- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- About Health Education Research
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction.
- < Previous
Young people and healthy eating: a systematic review of research on barriers and facilitators
- Article contents
- Figures & tables
- Supplementary Data
J Shepherd, A Harden, R Rees, G Brunton, J Garcia, S Oliver, A Oakley, Young people and healthy eating: a systematic review of research on barriers and facilitators, Health Education Research , Volume 21, Issue 2, 2006, Pages 239–257, https://doi.org/10.1093/her/cyh060
- Permissions Icon Permissions
A systematic review was conducted to examine the barriers to, and facilitators of, healthy eating among young people (11–16 years). The review focused on the wider determinants of health, examining community- and society-level interventions. Seven outcome evaluations and eight studies of young people's views were included. The effectiveness of the interventions was mixed, with improvements in knowledge and increases in healthy eating but differences according to gender. Barriers to healthy eating included poor school meal provision and ease of access to, relative cheapness of and personal taste preferences for fast food. Facilitators included support from family, wider availability of healthy foods, desire to look after one's appearance and will-power. Friends and teachers were generally not a common source of information. Some of the barriers and facilitators identified by young people had been addressed by soundly evaluated effective interventions, but significant gaps were identified where no evaluated interventions appear to have been published (e.g. better labelling of food products), or where there were no methodologically sound evaluations. Rigorous evaluation is required particularly to assess the effectiveness of increasing the availability of affordable healthy food in the public and private spaces occupied by young people.
Healthy eating contributes to an overall sense of well-being, and is a cornerstone in the prevention of a number of conditions, including heart disease, diabetes, high blood pressure, stroke, cancer, dental caries and asthma. For children and young people, healthy eating is particularly important for healthy growth and cognitive development. Eating behaviours adopted during this period are likely to be maintained into adulthood, underscoring the importance of encouraging healthy eating as early as possible [ 1 ]. Guidelines recommend consumption of at least five portions of fruit and vegetables a day, reduced intakes of saturated fat and salt and increased consumption of complex carbohydrates [ 2, 3 ]. Yet average consumption of fruit and vegetables in the UK is only about three portions a day [ 4 ]. A survey of young people aged 11–16 years found that nearly one in five did not eat breakfast before going to school [ 5 ]. Recent figures also show alarming numbers of obese and overweight children and young people [ 6 ]. Discussion about how to tackle the ‘epidemic’ of obesity is currently high on the health policy agenda [ 7 ], and effective health promotion remains a key strategy [ 8–10 ].
Evidence for the effectiveness of interventions is therefore needed to support policy and practice. The aim of this paper is to report a systematic review of the literature on young people and healthy eating. The objectives were
(i) to undertake a ‘systematic mapping’ of research on the barriers to, and facilitators of, healthy eating among young people, especially those from socially excluded groups (e.g. low-income, ethnic minority—in accordance with government health policy);
(ii) to prioritize a subset of studies to systematically review ‘in-depth’;
(iii) to ‘synthesize’ what is known from these studies about the barriers to, and facilitators of, healthy eating with young people, and how these can be addressed and
(iv) to identify gaps in existing research evidence.
General approach
This study followed standard procedures for a systematic review [ 11, 12 ]. It also sought to develop a novel approach in three key areas.
First, it adopted a conceptual framework of ‘barriers’ to and ‘facilitators’ of health. Research findings about the barriers to, and facilitators of, healthy eating among young people can help in the development of potentially effective intervention strategies. Interventions can aim to modify or remove barriers and use or build upon existing facilitators. This framework has been successfully applied in other related systematic reviews in the area of healthy eating in children [ 13 ], physical activity with children [ 14 ] and young people [ 15 ] and mental health with young people [16; S. Oliver, A. Harden, R. Rees, J. Shepherd, G. Brunton and A. Oakley, manuscript in preparation].
Second, the review was carried out in two stages: a systematic search for, and mapping of, literature on healthy eating with young people, followed by an in-depth systematic review of the quality and findings of a subset of these studies. The rationale for a two-stage review to ensure the review was as relevant as possible to users. By mapping a broad area of evidence, the key characteristics of the extant literature can be identified and discussed with review users, with the aim of prioritizing the most relevant research areas for systematic in-depth analysis [ 17, 18 ].
Third, the review utilized a ‘mixed methods’ triangulatory approach. Data from effectiveness studies (‘outcome evaluations’, primarily quantitative data) were combined with data from studies which described young people's views of factors influencing their healthy eating in negative or positive ways (‘views’ studies, primarily qualitative). We also sought data on young people's perceptions of interventions when these had been collected alongside outcomes data in outcome evaluations. However, the main source of young people's views was surveys or interview-based studies that were conducted independently of intervention evaluation (‘non-intervention’ research). The purpose was to enable us to ascertain not just whether interventions are effective, but whether they address issues important to young people, using their views as a marker of appropriateness. Few systematic reviews have attempted to synthesize evidence from both intervention and non-intervention research: most have been restricted to outcome evaluations. This study therefore represents one of the few attempts that have been made to date to integrate different study designs into systematic reviews of effectiveness [ 19–22 ].
Literature searching
A highly sensitive search strategy was developed to locate potentially relevant studies. A wide range of terms for healthy eating (e.g. nutrition, food preferences, feeding behaviour, diets and health food) were combined with health promotion terms or general or specific terms for determinants of health or ill-health (e.g. health promotion, behaviour modification, at-risk-populations, sociocultural factors and poverty) and with terms for young people (e.g. adolescent, teenager, young adult and youth). A number of electronic bibliographic databases were searched, including Medline, EMBASE, The Cochrane Library, PsycINFO, ERIC, Social Science Citation Index, CINAHL, BiblioMap and HealthPromis. The searches covered the full range of publication years available in each database up to 2001 (when the review was completed).
Full reports of potentially relevant studies identified from the literature search were obtained and classified (e.g. in terms of specific topic area, context, characteristics of young people, research design and methodological attributes).
Inclusion screening
Inclusion criteria were developed and applied to each study. The first round of screening was to identify studies to populate the map. To be included, a study had to (i) focus on healthy eating; (ii) include young people aged 11–16 years; (iii) be about the promotion of healthy eating, and/or the barriers to, or facilitators of, healthy eating; (iv) be a relevant study type: (a) an outcome evaluation or (b) a non-intervention study (e.g. cohort or case control studies, or interview studies) conducted in the UK only (to maximize relevance to UK policy and practice) and (v) be published in the English language.
The results of the map, which are reported in greater detail elsewhere [ 23 ], were used to prioritize a subset of policy relevant studies for the in-depth systematic review.
A second round of inclusion screening was performed. As before, all studies had to have healthy eating as their main focus and include young people aged 11–16 years. In addition, outcome evaluations had toFor a non-intervention study to be included it had to
(i) use a comparison or control group; report pre- and post-intervention data and, if a non-randomized trial, equivalent on sociodemographic characteristics and pre-intervention outcome variables (demonstrating their ‘potential soundness’ in advance of further quality assessment);
(ii) report an intervention that aims to make a change at the community or society level and
(iii) measure behavioural and/or physical health status outcomes.
(i) examine young people's attitudes, opinions, beliefs, feelings, understanding or experiences about healthy eating (rather than solely examine health status, behaviour or factual knowledge);
(ii) access views about one or more of the following: young people's definitions of and/or ideas about healthy eating, factors influencing their own or other young people's healthy eating and whether and how young people think healthy eating can be promoted and
(iii) privilege young people's views—presenting views directly as data that are valuable and interesting in themselves, rather than only as a route to generating variables to be tested in a predictive or causal model.
Non-intervention studies published before 1990 were excluded in order to maximize the relevance of the review findings to current policy issues.
Data extraction and quality assessment
All studies meeting inclusion criteria underwent data extraction and quality assessment, using a standardized framework [ 24 ]. Data for each study were entered independently by two researchers into a specialized computer database [ 25 ] (the full and final data extraction and quality assessment judgement for each study in the in-depth systematic review can be viewed on the Internet by visiting http://eppi.ioe.ac.uk ).
Outcome evaluations were considered methodologically ‘sound’ if they reported:Only studies meeting these criteria were used to draw conclusions about effectiveness. The results of the studies which did not meet these quality criteria were judged unclear.
(i) a control or comparison group equivalent to the intervention group on sociodemographic characteristics and pre-intervention outcome variables.
(ii) pre-intervention data for all individuals or groups recruited into the evaluation;
(iii) post-intervention data for all individuals or groups recruited into the evaluation and
(iv) on all outcomes, as described in the aims of the intervention.
Non-intervention studies were assessed according to a total of seven criteria (common to sets of criteria proposed by four research groups for qualitative research [ 26–29 ]):
(i) an explicit account of theoretical framework and/or the inclusion of a literature review which outlined a rationale for the intervention;
(ii) clearly stated aims and objectives;
(iii) a clear description of context which includes detail on factors important for interpreting the results;
(iv) a clear description of the sample;
(v) a clear description of methodology, including systematic data collection methods;
(vi) analysis of the data by more than one researcher and
(vii) the inclusion of sufficient original data to mediate between data and interpretation.
Data synthesis
Three types of analyses were performed: (i) narrative synthesis of outcome evaluations, (ii) narrative synthesis of non-intervention studies and (iii) synthesis of intervention and non-intervention studies together.
For the last of these a matrix was constructed which laid out the barriers and facilitators identified by young people alongside descriptions of the interventions included in the in-depth systematic review of outcome evaluations. The matrix was stratified by four analytical themes to characterize the levels at which the barriers and facilitators appeared to be operating: the school, family and friends, the self and practical and material resources. This methodology is described further elsewhere [ 20, 22, 30 ].
From the matrix it is possible to see:
(i) where barriers have been modified and/or facilitators built upon by soundly evaluated interventions, and ‘promising’ interventions which need further, more rigorous, evaluation (matches) and
(ii) where barriers have not been modified and facilitators not built upon by any evaluated intervention, necessitating the development and rigorous evaluation of new interventions (gaps).
Figure 1 outlines the number of studies included at various stages of the review. Of the total of 7048 reports identified, 135 reports (describing 116 studies) met the first round of screening and were included in the descriptive map. The results of the map are reported in detail in a separate publication—see Shepherd et al. [ 23 ] (the report can be downloaded free of charge via http://eppi.ioe.ac.uk ). A subset of 22 outcome evaluations and 8 studies of young people's views met the criteria for the in-depth systematic review.

The review process.
Outcome evaluations
Of the 22 outcome evaluations, most were conducted in the United States ( n = 16) [ 31–45 ], two in Finland [ 46, 47 ], and one each in the UK [ 48 ], Norway [ 49 ], Denmark [ 50 ] and Australia [ 51 ]. In addition to the main focus on promoting healthy eating, they also addressed other related issues including cardiovascular disease in general, tobacco use, accidents, obesity, alcohol and illicit drug use. Most were based in primary or secondary school settings and were delivered by teachers. Interventions varied considerably in content. While many involved some form of information provision, over half ( n = 13) involved attempts to make structural changes to young people's physical environments; half ( n = 11) trained parents in or about nutrition, seven developed health-screening resources, five provided feedback to young people on biological measures and their behavioural risk status and three aimed to provide social support systems for young people or others in the community. Social learning theory was the most common theoretical framework used to develop these interventions. Only a minority of studies included young people who could be considered socially excluded ( n = 6), primarily young people from ethnic minorities (e.g. African Americans and Hispanics).
Following detailed data extraction and critical appraisal, only seven of the 22 outcome evaluations were judged to be methodologically sound. For the remainder of this section we only report the results of these seven. Four of the seven were from the United States, with one each from the UK, Norway and Finland. The studies varied in the comprehensiveness of their reporting of the characteristics of the young people (e.g. sociodemographic/economic status). Most were White, living in middle class urban areas. All attended secondary schools. Table I details the interventions in these sound studies. Generally, they were multicomponent interventions in which classroom activities were complemented with school-wide initiatives and activities in the home. All but one of the seven sound evaluations included and an integral evaluation of the intervention processes. Some studies report results according to demographic characteristics such as age and gender.
Soundly evaluated outcome evaluations: study characteristics (n = 7)
| Author/Country/Design | Population | Setting | Objectives | Providers | Programme content |
| Klepp and Wilhelmsen [ ], Norway, CT (+PE) | Seventh grade (13 years old) students | Secondary schools | Teachers and peer educators | ||
| Moon [ ], UK, CT (+PE) | Year 8 and Year 11 pupils (aged 11–16 years) | Secondary schools | |||
| Nicklas [ ], USA, RCT (+PE) | Ninth grade (age range 14–15 years) at start; 3-year longitudinal cohort intervention | High schools | Objective of the ‘Gimme 5’ programme Objective of the parent programme ‘5 a Day For Better Health’: | Teachers, health educators and school catering personnel | |
| Perry [ ], USA, RCT (+PE) | Ninth grade (14- to 15-year-old pupils) | Suburban high school | Teachers administered the programme in general, with 30 class-elected peer leaders leading the class-based sessions | ||
| Vartiainen [ ], Finland, RCT (+PE) | 12- to 16-year-old students | Secondary schools in the Karelia and Kuopio regions of Finland | Health educators, school nurses, peer educators, school teachers | ||
| Walter I and II [ ], USA, RCT (+PE) | Fourth grade (mean age 9 years at start); 5-year longitudinal cohort intervention | Elementary and junior high schools | Teachers delivered the classroom component. Health and education professionals conducted risk factor examination screening |
| Author/Country/Design | Population | Setting | Objectives | Providers | Programme content |
| Klepp and Wilhelmsen [ ], Norway, CT (+PE) | Seventh grade (13 years old) students | Secondary schools | Teachers and peer educators | ||
| Moon [ ], UK, CT (+PE) | Year 8 and Year 11 pupils (aged 11–16 years) | Secondary schools | |||
| Nicklas [ ], USA, RCT (+PE) | Ninth grade (age range 14–15 years) at start; 3-year longitudinal cohort intervention | High schools | Objective of the ‘Gimme 5’ programme Objective of the parent programme ‘5 a Day For Better Health’: | Teachers, health educators and school catering personnel | |
| Perry [ ], USA, RCT (+PE) | Ninth grade (14- to 15-year-old pupils) | Suburban high school | Teachers administered the programme in general, with 30 class-elected peer leaders leading the class-based sessions | ||
| Vartiainen [ ], Finland, RCT (+PE) | 12- to 16-year-old students | Secondary schools in the Karelia and Kuopio regions of Finland | Health educators, school nurses, peer educators, school teachers | ||
| Walter I and II [ ], USA, RCT (+PE) | Fourth grade (mean age 9 years at start); 5-year longitudinal cohort intervention | Elementary and junior high schools | Teachers delivered the classroom component. Health and education professionals conducted risk factor examination screening |
RCT = Randomized Controlled Trial; CT = controlled trial (no randomization); PE = process evaluation.
Separate evaluations of the same intervention in two populations in New York (the Bronx and Westchester County).
The UK-based intervention was an award scheme (the ‘Wessex Healthy Schools Award’) that sought to make health-promoting changes in school ethos, organizational functioning and curriculum [ 48 ]. Changes made in schools included the introduction of health education curricula, as well as the setting of targets in key health promotion areas (including healthy eating). Knowledge levels, which were high at baseline, changed little over the course of the intervention. Intervention schools performed better in terms of healthy food choices (on audit scores). The impact on measures of healthy eating such as choosing healthy snacks varied according to age and sex. The intervention only appeared possibly to be effective for young women in Year 11 (aged 15–16 years) on these measures (statistical significance not reported).
The ‘Know Your Body’ intervention, a cardiovascular risk reduction programme, was evaluated in two separate studies in two demographically different areas of New York (the Bronx and Westchester County) [ 45 ]. Lasting for 5 years it comprised teacher-led classroom education, parental involvement activities and risk factor examination in elementary and junior high schools. In the Bronx evaluation, statistically significant increases in knowledge were reported, but favourable changes in cholesterol levels and dietary fat were not significant. In the Westchester County evaluation, we judged the effects to be unclear due to shortcomings in methods reported.
A second US-based study, the 3-year ‘Gimme 5’ programme [ 40 ], focused on increasing consumption of fruits and vegetables through a school-wide media campaign, complemented by classroom activities, parental involvement and changes to nutritional content of school meals. The intervention was effective at increasing knowledge (particularly among young women). Effects were measured in terms of changes in knowledge scores between baseline and two follow-up periods. Differences between the intervention and comparison group were significant at both follow-ups. There was a significant increase in consumption of fruit and vegetables in the intervention group, although this was not sustained.
In the third US study, the ‘Slice of Life’ intervention, peer leaders taught 10 sessions covering the benefits of fitness, healthy diets and issues concerning weight control [ 41 ]. School functioning was also addressed by student recommendations to school administrators. For young women, there were statistically significant differences between intervention and comparison groups on healthy eating scores, salt consumption scores, making healthy food choices, knowledge of healthy food, reading food labels for salt and fat content and awareness of healthy eating. However, among young men differences were only significant for salt and knowledge scores. The process evaluation suggested that having peers deliver training was acceptable to students and the peer-trainers themselves.
A Norwegian study evaluated a similar intervention to the ‘Slice of Life’ programme, employing peer educators to lead classroom activities and small group discussions on nutrition [ 49 ]. Students also analysed the availability of healthy food in their social and home environment and used a computer program to analyse the nutritional status of foods. There were significant intervention effects for reported healthy eating behaviour (but not maintained by young men) and for knowledge (not young women).
The second ‘North Karelia Youth Study’ in Finland featured classroom educational activities, a community media campaign, health-screening activities, changes to school meals and a health education initiative in the parents' workplace [ 47 ]. It was judged to be effective for healthy eating behaviour, reducing systolic blood pressure and modifying fat content of school meals, but less so for reducing cholesterol levels and diastolic blood pressure.
The evidence from the well-designed evaluations of the effectiveness of healthy eating initiatives is therefore mixed. Interventions tend to be more effective among young women than young men.
Young people's views
Table II describes the key characteristics of the eight studies of young people's views. The most consistently reported characteristics of the young people were age, gender and social class. Socioeconomic status was mixed, and in the two studies reporting ethnicity, the young people participating were predominantly White. Most studies collected data in mainstream schools and may therefore not be applicable to young people who infrequently or never attend school.
Characteristics of young people's views studies (n = 8)
| Study | Aims and objectives | Sample characteristics |
| Dennison and Shepherd [ ] | ||
| Harris [ ] | ||
| McDougall [ ] | ||
| Miles and Eid [ ] | ||
| Roberts [ ] | ||
| Ross [ ] | ||
| Watt and Sheiham [ ] | ||
| Watt and Sheiham [ ] |
| Study | Aims and objectives | Sample characteristics |
| Dennison and Shepherd [ ] | ||
| Harris [ ] | ||
| McDougall [ ] | ||
| Miles and Eid [ ] | ||
| Roberts [ ] | ||
| Ross [ ] | ||
| Watt and Sheiham [ ] | ||
| Watt and Sheiham [ ] |
All eight studies asked young people about their perceptions of, or attitudes towards, healthy eating, while none explicitly asked them what prevents them from eating healthily. Only two studies asked them what they think helps them to eat healthy foods, and only one asked for their ideas about what could or should be done to promote nutrition.
Young people tended to talk about food in terms of what they liked and disliked, rather than what was healthy/unhealthy. Healthy foods were predominantly associated with parents/adults and the home, while ‘fast food’ was associated with pleasure, friendship and social environments. Links were also made between food and appearance, with fast food perceived as having negative consequences on weight and facial appearance (and therefore a rationale for eating healthier foods). Attitudes towards healthy eating were generally positive, and the importance of a healthy diet was acknowledged. However, personal preferences for fast foods on grounds of taste tended to dominate food choice. Young people particularly valued the ability to choose what they eat.
Despite not being explicitly asked about barriers, young people discussed factors inhibiting their ability to eat healthily. These included poor availability of healthy meals at school, healthy foods sometimes being expensive and wide availability of, and personal preferences for, fast foods. Things that young people thought should be done to facilitate healthy eating included reducing the price of healthy snacks and better availability of healthy foods at school, at take-aways and in vending machines. Will-power and encouragement from the family were commonly mentioned support mechanisms for healthy eating, while teachers and peers were the least commonly cited sources of information on nutrition. Ideas for promoting healthy eating included the provision of information on nutritional content of school meals (mentioned by young women particularly) and better food labelling in general.
Table III shows the synthesis matrix which juxtaposes barriers and facilitators alongside results of outcome evaluations. There were some matches but also significant gaps between, on the one hand, what young people say are barriers to healthy eating, what helps them and what could or should be done and, on the other, soundly evaluated interventions that address these issues.
Synthesis matrix
| Young people's views on barriers and facilitators | Interventions which address barriers or build on facilitators identified by young people | ||
| Barriers | Facilitators | Soundly evaluated interventions ( = 7) | Other evaluated interventions ( = 15) |
| ) | ) | ) ) ) ) | ) ) |
| ) | |||
| ) | ) | ||
| ) | ) as well as with adulthood ( ) ) | ) ). | ) ) |
| ) | ) ) | ) (see also ) ) ) ) | |
| ) ) | ) | ) ) ) as above | ) as above |
| ) | ) | ) | |
| ) | ) | ) ) | ) ) |
| ) ) | ) as above None identified—research gap | ||
| ) ) | ) ) | ) ) ) | ) ) |
| ) | |||
| ) | ) | ||
| ) | |||
| Young people's views on barriers and facilitators | Interventions which address barriers or build on facilitators identified by young people | ||
| Barriers | Facilitators | Soundly evaluated interventions ( = 7) | Other evaluated interventions ( = 15) |
| ) | ) | ) ) ) ) | ) ) |
| ) | |||
| ) | ) | ||
| ) | ) as well as with adulthood ( ) ) | ) ). | ) ) |
| ) | ) ) | ) (see also ) ) ) ) | |
| ) ) | ) | ) ) ) as above | ) as above |
| ) | ) | ) | |
| ) | ) | ) ) | ) ) |
| ) ) | ) as above None identified—research gap | ||
| ) ) | ) ) | ) ) ) | ) ) |
| ) | |||
| ) | ) | ||
| ) | |||
Key to young people's views studies: Y1 , Dennison and Shepherd [ 56 ]; Y2 , Harris [ 57 ]; Y3 , McDougall [ 58 ]; Y4 , Miles and Eid [ 59 ]; Y5 , Roberts et al. [ 60 ]; Y6 , Ross [ 61 ]; Y7 , Watt and Sheiham [ 62 ]; Y8 , Watt and Sheiham [ 63 ]. Key to intervention studies: OE1 , Baranowski et al. [ 31 ]; OE2 , Bush et al. [ 32 ]; OE3 , Coates et al. [ 33 ]; OE4 , Ellison et al. [ 34 ]; OE5 , Flores [ 36 ]; OE6 , Fitzgibbon et al. [ 35 ]; OE7 , Hopper et al. [ 64 ]; OE8 , Holund [ 50 ]; OE9 , Kelder et al. [ 38 ]; OE10 , Klepp and Wilhelmsen [ 49 ]; OE11 , Moon et al. [ 48 ]; OE12 , Nader et al. [ 39 ]; OE13 , Nicklas et al. [ 40 ]; OE14 , Perry et al. [ 41 ]; OE15 , Petchers et al. [ 42 ]; OE16 , Schinke et al. [ 43 ]; OE17 , Wagner et al. [ 44 ]; OE18 , Vandongen et al. [ 51 ]; OE19 , Vartiainen et al. [ 46 ]; OE20 , Vartiainen et al. [ 47 ]; OE21 , Walter I [ 45 ]; OE22 , Walter II [ 45 ]. OE10, OE11, OE13, OE14, OE20, OE21 and OE22 denote a sound outcome evaluation. OE21 and OE22 are separate evaluations of the same intervention. Due to methodological limitations, we have judged the effects of OE22 to be unclear. Y1 and Y2 do not appear in the synthesis matrix as they did not explicitly report barriers or facilitators, and it was not possible for us to infer potential barriers or facilitators. However, these two studies did report what young people understood by healthy eating, their perceptions, and their views and opinions on the importance of eating a healthy diet. OE2, OE12, OE16 and OE17 do not appear in the synthesis matrix as they did not address any of the barriers or facilitators.
In terms of the school environment, most of the barriers identified by young people appear to have been addressed. At least two sound outcome evaluations demonstrated the effectiveness of increasing the availability of healthy foods in the school canteen [ 40, 47 ]. Furthermore, despite the low status of teachers and peers as sources of nutritional information, several soundly evaluated studies showed that they can be employed effectively to deliver nutrition interventions.
Young people associated parents and the home environment with healthy eating, and half of the sound outcome evaluations involved parents in the education of young people about nutrition. However, problems were sometimes experienced in securing parental attendance at intervention activities (e.g. seminar evenings). Why friends were not a common source of information about good nutrition is not clear. However, if peer pressure to eat unhealthy foods is a likely explanation, then it has been addressed by the peer-led interventions in three sound outcome evaluations (generally effectively) [ 41, 47, 49 ] and two outcome evaluations which did not meet the quality criteria (effectiveness unclear) [ 33, 50 ].
The fact that young people choose fast foods on grounds of taste has generally not been addressed by interventions, apart from one soundly evaluated effective intervention which included taste testings of fruit and vegetables [ 40 ]. Young people's concern over their appearance (which could be interpreted as both a barrier and a facilitator) has only been addressed in one of the sound outcome evaluations (which revealed an effective intervention) [ 41 ]. Will-power to eat healthy foods has only been examined in one outcome evaluation in the in-depth systematic review (judged to be sound and effective) (Walter I—Bronx evaluation) [ 45 ]. The need for information on nutrition was addressed by the majority of interventions in the in-depth systematic review. However, no studies were found which evaluated attempts to increase the nutritional content of school meals.
Barriers and facilitators relating to young people's practical and material resources were generally not addressed by interventions, soundly evaluated or otherwise. No studies were found which examined the effectiveness of interventions to lower the price of healthy foods. However, one soundly evaluated intervention was partially effective in increasing the availability of healthy snacks in community youth groups (Walter I—Bronx evaluation) [ 45 ]. At best, interventions have attempted to raise young people's awareness of environmental constraints on eating healthily, or encouraged them to lobby for increased availability of nutritious foods (in the case of the latter without reporting whether any changes have been effected as a result).
This review has systematically identified some of the barriers to, and facilitators of, healthy eating with young people, and illustrated to what extent they have been addressed by soundly evaluated effective interventions.
The evidence for effectiveness is mixed. Increases in knowledge of nutrition (measured in all but one study) were not consistent across studies, and changes in clinical risk factors (measured in two studies) varied, with one study detecting reductions in cholesterol and another detecting no change. Increases in reported healthy eating behaviour were observed, but mostly among young women revealing a distinct gender pattern in the findings. This was the case in four of the seven outcome evaluations (in which analysis was stratified by gender). The authors of one of the studies suggest that emphasis of the intervention on healthy weight management was more likely to appeal to young women. It was proposed that interventions directed at young men should stress the benefits of nutrition on strength, physical endurance and physical activity, particularly to appeal to those who exercise and play sports. Furthermore, age was a significant factor in determining effectiveness in one study [ 48 ]. Impact was greatest on young people in the 15- to 16-year age range (particularly for young women) in comparison with those aged 12–13 years, suggesting that dietary influences may vary with age. Tailoring the intervention to take account of age and gender is therefore crucial to ensure that interventions are as relevant and meaningful as possible.
Other systematic reviews of interventions to promote healthy eating (which included some of the studies with young people fitting the age range of this review) also show mixed results [ 52–55 ]. The findings of these reviews, while not being directly comparable in terms of conceptual framework, methods and age group, seem to offer some support for the findings of this review. The main message is that while there is some evidence to suggest effectiveness, the evidence base is limited. We have identified no comparable systematic reviews in this area.
Unlike other reviews, however, this study adopted a wider perspective through inclusion of studies of young people's views as well as effectiveness studies. A number of barriers to healthy eating were identified, including poor availability of healthy foods at school and in young people's social spaces, teachers and friends not always being a source of information/support for healthy eating, personal preferences for fast foods and healthy foods generally being expensive. Facilitating factors included information about nutritional content of foods/better labelling, parents and family members being supportive; healthy eating to improve or maintain one's personal appearance, will-power and better availability/lower pricing of healthy snacks.
Juxtaposing barriers and facilitators alongside effectiveness studies allowed us to examine the extent to which the needs of young people had been adequately addressed by evaluated interventions. To some extent they had. Most of the barriers and facilitators that related to the school and relationships with family and friends appear to have been taken into account by soundly evaluated interventions, although, as mentioned, their effectiveness varied. Many of the gaps tended to be in relation to young people as individuals (although our prioritization of interventions at the level of the community and society may have resulted in the exclusion of some of these interventions) and the wider determinants of health (‘practical and material resources’). Despite a wide search, we found few evaluations of strategies to improve nutritional labelling on foods particularly in schools or to increase the availability of affordable healthy foods particularly in settings where young people socialize. A number of initiatives are currently in place which may fill these gaps, but their effectiveness does not appear to have been reported yet. It is therefore crucial for any such schemes to be thoroughly evaluated and disseminated, at which point an updated systematic review would be timely.
This review is also constrained by the fact that its conclusions can only be supported by a relatively small proportion of the extant literature. Only seven of the 22 outcome evaluations identified were considered to be methodologically sound. As illustrated in Table III , a number of the remaining 15 interventions appear to modify barriers/build on facilitators but their results can only be judged unclear until more rigorous evaluation of these ‘promising’ interventions has been reported.
Finally, it is important to acknowledge that the majority of the outcome evaluations were conducted in the United States, and by virtue of the inclusion criteria, all the young people's views studies were UK based. The literature therefore might not be generalizable to other countries, where sociocultural values and socioeconomic circumstances may be quite different. Further evidence synthesis is needed on barriers to, and facilitators of, healthy eating and nutrition worldwide, particularly in developing countries.
The aim of this study was to survey what is known about the barriers to, and facilitators of, healthy eating among young people with a view to drawing out the implications for policy and practice. The review has mapped and quality screened the extant research in this area, and brought together the findings from evaluations of interventions aiming to promote healthy eating and studies which have elicited young people's views.
There has been much research activity in this area, yet it is disappointing that so few evaluation studies were methodologically strong enough to enable us to draw conclusions about effectiveness. There is some evidence to suggest that multicomponent school-based interventions can be effective, although effects tended to vary according to age and gender. Tailoring intervention messages accordingly is a promising approach which should therefore be evaluated. A key theme was the value young people place on choice and autonomy in relation to food. Increasing the provision and range of healthy, affordable snacks and meals in schools and social spaces will enable them to exercise their choice of healthier, tasty options.
We have identified that several barriers to, and facilitators of, healthy eating in young people have received little attention in evaluation research. Further work is needed to develop and evaluate interventions which modify or remove these barriers, and build on these facilitators. Further qualitative studies are also needed so that we can continue to listen to the views of young people. This is crucial if we are to develop and test meaningful, appropriate and effective health promotion strategies.
We would like to thank Chris Bonell and Dina Kiwan for undertaking data extraction. We would also like to acknowledge the invaluable help of Amanda Nicholas, James Thomas, Elaine Hogan, Sue Bowdler and Salma Master for support and helpful advice. The Department of Health, England, funds a specific programme of health promotion work at the EPPI-Centre. The views expressed in the report are those of the authors and not necessarily those of the Department of Health.
Google Scholar
Google Preview
- healthy diet
| Month: | Total Views: |
|---|---|
| November 2016 | 97 |
| December 2016 | 30 |
| January 2017 | 142 |
| February 2017 | 474 |
| March 2017 | 551 |
| April 2017 | 531 |
| May 2017 | 288 |
| June 2017 | 223 |
| July 2017 | 194 |
| August 2017 | 160 |
| September 2017 | 274 |
| October 2017 | 457 |
| November 2017 | 534 |
| December 2017 | 1,913 |
| January 2018 | 2,369 |
| February 2018 | 2,421 |
| March 2018 | 3,801 |
| April 2018 | 3,998 |
| May 2018 | 2,929 |
| June 2018 | 2,177 |
| July 2018 | 2,422 |
| August 2018 | 2,469 |
| September 2018 | 2,635 |
| October 2018 | 3,102 |
| November 2018 | 4,124 |
| December 2018 | 2,786 |
| January 2019 | 2,687 |
| February 2019 | 3,644 |
| March 2019 | 4,985 |
| April 2019 | 4,055 |
| May 2019 | 3,480 |
| June 2019 | 2,876 |
| July 2019 | 3,013 |
| August 2019 | 2,524 |
| September 2019 | 2,360 |
| October 2019 | 2,100 |
| November 2019 | 2,117 |
| December 2019 | 1,595 |
| January 2020 | 1,884 |
| February 2020 | 2,068 |
| March 2020 | 1,833 |
| April 2020 | 1,953 |
| May 2020 | 970 |
| June 2020 | 1,058 |
| July 2020 | 1,152 |
| August 2020 | 931 |
| September 2020 | 1,518 |
| October 2020 | 1,548 |
| November 2020 | 1,761 |
| December 2020 | 1,207 |
| January 2021 | 1,211 |
| February 2021 | 1,440 |
| March 2021 | 1,910 |
| April 2021 | 1,531 |
| May 2021 | 1,253 |
| June 2021 | 670 |
| July 2021 | 580 |
| August 2021 | 548 |
| September 2021 | 763 |
| October 2021 | 1,058 |
| November 2021 | 1,009 |
| December 2021 | 816 |
| January 2022 | 697 |
| February 2022 | 824 |
| March 2022 | 1,047 |
| April 2022 | 1,053 |
| May 2022 | 935 |
| June 2022 | 504 |
| July 2022 | 391 |
| August 2022 | 436 |
| September 2022 | 694 |
| October 2022 | 909 |
| November 2022 | 790 |
| December 2022 | 489 |
| January 2023 | 764 |
| February 2023 | 601 |
| March 2023 | 938 |
| April 2023 | 755 |
| May 2023 | 686 |
| June 2023 | 594 |
| July 2023 | 452 |
| August 2023 | 419 |
| September 2023 | 582 |
| October 2023 | 840 |
| November 2023 | 593 |
| December 2023 | 522 |
| January 2024 | 811 |
| February 2024 | 717 |
| March 2024 | 866 |
| April 2024 | 1,003 |
| May 2024 | 1,080 |
| June 2024 | 333 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1465-3648
- Print ISSN 0268-1153
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 06 December 2017
Food for thought: how nutrition impacts cognition and emotion
- Sarah J. Spencer 1 ,
- Aniko Korosi 2 ,
- Sophie Layé 3 ,
- Barbara Shukitt-Hale 4 &
- Ruth M. Barrientos 5
npj Science of Food volume 1 , Article number: 7 ( 2017 ) Cite this article
153k Accesses
148 Citations
192 Altmetric
Metrics details
- Neuroendocrine diseases
More than one-third of American adults are obese and statistics are similar worldwide. Caloric intake and diet composition have large and lasting effects on cognition and emotion, especially during critical periods in development, but the neural mechanisms for these effects are not well understood. A clear understanding of the cognitive–emotional processes underpinning desires to over-consume foods can assist more effective prevention and treatments of obesity. This review addresses recent work linking dietary fat intake and omega-3 polyunsaturated fatty acid dietary imbalance with inflammation in developing, adult, and aged brains. Thus, early-life diet and exposure to stress can lead to cognitive dysfunction throughout life and there is potential for early nutritional interventions (e.g., with essential micronutrients) for preventing these deficits. Likewise, acute consumption of a high-fat diet primes the hippocampus to produce a potentiated neuroinflammatory response to a mild immune challenge, causing memory deficits. Low dietary intake of omega-3 polyunsaturated fatty acids can also contribute to depression through its effects on endocannabinoid and inflammatory pathways in specific brain regions leading to synaptic phagocytosis by microglia in the hippocampus, contributing to memory loss. However, encouragingly, consumption of fruits and vegetables high in polyphenolics can prevent and even reverse age-related cognitive deficits by lowering oxidative stress and inflammation. Understanding relationships between diet, cognition, and emotion is necessary to uncover mechanisms involved in and strategies to prevent or attenuate comorbid neurological conditions in obese individuals.
Similar content being viewed by others
Investigating nutrient biomarkers of healthy brain aging: a multimodal brain imaging study

