An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Vet Sci

Therapy Dogs in Educational Settings: Guidelines and Recommendations for Implementation
Associated data.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Therapy dogs in educational settings have gained increase traction in recent years. Despite its potential benefits and popularity, there remain concerns of perceived risks such as sanitation, allergies, and safety issues, as well as a lack of guidelines, regulations and support resources available to school staff. Research is further lacking into the implementation process of therapy dog programs in educational settings. To construct a set of recommendations for school staff to achieve successful implementation of a therapy dog program, the present study investigated the perceived facilitative and impeding factors when implementing a therapy dog program. A total of 13 school staff and 2 coordinators from therapy dog organisations took part in an open-ended online survey and/or a semi-structured interview over the phone, with the aim of gathering their perspectives of implementing a therapy dog program in schools. The thematic analysis of the data indicated facilitative factors such as program flexibility, whole-school support, the need for communication and training for all staff, as well as dog welfare. Successful implementation of therapy dogs in an education setting appear to revolve around (1) flexibility of the dog therapy program to target school's needs, (2) qualities of program instigator, (3) whole-school support, (4) communication, training and education, (5) considerations for dog's welfare. Key barriers identified included a high workload, lack of guidelines on processes, lack of support from the school community, as well as the need for better understanding of the role of a therapy dog. The results highlighted the importance of a whole-school effort when implementing a therapy dog program, as well as the need for guidelines for assessing school readiness, key factors for consideration, and strategies to overcome challenges associated with program implementation.
Introduction
Therapy dogs and therapy dog organisations.
Therapy dogs in educational settings have gained traction in recent times. Increasingly, dogs have provided therapeutic support in early education settings, primary and secondary schools, as well as university settings to support students' well-being, promote a sense of belonging in school, reduce stress and anxiety, and even facilitate learning ( 1 – 3 ). Across the globe, the incorporation of a therapy dog as part of a school programs and activities such as dog-assisted reading programs, has increased exponentially in prevalence. For example, therapy dog organisations in Australia which conduct dog-assisted reading programs now include Story Dogs which originated in New South Wales, Delta Classroom Canines™ from Victoria, and Special Human Animal Relationships in Education (S.H.A.R.E. Reading Dogs program) from Gold Coast. Story Dogs, for example, presently partners with 247 schools across Australia and works with over 2,100 children each week ( 1 , 4 ).
Several terms describe how dogs provide therapeutic benefit. A therapy dog refers to a dog trained to provide therapeutic benefit mainly through Animal-Assisted Therapy (AAT), Animal-Assisted Intervention (AAI), or Animal-Assisted Education (AAE) ( 2 ). AAI, Animal Assisted Interventions, is an umbrella term that encompasses AAT, AAE, Animal Assisted Activity (AAA) and Animal Assisted Counselling (AAC) ( 5 ). The dog themselves do not provide therapy, but rather how they are engaged and connected with in the program is what may be therapeutic. The authors use the term “therapy dog” to attempt to differentiate between trained dogs for a purpose vs. dogs that have not undertaken training or are not accredited dogs. Therapy dogs are not therapists. Work with a dog may be therapeutic or it may be an activity such coaching or assisted reading where the dog's role is to be present but not necessarily actively engaged.
Therapy dogs are first selected for their temperament and subsequently trained together with their handler, usually by therapy dog organisations, to be calm and obedient such that there are able to provide emotional support, comfort, and companionship to different individuals in various educational, health care, and community settings ( 2 ). In AAT, the therapy dog forms part of a professional therapeutic treatment with a professional to deliver a specialised expertise and practise based on the professional's profession ( 2 ). For example, assisting a psychologist to provide regular, structured, and tailored intervention for a client with mental health concerns. In AAA, the relationship is more casual and typically designed to achieve broader goals and handled by volunteers who may not have specific professional training to provide interventions ( 6 , 7 ). An example of a therapy dog being involved in AAI is providing general comfort and companionship to patients at a hospital or to students at a university before an examination. Lastly in AAE, the therapy dog is in an educational setting to facilitate in the learning and education of students, for example, through dog-assisted reading programs. Therapy dogs are distinctively different from service or guide dogs, with the latter trained for the purpose of meeting the specific needs of one individual in the long term. For example, a service dog assisting a child with epilepsy is specifically trained to identify signs of a seizure, or a guide dog supporting an individual who is visually impaired to be independent in daily functioning.
Impact of Therapy Dogs on Children's Well-Being and Learning
There is preliminary evidence which suggests that therapy dogs can enhance children's well-being in a variety of settings from schools, hospitals, airports, and courtrooms. Therapy dogs have been found to reduce physiological symptoms of stress through lowering cortisol levels ( 8 ), increasing positive emotions ( 1 , 9 – 13 ), promoting engagement in learning activities and positive attitudes toward learning ( 6 , 11 , 14 , 15 ), reducing negative behaviours like task avoidance and aggression in the classroom ( 16 – 19 ), as well as encouraging prosocial behaviours and acting as a “social catalyst” to facilitate social interactions with others ( 16 – 18 , 20 , 21 ).
In addition, there is evidence indicating an association between well-being and learning outcomes ( 22 – 25 ). Children with higher levels of well-being learn more effectively, have lower levels of absenteeism at school, better academic engagement, and also have more satisfying and successful peer relationships ( 24 , 25 ). There is also an association between children's well-being and reading outcomes ( 22 , 23 ). Research on therapy dogs involved in facilitating well-being and learning outcomes such as reading through dog-assisted reading programs have found some promising results, although there are methodological limitations in some studies. For example, challenges in associating improvements to the therapy dog vs. other factors such as the program or person implementing the program. Despite these limitations, a systematic literature review by Hall et al. ( 26 ) found that dog-assisted reading programs generally show promising results such as gains in reading skills (e.g., reading accuracy, oral reading fluency, comprehension), as well as more positive attitudes and improved behaviours toward reading. While further research is warranted, researchers have proposed that participation in a therapy dog program like dog-assisted programs can lead to improvements in emotional and behavioural processes (e.g., reduced anxiety, increased self-esteem, enhanced motivation and hence, overall well-being), which in turn can facilitate learning and contribute to gains in learning outcomes like reading ( 26 ).
Concerns, Risks, and Objections
Despite the potential benefits of a therapy dog program, there are several concerns and challenges which might arise from successfully introducing a therapy dog into a school context. Primary concerns by schools include legal implications and liability, allergy concerns, hygiene and sanitation concerns, safety concerns, cultural differences, fear of dogs, animal welfare, funding associated with animal maintenance and program implementation, as well as a lack of administrative support ( 2 , 27 – 32 ).
The most common objection for introducing a therapy dog into a school setting is sanitation concerns. There is a common perception that dogs can be potential carriers of diseases and infections which can then be transmitted to human beings ( 30 ). Allergies due to animal dander, the most common source of allergic reactions, as well as safety concerns around dog bites in children and perceptions of dogs being fierce, aggressive, or protective in nature, are also major deterrents to approving the incorporation of a therapy dog in schools ( 28 , 30 ). Some cultures also regard dogs as unsanitary ( 28 , 30 ). In addition, there are ethical issues surrounding animal welfare such as ensuring that the therapy dog's needs are met in the school setting, is safe, and is not overworked ( 33 ).
Another barrier to implementing therapy dogs and programs into schools is funding as well as a lack of administrative and staff support. There are substantial costs involving a therapy dog. In addition to the usual costs associated with owning a dog, the costs associated with annual veterinary check-ups, vaccinations, as well as therapy dog training can be quite substantial ( 32 ). Most therapy dog work is voluntary ( 32 ). In school settings, it is usually the school counsellor, psychologist, teacher or principal who acts as both the owner and handler of the school's therapy dog ( 32 ). The handler usually takes on additional duties associated with the therapy dog on top of their usual duties. It has been found that a high staff workload is a negative factor of therapy dog program implementation across multiple settings ( 34 , 35 ). Often, the handler is responsible to feed, water, walk, groom, and care for the dog, in addition to planning and running all aspects of the therapy dog program independently ( 36 ). A lack of knowledge as well as resistance amongst other staff due to various reasons during the phases of therapy dog planning and implementation is also another challenge which handlers need to navigate. Overall, staff burnout, staffing and workload concerns, as well as staff attitudes toward a therapy dog program are key factors which require consideration before implementing a therapy dog program as they can have a significant negative effect on the uptake of therapy dog programs into multiple facilities ( 34 , 37 ). The preceding objections and concerns thus need to be addressed in future research and recognised as barriers to implementing programs in schools, in an effort for children to reap the potential benefits therapy dogs have to offer.
Implementation Science in Educational Settings
Implementation science promotes research findings in healthcare, community and policy contexts ( 38 ). It seeks to bridge the gap between research findings and applying those findings in real-world settings in a way that optimises positive outcomes ( 38 ). Implementation is not a single event but a process. To understand how successful a given implementation process is working, several factors including the acceptability of the program, appropriateness, adoption, feasibility, fidelity, implementation cost, coverage and sustainability need to be considered ( 39 , 40 ).
A scoping review of program implementation in the education setting identified several key factors for consideration when implementing a program ( 39 ). They found that implementation fidelity—the degree to which the intervention has been implemented as intended by its developers—was the most acknowledged and measured outcome for successful implementation of programs in education settings. Training and ongoing support for all stakeholders and participants through the provision of single or multiple days of workshop activities, as well as the provision of additional resources (e.g., support from experts, virtual technology) was also seen as a dominant strategy ( 39 ).
In addition, support for front-line staff was paramount for implementation success as educators often struggle when trying to apply the new practises in the classroom ( 39 ). Support provided through continuous feedback, supervision, coaching, and practise observation is critical in achieving successful implementation ( 41 – 47 ). Past research has also indicated the importance of leadership for the successful uptake of interventions into multiple settings ( 48 – 50 ). Aarons et al. ( 48 ) highlighted qualities such as creating a vision for the uptake of evidence-based interventions in the school or educational system, engaging faculty and other staff in this vision and its realisation, as well as being a role model in realising the vision. Displaying these leadership qualities have been found to provide front-line staff with clear expectations ( 39 ).
Guidelines and Regulations for Program Implementation
Given the concerns and challenges associated with implementing a therapy dog program in schools, as well as the various factors for consideration when implementing any new practise, it is critical that schools have guidelines on key considerations and processes to help them navigate this implementation process. There are currently few resources available for accessing guidelines, procedures and standards for implementing a therapy dog program into various settings and populations ( 51 – 54 ). For example, Fine ( 52 ) created guidelines and best practises for using dogs as therapeutic companions with multiple populations, including children, in therapeutic settings. He also included animal selection criteria, animal welfare, training and certification procedures, as well as ways to introduce a therapy dog to clients ( 52 ). The Delta Society's Pet Partner Program and Delta Society's ( 51 ) Standards of Practise for Animal- Assisted Activities and Therapy also provides guidance in administrative structure, standards of practise, personnel credentials, vocational profiles, treatment plan development, documentation, sample forms, and a bibliography ( 53 ). In addition, there are a number of guidelines in other settings such as healthcare facilities ( 15 , 54 – 57 ). Despite the wealth of information provided in the above guidelines, there are however no specific and evidence based guidelines on implementing a therapy dog program into a school setting (to the best of the authors knowledge). In addition, guides created by Departments of Education tend to focus on animals for teaching (e.g., science lessons), or assistance animals (e.g., guide dogs), or visiting animals with brief information emphasising the importance of animal welfare, safety, hygiene, and sanitation procedures when interacting with animals in other contexts (e.g., school excursions, classroom pets) rather than extensive guidelines and recommendations for therapy dog program implementation.
The Present Study
While therapy dog programs have increasingly been incorporated in many school settings, research exploring the specific concerns and challenges associated with implementation in schools are needed. Moreover, guidelines, policies and existing research into therapy dog programs is lacking. The current study examined the following three research questions:
- What are the facilitative factors associated with implementing a therapy dog program in schools?
- What are the perceived challenges and barriers with implementing a therapy dog program in schools?
- What support is required when implementing a therapy dog program in schools?
The results of the study informed a set of research-informed recommendations and guidelines outlining key factors for consideration when implementing a therapy dog program in school settings.
Research Design
A qualitative research design was employed using open-ended questionnaires in form of an online survey and/or semi-structured interviews completed over the phone.
Participants
Data was drawn from two participant groups: (i) schools with an existing therapy dog program, (ii) schools considering implementing a therapy dog program, and (iii) therapy dog organisations. All participants were recruited via email and snowballing. Recruitment for this study began with schools which approached the principal researchers to express their interest in implementing a therapy dog program in their school. Further snowball sampling and comprehensive investigation online were conducted to identify participants in all three groups who were emailed to seek their interest in taking part in the study.
Qualitative Interviews
Rapport building techniques were used, and a natural conversational tone was maintained by showing empathy, and using active listening skills (Irwin and Johnson, 2005). Probing questions gave school staff the opportunity to elaborate more than others depending on how much information they wished to share. For example, in one interview a participant stated they felt they were “flying-solo,” and the researcher followed with “What do you mean by flying-solo? Can you give me some more information on that experience?” The questionnaire questions (see Appendices A, D ) were used as a basis for the semi-structured interviews. All interviews were audio recorded and transcribed with the participants' consent. Participants were labelled by an assigned number (for the purpose of differentiating between participants and to have a chronological record of data collection) as well as their participation method (interview or survey) to maintain confidentiality.
Participants group 1 and 2 consisted of educational staff working in a school setting which included teachers, assistant principals, principals, junior heads of schools, coordinators of early learning centres, school psychologists as heads of well-being and specialist student empowerment teams. Participants were from primary schools, combined primary and secondary schools, and early learning centres in Australia. In total, thirteen school staff across three states in Australia (Victoria, New South Wales and Australian Capital Territory) took part in the study. Participant group 1 consisted of schools with an existing therapy dog program ( N = 9, 1 male and 8 females) and participant group 2 consisted of schools considering the implementation of a therapy dog program ( N = 4, 1 male and 3 females).
Therapy Dog Organisations
Participant group 3 consisted of staff from two therapy dog organisations, Story Dogs and Delta Therapy Dogs – both non-profit organisations which implement dog-assisted reading programs in schools across Australia. Participants were staff in managerial and coordinator roles ( N = 2, 2 females). The Story Dogs program is implemented mainly individually where a child reads one-on-one to a dog and handler team for ~20 min every week over at least two school terms. Dog and handlers may also be involved at whole of school assemblies on special occasions such as book week one or twice annually ( 1 ). Similarly, for Delta Therapy Dogs, the dog-assisted reading program takes place mainly individually or in small groups where the child or group of children read to a dog and handler team.
The demographic information of all participants is outlined in Table 1 .
Summary of demographic information for participants.
A mix of online surveys and semi-structured interviews were conducted with school participants (participant groups 1 and 2). Participants from therapy dog organisations (participant group 3) only completed the online survey. Both methods of data collection—the online survey and semi-structured interviews—involved similar questions. Three separate online surveys were constructed for (i) participants from schools considering a therapy dog program, (ii) participants from schools with an existing therapy dog program, and (iii) participants from therapy dog organisations. The Hexagon Tool developed by the National Implementation Research Network ( 58 ) was used to guide the construction of the open-ended surveys. The Hexagon Tool is designed for communities and organisations in any field to evaluate new and existing programs and practises to determine a program's fit within a given context ( 58 ). A sample question from the questionnaire for participant group 1 is “Are there any negative outcomes associated with having a therapy dog program in the school? If yes, what are they?” A sample question from the questionnaire for participant group 2 is “What are your main concerns and/or challenges about implementing a therapy dog program in your school?” A sample question from the questionnaire for participant group 3 is “How are concerns/challenges raised by schools addressed?”
Ethics was approved for the present study by the relevant University Human Research Ethics Committee as well as the Department of Education and Training. Participants who agreed to participate in the study via signed consent forms completed the online survey and/or indicated their interest to participate in a semi-structured interview. The online survey took around 15–30 min, while the semi-structured interviews conducted over the phone varied between 20 and 90 min.
Qualitative Methodology
The online surveys and semi-structured interviews identified participants views of therapy dog program implementation, perceived facilitative factors as well as barriers in school based setting. Thematic analysis was used to analyse all qualitative data using the framework by Clarke and Braun ( 59 ), as summarised in Table 2 . Overarching themes were identified in response to the three research questions. Inter-rater reliability was established through discussions with another researcher in the research team where sections of the transcribed interviews and surveys were analysed. Both researchers discussed and reviewed the transcripts and themes together whereby 2 themes that were not in agreement and omitted as the suggested themes did not represent the quotes. The researchers drew similar conclusions to the data on all other themes and identified similar themes for the sections of transcripts and surveys. Please see Table 3 which provides an overview of the common concerns and challenges of therapy dogs in educational settings and also strategies to manage and address them.
Braun and Clarke's ( 60 ) six-phase framework for thematic analysis.
Common concerns/challenges and strategies to manage/address them.
Facilitative Factors
Results gathered from participant groups 1 and 3 indicated that the perceived facilitative factors to successful implementation of a therapy dog program in schools were: (1) flexibility of program to meet school's needs, (2) qualities of program instigator, (3) whole-school support, (4) communication, training and education, (5) considerations for dog's welfare.
Flexibility of Program to Meet School's Needs
Schools found that having the therapy dog program evolve flexibly and organically according to the school's needs to be beneficial to staff and students, as well as fostered a sense of belonging. The dogs had the liberty and flexibility to roam free around classrooms at school and this allowed the dog's role to be adaptable to the needs of the students whenever it was required. The therapy dogs were also said to build trust with students, which formed meaningful relationships and fostered a sense of belonging to the school for students. For example interviewee 5 suggested “ I wanted him [the dog, Scruff] to grow up with the kids at the school and I think that's what made it even more special is the kids, like they feel Scruff [the dog] is theirs. We noticed over the five years that kids who struggled to transition to the next year got better because they had a dog at school, they wanted to come to school . They [the students] sort of built up their confidence and realised that Scruff is safe and he's not going to hurt them.” While participant 5 in the survey said: “ The [dog-assisted reading program] is run slightly differently at every school. We are able to adapt to most needs of the school. Such adaptations might be the time of visits.”
Qualities of Program Instigator or Coordinator
The qualities of the school staff who introduced and lead the therapy dog program was identified as critical in facilitating successful program implementation. This included being emotionally aware and considerate of the school community and its diversity, such as cultural sensitivities, differing perceptions of dogs, as well as taking into account the needs of those with allergies. Being cognizant of these differences (e.g., observing children's body language, when interacting with the dog, actively seeking views and feedback), taking into account their different needs (e.g., choosing a dog breed that is hypoallergenic to meet the needs of those who have allergies to dogs), and flexibly adapting the program (e.g., not allowing the dog to roam free for certain classes).
The willingness of the program instigator to take on responsibility and be invested in the program (e.g., committing additional time and attention to set up suitable environments, multitasking classroom duties and being a dog handler), being goal-orientated (e.g., researching on the impact of therapy dogs, having a clear purpose and direction on what outcomes they would like to achieve from the program), as well as being adequately prepared (e.g., ensuring the dog is adequately trained and prepared to enter the school environment) were also factors that were highlighted. Interviewee 7: “ I did research and made sure I read some articles, and made sure we had the right blurp on the website…about the benefits of having a dog, and we made we got the right breed and called a couple of primary schools that had already implemented the therapy dog program. We made sure we had him prepared for school and for children from the beginni ng.”
