- Patient Care & Health Information
- Diseases & Conditions
- Type 2 diabetes
Type 2 diabetes is usually diagnosed using the glycated hemoglobin (A1C) test. This blood test indicates your average blood sugar level for the past two to three months. Results are interpreted as follows:
- Below 5.7% is normal.
- 5.7% to 6.4% is diagnosed as prediabetes.
- 6.5% or higher on two separate tests indicates diabetes.
If the A1C test isn't available, or if you have certain conditions that interfere with an A1C test, your health care provider may use the following tests to diagnose diabetes:
Random blood sugar test. Blood sugar values are expressed in milligrams of sugar per deciliter ( mg/dL ) or millimoles of sugar per liter ( mmol/L ) of blood. Regardless of when you last ate, a level of 200 mg/dL (11.1 mmol/L ) or higher suggests diabetes, especially if you also have symptoms of diabetes, such as frequent urination and extreme thirst.
Fasting blood sugar test. A blood sample is taken after you haven't eaten overnight. Results are interpreted as follows:
- Less than 100 mg/dL (5.6 mmol/L ) is considered healthy.
- 100 to 125 mg/dL (5.6 to 6.9 mmol/L ) is diagnosed as prediabetes.
- 126 mg/dL (7 mmol/L ) or higher on two separate tests is diagnosed as diabetes.
Oral glucose tolerance test. This test is less commonly used than the others, except during pregnancy. You'll need to not eat for a certain amount of time and then drink a sugary liquid at your health care provider's office. Blood sugar levels then are tested periodically for two hours. Results are interpreted as follows:
- Less than 140 mg/dL (7.8 mmol/L ) after two hours is considered healthy.
- 140 to 199 mg/dL (7.8 mmol/L and 11.0 mmol/L ) is diagnosed as prediabetes.
- 200 mg/dL (11.1 mmol/L ) or higher after two hours suggests diabetes.
Screening. The American Diabetes Association recommends routine screening with diagnostic tests for type 2 diabetes in all adults age 35 or older and in the following groups:
- People younger than 35 who are overweight or obese and have one or more risk factors associated with diabetes.
- Women who have had gestational diabetes.
- People who have been diagnosed with prediabetes.
- Children who are overweight or obese and who have a family history of type 2 diabetes or other risk factors.

After a diagnosis
If you're diagnosed with diabetes, your health care provider may do other tests to distinguish between type 1 and type 2 diabetes because the two conditions often require different treatments.
Your health care provider will test A1C levels at least two times a year and when there are any changes in treatment. Target A1C goals vary depending on age and other factors. For most people, the American Diabetes Association recommends an A1C level below 7%.
You also receive tests to screen for complications of diabetes and other medical conditions.
More Information
- Glucose tolerance test
Management of type 2 diabetes includes:
- Healthy eating.
- Regular exercise.
- Weight loss.
- Possibly, diabetes medication or insulin therapy.
- Blood sugar monitoring.
These steps make it more likely that blood sugar will stay in a healthy range. And they may help to delay or prevent complications.
Healthy eating
There's no specific diabetes diet. However, it's important to center your diet around:
- A regular schedule for meals and healthy snacks.
- Smaller portion sizes.
- More high-fiber foods, such as fruits, nonstarchy vegetables and whole grains.
- Fewer refined grains, starchy vegetables and sweets.
- Modest servings of low-fat dairy, low-fat meats and fish.
- Healthy cooking oils, such as olive oil or canola oil.
- Fewer calories.
Your health care provider may recommend seeing a registered dietitian, who can help you:
- Identify healthy food choices.
- Plan well-balanced, nutritional meals.
- Develop new habits and address barriers to changing habits.
- Monitor carbohydrate intake to keep your blood sugar levels more stable.
Physical activity
Exercise is important for losing weight or maintaining a healthy weight. It also helps with managing blood sugar. Talk to your health care provider before starting or changing your exercise program to ensure that activities are safe for you.
- Aerobic exercise. Choose an aerobic exercise that you enjoy, such as walking, swimming, biking or running. Adults should aim for 30 minutes or more of moderate aerobic exercise on most days of the week, or at least 150 minutes a week.
- Resistance exercise. Resistance exercise increases your strength, balance and ability to perform activities of daily living more easily. Resistance training includes weightlifting, yoga and calisthenics. Adults living with type 2 diabetes should aim for 2 to 3 sessions of resistance exercise each week.
- Limit inactivity. Breaking up long periods of inactivity, such as sitting at the computer, can help control blood sugar levels. Take a few minutes to stand, walk around or do some light activity every 30 minutes.
Weight loss
Weight loss results in better control of blood sugar levels, cholesterol, triglycerides and blood pressure. If you're overweight, you may begin to see improvements in these factors after losing as little as 5% of your body weight. However, the more weight you lose, the greater the benefit to your health. In some cases, losing up to 15% of body weight may be recommended.
Your health care provider or dietitian can help you set appropriate weight-loss goals and encourage lifestyle changes to help you achieve them.
Monitoring your blood sugar
Your health care provider will advise you on how often to check your blood sugar level to make sure you remain within your target range. You may, for example, need to check it once a day and before or after exercise. If you take insulin, you may need to check your blood sugar multiple times a day.
Monitoring is usually done with a small, at-home device called a blood glucose meter, which measures the amount of sugar in a drop of blood. Keep a record of your measurements to share with your health care team.
Continuous glucose monitoring is an electronic system that records glucose levels every few minutes from a sensor placed under the skin. Information can be transmitted to a mobile device such as a phone, and the system can send alerts when levels are too high or too low.
Diabetes medications
If you can't maintain your target blood sugar level with diet and exercise, your health care provider may prescribe diabetes medications that help lower glucose levels, or your provider may suggest insulin therapy. Medicines for type 2 diabetes include the following.
Metformin (Fortamet, Glumetza, others) is generally the first medicine prescribed for type 2 diabetes. It works mainly by lowering glucose production in the liver and improving the body's sensitivity to insulin so it uses insulin more effectively.
Some people experience B-12 deficiency and may need to take supplements. Other possible side effects, which may improve over time, include:
- Abdominal pain.
Sulfonylureas help the body secrete more insulin. Examples include glyburide (DiaBeta, Glynase), glipizide (Glucotrol XL) and glimepiride (Amaryl). Possible side effects include:
- Low blood sugar.
- Weight gain.
Glinides stimulate the pancreas to secrete more insulin. They're faster acting than sulfonylureas. But their effect in the body is shorter. Examples include repaglinide and nateglinide. Possible side effects include:
Thiazolidinediones make the body's tissues more sensitive to insulin. An example of this medicine is pioglitazone (Actos). Possible side effects include:
- Risk of congestive heart failure.
- Risk of bladder cancer (pioglitazone).
- Risk of bone fractures.
DPP-4 inhibitors help reduce blood sugar levels but tend to have a very modest effect. Examples include sitagliptin (Januvia), saxagliptin (Onglyza) and linagliptin (Tradjenta). Possible side effects include:
- Risk of pancreatitis.
- Joint pain.
GLP-1 receptor agonists are injectable medications that slow digestion and help lower blood sugar levels. Their use is often associated with weight loss, and some may reduce the risk of heart attack and stroke. Examples include exenatide (Byetta, Bydureon Bcise), liraglutide (Saxenda, Victoza) and semaglutide (Rybelsus, Ozempic, Wegovy). Possible side effects include:
SGLT2 inhibitors affect the blood-filtering functions in the kidneys by blocking the return of glucose to the bloodstream. As a result, glucose is removed in the urine. These medicines may reduce the risk of heart attack and stroke in people with a high risk of those conditions. Examples include canagliflozin (Invokana), dapagliflozin (Farxiga) and empagliflozin (Jardiance). Possible side effects include:
- Vaginal yeast infections.
- Urinary tract infections.
- Low blood pressure.
- High cholesterol.
- Risk of gangrene.
- Risk of bone fractures (canagliflozin).
- Risk of amputation (canagliflozin).
Other medicines your health care provider might prescribe in addition to diabetes medications include blood pressure and cholesterol-lowering medicines, as well as low-dose aspirin, to help prevent heart and blood vessel disease.
Insulin therapy
Some people who have type 2 diabetes need insulin therapy. In the past, insulin therapy was used as a last resort, but today it may be prescribed sooner if blood sugar targets aren't met with lifestyle changes and other medicines.
Different types of insulin vary on how quickly they begin to work and how long they have an effect. Long-acting insulin, for example, is designed to work overnight or throughout the day to keep blood sugar levels stable. Short-acting insulin generally is used at mealtime.
Your health care provider will determine what type of insulin is right for you and when you should take it. Your insulin type, dosage and schedule may change depending on how stable your blood sugar levels are. Most types of insulin are taken by injection.
Side effects of insulin include the risk of low blood sugar — a condition called hypoglycemia — diabetic ketoacidosis and high triglycerides.
Weight-loss surgery
Weight-loss surgery changes the shape and function of the digestive system. This surgery may help you lose weight and manage type 2 diabetes and other conditions related to obesity. There are several surgical procedures. All of them help people lose weight by limiting how much food they can eat. Some procedures also limit the amount of nutrients the body can absorb.
Weight-loss surgery is only one part of an overall treatment plan. Treatment also includes diet and nutritional supplement guidelines, exercise and mental health care.
Generally, weight-loss surgery may be an option for adults living with type 2 diabetes who have a body mass index (BMI) of 35 or higher. BMI is a formula that uses weight and height to estimate body fat. Depending on the severity of diabetes or the presence of other medical conditions, surgery may be an option for someone with a BMI lower than 35.
Weight-loss surgery requires a lifelong commitment to lifestyle changes. Long-term side effects may include nutritional deficiencies and osteoporosis.
People living with type 2 diabetes often need to change their treatment plan during pregnancy and follow a diet that controls carbohydrates. Many people need insulin therapy during pregnancy. They also may need to stop other treatments, such as blood pressure medicines.
There is an increased risk during pregnancy of developing a condition that affects the eyes called diabetic retinopathy. In some cases, this condition may get worse during pregnancy. If you are pregnant, visit an ophthalmologist during each trimester of your pregnancy and one year after you give birth. Or as often as your health care provider suggests.
Signs of trouble
Regularly monitoring your blood sugar levels is important to avoid severe complications. Also, be aware of symptoms that may suggest irregular blood sugar levels and the need for immediate care:
High blood sugar. This condition also is called hyperglycemia. Eating certain foods or too much food, being sick, or not taking medications at the right time can cause high blood sugar. Symptoms include:
- Frequent urination.
- Increased thirst.
- Blurred vision.
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS). This life-threatening condition includes a blood sugar reading higher than 600 mg/dL (33.3 mmol/L ). HHNS may be more likely if you have an infection, are not taking medicines as prescribed, or take certain steroids or drugs that cause frequent urination. Symptoms include:
- Extreme thirst.
- Drowsiness.
- Dark urine.
Diabetic ketoacidosis. Diabetic ketoacidosis occurs when a lack of insulin results in the body breaking down fat for fuel rather than sugar. This results in a buildup of acids called ketones in the bloodstream. Triggers of diabetic ketoacidosis include certain illnesses, pregnancy, trauma and medicines — including the diabetes medicines called SGLT2 inhibitors.
The toxicity of the acids made by diabetic ketoacidosis can be life-threatening. In addition to the symptoms of hyperglycemia, such as frequent urination and increased thirst, ketoacidosis may cause:
- Shortness of breath.
- Fruity-smelling breath.
Low blood sugar. If your blood sugar level drops below your target range, it's known as low blood sugar. This condition also is called hypoglycemia. Your blood sugar level can drop for many reasons, including skipping a meal, unintentionally taking more medication than usual or being more physically active than usual. Symptoms include:
- Irritability.
- Heart palpitations.
- Slurred speech.
If you have symptoms of low blood sugar, drink or eat something that will quickly raise your blood sugar level. Examples include fruit juice, glucose tablets, hard candy or another source of sugar. Retest your blood in 15 minutes. If levels are not at your target, eat or drink another source of sugar. Eat a meal after your blood sugar level returns to normal.
If you lose consciousness, you need to be given an emergency injection of glucagon, a hormone that stimulates the release of sugar into the blood.
- Medications for type 2 diabetes
- GLP-1 agonists: Diabetes drugs and weight loss
- Bariatric surgery
- Endoscopic sleeve gastroplasty
- Gastric bypass (Roux-en-Y)
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Careful management of type 2 diabetes can reduce the risk of serious — even life-threatening — complications. Consider these tips:
- Commit to managing your diabetes. Learn all you can about type 2 diabetes. Make healthy eating and physical activity part of your daily routine.
- Work with your team. Establish a relationship with a certified diabetes education specialist, and ask your diabetes treatment team for help when you need it.
- Identify yourself. Wear a necklace or bracelet that says you are living with diabetes, especially if you take insulin or other blood sugar-lowering medicine.
- Schedule a yearly physical exam and regular eye exams. Your diabetes checkups aren't meant to replace regular physicals or routine eye exams.
- Keep your vaccinations up to date. High blood sugar can weaken your immune system. Get a flu shot every year. Your health care provider also may recommend the pneumonia vaccine. The Centers for Disease Control and Prevention (CDC) also recommends the hepatitis B vaccination if you haven't previously received this vaccine and you're 19 to 59 years old. Talk to your health care provider about other vaccinations you may need.
- Take care of your teeth. Diabetes may leave you prone to more-serious gum infections. Brush and floss your teeth regularly and schedule recommended dental exams. Contact your dentist right away if your gums bleed or look red or swollen.
- Pay attention to your feet. Wash your feet daily in lukewarm water, dry them gently, especially between the toes, and moisturize them with lotion. Check your feet every day for blisters, cuts, sores, redness and swelling. Contact your health care provider if you have a sore or other foot problem that isn't healing.
- Keep your blood pressure and cholesterol under control. Eating healthy foods and exercising regularly can go a long way toward controlling high blood pressure and cholesterol. Take medication as prescribed.
- If you smoke or use other types of tobacco, ask your health care provider to help you quit. Smoking increases your risk of diabetes complications. Talk to your health care provider about ways to stop using tobacco.
- Use alcohol sparingly. Depending on the type of drink, alcohol may lower or raise blood sugar levels. If you choose to drink alcohol, only do so with a meal. The recommendation is no more than one drink daily for women and no more than two drinks daily for men. Check your blood sugar frequently after drinking alcohol.
- Make healthy sleep a priority. Many people with type 2 diabetes have sleep problems. And not getting enough sleep may make it harder to keep blood sugar levels in a healthy range. If you have trouble sleeping, talk to your health care provider about treatment options.
- Caffeine: Does it affect blood sugar?
Alternative medicine
Many alternative medicine treatments claim to help people living with diabetes. According to the National Center for Complementary and Integrative Health, studies haven't provided enough evidence to recommend any alternative therapies for blood sugar management. Research has shown the following results about popular supplements for type 2 diabetes:
- Chromium supplements have been shown to have few or no benefits. Large doses can result in kidney damage, muscle problems and skin reactions.
- Magnesium supplements have shown benefits for blood sugar control in some but not all studies. Side effects include diarrhea and cramping. Very large doses — more than 5,000 mg a day — can be fatal.
- Cinnamon, in some studies, has lowered fasting glucose levels but not A1C levels. Therefore, there's no evidence of overall improved glucose management.
Talk to your health care provider before starting a dietary supplement or natural remedy. Do not replace your prescribed diabetes medicines with alternative medicines.
Coping and support
Type 2 diabetes is a serious disease, and following your diabetes treatment plan takes commitment. To effectively manage diabetes, you may need a good support network.
Anxiety and depression are common in people living with diabetes. Talking to a counselor or therapist may help you cope with the lifestyle changes and stress that come with a type 2 diabetes diagnosis.
Support groups can be good sources of diabetes education, emotional support and helpful information, such as how to find local resources or where to find carbohydrate counts for a favorite restaurant. If you're interested, your health care provider may be able to recommend a group in your area.
You can visit the American Diabetes Association website to check out local activities and support groups for people living with type 2 diabetes. The American Diabetes Association also offers online information and online forums where you can chat with others who are living with diabetes. You also can call the organization at 800-DIABETES ( 800-342-2383 ).
Preparing for your appointment
At your annual wellness visit, your health care provider can screen for diabetes and monitor and treat conditions that increase your risk of diabetes, such as high blood pressure, high cholesterol or a high BMI .
If you are seeing your health care provider because of symptoms that may be related to diabetes, you can prepare for your appointment by being ready to answer the following questions:
- When did your symptoms begin?
- Does anything improve the symptoms or worsen the symptoms?
- What medicines do you take regularly, including dietary supplements and herbal remedies?
- What are your typical daily meals? Do you eat between meals or before bedtime?
- How much alcohol do you drink?
- How much daily exercise do you get?
- Is there a history of diabetes in your family?
If you are diagnosed with diabetes, your health care provider may begin a treatment plan. Or you may be referred to a doctor who specializes in hormonal disorders, called an endocrinologist. Your care team also may include the following specialists:
- Certified diabetes education specialist.
- Foot doctor, also called a podiatrist.
- Doctor who specializes in eye care, called an ophthalmologist.
Talk to your health care provider about referrals to other specialists who may be providing care.
Questions for ongoing appointments
Before any appointment with a member of your treatment team, make sure you know whether there are any restrictions, such as not eating or drinking before taking a test. Questions that you should regularly talk about with your health care provider or other members of the team include:
- How often do I need to monitor my blood sugar, and what is my target range?
- What changes in my diet would help me better manage my blood sugar?
- What is the right dosage for prescribed medications?
- When do I take the medications? Do I take them with food?
- How does management of diabetes affect treatment for other conditions? How can I better coordinate treatments or care?
- When do I need to make a follow-up appointment?
- Under what conditions should I call you or seek emergency care?
- Are there brochures or online sources you recommend?
- Are there resources available if I'm having trouble paying for diabetes supplies?
What to expect from your doctor
Your health care provider is likely to ask you questions at your appointments. Those questions may include:
- Do you understand your treatment plan and feel confident you can follow it?
- How are you coping with diabetes?
- Have you had any low blood sugar?
- Do you know what to do if your blood sugar is too low or too high?
- What's a typical day's diet like?
- Are you exercising? If so, what type of exercise? How often?
- Do you sit for long periods of time?
- What challenges are you experiencing in managing your diabetes?
- Professional Practice Committee: Standards of Medical Care in Diabetes — 2020. Diabetes Care. 2020; doi:10.2337/dc20-Sppc.
- Diabetes mellitus. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetes-mellitus-dm. Accessed Dec. 7, 2020.
- Melmed S, et al. Williams Textbook of Endocrinology. 14th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Dec. 3, 2020.
- Diabetes overview. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/all-content. Accessed Dec. 4, 2020.
- AskMayoExpert. Type 2 diabetes. Mayo Clinic; 2018.
- Feldman M, et al., eds. Surgical and endoscopic treatment of obesity. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Oct. 20, 2020.
- Hypersmolar hyperglycemic state (HHS). Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/hyperosmolar-hyperglycemic-state-hhs. Accessed Dec. 11, 2020.
- Diabetic ketoacidosis (DKA). Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetic-ketoacidosis-dka. Accessed Dec. 11, 2020.
- Hypoglycemia. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/hypoglycemia. Accessed Dec. 11, 2020.
- 6 things to know about diabetes and dietary supplements. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/tips/things-to-know-about-type-diabetes-and-dietary-supplements. Accessed Dec. 11, 2020.
- Type 2 diabetes and dietary supplements: What the science says. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/providers/digest/type-2-diabetes-and-dietary-supplements-science. Accessed Dec. 11, 2020.
- Preventing diabetes problems. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/all-content. Accessed Dec. 3, 2020.
- Schillie S, et al. Prevention of hepatitis B virus infection in the United States: Recommendations of the Advisory Committee on Immunization Practices. MMWR Recommendations and Reports. 2018; doi:10.15585/mmwr.rr6701a1.
- Diabetes prevention: 5 tips for taking control
- Hyperinsulinemia: Is it diabetes?
Associated Procedures
News from mayo clinic.
- Mayo study uses electronic health record data to assess metformin failure risk, optimize care Feb. 10, 2023, 02:30 p.m. CDT
- Mayo Clinic Minute: Strategies to break the heart disease and diabetes link Nov. 28, 2022, 05:15 p.m. CDT
- Mayo Clinic Q and A: Diabetes risk in Hispanic people Oct. 20, 2022, 12:15 p.m. CDT
- The importance of diagnosing, treating diabetes in the Hispanic population in the US Sept. 28, 2022, 04:00 p.m. CDT
- Mayo Clinic Minute: Managing Type 2 diabetes Sept. 28, 2022, 02:30 p.m. CDT
Products & Services
- A Book: The Essential Diabetes Book
- A Book: The Mayo Clinic Diabetes Diet
- Assortment of Health Products from Mayo Clinic Store
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Division of General Internal Medicine
Diabetes self management patient education materials, table of contents.
Click on any of the links below to access helpful materials on managing all aspects of diabetes that can be printed and given to your patients .
Introductory Information
- Diabetes Mellitus Type 1 : Symptoms, diagnosis, prevention, and treatment (e.g., insulin)
- Diabetes Mellitus Type 2 : Symptoms, diagnosis, prevention, and treatment (e.g., medications)
- Women and Diabetes: Eating and weight, pregnancy, and heart disease
- Men and Diabetes: Sexual Issues and employment concerns
- Diabetes and Your Lifestyle : Exercise, traveling, employment, sexual issues, and special considerations for the elderly
General Self-Care (e.g., Blood Glucose, Foot Care)
Blood glucose.
- Pass This Test : Testing blood glucose levels
- Tool: Blood Sugar Monitoring Log (Oral Meds): Patient log to record levels
- Tool: Blood Sugar Monitoring Log (Insulin Meds): Patient log to monitor levels
- Tool: Foot Care Log : Patient log to record self-inspections and any problem areas
- Tool: Injection Sites : Patient log to help rotate injection sites
- Tool: Planning Your Exercise: Guide to help patients design an exercise program
- Tool: Physical Activity Log : Patient log to record physical activity
- Exercise in Disguise: Finding ways to exercise at home and outside of the gym
- Exercising Like Your Life Depends on It: Health benefits to exercising
- Hot Weather Exercise: Taking extra care when exercising in hot weather
Nutrition/Health
Diet/weight loss.
- Managing Type 2 Diabetes through Diet : Suggestions for balancing your diet
- Losing Weight When You Have Diabetes: Weight loss benefits, suggestions to start, and a brief discussion of weight loss drugs
- The Skinny on Visceral Fat : Dangers of visceral fat and exercise tips to reduce visceral fat
Meal Planning
- Tool: Shopping Guide and Nutrition Tips: Shopping list and money-saving tips
- Tool: Meal Planning Guides: Plate diagrams demonstrating appropriate portions
- Tool: Food Log : Patient log to record food and drink
- No More Carb Confusion : Understanding carbs and their effect on blood sugar
Smoking and Alcohol
- Mixing Alcohol with Diabetes: What drinking does to your body, and when it is ok
- Tool: Sick Day Guidelines: Tips, suggested foods, and patient log to record intake
- Diabetes and Stress : Immediate and long-term affects, and tips to manage stress
Medical Care Topics / Relation to Other Illnesses
- Infections and Diabetes: Explains increased chance for infections
- Make the DASH to Lower Your Blood Pressure : Nutrition tips to lower hypertension
Heart Smart
- Diabetes and Your Heart : "ABC" numbers and their link to heart disease
- Heart Smart Medications : Types of medications to prevent heart problems
- Young at Heart : Suggestions to reverse heart disease and tips for heart health
Vascular Disease
- Microvascular Disease Due to Diabetes: Discusses increased risk for eye and kidney problems
- Macrovascular Disease Due to Diabetes: Discusses increased risk for heart attack and stroke
- Preserving Kidney Function : Preserving Kidney function, especially when damage has already occurred
- Keeping Kidneys Healthy: Tips for kidney health and some "kidney-protective" meds
- Nine Ways to Avoid Diabetes Complications : Overview of tips to manage diabetes (healthy eating, activity, checking feet, etc.)
Other Topics
- Wake-up Call: Symptoms of sleep apnea, and the effects of lost sleep
Patient Education Library
Types of Physical Activity
Plan Your Plate
Best Foods For You: Making Healthy Food Choices
Your Mental Health and Diabetes
Fact Sheets
- At A Glance
- Diabetes and Prediabetes Fact Sheet
- On Your Way to Preventing Type 2 Diabetes
- Take Charge of Your Diabetes: Your Medicines
- Take Charge of Your Diabetes: Healthy Eyes
- Take Charge of Your Diabetes: Healthy Feet
- Take Charge of Your Diabetes: Healthy Teeth
- Take Charge of Your Diabetes: Healthy Ears
- Take Care of Your Kidneys and They Will Take Care of You
- How to Help a Loved One With Diabetes When You Live Far Apart
- Choosing Healthy Foods on Holidays and Special Occasions
- Tasty Recipes for People with Diabetes [PDF - 9 MB]
- Steps to Help You Stay Healthy With Diabetes
- 5 Questions to Ask Your Health Care Team
- Managing Diabetes: Medicare Coverage and Resources [PDF - 1 MB]
- Road to Health Toolkit (English) This collection of tools is tailored to African Americans and can be used to counsel and motivate those at high risk for type 2 diabetes.
- Road to Health Toolkit (Spanish)/Kit El camino hacia la buena salud This collection of tools can be used to counsel and motivate those at high risk for type 2 diabetes.
- Road to Health: Blaze Your Own Trail to Healthy Living [PDF – 6.91MB] This flipchart is culturally adapted to counsel and motivate American Indian people who are at risk for type 2 diabetes.
To receive updates about diabetes topics, enter your email address:
- Diabetes Home
- State, Local, and National Partner Diabetes Programs
- National Diabetes Prevention Program
- Native Diabetes Wellness Program
- Chronic Kidney Disease
- Vision Health Initiative
- Heart Disease and Stroke
- Overweight & Obesity
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- GP practice services
- Health advice
- Health research
- Medical professionals
- Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skin, nail and hair health
Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
Type 2 diabetes
Peer reviewed by Dr Krishna Vakharia, MRCGP Last updated by Dr Colin Tidy, MRCGP Last updated 26 Apr 2023
Meets Patient’s editorial guidelines
In this series: Type 2 diabetes treatment Type 2 diabetes diet
Type 2 diabetes can occur at any age, including during childhood, but it occurs mainly in people aged over 40. The first-line treatment is diet, weight control and physical activity.
The good news is that many people can stay well using these lifestyle measures. However if the blood sugar (glucose) level remains high then tablets to reduce the blood glucose level are usually advised. Insulin injections are needed in some cases. Other treatments include reducing blood pressure if it is high, lowering high cholesterol levels, and also other measures to reduce the risk of complications.
In this article :
What is type 2 diabetes, how common is type 2 diabetes, type 2 diabetes symptoms, type 2 diabetes diagnosis, type 2 diabetes complications, what are the aims of type 2 diabetes treatment, treatment aim 1 - keeping your blood sugar (glucose) level at normal levels, treatment aim 2 - to reduce other risk factors, treatment aim 3 - monitoring to detect and treat any complications promptly, immunisation.
Continue reading below
Playlist: What is Diabetes?

