
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Malpresentation
8-minute read
If you feel your waters break and you have been told that your baby is not in a head-first position, seek medical help immediately .
- Malpresentation is when your baby is not facing head-first down the birth canal as birth approaches.
- The most common type of malpresentation is breech — when your baby’s bottom or feet are facing downwards.
- A procedure called external cephalic version can sometimes turn a breech baby into a head-first position at 36 weeks.
- Most babies with malpresentation are born by caesarean, but you may be able to have a vaginal birth if your baby is breech.
- There is a serious risk of cord prolapse if your waters break and your baby is not head-first.
What are presentation and malpresentation?
‘Presentation’ describes how your baby is facing down the birth canal. The ‘presenting part’ is the part of your baby’s body that is against the cervix .
The ideal presentation is head-first, with the crown (top) of the baby’s head against the cervix, with the chin tucked into the baby’s chest. This is called ‘vertex presentation’.
If your baby is in any other position, it’s called ‘malpresentation’. Malpresentation can mean your baby’s face, brow, buttocks, foot, back, shoulder, arms or legs or the umbilical cord are against the cervix.
It’s safest for your baby’s head to come out first. If any other body part goes down the birth canal first, the risks to you and your baby may be higher. Malpresentation increases the chance that you will have a more complex vaginal birth or a caesarean.
If my baby is not head-first, what position could they be in?
Malpresentation is caused by your baby’s position (‘lie’). There are different types of malpresentation.
Breech presentation
This is when your baby is lying with their bottom or feet facing down. Sometimes one foot may enter the birth canal first (called a ‘footling presentation’).
Breech presentation is the most common type of malpresentation.
Face presentation
This is when your baby is head-first but stretching their neck, with their face against the cervix.
Transverse lie
This is when your baby is lying sideways. Their back, shoulders, arms or legs may be the first to enter the birth canal.
Oblique lie
This is when your baby is lying diagonally. No particular part of their body is against the cervix.
Unstable lie
This is when your baby continually changes their position after 36 weeks of pregnancy.
Cord presentation
This is when the umbilical cord is against the cervix, between your baby and the birth canal. It can happen in any situation where your baby’s presenting part is not sitting snugly in your pelvis. It can become an emergency if it leads to cord prolapse (when the cord is born before your baby, potentially reducing placental blood flow to your baby).
What is malposition?
If your baby is lying head-first, the best position for labour is when their face is towards your back.
If your baby is facing the front of your body (posterior position) or facing your side (transverse position) this is called malposition. Transverse position is not the same as transverse lie. A transverse position means your labour may take a bit longer and you might feel more pain in your back. Often your baby will move into a better position before or during labour.
Why might my baby be in the wrong position?
Malpresentation may be caused by:
- a low-lying placenta
- too much or too little amniotic fluid
- many previous pregnancies, making the muscles of the uterus less stable
- carrying twins or more
Often no cause is found.
Is it likely that my baby will be in the wrong position?
Many babies are in a breech position during pregnancy. They usually turn head-first as pregnancy progresses, and more than 9 in 10 babies in Australia have a vertex presentation (ideal presentation, head-first) at birth.
You are more likely to have a malpresentation if:
- this is your first baby
- you are over 40 years old
- you've had a previous breech baby
- you go into labour prematurely
How is malpresentation diagnosed?
Malpresentation is normally diagnosed when your doctor or midwife examines you, from 36 weeks of pregnancy. If it’s not clear, it can be confirmed with an ultrasound.
Can my baby’s position be changed?
If you are 36 weeks pregnant , it may be possible to gently turn your baby into a head-first position. This is done by an obstetrician using a technique called external cephalic version (ECV).
Some people try different postures or acupuncture to correct malpresentation, but there isn’t reliable evidence that either of these work.
Will I need a caesarean if my baby has a malpresentation?
Most babies with a malpresentation close to birth are born by caesarean . You may be able to have a vaginal birth with a breech baby, but you will need to go to a hospital that can offer you and your baby specialised care.
If your baby is breech, an elective (planned) caesarean is safer for your baby than a vaginal birth in the short term. However, in the longer term their health will be similar, on average, regardless of how they were born.
A vaginal birth is safer for you than an elective caesarean. However, about 4 in 10 people planning a vaginal breech birth end up needing an emergency caesarean . If this happens to you, the risk of complications will be higher.
Your doctor can talk to you about your options. Whether it’s safe for you to try a vaginal birth will depend on many factors. These include how big your baby is, the position of your baby, the structure of your pelvis and whether you’ve had a caesarean in the past.
What are the risks if I have my baby when it’s not head-first?
If your waters break when your baby is not head-first, there is a risk of cord prolapse. This is an emergency.
Vaginal breech birth
Risks to your baby can include:
- Erb’s palsy
- fractures, dislocations or other injuries
- bleeding in your baby’s brain
- low Apgar scores
- their head getting stuck – this is an emergency
Risks to you include:
- blood loss or blood clots
- infection in the wound
- problems with the anaesthetic
- damage to other organs nearby, such as your bladder
- a higher chance of problems in future pregnancies
- a longer recovery time than after a vaginal birth
Risks to your baby include:
- trouble with breathing — this is temporary
- getting a small cut during the surgery
Will I have a malpresentation in my future pregnancies?
If you had a malpresentation in one pregnancy, you have a higher chance of it happening again, but it won’t necessarily happen in future pregnancies. If you’re worried, it may help to talk to your doctor or midwife so they can explain what happened.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: July 2022
Related pages
Labour complications.
- Interventions during labour
- Giving birth - stages of labour
Breech pregnancy
Search our site for.
- Caesarean Section
- Foetal Version
Need more information?
Top results
When a baby is positioned bottom-down late in pregnancy, this is called the breech position. Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website

Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

Presentation and position of baby through pregnancy and at birth
Presentation and position refer to where your baby’s head and body is in relation to your birth canal. Learn why it’s important for labour and birth.