Whole-School Support
Participants expressed that the program was able to progress and develop with the help of parents and staff cooperation and from the backing of school staff, principal, and school council. The acceptance of the whole school community (e.g., being accepting and enthusiastic during the implementation process) facilitated the introduction of the dog to the school, as well as allowed the program instigator to be more confident in implementing the program. Interviewee 1: “ It's really that sense of community that helps . The parents are on board with the program . I think it would be very tricky to do it if the staff isn't in agreement with it . Being really supported by the school I think is absolutely necessary.” Interviewee 3: “ The whole community has really got around it. The school council was definitely a support…having this you know it just affirms that I had the right idea for the community.”
Communication, Education, and Training
Sharing and discussing key information on the role of a therapy dog, its possible outcomes and benefits, the training both handler and dog undergo, roles and responsibilities of school staff, risk management, as well as building students' knowledge about dogs prior to program implementation helped facilitate acceptance amongst children, parents, and school staff. Therapy dog organisations that conduct dog-assisted reading programs with schools also assign a coordinator to support the school and handlers, provide information packs and an orientation meeting to discuss key information, as well as are in regular contact with schools and handlers to obtain feedback. Interviewee 3: “I've been very specific with the staff on this is what you need to do, this is how you need to approach so I'm constantly trying to refine that interaction and training as I go.” Survey 5: “(We) provide adequate information on our risk minimisation strategies, current insurance held, and emergency procedures… We have a coordinator assigned to support our volunteers. This coordinator organises a school orientation meeting to set up the program in a new school with a new volunteer. This meeting includes the handler and the dog, the coordinator, any teachers involved and the key liaison person for the school. The meeting works out a day, time, and place for the reading sessions. It also introduces the handler and dog to the school.”
Consideration for Dog's Welfare
Ensuring that the therapy dog's needs and welfare are well-met and considered enabled them to thrive in the school setting. This included planning dog-specific and dog-friendly areas in the school, as well as scheduling down time and breaks for the dog. Interviewee 1: “ We are lucky we've got bog green ground. So instead of sitting in a classroom and talking to a child about whatever is going on, we tend to grab the dogs and take them with us for a walk around the oval.”
Challenges and Support Required
The following challenges and concerns were identified (1) flying solo: the workload of the instigator and handler, (2) winging it: lack of regulations, guidelines or research on implementing in schools, (3) community acceptance and buy-in, and (4) laying down foundations and acquiring therapy dog education.
Flying Solo: The Workload of the Instigator and Handler
Most participants were both the therapy dog handlers and instigators of the program. Difficulties faced include time constraints and added workload in addition to being a classroom staff. Participants expressed that while they were dedicated and invested in the program, they struggled with managing the responsibilities alone in the implementation process. Some participants stated that they would have appreciated other staff to be extension handlers or to take on a leadership role to share the workload of program implementation. Interviewee 5: “ I would've liked to do more but being a fulltime teacher, I just was restricted for time…and as it went on, I just got less and less support from staff involved…and the momentum stopped .”
Winging It: Lack of Regulations, Guidelines or Research
Some participants stated that they had trouble finding regulations or guidelines that could facilitate implementation of their program, as well as finding little research or literature on implementing therapy dog programs into educational settings. The lack of regulations and guidelines as resources for school staff attempting to implement a program was one of the main challenges and impeding factors associated with stunted development in the implementation process. School staff expressed that without having any existing policies or guidelines to follow they had to figure out implementation on their own without any support in how to implement a therapy dog program. Interviewee 3: “ It's a bit tricky on the policy side of things because of not having anything already existing for schools, I'm sort of working a little bit from scratch…it's just even trying to understand what it should be.” Survey 2: “ No research to share with community ideas on how to introduce the dog to the community in a positive way.”
Community Acceptance and Buy-In
All participants expressed the need for the whole school community to be open and accepting of the therapy dog program. They stated that without staff support, the process would be extremely difficult. Participants expressed that school staff's and students' resistance and reservations toward the program would be a key barrier. This included barriers like managing personal views about dogs as well as risk management (e.g., allergies). Survey 1: “ The challenges would be people that maybe aren't dog people.” Interviewee 6: “ Staff have said to me, ‘I wouldn't be happy with having a dog at the school… I don't think I would go ahead with a therapy dog unless I had a majority of buy-in from the staff.” Survey 5: “ Increase in occurrence of a student in the school being anaphylactic to dogs, thus the program cannot start.” Managing the rest of the students' expectations was also identified as a challenge. Survey 5: “ Every student wants to read to the dog and the majority of students in school will not get this opportunity.”
Laying Down Foundations and Acquiring Therapy Dog Education
A few participants identified the need for foundational knowledge about the role of the dog in the school as well as how best to involve the dog therapeutically and effectively in school. Interviewee 6: “ I think we would need skills on how to use the dog effectively…so some sort of PD for staff of what the role and function of a therapy dog is, and probably educating staff before even looking at getting a dog, so laying a foundation.”
Recommendation for Therapy Dog Program Implementation
What are some factors for consideration before implementing a therapy dog program.
Based on the qualitative analysis above of both the survey and interview data, as well as the literature the following factors are for consideration before implementing a therapy dog program:
Handler/Therapy Dog Factors
It is critical that the dogs receive appropriate certified training where they are rigorously trained and evaluated to be reliably non-aggressive to both people and other dogs regardless of circumstances, are highly adaptable, and can interact easily with people. During the training, handlers are also trained to meet welfare, safety and hygiene requirements for both the dog and students, and how to connect and engage with the dog therapeutically.
Handlers should be prepared to:
- Be personally and financially responsible for the dog's welfare and maintenance including safety, feeding, grooming, cleaning, and vaccination. In the event where the dog is involved in school programs regularly or in the long term, it is recommended for the handler to request financial support from school since the dog is part of an intervention employed for meeting the students' needs ( 27 ). In such cases, it is important to put the financial plans into a written budget outlining a list of all expenses required in order to deliver the program and share them with all responsible parties ( 29 ).
- Be vigilant in identifying signs and triggers of injury, distress, or exhaustion for their dogs and be able to respond accordingly. Regular breaks should be given to the dog. Suspension of the program may be required if the dog shows a negative behavioural change, fearful behaviour during interactions, or has medical concerns.
- Trouble-shoot when an incident occurs (e.g., when a student has a negative response to a dog), and adopt appropriate measures when needed (e.g., removal of the dog, medical care, debrief with student).
To facilitate successful implementation of therapy dog programs in schools, handlers should also have a good understanding of the impact of therapy dogs and how they may participate in various educational settings. Establishing a clear goal/purpose of the inclusion of a therapy dog in different school activities is essential – e.g., desired outcomes, who might benefit, and how ( 27 , 31 ) (Freeman et al., 2016). This facilitates planning of activities (e.g., frequency and duration of activities, how the dog may be incorporated safely and appropriately, anticipated risks and concerns) as well as the evaluation of outcomes. Handlers are also encouraged to be proactive in researching on the current evidence base about therapy dogs and communicating with others who have had experience implementing such a program ( 29 ).
School Factors
Leadership and whole-school support is essential in successful implementation of a therapy dog program ( 31 ). The following factors on the fit and capacity of the school to undertake a therapy dog program should be considered and discussed prior to implementation:
- ° Briefly explain the idea of involving a therapy dog in school and goals
- ° To obtain initial support
- ° Learn of any dog-related allergies or phobias
- ° Discuss and address any other concerns.
- It is recommended that a comprehensive handbook be constructed to clearly identify and explain the policies and procedures of how the dog will be included in the classroom and school activities ( 27 ).
- Stakeholders are likely to have varied concerns. Buy-in from can be facilitated by preparing information ahead of time (e.g., benefits of therapy dogs, their inclusion in schools), providing opportunities to ask questions, and preparing to respond to any potential concerns ( 56 ). Obtaining buy-in from school leaders ahead of time and presenting collaboratively to school staff is recommended ( 27 )
- Presence of 1 or 2 other school staff who can be involved in the therapy dog program to ensure that the handler is not the sole person managing the program. This is to ensure that the work load of undertaking a therapy dog program is balanced vis-à-vis other responsibilities the handler is fronting, collaborative planning and problem-solving of programs, and implementation of effective emergency protocols if more than one person is required (e.g., handler managing the dog, other school staff who may need to contact parents or debrief with a student).
- Logistical considerations such as appropriate indoor and outdoor areas for the dog and scheduling of activities and breaks for the dog
- School-wide protocols to address any sanitation or safety concerns, which would require training school staff and students on appropriate ways to interact with the dog and the training of emergency protocols (e.g., in the event of dog scratch or bite, students' adverse reactions).
- Communication plans for engaging parents and students about the program, addressing concerns (e.g., cultural differences, fear of dogs, allergies or medical concerns), as well as obtaining consent and assent.
- Possible funding (e.g., grooming and vaccination expenses, materials required)
- Adequate planning and preparation for introducing the therapy dog to school staff so that they are educated on appropriate animal care and behavioural expectations, and are able to step in when necessary in times of emergencies (e.g., negative dog reactions in students, emergency protocols).
Student Factors
Assessing the needs and suitability of students whom the dog might be working with is critical in ensuring that the therapy dog program goals are met, and student welfare is considered. This includes:
- Determining which students/classes are to participate in the therapy dog program – e.g., which students would benefit the most from this program? how should the program be structured to meet their needs best (e.g., whole-class, in groups, or individually)? How does a therapy dog program value-add to existing programs in meeting the needs of these students?
- Making suitable alternatives for children who are unable to participate (e.g., for cultural or religious reasons, allergies, fear of dogs) ( 29 )
- Deciding how expansive the program will become as it is unsurprising for many other children or families who might wish to participate after learning about the program ( 29 )
- Adequate planning and preparation for introducing the therapy dog to students so that they are educated on appropriate animal care and behavioural expectations.
Parent Factors
As with engaging school staff, early engagement of parents is also essential once there is clear direction that a therapy dog program may be introduced in school. Common concerns parents have include safety, hygiene, and allergic concerns ( 29 ), how the dog will be incorporated in learning activities ( 27 ), as well as cultural differences ( 28 ). Parents must be informed of procedures and processes, be given the opportunity to ask questions and voice concerns, and provide written consent signifying they understand and support the dog's inclusion ( 27 ).
Schools are advised to ensure that there is ample time to engage parents before the commencement of a therapy dog program. This includes parents who have provided consent to their child's participation and providing further information about the program and addressing concerns, parents who do not consent and need further information on how their children will be engaged in alternative ways, as well as parents of children who are not selected to participate in the program but wish to do so ( 29 ).
The findings from this study highlight insights into implementing a therapy dog program in school settings, particularly a whole-school effort in optimising the program to meet unique school needs, garnering support, as well as overcoming systemic barriers. This includes ensuring the flexibility of the therapy dog program to meet varying student needs, dedication and commitment of therapy dog program coordinators/handlers, acceptance and training of all of the school staff, support from school leadership, as well as adopting a team-based rather than individual-effort in program planning and implementation.
The findings on the importance of a whole-school approach are congruent with past research. Programs are more likely to excel when they are aimed to involve the whole-school community. Research indicates that positive program outcomes are facilitated when interventions are integrated into daily practise, the school culture and encourage collaborative efforts to include staff, families, teachers, and children ( 61 , 62 ). With students, this manifested as a sense of trust and connexion between the therapy dog and the school community. School staff placed importance on building foundations of trust and connexion with the students at the initial phases of implementation, as they first introduced the dog and their program to the school. With these foundations in place, the programs ran successfully and with ease, students reaped the most benefits when they formed a relationship with the dog and thus helped them connect more to the school community and have a stronger sense of belonging. A sense of belonging is also a strong indicator of a successful therapy dog program to promote well-being, which is congruent with the literature ( 63 – 65 ).
Another important feature is the support from leaders and a team-based approach in program implementation. Findings from this study indicated that it was mostly a single individual or program instigator/coordinator, often the dog handler and also school staff, who was solely responsible for the various stages of the program implementation, which contributed to heavy workload and potentially negative implications on the sustainability of the program. One of the key facilitative factors reported was for program instigators or coordinators to be willing to take on the diverse roles and responsibilities for successful program implementation, including acting as a promoter ( 66 ), as well as being emotionally aware and showing strong interpersonal skills as leaders of the program ( 67 ). All of which have been found to contribute to program success ( 39 , 40 ). However, it appears that this has also been reported as a barrier in this study due to the high workload of these staff. Instead, taking a team-based approach and understanding that there will be a need for “multiple actors” in the implementation process is critical ( 39 , 40 ).
A team-based approach to program implementation includes the support from school leaders as well as acceptance and buy-in of other school staff. Strong leadership was indicated as a strong focus for successful therapy dog program implementation, and this is also shown to be a measure of general program implementation success. Findings implied school staff needed to be prepared and goal-orientated for their program to be successful and for student reap the most benefits to their well-being. Moreover, school staff had to maintain throughout implementation a vision and a purpose, engage the whole community and constantly meeting their aims and outcomes of the program. This is congruent with the literature detailing the importance of these leadership qualities to be a role model for other staff and will provide these front-line staff with clear expectations for the program ( 39 , 48 – 50 ).
Another key feature for successful implementation is having a strong support network from the school community, including staff, parents, principal, school council and students. School staff expressed that having the community's support and alignment of goals and purposes made introducing the program to their school easier and with fewer complications. This is congruent with the research on implementation programs requiring empowerment, participation and education of the community, and lastly, multiple actors in implementation process (obtain broad-based support of school staff) ( 39 , 40 ).
A major factor that caused difficulties for school staff who had experienced implementation of a program was a lack of guidelines and regulations available for schools. The findings imply that for future practise, there needs to be further research in regulations and guidelines into therapy dog programs for schools and government support to provide policies and guidelines for schools to follow. This highlights the gap in the literature surrounding guidelines on implementation and regulations of having a therapy dog at a school. Moreover, these finding align with research on necessary implementation strategies such as government support, policy documents ( 68 ), oversight and possible regulations ( 39 , 40 ).
Acknowledging the limitations of the findings of this evaluation is important. The study was small, and only the perspectives of selected school staff and therapy dog coordinators were gathered. As most of the school staff and coordinators interviewed were leaders and initiators of the therapy dog program, their feedback might be slightly biased as they had an invested interest in seeing their program be successful. As a qualitative project, the aim of data collection was not to achieve a statistically representative sample. Instead it is to attain what Glaser and Strauss call “saturation of themes” of data collection until no new themes are generated. Samples sizes have been chosen based on my extensive experience with qualitative projects of this kind ( 69 ).
Obtaining information from other school staff who may not be directly involved in the program, students, as well as parents would be beneficial to gather a more holistic understanding of having a therapy dog program in school. In addition, each school is likely to have implemented their therapy dog program in different ways (e.g., number of days the dog was in the school, how students interacted with the dog specifically); this information was not gathered in this study. Given different schools also ran their programs in different manners, potentially impacting program outcomes. It is unclear if the structure of the therapy dog program in each context could have also affected the findings. A potential limitation may be geographic/regional applicability of this study. Additional, survey participants may not have had an interactive, back-and-forth opportunity to clarify information as much as interviewees may have had in a semi-structured interview, it is unclear how this may have affected data collection. Nonetheless, this study albeit small and limited, has laid the groundwork for further research in this field.
The overall findings from this evaluation highlight the facilitative factors and challenges, as well as key considerations when implementing a therapy dog program in schools, particularly the need to adopt a whole-school approach and involving multiple relevant stakeholders (e.g., handler, school leaders, school staff, students, parents) in the process. Successful implementation of therapy dogs in an education setting appear to revolve around (1) flexibility of the dog therapy program to target school's needs, (2) qualities of program instigator, (3) whole-school support, (4) communication, training and education, (5) considerations for dog's welfare. The results have also underscored the need for guidelines for schools to assess their readiness/feasibility of such a program, key factors for consideration, roles and responsibilities of key stakeholders, as well as strategies to manage challenges.
Data Availability Statement
Ethics statement.
The studies involving human participants were reviewed and approved by Monash University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding. This research was funded by the Monash Education early years and inclusive education and educational psychology academic research community.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fvets.2021.655104/full#supplementary-material
Increasing participation in research with therapy dogs: A qualitative study at a large urban mental health and addiction hospital
Affiliations.
- 1 Office of Education, Centre for Addiction and Mental Health, Toronto, Ontario, Canada.
- 2 Geriatric Mental Health Services, Centre for Addiction and Mental Health, Toronto, Ontario, Canada.
- 3 Complex Care & Recovery Program, Centre for Addiction and Mental Health, Toronto, Ontario, Canada.
- 4 Volunteer Services, Centre for Addiction and Mental Health, Toronto, Ontario, Canada.
- 5 Departments of Psychiatry and Family and Community Medicine, University of Toronto, Toronto, Ontario, Canada.
- 6 Wilson Centre, University Health Network and Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada.
- PMID: 32853258
- PMCID: PMC7451510
- DOI: 10.1371/journal.pone.0238096
The benefits of involving patients as partners in research across diverse medical and psychiatric settings are well established in the literature. However, researchers continue to struggle to access, engage and retain participants from hard-to-reach populations. The main objective of this study was to co-create pet therapy activities with patients admitted for serious and complex mental illness to a large urban mental health and addiction hospital. Informed by the principles of participatory action research methodology, we conducted focus group discussions with 38 inpatients in seven different clinical units. An experienced volunteer handler and a certified therapy dog helped facilitate our discussions. Participating researchers, recreational therapists, volunteer handlers and our participants all reported that the presence of a certified therapy dog at each of our discussions was integral to their success. Certified therapy dogs increased the motivation to participate in our study, helped to build rapport with participants and created connections in our discussions that enriched our data. To our knowledge our study is the first to demonstrate the value of using a therapy dog as a participatory research tool in a healthcare setting. The authors believe that therapy dogs are a low-tech intervention that could be used effectively to engage hard-to-reach populations in research about their treatment and care in a diverse range of medical settings. These findings support the creation of a pilot study to test the value of including therapy dogs in patient-centered research with vulnerable and hard-to-reach populations.
Publication types
- Research Support, Non-U.S. Gov't
- Animal Assisted Therapy / statistics & numerical data*
- Cities / statistics & numerical data*
- Hospitals / statistics & numerical data*
- Mental Health / statistics & numerical data*
- Patient Acceptance of Health Care / psychology
- Patient Acceptance of Health Care / statistics & numerical data*
- Pilot Projects
- Qualitative Research
- Substance-Related Disorders / therapy*
Grants and funding