Dr. Partha Kar, FRCP

How do you explain type 2 diabetes to your child?
Type 2 diabetes and its symptoms tend to develop gradually (over weeks or months). This is because in type 2 diabetes you still make insulin (unlike in type 1 diabetes ). However, you develop type 2 diabetes because:
You do not make enough insulin for your body's needs; or
The cells in your body do not use insulin properly. This is called insulin resistance. The cells in your body become resistant to normal levels of insulin. This means that you need more insulin than you normally make to keep the blood sugar (glucose) level down; or
A combination of the above two reasons.
You can learn more about insulin and blood glucose from our separate leaflet called Diabetes (Diabetes Mellitus) .
Type 2 diabetes is much more common than type 1 diabetes.
Type 2 diabetes develops mainly in people older than the age of 40 but type 2 diabetes is now becoming far more common in children and in young people.
The number of people with type 2 diabetes is increasing in the UK, as it is more common in people who are overweight or obese. It also tends to run in families. Type 2 diabetes is around five times more common in South Asian and African-Caribbean people (often developing before the age of 40 in this group). It is estimated that by 2025 more than 5 million people in the UK will be diagnosed with diabetes.
Playlist: Risks of Diabetes
Who is most at risk from type 2 diabetes.

Is type 2 diabetes hereditary?

How can I avoid getting a hypo?
Dr. Sarah Jarvis MBE, FRCGP

What can someone with type 1 diabetes do to stop their blood glucose going too high?
Other risk factors.
Having a first-degree relative with type 2 diabetes. (A first-degree relative is a parent, brother, sister, or child.)
Being overweight or obese .
Having a waist measuring more than 31.5 inches (80 cm) if you are a woman or more than 37 inches (94 cm) if you are a man. Where in your body you store excess weight is important. Central obesity (a big tummy) probably happens because of the effect of insulin pushing excess sugar into abdominal fat cells over the years.
Having pre-diabetes (impaired glucose tolerance) . Impaired glucose tolerance means that your blood sugar (glucose) levels are higher than normal but not high enough to have diabetes. People with impaired glucose tolerance have a high risk of developing diabetes and so impaired glucose tolerance is often called pre-diabetes.
Having diabetes or pre-diabetes when you were pregnant .
How do you know if you have type 2 diabetes?
As already mentioned, type 2 diabetes symptoms often come on gradually and can be quite vague at first. Many people have type 2 diabetes for a long period of time before their diagnosis is made.
The most common type 2 diabetes symptoms are:
Being thirsty a lot of the time.
Passing large amounts of urine.
Tiredness, which may be worse after meals.
The reason why you make a lot of urine and become thirsty is that if your blood sugar (glucose) rises too high (because insulin is not doing its job) the excess sugar leaks into your urine. This pulls out extra water through the kidneys.
As the type 2 diabetes symptoms may develop gradually, you can become used to being thirsty and tired and you may not recognise for some time that you are ill. Some people also develop blurred vision and frequent infections, such as recurring thrush.
However, some people with type 2 diabetes do not have any symptoms if the glucose level is not too high. But, even if you do not have symptoms, you should still have treatment to reduce the risk of developing complications.
Patient picks for Type 2 diabetes
Video: How do you know if you have type 2 diabetes?

Type 2 diabetes diet
How do you get tested for type 2 diabetes.
A simple dipstick test may detect sugar (glucose) in a sample of urine. However, this is not enough to make a definite diagnosis of type 2 diabetes. Therefore, a blood test called HbA1c is needed to make the diagnosis. The blood test detects the level of glucose in your blood . If the glucose level is high then it will confirm that you have type 2 diabetes.
Some people have to have two samples of blood taken and may be asked to fast. (Fasting means having nothing to eat or drink, other than water, from midnight before the blood test is performed.)
It is now recommended that the blood test for HbA1c can also be used as a test to diagnose type 2 diabetes. An HbA1c value of 48 mmol/mol (6.5%) or above is recommended as the blood level for diagnosing type 2 diabetes. An HbA1c blood test gives an average of how high your blood glucose levels have been over the preceding few months.
In many cases type 2 diabetes is diagnosed during a routine medical or when tests are done for an unrelated medical condition.
Short-term complication - a very high glucose level
This is rare with type 2 diabetes. It is more common in untreated type 1 diabetes when a very high level of blood sugar (glucose) can develop quickly. However, a very high glucose level develops in some people with untreated type 2 diabetes. A very high blood level of glucose can cause lack of fluid in the body (dehydration), drowsiness and serious illness which can be life-threatening.
Long-term complications
If your blood glucose level is higher than normal over a long period of time, it can gradually damage your blood vessels. This can occur even if the glucose level is not very high above the normal level. This may lead to some of the following complications (often years after you first develop type 2 diabetes):
Furring, or 'hardening', of the arteries (atheroma) . This can cause problems such as angina , heart attacks, stroke and poor circulation.
Kidney damage which sometimes develops into chronic kidney disease .
Eye problems which can affect vision (due to damage to the small arteries of the retina at the back of the eye).
Nerve damage .
Foot problems (due to poor circulation and nerve damage).
Impotence (again due to poor circulation and nerve damage).
Other rare problems.
The type and severity of long-term complications vary from case to case. You may not develop any at all. In general, the nearer your blood glucose level is to normal, the less your risk of developing complications . Your risk of developing complications is also reduced if you deal with any other risk factors that you may have, such as high blood pressure.
It has been found that people with type 2 diabetes are more at risk of periodontitis. This is a condition that destroys the tissues supporting your teeth. Untreated, this could lead to tooth loss. It can start with gingivitis which is an inflammation of the gums. Left untreated, this leads to periodontitis and further severe gum conditions.
At your annual review, your doctor will remind you to have checks with your dentist. If you do have periodontitis, managing this illness can improve blood sugar control so it is best to keep those regular reviews with your dentist.
Complications of type 2 diabetes treatment
Medications for type 2 diabetes, like most other medications, can cause side-effects in some people. You can find out more about diabetes medications and their side-effects from our separate leaflet called Type 2 Diabetes Treatment .
However, one important side-effect which can affect people taking insulin and/or certain diabetes tablets is hypoglycaemia (often called a 'hypo'). This occurs when the level of glucose becomes too low, usually under 4 mmol/L. Not all tablet medicines used for diabetes can cause a hypo - for example, metformin does not cause this.
A hypo may occur if you have too much diabetes medication, have delayed or missed a meal or snack, or have taken part in unplanned exercise or physical activity. You can find out more about the symptoms and treatments of hypos from our separate leaflet called Hypoglycaemia (Low Blood Sugar) .
Until about 20 years ago, the medication options for treatment of type 2 diabetes were fairly limited. Insulin, along with a group of medicines called the sulfonylureas, can cause hypos (as well as weight gain). In the last 20 years, as newer medication has been developed, many people do not need to take sulfonylureas. In fact, more and more people never need to take insulin as newer agents offer more options for type 2 diabetes treatment.
Note: hypoglycaemia does not occur if you are treated with diet alone .
If you have type 2 diabetes, you may think that keeping your blood sugar (glucose) at normal levels is all that matters. In fact, while that's important, there's more to treatment than this.
Lifestyle changes are an essential part of treatment for all people with type 2 diabetes, regardless of whether or not they take medication.
Many people with type 2 diabetes can reduce their blood glucose (and HbA1c) to a target level with changes to their diet, weight and exercise levels. However, if the blood sugar (or HbA1c) level remains too high after a trial of these measures for a few months, then medication is usually advised.
Diet, weight control and physical activity
Diet. What you eat is absolutely central to your blood glucose control, as well as your general health. Please read our separate leaflet called Type 2 Diabetes Diet for more information. Your practice nurse or dietician can give you more information and support.
Lose weight if you are overweight. Getting to a perfect weight is unrealistic for many people. However, losing some weight if you are obese or overweight will help to reduce your blood glucose and blood pressure levels (and have other health benefits too). Recent evidence from Professor Taylor, Newcastle University, has shown that weight loss alone can put diabetes into drug-free remission in at least a third of patients.
Do some physical activity regularly. If you are able, a minimum of 30 minutes' brisk walking at least five times a week is advised. Anything more vigorous and more often is even better - for example, swimming, cycling, jogging, dancing. Ideally, you should do an activity that gets you at least mildly out of breath and mildly sweaty. You can spread the activity over the day - for example, two fifteen-minute spells per day of brisk walking, cycling, dancing, etc. Regular physical activity also reduces your risk of having a heart attack or stroke.
Medication is not used instead of a healthy diet, weight control and physical activity - you should still do these things as well as take medication. See our separate leaflet called Type 2 Diabetes Treatment for more details .
How is the blood glucose level monitored?
The blood test that is mainly used to keep a check on your blood glucose level is called the HbA1c test . This test is commonly done every 2-6 months by your doctor or nurse.
The HbA1c test measures a part of the red blood cells. Glucose in the blood attaches to part of the red blood cells. This part can be measured and gives a good indication of your average blood glucose level over the preceding 1-3 months.
Type 2 diabetes treatment aims to lower your HbA1c to below a target level. Ideally, it is best to maintain HbA1c to less than 48 mmol/mol (6.5%). However, this may not always be possible to achieve and your target level of HbA1c should be agreed between you and your doctor.
If your HbA1c is above your target level then you may be advised to step up treatment (for example, to increase a dose of medication) to keep your blood glucose level down.
Some people with diabetes check their actual blood glucose level regularly with a blood glucose monitor. If you are advised to do this then your doctor or nurse will give you instructions on how to do it.
Continuous glucose monitoring (CGM) The National Institute for Health and Care Excellence (NICE) has recommended that CGM should be offered to some people using insulin several times a day. They recommend that your specialist team should offer this if:
You have repeated or severe episodes of hypoglycaemia ('hypos').
You have impaired hypoglycaemia awareness, where you don't recognise the early symptoms of hypos.
You have a condition or disability for which you can't use regular finger-prick testing.
You need to measure your blood glucose at least eight times a day.
You are less likely to develop complications of type 2 diabetes if you reduce any other risk factors. These are briefly mentioned below - see the separate leaflet called Cardiovascular Disease (Atheroma) for more details . Although everyone should aim to cut out preventable risk factors, people with diabetes have even more of a reason to do so.
Keep your blood pressure down
It is very important to have your blood pressure checked regularly. The combination of high blood pressure and diabetes is a particularly high risk factor for complications. Even mildly raised blood pressure should be treated if you have type 2 diabetes. Medication, often with two or even three different medicines, may be needed to keep your blood pressure down but remember weight loss and exercise can really help with this too.
See the separate leaflet called Diabetes and High Blood Pressure for more details.
If you smoke - now is the time to stop
Smoking is a major risk factor for complications . You should consult your practice nurse or attend a smoking cessation clinic - it's much easier to quit with support. As well as expert help and advice, medication or nicotine replacement therapy (nicotine gum, etc) may help you to stop.
Other medication
You will usually be advised to take a medicine to lower your cholesterol level . This will help to lower the risk of developing some complications such as heart disease , peripheral arterial disease and stroke .
Protect your kidneys
Keeping your blood glucose well controlled can reduce your risk of kidney damage. But a group of medications first developed to treat type 2 diabetes can provide added protection against developing and worsening chronic kidney disease.
These medicines, called SGLT-2 inhibitors, are now recommended for everyone with type 2 diabetes who has chronic kidney disease with protein in the urine. This is one of the reasons getting regular kidney checks (see below) is so important.
In fact, some medicines in this class are now used to protect the kidneys in people who have chronic kidney disease but who do not have diabetes.
You can find out more about the SGLT-2 inhibitors in our leaflet on type 2 diabetes treatment .
Most GP surgeries and hospitals have special diabetes clinics. Doctors, nurses, dieticians, specialists in foot care (podiatrists - previously called chiropodists), specialists in eye health (optometrists) and other healthcare workers all play a role in giving advice and checking on progress. Regular checks may include:
Checking levels of blood sugar (glucose), HbA1c, cholesterol and blood pressure.
Ongoing advice on diet and lifestyle.
Checking for early signs of complications - for example:
Eye checks - see more detail below.
Urine tests - which include testing for protein in the urine, which may indicate early kidney problems.
Foot checks - to help prevent foot ulcers .
Other blood tests - these include checks on kidney function and other general tests.
It is important to have regular checks, as some complications, particularly if detected early, can be treated or prevented from becoming worse.
Eye screening
Regular (at least yearly) eye checks can detect problems with the retina (a possible complication of diabetes), which can often be prevented from becoming worse. Increased pressure in the eye ( glaucoma ) is more common in people with diabetes and can usually be treated.
The National Institute for Health and Care Excellence (NICE) has updated its recommendations on eye screening and treatment in an update of its guidance on type 2 diabetes.
Eye checks usually include taking photographs of the back of your eye (retinal photography) to see whether there are any problems. This needs to be done at a specialist eye screening clinic.
The guidance recommends that:
You should be referred to a specialist local eye screening service as soon as you are diagnosed with type 2 diabetes.
If your eyesight suddenly deteriorates significantly without any obvious explanation, you should be referred to a specialist eye doctor (an ophthalmologist). How urgently you are referred will depend on your symptoms and personal circumstances.
You should be immunised against flu (each autumn) and also against pneumococcal germs (bacteria) - a vaccination just given once. These infections can be particularly unpleasant if you have diabetes.
Further reading and references
- Management of diabetes ; Scottish Intercollegiate Guidelines Network - SIGN (March 2010 - updated November 2017)
- Diabetes UK
- Diabetes and Bad Cholesterol Information Prescription ; Diabetes UK
- Diabetes (type 1 and type 2) in children and young people: diagnosis and management ; NICE Guidelines (Aug 2015 - updated May 2023)
- Type 2 diabetes in adults: management ; NICE Guidance (December 2015 - last updated June 2022)
- Information prescriptions - living well ; Diabetes UK
- d-Nav insulin management app for type 2 diabetes ; NICE Medtech innovation briefing, February 2022
- Diabetes - type 2 ; NICE CKS, November 2023 (UK access only)
- Type 2 diabetes in adults ; NICE Quality standard, March 2023
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 24 Mar 2028
26 apr 2023 | latest version.
Last updated by
Peer reviewed by

Feeling unwell?
Assess your symptoms online for free
You are now leaving the Lilly Medical Education website
The link you clicked on will take you to a site maintained by a third party, which is solely responsible for its content. Lilly USA, LLC does not control, influence, or endorse this site, and the opinions, claims, or comments expressed on this site should not be attributed to Lilly USA, LLC. Lilly USA, LLC is not responsible for the privacy policy of any third-party websites. We encourage you to read the privacy policy of every website you visit. Click "Continue" to proceed or "Return" to return to Lilly Medical Education.
Type 2 Diabetes Patient Case Simulation
Case Simulation 1
CLINIC- Sim : Simulating a Patient-Centered Approach to Optimize Early Glycemic and Weight Control in Type 2 Diabetes

Learn more about glycemic control and weight management in type 2 diabetes
Shared decision-making resources, watch an expert video on shared decision-making and download the conversation starter to aid in your patient interactions.
These videos were commissioned by Lilly and are intended to be used by HCPs who treat diabetes for medical, scientific and educational purposes. Video content is not approved for continuing education credit. Disclosures: Dr. Matt Capehorn
- Board member of the Association for the Study of Obesity (ASO)
- Faculty member of the Primary care Academy of Diabetes Specialists (PCADS)
- Expert Advisor to NICE
- Professional Advisor to the Obesity Empowerment Network (OEN)
- Director – RIO Weight management Limited
- Medical Director – Lighterlife (commercial VLCD company)
- Ad-hoc Medical Advisor – McDonalds UK
Advisory Boards: Lilly, Boehringer Ingelheim, Novo Nordisk; Speaker fees/travel: Lilly, Boehringer Ingelheim, Novo Nordisk; Research income (RIO): Lilly, Boehringer Ingelheim, Novo Nordisk
Patient Information

Expand accordion Patient Profile
- 47-year-old African American female
- Diagnosed with T2D 9 months ago
- HbA 1c since diagnosis: 8.7%
- Current treatment: 1000 mg metformin daily at diagnosis
- Followed by registered dietitian/nurse educator
Expand accordion Medical History
- Prediabetes for 2 years preceding diagnosis, tried to manage with diet and exercise
- Gestational diabetes with her second child
- Hypertension
- Mixed dyslipidemia
Expand accordion Family History
- T2D in father, maternal aunt
- CAD in father
- Hypertension in mother and father
Expand accordion Social History
- Married, has 2 children ages 10 and 15
- Never smoked or vaped, no illicit substances, rarely drinks alcohol
- High school math teacher
Expand accordion Physical Exam and Labs
- Normal eGFR, normal urine microalbumin
- BMI: 33 kg/m 2 (195 lbs)
- Blood pressure: 145/90 mmHg
- Total cholesterol: 210 mg/dL
- LDL cholesterol: 109 mg/dL
- HDL cholesterol: 44 mg/dL
- Triglycerides: 290 mg/dL

