Cell-Phone Addiction: A Review
Affiliations.
- 1 Department of Psychobiology, Psychology Faculty, Complutense University of Madrid (Universidad Complutense de Madrid) , Madrid , Spain.
- 2 Department of Psychobiology, Psychology Faculty, Complutense University of Madrid (Universidad Complutense de Madrid), Madrid, Spain; Clinical Management of Mental Health Unit, Biomedical Research Institute of Málaga, Regional University Hospital of Málaga (Unidad de Gestión Clínica de Salud Mental, Hospital Regional Universitario de Málaga, Instituto de Investigación Biomédica de Málaga - IBIMA), Málaga, Spain.
- 3 Istituto de Investigación i+12, Hospital Universitario 12 de Octubre de Madrid , Madrid , Spain.
- PMID: 27822187
- PMCID: PMC5076301
- DOI: 10.3389/fpsyt.2016.00175
We present a review of the studies that have been published about addiction to cell phones. We analyze the concept of cell-phone addiction as well as its prevalence, study methodologies, psychological features, and associated psychiatric comorbidities. Research in this field has generally evolved from a global view of the cell phone as a device to its analysis via applications and contents. The diversity of criteria and methodological approaches that have been used is notable, as is a certain lack of conceptual delimitation that has resulted in a broad spread of prevalent data. There is a consensus about the existence of cell-phone addiction, but the delimitation and criteria used by various researchers vary. Cell-phone addiction shows a distinct user profile that differentiates it from Internet addiction. Without evidence pointing to the influence of cultural level and socioeconomic status, the pattern of abuse is greatest among young people, primarily females. Intercultural and geographical differences have not been sufficiently studied. The problematic use of cell phones has been associated with personality variables, such as extraversion, neuroticism, self-esteem, impulsivity, self-identity, and self-image. Similarly, sleep disturbance, anxiety, stress, and, to a lesser extent, depression, which are also associated with Internet abuse, have been associated with problematic cell-phone use. In addition, the present review reveals the coexistence relationship between problematic cell-phone use and substance use such as tobacco and alcohol.
Keywords: addiction; behavioral addiction; cell-phone addiction; dependence; internet addiction.

Publication types
Advertisement
Is Mobile Addiction a Unique Addiction: Findings from an International Sample of University Students
- Original Article
- Published: 12 December 2019
- Volume 18 , pages 1360–1388, ( 2020 )
Cite this article

- Mark Douglas Whitaker 1 &
- Suzana Brown 1
853 Accesses
6 Citations
1 Altmetric
Explore all metrics
This research explores whether addictions around mobile phones should be treated more as a physiological or a psychological problem. A new survey about mobile addiction and time use (MATU), constructed from several studies, tests to what degree time use on mobile phones (a physiological cause) is correlated with four behavioral factors predicting proneness to addiction, respectively one physiological problem and three psychological problems: sensation seeking, impulsiveness, anxiety, and hopelessness. Equally, an index on how strongly students interpret that they have a mobile addiction problem was tested for whether it was correlated to the same four factors. A sample of 1219 students was drawn from four universities, three in the USA and one in South Korea. Correlations between six indexes were analyzed. Students who think they have a “mobile phone time use problem” do not report high (physiological) sensation seeking at all (0.18, p < 0.01) yet have higher correlations only with three psychological problems: impulsiveness (0.64, p < 0.01), hopelessness (0.47, p < 0.01), and anxiety (0.31, p < 0.01). On the other hand, the exact inverse occurs among actual sensation seekers with high time use (0.85, p < 0.01) who lack high correlations with three psychological problems (each below 0.15, p < .01). The pattern held across four different universities and two countries with minimal variations. Mobile addictions appear to be two different types of individualized problems instead of one: physiological problems for some (without major psychological problems) and psychological problems for others (without high time use). This research may help influence policy to target different individual problems in mobile addiction.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others
Problematic mobile phone use in adolescents: derivation of a short scale mppus-10.

Mobile phone dependence: Secondary school pupils’ attitudes
The prevalence and predictors of problematic mobile phone use: a 14-country empirical survey.
Nonetheless, for those interested in the ancillary question of whether our school-based samples are more or less representative than larger national samples, see Appendix 3.
As noted in Appendix 2, for this sole correlation, different disaggregated meso-level schools fail to show this same result as the full sample: sometimes showing the same lack of statistical significance as the full sample (School D), sometimes weakly positive and statistically significant (School B & C) and sometimes weakly negative and statistically significant (School A). This would seem to indicate varying meso-level issues of school culture or macro-level issues (as School A is the Korean university) equally are important in some way in mobile addiction as well. However, since this study is concerned with only the micro-level of analysis of mobile addiction, and since these micro-level findings are stronger than these meso-level findings in general, the discussion continues to discuss mostly Fig. 1 . Equally noted in Appendix 2 for the micro-level correlations, even disaggregated schools regularly show the same results as the full sample on the four micro-level behavioral factors. This indicates strong micro-level universalities and external validity to the micro-level findings.
Instead of a universal physiological relationship between school problems and mobile phone time use, as noted in disaggregated analysis in Appendix 2’s Table 4 , an intervening variable of a varying school culture (a meso-level correlation) seems to matter for a relatively minor influential relationship developing between school problems and mobile phone time use, instead of this correlation being a physiological universal. Moreover, across the four schools, disaggregated meso-level findings of correlation are mostly always smaller than more regularly stronger micro-level findings of correlation. These findings are seen as complementary factors in mobile addiction instead of opposed to each other.
This may be because some kinds of mobile phone use can be a connecting solace and socially affirming, instead of always escapist. Only a future analysis classifying which particular kinds of “apps” or behaviors on a mobile phone are interpreted by their users as individually escapist or socially affirming can resolve such an issue (Depner 2017 ).
Excluded analysis of a resilience index showed the same result. Contact authors for more information.
The authors will share the MATU survey with other researchers interested in widening the comparative analysis of mobile addition with the same survey instrument whether on these or other points.
Results not included for lack of space.
Akin, A., Altundag, Y., Turan, M., & Akin, U. (2014). The validity and reliability of the Turkish version of the smartphone addiction scale-short form for adolescent. Procedia - Social and Behavioral Sciences, 152 , 74–77.
Google Scholar
Alexander, B. (2001). The roots of addiction in free market society . Vancouver, Canada: Canadian Centre for Policy Alternatives. ( www.policyalternatives.ca )
Alexander, B. (2010). Globalization of addiction: A study in poverty of the spirit . Oxford, UK: Oxford University Press.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5). American Psychiatric Pub.
Andreassen, C. S., Billieux, J., Griffiths, M. D., Kuss, D. J., Demetrovics, Z., Mazzoni, E., & Pallesen, S. (2016). The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: A large-scale cross-sectional study. Psychology of Addictive Behaviors, 30 ( 2 ), 252–262. https://doi.org/10.1037/adb0000160 .
Article Google Scholar
Andreassen, C. S., Pallesen, S., & Griffiths, M. D. (2017). The relationship between addictive use of social media, narcissism, and self-esteem: Findings from a large national survey. Addictive Behaviors, 64 , 287–293. https://doi.org/10.1016/j.addbeh.2016.03.006 .
Article PubMed Google Scholar
Barratt, E. S., Patton, J., & Stanford, M. (1975). Barratt Impulsiveness Scale . Texas: Barratt-Psychiatry Medical Branch, University of Texas.
Bax, T. (2014). Youth and Internet addiction in China . New York City, NY: Routledge.
Beck, A. T., Weissman, A., Lester, D., & Trexler, L. (1974). The measurement of pessimism: The hopelessness scale. Journal of Consulting and Clinical Psychology, 42 (6), 861.
CAS PubMed Google Scholar
Billieux, J., Philippot, P., Schmid, C., Maurage, P., & Mol, J. (2014). Is dysfunctional use of the mobile phone a behavioural addiction? Confronting symptom based versus process-based approaches. Clinical Psychology & Psychotherapy, 22 (5), 460–468. https://doi.org/10.1002/cpp.1910 .
Billieux, J., Maurage, P., Lopez-Fernandez, O., Kuss, D., & Griffiths, M. D. (2015). Can disordered mobile phone use be considered a behavioral addiction? An update on current evidence and a comprehensive model for future research. Current Addiction Reports, 2 (2), 156–162. https://doi.org/10.1007/s40429-015-0054-y .
Boumosleh, J., & Jaalouk, D. (2017). Smartphone addiction among university students and its relationship with academic performance. Global Journal of Health Science, 10 (1), 48–59.
Cain, G. (2014). South Korean teens are so addicted to their smartphones that the government is taking action, The Business Insider , http://www.businessinsider.com/south-korea-concerned-about-smart-phone-usage-2014-4 (Accessed: December 14, 2017)
Ching, S. M., Yee, A., Ramachandran, V., Lim, S. M., Sulaiman, W. A., Foo, Y. L., & KeeHoo, F. (2015). Validation of a Malay Version of the Smartphone Addiction Scale among medical students in Malaysia. PLoS One, 10 (10), e0139337. https://doi.org/10.1371/journal.pone.0139337 .
Article CAS PubMed PubMed Central Google Scholar
Chiu, S-I. (2014). The relationship between life stress and smartphone addiction on taiwanese university student: A mediation model of learning self-Efficacy and social self-Efficacy. Computers in Human Behavior, 34 , 49-57
Choi, S. W., Kim, D. J., Choi, J. S., Ahn, H., Choi, E. J., Song, W. Y., & Youn, H. (2015). Comparison of risk and protective factors associated with smartphone addiction and Internet addiction. Journal of Behavioral Addictions, 4 (4), 308–314.
PubMed PubMed Central Google Scholar
Chóliz, M., Pinto, L., Phansalkar, S. S., Corr, E., Mujjahid, A., Flores, C., & Barrientos, P. E. (2016). Development of a brief multicultural version of the test of mobile phone dependence (TMDbrief) questionnaire. Frontiers in Psychology, 7 , 650. https://doi.org/10.3389/fpsyg.2016.00650 .
Article PubMed PubMed Central Google Scholar
Cohen, J. (1992). A power primer. Psychological Bulletin, 112 (1), 155.
Conrod, P. J. (2016). Personality-targeted interventions for substance use and misuse. Current Addiction Reports, 3 , 426–436.
Conrod, P. J., Pihl, R. O., & Vassileva, J. (1998). Differential sensitivity to alcohol reinforcement in groups of men at risk for distinct alcoholism subtypes in Alcoholism. Clinical and Experimental Research, 22 (3), 585–597.
CAS Google Scholar
Conrod, P. J., Stewart, S. H., Pihl, R. O., Côté, S., Fontaine, V., & Dongier, M. (2000). Efficacy of brief coping skills interventions that match different personality profiles of female substance abusers. Psychology of Addictive Behaviors, 14 (3), 231.
Conrod, P. J., Stewart, S. H., Comeau, N., & Maclean, A. M. (2006). Efficacy of cognitive–behavioral interventions targeting personality risk factors for youth alcohol misuse. Journal of Clinical Child and Adolescent Psychology, 35 (4), 550–563.
PubMed Google Scholar
Conrod, P. J., Castellanos-Ryan, N., & Strang, J. (2010). Brief, personality-targeted coping skills interventions and survival as a non–drug user over a 2-year period during adolescence. Archives of General Psychiatry, 67 (1), 85–93.
Cortina, J. M. (1993). What is coefficient alpha? An examination of theory and applications. Journal of Applied Psychology, 78 (1), 98.
Costello, A. B., & Osborne, J. W. (2005). Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Practical Assessment, Research, & Evaluation, 10 , 1-9
Courtwright, D. (2002). Forces of habit: Drugs and the making of the modern world . Cambridge, Massachusetts: Harvard University Press.
Cronbach, L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16 (3), 297–334.
Demirci, K., Orhan, H., Demirdas, A., Akpinar, A., & Sert, H. (2014). Validity and reliability of the Turkish version of the smartphone addiction scale in a younger population. Klinik Psikofarmakoloji Bulteni/Bulletin of Clinical Psychopharmacology, 24 ( 3 ), 226–234. https://doi.org/10.5455/bcp.20140710040824 .
Demirci, K., Akgonul, M., & Akpinar, A. (2015). Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. Journal of Behavioral Addictions, 4 ( 2 ), 85–92. https://doi.org/10.1556/2006.4.2015.010 .
Depner, R. A. (2017). In search of wholeness: An exploration of social connection as a mediating factor in addiction. Thesis, Masters of Counseling, City University of Seattle, Vancouver BC, Canada site.
DiClemente, C. C. (2003). Addiction and change: How addictions develop and addicted people recover . New York City: Guilford Press.
Dunckley, Victoria L. (2015). Chapter 1: Electronic screen syndrome: An unrecognized disorder, in Reset Your Child’s Brain: A Four Week Plan to End Meltdowns, Raise Grades, and Boost Social Skills by Reversing the Effects of Electronic Screen Time . Novato, California: New World Library.
Gentile, D. (2009). Pathological video game use among youth 8 to 18: A national study. Psychological Science, 20 (5), 594–602.
George, D. (2001). Preference pollution: How markets create the desires we dislike . University of Michigan Press.
Goodman, A. (1990). Addiction: Definition and implications. British Journal of Addiction, 85 ( 11 ), 1403–1408.
Griffiths, M. (2005). A ‘components’ model of addiction within a biopsychosocial framework. Journal of Substance Use, 10 (4), 191–197.
Griffiths, M. D. (2017). Behavioural addiction and substance addiction should be defined by their similarities not their dissimilarities. Addiction, 112 (10), 1718–1720.
Ha, J. H., Chin, B., Park, D. H., Ryu, S. H., & Yu, J. (2008). Characteristics of excessive cellular phone use in Korean adolescents. Cyberpsychology & Behavior, 11 ( 6 ), 783–784. https://doi.org/10.1089/cpb.2008.0096 .
Hamilton, M. A. X. (1959). The assessment of anxiety states by rating. Psychology and Psychotherapy: Theory, Research and Practice, 32 (1), 50–55.
Haug, S., Castro, R., Kwon, M., Filler, A., Kowatsch, T., & Schaub, M. (2015). Smartphone use and smartphone addiction among young people in Switzerland. Journal of Behavioral Addictions, 4 (4), 299–307. https://doi.org/10.1556/2006.4.2015.037 .
Hawi, N., & Samaha, M. (2016). To excel or not to excel: Strong evidence on the adverse effect of smartphone addiction on academic performance. Computers & Education, 98 , 81e89. https://doi.org/10.1016/j.compedu.2016.03.007 .
Hong, F. Y., Chiu, S. I., & Huang, D. H. (2012). A model of the relationship between psychological characteristics, mobile phone addiction and use of mobile phones by Taiwanese university female students. Computers in Human Behavior, 28 (6), 2152-2159.
Im, K. G., Hwang, S. J., Choi, M. A., Seo, N. R., & Byun, J. N. (2013). The correlation between smartphone addiction and psychiatric symptoms in college students. Journal of the Korean Society of School Health, 26 ( 2 ), 124–131.
Jenaro, C., Flores, N., Gómez-Vela, M., González-Gil, F., & Caballo, C. (2007). Problematic internet and cell phone use: Psychological, behavioral, and health correlates. Addiction Research & Theory, 15 (3), 309–320.
Jeong, S. H., Kim, H., Yum, J. Y., & Hwang, Y. (2016). What type of content are smartphone users addicted to? SNS vs. games. Computers in Human Behavior, 54 , 10–17. https://doi.org/10.1016/j.chb.2015.07.035 .
Jun, S. (2016). The reciprocal longitudinal relationships between mobile phone addiction and depressive symptoms among Korean adolescents. Computers in Human Behavior, 58 , 179–186.
Junco, R., & Cotten, S. R. (2012). No A 4 U: The relationship between multitasking and academic performance. Computers & Education, 59 , 505–514.
Kardaras, N. (2016). Glow kids: How screen addiction is hijacking our kids-and how to break the trance . St. Martin’s Press.
Khoury, J. M., de Freitas, A. A. C., Roque, M. A. V., Albuquerque, M. R., das Neves, M. D. C. L., & Garcia, F. D. (2017). Assessment of the accuracy of a new tool for the screening of smartphone addiction. PLoS One, 12 (5), e0176924. https://doi.org/10.1371/journal.pone.0176924 .
Kibona, L., & Mgaya, G. (2015). Smartphones’ effects on academic performance of higher learning students. Journal of Multidisciplinary Engineering Science and Technology, 2 (4), 777–784.
Kim D, Lee Y, Lee J, Nam JK. & Chung (2014). Development of Korean Smartphone Addiction Proneness Scale for Korean youth, PLoS One 9(5): e97920. Doi: https://doi.org/10.1371/jouornal.phone.0097920
Ko, C. H., Liu, G. C., Hsiao, S., Yen, Y. J., Yang, M. J., Lin, W. C., Yen, C. F., & Chen, C. S. (2009). Brain activities associated with gaming urge of online gaming addiction. Journal of Psychiatric Research, 43 (7), 739–747.
Kwon, M., Lee, J. Y., Won, W. Y., Park, J. W., Min, J. A., Hahn, C., & Kim, D. J. (2013). Development and Validation of a Smartphone Addiction Scale (SAS). PLoS One, 8 (2), e56936. https://doi.org/10.1371/journal.pone.0056936 .
Lee, E. B. (2015). Too much information heavy smartphone and Facebook utilization by African American young adults. Journal of Black Studies, 46 ( 1 ), 44–61. https://doi.org/10.1177/0021934714557034 .
Article CAS Google Scholar
Lee, M. J., Lee, J. S., Kang, M. H., Kim, C. E., Bae, J. N., & Choo, J. S. (2010). Characteristics of cellular phone use and its association with psychological problems among adolescents. Journal of the Korean Academy of Child and Adolescent Psychiatry, 21 ( 1 ), 31–36. https://doi.org/10.5765/jkacap.2010.21.1.031 .
Lepp, A., Barkley, J. E., & Karpinski, A. C. (2014). The relationship between cell phone use, academic performance, anxiety, and satisfaction with life in college students. Computers in Human Behavior, 31 , 343–350. https://doi.org/10.1016/j.chb.2013.10.049 .
Lepp, A., Barkley, J. E., & Karpinski, A. C. (2015) The relationship between cell phone use and academic performance in a sample of U.S. college students, SAGE Open January-March (1):1-9. doi: https://doi.org/10.1177/2158244015573169
Lettieri, D., Sayers, M., & Wallenstein, P. H. (Eds.). (1980). Theories on drug abuse: Selected contemporary perspectives, National Institute on Drug Abuse (NIDA) Research Monograph #30, Part of the U.S. Department of Health and Human Services . Washington, D. C.: US Gov’t Printing Office.
Leung, L. (2008). Linking psychological attributes to addiction and improper use of the mobile phone among adolescents in Hong Kong. Journal of Children and Media, 2 ( 2 ), 93–113. https://doi.org/10.1080/17482790802078565 .
Lin, Y. H., Chang, L. R., Lee, Y. H., Tseng, H. W., Kuo, T., & Chen, S. (2014). Development and validation of the Smartphone Addiction Inventory (SPAI). PLoS One, 9 ( 6 ), e98312.
Lin, T. T. C., Chiang, Y., & Jiang, Q. (2015). Sociable people beware? Investigating smartphone versus nonsmartphone dependency among young Singaporeans. Social Behavior and Personality, 43 ( 7 ), 1209–1216. https://doi.org/10.2224/sbp.2015.43.7.1209 .
Lindesmith, A. (1938). A sociological theory of drug addiction. American Journal of Sociology, 43 (4), 593–613. https://doi.org/10.1086/217773 .
Long, J., Liu, T.-Q., Liao, Y. H., Qi, C., He, H. Y., Chen, S. B., & Billieux, J. (2016). Prevalence and correlates of problematic smartphone use in a large random sample of Chinese undergraduates. BMC Psychiatry, 16 ( 1 ), 408. https://doi.org/10.1186/s12888-016-1083-3 .
Lopez-Fernandez, O., Griffiths, M. D., Kuss, D. J., Dawes, C., Pontes, H. M., Justice, L., Männikkö, N., et al. (2019). Cross-cultural validation of the Compulsive Internet Use Scale in four forms and eight languages. Cyberpsychology, Behavior and Social Networking, 22 ( 7 ), 451 – 464 .
Lu, X., Watanabe, J., Liu, Q., Uji, M., Shono, M., & Kitamura, T. (2011). Internet and mobile phone text-messaging dependency: Factor structure and correlation with dysphoric mood among Japanese adults. Computers in Human Behavior, 27 ( 5 ), 1702–1709. https://doi.org/10.1016/j.chb.2011.02.009 .
Mak, K. K., Lai, C. M., Watanabe, H., Kim, D. I., Bahar, N., Ramos, M., & Cheng, C. (2014). Epidemiology of internet behaviors and addiction among adolescents in six Asian countries. Cyberpsychology, Behavior and Social Networking, 17 (11), 720–728.
Marlatt, G. A., Baer, J. S., Donovan, D. M., & Kivlahan, D. R. (1988). Addictive behaviors: Etiology and treatment. Annual Review of Psychology, 39 (1), 223–252.
Martinotti, G., Villella, C., Di Thiene, D., Di Nicola, M., Bria, P., Conte, G., Cassano, M., Petruccelli, F., Corvasce, N., Janiri, L., & La Torre, G. (2011). Problematic mobile phone use in adolescence: A cross-sectional study. Journal of Public Health, 19 ( 6 ), 545–551. https://doi.org/10.1007/s10389-011-0422-6 .
McAuliffe, W., & Gordon, R. (1974). A test of Lindesmith’s theory of addiction: The frequency of euphoria among long-term addicts. American Journal of Sociology, 79 (4), 795–840 http://www.jstor.org/stable/2776345 .
Meerkerk, G.-J., Van Den Eijnden, R. J. J. M., Vermulst, A. A., & Garretsen, H. F. L. (2009). The Compulsive Internet Use Scale (CIUS): Some psychometric properties. CyberPsychology and Behavior, 12 ( 1 ), 1–6. https://doi.org/10.1089/cpb.2008.0181 .
Muñoz-Miralles, R., Raquel, O.-G., Rosa López-Morón, M., Batalla-Martínez, C., Manresa, J. M., Montellà-Jordana, N., Chamarro, A., Carbonell, X., & Torán-Monserrat, P. (2016). The problematic use of Information and Communication Technologies (ICT) in adolescents by the cross sectional JOITIC study. BMC Pediatrics, 16 , 140. https://doi.org/10.1186/s12887-016-0674-y .
Park, P. (1985). The supply side of drinking: Alcohol production and consumption in the United States before prohibition, Contemporary Drug Problems 12.
Park, N., & Lee, H. (2012). Social implications of smartphone use: Korean college students’ smartphone use and psychological well-being. Cyberpsychology, Behavior and Social Networking, 15 ( 9 ), 491–497. https://doi.org/10.1089/cyber.2011.0580 .
Pinna, F., Dell’Osso, B., Di Nicola, M., Janiri, L., Altamura, A. C., Carpiniello, B., & Hollander, E. (2015). Behavioural addictions and the transition from DSM-IV-TR to DSM-5. J Psychopathol, 21 ( 4 ), 380–389.
Pombo, S., & da Costa, N. F. (2016). Heroin addiction patterns of treatment-seeking patients, 1992-2013: comparison between pre- and post-drug policy reform in Portugal, in. Heroin Addiction: Related Clinical Problems, 18 (6), 51–60.
Sapacz, M., Rockman, G., & Clark, J. (2016). Are we addicted to our cell phones? Computers inHuman Behavior, 57 , 153–159.
Smart, RG. (1980). An availability-proneness theory of illicit drug abuse, in Theories on Drug Abuse: Selected Contemporary Perspectives , National Institute on Drug Abuse (NIDA) Research Monograph #30, part of the U.S. Department of Health and Human Services. (eds., Dan J. Lettieri, Mollie Sayers, Helen Wallenstein Pearson) Washington, D. C.: US Gov’t Printing Office. Pp. 46-49.
Starcevic, V., & Aboujaoude, E. (2016). Internet addiction: Reappraisal of an increasingly inadequate concept. CNS Spectrums, 22 (1), 7–13. https://doi.org/10.1017/S1092852915000863 .
Szasz, T. (2003/1974). Ceremonial chemistry: The ritual persecution of drugs, addicts, and pushers. Syracuse, New York: Syracuse University Press. Reprint.
Tavakolizadeh, J., Atarodi, A., Ahmadpour, S., & Pourgheisar, A. (2014). The prevalence of excessive mobile phone use and its relation with mental health status and demographic factors among the students of Gonabad University of Medical Sciences in 2011-2012. Razavi International Journal of Medicine, 2 ( 1 ), 1–7. https://doi.org/10.5812/rijm.15527 .
Teeson, M. (2002). Theories of addiction: causes and maintenance of addiction. In M. Teeson & L. Degenhardt (Eds.), Addictions: An Introduction . Psychology Press.
Walsh, S. P., White, K. M., & Young, R. M. (2008). Over-connected? A qualitative exploration of the relationship between Australian youth and their mobile phones. Journal of Adolescence, 31 ( 1 ), 77–92. https://doi.org/10.1016/j.adolescence.2007.04.004 .
Wang, J. L., Jackson, L. A., Zhang, D. J., & Su, Z. Q. (2012). The relationships among the Big Five Personality factors, self-esteem, narcissism, and sensation-seeking to Chinese University students’ uses of social networking sites (SNSs). Computers in Human Behavior, 28 ( 6 ), 2313–2319. https://doi.org/10.1016/j.chb.2012.07.001 .
Wang, H., Wang, M., & Wu, S. (2015). Mobile phone addiction symptom profiles related to interpersonal relationship and loneliness for college students: A latent profile analysis. Chinese Journal of Clinical Psychology, 23(5), 881-885. Retrieved from http://caod.oriprobe.com/articles/46926496/Mobile_Phone_Addiction_symptom_Profiles_Related_to_Interpersonal_Relat.htm (Accessed: October, 14, 2019)
Weinstein, A., & Lejoyeux, M. (2010). Internet addiction or excessive Internet use. The American Journal of Drug and Alcohol Abuse, 36 , 277–283.
Wu, A., Cheung, V., Ku, L., & Hung, W. (2013). Psychological risk factors of addiction to social networking sites among Chinese smartphone users. Journal of Behavioral Addictions, 2 ( 3 ), 160–166. https://doi.org/10.1556/JBA.2.2013.006 .
Young, K. S. (1996). Psychology of computer use: XL. Addictive use of the Internet: A case that breaks the stereotype. Psychological Reports, 79 (3), 899–902.
Young, K. S. (2004). Internet addiction: A new clinical phenomenon and its consequences. American Behavioral Scientist, 48 (4), 402–415.
Young, E. (2017). Iceland knows how to stop teen substance abuse but the rest of the world isn’t listening, Mosaic: The Science of Life https://mosaicscience.com/story/iceland-prevent-teensubstance-abuse (Accessed: December 22, 2017); Published by the Welcome Charitable Trust ( https://wellcome.ac.uk/ ).
Zuckerman, M., Kolin, E. A., Price, L., & Zoob, I. (1964). Development of a sensation-seeking scale. Journal of Consulting Psychology, 28 (6), 477.
Download references
Author information
Authors and affiliations.
Department of Technology and Society, Stony Brook University, SUNY Korea, Incheon, Incheon Global Campus, B310, 119 SongdoMoonhwa-Ro, Yeonsu-gu, 406-840, South Korea
Mark Douglas Whitaker & Suzana Brown
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Mark Douglas Whitaker .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest. No external funding was used in the creation of the Mobile Addiction and Time Use Survey (MATU) or ongoing data analysis.
The necessary ethical permissions were received from the Institutional Review Board at all four universities. Before completing the survey, participants were informed about the study protocol and gave their consent electronically.
Ethical Approval
All procedures performed in this study involving human participants were approved by and in accordance with the ethical standards of Institutional Research Review Boards of the four universities involved and with the 1964 Helsinki declaration and its later amendments.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1. Indices in the analysis based on questions from the survey on mobile addiction and time use (MATU)
In all indices, an asterisk on the question (*) indicates a reverse-coded question.
Index 1: School outcomes regarding mobile phone use
My school grades dropped because I use my mobile phone excessively.
I have a hard time finishing things because of using my mobile phone.
When I use my mobile phone, I think I would be more productive if I did not use it so much.
When I use my mobile phone, I feel I should be concentrating on study/work instead.
My mobile phone does not distract me from my studies.*
Index 2: Time use of mobile phones
Texting on mobile phones and on apps with chat options
Taking selfies or self-videos
Using a mobile phone for emails
Using a mobile phone for games
Using a mobile phone for social media, SNS, or community
Using a mobile phone for entertainment, TV, videos, audio, or radio
Using a mobile phone for shopping and consumer services (includes paying bills)
Using a mobile phone for web browsing
Using a mobile phone for learning and education
Using a mobile phone for daily personal appointments and contact information
Using mobile phone for ongoing coordination with groups for events and meetings
Index 3: Sensation seeking connected to mobile phone use
Using a mobile phone for shopping and consumer services
It passes the time when I am bored.
I use it when I have to wait for someone or something rather than do nothing.
Index 4: Impulsiveness connected to mobile phone use
Friends and acquaintances comment on my excessive use of mobile phone.
Family members complain that I use my mobile phone too much.
When I use my mobile phone, family members get angry.
People are offended that I’m not paying attention when I’m on my mobile phone.
Index 5: Anxiety connected to mobile phone use
I can’t imagine life without my mobile phone.
It would be painful for me if I couldn’t use my mobile phone.
I get anxious when I am without my mobile phone.
I panic when I can’t use my mobile phone.
It would be impossible for me to give up my mobile phone.
Index 6: Hopelessness associated with mobile phone use
How often do you feel sad?
How often do you avoid dealing with problems in your life?
How often do you feel hopeful about the future?*
When I can’t use my mobile phone, I feel like I have lost an entire world.
Using my mobile phone allows me to escape an unpleasant aspect of my life for a while.
When I use my mobile phone, I feel bad but I can’t stop using it.
Have you ever felt bad or guilty about your mobile phone usage?
Have people annoyed you by criticizing your mobile phone usage?
My whole personal and social life depends on my phone.
Using my mobile phone is more enjoyable than spending time with my family.
Using my mobile phone is more enjoyable than spending time with my friends.
Appendix 2. Disaggregated analysis of the six indices and the four schools show a lack of bias from any of the four schools in the sample and a lack of bias in the results as well
There were two potential problems identified, and both resolved, since either difference in respondent rates across all four schools or demographics of one school itself could skew the whole sample, the creation of the indices, and the results from the whole sample. Therefore before the main analysis, it was important first to validate that the aggregate sample lacks skew and is thus a legitimate basis to construct the analysis. Equally, it was important to provide evidence the indices are legitimate bases upon which to construct such analysis. Therefore, the same six indices were tested using the discrete school samples themselves via EFA and Cronbach’s alpha, and these results were compared to the results from the full sample on these two measures. It was reassuring that both these two potential problems of sample size differences and skewed index construction can be rejected. In comparing these disaggregated four samples’ index statistics to the full samples’ index statistics, all these indices’ statistics showed consistency in EFA Footnote 7 and in Cronbach’s alpha when compared to the full sample as shown in Table 3 .
Both tests upon the indices (Table 3 ) and the data findings (Table 4 ) indicated no school is a major outlier skewing the formation of the indices or the analysis in one way or another. For ease of comparison, Table 3 repeats Cronbach’s alpha for each of the six derived indexes using the full four-school sample ( n = 1219) from Table 2 , while presenting an additional 24 separate tests of Cronbach’s alpha for each of the six derived indexes for each of the four schools sampled, showing the major pattern is consistency across all four schools. This test of Cronbach’s alpha upon the disaggregated samples of data indicated all six indices are consistent across different schools in this sample. In addition, no single school in all six indices is an outlier skewing the indices or the later analysis, since noticeably either 3 of 4 schools or 4 of 4 schools in all rows all had generally the same Cronbach’s alpha for each index. Out of 24 tests, only School A in one index had a slightly lower Cronbach’s alpha than all the other 23 tests. Any Cronbach’s alpha above 0.7 is considered reasonable, and the single example of 0.58 is at a level considered only questionable, instead of doubtful. In short, the idea of a bias and skewing from uneven sampling and from particular school subsamples was rejected.
However, after assuring the lack of skew of any one particular school on the six indices, a similar question arises if any schools’ discrete samples themselves show different analytic results than the eight correlations in Fig. 1 and thus were potentially another source of bias and skew in the full sample. Therefore, in Table 4 below, a further test of pairwise correlation upon the disaggregated samples of data shows the same nine correlations as in Fig. 1 . It was found that all four disaggregated school samples have generally the same scored consistencies as the full sample even across these four widely different schools. As before, no single school in all indices is an outlier skewing the micro-level analysis since (once more) either 3 of 4 schools or 4 of 4 schools all had generally the same correlations or patterns for each index. For the micro-level analysis, out of 32 additional correlation tests in Table 4 , only 5 differences are observed. For School A, one index was without statistical significance between school problems and sensation seeking. School A had three other indices without statistical significance between raw actual time use and impulsiveness, anxiety, or hopelessness, and School C was the same between raw actual time use and impulsiveness. For the latter four, it will be shown that these lacks of statistical significance in only these four discrete areas (while holding to very high statistical significance in all other 28 areas) actually makes the unique bimodal argument in the main discussion about mobile addiction stronger rather than weaker by foreshadowing a stronger case about a lack of strong correlation between raw mobile phone time use and many behavioral problems.
In short, both tests of Cronbach’s alpha on the indices for individual schools and the tests of pairwise correlations on the relationships between the indices for individual schools in the results indicated no single school in all indices is a major outlier skewing results of the overall analysis. In Tables 3 and 4 , it is intriguing that the same comparative statistical patterns or ratios hold across all four schools’ discrete samples and internationally. In addition, Table 4 shows both internal validity of the indices as well as somewhat an external validity in the analysis since all four samples generally have the same patterns of mobile addiction. In conclusion to this Appendix, we tested and confirmed both the internal validity of the indices and the external validity of the results by showing four separate samples had generally the same indices and analysis results as the full sample.
Appendix 3. Distributions for the six indices based on the full sample ( n = 1219)
In Fig. 2 below, compared with two different national findings (Korea and US) or Korean-municipal findings (Cain 2014 ; Gentile 2009 ), our sample lacks any unrepresentative larger or smaller scale of extreme internet/mobile addictions. First, if around 4% of the wider population of Seoul was found to be extreme mobile addicts in terms of time use (Cain, 2005), this is comparable to the below distribution for time use (Index 2) in our international sample. Equally, given a rare national US sample judging youth on a similar internet gaming addiction, 8.5% were found to be in the most extreme category of internet gaming addicts (Gentile 2009 ). This is hardly different than similar measures of sensation seeking or impulsive behavior extremes in our international sample (below, Index 3 and 4). However, it has to be said that to our defense, our sample was not designed to answer questions about national prevalence of addiction or whether our sample was representative or not compared to a national study on our hypotheses (since such a national study on our hypotheses have yet to be done, so no comparisons are possible yet). Our sampled higher educational youth population is the one best chosen to fit the two literatures drawn upon that use the same demographics (about mobile phone influenced school outcomes, and about proneness to addictive behavior employed in Conrod’s research) that allow more legitimately used questions or conceptual ideas adapted from these literatures and allow comparisons there.