Therapy dogs can help reduce student stress, anxiety and improve school attendance
Educational Psychologist and Lecturer, Monash University
Senior Lecturer, Monash University
Disclosure statement
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
Monash University provides funding as a founding partner of The Conversation AU.
View all partners
In the wake of the schools shootings in Florida , therapy dogs have been used as a way to provide comfort and support for students returning to school. Research has shown therapy dogs can reduce stress and provide a sense of connection in difficult situations.
Given the impact therapy dogs can have on student well-being, schools and universities are increasingly adopting therapy dog programs as an inexpensive way of providing social and emotional support for students.
Read more: Police in schools: helpful or harmful? It depends on the model
What are therapy dogs?
It’s important to note therapy dogs are not service dogs. A service dog is an assistance dog that focuses on its owner to the exclusion of all else. Service dogs are trained to provide specific support for individuals with disabilities such as visual or hearing difficulties, seizure disorders, mobility challenges, and/or diabetes.
The role of therapy dogs is to react and respond to people and their environment, under the guidance and direction of their owner. For example, an individual might be encouraged to gently pat or talk to a dog to teach sensitive touch and help them be calm.

Therapy dogs can also be used as part of animal assisted therapy . This aims to improve a person’s social, cognitive and emotional functioning. A health care professional who uses a therapy dog in treatment may be viewed as less threatening , potentially increasing the connection between the client and professional.
There are also animal-assisted activities , which is an umbrella term covering many different ways animals can be used to help humans. One example is to facilitate emotional or physical mental health and wellbeing through pet therapy or the presence of therapy dogs. These activities aren’t necessarily overseen by a professional, nor are they specific psychological interventions.
Read more: More children are starting school depressed and anxious – without help, it will only get worse
Research suggests using therapy dogs in response to traumatic events can help reduce symptoms of depression, post traumatic stress disorder and anxiety.
So, what can happen psychologically for people using therapy dogs?
The human-animal bond
The human-animal bond can impact people and animals in positive ways. Research shows therapy dogs can reduce stress physiologically (cortisol levels) and increase attachment responses that trigger oxytocin – a hormone that increases trust in humans .
Dogs also react positively to animal-assisted activities. In response to the human-animal bond, dogs produce oxytocin and decrease their cortisol levels when connecting with their owner. Often dogs feel the same when engaging in animal assisted activities as if they were at home, depending on the environmental context.
Benefits of therapy dogs
Animal assisted therapy can:
teach empathy and appropriate interpersonal skills
help individuals develop social skills
be soothing and the presence of animals can more quickly build rapport between the professional and client , and
improve individual’s skills to pick up social cues imperative to human relationships. Professionals can process that information and use it to help clients see how their behaviour affects others .
More recently, therapy dogs are being used as a form of engagement with students at school and university.
Benefits of therapy dogs at school

A recent report highlighted children working with therapy dogs experienced increased motivation for learning, resulting in improved outcomes.
Therapy dogs are being used to support children with social and emotional learning needs, which in turn can assist with literacy development .
Research into the effects of therapy dogs in schools is showing a range of benefits including:
increase in school attendance
gains in confidence
decreases in learner anxiety behaviours resulting in improved learning outcomes, such as increases in reading and writing levels
positive changes towards learning and improved motivation , and
enhanced relationships with peers and teachers due to experiencing trust and unconditional love from a therapy dog. This in turn helps students learn how to express their feelings and enter into more trusting relationships.
Despite these known benefits, many schools choose not to have therapy dog programs due to perceived risks . These range from concerns about sanitation issues to the suitability of dog temperament when working with children. But therapy dogs and owners are carefully selected and put through a strict testing regime prior to acceptance into any program .
The main reason for the lack of take up has been linked to the limited research into the benefits of therapy dogs in schools.
Benefits of therapy dogs at university
Researchers have found university students reported significantly less stress and anxiety , and increased happiness and energy, immediately following spending time in a drop-in session with a dog present, when compared to a control group of students who didn’t spend any time with a therapy dog.
Read more: Hugs, drugs and choices: helping traumatised animals
Generally, therapy dog programs rely on volunteer organisations. One example is Story Dogs , who currently have 323 volunteer dog teams in 185 schools across NSW, Queensland, Victoria, Tasmania, SA, WA, and ACT. In total, they help 1,615 children each week.
Research into these programs is needed to help further understand the impacts of therapy dogs, especially on student learning and academic outcomes. Lack of funding is setting this research back. University partnerships are one solution to address this.
- Post-traumatic stress disorder (PTSD)
- student welfare
- Florida shooting
- therapy animals
- therapy dogs
- school stress

Lecturer / Senior Lecturer - Marketing

Content Coordinator

Assistant Editor - 1 year cadetship

Executive Dean, Faculty of Health

Lecturer/Senior Lecturer, Earth System Science (School of Science)
Just 10 minutes with a therapy dog may have profound health benefits — study
New research pinpoints the benefits of therapy dogs for alleviating pain, anxiety, and depression.