9 months since diagnosis The patient was diagnosed with type 2 diabetes, and her HbA 1c was 8.7% at the time. She was started on 1000 mg metformin daily. During that visit, she was advised on lifestyle modifications, including dietary changes to help both her diabetes and hypertension management, as well as recommendations to incorporate exercise. She was encouraged to start a statin for dyslipidemia but was too overwhelmed by her diabetes and declined statin therapy. At visit 2, her HbA 1c decreased to 7.9%. She again declined a statin and agreed to start an ACE inhibitor. Her metformin was titrated to 1500 mg total daily dose.
13 months since diagnosis (4-month follow-up)
- She returns 4 months later.
- She is taking a dose of 1500 mg metformin daily (500 mg in the morning and 1000 mg in the evening) without missing doses. She was not able to tolerate a dose of 1000 mg twice daily. Her HbA 1c has decreased to 7.7% from 7.9%, and her body weight remained stable.
- Blood pressure: 130/85 mmHg
- Total cholesterol: 205 mg/dL
- LDL cholesterol: 110 mg/dL
- HDL cholesterol: 43 mg/dL
- Triglycerides: 260 mg/dL
- She increased her physical activity by parking farther and trying to walk more, but often struggles to find the time to get more exercise in.
- She tries to eat more balanced meals with protein, vegetables and fewer carbohydrates; she finds it difficult to make multiple meals for her family members who prefer to keep to their old dietary routine.
- She is motivated to continue working on lifestyle changes and has agreed to start a statin.
Question #1
In addition to continuing metformin 1500 mg daily, which of the following may be the next best step.
Continue lifestyle modifications – she is very motivated and prefers not to start another medication
Start a sulfonylurea and continue lifestyle modifications
Start an incretin receptor agonist and continue lifestyle modifications
Start a DPP-4 inhibitor
Related Resources
Hear from Dr. Capehorn on collaborating with patients to individualize care.
VV-MED-145674
Patient-Physician Conversation Starter (PDF)
Tips and tricks to initiate patient centric conversations.
VV-MED-145677
Shared Decision-Making (PDF)
Support early glycemic control and weight management through shared decision-making.
VV-MED-148828
VV-MED-144376

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
ACP Guideline on Pharmacologic Treatments for Diabetes: Key Points
The following are key points to remember about a clinical guideline from the American College of Physicians (ACP) on newer pharmacologic treatments in adults with type 2 diabetes:
- Type 2 diabetes is associated with higher risk for mortality and morbidity, greater health care use, and greater costs when adults with diabetes are compared with those without diabetes.
- Major treatment goals for patients with type 2 diabetes include adequate glycemic control and primary and secondary prevention of atherosclerotic cardiovascular and kidney diseases, which account for nearly one half of all deaths among adults with type 2 diabetes.
- This guideline addresses effectiveness and harms of newer pharmacologic treatments to reduce the risk for all-cause mortality, cardiovascular morbidity, and progression of chronic kidney disease (CKD) in adults with type 2 diabetes.
- Newer pharmacologic treatments include glucagon-like peptide-1 (GLP-1) agonists (dulaglutide, exenatide, liraglutide, lixisenatide, and semaglutide), a GLP-1 agonist and glucose-dependent insulinotropic polypeptide agonist (tirzepatide), sodium–glucose cotransporter-2 (SGLT-2) inhibitors (canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin), dipeptidyl peptidase-4 (DPP-4) inhibitors (alogliptin, linagliptin, saxagliptin, and sitagliptin), and long-acting insulins (insulin glargine and insulin degludec).
- The ACP recommends adding an SGLT-2 inhibitor or GLP-1 agonist to metformin and lifestyle modifications in adults with type 2 diabetes and inadequate glycemic control (strong recommendation; high-certainty evidence).
- Use of an SGLT-2 inhibitor is recommended to reduce the risk for all-cause mortality, major adverse cardiovascular events (MACE), progression of CKD, and hospitalization due to congestive heart failure [CHF]. Clinicians should prioritize adding SGLT-2 inhibitors in patients with type 2 diabetes and CHF or CKD.
- Use of a GLP-1 agonist is recommended to reduce the risk for all-cause mortality, MACE, and stroke. Clinicians should prioritize adding GLP-1 agonists in patients with type 2 diabetes and an increased risk for stroke or for whom total body weight loss is an important treatment goal.
- The ACP recommends against adding a dipeptidyl peptidase-4 (DPP-4) inhibitor to metformin and lifestyle modifications in adults with type 2 diabetes and inadequate glycemic control to reduce morbidity and all-cause mortality (strong recommendation; high-certainty evidence).
- Metformin (unless contraindicated) and lifestyle modifications are the first steps in managing type 2 diabetes in most patients. When selecting an additional therapy, clinicians should consider the evidence of benefits, harms, patient burden, and cost of medications in addition to performing an individualized assessment of each patient’s preferences, glycemic control target, comorbid conditions, and risk for symptomatic hypoglycemia.
- Overall, clinicians should aim to achieve glycated hemoglobin (HbA 1c ) levels between 7% and 8% in most adults with type 2 diabetes and deintensify pharmacologic treatments in adults with HbA 1c levels <6.5%. An individualized glycemic goal should be based on risk for hypoglycemia, life expectancy, diabetes duration, established vascular complications, major comorbidities, patient preferences and access to resources, capacity for adequate monitoring of hypoglycemia, and other harms.
- Finally, type 2 diabetes management should be based on collaborative communication and goal setting among all team members, including clinical pharmacists, to reduce the risk for polypharmacy and associated harms.
Clinical Topics: Diabetes and Cardiometabolic Disease, Prevention
Keywords: Diabetes Mellitus, Type 2, Pharmaceutical Preparations
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
Contributor Disclosures
Please read the Disclaimer at the end of this page.
TYPE 2 DIABETES OVERVIEW
Type 2 diabetes mellitus is a disorder that is known for disrupting the way your body uses glucose (sugar); it also causes other problems with the way your body stores and processes other forms of energy, including fat.
All the cells in your body need sugar to work normally. Sugar gets into the cells with the help of a hormone called insulin. In type 2 diabetes, the body stops responding to normal or even high levels of insulin, and over time, the pancreas (an organ in the abdomen) does not make enough insulin to keep up with what the body needs. Being overweight, especially having extra fat stored in the liver and abdomen, even if weight is normal, increases the body's demand for insulin. This causes high blood sugar (glucose) levels, which can lead to problems if untreated. (See "Patient education: Type 2 diabetes: Overview (Beyond the Basics)" .)
People with type 2 diabetes require regular monitoring and ongoing treatment to maintain normal or near-normal blood sugar levels. Treatment includes lifestyle changes (including dietary changes and exercise to promote weight loss), self-care measures, and sometimes medications, which can minimize the risk of diabetes and cardiovascular (heart-related) complications.
This topic review will discuss the medical treatment of type 2 diabetes.
DIABETES CARE DURING THE COVID-19 PANDEMIC
COVID-19 stands for "coronavirus disease 2019." It is an infection caused by a virus called SARS-CoV-2. The virus first appeared in late 2019 and has since spread throughout the world.
People with certain underlying health conditions, including diabetes, are at increased risk of severe illness if they get COVID-19. COVID-19 infection can also lead to severe complications of diabetes, including diabetic ketoacidosis (DKA).
Getting vaccinated lowers the risk of severe illness; experts recommend COVID-19 vaccination for anyone with cancer or a history
TYPE 2 DIABETES TREATMENT GOALS
The main goals of treatment in type 2 diabetes are to keep your blood sugar levels within your goal range and treat other medical conditions that go along with diabetes (like high blood pressure); it is also very important to stop smoking if you smoke. These measures will reduce your risk of complications.
Blood sugar control — It is important to keep your blood sugar levels at goal levels. This can help prevent long-term complications that can result from poorly controlled blood sugar (including problems affecting the eyes, kidney, nervous system, and cardiovascular system).
Home blood sugar testing — Your doctor may instruct you to check your blood sugar yourself at home, especially if you take certain oral diabetes medicines or insulin. Home blood sugar testing is not usually necessary for people who manage their diabetes through diet only or with diabetes medications that do not cause low blood sugar.
A random blood sugar test is based on blood drawn at any time of day, regardless of when you last ate. A fasting blood sugar test is a blood test done after not eating or drinking for 8 to 12 hours (usually overnight). A normal fasting blood sugar is more than 70 mg/dL (3.9 mmol/L) but less than 100 mg/dL (5.6 mmol/L), although people with diabetes may have a different goal. Your doctor or nurse can help you set a blood sugar goal and show you exactly how to check your level. (See "Patient education: Glucose monitoring in diabetes (Beyond the Basics)" .)
A1C testing — Blood sugar control can also be estimated with a blood test called glycated hemoglobin, or "A1C." The A1C blood test measures your average blood sugar level over the past two to three months. The goal A1C for most young people with type 2 diabetes is 7 percent (53 mmol/mol) or less, which corresponds to an average blood sugar of approximately 150 mg/dL (8.3 mmol/L) ( table 1 ). Lowering your A1C level reduces your risk for kidney, eye, and nerve problems. For some people, a different A1C goal may be more appropriate. Your health care provider can help determine your A1C goal.
Reducing the risk of cardiovascular complications — The most common, serious, long-term complication of type 2 diabetes is cardiovascular disease, which can lead to problems like heart attack, stroke, and even death. On average, people with type 2 diabetes have twice the risk of cardiovascular disease as people without diabetes.
However, you can substantially lower your risk of cardiovascular disease by:
● Quitting smoking, if you smoke
● Managing high blood pressure and high cholesterol with diet, exercise, and medicines
● Taking a low-dose aspirin every day, if you have a history of heart attack or stroke or if your health care provider recommends this
Some studies have shown that lowering A1C levels with certain medications may also reduce your risk for cardiovascular disease. (See 'Type 2 diabetes medicines' below.)
A detailed discussion of ways to prevent complications is available separately. (See "Patient education: Preventing complications from diabetes (Beyond the Basics)" .)
DIET AND EXERCISE IN TYPE 2 DIABETES
Diet and exercise are the foundation of diabetes management.
Changes in diet can improve many aspects of type 2 diabetes, including helping to control your weight, blood pressure, and your body's ability to produce and respond to insulin. The single most important thing most people can do to improve diabetes management and weight is to avoid all sugary beverages, such as soft drinks or juices, or if this is not possible, to significantly limit consumption. Limiting overall food portion size is also very important. Detailed information about type 2 diabetes and diet is available separately. (See "Patient education: Type 2 diabetes and diet (Beyond the Basics)" .)
Regular exercise can also help control type 2 diabetes, even if you do not lose weight. Exercise is related to blood sugar control because it improves your body's response to insulin. (See "Patient education: Exercise and medical care for people with type 2 diabetes (Beyond the Basics)" .)
TYPE 2 DIABETES MEDICINES
A number of medications are available to treat type 2 diabetes.
Metformin — Most people who are newly diagnosed with type 2 diabetes will immediately begin a medicine called metformin (sample brand names: Glucophage, Glumetza, Riomet, Fortamet). Metformin improves how your body responds to insulin to reduce high blood sugar levels.
Metformin is a pill that is usually started with a once-daily dose with dinner (or your last meal of the day); a second daily dose (with breakfast) is added one to two weeks later. The dose may be increased every one to two weeks thereafter.
Side effects — Common side effects of metformin include nausea, diarrhea, and gas. These are usually not severe, especially if you take metformin along with food. The side effects usually improve after a few weeks.
People with severe kidney, liver, and heart disease and those who drink alcohol excessively should not take metformin. There are certain situations in which you should stop taking metformin, including if you develop acute or unstable heart failure, get a serious infection causing low blood pressure, become dehydrated, or have severely decreased kidney function. You will also need to stop your metformin before having surgery of any kind.
Adding a second medicine — Your doctor or nurse might recommend a second medication in addition to metformin. This may happen within the first two to three months if your blood sugar and A1C levels are still higher than your goal; otherwise, many people need to add a second glucose-lowering medication later (after several years of having diabetes). There are many available classes of medication that can be used with metformin or in combination with each other if metformin is contraindicated or not tolerated. (See "Patient education: Type 2 diabetes: Insulin treatment (Beyond the Basics)" .)
If your blood sugar levels are still high after two to three months but your A1C is close to the goal (generally between 7 and 8.5 percent), a second oral medicine might be added. If your A1C is higher than 9 percent, however, your doctor might recommend insulin (usually as a single daily injection) or a glucagon-like peptide-1 (GLP-1) or dual receptor agonist (a daily or weekly injection). The most appropriate second medicine depends upon several different factors, including your weight, risk of low blood sugar, other medical problems, and preferences, in addition to the efficacy, side effects, and cost of the medication.
Sulfonylureas — Sulfonylureas have been used to treat type 2 diabetes for many years. They work by increasing the amount of insulin your body makes and can lower blood sugar levels by approximately 20 percent. However, over time they gradually stop working. They are reasonable second agents because they are inexpensive, effective, universally available, and have a long-term track record. Most patients can take sulfonylureas even if they have an allergy to "sulfa" drugs. You should be very cautious taking a sulfonylurea if you have kidney failure.
A number of short-acting sulfonylureas are available (sample brand names: Glucotrol, Amaryl), and the choice between them depends mainly upon cost and availability.
If you take a sulfonylurea, you can develop low blood sugar, known as hypoglycemia. Low blood sugar symptoms can include:
● Feeling hungry
● Feeling anxious
● Feeling confused
Low blood sugar must be treated quickly by eating 10 to 15 grams of fast-acting carbohydrate (eg, fruit juice, hard candy, glucose tablets). It is possible to pass out if you do not treat low blood sugar quickly enough. To reduce the risk of low blood sugar when you are not eating, if you know you are going to miss a meal, you can skip the sulfonylurea tablet you would usually take before eating. A full discussion of low blood sugar is available separately. (See "Patient education: Hypoglycemia (low blood glucose) in people with diabetes (Beyond the Basics)" .)
DPP-4 inhibitors — This class of medicines, dipeptidyl peptidase-4 (DPP-4) inhibitors, includes sitagliptin (brand name: Januvia), saxagliptin (brand name: Onglyza), linagliptin (brand name: Tradjenta), alogliptin (brand name: Nesina), and vildagliptin (brand name: Galvus). Vildagliptin is available in some countries but not in the United States. These medicines lower blood sugar levels by increasing insulin release from the pancreas in response to a meal. They can be given alone in people who cannot tolerate the first-line medicine (metformin) or other medicines, or they can be given together with other oral medicines if blood sugar levels are still higher than the goal. These medicines do not cause hypoglycemia or changes in body weight. There have been rare reports of joint pain, pancreatitis, and severe skin reactions.
SGLT2 inhibitors — The sodium-glucose co-transporter 2 (SGLT2) inhibitors, canagliflozin (brand name: Invokana), empagliflozin (brand name: Jardiance), dapagliflozin (brand name: Farxiga), and ertugliflozin (brand name: Steglatro), lower blood sugar by increasing the excretion of sugar in the urine. They are variably effective, but on average, they are similar in potency to the DPP-4 inhibitors (see 'DPP-4 inhibitors' above). SGLT2 inhibitors may be a good choice for people with heart failure or chronic kidney disease because they have been shown to have some cardiovascular, renal, and mortality benefits.
SGLT2 inhibitors do not cause low blood sugar. They promote modest weight loss and blood pressure reduction. Side effects include genital yeast infections in men and women, urinary tract infections, and dehydration. Some medicines in this class have been associated with an increased risk of bone fracture or amputation. An uncommon but deadly infection of the tissue in the perineum (the area between the genitals and the anus) has also been reported in men and women.
SGLT2 inhibitors can increase the risk of diabetic ketoacidosis (DKA); this is a serious problem that can happen when acids called "ketones" build up in the blood. DKA can happen even when blood sugar is only mildly elevated. Blood ketones should be checked if symptoms of nausea and/or vomiting develop while taking SGLT2 inhibitors.
GLP-1 receptor agonists — The glucagon-like peptide-1 (GLP-1) receptor agonists are medications given by injection that increase insulin release in response to a meal and slow digestion. They include exenatide, dosed twice daily (brand name: Byetta); exenatide extended release, dosed weekly (brand name: Bydureon); liraglutide, dosed daily (brand name: Victoza); dulaglutide, dosed weekly (brand name: Trulicity); lixisenatide, dosed daily (brand name: Adlyxin); and semaglutide, dosed weekly as an injection (brand name: Ozempic) or daily as a tablet (brand name: Rybelsus). These medications are useful for people whose blood sugar is not controlled on the highest dose of one or two oral medicines. They may be especially helpful for overweight people who are gaining weight or struggling to lose weight on other diabetes medicines. Liraglutide, dulaglutide, or semaglutide injections are recommended for people who have, or are at high risk for, cardiovascular disease, as they have been shown to have cardiovascular benefits in these groups.
GLP-1 receptor agonists do not usually cause low blood sugar when used without other medications that cause low blood sugar. They promote loss of appetite and a sense of feeling full after eating a smaller amount of food, which helps with weight loss, but can also cause bothersome side effects, including nausea, vomiting, and diarrhea. Gastrointestinal side effects usually improve with time. Pancreatitis (inflammation of the pancreas) has been reported rarely in people taking GLP-1 receptor agonists, but it is not known if the medications caused the pancreatitis. They have also been associated with gall bladder disease. You should stop taking these medications if you develop severe abdominal pain. Exenatide and lixisenatide should not be used in people with abnormal kidney function, and liraglutide and dulaglutide should be used with caution in this situation. These drugs are generally expensive.
Meglitinides — Meglitinides include repaglinide (brand name: Prandin) and nateglinide (brand name: Starlix). They work to lower blood sugar levels, similar to the sulfonylureas, but they act more quickly than sulfonylureas and should be taken right before a meal; they might also be recommended in people who are allergic to sulfonylureas. They are taken in pill form. Meglitinides are not generally used as a first-line treatment, because they are more expensive than sulfonylureas. Repaglinide can be used in patients with kidney failure.
Thiazolidinediones — This class of medicines includes pioglitazone (brand name: Actos) and rosiglitazone (brand name: Avandia), which work to lower blood sugar levels by increasing the body's sensitivity to insulin. They are taken in pill form and usually in combination with other medicines such as metformin, a sulfonylurea, or insulin.
Common side effects of thiazolidinediones include:
● Weight gain.
● Swelling of the feet and ankles, which sometimes can be a sign of new or worsening heart failure. The risk of heart failure is small but serious. An early sign of heart failure is swelling of the feet and ankles. People who take thiazolidinediones should monitor for swelling.
● A small but serious increased risk of developing fluid retention at the back of the eyes (macular edema).
● A possible risk of developing certain types of cancer (like bladder cancer).
● An increased risk of bone fractures.
Alpha-glucosidase inhibitors — These medicines, which include acarbose (brand name: Precose) and miglitol (brand name: Glyset), work by interfering with the absorption of carbohydrates in the intestine. This helps to lower blood sugar levels but not as well as metformin or the sulfonylureas. They can be combined with other medicines if the first medicine does not lower blood sugar levels enough.
The main side effects of alpha-glucosidase inhibitors are gas (flatulence), diarrhea, and abdominal pain; starting with a low dose may minimize these side effects. The medicine is usually taken three times per day with the first bite of each meal.
Insulin — In the past, insulin treatment was reserved for patients with type 2 diabetes whose blood sugar was not controlled with oral medicines and lifestyle changes (ie, diet and exercise). However, there is increasing evidence that insulin treatment at earlier stages may improve overall diabetes management over time. Side effects include low blood sugar, if you take more insulin than your body needs, and weight gain. Adjusting the dose of insulin to the body's needs can minimize the risk of these side effects. It may be necessary to readjust your dose frequently.
In some situations, insulin injections (shots) can be used as a first-line treatment for type 2 diabetes. In other cases, insulin can be added to or substituted for oral medicines. If you take insulin, you will need to get comfortable giving yourself the injections or have a family member or housemate learn how to do it for you. More detailed information about insulin treatment is available separately. (See "Patient education: Type 2 diabetes: Insulin treatment (Beyond the Basics)" .)
LIVING WITH TYPE 2 DIABETES
Living with type 2 diabetes can be stressful. It is a lot of responsibility to have to monitor your blood sugar (if you need to do this), watch your diet, exercise regularly, keep all your appointments, and take your medications every day. It can also be scary to think about the potential complications of diabetes. It can help to involve your family and friends and make sure you have a solid support system in place to provide encouragement, reminders, and help as you need it.
It is not uncommon for stress to lead to burnout or even depression, and this can make taking care of yourself more difficult. Having an open and honest discussion with your doctor, nurse, or other health care provider can help you to understand your diagnosis, treatment plan, and what to do if you are overwhelmed. Some people also benefit from talking with a counselor or social worker to help them cope with their responsibilities and worries.
WHERE TO GET MORE INFORMATION
Your health care provider is the best source of information for questions and concerns related to your medical problem.
This article will be updated as needed on our website ( www.uptodate.com/patients ). Related topics for patients, as well as selected articles written for health care professionals, are also available. Some of the most relevant are listed below.
Patient level information — UpToDate offers two types of patient education materials.
The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials.
Patient education: Treatment for type 2 diabetes (The Basics) Patient education: Type 2 diabetes (The Basics) Patient education: Using insulin (The Basics) Patient education: Low blood sugar in people with diabetes (The Basics) Patient education: Metabolic dysfunction-associated steatotic liver disease (The Basics) Patient education: Exercise and movement (The Basics) Patient education: Carb counting for adults with diabetes (The Basics) Patient education: Lowering your risk of prediabetes and type 2 diabetes (The Basics) Patient education: Diabetic ketoacidosis (The Basics) Patient education: Hyperosmolar hyperglycemic state (The Basics) Patient education: How to give an insulin shot (The Basics) Patient education: How to use an insulin pen (The Basics)
Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon.
Patient education: Type 2 diabetes: Overview (Beyond the Basics) Patient education: Type 2 diabetes: Insulin treatment (Beyond the Basics) Patient education: Type 2 diabetes and diet (Beyond the Basics) Patient education: Glucose monitoring in diabetes (Beyond the Basics) Patient education: Hypoglycemia (low blood glucose) in people with diabetes (Beyond the Basics) Patient education: Exercise and medical care for people with type 2 diabetes (Beyond the Basics) Patient education: Preventing complications from diabetes (Beyond the Basics)
Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based. Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading.
Alpha-glucosidase inhibitors for treatment of diabetes mellitus Measurements of chronic glycemia in diabetes mellitus Glycemic management and vascular complications in type 2 diabetes mellitus Insulin therapy in type 2 diabetes mellitus Management of persistent hyperglycemia in type 2 diabetes mellitus Metformin in the treatment of adults with type 2 diabetes mellitus Overview of general medical care in nonpregnant adults with diabetes mellitus Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus Sulfonylureas and meglitinides in the treatment of type 2 diabetes mellitus Thiazolidinediones in the treatment of type 2 diabetes mellitus
The following organizations also provide reliable health information.
● National Library of Medicine
( www.nlm.nih.gov/medlineplus/healthtopics.html )
● American Diabetes Association (ADA)
(800)-DIABETES (800-342-2383)
( www.diabetes.org )
● Canadian Diabetes Associates
( www.diabetes.ca )
● US Center for Disease Control and Prevention
( www.cdc.gov/diabetes )
- Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Lancet 2004; 363:1589.
- Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998; 352:837.
- Nathan DM, Buse JB, Davidson MB, et al. Management of hyperglycemia in type 2 diabetes: A consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2006; 29:1963.
- Norris SL, Zhang X, Avenell A, et al. Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: a meta-analysis. Am J Med 2004; 117:762.
- Summary of Revisions: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020; 43:S4.