Distributions for the six indices based on the full sample ( n = 1219)
Rights and permissions
Reprints and permissions
About this article
Whitaker, M.D., Brown, S. Is Mobile Addiction a Unique Addiction: Findings from an International Sample of University Students. Int J Ment Health Addiction 18 , 1360–1388 (2020). https://doi.org/10.1007/s11469-019-00155-5
Download citation
Published : 12 December 2019
Issue Date : October 2020
DOI : https://doi.org/10.1007/s11469-019-00155-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychological
- Physiological
- Find a journal
- Publish with us
- Track your research
- Research article
- Open access
- Published: 11 September 2020
The relationship of smartphone addiction with psychological distress and neuroticism among university medical students
- Leonard Yik-Chuan Lei 1 ,
- Muhd Al-Aarifin Ismail ORCID: orcid.org/0000-0001-5117-0489 1 ,
- Jamilah Al-Muhammady Mohammad 1 &
- Muhamad Saiful Bahri Yusoff 1
BMC Psychology volume 8 , Article number: 97 ( 2020 ) Cite this article
28k Accesses
41 Citations
1 Altmetric
Metrics details
Smartphone plays a vital role in higher education as it serves as a device with multiple functions. Smartphone addiction was reported on the rise among college and university students. The addiction may result in unwanted consequences on their academic performance and psychological health. One factor that consistently relates to psychological distress and smartphone addiction is the neurotic personality trait. This study explored the relationship of smartphone addiction with psychological health and neuroticism among USM medical students.
A cross-sectional study was carried out on medical students in a public medical school. DASS-21, the neuroticism-subscale of USMaP-i and SAS-SV were administered to measure psychological distress, neuroticism, and smartphone addiction of the medical students. Spearman correlation was performed to examine the correlation between smartphone addiction with psychological distress and neuroticism. Simple linear regression was performed to investigate relationship factors of smartphone addiction.
A total of 574 medical students participated in this study. The prevalence of smartphone addiction was 40.6%. It was higher among male (49.2%) compared to female (36.6%) medical students. The result showed a fair positive correlation between smartphone addiction and psychological health (rdepression = 0.277, p -value < 0.001; ranxiety = 0.312, p-value < 0.001; rstress = 0.329, p-value < 0.001). However, there was a poor positive correlation between smartphone addiction and neuroticism (r = 0.173, p -value < 0.001). The simple linear regression showed a significant increase in the levels of depression, anxiety, stress and neuroticism upon one unit increase in smartphone addiction (bdepression = 0.101, p -value < 0.001; banxiety = 0.120, p-value < 0.001; bstress = 0.132, p-value < 0.001; bneuroticism = 0.404, p-value < 0.05). These results indicated significant relationships between smartphone addiction, psychological health and neuroticism.
This study suggested a high prevalence of smartphone addiction among medical students, particularly in male medical students. The smartphone addiction might lead to psychological problems and the most vulnerable group is the medical student with the neurotic personality trait.
Peer Review reports
Smartphones possess the means to enrich learning activities from medical education in undergraduate and postgraduate training [ 1 ]. For example, smartphones are used in the pursuit of finding solutions to patient care, improving lifelong medical education, and professional partners through the use of social media [ 2 ]. With the advent of smartphones, its uses in higher education cannot be ignored and need to be examined to explore the consequences of its application. Smartphones can be defined as a hand-held device built as a mobile computing platform with advanced computing ability and connectivity. It serves to combine the functions of portable media players, low-end compact digital cameras, pocket video cameras, and GPS navigation units [ 3 ]. Furthermore, smartphones are being used for more than just a phone but rather a device that provides multiple functions including surfing the internet, email, navigation, social networking, and games [ 4 ].
Smartphones are gaining increasing importance in health care and researchers and developers are enticed with their applications related to health [ 5 ]. These devices have multiple features that can be positively employed which include speedy access to information, enhanced organization, and instantaneous communication [ 6 ] and can with certainty be used to enhance education [ 7 ]. However, smartphone addiction is a vital issue in the global population with problems comprising physical difficulties like muscular pain and eye illnesses, and psychological difficulties such as auditory and tactile delusion [ 8 ].
The use of smartphones reached figures over 50% in the majority of developed countries [ 9 ]. Malaysian Communications and Multimedia Commission (MCMC) has reported that in Malaysia, 24.5 million users have access to the internet in 2016 [ 10 ]. Smartphone stays as the most popular gadget for users to enter the internet (89.4%) creating a mobile-oriented country [ 10 ]. Over the past several years, there has been an increasing amount of studies that explored smartphone addiction [ 11 , 12 , 13 , 14 ]. The bulk of these studies focused on smartphone addiction and its potential influences on individuals [ 15 ]. On top of that, among Malaysian medical schools, two studies showed the prevalence of at-risk cases of developing smartphone addiction: 46.9% in Universiti Putra Malaysia (UPM) [ 16 ] and 52.2% in Universiti Teknologi MARA (UiTM) [ 17 ]. Several studies have reported a high prevalence of smartphone addiction: the prevalence of smartphone addiction in a Malaysian medical school was 46.9% [ 16 ], Saudi Arabian university students was 48% [ 18 ], Saudi Arabian dental students was 71.9% [ 19 ] and Indian medical students was 85.4% [ 20 ]. Conversely, some studies have reported a low prevalence of smartphone addiction: the prevalence of smartphone addiction in Chinese medical college students was 29.8% [ 4 ], Saudi Arabian students was 33.2% [ 21 ] and Saudi Arabian medical students was 36.5% [ 22 ]. These results suggested more than a quarter of students in higher education experienced smartphone addiction that requires further exploration of possible factors contributing to it as well as its consequences on students’ wellbeing.
Previous studies have shown links between smartphone addiction and depression [ 23 , 24 , 25 ], smartphone addiction and anxiety [ 26 , 27 , 28 , 29 ], smartphone addiction and stress [ 11 , 30 ], smartphone addiction and neuroticism [ 27 , 31 ]. However, these studies are in the general population and university students. Our study is looking at the specific population of medical students in a public medical school. Also, to the best of our knowledge, there are no studies in medical students that links smartphone addiction, psychological distress, and neurotic traits. Medical students use smartphones to facilitate retrieving information resources [ 32 , 33 , 34 ]. There is almost universal ownership of smartphones among medical students [ 35 ]. The applications on smartphones in medical education have reported to increase student involvement, improve the feedback process, and enhance communication between student and teacher [ 36 , 37 , 38 , 39 ]. Instant messaging smartphone applications such as WhatsApp can be used as a method to facilitate communication and education among groups of medical students [ 40 ]. It is important to know the effect of the increased use of smartphones in relation to psychological distress among medical students.
The study of smartphone addiction among medical students become vital as it enlightens us on smartphone usage. In Malaysia, there have been numerous studies on smartphone addiction [ 41 , 42 ]. However, there are not many studies done on smartphone addiction and its effects on medical undergraduates. Individuals measured with the personality trait that is high in neuroticism may be predisposed to addiction and behavioural problems [ 43 ]. Thus, we also decided to include the personality trait neuroticism as it is linked to addiction [ 44 , 45 ], and we are interested in studying the relationship between neuroticism and smartphone addiction. Neuroticism is present among medical students [ 46 ]. Medical students with neurotic tendencies behave negatively to academic stress, and this becomes a contributing factor to low academic performance [ 46 ]. Students with neuroticism are more vulnerable to smartphone addiction which can lead to psychological distress. The current research may play a role in developing intervention measures such as behavioral therapies and counseling. It also may serve to help medical students improve their awareness of their emotionality and its effect on smartphone use. Therefore, the primary focus of this study is to investigate the relationship of smartphone addiction with psychological distress and neuroticism among medical students.
Research hypothesis
The prevalence of smartphone addiction among USM medical students is more than 40%.
There is a significant correlation between smartphone addiction and depression among USM medical students.
There is a significant correlation between smartphone addiction and anxiety among USM medical students.
There is a significant correlation between smartphone addiction and stress among USM medical students.
There is a significant correlation between smartphone addiction and neuroticism among USM medical students.
Depression, anxiety, stress, and neuroticism significantly predict the smartphone addiction level.
Study sample
A cross-sectional study was carried out on year 1 to year 5 medical students in a public medical school in Malaysia. Before handing out the questionnaires, all students were informed about the study and their participation was voluntary. An informed consent to participate and publication was obtained from all participants. Bias was not explored in this study.
Sampling method and calculation
The sample size was determined by the single proportion size formula. The initial sample size calculation was based on a pilot study that involved students and staff [ 17 ] and the largest sample size needed was 384. After taking into account, 30% drop-out rate, the total number of sample size was 384/ (1–0.3) = 548. All medical students were included, those who did not sign the consent form were excluded from the study.
Data collection tools
There were three psychometric instruments used in this study; 1) Depression Anxiety Stress Scales (DASS-21); 2) modified USM Personality Inventory (USMaP-i); and 3) Smartphone Addiction Scale – Short Version (SAS-SV).
The DASS instrument was first introduced by Lovibond and Lovibond (1995) and delivered a self-reporting measure, which was created to evaluate the features associated to anxiety, stress, and depression. For each DASS-21 subscale, the score must be multiplied by two to simulate the DASS-42 version: the range of score from 0 to 42. A high score in each subscale is equal to a high degree of symptoms [ 47 ]. In a validation study done, the internal consistency of each subscale was high ranging from 0.70 for the stress sub-scale to 0.88 for the overall scale. The scores on each of the three subscales and the combinations of two or three of them were able to identify mental disorders of depression and anxiety in women with a sensitivity of 79.1% and a specificity of 77% at the optimal cut off of > 33 [ 23 ].
Modified USMaP-i
The USM Personality Inventory was created to measure the Big-Five Personality traits and is identified to be a reliable and valid instrument to evaluate the personality traits of prospective medical students [ 48 ]. This inventory was created explicitly to identify personal traits of Malaysian candidates who seek to apply to the medical course in USM [ 48 ]. The 15-item version of USMaP-i showed an acceptable level of internal consistency with each personality domain ranged from 0.64 and 0.84 as reported on the International Personality Item Pool Website [ 49 ]. We selected the 3 items that represent neuroticism to assess the neuroticism personality trait. Neuroticism is usually associated with features like depression, distress, anxiety, moodiness, poor coping ability, and sadness [ 50 ]. The total Cronbach alpha for the neuroticism subscale for USMaP-I is 0.722 [ 26 , 49 ].
The smartphone addiction scale was first developed and validated by Kwon, Lee et al. (2013) as a way to evaluate smartphone addiction in teenagers. This scale has shown to be validated with high psychometric sound properties in various countries [ 3 , 12 , 16 , 27 , 51 ]. The Smartphone Addiction Scale - Short Version (SAS-SV) is a validated scale that consists of ten items in the questionnaire that are used to measure the levels of smartphone addiction [ 3 ]. The total score is from 10 to 60. The coefficient for Cronbach alpha correlation obtained is 0.91 for Smartphone Addiction Short Version [ 3 ]. The strength of SAS-SV is that it can be used to discern a potentially high-risk group for smartphone addiction, both in the educational field and community [ 3 ]. The cut-off point for significant smartphone addiction for male is 31 and female is 33 based on the recommendation by Kwon et al. (2013).
Data collection
Data collection was performed via a self-guided questionnaire. Individuals were screened for one inclusion criteria and one exclusion criteria. Individuals who were medical students were eligible to participate (inclusion criteria). Individuals who were not willing to participate were not included in the study (exclusion criteria). Participants who submitted incomplete responses were excluded from this study.
Ethical consideration
Ethical clearance was obtained from the Human Research Ethics Committee of USM (JEPeM) with study protocol code (USM/JEPeM/18070352). Signed consents were taken from medical students. Instructions and information about this study were given to them. Each medical student was given an ID for tracing and profiling purposes. They were informed that the results of this study will not affect their academic results in any way. The questionnaires were distributed to all medical students after lecture sessions.
Statistical analysis
The data was analyzed using Statistical Package for Social Sciences (SPSS) version 24. Spearman correlation and simple linear regression tests were performed to examine the relationships of smartphone addiction with psychological distress and neuroticism. To accurately represent the relationship of smartphone addiction and neuroticism, the items in the modified USMaP-i were recoded due to negative items present in the neuroticism subscale: (Question 6 + Question 10 + Question 14). In the regression analysis, depression, anxiety, stress and neuroticism are independent variables and smartphone addiction is the dependent variable. A single regression analysis is used to account for the effects of multicollinearity because the correlation coefficient values of stress, depression, anxiety and neurotic tendencies are large. This research was not designed to investigate the gender differences and its correlations with depression, anxiety, stress and neuroticism. Further gender issues are not within the scope of this study.
Response rate
The survey’s response rate was 83.9% (574 out of 674). There was a higher proportion of female medical students (68.5%) than male medical students (31.5%). Malay students were the majority (65.3%) followed by Chinese (16%), Indian (15.5%) and other races (3.1%). The majority of students were between 19 and 23 years old. The proportion of students in each year of study was more or less similar or equal in numbers. Medical students that did not participate in the survey for reasons of lack of interest, time constraints, and fatigue.
In this study, the prevalence of smartphone addiction found was 40.6%. There is a higher prevalence of male students addicted to smartphone (49.2%) compared to the female students (36.6%). The results of this analysis can be seen in Table 1 .
Correlation of smartphone addiction, psychological distress and neuroticism
The correlation analysis for smartphone addiction with psychological health and neuroticism is shown in Table 2 . The result showed a fair positive correlation between smartphone addiction and psychological health among USM medical students (rdepression = 0.277, p -value < 0.001; ranxiety = 0.312, p-value < 0.001; rstress = 0.329, p-value < 0.001). However, there was a poor positive correlation between smartphone addiction and neuroticism (r = 0.173, p -value < 0.001).
Assumption was not met as normality of distribution was violated.
Linear regression of smartphone addiction, psychological distress and neuroticism
The regression analysis for smartphone addiction with psychological health and neuroticism is shown in Table 3 . The simple linear regression study showed a significant increase in depression, anxiety, stress and neuroticism levels upon one unit increase in smartphone addiction (bdepression = 0.101, p -value < 0.001; banxiety = 0.120, p-value < 0.001; bstress = 0.132, p -value < 0.001; bneuroticism = 0.404, p-value < 0.05). These results indicated significant relationships between smartphone addiction, psychological health and neuroticism. Smartphone addiction is a significant relationship factor of depression, anxiety and stress, while neuroticism is a significant relationship factor of smartphone addiction.
Prevalence of smartphone addiction
The prevalence of smartphone addiction among USM medical students was 40.6%; hypothesis 1 assumes the prevalence of smartphone addiction among USM medical students is more than 40%. This study reported that there is a higher prevalence of smartphone addiction among male medical students compared to female medical students, which is similar to a few other studies [ 4 , 52 , 53 ]. Other studies found a higher prevalence of smartphone addiction in females compared to males [ 3 , 12 , 22 , 54 , 55 ]. Interestingly, previous studies [ 24 , 25 ] did not report that gender is associated with smartphone addiction. The high prevalence of smartphone addiction (40.6%) in this study may be explained by smartphones becoming the main communication device among Malaysians and elsewhere. The percentage of smartphone consumers gradually rose from 68.7% in 2016 to 75.9% in 2017 [ 10 ]. Another observation is that medical students are using smartphones for social media messaging services such as WhatsApp and WeChat for communication purposes as well as for their studies, hence smartphones are becoming a vital tool in personal and professional life [ 56 ]. A study reported that WhatsApp assisted in easy learning and provided a way for clear communication of knowledge in shorter periods [ 57 ]. The higher prevalence of smartphone addiction in male medical students may be due to male medical students using their smartphone more for their entertainment such as online games while females use their smartphones for social interactions [ 58 , 59 , 60 ].
Relationship between smartphone addiction and depression
This study found a significant and fair positive correlation (r = 0.277) between smartphone addiction and depression, as in research hypothesis 2. Likewise, previous studies among adults reported a strong positive correlation between smartphone addiction and depression [ 28 ]. Other findings further support the fact that high levels of smartphone addiction were correlated with depression [ 29 ]. In the Malaysian context, a study among university students showed students who had high scores of smartphone addiction reported high scores of depression [ 61 ] that suggests a relationship between smartphone addiction and depression. Another study found that the group with high smartphone use showed greater levels of depression compared to the low smartphone use group among university students in Turkey [ 12 ]. However, other studies have found no relationship between smartphone addiction and depression [ 62 ]. These facts consistently suggested a positive correlation between smartphone addiction and depression.
The regression analysis showed the increase of smartphone addiction scores leads to the increase of depression scores, indicating it is a relationship factor. These results are similar to previous findings, in which smartphone addiction was reported to be found as a predictor of depression for undergraduates in a local Malaysian university [ 61 ]. Another study also supports this finding, in which it reported the severity of smartphone use predicted depression [ 12 ]. Conversely, previous studies reported vice-versa whereby depression predicted smartphone addiction among university students [ 25 , 30 , 63 ]. These facts suggested that smartphone uses among university students should be considered as high-risk behaviour that negatively affects their psychological health. There are several possible explanations for our results. Individuals with mood disorders are more prone to become a smartphone addict [ 64 ]. Lemola et.al (2015) reported that using electronic media at night is associated with sleep disturbances and depressive symptoms. One study stated that individuals with lower levels of self-perceived health conditions and emotions tended to display an excessive use of smartphones [ 65 ]. This suggested that individuals were in a constant cycle of attempting to compensate for their perceived health status, without being fully aware that smartphone addiction has undesirable implications to their physical, emotional, and social well-being.
The relationship between smartphone addiction and depression is evident in this study and shows that medical students that have smartphone addiction are at risk of having depression. Medical students displaying high levels of smartphone addiction and depression should be observed and given help if necessary. This can be done by promoting the responsible usage of smartphone use among medical students in activities. Sensible usage of smartphones is suggested, especially on younger adults who could be at greater risk of depression [ 28 ].
Relationship between smartphone addiction and anxiety
The results of our study indicate that there was a fair positive correlation between (r = 0.312) smartphone addiction and anxiety, as in research hypothesis 3. Demirci et, al. (2015) has found that smartphone use severity was positively correlated with anxiety and that corresponds with the findings in our study. Several other studies describe smartphone addictions are reported to increase with anxiety levels [ 54 , 55 , 66 , 67 ].
Our regression analysis revealed that increased smartphone addiction scores are a significant relationship factor in increased anxiety scores. Demirci et, al. (2015) reported that smartphone use severity predicted anxiety and it is consistent with our findings. A study reported that smartphone addiction was reported to be found as a predictor of anxiety in Malaysian undergraduate students [ 61 ]. In contrast, previous studies reported that anxiety significantly predicted smartphone addiction [ 25 , 31 , 63 ].
A possible explanation for our results is medical students may habitually check their smartphones in the likelihood of reducing their anxiety by receiving assurance through messages from their friends. The pattern of an individual checking his or her phone and receiving notifications also function in getting social reassurance behaviour from friends [ 68 ]. This behaviour of seeking reassurance can generally include symptoms of loneliness, depression, and anxiety that is the driving factor for reassurance seeking [ 68 ].
Relationship between smartphone addiction and stress
The results of this study indicate that there was a fair positive correlation between (r = 0.329) smartphone addiction and stress, as in research hypothesis 4. In another important finding, Samaha et, al. (2016) show the results between the risk of smartphone and perceived stress, reporting a slight positive correlation with an elevated risk of smartphone addiction associated with elevated levels of perceived stress which supports our study. Previous studies reported that stress leads to smartphone use [ 56 , 69 ], while another study proposes that smartphone use may cause stress [ 70 ]. In our regression analysis, increased smartphone addiction scores are a significant relationship factor in increased stress scores. Conversely, in a sample of Taiwanese university students reported a positive predictive effect of family and emotional stresses on smartphone addiction [ 11 ].
There are several explanations for the study results. Medical students are under stressful medical training [ 71 ], therefore they are prone to being under stress which in turn lowers self-control which may increase their chances of smartphone addiction. Smartphone addiction is influenced by self-control [ 72 ]. Self-control is defined as the capacity to alter one’s responses, such as overriding some impulses to bring behavior in line with goals and standards [ 73 ]. According to Cho et, al. (2017), an increase in stress degree results in a lowered self-control ability, and reduction in self-control further increases the chances of smartphone addiction.
Relationship between smartphone addiction and neuroticism
In this study, the results indicate that there is a poor positive correlation between (r = 0.173) smartphone addiction and neuroticism, as in research hypothesis 5. Neuroticism was reported to be significantly related to excessive use of smartphones [ 55 ] and corresponded with the findings of our study. These results are similar to other study findings reported that individuals who possessed high levels of neuroticism also report a high level of smartphone addiction [ 74 ]. In another study, neuroticism predicts problematic smartphone use [ 75 ]. However, the study [ 76 ] did not report a significant relationship between neuroticism and problematic phone use. In our regression analysis, increased neuroticism scores are a significant relationship factor in increased smartphone addiction scores. It was found neurotic personality increased the degree of smartphone addiction [ 55 ]. Problematic mobile use is positively associated with neuroticism [ 77 ]. There are several explanations for this result, medical students may be more vulnerable to smartphone addiction. The neuroticism trait has been linked to smartphone addiction [ 78 , 79 ]. A study stated that neuroticism is associated with a chain-mediating effect with smartphone addiction and depression, all vital variables that deteriorate the quality of life [ 80 ]. Apart from that, another study showed that there is a positive relationship between neuroticism and smartphone use while driving [ 81 ]. Another possible explanation is that medical students with neuroticism may depend on their smartphones to get reassurance from their friends. Individuals with high neuroticism tend to use their smartphones to get emotional and social reassurance from their relationships [ 82 ].
Implications and future research
Depression, anxiety, stress and neuroticism significantly predict smartphone addiction level, as in research hypothesis 6. The results show that there is a high prevalence of smartphone addiction among medical students. This means that a large proportion of students are affected by smartphone over usage and suggests a widespread occurrence that needs to be addressed by all relevant parties. It raises a deep concern because academic performances may be affected by a large number of medical students with smartphone addiction. As a consequence of smartphone addiction, individuals with smartphone addiction might meet with difficulties such as interpersonal adjustments, managing time, and academic performance [ 83 ]. This might affect the performance of the medical school as a whole in terms of academic results. The high prevalence of smartphone addiction in this study shows that they are at risk to have problems. Medical students displaying high levels of smartphone addiction should be monitored and given further help. Prevention is better than cure, thus smartphone addiction among medical students is recommended for early detection so that appropriate interventions can be planned accordingly. We also have to take into account the high prevalence of male medical students. Several approaches can be suggested to medical students who require further help for smartphone addiction; namely cognitive-behavioral approach, motivational interviewing, and behavioural cognitive treatment [ 84 ]. The implications for the intervention from the results of the study are to provide a baseline for research incorporating approaches tailored for medical students with smartphone addiction. This should address the most vulnerable group of students with the neuroticism personality trait.
Limitations and future research
Considering limited undergraduate smartphone addiction studies in the local setting, the results reported in this study provide insights into the professional health care team. It should be noted that smartphone usage is culturally bound experience and will contrast across countries with varying degrees of technology availability and advances in that region. This study does not report cause and effect relationships. Confounding variables were not studied. For example, in the curriculum at the medical school, each student has to go through e-learning (teaching and learning activities) and assessment that requires smartphone use. This suggests that in reality the medical students may be tasked with activities that require them to use their smartphones for education purposes, i.e. hours spent on smartphones for assignments and lectures. Further research can build upon our findings and investigate screening and interventions for smartphone addiction among medical students.
Conclusions
This study found the prevalence of smartphone addiction among medical students was high, particularly in male medical students. The smartphone addiction might lead to psychological problems and the most vulnerable group was students with the neuroticism personality trait. Thus, there is a need to create and implement programs to promote healthy smartphone usage to minimize the impact of smartphone addiction on psychological health. By doing so, one may implement effective intervention and prevention strategies to groups of students with smartphone addiction. We believe that with a proper guidance; students may be able to use their smartphones more responsibly.
Availability of data and materials
Data generated and analysed during the current study are not publicly available as individual privacy could be comprised; however, may be available from the corresponding author on reasonable request and with the permission of the medical school.
Abbreviations
Depression Anxiety Stress Scale
Human Research Ethics Committee of University Sains Malaysia
Malaysian Communication and Multimedia Commission
Smartphone Addiction Scale Short Version
School of Medical Sciences
Universiti Teknologi MARA
Universiti Putra Malaysia
Universiti Sains Malaysia
iUniversiti Sains Malaysia Personality Inventory
Masters K, Ellaway RH, Topps D, Archibald D, Hogue RJ. Mobile technologies in medical education: AMEE guide no. 105. Med Teach. 2016;38(6):537–49.
PubMed Google Scholar
Joshi N, Lin M. The smartphone: how it is transforming medical education, patient care, and professional collaboration. African J Emergency Med. 2013;4(3):152–4.
Google Scholar
Kwon M, Kim D-J, Cho H, Yang S. The smartphone addiction scale: development and validation of a short version for adolescents. PLoS One. 2013;8(12):e83558.
PubMed PubMed Central Google Scholar
Chen B, Liu F, Ding S, Ying X, Wang L, Wen Y. Gender differences in factors associated with smartphone addiction: a cross-sectional study among medical college students. BMC Psychiatry. 2017;17(1):341.
Sandholzer M, Deutsch T, Frese T, Winter A. Predictors of students’ self-reported adoption of a smartphone application for medical education in general practice. BMC Med Educ. 2015;15(1):91.
Robinson T, Cronin T, Ibrahim H, Jinks M, Molitor T, Newman J, et al. Smartphone use and acceptability among clinical medical students: a questionnaire-based study. J Med Syst. 2013;37(3):9936.
Almunawar MN, Anshari M, Susanto H, Chen CK. Revealing customer behavior on smartphones. Int J Asian Business Information Manage (IJABIM). 2015;6(2):33–49.
De-Sola J, Talledo H, Rubio G, de Fonseca FR. Development of a mobile phone addiction craving scale and its validation in a Spanish adult population. Front Psych. 2017;8:90.
Van Deursen AJ, Bolle CL, Hegner SM, Kommers PA. Modeling habitual and addictive smartphone behavior: the role of smartphone usage types, emotional intelligence, social stress, self-regulation, age, and gender. Comput Hum Behav. 2015;45:411–20.
Malaysian Communications And Multimedia Comission. Hand phone users Survery 2017; 2017. Available from: https://www.mcmc.gov.my/skmmgovmy/media/General/pdf/HPUS2017.pdf .
Chiu S-I. The relationship between life stress and smartphone addiction on Taiwanese university student: a mediation model of learning self-efficacy and social self-efficacy. Comput Hum Behav. 2014;34:49–57.
Demirci K, Akgönül M, Akpinar A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J Behav Addict. 2015;4(2):85–92.
Ghosh A, Jha R, Malakar SK. Pattern of smartphone use among MBBS students in an Indian medical college. IJAR. 2016;2(5):389–92.
Gowthami S, Kumar S. Impact of smartphone: a pilot study on positive and negative effects. Int J Scientific Eng Appl Sci (IJSEAS). 2016;2(3):473–8.
Toda M, Monden K, Kubo K, Morimoto K. Mobile phone dependence and health-related lifestyle of university students. Soc Behav Personal Int J. 2006;34(10):1277–84.
Ching SM, Yee A, Ramachandran V, Lim SMS, Sulaiman WAW, Foo YL, et al. Validation of a Malay version of the smartphone addiction scale among medical students in Malaysia. PLoS One. 2015;10(10):e0139337.
Nikmat AW, Hashim NA, Saidi MF, Zaki NSM, Shukri NNH, Abdulla NB. The use and addiction to smart phones among medical students and staffs in a public University in Malaysia. Asean J Psychiatry. 2018;19(1):98–104.
Aljomaa SS, Qudah MFA, Albursan IS, Bakhiet SF, Abduljabbar AS. Smartphone addiction among university students in the light of some variables. Comput Hum Behav. 2016;61:155–64.
Venkatesh E, Al Jemal MY, Al Samani AS. Smart phone usage and addiction among dental students in Saudi Arabia: a cross sectional study. Int J Adolesc Med Health. 2017;31(1). https://doi.org/10.1515/ijamh-2016-0133 .
Sethuraman AR, Rao S, Charlette L, Thatkar PV, Vincent V. Smartphone addiction among medical college students in the Andaman and Nicobar Islands. Int J Commun Med Public Health. 2018;5(10):4273–7.
Qudah MFA, Albursan IS, Bakhiet SFA, Hassan EMAH, Alfnan AA, Aljomaa SS, et al. Smartphone Addiction and Its Relationship with Cyberbullying Among University Students. Int J Ment Health Ad. 2019;17(3):628–43.
Alhazmi AA, Alzahrani SH, Baig M, Salawati EM, Alkatheri A. Prevalence and factors associated with smartphone addiction among medical students at king Abdulaziz University, Jeddah; 2018.
Tran TD, Tran T, Fisher J. Validation of the depression anxiety stress scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC Psychiatry. 2013;13(1):24.
Alosaimi FD, Alyahya H, Alshahwan H, Mahyijari NA, Shaik SA. Smartphone addiction among university students in Riyadh, Saudi Arabia. Saudi Med J. 2016;37(6):675–83.
Matar Boumosleh J, Jaalouk D. Depression, anxiety, and smartphone addiction in university students- a cross sectional study. PLoS One. 2017;12(8):e0182239.
Yusoff MSB, Rahim AFA, Aziz RA, Pa MNM, Mey SC, Ja'afar R, et al. The validity and reliability of the USM personality inventory (USMaP-i): its use to identify personality of future medical students. Intern Med J. 2011;18(4):283–7.
Kwon M, Lee J-Y, Won W-Y, Park J-W, Min J-A, Hahn C, et al. Development and validation of a smartphone addiction scale (SAS). PLoS One. 2013;8(2):e56936.
Alhassan AA, Alqadhib EM, Taha NW, Alahmari RA, Salam M, Almutairi AF. The relationship between addiction to smartphone usage and depression among adults: a cross sectional study. BMC Psychiatry. 2018;18(1):148.
Bian M, Leung L. Linking loneliness, shyness, smartphone addiction symptoms, and patterns of smartphone use to social capital. Soc Sci Comput Rev. 2015;33(1):61–79.
M-o K, Kim H, Kim K, Ju S, Choi J, Yu M. Smartphone addiction: (focused depression, aggression and impulsion) among college students. Indian J Sci Technol. 2015;8(25):1–6.
Hong ENC, Hao LZ, Kumar R, Ramendran C, Kadiresan V. An effectiveness of human resource management practices on employee retention in institute of higher learning: a regression analysis. Int J Bus Res Manag. 2012;3(2):60–79.
Jamal A, Temsah M-H, Khan SA, Al-Eyadhy A, Koppel C, Chiang MF. Mobile phone use among medical residents: a cross-sectional multicenter survey in Saudi Arabia. JMIR Mhealth Uhealth. 2016;4(2):e61.
Robinson R. Spectrum of tablet computer use by medical students and residents at an academic medical center. PeerJ. 2015;3:e1133.
Pulijala Y, Ma M, Ju X, Benington P, Ayoub A. Efficacy of three-dimensional visualization in mobile apps for patient education regarding orthognathic surgery. Int J Oral Maxillofac Surg. 2016;45(9):1081–5.
Browne G, O’Reilly D, Waters C, Tummon O, Devitt D, Stewart B, et al. Smart-phone and medical app use amongst Irish medical students: a survey of use and attitudes. In: BMC proceedings; 2015. BioMed Central.
Cochrane T, editor Mobile social media as a catalyst for pedagogical change. EdMedia+ innovate learning; 2014: Association for the Advancement of computing in education (AACE).
Makoe M. Exploring the use of MXit: a cell-phone social network to facilitate learning in distance education. Open Learning. 2010;25(3):251–7.
Nicholson S. Socialization in the “virtual hallway”: instant messaging in the asynchronous web-based distance education classroom. Internet High Educ. 2002;5(4):363–72.
Rambe P, Bere A. Using mobile instant messaging to leverage learner participation and transform pedagogy at a S outh a frican U niversity of T echnology. Br J Educ Technol. 2013;44(4):544–61.
Raiman L, Antbring R, Mahmood A. WhatsApp messenger as a tool to supplement medical education for medical students on clinical attachment. BMC Med Educ. 2017;17(1):7.
Parasuraman S, Sam AT, Yee SWK, Chuon BLC, Ren LY. Smartphone usage and increased risk of mobile phone addiction: a concurrent study. Int J Pharmaceutical Investigation. 2017;7(3):125–31.
Hakkı B, Muhammed FP. Investigating the smart phone addictions of vocational school students from different variables. Malaysian Online J Educ Technol. 2018;6(4):40–52.
Shaffer HJ, Hall MN, Vander BJ. "computer addiction": a critical consideration. Am J Orthopsychiatry. 2000;70(2):162.
Andreassen CS, Griffiths MD, Gjertsen SR, Krossbakken E, Kvam S, Pallesen S. The relationships between behavioral addictions and the five-factor model of personality. J Behav Addict. 2013;2(2):90.
Tsai HF, Cheng SH, Yeh TL, Shih C-C, Chen KC, Yang YC, et al. The risk factors of internet addiction—a survey of university freshmen. Psychiatry Res. 2009;167(3):294–9.
Bhagat V, Nayak RD. Neuroticism and academic performance of medical students. Int J Humanit Soc Sci Invent. 2014;3(1):51–5.
Lovibond SH, Lovibond PF. Psychology Foundation of a. manual for the depression anxiety stress scales. Sydney: Psychology Foundation of Australia; 1995.
Yusoff MSB. Stability of the USMaP-i in measuring the big five personality traits. Intern Med J. 2013;20(1):1–3.
Yusoff MSB. Construct validity, internal consistency and normative data of the USMaP-i in a sample of medical students; 2013. p. 1–7.
Goldberg LR, Johnson JA, Eber HW, Hogan R, Ashton MC, Cloninger CR, et al. The international personality item pool and the future of public-domain personality measures. J Res Pers. 2006;40(1):84–96.
De Pasquale C, Sciacca F, Hichy Z. Italian validation of smartphone addiction scale short version for adolescents and young adults (SAS-SV). Psychology. 2017;8(10):1513.
Chóliz M. Mobile-phone addiction in adolescence: the test of mobile phone dependence (TMD). Progress Health Sci. 2012;2(1):33–44.
Dixit S, Shukla H, Bhagwat A, Bindal A, Goyal A, Zaidi AK, et al. A study to evaluate mobile phone dependence among students of a medical college and associated hospital of Central India. Indian J Commun Med. 2010;35(2):339.
Choi S-W, Kim D-J, Choi J-S, Ahn H, Choi E-J, Song W-Y, et al. Comparison of risk and protective factors associated with smartphone addiction and internet addiction. J Behav Addict. 2015;4(4):308–14.
Mok J-Y, Choi S-W, Kim D-J, Choi J-S, Lee J, Ahn H, et al. Latent class analysis on internet and smartphone addiction in college students. Neuropsychiatr Dis Treat. 2014;10:817.
Wang J-L, Wang H-Z, Gaskin J, Wang L-H. The role of stress and motivation in problematic smartphone use among college students. Comput Hum Behav. 2015;53:181–8.
Barhoumi C. The effectiveness of WhatsApp Mobile learning activities guided by activity theory on Students' knowledge management. Contemp Educ Technol. 2015;6(3):221–38.
Cooper A, Morahan-Martin J, Mathy RM, Maheu M. Toward an increased understanding of user demographics in online sexual activities. J Sex Marital Therapy. 2002;28(2):105–29.
Fattore L, Melis M, Fadda P, Fratta W. Sex differences in addictive disorders. Front Neuroendocrinol. 2014;35(3):272–84.
Johansson A, Götestam KG. Internet addiction: characteristics of a questionnaire and prevalence in Norwegian youth (12–18 years). Scand J Psychol. 2004;45(3):223–9.
Ithnain N, Ezzat Ghazali S, Jaafar N. Relationship between smartphone addiction with anxiety and depression among undergraduate students in Malaysia; 2018. p. 163–71.
Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A. Adolescents’ electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. J Youth Adolesc. 2015;44(2):405–18.
Aker S, Sahin MK, Sezgin S, Oguz G. Psychosocial factors affecting smartphone addiction in university students. J Addict Nurs. 2017;28(4):215–9.
Zhang KZ, Chen C, Lee MK. Understanding the role of motives in smartphone addictionPACIS; 2014.
Kim HJ, Min JY, Min KB. Association between psychological and self-assessed health status and smartphone overuse among Korean college students. J Ment Health. 2019;28(1):11–6.
Hwang K-H, Y-s Y, Cho O-H. Smartphone overuse and upper extremity pain, anxiety, depression, and interpersonal relationships among college students. J Korea Contents Assoc. 2012;12(10):365–75.
Haug S, Castro RP, Kwon M, Filler A, Kowatsch T, Schaub MP. Smartphone use and smartphone addiction among young people in Switzerland. J Behav Addict. 2015;4(4):299–307.
Billieux J, Maurage P, Lopez-Fernandez O, Kuss DJ, Griffiths MD. Can disordered mobile phone use be considered a behavioral addiction? An update on current evidence and a comprehensive model for future research. Curr Addict Rep. 2015;2(2):156–62.
Jeong S-H, Kim H, Yum J-Y, Hwang Y. What type of content are smartphone users addicted to?: SNS vs. games. Comput Hum Behav. 2016;54:10–7.
Murdock KK. Texting while stressed: implications for students’ burnout, sleep, and well-being. Psychol Pop Media Cult. 2013;2(4):207.
Yusoff MSB, Rahim AFA, Yaacob MJ. Prevalence and sources of stress among Universiti Sains Malaysia medical students. Malaysian J Medical Sci. 2010;17(1):30.
Kim N, Lee K. Effects of self-control and life stress on smart phone addiction of university students. J Korea Soc Health Informatics Stat. 2012;37(2):72–83.
Baumeister RF, Heatherton TF, Tice DM. Losing control: how and why people fail at self-regulation: academic press; 1994.
Toda M, Ezoe S, Mure K, Takeshita T. Relationship of smartphone dependence to general health status and personality traits among university students. Open J Prev Med. 2016;6(10):215–21.
Horwood S, Anglim J. Personality and problematic smartphone use: a facet-level analysis using the five factor model and HEXACO frameworks. Comput Hum Behav. 2018;85:349–59.
Bianchi A, Phillips JG. Psychological predictors of problem mobile phone use. Cyberpsychol Behav. 2005;8(1):39–51.
Augner C, Hacker GW. Associations between problematic mobile phone use and psychological parameters in young adults. Int J Public Health. 2012;57(2):437–41.
Pearson C, Hussain Z. Smartphone Use, Addiction, Narcissism, and Personality: A Mixed Methods Investigation. Int J Cyber Behav Psychol Learn. 2015;5:17–32.
Roberts JA, Pullig C, Manolis C. I need my smartphone: a hierarchical model of personality and cell-phone addiction. Personal Individ Differ. 2015;79:13–9.
Gao T, Xiang Y-T, Zhang H, Zhang Z, Mei S. Neuroticism and quality of life: multiple mediating effects of smartphone addiction and depression. Psychiatry Res. 2017;258:457–61.
Luria G. The mediating role of smartphone addiction on the relationship between personality and young drivers' smartphone use while driving. Transport Res F: Traffic Psychol Behav. 2018;59:203–11.
Kim J-H, Seo M, David P. Alleviating depression only to become problematic mobile phone users: can face-to-face communication be the antidote? Comput Hum Behav. 2015;51:440–7.
Hong F-Y, Chiu S-I, Huang D-H. A model of the relationship between psychological characteristics, mobile phone addiction and use of mobile phones by Taiwanese university female students. Comput Hum Behav. 2012;28(6):2152–9.
Kim H. Exercise rehabilitation for smartphone addiction. J Exercise Rehabilitation. 2013;9(6):500.
Download references
Acknowledgements
Not applicable.
The authors received no specific funding for this work.
Author information
Authors and affiliations.
Department of Medical Education, School of Medical Sciences, Universiti Sains Malaysia (USM), Health Campus, Kubang Kerian, Malaysia
Leonard Yik-Chuan Lei, Muhd Al-Aarifin Ismail, Jamilah Al-Muhammady Mohammad & Muhamad Saiful Bahri Yusoff
You can also search for this author in PubMed Google Scholar
Contributions
LLYC, the first author, made significant contributions to the research design, data collection and interpretation, and writing of the manuscript. MAAI, JAMM and MSBY who have expertise in quantitative research, were involved in the research design and the collection and interpretation of the data. MSBY contributed to the collection and interpretation of the data and the writing of the manuscript. MAAI, JAMM also contributed significantly to the writing of the manuscript. All the authors have critically reviewed and approved the final draft and are responsible for the content of the manuscript.
Author’s information
Ismail MA-A is a medical doctor and currently works as a Medical Educationist at the Medical Education Department, Universiti Sains Malaysia. He is coordinator for E-learning programme of the medical school. His research interest is in technology-enhanced teaching and learning and teaching evaluation.
Mohammad JA-M is a medical doctor and currently works as a Medical Educationist and Master in Science (Medical Education) Programme Coordinator at the Department of Medical Education, Universiti Sains Malaysia. Her research interests include mentoring, student assessment including formative assessment in teaching and learning.
Yusoff MSB is an Associate Professor and Head, Department of Medical Education, School of Medical Sciences USM. His research interest includes medical student wellbeing, assessment, validity, reliability, development of psychological measurement, stress management, medical student admission, feedback, emotional intelligence, and personality.
Corresponding author
Correspondence to Muhd Al-Aarifin Ismail .
Ethics declarations
Ethics approval and consent to participate.
Jawantankuasa Etika Penyelidikan Manusia Universiti Sains Malaysia (JEPeM) reviewed this study’s protocol code (USM/JEPeM/18070352) and granted ethical approval and consent from 18th October 2018 until 17th October 2019. Signed consents were taken from medical students taking part in the study.
Consent for publication
Written consent for publication was obtained from each participant.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lei, L.YC., Ismail, M.AA., Mohammad, J.AM. et al. The relationship of smartphone addiction with psychological distress and neuroticism among university medical students. BMC Psychol 8 , 97 (2020). https://doi.org/10.1186/s40359-020-00466-6
Download citation
Received : 09 March 2020
Accepted : 04 September 2020
Published : 11 September 2020
DOI : https://doi.org/10.1186/s40359-020-00466-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Smartphone addiction
- Medical students
- Psychological distress
- Neuroticism
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- Open access
- Published: 12 August 2022
Adolescent mobile phone addiction during the COVID-19 pandemic predicts subsequent suicide risk: a two-wave longitudinal study
- Gangqin Li 1 ,
- Aldo Alberto Conti 2 ,
- Changjian Qiu 3 &
- Wanjie Tang 2 , 3
BMC Public Health volume 22 , Article number: 1537 ( 2022 ) Cite this article
7383 Accesses
9 Citations
1 Altmetric
Metrics details
Both the rate of mobile phone addiction and suicidality among adolescents have increased during the pandemic lockdown. However, the relationship between mobile phone addiction and suicide risk and the underlying psychological mechanisms remains unknown. This study examined the associations between mobile phone addiction in adolescents during the first month of lockdown and the suicide risk in the subsequent five months. A two-wave short-term longitudinal web-based survey was conducted on 1609 senior high school students (mean age = 16.53 years, SD = 0.97 years; 63.5% female). At Time 1 (T1), the severity of mobile phone addiction and basic demographic information was collected from Feb 24 to 28, 2020 in Sichuan Province, China (at the pandemic’s peak). Five months later, between July 11 and July 23 (Time 2, T2), mobile phone addiction, daytime sleepiness, depression, and suicidality were measured within the past five months. The regression analysis revealed that mobile phone addiction during quarantine directly predicted suicidality within the next five months, even after controlling for the effect of depression and daytime sleepiness. Meanwhile, mobile phone addiction at T1 also indirectly predicted suicidality at T2, with depression and daytime sleepiness mediating this association. Programs targeting improvement of daytime sleepiness and depressive symptoms may be particularly effective in reducing suicide risk among adolescents with mobile phone addiction.
Peer Review reports
Introduction
COVID-19 emerged in late 2019 and forced many countries to implement quarantine measures, such as lockdowns, home confinement, self-isolation, and social distancing [ 1 ], which raise public health concerns [ 2 , 3 ]. Because school-aged children had to take online classes from home during the pandemic, there was a significant increase in their use of mobile phones [ 4 , 5 ], which led to the rise in mobile phone addiction [ 6 , 7 , 8 ]. It has also been found that pandemic lockdown measures resulted in a rise in negative emotions in adolescents, which manifested as sleep problems [ 9 ], anxiety, depression, and suicidality [ 10 , 11 , 12 , 13 , 14 ]. Indeed, youth suicide risk has become a significant global health concern during the pandemic [ 15 , 16 ]. However, neither the connection between mobile phone addiction and the increased suicide risk during the pandemic, nor the associated psychosocial mechanisms, have been adequately explored [ 17 , 18 ]. Therefore, to fully understand the underlying mechanisms in the relationship between adolescent mobile phone addiction and suicidality during the COVID-19 pandemic, there has been a call for more profound investigative research [ 19 , 20 , 21 , 22 ].
COVID-19 and suicidality
Many studies have investigated suicidality during the COVID-19 pandemic. For example, Every-Palmer et al. (2020) surveyed 2010 New Zealand adults in April 2020 and found that 6% had suicidal ideation and 2% had attempted suicide [ 23 ]. Iob et al. (2020) reported that 18% ( n = 7984) of 44,775 adults in the UK had experienced thoughts of suicide or self-harm, and 5% ( n = 2174) had harmed themselves at least once in the first month of the COVID-19 lockdown. Czeisler et al. (2020) surveyed 5412 United States adults and found that 10.7% had seriously considered suicide in the 30 days before completing the survey [ 24 ]. Wang et al. (2020) reported that 18.04% of 2031 undergraduate and graduate students in the United States had experienced suicidal ideation during the COVID-19 pandemic, and Sun et al. (2021) found that 19.56% of Chinese university students had had suicidal ideation during the COVID-19 quarantine. However, a study in Spain did not find any significant change in the overall suicidal ideation prevalence before and after the COVID-19 outbreak [ 25 ],. Similarly, Isumi et al. (2020) found that the suicide rates in children and adolescents under 20 during the school closures from March to May 2020 in Japan did not change significantly compared with the same period in 2018 and 2019.
Although many studies have investigated the rate of suicidal ideation or behaviors during the COVID-19 crisis, several research gaps need to be addressed: 1) the majority of the studies have only reported the rate of suicidal ideation, attempts, or behaviors, but few studies have investigated the underlying suicidality mechanisms; 2) most previous studies have been cross-sectional rather than longitudinal; however, as the pandemic psychological sequelae may persist for months and years to come and peak later than the actual pandemic [ 26 ], longitudinal or follow up studies are needed; 3) most studies on pandemic related suicidality have been conducted on adults, yet adolescents are vulnerable to negative emotions and may be particularly disposed to suicidality [ 27 , 28 ], therefore, longitudinal studies on suicidality and the related mechanisms in adolescents are needed.
Mobile phone addiction and suicidality
Mobile phone addiction is defined as the inability to regulate personal mobile phone use, which can eventually lead to symptoms similar to substance abuse disorders, such as compulsive use, withdrawal, cravings, loss of control, and mood dysregulation [ 29 ]. A significant increase in mobile phone use and addiction has been found in many COVID-19 studies. For example, Zhang et al. (2021) found an elevated risk of problematic mobile phone use in Chinese adults during the COVID-19 pandemic, with the prevalence being as high as 43.3%. Saadeh et al. (2021) reported a 62.4% mobile phone addiction prevalence in 6154 Jordanian undergraduates during the COVID-19 quarantine, and Caponnetto et al. (2021) and Serra et al. (2021) both found a growth in pathological cell phone use during the Italian COVID-19 lockdown.
Several studies have also found that mobile phone addiction could result in several physical and mental health issues, such as dry eyes, migraine headaches, sleep disorders, intellectual impairment, depression, and anxiety [ 30 , 31 , 32 ]. However, only a few studies have investigated the associations between mobile phone addiction and suicidality. For example, Chen et al. (2020) found that high mobile phone use intensity directly predicted suicide-related behaviors in Chinese adolescents and that depression mediated this relationship [ 33 ]. Ismail et al.(2020) found that smartphone addiction was positively associated with suicidality in Malaysian college students; however, no predictive effects were identified in this association [ 34 ].
Pathways from mobile phone addiction to suicidality
It has been found that mobile phone addiction can lead to adverse psychological sequelae, with depression and sleep disturbance being the most commonly reported [ 35 , 36 , 37 ]. For example, Lemola et al. (2015) found excessive mobile phone use at night to cause sleep difficulties, depression, and stress in adolescents [ 38 ]. Demirci et al. (2015) reported positive correlations between mobile phone addiction scale scores, depression levels, and sleep quality scores [ 39 ]. Thomee et al.’s (2011) longitudinal study revealed an association between high-frequency mobile phone use, sleep disturbances, and depression at a one-year follow-up on 4156 young adults [ 40 ]. Elhai et al.(2017) conducted a literature review and found that nine of 10 included studies reported at least medium effect size associations between problematic smartphone use and the depression severity [ 41 ]. Other cross-sectional studies revealed correlations between high levels of mobile phone addiction severity and poor sleep quality [ 42 , 43 , 44 ].
In addition to the association with mobile phone addiction, depression and sleep disorders have also been associated with suicidality [ 45 , 46 , 47 ]. For example, Bernert et al.’s (2015) systematic review concluded preliminary, converging evidence that sleep disturbances were an empirical risk factor for suicidal behaviors. Liu et al. (2004) found that sleeping less than eight hours and frequent nightmares were significantly associated with an increased risk of suicide attempts in adolescents. Wang et al. (2021) found that sleep disturbances could prospectively predict the development and persistence of suicidal ideation. Daytime sleepiness, defined as an inability to maintain wakefulness and alertness during the day [ 48 ], is one of the most common sleep disturbance sequelae [ 49 ], which is most directly associated with daytime dysfunction. Notably, studies have proposed that daytime sleepiness may mediate the association between mobile phone addiction and PTSD in adolescents during COVID-19 (Hu, Wang, et al., 2021). It is also possible for daytime sleepiness to play a mediating role between mobile phone addiction and suicidality [ 50 , 51 ].
Therefore, as mobile phone addiction can result in depression, sleep disturbances, and daytime sleepiness, which in turn may increase suicidality, it is reasonable to assume that depression and daytime sleepiness could mediate between mobile phone addiction and suicidality. However, the above evidence illustrates that only a few studies have explored the underlying mediating mechanisms between mobile phone addiction and suicidality in a longitudinal design. For instance, a Chinese study has shown that depression mediates the relationship between mobile phone addiction and suicidal behavior in adolescents in a cross-sectional study [ 52 ]. Another study found that insomnia and depression mediated the relationship between internet gaming addiction and suicidal ideation [ 53 ]. As prior studies have been primarily cross-sectional, there is a need to conduct longitudinal studies investigating these associations, and the underlying mechanisms, in adolescents during the COVID-19pandemic.
The present study
Research into the complex interactions and associations between mobile phone addiction, suicidality, depression, and daytime sleepiness could provide a more comprehensive understanding of the potential suicidality mechanisms. Therefore, this study was a two-wave longitudinal study aimed at investigating: (a) the severity of mobile phone addiction in Chinese adolescent students during the COVID-19 quarantine (Time 1, T1), and (b) the suicide risk five months later (Time 2, T2) when the pandemic was in remission in China. Specifically, we tested the following hypotheses: (1) That mobile phone addiction (T1) would be positively correlated with suicidality (T2); (2) That mobile phone addiction (T1) would predict suicidality (T2); (3) That depression and daytime sleepiness would mediate the link between mobile phone addiction (T1) and suicidality (T2). These findings may advance the understanding of how and when mobile phone addiction causes suicidality and how to protect adolescents from the unfavorable impacts of excessive mobile phone use.
Participants and procedures
Students from two senior high schools (12 ~ 18 years old, those over 18 are excluded) in Sichuan province, China, were invited to participate in an online survey for basic demographic information on mobile phone addiction from February 24 to 28, 2020 (T1, about one month after the national lockdown in China that began on January 21, 2020). Five months later, between July 11 and July 23 (Time 2, T2), mobile phone addiction, daytime sleepiness, depression, and suicidality in the past five months were measured. In Sichuan Province, the state lockdown was lifted at the end of March 2020, and students returned to school in early April. Therefore, the COVID-19 pandemic was considered in remission at Time 2.
This study was approved by the Ethics Committee of the Sichuan Psychological Society (NO. 2020_12). Informed consent was given online by participants and their statutory guardians. This survey was part of the Surveys on the Behavior and Psychological Health Project affected by COVID-19.
Measures included demographic variables, pandemic exposure questionnaires, and four psychopathological conditions, including mobile phone addiction, depressive symptoms, daytime sleepiness, and suicidal ideation or attempts. At T1, we measured mainly what happened in the past month, within the first month during the lockdown. At T2, we measured mainly what occurred in the past five months, that is, within the five months between T1 and T2.
Demographic variables and COVID-19 related exposure
Demographic information on age, gender, and grade level was collected. COVID-19 exposure was evaluated with three yes/no questions derived from previous traumatic studies [ 54 , 55 ], whether a friend or relative had been infected with COVID-19; whether the participants lived in a community in which someone was infected; whether the participants had a friend or relative who had died of COVID-19.
Mobile Phone Addiction Index (MPAI)
Mobile phone addiction at T1 was assessed using the Chinese version of the Mobile phone Addiction Index (MPAI) [ 56 ], which was a self-report questionnaire with 17 items under four subscales: losing control and receiving complaints; anxiety, and cravings; withdrawal/escape; and productivity loss. At T1, MPAI was measured within the first month of the lockdown. The participants were required to rate each item on a five-point Likert scale ranging from 1 = never to 5 = very often. The total MPAI score ranged from 17 to 85, with higher scores indicating a higher intensity of mobile phone use and 51 or above showing mobile phone addiction [ 57 ]. In the present study, the Cronbach’s a is 0.92 at T1 and 0.94 for the T2.
- Daytime sleepiness
The participants’ daytime sleepiness at T2 was evaluated using the Chinese Adolescent Daytime Sleepiness Scale (CADSS) [ 58 ] for the past five months between T1 and T2. The CADSS comprised seven items; each scored on a five-point Likert scale. Higher scores indicate more severe daytime sleepiness (Range = 7–35), and a score greater than 16 indicates excessive daytime sleepiness. In the current study, Cronbach’s α was 0.89.
Depression at T2 was assessed using the abbreviated Kutcher Adolescent Depression Scale (KADS) in the past five months, with six items and a self-report scale to diagnose adolescent depression and its severity [ 59 ]. This scale has been used on Chinese children and adolescents and has shown good internal and test–retest reliability [ 60 ]. The total KADS score ranged from 0 to 18, with scores ≥ 6 indicating possible depression. The Cronbach’s α in the current study was 0.91.
- Suicidality
At T2, suicidality in the past five months between T1 and T2 was measured using the modified Chinese version of the Suicidal Behaviors Questionnaire-Revised (SBQ-R) [ 61 ], which is a brief suicidality self-reported scale that has four questions, such as “Have you ever thought about or attempted to kill yourself in the past five months?” marked on a Likert scale on the frequency of suicidal ideation or attempts, with the total score ranging from 3 to 18 and scores ≥ 7 indicating a non-clinically significant risk of suicide. This questionnaire's good psychometric properties have been reported in previous studies on Chinese adolescents and young adults [ 62 ]. In the present study, Cronbach’s α was 0.76.
Data analysis
Pearson’s correlation analysis was used to examine the clinical variable associations; To identify whether and how much variance mobile phone addiction at T1 were independent predictors of subsequent suicidal risk, stepwise and enter regression analyses were carried out while controlling for demographic and COVID-19 exposure factors, daytime sleepiness, and depressive symptoms step by step. The mediation analysis adopts PROCESS model 6 [ 63 ], which allows four variables to exist in a chain effect to examine the mediating effects of daytime sleepiness/depression on the associations between mobile phone addiction and suicidality. The indirect effects and 95% bootstrap confidence intervals (CI) were calculated on 5000 bootstrapped samples as conducting the bootstrap resampling method requires at least 2000 replications [ 64 ] and more bootstrapped samples improve estimation [ 65 ]. The statistical analyses were conducted using SPSS version 22.0.
Demographic information and COVID-19 exposure
Two thousand three hundred ninety-nine participants were initially surveyed from the two senior high schools; 1609 (73.6%) completed the T1 and T2 surveys. The mean age for these 1609 adolescents (range 12 ~ 18 years old) was 16.53 (SD = 0.97) years, 1021 (63.5%) of whom were female. Three hundred and twenty-two (20.0%) students reported suicidal ideation or suicide attempts at T2, 207(64.3%) females. The detailed sample characteristics are presented in Table 1 . Suicidality stratified by demographic and exposure variables were displayed in Table 2 .
Correlations between the main variables
Mobile phone addiction at T1 was significantly correlated with daytime sleepiness ( r = 0.316), depression ( r = 0.312), and suicidality ( r = 0.289) at T2. Meanwhile, suicidality at T2 was significantly correlated with depression at T2 ( r = 0.469) and daytime sleepiness at T2 was also significantly correlated with suicidality at T2 ( r = 0.311). Details are present in Table 3 . The correlations between these four variables indicated that subsequent regression was needed.
The chain mediation model
The pathways between the main variables are shown in Table 4 and Fig. 1 . The total standardized effect of the three variables on the outcome variable of suicidality was 0.29 (95% CI [0.24, 0.34], F = 146.12, p < 0.001). Mobile phone addiction at T1 was significantly directly related to suicidality at T2 (β = 0.13; 95%CI: 0.08–0.17; p < 0.001). Additionally, Mobile phone addiction had indirect effects on suicidality at T2 through daytime sleepiness (β = 0.04, SE = 0.01, 95%CI = 0.02–0.06), and depression (β = 0.08, SE = 0.01, 95%CI = 0.06–0.11) respectively. Furthermore, mediation paths of mobile phone addiction → daytime sleepiness → depression → suicidality (β = 0.04, SE = 0.01, 95%CI = 0.03–0.05) was also identified by the mediation analyses.
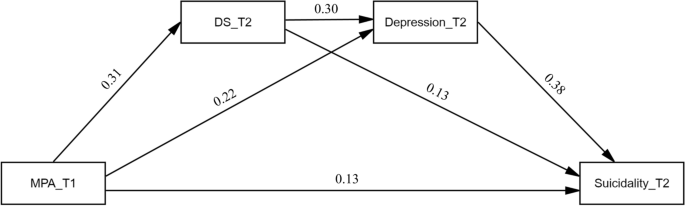
The standardized path coefficients in chain mediation model. MPA_T1: Time 1 smartphone addiction score; DS_T2: Time 2 daytime sleepiness score; Depression_T2: Time 2 depression score; Suicidality_T2: Time 2 suicidality score
Stepwise linear regression analysis results
In our data, earlier mobile phone addiction could directly predict subsequent suicidal risk when controlling for age, gender, exposures, depressive symptoms and daytime sleepiness (β = 0.13, t = 5.60, ΔR 2 = 0.015, p < 0.001) (see Table 5 ). Depression_T2 and daytime sleepiness_T2 were also significant risk factors for suicidality_T2 in the regression model, with depression showing the most statistical significance.
This study is one of the few longitudinal studies that have examined the associations between mobile phone addiction and suicidality in adolescents during COVID-19. It was found that mobile phone addiction during the COVID-19 quarantine period could directly predict suicidality in the subsequent five months even after controlling for the effect of depression and daytime sleepiness. In addition, mediation analysis showed that mobile phone addiction during the COVID-19 quarantine period could indirectly predict suicidality in the following five months, with depression and daytime sleepiness mediating in this association.
Mobile phone addiction predicts suicidality regardless of mental health problems and other covariables
The regression analysis revealed that mobile phone addiction during the COVID-19 quarantine period could directly predict suicidality independent of covariables such as mental health and psychosocial factors in the subsequent five months. Several previous correlation studies supported this result. For example, Steinbüchel reported that 48.3% of the patients with Internet addiction (with and without comorbidity) exhibited significantly more often suicidal symptoms as compared to healthy controls (3.5%) [ 66 ]. Two nationally representative surveys of U.S. adolescents ( N = 506,820) reported that among those who used electronic devices five or more hours a day, 48% had at least one suicide-related outcome [ 67 ]. Furthermore, the meta-analysis also found an increased risk of suicidal behavior in adolescents with internet addiction [ 68 ].
Our results confirmed and extended a previous cross-sectional study that internet overuse by children and adolescents in the context of COVID-19 could elevate their risks for self-injured behavior [ 69 ]. Actually, both the rate of phone addiction [ 70 ] and the risk of suicide [ 71 , 72 ] among teenagers have risen dramatically during the pandemic although few studies, especially longitudinal design, confirmed the relationship between mobile phone overuse and subsequent suicide risk. Therefore, our study has important implications for considering the important role of mobile phone addiction when enacting suicide prevention programs for adolescents.
Mobile phone addiction has been related to various negative psychosocial consequences, which may contribute to subsequent suicidality. Schutten et al. reported that heavy media addiction was at risk for problematic behaviors such as substance abuse, overeating, problematic gambling, and poor financial management [ 73 ]. These unhealthy lifestyles would result in poor life performance, daily life function, social relationships, and academic or occupational achievements [ 74 , 75 , 76 ]. Furthermore, heavy screen-addicted adolescents were also found to have less social support and attachment with family and peers[ 77 , 78 , 79 ]. Poor social support would increase the risk of further isolation and loneliness, leading to suicidality [ 80 , 81 , 82 ].
In addition to the negative psychosocial consequences, mobile phones and internet addiction has been also associated to structural and functional abnormalities in brain areas related to cognitive control and emotional regulation. For example, Cheng and Liu found that internet addiction subjects had decreased negative functional connectivity (FC) between the dorsolateral prefrontal cortex (DLPFC) and amygdala [ 83 ], which is responsible for emotion-cognition interactions [ 84 ]. Turel et al. showed that Facebook users with addiction-like symptoms have a hyperactive amygdala-striatal system [ 85 ]. He et al. found that social network site addiction is associated with a more impulsive brain system, manifested through reduced gray matter volumes in the amygdala bilaterally [ 86 ]. Similarly, Dong et al. found that males with Internet addiction showed significantly greater ‘Stroop effect’-related activity in the anterior and posterior cingulate cortices than healthy males, indicating diminished efficiency of response-inhibition processes [ 87 ].
Depression was a mediator between mobile phone addiction and suicidality
The mediation analysis identified a pathway from mobile phone addiction to depression to suicidality, which confirmed the mediating role of depression in the association between mobile phone addiction and suicidality. This result was consistent with a previous cross-sectional study reporting that depression mediated the relationship between high-intensity mobile phone use and suicide-related behaviors in Chinese adolescents [ 33 ]. Depression has been one of the most commonly reported adverse psychological sequelae associated with mobile phone addiction, which is characterized by depressive moods, such as adolescent feelings of irritability or emptiness, diminished interest, loss of pleasure, feelings of hopelessness and worthlessness, changes in appetite or sleep, and reduced energy or fatigue.
Several reasons have been proposed for the pathogenesis of addiction-related depression. First, mobile phone addiction can lead to work or school performance impairments [ 88 ], which could induce criticism, blame, or arguments from teachers and family members, which could, in turn, lead to impaired social relationships, low self-esteem, and negative emotions, such as depression [ 29 ]. This may result in a more compulsive mobile phone use to escape these real-world problems and alleviate any negative emotions [ 30 , 89 ]. Therefore, there seems to be a vicious cycle between mobile phone addiction and depression and subsequent suicidality risk [ 41 ]. As depression has long been recognized as one of the most critical risk factors for suicide prediction [ 45 , 47 ], more attention needs to be paid to its presence when screening people with mobile phone addiction and the intervening suicidality. As it may be challenging to evaluate the severity of the negative influence of mobile phone addiction and when and how to implement an intervention, the presence of depression could be a valuable warning sign; that is, greater attention should be focused on adolescent mobile phone addicts who also have depressive symptoms.
Daytime sleepiness was a mediator between mobile phone addiction and suicidality
The mediation analysis indicated that mobile phone addiction was associated with suicidality, and daytime sleepiness mediated this association. Daytime sleepiness, defined as the inability to maintain wakefulness and alertness during the day [ 48 ], is one of the most common sleep disturbance sequelae [ 49 ]. Adolescents with mobile phone addiction tend to spend more time on their mobile phones at night, which often leads to decreased sleep duration and circadian rhythm disturbances from the mobile phone’s light and electromagnetic fields that can negatively influence serum melatonin and cerebral blood flow [ 90 , 91 , 92 ]. Extensive mobile phone use can also result in frequent headaches, tension, fatigue, and vertigo [ 93 ], resulting in sleep disturbances.
Sleep disturbance has also been identified as a risk factor for suicidality [ 94 ]. For example, a recent two-year follow-up study found that shorter sleep duration at the baseline was associated with an increased suicidality risk in school-aged boys [ 95 ], and another longitudinal analysis found that short sleep durations predicted the onset or persistence of suicidal ideation [ 96 ]. One possible mechanism for this association may be that sleep deprivation and circadian disturbances compromise frontal lobe/executive functions, diminish problem-solving abilities, and increase impulsive behavior, increasing the likelihood of suicide [ 97 ]. Insufficient sleep can also lead to mood regulation impairments and improve suicide ideation [ 98 ] and has been associated with hypothalamus/hypothalamic–pituitary–adrenal (HPA) axis dysregulation, which has been linked to depression and suicidality risk [ 99 , 100 , 101 ].
Daytime sleepiness has been strongly associated with sleep disturbance, which is more directly associated with daytime dysfunction compared to sleep disturbance. This study identified the mediating role of daytime sleepiness on the association between mobile phone addiction and suicidality. Although these are only preliminary results, they highlight that it is essential to monitor daytime sleepiness carefully, especially in adolescents with mobile phone addiction.
Daytime sleepiness and depression as chain mediation between mobile phone addiction and suicidality
Our study adds to previous research showing that mobile phone addiction could affect daytime sleepiness which contributes to depressive symptoms, and subsequently increases the risk of suicide. This chain mediating effects highlights daytime sleepiness may be a precursor to depressive symptoms, especially among teenagers who are heavily exposed to mobile phone use. Our results were partly consistent with a previous Korean study indicating that insufficient sleep time and feeling sleepy during the day in adolescence was significantly associated with depression [ 102 ]. Therefore, monitoring sleep duration in adolescents and reducing daytime dozing may effectively reducing depressive symptoms, which in turn may lower the risk of suicide. The mechanism between daytime sleepiness and depressive symptoms may require more research to explore, such as longitudinal studies and a combination of biological and neuroscience research methods.
Limitations, strengths, and future directions
One of our strengths is the use of follow-up design to explore how mobile phone addiction predicts later suicide risk in a representative adolescent sample. The current study added further and reliable evidence for the relationship between adolescent behavior addiction and suicide risk, and provided evidence and reference for further intervention. There were several limitations in the present study. First, the study sample was recruited in areas classified as moderate risk COVID-19 prevalence areas, which means that the results are not necessarily applicable to adolescents in other areas. Second, the psychological variables investigated in the present study were limited; therefore, future studies could include more variables such as sleep disorders, anxiety, interpersonal relationships, and acute stress. Third, as no participant information was gathered before the pandemic, the pre-COVID mobile phone use, daytime sleepiness, depression, and suicidality were unknown. Fourth, since this study uses a self-assessment questionnaire, the subjective deviation is inevitable. More reliable tools such as face-to-face interviews or objective indicators are needed in future research. Fifth, because depression is positively correlated with daytime sleepiness, it is difficult to explore the causal relationship between the two because it is cross-sectional data, and future studies need to explore the causal connection in a longitudinal design. Finally, as the period between the two waves was relatively short, longitudinal studies over more extended periods and different survey waves would provide a more transparent, long-term picture.
Conclusion and implications
This study was one of the few studies that have examined the prospective associations between mobile phone addiction and suicidality in a short-term longitudinal study during COVID-19 in a large cohort of adolescents. The key findings were that mobile phone addiction during the COVID-19 quarantine period could, directly and indirectly, predict suicidality five months later when the pandemic was in remission. Depression and daytime sleepiness plays a mediating role in linking mobile phone addiction and suicidality. These findings confirmed the importance of long-term regular monitoring of suicide risk, depression, and daytime sleepiness in adolescents with mobile phone addiction. Long-term psychosocial care or support is needed for vulnerable adolescents with depression, and daytime sleepiness, as these could be warning signs for suicide risk detection, prevention, and intervention.
Availability of data and materials
Data could be obtained from the corresponding authors upon reasonable request.
Bedford J, Enria D, Giesecke J, Heymann DL, Ihekweazu C, Kobinger G, Lane HC, Memish Z, Oh Md, Sall AA, et al. COVID-19: towards controlling of a pandemic. The Lancet. 2020;395(10229):1015–8.
Article CAS Google Scholar
Zhang N, Yang S, Jia P. Cultivating resilience during the COVID-19 pandemic: A socioecological perspective. Annual Review of Psychology. 2022;73:575–98.
Article PubMed Google Scholar
Gonzalez-Mendez R, Díaz M. Volunteers’ compassion fatigue, compassion satisfaction, and post-traumatic growth during the SARS-CoV-2 lockdown in Spain: Self-compassion and self-determination as predictors. PLoS ONE. 2021;16(9): e0256854.
Article CAS PubMed PubMed Central Google Scholar
Li J, Zhan D, Zhou Y, Gao X. Loneliness and problematic mobile phone use among adolescents during the COVID-19 pandemic: The roles of escape motivation and self-control. Addict Behav. 2021;118: 106857.
Article PubMed PubMed Central Google Scholar
Masaeli N, Farhadi H. Prevalence of Internet-based addictive behaviors during COVID-19 pandemic: A systematic review. J Addict Dis. 2021;39(4):468–88.
Duan L, He J, Li M, Dai J, Zhou Y, Lai F, Zhu G. Based on a Decision Tree Model for Exploring the Risk Factors of Smartphone Addiction Among Children and Adolescents in China During the COVID-19 Pandemic. Front Psych. 2021;12:897.
Google Scholar
Chauhan N, Patra S, Bhargava R, Srivastava C, Gujar KV, Gupta N, Seshadri S. Exposure to smartphone and screen media in children and adolescents and COVID-19 pandemic. Journal of Indian Association for Child and Adolescent Mental Health-ISSN 0973–1342. 2021;7(2):219–29.
Article Google Scholar
Fernandes B, Uzun B, Aydin C, Tan-Mansukhani R, Vallejo A, Saldaña-Gutierrez A, Biswas UN, Essau CA. Internet use during COVID-19 lockdown among young people in low-and middle-income countries: Role of psychological wellbeing. Addictive Behaviors Reports. 2021;14: 100379.
Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, McKyer ELJ, Ahmed HU, Ma P. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;9:636.
Galea S, Merchant RM, Lurie N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Intern Med. 2020;180(6):817–8.
Article CAS PubMed Google Scholar
Li S, Wang Y, Xue J, Zhao N, Zhu T. The Impact of COVID-19 Epidemic Declaration on Psychological Consequences: A Study on Active Weibo Users. Int J Environ Res Public Health. 2020;17(6):2032.
Article CAS PubMed Central Google Scholar
Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2): e100213.
Twenge JM, Joiner TE. US Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress Anxiety. 2020;37(10):954–6.
Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2020;70:124.
Fitzpatrick KM, Harris C, Drawve G. How bad is it? Suicidality in the middle of the COVID-19 pandemic. Suicide and Life-Threatening Behavior. 2020;50(6):1241–9.
Hoekstra PJ. Suicidality in children and adolescents: lessons to be learned from the COVID-19 crisis. Eur Child Adolesc Psychiatry. 2020;29:737–8.
Fountoulakis KN, Apostolidou MK, Atsiova MB, Filippidou AK, Florou AK, Gousiou DS, Katsara AR, Mantzari SN, Padouva-Markoulaki M, Papatriantafyllou EI. Self-reported changes in anxiety, depression and suicidality during the COVID-19 lockdown in Greece. J Affect Disord. 2021;279:624–9.
Allan NP, Volarov M, Koscinski B, Pizzonia KL, Potter K, Accorso C, Saulnier KG, Ashrafioun L, Stecker T, Suhr J. Lonely, anxious, and uncertain: critical risk factors for suicidal desire during the COVID-19 pandemic. Psychiatry Res. 2021;304: 114144.
John A, Pirkis J, Gunnell D, Appleby L, Morrissey J. Trends in suicide during the covid-19 pandemic. BMJ. 2020;371: m4352.
Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, Khan M, O’Connor RC, Pirkis J, Appleby L, et al. Suicide risk and prevention during the COVID-19 pandemic. The Lancet Psychiatry. 2020;7(6):468–71.
Sher L. Suicide research and prevention during and after the COVID-19 pandemic. Acta Psychiatr Scand. 2020;142(5):353–4.
Que J, Yuan K, Gong Y, Meng S, Bao Y, Lu L. Raising awareness of suicide prevention during the COVID-19 pandemic. Neuropsychopharmacol Rep. 2020;40(4):392–5.
Every-Palmer S, Jenkins M, Gendall P, Hoek J, Beaglehole B, Bell C, Williman J, Rapsey C, Stanley J. Psychological distress, anxiety, family violence, suicidality, and wellbeing in New Zealand during the COVID-19 lockdown: A cross-sectional study. PLoS ONE. 2020;15(11): e0241658.
Czeisler ME, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic - United States, June 24–30, 2020. Mmwr-Morbidity and Mortality Weekly Report. 2020;69(32):1049–57.
Ayuso-Mateos JL, Morillo D, Haro JM, Olaya B, Lara E, Miret M. Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population. Epidemiol Psychiatr Sci. 2021;30: e49.
Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113(10):707–12.
Hawton K, Saunders KEA, O’Connor RC. Self-harm and suicide in adolescents. Lancet. 2012;379(9834):2373–82.
Picazo-Zappino J. Suicide among children and adolescents: a review. Actas Espanolas De Psiquiatria. 2014;42(3):125–32.
PubMed Google Scholar
Billieux J, Maurage P, Lopez-Fernandez O, Kuss DJ, Griffiths MD. Can Disordered Mobile Phone Use Be Considered a Behavioral Addiction? An Update on Current Evidence and a Comprehensive Model for Future Research. Curr Addict Rep. 2015;2(2):156–62.
Elhai JD, Levine JC, Dvorak RD, Hall BJ. Non-social features of smartphone use are most related to depression, anxiety and problematic smartphone use. Comput Hum Behav. 2017;69:75–82.
El-Sayed Desouky D, Abu-Zaid H. Mobile phone use pattern and addiction in relation to depression and anxiety. East Mediterr Health J. 2020;26(6):692–9.
Billieux J. Problematic Use of the Mobile Phone: A Literature Review and a Pathways Model. Current Psychiatry Reviews. 2012;8(4):299–307.
Chen RS, Liu JB, Cao XL, Duan SQ, Wen SY, Zhang SM, Xu JC, Lin L, Xue ZP, Lu JP. The relationship between mobile phone use and suicide -related behaviors among adolescents: The mediating role of depression and interpersonal problems. J Affect Disorders. 2020;269:101–7.
Ismail WSW, Sim ST, Tan KA, Bahar N, Ibrahim N, Mahadevan R, Jaafar NRN, Baharudin A, Aziz MA. The relations of internet and smartphone addictions to depression, anxiety, stress, and suicidality among public university students in Klang Valley. Malaysia Perspectives in Psychiatric Care. 2020;56(4):949–55.
Mahamid FA, Berte DZ, Bdier D. Problematic internet use and its association with sleep disturbance and life satisfaction among Palestinians during the COVID-19 pandemic. Curr Psychol. 2021:1–8. https://doi.org/10.1007/s12144-021-02124-5 .
Song Y, Sznajder K, Cui C, Yang Y, Li Y, Yang X. Anxiety and its relationship with sleep disturbance and problematic smartphone use among Chinese medical students during COVID-19 home confinement—A structural equation model analysis. J Affect Disord. 2022;296:315–21.
Oliveira T, Costa D, Alvim-Soares A, de Paula J, Kestelman I, Silva A, Malloy-Diniz L, Miranda D. Children’s behavioral problems, screen time, and sleep problems’ association with negative and positive parenting strategies during the COVID-19 outbreak in Brazil. Child Abuse Negl. 2022;130:105345.
Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A. Adolescents’ Electronic Media Use at Night, Sleep Disturbance, and Depressive Symptoms in the Smartphone Age. J Youth Adolesc. 2015;44(2):405–18.
Demirci K, Akgonul M, Akpinar A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J Behav Addict. 2015;4(2):85–92.
Thomee S, Harenstam A, Hagberg M. Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults - a prospective cohort study. Bmc Public Health. 2011;11:66.
Elhai JD, Dvorak RD, Levine JC, Hall BJ. Problematic smartphone use: A conceptual overview and systematic review of relations with anxiety and depression psychopathology. J Affect Disorders. 2017;207:251–9.
Ibrahim NK, Baharoon BS, Banjar WF, Jar AA, Ashor RM, Aman AA, Al-Ahmadi JR. Mobile Phone Addiction and Its Relationship to Sleep Quality and Academic Achievement of Medical Students at King Abdulaziz University, Jeddah, Saudi Arabia. J Res Health Sci. 2018;18(3):e00420.
PubMed PubMed Central Google Scholar
Liu QQ, Zhou ZK, Yang XJ, Kong FC, Niu GF, Fan CY. Mobile phone addiction and sleep quality among Chinese adolescents: A moderated mediation model. Comput Hum Behav. 2017;72:108–14.
Sahin S, Ozdemir K, Unsal A, Temiz N. Evaluation of mobile phone addiction level and sleep quality in university students. Pakistan Journal of Medical Sciences. 2013;29(4):913–8.
Omary A. National Prevalence Rates of Suicidal Ideation and Suicide Attempts Among Adults With and Without Depression. Journal of Nervous and Mental Disease. 2021;209(5):378–85.
Hardy P. Severe depression : morbidity-mortality and suicide. Encephale-Revue De Psychiatrie Clinique Biologique Et Therapeutique. 2009;35(7):S269–71.
Ribeiro JD, Huang XY, Fox KR, Franklin JC. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Brit J Psychiat. 2018;212(5):279–86.
Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–94.
Cerniglia L, Zoratto F, Cimino S, Laviola G, Ammaniti M, Adriani W. Internet Addiction in adolescence: Neurobiological, psychosocial and clinical issues. Neurosci Biobehav Rev. 2017;76(Pt A):174–84.
Guo W, Tao Y, Li X, Lin X, Meng Y, Yang X, Wang H, Zhang Y, Tang W, Wang Q. Associations of internet addiction severity with psychopathology, serious mental illness, and suicidality: large-sample cross-sectional study. J Med Internet Res. 2020;22(8): e17560.
Jasso-Medrano JL, Lopez-Rosales F. Measuring the relationship between social media use and addictive behavior and depression and suicide ideation among university students. Comput Hum Behav. 2018;87:183–91.
Chen R, Liu J, Cao X, Duan S, Wen S, Zhang S, Xu J, Lin L, Xue Z, Lu J. The relationship between mobile phone use and suicide-related behaviors among adolescents: the mediating role of depression and interpersonal problems. J Affect Disord. 2020;269:101–7.
Yu Y, Yang X, Wang S, Wang H, Chang R, Tsamlag L, Zhang S, Xu C, Yu X, Cai Y. Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai. China BMC psychiatry. 2020;20(1):1–9.
CAS Google Scholar
Roussos A, Goenjian AK, Steinberg AM, Sotiropoulou C, Kakaki M, Kabakos C, Karagianni S, Manouras V. Posttraumatic stress and depressive reactions among children and adolescents after the 1999 earthquake in Ano Liosia. Greece American Journal of Psychiatry. 2005;162(3):530–7.
Tang WJ, Zhao JD, Lu Y, Zha YL, Liu H, Sun Y, Zhang J, Yang YC, Xu JP. Suicidality, posttraumatic stress, and depressive reactions after earthquake and maltreatment: A cross-sectional survey of a random sample of 6132 chinese children and adolescents. J Affect Disorders. 2018;232:363–9.
Huang H, Niu L, Zhou C, Wu H. Reliability and validity of mobile phone addiction index for Chinese college students. Chin J Clin Psychol. 2014;22(5):835–8.
Bianchi A, Phillips JG. Psychological predictors of problem mobile phone use. Cyberpsychol Behav. 2005;8(1):39–51.
Liu X, Yang Y, Liu Z, Chen H, Fan F, Jia C. Psychometric assessment of the Chinese adolescent daytime sleepiness scale (CADSS). Sleep Biol Rhythms. 2017;15(3):207–16.
LeBlanc JC, Almudevar A, Brooks SJ, Kutcher S. Screening for adolescent depression: comparison of the Kutcher Adolescent Depression Scale with the Beck depression inventory. J Child Adolesc Psychopharmacol. 2002;12(2):113–26.
Shun CM, Jane CH, Jung SW, Nan LC, Cheng KC, Che HW, Sheue CY, Ping CH, Pesus C. A rapid screening test for depression in junior high school children. J Chin Med Assoc. 2011;74(8):363–8.
Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. 2001;8(4):443–54.
Fang Q, Freedenthal S, Osman A. Validation of the Suicide Resilience Inventory-25 with American and Chinese College Students. Suicide Life Threat Behav. 2015;45(1):51–64.
Hayes AF, Montoya AK, Rockwood NJ. The analysis of mechanisms and their contingencies: PROCESS versus structural equation modeling. Australas Mark J. 2017;25(1):76–81.
DiCiccio TJ, Efron B. Bootstrap confidence intervals. Stat Sci. 1996;11(3):189–228.
Martin MA, Roberts S. An evaluation of bootstrap methods for outlier detection in least squares regression. J Appl Stat. 2006;33(7):703–20.
Steinbuchel TA, Herpertz S, Dieris-Hirche J, Kehyayan A, Kulpmann I, Diers M, Te Wildt BT. Internet Addiction and Suicidality - A Comparison of Internet-Dependent and Non-Dependent Patients with Healthy Controls. Psychother Psychosom Med Psychol. 2020;70(11):457–66.
Twenge JM, Joiner TE, Rogers ML, Martin GN. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clinical Psychological Science. 2017;6(1):3–17.
Wang J, Hao Q-H, Tu Y, Peng W, Wang Y, Li H, Zhu T-M. Assessing the Association Between Internet Addiction Disorder and Health Risk Behaviors Among Adolescents and Young Adults: A Systematic Review and Meta-Analysis. Front Public Health. 2022;10:809232.
Deslandes SF, Coutinho T. The intensive use of the internet by children and adolescents in the context of COVID-19 and the risks for self-inflicted violence. Ciencia & saude coletiva. 2020;25:2479–86.
Marengo D, Fabris MA, Longobardi C, Settanni M. Smartphone and social media use contributed to individual tendencies towards social media addiction in Italian adolescents during the COVID-19 pandemic. Addict Behav. 2022;126: 107204.
Fortgang RG, Wang SB, Millner AJ, Reid-Russell A, Beukenhorst AL, Kleiman EM, Bentley KH, Zuromski KL, Al-Suwaidi M, Bird SA. Increase in suicidal thinking during COVID-19. Clinical Psychological Science. 2021;9(3):482–8.
Article PubMed Central Google Scholar
Plener PL. COVID-19 and nonsuicidal self-injury: the pandemic’s influence on an adolescent epidemic. Am J Public Health. 2021;111(2):195–6.
Schutten D, Stokes KA, Arnell KM. I want to media multitask and I want to do it now: Individual differences in media multitasking predict delay of gratification and system-1 thinking. Cogn Res. 2017;2(1):8.
Leung L, Lee PSN. Impact of Internet Literacy, Internet Addiction Symptoms, and Internet Activities on Academic Performance. Soc Sci Comput Rev. 2012;30(4):403–18.
Saraei F, Ebrahimi ME, Paydar MRZ. Relationship between Internet Addiction, Mental Health, and Academic Performance among Adolescents 15 to 18 Years Referred to Cafe-Net in Hamedan-Iran. Life Sci J. 2013;10(1):1260–7.
Nalwa K, Anand AP. Internet addiction in students: a cause of concern. Cyberpsychol Behav. 2003;6(6):653–6.
Wu XS, Zhang ZH, Zhao F, Wang WJ, Li YF, Bi LD, Qian ZZ, Lu SS, Feng F, Hu CY, et al. Prevalence of Internet addiction and its association with social support and other related factors among adolescents in China. J Adolescence. 2016;52:103–11.
Pea R, Nass C, Meheula L, Rance M, Kumar A, Bamford H, Nass M, Simha A, Stillerman B, Yang S, et al. Media Use, Face-to-Face Communication, Media Multitasking, and Social Well-Being Among 8- to 12-Year-Old Girls. Dev Psychol. 2012;48(2):327–36.
Richards R, McGee R, Williams SM, Welch D, Hancox RJ. Adolescent Screen Time and Attachment to Parents and Peers. Arch Pediat Adol Med. 2010;164(3):258–62.
Andreassen CS, Billieux J, Griffiths MD, Kuss DJ, Demetrovics Z, Mazzoni E, Pallesen S. The Relationship Between Addictive Use of Social Media and Video Games and Symptoms of Psychiatric Disorders: A Large-Scale Cross-Sectional Study. Psychol Addict Behav. 2016;30(2):252–62.
Boniel-Nissim M, Tabak I, Mazur J, Borraccino A, Brooks F, Gommans R, van der Sluijs W, Zsiros E, Craig W, Harel-Fisch Y, et al. Supportive communication with parents moderates the negative effects of electronic media use on life satisfaction during adolescence. Int J Public Health. 2015;60(2):189–98.
Mentzoni RA, Brunborg GS, Molde H, Myrseth H, Skouveroe KJM, Hetland J, Pallesen S. Problematic Video Game Use: Estimated Prevalence and Associations with Mental and Physical Health. Cyberpsych Beh Soc N. 2011;14(10):591–6.
Cheng HW, Liu J. Alterations in Amygdala Connectivity in Internet Addiction Disorder. Sci Rep-Uk. 2020;10(1):2370.
Pessoa L. On the relationship between emotion and cognition. Nat Rev Neurosci. 2008;9(2):148–58.
Turel O, He Q, Xue G, Xiao L, Bechara A. Examination of neural systems sub-serving facebook “addiction.” Psychol Rep. 2014;115(3):675–95.
He QH, Turel O, Brevers D, Bechara A. Excess social media use in normal populations is associated with amygdala-striatal but not with prefrontal morphology. Psychiat Res-Neuroim. 2017;269:31–5.
Dong G, Devito EE, Du X, Cui Z. Impaired inhibitory control in “internet addiction disorder”: a functional magnetic resonance imaging study. Psychiatry Res. 2012;203(2–3):153–8.
Vahedi Z, Saiphoo A. The association between smartphone use, stress, and anxiety: A meta-analytic review. Stress Health. 2018;34(3):347–58.
Kardefelt-Winther D. A conceptual and methodological critique of internet addiction research: Towards a model of compensatory internet use. Comput Hum Behav. 2014;31:351–4.
Shrivastava A, Saxena Y. Effect of mobile usage on serum melatonin levels among medical students. Indian J Physiol Pharmacol. 2014;58(4):395–9.
Loughran SP, Wood AW, Barton JM, Croft RJ, Thompson B, Stough C. The effect of electromagnetic fields emitted by mobile phones on human sleep. NeuroReport. 2005;16(17):1973–6.
Aalto S, Haarala C, Bruck A, Sipila H, Hamalainen H, Rinne JO. Mobile phone affects cerebral blood flow in humans. J Cereb Blood Flow Metab. 2006;26(7):885–90.
Al-Khlaiwi T, Meo SA. Association of mobile phone radiation with fatigue, headache, dizziness, tension and sleep disturbance in Saudi population. Saudi Med J. 2004;25(6):732–6.
Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep Disturbances as an Evidence-Based Suicide Risk Factor. Curr Psychiatry Rep. 2015;17(3):554.
Gong QH, Li SX, Wang SJ, Li H, Han LY. Sleep and suicidality in school-aged adolescents: A prospective study with 2-year follow-up. Psychiatry Res. 2020;287:112918.
Wang D, Ross B, Zhou X, Meng D, Zhu Z, Zhao J, Fan F, Liu X. Sleep disturbance predicts suicidal ideation during COVID-19 pandemic: A two-wave longitudinal survey. J Psychiatr Res. 2021;143:350–6.
Perlisa ML, Grandnerd MA, Chakravorty S, Bernertf RA, Browng GK, Thaseh ME. Suicide and sleep: Is it a bad thing to be awake when reason sleeps? Sleep Med Rev. 2016;29:101–7.
Sarchiapone M, Mandelli L, Carli V, Iosue M, Wasserman C, Hadlaczky G, Hoven CW, Apter A, Balazs J, Bobes J, et al. Hours of sleep in adolescents and its association with anxiety, emotional concerns, and suicidal ideation. Sleep Med. 2014;15(2):248–54.
Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. Journal of Endocrinology and Metabolism. 2005;90(5):3106–14.
Bao AM, Meynen G, Swaab DF. The stress system in depression and neurodegeneration: focus on the human hypothalamus. Brain Res Rev. 2008;57(2):531–53.
Kirkcaldy BD, Eysenck MW, Siefen GR. Psychological and social predictors of suicidal ideation among young adolescents. Sch Psychol Int. 2004;25(3):301–16.
Yang B, Choe K, Park Y, Kang Y. Associations among daytime sleepiness, depression and suicidal ideation in Korean adolescents. Int J Adolesc Med Health. 2019;31(2).
Download references
Acknowledgements
The authors wish to thank all study participants and all research collaborators.
This research was supported by grants from the China Postdoctoral Science Foundation (2018M643488) and the National Natural Science Foundation of China (81901928).
Author information
Authors and affiliations.
Department of Forensic Psychiatry, West China School of Basic Medical Sciences & Forensic Medicine, Sichuan University, Chengdu, Sichuan, China
Department of Child and Adolescent Psychiatry, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, UK
Aldo Alberto Conti & Wanjie Tang
Mental Health Centre, West China Hospital, Sichuan University, Chengdu, China
Changjian Qiu & Wanjie Tang
You can also search for this author in PubMed Google Scholar
Contributions
Wanjie Tang designed the study; Gangqin Li, Changjian Qiu, and Wanjie Tang wrote the main manuscript text, and Aldo Conti prepared Fig. 1 and Tables. All authors reviewed the manuscript.
Corresponding authors
Correspondence to Changjian Qiu or Wanjie Tang .
Ethics declarations
Ethics approval and consent to participate.
The authors assert that all procedures contributing to this work comply with the ethical standards of the Ethics Committee of Sichuan Psychological Society (NO. 2020_12) on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The informed consent was obtained from all the participants and their caregivers prior to the study.
Competing interests
All authors have no conflict of interest to declare.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Li, G., Conti, A.A., Qiu, C. et al. Adolescent mobile phone addiction during the COVID-19 pandemic predicts subsequent suicide risk: a two-wave longitudinal study. BMC Public Health 22 , 1537 (2022). https://doi.org/10.1186/s12889-022-13931-1
Download citation
Received : 13 June 2022
Accepted : 02 August 2022
Published : 12 August 2022
DOI : https://doi.org/10.1186/s12889-022-13931-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mobile phone addiction
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Are the Signs of Phone Addiction?
Warning Signs and How to Help
- Who Is at Risk
- Health Effects
- How to Break It
- When to Seek Help
While cell phones are integral to our daily lives and have numerous benefits, many people have developed what some researchers consider phone addiction symptoms that can have negative effects on well-being. According to some research, roughly 27.9% of young adults are addicted to their cell phones.
Read on to find out more about how cell phone addiction is defined, the risks involved, and how to identify and treat it.
Georgijevic / Getty Images
What Is Phone Addiction?
Cell phone addiction may be categorized as a type of behavioral addiction that presents when a person can't go without their cell phone, their excessive use causes adverse consequences, or they experience symptoms similar to withdrawal when they do.
While cell phone addiction is very real for the people experiencing it, it is not officially recognized as a mental health illness or an addiction in the fifth edition of the " Diagnostic and Statistical Manual of Mental Health Disorders " (DSM-5). However, it does present with similar characteristics as other behavioral addictions, such as gambling .