Neural correlates of obesity across the lifespan

Insights into the role of diet and dietary flavanols in cognitive aging: results of a randomized controlled trial
Introduction.
Cognitive and emotional dysfunctions are an increasing burden in our society. The exact factors and underlying mechanisms precipitating these disorders have not yet been elucidated. Next to our genetic makeup, the interplay between specific environmental challenges occurring during well-defined developmental periods seems to play an important role. Interestingly, such brain dysfunction most often co-occurs with metabolic disorders (e.g., obesity) and/or poor dietary habits; obesity and poor diet can lead to negative health implications including cognitive and mood dysfunctions, suggesting a strong interaction between these elements (Fig. 1 ). Obesity is a global phenomenon, with around 38% of adults and 18% of children and adolescents worldwide classified as either overweight or obese. 1 Even in the absence of obesity, poor diet is commonplace, 2 with, for instance, many eating foods that are highly processed and lacking in important polyphenols and anti-oxidants or that contain well-below the recommended levels of omega-3 polyunsaturated fatty acids (PUFA). In this review, we will discuss the extent of, and mechanisms for, diet’s influence on mood and cognition during different stages of life, with a focus on microglial activation, glucocorticoids and endocannabinoids (eCBs).
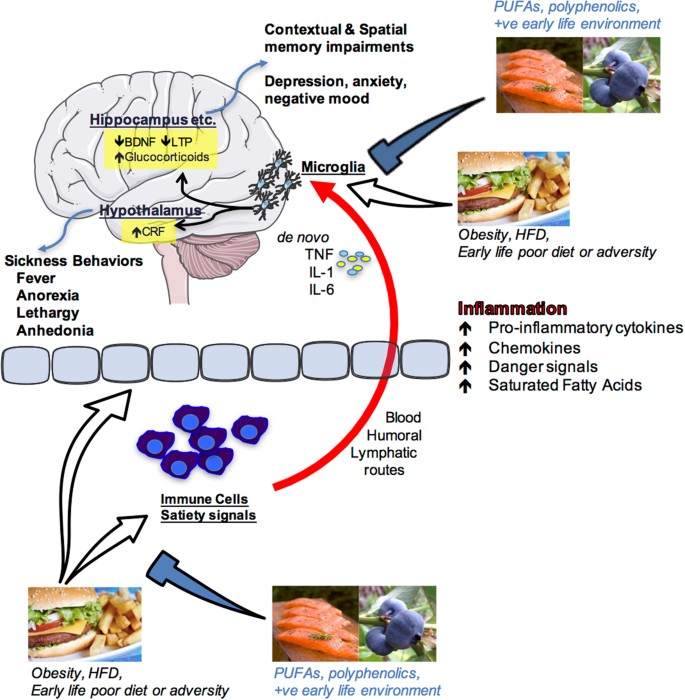
Schematic depiction of how nutrition influences cognition and emotion. Overeating, obesity, acute high-fat diet consumption, poor early-life diet or early life adversity can produce an inflammatory response in peripheral immune cells and centrally as well as having impact upon the blood–brain interface and circulating factors that regulate satiety. Peripheral pro-inflammatory molecules (cytokines, chemokines, danger signals, fatty acids) can signal the immune cells of the brain (most likely microglia) via blood-borne, humoral, and/or lymphatic routes. These signals can either sensitize or activate microglia leading to de novo production of pro-inflammatory molecules such as interleukin-1beta (IL1β), IL-6, and tumor necrosis factor alpha (TNFα) within brain structures that are known to mediate cognition (hippocampus) and emotion (hypothalamus, amygdala, prefrontal cortex and others). Amplified inflammation in these regions impairs proper functioning leading to memory impairments and/or depressive-like behaviors. Polyunsaturated fatty acids (PUFA), polyphenolics, and a positive (+ve) early life environment (appropriate nutrition and absence of significant stress or adversity) can prevent these negative outcomes by regulating peripheral and central immune cell activity. Images are adapted from Servier Medical Art, which is licensed under a Creative Commons Attribution 3.0 Unported License https://creativecommons.org/licenses/by/3.0/ . Salmon and hamburger images were downloaded from Bing.com with the License filter set to “free to share, and use commercially”. The blueberry image is courtesy of author Assistant Prof. Ruth Barrientos
Perinatal diet disrupts cognitive function long-term, a role for microglia
Poor diet in utero and during early postnatal life can cause lasting changes in many aspects of metabolic and central functions, including impairments in cognition and accelerated brain aging, 3 but see. 4 Maternal gestational diabetes and even a junk food diet in the non-diabetic can lead to metabolic complications, including diabetes and obesity in the offspring. 5 , 6 It can also cause changes in reward processing in the offspring brain such that they grow to prefer foods high in fat and sucrose. 7 , 8 Similarly, early introduction of solid food in children and high childhood consumption of fatty foods and sweetened drinks can accelerate weight gain and lead to metabolic complications long-term that may be associated with poorer executive function. 9 On the other hand, some dietary supplements can positively influence cognition, as is seen with supplementation of baby formula with long chain omega-3 PUFA improving cognition in babies. 10 In these randomized control trials (RCTs), an omega-3 PUFA-enriched formula beginning shortly after birth, or 6 weeks’ breast feeding, significantly improved performance of 9-month old babies on a problem solving task (a two-step task to retrieve a rattle, known to correlate with performance on IQ tasks).
From animal models, it is clear that the effects of diet in early life are far-reaching. Even obesity in rat sires (that play no part in rearing the offspring) leads to pancreatic beta cell dysfunction in female offspring, which can be passed on to the next generation. 11 Obesity and high-fat diet feeding in rat and mouse dams during pregnancy and lactation leads to impairments in several tests of mood, including those modeling depressive and anxious behaviors, as well as negatively impacting cognition. 12 Diet in the post-partum to weaning period can impact similar behaviors. 13
Additional to the impact of a prenatal diet, over-consumption of the mother’s milk during the first 3 weeks of a rat’s life leads to lasting obesity in males and females. 14 This neonatal overfeeding also disrupts cognitive function. For example, neonatally overfed rats perform poorly in the novel object recognition test and in the delayed spatial win-shift radial arm maze, as adults, compared with control rats. 15 These findings are interesting to compare with the effects of poor diet in adults where a longer-term high-fat diet (around 20 weeks in the rat) 16 , 17 , 18 and / or high-fat diet in conjunction with a pre-diabetic phenotype 19 is necessary to induce cognitive dysfunction. While there are no differences in post-learning synaptogenesis (synaptophysin) or apoptosis (caspase-3) to explain the effects seen in the neonatally overfed, these rats do have an impaired microglial response to the learning task. 15
Microglia are one of the major immune cell populations in the brain. In development, they are essential for synaptic pruning, while in a mature animal their major role is in mounting a pro-inflammatory immune response and phagocytosing pathogens and injured brain cells. 20 Hyper-activated microglia can lead to cognitive dysfunction through excess pro-inflammatory cytokine production causing impaired long-term potentiation-induction, reduced production of plasticity-related molecules including brain-derived neurotrophic factor and insulin-like growth factor-1, and reduced synaptic plasticity 20 However, an appropriate microglial response may also be essential for effective learning.
Neonatally overfed rats have more microglia in the CA1 region of the hippocampus at postnatal day 14, i.e., while they still have access to excess maternal milk and are undergoing accelerated weight gain. These microglia also have larger soma and retracted processes, indicative of a more activated phenotype. By the time these rats reach adulthood, there persists an increase in the area immunolabelled with microglial marker Iba1 in the dentate gyrus. In the neonatally overfed, the microglial response to a learning task is less robust than in controls. This effect is associated with a suppression of cell proliferation in control animals relative to the neonatally overfed, potentially to preserve existing neuronal networks and minimize novel inputs while learning takes place. 21 Interestingly, global inducible microglial and monocyte depletion can lead to improved performance in the Barnes maze, 22 suggesting withdrawal of microglial activity at specific learning phases is important for learning. These findings implicate microglia in the long-term effects of early life overfeeding on cognition suggesting normal microglia must be able to robustly respond to learning tasks and neonatal overfeeding impairs their ability to do so.
Neuroinflammatory processes, including the role of microglia, can clearly be impacted by neonatal diet and represent at least one contributing mechanism for how cognitive function is affected. Neuroinflammation and microglia can also be impacted by other early life events and play a significant role in how stress during development alters long-term physiology.
Early-life stress (ES) programs vulnerability to cognitive disorders
ES alters brain structure and function life-long, leading to increased vulnerability to develop emotional and cognitive disorders as is evident from several preclinical and clinical studies. 23 , 24 , 25 The exact underlying mechanisms for such programming remain elusive. There is extensive seminal work indicating a key role for sensory stimuli from the mother and neuroendocrine factors (e.g., stress hormones) in this programming, 26 , 27 however it has been recently suggested that these factors might act synergistically with metabolic and nutritional elements. 28 In fact, ES is associated with increased vulnerability to develop metabolic disorders such as obesity, which mostly co-occur with cognitive deficits, 29 , 30 and both ES and an adverse early nutritional environment lead to strikingly similar cognitive impairments later in life, 28 , 31 suggesting that metabolic factors and nutritional elements might mediate some of the ES effects on brain structure and function.
The brain has a very high demand for nutrients in this early period and nutritional imbalances affect normal neurodevelopment resulting in lasting cognitive deficits. 32 Understanding the role of metabolic factors and specific nutrients in this context is key to develop effective peripheral (e.g., nutritional) intervention strategies. A mouse model of the chronic ES of limited nesting and bedding material during the first postnatal week has been shown to lead to aberrant maternal care, which leads to cognitive decline in the ES offspring. 24 , 33 , 34
The hippocampus, a brain region key for cognitive functions, is permanently altered in its structure and function in these ES-exposed offspring. The hippocampus is in fact particularly sensitive to the early-life environment as it continues its development into the postnatal period. 35 Adult neurogenesis (AN) is a unique form of plasticity, which takes place in the hippocampus, consisting of the proliferation of neuronal progenitor cells that differentiate and mature into fully functional neurons that subsequently integrate into the existing hippocampal circuitry. These newly formed neurons are involved in various aspects of hippocampus-dependent learning and memory. 36 AN is affected persistently by ES 24 , 37 and, more precisely, while ES exposure initially increases neurogenesis (i.e., proliferation and differentiation of newborn cells) at postnatal day 9, at later time points (postnatal day 150), the survival of the newly born cells is reduced. 24 In addition, ES affects the neuroinflammatory profile in a lasting manner, with, for example, increased CD68 (phagocytic microglia expression) in adulthood. 38
Importantly, ES persistently affects peripheral adipose tissue metabolism as well. White adipose mass (WAT), plasma leptin (the adipokine released from the WAT) and leptin mRNA expression in WAT are persistently reduced in ES-exposed offspring. 39 In addition, exposure of ES mice to an unhealthy western style diet, leads to a higher increase in adiposity in these mice when compared to controls. These findings suggest that ES exposure leads to metabolic dysregulation and a greater vulnerability to develop obesity in a moderately obesogenic environment. Whether these metabolic alterations contribute to the ES-induced cognitive deficits warrants further investigation. 39
In addition to peripheral metabolism, ES-induced alterations in the nutritional composition of the dam’s milk, and/or nutrient intake/absorption by the pup 25 , 28 , 40 could have lasting consequences for brain structure and function. Indeed, the essential micronutrient, methionine, a critical component of the one-carbon (1-C) metabolism that is required for methylation, and for synthesis of proteins, phospholipids and neurotransmitters, is reduced after ES exposure in plasma and hippocampus of postnatal day 9 offspring. Importantly, a short supplementation of the maternal diet only during ES exposure with essential 1-C metabolism-associated micronutrients not only restores methionine levels peripherally as well as centrally, but rescues (some of) the effects of ES on hippocampal cognitive measures in adulthood and prevents the ES-induced hypothalamic-pituitary–adrenal axis hyperactivity at postnatal day 9. 25
These studies highlight the importance of studying metabolic factors and nutrients in the ES-induced effects on the brain. In the near future, it will be key to further understand the exact mechanisms mediating the effects of nutrients and metabolic factors and the windows of opportunity for interventions on brain function, as this will open entirely new avenues for targeted nutrition for vulnerable populations. However, while the early life period is a window of particular vulnerability to the programming effects of diet and other environmental influences, diet at other phases of life is also important in dictating mood and cognition.
Adult consumption of a high-fat diet: a vulnerability factor for hippocampal-dependent memory
Adults in developed countries are consuming diets higher in saturated fats and/or refined sugars than ever before. Indeed, recent reports show that approximately 12% of American adults’ daily energy intake comes from saturated fats and 13% from added sugars, 41 significantly more than what is recommended (5–10%) by the US Department of Agriculture and the Department of Health and Human Services. Not surprisingly, these dietary habits have contributed to the increasing prevalence of obesity among adults, which is currently approximately 37% in the US, a sharp rise from the 13% prevalence rate of 1960. 42
These statistics are alarming because aside from its well-known provocation of cardiovascular disease, metabolic syndrome, and type 2 diabetes, obesity has now also been associated with mild cognitive impairments and dementia. There is growing evidence that neuroinflammation may underlie obesity-induced cognitive deficits. 9 Recently, studies have demonstrated that short-term consumption (1–7 days) of an unhealthy diet (e.g., high saturated fat and/or high sugar) triggers neuroinflammatory processes, suggesting that obesity per se may not be necessary to cause cognitive disruptions. 43 , 44 For the last 10–15 years, the hypothalamus has received the vast majority of the attention with regard to obesity-induced neuroinflammatory responses and functional declines, 45 perhaps due to its close proximity to the third ventricle, circumventricular organs, and mediobasal eminence, where inflammatory signals from the periphery have easier entry into the brain. Indeed, long chain saturated fatty acids have been shown to directly pass into the hypothalamus producing an inflammatory response there through activation of toll-like receptor 4 signaling. 46 , 47 This active passage of saturated fatty acids, however, has not been observed in the hippocampus, a key brain region that mediates learning and memory. 46 Nonetheless, high-fat diet consumption has been demonstrated to impair hippocampus-dependent memory function in humans and rodents. For example, compared to rodents that consumed a control diet, those that consumed a high-fat and/or high-sugar diet exhibited robust impairments in various types of memory (e.g., spatial, contextual), as indicated by weaker performances in the Y-maze, 48 radial arm maze, 15 novel object recognition task, 15 novel place recognition task, 44 , 49 Morris water maze, 50 and contextual fear conditioning. 18 , 51 Also, adult humans who consumed a high-fat diet for 5 days exhibited significantly reduced focused attention and reduced retrieval speed of information from working and episodic memory, compared with those who consumed a standard diet. 52
Many of these studies, and others, have shown that high-fat diet-induced cognitive deteriorations are accompanied by elevated neuroinflammatory markers or responses in the hippocampus. 15 , 18 , 44 , 48 , 49 , 50 , 51 , 53 However, the mechanisms by which these neuroinflammatory processes signal and/or affect the hippocampus are not entirely clear. There is growing evidence that high-fat diets may compromise the hippocampus by sensitizing the immune cells (most likely microglia) of this brain structure, thus priming the inflammatory response to subsequent challenging stimuli. 18 , 50 , 51 For example, one study demonstrated that adult rats that had eaten a high-fat diet for 5 months exhibited a sensitized hippocampus such that when they received a relatively mild stressor (a single, 2 s, 1.5 mA footshock) following a learning session the neuroinflammatory response in the hippocampus was potentiated compared to the response of rats that had eaten the regular chow, and this response led to deficits in long-term contextual memory. 18 Another study showed that just 3 days of consuming a high-fat diet was sufficient to sensitize the hippocampus of adult rats. Here, a low-dose peripheral immune challenge (with lipopolysaccharide; LPS) produced an exaggerated neuroinflammatory response in the hippocampus of these rats compared to those that consumed the regular chow, and also led to contextual memory deficits. 51
Significantly elevated pro-inflammatory cytokines in the hippocampus have been shown to deteriorate various mechanisms that enable synaptic plasticity (such as long-term potentiation), and thus long-term memory. 54 Sobesky et al. 51 demonstrated that high-fat diet consumption primes the cells of the hippocampus by elevating the glucocorticoid steroid hormone corticosterone in this region. Despite its classic role as an immunosuppressant, there is increasing evidence demonstrating that corticosterone can prime hippocampal microglia and potentiate the inflammatory response to a subsequent challenge. 55 , 56 , 57 For example, Frank et al. 55 elegantly showed that when corticosterone was elevated prior to a peripheral immune challenge (LPS), the resulting inflammatory response in the hippocampus was potentiated. In contrast, when corticosterone was elevated after the immune challenge, the neuroinflammatory response was suppressed. These findings suggest that the temporal relationship between the corticosterone increase and the immune challenge dictates whether a pro-inflammatory or anti-inflammatory response will result. 55 Sobesky et al. 51 found that rats that consumed the high-fat diet for 3 days exhibited significantly increased levels of corticosterone in their hippocampus compared to rats that consumed the regular chow or a novel macronutrient-matched control diet. This high-fat diet-induced corticosterone rise was accompanied by increases in the endogenous danger-associated molecular pattern high-mobility group box 1 (HMGB1), the interleukin (IL)-1 inflammasome-associated protein NLRP3, and the microglial activation marker cd11b. high-fat diet alone did not, however, elevate the pro-inflammatory cytokine IL-1β unless rats were subsequently challenged with a low-dose of LPS. Thus, LPS challenge potentiated the pro-inflammatory response in the hippocampus of high-fat diet-fed rats compared to the response to LPS in chow-fed rats. To evaluate the role of corticosterone signaling in neuroinflammatory priming caused by consumption of high-fat diet, Sobesky et al. 51 administered the glucocorticoid receptor antagonist, mifepristone, prior to high-fat diet consumption. This resulted in a normalized hippocampal IL-1β response to low-dose LPS. Furthermore, mifepristone significantly reduced the high-fat diet + LPS-induced expression of HMGB1, IκBα, and NLRP3. Moreover, mifepristone treatment effectively prevented contextual memory deficits caused by high-fat diet consumption combined with LPS challenge. These data provide strong evidence for the idea that (a) high-fat diet consumption increases corticosterone within the hippocampus, and (b) this corticosterone is a key mediator in sensitizing microglia or other immune cells of the hippocampus; (c) sensitized microglia produce a potentiated neuroinflammatory response to subsequent immune or stressful challenges, thus producing cognitive deficits. Notably, though, while high-fat diet per se can have significant detrimental impact on cognitive processes, specific dietary components may be able to reverse these effects, omega-3 PUFA are one such potentially beneficial component.
Dietary omega-3 PUFA regulate neuroinflammation and eCBs: role in mood and cognitive disorders
Since their discovery in the early 20th century, considerable attention has been paid to the roles of PUFA in brain functions. Omega-3 and omega-6 PUFA are essential fatty acids, meaning that they have to be provided by the diet. Western diet contains excessive amounts of omega-6 PUFA as compared to omega-3 leading to an unbalanced ratio between these two fatty acids with cardiovascular and brain health consequences. Essential omega-3 and omega-6 fatty acids are found in green vegetables, seeds and nuts although coming from different sources with linolenic acid (LA, 18:2 omega-6) found in most plants, coconut and palm and α-linolenic acid (ALA, 18:3 omega-3) in green leafy vegetables, flax and walnuts. Once consumed, LA and ALA are metabolized into arachidonic acid (AA, 20:4 omega-6) and docosahexaenoic acid (DHA, 22:6 omega-3), respectively.
AA and DHA are the main omega-6 and omega-3 long chain PUFA found in the brain. Both long chain PUFA have pivotal roles in brain physiology as they regulate fundamental neurobiological processes, in particular the ones involved in cognition and mood. 58 , 59 AA and DHA are esterified to the phospholipid of neuronal and glial cell membranes with a total brain phospholipid proportion of around 10% for AA and 20% for DHA. Due to the limited capacity of the brain to synthesize long chain PUFA, preformed DHA can be provided by dietary supply of oily fishes. Hence, increased consumption of DHA-rich products results in a partial replacement of AA by DHA in brain cell membranes. 60 Conversely, a lower omega-3 PUFA intake leads to lower brain levels of DHA with increased AA levels. Higher AA and DHA are reported in women as compared to men, suggesting a gender difference in PUFA levels. 61 These differences could be linked to sex hormones as they differentially influence PUFA metabolism with estrogen stimulating, and testosterone inhibiting, the conversion of both omega-3 and omega-6 precursors into their respective long chain metabolites. However, whether these differences in PUFA have a role in specific brain diseases with a gender component has been poorly questioned and requires further investigation.
After its direct consumption and/or metabolization in the liver, DHA is increased in the blood and is likely to freely enter into the brain as non-esterified fatty acid. 58 More recently, Mfsd2a (major facilitator superfamily domain-containing protein 2a), which is expressed by brain endothelial cells and adiponectin receptor 1 in the retina, has been revealed to be important to DHA uptake and retention. 62
Abnormal omega-3 PUFA levels have been extensively described in both the peripheral tissues and in the brain of patients with mood disorders or cognitive decline, leading to a large number of RCTs aiming at evaluating the effectiveness of long chain omega-3 PUFA dietary supplementation on mood and cognitive disorders. 58 , 63 Overall, the results are discordant, due to the heterogeneity of methods used to evaluate the depressive and/or cognitive symptoms, the form, dose and duration of the omega-3 PUFA supplementation, the lack of evaluation of nutritional intake and metabolism of PUFA prior to starting the supplementation, or the lack of evaluation of genotype-associated risk factors. 64 However, despite the discrepancies in the results, it is important to note that several RCTs performed in patients with depressive disorders revealed an additional effect of long chain omega-3 PUFA supplementation to antidepressant treatments. 65 Of note, a recent study identifies that depressive patients presenting a high level of inflammatory markers are more responsive to long chain omega-3 PUFA supplementation. 66 This observation is highly relevant as these PUFA are potent regulators of inflammation 58 and inflammation is a crucial component of mood disorders. Concerning cognitive decline, despite poor positive results of PUFA dietary supplementation in Alzheimer’s disease (AD) patients, RCTs using DHA supplementation in subjects carrying the apolipoprotein E ε4 (APOE4) allele, a risk factor for AD, reveal an improvement of pre-dementia. 64 Overall, discrepancies in clinical studies strongly support the need for preclinical studies aimed at depicting the mechanisms of omega-3 PUFA on brain dysfunctions, which should help to better target populations at risk of cognitive and mood disorders. In addition, the consideration of omega-3 PUFA levels in food to cover the physiological requirement of these PUFA for an optimal brain function is a challenge for the food industry.
Through direct or indirect effects, DHA and AA modulate neurotransmission and neuroinflammation, which are key processes in cognition and mood. 58 , 59 Unesterified long chain PUFA are released from cell membranes upon the activation of phospholipase A2 (PLA2) to exert their effects. 67 Once released, AA and DHA are metabolized into bioactive mediators through cyclooxygenase (COX), lipoxygenases (LOX) and cytochrome P450. 68 The conversion of AA into several prostanoids, including prostaglandins (PG), leukotrienes (LT), thromboxanes (TX) and lipoxins (LX), is crucial in the progression of inflammation, including in the brain. 58 DHA is also metabolized through the COX/LOX pathways to generate metabolites with anti-inflammatory and pro-resolutive properties. 68 In the brain, LOX-derived specialized proresolving mediators (SPMs), neuroprotectin D1 (NPD1), resolvin D5 (RvD5), and maresin 1 (MaR1) are detected. 68 , 69 Some of these SPMs potently modulate neuroinflammation in vivo and in vitro, through their direct effect on microglia. 70 , 71 DHA and SPMs are impaired at the periphery and in the brains of AD patients. 72 , 73 Interestingly, decreased DHA distribution in AD patient brains correlates with synaptic loss rather than amyloid beta (Aβ) deposition. 74 In addition, DHA or SPMs promote phagocytosis of Aβ42 by microglia 75 and modulate microglia number and activation in vivo. 76 Whether SPMs play a role in the protective activity of long chain omega-3 PUFA in mood and cognitive disorders associated to neuroinflammation remains to be established.
eCBs are other key PUFA-derived lipid mediators in the brain. The main brain AA-derived eCBs are the fatty acid ethanolamides anandamide (AEA) and 2-arachidonoylglycerol (2-AG), while docosahexaenoylethanolamide (DHEA or synaptamide) is an eCB-like derived from DHA. 77 ECBs half-life in the brain is regulated by specific catabolizing enzymes fatty acid amide hydrolase for AEA and DHEA and monoacylglycerol lipase for 2-AG. Regarding neuroinflammatory processes, AA-derived eCBs are oxidized into bioactive PG by COX and LOX, which promote inflammation. 78 AEA and 2-AG bind to at least two cannabinoid receptors, type 1 (CB1) and type 2 (CB2), which are Gi/o protein-coupled with numerous signaling pathways in the brain. 79 , 80 DHEA has a lower binding affinity for CB1 and CB2 receptors as compared to AEA and 2-AG and rather bind GPR receptors, in particular GPR110 in the brain. The dietary omega-3/omega-6 PUFA ratio directly influences the proportion of ethanolamides derived from AA and DHA. 81 The modulation of eCB is accompanied by the impairment of neuronal CB1R activity and synaptic activity in several brain structures. 82 , 83 2-AG and AEA regulate synaptic function by suppressing excitatory and inhibitory synapse neurotransmitter release by acting as retrograde messengers at presynaptic CB1. 84 The importance of brain eCB signaling in the understanding of how altered dietary intake of PUFA correlates with a range of neurological disorders is of high interest. 81 However, other dietary factors may also contribute to improved cognition and prevention of cognitive disorders. Polyphenolic-rich foods are a further example that have been shown to have benefit, particularly in the context of aging.
Dietary interventions with polyphenolic-rich foods can improve neuronal and behavior deficits associated with aging
It is estimated that approximately 20% of the US total population will be older than 65 by the year 2050, which is almost double what it is today. 85 Additionally, the US is faced with an increasingly overweight/obese population that is at heightened risk for metabolic disorders, resulting in diabetes and cardiovascular disease, and concomitant behavioral impairment. Aging and metabolic dysregulation are both associated with numerous cognitive and motor deficits on tasks that require fine motor control, balance, short-term and long-term memory, or executive function. Studies in both humans and animal models have demonstrated that oxidative stress and inflammation, as well as impaired insulin resistance, are common features in cardio-metabolic and vascular disease, obesity, and age-related declines in cognitive and motor function. 86 Neuroinflammation occurs locally in the brain; however, peripheral inflammatory cells and circulating inflammatory mediators (e.g., cytokines) can also infiltrate the brain, and this occurs more readily as we age. 87 Therefore, strategies must be found to reduce oxidative and inflammatory vulnerability to age-related changes and reverse deficits in motor and cognitive function.
Targeting peripheral inflammation and insulin signaling could reduce insulin resistance and infiltration of inflammatory mediators into the brain and, as a result, reduce the incidence of a variety of age-related deficits. Studies have shown that plants, particularly colorful fruit or vegetable-bearing plants, contain polyphenolic compounds that have potent antioxidant and anti-inflammatory activities, 88 and increased fruit and vegetable intake has been associated with reduced fasting insulin levels. 89 Evidence is accumulating that consumption of these polyphenol-rich foods, particularly berry fruit, may be a strategy to forestall or even reverse age-related neuronal deficits resulting from neuroinflammation. 90 Recently this evidence has been extended to double-blind, placebo-controlled, randomized human intervention studies that have demonstrated that the consumption of flavonoid/polyphenols is associated with benefits to cognitive function. 91
Preclinical studies have led to the hypothesis that the key to reducing the incidence of age-related deficits in behavior is to alter the neuronal environment with polyphenolic-rich foods like berry fruit, such that neuroinflammation and oxidative stress, and the vulnerability to them, would be reduced. In early studies with animal models, crude blueberry (BB) or strawberry extracts significantly attenuated 92 and reversed 93 age-related motor and cognitive deficits in senescent rodents. BB supplementation also protected 9 month old C57Bl/6 mice against the damaging effects of consuming a high-fat diet. 94 Novel object recognition memory was impaired by the high-fat diet, but blueberry supplementation prevented recognition memory deficits in a time-dependent manner. Spatial memory, as measured by the Morris water maze, was also improved after 5 months on the diets. 94 Subsequent research suggested that berry fruit polyphenols may possess a multiplicity of actions in addition to their anti-inflammatory and antioxidant activities. 90 Additionally, the anthocyanins contained in blueberries have been shown to enter the brain, and their concentrations were correlated with cognitive performance. 95
Epidemiological studies that have focused on fruit and vegetable intake and cognitive function have also largely found that adequate consumption can prevent cognitive decline, while low intake is associated with increased cognitive decline. 85 Specifically, increased intake of blueberries and strawberries, as well as increased intakes of anthocyanidins and total flavanoids, were associated with slowing the rate of cognitive decline by up to 2.5 years. 96
The ability of berry fruit to protect against age-related cognitive decline has also been examined in a growing number of double-blind, placebo-controlled, randomized, human intervention studies. Thus, blueberry juice significantly improved word list recall and paired associate learning in older men and women with age-related memory decline that consumed it, relative to baseline, with paired associate learning also significantly improved relative to placebo controls. 97 A recent study 98 that measured similar cognitive tasks as those in the rodent studies, showed that freeze-dried blueberries (24 g/day, equivalent to one cup of fresh blueberries) for 90 days improved two measures of executive function in older adults (ages 60–75). Participants in the blueberry group showed significantly fewer repetition errors in the California Verbal Learning test as well as reduced switch cost on a task-switching test across study visits, relative to controls who consumed placebo powder. However, no improvement in gait or balance was observed following blueberry intake. 98 Finally, 12 weeks of blueberry concentrate supplementation improved brain perfusion, task-related activation, and cognitive function (i.e., working memory) in healthy older adults who consumed 30 mL blueberry concentrate providing 387 mg anthocyanidins. 99 These studies suggest that berry fruit might be an effective strategy to prevent, delay, or reverse cognitive dysfunction during aging.
Cognitive aging does not occur simultaneously across cognitive domains, with various domains peaking in early adulthood before reaching a plateau or declining. Therefore, interventions early in life may yield health benefits that are only measureable in later life. Blueberries have been shown to have positive cognitive benefits in two acute, cross-over designed studies in school-aged children (ages 7–10). The first study 100 showed that consumption of a flavonoid-rich blueberry (200 g) drink led to significantly better delayed word-list recall, compared to a matched vehicle group, on the Rey auditory-verbal learning test, suggesting more effective coding of memory items. However, there was no benefit of blueberry intervention on measures of attention, response inhibition, or visuospatial memory, and a negative impact on proactive interference. 100 The second study 100 by the same group examined cognition at baseline, and then 1.15, 3, and 6 h after consuming placebo (vehicle) or blueberry drinks containing 15 or 30 g freeze-dried wild blueberry (WBB) powder. Consumption of WBB powder improved recall at 1.15 h, improved delayed word recognition, which was sustained at each time point measured, and improved accuracy on a challenging interference task at 3 h. The best cognitive performance was seen after the 30 g dose, and particularly on those tasks with a higher cognitive demand. 100
As humans age, their ability to defend against the effects of oxidative stress and inflammation weakens, putting elderly people at increased risk for neuronal disease and degradation. Neuroprotective foods, such as berries and other dark-colored fruits, represent one way to protect aging brains against this damage by reducing inflammation and oxidative stress in the brain, thereby protecting against cognitive declines in aged populations.
This review has highlighted the latest advances in how foods and patterns of consumption at different times of development affect the brain, and the behavioral manifestations that may result from these effects. For example, early life overfeeding can permanently sensitize the brain’s neuroinflammatory response to challenging stimuli resulting in cognitive and immune dysfunctions throughout life. ES alters brain function, via metabolic and nutritional factors, to increase vulnerability to develop emotional and cognitive disorders. Long-term and short-term consumption of high saturated fatty foods during adulthood produces a sensitized inflammatory phenotype, via a glucocorticoid rise, in the hippocampus, leading to learning and memory vulnerabilities. Imbalance of omega-3 and omega-6 PUFA contribute to neurodevelopmental disorders by altering microglial activation resulting in abnormal formation of neuronal networks and activity. Finally, consumption of fruits and vegetables high in polyphenolics can prevent and reverse age-related cognitive deficits by lowering oxidative stress and inflammation. Collectively these data show that attention to dietary composition is important for lasting impact beyond the metabolic and highlight the promising likelihood that we may improve our cognition throughout life and into the aging period with simple dietary interventions. These data highlight the need for food industries and science, alike, to focus on research and development of nutritional strategies that are most appropriate to support our cognitive and emotional health; foods that are high in omega-3 PUFA and polyphenolics may be a promising place to start.
Data availability
No data sets were generated or analyzed during the current study.
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384 , 766–781 (2014).
Article Google Scholar
Imamura, F. et al. Dietary quality among men and women in 187 countries in 1990 and 2010: a systematic assessment. Lancet Glob. Health 3 , e132–e142 (2015).
de Rooij, S. R., Wouters, H., Yonker, J. E., Painter, R. C. & Roseboom, T. J. Prenatal undernutrition and cognitive function in late adulthood. Proc. Natl. Acad. Sci. USA 107 , 16881–16886 (2010).
de Groot, R. H. et al. Prenatal famine exposure and cognition at age 59 years. Int. J. Epidemiol. 40 , 327–337 (2011).
Dabelea, D. et al. Intrauterine exposure to diabetes conveys risks for type 2 diabetes and obesity: a study of discordant sibships. Diabetes 49 , 2208–2211 (2000).
Article CAS Google Scholar
Boney, C. M., Verma, A., Tucker, R. & Vohr, B. R. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics 115 , e290–296 (2005).
Ong, Z. Y. & Muhlhausler, B. S. Maternal “junk-food” feeding of rat dams alters food choices and development of the mesolimbic reward pathway in the offspring. FASEB. J. 25 , 2167–2179 (2011).
Gugusheff, J. R., Ong, Z. Y. & Muhlhausler, B. S. A maternal “junk-food” diet reduces sensitivity to the opioid antagonist naloxone in offspring postweaning. FASEB. J. 27 , 1275–1284 (2013).
Miller, A. A. & Spencer, S. J. Obesity and neuroinflammation: a pathway to cognitive impairment. Brain Behav. Immun. 42 , 10–21 (2014).
Drover, J., Hoffman, D. R., Castaneda, Y. S., Morale, S. E. & Birch, E. E. Three randomized controlled trials of early long-chain polyunsaturated fatty acid supplementation on means-end problem solving in 9-month-olds. Child Dev. 80 , 1376–1384 (2009).
Ng, S. F. et al. Chronic high-fat diet in fathers programs beta-cell dysfunction in female rat offspring. Nature 467 , 963–966 (2010).
Rivera, H. M., Christiansen, K. J. & Sullivan, E. L. The role of maternal obesity in the risk of neuropsychiatric disorders. Front. Neurosci. 9 , 194 (2015).
Bolton, J. L. & Bilbo, S. D. Developmental programming of brain and behavior by perinatal diet: focus on inflammatory mechanisms. Dialogues Clin. Neurosci. 16 , 307–320 (2014).
Google Scholar
Stefanidis, A. & Spencer, S. J. Effects of neonatal overfeeding on juvenile and adult feeding and energy expenditure in the rat. PLoS One 7 , e52130 (2012).
De Luca, S. N. et al. Early life overfeeding impairs spatial memory performance by reducing microglial sensitivity to learning. J. Neuroinflammation 13 , 112 (2016).
Jeon, B. T. et al. Resveratrol attenuates obesity-associated peripheral and central inflammation and improves memory deficit in mice fed a high-fat diet. Diabetes 61 , 1444–1454 (2012).
Lu, J. et al. Ursolic acid improves high fat diet-induced cognitive impairments by blocking endoplasmic reticulum stress and IkappaB kinase beta/nuclear factor-kappaB-mediated inflammatory pathways in mice. Brain Behav. Immun. 25 , 1658–1667 (2011).
Sobesky, J. L. et al. High-fat diet consumption disrupts memory and primes elevations in hippocampal IL-1beta, an effect that can be prevented with dietary reversal or IL-1 receptor antagonism. Brain Behav. Immun. 42 , 22–32 (2014).
Soares, E. et al. Spatial memory impairments in a prediabetic rat model. Neuroscience 250 , 565–577 (2013).
Di Benedetto, S., Muller, L., Wenger, E., Duzel, S. & Pawelec, G. Contribution of neuroinflammation and immunity to brain aging and the mitigating effects of physical and cognitive interventions. Neurosci. Biobehav. Rev. 75 , 114–128 (2017).
Dupret, D. et al. Spatial learning depends on both the addition and removal of new hippocampal neurons. PLoS Biol. 5 , e214 (2007).
Elmore, M. R. et al. Colony-stimulating factor 1 receptor signaling is necessary for microglia viability, unmasking a microglia progenitor cell in the adult brain. Neuron 82 , 380–397 (2014).
Heim, C., Newport, D. J., Mletzko, T., Miller, A. H. & Nemeroff, C. B. The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology 33 , 693–710 (2008).
Naninck, E. F. et al. Chronic early life stress alters developmental and adult neurogenesis and impairs cognitive function in mice. Hippocampus 25 , 309–328 (2015).
Naninck, E. F. et al. Early micronutrient supplementation protects against early stress-induced cognitive impairments. FASEB. J. 31 , 505–518 (2017).
Weaver, I. C. et al. Epigenetic programming by maternal behavior. Nat. Neurosci. 7 , 847–854 (2004).
Ivy, A. S. et al. Hippocampal dysfunction and cognitive impairments provoked by chronic early-life stress involve excessive activation of CRH receptors. J. Neurosci. 30 , 13005–13015 (2010).
Lucassen, P. J. et al. Perinatal programming of adult hippocampal structure and function; emerging roles of stress, nutrition and epigenetics. Trends Neurosci. 36 , 621–631 (2013).
Danese, A. & Tan, M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol. Psychiatry 19 , 544–554 (2014).
Maniam, J., Antoniadis, C. P., Wang, K. W. & Morris, M. J. Early life stress induced by limited nesting material produces metabolic resilience in response to a high-fat and high-sugar diet in male rats. Front. Endocrinol. 6 , 138 (2015).
Monk, C., Georgieff, M. K. & Osterholm, E. A. Research review: maternal prenatal distress and poor nutrition—mutually influencing risk factors affecting infant neurocognitive development. J. Child Psychol. Psychiatry 54 , 115–130 (2013).
Brown, A. S., van Os, J., Driessens, C., Hoek, H. W. & Susser, E. S. Further evidence of relation between prenatal famine and major affective disorder. Am. J. Psychiatry 157 , 190–195 (2000).
Ivy, A. S., Brunson, K. L., Sandman, C. & Baram, T. Z. Dysfunctional nurturing behavior in rat dams with limited access to nesting material: a clinically relevant model for early-life stress. Neuroscience 154 , 1132–1142 (2008).
Rice, C. J., Sandman, C. A., Lenjavi, M. R. & Baram, T. Z. A novel mouse model for acute and long-lasting consequences of early life stress. Endocrinology 149 , 4892–4900 (2008).
Pleasure, S. J., Collins, A. E. & Lowenstein, D. H. Unique expression patterns of cell fate molecules delineate sequential stages of dentate gyrus development. J. Neurosci. 20 , 6095–6105 (2000).
CAS Google Scholar
Oomen, C. A., Bekinschtein, P., Kent, B. A., Saksida, L. M. & Bussey, T. J. Adult hippocampal neurogenesis and its role in cognition. Wiley Interdiscip. Rev. Cogn. Sci. 5 , 573–587 (2014).
Korosi, A. et al. Early-life stress mediated modulation of adult neurogenesis and behavior. Behav. Brain Res. 227 , 400–409 (2012).
Hoeijmakers, L. et al. Early-life stress lastingly alters the neuroinflammatory response to amyloid pathology in an Alzheimer’s disease mouse model. Brain Behav. Immun. 63 , 160–175 (2017).
Yam, K. Y. et al. Exposure to chronic early-life stress lastingly alters the adipose tissue, the leptin system and changes the vulnerability to western-style diet later in life in mice. Psychoneuroendocrinology 77 , 186–195 (2017).
Yam, K. Y., Naninck, E. F., Schmidt, M. V., Lucassen, P. J. & Korosi, A. Early-life adversity programs emotional functions and the neuroendocrine stress system: the contribution of nutrition, metabolic hormones and epigenetic mechanisms. Stress 18 , 328–342 (2015).
Micha, R. et al. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys. BMJ 348 , g2272 (2014).
Fryar, C. D., Carroll, M. D. & Ogden, C. L. Prevalence of overweight, obesity, and extreme obesity among adults aged 20 and over: United States, 1960–1962 through 2013–2014. NCHS Data Brief , 1–6 (2016).
Thaler, J. P. et al. Obesity is associated with hypothalamic injury in rodents and humans. J. Clin. Invest. 122 , 153–162 (2012).
Beilharz, J. E., Maniam, J. & Morris, M. J. Short-term exposure to a diet high in fat and sugar, or liquid sugar, selectively impairs hippocampal-dependent memory, with differential impacts on inflammation. Behav. Brain Res. 306 , 1–7 (2016).
De Souza, C. T. et al. Consumption of a fat-rich diet activates a proinflammatory response and induces insulin resistance in the hypothalamus. Endocrinology 146 , 4192–4199 (2005).
Milanski, M. et al. Saturated fatty acids produce an inflammatory response predominantly through the activation of TLR4 signaling in hypothalamus: implications for the pathogenesis of obesity. J. Neurosci. 29 , 359–370 (2009).
Maric, T., Woodside, B. & Luheshi, G. N. The effects of dietary saturated fat on basal hypothalamic neuroinflammation in rats. Brain Behav. Immun. 36 , 35–45 (2014).
Almeida-Suhett, C. P., Graham, A., Chen, Y. & Deuster, P. Behavioral changes in male mice fed a high-fat diet are associated with IL-1beta expression in specific brain regions. Physiol. Behav. 169 , 130–140 (2017).
Tran, D. M. & Westbrook, R. F. A high-fat high-sugar diet-induced impairment in place-recognition memory is reversible and training-dependent. Appetite 110 , 61–71 (2017).
Boitard, C. et al. Impairment of hippocampal-dependent memory induced by juvenile high-fat diet intake is associated with enhanced hippocampal inflammation in rats. Brain Behav. Immun. 40 , 9–17 (2014).
Sobesky, J. L. et al. Glucocorticoids mediate short-term high-fat diet induction of neuroinflammatory priming, the NLRP3 inflammasome, and the danger signal HMGB1. eNeuro 3 , 1–17 (2016).
Holloway, C. J. et al. A high-fat diet impairs cardiac high-energy phosphate metabolism and cognitive function in healthy human subjects. Am. J. Clin. Nutr. 93 , 748–755 (2011).
Tantot, F. et al. The effect of high-fat diet consumption on appetitive instrumental behavior in rats. Appetite 108 , 203–211 (2017).
Barrientos, R. M., Kitt, M. M., Watkins, L. R. & Maier, S. F. Neuroinflammation in the normal aging hippocampus. Neuroscience 309 , 84–99 (2015).
Frank, M. G., Miguel, Z. D., Watkins, L. R. & Maier, S. F. Prior exposure to glucocorticoids sensitizes the neuroinflammatory and peripheral inflammatory responses to E. coli lipopolysaccharide. Brain Behav. Immun. 24 , 19–30 (2010).
Barrientos, R. M. et al. Greater glucocorticoid receptor activation in hippocampus of aged rats sensitizes microglia. Neurobiol. Aging 36 , 1483–1495 (2015).
Frank, M. G., Hershman, S. A., Weber, M. D., Watkins, L. R. & Maier, S. F. Chronic exposure to exogenous glucocorticoids primes microglia to pro-inflammatory stimuli and induces NLRP3 mRNA in the hippocampus. Psychoneuroendocrinology 40 , 191–200 (2014).
Bazinet, R. P. & Laye, S. Polyunsaturated fatty acids and their metabolites in brain function and disease. Nat. Rev. Neurosci. 15 , 771–785 (2014).
Joffre, C., Nadjar, A., Lebbadi, M., Calon, F. & Laye, S. n-3 LCPUFA improves cognition: the young, the old and the sick. Prostaglandins Leukot. Essent. Fat. Acids 91 , 1–20 (2014).
Joffre, C. et al. Modulation of brain PUFA content in different experimental models of mice. Prostaglandins Leukot. Essent. Fat. Acids 114 , 1–10 (2016).
Kitson, A. P., Stroud, C. K. & Stark, K. D. Elevated production of docosahexaenoic acid in females: potential molecular mechanisms. Lipids 45 , 209–224 (2010).
Nguyen, L. N. et al. Mfsd2a is a transporter for the essential omega-3 fatty acid docosahexaenoic acid. Nature 509 , 503–506 (2014).
Saunders, E. F. et al. Omega-3 and Omega-6 polyunsaturated fatty acids in bipolar disorder: a review of biomarker and treatment studies. J. Clin. Psychiatry 77 , e1301–e1308 (2016).
Yassine, H. N. et al. Association of docosahexaenoic acid supplementation with alzheimer disease stage in apolipoprotein E epsilon4 carriers: a review. JAMA. Neurol. 74 , 339–347 (2017).
Bozzatello, P., Brignolo, E., De Grandi, E. & Bellino, S. Supplementation with omega-3 fatty acids in psychiatric disorders: a review of literature data. J. Clin. Med. 5 , 1–43 (2016).
Rapaport, M. H. et al. Inflammation as a predictive biomarker for response to omega-3 fatty acids in major depressive disorder: a proof-of-concept study. Mol. Psychiatry 21 , 71–79 (2016).
Burke, J. E. & Dennis, E. A. Phospholipase A2 structure/function, mechanism, and signaling. J. Lipid Res. 50 Suppl, S237–242 (2009).
Serhan, C. N. Pro-resolving lipid mediators are leads for resolution physiology. Nature 510 , 92–101 (2014).
Bazan, N. G. The docosanoid neuroprotectin D1 induces homeostatic regulation of neuroinflammation and cell survival. Prostaglandins Leukot. Essent. Fat. Acids 88 , 127–129 (2013).
Rey, C. et al. Resolvin D1 and E1 promote resolution of inflammation in microglial cells in vitro. Brain Behav. Immun. 55 , 249–259 (2016).
Lukiw, W. J. & Bazan, N. G. Neuroinflammatory signaling upregulation in Alzheimer’s disease. Neurochem. Res. 25 , 1173–1184 (2000).
Zhu, M. et al. Pro-resolving lipid mediators improve neuronal survival and increase Abeta42 phagocytosis. Mol. Neurobiol. 53 , 2733–2749 (2016).
Freund-Levi, Y. et al. Effects of omega-3 fatty acids on inflammatory markers in cerebrospinal fluid and plasma in Alzheimer’s disease: the OmegAD study. Dement. Geriatr. Cogn. Disord. 27 , 481–490 (2009).
Yuki, D. et al. DHA-PC and PSD-95 decrease after loss of synaptophysin and before neuronal loss in patients with Alzheimer’s disease. Sci. Rep. 4 , 7130 (2014).
Hjorth, E. et al. Omega-3 fatty acids enhance phagocytosis of Alzheimer’s disease-related amyloid-beta42 by human microglia and decrease inflammatory markers. J. Alzheimers Dis. 35 , 697–713 (2013).
Hopperton, K. E., Trepanier, M. O., Giuliano, V. & Bazinet, R. P. Brain omega-3 polyunsaturated fatty acids modulate microglia cell number and morphology in response to intracerebroventricular amyloid-beta 1-40 in mice. J. Neuroinflammation 13 , 257 (2016).
Kim, H. Y. & Spector, A. A. Synaptamide, endocannabinoid-like derivative of docosahexaenoic acid with cannabinoid-independent function. Prostaglandins Leukot. Essent. Fat. Acids 88 , 121–125 (2013).
Alhouayek, M. & Muccioli, G. G. COX-2-derived endocannabinoid metabolites as novel inflammatory mediators. Trends Pharmacol. Sci. 35 , 284–292 (2014).
Marsicano, G. & Lutz, B. Neuromodulatory functions of the endocannabinoid system. J. Endocrinol. Invest. 29 , 27–46 (2006).
Stella, N. Cannabinoid and cannabinoid-like receptors in microglia, astrocytes, and astrocytomas. Glia 58 , 1017–1030 (2010).
Bosch-Bouju, C., Layé, S. Dietary Omega-6/Omega-3 and Endocannabinoids: Implications for Brain Health and Diseases in Cannabinoids in Health and Disease (ed Meccariello, R.) InTech. https://doi.org/10.5772/62498 (2016).
Lafourcade, M. et al. Nutritional omega-3 deficiency abolishes endocannabinoid-mediated neuronal functions. Nat. Neurosci. 14 , 345–350 (2011).
Thomazeau, A., Bosch-Bouju, C., Manzoni, O. & Laye, S. Nutritional n-3 PUFA deficiency abolishes endocannabinoid gating of hippocampal long-term potentiation. Cereb. Cortex 27 , 2571–2579 (2017).
Castillo, P. E., Younts, T. J., Chavez, A. E. & Hashimotodani, Y. Endocannabinoid signaling and synaptic function. Neuron 76 , 70–81 (2012).
Miller, M. G., Thangthaeng, N., Poulose, S. M. & Shukitt-Hale, B. Role of fruits, nuts, and vegetables in maintaining cognitive health. Exp. Gerontol. 94 , 24–28 (2016).
Panza, F. et al. Metabolic syndrome and cognitive impairment: current epidemiology and possible underlying mechanisms. J. Alzheimers Dis. 21 , 691–724 (2010).
McGeer, P. L. & McGeer, E. G. The inflammatory response system of brain: implications for therapy of Alzheimer and other neurodegenerative diseases. Brain Res. Brain Res. Rev. 21 , 195–218 (1995).
Stevenson, D. E. & Hurst, R. D. Polyphenolic phytochemicals—just antioxidants or much more? Cell. Mol. Life Sci. 64 , 2900–2916 (2007).
Cavallo, D. N., Horino, M. & McCarthy, W. J. Adult intake of minimally processed fruits and vegetables: associations with cardiometabolic disease risk factors. J. Acad. Nutr. Diet. 116 , 1387–1394 (2016).
Miller, M. G. & Shukitt-Hale, B. Berry fruit enhances beneficial signaling in the brain. J. Agric. Food Chem. 60 , 5709–5715 (2012).
Lamport, D. J., Saunders, C., Butler, L. T. & Spencer, J. P. Fruits, vegetables, 100% juices, and cognitive function. Nutr. Rev. 72 , 774–789 (2014).
Joseph, J. A. et al. Long-term dietary strawberry, spinach, or vitamin E supplementation retards the onset of age-related neuronal signal-transduction and cognitive behavioral deficits. J. Neurosci. 18 , 8047–8055 (1998).
Joseph, J. A. et al. Reversals of age-related declines in neuronal signal transduction, cognitive, and motor behavioral deficits with blueberry, spinach, or strawberry dietary supplementation. J. Neurosci. 19 , 8114–8121 (1999).
Carey, A. N., Gomes, S. M. & Shukitt-Hale, B. Blueberry supplementation improves memory in middle-aged mice fed a high-fat diet. J. Agric. Food Chem. 62 , 3972–3978 (2014).
Andres-Lacueva, C. et al. Anthocyanins in aged blueberry-fed rats are found centrally and may enhance memory. Nutr. Neurosci. 8 , 111–120 (2005).
Devore, E. E., Kang, J. H., Breteler, M. M. & Grodstein, F. Dietary intakes of berries and flavonoids in relation to cognitive decline. Ann. Neurol. 72 , 135–143 (2012).
Krikorian, R. et al. Blueberry supplementation improves memory in older adults. J. Agric. Food Chem. 58 , 3996–4000 (2010).
Miller, M. G., Hamilton, D. A., Joseph, J. A. & Shukitt-Hale, B. Dietary blueberry improves cognition among older adults in a randomized, double-blind, placebo-controlled trial. Eur. J. Nutr. https://doi.org/10.1007/s00394-017-1400-8 (2017).
Bowtell, J. L., Aboo-Bakkar, Z., Conway, M., Adlam, A. R. & Fulford, J. Enhanced task related brain activation and resting perfusion in healthy older adults after chronic blueberry supplementation. Appl. Physiol. Nutr. Metabol. 42 , 773–779 (2017).
Whyte, A. R. & Williams, C. M. Effects of a single dose of a flavonoid-rich blueberry drink on memory in 8 to 10 y old children. Nutrition 31 , 531–534 (2015).
Download references
Acknowledgements
This work was supported by funding from by a National Health and Medical Research Council Career Development Fellowship, a Club Melbourne Fellowship and a Brain Foundation Research Gift to S.J.S., an NWO Meervoud and NWO Food Cognition and Behavior (NWO-FCB), JPI-Nutricog to A.K., and funding from the USDA Intramural, U.S. Highbush Blueberry Council, and California Strawberry Commission to B.SH.
Author information
Authors and affiliations.
School of Health and Biomedical Sciences, RMIT University, Melbourne, VIC, 3788, Australia
Sarah J. Spencer
Swammerdam Institute for Life Sciences, Center for Neuroscience, University of Amsterdam, Amsterdam, 1098 XH, Netherlands
Aniko Korosi
Nutrition et Neurobiologie Intégrée, INRA, Bordeaux University, Bordeaux, UMR1286, France
Sophie Layé
USDA-ARS, Human Nutrition Research Center On Aging at Tufts University, Boston, MA, 02111-1524, USA
Barbara Shukitt-Hale
Department of Psychology & Neuroscience, and Center for Neuroscience, University of Colorado, Campus Box 345, Boulder, CO, 80309-0345, USA
Ruth M. Barrientos
You can also search for this author in PubMed Google Scholar
Contributions
All authors made substantial contributions to the design and conception of the work, drafting it, revising it critically for important intellectual content. All authors approve the completed version.
Corresponding author
Correspondence to Sarah J. Spencer .
Ethics declarations
Competing interests.
The authors declare that they have no competing financial interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Spencer, S.J., Korosi, A., Layé, S. et al. Food for thought: how nutrition impacts cognition and emotion. npj Sci Food 1 , 7 (2017). https://doi.org/10.1038/s41538-017-0008-y
Download citation
Received : 30 April 2017
Revised : 24 July 2017
Accepted : 10 August 2017
Published : 06 December 2017
DOI : https://doi.org/10.1038/s41538-017-0008-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Epigenetic orchestration of neurodegenerative disorders: a possible target for curcumin as a therapeutic.
- Shweta Tripathi
Neurochemical Research (2024)
Identifying distinct subtypes of mother-to-infant bonding using latent profile analysis in a nationwide Japanese study
- Kosuke Hagiwara
- Takahiro Tabuchi
Archives of Women's Mental Health (2024)
Nutritional strategies cause memory damage and alter biochemical parameters without causing neuroinflammation
- Keila Rufatto de Souza
- Nicole Alessandra Engel
- Gislaine Tezza Rezin
Metabolic Brain Disease (2024)
Exploring the effects of health behaviors and mental health on students’ academic achievement: a cross-sectional study on lebanese university students
- Dalal Hammoudi Halat
- Souheil Hallit
- Mohamad Rahal
BMC Public Health (2023)
Human nutritional relevance and suggested nutritional guidelines for vitamin A5/X and provitamin A5/X
- Torsten Bohn
- Julian Hellman-Regen
Nutrition & Metabolism (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Mindful Eating