Atypical Diabetes
Approach to the patient with atypical diabetes, atypical diabetes and precision medicine, article information, atypical diabetes: what have we learned and what does the future hold.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Stephen I. Stone , Ashok Balasubramanyam , Jennifer E. Posey; Atypical Diabetes: What Have We Learned and What Does the Future Hold?. Diabetes Care 19 April 2024; 47 (5): 770–781. https://doi.org/10.2337/dci23-0038
Download citation file:
- Ris (Zotero)
- Reference Manager
As our understanding of the pathophysiology of diabetes evolves, we increasingly recognize that many patients may have a form of diabetes that does not neatly fit with a diagnosis of either type 1 or type 2 diabetes. The discovery and description of these forms of “atypical diabetes” have led to major contributions to our collective understanding of the basic biology that drives insulin secretion, insulin resistance, and islet autoimmunity. These discoveries now pave the way to a better classification of diabetes based on distinct endotypes. In this review, we highlight the key biological and clinical insights that can be gained from studying known forms of atypical diabetes. Additionally, we provide a framework for identification of patients with atypical diabetes based on their clinical, metabolic, and molecular features. Helpful clinical and genetic resources for evaluating patients suspected of having atypical diabetes are provided. Therefore, appreciating the various endotypes associated with atypical diabetes will enhance diagnostic accuracy and facilitate targeted treatment decisions.
Graphical Abstract

It is now generally recognized that the binary categorization of diabetes into type 1 and type 2 is insufficient to capture the range of metabolic and clinical phenotypes, molecular mechanisms, and disease pathogenesis that lead to the final common end point of hyperglycemia. The frequency of non–type 1, non–type 2 diabetes—now referred to as “atypical diabetes”—is likely underestimated, and the proportion varies considerably (from 5% to 11%) depending on the ethnic and other characteristics of the population studied ( 1 ).
In this review, we seek to provide an overview of some of the characteristic features of well-described forms of atypical diabetes, including examples of those for which the etiological basis is known and others for which the etiological basis is not yet fully understood. Atypical diabetes is suspected in individuals who do not fit clearly into currently accepted criteria that define type 1 diabetes (T1D), type 2 diabetes (T2D), or secondary diabetes ( 1 , 2 ). We introduce the concept of endotypes, in which patients with diabetes can be clustered based on similar clinical or molecular/genetic mechanisms.
Below, we discuss several examples of atypical diabetes, their etiological or mechanistic bases, and their characteristic clinical features. We provide this section as a framework for approaching patients who do not fit accepted criteria of T1D or T2D—rather than as a comprehensive review of all forms of atypical diabetes ( Fig. 1 ).

Conceptualization of diabetes subtypes within three axes: insulin sensitivity, insulin secretion, and islet autoimmunity. The green area represents the normal inverse relationship between insulin sensitivity and insulin secretion. As an individual develops insulin resistance, there is an eventual loss of compensatory insulin secretion. This can result in impaired fasting glucose (pink) and insulin-resistant diabetes (type 2), as shown in dark blue. Autoimmune diabetes (T1D) is featured by overall insulin sensitivity, with near-absolute loss of insulin secretion and a high degree of islet autoimmunity. Individuals with LADA also manifest islet autoimmunity but retain insulin secretory capacity and remain insulin sensitive. Conversely, those with insulin resistance syndromes and lipodystrophies tend to have a high degree of insulin resistance and secrete high levels of insulin. Individuals with many monogenic and mitochondrial forms of diabetes secrete very low levels of insulin and remain insulin sensitive, but lack evidence of islet autoimmunity. KPD, defined according to presentation with DKA, includes four subtypes, each shown in light blue. Patients with A+β+ present with similar metabolic features compared to LADA. A+β− patients metabolically resemble T1D. A − β − individuals have near-complete insulin deficiency but lack evidence for islet autoimmunity. A − β+ patients often manifest insulin resistance with sustained insulin secretory reserve despite presentation with DKA.
Monogenic Diabetes
The term “monogenic diabetes” is typically used to describe nonsyndromic forms of diabetes with demonstration of Mendelian inheritance driven by damaging variants in a single gene. Maturity-onset diabetes of the young (MODY) and neonatal diabetes are the two most well-described forms of monogenic diabetes. Many genes responsible for these disorders are pivotal to β-cell development or function ( 3 ). Importantly, some forms of MODY have proven to be amenable to sulfonylureas, demonstrating an early opportunity for precision medicine in diabetes ( 4 ).
A strong family history of diabetes that typically follows an autosomal dominant pattern of inheritance, with multiple affected generations, is a common hallmark of monogenic diabetes. Affected relatives may be misdiagnosed with T1D or T2D ( 5 ). Distinctive presenting features for some subtypes of MODY may also provide an index of suspicion. A comprehensive review of all forms of MODY is outside of the scope of this review. However, below, we use GCK-MODY, HNF1A-MODY, and neonatal diabetes to illustrate some of the unique etiological and clinical features of monogenic forms of diabetes. Table 1 includes a review of several well-described forms of monogenic and neonatal diabetes, for which a genetic cause has been identified, defining clinical features, and microvascular complications ( 6 ).
Genetic causes of monogenic and neonatal diabetes
GCK-MODY (MODY 2)
GCK-MODY is the most common form of MODY, with demonstration of an autosomal dominant pattern of inheritance ( 7 ). It results from heterozygous pathogenic variants in GCK , the gene encoding glucokinase. Glucokinase performs the rate-limiting step in the conversion of glucose to glucose-6-phosphate within the pancreatic β-cell. Glucose-6-phosphate then enters the tricarboxylic acid cycle, and generates ATP, which triggers a cascade resulting in insulin secretion ( 8 ). Thus, GCK serves as the “glucostat” of the β-cell, regulating insulin secretion. Heterozygous inactivating GCK mutations result in a higher set point of glucose at which insulin is secreted ( 9 ).
Clinically, GCK-MODY presents as mild hyperglycemia in an individual lacking common metabolic risk factors for T2D ( 9 ). Patients often have a history of hemoglobin A 1c (HbA 1c ) levels that oscillate between prediabetes and mild diabetes levels. Importantly, patients with GCK-MODY are not at increased risk for micro- or macrovascular complications of hyperglycemia ( 10 ) and thus do not require pharmacotherapy. Rather, treatment of their diabetes is often frustrating to patients as it results in either no improvement in their blood glucose or significant hypoglycemia ( 11 ). Accurate diagnosis of this condition prevents unnecessary treatment, as microvascular complications of GCK-MODY–related diabetes are exceedingly rare ( 6 ).
HNF1A-MODY (MODY 3)
The second most common form of MODY is HNF1A-MODY. With HNF1A-MODY there is also demonstration of an autosomal dominant pattern of inheritance, and HNF1A-MODY results from heterozygous pathogenic variants in hepatocyte nuclear factor 1α ( HNF1A ) ( 12 ). HNF1A is an important β-cell transcription factor; thus, patients with HNF1A-MODY often develop insulin-deficient diabetes in the second to third decade of life ( 3 ). Microvascular complications of hyperglycemia are common in individuals with HNF1A-MODY without appropriate treatment ( 6 ).
Importantly, HNF1A-MODY is often successfully treated with sulfonylureas, particularly if recognized early in the course of disease ( 13 ). Often, recognition of one family member with HNF1A-MODY can inform cascade testing in family members, with substantial therapeutic impact.
Neonatal Diabetes
Most commonly, neonatal diabetes is caused by loss-of-function variants in the K ATP channel, composed of two subunits encoded by KCNJ11 ( Kir6.2 ) and ABCC8 ( SUR1 ) ( 14 ). Neonatal diabetes is typically diagnosed in the first 6 months of life, and where neonatal diabetes is not recognized early, infants may present with severe hyperglycemia and ketoacidosis ( 14 ). The severity and course of neonatal diabetes are quite variable, with some experiencing only transient metabolic dysregulation and others a more permanent form of diabetes. The most severe form of neonatal diabetes, which occurs in <1 in 1 million live births, is characterized by developmental Delay, Epilepsy, and Neonatal Diabetes (DEND). DEND typically will occur in the setting of KCNJ11 or ABCC8 mutations ( 15 ).
Oligogenic Forms of Diabetes
Initially the field of genetics and diabetes focused on highly penetrant, inherited forms of diabetes that resulted from mutations in a single gene (monogenic diabetes). However, with the explosion of genomic data becoming available over the last several years, attention is increasingly directed toward conditions in which two (digenic) or a few (oligogenic) genes with variant alleles contribute to an inherited form of diabetes. Often, these genes cluster in shared pathways, compounding the effect of multiple genes that individually would not result in significant disease ( 16 ). Examples include a case of digenic MODY with variants in HNF1A and HNF1B ( 17 ) or severe insulin resistance due to heterozygous variants in the PPARG and PPP1R3A genes ( 18 ). In other cases, additional genetic variation can explain variable or incomplete penetrance of the diabetes phenotype ( 19 ). Aided by recent advances in DNA-sequencing technology, increased ascertainment and deeper understanding of digenic and oligogenic models of atypical diabetes will continue to move the field of precision diabetes forward. Additionally, the field of genetics and diabetes has made significant progress in determining the polygenic (tens to hundreds of genes) risk for both T1D and T2D; however, this is outside of the scope of this review ( 20 ).
Syndromic Diabetes
Patients with syndromic forms of diabetes typically present with a range of atypical clinical features in addition to hyperglycemia. Unique combinations of syndromic features may arise from a single molecular defect and can provide a rationale for evaluation by an expert in medical genetics. As with monogenic diabetes, a positive family history may suggest a genetic etiology, although more severe conditions may result from de novo mutational events, thus appearing to be sporadic rather than familial. Similar to MODY, the genes responsible for syndromic forms of diabetes often encode proteins important for β-cell development, function, or survival. However, their expression in other tissues can lead to multiorgan involvement, with common examples including neurological involvement (microcephaly with simplified gyral pattern, epilepsy, and permanent neonatal diabetes syndrome, IER31P1 variants [ 21 ]), other endocrine features (neonatal diabetes mellitus with congenital hypothyroidism syndrome, GLIS3 variants [ 22 ]), skeletal involvement (Wolcott-Rallison syndrome, EIF2AK3 variants [ 21 ]), gastrointestinal involvement (Mitchell-Riley syndrome, RFX6 variants [ 23 ]), or immunological involvement (immunodysregulation, polyendocrinopathy, enteropathy X-linked syndrome, FOXP3 variants [ 24 ]). Below, we detail the characteristic features of Wolfram syndrome as one well-studied example of syndromic diabetes.
Wolfram Syndrome
Wolfram syndrome, also known as diabetes insipidus, diabetes mellitus, optic atrophy, deafness syndrome (DIDMOAD) ( 25 ), is caused by biallelic pathogenic variants in WFS1 or CISD2 and segregates in families in an autosomal recessive pattern. WFS1 encodes wolframin, a transmembrane protein in the endoplasmic reticulum. Aberrant wolframin function leads to endoplasmic reticulum stress and dysregulation of the unfolded protein response on which mature insulin synthesis relies. As such, Wolfram syndrome is considered one of the prototypical endoplasmic reticulum stress disorders ( 21 ).
Patients with classic Wolfram syndrome often present before 16 years of age with antibody-negative, insulin-deficient diabetes. They soon develop optic atrophy and can have additional features of sensorineural hearing impairment, diabetes insipidus, urinary tract abnormalities, progressive neurodegeneration, and psychiatric disorders ( 25 , 26 ). Individuals with Wolfram syndrome due to CISD2 variants tend to be more severely affected and may additionally develop gastrointestinal bleeding ( 27 ).
Mitochondrial Diabetes
Subtypes of mitochondrial diabetes result from mitochondrial dysfunction. The presenting features of mitochondrial disorders can be variable, with organ systems such as the pancreas (particularly β-cells) that require high levels of aerobic metabolism the most likely to be affected. A positive family history is often observed, manifesting as a strictly maternal inheritance pattern in conditions that are caused by variants encoded in the mitochondrial genome or as autosomal recessive inheritance in conditions caused by variants encoded in the nuclear genome. Proper diagnosis of mitochondrial forms of diabetes is paramount, as treatment with metformin, often a first-line medication for T2D, is contraindicated in mitochondrial diabetes due to the increased risk of provoking lactic acidosis ( 28 ).
Clinically, mitochondrial disorders display tremendous clinical and prognostic heterogeneity which is driven in part by the identity of the etiologic variant, its degree of heteroplasmy or homoplasmy (the fraction of mitochondrial genomes in which the variant is present) if encoded in the mitochondrial genome, and cell-to-cell and tissue-to-tissue heterogeneity that is observed in these conditions. The heteroplasmic mitochondrial genome variant c.3243A>G MT-TL1 illustrates some of this complexity: individuals with this variant may develop maternally inherited diabetes-deafness syndrome (MIDD), mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes (MELAS), Leigh syndrome, or a combination of other features observed in individuals with mitochondrial dysfunction. Diabetes, when it develops, may respond well to sulfonylureas or may be characterized by insulinopenia. Age of onset can range from early childhood to ≥40 years of age, although up to 9% of individuals will remain unaffected ( 29 ).
Lipodystrophic Forms of Diabetes
Lipodystrophic forms of diabetes are clinically characterized by loss of body fat, which may be generalized or involve limited areas of the body (“partial lipodystrophy”). Accompanying clinical characteristics include prominent musculature, phlebomegaly, severe hypertriglyceridemia, and profound hepatomegaly resulting from steatohepatitis ( 30 ). The hyperglycemia is driven by insulin resistance, which can manifest with severe acanthosis nigricans ( 30 ). Investigation of lipodystrophic syndromes has shed light on the key role of adipose tissue on metabolism and insulin sensitivity. One such adipokine, leptin, has multiple effects including the promotion of satiety ( 31 ). Another, adipokine, adiponectin, plays a key role in glucose regulation and fatty acid oxidation. Thus, together these hormones prevent complications of obesity and metabolic syndrome ( 31 ). Major categories of lipodystrophy ( 31 ) are summarized below and in Table 2 .
Major categories of lipodystrophies
Distribution limited under REMS program, a program to ensure that prescriptions are being used in accord with FDA-approved indications.
Congenital Generalized Lipodystrophy
Congenital generalized lipodystrophy (CGL) (Berardinelli-Seip syndrome) is characterized by near-complete lack of adipose tissue first diagnosed in infancy ( 32 ). Multiple autosomal recessive forms have been identified, associated with AGPAT2 , BSCL2 , CAV1 , PTRF , PCYT1A , and PPARG ( 30 ). Treatment for diabetes includes metformin and insulin. Notably, extremely high doses of insulin are often required ( 31 ). Fibric acid derivatives and/or statins may be needed to lower severe hypertriglyceridemia ( 31 ). Metreleptin, a recombinant human leptin analog, is approved by the U.S. Food and Drug Administration (FDA) for the treatment of CGL. Notably, metreleptin’s distribution is limited under a risk evaluation and mitigation strategy (REMS) program ( 31 ).
Familial Partial Lipodystrophy
Familial partial lipodystrophy (FPLD) is characterized by localized loss of fat in the limbs, buttocks, and hips. There is a concurrent accumulation of fat in other areas, often resulting in a cushingoid appearance ( 32 ). Unlike with CGL, patients with FPLD typically first present during adolescence ( 31 ). Most forms of FPLD are autosomal dominant and result from heterozygous variants in LMNA , PPARG , AKT2 , or PLIN1 ( 30 ). However, autosomal recessive FPLD also occurs, resulting from biallelic variants in CIDEC , LIPE , or PCYT1A ( 30 ). Diabetes can be treated with metformin, thiazolidinediones, and high-dose insulin. Patients with FPLD often require aggressive management for hypertension and hyperlipidemia ( 31 ).
Progeroid Syndromes
Progeroid syndromes mimic physiological aging. This can include features of premature wrinkles, greying and loss of hair, osteoarthritis, loss of muscle mass, and increased risk of cancer and heart disease ( 33 ). These conditions can result in partial or generalized loss of body fat, and present during childhood ( 31 ). Genes implicated in progeroid lipodystrophy include LMNA , ZMPSTE24 , SPRTN , WRN , BANF1 , FBN1 , CAV1 , POLD1 , and KCNJ6 ( 30 ). Many progeroid forms of lipodystrophy result in relatively mild to moderate diabetes and severe hypertriglyceridemia. Similar to other lipodystrophy syndromes, metformin, thiazolidinediones, and insulin are used in treatment ( 31 ).
Acquired Generalized Lipodystrophy
Acquired generalized lipodystrophy (AGL) (Lawrence syndrome) usually occurs before adolescence and results in progressive loss of whole-body fat ( 34 ). It is often associated with autoimmune diseases and thus is more common in females ( 34 ). Similar to CGL, AGL can be treated with metformin, sulfonylureas, thiazolidinediones, and high-dose insulin. Metreleptin is also FDA approved for the treatment of AGL under the REMS program ( 31 ).
Latent Autoimmune Diabetes
Latent autoimmune diabetes (LADA) is defined by the presence of islet autoantibodies but absence of insulin dependency for at least 6 months after initial diagnosis of diabetes in adults. Often, LADA patients are initially classified as having “T2D.” The frequency of LADA in cohorts of T2D patients varies between 5% and 13% ( 35 – 42 ) depending on geographic location, patient demographics, the numbers of autoantibodies tested, and the sensitivity and cutoffs of the autoantibody assays. Both clinical features and genetic associations suggest that LADA represents a pathophysiologic overlap between T1D and T2D. Genome-wide association studies of European patients diagnosed with LADA compared with both control subjects without diabetes and subjects with T1D and T2D showed genetic correlations with both T1D and T2D ( 43 ). In a subsequent study investigating the genetic etiology of LADA and childhood-onset T1D, both LADA and T1D were associated with MHC class II. However, only T1D was associated with MHC class I. These findings support the possibility that LADA and childhood-onset T1D indeed have distinct genetic bases ( 44 ). Endotypic heterogeneity in LADA could influence the natural history of β-cell dysfunction as well as treatment approaches in these patients ( 41 ). LADA is likely underdiagnosed in clinical practice, since physicians infrequently measure islet autoantibodies in adult patients who do not appear to require insulin therapy at the time of diagnosis. Widespread autoantibody testing in patients (especially nonobese patients) with “T2D” could improve the diagnostic yield, but this conclusion must be tempered with the understanding that true “positivity” in autoantibody assays may depend on the assays used, variable titers for determining cutoffs, the transient nature of some autoantibodies at lower titer, and ethnicity ( 38 , 45 – 49 ).
Ketosis-Prone Diabetes
The defining characteristic of ketosis-prone diabetes (KPD) is diabetic ketoacidosis (DKA) at presentation, in the absence of characteristic features of autoimmune T1D ( 50 ). Strikingly, this class of atypical diabetes is both clinically and etiologically heterogeneous. Four distinct subtypes of KPD have been defined based on quantitative measurements of antibody positivity (A+) or negativity (A−) and presence (β+) or absence (β−) of β-cell functional reserve ( 51 ). Within this classification, A+β− KPD most closely aligns with features of traditional, autoimmune T1D. A−β− KPD also resembles T1D, but does not have detectable islet autoantibodies. Additionally, A−β− KPD harbors a lower frequency of T1D-associated HLA susceptibility alleles ( 51 , 52 ), and demonstrates a lower T1D genetic risk score ( 53 ). Importantly, many patients with A−β− KPD either harbor pathogenic variants in essential β-cell transcription factors or demonstrate occult (T cell–mediated) islet autoimmunity ( 54 , 55 ). Individuals with A+β+ KPD are older and overweight at initial presentation with DKA and tend to have GAD65 autoantibodies with DPD epitope specificity ( 56 ) (which is associated with a milder form of islet autoimmunity) and to possess HLA alleles that are protective against islet autoimmunity ( 52 ). Patients with A−β+ KPD, specifically the subset termed “unprovoked” A−β+ KPD, superficially resemble patients with T2D but present with DKA despite adequate β-cell functional reserve ( 57 ). These patients are able to discontinue insulin therapy within 1–2 months after the initial index episode of DKA and may remain off insulin for several years, maintaining excellent glycemic control on oral therapy alone ( 57 ). Some patients with A−β+ KPD display hypercatabolism of the branched chain amino acid leucine, that explains in part their proclivity to developing ketoacidosis ( 58 ). Others have a defect in intracellular availability of arginine during periods of hyperglycemia, which severely blunts insulin secretory capacity during hyperglycemic crises ( 58 ). Studies in West African patients have suggested a role for herpesvirus 8 infection ( 59 ), and a report from Japan implicates insulin peptide–specific interferon-γ responses in the pathogenesis of KPD ( 60 ). The Aβ classification scheme for KPD has high accuracy in predicting glycemic control and insulin dependence among the different phenotypes of patients presenting with DKA, and pathophysiologic studies based on comparison of the different phenotypic subtypes have demonstrated its value as an endotypic classification ( 61 ).
Fulminant Diabetes
Fulminant diabetes has been described predominantly in patients living in Far Eastern countries. It is characterized by very sudden onset, with patients presenting usually with DKA but with normal or near-normal HbA 1c at diagnosis. Although fulminant diabetes is reported frequently as a subtype of T1D, the patients often lack the typical T1D-associated islet autoantibodies, and the HLA alleles and haplotypes associated with fulminant diabetes are different from those associated with typical autoimmune T1D. Unlike LADA, patients experience a rapid destruction of β-cells within weeks. This results in a discrepancy between their current blood glucose state and their HbA 1c ( 62 ).
Severe Insulin Resistance Syndromes
The etiology of many severe insulin resistance syndromes is not yet fully understood. However, early steps toward elucidation of critical mechanisms underlying disease pathogenesis have been made. Individuals with disorders of severe insulin resistance display features of hyperinsulinemia, such as severe acanthosis nigricans, and differ from those with lipodystrophy syndromes in that they do not manifest adipose tissue loss ( 63 ). Additional features may include hirsutism, polycystic ovary syndrome, impaired growth, and irregular menses. They often require substantial amounts of exogenous insulin to approach glucose homeostasis, and in some cases, hyperglycemia may be preceded by a period of hypoglycemia.
Abnormal function of the insulin signaling pathway drives a subset of severe insulin resistance syndromes, with loss-of-function variants in the gene encoding the insulin receptor ( INSR ). Notably, complete loss-of-function variants in INSR lead to an earlier-onset and more severe presentation of insulin resistance (Donohue syndrome) than with partial loss-of-function variants (Rabson-Mendenhall syndrome), providing a functional rationale for the molecular pathogenesis.
Early evidence suggests that severe insulin resistance syndromes may be amenable to precision therapeutics. For example, insulin sensitizers such as metformin and pioglitazone have shown efficacy in Rabson-Mendenhall syndrome ( 64 ). Other proposed treatment strategies exploit the shared structural homology and interrelated signaling pathways of insulin and insulin-like growth factor-1 (IGF-1); e.g., recombinant IGF-1 treatment can improve glucose control and overall life span in Donohue syndrome ( 65 ).
Type A insulin resistance syndrome results from heterozygous or mild homozygous mutations in INSR . It presents later in life, and women often struggle with menometrorrhagia, ovarian cysts, and subfertility ( 66 ). Type B insulin resistance syndrome, conversely, occurs due to polyclonal antibodies against the insulin receptor. It typically presents in adulthood, primarily in middle-aged women. Patients with type B insulin resistance syndrome will experience both hypo- and hyperglycemia based on antibody-mediated activation and subsequent downregulation of the insulin receptor ( 66 ). Often, type B insulin resistance is diagnosed in the setting of other autoimmune conditions or as part of a paraneoplastic syndrome ( 66 ). Insulin autoimmune syndrome (Hirata disease) is characterized by spontaneous episodes of hypoglycemia due to the presence of high titers of insulin autoantibodies ( 67 ).
Insulin-mediated pseudoacromegaly (IMPA) is an example of severe insulin resistance characterized by accelerated rather than impaired growth. First recognized in 1993, its etiology remained elusive until exome sequencing (ES) was applied for a female proband and sister sharing features of IMPA and their unaffected parents in 2020 ( 68 ). Variant analysis revealed a maternally inherited FGFR1 variant and a paternally inherited KLB variant in both the proband and her sister. Functional studies showed that these variants combined to reduce the insulin-sensitizing impact of FGF21, supporting a digenic model of inheritance in this family and providing the first molecular etiology of IMPA ( 68 ). These findings suggest the enticing possibility that treatment with FGF21 analogs or thiazolidinediones, which induce hepatic FGF21 expression, may be efficacious in this form of atypical diabetes ( 69 , 70 ).
Diabetes Secondary to Pancreatic Disease
Some forms of atypical diabetes are associated with exocrine pancreatic disease, and these are typically referred to as pancreatogenic diabetes, classified by the American Diabetes Association as type 3c diabetes. This class of atypical diabetes comprises a heterogeneous group of conditions that may be inherited or acquired, including cystic fibrosis, hemochromatosis, chronic pancreatitis, fibrocalculous pancreatopathy, pancreatic cancer, pancreatectomy, and congenital pancreatic agenesis ( 71 , 72 ). In many cases, the pathogenesis underlying diabetes development in these conditions is incompletely understood.
Additional Forms of Atypical Diabetes
The representative forms of atypical diabetes described above do not encompass all reported forms of this heterogeneous condition. In Table 3 , we provide a summary of the major forms of atypical diabetes currently known, with their key features manifested as presence or absence of insulin sensitivity, insulin secretion, and autoimmunity, as well as other distinctive clinical characteristics.
Key characteristics of major forms of atypical diabetes
The number of plus (+) and minus (−) signs indicates the degree of difference.
A summary of the approach to a patient with atypical diabetes is outlined in Fig. 2 .