What Is the DSM-5?
The DSM-5 is the American Psychiatric Association's official handbook that mental health professionals use to assess and diagnose a variety of mental health disorders.
There are reasons why smartphones are hard to put down. The sounds and vibrations catch our attention, and the games, notifications, social media, and messages provide instant gratification.
Smartphones offer a constant source of entertainment and distraction. Companies use persuasive design techniques with features like infinite scrolling, push notifications, and personalized content to keep us engaged and make it harder to disconnect.
Who Is at Risk of Phone Addiction?
The exact number of people addicted to their cell phones isn’t known. This is because it can be hard to quantify and many studies base their data on self-reporting methods.
Although anyone can be at risk for this type of addiction, it is most commonly found among adolescents. Some research indicates that about 20%–30% of adolescents and young adults have a phone addiction. Teens in particular use their phones with high frequency, while cell phone use tends to decrease gradually as a person gets older.
People who get phones at a younger age are also more likely to present with addictive behaviors than those who get them later in life.
Cell Phone Risk Between the Sexes
Both young boys and girls are at a higher risk of developing an addiction to their cell phones, but there may be somewhat different patterns of use. Girls typically use their phones for social interaction, while boys use phones for the same reason in addition to gaming applications. Males also show a higher tendency to use their phones in risky situations.
Social media addiction may go hand in hand with phone addiction. It is associated with poor sleep quality and depression. And, it is also correlated with body perception issues.
What Are the Symptoms of Phone Addiction?
Some new terms have emerged to describe the characteristics of phone addiction:
- Nomophobia : Fear tied to going without one’s phone
- Textaphrenia : Fear of the inability to receive or send text messages
- Ringxiety : Feeling as though a notification has come through on your phone when it hasn’t
- Textiety : Feeling anxious about receiving and responding to text messages immediately
Some symptoms of phone addiction include:
- You are constantly reaching for your phone.
- You spend much of your time on your phone.
- You wake in the night to check if your phone has any notifications.
- You feel negative emotions such as anger, sadness, or anxiety when you don’t have your phone or can’t check it.
- Using your phone has led to an injury or accident, such as a car crash from texting while driving.
- The amount of time you spend on your phone affects your professional or personal life.
- When you try to limit your phone use, you end up relapsing in a short time.
Signs From Others
While it can be difficult to notice your own phone addiction, one telltale sign you are forming an addiction is if someone in your life mentions your phone overuse to you. They may express concern about how much you are on your phone or your behavior while you are not using it.
What Are the Effects of Phone Addiction?
Studies show that cell phone overuse can have a negative impact on your health in a variety of ways.
Excessive smartphone use has been associated with physical and mental health problems in adolescents and young adults, including:
- Obsessive-compulsive disorder (OCD)
- Attention deficit hyperactivity disorder (ADHD)
- Alcohol use disorder
- Difficulties in cognitive-emotion regulation
- Impulsivity
- Impaired cognitive function
- Addiction to social networking
- Low self-esteem
Some other effects of phone addiction include:
- Muscle pain and stiffness
- Blurry vision
- Red or irritated eyes
- Auditory illusions (hearing your phone ring or vibrate when it’s not)
- Thumb or wrist pain
- Loss of interest in other activities you once enjoyed
- Insomnia and sleep disturbances
- Worsened school or work performance
- Heightened conflicts with your social group or family
- Feelings of irritability or unease when you don’t have your phone
- An increased risk of developing depression or anxiety
- Putting yourself in dangerous situations by using your phone when you shouldn’t be
- Feelings of guilt, helplessness, or loneliness when you go without your phone
Cell Phone Addiction and Dopamine
Cell phone addiction is similar to other types of addiction because of its effect on dopamine , a chemical in the body that causes feelings of pleasure. Cell phone use has been shown to stimulate the production and release of dopamine, which drives the need to use it more and more.
How to Break the Addiction
Breaking any type of addiction isn’t easy, but it is possible.
First, you must acknowledge the issues it's causing in your life. Once you have determined that you need to break your addiction, you can:
- Identify the reasons : Research has found that people who are on their phones constantly may be trying to escape issues or problems in their lives. By determining if the root cause of your phone addiction is to escape problems, you can address and treat the underlying issues.
- Consider therapy : Certain types of therapy , such as cognitive behavioral therapy (CBT) , have proven effective in helping people overcome addictions. Other types of effective therapies for addictions are contingency management, motivational interviewing , and couples counseling (if it is affecting your relationships).
Tips to Beat Phone Addiction on Your Own
While addictions often require professional help, not all people will want to go that route. If you want to try to get over phone addiction on your own you can:
- Buy a cellphone lockbox that only opens after a set amount of time. This will limit your use.
- Remove apps that take up the majority of your time.
- Eliminate notifications on your phone so you aren’t summoned to check it every time a notification appears.
- Charge your phone in an inaccessible place so it’s harder to get to.
- Try to replace phone use with other activities you enjoy.
- Switch to a non-smartphone.
How to Prevent Phone Addiction
The best prevention method for phone addiction is avoidance. If you have a phone, you can prevent becoming addicted by using it only when necessary. This means deleting any apps that don’t serve a purpose and using your time to connect with people in other ways.
For parents with young children, limit your child's phone use by only allowing them to use it on your terms, or avoid buying them a phone altogether until they are above a certain age. Since children in their teen years are most at risk, you could hold off on buying them a phone until it is absolutely necessary.
If your child must have a phone for safety reasons, consider buying a phone that doesn’t have the ability to download apps that may lead to addiction. This way they will still be able to contact you or their friends if they need to but will not have access to time-consuming apps.
When to Contact a Healthcare Provider
If you feel as though your phone use has begun to control your life, or your loved ones have mentioned their concerns to you, it may be time to seek out professional help.
You can do this by speaking to your healthcare provider for referrals to a therapist or by signing up for a digital detox—a time when you give up tech devices.
While not formally recognized by the DSM-5, problematic cell phone use shares many similarities with behavioral addictions. A person with a phone addiction will have difficulty staying off their phone and could lose interest in things they once enjoyed because of excessive phone use. Teens and young adults are most at risk of developing a phone addiction.
Signs of phone addiction include feeling irritable or negative when going without a phone, being unable to go without a phone for long periods, or using a phone so much that it negatively affects physical health or mental health.
While phone addiction does come with negative consequences, there are ways to beat it. A person can seek out professional help through a therapist or practice control techniques that limit phone use.
De-Sola Gutiérrez J, Rodríguez de Fonseca F, Rubio G. Cell-phone addiction: A review . Front Psychiatry. 2016;24(7):175. doi:10.3389/fpsyt.2016.00175
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders . Fifth Edition. American Psychiatric Association; 2013. doi:10.1176/appi.books.9780890425596
Lin YH, Chiang CL, Lin PH, Chang LR, Ko CH, Lee YH, Lin SH. Proposed diagnostic criteria for smartphone addiction . PLoS One. 2016;11(11):e0163010. doi:10.1371/journal.pone.0163010
Schulz van Endert T, Mohr PNC. Likes and impulsivity: Investigating the relationship between actual smartphone use and delay discounting . Xin B, ed. PLoS ONE. 2020;15(11):e0241383. doi: 10.1371/journal.pone.0241383
Chen X, Hedman A, Distler V, Koenig V. Do persuasive designs make smartphones more addictive? - A mixed-methods study on Chinese university students . Computers in Human Behavior Reports. 2023;10:100299. doi: 10.1016/j.chbr.2023.100299
Pew Research Center. Mobile Fact Sheet 2021 .
Shoukat S. Cell phone addiction and psychological and physiological health in adolescents . EXCLI J. 2019;18:47-50.
yi Lin L, Sidani JE, Shensa A, et al. Association between social media use and depression among U.S. young adults: research article: social media and depression . Depress Anxiety . 2016;33(4):323-331. doi:10.1002/da.22466
Çakmak S, Tanrıöver Ö. Is obesity and body perception disturbance related to social media addiction among university students? J Am Coll Health. 2022 Feb 14:1-8. doi:10.1080/07448481.2022.2034832
Addiction Center. Phone addiction: warning signs and treatment .
Wacks Y, Weinstein AM. Excessive Smartphone Use Is Associated With Health Problems in Adolescents and Young Adults . Front Psychiatry. 2021 May 28;12:669042. doi: 10.3389/fpsyt.2021.669042
Chun JW, Choi J, Kim JY, Cho H, Ahn KJ, Nam JH, Choi JS, Kim DJ. Altered brain activity and the effect of personality traits in excessive smartphone use during facial emotion processing . Sci Rep. 2017;7(1):12156. doi:10.1038/s41598-017-08824-y
Roberts JA, Yaya LH, Manolis C. The invisible addiction: cell-phone activities and addiction among male and female college students . J Behav Addict. 2014;3(4):254-265. doi:10.1556/JBA.3.2014.015
Seo HS, Jeong EK, Choi S, Kwon Y, Park HJ, Kim I. Changes of neurotransmitters in youth with internet and smartphone addiction: A comparison with healthy controls and changes after cognitive behavioral therapy . AJNR Am J Neuroradiol. 2020;41(7):1293-1301. doi:10.3174/ajnr.A6632
By Angelica Bottaro Bottaro has a Bachelor of Science in Psychology and an Advanced Diploma in Journalism. She is based in Canada.
ORIGINAL RESEARCH article
The association between smartphone addiction and sleep: a uk cross-sectional study of young adults.