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
- GP practice services
- Health advice
- Health research
- Medical professionals
Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skin, nail and hair health
Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
- Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
Malpresentations and malpositions
Peer reviewed by Dr Laurence Knott Last updated by Dr Colin Tidy, MRCGP Last updated 22 Jun 2021
Meets Patient’s editorial guidelines
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article :
Malpresentation, malposition.
Usually the fetal head engages in the occipito-anterior position (more often left occipito-anterior (LOA) rather than right) and then undergoes a short rotation to be directly occipito-anterior in the mid-cavity. Malpositions are abnormal positions of the vertex of the fetal head relative to the maternal pelvis. Malpresentations are all presentations of the fetus other than vertex.
Obstetrics - the pelvis and head

Continue reading below
Predisposing factors to malpresentation include:
Prematurity.
Multiple pregnancy.
Abnormalities of the uterus - eg, fibroids.
Partial septate uterus.
Abnormal fetus.
Placenta praevia.
Primiparity.
Breech presentation
See the separate Breech Presentations article for more detailed discussion.
Breech presentation is the most common malpresentation, with the majority discovered before labour. Breech presentation is much more common in premature labour.
Approximately one third are diagnosed during labour when the fetus can be directly palpated through the cervix.
After 37 weeks, external cephalic version can be attempted whereby an attempt is made to turn the baby manually by manipulating the pregnant mother's abdomen. This reduces the risk of non-cephalic delivery 1 .
Maternal postural techniques have also been tried but there is insufficient evidence to support these 2 .
Many women who have a breech presentation can deliver vaginally. Factors which make this less likely to be successful include 3 :
Hyperextended neck on ultrasound.
High estimated fetal weight (more than 3.8 kg).
Low estimated weight (less than tenth centile).
Footling presentation.
Evidence of antenatal fetal compromise.
Transverse lie 4
When the fetus is positioned with the head on one side of the pelvis and the buttocks in the other (transverse lie), vaginal delivery is impossible.
This requires caesarean section unless it converts or is converted late in pregnancy. The surgeon may be able to rotate the fetus through the wall of the uterus once the abdominal wall has been opened. Otherwise, a transverse uterine incision is needed to gain access to a fetal pole.
Internal podalic version is no longer attempted.
Transverse lie is associated with a risk of cord prolapse of up to 20%.
Occipito-posterior position
This is the most common malposition where the head initially engages normally but then the occiput rotates posteriorly rather than anteriorly. 5.2% of deliveries are persistent occipito-posterior 5 .
The occipito-posterior position results from a poorly flexed vertex. The anterior fontanelle (four radiating sutures) is felt anteriorly. The posterior fontanelle (three radiating sutures) may also be palpable posteriorly.
It may occur because of a flat sacrum, poorly flexed head or weak uterine contractions which may not push the head down into the pelvis with sufficient strength to produce correct rotation.
As occipito-posterior-position pregnancies often result in a long labour, close maternal and fetal monitoring are required. An epidural is often recommended and it is essential that adequate fluids be given to the mother.
The mother may get the urge to push before full dilatation but this must be discouraged. If the head comes into a face-to-pubis position then vaginal delivery is possible as long as there is a reasonable pelvic size. Otherwise, forceps or caesarean section may be required.

Occipito-transverse position
The head initially engages correctly but fails to rotate and remains in a transverse position.
Alternatives for delivery include manual rotation of fetal head using Kielland's forceps, or delivery using vacuum extraction. This is inappropriate if there is any fetal acidosis because of the risk of cerebral haemorrhage.
Therefore, there must be provision for a failure of forceps delivery to be changed immediately to a caesarean. The trial of forceps is therefore often performed in theatre. Some centres prefer to manage by caesarean section without trial of forceps.
Face presentations
Face presents for delivery if there is complete extension of the fetal head.
Face presentation occurs in 1 in 1,000 deliveries 5 .
With adequate pelvic size, and rotation of the head to the mento-anterior position, vaginal delivery should be achieved after a long labour.
Backwards rotation of the head to a mento-posterior position requires a caesarean section.
Brow positions
The fetal head stays between full extension and full flexion so that the biggest diameter (the mento-vertex) presents.
Brow presentation occurs in 0.14% of deliveries 5 .
Brow presentation is usually only diagnosed once labour is well established.
The anterior fontanelle and super orbital ridges are palpable on vaginal examination.
Unless the head flexes, a vaginal delivery is not possible, and a caesarean section is required.
Further reading and references
- Hofmeyr GJ, Kulier R, West HM ; External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2015 Apr 1;(4):CD000083. doi: 10.1002/14651858.CD000083.pub3.
- Hofmeyr GJ, Kulier R ; Cephalic version by postural management for breech presentation. Cochrane Database Syst Rev. 2012 Oct 17;10:CD000051. doi: 10.1002/14651858.CD000051.pub2.
- Management of Breech Presentation ; Royal College of Obstetricians and Gynaecologists (Mar 2017)
- Szaboova R, Sankaran S, Harding K, et al ; PLD.23 Management of transverse and unstable lie at term. Arch Dis Child Fetal Neonatal Ed. 2014 Jun;99 Suppl 1:A112-3. doi: 10.1136/archdischild-2014-306576.324.
- Gardberg M, Leonova Y, Laakkonen E ; Malpresentations - impact on mode of delivery. Acta Obstet Gynecol Scand. 2011 May;90(5):540-2. doi: 10.1111/j.1600-0412.2011.01105.x.
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 21 Jun 2026
22 jun 2021 | latest version.
Last updated by
Peer reviewed by

Feeling unwell?
Assess your symptoms online for free
GFMER Geneva Foundation for Medical Education and Research
- Annual reports
- GFMER members
- Country coordinators
- Obstetric fistula
- Cervical cancer
- Emergency and surgical care
- Picture of the week
- Social media
- Free medical journals
Obstetrics Simplified - Diaa M. EI-Mowafi
Shoulder Presentation (Transverse or Oblique lie)
- The longitudinal axis of the foetus does not coincide with that of the mother.