What Is It?
Mindful eating stems from the broader philosophy of mindfulness, a widespread, centuries-old practice used in many religions. Mindfulness is an intentional focus on one’s thoughts, emotions, and physical sensations in the present moment. Mindfulness targets becoming more aware of, rather than reacting to, one’s situation and choices. Eating mindfully means that you are using all of your physical and emotional senses to experience and enjoy the food choices you make. This helps to increase gratitude for food, which can improve the overall eating experience. Mindful eating encourages one to make choices that will be satisfying and nourishing to the body. However, it discourages “judging” one’s eating behaviors as there are different types of eating experiences. As we become more aware of our eating habits, we may take steps towards behavior changes that will benefit ourselves and our environment.
How It Works
Mindful eating focuses on your eating experiences, body-related sensations, and thoughts and feelings about food, with heightened awareness and without judgment. Attention is paid to the foods being chosen, internal and external physical cues, and your responses to those cues. [1] The goal is to promote a more enjoyable meal experience and understanding of the eating environment. Fung and colleagues described a mindful eating model that is guided by four aspects: what to eat , why we eat what we eat , how much to eat , and how to eat . [1]
Mindful eating:
- considers the wider spectrum of the meal: where the food came from, how it was prepared, and who prepared it
- notices internal and external cues that affect how much we eat
- notices how the food looks, tastes, smells, and feels in our bodies as we eat
- acknowledges how the body feels after eating the meal
- expresses gratitude for the meal
- may use deep breathing or meditation before or after the meal
- reflects on how our food choices affect our local and global environment
Seven practices of mindful eating
- Honor the food . Acknowledge where the food was grown and who prepared the meal. Eat without distractions to help deepen the eating experience.
- Engage all senses . Notice the sounds, colors, smells, tastes, and textures of the food and how you feel when eating. Pause periodically to engage these senses.
- Serve in modest portions . This can help avoid overeating and food waste. Use a dinner plate no larger than 9 inches across and fill it only once.
- Savor small bites, and chew thoroughly . These practices can help slow down the meal and fully experience the food’s flavors.
- Eat slowly to avoid overeating . If you eat slowly, you are more likely to recognize when you are feeling satisfied, or when you are about 80% full, and can stop eating.
- Don’t skip meals . Going too long without eating increases the risk of strong hunger, which may lead to the quickest and easiest food choice, not always a healthful one. Setting meals at around the same time each day, as well as planning for enough time to enjoy a meal or snack reduces these risks.
- Eat a plant-based diet, for your health and for the planet . Consider the long-term effects of eating certain foods. Processed meat and saturated fat are associated with an increased risk of colon cancer and heart disease . Production of animal-based foods like meat and dairy takes a heavier toll on our environment than plant-based foods.
Watch: Practicing mindful eating
The Research So Far
The opposite of mindful eating, sometimes referred to as mindless or distracted eating, is associated with anxiety, overeating, and weight gain. [3] Examples of mindless eating are eating while driving, while working, or viewing a television or other screen (phone, tablet). [4] Although socializing with friends and family during a meal can enhance an eating experience, talking on the phone or taking a work call while eating can detract from it. In these scenarios, one is not fully focused on and enjoying the meal experience. Interest in mindful eating has grown as a strategy to eat with less distractions and to improve eating behaviors.
Intervention studies have shown that mindfulness approaches can be an effective tool in the treatment of unfavorable behaviors such as emotional eating and binge eating that can lead to weight gain and obesity, although weight loss as an outcome measure is not always seen. [5-7] This may be due to differences in study design in which information on diet quality or weight loss may or may not be provided. Mindfulness addresses the shame and guilt associated with these behaviors by promoting a non-judgmental attitude. Mindfulness training develops the skills needed to be aware of and accept thoughts and emotions without judgment; it also distinguishes between emotional versus physical hunger cues. These skills can improve one’s ability to cope with the psychological distress that sometimes leads to binge eating. [6]
Mindful eating is sometimes associated with a higher diet quality, such as choosing fruit instead of sweets as a snack, or opting for smaller serving sizes of calorie-dense foods. [1]
- A literature review of 68 intervention and observational studies on mindfulness and mindful eating found that these strategies improved eating behaviors such as slowing down the pace of a meal and recognizing feelings of fullness and greater control over eating. [8] Slower eating was associated with eating less food, as participants felt fuller sooner. Mindfulness and mindful eating interventions appeared most successful in reducing binge eating and emotional eating. However, the review did not show that these interventions consistently reduced body weight. Limitation of the studies included small sample sizes, limited durations of about 6 months or less, lack of focus on diet quality, and lack of follow-up so that longer-term success was not determined.
- A randomized controlled trial following 194 adults with obesity (78% were women) for 5.5 months looked at the effects of a mindfulness intervention on mindful eating, sweets consumption, and fasting glucose levels. The participants were randomly assigned to one of two groups: a diet and exercise program with mindfulness concepts (stress reduction, chair yoga, meditation, affirmations) or the same program but without mindfulness concepts. After 12 months, the mindfulness group showed a decreased intake of sweets and maintenance of fasting blood glucose, as opposed to the control group showing increased fasting blood glucose. [9] The research authors also evaluated weight loss with these participants, but did not find a significant difference in weight changes between the mindfulness group and control group. [10]
- A small controlled trial of 50 adults with type 2 diabetes were randomized to either a 3-month mindful eating intervention that was focused on reducing overeating and improving eating regulation or to a diabetes self-management education (DSME) intervention that was focused on improving food choices. Both groups showed significant improvements in measures of depression, nutrition self-efficacy, and controlling overeating behaviors. Both groups lost weight during the intervention but there was no difference in amount of weight loss between groups. [11]
It is important to note that currently there is no standard for what defines mindful eating behavior, and there is no one widely recognized standardized protocol for mindful eating. Research uses a variety of mindfulness scales and questionnaires. Study designs often vary as well, with some protocols including a weight reduction component or basic education on diet quality, while others do not. Additional research is needed to determine what behaviors constitute a mindful eating practice so that a more standardized approach can be used in future studies. [1] Standardized tools can help to determine the longer-term impact of mindful eating on health behaviors and disease risk and prevention, and determine which groups of people may most benefit from mindfulness strategies. [1]
Mindfulness is a strategy used to address unfavorable eating behaviors in adults, and there is emerging interest in applying this method in adolescents and children due to the high prevalence of unhealthy food behaviors and obesity in younger ages. More than one-third of adolescents in the U.S. have overweight or obesity. Youth who have overweight/obesity are likely to experience weight-related stigma and bullying by their peers, which in turn can negatively affect eating behaviors and lead to eating disorders. [12] Studies have found that eating disorders are developing at younger ages, with an increased number of children younger than 12 years of age presenting for treatment. [12]
- A review of 15 studies of mindfulness-based interventions in adolescents found that mindfulness techniques were associated with reduced concerns about body shape, less dietary restraint, decreased weight, and less binge eating. [12] However, interestingly, the overall acceptability of the mindfulness-related interventions was rated low by the participants, compared with general health education. It is likely that the way mindful strategies are presented to younger ages needs better understanding as it may be different than in adults. An example could be using new online technologies that are specific to their developmental age and learning ability. The review also found that mindfulness in the form of meditation and mindful breathing can have significant effects on disordered eating through better stress management and reduced overeating caused by depression and anxiety.
- Studies are still scarce in children, but novel programs are emerging. A pilot mindful eating intervention was tested in a low-income school in California involving third-through-fifth grade children including Hispanic and non-Hispanic children. [13] The goal was to foster healthy eating behaviors in the children and their parents. The program included topics such as “Master Mindless Munching,” “Getting to Know Hunger and Fullness,” and “Sensational Senses,” and provided take-home activities to do with their parents. Surveys at the end of the program showed that the children and parents liked the activities, and there was an increase in parents serving nutritious meals and practicing mindfulness during meals (e.g., recognizing when hungry vs. full).
Potential Pitfalls
- Mindful eating is not intended to replace traditional treatments for severe clinical conditions such as eating disorders . Neurochemical imbalances are a risk factor for developing eating disorders such as bulimia and anorexia nervosa, and although mindfulness may be an effective component of a treatment plan, it should not be used as a sole treatment.
- May not be effective as a weight loss strategy on its own, but rather a complement to a weight loss program. Mindful eating embraces making food choices that promote well-being and increasing enjoyment of the eating experience. Traditional weight loss regimens focus on following a structured meal plan that may not necessarily be satisfying or enjoyable. Combining mindfulness with a meal plan under the guidance of a registered dietitian may reduce the risk of emotional overeating or binge eating. [14] Research has not consistently shown that mindfulness strategies lead to weight loss, but this may be due to the study design not including education on healthy eating choices as part of the mindfulness intervention.

Bottom Line
Mindful eating is an approach to eating that can complement any eating pattern. Research has shown that mindful eating can lead to greater psychological wellbeing, increased pleasure when eating, and body satisfaction. Combining behavioral strategies such as mindfulness training with nutrition knowledge can lead to healthful food choices that reduce the risk of chronic diseases, promote more enjoyable meal experiences, and support a healthy body image. More research is needed to examine whether mindful eating is an effective strategy for weight management.
Mindful eating in context of COVID-19
In the meantime, individuals may consider incorporating any number of mindful eating strategies in their daily lives alongside other important measures to help stay healthy during COVID-19 . For example:
- If you’re working from home and find that “office” time blends into all hours of the day, schedule times in your calendar to only eat : a lunch break away from your computer, a reserved time for dinner with your family, etc.
- If you find yourself standing in your pantry or staring in your refrigerator, pause and ask yourself: “am I truly hungry, or am I just bored or stressed?” If hungry, eat. If boredom or stress is the source, reroute your attention to an activity you enjoy, call a friend, or simply spend some time breathing.
- If you have a craving for comfort foods, pause and take a few in-breaths and out-breaths to be fully present with your craving. Take a portion of the food from the container (a handful of chips, a scoop of ice cream) and put it on a plate. Eat mindfully, savoring each bite.
A note about eating disorders : The COVID-19 pandemic may raise unique challenges for individuals with experience of eating disorders. [17] In the U.S., the National Eating Disorders Association has reported a significant increase in calls and messages for help as compared to a year ago. As noted, mindful eating is not intended to replace traditional treatments for severe clinical conditions such as eating disorders. If you or someone you know is struggling with an eating disorder, you can call the National Eating Disorders Association Helpline at 1-800-931-2237, or text “NEDA” to 741-741.
A note about food insecurity : Many individuals may be facing food shortages because of unemployment or other issues related to the pandemic. If you (or someone you know) are struggling to access enough food to keep yourself or your family healthy, there are several options to help. Learn more about navigating supplemental food resources .
- Healthy Weight
- The Best Diet: Quality Counts
- Diet Reviews
- Fung TT, Long MW, Hung P, Cheung LW. An expanded model for mindful eating for health promotion and sustainability: issues and challenges for dietetics practice. Journal of the Academy of Nutrition and Dietetics . 2016 Jul 1;116(7):1081-6.
- Hanh TN, Cheung L. Savor: Mindful Eating, Mindful Life . HarperCollins Publishers. 2010.
- Stanszus LS, Frank P, Geiger SM. Healthy eating and sustainable nutrition through mindfulness? Mixed method results of a controlled intervention study. Appetite . 2019 Oct 1;141:104325.
- Ogden J, Coop N, Cousins C, Crump R, Field L, Hughes S, Woodger N. Distraction, the desire to eat and food intake. Towards an expanded model of mindless eating. Appetite . 2013 Mar 1;62:119-26.
- Katterman SN, Kleinman BM, Hood MM, Nackers LM, Corsica JA. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eating behaviors . 2014 Apr 1;15(2):197-204.
- O’Reilly GA, Cook L, Spruijt‐Metz D, Black DS. Mindfulness‐based interventions for obesity‐related eating behaviours: a literature review. Obesity reviews . 2014 Jun;15(6):453-61.
- Ruffault A, Czernichow S, Hagger MS, Ferrand M, Erichot N, Carette C, Boujut E, Flahault C. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: A systematic review and meta-analysis. Obesity research & clinical practice . 2017 Sep 1;11(5):90-111.
- Warren JM, Smith N, Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: effectiveness and associated potential mechanisms. Nutrition research reviews . 2017 Dec;30(2):272-83. *Disclosure: Study was funded by Mondelez International.
- Mason AE, Epel ES, Kristeller J, Moran PJ, Dallman M, Lustig RH, Acree M, Bacchetti P, Laraia BA, Hecht FM, Daubenmier J. Effects of a mindfulness-based intervention on mindful eating, sweets consumption, and fasting glucose levels in obese adults: data from the SHINE randomized controlled trial. Journal of behavioral medicine . 2016 Apr 1;39(2):201-13.
- Daubenmier J, Moran PJ, Kristeller J, Acree M, Bacchetti P, Kemeny ME, Dallman M, Lustig RH, Grunfeld C, Nixon DF, Milush JM. Effects of a mindfulness‐based weight loss intervention in adults with obesity: A randomized clinical trial. Obesity . 2016 Apr;24(4):794-804.
- Miller CK, Kristeller JL, Headings A, Nagaraja H. Comparison of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a randomized controlled trial. Health Education & Behavior . 2014 Apr;41(2):145-54.
- Omiwole M, Richardson C, Huniewicz P, Dettmer E, Paslakis G. Review of mindfulness-related interventions to modify eating behaviors in adolescents. Nutrients . 2019 Dec;11(12):2917.
- Wylie A, Pierson S, Goto K, Giampaoli J. Evaluation of a mindful eating intervention curriculum among elementary school children and their parents. Journal of nutrition education and behavior . 2018 Feb 1;50(2):206-8.
- Tapper K, Shaw C, Ilsley J, Hill AJ, Bond FW, Moore L. Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite . 2009 Apr 1;52(2):396-404.
- Bhutani S, Cooper JA. COVID‐19 related home confinement in adults: weight gain risks and opportunities. Obesity . 2020 May 19.
- Clemmensen C, Petersen MB, Sørensen TI. Will the COVID-19 pandemic worsen the obesity epidemic?. Nature Reviews Endocrinology . 2020 Sep;16(9):469-70.
- Branley-Bell D, Talbot CV. Exploring the impact of the COVID-19 pandemic and UK lockdown on individuals with experience of eating disorders. Journal of Eating Disorders . 2-2020 Aug;8(44).
Last reviewed September 2020
Terms of Use
The contents of this website are for educational purposes and are not intended to offer personal medical advice. You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products.
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, students' knowledge of healthy food and their actual eating habits: a case study on the university of granada (spain).