For decades , doctors have informally deployed therapy dogs — canines that are trained to provide emotional support to people in hospitals, care homes, and other settings — as part of their patients’ health plans. But despite their longstanding clinical use, there’s been little evidence to show they actually work, until now.
Compared to significant research on the health benefits of dog ownership, there are very few controlled trials on the health outcomes of therapy dogs. A group of Canadian researchers recently set out to bridge this gap. Their work, which was published Wednesday in the journal PLOS One, reveals a small, but significant link between therapy dogs and improved mental health in emergency room patients.
“This is the first controlled trial of its kind that our team knows of in Canada,” Colleen Dell , a co-author on the study and an associate at the University of Saskatchewan’s School of Public Health, tells Inverse .
What’s new — The researchers found that spending just ten minutes with therapy dogs improved hospital patients’ overall well-being. Compared to patients who hadn’t spent time with therapy dogs, those who did reported significantly lower levels of anxiety and depression following the visit.
Patients who experienced the therapy dog visits also reported increased well-being compared to those who did not, as well as significantly lower pain ratings.
“These findings suggest that the therapy dog intervention had a positive effect on reducing participant pain,” the researchers write.
This study “offers a clearer understanding of the potential value of therapy dogs in the emergency department,” Dell says.

Doctors have utilized therapy dogs informally for years, but there have been few clinical trials conducted on the health benefits of these visits.
Why it matters — Patients commonly visit the emergency room to manage pain, and mental health concerns like anxiety often make the pain worse.
“People attend the Emergency Department primarily for pain, and associated anxiety can make it worse because of environmental stressors, such as bright lights and long wait times,” Dell says.
Therefore, understanding how one method of care — therapy dogs — impacts pain and mental health will be enormously valuable in improving patients’ well-being in these situations.
“Interacting with a therapy dog can make the ER visit a little calmer and help the patient and family realize that all the members of the ER staff are there to help and support them,” James Stempien , a co-author on the study and the provisional head of emergency medicine at the University of Saskatchewan in Canada, tells Inverse .
There’s also a timely reason for this study, the paper notes. As concern over the mounting opioid epidemic grows, clinicians are seeking alternative pain relief methods for their patients.
“There is a prior study that found involving therapy dogs in patient care plans following joint replacement surgery improved patient pain scores,” Dell says.
Another study found that the distraction therapy dogs provided did not reduce the patients’ source of pain but it did affect their perception of pain according to Dell. In a sense, doctors have been informally “ prescribing” people’s own pets to help them with depression and chronic pain, Dell explains.
“Many hospitals, care homes, jails, university campuses...are constantly asking that therapy dogs attend because they can assist people in numerous ways,” Dell says.
But Dell also stresses we need more research before therapy dogs can serve as a catch-all treatment for pain in emergency departments or other settings. After all, dogs are also “sentient beings” and not medications we can simply dole out, Dell says.