Approach to the patient with atypical diabetes. Features including the aspects of the clinical disease course, family history, and physical exam, as well as informative diagnostic tools, are outlined. When clinical investigation does not yield a definitive atypical diabetes diagnosis, research options may be considered. Image created with BioRender.com .
When to Suspect Atypical Diabetes?
As described above and in Table 3 , atypical diabetes in patients can present in a multitude of ways; hence, a thorough family history is very important. For example, many forms of monogenic diabetes are transmitted in an autosomal dominant manner ( 73 ). A family history of individuals presenting with similar features along multiple generations can be an important clue that prompts the clinician to perform further testing.
The presentation and progression of a patient’s illness can be another important distinguishing feature. For example, syndromic forms of diabetes will present with manifestations in specific affected organ systems. Patients with mitochondrial diabetes often present with deafness or lactic acidosis ( 28 ). A careful medical history can point to a diagnosis of pancreatogenic, fulminant, and slowly progressive forms of diabetes. Conversely, patients with the A−β+ and A+β+ subtypes of KPD will have a striking history of initial presentation with DKA, followed by insulin-free remission within 4–6 months ( 74 ).
Physical examination must be thorough, with specific attention paid to manifestations of insulin resistance, adipose tissue disorders, and the syndromes noted above. It is paramount to diagnose lipodystrophy, as identifying areas and patterns of adipose tissue loss can inform the diagnosis ( 30 ). Patients with lipodystrophic forms of diabetes will often have extremely elevated triglyceride and low HDL cholesterol levels. Patients with insulin resistance syndromes will have characteristic physical findings including severe acanthosis nigricans and hirsutism ( 63 ).
Clinical Tests That Help Identify and Classify Forms of Atypical Diabetes
It is very helpful to measure clinically reliable markers of islet autoimmunity, β-cell function, insulin sensitivity, and genetic variants underlying known forms of monogenic diabetes in patients suspected of having atypical diabetes.
Islet Autoimmunity
The four most common autoantibodies in people with autoimmune diabetes are autoantibodies against GAD (GAD65), islet antigen 2 (IA-2), insulin, and zinc transporter 8 (ZnT8) ( 49 ). Autoantibodies against insulin may be unreliable for patients already treated with exogenous insulin ( 75 ). Autoantibody positivity may wane with time ( 76 , 77 ); hence, it is important to try to measure these when a patient is first diagnosed with diabetes. Identification of patients with high titers of multiple islet autoantibodies strongly suggests autoimmune form of diabetes such as T1D, LADA, or an “A+” subtype of KPD ( 49 , 55 ). The significance of a low titer of a single diabetes autoantibody is not clear ( 78 – 80 ).
It is useful to measure serum insulin or C-peptide levels as a marker of the patient’s endogenous insulin secretory capacity ( 81 ). C-peptide is cleaved from proinsulin as it is processed into mature insulin and is not a component of therapeutic insulin preparations; hence, its serum level can reflect residual β-cell capacity ( 82 ). Different cutoffs of fasting C-peptide levels have been derived in different patient cohorts with varying clinical conditions for determination of whether a patient has adequate β-cell functional reserve ( 83 , 84 ).
For evaluation of insulin secretion in a dynamic fashion, patients can be evaluated with an oral glucose tolerance test (OGTT) ( 85 , 86 ). Glucose and insulin/C-peptide can be drawn at baseline and every 30 min over the course of 120 min after consumption of 75 g (or, in children, 1.75 g/kg) oral glucose solution ( 87 ). Insulin, C-peptide, and glucose data from an OGTT allow the endocrinologist to calculate a range of indices of insulin secretory capacity such as the C-peptide index (CPI): (C-peptide 30min − C-peptide 0min ) / (glucose 30min − glucose 0min ). CPI <0.245 is suggestive of insulin deficiency ( 88 ). Compared with an OGTT, the mixed-meal tolerance test (MMTT) generates a stronger β-cell response as incretin hormones are modulated by ingestion of glucose, protein, and fat ( 89 , 90 ). In the U.S., BOOST High Protein (Nestle Health Science) is commonly used as the “mixed meal,” at a dose of 6 mL/kg with a maximum dose of 360 mL in older children and adults ( 91 ). The OGTT and MMTT can also provide indirect evidence of insulin resistance if the stimulated C-peptide levels remain high throughout the 2-h test in the presence of sustained hyperglycemia ( 92 ).
When performing an OGTT or MMTT is not feasible, the insulin dose–adjusted HbA 1c (IDAA 1c ) measurement can be a helpful surrogate. The IDAA 1c is calculated as follows: HbA 1c (%) + [4 × insulin dose (units/kg/24 h)]. IDAA 1c ≤9 corresponds to a predicted stimulated C-peptide >0.9 ng/mL and partial recovery of β-cell function ( 93 ).
In considering a diagnosis of monogenic diabetes, online probability calculators are available to aid in clinical decision-making. By entering readily available demographic and clinical information such as age at diagnosis, BMI, insulin requirement, and HbA 1c into the calculator, the clinician can obtain a value that indicates the patient’s likelihood of having monogenic diabetes ( 94 ). Such tools provide decision support to order genetic testing and to convince third-party payers to approve such testing. Some literature suggests a cutoff of 36% probability with a positive predictive value of 74.4% in using the Exeter MODY probability calculator ( https://www.diabetesgenes.org/exeter-diabetes-app/ModyCalculator ) ( 87 ).
In the case of pancreatic diabetes, patients may have elevated fecal elastase ( 95 ). For patients with insulin-resistant forms of diabetes it may important to rule out Cushing disease by measuring 24-h urine free cortisol, measuring midnight salivary cortisol, or performing a low-dose dexamethasone suppression test ( 96 ). In the case of overgrowth syndromes, such as IMPA, it is important to rule out growth hormone excess by measuring IGF-1 and growth hormone or by performing a growth hormone suppression test ( 97 ).
Ordering and Interpreting Genetic Testing
Molecular genetic testing is a powerful tool to secure a diagnosis of single-gene atypical diabetes disorders and identify relatives at risk. Until recently, there were limited clinical guidelines regarding when to consider genetic testing for atypical diabetes. The International Society for Pediatric and Adolescent Diabetes (ISPAD) now provides a framework for consideration of testing for well-defined monogenic forms of atypical diabetes, including MODY and neonatal diabetes ( 98 ). Risk calculators, such as the Exeter MODY risk calculator, can provide a more objective approach to assessment of risk and stratification of patients who are most likely to benefit from molecular testing.
Genetic testing approaches have evolved in recent years, with broad-based molecular tests (exome sequencing [ES], array comparative genomic hybridization) demonstrating an increased diagnostic utility in comparisons with targeted gene panels that require a clinician to accurately presuppose the molecular diagnosis. Despite this evolution, some unique variants are most sensitively detected by methodologies other than ES or array comparative genomic hybridization, and the choice of testing should be informed by the sensitivity and specificity of available tests for the suspected diagnosis ( 99 ). From a practical standpoint in the clinic, gene panels and focused testing remain more accessible to many patients, due to high out-of-pocket costs and in some cases limited insurance coverage of ES testing. While the implementation of next-generation sequencing methods has had a tremendous impact on clinical diagnostics in rare disease, implicit bias remains a barrier to equitable access to testing and should be recognized and minimized ( 100 ).
Results of genetic testing can be complex. Pretest counseling of patients is important to address possible results and review the risks, benefits, and potential limitations of testing. Current American College of Medical Genetics and Genomics practice guidelines recommend that diagnostic laboratories follow a standardized interpretation process to classify variants along a spectrum from “benign” to “pathogenic” to describe their functional impact ( 101 ). Within this classification scheme are variants of uncertain significance, for which there is limited evidence to support a classification of “pathogenic/likely pathogenic” or “benign/likely benign.” Variants of uncertain significance can often present a challenge to the clinical interpretation and actionability of results. Fortunately, as new information comes to light about a variant, reanalysis of the patient’s genetic data can lead to more unequivocal reclassification of the variant as benign or pathogenic.
We characterize current precision medicine approaches to atypical diabetes in Table 4 . The future dream of precision diabetes is that all patients will receive a diagnosis of a specific form of diabetes based on an extensive, endotypic classification, with genome sequencing, transcriptomic, and metabolomic data available to clinicians to inform individualized management plans. Currently, such a classification does not exist and the clinical utility of such data in diabetes care is limited. The Rare and Atypical Diabetes Network (RADIANT) exemplifies this approach and research focus needed to elucidate all forms of atypical diabetes, their clinical characteristics, and their molecular and pathophysiological etiologies ( 2 ). This work will inform implementation of omics tools for diagnostic and therapeutic purposes and enable a more complete cataloging and classification of atypical diabetes. Such advances informing diabetes care at an individualized level will be truly transformative when achieved at scale, and current research in atypical diabetes is positioned to establish new standards for the implementation of multiomics in routine clinical care.
Precision approaches to atypical diabetes
SU, sulfonylureas; GLP-1 RA, glucagon-like peptide 1 receptor agonists; HTN, hypertension; IPEX syndrome, immunodysregulation, polyendocrinopathy, enteropathy X-linked syndrome; MEDS, microcephaly with simplified gyral pattern, epilepsy, and permanent neonatal diabetes syndrome; NDH, neonatal diabetes mellitus with congenital hypothyroidism; PCOS, polycystic ovary syndrome; SGLT-2i, sodium–glucose cotransporter 2 inhibitors; TG, triglycerides; TZDs, thiazolidinediones.
This article is featured in podcasts available at diabetesjournals.org/care/pages/diabetes_care_on_air .
Note Added in Proof. Between initial publication of this article online and its final publication online and in print, the genes KLF11 , PAX4 , and BLK were removed from Table 1 due to a recent refutation of their roles in monogenic diabetes.
Acknowledgments. J.E.P. is an editor of Diabetes Care but was not involved in any of the decisions regarding review of the manuscript or its acceptance.
Funding. S.I.S. is supported by a K08 grant from the National Institutes of Health (NIH) (DK124574). The authors are also supported by the RADIANT study, funded by the National Institute of Diabetes and Digestive and Kidney Diseases.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. S.I.S. researched and authored sections pertaining to monogenic, syndromic, mitochondrial, severe insulin resistance lipodystrophic, and pancreatic diabetes. S.I.S. also researched and authored the section on the approach to the patient with atypical diabetes. A.B. researched and authored sections on LADA, KPD, and fulminant diabetes. J.E.P. researched and authored sections on defining atypical diabetes, ordering and interpreting genetic testing, and atypical diabetes and precision medicine. All authors reviewed and edited the manuscript in its entirety.
Handling Editors. The journal editors responsible for overseeing the review of the manuscript were Steven E. Kahn and Adrian Vella.
Email alerts
- Online ISSN 1935-5548
- Print ISSN 0149-5992
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
BRIEF RESEARCH REPORT article
Usability evaluation of the educational website “understanding my diabetes” for mexican patients with type 2 diabetes.