- These are the most hazardous malpresentations due to mechanical difficulties that occur during labour .
- The oblique lie which is deviation of the head or the breech to one iliac fossa, is less hazardous as correction to a longitudinal lie is more feasible.
3-4% during the last quarter of pregnancy but 0.5% by the time labour commences.
Factors that
- change the shape of pelvis, uterus or foetus,
- allow free mobility of the foetus or
- Contracted pelvis.
- Lax abdominal wall.
- Uterine causes as bicornuate, subseptate and fibroid uterus.
- Pelvic masses as ovarian tumours.
- Multiple pregnancy.
- Polyhydramnios.
- Placenta praevia.
- Prematurity.
- Intrauterine foetal death.
The scapula is the denominator
- Left scapulo-anterior.
- Right scapulo-anterior.
- Right scapulo-posterior.
- Left scapulo-posterior.
Scapulo-anterior are more common than scapulo-posterior as the concavity of the front of the foetus tends to fit with the convexity of the maternal spines.
During pregnancy
- The abdomen is broader from side to side.
- Fundal level: lower than that corresponds to the period of amenorrhoea.
- Fundal grip: The fundus feels empty.
- Umbilical grip: The head is felt on one side while the breech one the other. In transverse lie, they are at the same level, while in oblique lie one pole, usually the head as it is heavier, is in a lower level i.e. in the iliac fossa.
- First pelvic grip: Empty lower uterine segment.
- FHS are best heard on one side of the umbilicus towards the foetal head.
- Confirms the diagnosis and may identify the cause as multiple pregnancy or placenta praevia.
During labour
In addition to the previous findings, vaginal examination reveals:
- The presenting part is high.
- Membranes are bulging.
- Premature rupture of membranes with prolapsed arm or cord is common. The dorsum of the supinated hand points to the foetal back and the thumb towards the head. The right hand of the foetus can be shacked, correctly by the right hand of the obstetrician and the left hand by the left one.
- When the cervix is sufficiently dilated particularly after rupture of the membranes, the scapula, acromion, clavicle, ribs and axilla can be felt.
Mechanism of Labour
As a rule no mechanism of labour should be anticipated in transverse lie and labour is obstructed.
If a patient is allowed to progress in labour with a neglected or unrecognized transverse lie, one of the following may occur:
- This is the usual and most common outcome.
- The lower uterine segment thins and ultimately ruptures.
- The foetus becomes hyperflexed, placental circulation is impaired, cord is prolapsed and compressed leading to foetal asphyxia and death.
- Rarely the foetal lie may be corrected by the splinting effect of the contracted uterine muscles so that the head presents.
- Rarely, by similar process the breech may come to present.
- Very rarely, if the foetus is very small or dead and macerated, the shoulder may be forced through the pelvis followed by the head and trunk.
- Very rarely, the head is retained above the pelvic brim, the neck greatly elongates, the breech descends followed by the trunk and the after -coming head, i.e. spontaneous version occurs in the pelvic cavity.
External cephalic version
Can be done in late pregnancy or even early in labour if the membranes are intact and vaginal delivery is feasible. In early labour, if version succeeded apply abdominal binder and rupture the membranes as if there are uterine contractions.
Internal podalic version
It is mainly indicated in 2nd twin of transverse lie and followed by breech extraction.
Prerequisites:
- General or epidural anaesthesia.
- Fully dilated cervix.
- Intact membranes or just ruptured.
Caesarean section
- It is the best and safest method of management in nearly all cases of persistent transverse or oblique lie even if the baby is dead.
- As rupture of membranes carries the risk of cord prolapse, an elective caesarean section should be planned before labour commences.
Neglected (Impacted) shoulder
Clinical picture (impending rupture uterus)
- Exhaustion and distress of the mother.
- Shoulder is impacted may be with prolapsed arm and / or cord.
- Membranes are ruptured since a time.
- Liquor is drained.
- The uterus is tonically contracted.
- The foetus is severely distressed or dead.
- Caesarean section is the safest procedure even if the baby is dead. A classical or low vertical incision in the uterus facilitates extraction of the foetus as a breech in such a condition.
- Any other manipulations will lead eventually to rupture uterus so they are contraindicated.
UNSTABLE LIE
A foetus which changes its lie frequently from transverse to oblique to longitudinal.
- Polyhydramnios.
- Prematurity and IUFD.
- Contracted pelvis.
- Placenta praevia.
- Pelvic tumours.
- Multiparae with a lax uterus and abdominal wall.
- Can be done whenever the woman is examined but in majority of cases it will recur so it is better to defer it until full term (37-40 weeks).
- After correcting the foetal lie to longitudinal, apply an abdominal binder, start oxytocin infusion and do amniotomy when the uterine contractions started and the presenting part is well settled into the pelvic brim.
- Failure of external version .
- Some do it selectively in cases discovered after 40 weeks’ gestation.
- Shoulder dystocia : Guidelines, reviews

- Pregnancy Week By Week
- Ovulation Calculator
Malpresentation and Malposition of the Fetus
A malpresentation or malposition of the fetus is when the fetus is in any abnormal position, other than vertex (head down) with the occiput anterior or posterior.
The following are considered malpresentations or malpositions:
Unstable lie
- Transverse presentation
- Oblique presentation
Face presentation
Brow presentation
Shoulder presentation
High head at term
- Prolapsed arm
The cause of a malpresentation can often not be clearly identified but it can be associated with the following:
- Preterm pregnancy
- Uterine anomalies
- Pelvic tumors eg f ibroids
- Placenta previa
- Grandmultiparty
- Contracted maternal pelvis
- Multiple gestation
- Too much amniotic fluyid (polyhydramnios)
- Short umbilical cord
- Fetal anomalies (e.g. anencephaly, hydro-cephalus)
- Abnormal fetal motor ability
There is an increased risk of neonatal and maternal complications associated with a malpresentation including neonatal and maternal trauma. If delivery is indicated, doing a cesarean delivery can significantly decrease the risk of complications.