- 1 Department of Biostatistics and Health Informatics, Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, United Kingdom
- 2 Population Policy Practice, National Institute of Health Research, Great Ormond Street Hospital Biomedical Research Centre Institute of Child Health, University College London, London, United Kingdom
- 3 Addictions Department, Institute of Psychiatry, Psychology & Neuroscience, King's College London, London, United Kingdom
- 4 South London and Maudsley NHS Foundation Trust, Beckenham, United Kingdom
Background: In a large UK study we investigated the relationship between smartphone addiction and sleep quality in a young adult population.
Methods: We undertook a large UK cross-sectional observational study of 1,043 participants aged 18 to 30 between January 21st and February 30th 2019. Participants completed the Smartphone Addiction Scale Short Version, an adapted Pittsburgh Sleep Quality Score Index and reported smartphone use reduction strategies using both in-person ( n = 968) and online ( n = 75) questionnaires. A crude and adjusted logistic regression was fitted to assess risk factors for smartphone addiction, and the association between smartphone addiction and poor sleep.
Results: One thousand seventy one questionnaires were returned, of which 1,043 participants were included, with median age 21.1 [interquartile range (IQR) 19–22]. Seven hundred and sixty three (73.2%) were female, and 406 reported smartphone addiction (38.9%). A large proportion of participants disclosed poor sleep (61.6%), and in those with smartphone addiction, 68.7% had poor sleep quality, compared to 57.1% of those without. Smartphone addiction was associated with poor sleep (aOR = 1.41, 95%CI: 1.06–1.87, p = 0.018).
Conclusions: Using a validated instrument, 39% young adults reported smartphone addiction. Smartphone addiction was associated with poor sleep, independent of duration of usage, indicating that length of time should not be used as a proxy for harmful usage.
Introduction
Smartphone use has become ubiquitous over the past decade. This has been accompanied by growing concerns around excessive and potentially harmful use ( 1 ). There are emerging reports of problematic behavior patterns in relation to smartphone use which mirror those of addiction ( 2 ). Although smartphone addiction is not formally recognized as a clinical diagnosis, it is a subject of active research. Validated instruments have been developed to characterize problematic smartphone use in terms of recognized dimensions of behavioral addiction with scores above which the research subject is considered to report smartphone addiction ( 3 , 4 ). Research subjects reporting smartphone addiction describe a decreased interest in face-to-face relationships, use despite knowledge of the negative consequences, impaired control over and pre-occupation with their devices, and anxiety when their phones are inaccessible; these are not unlike the symptom domains of substance use disorders or other behavioral addictions ( 2 , 5 – 7 ). Studies have highlighted associations of smartphone addiction with reduced productivity and with lower academic attainment ( 8 , 9 ), demonstrating the negative functional impact on young people's lives and future prospects. Indirect harms resulting from smartphone addiction include propensity for accidents, for example through use whilst driving, and potential contribution to the obesity crisis by facilitating sedentary lifestyles ( 10 , 11 ). Although at an early stage, there is also some neuroimaging evidence of volume and activity parallels between smartphone addiction and other addictions ( 12 ).
Studies to date have used the length of smartphone usage (measured as the total daily length of smartphone use) as an exposure indicative of problematic usage ( 13 ). However, while it is true that heavy use is seen in people with any addiction, it is also true that this is not sufficient for an addiction to be present, reflected in the ICD-11 criteria for gaming and gambling disorders ( 6 ) and in proposed diagnostic criteria for smartphone addiction ( 7 ). For an addiction to be present, subjective distress and functional impairment must also be present – in the case of smartphone addiction, neglect of other meaningful activities, pre-occupation with the phone, distress when access to the phone is not possible, and continued use despite evidence of harm. Measuring duration of use is an inexact proxy for addiction, as some people may experience the features of addiction with lower duration of use while others may use their phone in an adaptive way for long periods of time (for example, answering work emails during a long commute) but be able to put the phone down without distress and attend to appropriate activities such as communicating with family members, or going to bed on time ( 14 ).
It is important to note that smartphone addiction has several terms of reference including “nomophobia,” “problematic smartphone use,” and “smartphone dependence.” There is also a lack of consensus around whether putative “smartphone addiction” represents a distinct clinical identity and meets the criteria to be formally considered a behavioral addiction ( 15 , 16 ). Furthermore, it remains unclear whether this dependence is on the smartphone itself or on the apps available through the device; whether the phone itself is like a substance of abuse or more like the needle through which addictive apps are delivered ( 14 ). There are similar patterns of behavior associated with specific applications (e.g., Facebook addiction, Instagram addiction) that are being investigated in their own right, and it is possible that certain types of phone use (e.g., social media use) may have more addictive implications than others (e.g., calling, texting), as the former involves display and expectation of approval through the creation, sharing, and viewing of content, while the latter replicates face-to-face relationships in terms of one-to-one communication ( 17 , 18 ). Nevertheless, there is evidence of the existence of a behavioral phenotype that resembles addiction. The physical harms highlighted above, as well as emerging associations with psychiatric symptoms such anxiety and depressed mood indicate a pressing need to further investigate this growing phenomenon ( 19 ).
While the negative effects of screen time on sleep have been previously reported, smartphones are portable, hand-held devices that have much higher potential of interrupting sleep quality or quantity ( 20 ). Problematic smartphone use has been consistently linked to poor sleep in previous studies ( 4 , 21 ), and smartphone overuse has been associated with daytime tiredness, longer sleep latency, and reduced sleep duration ( 22 – 24 ). In particular, smartphone use close to sleep initiation has been shown to delay circadian rhythm and found associated with total sleep time, where longer usage was associated with poor sleep ( 25 ). Furthermore, poor sleep outcomes may mediate the relationships between smartphone addiction and psychopathological symptoms ( 26 ). However, despite consistent advice from health bodies concerning the negative impacts of smartphone use on sleep, the majority of adults in the UK use their phones during the night and close to bed time ( 27 ).
A recent international systematic review found that the prevalence of smartphone addiction was around 25% in teenagers and young people ( 4 ). The weight of this evidence was from South and East Asia, and it has been noted that levels of smartphone addiction are often higher in Asian samples than in Western populations, possibly reflecting cultural practices around internet and smartphone use ( 28 , 29 ). This study includes the largest UK sample to date to investigate the prevalence of smartphone addiction, and to clarify the association between smartphone addiction and sleep outcomes, in this population.
Study Design and Study Population
Participants were recruited opportunistically across multiple campuses at King's College London, England, between January 21st and February 4th, 2019. Participants were approached by researchers to describe the study, and invited to complete a paper-based case report form (CRF) based at four separate locations during the stated data collection period. Additionally, participants were invited to complete an identical online version of the CRF through an internal research recruitment process. Eligibility criteria included students at King's College London aged between 18 and 30 who owned a smartphone. Participants were excluded if they did not adequately complete the Smartphone Addiction Scale – Short version [SAS-SV [3]] or the adapted Pittsburgh Sleep Quality Index [PSQI ( 30 )]. The study was undertaken in accordance with the Declaration of Helsinki. Ethical approval was received from the King's College Research Ethics Office (Study ID: 9138; MRS-18/19-9138) and the full protocol is available on request. All face to face participants provided informed verbal consent prior to involvement and those submitting online gave consent by responding to the questionnaire.
The case report form (CRF) was co-developed amongst researchers, teenagers and young people with experience of smartphone use ( Supplementary Table 1 ). The CRF included demographic information, smartphone use characteristics, a validated scale for smartphone addiction [SAS-SV ( 3 )], an adapted sleep score based on the Pittsburgh Sleep Quality Instrument [PSQI ( 30 )], and a range of reduction strategies. To reduce perception bias, the CRF included neutral non-directive phrasing about smartphone use collecting both positive and negative aspects.
Smartphone Use Characteristics
Participants were asked about the quantity of smartphone use (the average length of daily time) and the timing of use.
Smartphone Addiction Scale – Short Version (SAS-SV)
The SAS-SV is a 10-question validated scale that was developed to assess smartphone addiction in children (mean age of 14.5) ( 3 ). Participants are asked to rate statements related to their smartphone use, such as “Using smartphone longer than intended” on a 6-point Likert scale, from “strongly disagree” (1) to “strongly agree” (6). The resulting total score is between 10 and 60, with higher totals indicating higher risk of smartphone addiction. Total scores of 31 and 33 were used as diagnostic thresholds for males and females respectively, in accordance with the original study which found strong internal consistency (Cronbach's alpha = 0.91, AUC = 0.96 for boys, AUC = 0.89 for girls). This scale has been widely used internationally and has been found to have similarly strong internal consistencies using the same thresholds for this study's age group ( 31 , 32 ).
Participants were asked to rate their subjective sleep quality on an average weeknight on a Likert scale of 1–10 and the number of hours they slept on an average weeknight on a Likert scale of <4 to 12, taking into account the expected average number of hours of sleep for adults, in order to assess sleep quality and duration. Participants were additionally asked the number of days a week they felt noticeably tired or fatigued during the day (0–7) and the number of nights a week where they felt it difficult to fall asleep (0–7) to measure daytime tiredness and sleep latency. Based on these responses, scores for each component were calculated, which were then combined to calculate a global sleep score, adapted from the Pittsburgh Sleep Quality Index [PSQI ( 30 )], where a score of ≤ 5 was considered good sleep ( 33 ).
Reduction Strategies
Commonly used strategies to reduce smartphone use included within the CRF were identified from the literature and through consultation with subject matter experts and young people ( Supplementary Table 2 ). Participants were asked to rate the effectiveness of any strategies employed from ineffective to very effective.
Sample Size Justification
Estimates of the prevalence of poor sleep prevalence are wide-ranging. At study conception it was estimated that 42% of participants without problematic smartphone usage would exhibit poor sleep ( 34 ), and this would increase to 55% in those exhibiting problematic smartphone usage ( 4 ). In order to detect this difference using an independent chi-squared test of proportions with 90% power and 5% significance, we would need to include 650 participants. Building on this, to account for 15% missing data, we would need to include at least 780 participants in total.
The primary outcome was the association between sleep quality and smartphone addiction. Secondary outcomes were to determine: the association of smartphone addiction with demographics and usage characteristics; and the impact of reduction strategies on mitigating the effect of smartphone addiction on sleep.
Statistical Analysis
Demographic and smartphone usage characteristics of the sample were summarized, comparing participants with good, and poor sleep. Crude logistic regression models were included, to assess poor sleep and demographic (site, sex, and age) and smartphone usage characteristics. An adjusted multivariable logistic regression was carried out fitting the demographic with important characteristics found from the crude univariable analyses.
Both crude odds ratio[s] (OR) and adjusted OR (aOR) were presented alongside their respective 95% confidence intervals (95%CI), and P -values (<0.05 considered statistically significant). SPSS Versions 25 and 26 (IBM Corp., Armonk, N.Y., USA) were used to input and analyse data.
To determine the association between smartphone addiction and the demographic and usage characteristics, a multivariable logistic model adjusting for the same covariates as for the primary outcome was created. Due to multi co-linearity total usage, latest time of use and usage cessation prior to sleep were not fitted within the same analysis models.
Missing Data and Population Under Investigation
Individuals with missing item data of no more than 30% of the SAS-SV, or the adapted sleep score were proportionally mean imputed ( 35 ). Due to the completeness of the data collected, a complete case analysis was used.
Role of the Funding Source
There was no funding source for this study. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Characteristics of the Participants
We received 1,071 completed CRFs, of which 1,043 participants were eligible and included (completion rate 97.8%). The 28 excluded participants were ineligible due to age, or non-completion of the SAS-SV or items from the PSQI score. Of those included, 38 of the SAS-SV score, and 85 of the adapted PSQI had a single item of each domain missing and were (within participant) domain mean-imputed.
The mean age of the included participants was 21.1 (IQR 19–22, range 18–30), where 92.1% ( n = 961) were aged under 26, and 73.2% ( n = 763) of the participants were female ( Table 1 ). In terms of smartphone usage, 23.7% ( n = 247) used their phones for 3 h per day, while 18.5% ( n = 193) used their phones for more than 5 h daily. A large proportion of the young adult population exhibited poor sleep quality (61.6%, n = 643). Of those exhibiting smartphone addiction, 68.7% ( n = 279) had poor sleep quality compared to 57.1% ( n = 364) of those not exhibiting smartphone addiction. Of those participants that ceased smartphone use with 30 min of initiating sleep, 61.4% ( n = 478) had poor sleep, compared to 53.6% ( n = 45) of those who ceased use more than 1 h prior to initiating sleep.
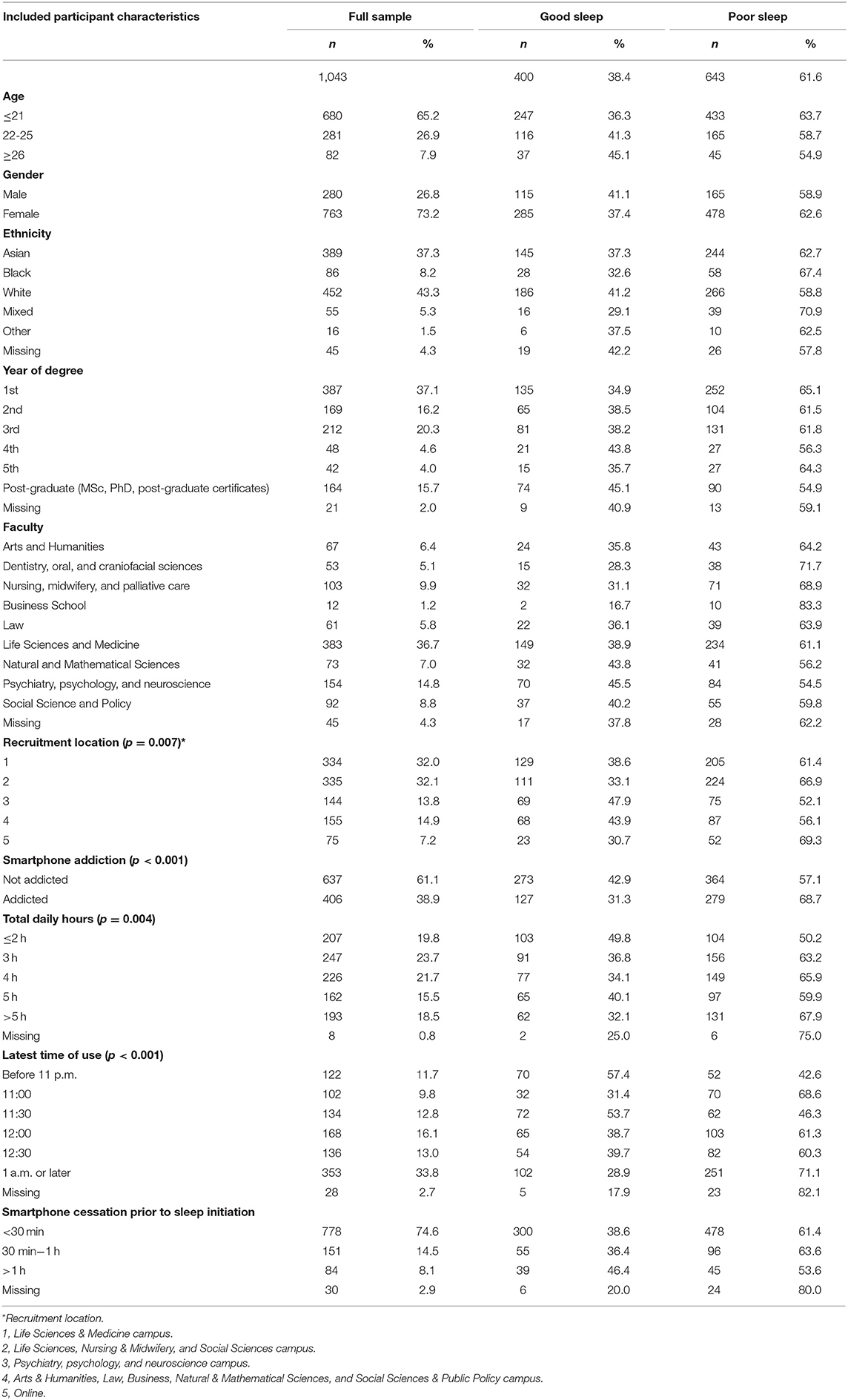
Table 1 . The included population sociodemographic and phone use characteristics.
Prevalence of Smartphone Addiction, Sociodemographic Characteristics and Smartphone Usage
The overall prevalence of smartphone addiction was 38.9% (95%CI: 35.9–41.9%; n = 406 / 1,043). This includes 35.7% of males who were addicted and 40.1% of females ( Table 3 ). For participants aged under 21 years, 42.2% exhibited smartphone addiction, compared to 34.2 and 28.0% of participants aged 22–25 years, and over 26 years, respectively. Of participants who used their smartphone for 2 or less hours per day, 20.3% were addicted, compared to 53.9% of those who used it for more than 5 h. Of those that stopped using their device more than an hour before bedtime, 23.8% exhibited addiction, compared to 42.0% of those stopping <30 min before bedtime ( Table 3 ).
Primary Outcome of Poor Sleep Associated With Smartphone Usage
We assessed demographic factors', phone usage characteristics', and reduction strategies' associations with poor sleep. Age, sex or site were not associated with poor sleep ( Table 2 ). There was an association between poor sleep and those addicted (compared to not addicted, OR = 1.65, 95%CI:1.27–2.14, p < 0.001); and screen time (compared to 3, 2 h OR = 0.59, 95%CI 0.41–0.86, p = 0.007).
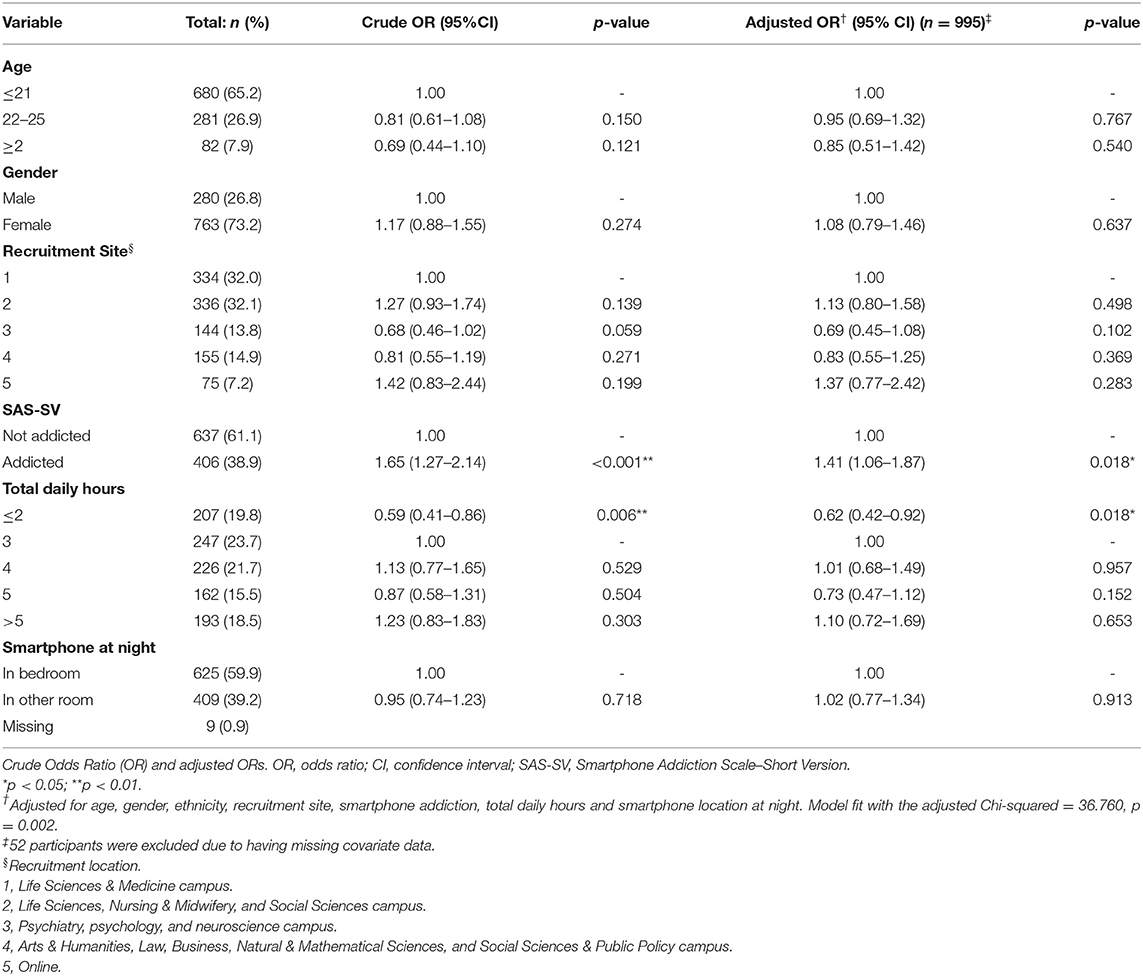
Table 2 . The association between poor sleep and smartphone addiction, using crude and multivariable logistic regression.
In the multivariable analysis after adjustment for age, gender, site, screen time, and location of phone at night, those addicted exhibited a 41% increased odds of poor sleep (aOR = 1.41, 95%CI: 1.06–1.87, p = 0.018) ( Table 2 ). Age, sex or site was not significantly associated with poor sleep. Total daily use of 2 or less hours reduced odds of poor sleep by 38% (aOR = 0.62, 95%CI: 0.42–0.92, p = 0.018).
Secondary Outcome of Demographics Associated With Smartphone Addiction
In a crude analysis, age, site and ethnicity were associated with smartphone addiction ( Table 3 ). There was a decreased odds of smartphone addiction in older groups, with 22–25 year olds having a 29% decreased odds compared with those 21 and younger (OR = 0.71, 95%CI: 0.53–0.95, p = 0.015), and participants 26 or older having a 47% decreased odds (OR = 0.53, 95%CI:0.32–0.89, p = 0.015). Those of Asian ethnicity had increased odds of addiction (OR = 1.75, 95%CI: 1.32–2.32, p < 0.001) when compared to a White reference population.
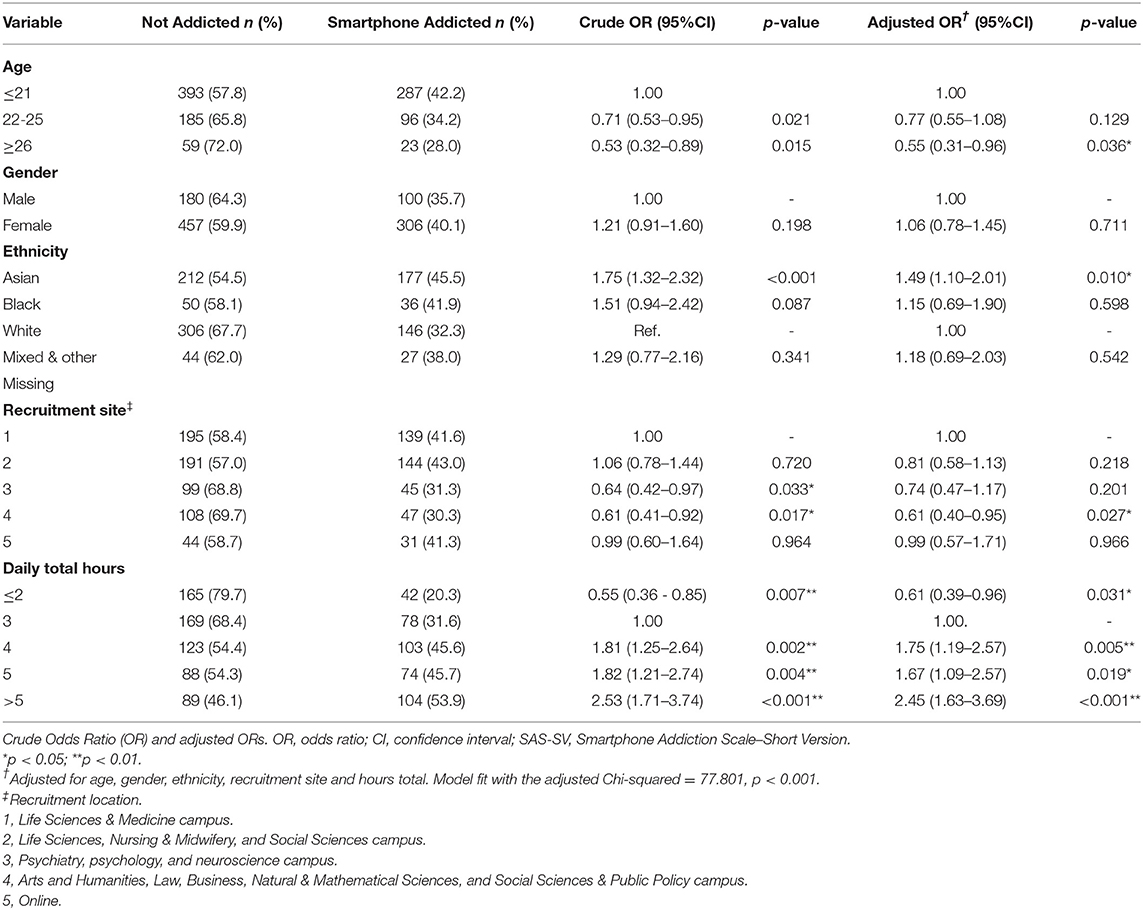
Table 3 . The association between sociodemographic factors and smartphone addiction, using crude and multivariable logistic regression.
The total number of hours spent on smartphones per day was significantly and positively associated with the SAS-SV score. After adjustment, age, ethnicity, site and screen time were associated with addiction.
Secondary Outcome of Smartphone Usage Characteristics and Addiction
Use for 2 h or less per day showed significantly decreased odds of smartphone addiction, compared with a reference of 3 h (OR = 0.55, 95%CI 0.36–0.85, p = 0.007, Table 4 ). Use for 5 or more hours per day showed a 2.5 times increase in odds (OR = 2.53, 95%CI: 1.71–3.74, p < 0.001). After adjustment for confounding factors, a consistent pattern of association was found between usage characteristics and addiction. There was a 39% reduction in odds of addiction for those using their phones for 2 h or less compared with typical usage of 3 h (aOR = 0.61; 95%CI 0.39–0.96; p = 0.031).
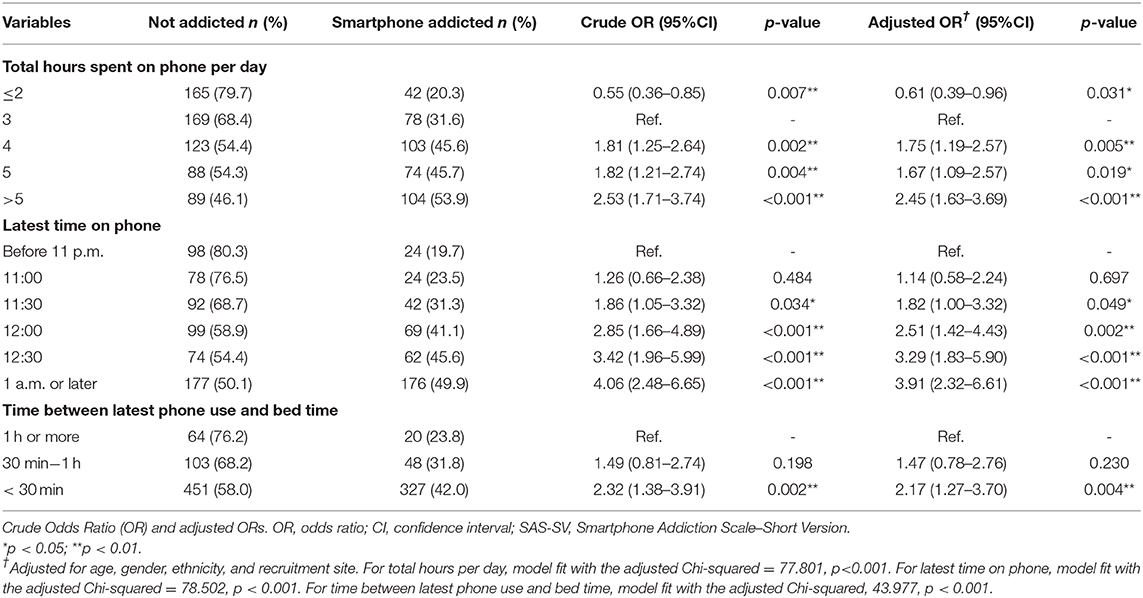
Table 4 . The association between smartphone use characteristics and smartphone addiction, using crude and multivariable logistic regression.
Later time of usage was also significantly associated with smartphone addiction in a crude logistic regression analysis ( Table 3 ). Use at 1 a.m. or later resulted in a four times increased risk of smartphone addiction, compared to those whose latest time of phone use was before 11 p.m. (OR = 4.06, 95%CI:2.48–6.65, p < 0.001). After adjustment, this finding remained consistent (aOR = 3.91, 95%CI:2.32–6.61, p < 0.001). Use within 30 min of initiating sleep resulted in a two times increased risk of smartphone addiction, which remained significant and consistent after adjustment (aOR = 2.17, 95%CI:1.27–3.70, p = 0.004).
Smartphone Usage Reduction Strategies
92.1% of participants attempted at least one reduction strategy ( Supplementary Tables 2 , 3 ). The most popular strategies were putting your phone on “do not disturb” or in “airplane mode” at night (67.7%); turning off notifications (68.4%); and putting your phone on silent (85.1%). Those who reported smartphone addiction used more strategies than those who did not (mean difference = 0.28, 95%CI: 0.021–0.54, p = 0.034).
This study included 1,043 young adults at a UK university and examined the phenomenon of smartphone addiction. The prevalence of smartphone addiction was 38.9%. Smartphone addiction had associations with both ethnicity and age. Smartphone addiction was associated with poorer sleep.
Our estimated prevalence is consistent with other reported studies in young adult populations globally, which are in the range of 30–45%, and with Yang et al. ( 29 ) who studied a similar university population in the UK ( 4 , 36 – 39 ). Noe et al. ( 40 ). estimate a UK prevalence of 19% using the SAS-SV with the same thresholds; however this study included an older population (up to 46 years) with a smaller sample size ( n = 64). The inverse association between age and smartphone addiction highlighted in our study may explain this variation in prevalence estimates. It is likely that differences in prevalence across the field may be due to the varying criteria of instruments used, or different applications of cut-off scores, and we have previously outlined the differences between the most widely used instruments [Sohn et al. ( 4 )].
Smartphone addiction was more prevalent amongst younger participants. This may reflect increased willingness amongst younger generations to adopt newer uses for smartphones (e.g., gaming, social media), which may confer greater risk of addiction ( 41 ). This could also related to younger participants potentially having more time for such endeavors. Participants from Asian ethnic backgrounds were at greater risk for smartphone indication, which may be due to cultural differences, such as social norms and characteristics including individualism ( 29 , 42 ). There was no association between smartphone addiction and gender, at odds with other studies which have found that females are more at risk, but it should be noted that the SAS-SV applied a gender-based standardized threshold to determine addiction ( 43 ).
Longer use was significantly associated with smartphone addiction, which is consistent with other studies that have found that increased exposure is linked with increased dependency ( 44 ). Furthermore, later time of use was also significantly associated with smartphone addiction, with use after 1 a.m. conferring a 3-fold increased risk. This association may be indicative of impaired control and use despite harm, which are a characteristic of a behavioral addiction. Smartphone ownership has previously been linked with more electronic media use in the night and later bedtimes in a survey of adolescents ( 45 ).
Our study provides further support to the growing body evidence that smartphone addiction has a deleterious impact on sleep ( 16 , 20 , 23 ). However, this relationship remained significant after adjusting for daily screen time (which was not seen as predictive after adjustment for smartphone addiction). This finding suggests that although duration of exposure, as with any addiction, is a risk factor for smartphone addiction, it is not the only determining component, reflecting the ICD-11 criteria for gaming and gambling disorders, in which duration of use may be one component of diagnosis but is not the only indicator ( 6 , 14 ). Furthermore, this result indicates that the relationship between sleep quality and smartphone addiction is not simply due to the duration of exposure, as suggested by other studies ( 46 ). It highlights that studies reporting a lack of association between smartphones and clinical outcome when using screen time alone should be interpreted with caution, as they have perhaps overlooked smartphone addiction as the harmful exposure ( 47 ).
The results of this study indicate that self-reported smartphone addiction is prevalent amongst young adults attending university and that it is linked with use at later times of the day in addition to total duration of use. Public health bodies should take this evidence into account when developing guidelines around smartphone use and sleep hygiene. Furthermore, clinicians, parents, and educators should be aware of the pervasiveness of smartphone addiction, and be prepared to consider the potential wide-reaching impact of smartphones on sleep. Despite the cross-sectional nature of this study, the findings suggest that the amount of time spent on their phones, and latest time of use can be indicative of those at risk for an addicted pattern of smartphone use. Should smartphone addiction become firmly established as a focus of clinical concern, those using their phones after midnight or using their phones for 4 or more hours per day are likely to be at high risk, and should guide administration of the SAS-SV. However, it should be noted that duration of smartphone use alone does not indicate smartphone addiction; it is merely indicates increased risk for development of this pattern of behavior. Future studies should examine longitudinal associations between smartphone use patterns and smartphone addiction, and between smartphone addiction and health harms, as well as exploring strategies to reduce harms, particularly in relation to sleep. As there is continued debate concerning the possibility that smartphones may be a means to access addictive material, such as social media applications or games, rather than the addiction themselves, future research should also focus on identifying types of use associated with higher risk of smartphone addiction.
This study collected data from a large sample of 18–30 year olds in the United Kingdom using a validated and widely used scale. There were several limitations to this study. Namely, due to the cross-sectional nature of data collection, no causal relationships can be drawn, and we cannot ignore the possibility of reverse causality. In particular, it is possible that poor sleep may be a result of concurrent mental health disorders that were not assessed for in this study, which may result in or be independently associated with increased smartphone usage and smartphone addiction risk. In addition, the self-reported data collection method we used may introduce common-method and response biases. Caution should be taken over the estimate of prevalence since a convenience sampling method was used. Additionally, caution should be taken in generalizing the results of this study, as the sampled population is not representative of the UK-wide population of young adults. Finally, these data were collected before the global pandemic, which may have led to a shift in smartphone usage patterns.
Conclusions
Smartphone addiction is prevalent and occurs more frequently amongst younger adults. Proxy measures of screen time were not synonymous with addiction; a validated addiction instrument should be used to capture this phenomenon. Those exhibiting smartphone addiction experienced poorer sleep.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical approval was received from the King's College Research Ethics Office (Study ID: 9138; MRS-18/19-9138). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
BC, NK, and SS: conceived the study, were responsible first draft of the manuscript, and approved the final draft of the manuscript. BC, NK, LK, and SS: generated the study material. LK and SS: collected the data. BC and SS: analyzed and interpreted the data. BC, NK, PR, and SS: edited the manuscript. BC was the study Guarantor. All authors contributed to the article and approved the submitted version.
Conflict of Interest
NK was employed by the NHS and was a trustee of the Gordon Moody Association. Her PhD (2010-2013) was joint-funded by the Wellcome Trust and GSK and during that time she received research materials from GSK and educational support from GSK and the Lundbeck Foundation. BC was partially supported by the Biomedical Research Centre at South London and Maudsley NHS Foundational Trust and King's College London.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.629407/full#supplementary-material
1. Van Velthoven MH, Powell J, Powell G. Problematic smartphone use: digital approaches to an emerging public health problem. Digital Health . (2018) 4:1–9. doi: 10.1177/2055207618759167
PubMed Abstract | CrossRef Full Text | Google Scholar
2. De-Sola Gutierrez J, Rodriguez de Fonseca F, Rubio G. Cell-phone addiction: a review. Front Psychiatry . (2016) 7:175. doi: 10.3389/fpsyt.2016.00175
CrossRef Full Text | Google Scholar
3. Kwon M, Kim D, Cho H, Yang S. The smartphone addiction scale: development and validation of a short version for adolescents. PLoS ONE . (2013) 8:e83558. doi: 10.1371/journal.pone.0083558
4. Sohn S, Rees P, Wildridge B, Kalk NJ, Carter B. Prevalence of problematic smartphone usage and associated mental health outcomes amongst children and young people: a systematic review, meta-analysis and GRADE of the evidence. BMC Psychiatry . (2019) 19:356. doi: 10.1186/s12888-019-2350-x
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-V. 5th Edn . American Psychiatric Publishing (2013). Available online at: https://dsm.psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596 (accessed January 21, 2021).
Google Scholar
6. World Health Organization. International Statistical Classification of Diseases and Related Health Problems . 11th Edn. (2018). Available online at: https://icd.who.int/browse11/l-m/en (accessed January 21, 2021).
7. Lin YH, Chiang CL, Lin PH, Chang LR, Ko CH, Lee YH, et al. Proposed diagnostic criteria for smartphone addiction. PLoS ONE . (2016) 11:e0163010. doi: 10.1371/journal.pone.0163010
8. Duke É, Montag C. Smartphone addiction, daily interruptions and self-reported productivity. Addict Behav Rep . (2017) 6:90–5. doi: 10.1016/j.abrep.2017.07.002
9. Grant JE, Lust K, Chamberlain SR. Problematic smartphone use associated with greater alcohol consumption, mental health issues, poorer academic performance, and impulsivity. J Behav Addict . (2019) 8:335–42. doi: 10.1556/2006.8.2019.32
10. Domoff SE, Sutherland EQ, Yokum S, Gearhardt AN. Adolescents' addictive phone use: associations with eating behaviors and adiposity. Int J Environ Res Public Health . (2020) 17:2861. doi: 10.3390/ijerph17082861
11. Xiang MQ, Lin L, Wang ZR, Li J, Xu Z, Hu M. Sedentary behavior and problematic smartphone use in Chinese adolescents: the moderating role of self-control. Front Psychol . (2020) 10:3032. doi: 10.3389/fpsyg.2019.03032
12. Horvath J, Mundinger C, Schmitgen MM, Wolf ND, Sambataro F, Hirjak D, et al. Structural and functional correlates of smartphone addiction. Addict Behav . (2020) 105:106334. doi: 10.1016/j.addbeh.2020.106334
13. Orben A, Przybylski AK. The association between adolescent well-being and digital technology use. Nat Hum Behav . (2019) 3:173–82. doi: 10.1038/s41562-018-0506-1
14. Kalk NJ, Carter B, Sohn S. Are smartphones addictive? An urgent question in the pandemic age. Health Policy Technol . (2021) (in press).
15. Billieux J, Maurage P, Lopez-fernandez O, Kuss DJ, Griffiths MD. Can disordered mobile phone use be considered a behavioral addiction? An update on current evidence and a comprehensive model for future research. Curr Addict Rep . (2015) 2:156–62. doi: 10.1007/s40429-015-0054-y
16. Panova T, Carbonell X. Is smartphone addiction really an addiction? J Behav Addict . (2018) 7:252–9. doi: 10.1556/2006.7.2018.49
17. Andreassen CS, Billieux J, Griffiths MD, Kuss DJ, Demetrovics Z, Mazzoni E, et al. The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: a large-scale cross-sectional study. Psychol Addict Behav . (2016) 30:252–62. doi: 10.1037/adb0000160
18. Kircaburun K, Griffiths MD. Instagram addiction and the big five of personality: the mediating role of self-liking. J Behav Addict. (2018) 7:158–70. doi: 10.1556/2006.7.2018.15
19. Demirci K, Akgönül M, Akpinar A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J Behav Addict . (2015) 4:85–92. doi: 10.1556/2006.4.2015.010
20. Carter B, Rees P, Hale L, Bhattacharjee D, Paradkar MS. Association between portable screen-based media device access or use and sleep outcomes a systematic review and meta-analysis. JAMA Pediatr . (2016) 170:1202–8. doi: 10.1001/jamapediatrics.2016.2341
21. Yang J, Fu X, Liao X, Li Y. Association of problematic smartphone use with poor sleep quality, depression, and anxiety: a systematic review and meta-analysis. Psychiatry Res. (2020) 284:112686. doi: 10.1016/j.psychres.2019.112686
22. Chung JE, Choi SA, Kim KT, Yee J, Kim JH, Seong JW, et al. Smartphone addiction risk and daytime sleepiness in Korean adolescents. J Paediatr Child Health. (2018) 54:800–6. doi: 10.1111/jpc.13901
23. Chindamo S, Buja A, DeBattisti E, Terraneo A, Marini E, Gomez Perez LJ, et al. Sleep and new media usage in toddlers. Eur J Pediatr. (2019) 178:483–90. doi: 10.1007/s00431-019-03318-7
24. Kim SY, Han S, Park E-J, Yoo HJ, Park D, Suh S, et al. The relationship between smartphone overuse and sleep in younger children: a prospective cohort study. J Clin Sleep Med . (2020) 16:1133–9. doi: 10.5664/jcsm.8446
25. Lin PH, Lee YC, Chen KL, Hsieh PL, Yang SY, Lin YL. The relationship between sleep quality and internet addiction among female college students. Front Neurosci . (2019) 13:599. doi: 10.3389/fnins.2019.00599
26. Zou L, Wu X, Tao S, Xu H, Xie Y, Yang Y, et al. Mediating effect of sleep quality on the relationship between problematic mobile phone use and depressive symptoms in college students. Front Psychiatry . (2019) 10:822. doi: 10.3389/fpsyt.2019.00822
27. Deloitte. State of the smart - Global Mobile Consumer Survey 2017: The UK Cut. Deloitte (2017). Available online at: https://www.deloitte.co.uk/mobileuk2017/assets/img/download/global-mobile-consumer-survey-2017_uk-cut.pdf (accessed November 11, 2019).
28. Lachmann B, Sindermann C, Sariyska RY, Luo R, Melchers MC, Becker B, et al. The role of empathy and life satisfaction in internet and smartphone use disorder. Frontiers in Psychology , 2018;9:398. doi: 10.3389/fpsyg.2018.00398
29. Yang Z, Asbury K, Griffiths MD. Do Chinese and British university students use smartphones differently? a cross-cultural mixed methods study. Int J Mental Health Addict. (2019) 17:644–57. doi: 10.1007/s11469-018-0024-4
30. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res . (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
31. Hawi NS, Samaha M. To excel or not to excel: strong evidence on the adverse effect of smartphone addiction on academic performance. Comput Educ . (2016) 98:81–9. doi: 10.1016/j.compedu.2016.03.007
32. Harris B, McCredie M, Fields S. Examining the psychometric properties of the smartphone addiction scale and its short version for use with emerging adults in the US. Comput Hum Behav Rep . (2020) 1:100011. doi: 10.1016/j.chbr.2020.100011
33. Dietch JR, Taylor DJ, Sethi K, Kelly K, Bramoweth AD, Roane BM. Psychometric evaluation of the PSQI in U.S. college students. J Clin Sleep Med . (2016) 12:1121–9. doi: 10.5664/jcsm.6050
34. Bruce ES, Lunt L, McDonagh JE. Sleep in adolescents and young adults. Clin Med J R Coll Physicians Lond . (2017) 17:424–8. doi: 10.7861/clinmedicine.17-5-424
35. Brain K, Lifford KJ, Carter B, Burke O, Mcronald F, Devaraj A, et al. Long-term psychosocial outcomes of low-dose CT screening: results of the UK lung cancer screening randomised controlled trial. Thorax . (2016) 71:996–1005. doi: 10.1136/thoraxjnl-2016-208283
36. Tateno M, Teo AR, Ukai W, Kanazawa J, Katsuki R, Kubo H, et al. Internet addiction, smartphone addiction, and hikikomori trait in Japanese young adult: social isolation and social network. Front Psychiatry . (2019) 10:455. doi: 10.3389/fpsyt.2019.00455
37. Karki S, Singh JP, Paudel G, Khatiwada S, Timilsina S. How addicted are newly admitted undergraduate medical students to smartphones?: a cross-sectional study from Chitwan medical college, Nepal. BMC Psychiatry . (2020) 20:95. doi: 10.1186/s12888-020-02507-1
38. Luk TT, Wang MP, Shen C, Wan A, Chau PH, Oliffe J, et al. Short version of the smartphone addiction scale in Chinese adults: psychometric properties, sociodemographic, and health behavioral correlates. J Behav Addict . (2018) 7:1157–65. doi: 10.1556/2006.7.2018.105
39. Mescollotto FF, Castro EM, Pelai EB, Pertille A, Bigaton DR. Translation of the short version of the smartphone addiction scale into Brazilian Portuguese: cross-cultural adaptation and testing of measurement properties. Braz J Phys Ther . (2019) 23:250–6. doi: 10.1016/j.bjpt.2018.08.013
40. Noë B, Turner LD, Linden DEJ, Allen SM, Winkens B, Whitaker RM. Identifying indicators of smartphone addiction through user-app interaction. Comput Hum Behav . (2019) 99:56–65. doi: 10.1016/j.chb.2019.04.023
41. Oviedo-Trespalacios O, Nandavar S, David J, Newton A, Demant D, Phillips JG. Problematic use of mobile phones in Australia… is it getting worse? Front Psychiatry . (2019) 10:105. doi: 10.3389/fpsyt.2019.00105
42. Jiang Q, Li Y, Shypenka V. Loneliness, individualism, and smartphone addiction among international students in China. Cyberpsychol Behav Soc Networking . (2018) 21:711–8. doi: 10.1089/cyber.2018.0115
43. Chen B, Liu F, Ding S, Ying X, Wang L, Wen Y. Gender differences in factors associated with smartphone addiction : a cross- sectional study among medical college students. BMC Psychiatry . (2017) 17:341. doi: 10.1186/s12888-017-1503-z
44. Cha S, Seo B. Smartphone use and smartphone addiction in middle school students in Korea: prevalence, social networking service, and game use. Health Psychology Open . (2018) 5:2055102918755046. doi: 10.1177/2055102918755046
45. Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A. Adolescents' electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. J Youth Adolesc . (2015) 44:405–18. doi: 10.1007/s10964-014-0176-x
46. Khouja JN, Munafò MR, Tilling K, Wiles NJ, Joinson C, Etchells PJ, et al. Is screen time associated with anxiety or depression in young people? Results from a UK birth cohort. BMC Public Health . (2019) 19:82. doi: 10.1186/s12889-018-6321-9
47. Przybylski AK, Orben A, Weinstein N. How much is too much? examining the relationship between digital screen engagement and psychosocial functioning in a confirmatory cohort study. J Am Acad Child Adolesc Psychiatry . (2020) 59:1080–8. doi: 10.1016/j.jaac.2019.06.017
Keywords: smartphone addiction, sleep, smartphone harm reduction strategies, screen time, young adults, behavioral addiction
Citation: Sohn SY, Krasnoff L, Rees P, Kalk NJ and Carter B (2021) The Association Between Smartphone Addiction and Sleep: A UK Cross-Sectional Study of Young Adults. Front. Psychiatry 12:629407. doi: 10.3389/fpsyt.2021.629407
Received: 14 November 2020; Accepted: 01 February 2021; Published: 02 March 2021.
Reviewed by:
Copyright © 2021 Sohn, Krasnoff, Rees, Kalk and Carter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ben Carter, ben.carter@kcl.ac.uk
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Share full article