- 1 Unidad de Investigación en Epidemiología Clínica, Hospital General Regional No. 1 “Dr. Carlos Mac Gregor Sánchez Navarro” Instituto Mexicano del Seguro Social, Ciudad de México, Mexico
- 2 Unidad de Medicina Familiar Número 7, Coordinación de Educación e Investigación en Salud, Instituto Mexicano del Seguro Social, Ciudad de México, Mexico
- 3 Departamento de Salud Publica, Facultad de Medicina, Universidad Nacional Autónoma de México, Ciudad de México, Mexico
Background: Diabetes education is an integral part of the treatment for the metabolic control of patients with diabetes. The use of the Internet as a tool for diabetes education, as well as its acceptance, is still under study.
Aim: To assess the usability of the educational website “I understand my diabetes” designed for patients with type 2 diabetes attending primary care clinics.
Material and method: A cross-sectional study was done in 110 patients with type 2 diabetes from two family medicine clinics, each of whom was assigned a user account on the educational website “Entiendo mi diabetes.” The web site assigned a user name and password to each patient. They were able to access the educational website at home. After a 15-day review period, participants were asked to evaluate usability using the Computer System Usability Questionnaire. Additionally, we developed an eight-item questionnaire usability focusing on diabetes care. Sociodemographic data, blood pressure, and anthropometric measurements were recorded. Glucose levels and lipid profiles were also measured.
Results: The patients with diabetes had a mean age of 52.7 years and a median of 5 years since they were diagnosed with diabetes. The website received a good usability rating from 89.1% of participants, with favorable assessments in all three dimensions: 87.3% for information, 85.5% for quality, and 88.2% for interface. Regarding usability specifically for diabetes care, 98.2% rated it as having good usability.
Conclusion: The website for education about the disease in patients “I understand my diabetes” had an adequate usability evaluation by patients, so they also considered it very useful for diabetes care. The diabetes care instrument had adequate usability and reliability.
Introduction
Type 2 diabetes (T2D) is defined as a group of metabolic disorders characterized by chronic hyperglycemia. It is the result of impaired insulin secretion, deficient effectiveness, or both conditions ( 1 ). Globally, in 2019, its estimated prevalence was 9.3%, affecting 463 million people, and it is projected to increase to 700 million by 2045. Moreover, it is estimated that approximately 50.1% of individuals with T2D are unaware of their condition ( 2 ).
In Mexico, the prevalence of T2D was 9.5% in 2016, and 18.3% (5.8% were new diagnosis) in 2022 ( 3 ). The objectives of comprehensive treatment are to achieve glycemic control with a glycated hemoglobin (HbA1c) level < 7%, with a primary focus on reducing long-term micro and macrovascular complications ( 4 ).
In the 2016 National Health and Nutrition Survey (Ensanut 2016) the researchers reported that 68.2% of the population diagnosed with diabetes in Mexico has poor metabolic control (HbA1c ≥ 7%) ( 5 ). Since this persistent poor glycemic control, the increase in the prevalence of T2D and the late diagnosis of the disease, it is necessary to promote strategies to adopting a healthy lifestyle and disease care. Metabolic control in patients with diabetes must have a comprehensive approach, according to the physician care, pharmacological treatment, and initiatives to promote a healthy lifestyle.
Diabetes education is a crucial component for instilling knowledge about the disease, promoting self-care, and encouraging positive lifestyle changes ( 6 , 7 ). Furthermore, evidence suggests that providing diabetes education reduces the risk of condition related mortality ( 8 ).
Over the past two decades, there has been a growing use of Health Information and Communication Technologies (ICTs) for providing diabetes education and monitoring indicators ( 9 ). It has been demonstrated that these tools can contribute to improving HbA1c levels, body composition, knowledge of the disease, and the adoption of a healthy lifestyle ( 9 , 10 ).
Nevertheless, it has been reported that educational websites lack validated information, have accessibility issues, and exhibit variability with regard to the quality of the information, its updating, ease of use and comprehension ( 11 , 12 ).
The term “usability” is defined as the degree to which users can perform tasks accurately and efficiently ( 13 ). According to the International Organization for Standardization (ISO 9241), usability refers to the efficiency, effectiveness, and satisfaction of users in a specific context ( 14 ). Usability reports exist for developments involving the use of ICTs in diabetes, indicating a range from 38 to 80% ( 15 , 16 ). Limitations include difficulty completing multiple steps to achieve an objective, limited functionality and interaction, navigation challenges, as well as a high abandonment rate. In addition, patient difficulties in accessing and experiencing educational websites have been documented ( 17 ).
The persistent increase of patients with diabetes makes it difficult to provide education about the disease in primary care; therefore, implementing strategies with the use of ICTs, designed by clinicians with experience in diabetes, as well as in the culture, educational level and social environment of the patients, becomes an imperative need. In this sense, it is required to have digital tools adapted to the end user, which are easy to use and understand, as well as useful to improve the knowledge of T2D and promote its care.
In Mexico, the usability of systems designed to provide diabetes education is even more limited than that reported in other countries. In this sense, our research group developed an educational site called “Understanding my diabetes” which was built by physicians, nutritionists, and diabetes educators with more than 10 years of experience. The diabetes web site was validated by a consensus of experts ( 18 ).
Therefore, the aim of this study is to measure the usability of the educational website “Understanding my diabetes” for ease awareness of the condition and improve self-management in patients with T2D, attending primary clinics care.
Materials and methods
Study design and population.
A descriptive cross-sectional study was conducted among patients affiliated with two family medicine clinics of the Instituto Mexicano del Seguro Social (Mexican Institute of Social Security, IMSS) in Mexico City from September 2021 to May 2022.
The study was approved by the Ethics and Research Committee at IMSS with registration number R-2021-3609-025. Patients were invited to participate in the study during their clinic appointments. The participating researchers provided information about the study to the patients, answered their questions and, once they decided to participate voluntarily, their consent was requested by signing the informed consent form.
The sample size was calculated based on the assessment of the usability of the educational program and findings reported in a similar study ( 19 ). A formula was used for proportion, with a confidence level of 95%, an expected proportion of 1.21, and a margin of error of 0.10, resulting in a total of 92 participants. To account for a 20% potential loss (participants cannot completing the assessment), 110 patients were included in the study.
Selection criteria
The study included patients who were previously diagnosed with T2D by their treating physician, aged 18 or older, and who had been diagnosed less than 10 years ago. Participants needed to be literate, to have access to a home computer or smartphone, and possess internet connectivity. Patients with severe complications of the disease, such as chronic kidney disease requiring replacement therapy, blindness, amputation, or any condition that hindered the evaluation of the educational website (visual impairment, or psychological conditions), were excluded.
Patients with severe complications of the disease, such as chronic kidney disease (patients that requiring replacement therapy), blindness, amputation, or any condition that hindered the evaluation of the educational website (visual impairment, or psychological conditions) were excluded ( Figure 1 ).
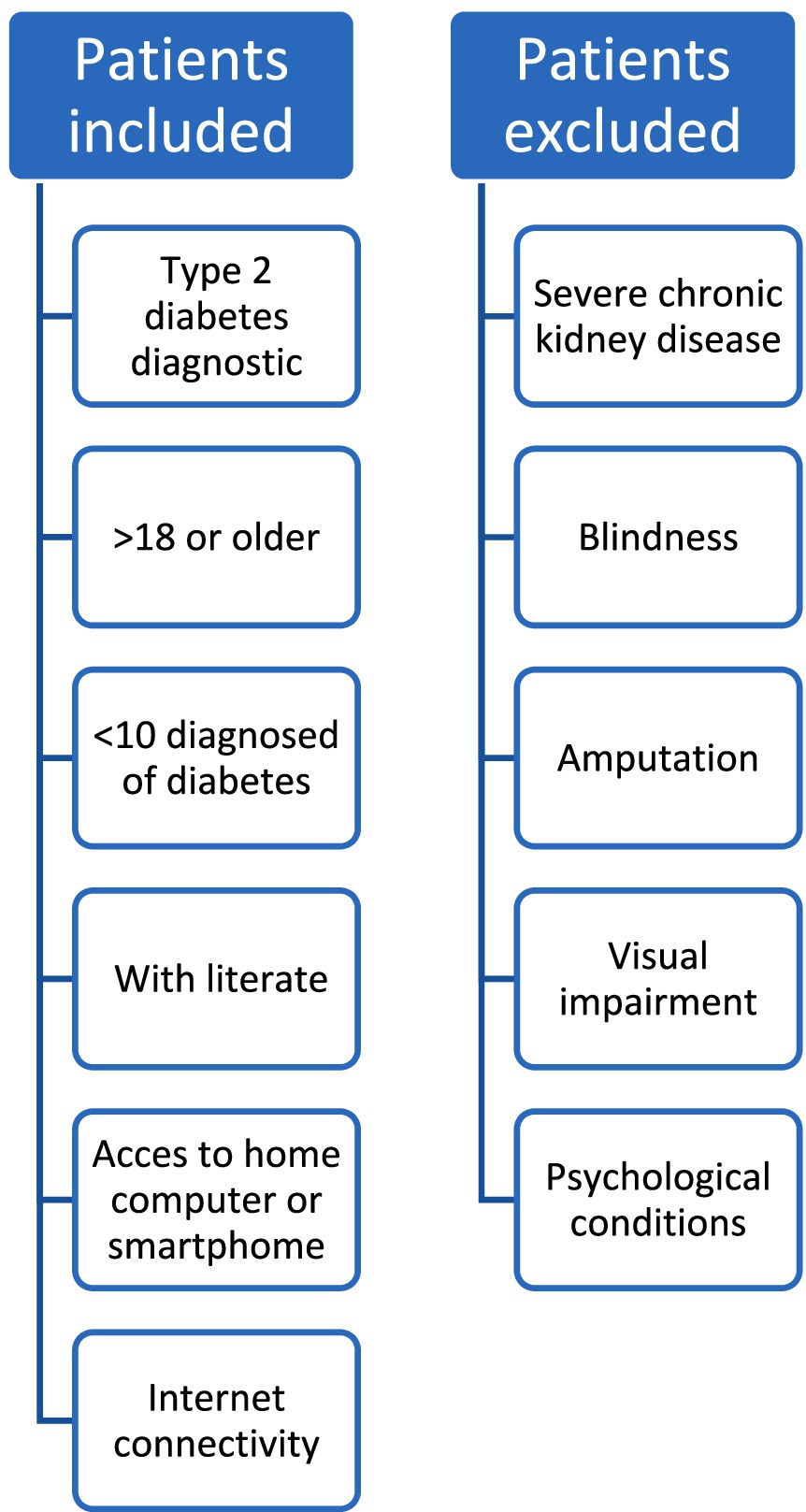
Figure 1 . Selection criteria.
Sociodemographic and clinical measurements
The collection of sociodemographic and clinical data was conducted by participating medical and nutrition staff. Blood pressure readings were recorded, measured by a healthcare professional on two occasions using a mercury sphygmomanometer, with a five-minute interval between each reading. Patients were requested to remain seated for more than 5 min before the readings. The recorded blood pressure value was the average of the two measurements.
Socioeconomic status
The socioeconomic status was assessed using the INEGI questionnaire known as AMAI, comprising 7 levels. To categorize participants into three socioeconomic classes, a scoring system defined by the authors of the instrument was employed: a score between 0 and 111 points indicated a low socioeconomic level, 112–204 points indicated a medium level, and a score of ≥205 indicated a high socioeconomic level ( 20 ).
Anthropometric measurements
Anthropometric measurements were recorded by two nutritionists who received prior training and standardization through a training course.
Two nutritionists took a training course for the standardization of measurements. They recorded the anthropometric measurements of the sample. They followed the Habitch method, adhering to the specifications recommended by Lohman and colleagues ( 21 , 22 ). Body weight was measured on a calibrated SECA ® model 813 scale, with participants wearing light clothing. Height was measured using a SECA ® model 220 stadiometer, with the patient positioned with their back to the scale following the Frankfort plane. The body mass index (BMI) was calculated.
Waist circumference (WC) was measured with a SECA® measuring tape, with the reference point at the midpoint between the lowest rib and the upper edge of the iliac crest on the right side. Both measurements were assessed at three different times, and the mean value of the second and third measurements was used for recording and analysis.
Biochemical measurements
Biochemical indicators were measured in venous blood after a 10-h fasting period. High-Performance Liquid Chromatography (HPLC) was employed. Automated photometry (Roche Cobas 800 c701) was used for the measurement of glucose, total cholesterol levels, and triglycerides.
Educational Website “Entiendo mi diabetes” in Spanish language. Este sitio web educativo fue desarrollado por el equipo investigador, compuesto de medicos especialistas de familia, de medicina interna, nutriólogos, epidemiologos, educadores en diabetes, informáticos, que participan con el equipo de investigación. The educational course was implemented on the Moodle platform at the website www.entiendomidiabetes.com by a team of web developers. The course comprises modules on understanding diabetes, pharmacological treatment, control indicators, nutrition, myths surrounding diabetes, complications related to the disease, depression, and family support. These modules are designed in a straightforward manner, incorporating visual resources and minimal text. The use of videos facilitates easy comprehension. Each module includes didactic or reinforcing activities with the aim of motivating patients to actively manage their health.
These educational modules were validated through an expert consensus, including physicians, nutritionists, psychologists, and diabetes educators. The validation process was conducted blindly and in pairs, assessing the content validity of the educational modules, which has been previously reported ( 18 ).
This course is managed over Moodle, the free open- source Learning Platform and can be visited at: http://entiendomidiabetes.com/moodle28/login/index.php .
Usability measurement instrument
The level of usability was assessed using the Computer System Usability Questionnaire (CSUQ), validated in the Mexican population ( 23 ).
The instrument comprises 16 items that evaluate three main domains: system quality (items 1–6), information quality (items 7–12), and interface quality (items 13–16). The instrument utilizes a 7-level Likert scale, ranging from completely disagree “1“to completely agree “7.” In order to assess usability, a total of 112 points were used, categorized into tercile: low usability (<37 points), moderate (38–74 points), and high usability (>75 points). Regarding the dimensions, for a maximum quality score of 42 points, (low quality ≤14 points, moderate 15 to 28 points, and high quality ≥29 points). Patients created their username and password for the educational site, and after interacting with the site, from login to the complete review of one of the modules, they were asked to complete the usability questionnaire.
Diabetes care instrument
A research team consisting of two-family physicians, two nutritionists, and two diabetes educators designed a 10-item questionnaire aimed at measuring usability for diabetes care. Following a second content analysis review, two items were eliminated as they were deemed repetitive. Eight items were included, focusing on measuring understanding of content (items 1 and 2), items directed toward positive changes in disease care (items 3–7), and likelihood to recommend the educational site to others (item 8). A Likert scale ranging from 1 to 7 was used. A score of 8–24 was considered low usability in diabetes care, 25–40 as moderate, and ≥41 as high usability.
Statistical analysis
The data were analyzed using the statistical package SPSS, version 25. Qualitative variables characterizing the population and the type of usability of the educational program are presented in frequencies and proportions. The Kolmogorov–Smirnov normality test was employed to identify the distribution of quantitative variables. For variables with a parametric distribution, mean and standard deviation were used, while for those with a non-parametric distribution, median and interquartile range were utilized.
The usability of each item in the instrument was measured through the mean and standard deviation.
To assess the scale reliability of the diabetes usability instrument CSUQ and the instrument of diabetes care, Cronbach’s alpha was calculated.
To identify the association between usability and qualitative variables with sociodemographic and clinical variables, the chi-square test was employed. A statistically significant difference was considered with a p -value < 0.05.
The sociodemographic characteristics and data of the studied population are presented in Table 1 .
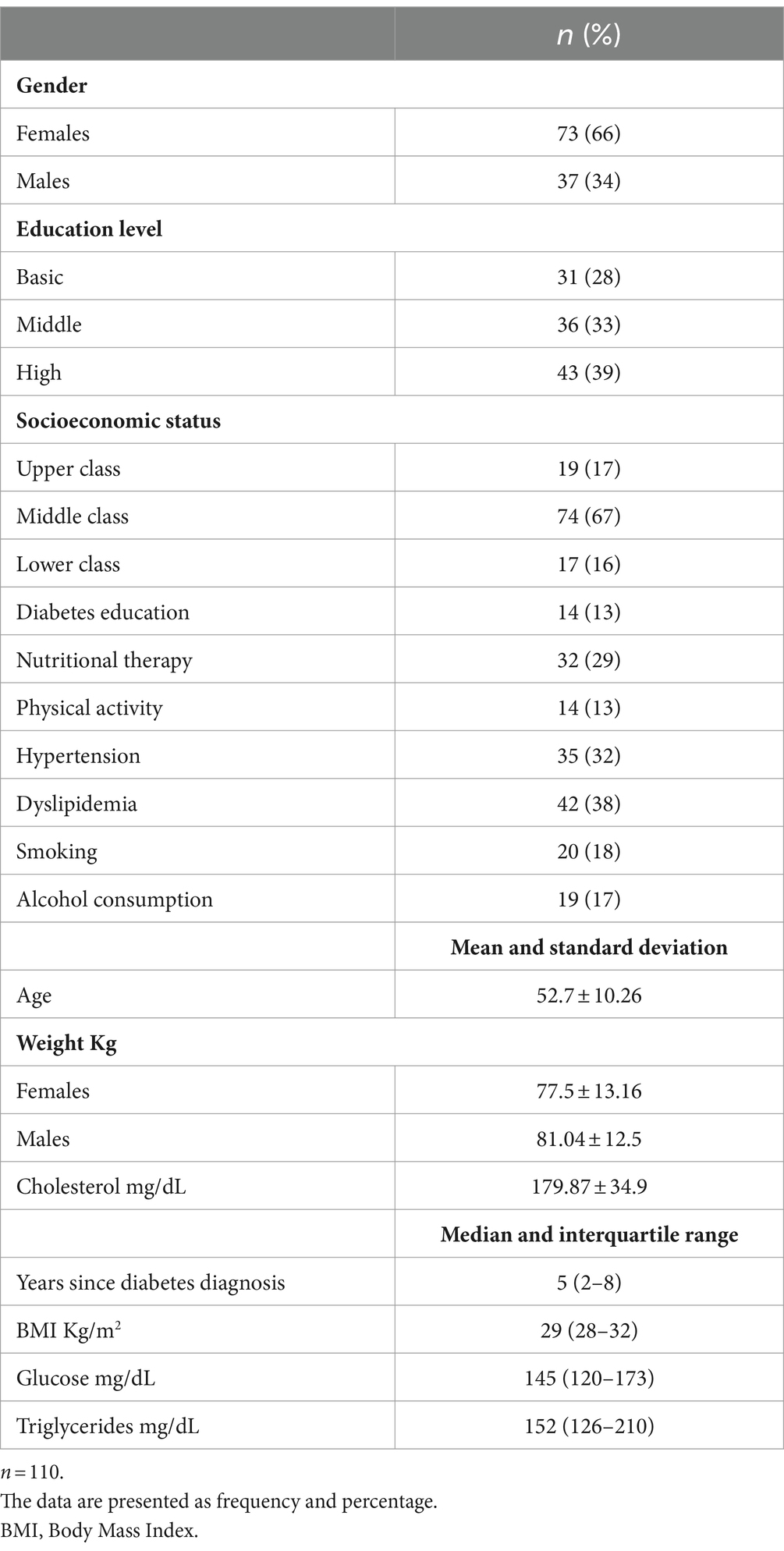
Table 1 . Sociodemographic characteristics of the studied population with diabetes.
A total of 110 patients were included, 66% were female. The average age of the study population was 52.7 ± 10.2 years, with a median diabetes diagnosis duration of 5 years. The most frequently reported level of education was higher education (39%), while the most frequently identified socioeconomic level was middle class, (67%). Thirteen percent received diabetic education and 32% of the patients studied received nutritional therapy previously.
Thirteen percent received diabetic education and 32% of the sample received nutritional therapy previously. The median BMI was 29 kg/m 2 , and fasting glucose was 145 mg/dL.
Table 2 displays the rating for each item in the usability instrument of the educational site. The highest average rating was 6.47 for the item addressing assistance in completing tasks, whereas the lowest was 6.03, pertaining to resolving issues on the website. The mean of usability of the educational website was 94.76 ± 15.48 and the reliability test was 0.97 ( Table 3 ). The usability of the website using the diabetes instrument shows that 98.2% of patients rated it as high and 1.2% as regular.
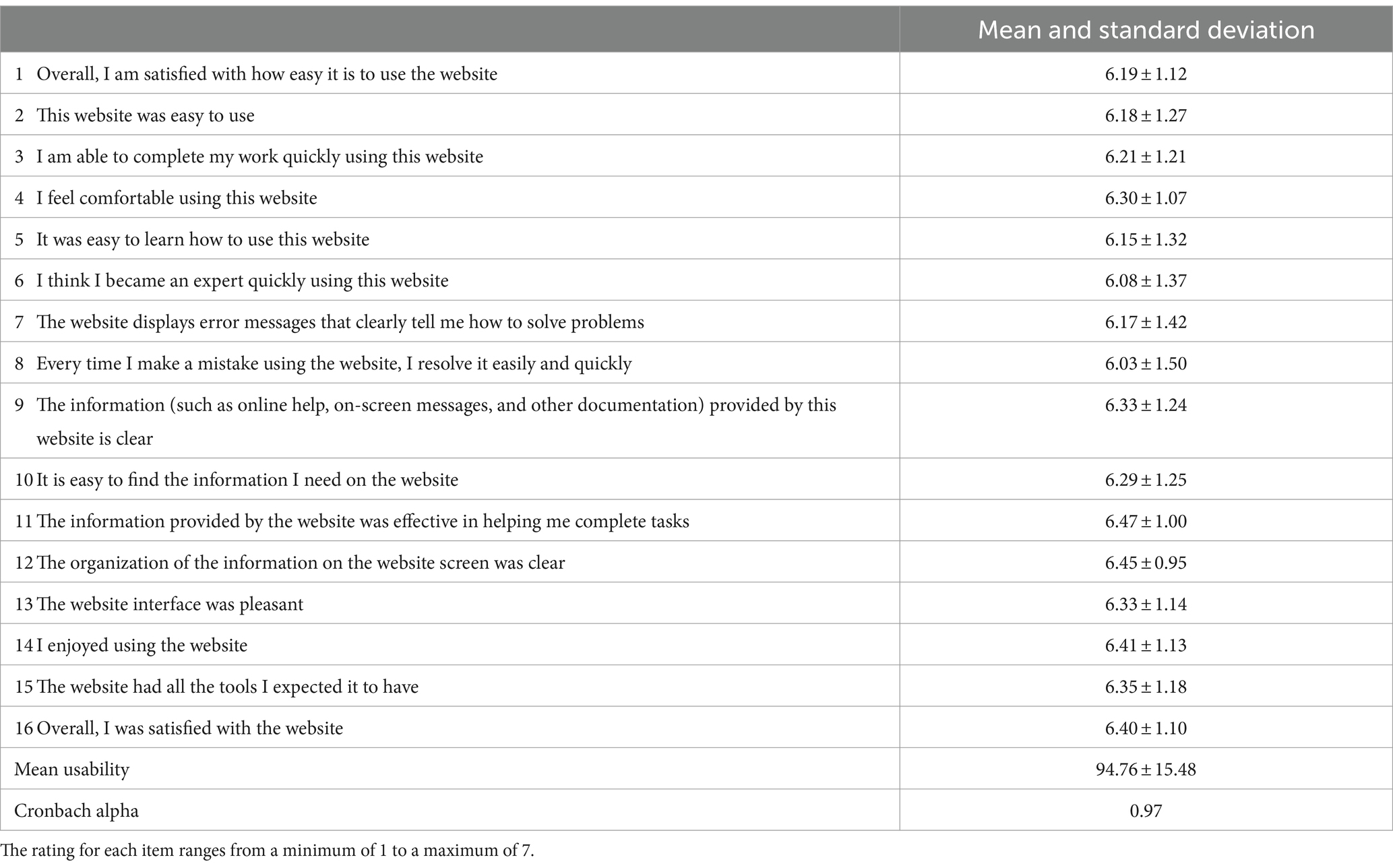
Table 2 . Usability rating of the educational website “Entiendo mi diabetes.”
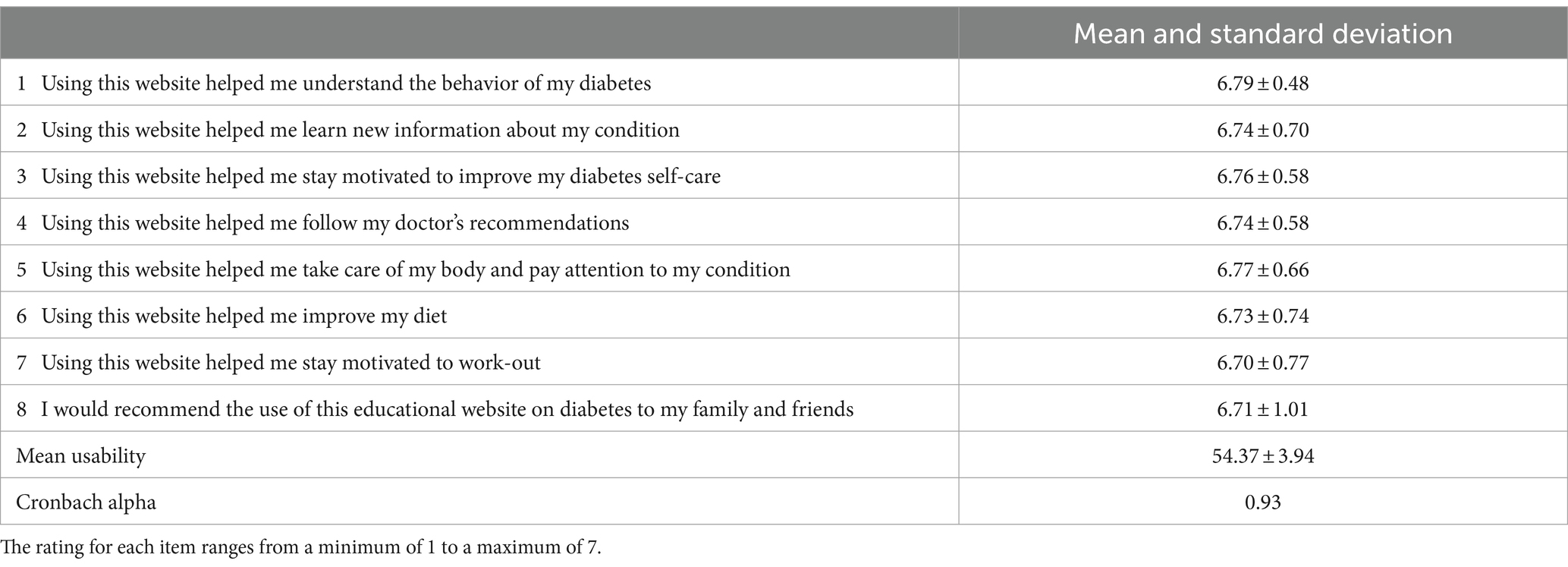
Table 3 . Usability level of the educational site related to aspects of diabetes care.
The usability description is presented in Figure 2 , revealing that 89.1% of the patients rated it as high usability, 9.1% as moderate, and 1.8% as low usability. In Figure 3 , the three dimensions of usability from the instrument are illustrated, indicating high usability across all three dimensions: 87.3% for information, 85.5% for quality, and 88.2% for the interface.
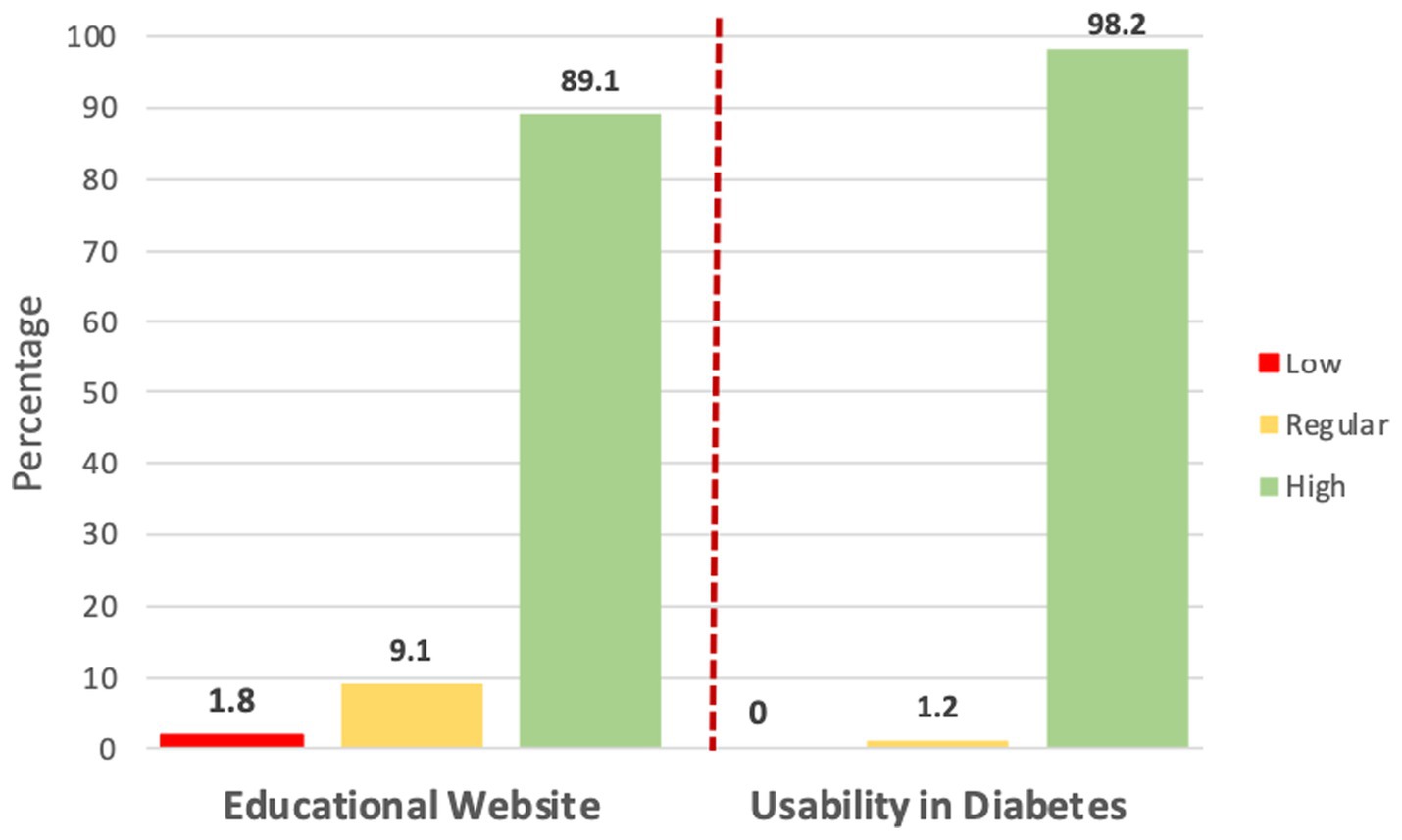
Figure 2 . Usability level of the educational website “Entiendo mi diabetes”.
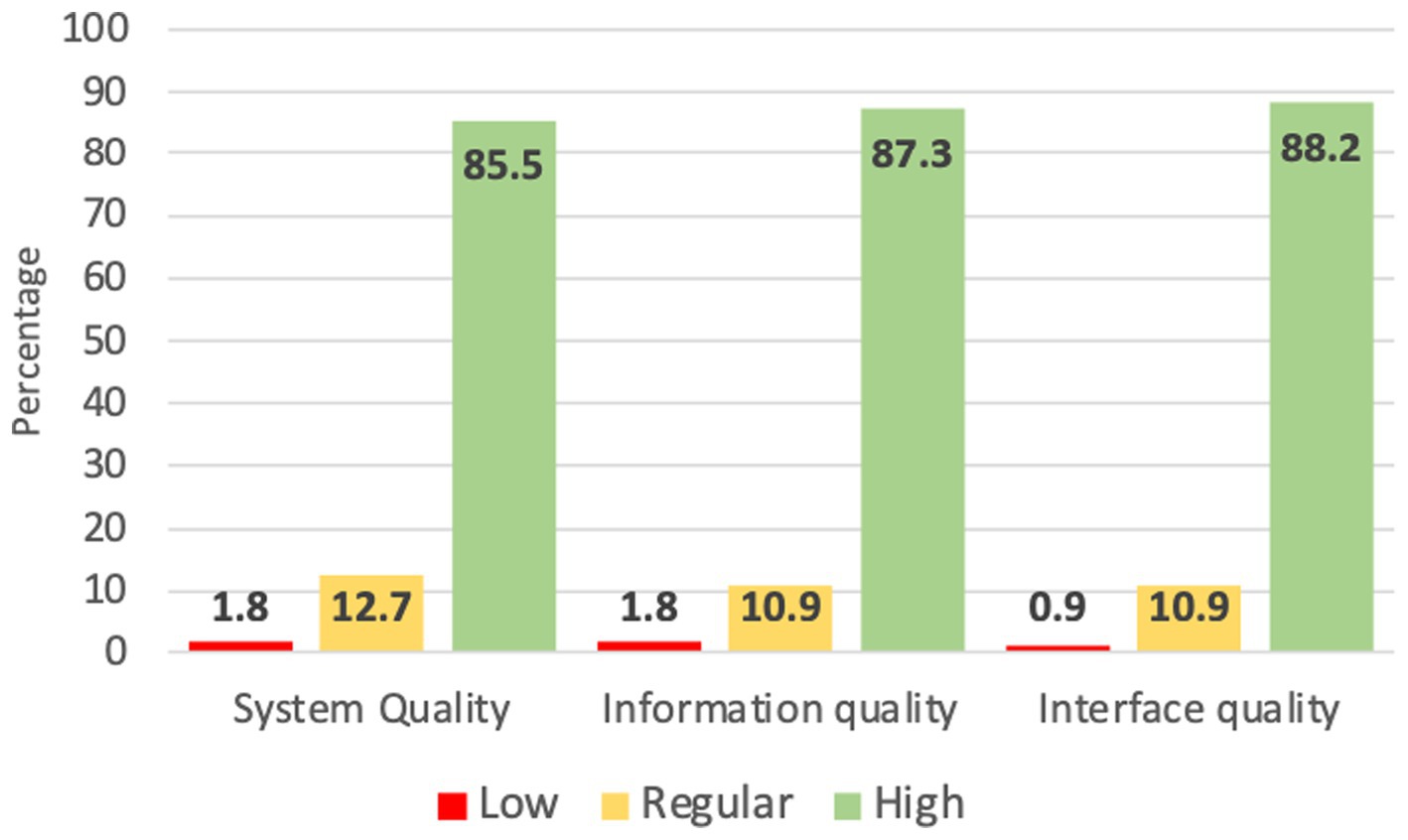
Figure 3 . Usability in the dimensions of the website “Entiendo mi diabetes”.