Transverse lie
Oblique lie
In most cases of a normal vertex (head down) presentation, the baby's head is flexed with the chin close to the baby's chest. In these cases, the presenting part is the occiput, the posterior part of the baby's head. If the baby's head is more but not completekly extended then the baby's brow presents towards the vagina. A brow presentation is rare, maybe happening in about 1 in 2,000 births, more likely in pwomen with their second or subsequent births. A baby with a brow presentation can only deliver vaginally if the head flexes or extends.
Prolapsed arm
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 99, Issue Suppl 1
- PLD.23 Management of transverse and unstable lie at term
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- R Szaboova ,
- S Sankaran ,
- K Harding ,
- King’s Health Partners, London, UK
Aims To determine current practice and outcomes in women admitted to antenatal ward with diagnosis of transverse or unstable lie.
Background Fetal lie (other than longitudinal) at term may predispose to prolapse of cord or fetal arm and uterine rupture. Local guidelines recommend admission at 37+0 (RCOG guidelines after 37+6 weeks) but give no specific recommendations regarding further management.
Methods A retrospective study was conducted at St Thomas’ Hospital, London from 2009–2012 of all women admitted with unstable/transverse lie. The diagnosis was based on ultrasound examination. Women with placenta praevia and non-singleton deliveries were excluded.
Results Study included 198 cases of unstable/transverse lie. 58% were admitted before 38 weeks. The average length of admission was 7 days (IQR 4–11). There were no cases of cord prolapse or need for an immediate caesarean section from the antenatal ward. 73% of women had a caesarean section at a median gestation of 39+1 weeks (IQR 38+4 – 40+2) although almost half of these (41%) had a cephalic presentation at the time of elective caesarean sections. None of these had an absolute indication for Caesarean section.
Discussion and conclusions The diagnosis of unstable/transverse lie leads to a prolonged inpatient stay and a high Caesarean section rate. From our study and the evidence from the available literature, we recommend delaying admission until at least 38 weeks and awaiting spontaneous version. Future research should focus on the safety of outpatient management with consideration of utilising techniques such as cervical length and fetal fibronectin.
https://doi.org/10.1136/archdischild-2014-306576.324
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Read the full text or download the PDF:
- Open access
- Published: 06 August 2019
Is this patient really “(un)stable”? How to describe cardiovascular dynamics in critically ill patients
- Jean-Louis Vincent ORCID: orcid.org/0000-0001-6011-6951 1 ,
- Maurizio Cecconi 2 &
- Bernd Saugel 3
Critical Care volume 23 , Article number: 272 ( 2019 ) Cite this article
39k Accesses
6 Citations
61 Altmetric
Metrics details
Earlier this week during rounds in the intensive care unit, a resident reported, “Mr S. became hemodynamically unstable so we had to give norepinephrine.” Later, another resident described a patient with acute respiratory distress syndrome who had been on renal replacement therapy for the last 36 h as being, “hemodynamically stable under 1 μg/kg/min of norepinephrine.” This led us to reflect on the meanings of these two words—“stable” and “unstable”—when describing cardiovascular dynamics in critically ill patients.
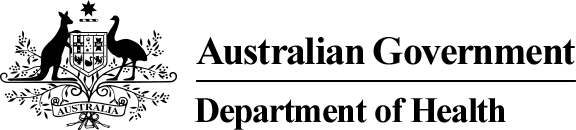
The terms hemodynamically “stable” and “unstable” are used frequently but what do they actually mean? And are they appropriate or even correct? Can a critically ill patient ever really be accurately described as being stable or unstable? A stable condition can be defined as a situation that does not change substantially over time. But surely all critically ill patients are per se un stable as, by the very nature of being critically ill, their physiological variables—including cardiovascular dynamics—change frequently over time [ 1 ]. Although vital signs can appear stable when a patient is receiving organ support, the patient is still critically ill. Terminology in such patients needs to be precise, and vague descriptive terms should be avoided. Indeed, there are no generally accepted and uniform definitions of the conditions stable and unstable, and the same patient may be classified as stable or unstable by different doctors and nurses depending on their clinical judgment, experience, and knowledge of the patient’s clinical course. In Fig. 1 , we propose some clinical scenarios that demonstrate these problems with the use of the words “stable” and “unstable” when describing cardiovascular dynamics in critically ill patients.
What is hemodynamic (in)stability
So, how should we describe these patients? To the first resident, we suggested that Mr. S. who had become “hemodynamically unstable” had actually developed circulatory shock and that this was the preferred term. To further describe the cardiovascular dynamics in this and similar patients, available objective criteria (blood pressure, cardiac output, rate of vasopressor or inotrope) should be used.
For the second resident, the problem is perhaps more related to interpretation than definition. The word “stable” often has positive connotations when used to refer to patient condition. When the resident described his patient as “being stable,” everyone agreed, knowing that this meant there had been no acute change in the patient’s condition or treatment. In fact, the patient still had profound circulatory shock. Using the word “stable” in such patients may even create a false sense of security for the care team, such that they begin to accept the critical state of the patient as “normal” and lessen efforts to try and resolve the serious condition. Additionally in this case, when the relatives called anxiously to get some news and the nurse said “the situation is stable,” this gave them the impression that their loved one was not getting worse, thus offering them some hope of recovery. Without further more detailed explanation, relatives may not understand that being stable in such critical conditions actually means the patient is not getting better and his/her chances of a positive outcome are likely getting worse. Indeed, the duration of shock is an important prognostic factor [ 2 , 3 ].
Although widely used among physicians and frequently present in the literature, the words “stable” and “unstable” to describe cardiovascular dynamics in critically ill patients can have different meanings to different people and in different situations, making them confusing word choices that should be avoided. We must be careful and precise with our choice of words to colleagues, patients, and families and avoid vague terms that could be misinterpreted. The word “stable” should not be used to describe a condition that remains critical, and “hemodynamic instability” should be described using objective criteria such as blood pressure, cardiac output, or vasopressor dose.