I’m Addicted to My Phone. How Can I Cut Back?
Whether smartphone overuse constitutes a true addiction is still up for debate, but experts say there are ways to scale down.
Credit... Aileen Son for The New York Times
Supported by
By Annie Sneed
- Published Feb. 8, 2022 Updated Feb. 9, 2022
Q: I have my phone with me at all times and check it hundreds of times a day. Are there any proven ways to treat screen addiction?
Our work, social lives and entertainment have become inextricably tied to our devices, and the pandemic has made matters worse. One Pew Research Center survey conducted in April, for instance, found that among the 81 percent of adults in the United States who used video calls to connect with others since the beginning of the pandemic, 40 percent said they felt “worn out or fatigued” from those calls, and 33 percent said they’ve tried to scale back the amount of time they spent on the internet or on their smartphones.
Not all smartphone use is bad, of course. Sometimes, smartphones “make us happier, enriched and connect us to other people,” said Adam Alter, a marketing and psychology professor at New York University’s Stern School of Business. But many people want to cut back, and experts say there are effective ways to do it.
Is it really possible to be addicted to a smartphone?
Smartphone overuse can manifest in many ways. Maybe you regularly stay up late scrolling through Instagram or TikTok. Or the allure of your smartphone makes it difficult to be fully present for yourself, your work or those around you.
Phone or screen overuse isn’t officially recognized as an addiction (or a substance use disorder, as experts call it) in the American Psychiatric Association’s official manual of mental disorders. But “there is a growing number of mental health specialists who recognize that people can get addicted to their smartphones,” said Dr. Anna Lembke, an addiction expert and a professor of psychiatry and behavioral sciences at Stanford University.
Dr. Lembke noted that an addiction is partially defined by the three C’s:
Control: Using a substance or performing a behavior (like gambling) in ways that would be considered out of control, or more so than intended.
Compulsion: Being intensely mentally preoccupied with and using a substance (or performing a behavior) automatically, without actively deciding to do so.
Consequences: Continued use in spite of negative social, physical and mental consequences.
Many of us can recognize some of these behaviors in our own phone use.
Dr. Alter, on the other hand, doesn’t consider smartphone or screen overuse as a true addiction, and both he and Dr. Lembke noted that there is disagreement within the health community about this. “I don’t think it rises to the level of a medical addiction,” Dr. Alter said. “To me it’s more of a cultural malady than anything.”
Regardless of how you define it, both experts say there are ways to reduce your phone use.
Take a ‘screen fast.’
One approach Dr. Lembke has found to be highly effective in her clinical practice is to completely avoid using all screens, not just phones, for anywhere from a day to a month. This strategy hasn’t been formally studied in screen overuse patients in particular, she said, but the evidence for its use with other types of addictions, like alcoholism, suggests it can be effective.
How long you decide to fast will depend on your level of use, Dr. Lembke said. The average person might start with a 24-hour fast, for example, while someone with a more severe case of screen overuse may want to avoid screens for longer. Of course, a true fast may not be practical for many people, whether because of work or personal reasons, but the goal is to get as close to full avoidance as possible.
Dr. Lembke warned that many people — even those with milder screen overuse — may notice withdrawal symptoms initially, like irritability or insomnia, but that over time they’ll start feeling better. In her 25 years of seeing patients, Dr. Lembke has noticed that by the end of a one-month fast, the majority of her patients usually “report less anxiety, less depression, sleeping better, more energy, getting more done, as well as being able to look back and see in a more cleareyed way exactly how their screen use was affecting their lives,” she said. Those who fast for less than a month will still see benefits, she said, though they likely won’t be as dramatic.
After abstaining from screens for a period, she recommended reflecting on how you want your relationship with your devices to look like going forward.
Set rules around your daily smartphone use.
Besides a screen fast, Dr. Lembke and Dr. Alter recommended finding other, less stringent, ways to distance yourself from your phone each day. That might mean allotting times of the day or days of the week when you don’t use your phone at all, such as before and after work. It may also mean leaving your phone in the other room, keeping it out of your bedroom or putting everyone’s phone in a box outside of the kitchen during dinnertime.
“It sounds trivial, like an old-fashioned analog solution. But we know from decades of psychology that things closest to us in physical space have the biggest effect on us psychologically,” Dr. Alter said. “If you allow your phone to join you in every experience, you’re going to be drawn to it and you’re going to use it. Whereas if you can’t physically reach it, you’re going to use it less.”
Make your smartphone less appealing.
You can also make your phone less visually engaging, by changing the screen to grayscale or turning off notifications, for example. Dr. Alter suggested periodically rearranging the apps on your phone so that they become harder to find and less likely to lure you into a mindless loop of checking and rechecking simply out of habit.
Both experts advised deleting certain types of apps — especially the ones you know that you have a hard time avoiding (or if you don’t want to delete those apps, you can move them to the last screen on your phone to make them less accessible).
“Use apps that enrich your life, that add value and meaning or that you need for work, not ones that take you down a rabbit hole,” Dr. Lembke said. And if the apps that add value to your life are the same ones that you feel addicted to, Dr. Lembke recommended creating some space using the tips above.
“The big question to ask yourself with screens is: ‘What else could I be doing right now? Is there something I could be doing that would be better for me?’” Dr. Alter said. “That’s important now more than ever because of how much time we’ve been forced to spend on screens during the pandemic.”
Annie Sneed is a science journalist who has written for Scientific American, Wired, Public Radio International and Fast Company.
How to Make Your Smartphone Better
The process of backing up your smartphone has become so simplified that it takes just a few screen taps to keep copies of your photos, videos, and other files stashed securely in case of an emergency.
These days, smartphones include tools to help you more easily connect with the people you want to contact — and avoid those you don’t. Here are some tips .
Trying to spend less time on your phone? The “Do Not Disturb” mode can help you set boundaries and signal that it may take you a while to respond .
To comply with recent European regulations, Apple will make a switch to USB-C charging for its iPhones. Here is how to navigate the change .
Photo apps have been using A.I. for years to give you control over the look of your images. Here’s how to take advantage of that .
Advertisement
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Behav Addict
- v.7(2); 2018 Jun
Is smartphone addiction really an addiction?
Tayana panova.
1 The Department of Psychology, Ramon Llull University, Barcelona, Spain
Xavier Carbonell
In light of the rise in research on technological addictions and smartphone addiction in particular, the aim of this paper was to review the relevant literature on the topic of smartphone addiction and determine whether this disorder exists or if it does not adequately satisfy the criteria for addiction.
We reviewed quantitative and qualitative studies on smartphone addiction and analyzed their methods and conclusions to make a determination on the suitability of the diagnosis “addiction” to excessive and problematic smartphone use.
Although the majority of research in the field declares that smartphones are addictive or takes the existence of smartphone addiction as granted, we did not find sufficient support from the addiction perspective to confirm the existence of smartphone addiction at this time. The behaviors observed in the research could be better labeled as problematic or maladaptive smartphone use and their consequences do not meet the severity levels of those caused by addiction.
Discussion and conclusions
Addiction is a disorder with severe effects on physical and psychological health. A behavior may have a similar presentation as addiction in terms of excessive use, impulse control problems, and negative consequences, but that does not mean that it should be considered an addiction. We propose moving away from the addiction framework when studying technological behaviors and using other terms such as “problematic use” to describe them. We recommend that problematic technology use is to be studied in its sociocultural context with an increased focus on its compensatory functions, motivations, and gratifications.
Introduction
The recent development of the multifunctional smartphone and its subsequent global popularity has changed the communication and information landscape; remolded the interests, values, and desires of many users; and triggered concerns around the world about overuse and addiction. In the past few years, there has been a surge in literature on behavioral addictions to studying ( Atroszko, Andreassen, Griffiths, & Pallesen, 2015 ), tanning ( Nolan & Feldman, 2009 ), cosmetic surgery ( Suissa, 2008 ), Argentinean tango ( Targhetta, Nalpas, & Perney, 2013 ), Harry Potter ( Rudski, Segal, & Kallen, 2009 ), and various other potential topics. This increase in interest is particularly notable in the discussion on mobile phone addiction ( Bianchi & Phillips, 2005 ; Billieux, Maurage, Lopez-Fernandez, Kuss, & Griffiths, 2015 ; Chóliz, 2010 ; Pedrero, Rodríguez, & Ruiz, 2012 ), which has more recently evolved into smartphone addiction.
Mobile phones and smartphones are both mobile, personal devices that indicate social identity and status, but the main differentiating feature between them is that a smartphone has permanent access to the Internet and consequently all of the Internet’s appealing and problematic content. Smartphones provide numerous gratifications, such as sociability, entertainment, information finding, time management, coping strategies, and social identity maintenance ( Bian & Leung, 2015 ; Kuss, Kanjo, et al., 2018 ; Kwon et al., 2013 ; Lin et al., 2014 ; Skierkowski & Wood, 2012 ). The smartphone has become an essential part of daily life and research has shown that certain people become so attached to their device that they experience separation anxiety when it is not with them ( Cheever, Rosen, Carrier, & Chavez, 2014 ; King et al., 2013 ). The device can even be comforting in times of stress, offering a “security blanket” effect whereby the initial negative response to a stressor is lowered in a similar way that occurs with children and a comfort object like a blanket ( Panova & Lleras, 2016 ).
The smartphone’s popularity and users’ deep connection with it has therefore awoken concerns about its addiction potential. The American Psychiatric Association ( APA, 2013 ) first categorized a behavior – gambling – as a non-substance-related addictive disorder and recommends further research on Internet gaming disorder. However, at this time, no mention has been made of smartphone addiction in either the DSM-5 or in the ICD-11’s draft. Nevertheless, research on smartphone and mobile phone addiction has notably increased in recent years ( Aljomaa, Mohammad, Albursan, Bakhiet, & Abduljabbar, 2016 ; Bian & Leung, 2015 ; Chiu, 2014 ; Darcin et al., 2016 ; Demirci, Akgönül, & Akpinar, 2015 ; Fu Yuan, Chiu, & Huang, 2012 ; Haug et al., 2015 ; Hawi & Samaha, 2016 ; Körmendi, Brutóczki, Végh, & Székely, 2016 ; Leung, 2007 ; Lin et al., 2014 ; Lopez-Fernandez, 2015 ; Roberts, Pullig, & Manolis, 2015 ; Salehan & Negahban, 2013 ; Van Deursen, Bolle, Hegner, & Kommers, 2015 ) and there seems to be a rising tendency to label popular technological behaviors as addictive.
Even though the disorder is not recognized in psychiatry manuals, screening studies estimate that smartphone addiction ranges from anywhere between just above 0% and 35%, with one study reporting that 48% of undergraduate university students were smartphone addicted ( Aljomaa et al., 2016 ), and the most frequent range being between 10% and 20% (see Billieux, Maurage, et al., 2015 and Carbonell et al., 2012 for a review). However, most of these studies use self-report measures, thereby relying on the accuracy of users’ perceptions about their own use, and each study uses different methods and questionnaires to determine the existence of addiction.
Before pathologizing technology-related behaviors, it is important to analyze them in context. For example, there has been a considerable amount of research conducted on smartphone addiction in countries, such as South Korea, China, and Taiwan ( Carbonell, Guardiola, Fuster, Gil, & Panova, 2016 ; Sánchez-Carbonell, Guardiola, Bellés, & Beranuy, 2005 ). It has been suggested that this may be because the cultural norms in some Asian societies make it difficult for people to find the time and opportunity to freely socialize with one another and be themselves, which in turn contributes to the high use of personal mobile devices ( Ito, 2005 ). Other culturally oriented studies have highlighted how the values of certain cultures are reflected and expressed in mobile phone behavior ( Horst & Miller, 2005 ; Leonardi, Leonardi, & Hudson, 2006 ). These studies suggest that the sociocultural context has an important influence on why and how certain smartphone behaviors occur and therefore should be considered when studying problematic use. Professional, social, and academic contexts should also be considered when studying problematic smartphone behavior, because much of smartphone use is dependent on professional, social, or academic demands.
Most of the smartphone addiction studies at the moment focus on discovering what percentage of the sample are smartphone-addicted and then looking for correlations between the addiction scores with various other behaviors and characteristics. However, at this time, there is not a strict set of standardized criteria applied to the diagnosis of smartphone addicts. Moreover, a critical analysis of whether smartphone use can even be considered addictive has not been conducted. With all the above in mind, this paper is going to consider whether smartphones can be considered addictive by analyzing the literature on the subject through the lens of addiction criteria and determining whether the concern about “smartphone addiction” is merited.
Smartphone Addiction Analyzed Through Addiction Criteria
In order for substance and behavioral addictions to be comparable, they must share the core symptoms of the disorder and have many similarities in phenomenology and adverse consequences. According to Goodman ( 1990 ), addiction defines a condition whereby a problematic behavior is characterized by (a) recurrent failure to control the behavior and (b) continuation of the behavior despite significant negative consequences. The well-accepted symptoms of addiction proposed by Griffiths are mood modification, tolerance, salience, withdrawal symptoms, conflict, and relapse ( Griffiths, 1995 , 2005 ). However, the descriptions of these criteria can cover a broad-spectrum of severity, which can be more or less significant. Recently, Saunders et al. ( 2017 ) stated that in the ICD-11 draft, the primary features of substance dependence are (a) a strong internal drive to use the substance, coupled with an impaired ability to control that use; (b) increasing priority given to using the substance than doing other activities; and (c) persistence of use despite harm and adverse consequences. On the topic of behavioral addiction specifically, Kardefelt-Winther et al. ( 2017 ) proposed a definition of two components: (a) significant functional impairment or distress as a direct consequence of the behavior and (b) persistence over time. We can therefore summarize the theoretical definition of addiction from its various sources by two key points: the (severe) harm, impairment, or negative consequences and the psychological (craving, salience, and loss of control) and physical dependence (tolerance and withdrawal) that leads one to carry on the behavior. At this point, we will review the critical criteria for addiction and determine how well smartphone addiction satisfies them.
Significant functional impairment
One of the essential features of a behavioral addiction should be the functional impairment in clinical settings ( Kardefelt-Winther et al., 2017 ). If the harm is not significantly severe, the disorder would be better classified as problematic or maladaptive use or else considered as a side effect/manifestation of another primary disorder. The screening studies have indicated negative consequences associated with high smartphone use, such as interpersonal and academic problems ( Bian & Leung, 2015 ; Darcin et al., 2016 ; Hawi & Samaha, 2016 ; Murdock, 2013 ). However, although face-to-face relationships may suffer with the prioritization of smartphone use over in vivo interaction and academic achievement may be negatively impacted by high use, these problems can also be associated with a variety of other reasons and stressors that are not considered to fall in the category of addiction.
A subsection of functional impairment related to addiction is also financial problems. With drug addictions, gambling addiction and others, one of the primary problems is the significant loss of money associated with maintaining the addiction. When Billieux, Van der Linden, and Rochat ( 2008 ) built the Problematic Mobile Phone Use Questionnaire (PMPU-Q), one of the dimensions they looked at was the financial problems associated with mobile phone use. However, this dimension has been excluded in the Problematic Mobile Phone Use Questionnaire – Revised ( Kuss, Harkin, Kanjo, & Billieux, 2018 ), because the new use policies and rates of telecommunications companies make it insignificant, once again highlighting the importance of a technology-related behavior’s sociocultural context.
It is also important to consider that although many studies have addressed the issue of smartphone addiction, it has not been reported in any of those reviewed that the researchers or the ethics committees in the universities felt the ethical obligation to provide a psychological treatment to the “phone addicts” identified in the research. This is itself an important indicator of the level of functional impairment exhibited by “addictive” smartphone use. It is necessary to distinguish serious psychopathology, such as addiction from passion, high engagement, lack of adaptive, self-control, or coping strategies, so that we do not undermine the severity of mental disorders ( Carbonell & Panova, 2017 ; Petry & O’Brien, 2013 ).
Severe physical consequences
One main characteristic of an addiction is the impairment of physical health. Smokers have little psychological impairment, but they suffer from demonstrable physical harm. This does not seem to be the case for smartphone use. There are no more physical consequences than mild tendinitis ( Fernandez-Guerrero, 2014 ) and anecdotal reports of suffering from lightheadedness or blurred vision, pain in the wrists, or at the back of the neck and urban incidents from people talking/texting while walking.
Tolerance, in the framework of mobile phone addiction, has been described as “ a gradual increase in mobile phone use to obtain the same level of satisfaction, as well as the need to substitute operative devices with the new models that appear on the market ” ( Chóliz, 2010 ). In the screening studies, the factor analysis put many items about loss of control in a tolerance factor, i.e, “ I try cutting my smartphone usage time, but I fail ” ( Kim, Lee, Lee, Nam, & Chung, 2014 ) and “ I use smartphone for a longer period of time and spend more money than I intended ” ( Lin et al., 2014 ). The number of hours employed on the phone is used as criteria without considering that smartphone use is a normalized part of everyday life in many societies today even when engaged with very frequently ( Kardefelt-Winther et al., 2017 ); therefore, increase in use should not be a valid criterion.
Other items used in questionnaires are vague, such as “ I need to spend an increasing amount of time on smartphone to achieve same satisfaction as before ” ( Lin et al., 2014 ). Although tolerance may be a true aspect of smartphone use, variables such as satisfaction and enjoyment are rarely operationalized and standardized, thereby leaving them open to interpretation by each participant. In addition, without exploring the motivations behind increased use of the smartphone, its consequences cannot be categorized as indicative of a disorder. For some, higher use of the device could mean being more active at work or increasing one’s social circle. As Billieux et al. ( 2014 ) concluded, inferring tolerance based on the increasing use of the mobile phone is highly tentative. Similarly, King, Herd, and Delfabbro ( 2018 ) conclude that the use of time spent with a technology as a measure of tolerance may be simple and objective but can be criticized, because it does not capture the essence of what people are actually doing with the technology and why. This same reasoning can be applied to smartphone-related tolerance measures, such as “time on the phone” or “number of messages.” Increased time on the smartphone and higher messaging behavior can be indicators of problematic use or they may indicate a promotion at work, new friends, etc. Therefore, a deeper analysis of motivations and gratifications associated with the behaviors is necessary.
In the Smartphone Addiction Scale ( Kwon et al., 2013 ), the item “ Having my smartphone in my mind even when I am not using it ” relates to the concept of salience. In Griffiths’ ( 2005 ) component model of addiction, salience is when the activity in question becomes the most important activity to the user and dominates their thinking. Although many smartphone users may agree that they think about the smartphone frequently, even when they are not using it, so much of a user’s social, professional, and personal life is mediated through the smartphone that we would argue it is reasonable for the device to be at the forefront of one’s thoughts and that this does not constitute an indicator of addiction.
It is not mandatory that a substance produces withdrawal to be considered a substance-use disorder (i.e., hallucinogens) and, besides that, withdrawal is not one of the criteria for gambling disorder ( APA, 2013 , p. 585). In the case of Internet gaming disorder, Kaptsis, King, Delfabbro, and Gradisar ( 2016 ) also concluded after a systematic review that available evidence on the existence of true addictive withdrawal in Internet gaming is very underdeveloped. But scholars in smartphone addiction found that some items could be grouped in a withdrawal factor when questionnaires were administered to their samples. Examples of items loading the withdrawal factor are: “ I feel restless and irritable when the smartphone is unavailable ” ( Lin et al., 2014 ), “ It would be painful if I am not allowed to use smartphone ” ( Kim et al., 2014 ), and “ Bringing my smartphone to the toilet even when I am in a hurry to get there ” ( Kwon et al., 2013 ). However, this reported discomfort of being far from the smartphone must be viewed in context.
For most users, after a period of time and adaptation, the multifaceted functionality of the smartphone becomes an essential part of everyday life, therefore not having it on hand leads to the need for restructuring and adapting one’s regular activities, something which is always initially uncomfortable and/or stressful. In addition, being far from the device can be a stressful state for many because of the awareness that their contacts, both personal and professional, will feel displeasure and/or offense at being ignored ( Thomée, Dellve, Harenstam, & Hagberg, 2010 ). Therefore, the reaction of stress at having this important tool missing is not abnormal. It is also important to note that smartphones are often expensive and contain sensitive personal information; therefore, a primary stressor during their absence may be a fear that the device can fall into the wrong hands, get damaged, or get stolen, which are normal reactions when viewed in context.
Loss of control
Loss of control is, besides craving and salience, a component of psychological dependence ( Sánchez-Carbonell, Beranuy, Castellana, Chamarro, & Oberst, 2008 ). In the case of smartphone use, the loss of control exhibited is still far beneath the threshold of severity that would merit clinical attention. Again, the screening test literature supports the evidence of psychological dependence and loss of control, but the level of its severity is not often reported or standardized. For example, items of loss of control are “ I try to spend less time on smartphone, but the efforts were in vain ” (see Lin et al., 2014 ); “ I fail to control the impulse to use smartphone ” (see Lin et al., 2014 ); and “ I find myself engaged on the mobile phone for longer periods of time than intended ” (see Bianchi & Phillips, 2005 ). However, even when a university student rates this type of item high on a Likert scale, the answer does not necessarily have clinical relevance ( Billieux, Schimmenti, Khazaal, Maurage, & Heeren, 2015 ; Kardefelt-Winther, 2015 ). If there is not a perceived severe consequence associated with failure to limit smartphone use and if there are perceived benefits of the activities on the smartphone, then this type of “loss of control” is not indicative of a “disorder.”
Stability of the dysfunctional behavior
There are no longitudinal studies to confirm stability and durability of the disorder. In behavioral and substance addictions, spontaneous remission ( Stall & Biernacki, 1986 ; Walters, 2000 ) may occur not because the disorder occurs and then spontaneously disappears but because there is no real disorder in the first place. However, there is insufficient research on the topic to make conclusions in this regard.
This condition is very distressing and harmful in substance addicts ( Marlatt & Gordon, 1985 ), but there is no information about relapse with the presumed smartphone addiction. However, this may be because there are no clinical samples and longitudinal studies.
“Better explained by”
Finally, one important criterion is that the disorder is not better explained by another condition. For example, the criteria B for gambling disorder is “The gambling behavior is not better explained by a manic episode” ( APA, 2013 ). As Billieux et al. ( 2014 ) have commented in their case study, “Thalia” could fit the criteria for mobile phone addiction but her condition could be better understood through a psychological process-based clinical formulation where the irrational beliefs about the self, the dependent relationship-maintenance style, the insecure attachment style, the low impulse control in emotional contexts, the repetitive negative thoughts, and the reassurance behaviors could better explain her mobile phone overuse. According to Billieux et al. ( 2014 ), this overuse should not be directly targeted by a psychological intervention but will improve as the emotional distress improves. The negative effects associated with smartphone use may therefore be better explained by other conditions in many other instances.
Issues with the Screening Studies
At present, we want to point out that the symptoms of smartphone addiction have been identified in screening and correlational studies with healthy people (many of the university students) instead of clinical samples (not identified). It is worth stating that Billieux, Schimmenti, et al. ( 2015 ); Carbonell and Panova ( 2017 ); and Kardefelt-Winther et al. ( 2017 ) have already criticized in detail how these studies give undue support to behavioral addictions and the same analysis could be applied to the smartphone. In the studies, the “addictive” use of the phone is first described according to a variety of psychological symptoms like excessive use, high economic cost, academic, work and family relationship impairment, tolerance, salience, withdrawal, and so on using a variety of diverse scales and questionnaires. After the often arbitrary definition of addictive smartphone use is outlined, screening tools identify the “addicts,” estimate their prevalence and correlate the “disorder” with various intrapsychic measures, such as shyness ( Bian & Leung, 2015 ), stress ( Chiu, 2014 ; Van Deursen et al., 2015 ), depression ( Demirci et al., 2015 ; Elhai, Levine, Dvorak, & Hall, 2016 ), self-esteem ( Fu Yuan et al., 2012 ), life satisfaction ( Hawi & Samaha, 2016 ), loneliness ( Bian & Leung, 2015 ), and self-perceived sleep disturbances ( Demirci et al., 2015 ) among others.
Regarding these studies, let us address some primary concerns: (a) there is a lack of longitudinal studies to confirm the disorder’s stability; (b) the screening instruments used are not valid for diagnosis; (c) there is a large probability of false positives; (d) there are many arbitrarily designed items like “ eleven or more calls or SMS messages per day (high use) ” (i.e, Thomée, Härenstam, & Hagberg, 2011 ); (e) exploratory studies rely on self-report data, which are collected using convenience samples; and (f) there is a lack of consistency in methodology, definitions, measurement, cut-off scores, and diagnostic criteria across studies. These concerns highlight the general lack of construct validity surrounding smartphone addiction research and the consequent lack of strength of its conclusions.
To study clinical-level impairment such as addiction, it is recommended to assess the functional impairment in clinical settings, supported by a health professional, rather than through surveys implemented in a healthy population ( Kardefelt-Winther et al., 2017 ). There is one case study reported in the academic literature on mobile phone addiction, in which the authors conclude that “… social network addiction is a better concept to describe Anette’s case than the cell phone addiction ” ( Körmendi et al., 2016 ). There is one other mobile phone addiction case study ( Billieux et al., 2014 ), but its presentation has only a pedagogical purpose.
Smartphone as an Object
The smartphone is a physical object used to access the Internet and its content. In comparison with substance addiction, this object would be like the glass in alcohol addiction or the needle in heroin addiction. “Needle addiction” ( Levine, 1974 ) and “bottle addiction” are visual words and are accepted in colloquial language, but the addiction is to the substance not to the vessel or to the route of administration. There is a tendency in research on this subject to address smartphones as a single addictive entity, measuring the level of “smartphone use” or “smartphone addiction,” although the smartphone itself is causing the problems in the way that a drug does. The physical, mobile aspect of the smartphone facilitates problematic Internet behaviors (i.e., obsessive social media use, porn, and gambling addiction) by making them accessible anytime and anywhere and therefore increasing how often they are used, but the problem is not the smartphone device itself. The problems arising from smartphone use are dependent on what activities the user engages with while on the smartphone, the motivations for engaging with these activities, and the gratifications received from them which then reinforce continued use ( Jeong, Kim, Yum, & Hwang, 2016 ; Lopez-Fernandez et al., 2017 ).
Confusing Smartphone Addiction with Other Addictions
In the discussion on technological addictions, it is important to distinguish between addictions to the Internet and addictions on the Internet ( Király et al., 2014 ). When a pathological gambler uses the Internet to play poker, it is more accurately an addiction on the Internet, secondary to his first problem (gambling). Another prevalent activity on the smartphone is game playing ( Balakrishnan & Griffiths, 2018 ; Lopez-Fernandez, Männikkö, Kääriäinen, Griffiths, & Kuss, 2018 ). Balakrishnan and Griffiths ( 2018 ) found frequent claims of “addictiveness” of smartphone games by game players; however, in this scenario, the potential addiction would be to the gaming behavior specifically, not to the device as a whole. Thus, to use the smartphone for gambling or to engage in other addictive behaviors should not be confused with a smartphone addiction ( Lopez-Fernandez et al., 2017 ).
Related to the above is the issue of the relationship between “smartphone addiction” and “Internet addiction.” The smartphone is used to access the Internet; therefore, if there is an addictive problem, it is with the Internet and not with the smartphone. This same reasoning has been used to distinguish between an Internet addiction and addictions to specific activities carried out on the network, with one of the most prevalent behaviors online being social networking ( Jeong et al., 2016 ; Muñoz-Miralles et al., 2013 ; Pontes, Szabo, & Griffiths, 2015 ; Salehan & Negahban, 2013 ). Since many people access their social networks on their device, it can lead to the impression of device addiction; however, the rationale of distinguishing the platform from the behavior needs to be observed. We argue that common behaviors conducted on the smartphone, such as specific Internet uses, social networking, and gaming, should be cautiously explored in the context of their own motivations, gratifications, and sociocultural context and not as components of a smartphone addiction.
Terminology
As we previously stated in the study of Carbonell and Panova ( 2017 ), the problems associated with the conceptualization and acceptance of technological and behavioral addictions may be, to a great degree, an issue related to the terminology. We would argue that it is unlikely that the majority of scientists in this field believe smartphone “addiction” is comparable to heroin or tobacco addiction in terms of the severity and/or associated health problems; however, there is no other accepted term for a behavior that manifests similar problems with a lack of self-control, attachment, high use, and problematic consequences. Therefore, for lack of a better word, “addiction” has become an accepted umbrella term. However, this is a problem because extending the term “addiction” to conditions better described as problematic or maladaptive use can undermine the integrity of this term and the severity of disorders that truly merit it. It can also misguide the research and treatment efforts for the current problem, because they are being designed within an addiction framework when in actuality a different approach may be more suitable and effective. Therefore, the authors propose seeking a different term to associate with this problem in the academic literature, such as problematic use. In fact, recent papers on the topic use alternative terms such as “problematic smartphone use” ( Kuss, Kanjo, et al., 2018 ) or “self-reported dependence on mobile phones” ( Lopez-Fernandez et al., 2017 ).
Conclusions
The aim of this study was to critically consider whether smartphone addiction exists. After reviewing the literature on smartphone addiction, we have concluded that the weakness of screening and correlational studies, the scarcity of the case and longitudinal studies, the vague definitions of the criteria for smartphone addiction, and the lack of severe psychological or physical consequences associated with it do not support the existence of smartphone addiction at this time and we therefore suggest moving away from an addiction framework when addressing and studying this issue.
Although certain parallels exist between classically defined addiction and high use of the smartphone, the levels of severity for smartphone use are much lower, an important fact since severity of impairment is one of the primary criteria for distinguishing between addiction and problematic behavior. A person who bites their nails compulsively also exhibits self-harm, loss of control, physical consequences, relapse, and craving, but we do not label it a nail-biting addiction. It is important not to diagnose excessive, maladaptive, or problematic behavior as an addictive in order to avoid generating false epidemics of misidentified pseudopatients ( Frances & Widiger, 2012 ) and pathologizing common behaviors ( Kardefelt-Winther et al., 2017 ).
It is important to note that research shows that smartphone use is associated with various problems. In correlational studies, overuse of the smartphone is associated with various mental health concerns, such as anxiety, depression, stress, and low self-esteem (for a review, see Elhai et al., 2016 ; Panova & Lleras, 2016 ). However, the existence of negative consequences is not the same as the existence of addiction. We would like to shift the perspective on this issue away from an addiction framework and view smartphone use in a context that considers the compensatory functions of the device and how it interacts with the user’s needs, desires, and primary disorders.
One reason that smartphone use may be pathologized is because the role the device plays in people’s lives is not yet fully understood. Surrat ( 1999 ) has explained how the limited understanding of any new information and communication technologies is often taken advantage of by the media who capitalize on the suspicion that accompanies new technological developments and publish sensationalist news stories about addictions and psychopathology, which contribute to the social construction of a pathology. More recently, Frances and Widiger ( 2012 ) have detailed a background of overdiagnosis in mental health. In our opinion, to consider intensive smartphone use a disorder in the same category as cocaine or alcohol addiction undermines the severity of addiction.
In summary, the smartphone’s defining features – portable, quick, convenient, and private – may facilitate the access to certain problematic behaviors and the corresponding rewards received from them that make the behaviors more frequent, but addiction is more than a matter of impulse-control and excessive behavior. Therefore, although the media may turn to terminology such as “addiction” because it seems like the closest metaphor for the technology-related behavioral problems, we are observing in society today, we believe it is the responsibility of academics to use more accurate language and diagnostic terms and at the current moment the research does not support the claim that addiction is a correct term for the problems associated with smartphone use. The use of smartphones and other devices are associated with various negative consequences and research on them should continue; however, in order to address and treat their associated problems accurately and effectively, they should not be misdiagnosed as consequences of addiction.
Funding Statement
Funding sources: No financial support was received for this study.
Authors’ contribution
Both the authors TP and XC developed the study aims; analyzed the papers referenced within; and actively participated in developing the critiques, theories, and conclusions expressed within the paper.
Conflict of interest
The authors declare no conflict of interest.
- Aljomaa S. S., Mohammad M. F., Albursan I. S., Bakhiet S. F., Abduljabbar A. S. (2016). Smartphone addiction among university students in the light of some variables . Computers in Human Behavior, 61, 155–164. doi: 10.1016/j.chb.2016.03.041 [ CrossRef ] [ Google Scholar ]
- American Psychiatric Association [APA]. (2013). Diagnostic and statistical manual of mental disorders (DSM-5) . Arlington, VA: American Psychiatric Association. [ Google Scholar ]
- Atroszko P. A., Andreassen C. S., Griffiths M. D., Pallesen S. (2015). Study addiction – A new area of psychological study: Conceptualization, assessment, and preliminary empirical findings . Journal of Behavioral Addictions, 4 ( 2 ), 75–84. doi: 10.1556/2006.4.2015.007 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Balakrishnan J., Griffiths M. D. (2018). Perceived addictiveness of smartphone games: A content analysis of game reviews by players . International Journal of Mental Health and Addiction . doi: 10.1007/s11469-018-9897-5 [ CrossRef ] [ Google Scholar ]
- Bian M., Leung L. (2015). Linking loneliness, shyness, smartphone addiction symptoms, and patterns of smartphone use to social capital . Social Science Computer Review, 33 ( 1 ), 61–79. doi: 10.1177/0894439314528779 [ CrossRef ] [ Google Scholar ]
- Bianchi A., Phillips J. G. (2005). Psychological predictors of problem mobile phone use . CyberPsychology & Behavior, 8 ( 1 ), 39–51. doi: 10.1089/cpb.2005.8.39 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Billieux J., Maurage P., Lopez-Fernandez O., Kuss D. J., Griffiths M. D. (2015). Can disordered mobile phone use be considered a behavioral addiction? An update on current evidence and a comprehensive model for future research . Current Addiction Reports, 2 ( 2 ), 156–162. doi: 10.1007/s40429-015-0054-y [ CrossRef ] [ Google Scholar ]
- Billieux J., Philippot P., Schmid C., Maurage P., De Mol J., Van der Linden M. (2014). Is dysfunctional use of the mobile phone a behavioural addiction? Confronting symptom-based versus process-based approaches . Clinical Psychology and Psychotherapy, 22 ( 5 ), 460–468. doi: 10.1002/cpp.191010.1002/cpp.1910 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Billieux J., Schimmenti A., Khazaal Y., Maurage P., Heeren A. (2015). Are we overpathologizing everyday life? A tenable blueprint for behavioral addiction research . Journal of Behavioral Addictions, 4 ( 3 ), 119–123. doi: 10.1556/2006.4.2015.009 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Billieux J., Van der Linden M., Rochat L. (2008). The role of impulsivity in actual and problematic use of the mobile phone . Applied Cognitive Psychology, 22 ( 9 ), 1195–1210. doi: 10.1002/acp.1429 [ CrossRef ] [ Google Scholar ]
- Carbonell X., Chamarro A., Griffiths M. D., Oberst U., Cladellas R., Talarn A. (2012). Problematic Internet and cell phone use in Spanish teenagers and young students . Anales de Psicología, 28 ( 3 ), 789–796. doi: 10.6018/analesps.28.3.156061 [ CrossRef ] [ Google Scholar ]
- Carbonell X., Guardiola E., Fuster H., Gil F., Panova T. (2016). Trends in scientific literature on addiction to the Internet, video games, and cell phones from 2006 to 2010 . International Journal of Preventive Medicine, 7 ( 1 ), 63. doi: 10.4103/2008-7802.179511 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carbonell X., Panova T. (2017). A critical consideration of social networking sites’ addiction potential . Addiction Research & Theory, 25 ( 1 ), 48–57. doi: 10.1080/16066359.2016.1197915 [ CrossRef ] [ Google Scholar ]
- Cheever N., Rosen L., Carrier L. M., Chavez A. (2014). Out of sight is not out of mind: The impact of restricting wireless mobile device use on anxiety levels among low, moderate and high users . Computers in Human Behavior, 37, 290–297. doi: 10.1016/j.chb.2014.05.002 [ CrossRef ] [ Google Scholar ]
- Chiu S.-I. (2014). The relationship between life stress and smartphone addiction on Taiwanese university student: A mediation model of learning self-efficacy and social self-efficacy . Computers in Human Behavior, 34, 49–57. doi: 10.1016/j.chb.2014.01.024 [ CrossRef ] [ Google Scholar ]
- Chóliz M. (2010). Mobile phone addiction: A point of issue . Addiction, 105 ( 2 ), 373–374. doi: 10.1111/j.1360-0443.2009.02854.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Darcin A. E., Kose S., Noyan C. O., Nurmedov S., Yılmaz O., Dilbaz N. (2016). Smartphone addiction and its relationship with social anxiety and loneliness . Behaviour and Information Technology, 35 ( 7 ), 520–525. doi: 10.1080/0144929X.2016.1158319 [ CrossRef ] [ Google Scholar ]
- Demirci K., Akgönül M., Akpinar A. (2015). Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students . Journal of Behavioral Addictions, 4 ( 2 ), 85–92. doi: 10.1556/2006.4.2015.010 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elhai J. D., Levine J. C., Dvorak R. D., Hall B. J. (2016). Fear of missing out, need for touch, anxiety and depression are related to problematic smartphone use . Computers in Human Behavior, 63, 509–516. doi: 10.1016/j.chb.2016.05.079 [ CrossRef ] [ Google Scholar ]
- Fernandez-Guerrero I. M. (2014). WhatsAppitis . The Lancet, 383 ( 9922 ), 1040. doi: 10.1016/S0140-6736(14)60519-5 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frances A. J., Widiger T. (2012). Psychiatric diagnosis: Lessons from the DSM-IV past and cautions for the DSM-5 future . Annual Review of Clinical Psychology, 8 ( 1 ), 109–130. doi: 10.1146/annurev-clinpsy-032511-143102 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fu Yuan H., Chiu S.-I., Huang D.-H. (2012). A model of the relationship between psychological characteristics, mobile phone addiction and use of mobile phones by Taiwanese university female students . Computers in Human Behavior, 28 ( 6 ), 2152–2159. doi: 10.1016/j.chb.2012.06.020 [ CrossRef ] [ Google Scholar ]
- Goodman M. D. (1990). Addiction: Definition and implications . British Journal of Addictions, 85 ( 11 ), 1403–1408. doi: 10.1111/j.1360-0443.1990.tb01620.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Griffiths M. D. (1995). Technological addictions . Clinical Psychology Forum, 76, 14–19. [ Google Scholar ]
- Griffiths M. D. (2005). A “components” model of addiction within a biopsychosocial framework . Journal of Substance Use, 10 ( 4 ), 191–197. doi: 10.1080/14659890500114359 [ CrossRef ] [ Google Scholar ]
- Haug S., Castro R. P., Kwon M., Filler A., Kowatsch T., Schaub M. P. (2015). Smartphone use and smartphone addiction among young people in Switzerland . Journal of Behavioral Addictions, 4 ( 4 ), 299–307. doi: 10.1556/2006.4.2015.037 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hawi N. S., Samaha M. (2016). To excel or not to excel: Strong evidence on the adverse effect of smartphone addiction on academic performance . Computers & Education, 98, 81–89. doi: 10.1016/j.compedu.2016.03.007 [ CrossRef ] [ Google Scholar ]
- Horst H., Miller D. (2005). From kinship to link-up: Cell phones and social networking in Jamaica . Current Anthropology, 46 ( 5 ), 755–778. doi: 10.1086/432650 [ CrossRef ] [ Google Scholar ]
- Ito M. (2005). Mobile phones, Japanese youth, and the re-placement of social contact . In Ling R., Pedersen P. (Eds.), Mobile communications: Re-negotiation of the social sphere (pp. 131–148). London: Springer. [ Google Scholar ]
- Jeong S. H., Kim H., Yum J. Y., Hwang Y. (2016). What type of content are smartphone users addicted to?: SNS vs. games . Computers in Human Behavior, 54, 10–17. doi: 10.1016/j.chb.2015.07.035 [ CrossRef ] [ Google Scholar ]
- Kaptsis D., King D. L., Delfabbro P. H., Gradisar M. (2016). Withdrawal symptoms in Internet gaming disorder: A systematic review . Clinical Psychology Review, 43, 58–66. doi: 10.1016/j.cpr.2015.11.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kardefelt-Winther D. (2015). Commentary on: Are we overpathologizing everyday life? A tenable blueprint for behavioral addiction research. Problems with atheorical and confirmatory reserach approaches in the study of behavioral addictions . Journal of Behavioral Addictions, 4 ( 3 ), 126–129. doi: 10.1556/2006.4.2015.019 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kardefelt-Winther D., Heeren A., Schimmenti A., van Rooij A., Maurage P., Carras M., Edman J., Blaszczynski A., Khazaal Y., Billieux J. (2017). How can we conceptualize behavioural addiction without pathologizing common behaviours? Addiction, 112 ( 10 ), 1709–1715. doi: 10.1111/add.13763 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kim D., Lee Y., Lee J., Nam J. K., Chung Y. (2014). Development of Korean Smartphone Addiction Proneness Scale for youth . PLoS One, 9 ( 5 ), e97920. doi: 10.1371/journal.pone.0097920 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- King A. L., Valença A. M., Silva A. C., Baczynski T., Carvalho M. R., Nardi A. E. (2013). Nomophobia: Dependency on virtual environments or social phobia? Computers in Human Behavior, 29 ( 1 ), 140–144. doi: 10.1016/j.chb.2012.07.025 [ CrossRef ] [ Google Scholar ]
- King D. L., Herd M. C. E., Delfabbro P. H. (2018). Motivational components of tolerance in Internet gaming disorder . Computers in Human Behavior, 78, 133–141. doi: 10.1016/j.chb.2017.09.023 [ CrossRef ] [ Google Scholar ]
- Király O., Griffiths M. D., Urbán R., Farkas J., Kökönyei G., Elekes Z., Tamás D., Demetrovics Z. (2014). Problematic Internet use and problematic online gaming are not the same: Findings from a large nationally representative adolescent sample . Cyberpsychology, Behavior and Social Networking, 17 ( 12 ), 749–754. doi: 10.1089/cyber.2014.0475 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Körmendi A., Brutóczki Z., Végh B. P., Székely R. (2016). Smartphone use can be addictive? A case report . Journal of Behavioral Addictions, 5 ( 3 ), 548–552. doi: 10.1556/2006.5.2016.033 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kuss D., Harkin L., Kanjo E., Billieux J. (2018). Problematic smartphone use: Investigating contemporary experiences using a convergent design . International Journal of Environmental Research and Public Health, 15 ( 1 ), 142. doi: 10.3390/ijerph15010142 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kuss D. J., Kanjo E., Crook-Rumsey M., Kibowski F., Wang G. Y., Sumich A. (2018). Problematic mobile phone use and addiction across generations: The roles of psychopathological symptoms and smartphone use . Journal of Technology in Behavioral Science . doi: 10.1007/s41347-017-0041-3 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kwon M., Lee J. Y., Won W. Y., Park J. W., Min J. A., Hahn C., Gu X., Choi J.-H., Kim D. J. (2013). Development and validation of a Smartphone Addiction Scale (SAS) . PLoS One, 8 ( 2 ), e56936. doi: 10.1371/journal.pone.0056936 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leonardi P., Leonardi M. E., Hudson E. (2006). Culture, organization, and contradiction in the social construction of technology: Adoption and use of the cell phone across three cultures . In Kavoori A., Arceneaux N. (Eds.), The cell phone reader: Essays in social transformation (pp. 205–225). New York, NY: Peter Lang. [ Google Scholar ]
- Leung L. (2007). Leisure boredom, sensation seeking, self-esteem, addiction symptoms and patterns of mobile phone use . In Konijn E. A., Utz S., Tanis M., Barnes S. B. (Eds.), Mediated Interpersonal Communication (pp. 359–381). New York: Routledge. [ Google Scholar ]
- Levine D. G. (1974). “Needle Freaks”: Compulsive self-injection drug users . The American Journal of Psychiatry, 131 ( 3 ), 297–300. doi: 10.1176/ajp.131.3.297 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lin Y. H., Chang L. R., Lee Y. H., Tseng H. W., Kuo T. B. J., Chen S. H. (2014). Development and validation of the Smartphone Addiction Inventory (SPAI) . PLoS One, 9 ( 6 ), e98312. doi: 10.1371/journal.pone.0098312 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lopez-Fernandez O. (2015). Short version of the Smartphone Addiction Scale adapted to Spanish and French: Towards a cross-cultural research in problematic mobile phone use . Addictive Behaviors, 64, 275–280. doi: 10.1016/j.addbeh.2015.11.013 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lopez-Fernandez O., Kuss D., Romo L., Morvan Y., Kern L., Graziani P., Rousseau A., Rumpf H. J., Bischof A., Gässler A. K., Schimmenti A., Passanisi A., Männikkö N., Kääriänen M., Demetrovics Z., Király O., Chóliz M., Zacarés J. J., Serra E., Griffiths M. D., Pontes H. M., Lelonek-Kuleta B., Chwaszcz J., Zullino D., Rochat L., Achab S., Billieux J. (2017). Self-reported dependence on mobile phones in young adults: A European cross-cultural empirical survey . Journal of Behavioral Addictions, 6 ( 2 ), 168–177. doi: 10.1556/2006.6.2017.020 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lopez-Fernandez O., Männikkö N., Kääriäinen M., Griffiths M. D., Kuss D. J. (2018). Mobile gaming and problematic smartphone use: A comparative study between Belgium and Finland . Journal of Behavioral Addictions, 7 ( 1 ), 88–99. doi: 10.1556/2006.6.2017.080 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Marlatt G. A., Gordon J. R. (1985). Relapse prevention . New York, NY: Guilford. [ Google Scholar ]
- Muñoz-Miralles R., Ortega-González R., Batalla-Martínez C., López-Morón M. R., Manresa J. M., Torán-Monserrat P. (2013). Acceso y uso de nuevas tecnologías entre los jóvenes de educación secundaria, implicaciones en salud. Estudio JOITIC [Access and use of new information and telecommunication technologies among teenagers at high school, health implications. JOITIC Study]. Atencion Primaria, 46 ( 2 ), 77–88. doi: 10.1016/j.aprim.2013.06.001 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Murdock K. K. (2013). Texting while stressed: Implications for students’ burnout, sleep, and well-being . Psychology of Popular Media Culture, 2 ( 4 ), 207–221. doi: 10.1037/ppm0000012 [ CrossRef ] [ Google Scholar ]
- Nolan B. V., Feldman S. R. (2009). Ultraviolet tanning addiction . Dermatologic Clinics, 27 ( 2 ), 109–112. doi: 10.1016/j.det.2008.11.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Panova T., Lleras A. (2016). Avoidance or boredom: Negative mental health outcomes associated with use of information and communication technologies depend on users’ motivations . Computers in Human Behavior, 58, 249–258. doi: 10.1016/j.chb.2015.12.062 [ CrossRef ] [ Google Scholar ]
- Pedrero E. J., Rodríguez M. T., Ruiz J. M. (2012). Adicción o abuso del teléfono móvil. Revisión de la literatura [Mobile phone abuse or addiction. A review of the literature]. Adicciones, 24 ( 2 ), 139–152. doi: 10.20882/adicciones.107 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Petry N. M., O’Brien C. P. (2013). Internet gaming disorder and the DSM-5 . Addiction, 108 ( 7 ), 1186–1187. doi: 10.1111/add.12162 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pontes H. M., Szabo A., Griffiths M. D. (2015). The impact of Internet-based specific activities on the perceptions of Internet addiction, quality of life, and excessive usage: A cross-sectional study . Addictive Behaviors Reports, 1, 19–25. doi: 10.1016/j.abrep.2015.03.002 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roberts J. A., Pullig C., Manolis C. (2015). I need my smartphone: A hierarchical model of personality and cell-phone addiction . Personality and Individual Differences, 79, 13–19. doi: 10.1016/j.paid.2015.01.049 [ CrossRef ] [ Google Scholar ]
- Rudski J. M., Segal C., Kallen E. (2009). Harry Potter and the end of the road: Parallels with addiction . Addiction Research & Theory, 17 ( 3 ), 260–277. doi: 10.1080/16066350802334595 [ CrossRef ] [ Google Scholar ]
- Salehan M., Negahban A. (2013). Social networking on smartphones: When mobile phones become addictive . Computers in Human Behavior, 29 ( 6 ), 2632–2639. doi: 10.1016/j.chb.2013.07.003 [ CrossRef ] [ Google Scholar ]
- Sánchez-Carbonell X., Guardiola E., Bellés A., Beranuy M. (2005). European Union scientific production on alcohol and drug misuse (1976–2000) . Addiction, 100 ( 8 ), 1166–1174. doi: 10.1111/j.1360-0443.2005.01135.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sánchez-Carbonell X., Beranuy M., Castellana M., Chamarro A., Oberst U. (2008). La adiccion a Internet y al móvil: ¿Moda o trastorno? [Internet and mobile phone addiction: A passing fad or a disorder?]. Adicciones, 20 ( 2 ), 149–160. doi: 10.20882/adicciones.279 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Saunders J. B., Hao W., Long J., King D. L., Mann K., Fauth-Bühler M., Rumpf H. J., Bowden-Jones H., Rahimi-Movaghar A., Chung T., Chan E., Bahar N., Achab S., Lee H. K., Potenza M., Petry N., Spritzer D., Ambekar A., Derevensky J., Griffiths M. D., Pontes H. M., Kuss D., Higuchi S., Mihara S., Assangangkornchai S., Sharma M., Kashef A. E., Ip P., Farrell M., Scafato E., Carragher N., Poznyak V. (2017). Gaming disorder: Its delineation as an important condition for diagnosis, management, and prevention . Journal of Behavioral Addictions, 6 ( 3 ), 271–279. doi: 10.1556/2006.6.2017.039 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Skierkowski D., Wood R. M. (2012). To text or not to text? The importance of text messaging among college-aged youth . Computers in Human Behavior, 28 ( 2 ), 744–756. doi: 10.1016/j.chb.2011.11.023 [ CrossRef ] [ Google Scholar ]
- Stall R., Biernacki P. (1986). Spontaneous remission from the problematic use of substances: An inductive model derived from a comparative analysis of the alcohol, opiate, tobacco, and food/obesity literatures . International Journal of the Addictions, 21 ( 1 ), 1–23. doi: 10.3109/10826088609063434 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Suissa A. J. (2008). Addiction to cosmetic surgery: Representations and medicalization of the body . International Journal of Mental Health and Addiction, 6 ( 4 ), 619–630. doi: 10.1007/s11469-008-9164-2 [ CrossRef ] [ Google Scholar ]
- Surrat C. G. (1999). Netaholics?: The creation of a pathology . New York, NY: Nova Science. [ Google Scholar ]
- Targhetta R., Nalpas B., Perney P. (2013). Argentine tango: Another behavioral addiction? Journal of Behavioral Addictions, 2 ( 3 ), 179–186. doi: 10.1556/JBA.2.2013.007 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thomée S., Dellve L., Harenstam A., Hagberg M. (2010). Perceived connections between information and communication technology use and mental symptoms among young adults – A qualitative study . BMC Public Health, 10 ( 1 ), 66. doi: 10.1186/1471-2458-10-66 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thomée S., Härenstam A., Hagberg M. (2011). Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults – A prospective cohort study . BMC Public Health, 11 ( 1 ), 66. doi: 10.1186/1471-2458-11-66 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Van Deursen A. J. A. M., Bolle C. L., Hegner S. M., Kommers P. A. M. (2015). Modeling habitual and addictive smartphone behavior. The role of smartphone usage types, emotional intelligence, social stress, self-regulation, age, and gender . Computers in Human Behavior, 45, 411–420. doi: 10.1016/j.chb.2014.12.039 [ CrossRef ] [ Google Scholar ]
- Walters G. D. (2000). Spontaneous remission from alcohol, tobacco, and other drug abuse: Seeking quantitative answers to qualitative questions . The American Journal of Drug and Alcohol Abuse, 26 ( 3 ), 443–460. doi: 10.1081/ADA-100100255 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cell Phone Addiction: The Statistics…
Cell Phone Addiction: The Statistics of Gadget Dependency