Therapy dogs can help ease pain and reduce anxiety for emergency department patients, the study finds.
How they made the discovery — Researchers recruited hundreds of patients at the Royal University Hospital Emergency Department to participate in their trial; the hospital has a longstanding therapy dog program.
Ultimately, 97 patients were selected to receive therapy dog visits, while 101 patients participated in the control group that did not receive such therapy. Researchers measured the patients’ pain severity, anxiety, depression, and general well-being on a rating scale according to the Edmonton Symptom Assessment System. Higher ratings indicated worse patient outcomes.
On average, therapy dogs spent ten minutes with each patient. The researchers conducted follow-up visits and used a quantitative data analysis program to determine the differences in patients’ scores before and after therapy dog visits. Finally, researchers also reviewed any pain medications patients were taking to ensure they were accurately measuring the effects of the therapy dogs and not other factors.
What’s next — While these findings are significant, the researchers are also quick to point out there are considerable limitations in their study. For one thing, the sample size of participants is small.
The researchers write that “a larger sample would be needed to examine the interaction of multiple key demographic independent variables,” such as the therapy dog’s experience levels and patient backgrounds such as ethnicity or age.
Other factors, like the potential impact of the dogs’ human handlers on therapeutic benefits, will require further study in future research to “even more precisely isolate what is happening for the patient,” Dell says.
For now, though, the new work provides tangible proof of a treatment for pain that doctors and patients have long known works.
This article was originally published on March 13, 2022
- Research article
- Open access
- Published: 06 September 2019
Effectiveness of the dog therapy for patients with dementia - a systematic review
- Blanka Klimova 1 ,
- Josef Toman 1 &
- Kamil Kuca ORCID: orcid.org/0000-0001-9664-1109 2 , 3
BMC Psychiatry volume 19 , Article number: 276 ( 2019 ) Cite this article
36k Accesses
28 Citations
64 Altmetric
Metrics details
Dementia represents a mental and economic burden for both patients and their caregivers. Therefore, the aim of this study is to explore the effectiveness of animal assisted therapy (AAT) with special focus on canis therapy among people with dementia, specifically Alzheimer’s disease.
The key method of this review study is a systematic review of the research studies detected in the Web of Science, Scopus and PubMed. The search was conducted for the studies dating from 2016 till 31 August 2018 because several review studies were published before. Eventually, only six studies were involved into the final analysis.
The findings of this review, based on significant effect sizes, reveal that AAT may work as a beneficial and effective complementary treatment, especially in the area of behavioral and psychological symptoms, for patients with different degree of dementia severity if AAT is targeted at their specific needs and interests.
Conclusions
More research in the area of methodology for the implementation of AAT is necessary, and more research should be conducted with respect to the use of AAT for the improvement of cognitive functions in people with dementia.
Peer Review reports
Nowadays, the number of people suffering from dementia worldwide, particularly Alzheimer’s disease, reaches about 50 million. It is estimated that every year there occur about 10 million new cases [ 1 ]. Dementia is a neurodegenerative syndrome, which causes deterioration of cognitive functions, especially thinking, orientation, memory, or communication. The cognitive impairment is usually accompanied with other symptoms such as behavioral disorders, difficulties in walking, sleeping, or sexual problems [ 2 ].
Dementia results from different diseases, for example, strokes, malnutrition, or brain tumors [ 3 ]. Alzheimer’s disease (AD) seems to be the most common form of dementia and contributes to 70% of dementia cases. The other most frequent types of dementia are vascular dementia, dementia with Lewy bodies, Parkinson’s disease dementia, frontotemporal dementia/ degeneration, and mixed dementia [ 4 ]. Dementia usually starts to affect people at the age of 60+ years. But, for example, frontotemporal dementia occurs as early as at the age of 45 [ 5 ]. At present, dementia symptoms cannot be cured and inevitably lead to patient’s disability and eventually, to his/her death. Depression and cognitive decline especially result in patient’s mortality among the elderly people with dementia [ 6 , 7 ]. Adequate medications can for some time postpone this process. Nevertheless, the symptoms of dementia steadily deteriorate and the patient cannot look after himself/ herself. S/he has to rely on somebody else in this respect, most often on his/her family member. For instance, in the year of 2016, about 16 million of informal carers delivered 18 billion hours of care [ 8 ]. This care inevitably impacts these informal carers, especially physically, emotionally, but also financially since they usually must quit their job to take care of their loved ones [ 9 ]. Therefore, dementia significantly influences not only patients, but also their carers [ 10 ]. For this reason, scientists worldwide are seeking non-pharmacological strategies that can enhance or maintain cognitive functions and psychical symptoms of these people in order to help them in maintaining quality of their life and reducing the overall economic burden. These alternative approaches are non-invasive, with minimum side effects and definitely less costly [ 11 ]. One such non-pharmacological therapy is animal assisted therapy.
Animal-assisted therapy (AAT) can be defined as a goal directed intervention in which an animal meeting specific criteria is an integral part of the treatment process [ 12 ]. AAT is usually performed by health or human service providers. These are, for instance, registered nurses, nursing assistants, or occupational therapists [ 13 ]. The aim of AAT is to enhance physical, social, emotional, or cognitive functions in both healthy and unhealthy individuals and thus, contribute to the improvement of person’s well-being. AAT can take a form of individual or group interventions [ 12 ].
As research [ 14 ] shows, AAT improves a person’s mental and physical health. In the area of mental health, it releases an automatic relaxation response, reduces the feeling of anxiety, contributes to the lowering of loneliness, or help in the recall of memories. In the area of physical health, AAT helps to reduce blood pressure and improves cardiovascular health, decreases the amount of medications, reduces physical pain, or helps children with autism to get engaged in social interactions. For individuals with dementia, AAT has the following specific benefits:
it contributes to slightly higher physical activity; people can pet the animal, such a dog, or in better cases, they can go for a walk [ 15 , 16 ];
it can relieve the so-called sundown syndrome, which manifests itself in increased agitation, restlessness, disorientation and aggressive behavior [ 15 , 17 ];
it can improve short-term memory and communication skills [ 15 , 18 ];
it enhances eating habits [ 16 ];
it reduces loneliness [ 15 , 17 , 18 ].
In fact, when patients pet or cuddle their animal, their body releases endorphins and other hormones such as oxytocin, prolactin and dopamine. This contributes to the benefits described above [ 19 ]. As Jo [ 19 ] indicates, the most suitable animals for ATT are fish, cats, dogs and horses. Most recently, robots disguised as animals also started to be used in ATT [ 20 ]. They appear to have similar positive effects without the negative aspects of traditional pets such as allergies, infections, or biting [ 21 ]. As Petersen et al. [ 21 ] demonstrated in their study, these animal robots can reduce stress and anxiety in people with dementia and decrease the use of psychoactive medications and pain medications among them.
Although several review studies [ 22 , 23 , 24 , 25 ] had been already published, this review includes the latest studies on this topic, which were not included in these reviews with one exception in [ 25 ]. In addition, this review apart from the effect of canis therapy on the reduction of behavioral symptoms of dementia explores also its effect on the reduction of cognitive symptoms of dementia. In this respect it differs from the latest systematic review by Yakimicki et al. [ 26 ] who did not concentrate on the relationship between the cognitive symptoms of dementia and animal-assisted interventions.
Thus, the purpose of this study is to systematically review evidence from controlled trials, case reports, observational or experimental studies in order to find out the answer to the question whether animal assisted therapy with a special focus on canis therapy among people with dementia is effective in reducing cognitive and behavioral symptoms of dementia.
The authors performed a systematic review of research studies detected in the Web of Science, Scopus and PubMed. The search keywords were as follows: animal assisted therapy AND dementia , animal assisted therapy AND Alzheimer’s disease, canis therapy AND dementia, canis therapy AND Alzheimer’s disease, dog therapy AND dementia, dog therapy AND Alzheimer’s disease . The search was conducted for the studies dated from 2016 till 31 August 2018.
Two (BK and JT) of the authors identified and screened the relevant articles. Altogether 107 articles were detected in the databases mentioned above. Most of the studies were detected in Web of Science (62), followed by Scopus (30), and PubMed (15). After a thorough review of the titles and abstracts (53) and their duplication (22) of the selected studies, 32 studies were screened and after that, 21 studies remained for the full-text analysis.
These full-text articles were then analyzed and evaluated on the basis of the following inclusion and exclusion criteria. The inclusion criteria, based on PICOS guidelines, were as follows:
The articles had to be published between January 1, 2016, and August 31, 2018.
Only English peer-reviewed journal articles were involved.
The subjects had to be patients with dementia.
The intervention had to include a dog therapy.
Only randomized controlled trials, experimental/cross-sectional studies, case reports, or observational studies were involved.
The primary outcome focused on the reduction of dementia symptoms, especially cognitive decline among patients with dementia.
The exclusion criteria were as follows:
Descriptive or review studies on the research topic were excluded from the analysis.
Studies whose subjects were not all patients with dementia were also excluded, e.g. [ 27 ].
Studies which did not focus on dog therapy were not involved either, e.g. [ 21 ].
In addition, a backward search was also performed, i.e., references of detected studies were evaluated for relevant research studies that authors might have missed during their search. In addition, a google search was conducted in order to detect unpublished (grey) literature. After this, another two articles have been identified. Thus, altogether six research articles were eventually analyzed and evaluated.
Two authors (BK and JT) performed an independent quality assessment of these studies. They read the articles to assess eligibility and to determine the quality. The basic quality criteria were adequately described study design, participant characteristics, control conditions, outcome measures, and key findings, with special focus on statistically significant differences (Table 1 ). The authors selected these basic quality criteria using Health Evidence Quality Assessment Tool for review articles [ 31 ].
Figure 1 below then describes the selection procedure of the detected studies.
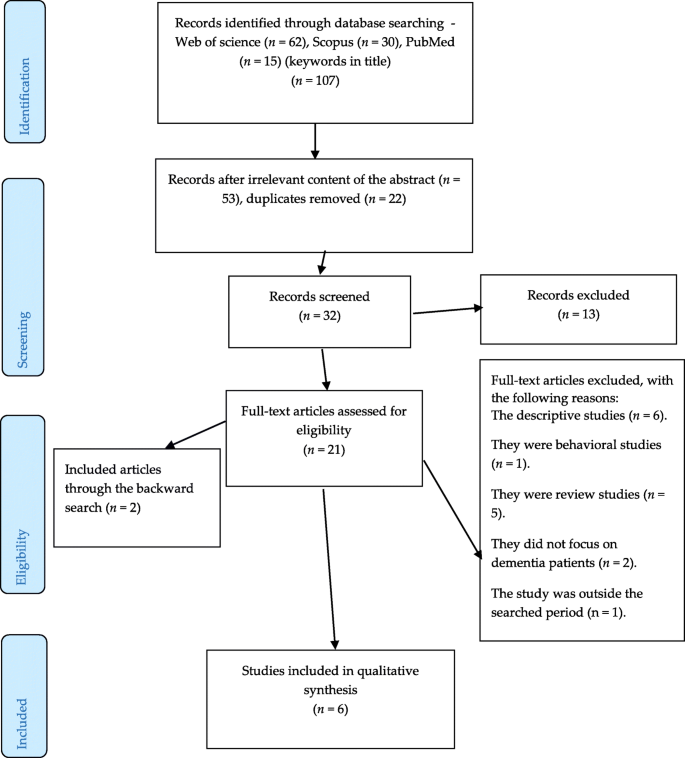
An overview of the selection procedure
Altogether six original studies on the research topic were identified. Three studies were controlled studies [ 28 , 29 , 30 ], two studies were experimental studies [ 17 , 18 ] and one study was an observational study [ 13 ]. As for the country of origin, most of the research in this area has been conducted in Scandinavian countries [ 13 , 17 , 29 , 30 ], followed by Italy [ 28 ] and USA [ 18 ]. The key area of assessment focused on behavioral symptoms of patients with all severity of dementia [ 13 , 18 , 29 , 30 ]. Apart from that, one study [ 28 ] explored cognitive functions and one study [ 17 ] concentrated on physical health and more specifically, on balance. The sample of subjects ranged from 5 to 80 older individuals with the mean age between 75 to 95 years. Not surprisingly, there were more female participants than male participants if taking into account their age. The intervention period lasted from two weeks to six months. All control groups were passive. The main outcome measures comprised standardized tests such as Mini-Mental State Examination, Geriatric Depression Scale, Clinical Dementia Rating, or Quality of Life in Late-stage Dementia. The results of all identified studies indicate that the AAT or AAA therapies with a dog have a positive impact on mental and physical health of the subjects with dementia as the effect sizes show. Based on the basic quality criteria, only the study by Swall et al. [ 13 ] seems to be less reliable quality. The findings of the detected studies are summarized in alphabetical order of their first author in Table 1 below.
As the findings of the studies in Table 1 show, AAT or AAA therapies may be effective in the care about patients with dementia. They especially positively enhance patients’ behavior since while being with a dog, patients appear to be calm, relaxed and contented, which results in the reduction of their feelings of depression, anxiety, agitation, and aggression [ 13 , 17 , 18 , 28 , 30 ]. This was also supported by significant effect sizes [ 17 , 18 , 28 ]. In addition, AAT/AAA contributes to the improvement of social behavior; the presence of a dog stimulates patients to interact and thus reduces their social isolation and loneliness. These findings have been also confirmed by other review studies, e.g. [ 22 , 23 , 25 , 26 ], and in most previous empirical studies, e.g. [ 32 , 33 ]. The repeated multimodal stimulations (verbal, visual, tactile) as seen in the study by Menna et al. [ 28 ] prove to be feasible and effective. In this study, the intervention took the form of structured play with a dog, which acted as a therapeutic and social agent.
Furthermore, dog therapy can be effective in the improvement of patients’ physical health as it was proved in the study on balance by Olsen et al. [ 29 ], in which AAA had a significant effect ( p = 0.03) on improving subjects’ balance and preventing risks of fall in comparison with the control group. The researchers engaged patients in active interactions with the dog and the patients, for example, had to bend down to pick the ball or they leaned forward to pet the dog. All these movements required a good posture control. Positive outcomes in the area of physical health were also studied by Cherniack and Cherniack [ 24 ], but with modest results.
In addition, dog therapy may also be beneficial for the improvement of cognitive functions as it was demonstrated by Menna et al. [ 28 ], although with modest effects. Interaction with the dog namely requires from the patient to pay attention, orientation in his/her environment, or simply it evokes in him/her memories from the past.
Olsen et al. [ 17 ] in their study also point out that the severity of dementia should be considered when planning AAT/AAA since patients with severe dementia had different needs and they demand more care and time. Therefore, AAT/AAA should be tailored to their specific needs and interests and aim at the person-centered dementia care [ 13 ].
The limitation of this study consists in analyzing the results of studies with different methodological approaches to AAT or AAA, small subject samples, as well as with different intervention periods. In addition, there was only one study [ 30 ], which also measured the effect after the follow up period. All these aspects then might have an impact on the overestimation of the discussed findings. Therefore, standard guidelines for the implementation of AAT are needed [ 22 ].
The findings of this study reveal that AAT may work as a beneficial and effective complementary treatment (especially in the area of behavioral and psychological symptoms) for patients with different degree of dementia severity if AAT is targeted at their specific needs and interests. Nevertheless, more research in the area of methodology for the implementation of AAT is necessary, as well as more research should be conducted with respect to the use of AAT for the improvement of cognitive functions in people with dementia.
Availability of data and materials
The search strategies used in this systematic review have been included in the Methods and all of the manuscripts informing this systematic review are listed in Table 1 .
Abbreviations
animal assisted activity
animal assisted therapy
Alzheimer’s disease
Clinical Dementia Rating
Geriatric Depression Scale
Mini-mental State Examination
Quality of Life
reality orientation therapy
Langa KM. Is the risk of Alzheimer’s disease and dementia declining? Alzheimers Res Ther. 2015;7:1–4.
Article Google Scholar
Klimova B, Maresova P. Computer-based training programs for older people with mild cognitive impairment and/or dementia. Front Hum Neurosci. 2017;11:262.
Article PubMed PubMed Central Google Scholar
Klimova B, Semradova I. Cognitive decline in dementia with special focus on language impairments. In: Bekirogullari Z, Minas MY, Thambusamy RX, editors European Proceedings of Social and Behavioural Sciences Cyprus: Nicosia; 2016. pp. 86–90.
Alzheimer’s Society. Alzheimer’s disease. https://www.alzheimers.org.uk/info/20007/types_of_dementia/2/alzheimers_disease . Accessed 12 Jul 2018.
Alzheimer’s & Dementia. Types of dementia. https://www.alz.org/dementia/types-of-dementia.asp . Accessed 28 Jul 2018.
Fu CC, Lee YM, Chen JD. Association between depressive symptoms and twelve-year mortality among elderly in a rural community in Taiwan. J Formos Med Assoc. 2003;102(4):234–9.
PubMed Google Scholar
Tierney MC, Naglie G, Upshur R, Jaakkimainen L, Moineddin R, Charles J, Ganguli M. Factors associated with primary care physicians’ recognition of cognitive impairment in their older patients. Alzheimer Dis Assoc Disord. 2014;28(4):320–5.
Alzheimer’s Statistics. https://www.alzheimers.net/resources/alzheimers-statistics/. Accessed 12 Jul 2018.
Maresova P, Klimova B, Novotny M, Kuca K. Alzheimer’s disease and Parkinson’s diseases: expected economic impact on Europe – a call for a uniform European strategy. J Alzheimers Dis. 2016;54:1123–33.
Article PubMed Google Scholar
Klimova B, Valis M, Kuca K. Potential of mobile technologies and applications in the detection of mild cognitive impairment among older generation groups. Soc Work Health Care. 2017;56(7):588–99.
Klimova B, Kuca K. Alzheimer’s disease: potential preventive, non-invasive, intervention strategies in lowering the risk of cognitive decline – a review study. JAB. 2015;13(4):257–61.
AWMA. Animal-assisted interventions: definitions. https://www.avma.org/KB/Policies/Pages/Animal-Assisted-Interventions-Definitions.aspx . Accessed 28 Jul 2018.
Swall A, Ebbeskog B, Hagelin CL, Fagerberg I. Stepping out of the shadows of Alzheimer’s disease: a phenomenological hermeneutic study of older people with Alzheimer’s disease caring for a therapy dog. Int J Qual Stud Health Well Being. 2017;12(1). https://doi.org/10.1080/17482631.2017.1347013 .
UCLA Health. Animal-assisted therapy research findings. https://www.uclahealth.org/pac/animal-assisted-therapy . Accessed 12 Jul 2018.
Beck A. Research shows therapy dogs can help Alzheimer’s patients with sundown syndrome. https://www.onecallmedicalalert.com/blog/2013/06/alzheimers-article/ . Accessed 28 Jul 2018.
Vann MR. How animal therapy helps dementia patients. https://www.everydayhealth.com/alzheimers/how-animal-therapy-helps-dementia-patients.aspx . Accessed 12 Jul 2018.
Olsen C, Pedersen I, Bergland A, Enders-Slegers MJ, Ihlebæk C. Engagement in elderly persons with dementia attending animal-assisted group activity. Dementia. 2016. https://doi.org/10.1177/1471301216667320 .
Pope WS, Hunt C, Ellison K. Animal assisted therapy for elderly residents of a skilled nursing facility. Journal of Nursing Education and Practice. 2016;6(9):56–62.
Jo C. The surprising power of pet therapy for dementia. https://www.caring.com/articles/pet-therapy-dementia . Accessed 12 Jul 2018.
Kumfor F. Robotic animals may help some people with dementia. https://theconversation.com/robotic-animals-may-help-some-people-with-dementia-20613 . Accessed 12 Jul 2018.
Petersen S, Houston S, Qin H, Tagne C, Studeley J. The utilization of robotic pets in dementia care. JAD. 2017;55(2):569–74.
Bennett SJ. The benefits of exposure to animals for persons with dementia: a literature review. Undergraduate research symposium. MN: Mankato. April 21, 2014. https://cornerstone.lib.mnsu.edu/urs/2014/oral_session_03/2 , 2014. Accessed 12 Jul 2018.
Bernabei V, de Ronchi D, La Ferla T, Moretti F, Tonelli L, Ferrari B, Forlani M, Atti AR. Animal-assisted interventions for elderly patients affected by dementia or psychiatric disorders: a review. J Psychiatr Res. 2013;47(6):762–73.
Article CAS PubMed Google Scholar
Cherniack EP, Cherniack AR. The benefit of pets and animal-assisted therapy to the health of older individuals. Curr Gerontol Geriatr Res. 2014;2014:623203.
Lundqvist M, Carlsson P, Sjödahl R, Theodorsson E, Levin LA. Patient benefit of dog-assisted interventions in health care: a systematic review. BMC Complement Altern Med. 2017;17(1):358.
Yakimicki ML, Edwards NE, Richards E, Beck AM. Animal-assisted intervention and dementia: a systematic review. Clin Nurs Res 2018;1:1054773818756987.
Thodberg K, Sørensen LU, Christensen JW, Poulsen PH, Houbak B, Damgaard V, Keseler I, Edwards D, Videbech PB. Therapeutic effects of dog visits in nursing homes for the elderly. Psychogeriatrics. 2016;16(5):289–97.
Menna LF, Santaniello A, Gerardi F, Di Maggio A, Milan G. Evaluation of the efficacy of animal-assisted therapy based on the reality orientation therapy protocol in Alzheimer's disease patients: a pilot study. Psychogeriatrics. 2016;16:240–6.
Olsen C, Pedersen I, Bergland A, Enders-Slegers MJ, Ihlebæk C. Effect of animal-assisted activity on balance and quality of life in home-dwelling persons with dementia. Geriatr Nurs. 2016;37(4):284–91.
Olsen C, Pedersen I, Bergland A, Enders-Slegers MJ, Patil G, Ihlebaek C. Effect of animal-assisted interventions on depression, agitation and quality of life in nursing home residents suffering from cognitive impairment or dementia: a cluster randomized controlled trial. Int J Geriatr Psychiatry. 2016;31(12):1312–21.
Health Evidence Quality Assessment Tool for review articles. 2005. https://www.healthevidence.org/documents/our-appraisal-tools/quality-assessment-tool-dictionary-en.pdf . Accessed 10 April 2019.
Le Roux MC, Kemp R. Effect of a companion dog on depression and anxiety levels of elderly residents in a long-term care facility. Psychogeriatrics. 2009;9:23–6.
Travers C, Perkins J, Rand J, Barlett H, Morton J. An evaluation of dog-assisted therapy for residents of aged care facilities with dementia. Anthrozoos. 2015;26(2):213–25.
Download references
Acknowledgments
The paper is supported by the project Excellence 2019, run at the Faculty of Informatics and Management of the University of Hradec Kralove, Czech Republic, whose members participated in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and affiliations.
Department of Applied Linguistics, Faculty of Informatics and Management, University of Hradec Kralove, Hradec Kralove, Czech Republic
Blanka Klimova & Josef Toman
Biomedical Research Centre, University Hospital Hradec Kralove, Hradec Kralove, Czech Republic
Centre for Basic and Applied Research, Faculty of Informatics and Management, University of Hradec Kralove, Sokolska 581, Hradec Kralove, Czech Republic
You can also search for this author in PubMed Google Scholar
Contributions
BK, JT and KK equally contributed to the drafting, analyses and final version of the whole manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Kamil Kuca .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Klimova, B., Toman, J. & Kuca, K. Effectiveness of the dog therapy for patients with dementia - a systematic review. BMC Psychiatry 19 , 276 (2019). https://doi.org/10.1186/s12888-019-2245-x
Download citation
Received : 20 February 2019
Accepted : 19 August 2019
Published : 06 September 2019
DOI : https://doi.org/10.1186/s12888-019-2245-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Intervention
- Effectiveness
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Increasing participation in research with therapy dogs: A qualitative study at a large urban mental health and addiction hospital
Contributed equally to this work with: Laura Sikstrom, Sophie Soklaridis
Roles Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing
Affiliation Office of Education, Centre for Addiction and Mental Health, Toronto, Ontario, Canada
Roles Conceptualization, Investigation, Writing – review & editing
¶ ‡ These authors also contributed equally to this work.
Roles Formal analysis, Investigation, Writing – review & editing
Roles Investigation, Writing – review & editing
Affiliation Geriatric Mental Health Services, Centre for Addiction and Mental Health, Toronto, Ontario, Canada
Affiliation Complex Care & Recovery Program, Centre for Addiction and Mental Health, Toronto, Ontario, Canada
Roles Conceptualization, Funding acquisition, Methodology, Writing – review & editing
Affiliation Volunteer Services, Centre for Addiction and Mental Health, Toronto, Ontario, Canada
Roles Funding acquisition, Writing – review & editing
Roles Conceptualization, Methodology, Resources, Supervision, Writing – review & editing
* E-mail: [email protected]
Affiliations Office of Education, Centre for Addiction and Mental Health, Toronto, Ontario, Canada, Departments of Psychiatry and Family and Community Medicine, University of Toronto, Toronto, Ontario, Canada, Wilson Centre, University Health Network and Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada
- Laura Sikstrom,
- Tamar Meyer,
- Eva Katz,
- Man-Man Choi,
- Margaret Darragh,
- Amanda Cutler-Palma,
- Theresa Conforti,
- Csilla Kalocsai,
- Sophie Soklaridis