Regarding the average rating of the 8 items in the instrument aimed at measuring usability in diabetes care, 98.2% rated it as having high usability. The highest average rating was related to understanding the behavior of diabetes (6.79), while the lowest was motivation for physical exercise (6.70). The overall mean usability of the diabetes care instrument was 54.37 ± 3.94 and the reliability value was 0.93.
Low, moderate, and high usability were compared with sociodemographic variables, prior diabetes education, socioeconomic level, education level, and marital status, with no statistically significant differences found among them. There was no difference between glycemic control and type of usability; the data are presented in Table 4 .
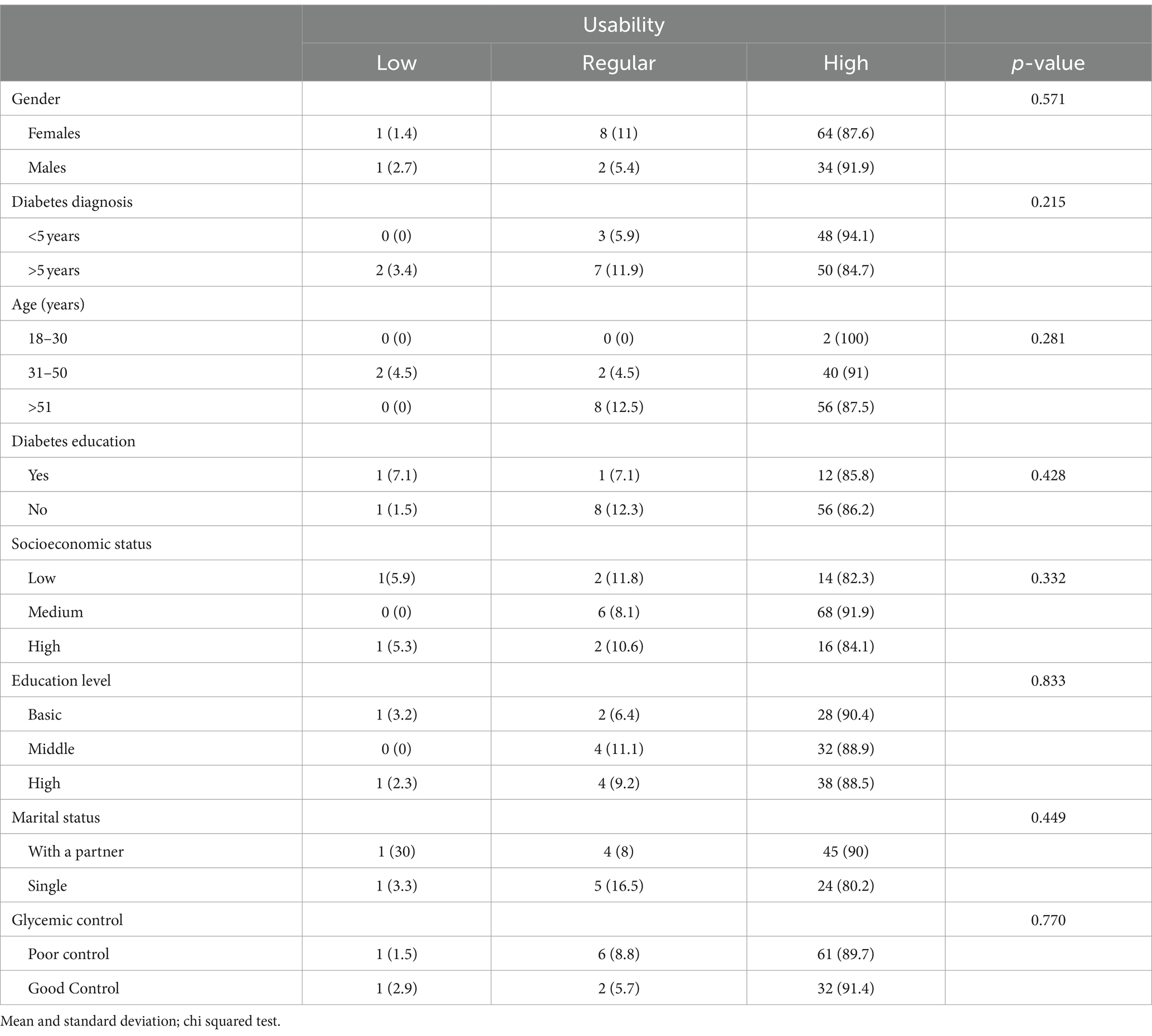
Table 4 . Usability level and its association with sociodemographic and clinical variables.
Diabetes education is a fundamental component of comprehensive patient care and is essential for achieving metabolic control, as well as reducing or preventing the complications associated with the disease. Information and Communication Technologies (ICTs) are valuable tools, especially in healthcare areas where there is a high demand for medical care.
In the present study, the usability of an educational website on diabetes is reported, with 89% of patients rating the educational tool as highly usable. Nine out of ten patients found it useful, easy to use, and of adequate quality. Authors who have assessed usability in patients with diabetes using an app have consistently rated ease of use and learning highly, while the lowest ratings were for trust and quality of interaction with the app. Additionally, those with a lower educational level tended to rate it more favorably ( 19 ). It has been reported that with the implementation of web-based educational programs, patients with lower diabetes education have a higher perception of the risk of complications. In this study, however, no differences in the usability of the educational program were found when comparing it with the level of education or socioeconomic status ( 24 ). This could be explained by the fact that the website “Entiendo mi diabetes” included simple, easily understandable information presented interactively to facilitate patient understanding and action in caring for their health. Even though age could be a limiting factor for the use of educational tools with ICTs, no differences in usability were observed.
When considering the dimensions of the usability instrument, more than 85% of the studied patients believed that the educational program met, provided adequate information, and was easy to use. It is important to highlight aspects of quality that the educational content was designed by nutritionists and clinical doctors specializing in diabetes care in primary care clinics. Moreover, it underwent a validation process by clinical experts.
Other authors have assessed usability using the CSUQ program, and this study is one of the few that has demonstrated the level of usability of an educational program, finding a higher rating than what other authors have reported ( 25 , 26 ).
It was observed that patients perceive an adequate system quality, meeting expectations, and the interface quality proves to be intuitive, generating user satisfaction. These results align with findings from other authors, suggesting that usability improves when a multidisciplinary team is involved in creating educational programs for patients. However, it becomes more valuable when patients are involved in the evaluation process ( 27 ).
It is essential to highlight that only 29% of the population had received in-person diabetes education at their clinic. Therefore, continuing the development of web-focused educational materials can be of significant value, enabling patients to receive diabetes education remotely. Additionally, it can serve as a motivating factor for them to manage their condition effectively from the time they receive a diagnosis.
In this regard, healthcare professionals are typically the ones evaluating educational programs. Therefore, it becomes necessary for the system’s quality to meet user expectations, to assess the quality of information and its comprehension, and ensure that the interface is intuitive for the user. Other authors have reported the usability of an app prototype for diabetic foot self-care in end-users, identifying high usability due to the fact that the tool was centered around user needs and requirements ( 28 ).
Prior to implementing an educational program using ICTs, evaluation by experts in the medical, nutrition, and diabetes education fields, as well as by software developers for its implementation, is crucial. Finally, the development should undergo assessment by end users. One of the strengths of this study was the design of an instrument to measure usability focused on aspects of diabetes care. The instrument developed had adequate reliability, with a Cronbach’s Alpha value of 0.93. It was found that 98% of participants considered the educational program useful for understanding the disease, for promoting diabetes care and adherence to diet and exercise. To date, there is limited information on patient satisfaction for diabetes management websites in Mexico.
Among the limitations of the present study is the cross-sectional design. Future studies should assess the usability at various stages throughout the duration of an educational program. Additionally, there should be increased participation of women in the study, as they are the ones who most frequently seek medical attention.
It is crucial that healthcare professionals become guides in the use of technologies as new methods of learning. It has been reported that this approach increases patient trust, a better adherence to treatment and motivation in health education can be achieved ( 29 , 30 ). When the patients become acquainted with an education web site it is necessary and very important the follow-up by healthcare professionals. This contributes to assessing the long-term effectiveness of interventions of ICTs.
On the other hand, in patients with type 2 diabetes in Mexico, poor glycemic control has been reported in 2016 National Health and Nutrition Survey (Ensanut 2016). This survey showed that 68.2% of patients do not achieve metabolic control, furthermore they present a late diagnosis, and high prevalence of overweight and obesity. Then, with this conditions, the sample have a higher risk of developing complications of the disease, such as kidney or cardiovascular disease ( 5 ).
There is a high demand for health services for patients with type 2 diabetes in primary care units in Mexico. By the year 2022, it was estimated that the IMSS would care for 4.2 million patients with diabetes. 64% of the care in primary care clinics at the IMSS was for diabetes ( 31 ).
According to this high demand for health care, provide diabetes education becomes a complex task. Therefore, digital tools to provide pharmacological treatment and diabetes education at a distance could contribute to improve metabolic control, promove a healthy lifestyle and acquire knowledge of diabetes to avoid complications of the disease. In addition, providing diabetes education through ICTs could reduce the costs of the disease in patients with type 2 diabetes, as well as improve the perception of their quality of life, as previously reported ( 32 ).
The educational diabetes website received a high usability rating from nine out of ten patients. Furthermore, the study revealed that the educational program was deemed useful and easily comprehensible, addressing key aspects to inform and motivate self-care in diabetes. User interaction and satisfaction remained unaffected by factors such as age, education, or socioeconomic status. Assessing usability is crucial for enhancing the end-user experience, with significant implications for adherence and motivation in utilizing digital tools for health education. There is an emphasis on the importance of granting patients access to new knowledge through simple and user-friendly tools, underscoring the need for reinforcement by healthcare professionals.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by COMITE DE ETICA E INVESTIGACIÓN, INSTITUTO MEXICANO DEL SEGURO SOCIAL. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
GO: Investigation, Validation, Writing – original draft. SV: Investigation, Writing – original draft. CI: Investigation, Writing – original draft, Methodology. AM: Writing – original draft, Conceptualization, Formal analysis. LV: Conceptualization, Formal analysis, Investigation, Methodology, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article. This study received funding from the Instituto Mexicano del Seguro Social, in the call for priority projects, with a number in the Fund FIS/IMSS/PROT/PRIO/18/O84.
Acknowledgments
The authors would like to thank the authorities of the participating clinics for the facilities granted to carry out this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Petersmann, A, Müller-Wieland, D, Müller, UA, Landgraf, R, Nauck, M, Freckmann, G, et al. Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes . (2019) 127:S1–7. doi: 10.1055/a-1018-9078
Crossref Full Text | Google Scholar
2. Saeedi, P, Petersohn, I, Salpea, P, Malanda, B, Karuranga, S, Unwin, N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9(th) edition. Diabetes Res Clin Pract . (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
PubMed Abstract | Crossref Full Text | Google Scholar
3. Basto-Abreu, A, López-Olmedo, N, Rojas-Martínez, R, Aguilar-Salinas, CA, Moreno-Banda, GL, Carnalla, M, et al. Prevalencia de prediabetes y diabetes en México: Ensanut 2022. Salud Publica Mex . (2023) 65:s163–8. doi: 10.21149/14832
4. American Diabetes Association Professional Practice Committee . Improving care and promoting health in populations: standards of medical Care in Diabetes-2022. Diabetes Care . (2022) 45:S8–s16. doi: 10.2337/dc22-S001
5. Basto-Abreu, A, Barrientos-Gutiérrez, T, Rojas-Martínez, R, Aguilar-Salinas, CA, López-Olmedo, N, De la Cruz-Góngora, V, et al. Prevalence of diabetes and poor glycemic control in Mexico: results from Ensanut 2016. Salud Publica Mex . (2020) 62:50–9. doi: 10.21149/10752
6. Davis, J, Fischl, AH, Beck, J, Browning, L, Carter, A, Condon, JE, et al. 2022 National Standards for diabetes self-management education and support. Sci Diab Self Manag Care . (2022) 48:44–59. doi: 10.1177/26350106211072203
7. Chrvala, CA, Sherr, D, and Lipman, RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ Couns . (2016) 99:926–43. doi: 10.1016/j.pec.2015.11.003
8. He, X, Li, J, Wang, B, Yao, Q, Li, L, Song, R, et al. Diabetes self-management education reduces risk of all-cause mortality in type 2 diabetes patients: a systematic review and meta-analysis. Endocrine . (2017) 55:712–31. doi: 10.1007/s12020-016-1168-2
9. ElSayed, NA, Aleppo, G, Aroda, VR, Bannuru, RR, Brown, FM, Bruemmer, D, et al. 2. Classification and diagnosis of diabetes: standards of care in diabetes—2023. Diabetes Care . (2023) 46:S19–40. doi: 10.2337/dc23-S002
10. Velázquez-López, L, Muñoz-Torres, AV, Medina-Bravo, P, Vilchis-Gil, J, Klϋnder-Klϋnder, M, and Escobedo-de la Peña, J. Multimedia education program and nutrition therapy improves HbA1c, weight, and lipid profile of patients with type 2 diabetes: a randomized clinical trial. Endocrine . (2017) 58:236–45. doi: 10.1007/s12020-017-1416-0
11. Holtz, BE . Evaluating the most popular diabetes websites in the USA: a content analysis. Health Promot Int . (2020) 35:1394–405. doi: 10.1093/heapro/daaa008
12. Guan, Y, Maloney, KA, Roter, DL, and Pollin, TI. Evaluation of the informational content, readability and comprehensibility of online health information on monogenic diabetes. J Genet Couns . (2018) 27:608–15. doi: 10.1007/s10897-017-0155-y
13. Cockton, G . The encyclopedia of human-computer interaction: Usability evaluation. Obtenido de Interaccion Design Foundation (2012).
Google Scholar
14. ISO . ISO W. 9241-11. Ergonomic requirements for office work with visual display terminals (VDTs). The International Organization for Standardization . (1998) 45
15. Fu, H, McMahon, SK, Gross, CR, Adam, TJ, and Wyman, JF. Usability and clinical efficacy of diabetes mobile applications for adults with type 2 diabetes: A systematic review. Diabetes Res Clin Pract . (2017) 131:70–81. doi: 10.1016/j.diabres.2017.06.016
16. Yu, CH, Parsons, J, Mamdani, M, Lebovic, G, Shah, BR, Bhattacharyya, O, et al. Designing and evaluating a web-based self-management site for patients with type 2 diabetes--systematic website development and study protocol. BMC Med Inform Decis Mak . (2012) 12:57. doi: 10.1186/1472-6947-12-57
17. Georgsson, M, and Staggers, N. Patients' perceptions and experiences of a mHealth diabetes self-management system. Comput Inform Nurs . (2017) 35:122–30. doi: 10.1097/CIN.0000000000000296
18. Velázquez López, L, Achar de la Macorra, R, Colin Ramirez, E, Muñoz Torres, AV, Pineda Del Aguila, I, Medina Bravo, PG, et al. The diabetes education material on diabetes for website: results of a validation process. J Healthc Qual Res . (2023) 38:346–53. doi: 10.1016/j.jhqr.2023.07.001
19. Janatkhah, R, Tabari-Khomeiran, R, Asadi-Louyeh, A, and Kazemnejad, E. Usability of a disease management Mobile application as perceived by patients with diabetes. Comput Inform Nurs . (2019) 37:413–9. doi: 10.1097/CIN.0000000000000532
20. AMAI ANSE . Nota Metodológica. Asociación Mexicana de Agencias de Inteligencia de Mercado y Opinión. Comité de Nivel Socioeconómico AMAI (2017) (2018).
21. Habicht, J . Standardization of quantitative epidemiological methods in the field. Bol Oficina Sanit Panam . (1974) 76:375–84.
PubMed Abstract | Google Scholar
22. Lohman, TG, Roche, AF, and Martorell, R. Anthropometric standardization reference manual (1988).
23. MarÃ-A Isolde Hedlefs, A, Gl, ADLG, Martha Patricia Sã¡nchez, M, and Andrea Abigail Garza, V. Adaptacià 3 n al español del Cuestionario de Usabilidad de Sistemas Informáticos CSUQ / Spanish language adaptation of the computer systems usability questionnaire CSUQ. RECI Revista Iberoamericana de las Ciencias Computacionales e Informática . (2016) 4:84. doi: 10.23913/reci.v4i8.35
24. Gerber, BS, Brodsky, IG, Lawless, KA, Smolin, LI, Arozullah, AM, Smith, EV, et al. Implementation and evaluation of a low-literacy diabetes education computer multimedia application. Diabetes Care . (2005) 28:1574–80. doi: 10.2337/diacare.28.7.1574
25. Baghaei, N, Nandigam, D, Casey, J, Direito, A, and Maddison, R. Diabetic Mario: designing and evaluating Mobile games for diabetes education. Games Health J . (2016) 5:270–8. doi: 10.1089/g4h.2015.0038
26. Vaziri, DD, Aal, K, Ogonowski, C, Von Rekowski, T, Kroll, M, Marston, HR, et al. Exploring user experience and technology acceptance for a fall prevention system: results from a randomized clinical trial and a living lab. Eur Rev Aging Phys Act . (2016) 13:6. doi: 10.1186/s11556-016-0165-z
27. Poduval, S, Ross, J, Pal, K, Newhouse, N, Hamilton, F, and Murray, E. Web-based structured education for type 2 diabetes: interdisciplinary user-centered design approach. JMIR Hum Factors . (2022) 9:e31567. doi: 10.2196/31567
28. Marques, ADB, Moreira, TMM, Jorge, TV, Rabelo, SMS, Carvalho, R, and Felipe, GF. Usability of a mobile application on diabetic foot self-care. Rev Bras Enferm . (2020) 73:e20180862. doi: 10.1590/0034-7167-2018-0862
29. Lee, JJN, Abdul Aziz, A, Chan, ST, Raja Abdul Sahrizan, R, Ooi, AYY, Teh, YT, et al. Effects of mobile health interventions on health-related outcomes in older adults with type 2 diabetes: A systematic review and meta-analysis. J Diabetes . (2023) 15:47–57. doi: 10.1111/1753-0407.13346
30. Fang, Y, Chau, AKC, Wong, A, Fung, HH, and Woo, J. Information and communicative technology use enhances psychological well-being of older adults: the roles of age, social connectedness, and frailty status. Aging Ment Health . (2018) 22:1516–24. doi: 10.1080/13607863.2017.1358354
31. Medina-Chávez, JH, Vázquez-Parrodi, M, Mendoza-Martínez, P, Ríos-Mejía, ED, de Anda-Garay, JC, and Balandrán-Duarte, DA. Protocolo de Atención Integral: prevención, diagnóstico y tratamiento de diabetes mellitus 2. Rev Med Inst Mex Seguro Soc . (2022) 60:S4.
32. Cunningham, SG, Stoddart, A, Wild, SH, Conway, NJ, Gray, AM, and Wake, DJ. Cost-utility of an online education platform and diabetes personal health record: analysis over ten years. J Diabetes Sci Technol . (2023) 17:715–26. doi: 10.1177/19322968211069172
Keywords: type 2 diabetes, health information technology, usability, website, diabetes education
Citation: Ortíz GO, Vega García S, Islas Salinas C, Muñoz Torres AV and Velázquez López L (2024) Usability evaluation of the educational website “understanding my diabetes” for Mexican patients with type 2 diabetes. Front. Public Health . 12:1394066. doi: 10.3389/fpubh.2024.1394066
Received: 29 February 2024; Accepted: 23 April 2024; Published: 10 May 2024.
Reviewed by:
Copyright © 2024 Ortíz, Vega García, Islas Salinas, Muñoz Torres and Velázquez López. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lubia Velázquez López, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Prediction model for low bone mass mineral density in type 2 diabetes: an observational cross-sectional study
- Original Article
- Published: 09 May 2024
Cite this article