The prevalence of smartphones is nothing short of a phenomenon. Apple debuted the iPhone more than 10 years ago, and its introduction to the world created a consumer need that previously didn’t exist.
Now that 56 percent of Americans own smartphones , we use our mobile gadgets to work, play, share, learn, communicate, and stave off boredom. However, the increase in reliance on technology has a downside: People are relying more and more on their smartphones äóî sometimes to an unhealthy degree. “Technological addiction can happen to anyone,” digital detox expert Holland Haiis told CNN . She also described technology as “the new 21 st century addiction.”
Tech dependency is a modern issue that is growing in relevance as more and more people utilize mobile technology. Dr. Russell Belk’s Extended Self Theory suggests that our possessions, such as smartphones, have become integral to how humans operate on a daily basis. They became an extension of the self, so that separation from devices can cause anxiety, irritability, and even psychological symptoms similar to substance addiction for some. What are the facts behind tech dependency, and who does it affect?
People Touch Their Phones an Average of 2,617 Times Per Day
According to recent research from dscout, people tap, swipe, and click an average of 2,617 times per day . For the top 10 percent of users, this number doubled to 5,427 touches per day. That’s about 1 million touches per year and 2.42 hours of phone screen time per day. More serious users interacted with their phones even more, at 3.75 hours per day. This data includes all types of interactions, from reading and sending texts to scrolling on social media. How much time we spend on our phones each day is indicative of the important role these devices play in our lives.
iPhone Owners Unlock Their Phones 80 Times Per Day
iPhone users unlock their phones an average of 80 times per day , while a study of Android users found that they unlock their phones 110 times per day, according to Business Insider . This means that, in an average day of usage, iPhone users check their phones six to seven times per hour, or once every 10 minutes. Frequent usage can have a negative effect on communication with others during social engagements and is often seen as disruptive. In some cases, it might be said that we have become more concerned with digital interaction than with the social interactions that happen face to face.
Americans Spend an Average of 5 Hours Per Day Browsing
The time we spend on our mobile devices continues to increase. In fact, according to data by Flurry Mobile, “the average U.S. consumer spends a whopping 5 hours a day on these devices. That is a 20% increase in time-spent compared to Q4 2015.” This kind of abundant usage is fueling greater demand for trained IT and other tech professionals.
Interested in a Career in Technology?
Pursue your career in technology and cybersecurity today with King University. With year-round courses, a generous credit transfer policy, accelerated programs, and affordable tuition, you can discover how King can help you achieve your goals.
50 Percent of Young People Admit Cell Phone Addiction
A recent poll on mobile device usage from Common Sense Media found that 50 percent of teens said they “feel addicted” to their mobile devices. At 59 percent, even more parents thought their teens were addicted, CNN says. The survey asked more than 1,200 parents and teenagers about mobile device usage and family conflict.
According to Fortune , “Social media may be particularly entrancing , with notifications from apps like Facebook and Twitter providing jolts of pleasure in some ways similar to the effects of drugs and gambling.” Because today’s young people are digital natives, this level of use indicates that mobile technology will remain a staple in our society.
Signs and Symptoms of Cell Phone Addiction
The following are some of the signs and symptoms of cell phone addiction, according to Entrepreneur .
- Reaching for the phone first thing in the morning: When something becomes a vital part of your daily routine, it can affect thinking and emotions. As Entrepreneur notes, 68 percent of adults sleep with their phones near the bed.
- Using cell phones when bored: Many people experience feelings of excitement or euphoria before or after using their smartphone. This creates a highly addictive response, causing them to want to repeat the action over and over, the same article explains.
- Increasing cell phone use: “Tolerance is the need to receive an ever-increasing dose to reach the desired high, and is similar to alcohol abuse. And with the increasing number of new uses for the cell phone, and the proliferation of available downloads, it is easy to access the next exciting new thing,” Entrepreneur notes.
- Becoming anxious or agitated when the cell phone is out of sight: Symptoms like stress, irritability, and panic that occur when individuals can’t find their phone or are separated from it indicate that they have formed a dependency. Entrepreneur cites research that notes “Sixty-eight percent of all adults have an irrational fear of losing their phone.”
- People complain about cell phone use: If loved ones frequently mention that individuals are always on their phone and that it bothers them, it is likely time to cut back. Smartphone use could be negatively impacting social life or family time.
- Inability to cut back on cell phone use: “Relapse occurs when you set every intention to cut back on your phone use, but find yourself reaching for it with a force that seems beyond your control,” Entrepreneur explains.
Other signs of tech dependency include using a device to bypass negative feelings or forget a troubling event, losing track of time while on the device, and physical repercussions such as eye strain, neck pain, and more. It is important to note that, while internet addiction is viewed as a public health issue in other places, “it is not yet a recognized disorder in the United States,” according to CNN.
Online Education at King University
For better or worse, mobile technology is here to stay. The widespread (and growing) use of smartphones and other mobile devices is driving serious growth in the information technology industry, which is ideal for those interested in this career path. According to the Bureau of Labor Statistics, employment of computer and information technology occupations is expected to grow 12 percent through 2024, with almost 500,000 new jobs being added to the workforce.
King University’s online bachelor’s degree in information technology is designed for professionals who are ready to excel in technology-based careers. Through specialized coursework in relevant fields like cybersecurity, graduates are ready to face the challenges of the modern workplace.
For those more interested in the psychological motivations behind technology use , King University offers an online bachelor’s in psychology . King’s online psychology degree is designed to prepare students with the skills they need for many mental health and social services careers. This program teaches students key competencies in psychology, communication, research, and critical thinking. Students develop their knowledge of psychological behavior.
Undergraduate coursework for both these programs may be completed in as little as 16 months. Learn more about King University’s online program options today and discover how King can help you enhance your knowledge and qualify for the job you want.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Radiation
- Food Irradiation
- Radiation Safety
- Radiation in Your Life
- Radiation and Your Health Features
- Dose Reconstruction
Facts About Cell Phones and Your Health
At a glance.
Most of us depend on cell phones every day. Some people wonder if cell phones can cause health problems. Here’s what you should know about cell phones and your health.