- Published: August 27, 2020
- https://doi.org/10.1371/journal.pone.0238096
- Reader Comments
The benefits of involving patients as partners in research across diverse medical and psychiatric settings are well established in the literature. However, researchers continue to struggle to access, engage and retain participants from hard-to-reach populations. The main objective of this study was to co-create pet therapy activities with patients admitted for serious and complex mental illness to a large urban mental health and addiction hospital. Informed by the principles of participatory action research methodology, we conducted focus group discussions with 38 inpatients in seven different clinical units. An experienced volunteer handler and a certified therapy dog helped facilitate our discussions. Participating researchers, recreational therapists, volunteer handlers and our participants all reported that the presence of a certified therapy dog at each of our discussions was integral to their success. Certified therapy dogs increased the motivation to participate in our study, helped to build rapport with participants and created connections in our discussions that enriched our data. To our knowledge our study is the first to demonstrate the value of using a therapy dog as a participatory research tool in a healthcare setting. The authors believe that therapy dogs are a low-tech intervention that could be used effectively to engage hard-to-reach populations in research about their treatment and care in a diverse range of medical settings. These findings support the creation of a pilot study to test the value of including therapy dogs in patient-centered research with vulnerable and hard-to-reach populations.
Citation: Sikstrom L, Meyer T, Katz E, Choi M-M, Darragh M, Cutler-Palma A, et al. (2020) Increasing participation in research with therapy dogs: A qualitative study at a large urban mental health and addiction hospital. PLoS ONE 15(8): e0238096. https://doi.org/10.1371/journal.pone.0238096
Editor: Rosemary Frey, University of Auckland, NEW ZEALAND
Received: October 10, 2019; Accepted: August 9, 2020; Published: August 27, 2020
Copyright: © 2020 Sikstrom et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: Our study was funded by a Nestle-Purina Animal-Human Bond grant. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: Our study was funded by a Nestle-Purina Animal-Human Bond grant. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. In addition, this does not alter our adherence to PLOS ONE policies on sharing data and materials.
Introduction
The benefits of involving patients as partners in research across diverse medical and psychiatric settings are well established in the literature. [ 1 ] However, the failure to recruit, engage and retain hard-to-reach populations limits the scope of these efforts. [ 2 , 3 , 4 ] Significantly, unequal representation in research undermines patient outcomes for vulnerable and disadvantaged groups. [ 5 ] Moreover many qualitative research techniques rely on the desire and ability of the patient to effectively communicate their perspectives to researchers, which can be difficult in the midst of a mental health crisis. [ 6 , 7 ] While a range of techniques have been developed to recruit and engage patients in health research, to our knowledge our study is the first to demonstrate the value of using a certified therapy dog as a participatory research tool in a healthcare setting. [ 8 ] Somewhat unexpectedly we found that therapy dogs buffer the power and communication gaps between researchers and patients hospitalized with complex and serious mental illness. Therapy dogs increased the motivation to participate in our study, helped to build rapport with participants and created connections that enriched our data. Although high-tech innovations are revolutionizing healthcare and patient outcomes, our study provides evidence that therapy dogs are a “no-tech” and low cost intervention that both humanizes the hospital experience and significantly improve efforts to engage patients in research.
In recent years, the benefits of animal-human interactions, particularly with dogs, across diverse medical and psychiatric settings has been well established in the literature. Canine Assisted Interventions (CAI) bring together credentialed canine-human teams to enhance human well-being. [ 9 ] There is growing evidence on the positive impact of animal-human interactions. For example, it has been documented to reduce cardiovascular stress, [ 10 ] enhance immune factors, [ 11 ] decrease pain, [ 12 ] improve mood, [ 13 ] reduce cortisol levels, [ 14 ] decrease fear and anxiety, [ 15 ] and create an overall humanizing atmosphere within a hospital setting. [ 16 ] Specific to mental health, a meta-analysis of the effects of CAI on depression identified effects of medium magnitude. [ 17 ] A literature review concludes that CAI may also ameliorate the behavioral and psychological symptoms of dementia. [ 18 ] However, there is no available literature on CAI initiatives that have been designed with input from patients. Recently, a move towards building opportunities for greater collaboration with patients within the mental health and addictions system has occurred. Thus, our exploratory qualitative study was designed to emphasize the value of the patient voice within clinical settings. [ 19 ] Our aim was to co-develop our CAI activities (herein referred to colloquially as “Pet Therapy”) with patients at the Centre for Addiction and Mental Health (CAMH), which is North America’s largest mental health and addiction hospital. Although we were successful at co-creating meaningful activities with patients, this is not the focus of this article. Rather our aim is to illustrate the value of including a therapy dog in qualitative research activities with hard-to-reach populations.
CAMH has more than 34,000 unique patients per year. CAMH’s “Pet Therapy” consists of 40 dogs and their volunteer handlers. Dogs are screened, tested and evaluated before they can be part of CAMH’s Pet Therapy program. On average 70% of the dogs pass the assessment, which focuses on ascertaining a dog’s response to unpredictable situations, commands, loud noises and strangers. Once the dogs are evaluated and pass, the volunteer handlers are interviewed, trained and placed in a specific clinical unit. Volunteers visit one to two units per week for 30 minutes to one hour at a time. Pet Therapy activities are highly variable across the hospital but typically involve an informal gathering of interested patients who pet, play and chat with the visiting dog and handler. There are also one-on-one visits and more informal gatherings at the library. Pet Therapy is a very popular program with patients and staff. All of the dogs used in this study have been tested and certified to work in clinical settings and were accompanied by their handler the entire time.
The findings presented here are part of an exploratory patient engagement project at CAMH on Canine Assisted Therapy activities. Our research question was: How can patients partner with the volunteer handlers and dogs at CAMH to co-create activities that are meaningful to them, improve their recovery process and humanize the psychiatric hospital experience?
To engage patients at CAMH as research partners our methodology was informed by the principles of Participatory Action Research (PAR). PAR differs from other methods of mental health research due to its focus on reflection, data collection, and action that works to improve health and reduce health inequities by involving the individuals affected. [ 20 ] One benefit of PAR is that researchers often design the research questions and methodology with potential participants to ensure that the questions are considered both relevant and beneficial to the population being studied. [ 21 ] In our study, one strategy we used was to work with volunteer handlers to refine our discussion guide. A second (unintentional) strategy was to bring pet therapy dogs to all our research activities. The impact of this decision on our research is the focus of this article. Ethics approval for this study was granted by the Research Ethics Board at CAMH.
Our recruitment strategy involved a five step process between September and December 2018. First, we sent a recruitment email to all of the pet therapy volunteer handlers at CAMH asking if they would like to co-facilitate a focus group discussion (FGD) on pet therapy with patients. Seven handlers expressed immediate interest. These handlers had a combined total of 20 years of experience conducting pet therapy visits on clinical units at CAMH. This meant that in some cases they had established relationships with some of the participants in our study. Second, we reached out to the recreational therapist (RT) on the clinical units where these handlers volunteered to describe the aims of the study and obtained their permission to hold a FGD on their unit. All of the units we approached agreed to participate in our study. Third, all of the volunteer handlers participated in a webinar on PAR methodology and facilitation skills. At this stage we consulted with the handlers to determine whether they felt able to co-facilitate a FGD while also monitoring their dog’s interactions with patients. Handlers decided unanimously that they would like to bring their dogs to each FGD.
Fourth, handlers, RTs and researchers informed inpatients of our study face-to-face during a community meeting held on each clinical unit. A researcher [LS] and volunteer handlers also informed patients of the study in person during regularly scheduled pet therapy visits held on these clinical units. In addition to communicating the aims of our study in person we also distributed a letter of information for those interested in learning more about our study. Finally, patients expressed their interest in participating to the RT, who then coordinated the best time and place to hold our discussion. All potential participants were informed of the aims of the study and that their participation was voluntary. Written informed consent was obtained from all participants on the day of the scheduled FGD. All of our participants were also informed that their participation (or lack thereof) would have no effect on their care. One patient declined to participate after expressing initial interest but did not provide a reason for his refusal.
We held a total of seven FGD with 38 patients (18 men, 20 women). We conducted our FGD on seven of the 23 clinical units at CAMH that offer pet therapy to patients (see Table 1 ). All of our participants had been admitted to a clinical unit at CAMH for a minimum of 72 hours and up to 4 years. Two of our FGD took place on forensics unit, thus our participants may disproportionately represent those with mental illness that have had encounters with the law. Our participants ranged in age from 18 to 88years. We did not ask any questions about their personal medical histories. We did not witness any signs of distress in the dogs during our FGD. The dogs appeared happy and relaxed and moved from patient to patient seeking pets and dog treats. However, handlers did report that their dogs occasionally demonstrated signs of distress on units during official pet therapy visits. For example, on one unit an acute patient became very loud and aggressive and the dog indicated that they wanted to leave by heading towards the exit.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0238096.t001
Each FGD was held in a private activity room on each clinical unit and co-facilitated by a medical anthropologist [LS] and a volunteer handler. RTs participated in three of the seven FGD due to hospital regulations about the staff supervision of patients with a recent history of violent outbursts. Any inpatient with an interest in pet therapy was eligible to participate in this study. However, in a few instances the RT identified patients that were having difficulties related to their illness (e.g. hallucinations, erratic behavior, or violent outbursts) and were excluded from participating on the day of our FGD. In addition, patients who required a substitute decision-maker to consent were excluded from this study (e.g. patients with advanced dementia). Outpatients/ambulatory patients were also excluded from this study since our study was concerned with the experience of hospitalization from the patient’s perspective. Most participants had attended pet therapy activities at least once prior to our FGD. Two of our participants had a very limited capacity to communicate verbally (e.g. one participant experiences selective mutism), however the presence of the dog helped buffer these communication challenges and enabled us to successfully engage the patient’s perspective of a hospital-based pet therapy program.
Each FGD lasted between 50–90 minutes. We asked participants about their previous experiences with pet therapy, what they liked best about pet therapy and if they had any negative experiences with pet therapy (see S1 Appendix A ). FGDs are a useful methodological technique for many reasons but for this article we illustrate their ability to capture communication between research participants to generate data. [ 22 ] In particular, a medical anthropologist with ethnographic expertise [LS] took field notes during each FGD on the kinds of social interactions generated by the dog’s presence. In addition, researchers documented the main discussion points on a flip chart. In addition, at the end of each FGD we summarized the main points with our participants to check for accuracy. We did not check for accuracy after the analysis was complete (member checking) due to the transience and memory loss of many of our research participants. Using an iterative research process we reflected on these observations after each FGD to refine our discussion guide and make further observations. Thus, our findings reflect not only what was said explicitly during each FGD but also draw upon observations about how the therapy dog influenced the social interactions between patients and researchers.
Each FGD was also audio recorded and transcribed. A qualitative computer software package, Dedoose, was used to analyze and code the data. First, LS coded for general descriptive codes (e.g. meaning of pet therapy). Next, these primary descriptive codes were synthesized into axial codes. Axial coding in grounded theory is the process of relating categories and concepts to each other via inductive and deductive thinking. [ 23 ] Our axial codes reflected three major themes that emerged from both our observations and our participants’ verbal responses during the FGD: motivation, rapport and connection. Given our methodological approach, the positionality of our research team is relevant. Within our authorship team we have a mix of social scientists, recreational therapists and volunteer handlers. Our lead author (LS) for example, was a skeptic. She had no previous experience with pet therapy, or dogs, and her surprise at the ability of certified therapy dogs to enrich our data, was the impetus behind writing this paper. Whereas the seven other members of our team had extensiveexperience with pet therapy on various inpatient units at CAMH. Our varied experiences with pet therapy and the ways in which these experiences have influenced our thinking were the topic of many collaborative analytical conversations.
Rich and detailed qualitative data is only possible if participants are both willing and able to share their experiences. Our study demonstrated that the presence of a certified therapy dog increased many patients’ motivation to participate in our study, improved the ability of researchers to build rapport with participants and helped create a safe and open atmosphere that enabled patients to connect with each other and researchers. In short, therapy dogs bridge the gap between hard-to-reach populations and researchers, enabling research participants to share their lived experiences in a group setting (see Fig 1 ). We discuss each of these findings in more detail below.
https://doi.org/10.1371/journal.pone.0238096.g001
Patients with depression, schizophrenia and dementia in particular often lack the motivation to complete everyday tasks. [ 24 ] In our study, the therapy dog helped counter-act the tendency of patients with mental illness to self-isolate. [ 25 ] For example, on the day of our FGD in the schizophrenia unit a patient that had expressed an interest in participating was having what was described by the RT to be a “a very bad day”. The researcher and the handler found him curled up in a ball in his room; he had not eaten or bathed all day. The dog jumped up on the bed and the patient reached out to pet and whisper something to him. A few minutes later he joined us for the FGD and later commented on how meaningful that brief one-on-one interaction with the dog was for him. In particular, patients enjoyed the opportunity to touch and be touched by another living being, something that was not always possible with fellow patients or staff. For example:
“They make you feel loved… When this dog licked my hand, it’s wow.” [Forensics]
Many participants also reported feeling more joyful and energized because of the dog’s presence. For example:
“I was feeling very down before he came, but now I’m: ‘George Michael, wake me up…’ Energized.” [GAU-B]. “I’m so excited. He [the dog] is the reason I didn’t stay in my room after group [therapy]. I was going to go to sleep. But I kept asking, where’s the dog? Where’s the dog?” [WIU]. “It [pet therapy] means I’m going to have a really good time.” [Acute Care -Schizophrenia].
RTs echoed these sentiments by noting that many asocial patients will leave their rooms to interact with a dog.
Building rapport is also critical to the success of qualitative research. Rapport is often established through the reciprocal exchange of neutral information about the weather, food or other shared experiences, or what we typically call “small talk”. [ 26 ] In the recruitment phase of this research, “small talk” with patients using the usual standbys, like “what brings you here?”, “how’s the food?” and “it’s so nice outside today, isn’t it?” would be inappropriate given that most in-patients have very limited access to the outdoors. The inability to create small talk in the typical manner can make it difficult to build rapport and create a common ground with research participants. However, talking about the dog was always appropriate. For example:
“It helps break the ice… With a dog around there is always something to talk about, right, and it’s not awkward. Maybe that’s what it is, it’s not awkward.” [WSFU]. “Since the dog died my wife and I have been hollering at each other, because [dogs], they’re buffers . They keep the conversation going…. Buffers , they are, the effect” [Emphasis ours, GAU-A].
We regularly engaged in simple conversations about the dog’s size, age, breed, training, behavior, and personality. It was through these routine exchanges of neutral information that we established a comfortable and open atmosphere that helped buffer the power gap between researchers and patients. For example:
“You just want to feel regular, because the pets do not make you feel as if you’re a patient. They treat you different… Like a human being.” [Forensics]. “So maybe it [dogs] helps people get along with other people better. It makes people better socializing with adults or other people their own age.” [WSFU].
The ability to build rapport with patients in a way that made them feel “like a human being” was critical to our success since it enabled us hold thoughtful discussions with a range of participants experiencing acute symptoms of mental illness.
In this context, we were also working with vulnerable and socially disadvantaged populations who had many negative and sometimes violent experiences with the general public and/or encounters with the law. [ 27 ] For example:
“The thing that brightens up my day everyday if I’m out there panhandling and there are cops… but seeing someone walk by with a really cute dog and they let me pet it.. I like dogs more than people.” [GPU].
Many participants also described feeling isolated, dismissed and forgotten during most of their everyday social interactions. For example:
“He [the dog] listens. At least he listens. He’s not like most people, just ignore me.” [GAU-A].
Several participants also explained that they enjoyed pet therapy because they received so few visitors during their in-patient hospitalization. For example:
“I think it’s a way of connecting because people have their limits. You can’t walk up to somebody and comb their hair. So the animals provide an outlet.” [WSFU]. “If you don’t speak to anyone, you don’t socialize, you don’t go anywhere, by interacting with an animal you become more open to doing things with other people because you have the trust factor. You feel more comfortable interacting with another person through pet therapy . It will help you open up .” [Forensics].
Moreover, participants described their daily lives as inpatients as entailing a tremendous amount of compliance with hospital rules and regulations. These interpersonal dynamics can make it difficult for researchers to overcome the power imbalances that exist between researchers and participants. [ 28 ] In our FGD, the therapy dog clearly helped us connect to patients through the dog. Many participants described feeling more open and trusting with the therapy dog present. Petting and interacting with the dog also helped humanize these encounters and brought comfort to many patients in the midst of a mental health crisis.
More importantly, we found that the relaxed and open atmosphere created by the dog’s presence meant that participants more easily connected to their own experiences and memories. Without prompting, many participants told us detailed stories about their life histories. Many participants explicitly connected the dog’s presence to specific memories:
“I have always been around animals and worked on a farm, so it has been a good connection for me, memories… The memories it brings back,” [GPU]. “It reminds me of when I was on the outside in the neighborhood, even when I was a little guy… It reminds me of that and it’s a good feeling.” [Forensics].
Also, during the recruitment phase of this project we were chatting amiably for at least an hour with a group of participants during their regular pet therapy visit. One young man visibly enjoyed the dog and spent a great deal of time petting him. About thirty minutes into our visit he began to describe his entry into drug addiction. He started by telling us that he had to leave his dog behind when he went out West to find work. He described to us how lonely and boring this work camp had been. His counsellor told us afterwards that it was the first time she had ever heard him talk for any length of time. This effect was notable on every unit and was particularly useful for helping us prompt participants with memory problems (e.g. dementia) or help agitated participants focus on the topic at hand.
Participants routinely described the dog’s presence as a comfort that helped them navigate their social interactions with researchers and their fellow focus group participants more successfully. For example:
“The [dog] is opening everybody’s heart up.” [WIU]. “For me, I would say it’s comforting… because they don’t speak and I find I’m communicating with them on a different level. It’s different in a good way… They’re usually very friendly and you enjoy being with them, which is nice, and you feel a sense of connection.” [GPU]. “I think a lot of people are actively trying to deal with their personal boundaries, and it’s not that they’re too broad, sometimes people are too uptight. And I know I am one of those people.” [WSFU].
As experienced researchers, we can think of no other mechanism that so quickly and easily created an environment of trust and reciprocity.
Although our participants were hospitalized for acute symptoms of mental illness, nearly all were able to clearly articulate their likes and dislikes about pet therapy in a group setting. Our findings show that the presence of a therapy dog improved the depth and quality of the data we collected (see Fig 2 ). The dog served as a buffer by decreasing the power imbalance between the researchers and participants. In particular, therapy dogs add value in settings where it is difficult to build rapport or find common ground and where people may struggle to feel comfortable with individuals in authority. Similar to Kate Fox’s observations that “weather speak” is a form of code that enables people to overcome any natural reserve and talk to eachother; [ 29 ] “dog speak”, or conversation about a dog’s age, temperament and breed, helped us build rapport with our participants, which ultimately enriched our data. Significantly, the benefits of a certified therapy dog may also hold for individuals who do not enjoy dogs. For example, one of our participants’ did not like dogs but stated that she attended every pet therapy visit because they enjoyed the social interactions catalyzed by the dog’s presence. [ 30 ] In fact, during our FGD she kept herself behind a table so that the dog could not come up and interact with her, but told us she enjoyed the atmosphere generated by the dog’s presence.
https://doi.org/10.1371/journal.pone.0238096.g002
Although there is a very large body of scholarship that explores the potential of various technological innovations to support patient engagement almost no attention has been paid to the role that animals, especially certified therapy dogs, might play at mediating social interactions during patient engaged research. An emerging body of research on interspecies interactions suggests that human and non-human actors mutually perceive and affect one another in particular material and social contexts. [ 27 , 31 , 32 ] For example, Solomon adapts Levinson’s (2006) metaphor of the “interaction engine” to argue that certified therapy dogs guide humans into rich social interactions by increasing their communication and affective ties with others (2008: 149). [ 33 ] McNicholas and Collis (2000) also illustrate how dogs enhance human well-being by strengthening social ties between people. [ 30 ] By paying attention to these dynamics our study highlights the benefit of using therapy dogs as a no-tech and low-cost alternative to buffer challenging social encounters and enhance the richness of qualitative data.
Our qualitative study indicates that the presence of a therapy dog during our research activities increased the motivation to participate in our study, helped to build rapport with participants and created connections that enriched our data. These findings indicate that certified therapy dogs could be used effectively to engage participants in research about their treatment and care in a diverse range of medical settings. The ability of dogs to help our participants connect to their own memories and stay focused also suggests that therapy dogs might also be useful in clinical practice when taking medical histories or when discussing sensitive topics or traumatic events. [ 13 ] Further research on the impact of certified therapy dogs in clinical settings has not only the potential to humanize hospitalization of patients, but also to contribute to redressing some of the power imbalances that exist within research encounters.
Supporting information
S1 appendix. focus group discussion guide..
https://doi.org/10.1371/journal.pone.0238096.s001
Acknowledgments
We wish to thank all of the volunteer handlers and their dogs for supporting this research, recreational therapists for coordinating the research on each clinical inpatient unit and all of the patients for their time and thoughtful contributions.
- View Article
- PubMed/NCBI
- Google Scholar
- 8. Gubrium A, Harper K. Participatory visual and digital methods. New York: Routledge; 2013.
- 9. Binfet JT, Kjellstrand Hartwig E. Canine-Assisted Interventions: A Comprehensive Guide to Credentialing Therapy Dog Teams. New York: Routledge; 2020.
- 20. Kindon S, Pain R, Kesby M. Participatory Action Research Approaches and Methods: Connecting People, Participation and Place. Abingdon, UK: Routledge; 2007.
- 23. Charmaz K. Constructing grounded theory. 2nd ed. London: Sage; 2014.
- 29. Fox K. Watching the English: The hidden rules of English behavior. Boston: Hodder & Stoughton; 2014[2008].
- 32. Wilson EO. Biophilia: The human bond with other species. Cambridge: Harvard University Press; 2009[1984].
- 33. Levinson Stephen C. On the Human "Interaction Engine." In Roots of Human Sociality: Culture, Cognition and Interaction. Enfield Nick J and Levinson Stephen C, eds. 2006; 39–69. New York: Berg.
- University Libraries Databases
- WMU Research Guides
Therapy Dogs in the Libraries
- Therapy Dogs
Why we invite dogs to the library:
- Help relieve stress and anxiety during the semester.
- Create a welcoming and inclusive space in the libraries.
- To give students a way to connect to animals, especially if they are missing their pets at home.
- By having more therapy animals on campus, this could potentially reduce the number of individual requests for support animals campus-wide.
When we invite dogs to the library:
- Finals week.
- Mid-term breaks.
- Days and evenings depending on need or time of the semester.
- Other special events and programming like Waldo Fest.
- Sunny visiting Waldo during Finals Week