- Department of Sociology, Faculty of Political Sciences and Sociology, University of Granada, Granada, Spain
This article focuses on an analysis of the discourses produced during 34 semi-structured interviews (17 men and 17 women) conducted at the University of Granada (Spain) with undergraduate, Master, and Ph.D. students. The interviewees were between 20 and 44 years old. It was observed that the fact of having a high educational level did not prevent University students from eating unhealthily. There is a gap between the fact that 97.1% of 34 students interviewed (that is, 33 of them) know what healthy food is and their self-perception about whether or not what they are eating is healthy, since in 41.2% of them said self-perception is negative. This gap narrows as the interviewees' age increases and their socio-economic and vital situation is stabilizing which favors that their eating habits become more regular and healthier. Thus, all the interviewees aged 27 or over self-perceived that they were eating healthily. But the biggest differences are those that have to do with the gender of interviewees. Thus, while 23.5% of women interviewed perceived that they were not eating healthy, 76.5% of them felt that they were eating healthy. However, among the men interviewed, these percentages were somehow reversed, in such a way that 58.8% of them believed that they were not eating healthy, compared to 41.2% of them who indicated that they were eating healthy. Therefore, the investigation revealed that women tend to have the best chances of assuming healthy eating habits. Male students living outside the family home or without female partners exhibited greater feeding problems, while females living under similar conditions tended to display healthier eating habits. This is related to the fact that women have traditionally been in charge of acquiring and preparing food. So, women's food education has not been restricted to the mere transmission to them of knowledge about what healthy food is, but from their childhood they were food trained through their active involvement in practical experiences. Obviously, the solution proposed to this male disadvantage is to not perpetuate macho gender stereotypes that assign women the role of home caregivers, but to seek that both women and men have the opportunity and the duty to experience equally those practical experiences that involve the tasks of the acquisition and preparation of food. Working to achieve a situation like this, not only promotes progress in gender equality, but also helps to overcome the lower training of men to perform the tasks inherent in their diet.
Introduction
Beyond being an action, whose only purpose is to satisfy one of the most primitive needs of human beings, feeding should be understood as a social practice that is socially constructed and/or reconstructed over time ( Berger and Luckmann, 1979 ; Verplanken and Faes, 1999 ; García-Cardona et al., 2008 ). The family home is the first environment of socialization and personality formation ( Isaza, 2012 ). Thus, the family home constitutes the primary social space in which individuals' practices, customs, gender identity/roles and social habits begin to develop; particularly, individuals' eating habits. Such habits are understood here as the set of feeding-related social customs that influence the way people prepare, consume, or even select food. Therefore, preparing and consuming food are cultural behaviors that provide individuals with an identity ( Fischler, 1980 ; FAO, 2008 ; Barilla Center for Food Nutrition, 2009 ; Almerico, 2014 ; Cox, 2014 ; Silva et al., 2014 ; The Nielsen Company, 2015 ; Levine et al., 2016 ). The food people consume and how the food is consumed are essential determinants of health. Regarding this matter, here we mention only a few references from an abundant bibliography ( Willett et al., 1995 ; Martín Criado, 2004 ; Díaz-Méndez and Gómez-Benito, 2008 ; Gracia-Arnáiz, 2010 ; Guenther et al., 2013 ; Martinez-Lacoba et al., 2018 ).
Growing concerns about eating healthy foods have emerged as the consumption of industrially produced foods has augmented, and the negative consequences of industrially produced foods are increasingly acknowledged. Obesity is among the most widespread consequences. For instance, according to the Organization for Economic Co-operation and Development ( OECD, 2017a ), obesity has rapidly increased in OECD countries from 2010 and not only among adults, since children constitute 24.6% of the overweight population. Additionally, the OECD (2017a) reported that 19.5% of the population in Europe was overweight or obese in 2015, and this percentage exceeded that in other countries, such as Korea and Japan (6%), but was less than that in New Zealand, Mexico, and the United States (30%). Therefore, unsurprisingly, ischemic heart disease (10.6% in women and 12.8% in men) and heart attacks (8.2% in women and 7% in men) are currently among the main causes of death in Europe.
In the Spanish context, people are attempting to acquire better eating habits, as indicated by the Organization of Consumers and Users ( OCU, 2017 ). According to data from an OCU interview, the respondents reduced their consumption of sugar-sweetened beverages by 56%, pastries and sweets by 47%, and alcohol by 38%, while the consumption of fruits has increased by 30% and vegetables by 31%. Among all explanations given by the interviewees about these changes, their concern regarding their health was the most frequent, which is in line with the growing awareness that food plays a key role in people's health ( Cubero-Juánez et al., 2017 ; De Ridder et al., 2017 ; Dernini et al., 2017 ; Grosso et al., 2017 ; Oliffe et al., 2017 ; WHO, 2018 ). However, despite efforts to improve their eating habits, Spanish people have not yet managed to consume the healthiest possible diets ( OCU, 2019 ).
According to the National Institute of Statistics ( INE ), in 2019 , 18.7% of Spaniards aged 16 years and over reported that their health was “very good,” while 56.6% of the respondents described their health as “good.” Only 5.6% of the population considered their health “bad,” and 1.5% of the population considered their heath “very bad.” Regarding the healthiness of food, a report by OCU (2017) pointed out that 6% of Spaniards consumed more sweets and sweetened beverages, 7% of Spaniards consumed less fruit, and 5% of Spaniards consumed fewer vegetables than 2 years before. Among the reasons given in the report, the Spaniards indicated that they did not changed their bad eating habits due to the lack of time or will. However, Spaniards are not the only individuals who show the consequences of adopting unhealthy eating habits. Thus, regarding the percentage of individuals who are obese or overweight due to inadequate nutrition, some European Union countries are even above the Spanish average (16.7%), such as the United Kingdom (26.9%), Germany (23.6%), and Luxembourg (22.6%) ( OECD, 2017b ).
In these circumstances, as this article shows, even the fact of having a high level of studies, does not guarantee the strengthening of good and healthy eating practices among the University students interviewed ( Entrena-Durán et al., 2020 ). Thus, as revealed by the research “Effects of Age and Gender Identity on the Healthiness of University Students' Eating Habits in Spain” on which the writing of this article has been based, all the interviewees know what constitutes healthy food because of their elevated educational level. However, this knowledge does not always lead them to eat healthy. Achieving a healthy diet also requires the internalization and implementation of daily healthy eating habits. For that reason, the subsequent analysis focuses on the role that age and gender identity play in facilitating or hindering the acquisition of such habits to young men and women interviewed for this study.
Materials and Methods
This research study analyzed the eating habits reported in the interviews with a group of students at Granada University (Spain). In this regard, we clarify here that we have focused our research on University students because this social group is very appropriate to study how life crises (these usually appear as a consequence of the change processes in which people are involved) affect to eating patterns and habits. Thus, when young students enter the University, they usually undergo a deep change and an important life crisis, since many of them have to leave their home and move away from their families. As a consequence, these students experience the loss of the relatively stable living environment where they have resided until then, in which their diet, analogous to the generality of their life, has usually been regulated by their parents; mainly by their mothers, who have been responsible for the tasks of acquisition and preparation of food for the family.
All these sudden changes explain that a series of eating problems, such as the irregularity in meal times, the excessive consumption of fast food, the follow-up of nutritionally inadequate diets or the high incidence of eating disorders, are frequent among the University population ( Ruiz-Moreno et al., 2013 ).
A qualitative study, based on semi-structured interviews, was carried out in order to understand the knowledge the subjects analyzed have about the motivations behind the aforementioned eating problems. The qualitative methodology of our research has allowed us to comprehend, through the analysis of discourses produced by the students interviewed, how these students experience and explain their eating disorders.
We selected our sample among students of the University of Granada, but this should not be understood in the sense that we have limited ourselves to doing research with local students. In fact, this limitation has not occurred because the University of Granada has an outstanding national and international position. Thus, the 2020 edition of the Academic Ranking of World Universities (ARWU), also known as the Shanghai Ranking, has placed the University of Granada among the 300 best Universities in the world. In this Ranking, as has been happening in the last 5 years, the UGR appears in positions 201–300, where the Autonomous University of Barcelona, the Complutense University of Madrid and the University of Valencia are also located. This circumstance, together with the fact that the University of Granada has a long tradition of international academic cooperation, explains that many students come to Granada from all over Spain, as well as from very different countries abroad; mainly, from the European Union (EU). Particularly, with regard to the EU, the University of Granada is the Spanish University that accepts more foreign students within the framework of the Erasmus Program. So, as can be seen in Table 1 , in the selected sample for this study only 14 students are from the municipality of Granada or its province, while the remaining 20 students interviewed came from other Spanish provinces or even from abroad. In other words, 41.2% of those interviewees are from Granada or its province and 58.8% of them came from other parts of Spain, and even some of these students are from foreign countries.
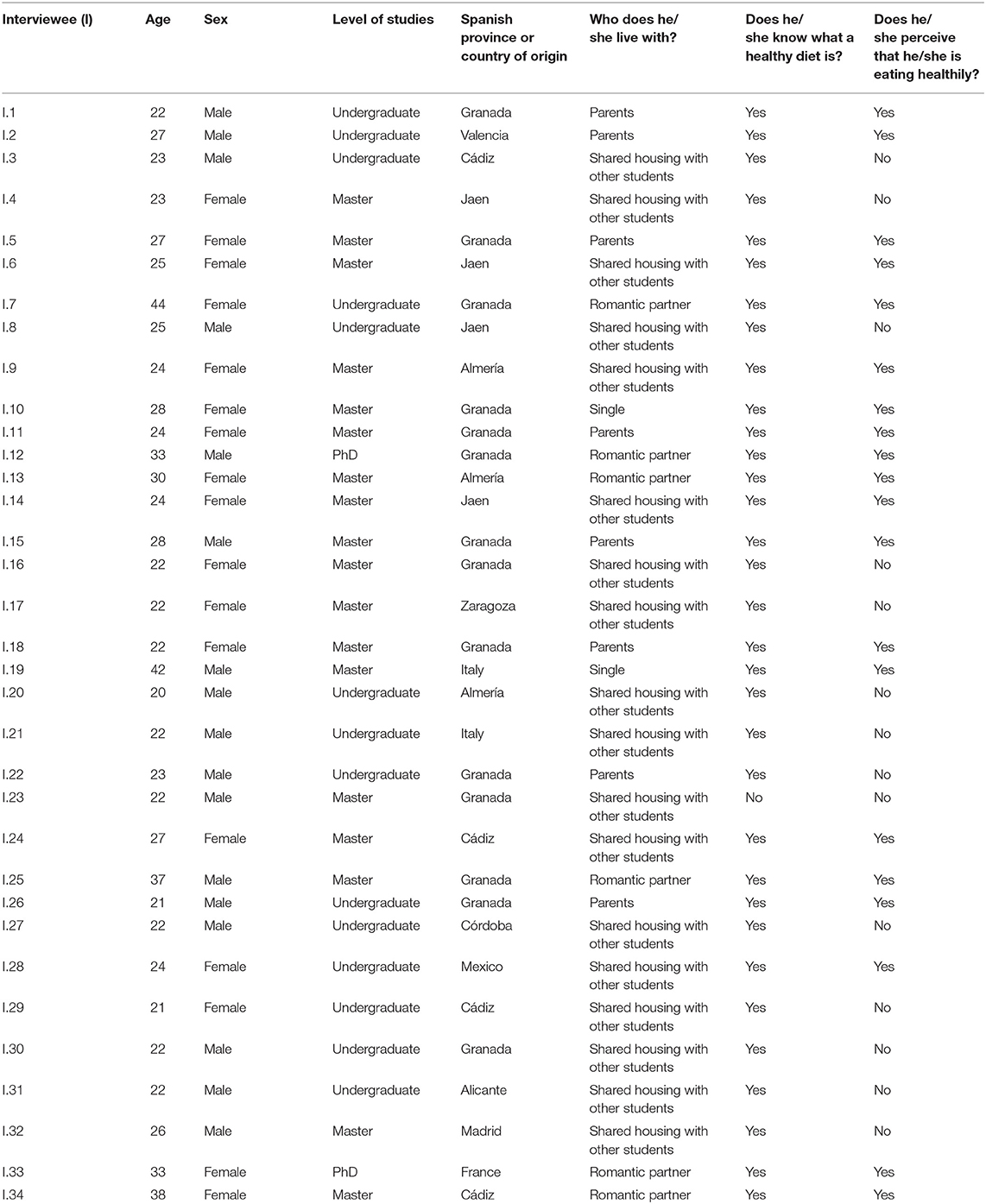
Table 1 . List of interviewees.
The selected sample contained a group of 14 undergraduate, 18 Master, and 2 Ph.D. students which were chosen using a non-probability purposive sampling method. Therefore, we interviewed 34 students (17 women and 17 men) who were between the ages of 20 and 44. The leading reason for deciding to conclude the fieldwork with 34 interviews was because we saw no additional information was obtained from the new interviews done.
The 34 students interviewed were not told that we were going to investigate the influence of their age and gender identity on the healthiness of their eating habits. They were only told that our interviews were intended to both know their self-perception about their own eating behaviors and their opinions regarding the healthiness of eating habits in Spain.
The interviews lasted between 45 and 60 min, depending on the respondents' motivation in answering the questions. Most participants in this study were highly receptive and communicative. All interviews were recorded with the prior consent of the interviewees.
After all interviews were done, we analyzed all collected information. First, we focused on assessing whether the interviewees were aware of the need to adopt healthy eating habits and how to identify healthy food. Once we verified that 97.1% of 34 interviewees (that is, 33 of them) were aware of these feeding issues (mainly due to their educational level), we investigated the reasons why this awareness or conscience did not motivate many of them to change their eating habits to healthier ones, so that, there is a gap between what the interviewees thought they knew and their real eating behaviors.
As just said, there is a gap between the fact that 33 of 34 students interviewed (that is, 97.1% of them) know what healthy food is and their self-perception about whether or not what they are eating is healthy (see Table 1 ). So, in 14 of them said self-perception is negative; that is in 41.2% of the selected sample. This gap narrows as the interviewees' age increases and their socio-economic and vital situation is stabilizing, which favors that their eating habits become more regular and healthier. Thus, all the interviewees aged 27 or over self-perceived that they were eating healthily. But the biggest differences are those that have to do with the gender of interviewees.
Likewise, Table 1 shows how only 4 of the 17 women interviewed perceive that they do not eat healthy, while 13 of them perceive that they eat healthy. As for men, there are 10 who perceive that they do not eat healthy and 7 who think that they eat healthy. But, it should be noted the fact that four of these men live with their parents, two with their female romantic partners and only one lives alone, but he is 42 years old and, therefore, he is more aware of the need to eat healthy. In other words, there are important differences according to gender in the perceptions of the interviewees about the healthiness of their diet. Thus, while 23.5% of women interviewed perceived that they were not eating healthy, 76.5% of them felt that they were eating healthy. However, among the men interviewed, these percentages were somehow reversed, in such a way that 58.8% of them believed that they were not eating healthy, compared to 41.2% of them who affirmed that they were eating healthy.
Moreover, one significant thing we note in this research is that, due to their high educational level, the generality of interviewees, regardless of their gender, show an absolute distrust of advertisements. Therefore, all University students analyzed seemed to be aware of the “tricks” used by advertising to cajole and attract consumers toward their products regardless of whether such products are healthy. Both women and men revealed some distrust of food ads.
“Often, the labeling of products is pure marketing, selling methods that companies have to create new demands for consumers. For instance, people want to be healthier, and the response of companies is offering milk with added calcium or omega 3, which was not initially demanded by the people. All our lives, we have taken untreated milk that was healthy, but now, they are selling us Premium milk, which is milk with new additives. So, a demand that you did not have before is now being produced” (Man, 37 years old).
However, surprisingly, only 7 of 34 interviewed students (that is, 20.6% of them) openly stated that they usually read the labels of the foods they consume. Only two of these seven students were men, but they were especially motivated to verify these labels since they were both vegans.
“I look at the labels of products, their images, their presentation. I try not to buy many packaged products because they put many images of trees and/or fruits. and so, they try to deceive us. However, sometimes, I have bought these kinds of products, and when I think about it later, I say to myself ‘I've let myself be cajoled’, but anyway. I think so many products are being sold to us in this way now” (Man, 22 years old).
The importance of regulating food advertising was also noted by the interviewees with an emphasis on advertising targeting children.
“It is necessary to intensify and improve the regulations of industrial food advertising (industrial bakery, sugary soft drinks and so on) above all in children's programs since children are very vulnerable. Although, often, children are not the ones who buy the food they see in the ads of the supermarket, but their parents buy it.” (Man, 42 years old).
As shown in Table 1 , the aforementioned fact that 97.1% of 34 interviewed (that is, 33 of them) clearly distinguished between healthy and unhealthy food does not mean that 97.1% of students eat healthily. So, 32 interviewees (namely, 94.1% of them) confessed that they allowed themselves one or another “whim” in their everyday lives. For instance, the respondents consumed precooked foods, such as pizza and lasagna, and industrially manufactured sweets and ice cream. Furthermore, while 22 interviewees (namely, 64.7% of interviewees) said that they had some concern about their diet, the fact is that only 15 students (44.1% of them) expressed a settled intention to get a healthy diet. Most of these students were women, although the case of some men is also significant, such as this 27-year-old man, for whom a healthy diet is the one that is as varied as possible.
“I am quite influenced by my grandmother's meals; so, what I usually prepare to eat is traditional meals, such as lentil soups or stews… I do not usually repeat the meal in the same week; so, what I understand for a healthy diet is to eat as much variety as possible” (Man, 27 years old).
In particular, 14 students (41.2% of the sample), of which 8 were women, said they were selective regarding the foods they consumed, and they attempted to review the labels and composition of each product. Nevertheless, most interviewees (58.8% of them) said that they do not usually review the labels of products because they do not understand them, or they lack the time. Moreover, when they review the labels, they are rushed and only superficially read them.
“I don't pay attention to labels basically because I cannot understand them. There are all ingredients, but when you start reading something called ‘E’ and this kind of things… I cannot understand them” (Man, 27 years old).
“Sometimes when I buy frozen foods, I see the labels… When the freezing process began, the expiration date, if it has saturated fats. but the truth is that it is not something that I usually do” (Woman, 24 years old).
“The truth is that I do not look at the label in detail. I do not look at all the components that the product has” (Woman, 33 years old).
Additionally, as shown in Table 1 , we try to find out if the place where the interviewees lived significantly influenced their eating habits. In this sense, the analysis of 34 conducted interviews revealed that 8 University students (23.5% of them) were still living with their parents (3 women and 5 men), 18 University students (52.9% of them) shared housing with other students (9 women and 9 men), 6 University students (17.6% of them) lived with their romantic partners (4 women and 2 men), and only 2 University students (5.9% of them) lived single (1 woman and 1 man). In this regard, those 8 students who still lived with their families were the ones who ate more healthily, mainly because, in this case, their mothers were the ones who acquired and cooked the food.
The Decisive Influence of Age and Gender
However, what decisively influenced the interviewees' eating behaviors was their age and gender. Firstly, we observed that the concern in buying healthy foods grew as the age of the interviewees increased. Particularly, students aged 27 years or older (that is, 35.3% of the interviewees) showed great interest in maintaining the type of diet that they thought was most beneficial to their health.
“I do not drink milk anymore. Some people have told us that it is not recommendable to drink so much milk at a certain age. My partner has high cholesterol, and we had to change our diet …I think that is also due to the fact that we are getting older… hahaha … We try to do some exercise as well” (Woman, 44 years old).
Those University students who showed a lower degree of involvement in the tasks of buying and cooking food were aged between 20 and 26 years; namely, 64.7% of the selected sample. These students, who are the youngest of this sample, are highly dependent on their parents for performing tasks, especially their mothers. Thus, these often continue providing containers with frozen food they had prepared to their sons even after they have left the family home. Focusing on the gender variable, we observed that the said dependency is lower among women, and only three of nine women students sharing housing with other students (33.3% of them) admitted that they received meals prepared by their mothers, even though they no longer resided under the same roof. However, only one of nine male students in the aforementioned residential situation (11.1% of them) said that he prepares his own food without any help, while most young male interviewees showed that they were strongly dependent not only on their mothers but also on other women (romantic partners or female companions with which they shared housing) in terms of buying and/or cooking food. In other words, 88.9% of these students used to ignore these tasks and leave them in female hands.
“I have been living out of my parents' home for 3 years. My first year was a bit disastrous in terms of my feeding… I lost 10 kg because I only ate some pasta and rice… it was definitely a critical point in my feeding. Fortunately, my nourishment improved when I started living with a woman flatmate, but, when she left the floor, I lost weight again. Now, I'm trying to improve my diet a bit” (Man, 20 years old).
Unfortunately, this situation does not change significantly as the interviewees age. Those male students aged over 27 years who reside with their romantic partners continue to show a strong dependence on women for activities, such as purchasing food and cooking.
“When I eat alone, I do not have control over the food that I eat. When I lived with my parents, they used to manage everything about feeding, and my partner currently helps me. I thought that it is because of this kind of life in which we need to do lots of things and all them so quickly that we do not have time enough to eat” (Man, 33 years old).
Justifications to Explain Eating Habits
One of justifications used by some students to explain why they are not eating healthily is the lack of time in their daily lives. So, 7 of the 34 interviewees (20.6% of selected sample) said that they did not have enough time to eat a healthy diet. Two of these students were women and the remaining five were men. Besides, 14 students said that they had time to prepare all their meals; that is, 41.2% of the selected sample. Ten of these 14 students (namely, 71.4% of them) were women and the remaining four were men, including the two aforementioned men who were vegans; thus, they were strongly motivated to devote enough daily time to prepare their food.
“The great majority of my friends eat really unhealthy; they do not do exercise, and they eat a lot of fried food. I think that it is because they are lazy or maybe because of the stress of working all day, and they directly think, ‘Well, for just one day in which I can allow a whim, I'm going to eat a soup? Not at all” (Man, 25 years old).
Nevertheless, the remaining 13 students (38.2% of the selected sample) openly stated that they had no time problems related to feeding, either because they were living with their parents or because they often received frozen food cooked by their mothers. In particular, with reference to these 13 students (5 women and 8 men) it should be noted that, in addition to the key role played by mothers, men mentioned that their female partners are mainly responsible for preparing and cooking food. Therefore, these female partners could be perpetuating the same role in some way that they see their mothers perform, i.e., the main individual responsible for feeding the family. In fact, these mothers assume and internalize the function that “male domination” ( Bourdieu, 2001 ) has assigned to them so intensely that they often do not allow their daughters to work in the kitchen while they are inside it.
“When I live with my mother, I do not make my own meal, but when I live alone, I do everything by myself. This is not because I do not want to do it, but it is because my mother prefers doing all household tasks without any sort of help. She told me, ‘no, no, get out of the kitchen!’; so… how can I learn?” (Woman, 21 years old).
Furthermore, 26.5% of interviewees (5 men and 4 women) mentioned direct and conscious social pressure as an influential factor on their eating habits.
“Maybe, if you go out with your friends on weekends, you are more exposed to eat some inappropriate food, such as burgers or some fried food… And, in case you prefer another healthier meal, they automatically look at you as weird or something like this…” (Man, 25 years old).
“I do not usually eat snacks. I eat them when I meet with some friends” (Man, 22 years old).
In addition to friends, social pressure may also come from some relatives, romantic partners, or even flatmates. In all these cases, the way social pressure is exercised varies according to the age of those who experience it. Primarily, age determines the settings where such pressure is exerted. In this regard, although students older than 30 years refer to such settings as “small meetings with friends,” younger students talk about getting together in an apartment to play video games or going to bars to “take tapas.”
“I usually buy snacks, but it is because my husband and my little son like them. I do not like snacks; so, I do not eat them. I mostly prefer doing varied meals for them, such as fruits or vegetables… This is what I understand for healthy diet” (Woman, 33 years old).
“I usually eat some snacks just when I meet with some friends to watch a football match or dinner. but I do not consume them on my own. With these products, it happens to me, I think, what happens to us all. this feeling of saying ‘take them away from me because otherwise I cannot stop eating them!’ It is true; they are good. I suppose that is because of the additives or aromas they have.” (Man, 37 years old).
Last but not least, the price of the products was another of the interviewees' arguments to justify their unhealthy eating habits. Thus, most students agreed that the healthiness of a food product is lower when the price is cheaper. Consistently, 19 of the 34 interviewees (55.9% of the selected sample) explicitly said that they had more or less difficulties (depending on their respective living standards) to eat healthy due to the high prices of organic or natural products compared to the prices of industrially processed foods, which they perceived as less healthy. Nine of these 19 students were men aged between 20 and 28 years, while the other 10 students were women aged between 21 and 27 years.
“When I was a degree student, I ate lots of pre-cooked food because I preferred to save my money for other things, such as going out with friends, for example” (Man, 26 years old).
However, the importance of price decreases as the University students become economically independent from their parents and their age and purchasing power increase. This change is particularly observed among those female students who are 27 years old or older.
“I usually buy organic/local food products, such as vegetables or meat, in local markets or corner shops… I do not usually take into account their price, but what drives me to purchase these products is that they inspire more confidence in me than those from great supermarkets because you meet the owner, and you can know everything about the product just by asking him/her” (Woman, 44 years old).
Particularly, the students most interested in eating a healthy diet are also those who are the most concerned about buying food products whose healthiness they trust. But, even in this case, price continues to have much influence on deciding what to buy or what can be bought. Some students suggested the need to implement policies to solve this problem.
“I think that we should encourage more local products. that is, that people consume more of this type of product than foreign ones. Perhaps governments should encourage more consumption of local foods by subsidizing them or establishing certain norms for the market” (Woman, 27 years old).
The authors of this work are fully aware that the discussion on the factors that influence eating habits and affect their greater or lesser healthiness does not end with age, gender and other factors that we have considered in this research. In this regard, numerous studies have demonstrated that the educational status, the income level, the role of agri-food supply chains and the lesser or greater accessibility to these by people, the occupation and even social class are factors that can influence people's feeding habits ( De Irala-Estévez et al., 2000 ; Trichopoulou et al., 2002 ; Darmon and Drewnowski, 2008 ; Cobb-Clark et al., 2012 ; Horská et al., 2020 ). However, these factors are not the only ones that determine individuals' eating habits, since other external or environmental factors alter these habits and are beyond an individual's control. Examples of these factors include the characteristic cultures of the social and/or geographical context in which a person lives or has grown and food advertising ( Troncoso and Amaya, 2009 ; Saucedo et al., 2010 ; Ganasegeran et al., 2012 ; Robinson et al., 2013 ; Becerra et al., 2015 ; WHO, 2018 ; Higgs and Ruddock, 2020 ).
Currently, concerns about people's health since childhood and throughout their entire adulthood are increasing. Demands for natural and healthy foods by consumers are growing ( De Ridder et al., 2017 ; Dernini et al., 2017 ; Oliffe et al., 2017 ; Parham et al., 2017 ; Vallejo-Alviter and Martínez-Moctezuma, 2017 ). In this context, in which daily lives of people take place, the said demands are often manipulated by marketing strategies used by the food industry. Thus, a series of foods that are actually industrial products are presented as natural and/or ecological and, therefore, good for health, which has become an advertising hook for this type of processed foods.
Usually, advertising, rather than reliably reporting the quality and characteristics of the products offered or promoting a healthy diet, reflects marketing strategies that create symbolic necessities in a consumption society. Now, in this society, individuals seek to face new experiences and feelings or simply publicly show their identities by purchasing certain material goods ( Ibáñez, 1997 ). Thus, unsurprisingly, the WHO (2014 , 2018 , 2020) openly criticized current advertising campaigns for promoting food products without being entirely honest with consumers, and subsequently, the WHO noted the urgency of persuading governmental institutions to take action to address this issue.
Regarding the control of food advertising in Spain, the Spanish Ministry of Health (SPH) published the so-called PAOS code in 2005 (Advertising (Publicidad), Activity (Actividad), Obesity (Obesidad), and Health (Salud) [PAOS]) ( SPH, 2005 ; AECOSAN, 2012 ). In collaboration with a group of companies voluntarily committed to the cause, the Ministry intended to co-regulate the food and drink products advertised to children to prevent obesity and promote health among them ( González-Díaz, 2013 ). Nonetheless, despite all the ethical rules established in this code for the development, creation and dissemination of advertising messages to children, there exists still a high degree of non-compliance with the PAOS code, at least regarding television commercials. Thus, as shown in a recent article ( León-Flández et al., 2017 ), up to 88.3% of television advertisements for foods and beverages targeting minors violated the code in some way in 2012, while in 2008, the degree of noncompliance was 49.3%. Notably, non-compliance was greater in the commercials aired on children's channels (92.3%) than in commercials airing on channels targeting the entire population (81.5%). In this context, the aforementioned article proposed more restrictive and legal measures for food advertising to children, with healthy products being the only suitable products that can be advertised to minors.
Nonetheless, the problems caused by unhealthy feeding practices cannot be solved only by the enactment of prohibitive or restrictive new laws or measures that are often not complied with. Furthermore, this issue cannot only be resolved by doctors and nutritionists prescribing highly strict diets that are demoralizing to those who are unable to follow them ( Pérez-Rodrigo and Aranceta, 2001 ; Worsley, 2002 ; Bandura, 2004 ; Kupolati et al., 2015 ; Nguyen et al., 2015 ; OECD, 2017b ; Rush and Yan, 2017 ). Of course, both the regulation of food advertising and the work of nutritionists or doctors are essential factors for expanding and strengthening healthy eating habits among the population ( Worsley, 2002 ; Maixé-Altés, 2009 ; Robinson et al., 2013 ; Perveen, 2017 ; Rush and Yan, 2017 ; Schneider et al., 2017 ). Nevertheless, even though these factors may have an undeniable impact on the improvement in food health, they alone do not ensure that progress toward healthier eating practices is achieved. Even improving people's education cannot guarantee the strengthening of such practices, such as we have shown in this article ( Entrena-Durán et al., 2020 ).
The University students interviewed here have reached a high educational level, and consequently they engage in critical thinking that allows them to clearly discern between healthy and unhealthy food. However, this fact does not guarantee that all these students eat healthily. On the contrary, there is a gap between what the students know and how a significant proportion of them actually behave, and between what they express in their discourses and the concrete practices or eating habits they perceive or say they follow in their daily lives ( Martín Criado, 1998 ).
Our study has helped to reveal some of the causes behind this gap. So, the fact of focusing exclusively on University students has allowed this research to demonstrate that the circumstance of having a high educational level is not enough to ensure that there will be healthy eating habits. In addition to the educational level, a decisive element in order to achieve a healthy diet is to internalize food habits that make it possible. We have seen that these habits are strengthened as the interviewees' age increases. We have also found that most of women interviewed show healthier eating habits.
In the first place, we have observed that, as their age increases, the socio-economic and vital situation of interviewees is stabilizing, which favors that their eating habits become more regular and healthier, and this happens at the same time that the interviewees' awareness of the need to lead a more regulated and healthy lifestyle augments.
Secondly, with respect to gender, our research has shown that food education is more effective among women. This is so because women have traditionally been in charge of acquiring and preparing food at their homes. In other words, women's food education has not been restricted to the mere transmission to them of knowledge about what healthy food is, but from their childhood they were food trained through their active involvement in practical experiences. All this explains both why healthy eating habits are more strongly rooted in women and why these tend to have the best chances of assuming such habits.
Regarding Bourdieu's Concepts and the Assumption of Healthy Eating Habits
To understand eating habits shaping and assumption by individuals and the implementation of these habits, we can be inspired by the habitus and field concepts of Bourdieu (1991) . Therefore, the present study reveals that the reason why people eat healthily does not only depend on their knowledge of healthy food, but healthy eating is strongly influenced (hindered or furthered) by the habitus acquired by individuals. Moreover, in the case of the University students studied here, the strength of their eating habitus fluctuates according to their age and gender. These two variables, together with the specific contexts in which they act, constitute the particular circumstances under which people's eating habits develop day-by-day. In turn, the said circumstances play a key role in the processes of shaping, assuming and implementing eating habits and, according to Bourdieu, they create a sort of field (i.e., a social game space or scenario ) in which the production and reproduction of feeding-related discourses, practices and habits occur. Particularly, in the case of women, their socialization in the procurement and preparation of food has created a very optimal field for their internalization and effective assumption of a healthy food habitus , which according to Bourdieu, could be understood as the assumption of a set of durable dispositions or predispositions to buy, prepare and eat healthy food. We make this assertion based on the fact that, for Bourdieu (1991) , the habitus can be understood as a system of durable and transposable predispositions and dispositions that operate as schemes that generate and organize social practices. Simultaneously, these schemes incline people to act, perceive, value, feel and think in a certain way.
So understood, the habitus concept is very fruitful in explaining women's predisposition to assume the gender role of performing the tasks of buying, cooking and feeding their family group. Thus, women internalize a gender role that is nothing more than a product of history, i.e., a social construction. They assume this role as inherent to their gender identity, as if it were innate to their female nature and accept their supposed natural-psychological aptitudes for the said tasks. By acting in this way, women contribute to the reproduction of “male domination” over them while such domination is simultaneously legitimized as being grounded in biology ( Bourdieu, 2001 ).
According to this logic, the biological nature of men renders them better prepared than women to function outside the home. Thus, a fact whose causes are merely social tends to be legitimized as natural because men often have greater access to and control over the material and symbolic resources that underpin their predominance in the public sphere. Consistently, men—and society at large—think that when they are responsible for household chores, such as feeding the family, they are performing an exceptional task that is not inherent to their masculine nature. Men improve their self-esteem by assuming this role and achieve a social recognition that is based on a macho thought regardless of their intentions. This thought could be formulated as “what a good person that man is who help his wife with domestic chores and taking responsibility for these tasks when she is not at home or is sick.”
In contrast, even upon entering the public sphere, women have fewer opportunities to avoid their role as home caregivers. This role has been strongly internalized by most women as an inherent obligation due to their gender; thus, they tend to be highly self-demanding and blame themselves when they feel that they have failed their main responsibility when their home is not working well.
In particular, Bourdieu's (1991 ; 2001 ) conceptual framework and theories of gender socialization can be very useful tools for explaining the guilt that many women experience when they work outside the home and cannot exclusively dedicate themselves to household tasks. Some authors have noted that as long as home care is understood as a process associated with and undertaken by women, our society will not overcome labor, social and political segregation ( Doucet, 2009 ; Skærbæk, 2011 ). These authors emphasize that home caregiving should be understood as an existential condition of life that affects both men and women.
Unfortunately, the present study has shown that gender inequalities persist even among University students. Thus, both students sharing the same apartment and heterosexual couples living together, share a common situation in which the women continue to perform most of the domestic chores. In consequence, improving individuals' educational levels is insufficient. In addition, working on relations between genders is necessary for achieving a complete and effective redefinition of their habitus ( Bourdieu, 1991 ) in such a way that any predisposition or inclination that tends to legitimize or naturalize gender inequalities disappears. To achieve this goal, we must seek to inculcate egalitarian habits of behavior and relationship between both sexes from childhood. Undoubtedly, this task requires family socialization, training for gender equality at the different educational levels, and the media in general to stop the macho portrayals and stereotypes.
Consistently, men must be educated to be equally involved in domestic responsibilities and particularly to believe that the time devoted to feeding is not lost but instead is beneficial in terms of improving their health and because of the creativity it entails.
Some Limitations of Our Study and Suggestions for Future Research
The qualitative methodology of our research has permitted us to see, through the analysis of their discourses, how the interviewees experience and explain their food problems. The analysis of these discourses has allowed us to collect comprehensive information regarding the perceptions of both healthy food and healthy eating habits in Spain. Such depth of information could not have been obtained through a quantitative survey. However, this research has some limitations.
Interviewing an entire group of students who live together in the same flat could be beneficial, since this could allow us to contrast all information provided by each student. Nevertheless, it was not possible for the interviewees to bring their roommates to the interview, likely because of the lack of strong relational links between the flatmates.
Moreover, a comparative investigation that involved samples from different universities could have been intriguing. Nonetheless, such a study would require financial resources, which we lack. However, while it is true that the interviews were conducted exclusively at the University of Granada, as explained above, we selected a sample of interviewees in which we included a majority of students from outside Granada. Therefore, in some way, our sample is something representative to allow a certain degree of extrapolation of the results obtained here to other University contexts.
Recommendations for Policy Makers
Public policies can contribute by creating conditions that enable people to more easily develop healthy eating habits. For instance, by forcing the food industry to put clearer labeling. Moreover, such policies must ensure a sufficient supply of healthy food at affordable prices and they should promote and/or support food education. This education should focus not only on transmitting knowledge regarding healthy food, but also on training people to develop predispositions toward this type of food and acquire a healthy food habitus ( Bourdieu, 1991 ). Thus, it is very necessary to inculcate healthy eating habits in people through practical experiences. For example, by means of promoting access to rural environments and contact with nature from early childhood (through visits to school farms, field trips, etc.) not only to encourage greater physical exercise, but also to favor both knowledge of traditional and/or ecological products and some practical knowledge about sustainable and healthy food ( Paddock, 2017 ).
Educational actions, such as those abovementioned, favor the incorporation of healthy eating habits, which are best achieved when an adequate field or social game space is created for this purpose. This field has to be built by implementing policies, such as the creation of employment and improvements in wages and quality of work, which could increase people's purchasing power. These policies should be combined with all these other measures aimed at facilitating accessibility to healthy foods.
Furthermore, the consolidation of healthy food habits can be greatly favored by implementing policies that encourage the creation of conditions under which both men and women have more time to live with their families and perform household chores. Overall, these conditions could contribute to facilitating all members of the family to assume the responsibilities inherent in the acquisition and purchasing of food regardless of their gender.
The present study suggests that, in their position, women have some advantages over men in developing healthy food habits. Obviously, a solution is to not perpetuate macho gender stereotypes that assign women the role of home caregivers, but to seek the establishment of a society in which the economic value of domestic labor is recognized and women and men should have the opportunity, and the duty, to experience equally those practical experiences that involve the tasks of the acquisition and preparation of food. The fact of working for the achievement of a socioeconomic situation in which this is possible, not only has a positive impact on the advancement of gender equality, but also it contributes to creating more adequate conditions to overcome the disadvantages men have due to their lack of training to perform the home care services and, in particular, the tasks of buying and preparing food, either for themselves or for their families.
Data Availability Statement
The datasets on which the writing of this article has been based are not made available to readers. The main reason for this is to prevent the people interviewed for this research from being identified. Any additional clarification about the interviews conducted may be requested from the corresponding author of this paper. Requests to access the datasets should be directed to fentrena@ugr.es .
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee in Human Research of the University of Granada. The participants provided their written informed consent to participate in this study.
Author Contributions
FE-D and HB-L: conception, conceptualization, design, original draft, methodology, research, and analysis. FE-D and J-MV-G: methodology, analysis, writing, and final review. All authors have read and agreed to the published version of the manuscript.
No scholarship or financial aid was requested or granted specifically for conducting the research on which this study is based. However, such research was carried out within the framework of the Research Group Social Problems in Andalusia (SEJ-129), which is financed by the Regional Government of Andalusia and the Government of the Spanish State.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank all those University students who kindly participated in this research.
AECOSAN (2012). Código de Corregulación de la Publicidad de Alimentos y Bebidas Dirigida a Menores, Prevención de la Obesidad y Salud . 1–18. Available online at: http://www.aecosan.msssi.gob.es/AECOSAN/docs/documentos/nutricion/Nuevo_Codigo_PAOS_2012_espanol.pdf (accessed November 25, 2020).
Google Scholar
Almerico, G. M. (2014). Food and identity: food studies, cultural, and personal identity. J. Int. Bus. Cult. Stud. 8, 1–7. Available online at: https://www.aabri.com/manuscripts/141797.pdf (accessed January 25, 2021).
Bandura, A. (2004). Health promotion by social cognitive means. Heal. Educ. Behav. 31, 143–164. doi: 10.1177/1090198104263660
PubMed Abstract | CrossRef Full Text | Google Scholar
Barilla Center for Food and Nutrition (2009). La Dimens. Cult. del cibo, 36 . Available online at: https://www.barillacfn.com/m/publications/pp-dimensione-culturale-cibo.pdf (accessed February 2, 2021).
Becerra, F., Pinzón, G., and Vargas, M. (2015). Practicas alimentarias de un grupo de estudiantes universitarios y las dificultades percibidas para realizar una alimentación saludable. Rev. Fac. Med. 63, 457–463. doi: 10.15446/revfacmed.v63n3.48516
CrossRef Full Text | Google Scholar
Berger, P. L., and Luckmann, T. (1979). La Construcción Social de la Realidad . Buenos Aires: Amorrortu.
Bourdieu, P. (1991). El Sentido Práctico . Madrid: Taurus.
Bourdieu, P. (2001). Masculine Domination . Palo Alto, CA: Stanford University Press.
Cobb-Clark, D. A., Kassenboehmer, S. C., and Schurer, S. (2012). Healthy habits: the connection between diet, exercise, and locus of control. SSRN Electron. J. doi: 10.2139/ssrn.2146274. Available online at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2146274# (accessed January 20, 2021).
Cox, R. (2014). Food and eating: an anthropological perspective. Soc. Issues Res. 1–22. Available online at: http://www.sirc.org/publik/foxfood.pdf (accessed on December 22, 2020).
Cubero-Juánez, J., Franco-Reynolds, L., Calderón, M., Caro, B., Rodrigo, M., and Ruiz, C. (2017). El desayuno escolar; una intervención educativa en alimentación y nutrición saludable. Didáctica las Ciencias Exp. Soc. 32, 171–182. doi: 10.7203/dces.32.4546
Darmon, N., and Drewnowski, A. (2008). Does social class predict diet quality? Am. J. Clin. Nutr. 87, 1107–1117. doi: 10.1093/ajcn/87.5.1107
De Irala-Estévez, J., Groth, M., Johansson, L., Oltersdorf, U., Prättälä, R., and Martínez-González, M. A. (2000). A systematic review of socio-economic differences in food habits in Europe: consumption of fruit and vegetables. Eur. J. Clin. Nutr. 54, 706–714. doi: 10.1038/sj.ejcn.1601080
De Ridder, D., Kroese, F., Evers, C., Adriaanse, M., and Gillebaart, M. (2017). Healthy diet: health impact, prevalence, correlates, and interventions. Psychol. Heal. 32, 907–941. doi: 10.1080/08870446.2017.1316849
Dernini, S., Berry, E. M., Serra-Majem, L., La Vecchia, C., Capone, R., Medina, F. X., et al. (2017). Med Diet 4.0: the mediterranean diet with four sustainable benefits. Public Health Nutr. 20, 1322–1330. doi: 10.1017/S1368980016003177
Díaz-Méndez, C., and Gómez-Benito, C., (eds.). (2008). Alimentación, Consumo y Salud (Colección Estudios Sociales, num. 24) . Barcelona: Fundación “la Caixa”.
Doucet, A. (2009). Gender equality and gender differences: parenting, habitus and embodiment. Can. Rev. Sociol. 48, 99–117. doi: 10.1111/j.1755-618x.2009.01206.x
Entrena-Durán, F., Baldan-Lozano, H., and Valdera-Gil, J. M. (2020). “La salubridad de los hábitos alimenticios de los estudiantes universitarios: un estudio de caso,” in Análisis y Enfoques Novedosos Para Contenidos Culturales , ed M. Rodorigo (Valencia: Tirant lo Blanch).
FAO (2008). Doc. apoyo para la Asign. Ciencia, Salud y Medio Educ. en Nutr. Segur. y huertos Esc. , 84. Food and Agriculture Organization of the United Nations. Available online at: http://www.fao.org/3/a-am278s.pdf (accessed February 1, 2021).
Fischler, C. (1980). Food habits, social change and the nature/culture dilemma. Soc. Sci. Inf. 19, 937–953. doi: 10.1177/053901848001900603
Ganasegeran, K., Al-Dubai, S. A. R., Qureshi, A. M., Al-Abed, A. A. A., Am, R., and Aljunid, S. M. (2012). Social and psychological factors affecting eating habits among University students in a Malaysian medical school: a cross-sectional study. Nutr. J. 11:48. doi: 10.1186/1475-2891-11-48
García-Cardona, M., Pardío-López, J., Arroyo-Acevedo, P., Fernández-García, V., and García, M. (2008). Dinàmica familiar y su relaciòn con hàbitos alimentarios. Estud. sobre las Cult. Contemp. XIV , 27, 9–46. Available online at: https://www.redalyc.org/articulo.oa?id=31602702 (accessed January 20, 2021).
González-Díaz, C. (2013). La publicidad dirigida a niños en el sector de la alimentación: un estudio atendiendo al tipo de producto/Food advertising targeted to children: a study on type product. Hist. Comun. Soc. 18, 175–187. doi: 10.5209/rev_HICS.2013.v18.44235
Gracia-Arnáiz, M. (2010). Alimentación y cultura en España: una aproximación desde la antropología social. Phys. Rev. Saúde Colet. 20, 357–386. doi: 10.1590/S0103-73312010000200003
Grosso, G., Bella, F., Godos, J., Sciacca, S., Del Rio, D., Ray, S., et al. (2017). Possible role of diet in cancer: systematic review and multiple meta-analyses of dietary patterns, lifestyle factors, and cancer risk. Nutr. Rev. 75, 405–419. doi: 10.1093/nutrit/nux012
Guenther, P. M., Casavale, K. O., Reedy, J., Kirkpatrick, S. I., Hiza, H. A. B., Kuczynski, K. J., et al. (2013). Update of the Healthy Eating Index: HEI-2010. J. Acad. Nutr. Diet. 113, 569–580. doi: 10.1016/j.jand.2012.12.016
Higgs, S., and Ruddock, H. (2020). “Social influences on eating,” in Handbook of Eating and Drinking (Cham: Springer International Publishing), 277–291. doi: 10.1007/978-3-030-14504-0_27
Horská, E., Petrilák, M., Šedík, P., and Nagyová, L. (2020). Factors influencing the sale of local products through short supply chains: a case of family dairy farms in Slovakia. Sustainability 12:8499. doi: 10.3390/su12208499
Ibáñez, J. (1997). Por Una Sociología de la Vida Cotidiana . Madrid: Siglo XXI.
INE (2019). Indicadores Calid. Vida Salud autopercibida . INE (Instituto Nacional de Estadística). Available online at: https://www.ine.es/ss/Satellite?L=es_ESandc=INESeccion_Candcid=1259944485720andp=1254735110672andpagename=ProductosYServicios%2FPYSLayoutandparam1=PYSDetalleFichaIndicadorandparam3=1259937499084andrendermode=pr+eviewnoinsite (accessed February 2, 2021).
Isaza, L. (2012). El contexto familiar: un factor determinante en el desarrollo social de los niños y las niñas. Rev. Electrón. Psicol. Soc. 23, 1–6. Available online at: https://www.funlam.edu.co/revistas/index.php/poiesis/article/view/332/305 (accessed February 14, 2021).
Kupolati, M. D., Gericke, G. J., and MacIntyre, U. E. (2015). Teachers' perceptions of school nutrition education's influence on eating behaviours of learners in the Bronkhorstspruit District. South African J. Educ. 35:1049. doi: 10.15700/saje.v35n2a1049
León-Flández, K., Rico-Gómez, A., Moya-Geromin, M., Romero-Fernández, M., Bosqued-Estefania, M. J., Damián, J., et al. (2017). Evaluation of compliance with the Spanish Code of self-regulation of food and drinks advertising directed at children under the age of 12 years in Spain, 2012. Public Health 150, 121–129. doi: 10.1016/j.puhe.2017.05.013
Levine, C. S., Miyamoto, Y., Markus, H. R., Rigotti, A., Boylan, J. M., Park, J., et al. (2016). Culture and healthy eating: the role of independence and interdependence in the United States and Japan. Personal. Soc. Psychol. Bull. 42, 1335–1348. doi: 10.1177/0146167216658645
Maixé-Altés, J. (2009). La modernización de la distribución alimentaria en España, 1947-1995. Rev. Hist. Ind. 18, 125–160. Available online at: https://revistes.ub.edu/index.php/HistoriaIndustrial/article/view/20486 (accessed January 20, 2021).
Martín Criado, E. (1998). Los decires y los haceres. Pap. Rev. Sociol. 56, 57–71. doi: 10.5565/rev/papers.1944
Martín Criado, E. (2004). El valor de la buena madre: oficio de ama de casa, alimentación y salud entre las mujeres de clases populares. Rev. Espan. Sociol . 93–118. Available online at: https://recyt.fecyt.es/index.php/res/article/view/64944/39354 (accessed February 18, 2021).
Martinez-Lacoba, R., Pardo-Garcia, I., Amo-Saus, E., and Escribano-Sotos, F. (2018). Mediterranean diet and health outcomes: a systematic meta-review. Eur. J. Public Health 28, 955–961. doi: 10.1093/eurpub/cky113
Nguyen, B. H., Nguyen, C. P., McPhee, S. J., Stewart, S. L., Bui-Tong, N., and Nguyen, T. T. (2015). Cognitive interviews of vietnamese americans on healthy eating and physical activity health educational materials. Ecol. Food Nutr. 54, 455–469. doi: 10.1080/03670244.2015.1015119
OCU (2017). OCU Inf. Los Españoles Quieren Aliment. Mejor. Pero no lo Consiguen . OCU (Organization of Consumers and Users). Available at: https://www.ocu.org/organizacion/prensa/notas-de-prensa/2017/habitos-alimentarios-250817 (accessed December 28, 2020).
OCU (2019). “ 10% menos de azúcar, grasas saturadas y sal en alimentos procesados? #NoCuela. OCU (Organization of Consumers and Users). Available online at: https://www.ocu.org/alimentacion/alimentos/noticias/alimentos-procesados-reducir-grasa-azucar-plan (accessed November 29, 2020).
OECD (2017a). Obes. Updat. 2017 . OECD (Organization for Economic Co-operation and Development). Available at: https://www.oecd.org/els/health-systems/Obesity-Update-2017.pdf (accessed November 27, 2020).
OECD (2017b). Heal. a Glance 2017 OECD Indic . OECD (Organization for Economic Co-operation and Development). Available online at: https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2017_health_glance-2017-en (accessed October 25, 2020).
Oliffe, J. L., Bottorff, J. L., Sharp, P., Caperchione, C. M., Johnson, S. T., Healy, T., et al. (2017). Healthy eating and active living: rural-based working men's perspectives. Am. J. Mens. Health 11, 1664–1672. doi: 10.1177/1557988315619372
Paddock, J. (2017). Household consumption and environmental change: rethinking the policy problem through narratives of food practice. J. Consum. Cult. 17, 122–139. doi: 10.1177/1469540515586869
Parham, S. C., Kavanagh, D. J., Gericke, C. A., King, N., May, J., and Andrade, J. (2017). Assessment of motivational cognitions in diabetes self-care: the motivation thought frequency scales for glucose testing, physical activity and healthy eating. Int. J. Behav. Med. 24, 447–456. doi: 10.1007/s12529-016-9607-2
Pérez-Rodrigo, C., and Aranceta, J. (2001). School-based nutrition education: lessons learned and new perspectives. Public Health Nutr. 4, 131–139. doi: 10.1079/PHN2000108
Perveen, R. (2017). Assessing the influence of nutrition education among adolescent girls (13-16 years). Adv. Obesity, Weight Manag. Control 6, 144–147. doi: 10.15406/aowmc.2017.06.00167
CrossRef Full Text
Robinson, E., Blissett, J., and Higgs, S. (2013). Social influences on eating: implications for nutritional interventions. Nutr. Res. Rev. 26, 166–176. doi: 10.1017/S0954422413000127
Ruiz-Moreno, E., Del-Pozo-de-la-Calle, S., Valero-Gaspar, T., Ávila-Torres, J. M., and Varela-Moreiras, G. (2013). Estudio de Hábitos Alimentarios y Estilos de Vida de los Universitarios Españoles. Patrón de consumo de bebidas fermentadas. Fund. Española la Nutr . 1–32. Available online at: http://www.fen.org.es/storage/app/media/imgPublicaciones/30092014131915.pdf (accessed November 24, 2020).
Rush, E. C., and Yan, M. R. (2017). Evolution not revolution: nutrition and obesity. Nutrients 9:519. doi: 10.3390/nu9050519
Saucedo, T., Peña, A., Fernández, L., García, A., and Jiménez, R. (2010). Identificación de factores de riesgo asociados a trastornos de la conducta alimentaria y su relación con el Índice de Masa Corporal en universitarios del Instituto de Ciencias de la Salud. Rev. Med. UV 10, 16–23. Available online at: https://www.medigraphic.com/pdfs/veracruzana/muv-2010/muv102c.pdf (accessed December 16, 2020).
Schneider, S., Diehl, K., Görig, T., Schilling, L., De Bock, F., Hoffmann, K., et al. (2017). Contextual influences on physical activity and eating habits-options for action on the community level. BMC Public Health 17:760. doi: 10.1186/s12889-017-4790-x
Silva, T. H., Vaz De Melo, P. O. S., Almeida, J., Musolesi, M., and Loureiro, A. (2014). “You are what you eat (and Drink): identifying cultural boundaries by analyzing food and drink habits in foursquare,” in Proceedings of the 8th International Conference on Weblogs and Social Media, ICWSM 2014 (Palo Alto, CA: The AAAI Press), 466–475.
Skærbæk, E. (2011). Navigating in the landscape of care: A critical reflection on theory and practise of care and ethics. in Health Care Analysis (Kluwer Academic Publishers) , 41–50. doi: 10.1007/s10728-010-0157-5
SPH (2005). SPH (Spanish Ministry of Health). Mañana entra en vigor el Código PAOS autorregulación la Public. Destin. a menores para Combat. la Obes. Infant . Available online at: http://www.fundaciondiabetes.org/upload/noticias/4694/23.pdf (accessed January 18, 2021).
The Nielsen Company (2015). We Are What We Eat, 27 . Available online at: https://www.nielsen.com/wp-content/uploads/sites/3/2019/04/Nielsen20Global20Health20and20Wellness20Report20-20January202015-1.pdf (accessed January 26, 2021).
Trichopoulou, A., Naska, A., and Costacou, T. (2002). Disparities in food habits across Europe. Proc. Nutr. Soc. 61, 553–558. doi: 10.1079/PNS2002188
Troncoso, P. C., and Amaya, P. J. P. (2009). Factores sociales en las conductas alimentarias de estudiantes universitarios. Rev. Chil. Nutr. 36, 1090–1097. doi: 10.4067/S0717-75182009000400005
Vallejo-Alviter, N. G., and Martínez-Moctezuma, E. (2017). Impacto de la promoción de estilos de vida saludable para mejorar la calidad de vida. Drugs Addict. Behav. 2, 225–235. doi: 10.21501/24631779.2442
Verplanken, B., and Faes, S. (1999). Good intentions, bad habits, and effects of forming implementation intentions on healthy eating. Eur. J. Soc. Psychol. 29, 591–604. doi: 10.1002/(SICI)1099-0992(199908/09)29:5/6<591::AID-EJSP948>3.0.CO;2-H
WHO (2014). “European food and nutrition action plan 2015 – 2020,” in Regional Committee For Europe 64th Session (Copenhagen).
WHO (2018). Better Food and Nutrition in Europe: A Progress Report Monitoring Policy Implementation in the WHO European Region . World Heal. Organ. Reg. Off. Eur., 51.
WHO (2020). World Health Statistics 2020: Monitoring Health for the SDGs, Sustainable Development Goals .
Willett, W. C., Sacks, F., Trichopoulou, A., Drescher, G., Ferro-Luzzi, A., Helsing, E., et al. (1995). Mediterranean diet pyramid: a cultural model for healthy eating. Am. J. Clin. Nutr. 61, 14025–14065. doi: 10.1093/ajcn/61.6.1402S
Worsley, A. (2002). Nutrition knowledge and food consumption: can nutrition knowledge change food behaviour? Asia Pac. J. Clin. Nutr. 11(Suppl 3), S579–S585. doi: 10.1046/j.1440-6047.11.supp3.7.x
Annex: Questionnaire Used to Do the Interviews
We asked the interviewees open questions. Before starting the interviews, we read them the following paragraph:
“Dear student,
We invite you to participate in this project on the eating habits of the University's student population, whose basic objective is to analyze these habits and the greater or lesser healthiness of them from the self-perception that the own students have. Your participation is totally voluntary. We need you to answer a semi-structured interview, which you are free to interrupt when you deem it convenient or to refuse to answer any of the questions. To enable the analysis of the results, the interview must be recorded. However, this audio will not be used to disclose your personal data at any time. In fact, you will not even be asked your name during the recording and you will only be asked to indicate your age, the type of studies you do, if you live with your parents or with other students, as well as other information. The objective of this is that we who do this research can classify and then study the information you provide us, which will be considered in an aggregate manner, without linking it to your name or any other data from which you can be identified. The recording will be used exclusively to extract the information provided with the aforementioned study purpose. Your participation in the interview, voluntary, and unpaid, assumes that you authorize the use of the information you provide us. However, at any time you can decide to withdraw from the survey and demand that the information you have up to that moment be destroyed. Your participation in the current investigation, or your refusal to do so, will not affect in any way the qualification of any of the matters you are currently studying or your possibilities of academic promotion.”
Next, we made the interviews in which we asked the following open questions:
Summary of the interview guide
Opening questions: How old are you? What are you studying at University? Where do you live? Who do you live with?
Topic 1: Daily routine related to eating habits.
Do you make your own purchases? If you do not , why? Who makes the purchases in your home? If you do , how much time do you spend making purchases on average? Do you cook in your house? If you do not , who cooks in your house? Why? If you do , how much time do you spend cooking on average daily? Do you pay attention to the labels on eating products? In the case that you do not live with your parents, do you need any help preparing your own meals? If yes, who usually helps you and how? The interviewees have to explain their answers .
Topic 2: Personal knowledge of and putting into practice healthy eating habits.
I am going to mention some eating products, and you [interviewee] have to say which product is healthy and which is not. Any answer provided by an interviewee must be explained . What would you consider a healthy diet? Do you consider your eating habits healthy? Regardless of his/her answer, he/she must explain .
Topic 3: Problems found by interviewees and possible solutions.
In your opinion, what social, cultural, economic or political problems can hinder the strengthening of healthy eating habits within Spanish society? Please, describe and explain these problems in greater depth. What types of solutions do you think can help solve these problems? Please, explain in greater depth.
Keywords: food healthiness, students, feeding, self-perception of food, effects of age and gender, discourse analysis
Citation: Entrena-Durán F, Baldan-Lozano H and Valdera-Gil J-M (2021) Students' Knowledge of Healthy Food and Their Actual Eating Habits: A Case Study on the University of Granada (Spain). Front. Sustain. Food Syst. 5:687574. doi: 10.3389/fsufs.2021.687574
Received: 29 March 2021; Accepted: 25 May 2021; Published: 18 June 2021.
Reviewed by:
Copyright © 2021 Entrena-Durán, Baldan-Lozano and Valdera-Gil. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Francisco Entrena-Durán, fentrena@ugr.es
This article is part of the Research Topic
Consumer Behavior and Sustainability in the Food Chain
- Eating Behavior
- Health Psychology
- Food Habits
Modern Food Habits and Its Impact on Human Health
- August 2023
- International Journal of Innovative Research in Engineering & Management 10(4):182-185
- 10(4):182-185
- This person is not on ResearchGate, or hasn't claimed this research yet.
Abstract and Figures

