invariance was tested by constraining the item intercepts over time. The constraints applied in the metric invariance model were retained [ 51 ]. For the last step of testing measurement invariance (residual or strict invariance; M RI ), the residual variables were also set equal over time. If residual invariance is supported, differences in the observed variables can exclusively be attributed to differences in the variances of the latent variables.
We used the Satorra-Bentler chi-square difference test to evaluate the superiority of a more stringent model [ 52 ]. We assumed the model with the largest number of invariance restrictions – which still has an acceptable fit and no substantial deterioration of the chi-square value – to be the final model [ 53 ]. Following previous recommendations, we considered a decrease in CFI of 0.01 and an increase in RMSEA of 0.015 as unacceptable to establish measurement invariance [ 54 ]. If a more stringent model had a significant worse chi-square value, but the model fit was still acceptable and the deterioration in model fit fell within the change criteria recommended for CFI and RMSEA values, we still considered the more stringent model to be superior.
Hypotheses testing
As recommended by Dormann et al. [ 55 ], we applied autoregressive time-lagged panel models to test our hypotheses. In the first step, we specified a model (M 0 ) that only included the stabilities of the three variables (procrastination, perceived stress, depression and anxiety symptoms) over time. In the next step (M 1 ), we added the time-lagged effects from procrastination (T1) to perceived stress (T2) and from procrastination (T2) to perceived stress (T3) as well as from perceived stress (T1) to depression and anxiety symptoms (T2) and from perceived stress (T2) to depression and anxiety symptoms (T3). Additionally, we included a direct path from procrastination (T1) to depression and anxiety symptoms (T3). If this path becomes significant, we can assume a partial mediation [ 55 ]. Otherwise, we can assume a full mediation. We compared these nested models using the Satorra-Bentler chi-square difference test and the Akaike information criterion (AIC). The chi-square difference value should either be non-significant, indicating that the proposed model including our hypotheses (M 1 ) does not have a significant worse model fit than the model including only stabilities (M 0 ), or, if significant, it should be in the direction that M 1 fits the data better than M 0 . Regarding the AIC, M 1 should have a lower value than M 0 .
Table 1 displays the means, standard deviations, internal consistencies (Cronbach’s alpha), and stabilities (correlations) of all study variables. The alpha values of procrastination, perceived stress, and depression and anxiety symptoms are classified as good (> 0.80) [ 56 ]. The correlation matrix of the manifest variables used for the analyses can be found in the Additional file 1: Table S3 .
We observed the highest test-retest reliabilities for procrastination ( r ≥ .74). The test-retest reliabilities for depression and anxiety symptoms ( r ≥ .64) and for perceived stress ( r ≥ .54) were a bit lower (see Table 1 ). The pattern of correlations shows a medium to large but positive relationship between procrastination and depression and anxiety symptoms [ 57 , 58 ]. The association between procrastination and perceived stress was small, the one between perceived stress and depression and anxiety symptoms very large (see Table 1 ).
Confirmatory factor analysis showed an acceptable to good fit (x 2 (41) = 118.618, p < .001; SRMR = 0.042; RMSEA = 0.071; TLI = 0.95; CFI = 0.97). When testing for measurement invariance over time for each construct, the residual invariance models with indicator specific factors provided good fit to the data (M RI ; see Table 2 ), suggesting that differences in the observed variables can exclusively be attributed to differences of the latent variables. We then specified and tested the measurement model of the latent constructs prior to model testing based on the items of procrastination, perceived stress, and depression and anxiety symptoms. The measurement model fitted the data well (M M ; see Table 3 ). All items loaded solidly on their respective factors (0.791 ≤ β ≤ 0.987; p < .001).
To test our hypotheses, we analyzed the two models described in the methods section.
The fit of the stability model (M 0 ) was acceptable (see Table 3 ). Procrastination was stable over time, with stabilities above 0.82. The stabilities of perceived stress as well as depression and anxiety symptoms were somewhat lower, ranging from 0.559 (T1 -> T2) to 0.696 (T2 -> T3) for perceived stress and from 0.713 (T2 -> T3) to 0.770 (T1 -> T2) for depression and anxiety symptoms, respectively.
The autoregressive mediation model (M 1 ) fitted the data significantly better than M 0 . The direct path from procrastination (T1) to depression and anxiety symptoms (T3) was significant (β = 0.16; p < .001), however, none of the mediated paths (from procrastination (T1) to perceived stress (T2) and from perceived stress (T2) to depression and anxiety symptoms (T3)) proved to be substantial. Also, the time-lagged paths from perceived stress (T1) to depression and anxiety symptoms (T2) and from procrastination (T2) to perceived stress (T3) were not substantial either (see Fig. 3 ).
To examine whether the hypothesized effects would occur over a one-year period rather than a six-months period, we specified an additional model with paths from procrastination (T1) to perceived stress (T3) and from perceived stress (T1) to depression and anxiety symptoms (T3), also including the stabilities of the three constructs as in the stability model M 0 . The model showed an acceptable fit (χ 2 (486) = 831.281, p < .001; RMSEA = 0.048; SRMR = 0.091; TLI = 0.95; CFI = 0.95), but neither of the two paths were significant.
Therefore, our hypotheses, that procrastination leads to perceived stress over time (H1) and that perceived stress leads to depression and anxiety symptoms over time (H2) must be rejected. We could only partially confirm our third hypothesis, that procrastination leads to depression and anxiety over time, mediated by perceived stress (H3), since procrastination did lead to depression and anxiety symptoms over time. However, this effect was not mediated by perceived stress.
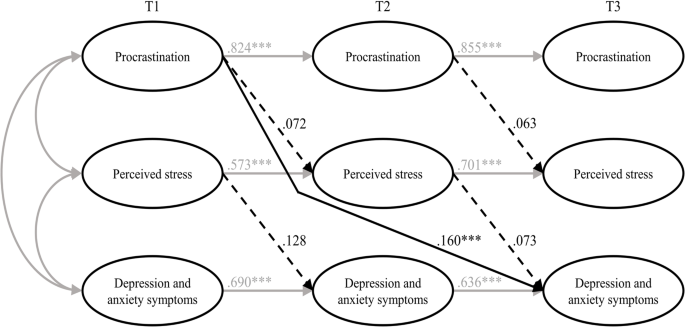
Results of the estimated model including all hypotheses (M 1 ). Note Non-significant paths are dotted. T1 = time 1; T2 = time 2; T3 = time 3. *** p < .001
To sum up, we tried to examine the harmful consequences of procrastination on students’ stress and mental health. Hence, we selected the procrastination-health model by Sirois [ 9 ] as a theoretical foundation and tried to evaluate some of its key assumptions in a temporal perspective. The author assumes that trait procrastination leads to (chronic) disease via (chronic) stress. We chose depression and anxiety symptoms as indicators for (chronic) disease and postulated, in line with the key assumptions of the procrastination-health model, that procrastination leads to perceived stress over time (H1), that perceived stress leads to depression and anxiety symptoms over time (H2), and that procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress (H3). To examine these relationships properly, we collected longitudinal data from students at three occasions over a one-year period and analyzed the data using autoregressive time-lagged panel models. Our first and second hypotheses had to be rejected: Procrastination did not lead to perceived stress over time, and perceived stress did not lead to depression and anxiety symptoms over time. However, procrastination did lead to depression and anxiety symptoms over time – which is in line with our third hypothesis – but perceived stress was not a mediator of this effect. Therefore, we could only partially confirm our third hypothesis.
Our results contradict previous studies on the stress-related pathway of the procrastination-health model, which consistently found support for the role of (chronic) stress in the relationship between trait procrastination and (chronic) disease. Since most of these studies were cross-sectional, though, the causal direction of these effects remained uncertain. There are two longitudinal studies that confirm the stress-related pathway of the procrastination-health model [ 27 , 28 ], but both studies examined short-term effects (≤ 3 months), whereas we focused on more long-term effects. Therefore, the divergent findings may indicate that there are short-term, but no long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress.
Our results especially raise the question whether trait procrastination leads to (chronic) stress in the long term. Looking at previous longitudinal studies on the effect of procrastination on stress, the following stands out: At shorter study periods of two weeks [ 27 ] and four weeks [ 28 ], the effect of procrastination on stress appears to be present. At longer study periods of seven weeks [ 59 ], three months [ 28 ], six months, and twelve months, as in our study, the effect of procrastination on stress does not appear to be present. There is one longitudinal study in which procrastination was a significant predictor of stress symptoms nine months later [ 34 ]. The results of this study should be interpreted with caution, though, because the outbreak of the COVID-19 pandemic fell within the study period, which could have contributed to increased stress symptoms [ 60 ]. Unfortunately, Johansson et al. [ 34 ] did not report whether average stress symptoms increased during their study. In one of the two studies conducted by Fincham and May [ 59 ], the COVID-19 pandemic outbreak also fell within their seven-week study period. However, they reported that in their study, average stress symptoms did not increase from baseline to follow-up. Taken together, the findings suggest that procrastination can cause acute stress in the short term, for example during times when many tasks need to be completed, such as at the end of a semester, but that procrastination does not lead to chronic stress over time. It seems possible that students are able to recover during the semester from the stress their procrastination caused at the end of the previous semester. Because of their procrastination, they may also have more time to engage in relaxing activities, which could further mitigate the effect of procrastination on stress. Our conclusions are supported by an early and well-known longitudinal study by Tice and Baumeister [ 61 ], which compared procrastinating and non-procrastinating students with regard to their health. They found that procrastinators experienced less stress than their non-procrastinating peers at the beginning of the semester, but more at the end of the semester. Additionally, our conclusions are in line with an interview study in which university students were asked about the consequences of their procrastination [ 62 ]. The students reported that, due to their procrastination, they experience high levels of stress during periods with heavy workloads (e.g., before deadlines or exams). However, the stress does not last, instead, it is relieved immediately after these periods.
Even though research indicates, in line with the assumptions of the procrastination-health model, that stress is a risk factor for physical and mental disorders [ 63 , 64 , 65 , 66 ], perceived stress did not have a significant effect on depression and anxiety symptoms in our study. The relationship between stress and mental health is complex, as people respond to stress in many different ways. While some develop stress-related mental disorders, others experience mild psychological symptoms or no symptoms at all [ 67 ]. This can be explained with the help of vulnerability-stress models. According to vulnerability-stress models, mental illnesses emerge from an interaction of vulnerabilities (e.g., genetic factors, difficult family backgrounds, or weak coping abilities) and stress (e.g., minor or major life events or daily hassles) [ 68 , 69 ]. The stress perceived by the students in our sample may not be sufficient enough on its own, without the presence of other risk factors, to cause depression and anxiety symptoms. However, since we did not assess individual vulnerability and stress factors in our study, these considerations are mere speculation.
In our study, procrastination led to depression and anxiety symptoms over time, which is consistent with the procrastination-health model as well as previous cross-sectional and longitudinal evidence [ 18 , 21 , 31 , 32 , 33 , 34 ]. However, it is still unclear by which mechanisms this effect is mediated, as perceived stress did not prove to be a substantial mediator in our study. One possible mechanism would be that procrastination impairs affective well-being [ 70 ] and creates negative feelings, such as shame, guilt, regret, and anger [ 20 , 21 , 22 , 62 , 71 ], which in turn could lead to depression and anxiety symptoms [ 23 , 24 , 25 ]. Other potential mediators of the relationship between procrastination and depression and anxiety symptoms emerge from the behavioral pathway of the procrastination-health model, suggesting that poor health-related behaviors mediate the effect of trait procrastination on (chronic) disease. Although evidence for this is still scarce, the results of one cross-sectional study, for example, indicate that poor sleep quality might mediate the effect of procrastination on depression and anxiety symptoms [ 35 ].
In summary, we found that procrastination leads to depression and anxiety symptoms over time and that perceived stress is not a mediator of this effect. We could not show that procrastination leads to perceived stress over time, nor that perceived stress leads to depression and anxiety symptoms over time. For the most part, the relationships between procrastination, perceived stress, and depression and anxiety symptoms did not match the relationships between trait procrastination, (chronic) stress, and (chronic) disease as assumed in the procrastination-health model. Explanations for this could be that procrastination might only lead to perceived stress in the short term, for example, during preparations for end-of-semester exams, and that perceived stress may not be sufficient enough on its own, without the presence of other risk factors, to cause depression and anxiety symptoms. In conclusion, we could not confirm long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, as assumed for the stress-related pathway of the procrastination-health model.
Limitations and suggestions for future research
In our study, we tried to draw causal conclusions about the harmful consequences of procrastination on students’ stress and mental health. However, since procrastination is a trait that cannot be manipulated experimentally, we have conducted an observational rather than an experimental study, which makes causal inferences more difficult. Nonetheless, a major strength of our study is that we used a longitudinal design with three waves. This made it possible to draw conclusions about the causal direction of the effects, as in hardly any other study targeting consequences of procrastination on health before [ 4 , 28 , 55 ]. Therefore, we strongly recommend using a similar longitudinal design in future studies on the procrastination-health model or on consequences of procrastination on health in general.
We chose a time lag of six months between each of the three measurement occasions to examine long-term effects of procrastination on depression and anxiety symptoms mediated by perceived stress. However, more than six months may be necessary for the hypothesized effects to occur [ 72 ]. The fact that the temporal stabilities of the examined constructs were moderate or high (0.559 ≤ β ≤ 0.854) [ 73 , 74 ] also suggests that the time lags may have been too short. The larger the time lag, the lower the temporal stabilities, as shown for depression and anxiety symptoms, for example [ 75 ]. High temporal stabilities make it more difficult to detect an effect that actually exists [ 76 ]. Nonetheless, Dormann and Griffin [ 77 ] recommend using shorter time lags of less than one year, even with high stabilities, because of other influential factors, such as unmeasured third variables. Therefore, our time lags of six months seem appropriate.
It should be discussed, though, whether it is possible to detect long-term effects of the stress-related pathway of the procrastination-health model within a total study period of one year. Sirois [ 9 ] distinguishes between short-term and long-term effects of procrastination on health mediated by stress, but does not address how long it might take for long-term effects to occur or when effects can be considered long-term instead of short-term. The fact that an effect of procrastination on stress is evident at shorter study periods of four weeks or less but in most cases not at longer study periods of seven weeks or more, as we mentioned earlier, could indicate that short-term effects occur within the time frame of one to three months, considering the entire stress-related pathway. Hence, it seems appropriate to assume that we have examined rather long-term effects, given our study period of six and twelve months. Nevertheless, it would be beneficial to use varying study periods in future studies, in order to be able to determine when effects can be considered long-term.
Concerning long-term effects of the stress-related pathway, Sirois [ 9 ] assumes that chronic procrastination causes chronic stress, which leads to chronic diseases over time. The term “chronic stress” refers to prolonged stress episodes associated with permanent tension. The instrument we used captures perceived stress over the last four weeks. Even though the perceived stress of the students in our sample was relatively stable (0.559 ≤ β ≤ 0.696), we do not know how much fluctuation occurred between each of the three occasions. However, there is some evidence suggesting that perceived stress is strongly associated with chronic stress [ 78 ]. Thus, it seems acceptable that we used perceived stress as an indicator for chronic stress in our study. For future studies, we still suggest the use of an instrument that can more accurately reflect chronic stress, for example, the Trier Inventory for Chronic Stress (TICS) [ 79 ].
It is also possible that the occasions were inconveniently chosen, as they all took place in a critical academic period near the end of the semester, just before the examination period began. We chose a similar period in the semester for each occasion for the sake of comparability. However, it is possible that, during this preparation periods, stress levels peaked and procrastinators procrastinated less because they had to catch up after delaying their work. This could have introduced bias to the data. Therefore, in future studies, investigation periods should be chosen that are closer to the beginning or in the middle of a semester.
Furthermore, Sirois [ 9 ] did not really explain her understanding of “chronic disease”. However, it seems clear that physical illnesses, such as diabetes or cardiovascular diseases, are meant. Depression and anxiety symptoms, which we chose as indicators for chronic disease, represent mental health complaints that do not have to be at the level of a major depressive disorder or an anxiety disorder, in terms of their quantity, intensity, or duration [ 40 ]. But they can be viewed as precursors to a major depressive disorder or an anxiety disorder. Therefore, given our study period of one year, it seems appropriate to use depression and anxiety symptoms as indicators for chronic disease. At longer study periods, we would expect these mental health complaints to manifest as mental disorders. Moreover, the procrastination-health model was originally designed to be applied to physical diseases [ 3 ]. Perhaps, the model assumptions are more applicable to physical diseases than to mental disorders. By applying parts of the model to mental health complaints, we have taken an important step towards finding out whether the model is applicable to mental disorders as well. Future studies should examine additional long-term health outcomes, both physical and psychological. This would help to determine whether trait procrastination has varying effects on different diseases over time. Furthermore, we suggest including individual vulnerability and stress factors in future studies in order to be able to analyze the effect of (chronic) stress on (chronic) diseases in a more differentiated way.
Regarding our sample, 3,420 students took part at the first occasion, but only 392 participated three times, which results in a dropout rate of 88.5%. At the second and third occasion, invitation e-mails were only sent to participants who had indicated at the previous occasion that they would be willing to participate in a repeat survey and provided their e-mail address. This is probably one of the main reasons for our high dropout rate. Other reasons could be that the students did not receive any incentives for participating in our study and that some may have graduated between the occasions. Selective dropout analysis revealed that the mean score of procrastination was lower in the group that participated in all three waves ( n = 392) compared to the group that participated in the first wave ( n = 3,420). One reason for this could be that those who have a higher tendency to procrastinate were more likely to procrastinate on filling out our survey at the second and third occasion. The findings of our dropout analysis should be kept in mind when interpreting our results, as lower levels of procrastination may have eliminated an effect on perceived stress or on depression and anxiety symptoms. Additionally, across all age groups in population-representative samples, the student age group reports having the best subjective health [ 80 ]. Therefore, it is possible that they are more resilient to stress and experience less impairment of well-being than other age groups. Hence, we recommend that future studies focus on other age groups as well.
It is generally assumed that procrastination leads to lower academic performance, health impairment, and poor health-related behavior. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. In consequence, the aim of our study was to examine the effect of procrastination on mental health over time and stress as a possible facilitator of this relationship. We selected the procrastination-health model as a theoretical foundation and used the stress-related pathway of the model, assuming that trait procrastination leads to (chronic) disease via (chronic) stress. We chose depression and anxiety symptoms as indicators for (chronic) disease and collected longitudinal data from students at three occasions over a one-year period. This allowed us to draw conclusions about the causal direction of the effects, as in hardly any other study examining consequences of procrastination on (mental) health before. Our results indicate that procrastination leads to depression and anxiety symptoms over time and that perceived stress is not a mediator of this effect. We could not show that procrastination leads to perceived stress over time, nor that perceived stress leads to depression and anxiety symptoms over time. Explanations for this could be that procrastination might only lead to perceived stress in the short term, for example, during preparations for end-of-semester exams, and that perceived stress may not be sufficient on its own, that is, without the presence of other risk factors, to cause depression and anxiety symptoms. Overall, we could not confirm long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, as assumed for the stress-related pathway of the procrastination-health model. Our study emphasizes the importance of identifying the consequences procrastination can have on health and well-being and determining by which mechanisms they are mediated. Only then will it be possible to develop interventions that can prevent negative health consequences of procrastination. Further health outcomes and possible mediators should be explored in future studies, using a similar longitudinal design.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
University Health Report at Freie Universität Berlin.