Finding and schedulin g therapy dogs:
- We first identified our regulars through a local Facebook group organized by Dr. Moe. We now have a core group of 5-7 dog/handler teams who volunteer in the library. However, we do welcome new teams!
- They are volunteers and not reimbursed. Some are provided with parking passes.
- Walk them through the space to help dog acclimate to library.
- Put them in a public, loud area that is highly visible with a lot of traffic. We set them up on the first floor off of the main entrance.
- Advertise in and outside of the library.
- For larger events we have scheduled up to four dogs simultaneously.
- For longer events, we schedule dogs in 2 hour blocks during the event.
- Review ground rules: Do not disturb students at computers or in quiet areas because they may be testing. Reiterate University Libraries values of welcoming and inclusive environment.
- Chloe visiting Waldo during mid-term art breaks.

Institutional logistics
- We require approval from the Vice-President of Student Affairs for all therapy dog visits. We were able to receive a blanket approval for all therapy dog visits.
- Certified therapy dogs only allowed.
- Request certification documentation from the handler. In our case, most dogs are certified through the Alliance of Therapy Dogs. Certification is also proof of insurance.
- Keep copy of certification with Library Office Manager.
- Arthur visiting during mid-terms Art Break

Who we partner with:
- Dr. Angie Moe, Therapy Dog Clinic Coordinator and Professor of Sociology.
- We identify therapy dogs through a local Facebook group run by Dr. Moe.
- We also participate in therapy dog training and serve as a site visit.
- Therapy Dogs in Training Visiting Waldo

What to ask the handler:
- What are the dog's needs?
- What is their max time for an event?
- Do they need scheduled breaks and where would an ideal location be?
- Can they handle a high capacity of students (we average 60-80 individual visitors in a 2-hour time frame, and have had up to 100; there are often 5-10 visitors at any one time)?
- Will they do well with another therapy dog nearby or should they be scheduled alone?
- Q visiting Waldo During Art Break

- Last Updated: May 15, 2024 3:24 PM
- URL: https://libguides.wmich.edu/therapydogs

Nature of Home
Puppy Prescriptions: The 10 Best Therapy Dog Breeds
Posted: May 18, 2024 | Last updated: May 18, 2024

Feeling overwhelmed by pressure? A furry therapist may be just what the doctor ordered.
New research from Washington State University reveals that students who regularly interacted with therapy dogs showed improvements in concentration, memory, and relaxation compared to those without 1 .
With proven benefits like reduced stress hormones, elevated moods, and better mental health from animal interactions, therapy dogs are making their way to campuses, hospitals, offices, and other high stress locations.
While all dogs can be therapy dogs, there are certain breeds that are particularly well-suited for this rewarding work. Here’s the ten best therapy dog breeds.

1. Labrador Retriever: America’s Favorite Therapy Dog
Friendly, intelligent Labrador Retrievers top the list of ideal therapy dogs. Their gentle, affectionate nature endears them to people of all ages. Labs eagerly aim to please, making them a hit when visiting hospitals or nursing homes.
Numerous research highlights their calm, patient temperament ( ref ) – perfect for providing comfort through cuddling or a reassuring lick when someone feels stressed.

2. Golden Retriever: Heart of Gold
Golden Retrievers are another breed that excels in the therapy dog realm. Their gentle dispositions, eagerness to please, and natural affinity for people make them ideal companions for individuals in need of comfort and emotional support.
These dogs are often described as “gentle giants,” and their warm, loving nature can melt even the hardest of hearts . Golden Retrievers are known for their patience and ability to remain calm in various situations, making them well-suited for therapy work in settings like hospitals or schools.

3. Poodle: A Hypoallergenic Helper
Poodles are brilliant, active, and highly trainable dogs that make excellent therapy companions. Both Standard and Miniature Poodles are popular choices for therapy work due to their hypoallergenic coats, which can be beneficial for individuals with allergies.

4. Cavalier King Charles Spaniel: Small Dog, Big Heart
With their gentle, affectionate personalities and calm demeanors, Cavalier King Charles Spaniels are natural-born therapy dogs. These small but mighty canines are known for their love of cuddling and their ability to bring joy and comfort to those around them.
Cavaliers are often described as “lap dogs” due to their tendency to seek out human companionship and their willingness to snuggle up close.

5. Boxer: A Playful & Protective Companion
Boxers defy their muscular appearance when it comes to therapy work. Don’t be fooled – these goofy companions have the patience of saints around people. Their loyalty and friendly antics win over children and adults alike. Sturdy Boxers can withstand accidental roughhousing, making them great therapy partners for kids.

6. Corgi: Fun-Sized Friend
Don’t overlook the mighty Corgi! These small but mighty herders pack huge therapy dog potential in a portable package.
Outgoing, adaptable Corgis excel at bringing smiles to faces young and old with their playful antics. Their long, low stature gives easy access to those in wheelchairs or beds.


7. Bulldog: The Wrinkly Charmer
Despite their somewhat fierce appearance, Bulldogs are calm, relaxed companions at heart.
With their low energy levels and tendency to love lounging, Bulldogs provide a therapeutic presence just by being their mellow selves. They are gentle, patient, and tolerant with all, even when stressed – making them excellent therapy dogs. Bulldogs love to lean in for warmth and affection.

8. Newfoundland: The Wrinkly Charmer
Newfoundlands’ imposing size belies their incredibly gentle souls, perfectly suited for therapy roles. Imagine the comfort a friendly giant like this can provide patients or residents just by being present. Their patience shines when working with children. Newfies offer a reassuring, secure presence.