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Sam Kafai Yahyavi

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment case
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
Healthy diet
- A healthy diet helps to protect against malnutrition in all its forms, as well as noncommunicable diseases (NCDs), including diabetes, heart disease, stroke and cancer.
- Unhealthy diet and lack of physical activity are leading global risks to health.
- Healthy dietary practices start early in life – breastfeeding fosters healthy growth and improves cognitive development, and may have longer term health benefits such as reducing the risk of becoming overweight or obese and developing NCDs later in life.
- Energy intake (calories) should be in balance with energy expenditure. To avoid unhealthy weight gain, total fat should not exceed 30% of total energy intake (1, 2, 3). Intake of saturated fats should be less than 10% of total energy intake, and intake of trans-fats less than 1% of total energy intake, with a shift in fat consumption away from saturated fats and trans-fats to unsaturated fats (3), and towards the goal of eliminating industrially-produced trans-fats (4, 5, 6).
- Limiting intake of free sugars to less than 10% of total energy intake (2, 7) is part of a healthy diet. A further reduction to less than 5% of total energy intake is suggested for additional health benefits (7).
- Keeping salt intake to less than 5 g per day (equivalent to sodium intake of less than 2 g per day) helps to prevent hypertension, and reduces the risk of heart disease and stroke in the adult population (8).
- WHO Member States have agreed to reduce the global population’s intake of salt by 30% by 2025; they have also agreed to halt the rise in diabetes and obesity in adults and adolescents as well as in childhood overweight by 2025 (9, 10).
Consuming a healthy diet throughout the life-course helps to prevent malnutrition in all its forms as well as a range of noncommunicable diseases (NCDs) and conditions. However, increased production of processed foods, rapid urbanization and changing lifestyles have led to a shift in dietary patterns. People are now consuming more foods high in energy, fats, free sugars and salt/sodium, and many people do not eat enough fruit, vegetables and other dietary fibre such as whole grains.
The exact make-up of a diversified, balanced and healthy diet will vary depending on individual characteristics (e.g. age, gender, lifestyle and degree of physical activity), cultural context, locally available foods and dietary customs. However, the basic principles of what constitutes a healthy diet remain the same.
A healthy diet includes the following:
- Fruit, vegetables, legumes (e.g. lentils and beans), nuts and whole grains (e.g. unprocessed maize, millet, oats, wheat and brown rice).
- At least 400 g (i.e. five portions) of fruit and vegetables per day (2) , excluding potatoes, sweet potatoes, cassava and other starchy roots.
- Less than 10% of total energy intake from free sugars (2, 7) , which is equivalent to 50 g (or about 12 level teaspoons) for a person of healthy body weight consuming about 2000 calories per day, but ideally is less than 5% of total energy intake for additional health benefits (7) . Free sugars are all sugars added to foods or drinks by the manufacturer, cook or consumer, as well as sugars naturally present in honey, syrups, fruit juices and fruit juice concentrates.
- Less than 30% of total energy intake from fats (1, 2, 3) . Unsaturated fats (found in fish, avocado and nuts, and in sunflower, soybean, canola and olive oils) are preferable to saturated fats (found in fatty meat, butter, palm and coconut oil, cream, cheese, ghee and lard) and trans- fats of all kinds, including both industrially-produced trans- fats (found in baked and fried foods, and pre-packaged snacks and foods, such as frozen pizza, pies, cookies, biscuits, wafers, and cooking oils and spreads) and ruminant trans- fats (found in meat and dairy foods from ruminant animals, such as cows, sheep, goats and camels). It is suggested that the intake of saturated fats be reduced to less than 10% of total energy intake and trans- fats to less than 1% of total energy intake (5) . In particular, industrially-produced trans -fats are not part of a healthy diet and should be avoided (4, 6) .
- Less than 5 g of salt (equivalent to about one teaspoon) per day (8). Salt should be iodized.
For infants and young children
In the first 2 years of a child’s life, optimal nutrition fosters healthy growth and improves cognitive development. It also reduces the risk of becoming overweight or obese and developing NCDs later in life.
Advice on a healthy diet for infants and children is similar to that for adults, but the following elements are also important:
- Infants should be breastfed exclusively during the first 6 months of life.
- Infants should be breastfed continuously until 2 years of age and beyond.
- From 6 months of age, breast milk should be complemented with a variety of adequate, safe and nutrient-dense foods. Salt and sugars should not be added to complementary foods.
Practical advice on maintaining a healthy diet
Fruit and vegetables.
Eating at least 400 g, or five portions, of fruit and vegetables per day reduces the risk of NCDs (2) and helps to ensure an adequate daily intake of dietary fibre.
Fruit and vegetable intake can be improved by:
- always including vegetables in meals;
- eating fresh fruit and raw vegetables as snacks;
- eating fresh fruit and vegetables that are in season; and
- eating a variety of fruit and vegetables.
Reducing the amount of total fat intake to less than 30% of total energy intake helps to prevent unhealthy weight gain in the adult population (1, 2, 3) . Also, the risk of developing NCDs is lowered by:
- reducing saturated fats to less than 10% of total energy intake;
- reducing trans -fats to less than 1% of total energy intake; and
- replacing both saturated fats and trans- fats with unsaturated fats (2, 3) – in particular, with polyunsaturated fats.
Fat intake, especially saturated fat and industrially-produced trans- fat intake, can be reduced by:
- steaming or boiling instead of frying when cooking;
- replacing butter, lard and ghee with oils rich in polyunsaturated fats, such as soybean, canola (rapeseed), corn, safflower and sunflower oils;
- eating reduced-fat dairy foods and lean meats, or trimming visible fat from meat; and
- limiting the consumption of baked and fried foods, and pre-packaged snacks and foods (e.g. doughnuts, cakes, pies, cookies, biscuits and wafers) that contain industrially-produced trans- fats.
Salt, sodium and potassium
Most people consume too much sodium through salt (corresponding to consuming an average of 9–12 g of salt per day) and not enough potassium (less than 3.5 g). High sodium intake and insufficient potassium intake contribute to high blood pressure, which in turn increases the risk of heart disease and stroke (8, 11) .
Reducing salt intake to the recommended level of less than 5 g per day could prevent 1.7 million deaths each year (12) .
People are often unaware of the amount of salt they consume. In many countries, most salt comes from processed foods (e.g. ready meals; processed meats such as bacon, ham and salami; cheese; and salty snacks) or from foods consumed frequently in large amounts (e.g. bread). Salt is also added to foods during cooking (e.g. bouillon, stock cubes, soy sauce and fish sauce) or at the point of consumption (e.g. table salt).
Salt intake can be reduced by:
- limiting the amount of salt and high-sodium condiments (e.g. soy sauce, fish sauce and bouillon) when cooking and preparing foods;
- not having salt or high-sodium sauces on the table;
- limiting the consumption of salty snacks; and
- choosing products with lower sodium content.
Some food manufacturers are reformulating recipes to reduce the sodium content of their products, and people should be encouraged to check nutrition labels to see how much sodium is in a product before purchasing or consuming it.
Potassium can mitigate the negative effects of elevated sodium consumption on blood pressure. Intake of potassium can be increased by consuming fresh fruit and vegetables.
In both adults and children, the intake of free sugars should be reduced to less than 10% of total energy intake (2, 7) . A reduction to less than 5% of total energy intake would provide additional health benefits (7) .
Consuming free sugars increases the risk of dental caries (tooth decay). Excess calories from foods and drinks high in free sugars also contribute to unhealthy weight gain, which can lead to overweight and obesity. Recent evidence also shows that free sugars influence blood pressure and serum lipids, and suggests that a reduction in free sugars intake reduces risk factors for cardiovascular diseases (13) .
Sugars intake can be reduced by:
- limiting the consumption of foods and drinks containing high amounts of sugars, such as sugary snacks, candies and sugar-sweetened beverages (i.e. all types of beverages containing free sugars – these include carbonated or non‐carbonated soft drinks, fruit or vegetable juices and drinks, liquid and powder concentrates, flavoured water, energy and sports drinks, ready‐to‐drink tea, ready‐to‐drink coffee and flavoured milk drinks); and
- eating fresh fruit and raw vegetables as snacks instead of sugary snacks.
How to promote healthy diets
Diet evolves over time, being influenced by many social and economic factors that interact in a complex manner to shape individual dietary patterns. These factors include income, food prices (which will affect the availability and affordability of healthy foods), individual preferences and beliefs, cultural traditions, and geographical and environmental aspects (including climate change). Therefore, promoting a healthy food environment – including food systems that promote a diversified, balanced and healthy diet – requires the involvement of multiple sectors and stakeholders, including government, and the public and private sectors.
Governments have a central role in creating a healthy food environment that enables people to adopt and maintain healthy dietary practices. Effective actions by policy-makers to create a healthy food environment include the following:
- Creating coherence in national policies and investment plans – including trade, food and agricultural policies – to promote a healthy diet and protect public health through:
- increasing incentives for producers and retailers to grow, use and sell fresh fruit and vegetables;
- reducing incentives for the food industry to continue or increase production of processed foods containing high levels of saturated fats, trans -fats, free sugars and salt/sodium;
- encouraging reformulation of food products to reduce the contents of saturated fats, trans- fats, free sugars and salt/sodium, with the goal of eliminating industrially-produced trans- fats;
- implementing the WHO recommendations on the marketing of foods and non-alcoholic beverages to children;
- establishing standards to foster healthy dietary practices through ensuring the availability of healthy, nutritious, safe and affordable foods in pre-schools, schools, other public institutions and the workplace;
- exploring regulatory and voluntary instruments (e.g. marketing regulations and nutrition labelling policies), and economic incentives or disincentives (e.g. taxation and subsidies) to promote a healthy diet; and
- encouraging transnational, national and local food services and catering outlets to improve the nutritional quality of their foods – ensuring the availability and affordability of healthy choices – and review portion sizes and pricing.
- Encouraging consumer demand for healthy foods and meals through:
- promoting consumer awareness of a healthy diet;
- developing school policies and programmes that encourage children to adopt and maintain a healthy diet;
- educating children, adolescents and adults about nutrition and healthy dietary practices;
- encouraging culinary skills, including in children through schools;
- supporting point-of-sale information, including through nutrition labelling that ensures accurate, standardized and comprehensible information on nutrient contents in foods (in line with the Codex Alimentarius Commission guidelines), with the addition of front-of-pack labelling to facilitate consumer understanding; and
- providing nutrition and dietary counselling at primary health-care facilities.
- Promoting appropriate infant and young child feeding practices through:
- implementing the International Code of Marketing of Breast-milk Substitutes and subsequent relevant World Health Assembly resolutions;
- implementing policies and practices to promote protection of working mothers; and
- promoting, protecting and supporting breastfeeding in health services and the community, including through the Baby-friendly Hospital Initiative.
WHO response
The “WHO Global Strategy on Diet, Physical Activity and Health” (14) was adopted in 2004 by the Health Assembly. The strategy called on governments, WHO, international partners, the private sector and civil society to take action at global, regional and local levels to support healthy diets and physical activity.
In 2010, the Health Assembly endorsed a set of recommendations on the marketing of foods and non-alcoholic beverages to children (15) . These recommendations guide countries in designing new policies and improving existing ones to reduce the impact on children of the marketing of foods and non-alcoholic beverages to children. WHO has also developed region-specific tools (such as regional nutrient profile models) that countries can use to implement the marketing recommendations.
In 2012, the Health Assembly adopted a “Comprehensive Implementation Plan on Maternal, Infant and Young Child Nutrition” and six global nutrition targets to be achieved by 2025, including the reduction of stunting, wasting and overweight in children, the improvement of breastfeeding, and the reduction of anaemia and low birthweight (9) .
In 2013, the Health Assembly agreed to nine global voluntary targets for the prevention and control of NCDs. These targets include a halt to the rise in diabetes and obesity, and a 30% relative reduction in the intake of salt by 2025. The “Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020” (10) provides guidance and policy options for Member States, WHO and other United Nations agencies to achieve the targets.
With many countries now seeing a rapid rise in obesity among infants and children, in May 2014 WHO set up the Commission on Ending Childhood Obesity. In 2016, the Commission proposed a set of recommendations to successfully tackle childhood and adolescent obesity in different contexts around the world (16) .
In November 2014, WHO organized, jointly with the Food and Agriculture Organization of the United Nations (FAO), the Second International Conference on Nutrition (ICN2). ICN2 adopted the Rome Declaration on Nutrition (17), and the Framework for Action (18) which recommends a set of policy options and strategies to promote diversified, safe and healthy diets at all stages of life. WHO is helping countries to implement the commitments made at ICN2.
In May 2018, the Health Assembly approved the 13th General Programme of Work (GPW13), which will guide the work of WHO in 2019–2023 (19) . Reduction of salt/sodium intake and elimination of industrially-produced trans- fats from the food supply are identified in GPW13 as part of WHO’s priority actions to achieve the aims of ensuring healthy lives and promote well-being for all at all ages. To support Member States in taking necessary actions to eliminate industrially-produced trans- fats, WHO has developed a roadmap for countries (the REPLACE action package) to help accelerate actions (6) .
(1) Hooper L, Abdelhamid A, Bunn D, Brown T, Summerbell CD, Skeaff CM. Effects of total fat intake on body weight. Cochrane Database Syst Rev. 2015; (8):CD011834.
(2) Diet, nutrition and the prevention of chronic diseases: report of a Joint WHO/FAO Expert Consultation. WHO Technical Report Series, No. 916. Geneva: World Health Organization; 2003.
(3) Fats and fatty acids in human nutrition: report of an expert consultation. FAO Food and Nutrition Paper 91. Rome: Food and Agriculture Organization of the United Nations; 2010.
(4) Nishida C, Uauy R. WHO scientific update on health consequences of trans fatty acids: introduction. Eur J Clin Nutr. 2009; 63 Suppl 2:S1–4.
(5) Guidelines: Saturated fatty acid and trans -fatty acid intake for adults and children. Geneva: World Health Organization; 2018 (Draft issued for public consultation in May 2018).
(6) REPLACE: An action package to eliminate industrially-produced trans -fatty acids. WHO/NMH/NHD/18.4. Geneva: World Health Organization; 2018.
(7) Guideline: Sugars intake for adults and children. Geneva: World Health Organization; 2015.
(8) Guideline: Sodium intake for adults and children. Geneva: World Health Organization; 2012.
(9) Comprehensive implementation plan on maternal, infant and young child nutrition. Geneva: World Health Organization; 2014.
(10) Global action plan for the prevention and control of NCDs 2013–2020. Geneva: World Health Organization; 2013.
(11) Guideline: Potassium intake for adults and children. Geneva: World Health Organization; 2012.
(12) Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014; 371(7):624–34.
(13) Te Morenga LA, Howatson A, Jones RM, Mann J. Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids. AJCN. 2014; 100(1): 65–79.
(14) Global strategy on diet, physical activity and health. Geneva: World Health Organization; 2004.
(15) Set of recommendations on the marketing of foods and non-alcoholic beverages to children. Geneva: World Health Organization; 2010.
(16) Report of the Commission on Ending Childhood Obesity. Geneva: World Health Organization; 2016.
(17) Rome Declaration on Nutrition. Second International Conference on Nutrition. Rome: Food and Agriculture Organization of the United Nations/World Health Organization; 2014.
(18) Framework for Action. Second International Conference on Nutrition. Rome: Food and Agriculture Organization of the United Nations/World Health Organization; 2014.
(19) Thirteenth general programme of work, 2019–2023. Geneva: World Health Organization; 2018.
- Preventing noncommunicable diseases
- Global nutrition targets 2025: policy brief series
- Global database on the Implementation of Food and Nutrition Action (GIFNA)
- Five keys to safer food
- 5 keys to a healthy diet
- International food standards (Codex Alimentarius)
- Comprehensive implementation plan on maternal, infant and young child nutrition
- WHO Recommendations on the marketing of foods and non-alcoholic beverages to children
- Global Action Plan for the Prevention and Control of NCDs
- Guideline: sodium intake for adults and children
- Guideline: potassium intake for adults and children
- Preparation and use of food-based dietary guidelines
Appointments at Mayo Clinic
- Nutrition and healthy eating
- Nutrition basics
- Healthy diets
- Healthy cooking
- Healthy menus and shopping strategies
- Nutritional supplements
Do you feel like you can't keep up with the latest nutrition news because it's always changing? It's true that knowledge about nutrition and diet evolves over time. But there are some nutrition basics that can help you sort through the latest research and advice.
Nutrition basics come down to eating wholesome foods that support your health.
Want to go beyond the basics? Talk to a healthcare professional, such as a dietitian. You can ask for diet advice that takes into account your health, lifestyle and food preferences.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- 2020-2025 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://www.dietaryguidelines.gov. Accessed June 13, 2023.
- Zeratsky KA (expert opinion). Mayo Clinic. June 21, 2023.
- Hensrud DD, ed. Add 5 habits. In: The Mayo Clinic Diet. 3rd ed. Mayo Clinic Press; 2023.
- Dietary supplements: What you need to know. Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/WYNTK-Consumer/ Accessed June 13, 2023.
- Vitamins, minerals and supplements: Do you need to take them? Academy of Nutrition and Dietetics. https://www.eatright.org/health/essential-nutrients/supplements/vitamins-minerals-and-supplements-do-you-need-to-take-them. Accessed June 22, 2023.
Products and Services
- Available Health Products from Mayo Clinic Store
- A Book: Cook Smart, Eat Well
- Nutritional Supplements at Mayo Clinic Store
- A Book: The Mayo Clinic Diet Bundle
- The Mayo Clinic Diet Online
- A Book: Mayo Clinic on High Blood Pressure
- A Book: Live Younger Longer
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Guide to Home Remedies
- A Book: Mayo Clinic on Digestive Health
- Health foods
- Antioxidants
- Alcohol use
- Alkaline water
- Artificial sweeteners and other sugar substitutes
- Autism spectrum disorder and digestive symptoms
- Breastfeeding nutrition: Tips for moms
- Butter vs. margarine
- Caffeine content
- Caffeine: How much is too much?
- Is caffeine dehydrating?
- Timing calcium supplements
- Calorie calculator
- COVID-19 and vitamin D
- Can vitamins help prevent a heart attack?
- Can whole-grain foods lower blood pressure?
- Can zinc supplements help treat hidradenitis suppurativa?
- Carbohydrates
- Chart of high-fiber foods
- Cholesterol: Top foods to improve your numbers
- Clear liquid diet
- Coconut water: Is it super hydrating?
- Coffee and health
- Cuts of beef
- DASH diet: Recommended servings
- Sample DASH menus
- Diet soda: How much is too much?
- Dietary fats
- Dietary fiber
- Diverticulitis attack triggers
- Diverticulitis diet
- Vitamin C and mood
- Prickly pear cactus
- Does soy really affect breast cancer risk?
- Don't get tricked by these 3 heart-health myths
- Eggs and cholesterol
- Enlarged prostate: Does diet play a role?
- Fasting diet: Can it improve my heart health?
- Fiber supplements
- Ground flaxseed
- Food safety
- Foodborne illness
- Gluten sensitivity and psoriasis: What's the connection?
- Gluten-free diet
- Gout diet: What's allowed, what's not
- Grass-fed beef
- Guide to herbs and spices
- Healthy meals start with planning
- Heartburn medicines and B-12 deficiency
- High-protein diets
- How to track saturated fat
- Intermittent fasting
- Is there a special diet for Crohn's disease?
- Low-fiber diet
- Low-glycemic index diet
- Meatless meals
- Mediterranean diet
- Menus for heart-healthy eating
- Moldy cheese
- Monosodium glutamate (MSG)
- Multivitamins for kids
- Nuts and your heart: Eating nuts for heart health
- Omega-3 in fish
- Omega-6 fatty acids
- Organic foods
- Phenylalanine
- Picnic Problems: High Sodium
- Portion control
- Prenatal vitamins
- Probiotics and prebiotics
- Safely reheat leftovers
- Sea salt vs. table salt
- Taurine in energy drinks
- Nutrition and pain
- Vitamin C megadoses
- Underweight: Add pounds healthfully
- Vegetarian diet
- Vitamin D and MS: Any connection?
- Vitamin D deficiency
- Can a lack of vitamin D cause high blood pressure?
- Vitamin D for babies
- Vitamin D toxicity
- Vitamins for MS: Do supplements make a difference?
- Water after meals
- Daily water requirement
- What is BPA?
- Whole grains
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle

We’re transforming healthcare
Make a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
- The New Food Fights: U.S. Public Divides Over Food Science
- 1. Public views about Americans’ eating habits
Table of Contents
- 2. Americans’ views about and consumption of organic foods
- 3. Public opinion about genetically modified foods and trust in scientists connected with these foods
- About this report
- Acknowledgments
- Methodology
The American food scene has undergone considerable change over the past two decades. During this period, the public has seen the introduction of genetically modified crops, the mainstreaming of organic foods into America’s supermarkets, 4 and the proliferation of chefs elevated to celebrity status within popular culture.
Over the same period, there has been a marked increase in public health concerns about the growing prevalence of obesity among both children and adults. Perhaps sparked by thinking from people such as Michael Pollan, 5 Mark Bittman, 6 and documentaries such as Morgan Spurlock’s “Super Size Me,” Americans thinking about food has shifted dramatically.
Concerns about obesity, food allergies and other health effects of food are fueling a new level of scrutiny of chemicals and additives in foods and contribute to shifting notions about portion size, sugar and fat content. 7 Consumption of sugary sodas has dropped to a 30-year low while sales of bottled and flavored water rose dramatically over the past few decades. Zero-calorie diet sodas long held allure for Americans concerned about their weight, but sales of diet sodas have also dropped, with at least some arguing that the decline has been fueled by growing public concern about ingesting artificial sweeteners and other food additives. 8 America’s love affair with fast-food chains is on the wane, with “fast casual” brands that offer convenient options which focus on natural, fresh ingredients gaining favor. 9
To some degree this is reflected in the emergence of distinct groups that can be identified by their focus on food issues and personal eating habits. New thinking about ways to eat healthy helped launch a number of eating “movements” with proponents arguing that Paleo, anti-inflammatory or vegan diets bring health benefits along with better weight control. Food and the way we eat has become a potential source of social friction as people follow their own ideologies about what to eat and how foods connect with people’s ailments.
During this same period, there have been sometimes strident public debates over science-related topics – most prominently on climate change, but also on a host of others including the environmental impacts of fracking and nuclear power, the safety of childhood vaccines and, of course, the safety of genetically modified foods. A previous Pew Research Center report showed that public attitudes on a wide range of science issues were widely divergent from those of members of the American Association of Advancement of Science (AAAS). In fact, the largest differences between the public and members of the AAAS were beliefs about the safety of eating genetically modified (GM) foods. Nearly nine-in-ten (88%) AAAS members said it is generally safe to eat GM foods compared with 37% of the general public, a difference of 51 percentage points. The wide differences of opinion over GM foods is connected with a broader public discourse over the role of science research and, perhaps, scientific expertise in understanding and crafting policy solutions.
This new Pew Research Center survey explores public thinking about scientists and their research on GM foods in some detail. As such, this survey can help address the ways in which public views of and trust in scientists may contribute to an opinion divide between the public and members of the scientific community on these issues.
In broad strokes, the survey shows that Americans believe the public is paying more attention to healthy eating today than they did 20 years ago. But, it is not clear to the public whether people are actually eating healthier today. About half of U.S. adults think the eating habits of Americans are less healthy today than they were 20 years ago and most point the blame at both the quantity and quality of what people eat.
Many Americans adopt their own food and eating philosophies because they have to – or want to. Some 15% of U.S. adults say they have at least mild allergies to one or more foods and another 17% have intolerances to foods. Food allergies are more common among women, blacks and people with chronic lung conditions such as asthma. A small minority of Americans describe themselves as either strictly or mostly eating vegan or vegetarian diets.
Americans are paying attention to healthy eating, but many miss the mark

Collectively, the American public is paying more attention to healthy eating, but not fully embracing what they learn. At least, that’s how most Americans see things, according to this survey.
Some 54% of Americans say that compared with 20 years ago, people in the U.S. pay more attention to eating healthy foods today. Smaller shares say people pay less attention (26%) or about the same amount of attention (19%) to eating healthy today.