Abbreviations
Comparative fit index
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
Generalized Anxiety Disorder Scale-2
Heidelberger Stress Index
Hypothalamic-pituitary-adrenocortical
Robust maximum likelihood estimation
Short form of the Procrastination Questionnaire for Students
Patient Health Questionnaire-2
Patient Health Questionnaire-4
Root mean square error of approximation
Structural equation modeling
Standardized root mean square residual
Tucker-Lewis index
Lu D, He Y, Tan Y, Gender S, Status. Cultural differences, Education, family size and procrastination: a sociodemographic Meta-analysis. Front Psychol. 2021. https://doi.org/10.3389/fpsyg.2021.719425 .
Article PubMed PubMed Central Google Scholar
Yan B, Zhang X. What research has been conducted on Procrastination? Evidence from a systematical bibliometric analysis. Front Psychol. 2022. https://doi.org/10.3389/fpsyg.2022.809044 .
Sirois FM, Melia-Gordon ML, Pychyl TA. I’ll look after my health, later: an investigation of procrastination and health. Pers Individ Dif. 2003;35:1167–84. https://doi.org/10.1016/S0191-8869(02)00326-4 .
Article Google Scholar
Grunschel C. Akademische Prokrastination: Eine qualitative und quantitative Untersuchung von Gründen und Konsequenzen [Unpublished doctoral dissertation]: Universität Bielefeld; 2013.
Steel P. The Nature of Procrastination: a Meta-Analytic and Theoretical Review of Quintessential Self-Regulatory failure. Psychol Bull. 2007;133:65–94. https://doi.org/10.1037/0033-2909.133.1.65 .
Article PubMed Google Scholar
Corkin DM, Yu SL, Lindt SF. Comparing active delay and procrastination from a self-regulated learning perspective. Learn Individ Differ. 2011;21:602–6. https://doi.org/10.1016/j.lindif.2011.07.005 .
Balkis M, Duru E. Procrastination, self-regulation failure, academic life satisfaction, and affective well-being: underregulation or misregulation form. Eur J Psychol Educ. 2016;31:439–59. https://doi.org/10.1007/s10212-015-0266-5 .
Schulz N. Procrastination und Planung – Eine Untersuchung zum Einfluss von Aufschiebeverhalten und Depressivität auf unterschiedliche Planungskompetenzen [Doctoral dissertation]: Westfälische Wilhelms-Universität Münster; 2007.
Sirois FM. Procrastination, stress, and Chronic Health conditions: a temporal perspective. In: Sirois FM, Pychyl TA, editors. Procrastination, Health, and well-being. London: Academic; 2016. pp. 67–92. https://doi.org/10.1016/B978-0-12-802862-9.00004-9 .
Harriott J, Ferrari JR. Prevalence of procrastination among samples of adults. Psychol Rep. 1996;78:611–6. https://doi.org/10.2466/pr0.1996.78.2.611 .
Ferrari JR, O’Callaghan J, Newbegin I. Prevalence of Procrastination in the United States, United Kingdom, and Australia: Arousal and Avoidance delays among adults. N Am J Psychol. 2005;7:1–6.
Google Scholar
Ferrari JR, Díaz-Morales JF, O’Callaghan J, Díaz K, Argumedo D. Frequent behavioral Delay tendencies by adults. J Cross Cult Psychol. 2007;38:458–64. https://doi.org/10.1177/0022022107302314 .
Day V, Mensink D, O’Sullivan M. Patterns of academic procrastination. JCRL. 2000;30:120–34. https://doi.org/10.1080/10790195.2000.10850090 .
Höcker A, Engberding M, Rist F, Prokrastination. Ein Manual Zur Behandlung Des Pathologischen Aufschiebens. 2nd ed. Göttingen: Hogrefe; 2017.
Kim KR, Seo EH. The relationship between procrastination and academic performance: a meta-analysis. Pers Individ Dif. 2015;82:26–33. https://doi.org/10.1016/j.paid.2015.02.038 .
Khalid A, Zhang Q, Wang W, Ghaffari AS, Pan F. The relationship between procrastination, perceived stress, saliva alpha-amylase level and parenting styles in Chinese first year medical students. Psychol Res Behav Manag. 2019;12:489–98. https://doi.org/10.2147/PRBM.S207430 .
Sirois FM. I’ll look after my health, later: a replication and extension of the procrastination–health model with community-dwelling adults. Pers Individ Dif. 2007;43:15–26. https://doi.org/10.1016/j.paid.2006.11.003 .
Reinecke L, Meier A, Aufenanger S, Beutel ME, Dreier M, Quiring O, et al. Permanently online and permanently procrastinating? The mediating role of internet use for the effects of trait procrastination on psychological health and well-being. New Media Soc. 2018;20:862–80. https://doi.org/10.1177/1461444816675437 .
Westgate EC, Wormington SV, Oleson KC, Lindgren KP. Productive procrastination: academic procrastination style predicts academic and alcohol outcomes. J Appl Soc Psychol. 2017;47:124–35. https://doi.org/10.1111/jasp.12417 .
Feyzi Behnagh R, Ferrari JR. Exploring 40 years on affective correlates to procrastination: a literature review of situational and dispositional types. Curr Psychol. 2022;41:1097–111. https://doi.org/10.1007/s12144-021-02653-z .
Rahimi S, Hall NC, Sticca F. Understanding academic procrastination: a longitudinal analysis of procrastination and emotions in undergraduate and graduate students. Motiv Emot. 2023. https://doi.org/10.1007/s11031-023-10010-9 .
Patrzek J, Grunschel C, Fries S. Academic procrastination: the perspective of University counsellors. Int J Adv Counselling. 2012;34:185–201. https://doi.org/10.1007/s10447-012-9150-z .
Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. J Abnorm Psychol. 1988;97:346–53. https://doi.org/10.1037//0021-843x.97.3.346 .
Cândea D-M, Szentagotai-Tătar A. Shame-proneness, guilt-proneness and anxiety symptoms: a meta-analysis. J Anxiety Disord. 2018;58:78–106. https://doi.org/10.1016/j.janxdis.2018.07.005 .
Young CM, Neighbors C, DiBello AM, Traylor ZK, Tomkins M. Shame and guilt-proneness as mediators of associations between General Causality orientations and depressive symptoms. J Soc Clin Psychol. 2016;35:357–70. https://doi.org/10.1521/jscp.2016.35.5.357 .
Stead R, Shanahan MJ, Neufeld RW. I’ll go to therapy, eventually: Procrastination, stress and mental health. Pers Individ Dif. 2010;49:175–80. https://doi.org/10.1016/j.paid.2010.03.028 .
Dow NM. Procrastination, stress, and sleep in tertiary students [Master’s thesis]: University of Canterbury; 2018.
Sirois FM, Stride CB, Pychyl TA. Procrastination and health: a longitudinal test of the roles of stress and health behaviours. Br J Health Psychol. 2023. https://doi.org/10.1111/bjhp.12658 .
Hofmann F-H, Sperth M, Holm-Hadulla RM. Psychische Belastungen Und Probleme Studierender. Psychotherapeut. 2017;62:395–402. https://doi.org/10.1007/s00278-017-0224-6 .
Liu CH, Stevens C, Wong SHM, Yasui M, Chen JA. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: implications for addressing disparities in service use. Depress Anxiety. 2019;36:8–17. https://doi.org/10.1002/da.22830 .
Aftab S, Klibert J, Holtzman N, Qadeer K, Aftab S. Schemas mediate the Link between Procrastination and Depression: results from the United States and Pakistan. J Rat-Emo Cognitive-Behav Ther. 2017;35:329–45. https://doi.org/10.1007/s10942-017-0263-5 .
Flett AL, Haghbin M, Pychyl TA. Procrastination and depression from a cognitive perspective: an exploration of the associations among Procrastinatory Automatic thoughts, rumination, and Mindfulness. J Rat-Emo Cognitive-Behav Ther. 2016;34:169–86. https://doi.org/10.1007/s10942-016-0235-1 .
Saddler CD, Sacks LA. Multidimensional perfectionism and academic procrastination: relationships with Depression in University students. Psychol Rep. 1993;73:863–71. https://doi.org/10.1177/00332941930733pt123 .
Johansson F, Rozental A, Edlund K, Côté P, Sundberg T, Onell C, et al. Associations between procrastination and subsequent Health outcomes among University students in Sweden. JAMA Netw Open. 2023. https://doi.org/10.1001/jamanetworkopen.2022.49346 .
Gusy B, Jochmann A, Lesener T, Wolter C, Blaszcyk W. „Get it done – schadet Aufschieben Der Gesundheit? Präv Gesundheitsf. 2023;18:228–33. https://doi.org/10.1007/s11553-022-00950-4 .
Glöckner-Rist A, Engberding M, Höcker A, Rist F. Prokrastinationsfragebogen für Studierende (PFS): Zusammenstellung sozialwissenschaftlicher items und Skalen. ZIS - GESIS Leibniz Institute for the Social Sciences; 2014.
Klingsieck KB, Fries S. Allgemeine Prokrastination: Entwicklung Und Validierung Einer Deutschsprachigen Kurzskala Der General Procrastination Scale (Lay, 1986). Diagnostica. 2012;58:182–93. https://doi.org/10.1026/0012-1924/a000060 .
Lay CH. At last, my research article on procrastination. J Res Pers. 1986;20:474–95. https://doi.org/10.1016/0092-6566(86)90127-3 .
Schmidt LI, Obergfell J. Zwangsjacke Bachelor?! Stressempfinden Und Gesundheit Studierender: Der Einfluss Von Anforderungen Und Entscheidungsfreiräumen Bei Bachelor- Und Diplomstudierenden Nach Karaseks Demand-Control-Modell. Saarbrücken: VDM Verlag Dr. Müller; 2011.
Kroenke K, Spitzer RL, Williams JB, Löwe B. An Ultra-brief Screening Scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–21. https://doi.org/10.1016/S0033-3182(09)70864-3 .
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA. 1999;282:1737–44. https://doi.org/10.1001/jama.282.18.1737 .
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item Depression Screener. Med Care. 2003;41:1284–92.
Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in Primary Care: prevalence, impairment, Comorbidity, and detection. Ann Intern Med. 2007;146:317–25. https://doi.org/10.7326/0003-4819-146-5-200703060-00004 .
Khubchandani J, Brey R, Kotecki J, Kleinfelder J, Anderson J. The Psychometric properties of PHQ-4 depression and anxiety screening scale among College Students. Arch Psychiatr Nurs. 2016;30:457–62. https://doi.org/10.1016/j.apnu.2016.01.014 .
Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disorders. 2010;122:86–95. https://doi.org/10.1016/j.jad.2009.06.019 .
Boomsma A, Hoogland JJ. The robustness of LISREL modeling revisited. In: Cudeck R, Du Toit S, Sörbom D, editors. Structural equation modeling: Present and Future: a festschrift in honor of Karl Jöreskog. Lincolnwood: Scientific Software International; 2001. pp. 139–68.
Hu L, Bentler PM. Fit indices in Covariance structure modeling: sensitivity to Underparameterized Model Misspecification. Psychol Methods. 1998;3:424–53. https://doi.org/10.1037/1082-989X.3.4.424 .
Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: test of significance and descriptive goodness-of-fit measures. MPR. 2003;8:23–74.
Hu L, Bentler PM. Cutoff criteria for fit indexes in Covariance structure analysis: conventional criteria Versus New Alternatives. Struct Equ Model. 1999;6:1–55. https://doi.org/10.1080/10705519909540118 .
Geiser C, Eid M, Nussbeck FW, Courvoisier DS, Cole DA. Analyzing true change in Longitudinal Multitrait-Multimethod studies: application of a Multimethod Change Model to Depression and anxiety in children. Dev Psychol. 2010;46:29–45. https://doi.org/10.1037/a0017888 .
Putnick DL, Bornstein MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. 2016;41:71–90. https://doi.org/10.1016/j.dr.2016.06.004 .
Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–14. https://doi.org/10.1007/BF02296192 .
Geiser C. Datenanalyse Mit Mplus: Eine Anwendungsorientierte Einführung. Wiesbaden: VS Verlag für Sozialwissenschaften; 2010.
Book Google Scholar
Chen F, Curran PJ, Bollen KA, Kirby J, Paxton P. An empirical evaluation of the use of fixed cutoff points in RMSEA Test Statistic in Structural equation models. Sociol Methods Res. 2008;36:462–94. https://doi.org/10.1177/0049124108314720 .
Dormann C, Zapf D, Perels F. Quer- und Längsschnittstudien in der Arbeitspsychologie [Cross-sectional and longitudinal studies in occupational psychology.]. In: Kleinbeck U, Schmidt K-H,Enzyklopädie der Psychologie [Encyclopedia of psychology]:, Themenbereich D, Serie III, Band 1, Arbeitspsychologie [Subject Area, Series D. III, Volume 1, Industrial Psychology]. Göttingen: Hogrefe Verlag; 2010. pp. 923–1001.
Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994.
Gignac GE, Szodorai ET. Effect size guidelines for individual differences researchers. Pers Indiv Differ. 2016;102:74–8. https://doi.org/10.1016/j.paid.2016.06.069 .
Funder DC, Ozer DJ. Evaluating effect size in Psychological Research: sense and nonsense. Adv Methods Practices Psychol Sci. 2019;2:156–68. https://doi.org/10.1177/2515245919847202 .
Fincham FD, May RW. My stress led me to procrastinate: temporal relations between perceived stress and academic procrastination. Coll Stud J. 2021;55:413–21.
Daniali H, Martinussen M, Flaten MA. A Global Meta-Analysis of Depression, anxiety, and stress before and during COVID-19. Health Psychol. 2023;42:124–38. https://doi.org/10.1037/hea0001259 .
Tice DM, Baumeister RF. Longitudinal study of procrastination, performance, stress, and Health: the costs and benefits of Dawdling. Psychol Sci. 1997;8:454–8. https://doi.org/10.1111/j.1467-9280.1997.tb00460.x .
Schraw G, Wadkins T, Olafson L. Doing the things we do: a grounded theory of academic procrastination. J Educ Psychol. 2007;99:12–25. https://doi.org/10.1037/0022-0663.99.1.12 .
Slavich GM. Life Stress and Health: a review of conceptual issues and recent findings. Teach Psychol. 2016;43:346–55. https://doi.org/10.1177/0098628316662768 .
Phillips AC, Carroll D, Der G. Negative life events and symptoms of depression and anxiety: stress causation and/or stress generation. Anxiety Stress Coping. 2015;28:357–71. https://doi.org/10.1080/10615806.2015.1005078 .
Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. https://doi.org/10.1146/annurev.clinpsy.1.102803.143938 .
Blazer D, Hughes D, George LK. Stressful life events and the onset of a generalized anxiety syndrome. Am J Psychiatry. 1987;144:1178–83. https://doi.org/10.1176/ajp.144.9.1178 .
Southwick SM, Charney DS. The Science of Resilience: implications for the Prevention and Treatment of Depression. Science. 2012;338:79–82. https://doi.org/10.1126/science.1222942 .
Ingram RE, Luxton DD. Vulnerability-stress models. In: Hankin BL, Abela JR, editors. Development of psychopathology: a vulnerability-stress perspective. Thousand Oaks: Sage; 2005. pp. 32–46.
Chapter Google Scholar
Maercker A. Modelle Der Klinischen Psychologie. In: Petermann F, Maercker A, Lutz W, Stangier U, editors. Klinische psychologie – Grundlagen. Göttingen: Hogrefe; 2018. pp. 13–31.
Krause K, Freund AM. Delay or procrastination – a comparison of self-report and behavioral measures of procrastination and their impact on affective well-being. Pers Individ Dif. 2014;63:75–80. https://doi.org/10.1016/j.paid.2014.01.050 .
Grunschel C, Patrzek J, Fries S. Exploring reasons and consequences of academic procrastination: an interview study. Eur J Psychol Educ. 2013;28:841–61. https://doi.org/10.1007/s10212-012-0143-4 .
Dwyer JH. Statistical models for the social and behavioral sciences. New York: Oxford University Press; 1983.
Cohen JA, Power Primer. Psychol Bull. 1992;112:155–9. https://doi.org/10.1037//0033-2909.112.1.155 .
Ferguson CJ. An effect size primer: a Guide for clinicians and Researchers. Prof Psychol Res Pr. 2009;40:532–8. https://doi.org/10.1037/a0015808 .
Hinz A, Berth H, Kittel J, Singer S. Die zeitliche Stabilität (Test-Retest-Reliabilität) Von Angst Und Depressivität Bei Patienten Und in Der Allgemeinbevölkerung. Z Med Psychol. 2011;20:24–31. https://doi.org/10.3233/ZMP-2010-2012 .
Adachi P, Willoughby T. Interpreting effect sizes when controlling for stability effects in longitudinal autoregressive models: implications for psychological science. Eur J Dev Psychol. 2015;12:116–28. https://doi.org/10.1080/17405629.2014.963549 .
Dormann C, Griffin M. Optimal time lags in Panel studies. Psychol Methods. 2015;20:489–505. https://doi.org/10.1037/met0000041 .
Weckesser LJ, Dietz F, Schmidt K, Grass J, Kirschbaum C, Miller R. The psychometric properties and temporal dynamics of subjective stress, retrospectively assessed by different informants and questionnaires, and hair cortisol concentrations. Sci Rep. 2019. https://doi.org/10.1038/s41598-018-37526-2 .
Schulz P, Schlotz W, Becker P. TICS: Trierer Inventar Zum chronischen stress. Göttingen: Hogrefe; 2004.
Heidemann C, Scheidt-Nave C, Beyer A-K, Baumert J, Thamm R, Maier B, et al. Health situation of adults in Germany - results for selected indicators from GEDA 2019/2020-EHIS. J Health Monit. 2021;6:3–25. https://doi.org/10.25646/8459 .
Download references
Acknowledgements
Not applicable.
Open Access Funding provided by Freie Universität Berlin.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Division of Prevention and Psychosocial Health Research, Department of Education and Psychology, Freie Universität Berlin, Habelschwerdter Allee 45, 14195, Berlin, Germany
Anna Jochmann, Burkhard Gusy, Tino Lesener & Christine Wolter
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: A.J., B.G., T.L.; methodology: B.G., A.J.; validation: B.G.; formal analysis: A.J., B.G.; investigation: C.W., T.L., B.G.; data curation: C.W., T.L., B.G.; writing–original draft preparation: A.J., B.G.; writing–review and editing: A.J., T.L., B.G., C.W.; visualization: A.J., B.G.; supervision: B.G., T.L.; project administration: C.W., T.L., B.G.; All authors contributed to the article and approved the submitted version.
Corresponding authors
Correspondence to Anna Jochmann or Burkhard Gusy .
Ethics declarations
Ethics approval and consent to participate.
This study was performed in line with the principles of the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the Department of Education and Psychology, Freie Universität Berlin. All methods were carried out in accordance with relevant guidelines and regulations. The participants provided their written informed consent to participate in this study.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Selective dropout analysis and correlation matrix of the manifest variables
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jochmann, A., Gusy, B., Lesener, T. et al. Procrastination, depression and anxiety symptoms in university students: a three-wave longitudinal study on the mediating role of perceived stress. BMC Psychol 12 , 276 (2024). https://doi.org/10.1186/s40359-024-01761-2
Download citation
Received : 25 May 2023
Accepted : 02 May 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s40359-024-01761-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Student health
- Longitudinal study
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Depression rates among US adults reach new high: Gallup
Nearly 30% of adults say they've been diagnosed with depression at some point.