Common Questions
Can using a cell phone cause cancer.
There is no scientific evidence that provides a definite answer to the question. Some organizations recommend caution in cell phone use. More research is needed before we know if using cell phones causes health effects.
Do cell phones give off (emit) radiation?
Yes – cell phones and cordless phones use radiofrequency (RF) radiation to send signals. RF radiation is different from other types of radiation (like x-rays) that we know can be harmful. We don’t know for sure if RF radiation from cell phones can cause health problems years later. The International Agency for Research on Cancer (IARC) has classified RF radiation as a “possible human carcinogen.” (A carcinogen is an agent that causes cancer.)
Should people stop using cell phones?
At this time we do not have the science to link health problems to cell phone use. Scientific studies are under way to determine whether cell phone use may cause health effects. It is also important to consider the benefits of cell phones. Their use can be valuable in an urgent or emergency situation – and even save lives.
If you are worried about cell phone use, follow the tips below.
What research is being done to learn more about cell phones and health?
Scientists are continuing to study the possible health effects of cell phone use. For example, the World Health Organization (WHO) is currently looking into how cell phones may affect:
- Some types of tumors (a lump or growth)
In the News
Cell phone tips.
To reduce radiofrequency (RF) radiation near your body:
- Get a hands-free headset that connects directly to your phone.
- Use speaker-phone more often.
In the past, RF radiation interfered with the operation of some pacemakers. If you have a pacemaker and are concerned about how your cell phone use may affect it, contact your healthcare provider.
For more information, visit
- The Federal Communications Commission
- World Health Organization
- The Food and Drug Administration
Radiation and Your Health
Information about what radiation is and the many sources of radiation in our lives.
Watch CBS News
Older Americans are suffering from cellphone addiction just as much as teens, research found
No TikTok? No problem. Here's why you shouldn't rush to buy your child a phone.
With so many kids online so much of the time, our children are more exposed than ever to dangers they're not ready to guard themselves against..