But 54% of Americans say eating habits in the U.S. are less healthy than they were 20 years ago. A minority (29%) say eating habits are healthier today, while 17% say they are about the same.
The public points the finger at both quality and quantity in Americans’ eating habits. When asked which is the bigger source of problems in Americans’ eating habits, more say the issue is what people eat, not how much (24% vs. 12%). But a 63% majority says that both are equally big problems in the U.S. today.
These beliefs are somewhat tied to people’s focus on food issues. People who care a great deal about the issue of GM foods are particularly likely to say Americans’ eating habits have deteriorated over the past two decades: 67% hold this view, compared with 53% among those not at all or not too concerned about the GM foods issue. People focused on eating healthy and nutritious are relatively more inclined to say the types of food people eat is a bigger problem in the U.S. today than the overall amount (34%, compared with 21% among those not at all or not too focused on healthy and nutritious eating.)

What’s driving public attention to eating? One factor may be a belief in the oft-repeated adage “you are what you eat.” Roughly seven-in-ten adults (72%) say that healthy eating habits are very important for improving a person’s chances of living a long and healthy life.
A similar share (71%) says getting enough exercise is very important. Some 61% say safe and healthy housing conditions are very important. But fewer – 47% – believe genetics and hereditary factors are critical to improving a person’s chances of a long and healthy life. Thus, most Americans consider their future health within their own grasps — if only they eat and exercise adequately.
People focused on food issues are particularly likely to believe that healthy eating habits are important. Fully 86% of those focused on eating healthy and nutritious say that healthy eating habits are very important, compared with 56% among those with little focus on eating healthy and nutritious. And, 87% of those with a deep personal concern about the issue of GM foods say that healthy eating habits are very important for a long and healthy life, compared with 68% among those with no or not too much concern about the GM foods issue.
Americans have a variety of eating styles and philosophies about food

Americans have many different approaches to eating. More say they focus on taste and nutrition than say they focus on convenience. Almost one-quarter (23%) of Americans say the statement “I focus on the taste sensations of every meal” describes them very well, while another 53% say this statement describes them fairly well. Similar shares say their “main focus is on eating healthy and nutritious,” with 18% saying this statement describes them very well and 55% saying it describes them fairly well.
Smaller shares say the statements “I usually eat whatever is easy and most convenient” and “I eat when necessary but don’t care very much about what I eat,” describe them very well (12% and 7%, respectively). People with a particular concern about the GM foods issue and people focused on eating healthy and nutritious are less likely to describe themselves as unconcerned about what they eat.

But, when Americans judge their own eating habits, a majority see themselves falling short. Some 58% of U.S. adults say that “most days I should probably be eating healthier.” About four-in-ten (41%) hit their eating targets about right, saying they eat about what they should most days.
Those who are focused on eating healthy are, by and large, satisfied with their eating. Seven-in-ten (70%) of this group says they eat about what they should on most days. By contrast, 86% of people who describe themselves as not at all or not too focused on healthy eating say they should probably be eating healthier on most days.
There are more modest differences in eating assessments by degree of concern about the issue of GM foods; 51% of those who care a great deal about the issue of GM foods says they eat about they should most days, compared with 37% of those with no particular concern or not too much concern about this issue.
Sizable minority of Americans have food allergies or intolerances to foods
More children and adults are experiencing allergic reactions to foods today. Concern about food allergies and sensitivities can be seen in many places – from the regulations governing the public school lunch program to the way restaurants and food manufacturers package and offer alternatives to the most common allergens. 10 For example, people with lactose intolerance can now choose from a wide range of milk and dairy alternatives made from soy and nuts. People allergic to the gluten in wheat can choose among special menu selections, even whole bakeries devoted to gluten-free options.

About 15% of U.S. adults say they have severe, moderate or mild allergies to at least one kind of food. Another 17% of adults have food intolerances, but no food allergies. Roughly seven-in-ten of the adult public (69%) has no food intolerances or allergies.
More women than men report food allergies. About two-in-ten (19%) women say they have severe, moderate or mild food allergies, compared with 11% of men. And, blacks are more likely to say they have food allergies (27%) than either whites (13%) or Hispanics (11%). In other respects, those with food allergies reflect a mix of demographic and educational backgrounds 11
The Center for Disease Control and Prevention reports a higher prevalence of asthma among children with food allergies. The Pew Research Center survey finds 29% of adults with asthma or another chronic lung condition have food allergies, compared with 12% among those who do not have chronic lung conditions.
Vegans and vegetarians are a small minority of U.S., but they are a bit more common among younger generations and liberal Democrats

Vegetarianism has been around for centuries and interest in following this diet – most commonly defined as omitting meat and fish – has waxed and waned over time. Today, vegetarian options are commonplace at many restaurants and food proprietors. Some of those who avoid meat and fish go a step further; vegans typically omit all foods that originate from animals including eggs and dairy products. But some people who consider themselves either vegetarian or vegan are “flexible” about what they eat and at least occasionally veer from these eating principles.
The Pew Research Center survey asked for people’s own assessment of whether the terms vegan and vegetarian applied to them. A small minority – 9% – of U.S. adults identifies as either strict vegetarians or vegans (3%) or as mostly vegetarian or vegan (6%). The vast majority of Americans (91%) say they are neither vegetarian nor vegan.
Younger generations are more likely than others to identify as at least mostly vegan or vegetarian. Some 12% of adults ages 18 to 49 are at least mostly vegan or vegetarian, compared with 5% among those ages 50 and older. Men and women are equally likely to be vegan or vegetarian. There are no differences across region of the country, education or family income in the share who is vegan or vegetarian. There are more liberal Democrats in the vegan and vegetarian group, however. Some 15% of liberal Democrats are at least mostly vegan or vegetarian, compared 4% among conservative Republicans. 12
People who have food allergies are more likely to be vegan or vegetarian, suggesting that some food restrictions stem from adverse reactions to certain foods. Among adults with food allergies, 21% identify as strictly or mostly following vegan or vegetarian diets. Just 8% of adults with food intolerances (but no allergies) and 6% of adults with neither food allergies nor intolerances are vegan or vegetarian. Thus, about a third of people who identify as at least mostly vegan or vegetarian also report food allergies.
Social networks: friends eat like friends
People tend to cluster together in social networks with others who are similar. The Pew Research Center survey finds this social pattern also occurs when it comes to people’s eating philosophies and dietary habits.

Most Americans say that at least some of their closest friends and family focus on eating healthy and nutritious. Some 68% say this, while 32% say only a few or none of their friends and family does this.
Adults who say the statement “my main focus is on eating healthy and nutritious” describes them at least very or fairly well are more likely to say at least some of their closest family and friends do the same.

A minority of the population (24%) says that most or some of their closest family and friends have food intolerances or food allergies. Among those who say that they, personally, have severe to mild allergies to some foods, a larger share (51%) says at least some of their closest family and friends also have intolerances or allergies.

A similar pattern occurs when it comes to vegetarians and vegans. Some 12% of U.S. adults say that at least some of their close family and friends are vegan or vegetarian. But there are stark differences in social network composition among those who are, personally, vegan or vegetarian and those who are not. Fully 52% of people who are at least mostly vegan or vegetarian say that some or most of their closest family and friends also follow vegan or vegetarian diets. Just 8% of people who are not themselves vegan or vegetarian say the same.
Many Americans say it’s good party hosting behavior to inquire about food restrictions; few say it bothers them when guests ask for dietary accommodations

Businesses have changed what foods they offer and how foods are packaged to accommodate Americans’ diverse dietary needs and preferences over the past decade or more. What do people think about accommodating people’s eating needs and preferences at private social gatherings? The Pew Research Center survey finds 37% of Americans say that, when hosting social gatherings, the host should always ask guests ahead of time if they have any food restrictions or allergies. One-quarter say they should do this sometimes, while 37% believe the host should never or not too often ask about food restrictions before hosting social gatherings.

When they are the host, a minority (31%) of Americans say it bothers them at least some when guests ask for special kinds of food options at their social gatherings. Larger shares say it bothers them not too much (37%) or not at all (30%) when someone asks for special food accommodations at their social gatherings.
Americans’ beliefs about proper hosting behavior tend to be related to their own food ideologies. About half (49%) of those with a deep personal concern about the GM foods issue say that hosts should always ask guests about dietary needs; this compares with 32% of those with no or not too much concern about the GM foods issue. But people who themselves have food allergies are about equally likely as other adults to say that a host should ask about food allergies ahead of a gathering. And, like other Americans, a minority of those focused on food issues say they are bothered at least some when guests ask for special food options at a gathering they host.
Food studies and their conflicting findings abound, but most Americans see this as a sign of progress

A clear sign that many Americans are thinking about food is that they are paying attention to news and research studies on the subject. Fully two-thirds (66%) of the public says they hear or read news stories about the health effects of what people eat and drink every day (23%) or a few times a week (43%). About one-quarter (24%) say they see these news stories a few times a month while 9% report seeing these stories less often than that.
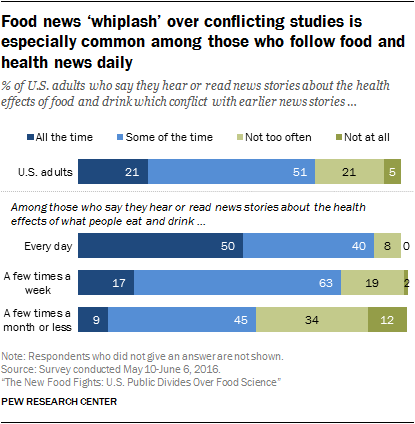
And many Americans perceive such studies as contradicting prior news reports at least some of the time. About half of U.S. adults (51%) say they hear or read news stories about the health effects of foods that conflict with earlier studies some of the time and roughly one-in-five (21%) say this occurs all the time. A minority of Americans (26%) say this does not occur at all or not too often.
People who regularly follow news about food and health issues are particularly likely to see news stories with contradictory findings. Some 50% of Americans who follow news about the health effects of foods on a daily basis say they see conflicting news reports about food all the time. Just 17% of those who hear or read food news a few times a week say that conflicting stories about the health effects of food and drink occur all the time and 9% of people who less regularly attend to food news say conflicting reports occur all the time.
There is considerable concern in the science community that this whiplash effect might confuse Americans and affect their views of the trustworthiness of science findings. The survey included two questions to shed light on how the public makes sense of contradictory findings about the health effects of foods.

A majority of the American public (61%) says “new research is constantly improving our understanding about the health effects of what people eat and drink, so it makes sense that these findings conflict with prior studies,” while a 37% minority says “research about the health effects of what people eat and drink cannot really be trusted because so many studies conflict with each other.”
People’s focus on food issues is not strongly related to beliefs about news stories with conflicting findings. Instead, people’s general levels of knowledge about science, based on a nine-item index, tie to how people make sense of conflicting food studies in the news. Some 74% of those high in science knowledge say studies with findings that conflict with prior studies are signs that new research is constantly improving. But those in low science knowledge are closely divided over whether such studies are signs of improving research (46%) or show that food research cannot really be trusted (50%).
And, fully 72% of U.S. adults say even though new studies sometimes conflict with prior findings “the core ideas about how to eat healthy are pretty well understood.” Only one-quarter of the public (25%) feels overwhelmed by the inconsistent findings, saying, “It is difficult to know how to eat healthy because there is so much conflicting information.”

Here, too, beliefs are closely linked with people’s level of knowledge about science. Fully 92% of those high in science knowledge say the core ideas about how to eat healthy are pretty well understood as do 78% of those with medium science knowledge. But those low in science knowledge are closely split with half (50%) saying the core ideas of how to eat healthy are pretty well understood and 47% saying it is difficult to know how to eat healthy because there is so much conflicting information. Thus, Americans with less grounding in science information appear to be more confused by and distrustful of research with contradictory findings about food and health effects.
- Catherine Greene, Seth J. Wechsler, Aaron Adalja and James Hanson, Feb. 2016. “ Economic Issues in the Coexistence of Organic, Genetically Engineered (GE) and non-GE Crops ” Economic Research Service, U.S. Department of Agriculture. ↩
- Michael Pollan. 2006. “The Omnivore’s Dilemma: A Natural History of Four Meals” New York: Penguin Press. ↩
- See for example, the opening column for ‘The Flexitarian,’ Mark Bittman, “ Healthy, Meet Delicious ,” New York Times, April 23, 2013. ↩
- See for example, Hans Taparia and Pamela Koch, “ A Seismic Shift in How People Eat ,” New York Times, Nov. 6, 2015. Scott Mowbray, “ The Rise of the New Food Culture ,” The Huffington Post, Dec 10, 2012. Jeff Green and Craig Giammona. “ How Halal Food Became a $20 Billion Hit in America ,” Bloomberg, Sept. 14, 2016. ↩
- See Sanger-Katz, Margot. “ The Decline of ‘Big Soda,’ ” New York Times, Oct. 2, 2015. ↩
- See Specter, Michael. “ Freedom from Fries: Can fast food be good for you? ” The New Yorker, Nov. 2, 2015. ↩
- A report by the CDC finds an increase in reported food allergies among children between 1997 and 2011. ↩
- Differences by gender and race in self-report food allergies are consistent with a report from the National Health and Nutrition Examination Survey conducted by the Center for Disease Control and Prevention. ↩
- These figures combine those who identify as either Democratic or Republican with independents who lean to each party, respectively. ↩
Sign up for our weekly newsletter
Fresh data delivery Saturday mornings
Sign up for The Briefing
Weekly updates on the world of news & information
- Climate, Energy & Environment
- Emerging Technology
- Health Policy
- Medicine & Health
Most Popular
Report materials.
- American Trends Panel Wave 17
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
© 2024 Pew Research Center

Personalize Your Experience
Log in or create an account for a personalized experience based on your selected interests.
Already have an account? Log In
Free standard shipping is valid on orders of $45 or more (after promotions and discounts are applied, regular shipping rates do not qualify as part of the $45 or more) shipped to US addresses only. Not valid on previous purchases or when combined with any other promotional offers.
Register for an enhanced, personalized experience.
Receive free access to exclusive content, a personalized homepage based on your interests, and a weekly newsletter with topics of your choice.
Home / Nutrition & Fitness / 11 tips for healthier eating habits
11 tips for healthier eating habits
A healthy diet can help reduce the risk of some health conditions. Picking up some beneficial habits now might help avoid having to make abrupt changes later.
Please login to bookmark

Eating habits often begin in childhood. Some are healthy, like grabbing your water bottle when you leave the house and layering lettuce and tomato on a sandwich. Some are not so healthy, like drinking soda throughout the day.
You might not think about those established habits — until you have a reason to. Sometimes a test result showing high cholesterol, blood pressure or blood sugar inspires change. Even without a diagnosis, it’s always a good time to adopt healthier eating habits. Making diet changes can help reduce the risk of chronic disease. Diet is linked to heart disease, type 2 diabetes and 13 kinds of cancer.
The majority of Americans don’t eat a healthy diet, according to the American Heart Association. Of course, it’s not all by choice. Systems are in place that make it easier and cheaper to grab a fast-food meal on the way home than it is to buy and prep ingredients for dinner. If you work two jobs, have kids who are picky eaters or don’t live near a grocery store, eating nutrient-rich foods can be even more challenging.
Making changes to diet habits isn’t always as easy as social media influencers might make it sound either. Research shows that the more often a person eats high-sugar or high-fat foods, the more they develop a taste for them. That makes habits even harder to break.
Here are some tips from Mayo Clinic experts for adding some healthy eating habits.
Learn the basics of a healthy diet
The diet you follow should fit your tastes, lifestyle and budget. It shouldn’t be so restrictive that you can’t follow it indefinitely. Here are some basics for a healthy diet:
- Eat more vegetables and fruits. Most Americans don’t get the recommended five or more servings per day, so look for opportunities to add more fresh, frozen, or canned fruits and vegetables. When comparing canned options, look for low-sodium vegetables and fruit packed in juice or water rather than syrup.
- Pick whole grains. When you look at the ingredients list on foods like bread and cereal, look for the words “whole wheat” or “whole grain.” An easy guideline is to pick the one with the most grams of fiber per serving. You also can include brown rice, quinoa, millet and oats in your diet.
- Limit unhealthy fats. Saturated fats are mostly found in animal products like meat, cheese and butter. To help with healthy blood pressure levels , try to keep your intake of saturated fats to 13 grams per day. Avoid trans fats as much as possible.
- Choose low-fat protein. Try to use fewer red and processed meats like bacon, sausage, and breaded chicken. Instead, choose eggs, beans, turkey, chicken, fish, lean beef and low-fat dairy.
- Reduce salt intake. Healthy adults should try to limit their sodium to 2,300 milligrams of sodium a day, which is about a teaspoon of salt.
Make a plan
It might help to track your food for a few days. Use an app or write down what you ate and when. You could make notes about your mood or your hunger level when you ate. You might notice that you:
- Snack while cooking.
- Keep eating even if you’re full so you don’t waste food.
- Eat while distracted, such as while scrolling social media.
- Always crave something sweet after dinner.
- Get tempted by the menu of pastry offerings when you stop for coffee.
With this information, you can start looking for patterns you want to break. Some of the following tips might work for you.
Start with an easy one. It’s hard to change everything at once, so start with the healthy habit that would be easiest for you. It might be adding a vegetable to dinner or using brown rice instead of white.
Make an impact. If you’re trying to reduce your sugar intake, for example, start with the biggest sources of sugar, like desserts and sweetened beverages. Don’t worry so much about the sugar in your condiments or salad dressings.
Add instead of subtract. Rather than making cuts, think about what you can add. You might have a serving of fruit with breakfast or enjoy a walk after lunch. Focus on what you can have. That might leave less time in your day or room in your belly for habits you want to break.
Cut your portion sizes. You can enjoy your favorite foods and still cut your sugar or saturated fat intake. Try switching to a small soda, sharing dessert with a friend or using less butter on your toast.
Drink water. Sometimes thirst is mistaken for hunger. Sipping water throughout the day helps keep you full and hydrated.
Sit at the table to eat. Stepping away from your desk or phone will allow you to focus on your food and internal cues for hunger or fullness.
Find a replacement. If you eat out of habit, can you find a different habit? Consider having fruit for dessert. Or go for a walk until the craving subsides. Cravings come like waves. If you ride them out, they will pass.
Relax. People don ‘ t always make the healthiest choices when tired or stressed. Sometimes improving your diet comes from prioritizing sleep or stress management.
Remember why. Think about why forming healthier habits is important to you. Maybe you want more energy to finish projects around the house or to keep up on the company softball team. Consider setting a picture of your healthy-habit motivation as the lock screen of your phone or writing a note to yourself.
Ask for support. Tell your loved ones about your goals and what you’re doing. Ask them to support your efforts. You might even inspire them to make their own healthy changes.
Accept imperfections. Having a doughnut in the breakroom or an extra slice of pizza at dinner doesn’t mean all progress is lost. No side order of guilt needed.
A dietitian can help
You don’t have to make diet changes on your own. Ask your health care team for a referral to a dietitian. The dietitian can help you find solutions that work for your lifestyle and budget. You also can find professional and community support with the Mayo Clinic Diet .

Relevant reading
The Mayo Clinic Diabetes Diet, 3rd Edition
This adaptation of the #1 New York Times bestselling book, The Mayo Clinic Diet, provides those living with type 2 diabetes a simple and straightforward guide to losing weight and keeping it off.

Discover more Nutrition & Fitness content from articles, podcasts, to videos.
You May Also Enjoy

by Donald D. Hensrud, M.D., M.S.

Privacy Policy
We've made some updates to our Privacy Policy. Please take a moment to review.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- Health Topics
- < Back To Heart-Healthy Living
- Choose Heart-Healthy Foods
- What Is Heart-Healthy Living?
- Understand Your Risk for Heart Disease
- Get Your Blood Pressure and Cholesterol Checked
- Aim for a Healthy Weight
- Get Regular Physical Activity
- Manage Stress
- Quit Smoking
- Get Enough Good-Quality Sleep
MORE INFORMATION
Heart-Healthy Living Choose Heart-Healthy Foods
Language switcher.
Heart-healthy eating involves choosing certain foods, such as fruits and vegetables, while limiting others, such as saturated fats and added sugars.
Your doctor may recommend the heart-healthy Dietary Approaches to Stop Hypertension (DASH) eating plan because it has been proven to lower high blood pressure and “bad” LDL cholesterol in the blood. See Delicious Heart-Healthy Eating for recipes, cooking tips, and more information.
Foods to eat
These foods are the foundation of a heart-healthy eating plan.
- Vegetables such as leafy greens (spinach, collard greens, kale, cabbage), broccoli, and carrots
- Fruits such as apples, bananas, oranges, pears, grapes, and prunes
- Whole grains such as plain oatmeal, brown rice, and whole-grain bread or tortillas
- Fat-free or low-fat dairy foods such as milk, cheese, or yogurt
- Fish high in omega-3 fatty acids (salmon, tuna, and trout)
- Lean meats such as 95% lean ground beef or pork tenderloin or skinless chicken or turkey
- Nuts, seeds, and soy products (tofu)
- Legumes such as kidney beans, lentils, chickpeas, black-eyed peas, and lima beans
- Canola, corn, olive, safflower, sesame, sunflower, and soybean oils (not coconut or palm oil)
- Nuts such as walnuts, almonds, and pine nuts
- Nut and seed butters
- Salmon and trout
- Seeds (sesame, sunflower, pumpkin, or flax)
Foods to limit
A heart-healthy eating plan limits sodium (salt), saturated fat, added sugars, and alcohol. Understanding nutrition labels can help you choose healthier foods.
Limit sodium
Adults and children over age 14 should eat less than 2,300 milligrams of sodium a day. Children younger than age 14 may need to eat even less sodium each day based on their sex and age. If you have high blood pressure , you may need to limit sodium even more. Talk to your healthcare provider about the amount of sodium that is right for you or your child.
Try these shopping and cooking tips to help you choose and prepare foods that are lower in sodium:
- Read food labels and choose products that have less sodium for the same serving size.
- Choose low-sodium , reduced-sodium, or no-salt-added products.
- Choose fresh, frozen, or no-salt-added foods instead of pre-seasoned, sauce-marinated, brined, or processed meats, poultry, and vegetables.
- Eat at home more often so you can cook food from scratch, which will allow you to control the amount of sodium in your meals.
- Flavor foods with herbs and spice s instead of salt.
- When cooking, limit your use of premade sauces, mixes, and instant products such as rice, noodles, and ready-made pasta.

Tips to Reduce Salt and Sodium
Learn about how to cut down the amount of salt you take in each day with the Tips to Reduce Salt and Sodium tip sheet.
Limit saturated fats
Saturated or “bad” fats come from animal sources such as butter, cheese, and fatty meats. They should make up less than 10% of your daily calories. Unsaturated fats are also known as “good” fats and are found in vegetable oils and nuts.
Read food labels and choose foods that are lower in saturated fats and higher in unsaturated fats.
- Eat leaner, lower-fat, and skinless meats instead of fatty cuts of meat and chicken with skin.
- Consume lower-fat dairy products instead of whole-milk.
- Use certain vegetable oils (such as olive and canola oil) instead of butter, lard, and coconut and palm oils.
Limit added sugars
You should limit the amount of calories you get each day from added sugars. This will help you choose nutrient-rich foods and stay within your daily calorie limit.
Some foods, such as fruit, contain natural sugars. Added sugars do not occur naturally in foods but instead are used to sweeten foods and drinks. They include brown sugar, corn syrup, dextrose, fructose, glucose, high-fructose corn syrup, raw sugar, and sucrose.
In the United States, sweetened drinks, snacks, and sweets are the major sources of added sugars.
- Sweetened drinks include soft drinks or sodas, fruit drinks, sweetened coffee and tea, energy drinks, alcoholic drinks, and favored waters. Sweetened drinks account for about half of all added sugars consumed.
- Snacks and sweets include grain-based desserts such as cakes, pies, cookies, brownies, doughnuts; dairy desserts such as ice cream, frozen desserts, and pudding; candies; sugars; jams; syrups; and sweet toppings.
Lower how much sugar you eat or drink.
- Choose drinks without added sugar such as water, low-fat or fat-free milk, or 100% vegetable juice.
- Choose unsweetened foods for snacks or dessert.
- Eat sweetened drinks, snacks, and desserts less often and in smaller amounts.
Limit alcohol
Talk to your healthcare provider about how much alcohol you drink. They may recommend that you reduce the amount of alcohol you drink or that you stop drinking alcohol. Alcohol can:
- Add calories to your daily diet and possibly cause you to gain weight
- Raise your blood pressure and levels of triglycerides fats in your blood
- Contribute to or worsen heart failure in some people, such as some people who have cardiomyopathy
- Raise your risk of other diseases such as cancer
If you do not drink, you should not start. You should not drink if you are pregnant, are under the age of 21, taking certain medicines, or if you have certain medical conditions, including heart failure.
How much should you eat?
You should eat the right amount of calories for your body, which will vary based on your sex, age, and physical activity level. Remember that some healthy foods, including oils and dairy, can still have a lot of calories. Some fruits can have a lot of natural sugar, especially when they are dried. Develop a personalized food plan at Get Your MyPlate Plan .
You can visit the U.S. Department of Health and Human Services’ and U.S. Department of Agriculture’s 2020–2025 Dietary Guidelines for Americans has information about healthy eating and recommendations for healthy eating patterns.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.
Testing fitness of aging brain

DNR orders for Down syndrome patients far exceeded pandemic norm

Researchers reverse hair loss caused by alopecia

Stephanie Mitchell/Harvard Staff Photographer
Binge eating appears more widespread, persistent than thought
New research takes broader, deeper look at common, but poorly understood, disorder
Alvin Powell
Harvard Staff Writer
Binge eating is one of the world’s most common eating disorders but is poorly understood. Kristin Javaras , assistant professor of psychology at Harvard Medical School’s Department of Psychiatry and instructor in epidemiology at Harvard T.H. Chan School of Public Health , recently shed light on the subject in a study, published in the journal Psychological Medicine. The findings showed that earlier research, which focused on younger women, underestimated how chronic the problem can be for many in the broader population, lasting for years or even decades. Javaras, who is also associated psychologist at McLean Hospital’s Division of Women’s Mental Health, spoke to the Gazette about her recent research.
What is binge eating?
Binge-eating disorder is characterized by binge eating episodes, which have two components, according to the DSM — the reference manual for diagnoses. One is an objectively large amount of food. Second — and most importantly — there’s a sense of loss of control, a feeling that you can’t stop or you can’t avoid starting. Some people feel like they’re driven by a motor, and they can’t stop until either they feel so sick that they have to or the food is gone.
These episodes are often characterized by eating quickly and eating alone and accompanied by a feeling of shame. People have recurrent episodes. So, if the person experiences marked distress around binge eating and isn’t engaged in compensatory behaviors that you see in bulimia nervosa — purging regularly, using laxatives or diuretics, extreme dieting or fasting, or engaging in excessive or compulsive exercise — there would be a diagnosis of binge-eating disorder.
“When people diet and think, ‘I’m going to try to eat as little as possible,’ that sets them up to engage in binge eating.”
When you say “an objectively large amount,” we’re not talking about Thanksgiving dinner or another holiday where we’re socialized to overeat? How do we know the difference?
If it is typical for a circumstance, it is not binge eating. Likewise, if there’s no loss of control it’s not binge eating. For instance, if I want to run a marathon tomorrow and I eat a large amount of pasta intentionally, with a sense of control, that wouldn’t be binge eating.
It can be tricky to evaluate, but the question is whether it’s an objectively large amount for that person in that context. So Thanksgiving typically wouldn’t count unless it was far beyond what other people are eating, and accompanied by a sense of loss of control.
Does it have to be every day? Once a month?
The diagnostic guidelines have changed recently. In DSM-4, it was two days a week, while in DSM-5 it is one episode a week. But there are people for whom it doesn’t happen as frequently, but the binges are very upsetting. They technically don’t meet DSM-5’s definition of binge-eating disorder, but it could still be very clinically significant, even if it’s not happening once a week. It’s important to note that the study we’re talking about was done under DSM-4.
What is the harm if you binge once a week and eat normally the rest of the week? Weight gain? Poor nutrition?
We know that binge eating does have metabolic consequences. There is a study that shows if you eat the same amount of food in a very short period of time, it’s metabolically worse for you than if you ate it over a whole day, particularly the types of foods that are consumed in a binge, which tend to be highly palatable and have metabolic consequences.
But what’s more important are the psychological effects. People are often restricting to some degree: not eating enough, not allowing themselves to eat certain types of foods. They hold beliefs like, “I should never eat X” or “This food is bad.” There’s a lot of binary thinking and people often feel extremely negatively about their bodies.
The binge eating is in the DSM, but for those of us in practice, we see it as one symptom among many in the eating disorder. Addressing restriction — getting people to eat regularly — is one of the most potent interventions. Often people feel that, because they are at a higher weight, they should be dieting all the time. And when people diet and think, “I’m going to try to eat as little as possible,” that sets them up to engage in binge eating.
“A lot of the initial studies on eating disorders were based on treatment-seeking samples, which are, by definition, not representative. Anyone can get an eating disorder.”
What’s the prevalence of binge eating in society?
That’s a tricky question because the research doesn’t entirely agree. The National Comorbidity Survey Replication, which was done in 2007 by my mentor, Jim Hudson, and Ron Kessler, suggested that the prevalence of DSM-4 binge-eating disorder was around 2.6 percent [chance over a] lifetime in the U.S.
DSM-5, because it’s a broader category, would be higher than that. A more recent study by Udo and Grilo in 2018 was just under 1 percent lifetime. There are some methodological reasons why they may differ, so it’s hard to get a clear estimate, but I’d say somewhere between 1 and 3 percent lifetime in the U.S.
So millions of people. Is it the most common eating disorder?
Yes, it is — in the U.S. and globally — though we don’t have good data from some regions of the world.
Let’s talk about your study. You were trying to settle differences in earlier studies about how long binge-eating disorder takes to resolve on its own. What did you find?
My mentors, Jim Hudson and [Harrison] Skip Pope, did a family study of binge-eating disorder in the early aughts. They subsequently followed the study participants forward for five years, re-interviewing them every 2.5 years.
They thus had really unique, valuable data on the disorder’s duration, and I suggested we look at both remission and relapse, and also use machine learning to see if we can predict whether somebody will go into remission. Our analyses showed that although there is improvement over time, the disorder doesn’t just vanish after a few months for most people in our sample.
And the key finding was focused on it resolving naturally, not with treatment?
That’s why this study is so important. We already have very good data on how people respond to treatment. But because they’re getting treatment, it’s not a representative sample of what happens in the real world.
We found that, at 2.5 years, about 15 percent of people had moved into remission, with no binge-eating episodes for three months. At five years, that was a little over 20 percent. And a little less than two-thirds of people still had full DSM-4 binge-eating disorder at 2.5 years. A little under half still had the disorder at five years. The rest were somewhere in the middle: They didn’t meet the DSM-4 criteria for binge-eating disorder, but they weren’t fully in remission.
I should also mention that this was snapshot data at 2.5 and 5 years, but people move around in between. When we looked at the in-between data, based on people’s retrospective report of what had happened over the 2.5 years, we see some people are experiencing remission, but relapse is fairly common, and the median time to remission is over 60 months.
And that is different from the other studies you looked at?
There were a couple of levels. The older prospective studies were small, under 50 people, excluded males, and the participants tended to be younger.
We know that, for younger people with eating disorders, presentations can change more rapidly than someone who’s had binge-eating disorder for 20 years. Those studies suggest that only a minority of people still had a full threshold of binge-eating disorder at two to five years of follow-up.
But also we knew that the individuals in those studies were young, were mostly at lower BMI, and there were no men. Our sample had a much wider age range, was primarily high BMI, as well as being a bigger sample.
Were the samples in these older studies representative of outdated societal perceptions about who is affected by binge-eating disorder?
A lot of the initial studies on eating disorders were based on treatment-seeking samples, which are, by definition, not representative. Anyone can get an eating disorder.
Does this work say anything about treatment?
It does, although it requires making a few assumptions. If you look at the longer-term outcomes seen in high-quality, randomized controlled trials of psychotherapy for binge-eating disorder, the percent of people experiencing remission is higher than in our study. That suggests that people would get better faster with treatment than they would under natural circumstances.
I don’t want people to feel hopeless after seeing our study. There are effective treatments for binge-eating disorder, including one FDA-approved medication, lisdexamfetamine, and multiple evidence-based psychotherapies. Although our treatments are not perfect, they do help many people.
Share this article
You might like.
Most voters back cognitive exams for older politicians. What do they measure?