Depression rates in the United States are skyrocketing, particularly among young adults and women, a new poll shows.
The survey , published by Gallup on Wednesday, found 29% of U.S. adults report being diagnosed with depression at some point during their lifetimes, an increase from 19.6% in 2015.
Meanwhile, 17.8% of those aged 18 and older either currently have or are currently being treated for depression, up from 10.5% in 2015.
According to Gallup, both rates are the highest ever recorded by the analytics company since it began tracking depression rates.
MORE: Teen girls are experiencing record-high levels of sadness and violence: CDC
"I think the results are startling," Dan Witters, research director of the Gallup National Health and Well-Being, told ABC News. "The disproportionate manner in which some groups have been affected by this makes sense to me based upon what we know about other research and those sharp increases in those depression rates among those adults under 30, women too, Blacks and Hispanics, they are really eye-popping."
Although the COVID-19 pandemic can't be blamed completely for the increasing rates, it definitely was a major factor, Witters said.
"Both of these rates had kind of been coming up over the years pre-pandemic," he said. "And you don't want to get too far out in front of your skis as far as putting all the blame on the pandemic."
He went on, "There's plenty of other big factors out there that could be relevant to these increasing rates that we've been measuring but the pandemic's a big one and indeed the rates have really come up significantly in the years since COVID hit."

More than 5,100 adults were surveyed in all 50 states and the District of Columbia during the last week of February 2023. The results are part of the larger ongoing Gallup National Health and Well-Being Index, which seeks to track and understand factors that drive well-being.
Results showed rates are rising fastest among certain groups, particularly young adults and women.
Women's rates of depression during their lifetimes climbed from 26.2% in 2017 to 36.7% in 2023. Rates of those with current depression increased from 17.6% to 23.8% over the same period.
By comparison, men with depression during their lifetimes saw a smaller increase from 17.7% in 2017 to 20.4% in 2023. Current rates for depression rose from 9.3% to 11.3%.
Witters said women have historically had higher rates of depression than men. COVID, however, may have led to a jump in these rates due to women being disproportionately forced to leave the workforce to take care of children at home and that fact that they make up a higher percentage of frontline health care workers.
MORE: Suicides rose in 2021 after 2 years of declines, CDC report finds
Breakdowns by age showed one-third of younger adults between ages 18 to 29 reported being diagnosed with depression at some point in their lives, up from 20.4% in 2017. Additionally, 24.6% said they currently have depression, an increase from 13% in 2017.
Trending Reader Picks

PGA winner Grayson Murray died by suicide: Family
- May 26, 11:51 AM

Lawmaker's daughter, son-in-law killed in Haiti
- May 24, 1:18 PM

Johnson disappointed with chaotic House meeting
- May 17, 3:34 PM
Witters pointed to other research showing a growing mental health crisis among young people in the U.S.
"Obviously social media predates 2017, but social media had the effect on a lot of kids where they feel left out, they feel compelled to look at social media, and they see people out having fun, and they're not a part of it," he said. "They can get ostracized through social media."
Adults aged 65 and older had the smallest increase for depression and were the only group that saw a decrease in rates of current depression from 2021.
When it came to breakdowns by race/ethnicity, results showed rates for Black and Hispanic adults are rising at about twice the rate of white adults.
The percentage of Black adults diagnosed with depression at some point in their lifetime rose from 20.1% to 34.4% between 2017 and 2023. For Hispanic adults, the percentage jumped from 18.4% to 31.3% over the same period.

Comparatively, white adults saw their rates increase from 22.3% in 2017 to 29% in 2023.
"For a long time, white America and white adults were reporting a clinical diagnosis of depression at rates that exceed Black and Hispanic adults," Witters said. "These big increases ... really show the strain that Black and Hispanic Americans have been under since 2017."
Black and Hispanic Americans were more likely to lose their jobs in the early days of the pandemic, he said, and events such as the death of George Floyd in May 2020 may have also contributed to depression.
"When the pandemic first hit, across all adults, negative emotional experiences [tracked by Gallup] such as sadness and anger went up a little but didn't really change that much," Witters said. "You fast forward a couple of months and you get to kind of the latter part of May and into June, anger and sadness were up over 10 percentage points."
ABC News' Dr. Amanda Kravitz contributed to this report.
Related Topics
- Mental Health

'Super Size Me' documentary filmmaker dies
- May 24, 11:43 AM

US man sentenced for having ammo in Turks & Caicos
- May 24, 1:01 PM
ABC News Live
24/7 coverage of breaking news and live events
ORIGINAL RESEARCH article
Evolution and emerging trends in depression research from 2004 to 2019: a literature visualization analysis.

- 1 School of Traditional Chinese Medicine, Beijing University of Chinese Medicine, Beijing, China
- 2 School of Life Sciences, Beijing University of Chinese Medicine, Beijing, China
Depression has become a major threat to human health, and researchers around the world are actively engaged in research on depression. In order to promote closer research, the study of the global depression knowledge map is significant. This study aims to map the knowledge map of depression research and show the current research distribution, hotspots, frontiers, and trends in the field of depression research, providing researchers with worthwhile information and ideas. Based on the Web of Science core collection of depression research from 2004 to 2019, this study systematically analyzed the country, journal, category, author, institution, cited article, and keyword aspects using bibliometric and data visualization methods. A relationship network of depression research was established, highlighting the highly influential countries, journals, categories, authors, institutions, cited articles, and keywords in this research field. The study identifies great research potential in the field of depression, provides scientific guidance for researchers to find potential collaborations through collaboration networks and coexistence networks, and systematically and accurately presents the hotspots, frontiers, and shortcomings of depression research through the knowledge map of global research on depression with the help of information analysis and fusion methods, which provides valuable information for researchers and institutions to determine meaningful research directions.
Introduction
Health issues are becoming more and more important to people due to the continuous development of health care. The social pressures on people are becoming more and more pronounced in a social environment that is developing at an increasing rate. Prolonged exposure to stress can have a negative impact on brain development ( 1 ), and depression is one of the more typical disorders that accompany it. Stress will increase the incidence of depression ( 2 ), depression has become a common disease ( 3 ), endangering people's physical health. Depression is a debilitating mental illness with mood disorders, also known as major depression, clinical depression, or melancholia. In human studies of the disease, it has been found that depression accounts for a large proportion of the affected population. According to the latest data from the World Health Organization (WHO) statistics in 2019, there are more than 350 million people with depression worldwide, with an increase of about 18% in the last decade and an estimated lifetime prevalence of 15% ( 4 ), it is a major cause of global disability and disease burden ( 5 ), and depression has quietly become a disease that threatens hundreds of millions of people worldwide.
Along with the rise of science communication research, the quantification of science is also flourishing. As a combination of “data science” and modern science, bibliometrics takes advantage of the explosive growth of research output in the era of big data, and uses topics, authors, publications, keywords, references, citations, etc. as research targets to reveal the current status and impact of the discipline more accurately and scientifically. Whereas, there is not a wealth of bibliometric studies related to depression. Fusar-Poli et al. ( 6 ) used bibliometrics to systematically evaluate cross-diagnostic psychiatry. Hammarström et al. ( 7 ) used bibliometrics to analyze the scientific quality of gender-related explanatory models of depression in the medical database PubMed. Tran et al. ( 8 ) used the bibliometric analysis of research progress and effective interventions for depression in AIDS patients. Wang et al. ( 9 ) used bibliometric methods to analyze scientific studies on the comorbidity of pain and depression. Shi et al. ( 10 ) performed a bibliometric analysis of the top 100 cited articles on biomarkers in the field of depression. Dongping et al. ( 11 ) used bibliometric analysis of studies on the association between depression and gut flora. An Chunping et al. ( 12 ) analyzed the literature on acupuncture for depression included in PubMed based on bibliometrics. Yi and Xiaoli ( 13 ) used a bibliometric method to analyze the characteristics of the literature on the treatment of depression by Chinese medicine in the last 10 years. Zhou and Yan ( 14 ) used bibliometric method to analyze the distribution of scientific and technological achievements on depression in Peoples R China. Guaijuan ( 15 ) performed a bibliometric analysis of the interrelationship between psoriasis and depression. Econometric analysis of the relationship between vitamin D deficiency and depression was performed by Yunzhi et al. ( 16 ) and Shauni et al. ( 17 ) performed a bibliometric analysis of domestic and international research papers on depression-related genes from 2003 to 2007. A previous review of depression-related bibliometric studies revealed that there is no bibliometric analysis of global studies in the field of depression, including country network analysis, journal network analysis, category network analysis, author network analysis, institutional network analysis, literature co-citation analysis, keyword co-presentation analysis, and cluster analysis.
The aim of this study was to conduct a comprehensive and systematic literature-based data mining and metrics analysis of depression-related research. More specifically, this analysis focuses on cooperative network and co-presentation analysis, based on the 36,477 papers included in the Web of Science Core Collection database from 2004 to 2019, and provides an in-depth analysis of cooperative network, co-presentation network, and co-citation through modern metrics and data visualization methods. Through the mining of key data, the data correlation is further explored, and the results obtained can be used to scientifically and reasonably predict the depression-related information. This study aims to show the spatial and temporal distribution of research countries, journals, authors, and institutions in the field of depression in a more concise manner through a relational network. A deeper understanding of the internal structure of the research community will help researchers and institutions to establish more accurate and effective global collaborations, in line with the trend of human destiny and globalization. In addition, the study will allow for the timely identification of gaps in current research. A more targeted research direction will be established, a more complete picture of the new developments in the field of depression today will be obtained, and the research protocol will be informed for further adjustments. The results of these analyses will help researchers understand the evolution of this field of study. Overall, this paper uses literature data analysis to find research hotspots in the field of depression, analyze the knowledge structure within different studies, and provide a basis for predicting research frontiers. This study analyzed the literature in the field of depression using CiteSpace 5.8.R2 (64-bit) to analyze collaborative networks, including country network analysis, journal network analysis, category network analysis, researcher network analysis, and institutional network analysis using CiteSpace 5.8.R2 (64-bit). In addition, literature co-citation, keyword co-presentation, and cluster analysis of depression research hotspots were also performed. Thus, exploring the knowledge dimensions of the field, quantifying the research patterns in the field, and uncovering emerging trends in the field will help to obtain more accurate and complete information. The large amount of current research results related to depression will be presented more intuitively and accurately with the medium of information technology, and the scientific evaluation of research themes and trend prediction will be provided from a new perspective.
Data Sources
The data in this paper comes from the Web of Science (WoS) core collection. The time years were selected as 2004–2019. First, the literature was retrieved after entering “depression” using the title search method. A total of 73,829 articles, excluding “depression” as “suppression,” “decline,” “sunken,” “pothole,” “slump,” “low pressure,” “frustration.” The total number of articles with other meanings such as “depression” was 5,606, and the total number of valid articles related to depression was 68,223. Next, the title search method was used to search for studies related to “major depressive disorder” not “depression,” and a total of 8,070 articles were retrieved. For the two search strategies, a total of 76,293 records were collected. The relevant literature retrieved under the two methods were combined and exported in “plain text” file format. The exported records included: “full records and references cited.” CiteSpace processed the data to obtain 41,408 valid records, covering all depression-related research articles for the period 2004–2019, and used this as the basis for analysis.
Processing Tools
CiteSpace ( 18 ), developed by Chao-Mei Chen, a professor in the School of Information Science and Technology at Drexel University, is a Java-based program with powerful data visualization capabilities and is one of the most widely used knowledge mapping tools. The software version used in this study is CiteSpace 5.8.R2 (64-bit).
Methods of Analysis
This study uses bibliometrics and data visualization as analytical methods. First, the application of bibliometrics to the field of depression helped to identify established and emerging research clusters, demonstrating the value of research in this area. Second, data visualization provides multiple perspectives on the data, presenting correlations in a clearer “knowledge graph” that can reveal underestimated and overlooked trends, patterns, and differences ( 19 ). CiteSpace is mainly based on the “co-occurrence clustering idea,” which extracts the information units (keywords, authors, institutions, countries, journals, etc.) in the data by classification, and then further reconstructs the data in the information units to form networks based on different types and strengths of connections (e.g., keyword co-occurrence, author collaboration, etc.). The resulting networks include nodes and links, where the nodes represent the information units of the literature and the links represent the existence of connections (co-occurrence) between the nodes. Finally, the network is measured, statistically analyzed, and presented in a visual way. The analysis needs to focus on: the overall structure of the network, key nodes and paths. The key evaluation indicators in this study are: betweenness centrality, year, keyword frequency, and burst strength. Betweenness centrality (BC) is the number of times a node acts as the shortest bridge between two other nodes. The higher the number of times a node acts as an “intermediary,” the greater its betweenness centrality. Betweenness centrality is a measure of the importance of articles found and measured by nodes in the network by labeling the category (or authors, journals, institutions, etc.) with purple circles. There may be many shortest paths between two nodes in the network, and by counting all the shortest paths of any two nodes in the network, if many of the shortest paths pass through a node, then the node is considered to have high betweenness centrality. In CiteSpace, nodes with betweenness centrality over 0.1 are called critical nodes. Year, which represents the publication time of the article. Frequency, which represents the number of occurrences. Burst strength, an indicator used to measure articles with sudden rise or sudden decline in citations. Nodes with high burst strength usually represent a shift in a certain research area and need to be focused on, and the burst article points are indicated in red. The nodes and their sizes and colors are first analyzed initially, and further analyzed by betweenness centrality indicators for evaluation. Each node represents an article, and the larger the node, the greater the frequency of the keyword word and the greater the relevance to the topic. Similarly, the color of the node represents time: the warmer the color, the more recent the time; the colder the color, the older the era; the node with a purple outer ring is a node with high betweenness centrality; the color of each annual ring can determine the time distribution: the color of the annual ring represents the corresponding time, and the thickness of one annual ring is proportional to the number of articles within the corresponding time division; the dominant color can reflect the relative concentration of the emergence time; the node The appearance of red annual rings in the annual rings means hot spots, and the frequency of citations has been or is still increasing rapidly.
Large-Scale Assessment
Country analysis.
During the period 2004–2019, a total of 157 countries/territories have conducted research on depression, which is about 67.38% of 233 countries/territories worldwide. This shows that depression is receiving attention from many countries/regions around the world. Figure 1 shows the geographical distribution of published articles for 157 countries. The top 15 countries are ranked according to the number of articles published. Table 1 lists the top 15 countries with the highest number of publications in the field of depression worldwide from 2004 to 2019. These 15 countries include 4 Asian countries (Peoples R China, Japan, South Korea, Turkey), 2 North American countries (USA, Canada), 1 South American country (Brazil), 7 European countries (UK, Germany, Netherlands, Italy, France, Spain, Sweden), and 1 Oceania country (Australia).
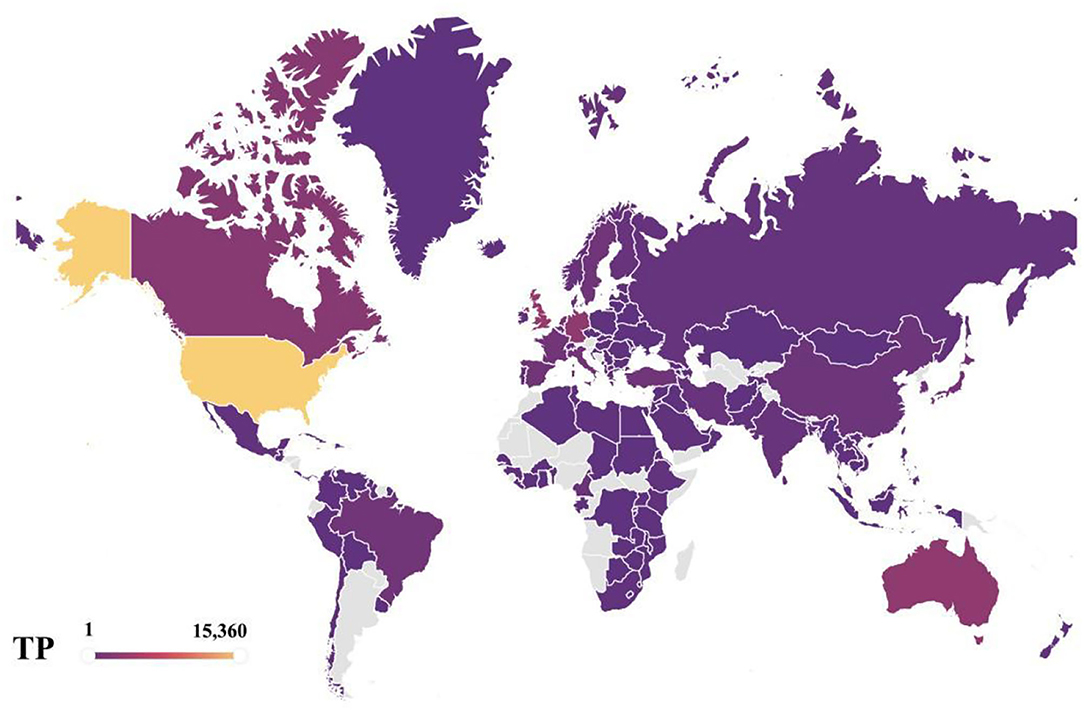
Figure 1 . Geographical distributions of publications, 2004–2019.
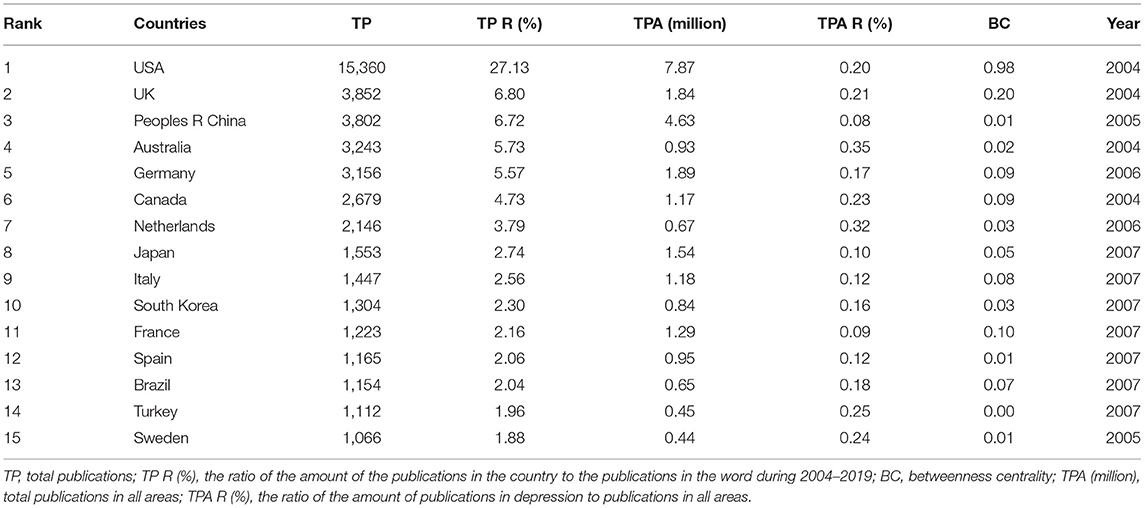
Table 1 . The top 15 productive countries.