Availability of data and materials
Not applicable.
Frost P, Wise MP. Recognition and early management of the critically ill ward patient. Br J Hosp Med (Lond). 2007;68:M180–3.
Article Google Scholar
Vincent JL, Nielsen ND, Shapiro NI, et al. Mean arterial pressure and mortality in patients with distributive shock: a retrospective analysis of the MIMIC-III database. Ann Intensive Care. 2018;8:107.
Maheshwari K, Nathanson BH, Munson SH, et al. The relationship between ICU hypotension and in-hospital mortality and morbidity in septic patients. Intensive Care Med. 2018;44:857–67.
Download references
Acknowledgements
Author information, authors and affiliations.
Department of Intensive Care, Erasme Hospital, Université libre de Bruxelles, 1170, Brussels, Belgium
Jean-Louis Vincent
Department of Anesthesia and Intensive Care Units, Humanitas Research Hospital, 20089, Milan, Italy
Maurizio Cecconi
Department of Anesthesiology, Center of Anesthesiology and Intensive Care Medicine, University Medical Center Hamburg-Eppendorf, 20246, Hamburg, Germany
Bernd Saugel
You can also search for this author in PubMed Google Scholar
Contributions
JLV wrote the first draft. MC and BS critically revised the content. All authors read and approved the final manuscript before submission.
Corresponding author
Correspondence to Jean-Louis Vincent .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
JLV is the Editor-in-Chief of Critical Care . He has no other conflicts of interest to declare related to this manuscript. The other authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Vincent, JL., Cecconi, M. & Saugel, B. Is this patient really “(un)stable”? How to describe cardiovascular dynamics in critically ill patients. Crit Care 23 , 272 (2019). https://doi.org/10.1186/s13054-019-2551-1
Download citation
Received : 06 April 2019
Accepted : 23 July 2019
Published : 06 August 2019
DOI : https://doi.org/10.1186/s13054-019-2551-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Critical Care
ISSN: 1364-8535
- Submission enquiries: [email protected]
More From Forbes
Unleashing engagement: 4 ways to reimagine stale presentations.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Lux Narayan is the CEO and co-founder of StreamAlive , a leading audience engagement platform for live sessions.
In my career, I’ve given more presentations than I can count. In fact, I think I’ve been presenting for a living all along. As a founder, I motivated hundreds of employees, as a TED speaker , I connected with like-minded leaders and as an amateur stand-up comedian, I facilitated connection through laughter.
And for as many successful presentations I've given, I've still failed many times—some stand-up sets left me yearning for a sitcom laugh track to fill the silence after a flopped joke. There were corporate presentations where I could not keep the audience’s attention, rendering my message ineffective. But the underlying truth of every presentation I've ever given is a desire to engage, connect and make my audience feel seen.
Today in the workplace, more technology than ever before is competing for our limited attention. In remote and hybrid environments, virtual meetings and presentations fill our calendars, but few are efficient or productive. According to a 2022 study from meeting analytics startup Read AI, 40% of virtual meeting participants have below-average or poor engagement, and 22% don’t say a single word. With more meetings on the calendar than ever, productivity and employee satisfaction can both take a huge hit from low meeting engagement.
I’ve spent a fair part of my life designing presentations that capture audiences’ attention and I’ve found ways to cut through the noise. Here are my four most essential pieces of advice for guaranteeing engagement in every presentation you lead, so your presentations can feel more like conversations.
‘Ghost Of Tsushima’ Is Already Flooded With Negative Reviews On Steam
Wwe smackdown results winners and grades with stratton vs belair, biden trump debates what to know as trump pushes for 2 more faceoffs, 1. less talking, more listening.
Shifting your mindset from "presenting" to "listening" is the key to hosting effective virtual meetings. No matter their size, online meetings that put attendees at the center of the conversation and invite everyone to participate create an environment that mimics successful in-person meetings. Presenters can stimulate spontaneous conversation and ensure that every attendee feels included by focusing on asking questions and listening for understanding.
It may seem counterintuitive to ask a keynote presenter to present less, but presentations, especially virtual ones, often feel too much like monologues. In many meetings, it has become the norm for most participants to be "cameras off," further emphasizing the disconnect between the presenter and the audience.
A good presenter focuses on dialogue and looks for information from their audience to guide them on how to move forward, adjusting the presentation in real time. In a classroom, lecturers can poll students to check for understanding. Poor or inconclusive responses can indicate that the presenter needs to go over the material in more detail.
After all, "listening" to your audience does not always mean they are communicating verbally. It just means they are being heard.
2. Foster Channels For Interaction
In a perfect world, your audience is full of ideas and eager to participate, but in reality, they likely need some encouragement. Building avenues for engagement into your presentation is often the best way to facilitate discussion.
To break through the monotony, find a way to "interrupt" your audience. Pausing for questions is not enough. Polls, interactive maps, games and other tools bring a light, easy tone to your content, as well as acting as a natural break and signaling to the audience that it’s time to speak up.
3. Pass The Microphone To The Audience
Participatory meeting culture goes beyond added visual elements. To truly upgrade the audience’s experience, encourage attendees to lead the discussion, foster the conversation and connect. At StreamAlive, we lean heavily on our virtual platform’s native chat function to engage with participants. For example, in our live streams and demos, we visualize the chat in real time and use AI to collect every question and link shared in the chat. That way, we can answer "FAQs" in our post-event email.
Directing attendees to the chat creates a sense of community anchored in the "now" and founded in shared interests, which drives better engagement. I encourage presenters to explore tools outside of their video conferencing platform’s integrated features to push the boundaries of creativity when presenting. Marketplaces like Zoom’s Essential Apps are a goldmine of resources to help level up your presentations beyond the status quo.
4. Visual Storytelling
Visual aids are crucial to the 65% of people identified as visual learners . Instead of using unrelated stock images merely to break up text, reinforce your message with strategic visuals woven into your storytelling. Each image should clearly contribute to the narrative of the presentation, and be used to reinforce key points and create a cohesive story. In the case of our platform, audiences contribute to live, onscreen visuals (like real-time polls or interactive maps, for example) that help ensure everyone is included in the conversation. The visuals evolve with audience participation.