Co-author sees need for additional research and earlier, deeper conversations around care

Treatment holds promise for painlessly targeting affected areas without weakening immune system
- Open access
- Published: 17 June 2024
Cognition of diet quality and dietary management in elderly patients with coronary and other atherosclerotic vascular disease in western China, a qualitative research study
- Jiamengying Chen 1 na1 ,
- Xiaojie Li 1 na1 ,
- Yun Wang 2 ,
- Chunling Zhang 3 ,
- Li Yang 3 ,
- Lvheng Zhao 1 ,
- Qingqing Zhu 1 ,
- Li Wang 4 &
- Yixia Zhou 1 , 2
BMC Geriatrics volume 24 , Article number: 525 ( 2024 ) Cite this article
11 Accesses
Metrics details
Healthy eating is one of the most important nonpharmacologic treatments for patients with atherosclerosis(AS). However, it is unclear how elderly AS patients in western China perceive their dietary status and which type of nutritional assistance they would be willing to receive. Therefore, the primary purpose of this study was to understand the level of knowledge about current dietary habits and healthy eating habits among elderly AS patients in western China, and the secondary purpose was to identify acceptable nutritional assistance measures or pathways for those patients to help them manage disease progression.
An implementation study approach was used to recruit elderly patients with AS-related diseases in western China for semistructured interviews.
14 participants were included in the study, and the following three themes were identified from the interviews:(1) the diet with regional characteristics; (2) low nutrition-related health literacy; (3) complex attitudes towards nutritional assistance. Most participants had misconceptions about healthy eating, and the sources of their knowledge might not be trustworthy. Participants expressed a preference for personalized nutritional assistance, especially that provided by medical-nursing combined institutions.
Patients in western China need nutritional assistance for their regional dietary habits; therefore, healthy dietary patterns consistent with the regional culture are proposed to improve the prevailing lack of knowledge about healthy diets, improve the dietary structure of patients, and control the development of the disease.
Peer Review reports
Patients generally misunderstand dietary information, and their perceptions of dietary quality are different. With improvements in people’s living standards and a general lack of exercise, the incidence of atherosclerosis (AS) is increasing annually. The main incidence group is still the elderly population [ 1 ], and this disease has brought a greater economic burden to people and medical systems [ 2 ].
Poor eating habits are a definite risk factor for AS and one of the important risk factors associated with the burden of cardiovascular disease (CVD) [ 3 ]. In 2016, 2.1 million global deaths from CVD were linked to poor eating habits [ 4 ]. Many studies had shown that most people with AS have poor diet quality and poor knowledge of healthy diets [ 5 ]. Global comparative risk assessment studies have estimated that hundreds of thousands or even millions of deaths in patients with CVD can be attributed to the effects of certain diets and environments [ 6 ]. In China, many scholars had investigated the dietary behaviour of patients with AS. With the further development of the economy and the steady increase in the degree of urbanization [ 7 ], Chinese consumption of fruits, dairy products, snacks, fast food and beverages is increasing significantly, and the dietary pattern is gradually shifting to a high-fat Western diet [ 8 ]. This tendency may be closely related to the increasing incidence of AS-related diseases. China is a vast country, which leads to different eating habits among people in different regions. A study of 11,512 respondents in 47 provinces of China showed that the mortality rate of CVD in the central and western regions was greater than that in the eastern provinces of China, and poor eating habits were one of the risk factors for death. However, we found that the current research is still targeting individuals living in the eastern and northern regions of China [ 9 ]. There is a lack of surveys on people in western China, which may lead to a lack of targeted and personalized nutritional assistance for this population [ 10 ].
Nutritional assistance methods include providing relevant dietary advice [ 11 ], diet intervention measures [ 12 ], diet patterns [ 13 ], nutritional supplements [ 14 ], etc. In previous studies, health education related to diet management has been shown to effectively improve the disease awareness of patients with AS and to have a positive impact on some of its indicators, such as blood lipid levels and body mass index [ 15 ]. Before designing interventions, some investigators did not consider whether participants were willing to accept nutritional assistance, and they lacked an understanding of the participants’ daily life [ 16 ]. Moreover, researchers and clinical staff may be biased against interventions recognized by patients [ 17 ]. The incorporation of the perspective of patients can help researchers explore new interventions or discover new understandings of existing interventions to form higher-quality research. Understanding local eating habits in advance can also help researchers better identify the possible bad eating behaviours of the target group and develop more targeted interventions [ 18 ].
The main purpose of this study was to explore the views of patients with coronary and other atherosclerotic vascular diseases in western China on dietary quality and previously received dietary recommendations or nutritional assistance. The secondary purpose was to determine which nutritional assistance methods are acceptable for these patients to help them improve their health management.
Qualitative approach & research paradigm
This was a qualitative study, and we used a semistructured interview method. Mainly, we discussed how patients with coronary and other atherosclerotic vascular diseases viewed their dietary habits and intake, as well as their views on various nutritional assistance methods and approaches, and explored their feelings and expectations regarding nutritional assistance.
Researcher characteristics and reflexivity
Two researchers (Li Wang, Yixia Zhou) were responsible for the research design, and 1 researcher (Li Yang) who had a clinical nurse–patient relationship with the interviewees recruited and screened participants with the assistance of 3 researchers (Lvheng Zhao, Qingqing Zhu, Yun Wang). Two researchers (Jiamengying Chen, Xiaojie Li) conducted patient interviews under the supervision of a nutrition expert (Chunling Zhang) and entered and analysed the data. A total of 9 researchers participated in this study, all of whom had research/work backgrounds related to nutrition or CVD.
From March 2023 to June 2023, elderly people who visited 3 medical institutions in Guizhou Province, China, were selected as interviewees using purposive sampling methods. The average number of elderly people in the 3 medical institutions is approximately 80 per week. A stable medical team provides medical security and regularly carries out cardiac rehabilitation and other services.
Sampling strategy
The inclusion criteria for patients were as follows: (1) \(\ge\) 60 years old; (2) diagnosed with coronary or other atherosclerotic vascular disease [ 19 ]; (3) clear thinking, able to speak Chinese fluently, including Mandarin or dialect; and (4) signed written informed consent form to voluntarily participate in the study. The exclusion criteria were as follows: (1) cognitive impairment, (2) communication barriers.
After ethical review, posters were placed in cardiovascular clinics and nutrition clinics of medical institutions to recruit volunteers to participate in the study. Information on the poster included the purpose of the study, inclusion and exclusion criteria, and contact information for the principal investigator (Jiamengying Chen, Xiaojie Li). The posters were posted from February 2023 to May 2023, and 16 elderly patients with AS were invited to participate. Due to data saturation, a total of 14 elderly patients with AS were finally interviewed and numbered P1 to P14.
Before beginning the study, the researchers invited potential participants, explained the purpose and methods of the study to the participants who were willing to participate in the study, and interviewed the participants with their consent.
Ethical issues pertaining to human subjects
Before the start of the study, the research team provided written informed consent forms to the eligible participants. This study was approved by the the Ethics Committee of The Second Affiliated Hospital of Guizhou University of Traditional Chinese Medicine (No.: KYW2022007).
Data collection and instruments
Participants participated in research interviews from March 2023 to June 2023. The interviews were conducted in a separate lounge of the medical institutions to ensure participants’ privacy. After obtaining the participants’ consent, the researchers recorded the entire interview, and all recordings were obtained using the same electronic device. All participants were interviewed by the same researcher and supervised by the chief nurses on the research team. The participants had the right to know the educational level, professional title and other information about the researchers.
According to the purpose of the study, the members of the research group conducted a literature review in advance, discussed and formulated the interview outline, and conducted a pre-interview with 2 participants in advance. According to the interview results, the outline was modified, and the interview outline applied in this survey was finally determined. The interview outline consisted of open and closed questions. The main topics of discussion were the participants’ views on the current quality of their diet, whether they feel that their diet should be improved, and whether they were willing to accept medical assistance related to diet management. In addition, the researchers asked participants whether they had received diet-related or nutritionist guidance.
At the end of the interview, the researchers listed many types of nutritional assistance or approaches to participants and asked them to provide preferences for each type of nutritional assistance or approach. Before the interview, the researchers used a warm-up question to create a friendly atmosphere between the interviewer and the interviewee: “If you do not mind, could you tell me something about your AS-related disease?”
Clinical measures
The researchers collected information such as the participants’ age, sex, and types of disease. This information was collected to provide a sufficient sample description and determine whether there was heterogeneity.
Units of study
In this study, the saturation of data collection was used as the end point of the interview process; that is, if the data analysis was repeated with the previous data, and no new coding appeared, then the interview process was considered to be completed. After data saturation, 2 participants were interviewed to ensure that no new coding appeared [ 20 ]. The interview time ranged from 11 minutes and 08 seconds to 27 minutes and 35 seconds, with an average time of 17 minutes and 42 seconds.
Data processing
During the interview, the researcher recorded the patient’s intonation, speech rate, expression, gesture and so on. To reduce the researchers’ memory bias, the recordings were converted into text within 24 hours after the end of the interview and supplemented and modified in combination with the notes of on-site observation [ 21 ] .
Data analysis
This study was conducted by 2 researchers (Jiamengying Chen, Xiaojie Li) using the Colaizzi seven-step method of phenomenological research to guide the data analysis. The 2 researchers independently and repeatedly listened to the audio recordings of the interviews, verified the content, and ultimately analysed the data separately.
During the study, the researcher verified unclear statements in the recordings by contacting the respondent via WeChat or telephone. In addition, the transcribed notes and the themes generated from the analysis were confirmed with the interviewees to ensure that their views were authentically recorded. After the information was completed for thematic extraction and coding, the research team held 1 team meeting to review it. All the researchers commented on and ultimately agreed on the themes and coding of the interviews.
Participant characteristics
Fourteen elderly patients with atherosclerotic vascular disease, with an average age of 75 years, were included in the study. Five participants were male, and 9 participants were female. The disease categories included coronary atherosclerotic heart disease, cerebral infarction, and carotid atherosclerotic plaque. Participant information is shown in Table 1 .
The results of this study show the acceptability of the current dietary status, the understanding of previous nutritional assistance, and the methods of future nutritional assistance in elderly patients with AS-related diseases in western China. The following 3 themes emerged from this study: (1) the diet with regional characteristics; (2) low nutrition-related health literacy; (3) complex attitudes towards nutritional assistance.
The diet with regional characteristics
In terms of staple food preferences, most of the elderly people included in this study claimed that they consumed rice vermicelli for breakfast and lunch because it is “easily digestible” (P3, female, 71 years old). They liked to add animal fats when eating rice vermicelli or noodles (especially ChangWang noodles from Guizhou, China), even if they knew that animal fats can be harmful to the body. These animal fats included solid animal fats and fried animal fats (known as CuiShao) to increase the flavour of the food. Another common breakfast choice among these participants was steamed glutinous rice with chili oil, soy sauce and a variety of side dishes, including “CuiShao”, bacon or sausage, fried peanuts and so on. The family members met the participants’ requests and provided them with this type of food.
“I eat either rice vermicelli or ChangWang noodles every morning. Sometimes (I) do not want to go downstairs, and I let my son or daughter bring it back to me. I think ChangWang noodles need a lot of “CuiShao” to be delicious.”
(P14; Male, 73 years old)
Some participants also said that they were not keen on eating refined rice products or noodles but preferred coarse grains, mainly including “corns, sweet potatoes, and potatoes, because this state produces potatoes” (P8; Female, 66 year old). The discussed cooking methods for the potatoes mainly including frying, fire baking and stir-frying.
“I liked to eat potatoes when I was young, and I also like to eat them now. When I was younger, I would bake my potatoes, but now I prefer fried potatoes.”
(P12; Male, 81 year old)
Some male participants favoured alcohol. They mainly consumed Chinese Baijiu, but all of them reduced their alcohol consumption after learning that they suffered from AS-related diseases. Female participants widely mentioned that they would like to drink Chinese rice wine (Mijiu) (especially homemade) rather than Chinese Baijiu and considered Chinese rice wine (Mijiu) consumption a habit that “everyone in Guizhou should have” (P9; Female, 83 year old).
“I used to drink at least 100 ml of Chinese baijiu; after learning that I was sick, I quit drinking.”
(P13; Male, 64 year old)
Most participants believed that their dietary intake was healthy, while some participants said that after the diagnosis of AS-related diseases, they consciously chose to eat more vegetarian foods, such as ‘Suguadou’, a specialty of Guizhou Province, China, and avoid consuming animal fats.
“After I got sick, I gained some knowledge from the newspaper and TV. It was said that eating a vegetarian diet is good for my health. [Now] I eat a vegetarian diet and do not eat chicken, duck or fish.”
(P2; Female, 61 year old)
Other participants said that they liked and frequently ate “red sour soup”, a Chinese Guizhou specialty, 2 to 3 times a week, or even more frequently. They cooked “red sour soup” in dishes by adding water or soup stock and boiled freshwater fish, lean meat and vegetables. They expressed their preference for ethnic-specific eating habits, and even if they chose to eat out, they would more frequently choose restaurants that sell “red sour soup” because “fish is easy to digest for elderly individuals, so we eat fish in sour soup at restaurants, and we like that too” (P13; Male, 64 year old). Some participants expressed their recognition of the simple cooking method of “red sour soup”. Many participants mentioned their decreasing food intake after entering old age, and they indicated that “I cannot eat much, and they say that the amount of one meal I eat is equal to the amount of one meal that a cat eats” (P4; Female, 77 year old), emphasizing “You need to eat something sour to get an appetite” (P3; Female, 71 year old).
“People in Guizhou should eat red sour soup; I have to eat it several times a week.”
(P11; Male, 82 year old)
For the intake of fruit, many participants thought that fruit consumption was a treat because their family or caregivers did not allow them to eat too much other food outside of dinner, and being provided with fruit could make them feel happy. “They did not allow me to eat too much fruit, and every time I ate fruit, they were worried that my blood sugar would rise” (P1; Female, 90 year old). The participants usually actively discussed their preferences for fruits, including buying their favourite fruits at the market or asking their caregivers to provide some fruits. Some participants mentioned that they liked to drink rosa roxburghii Tratt (RRT) juice or directly ate sliced fresh RRT for “vitamin C supplementation” (P9; Female, 83 year old).
“This plant [RRT] was widely cultivated in my hometown, and when it was ripe, we picked the fruit and ate it. It became a habit!”
(P7; Male, 80 year old)
Low nutrition-related health literacy
Most of the participants did not receive professional nutritionist consulting services and did not know that the hospital had nutrition-related departments. Some participants mentioned that when visiting a hospital, doctors or nurses mentioned diet-related knowledge, such as avoiding a greasy diet and not eating animal fats, but rarely explained the reasons.
“Nutrition department? The hospital has this department?” I do not know what to eat, so the doctor told me, ‘eat less oil and less salt.’ However, he did not tell me why”.
(P3; Female, 71 year old)
The majority of participants stated that they could use the internet to gain much knowledge about healthy eating patterns. In addition to professional notification, participants also obtained diet-related knowledge through newspapers, television, online short video publicity, family notification, etc. “(I) watched many of these kinds of videos on my telephone” (P5; Female, 62 year old). However, they had no way to tell whether the information was correct These information sources contained contradictory content, which made participants unable to distinguish the correctness of the information. Other participants said that they could not learn diet-related knowledge through commonly used health education methods, such as public accounts, videos, and brochures, in tertiary hospitals due to the degradation of vision and hearing caused by age.
“I’m old, my eyesight is poor, and I cannot see with my glasses! I also want to read the brochure [on nutrition], but I cannot see it clearly”.
Most participants could list the relevant nutritional knowledge they knew, and they also performed a small number of healthy eating behaviours, such as the most basic behaviours: quitting smoking and drinking. They believed that the implementation of a healthy diet contributes to recovery from the diseases.
“I stopped smoking or drinking after I got sick! I know that these [cigarettes, alcohol] are not good for the body” .
Some participants blindly implemented diet-related knowledge after acquiring it. These participants believed that consuming dietary supplements can ensure good health, so visiting medical institutions was unnecessary. They thought that the greater the intake of dietary supplements, the better the body they would have, even if their health might be harmed by excessive intake.
“I hardly go to the hospital because I eat a lot of health supplements; my body is fine, and I am fine”.
(P8; Female, 66 year old).
Although in medical institutions, participants received health education on diet-related knowledge, not all patients were able to effectively implement the information. Some patients were not willing to implement the recommended healthy eating patterns, and they did not want to change their preferences. The participants had different understandings of healthy eating patterns. Some participants were aware of systematic dietary patterns that they described as “good” but “difficult to implement” (P2; Female, 61 year old). Others described these eating patterns as “unpalatable”. A common view is that the ingredients of these dietary patterns are difficult or inaccessible to them.
“No, no, [they want me to] eat so many vegetables, like I am a rabbit! I have maintained my eating habits for so many years and cannot change them. These diets are weird; I do not eat avocados, I do not eat oats. If I can live to be a hundred years old if I eat these things, then I would rather die at age eighty”.
(P1; Female, 90 year old)
In addition, many participants said that doctors and nurses could not monitor whether they consumed a healthy diet after leaving hospitals. It is difficult to follow a healthy diet after discharge, especially when most patients and their families do not have a medical background.
“After I was discharged from the hospital, they [the doctors and nurses] did not know what I was eating at home. Doctors and nurses are very busy with work; how can there be time to help us with our eating?”
Complex attitudes towards nutritional assistance
Participants generally expressed fear of diseases. They said, “This disease will stay with me for the rest of my life, and I cannot cure it” (P12; Male, 81 year old). These participants elaborated on their desire to become healthier through nutritional assistance, and they also tended to be more willing to receive dietary-related guidance and assistance and viewed the role of nutritional assistance in delaying the development of AS positively. Personalized nutritional assistance received a positive response from the participants, and they were willing to try nutritional assistance that would help them.
“I dare not to do anything when I suffer from this disease because I fear that something will happen to my blood vessels..... Of course, it is good to be able to eat healthier; people live to eat three meals a day. If the meal tastes good and the body can be healthy, then I will wake up laughing in my dreams” .
The vast majority of participants expressed their willingness to use customized recipes, diet lists, etc., but the implementation process required the understanding and support of their families. Two male participants said that “My wife is the head of the family”, and whether to use custom recipes and diet lists required the cooperation and consent of his wife. Other patients said that because they are old, whether they could cook according to the recipe required the cooperation of their sons and daughters or caregivers (paid by the elderly individuals themselves or their families).
“We are all old and need help with daily activities such as eating and dressing. Some things require children’s help to achieve”.
(P6; Female, 81 year old)
Some participants were not very skilled in the operation of electronic devices such as telephone, computers, or televisions. They also suffered from diseases that caused them to be unable to use communication devices such as telephone. Therefore, they could not receive online health education. They only accepted one-to-one or one-to-many nutritional assistance methods that were held offline. However, some participants mentioned that they would selectively adopt the nutritional recommendations made in the meetings for the public because “not all of them suit me” (P1, female, 90 years old). Other participants suggested that they prefer to use remote online methods for meetings because they “do not have the time or energy to attend the meeting, and it is not safe if the meeting place is far away” (P7; Male, 80 year old); they were worried about traffic safety between hospitals and therefore could not attend the meetings.
“I am old, and I have no idea how to use telephone or computers for online meetings. So, I prefer offline meetings where we do whatever the doctors and nurses say” .
(P14; Male, 73 year old).
Some participants were more likely to take dietary supplements such as vitamins rather than considering other forms of nutritional assistance first. Other participants had their own views on dietary supplements; they might try to consume fresh or “medicinal” (P1; Female, 90 year old) ingredients instead of the dietary supplements prescribed by their doctors. Due to the severity of AS-related diseases, these participants were willing to receive various forms of nutritional assistance. Other participants expressed that they had too much concern and distrust regarding the use of dietary supplements. Some participants were worried about the interaction between dietary supplements and the drug treatment they were currently receiving, while other participants thought that were already using too many oral drugs, and whether dietary supplements were useful was uncertain.
“There are a lot of bad people [selling dietary supplements] now, and it is hard to identify who is good and who is bad”.
Some participants showed the opposite attitude towards nutritional assistance; they believed that they were old enough to receive intervention for their diet. Regarding the malignant cardiovascular events, cerebrovascular events, and amputations that could result from AS-related diseases, these participants stated that they “did not know and did not understand how it could be so serious” (P9; Female, 83 year old).
“I’m so old, I should eat what I want to eat” .
Most of the participants expressed their willingness to try nutritional assistance measures, which were considered beneficial for delaying the development of AS, including medical-nursing combined institutions that could provide them with a diet, but those facilities put forwards higher requirements on the price and quality of the meals. If they did not meet the requirements, they would not choose this nutritional assistance measure.
“The community should do something practical for us old people. We will eat what is good, and we do not eat what is bad”.
Some participants said they were concerned about the price of the diet provided by the medical-nursing combined institutions and were worried about their economic situation. When their income was not enough to pay for the diet provided by the medical and nursing institutions, they would not choose this method. Less income had taken away their freedom of consumption.
“We are all rural people, we have no income, and the cost of eating out is equal to the cost of a few days of our daily life..... If the food is very expensive, we will definitely be unwilling to eat it” .
The results of this study showed the acceptability of the current dietary status, the understanding of previous nutritional assistance, and the methods of future nutritional assistance in elderly patients with AS-related diseases in western China. The theme generated in this study shows that the factors affecting dietary status are multifaceted and complex, and the participants’ dietary preferences had obvious regional characteristics.
The first theme generated by this qualitative research is that the diet with regional characteristics. In this topic, we explored the relationship between participants and their food choices. We found that the participants’ diets had strong regional characteristics, reflecting the regional characteristics of the provinces in western China. The diagnosis of AS-related diseases resulted in some patients changing their eating habits, following the health education of doctors or nurses and choosing to limit alcohol consumption and eat more vegetables. For other participants, there were some difficulties in adhering to healthy eating habits; for example, the tastes and dietary preferences formed during perennial life are difficult to change. The second theme was centred on the implementation of nutritional assistance by participants. We measured participants’ understanding and implantation of knowledge about a healthy diet, which reflected their general misunderstanding of healthy diet knowledge. The third theme was that attitudes towards nutritional assistance were complex; we summarized the participants’ attitudes towards a variety of nutritional assistance approaches. Research has shown that most participants were welcoming and receptive to nutritional assistance, but other patients expressed a resistant attitude. Some participants highlighted their concerns about the price of food.
The participants discussed their current dietary intake with the researchers. In this component of the study, the participants’ dietary preferences showed obvious regionality. This study showed that the mainstream staple food choices for elderly patients with AS-related diseases in western China include rice (including refined rice and its products), glutinous rice, and some coarse grains, such as potatoes and corn. Such staple food choices were suitable for local geographical conditions but might adversely affect the health of participants. Rice products, such as rice vermicelli, were one of the main food choices that participants were interested in. They often mentioned mutton rice vermicelli, beef rice vermicelli, chili chicken rice vermicelli and so on. Most commonly, rice vermicelli and noodles were cooked in boiling water and then put into seasoned broth. Studies have shown that cooked rice flour is a moderate-GI food [ 22 ], and a higher GI index has been shown to be significantly associated with an increased risk of CVD [ 23 ]. Postprandial hyperglycaemia can lead to elevated triglycerides and increased oxidative stress, which have a negative impact on the vascular endothelium [ 24 ].
The participants often mentioned “Cuishao”, bacon, sausage, and fried peanuts. Cuishao is a unique snack and was popular among people living in Guizhou Province, China. Pork (i.e., pork belly meat with more adipose tissue mixed with lean meat) was used as the raw material, and seasonings were added to marinate and then fry the meat. The fried “Cuishao” contained a large amount of oil. Excessive intake of oil can cause a variety of adverse effects on health and may lead to a greater risk of disease, including hypertension, AS and cancer [ 25 ]. During the frying process, a series of chemical reactions, such as the oil oxidation reaction, Maillard reaction and oxidative degradation of proteins, occur in the matrix of fried meat products. These chemical reactions lead to the production of harmful substances, such as trans fatty acids (TFAs), in fried meat products [ 26 ]. Studies have shown that excessive intake of TFAs promotes vascular inflammation and oxidative stress and accelerates the development of AS [ 27 ]. Numerous academic organizations have recommended that the intake of saturated fatty acids and TFAs should be limited to regulate blood lipid levels in high-risk populations [ 28 ]. Importantly, even though the potatoes that people in western China like to eat are a good source of carbohydrates [ 29 ], the frying cooking method leads to an increase in the risk of noninfectious diseases such as CVD and diabetes by affecting inflammatory factors and vascular endothelial function [ 30 ]. This showed that when designing a diet plan for patients with AS-related diseases in western China, the patients should be asked to limit their intake of fried, high-fat foods, even if they like to eat these foods.
Most participants took the initiative to adjust their diet after being diagnosed with the disease. Some participants indicated that they had actively chosen a vegetarian diet or consciously tended to eat vegetables and fruits. People in western China often use boiled water to cook vegetables when they choose to eat vegetables and form a local characteristic dish, “Suguadou”. Commonly consumed vegetable types included kidney beans, immature pumpkin. Studies have shown that the choice of cooking method is related to cardiovascular risk factors. In addition to raw food, boiling is also a healthier cooking method, which is related to healthier cardiovascular conditions [ 31 ]. Boiled cooking methods could also better retain antioxidant compounds in vegetables. We found that people in western China like to eat a seasonal fruit called RRT in summer. This fruit is a medicinal plant and traditional food in western China. In recent years, studies have shown that RRT is rich in vitamin C [ 32 ]. The presence of other substances (organic acids, flavonoids, polyphenols, etc.) can improve dyslipidaemia through the intestinal flora [ 33 ]. Therefore, eating RRT or drinking freshly squeezed fruit juice might improve AS-related diseases.
In addition, people in western China were also keen to eat “red sour soup”. “Red sour soup” is a common fermented seasoning in Guizhou Province, China. It is mainly fermented with “Maolaguo”, red peppers, etc., followed by the addition of Litsea cubeba fruit essential oil [ 34 ]. People often use “red sour soup” to cook vegetables, lean meat slices, fish slices and so on. Studies have shown that “red sour soup” can alleviate nonalcoholic fatty liver disease induced by a high-fat diet in rats and reduce body mass index, total cholesterol, triglyceride, and insulin resistance [ 35 ]. According to a study by Yang et al. [ 36 ], red sour soup can prevent and treat hyperlipidaemia in obese rats by regulating the AMPK signalling pathway, which might be related to the antioxidant and anti-atherosclerotic effects of lycopene and capsaicin, which are abundant among the red sour soup raw materials [ 37 ].
Studies have shown that the fermentation process of red sour soup will produce beneficial bacteria such as Lactobacilli, Acetobacter , and Leuconostoc and acid substances such as lactic acid, acetic acid and citric acid [ 38 ]. These acids regulate inflammation and promote immunity, neuroprotection, and anti-ageing activity [ 39 ]. However, the impact of food as a whole on the health of organisms rather than the impact of a single component of food [ 40 ] should be noted. Therefore, it is necessary to comprehensively consider the impact of red sour soup on human health; that is, the beneficial effects of red sour soup on human health are due to its rich bioactive substances and beneficial components produced during fermentation.
Notably, some male participants mentioned frequent consumption of alcohol. Studies have shown that higher alcohol intake increases the risk of CVD mortality in Chinese men and that alcohol intake does not have a protective effect on CVD [ 41 ]. Although participants might reduce or stop consuming alcohol after the diagnosis of AS-related diseases, past studies have shown that patients who continue to drink alcohol have a similar risk of death to those who have quit [ 42 ]. This suggested that the harm caused to the human body by alcohol consumption is permanent, even if the patient has chosen to quit drinking alcohol.
This study revealed that participants generally lack healthy eating knowledge. Research has shown that among participants, there is a widespread bias towards certain types of food and a misconception regarding nutritional assistance. A survey of elderly individuals [ 43 ] revealed similar findings; for example, some participants believed that “thin” is healthy and “fat” is unhealthy, and they believed that fat, sugar, etc., are “bad” foods and prefer vegetarian food [ 44 ]. However, studies have shown that proper fat intake is beneficial to human health, and people should consume a certain amount of high-quality fat and reduce saturated fat intake [ 45 ]. The intake of omega-3 fatty acids had some benefits for participants with cardiovascular and cerebrovascular diseases [ 46 ]. Many studies have shown that a plant-based diet can promote vascular endothelial protection and reduce the generation of harmful factors in endothelial cells, which is beneficial for treating AS-related diseases [ 47 ]. A meta-analysis of 55 studies showed that compared to other eating patterns, plant-based diets and whole-grain foods are associated with better prevention of coronary heart disease and multiple metabolic diseases [ 48 ]. However, it is worth noting that even though plant-based diets have been shown to be beneficial to human health, all dietary patterns are associated with potential nutritional risks [ 49 ]. Studies have shown that long-term intake of a vegan diet may lead to a lack of micronutrients, resulting in potential nutritional risks [ 50 ]. Therefore, for elderly patients with AS-related diseases, dietary guidance should include prompting patients to choose a balanced diet, consuming abundant plant-based foods, and correcting their misunderstanding regarding their current dietary patterns.
In contrast, there were also some participants who had received relevant health education, but the information provided by the internet may conflict with it, making it difficult for them to consume a healthy diet. Numerous studies have shown that the quality of health-related information that patients can learn on the internet is mixed [ 51 ]. Many sources of information were nonprofessionals who had not received medical professional training, which leads to mixed and inaccurate or biased information that may mislead patients and even have a negative impact on their health [ 52 ]. However, even if there was erroneous or unconfirmed information, viewing internet videos was still a popular method of health education for patients. Health education, in which professional people use networks, can significantly improve patients’ compliance behaviour and reduce costs [ 53 ]. However, in this survey, some participants were unable to obtain health knowledge by reading or watching videos because of old age, illness or disability. At the same time, some participants suggested that after leaving the medical environment, doctors or nurses could not guide and supervise their diet, which led them to collect relevant health knowledge in other ways, and their compliance behaviour gradually decreased over time. Doctors or nurses should carry out continuous and personalized health education for patients. Notably, only providing advice on improving diet and activity behaviours is not enough to change and maintain these behaviours in the long run. Effective health education that supports behavioural changes requires effective incentives and promotion, including environmental support [ 54 ], and provides patients with intervention methods suitable for their culture, age and other characteristics [ 55 ].
The majority of participants accepted nutritional assistance. Our survey showed that elderly participants with AS-related diseases need personalized nutritional assistance to improve their physical condition. In addition to the need for nutritional assistance, they also need corresponding dietary support from the government or institutions because the diseases limits their physical movement [ 56 ]. At the same time, because of the decline in functional living ability, many participants showed dependence on their families. This finding was consistent with most studies [ 57 ]. With the widespread promotion of medical-nursing combinations in China, meals are increasingly being prepared by medical-nursing combined institutions rather than by the patients themselves, community health service institutions, etc., to improve diet quality. Based on the patient interviews, we found that the nutritional assistance provided by medical-nursing combined institutions may be more suitable for and accepted by elderly patients with AS-related diseases. Medical-nursing combined institutions could help elderly people with full and partial disability to solve the problems of meals, medical treatment and self-care at a lower cost. In some European and American countries, there have been similar nutritional assistance models for elderly people, but most of them involve modelled nutrition management, such as communities providing three meals a day to elderly people in the form of meal boxes. However, this intervention model cannot be used for personalized service [ 58 ].
In contrast, some participants thought that they did not need to receive nutritional assistance. They held the mentality of ‘being so old’ and had a resistant and unacceptable attitude towards nutritional assistance. This might be because they think they were old enough to no longer have to put much effort into fighting the death caused by the diseases. This study revealed that elderly people with increasing age are becoming increasingly more deeply aware of the limitations of their lives. They could accept death as an inevitable event and reduce their avoidance of death [ 59 ]. However, it should be noted that the participants’ lack of healthy diet knowledge may have led them to mistakenly believe that diet cannot significantly improve the clinical manifestations of AS-related diseases, so they still maintain unhealthy eating habits and refuse to perform healthy lifestyles. Moreover, these participants might underestimate the consequences of poor lifestyles, resulting in serious cardiovascular events, including vascular obstruction and vascular rupture. These conditions might lead to paralysis, dysphagia and other symptoms, which would result in reduced or even loss of self-care ability and a significant reduction in quality of life [ 60 ].
This study has several limitations. The research team tried to recruit participants with heterogeneous characteristics, including age, sex, family status, and education level. However, due to the purposive sampling method, the results of this study may not be extended to the wider Chinese or international population of elderly patients with coronary and other atherosclerotic vascular diseases. This study excluded individuals who did not speak Chinese. Therefore, we cannot determine whether the samples of this study included multicultural or multiethnic groups.
This study showed that elderly patients with coronary and other atherosclerotic vascular diseases who are living in western China have regional dietary preferences, which may have a certain impact on their disease development. They have different views due to differences in sex, disease status, personal habits, and modes of receiving dietary knowledge. These views are mainly regarding their own dietary status, cooking behaviours, and dietary management models. Regional and individual differences may influence the effects of diet management. In the future, for research regarding the dietary management of elderly patients with coronary and other atherosclerotic vascular diseases in western China, researchers should conduct personalized and sex-specific dietary management interventions according to their regional dietary preferences and consider whether individual patients are able to receive relevant nutritional assistance. Medical and nursing combination institutions can provide them with modelled nutrition management, such as providing three meals in the form of lunch boxes or open canteens. They can also use a variety of methods, such as face-to-face conversations and meetings, to provide them with dietary advice and flexibly use the internet to achieve online intervention. Changes in dietary behaviour may have a positive impact on the overall dietary quality of this population and may improve the patient’s disease status and prognosis.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due ethical reasons but are available from the corresponding author on reasonable request.
Abbreviations
- Atherosclerosis
Cardiovascular Disease
rosa roxburghii Tratt
Tras Fatty Acid
Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16(4):203–12. https://doi.org/10.1038/s41569-018-0119-4 .
Article PubMed Google Scholar
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010 . GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group.
Article PubMed PubMed Central Google Scholar
Li Y, Wang DD, Ley SH, Howard AG, He Y, Lu Y, et al. Potential Impact of Time Trend of Life-Style Factors on Cardiovascular Disease Burden in China. J Am Coll Cardiol. 2016;68(8):818–33. https://doi.org/10.1016/j.jacc.2016.06.011 .
Meier T, Grafe K, Senn F, Sur P, Stangl GI, Dawczynski C, et al. Cardiovascular mortality attributable to dietary risk factors in 51 countries in the WHO European Region from 1990 to 2016: a systematic analysis of the Global Burden of Disease Study. Eur J Epidemiol. 2019;34(1):37–55. https://doi.org/10.1007/s10654-018-0473-x .
Bush RL, Kallen MA, Liles DR, Bates JT, Petersen LA. Knowledge and awareness of peripheral vascular disease are poor among women at risk for cardiovascular disease. J Surg Res. 2008;145(2):313–9. https://doi.org/10.1016/j.jss.2007.03.022 .
Tzoulaki I, Elliott P, Kontis V, Ezzati M. Worldwide Exposures to Cardiovascular Risk Factors and Associated Health Effects: Current Knowledge and Data Gaps. Circulation. 2016;133(23):2314–33. https://doi.org/10.1161/CIRCULATIONAHA.115.008718 .
Zhai FY, SF D, Wang ZH, Zhang JG, WW D, Popkin BM. Dynamics of the Chinese diet and the role of urbanicity, 1991-2011. Obes Rev. 2014;15 Suppl 1(0 1):16–26. https://doi.org/10.1111/obr.12124 .
Bu T, Tang D, Liu Y, Chen D. Trends in Dietary Patterns and Diet-related Behaviors in China. Am J Health Behav. 2021;45(2):371–83. https://doi.org/10.5993/AJHB.45.2.15 .
Li S, Liu Z, Joseph P, Hu B, Yin L, Tse LA, et al. Modifiable risk factors associated with cardiovascular disease and mortality in China: a PURE substudy. Eur Heart J. 2022;43(30):2852–63. https://doi.org/10.1093/eurheartj/ehac268 .
Liu H, Lin W, Tu K, Zhou Q, Wang C, Sun M, et al. Prevalence, awareness, treatment, and risk factor control of high atherosclerotic cardiovascular disease risk in Guangzhou. China Front Cardiovasc Med. 2023;10:1092058. https://doi.org/10.3389/fcvm.2023.1092058 .
Article CAS PubMed Google Scholar
Kohler AK, Jaarsma T, Tingstrom P, Nilsson S. The effect of problem-based learning after coronary heart disease - a randomised study in primary health care (COR-PRIM). BMC Cardiovasc Disord. 2020;20(1):370. https://doi.org/10.1186/s12872-020-01647-2 .
Anto L, Blesso CN. Interplay between diet, the gut microbiome, and atherosclerosis: Role of dysbiosis and microbial metabolites on inflammation and disordered lipid metabolism. J Nutr Biochem. 2022;105:108991. https://doi.org/10.1016/j.jnutbio.2022.108991 .
Mateo-Gallego R, Uzhova I, Moreno-Franco B, Leon-Latre M, Casasnovas JA, Laclaustra M, et al. Adherence to a Mediterranean diet is associated with the presence and extension of atherosclerotic plaques in middle-aged asymptomatic adults: The Aragon Workers’ Health Study. J Clin Lipidol. 2017;11(6):1372-1382.e4. https://doi.org/10.1016/j.jacl.2017.08.007 .
Assies JM, Saltz MD, Peters F, Behrendt CA, Jagodzinski A, Petersen EL, et al. Cross-Sectional Association of Dietary Patterns and Supplement Intake with Presence and Gray-Scale Median of Carotid Plaques-A Comparison between Women and Men in the Population-Based Hamburg City Health Study. Nutrients. 2023;15(6). https://doi.org/10.3390/nu15061468 .
Andreae C, Tingstrom P, Nilsson S, Jaarsma T, Karlsson N, Karner KA. Does problem-based learning improve patient empowerment and cardiac risk factors in patients with coronary heart disease in a Swedish primary care setting? A long-term prospective, randomised, parallel single randomised trial (COR-PRIM). BMJ Open. 2023;13(2):e065230. https://doi.org/10.1136/bmjopen-2022-065230 .
Kodapally B, Vilane Z, Nsamba J, Joseph A, Mathews E, Thankappan KR. The suitability, acceptability, and feasibility of a culturally contextualized low-calorie diet among women at high risk for diabetes mellitus in Kerala: a mixed-methods study. Int J Diabetes Dev Ctries. 2022:1–16. https://doi.org/10.1007/s13410-022-01134-8 .
Marcelin JR, Siraj DS, Victor R, Kotadia S, Maldonado YA. The Impact of Unconscious Bias in Healthcare: How to Recognize and Mitigate It. J Infect Dis. 2019;220(220 Suppl 2):S62–73. https://doi.org/10.1093/infdis/jiz214 .
Xiao S, Chen Z, Mai T, Cai J, Chen Y, Tang X, et al. Analysis of the association between dietary patterns and nonalcoholic fatty liver disease in a county in Guangxi. BMC Gastroenterol. 2023;23(1):309. https://doi.org/10.1186/s12876-023-02864-7 .
Smith SJ, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58(23):2432–46. https://doi.org/10.1016/j.jacc.2011.10.824 .
Lin LC. Data management and security in qualitative research. Dimens Crit Care Nurs. 2009;28(3):132–7. https://doi.org/10.1097/DCC.0b013e31819aeff6 .
Saddler D. The qualitative research methodology. Gastroenterol Nurs. 2008;31(1):72–4. https://doi.org/10.1097/01.SGA.0000310941.15541.f8 .
Chen YJ, Sun FH, Wong SH, Huang YJ. Glycemic index and glycemic load of selected Chinese traditional foods. World J Gastroenterol. 2010;16(12):1512–7. https://doi.org/10.3748/wjg.v16.i12.1512 .
Article CAS PubMed PubMed Central Google Scholar
Ma XY, Liu JP, Song ZY. Glycemic load, glycemic index and risk of cardiovascular diseases: meta-analyses of prospective studies. Atherosclerosis. 2012;223(2):491–6. https://doi.org/10.1016/j.atherosclerosis.2012.05.028 .
Dickinson S, Brand-Miller J. Glycemic index, postprandial glycemia and cardiovascular disease. Curr Opin Lipidol. 2005;16(1):69–75. https://doi.org/10.1097/00041433-200502000-00012 .
Grootveld M, Addis PB, Le Gresley A. Editorial: Dietary Lipid Oxidation and Fried Food Toxicology. Front Nutr. 2022;9:858063. https://doi.org/10.3389/fnut.2022.858063 .
Nie W, Cai K, Li Y, Tu Z, Hu B, Zhou C, et al. Study of polycyclic aromatic hydrocarbons generated from fatty acids by a model system. J Sci Food Agric. 2019;99(7):3548–54. https://doi.org/10.1002/jsfa.9575 .
Hirata Y. trans-Fatty Acids as an Enhancer of Inflammation and Cell Death: Molecular Basis for Their Pathological Actions. Biol Pharm Bull. 2021;44(10):1349–56. https://doi.org/10.1248/bpb.b21-00449 .
Wojda A, Janczy A, Malgorzewicz S. Mediterranean, vegetarian and vegan diets as practical outtakes of EAS and ACC/AHA recommendations for lowering lipid profile. Acta Biochim Pol. 2021;68(1):41–8. https://doi.org/10.18388/abp.2020_5515 .
Moser S, Aragon I, Furrer A, Van Klinken JW, Kaczmarczyk M, Lee BH, et al. Potato phenolics impact starch digestion and glucose transport in model systems but translation to phenolic rich potato chips results in only modest modification of glycemic response in humans. Nutr Res. 2018;52:57–70. https://doi.org/10.1016/j.nutres.2018.02.001 .
Halton TL, Willett WC, Liu S, Manson JE, Stampfer MJ, Hu FB. Potato and french fry consumption and risk of type 2 diabetes in women. Am J Clin Nutr. 2006;83(2):284–90. https://doi.org/10.1093/ajcn/83.2.284 .
Rodriguez-Ayala M, Sandoval-Insausti H, Bayan-Bravo A, Banegas JR, Donat-Vargas C, Ortola R, et al. Cooking Methods and Their Relationship with Anthropometrics and Cardiovascular Risk Factors among Older Spanish Adults. Nutrients. 2022;14(16). https://doi.org/10.3390/nu14163426 .
Wang LT, Lv MJ, An JY, Fan XH, Dong MZ, Zhang SD, et al. Botanical characteristics, phytochemistry and related biological activities of Rosa roxburghii Tratt fruit, and its potential use in functional foods: a review. Food Funct. 2021;12(4):1432–51. https://doi.org/10.1039/d0fo02603d .
Ji J, Zhang S, Yuan M, Zhang M, Tang L, Wang P, et al. Fermented Rosa Roxburghii Tratt Juice Alleviates High-Fat Diet-Induced Hyperlipidemia in Rats by Modulating Gut Microbiota and Metabolites. Front Pharmacol. 2022;13:883629. https://doi.org/10.3389/fphar.2022.883629 .
Lin LJ, Zeng J, Tian QM, Ding XQ, Zhang XY, Gao XY. Effect of the bacterial community on the volatile flavour profile of a Chinese fermented condiment - Red sour soup - During fermentation. Food Res Int. 2022;155:111059. https://doi.org/10.1016/j.foodres.2022.111059 .
Cong S, Li Z, Yu L, Liu Y, Hu Y, Bi Y, et al. Integrative proteomic and lipidomic analysis of Kaili Sour Soup-mediated attenuation of high-fat diet-induced nonalcoholic fatty liver disease in a rat model. Nutr Metab (Lond). 2021;18(1):26. https://doi.org/10.1186/s12986-021-00553-4 .
Yang H, Xie J, Wang N, Zhou Q, Lu Y, Qu Z, et al. Effects of Miao sour soup on hyperlipidemia in high-fat diet-induced obese rats via the AMPK signaling pathway. Food Sci Nutr. 2021;9(8):4266–77. https://doi.org/10.1002/fsn3.2394 .
Gomez-Sierra T, Eugenio-Perez D, Sanchez-Chinchillas A, Pedraza-Chaverri J. Role of food-derived antioxidants against cisplatin induced-nephrotoxicity. Food Chem Toxicol. 2018;120:230–42. https://doi.org/10.1016/j.fct.2018.07.018 .
Zhou Q, Qu Z, Wang N, Liu H, Yang H, Wang H. Miao sour soup influences serum lipid via regulation of high-fat diet-induced intestinal flora in obese rats. Food Sci Nutr. 2023;11(5):2232–42. https://doi.org/10.1002/fsn3.3136 .
Maruta H, Abe R, Yamashita H. Effect of Long-Term Supplementation with Acetic Acid on the Skeletal Muscle of Aging Sprague Dawley Rats. Int J Mol Sci. 2022;23(9). https://doi.org/10.3390/ijms23094691 .
Braconi D, Bernardini G, Millucci L, Santucci A. Foodomics for human health: current status and perspectives. Expert Rev Proteomics. 2018;15(2):153–64. https://doi.org/10.1080/14789450.2018.1421072 .
Millwood IY, Im PK, Bennett D, Hariri P, Yang L, H D, et al. Alcohol intake and cause-specific mortality: conventional and genetic evidence in a prospective cohort study of 512 000 adults in China. Lancet Public Health. 2023;8(12):e956–67. https://doi.org/10.1016/S2468-2667(23)00217-7 . China Kadoorie Biobank Collaborative Group.
Ding C, O’Neill D, Britton A. Trajectories of alcohol consumption in relation to all-cause mortality in patients with cardiovascular disease: a 35-year prospective cohort study. Addiction. 2022;117(7):1920–30. https://doi.org/10.1111/add.15850 .
Avgerinou C, Bhanu C, Walters K, Croker H, Liljas A, Rea J, et al. Exploring the views and dietary practices of older people at risk of malnutrition and their carers: a qualitative study. Nutrients. 2019;11(6). https://doi.org/10.3390/nu11061281 .
Lawrence GD. Dietary fats and health: dietary recommendations in the context of scientific evidence. Adv Nutr. 2013;4(3):294–302. https://doi.org/10.3945/an.113.003657 .
Sacks FM, Lichtenstein AH, Wu J, Appel LJ, Creager MA, Kris-Etherton PM, et al. Dietary Fats and Cardiovascular Disease: A Presidential Advisory From the American Heart Association. Circulation. 2017;136(3):e1–23. https://doi.org/10.1161/CIR.0000000000000510 . American Heart Association.
Shahidi F, Ambigaipalan P. Omega-3 Polyunsaturated Fatty Acids and Their Health Benefits. Annu Rev Food Sci Technol. 2018;9:345–81. https://doi.org/10.1146/annurev-food-111317-095850 .
Tuso P, Stoll SR, Li WW. A plant-based diet, atherogenesis, and coronary artery disease prevention. Perm J. 2015;19(1):62–7. https://doi.org/10.7812/TPP/14-036 .
Mehta P, Tawfeeq S, Padte S, Sunasra R, Desai H, Surani S, et al. Plant-based diet and its effect on coronary artery disease: A narrative review. World J Clin Cases. 2023;11(20):4752–62. https://doi.org/10.12998/wjcc.v11.i20.4752 .
Neufingerl N, Eilander A. Nutrient Intake and Status in Adults Consuming Plant-Based Diets Compared to Meat-Eaters: A Systematic Review. Nutrients. 2021;14(1). https://doi.org/10.3390/nu14010029 .
Bakaloudi DR, Halloran A, Rippin HL, Oikonomidou AC, Dardavesis TI, Williams J, et al. Intake and adequacy of the vegan diet. A systematic review of the evidence. Clin Nutr. 2021;40(5):3503–21. https://doi.org/10.1016/j.clnu.2020.11.035 .
He Z, Wang Z, Song Y, Liu Y, Kang L, Fang X, et al. The Reliability and Quality of Short Videos as a Source of Dietary Guidance for Inflammatory Bowel Disease: Cross-sectional Study. J Med Internet Res. 2023;25:e41518. https://doi.org/10.2196/41518 .
Fortinsky KJ, Fournier MR, Benchimol EI. Internet and electronic resources for inflammatory bowel disease: a primer for providers and patients. Inflamm Bowel Dis. 2012;18(6):1156–63. https://doi.org/10.1002/ibd.22834 .
Heida A, Dijkstra A, Muller KA, Rossen JW, Kindermann A, Kokke F, et al. Efficacy of home telemonitoring versus conventional follow-up: a randomized controlled trial among teenagers with inflammatory bowel disease. J Crohns Colitis. 2018;12(4):432–41. https://doi.org/10.1093/ecco-jcc/jjx169 .
Michie S, Wood CE, Johnston M, Abraham C, Francis JJ, Hardeman W. Behaviour change techniques: the development and evaluation of a taxonomic method for reporting and describing behaviour change interventions (a suite of five studies involving consensus methods, randomised controlled trials and analysis of qualitative data). Health Technol Assess. 2015;19(99):1–188. https://doi.org/10.3310/hta19990 .
Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30(2):133–46. https://doi.org/10.1177/1090198102251021 .
Robinson SM. Improving nutrition to support healthy ageing: what are the opportunities for intervention? Proc Nutr Soc. 2018;77(3):257–64. https://doi.org/10.1017/S0029665117004037 .
Rohnsch G, Hamel K. Co-production in coping with care dependency in Germany: how can integrated local care centres contribute? Health Soc Care Community. 2021;29(6):1868–75. https://doi.org/10.1111/hsc.13300 .
Lee JS, Johnson MA, Brown A. Older Americans act nutrition program improves participants’ food security in Georgia. J Nutr Gerontol Geriatr. 2011;30(2):122–39. https://doi.org/10.1080/21551197.2011.566526 .
Mayahara M, Paun O. Mental Health of Older Adults at the End of Life. J Psychosoc Nurs Ment Health Serv. 2023;61(1):12–5. https://doi.org/10.3928/02793695-20221207-03 .
Chow CK, Jolly S, Rao-Melacini P, Fox KA, Anand SS, Yusuf S. Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation. 2010;121(6):750–8. https://doi.org/10.1161/CIRCULATIONAHA.109.891523 .
Download references
Acknowledgements
We would like to thank all the participants in this study for their willingness to participate in this study and to express their views honestly.
This research was funded by the following projects: nsfc-funded project-The mechanism of MCPIP1 regulating Myocardin in vascular smooth muscle cells on atherosclerosis (No.82160099); Science and Technology Plan Project of Guizhou Province-Construction and Application of Internet of Things + Traditional Chinese Medicine Characteristic Intelligent Health Care System (No.Qiankehe support [2022] generally 263); Guizhou Provincial Health Commission Project (No.WJW-llc-H2021(11-01)).
Author information
Jiamengying Chen and Xiaojie Li contributed equally to this work.
Authors and Affiliations
Nursing School, Guizhou University of Traditional Chinese Medicine, Guiyang City, Guizhou Province, China
Jiamengying Chen, Xiaojie Li, Lvheng Zhao, Qingqing Zhu & Yixia Zhou
Nursing School, Guizhou Medical University, Guiyang City, Guizhou Province, China
Yun Wang & Yixia Zhou
The Second Affiliated Hospital, Guizhou University of Traditional Chinese Medicine, Guiyang City, Guizhou Province, China
Chunling Zhang & Li Yang
School of Nursing, Suzhou Medical College of Soochow University, Suzhou City, Jiangsu Province, China
You can also search for this author in PubMed Google Scholar
Contributions
Data curation, J.C., X.L., Y.W. and L.Z.; Investigation, J.C., X.L. and Q.Z.; Methodology, Y.Z. and L.W.; Interviewees recruited, C.Z., L.Y., L.Z, Q.Z. and Y.W.; Writing original manuscript, J.C.; Revised the manuscript, X.L. and L.W.
Corresponding authors
Correspondence to Li Wang or Yixia Zhou .
Ethics declarations
Ethics approval and consent to participate.
This study was conducted according to the Helsinki Declaration and approved by the Ethics Committee of The Second Affiliated Hospital of Guizhou University of Traditional Chinese Medicine. No.KYW2022007. Participants were fully informed about the study’s purpose, procedures. Participants’ personal information and data were kept confidential. If disclosure is required, it is carried out in accordance with the requirements of legal and ethical guidelines.
Consent for publication
Not applicable. The real names and personal information of the participants in this study has been kept anonymous and confidential.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chen, J., Li, X., Wang, Y. et al. Cognition of diet quality and dietary management in elderly patients with coronary and other atherosclerotic vascular disease in western China, a qualitative research study. BMC Geriatr 24 , 525 (2024). https://doi.org/10.1186/s12877-024-05058-2
Download citation
Received : 27 September 2023
Accepted : 08 May 2024
Published : 17 June 2024
DOI : https://doi.org/10.1186/s12877-024-05058-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nutritional assistance
- Qualitative research
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.369; 2020
Food for Thought 2020
Food and mood: how do diet and nutrition affect mental wellbeing, joseph firth.
1 Division of Psychology and Mental Health, Faculty of Biology, Medicine and Health, Oxford Road, University of Manchester, Manchester M13 9PL, UK
2 NICM Health Research Institute, Western Sydney University, Westmead, Australia
James E Gangwisch
3 Department of Psychiatry, Columbia University Vagelos College of Physicians and Surgeons, New York, USA
4 New York State Psychiatric Institute, New York, NY, USA
Alessandra Borsini
5 Section of Stress, Psychiatry and Immunology Laboratory, Institute of Psychiatry, Psychology and Neuroscience, Department of Psychological Medicine, King’s College London, London, UK
Robyn E Wootton
6 School of Psychological Science, University of Bristol, Bristol, UK
7 MRC Integrative Epidemiology Unit, Oakfield House, Bristol, UK
8 NIHR Biomedical Research Centre, University Hospitals Bristol NHS Foundation Trust and University of Bristol, Bristol, UK
Emeran A Mayer
9 G Oppenheimer Center for Neurobiology of Stress and Resilience, UCLA Vatche and Tamar Manoukian Division of Digestive Diseases, UCLA, Los Angeles, CA, USA
10 UCLA Microbiome Center, David Geffen School of Medicine, UCLA, Los Angeles, CA, USA
Poor nutrition may be a causal factor in the experience of low mood, and improving diet may help to protect not only the physical health but also the mental health of the population, say Joseph Firth and colleagues
Key messages
- Healthy eating patterns, such as the Mediterranean diet, are associated with better mental health than “unhealthy” eating patterns, such as the Western diet
- The effects of certain foods or dietary patterns on glycaemia, immune activation, and the gut microbiome may play a role in the relationships between food and mood
- More research is needed to understand the mechanisms that link food and mental wellbeing and determine how and when nutrition can be used to improve mental health
Depression and anxiety are the most common mental health conditions worldwide, making them a leading cause of disability. 1 Even beyond diagnosed conditions, subclinical symptoms of depression and anxiety affect the wellbeing and functioning of a large proportion of the population. 2 Therefore, new approaches to managing both clinically diagnosed and subclinical depression and anxiety are needed.
In recent years, the relationships between nutrition and mental health have gained considerable interest. Indeed, epidemiological research has observed that adherence to healthy or Mediterranean dietary patterns—high consumption of fruits, vegetables, nuts, and legumes; moderate consumption of poultry, eggs, and dairy products; and only occasional consumption of red meat—is associated with a reduced risk of depression. 3 However, the nature of these relations is complicated by the clear potential for reverse causality between diet and mental health ( fig 1 ). For example, alterations in food choices or preferences in response to our temporary psychological state—such as “comfort foods” in times of low mood, or changes in appetite from stress—are common human experiences. In addition, relationships between nutrition and longstanding mental illness are compounded by barriers to maintaining a healthy diet. These barriers disproportionality affect people with mental illness and include the financial and environmental determinants of health, and even the appetite inducing effects of psychiatric medications. 4