Overall, the main distribution of these articles is in USA and some European countries, such as UK, Germany, Netherlands, Italy, France, Spain, and Sweden. This means that these countries are more interested and focused on research on depression compared to others. The total number of publications across all research areas in the Web of Science core collection is similar to the distribution of depression research areas, with the trend toward USA, UK, and Peoples R China as leading countries being unmistakable, and USA has been a leader in the field of depression, with far more articles published than any other country. It can also be seen that USA is the country with the highest betweenness centrality in the network of national collaborations analyzed in this paper. USA research in the field of depression is closely linked to global research, and is an important part of the global collaborative network for depression research. As of 2019, the total number of articles published in depression performance research in USA represents 27.13% of the total number of articles published in depression worldwide, which is ~4 times more than the second-place country, UK, which is far ahead of other countries. Peoples R China, as the third most published country, has a dominant number of articles, but its betweenness centrality is 0.01, reflecting the fact that Peoples R China has less collaborative research with other countries, so Peoples R China should strengthen its foreign collaborative research and actively establish global scientific research partnerships to seek development and generate breakthroughs in cooperation. The average percentage of scientific research on depression in each country is about 0.19%, also highlighting the urgent need to address depression as one of the global human health problems. The four Asian countries included in the top 15 countries are Peoples R China, Japan, South Korea, and Turkey, with Peoples R China ranking third with 6.72% of the total number of all articles counted. The distribution may be explained by the fact that Peoples R China is the largest developing country with a rapid development rate as the largest. Along with the steady rise in the country's economic power, people are creating economic benefits and their health is becoming a consumable commodity. The lifetime prevalence and duration of depression varies by country and region ( 2 ), but the high prevalence and persistence of depression worldwide confirms the increasing severity of the disease worldwide. The WHO estimates that more than 300 million people, or 4.4% of the world's population, suffer from depression ( 20 ), with the number of people suffering from depression increasing at a patient rate of 18.4% between 2005 and 2015. Depression, one of the most prevalent mental illnesses of our time, has caused both physical and psychological harm to many people, and it has become the leading cause of disability worldwide today, and in this context, there is increased interest and focus on research into depression. It is expected that a more comprehensive understanding of depression and finding ways to prevent and cope with the occurrence of this disease can help people get rid of the pain and shadow brought by depression, obtain a healthy and comfortable physical and mental environment and physical health, and make Chinese contributions to the cause of human health. Undoubtedly, the occurrence of depressive illnesses in the context of irreversible human social development has stimulated a vigorous scientific research environment on depression in Peoples R China and other developing countries and contributed to the improvement of research capacity in these countries. Moreover, from a different perspective, the geographical distribution of articles in this field also represents the fundamental position of the country in the overall scientific and academic research field.
Growth Trend Analysis
Figure 2 depicts the distribution of 38,433 articles from the top 10 countries in terms of the number of publications and the trend of growth during 2004–2019.
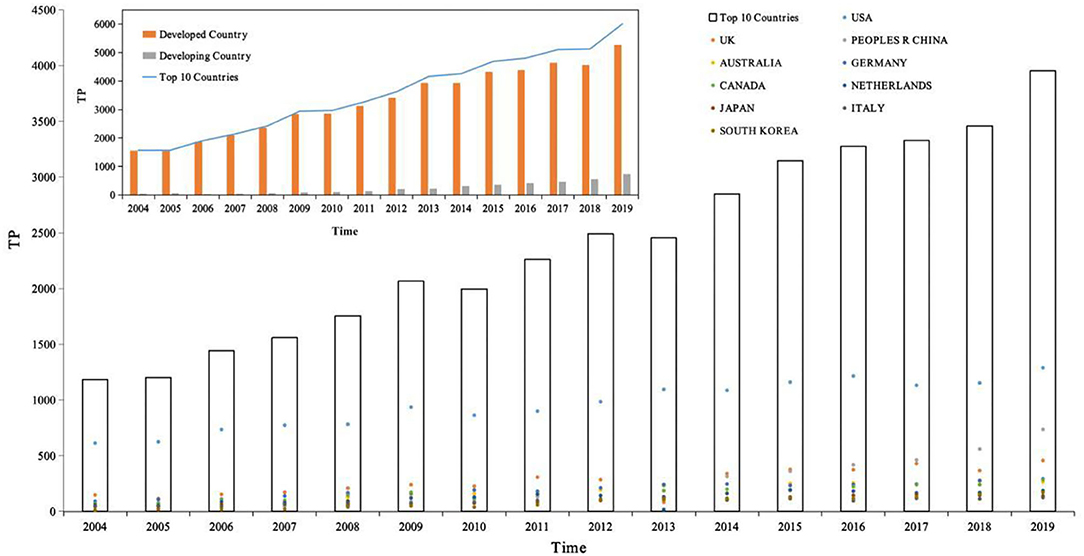
Figure 2 . The distribution of publications in top 10 productive countries, 2004–2019. Source: author's calculation. National development classification criteria refer to “Human Development Report 2020” ( 21 ).
First, the number of articles published per year for the top 10 countries in terms of productivity was counted and then the white bar chart in Figure 2 was plotted, with the year as the horizontal coordinate and total publications as the vertical coordinate, showing the distribution of the productivity of articles in the field of depression per year. The total number of publications for the period 2004–2019 is 38,433. Based on the white bars and line graphs in Figure 2 , we can divide this time period into three growth periods. The number of publications in each growth period is calculated based on the number of publications per year. As can be seen from the figure, the period 2004–2019 can be divided into three main growth periods, namely 2004–2009, 2010–2012, and 2013–2019, the first growth period being from 2004 to 2009, the number of publications totaled 6,749, accounting for 23.97% of all publications; from 2010 to 2012, the number of publications totaled 8,236, accounting for 17.56% of all publications; and from 2013 to 2019, the number of publications totaled 22,473, accounting for 58.47% of all publications. Of these, 2006 was the first year of sharp growth with an annual growth rate of 19.97%, 2009 was the second year of sharp growth with an annual growth rate of 17.64%, and 2008 was the third year of sharp growth with an annual growth rate of 16.09%. In the last 5 years, 2019 has also shown a sharp growth trend with a growth rate of 14.34%. Notably, in 2010 and 2013, there was negative growth with the growth rate of −3.39 and −1.45%. In the last 10 years, depression research has become one of the most valuable areas of human research. It can also be noted that the number of publications in the field of depression in these 10 countries has been increasing year after year.
Second, the analysis is conducted from the perspective of national development, divided into developed and developing countries, as shown in the orange bar chart in Figure 2 , where the horizontal coordinate is year and the vertical coordinate is total publications, comparing the article productivity variability between developed and developing countries. The top 10 most productive countries in the field of depression globally include nine developed countries and one developing country, respectively. During the period 2004–2019, 34,631 papers were published in developed countries and 3,802 papers were published in developing countries, with developed countries accounting for 90.11% of the 38,433 articles and developing countries accounting for 9.89%, and the total number of publications in developed countries was about 9 times higher than that in developing countries. During the period 2004–2019, the number of publications in developed countries showed negative growth in 2 years (2010 and 2013) with growth rates of −3.39 and −1.45%, respectively. The rest of the years showed positive growth with growth rates of 1.52% (2005), 19.97 (2006), 8.11 (2007), 12.70 (2008), 17.64 (2009), 13.22 (2011), 10.17 (2012), 16.09 (2014), 10.46 (2015), 4.10 (2016), 1.59 (2017), 3.91 (2018), and 14.34 (2019), showing three periods of positive growth: 2004–2009, 2011–2012, and 2014–2019, with the highest growth rate of 19.97% in 2006. Recent years have also shown a higher growth trend, with a growth rate of 14.34% in 2019. It is worth noting that developing countries have been showing positive growth in the number of articles in the period 2004–2019, with annual growth rates of 81.25 (2005), 17.24 (2006), 35.29 (2007), 19.57 (2008), 65.45 (2009), 13.19 (2010), 29.13 (2011), 54.89 (2012), 12.14 (2013), 36.36 (2014), 14.92 (2015), 16.02 (2016), 10.24 (2017), 21.17 (2018), and 31.37 (2019), with the highest growth rate of 81.25% in 2005. In the field of depression research, developed countries are still the main force and occupy an important position.
Further, 10 countries with the highest productivity in the field of depression are compared, total publications in the vertical coordinate, and the colored scatter plot contains 10 colored dots, representing 10 different countries. On the one hand, the variability of the contributions of different countries in the same time frame can be compared horizontally. On the other hand, it is possible to compare vertically the variability of the growth of different countries over time. Among them, USA, with about 40.29% of the world's publications in the field of depression, has always been a leader in the field of depression with its rich research results. Peoples R China, as the only developing country, ranks 3rd in the top 10 countries with high production of research papers in the field of depression, and Peoples R China's research in the field of depression has shown a rapid growth trend, and by 2016, it has jumped to become the 2nd largest country in the world, with the number of published papers increasing year by year, which has a broad prospect and great potential for development.
Distribution of Periodicals
Table 2 lists the top 15 journals in order of number of journal co-citations. In the field of depression, the top 15 cited journals accounted for 19.06% of the total number of co-citations, nearly one in five of the total number of journal co-citations. In particular, the top 3 journals were ARCH GEN PSYCHIAT (ARCHIVES OF GENERAL PSYCHIATRY), J AFFECT DISORDERS (JOURNAL OF AFFECTIVE DISORDERS), and AM J PSYCHIAT (AMERICAN JOURNAL OF PSYCHIATRY), with co-citation counts of 20,499, 20,302, and 20,143, with co-citation rates of 2.09, 2.07, and 2.06%, respectively. The main research area of ARCH GEN PSYCHIAT is Psychiatry; the main research area of the journal J AFFECT DISORDERS is Neurosciences and Neurology, Psychiatry; AM J PSYCHIAT is the main research area of Psychiatry, and the three journals have “psychiatry” in common, making them the most frequently co-cited journals in the field of depression.
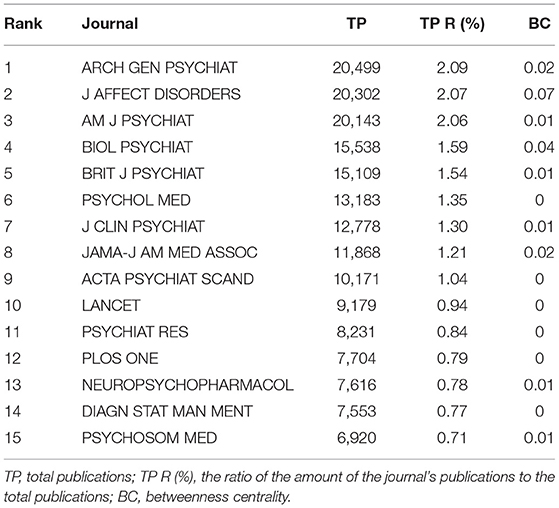
Table 2 . The top 15 co-cited journals.
Figure 3 shows the network relationship graph of the cited journals from 2004 to 2019. The figure takes g-index as the selection criteria, the scale factor k = 25 to include more nodes. Each node of the graph represents each journal, the node size represents the number of citation frequencies, the label size represents the size of the betweenness centrality of the journal in the network, and the links between journals represent the co-citation relationships. The journal co-citation map reflects the structure of the journals, indicating that there are links between journals and that the journals include similar research topics. These journals included research topics related to neuroscience, psychiatry, neurology, and psychology. The journal with betweenness centrality size in the top 1 was ARCH GEN PSYCHIAT, with betweenness centrality size of 0.07, and impact shadows of 14.48. ARCH GEN PSYCHIAT, has research themes of Psychiatry. In all, these journals in Figure 3 occupy an important position in the journal's co-citation network and have strong links with other journals.
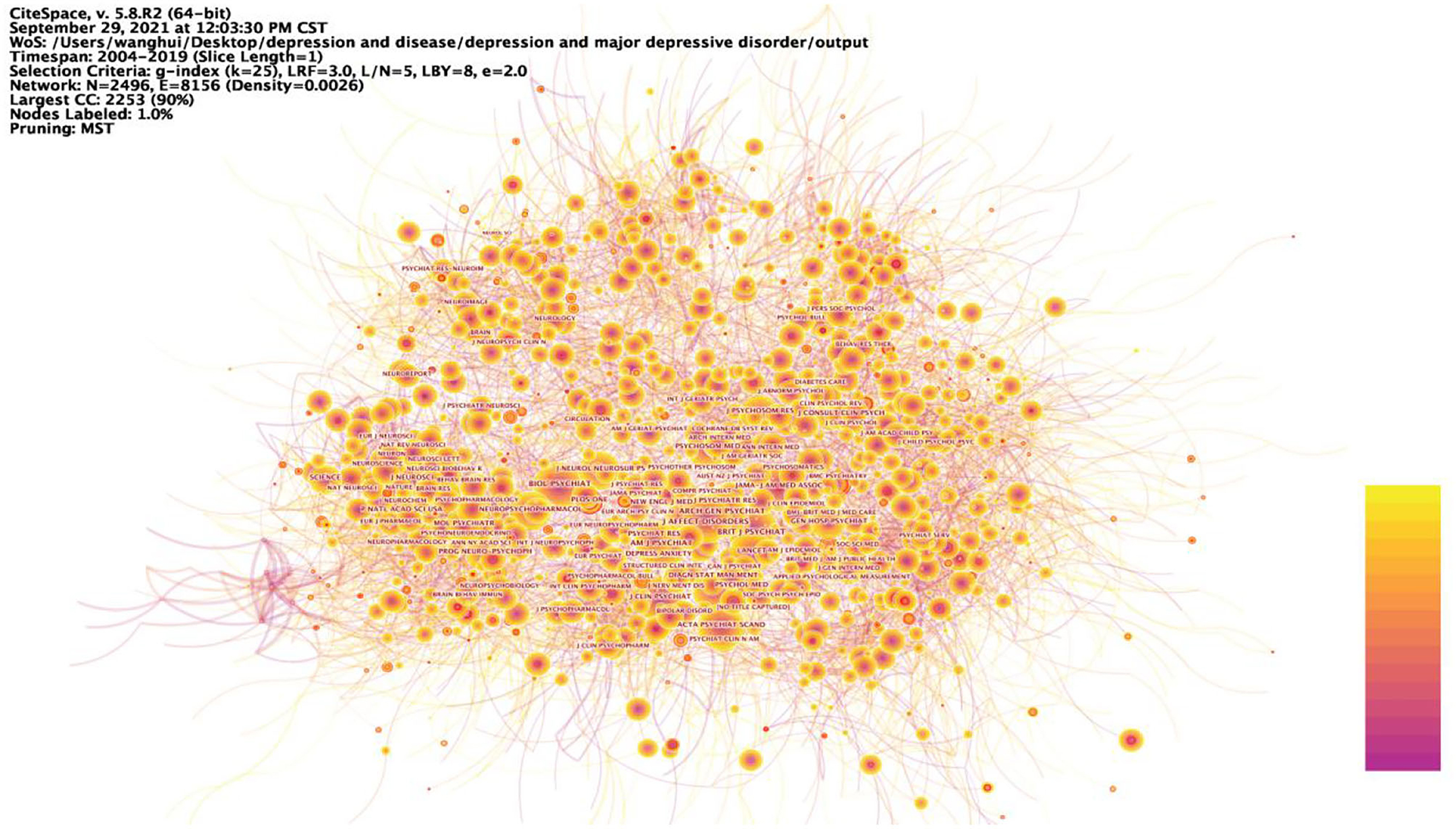
Figure 3 . Prominent journals involved in depression. The betweenness centrality of a node in the network measures the importance of the position of the node in the network. Two types of nodes may have high betweenness centrality scores: (1) Nodes that are highly connected to other nodes, (2) Nodes are positioned between different groups of nodes. The lines represent the link between two different nodes.
Distribution of Categories
Table 3 lists the 15 most popular categories in the field of depression research during the period 2004–2019. In general, the main disciplines involved are neuroscience, psychology, pharmacy, medicine, and health care, which are closely related to human life and health issues. Of these, psychiatry accounted for 20.78%, or about one-five, making it the most researched category. The study of depression focuses on neuroscience, reflecting the essential characteristics of depression as a category of mental illness and better reflecting the fact that depression is an important link in the human public health care. In addition, Table 3 shows that the category with the highest betweenness centrality is Neuroscience, followed by Public, Environment & Occupational Health, and then Pharmacology & Pharmacy, with betweenness centrality of 0.16, 0.13, and 0.11, respectively. It is found that the research categories of depression are also centered on disciplines such as neuroscience, public health and pharmacology, indicating that research on depression requires a high degree of integration of multidisciplinary knowledge and integration of information from various disciplines in order to have a more comprehensive and in-depth understanding of the depression.
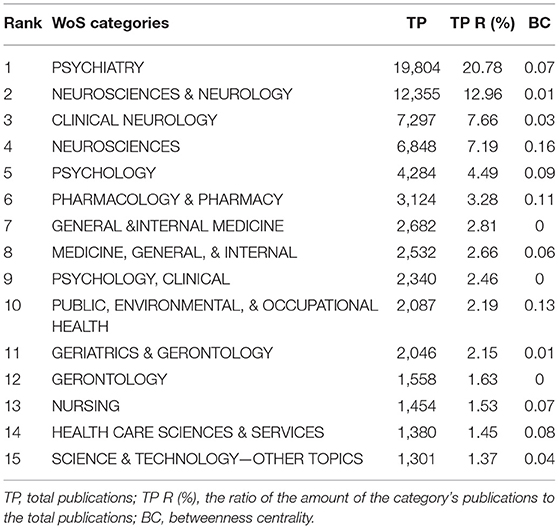
Table 3 . The top 15 productive categories, 2004–2019.
Figure 4 shows the nine categories with the betweenness centrality in the category research network, with Neuroscience being the node with the highest betweenness centrality in this network, meaning that Neuroscience is most strongly linked to all research categories in the field of depression research. Depression is a debilitating psychiatric disorder with mood disorders. It is worth noting that the development of depression not only has psychological effects on humans, but also triggers many somatic symptoms that have a bad impact on their daily work and life, giving rise to the second major mediating central point of research with public health as its theme. The somatization symptoms of depression often manifest as abnormalities in the cardiovascular system, and many studies have looked at the pathology of the cardiovascular system in the hope of finding factors that influence the onset of depression, mechanisms that trigger it or new ways to treat it. Thus, depression involves not only the nervous system, but also interacts with the human cardiovascular system, for example, and the complexity of depression dictates that the study of depression is an in-depth study based on complex systems.