With longer, text-based presentations, attendees might zone out, missing crucial information. To counteract this, mimic the flow of normal conversation. Think about how long it is appropriate to monopolize a dinner table conversation before inviting someone else to participate by asking a question. The same holds true for punctuating your presentation with helpful images and audience participation. We are used to engaging in short bursts and engagement is rich when conversation flows naturally.
Structuring your presentation with a clear visual flow means images will serve as "breadcrumbs" to help attendees follow along and reconnect if their attention lapses. Summarize what has happened so far and give your audience a preview of what will happen next.
On Your Way To Better Presentations
Improving virtual meetings involves more than new technologies or adding features; it requires rethinking engagement strategies. Focus on listening, engaging and visually guiding your audience to transform routine sessions into dynamic, effective communication platforms. This approach will improve the overall meeting experience, making virtual gatherings something participants look forward to.
Remember, as Maya Angelou once wrote, "At the end of the day, people won’t remember what you said, they'll remember how you made them feel."
Forbes Business Council is the foremost growth and networking organization for business owners and leaders. Do I qualify?

- Editorial Standards
- Reprints & Permissions
At revered Black school, Biden leans into faith and tells grads he hears voices of dissent
ATLANTA – President Joe Biden on Sunday warned graduates at one of the country's most revered African American academic institutions of "extremist forces aligned against the meaning and message of Morehouse" College in a commencement address that sought to lay out the stakes of the 2024 election.
"Graduates, this is what we're up against," Biden said during a 27-minute speech that leaned heavily into themes of faith and democracy in an appeal to Black voters. "They peddle a fiction, a character about what being a man is about − tough talk, abusing power, bigotry. Their idea of being a man is toxic."
"But that's not you. It's not us," he said.
Biden's remarks to the 414 graduates at Morehouse , an all-male historically Black college in Atlanta, came as he is struggling to unite Black voters , particularly Black men, around his candidacy. Many Morehouse students and faculty criticized Biden's participation when it was announced because of his support for Israel's war in Gaza.
"In a democracy, we debate dissent about America's role in the world. I want to say this very clearly: I support peaceful, nonviolent protest," Biden said on Sunday in response to the complaints. "Your voices should be heard. I promise you, I hear them."
Prep for the polls: See who is running for president and compare where they stand on key issues in our Voter Guide
No major disruptions, but peaceful protests target Biden
Although there were no major disruptions during Biden's speech, a few students walked out when Biden received an honorary Morehouse degree. More than a dozen graduates and at least three faculty members wore keffiyehs, while one student entered the ceremony draped in a Palestinian flag.
As Biden delivered his address, at least one female faculty member stood in the opposite direction, her fist raised, in a sign of protest.
Biden, wearing a maroon gown at the outdoor ceremony, said his administration is "working around the clock for more than just one cease-fire," but also to "bring the region together." He reiterated his support for a two-state solution in which Israelis and Palestinians live in peace.
"This is one of the hardest, most complicated problems in the world. There's nothing easy about it," Biden said. "I know it angers and frustrates many of you, including my family, but most of all, I know it breaks your heart. It breaks mine as well."
Biden added that leadership is about "fighting through the most intractable problems" to "find a solution by doing what you believe is right, even when it's hard and lonely."
About a mile away, pro-Palestinian protesters held a rally organized under the banner of "Say No to Genocide Joe Speaking at Morehouse." Morehouse's valedictorian also raised Israel's war in Gaza during his remarks before Biden took the lectern.
"It is my stance as a Morehouse man – nay as a human being – to call for an immediate and the permanent cease-fire in the Gaza Strip," graduating senior DeAngelo Jeremiah Fletcher said, with Biden sitting just steps behind him. Biden applauded in response.
Biden touts record with Black voters
Polling shows Biden is vastly underperforming his 2020 performance among Black voters, a reliably Democratic constituency, as some drift to Donald Trump, the former president and presumptive Republican nominee.
A New York Times/Siena College poll of six battleground states, including Georgia, found Biden has support from 60% of Black voters and Trump, while Trump is backed by 20% of Black voters. Biden won Black voters in the 2020 election by a 87%-12% margin, according to exit polls.
Ahead of Biden's arrival, Anwar Karim, a sophomore studying film at Morehouse and a member of Atlanta University Center Students for Justice in Palestine, told USA TODAY he was disappointed in his school’s choice of commencement speaker. He also decried Morehouse’s decision to award Biden an honorary degree, which is typically awarded to the school’s commencement speaker after a faculty vote.
“Morehouse College is dedicated to producing men of consequence who lead lives of service and leadership, and I just have to beg the question, when it comes to Biden, what is an example of his leadership?” Karim said Friday.
Biden commits to showing 'democracy is still the way'
In his speech, Biden touted his presidency as one that has delivered to Black Americans, pointing to efforts to invest in Black families and communities, cut child poverty, expand work opportunities, reduce prescription drug prices and cut student loan debt. He called out the "poison of white supremacy" and "systemic racism."
He said he is committed to "show that democracy, democracy, democracy is still the way," even in the face of inequality for Black Americans.
"What is democracy if Black men are being killed in the street? What is democracy if the trail of broken promises still leave Black communities behind?" Biden said. "What is democracy if you have to be ten times better than anyone else to get a fair shot? Most of all, what does it mean, as you've heard before, to be a Black man who loves his country even if it doesn't love him back in equal measure?"
Biden railed against new voting restrictions in Georgia and the "constant attacks on Black election workers." He also said those who stormed the U.S. Capitol on Jan. 6, 2021 "are called patriots by some," a clear reference to Trump.
“Not in my house," Biden said.