Hypothesised relationship between diet, physical health, and mental health. The dashed line is the focus of this article.
While acknowledging the complex, multidirectional nature of the relationships between diet and mental health ( fig 1 ), in this article we focus on the ways in which certain foods and dietary patterns could affect mental health.
Mood and carbohydrates
Consumption of highly refined carbohydrates can increase the risk of obesity and diabetes. 5 Glycaemic index is a relative ranking of carbohydrate in foods according to the speed at which they are digested, absorbed, metabolised, and ultimately affect blood glucose and insulin levels. As well as the physical health risks, diets with a high glycaemic index and load (eg, diets containing high amounts of refined carbohydrates and sugars) may also have a detrimental effect on psychological wellbeing; data from longitudinal research show an association between progressively higher dietary glycaemic index and the incidence of depressive symptoms. 6 Clinical studies have also shown potential causal effects of refined carbohydrates on mood; experimental exposure to diets with a high glycaemic load in controlled settings increases depressive symptoms in healthy volunteers, with a moderately large effect. 7
Although mood itself can affect our food choices, plausible mechanisms exist by which high consumption of processed carbohydrates could increase the risk of depression and anxiety—for example, through repeated and rapid increases and decreases in blood glucose. Measures of glycaemic index and glycaemic load can be used to estimate glycaemia and insulin demand in healthy individuals after eating. 8 Thus, high dietary glycaemic load, and the resultant compensatory responses, could lower plasma glucose to concentrations that trigger the secretion of autonomic counter-regulatory hormones such as cortisol, adrenaline, growth hormone, and glucagon. 5 9 The potential effects of this response on mood have been examined in experimental human research of stepped reductions in plasma glucose concentrations conducted under laboratory conditions through glucose perfusion. These findings showed that such counter-regulatory hormones may cause changes in anxiety, irritability, and hunger. 10 In addition, observational research has found that recurrent hypoglycaemia (low blood sugar) is associated with mood disorders. 9
The hypothesis that repeated and rapid increases and decreases in blood glucose explain how consumption of refined carbohydrate could affect psychological state appears to be a good fit given the relatively fast effect of diets with a high glycaemic index or load on depressive symptoms observed in human studies. 7 However, other processes may explain the observed relationships. For instance, diets with a high glycaemic index are a risk factor for diabetes, 5 which is often a comorbid condition with depression. 4 11 While the main models of disease pathophysiology in diabetes and mental illness are separate, common abnormalities in insulin resistance, brain volume, and neurocognitive performance in both conditions support the hypothesis that these conditions have overlapping pathophysiology. 12 Furthermore, the inflammatory response to foods with a high glycaemic index 13 raises the possibility that diets with a high glycaemic index are associated with symptoms of depression through the broader connections between mental health and immune activation.
Diet, immune activation, and depression
Studies have found that sustained adherence to Mediterranean dietary patterns can reduce markers of inflammation in humans. 14 On the other hand, high calorie meals rich in saturated fat appear to stimulate immune activation. 13 15 Indeed, the inflammatory effects of a diet high in calories and saturated fat have been proposed as one mechanism through which the Western diet may have detrimental effects on brain health, including cognitive decline, hippocampal dysfunction, and damage to the blood-brain barrier. 15 Since various mental health conditions, including mood disorders, have been linked to heightened inflammation, 16 this mechanism also presents a pathway through which poor diet could increase the risk of depression. This hypothesis is supported by observational studies which have shown that people with depression score significantly higher on measures of “dietary inflammation,” 3 17 characterised by a greater consumption of foods that are associated with inflammation (eg, trans fats and refined carbohydrates) and lower intakes of nutritional foods, which are thought to have anti-inflammatory properties (eg, omega-3 fats). However, the causal roles of dietary inflammation in mental health have not yet been established.
Nonetheless, randomised controlled trials of anti-inflammatory agents (eg, cytokine inhibitors and non-steroidal anti-inflammatory drugs) have found that these agents can significantly reduce depressive symptoms. 18 Specific nutritional components (eg, polyphenols and polyunsaturated fats) and general dietary patterns (eg, consumption of a Mediterranean diet) may also have anti-inflammatory effects, 14 19 20 which raises the possibility that certain foods could relieve or prevent depressive symptoms associated with heightened inflammatory status. 21 A recent study provides preliminary support for this possibility. 20 The study shows that medications that stimulate inflammation typically induce depressive states in people treated, and that giving omega-3 fatty acids, which have anti-inflammatory properties, before the medication seems to prevent the onset of cytokine induced depression. 20
However, the complexity of the hypothesised three way relation between diet, inflammation, and depression is compounded by several important modifiers. For example, recent clinical research has observed that stressors experienced the previous day, or a personal history of major depressive disorders, may cancel out the beneficial effects of healthy food choices on inflammation and mood. 22 Furthermore, as heightened inflammation occurs in only some clinically depressed individuals, anti-inflammatory interventions may only benefit certain people characterised by an “inflammatory phenotype,” or those with comorbid inflammatory conditions. 18 Further interventional research is needed to establish if improvements in immune regulation, induced by diet, can reduce depressive symptoms in those affected by inflammatory conditions.
Brain, gut microbiome, and mood
A more recent explanation for the way in which our food may affect our mental wellbeing is the effect of dietary patterns on the gut microbiome—a broad term that refers to the trillions of microbial organisms, including bacteria, viruses, and archaea, living in the human gut. The gut microbiome interacts with the brain in bidirectional ways using neural, inflammatory, and hormonal signalling pathways. 23 The role of altered interactions between the brain and gut microbiome on mental health has been proposed on the basis of the following evidence: emotion-like behaviour in rodents changes with changes in the gut microbiome, 24 major depressive disorder in humans is associated with alterations of the gut microbiome, 25 and transfer of faecal gut microbiota from humans with depression into rodents appears to induce animal behaviours that are hypothesised to indicate depression-like states. 25 26 Such findings suggest a role of altered neuroactive microbial metabolites in depressive symptoms.
In addition to genetic factors and exposure to antibiotics, diet is a potentially modifiable determinant of the diversity, relative abundance, and functionality of the gut microbiome throughout life. For instance, the neurocognitive effects of the Western diet, and the possible mediating role of low grade systemic immune activation (as discussed above) may result from a compromised mucus layer with or without increased epithelial permeability. Such a decrease in the function of the gut barrier is sometimes referred to as a “leaky gut” and has been linked to an “unhealthy” gut microbiome resulting from a diet low in fibre and high in saturated fats, refined sugars, and artificial sweeteners. 15 23 27 Conversely, the consumption of a diet high in fibres, polyphenols, and unsaturated fatty acids (as found in a Mediterranean diet) can promote gut microbial taxa which can metabolise these food sources into anti-inflammatory metabolites, 15 28 such as short chain fatty acids, while lowering the production of secondary bile acids and p-cresol. Moreover, a recent study found that the ingestion of probiotics by healthy individuals, which theoretically target the gut microbiome, can alter the brain’s response to a task that requires emotional attention 29 and may even reduce symptoms of depression. 30 When viewed together, these studies provide promising evidence supporting a role of the gut microbiome in modulating processes that regulate emotion in the human brain. However, no causal relationship between specific microbes, or their metabolites, and complex human emotions has been established so far. Furthermore, whether changes to the gut microbiome induced by diet can affect depressive symptoms or clinical depressive disorders, and the time in which this could feasibly occur, remains to be shown.
Priorities and next steps
In moving forward within this active field of research, it is firstly important not to lose sight of the wood for the trees—that is, become too focused on the details and not pay attention to the bigger questions. Whereas discovering the anti-inflammatory properties of a single nutrient or uncovering the subtleties of interactions between the gut and the brain may shed new light on how food may influence mood, it is important not to neglect the existing knowledge on other ways diet may affect mental health. For example, the later consequences of a poor diet include obesity and diabetes, which have already been shown to be associated with poorer mental health. 11 31 32 33 A full discussion of the effect of these comorbidities is beyond the scope of our article (see fig 1 ), but it is important to acknowledge that developing public health initiatives that effectively tackle the established risk factors of physical and mental comorbidities is a priority for improving population health.
Further work is needed to improve our understanding of the complex pathways through which diet and nutrition can influence the brain. Such knowledge could lead to investigations of targeted, even personalised, interventions to improve mood, anxiety, or other symptoms through nutritional approaches. However, these possibilities are speculative at the moment, and more interventional research is needed to establish if, how, and when dietary interventions can be used to prevent mental illness or reduce symptoms in those living with such conditions. Of note, a recent large clinical trial found no significant benefits of a behavioural intervention promoting a Mediterranean diet for adults with subclinical depressive symptoms. 34 On the other hand, several recent smaller trials in individuals with current depression observed moderately large improvements from interventions based on the Mediterranean diet. 35 36 37 Such results, however, must be considered within the context of the effect of people’s expectations, particularly given that individuals’ beliefs about the quality of their food or diet may also have a marked effect on their sense of overall health and wellbeing. 38 Nonetheless, even aside from psychological effects, consideration of dietary factors within mental healthcare may help improve physical health outcomes, given the higher rates of cardiometabolic diseases observed in people with mental illness. 33
At the same time, it is important to be remember that the causes of mental illness are many and varied, and they will often present and persist independently of nutrition and diet. Thus, the increased understanding of potential connections between food and mental wellbeing should never be used to support automatic assumptions, or stigmatisation, about an individual’s dietary choices and their mental health. Indeed, such stigmatisation could be itself be a casual pathway to increasing the risk of poorer mental health. Nonetheless, a promising message for public health and clinical settings is emerging from the ongoing research. This message supports the idea that creating environments and developing measures that promote healthy, nutritious diets, while decreasing the consumption of highly processed and refined “junk” foods may provide benefits even beyond the well known effects on physical health, including improved psychological wellbeing.
Contributors and sources: JF has expertise in the interaction between physical and mental health, particularly the role of lifestyle and behavioural health factors in mental health promotion. JEG’s area of expertise is the study of the relationship between sleep duration, nutrition, psychiatric disorders, and cardiometabolic diseases. AB leads research investigating the molecular mechanisms underlying the effect of stress and inflammation on human hippocampal neurogenesis, and how nutritional components and their metabolites can prevent changes induced by those conditions. REW has expertise in genetic epidemiology approaches to examining casual relations between health behaviours and mental illness. EAM has expertise in brain and gut interactions and microbiome interactions. All authors contributed to, read, and approved the paper, and all the information was sourced from articles published in peer reviewed research journals. JF is the guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare the following: JF is supported by a University of Manchester Presidential Fellowship and a UK Research and Innovation Future Leaders Fellowship and has received support from a NICM-Blackmores Institute Fellowship. JEG served on the medical advisory board on insomnia in the cardiovascular patient population for the drug company Eisai. AB has received research funding from Johnson & Johnson for research on depression and inflammation, the UK Medical Research Council, the European Commission Horizon 2020, the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust, and King’s College London. REW receives funding from the National Institute for Health Research Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. EAM has served on the external advisory boards of Danone, Viome, Amare, Axial Biotherapeutics, Pendulum, Ubiome, Bloom Science, Mahana Therapeutics, and APC Microbiome Ireland, and he receives royalties from Harper & Collins for his book The Mind Gut Connection. He is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and the US Department of Defense. The views expressed are those of the authors and not necessarily those of the organisations above.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of series commissioned by The BMJ. Open access fees are paid by Swiss Re, which had no input into the commissioning or peer review of the articles. T he BMJ thanks the series advisers, Nita Forouhi, Dariush Mozaffarian, and Anna Lartey for valuable advice and guiding selection of topics in the series.

IMAGES
VIDEO
COMMENTS
Research suggests that "healthy" food choices such as eating fruits and vegetables have not only physical but also mental health benefits and might be a long-term investment in future well-being.
3.2. Eating Habits. The analysis of eating habits showed that the students usually consumed 3-4 meals a day . The males ate meals at fixed times more often than the females (p = 0.012). Most of the students (approximately 83%) ate between meals, usually from several times a week to several times a day.
1. Introduction. Eating habits are defined as "conscious, collective, and repetitive behaviors, which lead people to select, consume, and use certain foods or diets, in response to social and cultural influences" [].University students are in a stage of change that renders them more susceptible to the development of unhealthy eating habits.
1. Background. Climate change induced by global agriculture, increasing population, and the epidemic of non-communicable diseases (NCDs) are the global major challenges [] that have established a tightly linked population-environment-health trilemma and present strong interactions often driven by dietary changes [].Healthy eating is regarded as a vital alleviator of confronting the three ...
Intervention covered knowledge about benefits of fitness, characteristics of a heart healthy diet, social influences on eating and exercise habits and issues to do with weight control. Environmental influences (e.g. provision of health food options in school canteen) were identified and strategies for improvement were presented to school personnel
Beyond immunity, research has shown that individuals following five key habits—eating a healthy diet, exercising regularly, keeping a healthy body weight, not drinking too much alcohol, and not smoking—live more than a decade longer than those who don't. Plus, maintaining these practices may not only help us live longer, but also better.
Eating habits (and health outcomes) typically vary with age. Although we control for age and its square in the benchmark specification, we conduct an additional robustness check using the 2021 Wave of the Multipurpose Survey: Aspects of Daily Life. ... Future research might apply models of habit formation more widely when studying parental ...
We were also interested in exploring whether the type of stress measure moderated the strength of the relationship between stress and eating. Previous research has found associations between stress and eating habits using different types of study design, including stress induction paradigms (e.g., Oliver et al., Citation 2000), daily diary ...
Interestingly, such brain dysfunction most often co-occurs with metabolic disorders (e.g., obesity) and/or poor dietary habits; obesity and poor diet can lead to negative health implications ...
Studies on breakfast habits by surveys have found that never eating breakfast is associated with increased risk for T2D, obesity, and CVD. However, these studies also showed that breakfast skipping is associated with late-night eating, variable eating patterns, and poor food quality (i.e., increased high-fat/high-sugar snacking and reduced ...
A meta-analysis on implementation intentions and healthy eating demonstrated that these intentions can indeed affect eating behaviour (Adriaanse et al., Citation 2011), although the effect on increasing healthy eating was stronger (d = .51) than on decreasing unhealthy eating (d = .29). Apart from having habits that guide eating behaviour ...
Mindful eating focuses on your eating experiences, body-related sensations, and thoughts and feelings about food, with heightened awareness and without judgment. Attention is paid to the foods being chosen, internal and external physical cues, and your responses to those cues. [1] The goal is to promote a more enjoyable meal experience and ...
This research study analyzed the eating habits reported in the interviews with a group of students at Granada University (Spain). In this regard, we clarify here that we have focused our research on University students because this social group is very appropriate to study how life crises (these usually appear as a consequence of the change ...
Understanding and addressing the impact of these modern food habits on health is crucial for promoting healthier lifestyles and preventing the associated health risks. In figure 1 around 41.4% of ...
The purpose of this explorative study was to use a qualitative research design to analyze the factors (barriers and enablers) that US college students perceived as influencing healthy eating behaviors. A group of Cornell University students ( n = 35) participated in six semi-structured focus groups. A qualitative software, CAQDAS Nvivo11 Plus ...
Limiting intake of free sugars to less than 10% of total energy intake (2, 7) is part of a healthy diet. A further reduction to less than 5% of total energy intake is suggested for additional health benefits (7). Keeping salt intake to less than 5 g per day (equivalent to sodium intake of less than 2 g per day) helps to prevent hypertension ...
Do watch your portion sizes. Do allow yourself to eat a range of foods without forbidding a particular food. Do give yourself encouragement. Do look for a support person to help you stay motivated ...
You can master healthy eating by learning how to plan meals and shop smart, and by practicing healthy-cooking techniques. ... But there are some nutrition basics that can help you sort through the latest research and advice. ... ed. Add 5 habits. In: The Mayo Clinic Diet. 3rd ed. Mayo Clinic Press; 2023.
Healthy Eating Behaviors in Children 2 to 8 Years. Durham, NC: Healthy Eating Research; 2021. Available at: https://healthyeatingresearch.org. Acknowledgements The expert panel was supported by Healthy Eating Research (HER), a national program of the Robert Wood Johnson Foundation. HER and the authors thank the expert panel
A minority (29%) say eating habits are healthier today, while 17% say they are about the same. The public points the finger at both quality and quantity in Americans' eating habits. When asked which is the bigger source of problems in Americans' eating habits, more say the issue is what people eat, not how much (24% vs. 12%).
Research shows that the more often a person eats high-sugar or high-fat foods, the more they develop a taste for them. That makes habits even harder to break. Here are some tips from Mayo Clinic experts for adding some healthy eating habits. Learn the basics of a healthy diet. The diet you follow should fit your tastes, lifestyle and budget. It ...
To promote healthy eating habits and regular physical activity in learners, parents and educators by means of an action planning process ... are as a result of dietary habits and ethnicity and socio-economic status are identified as determinants of health eating. Thus, future research should not exclude these specific groups as European ...
A heart-healthy eating plan limits sodium (salt), saturated fat, added sugars, and alcohol. Understanding nutrition labels can help you choose healthier foods.. Limit sodium. Adults and children over age 14 should eat less than 2,300 milligrams of sodium a day. Children younger than age 14 may need to eat even less sodium each day based on their sex and age.
What's the prevalence of binge eating in society? That's a tricky question because the research doesn't entirely agree. The National Comorbidity Survey Replication, which was done in 2007 by my mentor, Jim Hudson, and Ron Kessler, suggested that the prevalence of DSM-4 binge-eating disorder was around 2.6 percent [chance over a] lifetime in the U.S.
Healthy eating is one of the most important nonpharmacologic treatments for patients with atherosclerosis(AS). However, it is unclear how elderly AS patients in western China perceive their dietary status and which type of nutritional assistance they would be willing to receive. Therefore, the primary purpose of this study was to understand the level of knowledge about current dietary habits ...
Healthy eating patterns, such as the Mediterranean diet, are associated with better mental health than "unhealthy" eating patterns, such as the Western diet. The effects of certain foods or dietary patterns on glycaemia, immune activation, and the gut microbiome may play a role in the relationships between food and mood.
Background: The Dutch Eating Behavior Questionnaire (DEBQ) is a widely used self-report measure of eating styles, i.e., emotional, restrained, and external. A short and reliable version is useful for screening, routine assessments, and multipurpose surveys. Objective: The short version of the DEBQ by Bailly et al. (2012) was validated in the Italian context in two studies.