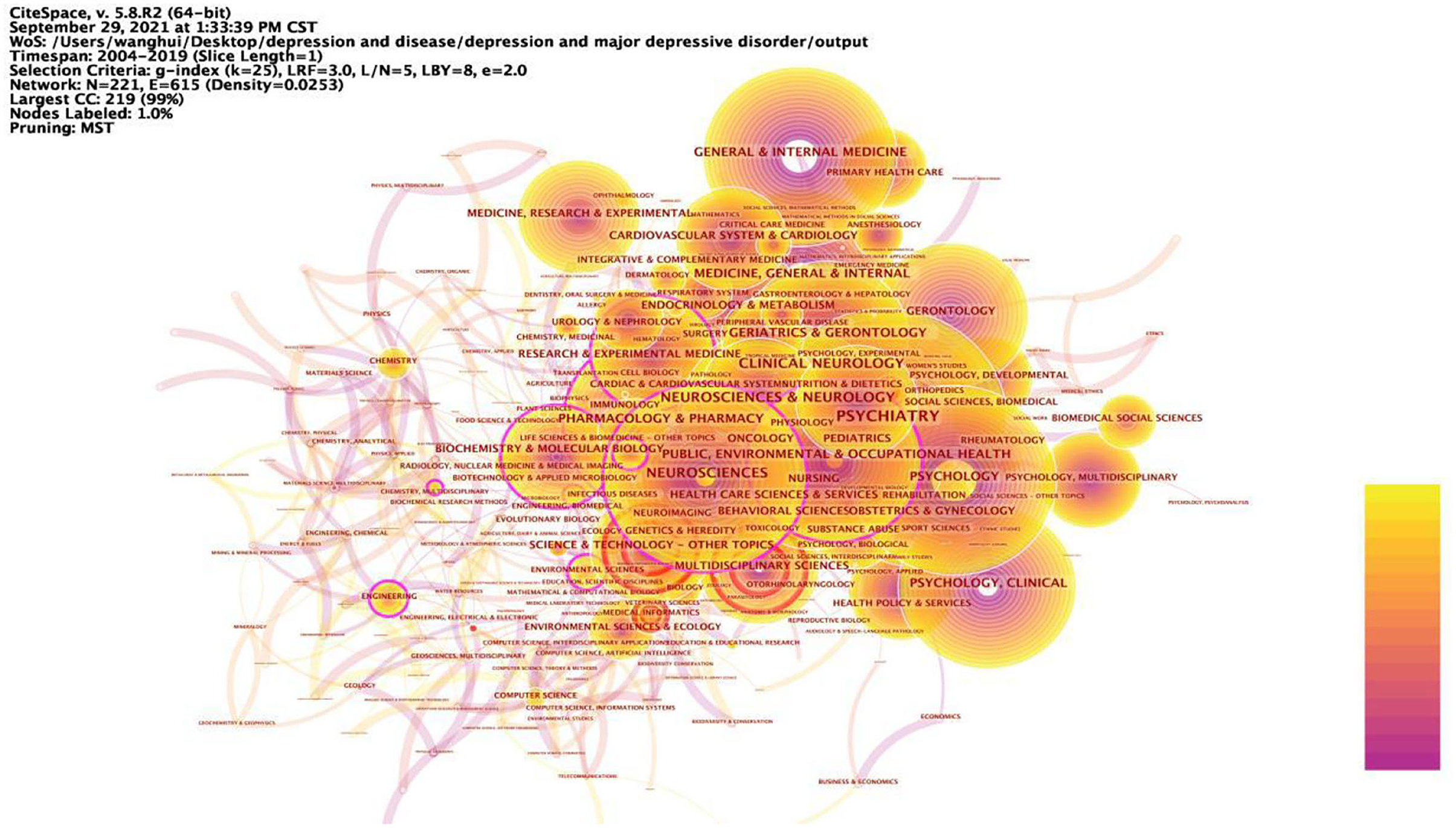
Figure 4 . Prominent categories involved in depression, 2004–2019. The betweenness centrality of a node in the network measures the importance of the position of the node in the network. Two types of nodes may have high betweenness centrality scores: (1) Nodes that are highly connected to other nodes, (2) Nodes are positioned between different groups of nodes. The lines represent the link between two different nodes.
Author Statistics
The results of the analysis showed that there were many researchers working in the field of depression over the past 16 years, and 63 of the authors published at least 30 articles related to depression. Table 4 lists the 15 authors with the highest number of articles published. It includes the rank of the number of articles published, author, country, number of articles published in depression-related studies, total number of articles included in Web of Science, total number of citations, average number of citations, and H-index. According to the statistics, seven of the top 15 authors are from USA, three from the Netherlands, one from Canada, one from Australia, one from New Zealand, one from Italy, and one from Germany. From this, it can be seen that these productive authors are from developed countries, thus it can be inferred that developed countries have a better research environment, more advanced research technology and more abundant research funding. The evaluation indicators in the author co-occurrence network are frequency, betweenness centrality and time of first appearance. The higher the frequency, i.e., the higher the number of collaborative publications, the more collaboration, the higher the information dissemination rate, the three authors with the highest frequency in this author co-occurrence network are MAURIZIO FAVA, BRENDA W. J. H. PENNINX, MADHUKAR H. TRIVEDI; the higher the betweenness centrality, i.e., the closer the relationship with other authors, the more collaboration, the higher the information dissemination rate, the three authors with the highest betweenness centrality are the three authors with the highest betweenness centrality are MICHAEL E. THASE, A. JOHN RUSH; the time of first appearance, i.e., the longer the influence generated by the author's research, the higher the information dissemination rate; in addition, the impact factor and citations can also reflect the information dissemination efficiency of the authors.
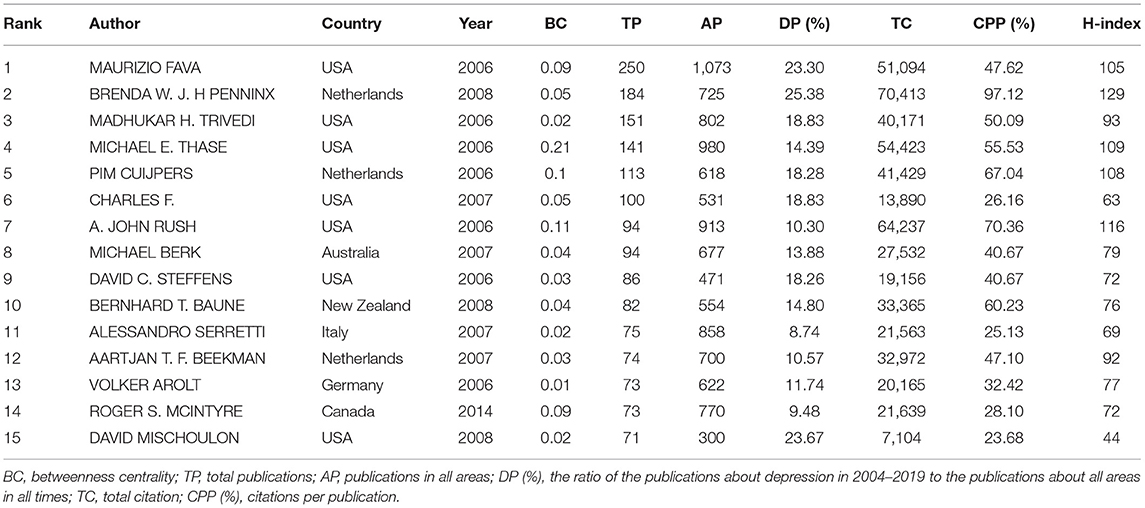
Table 4 . The top 15 authors in network of co-authorship, 2004–2019.
The timezone view ( Figure 5 ) in the author co-occurrence network clearly shows the updates and interactions of author collaborations, for example. All nodes are positioned in a two-dimensional coordinate with the horizontal axis of time, and according to the time of first posting, the nodes are set in different time zones, and their positions are sequentially upward with the time axis, showing a left-to-right, bottom-up knowledge evolution diagram. The time period 2004–2019 is divided into 16 time zones, one for each year, and each circle in the figure represents an author, and the time zone in which the circle appears is the year when the author first published an article in the data set of this study. The closer the color, the warmer the color, the closer the time, the colder the color, the older the era, the thickness of an annual circle, and the number of articles within the corresponding time division is proportional, the dominant color can reflect the relative concentration of the emergence time, the nodes appear in the annual circle of the red annual circle, that is, on behalf of the hot spot, the frequency of being cited was or is still increasing sharply. Nodes with purple outer circles are nodes with high betweenness centrality. The time zone view demonstrates the growth of author collaboration in the field, and it can be found from the graph that the number of author collaborations increases over time, and the frequency of publications in the author collaboration network is high; observe that the thickness of the warm annual rings in the graph is much greater than the thickness of the cold annual rings, which represents the increase of collaboration in time; there are many authors in all time zones, which indicates that there are many research collaborations and achievements in the field, and the field is in a period of collaborative prosperity. The linkage relationship between the sub-time-periods can be seen by the linkage relationship between the time periods, and it can be found from the figure that there are many linkages in the field in all time periods, which indicates that the author collaboration in the field of depression research is strong.
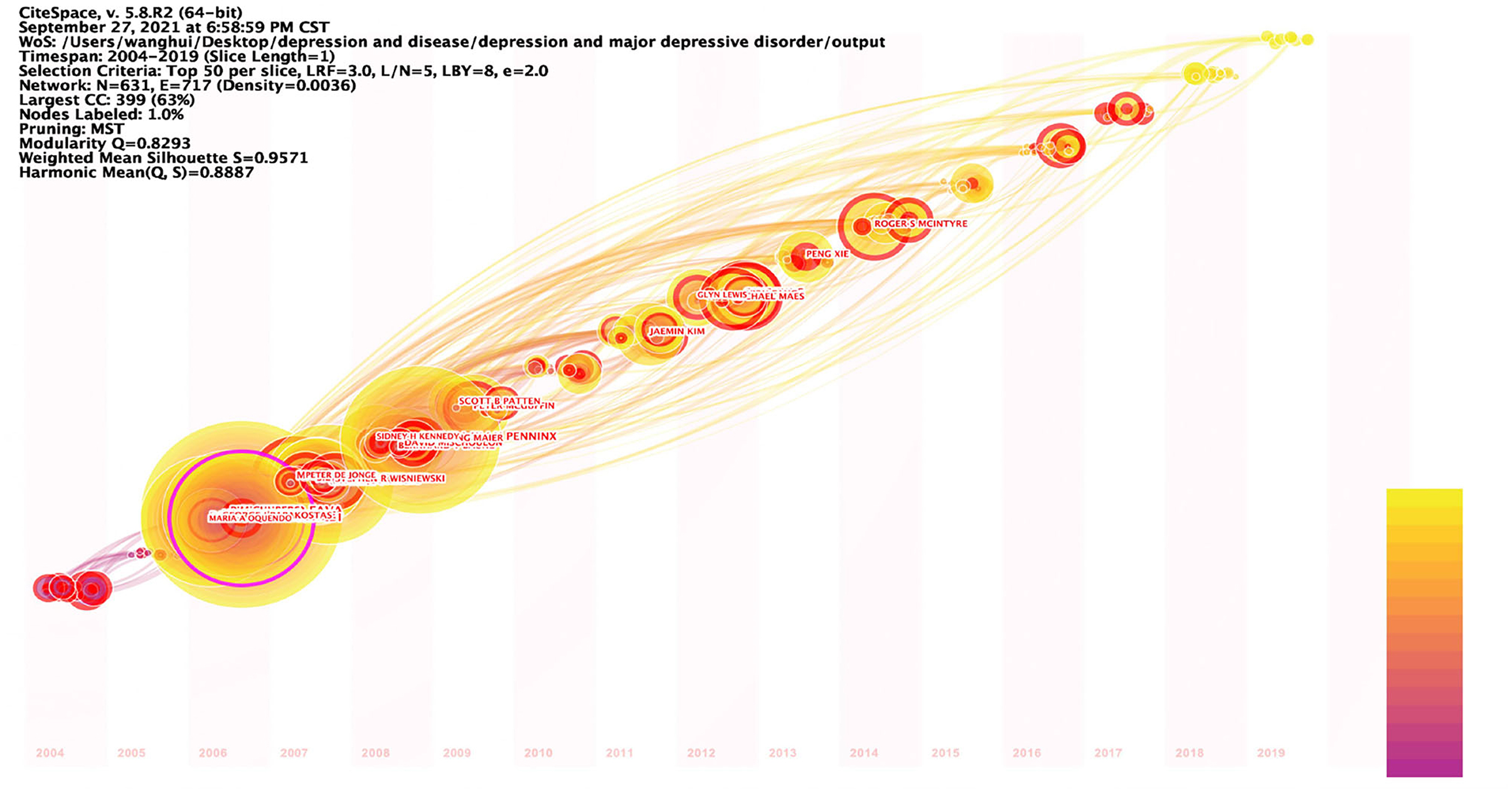
Figure 5 . Timezone view of the author's co-existing network in depression, 2004–2019. The circle represents the author, the time zone in which the circle appears is the year in which the author first published in this study dataset, the radius of the circle represents the frequency of appearance, the color represents the different posting times, the lines represent the connections between authors, and the time zone diagram shows the evolution of author collaboration.
Institutional Statistics
Table 5 lists the top 15 research institutions in network of co-authors' institutions. These include 10 American research institutions, two Netherlands research institutions, one UK research institution, one Canadian research institution and one Australian research institution, all of which, according to the statistics, are from developed countries. Of these influential research institutions, 66.7% are from USA. Figure 6 shows the collaborative network with these influential research institutions as nodes. Kings Coll London (0.2), Univ Michigan (0.17), Univ Toronto (0.15), Stanford Univ (0.14), Univ Penn (0.14), Univ Pittsburgh (0.14), Univ Melbourne (0.12), Virginia Commonwealth Univ (0.12), Columbia Univ (0.1), Duke Univ (0.1), Massachusetts Gen Hosp (0.1), Vrije Univ Amsterdam (0.1), with betweenness centrality >0.1. Kings Coll London has a central place in this collaborative network and is influential in the field of depression research. Table 6 lists the 15 institutions with the strong burst strength. The top 3 institutions are all from USA. Univ Copenhagen, Univ Illinois, Harvard Med Sch, Boston Univ, Univ Adelaide, Heidelberg Univ, Univ New South Wales, and Icahn Sch Med Mt Sinai have had strong burst strength in recent years. It suggests that these institutions may have made a greater contribution to the field of depression over the course of this year and more attention could be paid to their research.
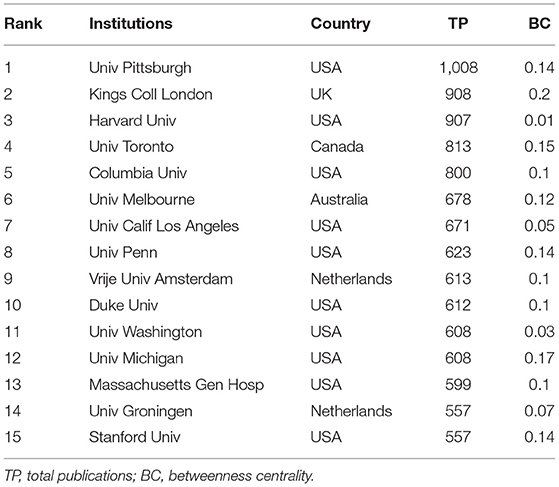
Table 5 . The top 15 institutions in network of co-authors' institutions, 2004–2019.
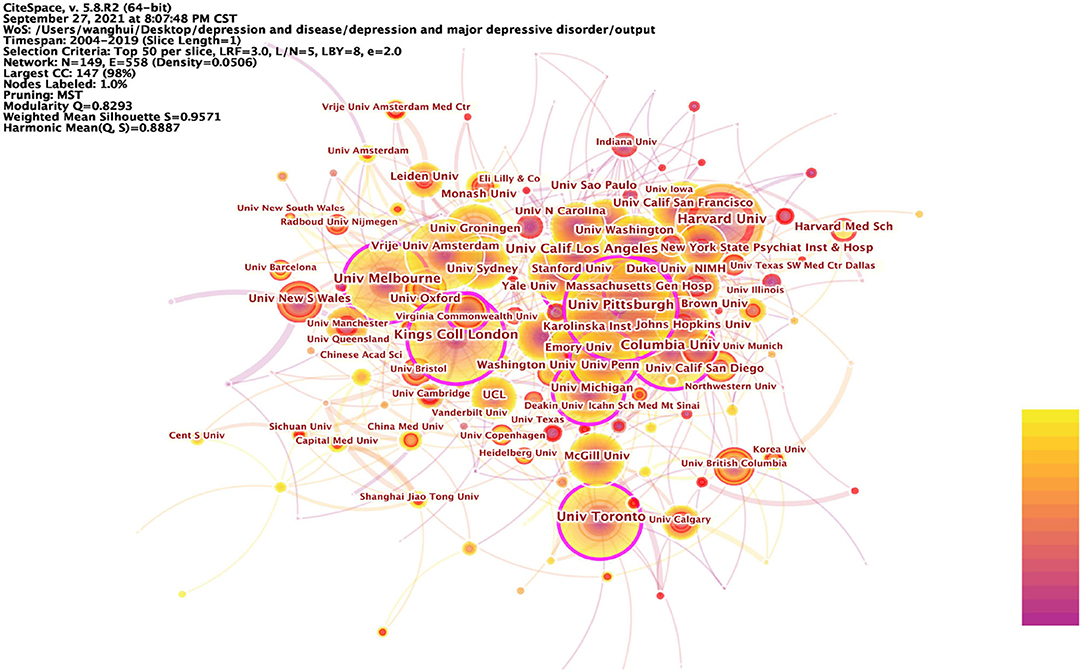
Figure 6 . Prominent institutions involved in depression, 2004–2019. The betweenness centrality of a node in the network measures the importance of the position of the node in the network. Two types of nodes may have high betweenness centrality scores: (1) Nodes that are highly connected to other nodes, (2) Nodes are positioned between different groups of nodes. The lines represent the link between two different nodes.
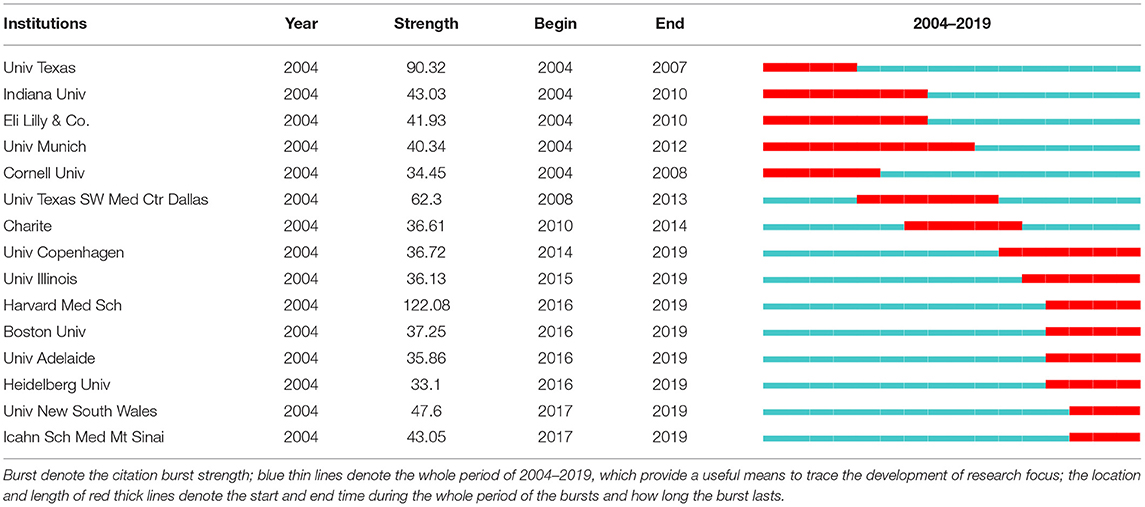
Table 6 . The top 15 institutions with the strongest citation bursts, 2004–2019.