The longer I am a mother , the more I find myself reflecting on my childhood and how it compares and contrasts with my daughters' lives.
So much is the same: picky eaters, feet that grow out of new shoes too fast, tears spilled over math homework and talks about who said what to whom on the playground.
But there is one thing that makes everything about being a kid so different today: cellphones .
Phones have changed how kids interact
When I was in third grade, about 1992, my small, private school in Denver had one big hulk of a computer that we wheeled around the whole building for each classroom to use.
Today, kids as young as 8 (or less) have social media accounts on their own smartphones, where they spend hours every day living entire lives in a 4x7 inch screen. Incessantly scrolling, chatting and comparing.
I get why parents want their kids to have phones: mainly to stay in touch. I also get that screen time for kids and teens means free time for us. When we are constantly being emailed and texted, when the demands to do so many things professionally and for our kids are at an all-time high, when we want a minute to scroll mindlessly as we descend down the rabbit hole that is Pinterest (or pick your poison), cellphones and tablets provide momentary respite from our overbooked days.
And there's nothing new about warning of the dangers of cellphones for kids (or for us). But phones are so ubiquitous that we read the bad news about the latest study, feel guilty and quickly move on.
I want to remind you why we should be thinking, and talking, about our kids' cellphone use.
Phones are everywhere: 95% of teens say they have access to a cellphone, and 58% of teens report using TikTok daily, according to a 2023 Pew Research Center survey .
With that many kids online, that much of the time, our children are more exposed than ever to dangers they're not ready to guard themselves against: stolen identities, pornography, pedophilia, the list goes on.
More from Carli Pierson on parenting: My 8-year-old daughter got her first sleepover invite. There's no way she's going.
There's also the issue of how phones and social media make kids feel about themselves. In " The Conquest of Happiness ," Bertrand Russell wrote: "The habit of thinking in terms of comparison is a fatal one."
But that's what social media is – one big social comparison. Who has a better body? Who has more money? Who has a more interesting life? More friends? More likes?
For teens and preteens with all the additional difficulties that accompany those years, that sounds like a heavy burden. And it is: Teen suicide rates are rising , and while social media isn't the only factor, in some cases we know it's a contributor .
Should kids be allowed to have phones?
I have other questions that the research doesn't answer.
What is smartphone use doing to kids' ability to be creative? How will that affect their capacity to deal with the parade of letdowns and monotony that is such a integral part of human existence? When our children grow up, will they be able to handle not being entertained? Will they be able to carry a conversation?
Harvey Weinstein case and #MeToo: Why was his conviction for sexual crimes overturned? Sometimes the courts get things wrong.
Phones and kids should be an ongoing conversation in our homes. We should be talking about the dangers of addiction. We need to teach them that obsessing over other people's lives, or comparing themselves with another person they may or may not know, isn't healthy or helpful. We want to show them that being able to strike up, hold and gracefully walk away from a conversation is an art that needs practice. And they need to understand that being bored is OK.
Now, I am not a masochist – my kids have tablets that they watch movies and play games on. I am not saying kids should never have a phone or a tablet.
But kids and parents need to do more handholding and hugging, more talking and discussing, more daydreaming. We need to get back to resting in the grass and experiencing that peaceful feeling of watching the clouds float by. And we need fewer handheld objects to distract and entertain us.
Life is short, childhood is even shorter. Let's work harder to save our kids from a childhood spent inside a phone.
Carli Pierson is a digital editor at USA TODAY and a New York-licensed attorney.

Is Your Child Struggling With Mobile Addiction? 5 Ways To Help Them
C hildren, in today’s time, are getting addicted to mobile phones more than ever. From children to adults, everyone is seen spending too much time on electronic gadgets including smartphones, tablets and laptops. This excessive use is not only deteriorating their physical health, but is also taking a toll on their mental well-being. This is the reason incidents like children committing suicide are coming to the forefront. A recent case is from Ambikapur in Chhattisgarh. In the state, a 15-year-old minor consumed a poisonous substance after not receiving the money for a mobile phone. He was then rushed to the medical college. Psychiatrist of Government Medical College, Dr Vivek Kumar, has recently talked about how mobile addiction can be disruptive to a child’s health. He has shared certain methods how parents can help their child get rid of mobile addiction.
Set Time Limit:
The first and foremost thing is to reduce the number of hours your child spends on mobile phones. As a parent, it is your responsibility to keep track of your child’s daily activities. Plan a proper routine and include some time when a child can use mobile phones. This habit will help your child to lead a healthy life.
Healthy Diet:
It is quintessential to follow a healthy diet plan for the well-being of your child. Motivate them to play outdoor games with their friends despite spending time playing mobile games. Introduce your children to some new outdoor games that they can play along with their pals.
Healthy Sleep Cycle:
Using your phone before sleeping should be avoided at any cost. If your child has a habit of scrolling social media posts just before his bedtime. Stop and educate him about its consequences. Experts suggest phones should be kept aside at least 2 hours before sleeping.
Become Their Friends:
Every parent wants their children to share their sorrows and secrets with them openly. While donning the hat of being a good parent, many forget to understand their children from their viewpoint. If you want your kid to nurture a healthy lifestyle, then you must become his/her friend first. This will not only strengthen your relationship with the child, but will also keep a tab on their mental health.
Educate children on the harmful effects of excess screen time:
Before asking your child to cut down their screen time, take a few minutes to underscore the side effects of too much screen time. Setting new rules without highlighting the reasons will only make the situation worse. Explain the negative effects of using mobile phones beforehand in a language that they will understand.


Binge drinking is a growing public health crisis − a neurobiologist explains how research on alcohol use disorder has shifted
Assistant Professor of Biology, Biomedical Engineering and Pharmacology, Penn State
Disclosure statement
Nikki Crowley receives funding from The National Institutes of Health, The Brain and Behavior Research Foundation, and the Penn State Huck Institutes of the Life Sciences endowment funds.
Penn State provides funding as a founding partner of The Conversation US.
View all partners
With the new Amy Winehouse biopic “Back to Black ” in U.S. theaters as of May 17, 2024, the late singer’s relationship with alcohol and drugs is under scrutiny again. In July 2011, Winehouse was found dead in her flat in north London from “death by misadventure” at the age of 27. That’s the official British term used for accidental death caused by a voluntary risk.
Her blood alcohol concentration was 0.416%, more than five times the legal intoxication limit in the U.S. – leading her cause of death to be later adjusted to include “alcohol toxicity” following a second coroner’s inquest.
Nearly 13 years later, alcohol consumption and binge drinking remain a major public health crisis , not just in the U.K. but also in the U.S.
Roughly 1 in 5 U.S. adults report binge drinking at least once a week, with an average of seven drinks per binge episode . This is well over the amount of alcohol thought to produce legal intoxication, commonly defined as a blood alcohol concentration over 0.08% – on average, four drinks in two hours for women, five drinks in two hours for men.
Among women, days of “heavy drinking” increased 41% during the COVID-19 pandemic compared with pre-pandemic levels , and adult women in their 30s and 40s are rapidly increasing their rates of binge drinking , with no evidence of these trends slowing down. Despite efforts to comprehend the overall biology of substance use disorders, scientists’ and physicians’ understanding of the relationship between women’s health and binge drinking has lagged behind.
I am a neurobiologist focused on understanding the chemicals and brain regions that underlie addiction to alcohol . I study how neuropeptides – unique signaling molecules in the prefrontal cortex , one of the key brain regions in decision-making, risk-taking and reward – are altered by repeated exposure to binge alcohol consumption in animal models.
My lab focuses on understanding how things like alcohol alter these brain systems before diagnosable addiction, so that we can better inform efforts toward both prevention and treatment.
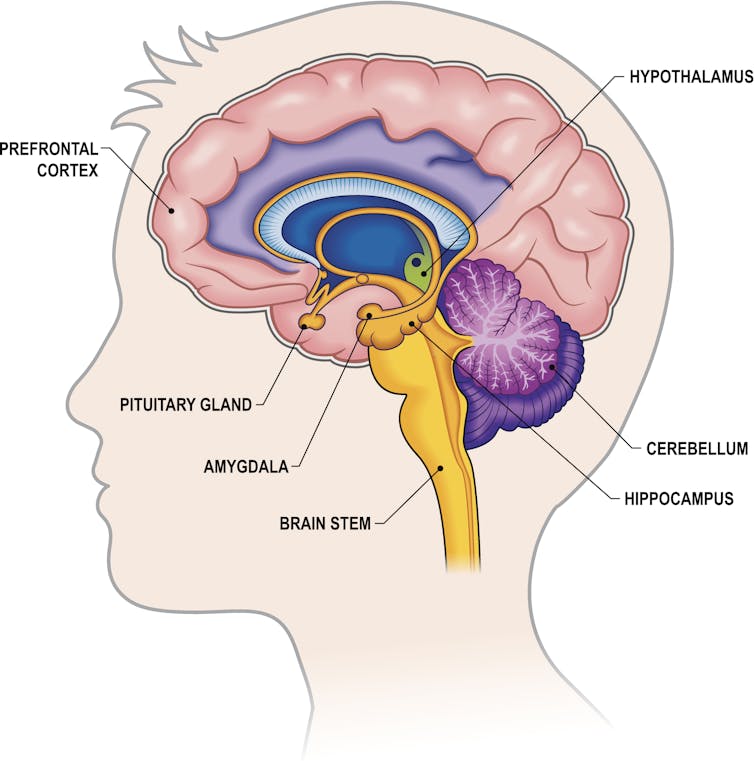
The biology of addiction
While problematic alcohol consumption has likely occurred as long as alcohol has existed, it wasn’t until 2011 that the American Society of Addiction Medicine recognized substance addiction as a brain disorder – the same year as Winehouse’s death. A diagnosis of an alcohol use disorder is now used over outdated terms such as labeling an individual as an alcoholic or having alcoholism.
Researchers and clinicians have made great strides in understanding how and why drugs – including alcohol, a drug – alter the brain. Often, people consume a drug like alcohol because of the rewarding and positive feelings it creates, such as enjoying drinks with friends or celebrating a milestone with a loved one. But what starts off as manageable consumption of alcohol can quickly devolve into cycles of excessive alcohol consumption followed by drug withdrawal.
While all forms of alcohol consumption come with health risks, binge drinking appears to be particularly dangerous due to how repeated cycling between a high state and a withdrawal state affect the brain. For example, for some people, alcohol use can lead to “ hangxiety ,” the feeling of anxiety that can accompany a hangover.
Repeated episodes of drinking and drunkenness, coupled with withdrawal, can spiral, leading to relapse and reuse of alcohol. In other words, alcohol use shifts from being rewarding to just trying to prevent feeling bad.
It makes sense. With repeated alcohol use over time, the areas of the brain engaged by alcohol can shift away from those traditionally associated with drug use and reward or pleasure to brain regions more typically engaged during stress and anxiety .
All of these stages of drinking, from the enjoyment of alcohol to withdrawal to the cycles of craving, continuously alter the brain and its communication pathways . Alcohol can affect several dozen neurotransmitters and receptors , making understanding its mechanism of action in the brain complicated.
Work in my lab focuses on understanding how alcohol consumption changes the way neurons within the prefrontal cortex communicate with each other. Neurons are the brain’s key communicator, sending both electrical and chemical signals within the brain and to the rest of your body.
What we’ve found in animal models of binge drinking is that certain subtypes of neurons lose the ability to talk to each other appropriately. In some cases, binge drinking can permanently remodel the brain. Even after a prolonged period of abstinence, conversations between the neurons don’t return to normal .
These changes in the brain can appear even before there are noticeable changes in behavior . This could mean that the neurobiological underpinnings of addiction may take root well before an individual or their loved ones suspect a problem with alcohol.
Researchers like us don’t yet fully understand why some people may be more susceptible to this shift, but it likely has to do with genetic and biological factors, as well as the patterns and circumstances under which alcohol is consumed.
Women are forgotten
While researchers are increasingly understanding the medley of biological factors that underlie addiction, there’s one population that’s been largely overlooked until now: women.
Women may be more likely than men to have some of the most catastrophic health effects caused by alcohol use, such as liver issues, cardiovascular disease and cancer . Middle-aged women are now at the highest risk for binge drinking compared with other populations.
When women consume even moderate levels of alcohol, their risk for various cancers goes up, including digestive, breast and pancreatic cancer , among other health problems – and even death. So the worsening rates of alcohol use disorder in women prompt the need for a greater focus on women in the research and the search for treatments.
Yet, women have long been underrepresented in biomedical research.
It wasn’t until 1993 that clinical research funded by the National Institutes of Health was required to include women as research subjects. In fact, the NIH did not even require sex as a biological variable to be considered by federally funded researchers until 2016. When women are excluded from biomedical research, it leaves doctors and researchers with an incomplete understanding of health and disease, including alcohol addiction.
There is also increasing evidence that addictive substances can interact with cycling sex hormones such as estrogen and progesterone . For instance, research has shown that when estrogen levels are high, like before ovulation, alcohol might feel more rewarding , which could drive higher levels of binge drinking. Currently, researchers don’t know the full extent of the interaction between these natural biological rhythms or other unique biological factors involved in women’s health and propensity for alcohol addiction.

Looking ahead
Researchers and lawmakers are recognizing the vital need for increased research on women’s health. Major federal investments into women’s health research are a vital step toward developing better prevention and treatment options for women.
While women like Amy Winehouse may have been forced to struggle both privately and publicly with substance use disorders and alcohol, the increasing focus of research on addiction to alcohol and other substances as a brain disorder will open new treatment avenues for those suffering from the consequences.
For more information on alcohol use disorder, causes, prevention and treatments, visit the National Institute on Alcohol Abuse and Alcoholism .
- Amy Winehouse
- Binge drinking
- Neurobiology
- Intoxication
- Alcohol consumption
- Alcohol use
- Alcohol use disorder
- COVID-19 pandemic

Senior Research Fellow - Women's Health Services

Senior Lecturer in Periodontics

Lecturer / Senior Lecturer - Marketing

Assistant Editor - 1 year cadetship

Executive Dean, Faculty of Health
Millennials are furious that Gen Z have ‘killed’ the art of clubbing
A teenage “rite of passage” is disappearing, experts are warning – and Millennials are furious it is being “forgotten”.

Matildas star honoured in perfect way

‘Shocking’: Huge payday blow for viral gamer

Mum killed by 13 dogs in vicious attack
Gen Z’s addiction to their phones is killing the art of clubbing, with experts stating modern tech is destroying the beloved Millennial “rite of passage”.
The number of Australian nightclubs reduced from 482 to 355 in recent years, according to IBISWorld .
While the pandemic contributed in the decline of nightclub popularity, research shows there are a multitude of factors at play, including a slump in alcohol consumption among younger demographics and soaring cost of living pressures.
But industry experts state phones are one of the biggest reasons clubbing has completely changed.
“Clubbing is a much different beast these days, it was more wild back in the days, these days not so much,” Ben Nott, a professional DJ who is about to open Sydney’s newest restaurant meets club lounge, told news.com.au.
“Phones are a real hindrance as Gen Z like to record a lot, but you can’t watch a show through a screen all night.
“Younger clubbers, and people in general thesedays, tend to have a much shorter attention span, which also makes it harder for people putting on club nights.”
Millennials, who couldn’t wait to come of age at 18 to dance the night away in a sweaty room with complete strangers, have also declared the cult-weekend activity is “dying”.
Christina Najjar, a popular influencer known as Tinx, recently shared her “concerns” on the topic on the Trash Tuesday Podcast – prompting hordes of fellow 30-somethings to weigh in on the debate.
“I am very concerned about the future of my culture which is clubbing,” she said in a clip , posted on TikTok .
“I’m gonna write some letters to authorities soon.
“This is a dying art, they’re [Gen Z] are forgetting this craft, and how to do it.
“The young girls don’t even know how to dance on a table in a heel.”

Dane Gorrel, director at Sydney’s Club 77 , weighed in on this, noting it’s not just night-life that phones have changed forever.
“I think phones and social media in general are killing a lot of experiences, not just in nightclubs,” he told news.com.au.
“For me going to a nightclub has always been about listening to forward-thinking electronic music and connecting with like minded individuals, it’s about becoming a part of that community.
“Phones definitely take away from that experience and this is something that needs to change.”

Many agree with this, remarking mobile phones are the notable difference between the two generations in an array of posts on social media.
“2000’s clubbing was an art. No cell phone in sight, maybe a disposable camera, and the hope of no finger on the flash,” one said on TikTok.
“Mobile phones killed the fun, dance floors are a joke now, you can’t be free without someone catching it on camera,” another raged.
Someone else chipped in: “Just stop holding phones up on the dancefloor, it’s infuriating.”
It’s a sentiment shared by another TikTok video that went viral recently, which showed a DJ surrounded by young people who were all recording his set on their smart devices.
“This is why I think phones should be banned in all clubs,” Simon Doherty, who posted the clip , states.
“The sea of people who are all just filming on their phones, they don’t even move when the tune drops.
“No expression, no dancing, no losing yourself. Just filming.”

Some nightclubs have already started listening to these common complaints, with a popular venue on the party island of Ibiza recently introducing a “no phones on the dancefloor policy”.
“From open to close we take pride in creating a totally unique environment, centred around the mystical Temple, it’s a proper session where we lose our inhibitions and can enjoy a sense of freedom as we enforce our groundbreaking ‘No Phones’ policy inside the room,” Hï Ibiza said in a statement last week.
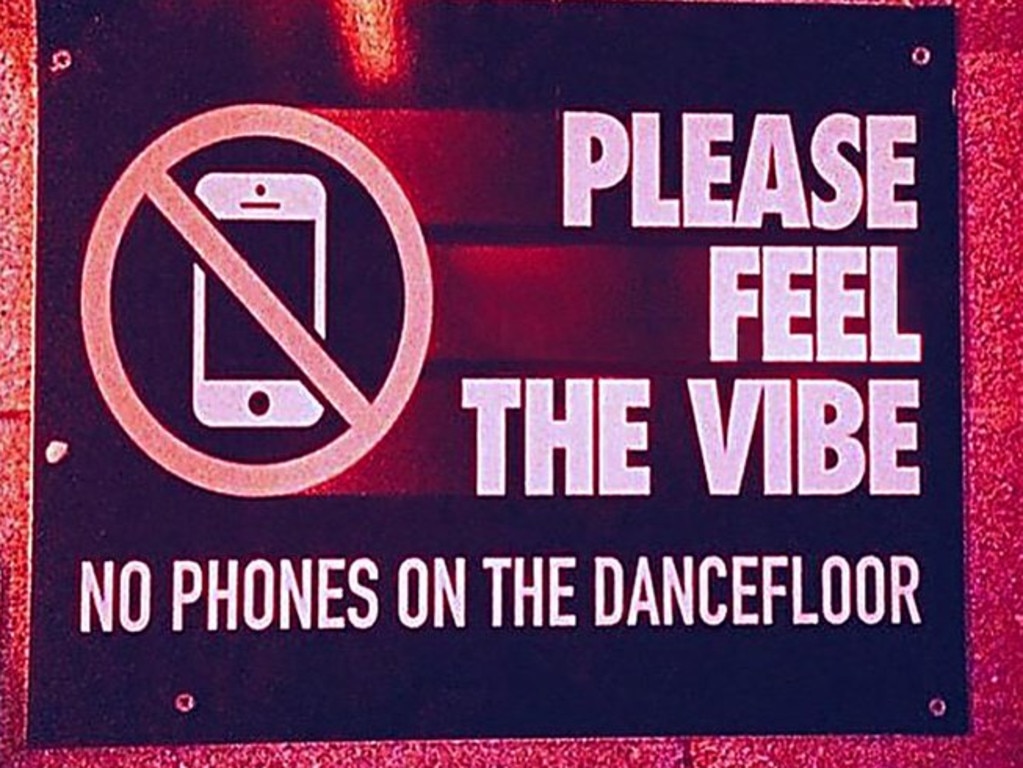
Mr Nott, whose new venue Lucky Cat Dumpling Bar & Lounge will open on Sydney’s Oxford Street in a matter of weeks, said while phones were a catalyst, the global lockdown couldn’t be ignored.
“Covid changed things. People’s habits about going out shifted, a lot of the older crowds didn’t come back and the younger generation missed out on clubbing at a crucial age,” he told news.com.au.
“Add this to cost of living, plus less work and wage increases and lack of venues / events, its really not a surprise the industry has been forced to adapt.”

Mr Gorrel, whose venue has been running in Darlinghurst for 25 years, agreed, revealing clubs were being re-imagined to suit modern tastes.
“It’s constantly changing and evolving and this is what I think makes nightclubs and music so special,” he told news.com.au.
“There’s always something new on the horizon and that’s really exciting.
“We’re currently experiencing week on week growth and our community is only getting stronger. While offerings are smaller, it doesn’t feel like the night-life scene is on the decline, which is a great thing.”
More Coverage

It seems Millennials aren’t willing to budge on their views, declaring Gen Z – who have previously been described as “generation stay-at-home” – are “missing out”.
“Clubbing back in the day was honestly the best. That’s how most of us met our husbands,” one argued.
As one declared: “Spent my 20s clubbing. It was wild yet utterly glorious.”
Matildas star Mary Fowler, won Australia’s hearts during the Women’s World Cup in 2023, is being honoured in the perfect way.
Belle Delphine earned thousands selling a gross item to men – but years later, she’s revealed the “shocking” truth about the bizarre cash grab.
A mother has been killed and her son critically injured after being viciously mauled by a pack of 13 dogs.

IMAGES
VIDEO
COMMENTS
In 2007, computer-based phones (smartphones) were introduced . Since then, smartphones have become an indispensable part of daily life in all communities and countries. ... (SA) has also been studied based on previous internet addiction research . Smartphones distinguish their use from traditional Internet use on computers or laptops because ...
Research says "when cell phone use becomes an addiction, the behavior becomes stressful". Salvatore Insiga, a neurosurgeon at Northwell Health's Neuroscience Institute in Manhasset, New York, considered that nonetheless that there is no solid proof between cell phone radiation and tumor risk but the possibility still exists.
We conducted a meta-analysis of studies published between 2014 and 2020 that used the Smartphone Addiction Scale, the most common measure of problematic smartphone use. We focused on adolescents and young adults (aged 15 to 35) since they tend to have the highest screen time and smartphone ownership rates. Across 24 countries, 83 samples, and ...
A dominating research field was excessive or problematic use, i.e., where intense mobile phone use is described as a behavioral addiction and/or pathological. A large amount of instruments to measure excessive or problematic use occurred, and problematic use was associated with several adverse outcomes, such as depression, anxiety, and sleep ...
Overall, Table 2 shows that smartphone addiction was associated with statistically significant effect sizes. Under the fixed-effect model, there was a statistically significant difference between the weighted mean correlation of the dissertation (r = −0.26) and journal (r = −0.06).The between-levels difference was statistically significant, Q B (1) = 27.65, p < .001, and findings showed ...
Abstract. We present a review of the studies that have been published about addiction to cell phones. We analyze the concept of cell-phone addiction as well as its prevalence, study methodologies, psychological features, and associated psychiatric comorbidities. Research in this field has generally evolved from a global view of the cell phone ...
Another line of research accepts the concept of cell-phone addiction, broadening the possibilities and defining the behavior, together with the term "addiction" related to compulsive behavior (), dependent behavior (34, 45, 67, 85, 87), and problematic, excessive, or pathological use (62, 80, 88), which leads to evaluation instruments with relatively broad behavioral ranges.
We present a review of the studies that have been published about addiction to cell phones. We analyze the concept of cell-phone addiction as well as its prevalence, study methodologies, psychological features, and associated psychiatric comorbidities. Research in this field has generally evolved from a global view of the cell phone as a device to its analysis via applications and contents ...
This research explores whether addictions around mobile phones should be treated more as a physiological or a psychological problem. A new survey about mobile addiction and time use (MATU), constructed from several studies, tests to what degree time use on mobile phones (a physiological cause) is correlated with four behavioral factors predicting proneness to addiction, respectively one ...
Depression, anxiety, stress and neuroticism significantly predict smartphone addiction level, as in research hypothesis 6. The results show that there is a high prevalence of smartphone addiction among medical students. ... Makoe M. Exploring the use of MXit: a cell-phone social network to facilitate learning in distance education. Open ...
Both the rate of mobile phone addiction and suicidality among adolescents have increased during the pandemic lockdown. However, the relationship between mobile phone addiction and suicide risk and the underlying psychological mechanisms remains unknown. This study examined the associations between mobile phone addiction in adolescents during the first month of lockdown and the suicide risk in ...
used in research on both cell phone and subs tance addiction (128). e FFM establishes ve dimension s of personality (extraversion, openness to experience or change, conscientiousness, agr eeable -
While cell phones are integral to our daily lives and have numerous benefits, many people have developed what some researchers consider phone addiction symptoms that can have negative effects on well-being. According to some research, roughly 27.9% of young adults are addicted to their cell phones.
phones and exper iencing distress on separation . multitude of studies have documented that mobile. phone addiction would bring about negative impacts. on physi cal and mental health as well as ...
Prevalence of Smartphone Addiction, Sociodemographic Characteristics and Smartphone Usage. The overall prevalence of smartphone addiction was 38.9% (95%CI: 35.9-41.9%; n = 406/1,043).This includes 35.7% of males who were addicted and 40.1% of females ().For participants aged under 21 years, 42.2% exhibited smartphone addiction, compared to 34.2 and 28.0% of participants aged 22-25 years ...
Smartphones currently dominate people's lives and interests due to their increased affordability and functionality. However, the negative aspects of smartphone use, such as smartphone addiction, have recently been brought up. This study utilized a qualitative approach to explore the symptoms of smartphone addiction among working adults in China and the psychological factors that affect such ...
Dr. Lembke noted that an addiction is partially defined by the three C's: Control: Using a substance or performing a behavior (like gambling) in ways that would be considered out of control, or ...
Cell-phone addiction shows a distinct user profile that differentiates it from Internet addiction. Without evidence pointing to the influence of cultural level and socioeconomic status, the pattern of abuse is greatest among young people, primarily females. ... Undoubtedly, the greatest roadblock to research in cell-phone abuse is the diversity ...
The American Psychiatric Association ( APA, 2013) first categorized a behavior - gambling - as a non-substance-related addictive disorder and recommends further research on Internet gaming disorder. However, at this time, no mention has been made of smartphone addiction in either the DSM-5 or in the ICD-11's draft.
Signs and Symptoms of Cell Phone Addiction. The following are some of the signs and symptoms of cell phone addiction, according to Entrepreneur. Reaching for the phone first thing in the morning: When something becomes a vital part of your daily routine, it can affect thinking and emotions. As Entrepreneur notes, 68 percent of adults sleep with ...
Smartphone addiction affects families in so many ways and if anything the grown-ups using their phones so much is perpetuating kids using them more. So it's no surprise that phone addiction is a ...
Cell phone tips. To reduce radiofrequency (RF) radiation near your body: Get a hands-free headset that connects directly to your phone. Use speaker-phone more often. In the past, RF radiation interfered with the operation of some pacemakers. If you have a pacemaker and are concerned about how your cell phone use may affect it, contact your ...
Cold Turkey Won't Fix Phone Addiction. The vast majority of the "fixes" inside and outside of the office focus on restricting or limiting access to phones and social media, an approach that ...
Older Americans are suffering from cellphone addiction just as much as teens, research found Research found the average adult spends more than four hours on their phone daily and much of this time ...
Phones are everywhere: 95% of teens say they have access to a cellphone, and 58% of teens report using TikTok daily, according to a 2023 Pew Research Center survey.. With that many kids online ...
In the state, a 15-year-old minor consumed a poisonous substance after not receiving the money for a mobile phone. He was then rushed to the medical college. Psychiatrist of Government Medical ...
Conducted by the NORC — previously called the National Opinion Research Center — at the University of Chicago, the research includes 1,274 teens (ages 14 to 17) and young adults (ages 18 to 22 ...
When women are excluded from biomedical research, it leaves doctors and researchers with an incomplete understanding of health and disease, including alcohol addiction.
In the United States today, the weight of mental health challenges looms large. During the Activate 2023 conference last fall hosted by Mindful Philanthropy, a nonprofit organization dedicated to increasing high-impact funding of mental health, presenters shared alarming statistics that underscore the urgency of addressing mental health issues.
Gen Z's addiction to their phones is killing the art of clubbing, with experts stating modern tech is destroying the beloved Millennial "rite of passage".