In the days leading up to his Morehouse visit, the White House focused on Black outreach. Biden met on Thursday with plaintiffs of the landmark Brown v. Board of Education Supreme Court decision, on the 70th anniversary of the dismantling of the "separate but equal" precedent. On Friday, Biden met with leaders of the "Divine Nine" HBCU sororities and fraternities.
More: In a nod to history, Biden meets with Brown v. Board of Education families
In Atlanta on Saturday, Biden spoke to Morehouse alumni and others at a campaign event at Mary Mac's Tea Room. "The fact is, this election, lots at stake, lots at stake. It's not about me. It's about the alternative as well," Biden said. "My opponent's not a good loser, but he is a loser."
Introducing Biden, Morehouse President David Thomas said, "No administration in history, since the inception of historically Black colleges and universities, has invested more in our institutions than the Biden administration."
"And if you look at his policies, it is very clear that those investments are not charity," Thomas said.
Biden, 81, closed his remarks with a reference to his age, a liability that has hung over his reelection. When he started his political career, Biden said he was told he was "too young." Now he hears he's "too old."
"Whether you're young or old, I know what endures: The strength and wisdom of faith endures. And my challenge to you is to still keep the faith as long as you can," Biden said. "Together we're capable of building a democracy worthy of our dreams."
AI + Machine Learning , Announcements , Azure AI Content Safety , Azure AI Studio , Azure OpenAI Service , Partners
Introducing GPT-4o: OpenAI’s new flagship multimodal model now in preview on Azure
By Eric Boyd Corporate Vice President, Azure AI Platform, Microsoft
Posted on May 13, 2024 2 min read
- Tag: Copilot
- Tag: Generative AI
Microsoft is thrilled to announce the launch of GPT-4o, OpenAI’s new flagship model on Azure AI. This groundbreaking multimodal model integrates text, vision, and audio capabilities, setting a new standard for generative and conversational AI experiences. GPT-4o is available now in Azure OpenAI Service, to try in preview , with support for text and image.
Azure OpenAI Service

A step forward in generative AI for Azure OpenAI Service
GPT-4o offers a shift in how AI models interact with multimodal inputs. By seamlessly combining text, images, and audio, GPT-4o provides a richer, more engaging user experience.
Launch highlights: Immediate access and what you can expect
Azure OpenAI Service customers can explore GPT-4o’s extensive capabilities through a preview playground in Azure OpenAI Studio starting today in two regions in the US. This initial release focuses on text and vision inputs to provide a glimpse into the model’s potential, paving the way for further capabilities like audio and video.
Efficiency and cost-effectiveness
GPT-4o is engineered for speed and efficiency. Its advanced ability to handle complex queries with minimal resources can translate into cost savings and performance.
Potential use cases to explore with GPT-4o
The introduction of GPT-4o opens numerous possibilities for businesses in various sectors:
- Enhanced customer service : By integrating diverse data inputs, GPT-4o enables more dynamic and comprehensive customer support interactions.
- Advanced analytics : Leverage GPT-4o’s capability to process and analyze different types of data to enhance decision-making and uncover deeper insights.
- Content innovation : Use GPT-4o’s generative capabilities to create engaging and diverse content formats, catering to a broad range of consumer preferences.
Exciting future developments: GPT-4o at Microsoft Build 2024
We are eager to share more about GPT-4o and other Azure AI updates at Microsoft Build 2024 , to help developers further unlock the power of generative AI.
Get started with Azure OpenAI Service
Begin your journey with GPT-4o and Azure OpenAI Service by taking the following steps:
- Try out GPT-4o in Azure OpenAI Service Chat Playground (in preview).
- If you are not a current Azure OpenAI Service customer, apply for access by completing this form .
- Learn more about Azure OpenAI Service and the latest enhancements.
- Understand responsible AI tooling available in Azure with Azure AI Content Safety .
- Review the OpenAI blog on GPT-4o.
Let us know what you think of Azure and what you would like to see in the future.
Provide feedback
Build your cloud computing and Azure skills with free courses by Microsoft Learn.
Explore Azure learning
Related posts
AI + Machine Learning , Azure AI Studio , Customer stories
3 ways Microsoft Azure AI Studio helps accelerate the AI development journey chevron_right
AI + Machine Learning , Analyst Reports , Azure AI , Azure AI Content Safety , Azure AI Search , Azure AI Services , Azure AI Studio , Azure OpenAI Service , Partners
Microsoft is a Leader in the 2024 Gartner® Magic Quadrant™ for Cloud AI Developer Services chevron_right
AI + Machine Learning , Azure AI , Azure AI Content Safety , Azure Cognitive Search , Azure Kubernetes Service (AKS) , Azure OpenAI Service , Customer stories
AI-powered dialogues: Global telecommunications with Azure OpenAI Service chevron_right
AI + Machine Learning , Azure AI , Azure AI Content Safety , Azure OpenAI Service , Customer stories
Generative AI and the path to personalized medicine with Microsoft Azure chevron_right
Join the conversation, leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
I understand by submitting this form Microsoft is collecting my name, email and comment as a means to track comments on this website. This information will also be processed by an outside service for Spam protection. For more information, please review our Privacy Policy and Terms of Use .
I agree to the above

IMAGES
VIDEO
COMMENTS
Lie - the relationship between the long axis of the fetus and the mother. Presentation - the fetal part that first enters the maternal pelvis. Position - the position of the fetal head as it exits the birth canal. Other positions include occipito-posterior and occipito-transverse. Note: Breech presentation is the most common ...
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.. In brow presentation, the neck is moderately arched so that the brow presents first.. Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor.
In cephalic presentation in a well-flexed fetus, the occiput is the point of direction. The fetal position refers to the location of the point of direction with reference to the four quadrants of the maternal outlet as viewed by the examiner. Thus, position may be right or left as well as anterior or posterior. Unstable lie
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant patient's spine) with the face and body angled to one side and the neck flexed. Abnormal presentations include face, brow, breech, and shoulder.