Summing up the above analysis, it can be seen that the research institutions in USA are at the center of the depression research field, are at the top of the world in terms of quantity and quality of research, and are showing continuous growth in vitality. Research institutions in USA, as pioneers among all research institutions, lead and drive the development of depression research and play an important role in cutting-edge research in the field of depression.
Article Citations
Table 7 lists the 16 articles that have been cited more than 1,000 times within the statistical range of this paper from 2004 to 2019. As can be seen from the table, the most cited article was written by Dowlati et al. from Canada and published in BIOLOGICAL PSYCHIATRY 2010, which was cited 2,556 times. In addition, 11 of these 16 highly cited articles were from the USA. Notably, two articles by Kroenke, K as first author appear in this list, ranked 7th and 11th, respectively. In addition, there are three articles from Canada, one article from Switzerland, and one article from the UK. And interestingly, all of these countries are developed countries. It can be reflected that developed countries have ample research experience and high quality of research in the field of depression research. On the other hand, it also reflects that depression is a key concern in developed countries. These highly cited articles provide useful information to many researchers and are of high academic and exploratory value.
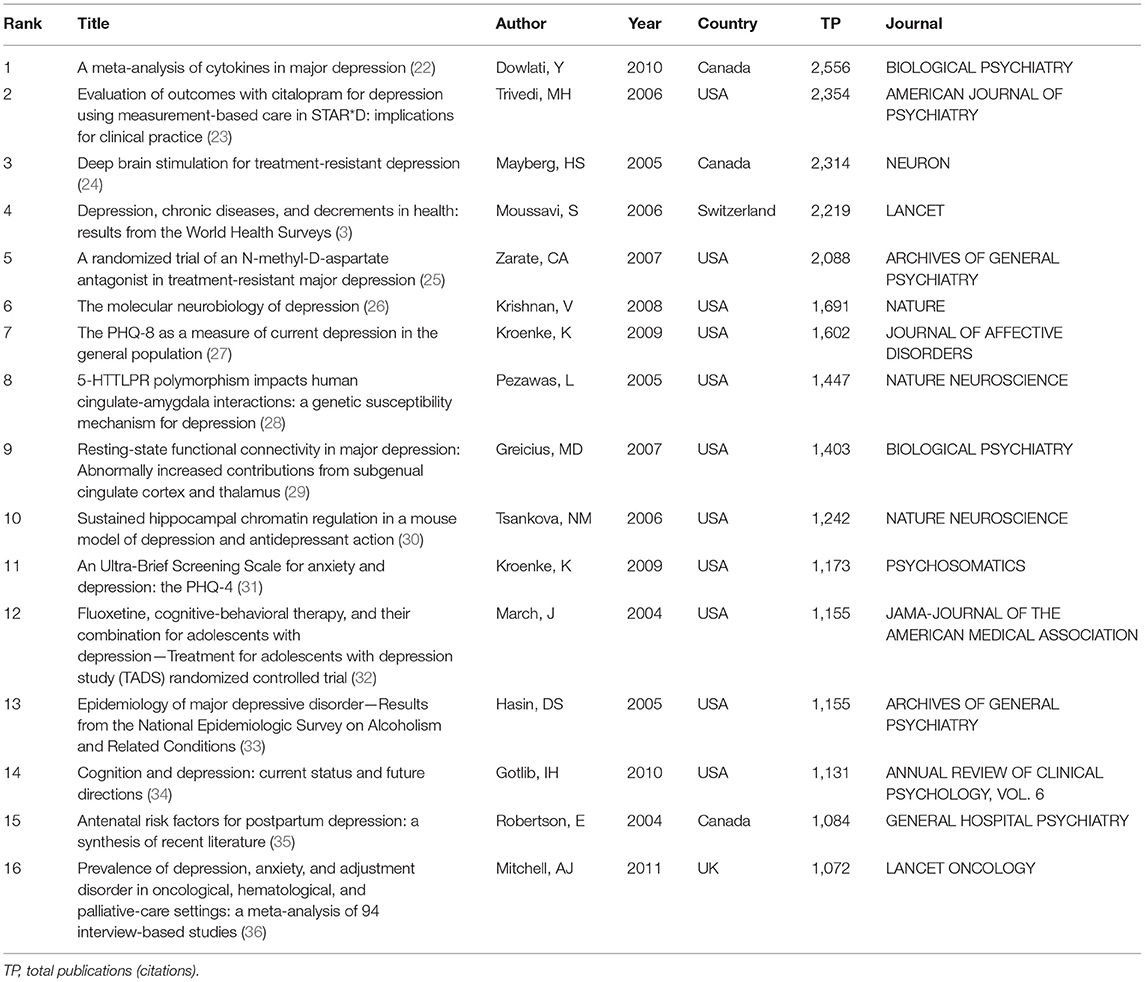
Table 7 . The top 15 frequency cited articles, 2004–2019.
Research Hotspots Ang Frontiers
Keyword analysis.
The keyword analysis of depression yielded the 25 most frequent keywords in Table 8 and the keyword co-occurrence network in Figure 7 . Also, the data from this study were detected by burst, the 25 keywords with the strongest burst strength were obtained in Table 9 . These results bring out the popular and cutting-edge research directions in the field clearly.
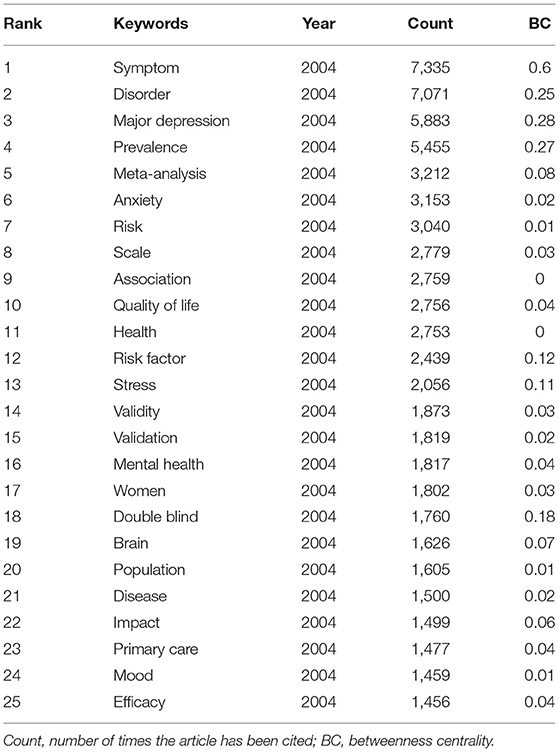
Table 8 . Top 25 frequent keywords in the period of 2004–2019.
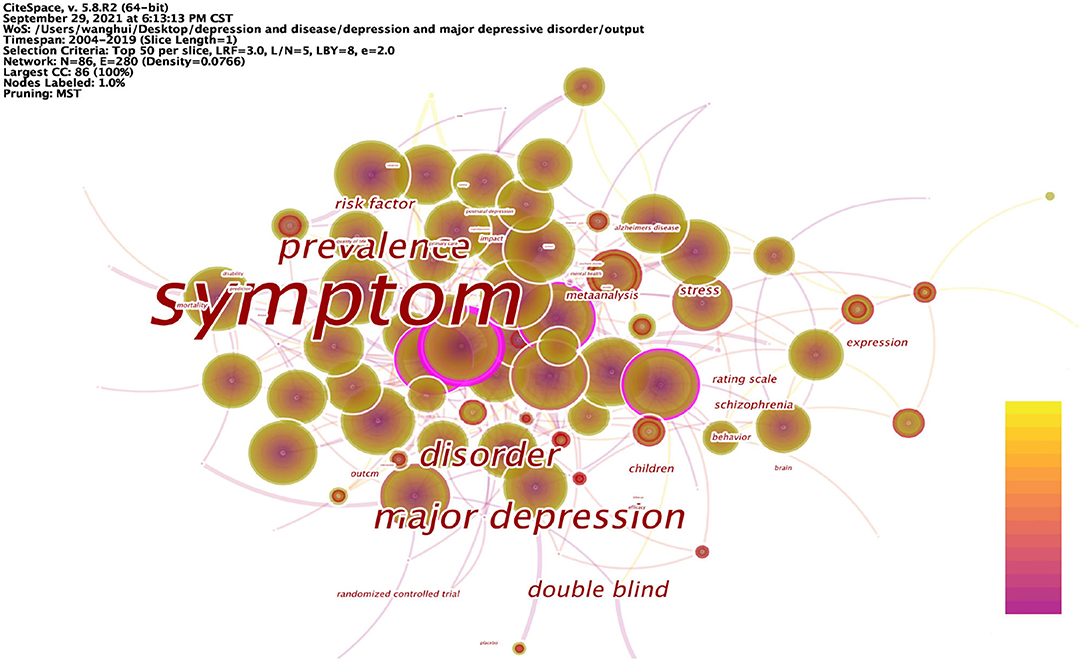
Figure 7 . Keyword co-occurrence network in depression, 2004–2019.

Table 9 . Top 25 keywords with strongest citation bursts in the period of 2004–2019.
The articles on depression during 2004–2019 were analyzed in 1-year time slices, and the top 25 keywords with the highest frequency of occurrence were selected from each slice to obtain the keyword network shown in Table 8 . The top 25 keywords with the highest frequencies were: symptom, disorder, major depression, prevalence, meta-analysis, anxiety, risk, scale, association, quality of life, health, risk factor, stress, validity, validation, mental health, women, double blind, brain, population, disease, impact, primary care, mood, and efficacy. High-frequency nodes respond to popular keywords and are an important basis for the field of depression research.
Figure 7 shows the co-occurrence network mapping of keywords regarding depression research. Each circle in the figure is a node representing a keyword, and the greater the betweenness centrality, the more critical the position of the node in the network. The top 10 keywords in terms of betweenness centrality are: symptom (0.6), major depression (0.28), prevalence (0.27), disorder (0.25), double blind (0.18), risk factor (0.12), stress (0.11), children (0.1), schizophrenia (0.1), and expression (0.1). Nodes with high betweenness centrality reflect that the keyword forms a co-occurrence relationship with multiple other keywords in the domain. A higher betweenness centrality indicates that it is more related to other keywords, and therefore, the node plays an important role in the study. Relatively speaking, these nodes represent the main research directions in the field of depression; they are also the key research directions in this period, and to a certain extent, represent the research hotspots in this period.
Burst detection was performed on the keywords, and the 25 keywords with the strongest strength were extracted, as shown in Table 9 . These keywords contain: fluoxetine, community, follow up, illness, psychiatric disorder, dementia, trial, placebo, disability, serotonin reuptake inhibitor, myocardial infarction, hospital anxiety, antidepressant treatment, late life depression, United States, epidemiology, major depression, model, severity, adolescent, people, prefrontal cortex, management, meta-analysis, and expression. The keywords that burst earlier include fluoxetine (2004), community (2004), follow up (2004), illness (2004), and psychiatric disorder (2004), are keywords that imply that researchers focused on themes early in the field of depression. As researchers continue to explore, the study of depression is changing day by day, and the keywords that have burst in recent years are people (2015), prefrontal cortex (2016), management (2016), meta-analysis (2017), and expression (2017). Reflecting the fact that depression research in recent years has mainly focused on human subjects, the focus has been on the characterization of populations with depression onset. The relationship between depression and the brain has aroused the curiosity of researchers, what exactly are the causes that trigger depression and what are the effects of depression for the manifestation of depression have caused a wide range of discussions in the research community, and the topics related to it have become the most popular studies and have been the focus of research in recent years. All of these research areas showed considerable growth, indicating that research into this area is gaining traction, suggesting that it is becoming a future research priority. The keywords with the strongest burst strength are fluoxetine (111.2), community (110.08), antidepressant treatment (94.28), severity (88.35), meta-analysis (86.42), people (85.33), and follow up (84.46). The rapid growth of research based on these keywords indicates that these topics are the most promising and interesting. The keywords that has been around the longest burst are follow up (2004–2013), model (2013–2019), hospital anxiety (2008–2013), severity (2014–2019), and psychiatric disorder (2004–2008), researchers have invested a lot of research time in these research directions, making many research results, and responding to the exploratory value and significance of research on these topics. At the same time, the longer duration of burst also proves that these research directions have research potential and important value.
Research Hotspots
Hotspots must mainly have the characteristics of high frequency, high betweenness centrality, strong burst, and time of emergence can be used as secondary evaluation indicators. The higher the number of occurrences, the higher the degree of popularity and attention. The higher betweenness centrality means the greater the influence and the higher the importance. Nodes with strong burst usually represent key shift nodes and need to be focused on. The time can be dynamically adjusted according to the target time horizon of the analysis. Thus, based on the results of statistical analysis, it is clear that the research hotspots in the field of depression can be divided into four main areas: etiology (external factors, internal factors), impact (quality of life, disease symptoms, co-morbid symptoms), treatment (interventions, drug development, care modalities), and assessment (population, size, symptoms, duration of disease, morbidity, mortality, effectiveness).
Risk factors for depression include a family history of depression, early life abuse and neglect, and female sexuality and recent life stressors. Physical illnesses also increase the risk of depression, particularly increasing the prevalence associated with metabolic (e.g., cardiovascular disease) and autoimmune disorders.
Research on the etiology of depression can be divided into internal and external factors. In recent years, researchers have increasingly focused on the impact of external factors on depression. Depression is influenced by environmental factors related to social issues, such as childhood experiences, social interactions, and lifestyles. Adverse childhood experiences are risk factors for depression and anxiety in adolescence ( 37 ) and are a common pathway to depression in adults ( 38 ). Poor interpersonal relationships with classmates, family, teachers, and friends increase the prevalence of depression in adolescents ( 39 ). Related studies assessed three important, specific indicators of the self-esteem domain: social confidence, academic ability, and appearance ( 40 ). The results suggest that these three dimensions of self-esteem are key risk factors for increased depressive symptoms in Chinese adolescents. The vulnerability model ( 41 ) suggests that low self-esteem is a causal risk factor for depression, and low self-esteem is thought to be one of the main causes of the onset and progression of depression, with individuals who exhibit low self-esteem being more likely to develop social anxiety and social withdrawal, and thus having a sense of isolation ( 42 ), which in turn leads to subsequent depression. Loneliness predicts depression in adolescents. Individuals with high levels of loneliness experience more stress and tension from psychological and physical sources in their daily lives, which, combined with insufficient care from society, can lead to depression ( 43 ). A mechanism of association exists between life events and mood disorders, with negative life events being directly associated with depressive symptoms ( 44 ). In a cross-sectional study conducted in Shanghai, the prevalence of depression was higher among people who worked longer hours, and daily lifestyle greatly influenced the prevalence of depression ( 45 ). A number of studies in recent years have presented a number of interesting ideas, and they suggest that depression is related to different environmental factors, such as temperature, sunlight hours, and air pollution. Environmental factors have been associated with suicidal behavior. Traffic noise is a variable that triggers depression and is associated with personality disorders such as depression ( 46 ). The harmful effects of air pollution on mental health, inhalation of air pollutants can trigger neuroinflammation and oxidative stress and induce dopaminergic neurotoxicity. A study showed that depression was associated with an increase in ambient fine particulate matter (PM2.5) ( 47 ).
Increased inflammation is a feature of many diseases and even systemic disorders, such as some autoimmune diseases [e.g., type 1 diabetes ( 48 ) or rheumatoid arthritis ( 49 )] and infectious diseases [e.g., hepatitis and sepsis ( 50 )], are associated with an inflammatory response and have been found to increase the risk of depression. A growing body of evidence supports a bidirectional association between depression and inflammatory processes, with stressors and pathogens leading to excessive or prolonged inflammatory responses when combined with predisposing factors (e.g., childhood adversity and modifying factors such as obesity). The resulting illnesses (e.g., pain, sleep disorders), depressive symptoms, and negative health (e.g., poor diet, sedentary lifestyle) may act as mediating pathways leading to inflammation and depression. In terms of mechanistic pathways, cytokines induce depression by affecting different mood-related processes. Elevated inflammatory signals can dysregulate the metabolism of neurotransmitters, damaging neurons, and thus altering neural activity in the brain. In addition cytokines can modulate depression by regulating hormone levels. Inflammation can have different effects on different populations depending on individual physiology, and even lower levels of inflammation may have a depressive effect on vulnerable individuals. This may be due to lower parasympathetic activity, poorer sensitivity to glucocorticoid inhibitory feedback, a greater response to social threat in the anterior oral cortex or amygdala and a smaller hippocampus. Indeed, these are all factors associated with major depression that can affect the sensitivity to the inhibitory consequences of inflammatory stimuli.
Depression triggers many somatization symptoms, which can manifest as insomnia, menopausal syndrome, cardiovascular problems, pain, and other somatic symptoms. There is a link between sleep deprivation and depression, with insomnia being a trigger and maintenance of depression, and more severe insomnia and chronic symptoms predicting more severe depression. Major depression is considered to be an independent risk factor for the development of coronary heart disease and a predictor of cardiovascular events ( 51 ). Patients with depression are extremely sensitive to pain and have increased pain perception ( 52 ) and is associated with an increased risk of suicide ( 53 , 54 ), and generally the symptoms of these pains are not relieved by medication.
Studies have shown that depression triggers an inflammatory response, promoting an increase in cytokines in response to stressors vs. pathogens. For example, mild depressive symptoms have been associated with an amplified and prolonged inflammatory response ( 55 , 56 ) following influenza vaccination in older adults and pregnant women. Among women who have recently given birth, those with a lifetime history of major depression have greater increases in both serum IL-6 and soluble IL-6 receptors after delivery than women without a history of depression ( 57 ). Pro-inflammatory agents, such as interferon-alpha (IFN-alpha), for specific somatization disorders [e.g., hepatitis C or malignant melanoma ( 58 , 59 )], although effective for somatic disorders, pro-inflammatory therapy often leads to psychiatric side effects. Up to 80% of patients treated with IFN-α have been reported to suffer from mild to moderate depressive symptoms.
Clinical trials have shown better antidepressant treatment with anti-inflammatory drugs compared to placebo, either as monotherapy ( 60 , 61 ) or as an add-on treatment ( 62 – 65 ) to antidepressants ( 66 , 67 ). However, findings like whether NSAIDs can be safely used in combination with antidepressants are controversial. Patients with depression often suffer from somatic co-morbidities, which must be included in the benefit/risk assessment. It is important to consider the type of medication, duration of treatment, and dose, and always balance the potential treatment effect with the risk of adverse events in individual patients. Depression, childhood adversity, stressors, and diet all affect the gut microbiota and promote gut permeability, another pathway that enhances the inflammatory response, and effective depression treatment may have profound effects on mood, inflammation, and health. Early in life gut flora colonization is associated with hypothalamic-pituitary-adrenal (HPA) axis activation and affects the enteric nervous system, which is associated with the risk of major depression, gut flora dysbiosis leads to the onset of TLR4-mediated inflammatory responses, and pro-inflammatory factors are closely associated with depression. Clinical studies have shown that in the gut flora of depressed patients, pro-inflammatory bacteria such as Enterobacteriaceae and Desulfovibrio are enriched, while short-chain fatty acid producing bacteria are reduced, and some of these bacterial taxa may transmit peripheral inflammation into the brain via the brain-gut axis ( 68 ). In addition, gut flora can affect the immune system by modulating neurotransmitters (5-hydroxytryptamine, gamma-aminobutyric acid, norepinephrine, etc.), which in turn can influence the development of depression ( 69 ). Therefore, antidepressant drugs targeting gut flora are a future research direction, and diet can have a significant impact on mood by regulating gut flora.