- Cheng Ji 1 , 2 na1 ,
- Jie Ma 3 na1 ,
- Lingjun Sun 4 na1 ,
- Lijuan Liu 3 ,
- Lijun Wang 3 ,
- Weihong Ge 1 &
Considering the prevalence of type 2 diabetes (T2D), osteoporosis should be considered a serious complication. However, an effective tool for the assessment of low bone mass mineral density (BMD) in T2D patients is not currently available. Therefore, the aim of our study was to establish a simple-to-use risk assessment tool by exploring risk factors for low BMD in T2D patients.
This study included 436 patients with a low BMD and 381 patients with a normal BMD. Multiple logistic regression analysis was performed to evaluate risk factors for low BMD in T2D patients. A nomogram was then developed from these results. A receiver operating characteristic (ROC) curve, calibration plot, and goodness-of-fit test were used to validate the nomogram. The clinical utility of the nomogram was also assessed.
Multivariate logistic regression indicated that age, sex, education, body mass index (BMI), fasting C-peptide, high-density cholesterol (HDL), alkaline phosphatase (ALP), estimated glomerular filtration rate (eGFR), and type I collagen carboxy terminal peptide (S-CTX) were independent predictors for low BMD in T2D patients. The nomogram was developed from these variables using both the unadjusted area under the curve (AUC) and the bootstrap-corrected AUC (0.828). Calibration plots and the goodness-of-fit test demonstrated that the nomogram was well calibrated.
Conclusions
The nomogram-illustrated model can be used by clinicians to easily predict the risk of low BMD in T2D patients. Our study also revealed that common factors are independent predictors of low BMD risk. Our results provide a new strategy for the prediction, investigation, and facilitation of low BMD in T2D patients.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Data availability
The datasets generated and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
P. Saeedi, I. Petersohn, P. Salpea, B. Malanda, S. Karuranga, N. Unwin et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Pract. 157 , 107843 (2019)
Article PubMed Google Scholar
V. Tai, W. Leung, A. Grey, I.R. Reid, M.J. Bolland, Calcium intake and bone mineral density: systematic review and meta-analysis. BMJ 351 , h4183 (2015)
Article PubMed PubMed Central Google Scholar
I. Perez-Diaz, G. Sebastian-Barajas, Z.G. Hernandez-Flores, R. Rivera-Moscoso, H.K. Osorio-Landa, A. Flores-Rebollar, The impact of vitamin D levels on glycemic control and bone mineral density in postmenopausal women with type 2 diabetes. J. Endocrinol. Investig. 38 , 1365–1372 (2015)
Article CAS Google Scholar
P. Jackuliak, J. Payer, Osteoporosis, fractures, and diabetes. Int. J. Endocrinol. 2014 , 1–10 (2014).
Article Google Scholar
A. H. Mohammed, Sweet Bones: The pathogenesis of bone alteration in diabetes. J. Diabetes Res. 2016 , 1–5 (2016).
Google Scholar
N. Bonnet, Bone-derived factors: a new gateway to regulate glycemia. Calcif. Tissue Int. 100 , 174–183 (2017)
Article CAS PubMed Google Scholar
Z. VoVokó, K. Gáspár, A. Inotai, C. Horváth, K. Bors, G. Speer, Osteoporotic fractures may impair life as much as the complications of diabetes. J. Eval. Clin. Pract. 23 , 1375–1380 (2017)
J. Panula, H. Pihlajamäki, V.M. Mattila, P. Jaatinen, T. Vahlberg, P. Aarnio et al. Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet. Disord. 12 , 105 (2011)
R. Hasserius, M.K. Karlsson, B. Jonsson, I. Redlund-Johnell, O. Johnell, Long-term morbidity and mortality after a clinically diagnosed vertebral fracture in the elderly–a 12-and 22-year follow-up of 257 patients. Calcif. Tissue Int. 76 , 235–242 (2005)
E. Hernlund, A. Svedbom, M. Ivergård, J. Compston, C. Cooper, J. Stenmark et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch. Osteoporos. 8 , 136 (2013)
Article CAS PubMed PubMed Central Google Scholar
L. Si, T.M. Winzenberg, Q. Jiang, M. Chen, A.J. Palmer, Projection of osteoporosis-related fractures and costs in China: 2010-2050. Osteoporos. Int. 26 , 1929–1937 (2015)
J. Starup-Linde, M. Frost, P. Vestergaard, B. Abrahamsen, Epidemiology of fractures in diabetes. Calcif. Tissue Int. 100 , 109–121 (2017)
R. Tibshirani, Regression shrinkage and selection via the lasso: a retrospective. J. R. Stat. Soc.: Ser. B (Stat. Methodol.) 73 , 273–282 (2011)
S.H. Tella, J.C. Gallagher, Prevention and treatment of postmenopausal osteoporosis. J. Steroid Biochem. Mol. Biol. 142 , 155–170 (2014)
P. Garnero, E. Sornay-Rendu, F. Duboeuf, P.D. Delmas, Markers of bone turnover predict postmenopausal forearm bone loss over 4 years: the OFELY study. J. Bone Miner. Res. 14 , 1614–1621 (2011)
C. De-Laet, J.A. Kanis, A. Odén, H. Johanson, O. Johnell, P. Delmas et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos. Int. 16 , 1330–1338 (2005)
V. Benetou, P. Orfanos, D. Feskanich, K. Michaëlsson, U. Pettersson-Kymmer, L.A. Ahmed et al. Education, marital status, and risk of hip fractures in older men and women: the CHANCES project. Osteoporos. Int. 26 , 1733–1746 (2015)
H. Nakagawa, M. Kamimura, K. Takahara, H. Hashidate, A. Kawaguchi, S. Uchiyama et al. Changes in total alkaline phosphatase level after hip fracture: comparison between femoral neck and trochanter fractures. J. Orthop. Sci. 11 , 135–139 (2006)
K.Y. Kang, Y.S. Hong, S.H. Park, J.H. Ju, Increased serum alkaline phosphatase levels correlate with high disease activity and low bone mass mineral density in patients with axial spondyloarthritis. Semin. Arthritis Rheum. 45 , 202–207 (2015)
M.A. Hansen, K. Overgaard, B.J. Riis, C. Christiansen, Role of peak bone mass and bone loss in postmenopausal osteoporosis: 12 year study. BMJ 303 , 961–964 (1991)
M. Li, Y. Li, W. Deng, Z. Zhang, Z. Deng, Y. Hu et al. Chinese bone turnover marker study: reference ranges for C-terminal telopeptide of type I collagen and procollagen I N-terminal peptide by age and gender. PLoS One 9 , e103841 (2014)
K.C. Tsolis, E.S. Bei, I. Papathanasiou, F. Kostopoulou, V. Gkretsi, K. kalantzaki et al. Comparative proteomic analysis of hypertrophic chondrocytes in osteoarthritis. Clin. Proteom. 12 , 12 (2015)
D.J. Papachristou, H.C. Blair, Bone and high-density lipoprotein: the beginning of a beautiful friendship. World J. Orthop. 7 , 74–77 (2016)
N.I. Papachristou, H.C. Blair, K.E. Kypreos, D.J. Papachristou, High-density lipoprotein (HDL) metabolism and bone mass. J. Endocrinol. 233 , R95–R107 (2017)
I.K. Jeong, S.W. Cho, S.W. Kim, H.J. Choi, K.S. Park, S.Y. Kim et al. Lipid profiles and bone mineral density in pre- and postmenopausal women in Korea. Calcif. Tissue Int. 87 , 507–512 (2010)
K.C. Kim, D.H. Shin, S.Y. Lee, J.A. Im, D.C. Lee, Relation between obesity and bone mineral density and vertebral fractures in Korean postmenopausal women. Yonsei Med. J. 51 , 857–863 (2010)
S. Nagpal, S. Na, R. Rathnachalam, Noncalcemic actions of vitamin D receptor ligands. Endocr. Rev. 26 , 662–687 (2005)
A.G. Pittas, J. Lau, F.B. Hu, B. Dawson-Hughes, The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 92 , 2017–2029 (2007)
Y. Song, L. Wang, A.G. Pittas, L.C. Del Gobbo, C. Zhang, J.E. Manson et al. Blood 25-Hydroxy Vitamin D Levels and Incident Type 2 Diabetes. Diabetes Care 36 , 1422–1428 (2013)
R. BaBasu, E. Breda, A.L. Oberg, C.C. Powell, C. Dalla Man, A. Basu et al. Mechanisms of the age-associated deterioration in glucose tolerance: contribution of alterations in insulin secretion, action, and clearance. Diabetes 52 , 1738–1748 (2003)
A. Udristioiu, Alkaline Phosphatase Isoenzymes and Leukocyte Alkaline Phosphatase Score in Patients with Acute and Chronic Disease: a Brief Review. Br. J. Med. Med. Res. 4 , 340–350 (2013)
S. Baim, P.D. Miller, Perspective: assessing the clinical utility of serum CTX in postmenopausal osteoporosis and its use in predicting risk of osteonecrosis of the jaw. J. Bone Min. Res 24 , 561–574 (2009)
S. Vasikaran, C. Cooper, R. Eastell, A. Griesmacher, H.A. Morris, T. Trenti et al. International Osteoporosis Foundation and International Federation of Clinical Chemistry and Laboratory Medicine position on bone marker standards in osteoporosis. Clin. Chem. Lab Med. 49 , 1271–1274 (2011)
P. Garnero, E. Hausherr, M.C. Chapuy, C. Marcelli, H. Grandjean, C. Muller et al. Markers of bone resorption predict hip fracture in elderly women: the EPIDOS Prospective Study. J. Bone Min. Res. 11 , 1531–1538 (1996)
N. Napoli, R. Strollo, D. Sprini, E. Maddaloni, G.B. Rini, E. Carmina, Serum 25-OH Vitamin D in relation to Bone Mineral Density and Bone Turnover. Int. J. Endocrinol. 2014 , 487463 (2014)
Download references
Acknowledgements
The authors thank Daphne Liao, Pharm.D. and Lei Zou, Pharm.D of MCPHS University for linguistic review of the manuscript.
This work was supported by the Pharmacy Scientific Research Project of Zhengda Tianqing Hospital of Jiangsu Pharmaceutical Association (grant numbers:TQ2021006) and the Clinical Research Special Fund Cultivation Project of Nanjing Drum Tower Hospital (grant numbers:2021-LCYJ-PY-33).
Author information
These authors contributed equally: Cheng Ji, Jie Ma, Lingjun Sun
Authors and Affiliations
Department of Pharmacy, Drum Tower Hospital Affiliated to Nanjing University Medical School, Nanjing, Jiangsu, China
Cheng Ji & Weihong Ge
Nanjing Medical Center for Clinical Pharmacy, Nanjing, Jiangsu, China
Department of Pharmacy, Peking University Shenzhen Hospital, Shenzhen, Guangdong, China
Jie Ma, Lijuan Liu & Lijun Wang
Department of Endocrinology, The Fourth Affiliated Hospital of Nanjing Medical University, Nanjing, Jiangsu, China
Lingjun Sun
Department of Pharmacy, The First Hospital Affiliated to China Pharmaceutical University, Nanjing, Jiangsu, China
Department of Endocrinology, Drum Tower Hospital Affiliated to Nanjing University Medical School, Nanjing, Jiangsu, China
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Weihong Ge or Yan Bi .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Ethics approval and consent to participate
All procedures of the research were performed in accordance with ethical principles for medical research involving human subjects of the 1964 Helsinki Declaration and its later amendments. The study was approved by the Clinical Research Ethics Committee of the Nanjing drum tower hospital. All participants had signed the informed consent form.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Ji, C., Ma, J., Sun, L. et al. Prediction model for low bone mass mineral density in type 2 diabetes: an observational cross-sectional study. Endocrine (2024). https://doi.org/10.1007/s12020-023-03500-w
Download citation
Published : 09 May 2024
DOI : https://doi.org/10.1007/s12020-023-03500-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Type 2 diabetes
- Osteoporosis
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Type 2 diabetes mellitus is a disorder that is known for disrupting the way your body uses glucose (sugar); it also causes other problems with the way your body stores and processes other forms of energy, including fat. All the cells in your body need sugar to work normally. Sugar gets into the cells with the help of a hormone called insulin.
Insulin is a hormone made by your pancreas that acts like a key to let blood sugar into the cells in your body for use as energy. If you have type 2 diabetes, cells don't respond normally to insulin; this is called insulin resistance. Your pancreas makes more insulin to try to get cells to respond. Eventually your pancreas can't keep up ...
Education and Support. Diabetes is complicated, and it takes practice to manage it in your everyday life. You may be wondering about eating balanced meals, engaging in safe physical activity, checking blood sugar, or giving yourself injectable medicines. Diabetes self-management education and support (DSMES) services help you with all these ...
Causes. Type 2 diabetes is mainly the result of two problems: Cells in muscle, fat and the liver become resistant to insulin As a result, the cells don't take in enough sugar. The pancreas can't make enough insulin to keep blood sugar levels within a healthy range. Exactly why this happens is not known.
Understanding Type 2 Diabetes. The following symptoms of diabetes are typical. However, some people with type 2 diabetes have symptoms so mild that they go unnoticed. Common symptoms of diabetes: Urinating often. Feeling very thirsty. Feeling very hungry—even though you are eating. Extreme fatigue. Blurry vision.
140 to 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) is diagnosed as prediabetes. 200 mg/dL (11.1 mmol/L) or higher after two hours suggests diabetes. Screening. The American Diabetes Association recommends routine screening with diagnostic tests for type 2 diabetes in all adults age 35 or older and in the following groups:
In this section you will learn: Basic Facts About Diabetes: The definition, symptoms, diagnosis, and goals of treatment. What is type 2 diabetes?: Information about how people develop type 2 diabetes and who gets type 2 diabetes. How The Body Processes Sugar: Information about the natural control of blood sugar, and what is different when you ...
The modules can be read in any order. However, if you are newly diagnosed, it is best to start at the beginning in Understanding Diabetes, and work your way through the material. Below you will find a guide to each module. As you will see, depending upon your individual therapy, you can choose exercise guidelines and self-management sections ...
The three main types of diabetes are type 1, type 2, and gestational diabetes. People can develop diabetes at any age. Both women and men can develop diabetes. Type 1 Diabetes Type 1 diabetes, which used to be called juvenile diabetes, develops most often in young people; however, type 1 diabetes can also develop in adults. In type 1 diabetes, your
Listen to the newest episodes of our podcast. Our podcast episodes feature special guests ranging from patients, advocates, experts and more. Our conversations focus on practical information about diabetes. Experts in various fields related to diabetes will give advice about day-to-day living. Patients share their stories.
Type 2 diabetes is a chronic disease that requires several daily self-management decisions and complex care activities. Clinical management of diabetes and teaching patients diabetes self-management skills are necessary for optimal type 2 diabetes control. Diabetes self-management education (DSME) and support require time and resources.
Podemos ayudarte. Whatever your diabetes device or medication needs, ADA's Consumer Guide can help. Get ADA gear, meal planning resources, and access our publications. Get resources for professionals. If you or a loved one has diabetes or prediabetes, we have resources for you. From diabetes support groups to insulin affordability resources ...
Click on any of the links below to access helpful materials on managing all aspects of diabetes that can be printed and given to your patients . Introductory Information. Diabetes Mellitus Type 1: Symptoms, diagnosis, prevention, and treatment (e.g., insulin) Diabetes Mellitus Type 2: Symptoms, diagnosis, prevention, and treatment (e.g ...
Diabetes Advisor VISIT DIABETES.ORG OR CALL 800-DIABETES (800-342-2383) FOR MORE RESOURCES FROM THE AMERICAN DIABETES ASSOCIATION.® Understanding Type 2 Diabetes Needing to take medication, including insulin, to manage your type 2 diabetes does not mean you failed. Taking medication is simply part of good diabetes management. The most important
Learn about ADA's work with the National Diabetes Prevention Program. Consumer Guide. Explore products for diabetes management ... Patient Education Library ... Audience. Resource Type. Sort by: Date. Alphabetical. Relevancy. Resource Language: English. Types of Physical Activity. Learn more about the options and types of physical activity that ...
Treatment for type 2 diabetes. The treatment for type 2 diabetes may be a simple as lifestyle changes (diet, exercise and weight management) with one or two pills to many different pills and/or insulin or other injected medications. Your medical team will help you decide the best choices for you. Pills. Other medications.
Learn about diabetes and prediabetes, how to prevent complications, and how to take charge of your health with diabetes. Find fact sheets on topics such as healthy eating, medicines, eyes, feet, teeth, ears, mental health, and more.
As already mentioned, type 2 diabetes symptoms often come on gradually and can be quite vague at first. Many people have type 2 diabetes for a long period of time before their diagnosis is made. The most common type 2 diabetes symptoms are: Being thirsty a lot of the time. Passing large amounts of urine.
But with type 2 diabetes, your body doesn't make enough insulin, use it well, or both—and your body's cells can't use blood glucose for the energy it needs. When blood glucose isn't used and your blood glucose levels rise, it can cause serious problems. Taking medication. Medication is an important part of managing type 2 diabetes.
Patient Education Resources Independent Medical Education ... Type 2 Diabetes Patient Case Simulation ... Simulating a Patient-Centered Approach to Optimize Early Glycemic and Weight Control in Type 2 Diabetes. Learn more about glycemic control and weight management in type 2 diabetes. Start Simulation
Use of an SGLT-2 inhibitor is recommended to reduce the risk for all-cause mortality, major adverse cardiovascular events (MACE), progression of CKD, and hospitalization due to congestive heart failure [CHF]. Clinicians should prioritize adding SGLT-2 inhibitors in patients with type 2 diabetes and CHF or CKD.
The A1C blood test measures your average blood sugar level over the past two to three months. The goal A1C for most young people with type 2 diabetes is 7 percent (53 mmol/mol) or less, which corresponds to an average blood sugar of approximately 150 mg/dL (8.3 mmol/L) ( table 1 ). Lowering your A1C level reduces your risk for kidney, eye, and ...
Atypical diabetes is suspected in individuals who do not fit clearly into currently accepted criteria that define type 1 diabetes (T1D), type 2 diabetes (T2D), or secondary diabetes (1,2). We introduce the concept of endotypes, in which patients with diabetes can be clustered based on similar clinical or molecular/genetic mechanisms.
Introduction. Type 2 diabetes (T2D) is defined as a group of metabolic disorders characterized by chronic hyperglycemia. It is the result of impaired insulin secretion, deficient effectiveness, or both conditions ().Globally, in 2019, its estimated prevalence was 9.3%, affecting 463 million people, and it is projected to increase to 700 million by 2045.
Purpose Considering the prevalence of type 2 diabetes (T2D), osteoporosis should be considered a serious complication. However, an effective tool for the assessment of low bone mass mineral density (BMD) in T2D patients is not currently available. Therefore, the aim of our study was to establish a simple-to-use risk assessment tool by exploring risk factors for low BMD in T2D patients. Methods ...
About Linagliptin. Linagliptin has been simplifying type 2 diabetes for many Filipino doctors and patients nationwide. 3 Linagliptin provides consistent HbA1c lowering regardless of the patient's kidney and liver function, BMI, age, background T2D therapy, disease duration or ethnicity. It has the highest affinity and highest potency with the lowest renal excretion of only 5% which makes it a ...
Have a body mass index (BMI) of 27kg/m2 or greater and at least one weight-related condition, such as high blood pressure, Type 2 diabetes or high cholesterol; Have a BMI of 30kg/m2 or greater; Avoid semaglutide if you have: History of medullary thyroid cancer; History of gallbladder disease; History of pancreatitis