Malpresentation can mean your baby's face, brow, buttocks, foot, back, shoulder, arms or legs or the umbilical cord are against the cervix. It's safest for your baby's head to come out first. If any other body part goes down the birth canal first, the risks to you and your baby may be higher. Malpresentation increases the chance that you ...
Fetal presentation is a reference to the part of the fetus that is overlying the maternal pelvic inlet. The most common relationship between fetus and mother is the longitudinal lie, cephalic presentation. A breech fetus also is a longitudinal lie, with the fetal buttocks as the presenting part.
Breech presentation is the most common malpresentation, with the majority discovered before labour. ... Szaboova R, Sankaran S, Harding K, et al; PLD.23 Management of transverse and unstable lie at term. Arch Dis Child Fetal Neonatal Ed. 2014 Jun;99 Suppl 1:A112-3. doi: 10.1136/archdischild-2014-306576.324.
Shoulder Presentation (Transverse or Oblique lie) Definition. The longitudinal axis of the foetus does not coincide with that of the mother. These are the most hazardous malpresentations due to mechanical difficulties that occur during labour . The oblique lie which is deviation of the head or the breech to one iliac fossa, is less hazardous as ...
Unstable lie Breech Transverse lie Oblique lie Face presentation Brow presentation . In most cases of a normal vertex (head down) presentation, the baby's head is flexed with the chin close to the baby's chest. In these cases, the presenting part is the occiput, the posterior part of the baby's head.
The concepts of breech presentation, unstable lie, malpresentations, and malposition have not changed for many years but the diagnostic tools and management options change periodically as new management techniques are developed and the evidence for their use improves. Early in pregnancy the position, presentation, and lie of a fetus are ...
Definition: Relationship between the longitudinal axis of fetus and mother: longitudinal (resulting in either cephalic or breech presentation) oblique (unstable, will eventually become either transverse or longitudinal) transverse (resulting in shoulder presentation) back up; back down (indication for vertical uterine incision during cesarean ...
The Trusted Provider of Medical Information since 1899
An unstable lie is the term given to a fetus that continues to change its position and does not maintain a longitudinal lie at term (≥ 37 weeks). ... A fetus that does not maintain a cephalic presentation and longitudinal lie at term may reduce the possibility of a normal vaginal delivery. Women with an unstable lie or
3. Perform a CTG for 20 minutes, or cease earlier if the CTG meets the definition of normal prior to 20 minutes. 4. Check a formal ultrasound has been performed within 24 hours of the procedure. Ensure the presentation is still breech by use of the real time scanner. 5. Confirm the Medical Officer performing the procedure is available in 30 minutes
Breech presentation is the most commonly encountered malpresentation. Since publication of the Term Breech Trial that showed benefits for the fetus in undertaking caesarean section, there has been a large shift in practice. Nonetheless the fact remains that most babies will not be compromised by planning a vaginal birth, and maternal requests for vaginal delivery are not unreasonable. Many ...
A malpresentation is diagnosed when any part of the baby is presenting to the maternal pelvis other than the vertex of the fetal head. A malposition is diagnosed when the fetal head is in any position other than occipito-anterior (OA) flexed vertex. Both malpresentation and malposition are associated with prolonged or obstructed labour, fetal and maternal morbidity, and potential mortality, if ...
We have observed that there is significant variation in practice and a lack of published evidence on the management of unstable/transverse/oblique lie at term in the modern obstetric practice. The RCOG Green-top Guideline No.50 recommends elective admission after 37 + 0 weeks gestation and immediate admission with signs of labour or rupture of membranes (SROM) to reduce risk of cord prolapse [1].
A normal fetal lie is an ideal position for labor and baby delivery in which the baby is head-down with the chin tucked into its chest. The back of the head is positioned so that it is ready to enter the pelvis. The fetus faces the mother's back, called cephalic presentation, and the babies mostly settle in this position by 32 to 36 weeks of ...
Aims To determine current practice and outcomes in women admitted to antenatal ward with diagnosis of transverse or unstable lie. Background Fetal lie (other than longitudinal) at term may predispose to prolapse of cord or fetal arm and uterine rupture. Local guidelines recommend admission at 37+0 (RCOG guidelines after 37+6 weeks) but give no specific recommendations regarding further management.
Unstable angina, one of several acute coronary syndromes, causes unexpected chest pain, and usually occurs while resting.The most common cause is reduced blood flow to the heart muscle because the coronary arteries are narrowed by fatty buildups (atherosclerosis) that can rupture, causing injury to the coronary blood vessel.This results in blood clotting, which blocks blood flow to the heart ...
Although widely used among physicians and frequently present in the literature, the words "stable" and "unstable" to describe cardiovascular dynamics in critically ill patients can have different meanings to different people and in different situations, making them confusing word choices that should be avoided.
The documentation should state "evolving clinical presentation with changing characteristics" and describe what has been changing and what will be monitored, such as fluctuating pain, swelling, changes in vital signs, etc., to support an "evolving" clinical presentation statement. UNSTABLE and unpredictable characteristics are evident ...
1. Less Talking, More Listening. Shifting your mindset from "presenting" to "listening" is the key to hosting effective virtual meetings. No matter their size, online meetings that put attendees ...
President Joe Biden's commencement address at Morehouse College saw some peaceful protests from students and faculty but no major disruptions.
OpenAI, in partnership with Microsoft, announces GPT-4o, a groundbreaking multimodal model for text, vision, and audio capabilities. Learn more.
Establishing reliable and effective prediction models is a major research priority for air quality parameter monitoring and prediction and is utilized extensively in numerous fields. The sample dataset of air quality metrics often established has missing data and outliers because of certain uncontrollable causes. A broad learning system based on a semi-supervised mechanism is built to address ...
The pseudo-spin symmetry (PSS) provides an important angle to understand nuclear microscopic structure and the novel phenomena found in unstable nuclei. The relativistic Hartree-Fock (RHF) theory, that takes the important degrees of freedom associated with the π-meson and ρ-tensor (ρ-T) couplings into account, provides an appropriate description of the PSS restoration in realistic nuclei ...