As the molecular basis of clinical depression remains unclear, and treatments and therapeutic effects are limited and associated with side effects, researchers have worked to discover new treatment modalities for depression. High-amplitude low-frequency musical impulse stimulation as an additional treatment modality seems to produce beneficial effects ( 70 ). Studies have found electroconvulsive therapy to be one of the most effective antidepressant treatment therapies ( 71 ). Physical exercise can promote molecular changes that lead to a shift from a chronic pro-inflammatory to an anti-inflammatory state in the peripheral and central nervous system ( 72 ). Aromatherapy is widely used in the treatment of central nervous system disorders ( 73 ). By activating the parasympathetic nervous system, qigong can be effective in reducing depression ( 74 ). The exploration of these new treatment modalities provides more reference options for the treatment of depression.
Large-scale assessments of depression have found that the probability of developing depression varies across populations. Depression affects some specific populations more significantly, for example: adolescents, mothers, and older adults. Depression is one of the disorders that predispose to adolescence, and depression is associated with an increased risk of suicide among college students ( 75 ). Many women develop depression after childbirth. Depression that develops after childbirth is one of the most common complications for women in the postpartum period ( 76 ). The health of children born to mothers who suffer from postpartum depression can also be adversely affected ( 77 ). Depression can cause many symptoms within the central nervous system, especially in the elderly population ( 78 ).
Furthermore, one of the most consistent findings of the association between inflammation and depression is the elevated levels of peripheral pro-inflammatory markers in depressed individuals, and peripheral pro-inflammatory marker levels can also be used as a basis for the assessment of depressed patients. Studies have shown that the following pro-inflammatory markers have been found to be at increased levels in depressed individuals: CRP ( 79 , 80 ), IL-6 ( 22 , 79 , 81 , 82 ), TNF–α, and interleukin-1 receptor antagonist (IL-1ra) ( 79 , 82 ), however, this association is not unidirectional and the subsequent development of depression also increases pro-inflammatory markers ( 82 , 83 ). These biomarkers are of great interest, and depressed patients with increased inflammatory markers may represent a relatively drug-resistant population.
Frontier Analysis
The exploration and analysis of frontier areas of depression were based on the results of the analysis of the previous section on keywords. According to the evaluation index and analysis idea of this study, the frontier research topics need to have the following four characteristics: low to medium frequency, strong burst, high betweenness centrality, and the research direction in recent years. Therefore, combining the results of keyword analysis and these characteristics, it can be found that the frontier research on depression also becomes clear.
Research on Depression Characterized by Psychosexual Disorders
Exploration of biological mechanisms based on depression-associated neurological disorders and analysis of depression from a neurological perspective have always been the focus of research. Activation of neuroinflammatory pathways may contribute to the development of depression ( 84 ). A research model based on the microbial-gut-brain axis facilitates the neurobiology of depression ( 85 ). Some probiotics positively affect the central nervous system due to modulation of neuroinflammation and thus may be able to modulate depression ( 86 ). The combination of environmental issues and the neurobiological study of depression opens new research directions ( 46 ).
Research on Relevant Models of Depression
How to develop a model that meets the purpose of the study determines the outcome of the study and has become the direction that researchers have been exploring in recent years. Martínez et al. ( 87 ) developed a predictive model to assess factors that modify the treatment pathway for postpartum depression. Nie et al. ( 88 ) extended the work on predictive modeling of treatment-resistant depression to establish a predictive model for treatment-resistant depression. Rational modeling methods and behavioral testing facilitate a more comprehensive exploration of depression, with richer studies and more scientifically valid findings.
Research and Characterization of the Depressed Patient Population
Current research on special groups and depression has received much attention. In a study of a group of children, 4% were found to suffer from depression ( 89 ). The diagnosis and treatment of mental health disorders is an important component of pediatric care. Second, some studies of populations with distinct characteristics have been based primarily on female populations. Maternal perinatal depression is also a common mental disorder with a prevalence of over 10% ( 90 ). In addition, geriatric depression is a chronic and specific disorder ( 91 ). Studies based on these populations highlight the characteristics of the disorder more directly than large-scale population explorations and are useful for conducting extended explorations from specific to generalized.
Somatic Comorbidities Associated With Depression
Depression often accompanies the onset and development of many other disorders, making the study of physical comorbidities associated with depression a new landing place for depression research. Depression is a complication of many neurological or psychopathological disorders. Depression is a common co-morbidity of glioblastoma multiforme ( 92 ). Depression is an important disorder associated with stroke ( 93 ). Chronic liver disease is associated with depression ( 94 ). The link between depressive and anxiety states and cancer has been well-documented ( 95 ). In conclusion, depression is associated with an increased risk of lung, oral, prostate, and skin cancers, an increased risk of cancer-specific death from lung, bladder, breast, colorectal, hematopoietic system, kidney, and prostate cancers, and an increased risk of all-cause mortality in lung cancer patients. The early detection and effective intervention of depression and its complications has public health and clinical implications.
Research on Mechanisms of Depression
Research based on the mechanisms of depression includes the study of disease pathogenesis, the study of drug action mechanisms, and the study of disease treatment mechanisms. Research on the pathogenesis of depression has focused more on the study of the hypothalamic-pituitary-adrenal axis. Social pressure can change the hypothalamic-pituitary-adrenal axis ( 96 ). Studies on the mechanism of action of drugs are mostly based on their effects on the central nervous system. The antidepressant effects of Tanshinone IIA are mediated by the ERK-CREB-BDNF pathway in the hippocampus of mice ( 97 ). Research on the mechanisms of depression treatment has also centered on the central nervous system. It has been shown that the vagus nerve can transmit signals to the brain that can lead to a reduction in depressive behavior ( 98 ).
In this study, based on the 2004–2019 time period, this wealth of data is effectively integrated through data analysis and processing to reproduce the research process in a particular field and to co-present global trends in homogenous fields while organizing past research.
Journals that have made outstanding contributions in this field include ARCH GEN PSYCHIAT, J AFFECT DISORDERS and AM J PSYCHIAT. PSYCHIATRY, NEUROSCIENCES & NEUROLOGY and CLINICAL NEUROLOGY are the three most popular categories. The three researchers with the highest number of articles were MAURIZIO FAVA (USA), BRENDA W. J. H. PENNINX (NETHERLANDS) and MADHUKAR H TRIVEDI (USA). Univ Pittsburgh (USA), Kings Coll London (UK) and Harvard Univ (USA) are three of the most productive and influential research institutions. A Meta-Analysis of Cytokines in Major Depression, Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: Implications for clinical practice and Deep brain stimulation for treatment-resistant depression are key articles. Through keyword analysis, a distribution network centered on depression was formed. Although there are good trends in the research on depression, there are still many directions to be explored in depth. Some recommendations regarding depression are as follows.
(1) The prevention of depression can be considered by focusing on treating external factors and guiding the individual.
Faced with the rising incidence of depression worldwide and the difficulty of treating depression, researchers can think more about how to prevent the occurrence of depression. Depressed moods are often the result of stress, not only social pressures on the individual, but also environmental pressures in the developmental process, which in turn have an unhealthy relationship with the body and increase the likelihood of depression. The correlation between external factors and depression is less well-studied, but the control of external factors may be more effective in the short term than in the long term, and may be guided by self-adjustment to avoid major depressive disorder.
(2) The measurement and evaluation of the degree of depression should be developed in the direction of precision.
In the course of research, it has been found that the Depression Rating Scale is mostly used for the detection and evaluation of depression. This kind of assessment is more objective, but it still lacks accuracy, and the research on measurement techniques and methods is less, which is still at a low stage. Patients with depression usually have a variety of causes, conditions, and duration of illness that determine the degree of depression. Therefore, whether these scales can truly accurately measure depression in depressed patients needs further consideration. Accurate measurement is an important basis for evidence-based treatment of depression, and thus how to achieve accurate measurement of depression is a research direction that researchers can move toward.
Therefore, there is an urgent need for further research to address these issues.
A systematic analysis of research in the field of depression in this study concludes that the distribution of countries, journals, categories, authors, institutions, and citations may help researchers and research institutions to establish closer collaboration, develop appropriate publication plans, grasp research hotspots, identify valuable research ideas, understand current emerging research, and determine research directions. In addition, there are still some limitations that can be overcome in future work. First, due to the lack of author and address information in older published articles, it may not be possible to accurately calculate their collaboration; second, although the data scope of this paper is limited to the Web of Science, it can adequately meet our objectives.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
HW conceived and designed the analysis, collected the data, performed the analysis, and wrote the paper. XT, XW, and YW conceived and designed the analysis. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China under Grant No. 81973495.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. (2009) 10:434–45. doi: 10.1038/nrn2639
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. (2013) 34:119–38. doi: 10.1146/annurev-publhealth-031912-114409
3. Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. (2007) 370:851–8. doi: 10.1016/S0140-6736(07)61415-9
4. Peter Heutink MR. The genetics of MDD – a review of challenges and opportunities. J Depress Anxiety. (2014) 3:150. doi: 10.4172/2167-1044.1000150
CrossRef Full Text | Google Scholar
5. Melchior M, Caspi A, Milne BJ, Danese A, Poulton R, Moffitt TE. Work stress precipitates depression and anxiety in young, working women and men. Psychol Med. (2007) 37:1119–29. doi: 10.1017/S0033291707000414
6. Fusar-Poli P, Solmi M, Brondino N, Davies C, Chae C, Politi P, et al. Transdiagnostic psychiatry: a systematic review. World Psychiatry. (2019) 18:192–207. doi: 10.1002/wps.20631
7. Hammarström A, Lehti A, Danielsson U, Bengs C, Johansson EE. Gender-related explanatory models of depression: a critical evaluation of medical articles. Public Health. (2009) 123:689–93. doi: 10.1016/j.puhe.2009.09.010
8. Tran BX, Ho RCM, Ho CSH, Latkin CA, Phan HT, Ha GH, et al. Depression among patients with HIV/AIDS: research development and effective interventions (gapresearch). Int J Environ Res Public Health. (2019) 16:1772. doi: 10.3390/ijerph16101772
9. Wang XQ, Peng MS, Weng LM, Zheng YL, Zhang ZJ, Chen PJ. Bibliometric study of the comorbidity of pain and depression research. Neural Plast. (2019) 2019:1657498. doi: 10.1155/2019/1657498
10. Shi S, Gao Y, Sun Y, Liu M, Shao L, Zhang J, et al. The top-100 cited articles on biomarkers in the depression field: a bibliometric analysis. Psychol Heal Med. (2020) 26:533–42. doi: 10.1080/13548506.2020.1752924
11. Dongping G, Ami D, Ranran D, Yuan Y, Xiaobei S, Xiaoyao W, et al. A study of the relationship between depression and intestinal flora based on bibliometrics. China Med Her. (2017) 14:173–6.
12. Chunping A, Haiyan W, Nina H, Pinghui H. Bibiometrics analysis of acupuncture for treating depression based on GoPubMed. J Clin Acupunct Moxibustion. (2017) 33:54–7.
13. Yi Y, Xiaoli W. Bibiometrics analysis of acupuncture for treating depression based on GoPubMed. Mod Chinese Med. (2012) 14:35–8. doi: 10.13313/j.issn.1673-4890.2012.09.013
CrossRef Full Text
14. Zhou X, Yan F. Analysis on scientific and technological achievements in the field of depression during 1999-2017. J Prev Med Inf. (2019) 35:777–82.
15. Guaijuan W. Bibliometric analysis of literatures of psoriasis and depression based on GoPubmed. J Dermatol Venereol. (2017) 39:391–4.
16. Yunzhi C, Jie G, Yihui C, Chen G, Chen W, Wang H, et al. A Bibliometric analysis on research of vitamin D deficiency and depression caused. J Guiyang Coll Tradit Chinese Med. (2016) 38:32–5.
17. Shaoni L, Shumin R, Chunhui Z, Yongxiao T, Qizheng Z. Bibliometric analysis of depression-related genes. Chinese J Med Libr Inf Sci. (2009) 18:75–8.
18. Chen C. CiteSpace II: detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol. (2014) 57:359–77. doi: 10.1002/asi.20317
19. Elgendi M. Scientists need data visualization training. Nat Biotechnol. (2017) 35:990–1. doi: 10.1038/nbt.3986
20. World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates (2017).
Google Scholar
21. World Health Organization. Human Development Report 2020 (2020).
22. Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, et al. A meta-analysis of cytokines in major depression. Biol Psychiatry. (2010) 67:446–57. doi: 10.1016/j.biopsych.2009.09.033
23. Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR * D: implications for clinical practice. Am J Psychiatry. (2006) 163:28–40. doi: 10.1176/appi.ajp.163.1.28
24. Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, et al. Deep brain stimulation for treatment-resistant depression. Neuron. (2005) 45:651–60. doi: 10.1016/j.neuron.2005.02.014
25. Zarate CA, Jr., Singh JB, Carlson PJ, Brutsche NE, Ameli R, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry . (2006) 67:793–802. doi: 10.1001/archgenpsychiatry.2010.90
26. Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature. (2008) 455:894–902. doi: 10.1038/nature07455
27. Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. (2009) 114:163–73. doi: 10.1016/j.jad.2008.06.026
28. Pezawas L, Meyer-Lindenberg A, Drabant EM, Verchinski BA, Munoz KE, Kolachana BS, et al. 5-HTTLPR polymorphism impacts human cingulate-amygdala interactions: a genetic susceptibility mechanism for depression. Nat Neurosci. (2005) 8:828–34. doi: 10.1038/nn1463
29. Greicius MD, Flores BH, Menon V, Glover GH, Solvason HB, Kenna H, et al. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol Psychiatry. (2007) 62:429–37. doi: 10.1016/j.biopsych.2006.09.020
30. Tsankova NM, Berton O, Renthal W, Kumar A, Neve RL, Nestler EJ. Sustained hippocampal chromatin regulation in a mouse model of depression and antidepressant action. Nat Neurosci. (2006) 9:519–25. doi: 10.1038/nn1659
31. Kroenke K, Spitzer RL, Williams JBW, Löwe B. An Ultra-Brief Screening Scale for anxiety and depression: the PHQ−4. Psychosomatics. (2009) 50:613–21. doi: 10.1016/s0033-3182(09)70864-3
32. March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents with Depression Study (TADS) randomized controlled trial. J Pediatr. (2005) 146:145. doi: 10.1016/j.jpeds.2004.10.032
33. Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder. Arch Gen Psychiatry. (2005) 62:1097. doi: 10.1001/archpsyc.62.10.1097
34. Gotlib IH, Joormann J. Cognition and depression: current status and future directions. Annu Rev Clin Psychol. (2010) 6:285–312. doi: 10.1146/annurev.clinpsy.121208.131305
35. Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. (2004) 26:289–95. doi: 10.1016/j.genhosppsych.2004.02.006
36. Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. (2011) 12:160–74. doi: 10.1016/S1470-2045(11)70002-X
37. Wang D, Jiang Q, Yang Z, Choi JK. The longitudinal influences of adverse childhood experiences and positive childhood experiences at family, school, and neighborhood on adolescent depression and anxiety. J Affect Disord. (2021) 292:542–51. doi: 10.1016/j.jad.2021.05.108
38. LeMasters K, Bates LM, Chung EO, Gallis JA, Hagaman A, Scherer E, et al. Adverse childhood experiences and depression among women in rural Pakistan. BMC Public Health. (2021) 21:400. doi: 10.1186/s12889-021-10409-4
39. Zhao Y, Zhao Y, Lee YT, Chen L. Cumulative interpersonal relationship risk and resilience models for bullying victimization and depression in adolescents. Pers Individ Dif. (2020) 155:109706. doi: 10.1016/j.paid.2019.109706
40. Zhou J, Li X, Tian L, Huebner ES. Longitudinal association between low self-esteem and depression in early adolescents: the role of rejection sensitivity and loneliness. Psychol Psychother Theor Res Pract. (2020) 93:54–71. doi: 10.1111/papt.12207
41. Butler AC, Hokanson JE, Flynn HA. A comparison of self-esteem lability and low trait self-esteem as vulnerability factors for depression. J Pers Soc Psychol. (1994) 66:166–77. doi: 10.1037/0022-3514.66.1.166
42. Watson J, Nesdale D. Rejection sensitivity, social withdrawal, and loneliness in young adults. J Appl Soc Psychol. (2012) 42:1984–2005. doi: 10.1111/j.1559-1816.2012.00927.x
43. Teo AR, Marsh HE, Forsberg CW, Nicolaidis C, Chen JI, Newsom J, et al. Loneliness is closely associated with depression outcomes and suicidal ideation among military veterans in primary care. J Affect Disord. (2018) 230:42–9. doi: 10.1016/j.jad.2018.01.003
44. Sarubin N, Goerigk S, Padberg F, Übleis A, Jobst A, Erfurt L, et al. Self-esteem fully mediates positive life events and depressive symptoms in a sample of 173 patients with affective disorders. Psychol Psychother Theor Res Pract. (2020) 93:21–35. doi: 10.1111/papt.12205
45. Li Z, Dai J, Wu N, Jia Y, Gao J, Fu H. Effect of long working hours on depression and mental well-being among employees in Shanghai: the role of having leisure hobbies. Int J Environ Res Public Health. (2019) 16:4980. doi: 10.3390/ijerph16244980
46. Díaz J, López-Bueno JA, López-Ossorio JJ, Gónzález JL, Sánchez F, Linares C. Short-term effects of traffic noise on suicides and emergency hospital admissions due to anxiety and depression in Madrid (Spain). Sci Total Environ. (2020) 710:136315. doi: 10.1016/j.scitotenv.2019.136315
47. Fan SJ, Heinrich J, Bloom MS, Zhao TY, Shi TX, Feng WR, et al. Ambient air pollution and depression: a systematic review with meta-analysis up to 2019. Sci Total Environ . (2020) 701:134721. doi: 10.1016/j.scitotenv.2019.134721
48. Korczak DJ, Pereira S, Koulajian K, Matejcek A, Giacca A. Type 1 diabetes mellitus and major depressive disorder: evidence for a biological link. Diabetologia. (2011) 54:2483–93. doi: 10.1007/s00125-011-2240-3
49. Dickens C, McGowan L, Clark-Carter D, Creed F. Depression in rheumatoid arthritis: a systematic review of the literature with meta-analysis. Psychosom Med. (2002) 64:52–60. doi: 10.1097/00006842-200201000-00008
50. Benros ME, Waltoft BL, Nordentoft M, Ostergaard SD, Eaton WW, Krogh J, et al. Autoimmune diseases and severe infections as risk factors for mood disorders a nationwide study. JAMA Psychiatry. (2013) 70:812–20. doi: 10.1001/jamapsychiatry.2013.1111
51. Charlson FJ, Stapelberg NJC, Baxter AJ, Whiteford HA. Should global burden of disease estimates include depression as a risk factor for coronary heart disease? BMC Med. (2011) 9:47. doi: 10.1186/1741-7015-9-47
52. Velly AM, Mohit S. Epidemiology of pain and relation to psychiatric disorders. Prog Neuro Psychopharmacol Biol Psychiatry. (2018) 87:159–67. doi: 10.1016/j.pnpbp.2017.05.012
53. Razali SM, Khalib AQ. Pain symptoms in Malay patients with major depression. Asian J Psychiatr. (2012) 5:297–302. doi: 10.1016/j.ajp.2012.02.015
54. Bahk WM, Park S, Jon DI, Yoon BH, Min KJ, Hong JP. Relationship between painful physical symptoms and severity of depressive symptomatology and suicidality. Psychiatry Res. (2011) 189:357–61. doi: 10.1016/j.psychres.2011.01.009
55. Glaser R, Robles TF, Sheridan J, Malarkey WB, Kiecolt-Glaser JK. Mild depressive symptoms are associated with amplified and prolonged inflammatory responses after influenza virus vaccination in older adults. Arch Gen Psychiatry. (2003) 60:1009–14. doi: 10.1001/archpsyc.60.10.1009
56. Christian LM, Franco A, Iams JD, Sheridan J, Glaser R. Depressive symptoms predict exaggerated inflammatory responses to an in vivo immune challenge among pregnant women. Brain Behav Immun. (2010) 24:49–53. doi: 10.1016/j.bbi.2009.05.055
57. Maes M, Ombelet W, De Jongh R, Kenis G, Bosmans E. The inflammatory response following delivery is amplified in women who previously suffered from major depression, suggesting that major depression is accompanied by a sensitization of the inflammatory response system. J Affect Disord. (2001) 63:85–92. doi: 10.1016/S0165-0327(00)00156-7
58. Friebe A, Horn M, Schmidt F, Janssen G, Schmid-Wendtner MH, Volkenandt M, et al. Dose-dependent development of depressive symptoms during adjuvant interferon-α treatment of patients with malignant melanoma. Psychosomatics . (2010) 51:466–73. doi: 10.1016/s0033-3182(10)70738-6
59. Eggermont AM, Suciu S, Santinami M, Testori A, Kruit WH, Marsden J, et al. Adjuvant therapy with pegylated interferon alfa-2b versus observation alone in resected stage III melanoma: final results of EORTC 18991, a randomised phase III trial. Lancet. (2008) 372:117–26. doi: 10.1016/S0140-6736(08)61033-8
60. Tyring S, Gottlieb A, Papp K, Gordon K, Leonardi C, Wang A, et al. Etanercept and clinical outcomes, fatigue, and depression in psoriasis: double-blind placebo-controlled randomised phase III trial. Lancet. (2006) 367:29–35. doi: 10.1016/S0140-6736(05)67763-X
61. Iyengar RL, Gandhi S, Aneja A, Thorpe K, Razzouk L, Greenberg J, et al. NSAIDs are associated with lower depression scores in patients with osteoarthritis. Am J Med . (2013) 126:1017.e11–8. doi: 10.1016/j.amjmed.2013.02.037
62. Müller N, Schwarz MJ, Dehning S, Douhe A, Cerovecki A, Goldstein-Müller B, et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol Psychiatry. (2006) 11:680–4. doi: 10.1038/sj.mp.4001805
63. Akhondzadeh S, Jafari S, Raisi F, Nasehi AA, Ghoreishi A, Salehi B, et al. Clinical trial of adjunctive celecoxib treatment in patients with major depression: a double blind and placebo controlled trial. Depress Anxiety. (2009) 26:607–11. doi: 10.1002/da.20589
64. Abbasi SH, Hosseini F, Modabbernia A, Ashrafi M, Akhondzadeh S. Effect of celecoxib add-on treatment on symptoms and serum IL-6 concentrations in patients with major depressive disorder: Randomized double-blind placebo-controlled study. J Affect Disord. (2012) 141:308–14. doi: 10.1016/j.jad.2012.03.033
65. Majd M, Hashemian F, Hosseinib SM, Shariatpanahi MV, Sharifid A. A randomized, double-blind, placebo-controlled trial of celecoxib augmentation of sertraline in treatment of drug-naive depressed women: a pilot study. Iran J Pharm Res. (2015) 14:891–9. doi: 10.22037/ijpr.2015.1637
66. Warner-Schmidt JL, Vanover KE, Chen EY, Marshall JJ, Greengard P. Antidepressant effects of selective serotonin reuptake inhibitors (SSRIs) are attenuated by antiinflammatory drugs in mice and humans. Proc Natl Acad Sci USA. (2011) 108:9262–7. doi: 10.1073/pnas.1104836108
67. Uher R, E TK, Tracy D, Wolfgang M, Ole M, Joanna H, et al. An inflammatory biomarker as a differential predictor of outcome of depression treatment with escitalopram and nortriptyline. Am J Psychiatry. (2014) 171:1278–86. doi: 10.1176/appi.ajp.2014.14010094
68. Simpson CA, Diaz-Arteche C, Eliby D, Schwartz OS, Simmons JG, Cowan CSM. The gut microbiota in anxiety and depression – a systematic review. Clin Psychol Rev. (2021) 83:101943. doi: 10.1016/j.cpr.2020.101943
69. Yang Z, Li J, Gui X, Shi X, Bao Z, Han H, et al. Updated review of research on the gut microbiota and their relation to depression in animals and human beings. Mol Psychiatry. (2020) 25:2759–72. doi: 10.1038/s41380-020-0729-1
70. Sigurdardóttir GA, Nielsen PM, Rønager J, Wang AG. A pilot study on high amplitude low frequency–music impulse stimulation as an add-on treatment for depression. Brain Behav. (2019) 9:e01399. doi: 10.1002/brb3.1399
71. Maffioletti E, Gennarelli M, Gainelli G, Bocchio-Chiavetto L, Bortolomasi M, Minelli A. BDNF genotype and baseline serum levels in relation to electroconvulsive therapy effectiveness in treatment-resistant depressed patients. J ECT. (2019) 35:189–94. doi: 10.1097/YCT.0000000000000583
72. Ignácio ZM, da Silva RS, Plissari ME, Quevedo J, Réus GZ. Physical exercise and neuroinflammation in major depressive disorder. Mol Neurobiol. (2019) 56:8323–35. doi: 10.1007/s12035-019-01670-1
73. Lu Z, Zhang T, Wang X, Wang J, Shen J, Xiao Z, et al. Zwitterionic polymer-based nanoparticles encapsulated with linalool for regulating central nervous system. ACS Biomater Sci Eng. (2020) 6:442–9. doi: 10.1021/acsbiomaterials.9b01451
74. Koo JW, Chaudhury D, Han MH, Nestler EJ. Role of mesolimbic brain-derived neurotrophic factor in depression. Biol Psychiatry. (2019) 86:738–48. doi: 10.1016/j.biopsych.2019.05.020
75. Seppälä EM, Bradley C, Moeller J, Harouni L, Nandamudi D, Brackett MA. Promoting mental health and psychological thriving in university students: a randomized controlled trial of three well-being interventions. Front Psychiatry. (2020) 11:590. doi: 10.3389/fpsyt.2020.00590
76. Weissman M, Olfson M. Depression in women: implications for health care research. Science. (1995) 269:799–801. doi: 10.2105/AJPH.2020.305798
77. Savory K, Garay SM, Sumption LA, Kelleher JS, Daughters K, Janssen AB, et al. Prenatal symptoms of anxiety and depression associated with sex differences in both maternal perceptions of one year old infant temperament and researcher observed infant characteristics. J Affect Disord. (2020) 264:383–92. doi: 10.1016/j.jad.2019.11.057
78. Eraydin IE, Mueller C, Corbett A, Ballard C, Brooker H, Wesnes K, et al. Investigating the relationship between age of onset of depressive disorder and cognitive function. Int J Geriatr Psychiatry. (2019) 34:38–46. doi: 10.1002/gps.4979
79. Howren MB, Lamkin DM, Suls J. Associations of depression with c-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. (2009) 71:171–86. doi: 10.1097/PSY.0b013e3181907c1b
80. Wium-Andersen MK, Ørsted DD, Nielsen SF, Nordestgaard BG. Elevated C-reactive protein levels, psychological distress, and depression in 73131 individuals. JAMA Psychiatry. (2013) 70:176–84. doi: 10.1001/2013.jamapsychiatry.102
81. Liu Y, Ho RCM, Mak A. Interleukin (IL)-6, tumour necrosis factor alpha (TNF-α) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: a meta-analysis and meta-regression. J Affect Disord. (2012) 139:230–9. doi: 10.1016/j.jad.2011.08.003
82. Dahl J, Ormstad H, Aass HCD, Malt UF, Bendz LT, Sandvik L, et al. The plasma levels of various cytokines are increased during ongoing depression and are reduced to normal levels after recovery. Psychoneuroendocrinology. (2014) 45:77–86. doi: 10.1016/j.psyneuen.2014.03.019
83. Khandaker GM, Pearson RM, Zammit S, Lewis G, Jones PB. Association of serum interleukin 6 and C-reactive protein in childhood with depression and psychosis in young adult life a population-based longitudinal study. JAMA Psychiatry. (2014) 71:1121–8. doi: 10.1001/jamapsychiatry.2014.1332
84. Zhang Z, xuan, Li E, Yan J, ping, Fu W, Shen P, Tian SW, et al. Apelin attenuates depressive-like behavior and neuroinflammation in rats co-treated with chronic stress and lipopolysaccharide. Neuropeptides. (2019) 77:101959. doi: 10.1016/j.npep.2019.101959
85. Tian P, O'Riordan KJ, Lee Y, kun, Wang G, Zhao J, Zhang H, et al. Towards a psychobiotic therapy for depression: Bifidobacterium breve CCFM1025 reverses chronic stress-induced depressive symptoms and gut microbial abnormalities in mice. Neurobiol Stress. (2020) 12:100216. doi: 10.1016/j.ynstr.2020.100216
86. Paiva IHR, Duarte-Silva E, Peixoto CA. The role of prebiotics in cognition, anxiety, and depression. Eur Neuropsychopharmacol. (2020) 34:1–18. doi: 10.1016/j.euroneuro.2020.03.006
87. Martínez P, Vöhringer PA, Rojas G. Barreiras de acesso a tratamento para mães com depressão pós-parto em centros de atenção primária: Um modelo preditivo. Rev Lat Am Enfermagem. (2016) 24:e2675. doi: 10.1590/1518-8345.0982.2675
88. Nie Z, Vairavan S, Narayan VA, Ye J, Li QS. Predictive modeling of treatment resistant depression using data from STARD and an independent clinical study. PLoS ONE. (2018) 13:e0197268. doi: 10.1371/journal.pone.0197268
89. Elmore AL, Crouch E. The Association of adverse childhood experiences with anxiety and depression for children and youth, 8 to 17 years of age. Acad Pediatr. (2020) 20:600–8. doi: 10.1016/j.acap.2020.02.012
90. Cheng B, Wang X, Zhou Y, Li J, Zhao Y, Xia S, et al. Regional cerebral activity abnormality in pregnant women with antenatal depression. J Affect Disord. (2020) 274:381–8. doi: 10.1016/j.jad.2020.05.107
91. Senel B, Özel-Kizil ET, Sorgun MH, Tezcan-Aydemir S, Kirici S. Transcranial sonography imaging of brainstem raphe, substantia nigra and cerebral ventricles in patients with geriatric depression. Int J Geriatr Psychiatry. (2020) 35:702–11. doi: 10.1002/gps.5287
PubMed Abstract | CrossRef Full Text
92. Mugge L, Mansour TR, Crippen M, Alam Y, Schroeder J. Depression and glioblastoma, complicated concomitant diseases: a systemic review of published literature. Neurosurg Rev. (2020) 43:497–511. doi: 10.1007/s10143-018-1017-2
93. Allida S, Kl C, Cf H, Lang H, House A, Ml H. Pharmacological, psychological, and non-invasive brain stimulation interventions for treating depression after stroke. Cochrane Database Syst Rev. (2020) 1:CD003437. doi: 10.1002/14651858.CD003437.pub4
94. Lee K, Otgonsuren M, Younoszai Z, Mir HM, Younossi ZM. Association of chronic liver disease with depression: a population-based study. Psychosomatics. (2013) 54:52–9. doi: 10.1016/j.psym.2012.09.005
95. Wang YH, Li JQ, Shi JF, Que JY, Liu JJ, Lappin JM, et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry. (2020) 25:1487–99. doi: 10.1038/s41380-019-0595-x
96. Colaianna M, Schiavone S, Zotti M, Tucci P, Morgese MG, Bäckdahl L, et al. Neuroendocrine profile in a rat model of psychosocial stress: relation to oxidative stress. Antioxida Redox Signal. (2013) 18:1385–99. doi: 10.1089/ars.2012.4569
97. Lu J, Zhou H, Meng D, Zhang J, Pan K, Wan B, et al. Tanshinone IIA Improves depression-like behavior in mice by activating the ERK-CREB-BDNF signaling pathway. Neuroscience. (2020) 430:1–11. doi: 10.1016/j.neuroscience.2020.01.026
98. McVey Neufeld KA, Bienenstock J, Bharwani A, Champagne-Jorgensen K, Mao YK, West C, et al. Oral selective serotonin reuptake inhibitors activate vagus nerve dependent gut-brain signalling. Sci Rep. (2019) 9:14290. doi: 10.1038/s41598-019-50807-8
Keywords: depression, major depressive disorder, bibliometrics, visual analysis, knowledge graphs, CiteSpace
Citation: Wang H, Tian X, Wang X and Wang Y (2021) Evolution and Emerging Trends in Depression Research From 2004 to 2019: A Literature Visualization Analysis. Front. Psychiatry 12:705749. doi: 10.3389/fpsyt.2021.705749
Received: 06 May 2021; Accepted: 05 October 2021; Published: 29 October 2021.
Reviewed by:
Copyright © 2021 Wang, Tian, Wang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun Wang, wangyun@bucm.edu.cn
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

IMAGES
VIDEO
COMMENTS
In this paper, we describe and present the vast, fragmented, and complex literature related to this topic. This review may be used to guide practice, public health efforts, policy, and research related to mental health and, specifically, depression. ... This paper discusses key areas in depression research; however, an exhaustive discussion of ...
Our lack of knowledge cannot be put down to a scarcity of research in existing treatments. In the past decades, more than 500 randomised trials have examined the effects of antidepressant medications, and more than 600 trials have examined the effects of psychotherapies for depression (although comparatively few are conducted for early-onset depression).
In line with the Research Domain Criteria Project launched by the National Institute of Mental Health (Insel, 2014; Insel et al., 2010), a distinguished aim in developing an integrated neuroscientific model of depression therefore has to be the separation of distinct aetiological and pathophysiological trajectories which, although eventually ...
The paper gives a complete overview of what is known about therapies for depression. ... we have developed a 'Meta-analytic Research Domain' (MARD) of all randomized trials of psychological treatments of depression. ... Depression in most studies was moderate to severe. Response (50 % improvement between baseline and endpoint) was the main ...
The current speed of progress in depression research is simply remarkable. We have therefore been able to create a second special issue of Molecular Psychiatry, 2020, focused on depression, with ...
Authors of papers were contacted for clarification when data was missing or unclear. ... with most research on depression focusing on the 5-HT 1A receptor [11, 34].
Its severe form, major depression is classified as a mood disorder. Latest Research and Reviews Astrocytic ALKBH5 in stress response contributes to depressive-like behaviors in mice
Abstract. One of the most consistent findings in the depression literature is that stressful life events predict the onset and course of depressive episodes. Cognitive and biological responses to life stressors have both been identified, albeit largely independently, as central to understanding the association between stress and depression.
Abstract. Major depression is a mood disorder characterized by a sense of inadequacy, despondency, decreased activity, pessimism, anhedonia and sadness where these symptoms severely disrupt and ...
In addition, initial presentation with social phobia was associated with a 5.7-fold increased risk of developing major depressive disorder. These associations between anxiety and depression can be traced back even earlier in life. For example, childhood behavioral inhibition in response to novelty or strangers, or an extreme anxious temperament ...
In this second episode of a four-part Double Take video miniseries on depression from the New England Journal of Medicine, Drs. Anderson, Teel, and Scott-Vernaglia discuss available treatments for ...
R. McShaneN Engl J Med 2023;389:1333-1334. Depression can become self-perpetuating as occupational, relationship, and social losses accrue. Sustained remission is achieved in less than half of ...
Analysis of Published Papers. In the past decade, the total number of papers on depression published worldwide has increased year by year as shown in Fig. 1A. Searching the Web of Science database, we found a total of 43,863 papers published in the field of depression from 2009 to 2019 (search strategy: TI = (depression$) or ts = ("major depressive disorder$")) and py = (2009-2019), Articles).
To improve our understanding, some research has been undertaken in which YP themselves are asked about their experience of depression. In a questionnaire study involving adolescents with depression in New Zealand, the researchers identified the aforementioned irritability as the most common characteristic alongside interpersonal problems and ...
Importance Adolescent depression is characterized by diverse symptom trajectories over time and has a strong genetic influence. Research has determined genetic overlap between depression and other psychiatric conditions; investigating the shared genetic architecture of heterogeneous depression trajectories is crucial for understanding disease etiology, prediction, and early intervention.
The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1, 385-401 (1977). ... Calls for Papers Guide to referees ...
Depression is a top mental health concern among undergraduates and has been shown to disproportionately affect individuals who are underserved and underrepresented in science. As we aim to create a more inclusive scientific community, we argue that we need to examine the relationship between depression and scientific research. While studies have identified aspects of research that affect ...
The possible causes of depression are many and not yet well understood. However, it most likely results from an interplay of genetic vulnerability and environmental factors. Your depression research paper could explore one or more of these causes and reference the latest research on the topic. For instance, how does an imbalance in brain ...
Common signs and symptoms of depression include: Persistent sad, anxious, or "empty" mood. Feelings of hopelessness or pessimism. Feelings of irritability, frustration‚ or restlessness. Feelings of guilt, worthlessness, or helplessness. Loss of interest or pleasure in hobbies and activities. Fatigue, lack of energy, or feeling slowed down.
Research paper. The impact of depression-mediated gut microbiota composition on Irritable Bowel Syndrome: A Mendelian study. ... (DSM) and the International Classification of Diseases (ICD). According to the DSM-5 standards, the diagnosis of depression primarily involves experiencing persistent sadness or loss of interest for at least two weeks ...
DOI: 10.4103/indianjpsychiatry.indianjpsychiatry_154_24 Corpus ID: 269944510; Revisiting depression: Nosological challenges in the third millennium @article{Singh2024RevisitingDN, title={Revisiting depression: Nosological challenges in the third millennium}, author={Gurvinder Pal Singh and Sahildeep Kaur and Sharanjot Kaur and Muskan Bansal and Pratiksha Bugalia}, journal={Indian Journal of ...
The immediate effect is not further explained. Research suggests that procrastination creates negative feelings, such as shame, guilt, regret, and anger [20,21,22].The described feelings could have a detrimental effect on mental health [23,24,25].The first mediated pathway leads from trait procrastination to (chronic) disease via (chronic) stress.
The survey, published by Gallup on Wednesday, found 29% of U.S. adults report being diagnosed with depression at some point during their lifetimes, an increase from 19.6% in 2015. Meanwhile, 17.8% ...
Econometric analysis of the relationship between vitamin D deficiency and depression was performed by Yunzhi et al. and Shauni et al. performed a bibliometric analysis of domestic and international research papers on depression-related genes from 2003 to 2007. A previous review of depression-related bibliometric studies revealed that there is ...