9. Bernese Mountain Dog: Gentle Giant with a Heart of Gold
Bernese Mountain Dogs are large, powerful dogs with a gentle and nurturing nature that makes them wonderful therapy companions. These beautiful dogs are known for their calm and patient demeanor, as well as their ability to provide a sense of security and comfort.
Despite their size, Bernese Mountain Dogs are incredibly gentle and affectionate, with a natural ability to connect with people of all ages.

10. Mixed Breeds: A Unique Blend
While purebreds get top therapy dog billing, mixed-breed pups can be equally well-suited for this special work. A mutt from the shelter may possess the ideal temperament when properly trained and socialized. Giving a rescue dog a forever home while providing therapy is a double win!

How to Train Your Dog for Therapy Work
Now that you’ve learned about the top therapy dog breeds, you may be wondering how to train your furry friend for this rewarding work. Here are some key steps to follow:
- Start with basic obedience training : A well-behaved dog is essential for therapy work. Enroll your pup in basic obedience classes to teach them commands like sit, stay, come, and heel.
- Socialize your dog : Therapy dogs need to be comfortable around people of all ages, sizes, and abilities. Expose your dog to various sights, sounds, and situations to help them become well-adjusted and confident.
- Consider the Canine Good Citizen (CGC) test : Many therapy dog organizations require dogs to pass the CGC test, which evaluates their temperament and obedience skills. ( ref )
- Enroll in a therapy dog training program : Look for reputable organizations that offer therapy dog training and certification programs. These programs will teach you and your dog the specific skills needed for therapy work.
- Practice, practice, practice : Once you’ve completed the necessary training, continue to practice and reinforce the skills your dog has learned. Consistency and positive reinforcement are key to maintaining their therapy dog skills.

The Making of a Therapy Dog
If you’re considering getting a therapy dog or volunteering with one, any of the breeds mentioned in this article would be an excellent choice. No matter the breed, any well-behaved, people-friendly pup can potentially become a valued therapy dog with the right preparation.
Always remember that the key to being a successful therapy dog is having a calm, gentle, and affectionate disposition, as well as the ability to remain composed in various situations.
- https://journals.sagepub.com/doi/10.1177/2332858419852592
More for You
Scarlett Johansson said she was forced to hire legal counsel to deal with Sam Altman and OpenAI
'American Idol' Winner Abi Carter on What Luke Bryan Told Her After Finale
Here's What Happens When You Eat Cashews Every Day
12 Strange Facts About Redheads You Never Knew
10 best new Netflix originals you need to add to your watch list
Jon Lovitz: It seems the parties 'switched completely' on Israel
Fans Blasting Caitlin Clark Teammate After Indiana Fever's Fourth-Straight Loss
Kevin Costner Pays Tribute to 'Yellowstone' Costar Dabney Coleman
4 Chain Restaurants With The Absolute Best Chicken Pot Pie And 4 With The Worst
What Type Of Engines Do F1 Cars Use And How Much Horsepower Do They Have?
Drinking Water Warning Issued Nationwide
‘Tracker': Justin Hartley Breaks Down Finale Cliffhanger That Will "Lead To A Bigger Mystery" In Season 2
Patricia Heaton defends Chiefs kicker following graduation speech backlash: 'He's not a monster'
The World’s 25 Most Breathtaking Stained Glass Windows
4 things nobody tells you about the first 6 months of retirement — and what changes you can make so you can enjoy your ‘new normal’
10 Of The Fastest Cars Built With A V12 Engine
Kevin Costner Can't Hold Back Tears as His Western Epic ‘Horizon' Earns 7-Minute Cannes Standing Ovation, Promises ‘3 More' Installments
20 Best Sandwiches in America You Need to Try At Least Once
‘Friends’ star Courteney Cox says Matthew Perry ‘visits me a lot,’ still feels sense he is ‘around, for sure’
Controversial oil and gas company files for Chapter 11 bankruptcy
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Guidelines and Guidance Library
- Core Practices
- Isolation Precautions Guideline
- Disinfection and Sterilization Guideline
- Environmental Infection Control Guidelines
- Hand Hygiene Guidelines
- Multidrug-resistant Organisms (MDRO) Management Guidelines
- Catheter-Associated Urinary Tract Infections (CAUTI) Prevention Guideline
- Tools and resources
- Evaluating Environmental Cleaning
H. Animals in Health-Care Facilities
At a glance.
Guidelines for animals in healthcare facilities from the Guidelines for Environmental Infection Control in Health-Care Facilities (2003).
1. General Information
Format change [february 2017] .
Animals in health-care facilities traditionally have been limited to laboratories and research areas. However, their presence in patient-care areas is now more frequent, both in acute-care and long-term care settings, prompting consideration for the potential transmission of zoonotic pathogens from animals to humans in these settings. Although dogs and cats may be commonly encountered in health-care settings, other animals (e.g., fish, birds, non-human primates, rabbits, rodents, and reptiles) also can be present as research, resident, or service animals. These animals can serve as sources of zoonotic pathogens that could potentially infect patients and health-care workers (Table 26). 1327–1340 Animals potentially can serve as reservoirs for antibiotic-resistant microorganisms, which can be introduced to the health-care setting while the animal is present. VRE have been isolated from both farm animals and pets, 1341 and a cat in a geriatric care center was found to be colonized with MRSA. 1342
Table 26. Examples of diseases associated with zoonotic transmission* (This table does not include vector-borne diseases.)
Table 26a. virus, table 26b. bacteria, table 26c. parasites, table 26d. fungi.
* Material in this table is adapted from reference 1331 and used with permission of the publisher (Lippincott Williams and Wilkins).
§ Reptiles include lizards, snakes, and turtles. Rodents include hamsters, mice, and rats.
- + Indicates that the pathogen associated with the infection has been isolated from animals and is considered to pose potential risk to humans.
Zoonoses can be transmitted from animals to humans either directly or indirectly via bites, scratches, aerosols, ectoparasites, accidental ingestion, or contact with contaminated soil, food, water, or unpasteurized milk. 1331, 1332, 1343–1345 Colonization and hand transferral of pathogens acquired from pets in health-care workers' homes represent potential sources and modes of transmission of zoonotic pathogens in health-care settings. An outbreak of infections caused by a yeast ( Malassezia pachydermatis ) among newborns was traced to transfer of the yeast from the hands of health-care workers with pet dogs at home. 1346 In addition, an outbreak of ringworm in a NICU caused by Microsporum canis was associated with a nurse and her cat, 1347 and an outbreak of Rhodococcus (Gordona) bronchialis sternal SSIs after coronary-artery bypass surgery was traced to a colonized nurse whose dogs were culture-positive for the organism. 1348 In the latter outbreak, whether the dogs were the sole source of the organism and whether other environmental reservoirs contributed to the outbreak are unknown. Nonetheless, limited data indicate that outbreaks of infectious disease have occurred as a result of contact with animals in areas housing immunocompetent patients. However, the low frequency of outbreaks may result from
- the relatively limited presence of the animals in health-care facilities and
- the immunocompetency of the patients involved in the encounters.
Formal scientific studies to evaluate potential risks of transmission of zoonoses in health-care settings outside of the laboratory are lacking.
2. Animal-Assisted Activities, Animal-Assisted Therapy, and Resident Animals
Animal-Assisted Activities (AAA) are those programs that enhance the patients' quality of life. These programs allow patients to visit animals in either a common, central location in the facility or in individual patient rooms. A group session with the animals enhances opportunities for ambulatory patients and facility residents to interact with caregivers, family members, and volunteers. 1349–1351 Alternatively, allowing the animals access to individual rooms provides the same opportunity to non-ambulatory patients and patients for whom privacy or dignity issues are a consideration. The decision to allow this access to patients' rooms should be made on a case-by-case basis, with the consultation and consent of the attending physician and nursing staff.
Animal-Assisted Therapy (AAT) is a goal-directed intervention that incorporates an animal into the treatment process provided by a credentialed therapist. 1330, 1331 The concept for AAT arose from the observation that some patients with pets at home recover from surgical and medical procedures more rapidly than patients without pets. 1352, 1353 Contact with animals is considered beneficial for enhancing wellness in certain patient populations (e.g., children, the elderly, and extended-care hospitalized patients). 1349, 1354–1357 However, evidence supporting this benefit is largely derived from anecdotal reports and observations of patient/animal interactions. 1357–1359 Guidelines for establishing AAT programs are available for facilities considering this option. 1360
The incorporation of non-human primates into an AAA or AAT program is not encouraged because of concerns regarding potential disease transmission from and unpredictable behavior of these animals. 1361, 1362 Animals participating in either AAA or AAT sessions should be in good health and up-to-date with recommended immunizations and prophylactic medications (e.g., heartworm prevention) as determined by a licensed veterinarian based on local needs and recommendations. Regular re-evaluation of the animal's health and behavior status is essential. 1360 Animals should be routinely screened for enteric parasites and/or have evidence of a recently completed antihelminthic regimen. 1363 They should also be free of ectoparasites (e.g., fleas and ticks) and should have no sutures, open wounds, or obvious dermatologic lesions that could be associated with bacterial, fungal, or viral infections or parasitic infestations. Incorporating young animals (i.e., those aged <1 year) into these programs is not encouraged because of issues regarding unpredictable behavior and elimination control. Additionally, health of these animals at risk. Animals should be clean and well-groomed. The visits must be supervised by persons who know the animals and their behavior. Animal handlers should be trained in these activities and receive site-specific orientation to ensure that they work efficiently with the staff in the specific health-care environment. 1360 Additionally, animal handlers should be in good health. 1360
The most important infection-control measure to prevent potential disease transmission is strict enforcement of hand-hygiene measures (e.g., using either soap and water or an alcohol-based hand rub) for all patients, staff, and residents after handling the animals. 1355, 1364 Care should also be taken to avoid direct contact with animal urine or feces. Clean-up of these substances from environmental surfaces requires gloves and the use of leak-resistant plastic bags to discard absorbent material used in the process. 2 The area must be cleaned after visits according to standard cleaning procedures.
The American Academy of Allergy, Asthma, and Immunology estimates that dog or cat allergies occur in approximately 15% of the population. 1365 Minimizing contact with animal saliva, dander, and/or urine helps to mitigate allergic responses. 1365–1367 Some facilities may not allow animal visitation for patients with
- underlying asthma,
- known allergies to cat or dog hair,
- respiratory allergies of unknown etiology, and
- immunosuppressive disorders.
Hair shedding can be minimized by processes that remove dead hair (e.g., grooming) and that prevent the shedding of dead hair (e.g., therapy capes for dogs). Allergens can be minimized by bathing therapy animals within 24 hours of a visit. 1333, 1368
Animal therapists and handlers must take precautions to prevent animal bites. Common pathogens associated with animal bites include Capnocytophaga canimorsus, Pasteurella spp., Staphylococcus spp., and Streptococcus spp. Selecting well-behaved and well-trained animals for these programs greatly decreases the incidence of bites. Rodents, exotic species, wild/domestic animals (i.e., wolf-dog hybrids), and wild animals whose behavior is unpredictable should be excluded from AAA or AAT programs. A well-trained animal handler should be able to recognize stress in the animal and to determine when to terminate a session to minimize risk. When an animal bites a person during AAA or AAT, the animal is to be permanently removed from the program. If a bite does occur, the wound must be cleansed immediately and monitored for subsequent infection. Most infections can be treated with antibiotics, and antibiotics often are prescribed prophylactically in these situations.
The health-care facility's infection-control staff should participate actively in planning for and coordinating AAA and AAT sessions. Many facilities do not offer AAA or AAT programs for severely immunocompromised patients (e.g., HSCT patients and patients on corticosteroid therapy). 1339 The question of whether family pets or companion animals can visit terminally-ill HSCT patients or other severely immunosuppressed patients is best handled on a case-by-case basis, although animals should not be brought into the HSCT unit or any other unit housing severely immunosuppressed patients. An in-depth discussion of this issue is presented elsewhere. 1366
Immunocompromised patients who have been discharged from a health-care facility may be at higher risk for acquiring some pet-related zoonoses. Although guidelines have been developed to minimize the risk of disease transmission to HIV-infected patients, 8 these recommendations may be applicable for patients with other immunosuppressive disorders. In addition to handwashing or hand hygiene, these recommendations include avoiding contact with
- animal feces and soiled litter box materials,
- animals with diarrhea,
- very young animals (i.e., dogs <6 months of age and cats <1 year of age), and
- exotic animals and reptiles. 8
Pets or companion animals with diarrhea should receive veterinary care to resolve their condition.
Many health-care facilities are adopting more home-like environments for residential-care or extended-stay patients in acute-care settings, and resident animals are one element of this approach. 1369 One concept, the "Eden Alternative," incorporates children, plants, and animals (e.g., dogs, cats, fish, birds, rabbits, and rodents) into the daily care setting. 1370, 1371 The concept of working with resident animals has not been scientifically evaluated. Several issues beyond the benefits of therapy must be considered before embarking on such a program, including
- whether the animals will come into direct contact with patients and/or be allowed to roam freely in the facility
- how the staff will provide care for the animals;
- the management of patients’ or residents’ allergies, asthma, and phobias;
- precautionary measures to prevent bites and scratches; and
- measures to properly manage the disposal of animal feces and urine, thereby preventing environmental contamination by zoonotic microorganisms (e.g., Toxoplasma spp. , Toxocara spp., and Ancylostoma spp.). 1372, 1373
Few data document a link between health-care acquired infection rates and frequency of cleaning fish tanks or rodent cages. Skin infections caused by Mycobacterium marinum have been described among persons who have fish aquariums at home. 1374, 1375 Nevertheless, immunocompromised patients should avoid direct contact with fish tanks and cages and the aerosols that these items produce. Further, fish tanks should be kept clean on a regular basis as determined by facility policy, and this task should be performed by gloved staff members who are not responsible for patient care. The use of the infection-control risk assessment can help determine whether a fish tank poses a risk for patient or resident safety and health in these situations. No evidence, however, links the incidence of health-care acquired infections among immunocompetent patients or residents with the presence of a properly cleaned and maintained fish tank, even in dining areas. As a general preventive measure, resident animal programs are advised to restrict animals from
- food preparation kitchens,
- central sterile supply and any storage areas for clean supplies, and
- medication preparation areas.
Resident-animal programs in acute-care facilities should not allow the animals into the isolation areas, protective environments, ORs, or any area where immunocompromised patients are housed. Patients and staff routinely should wash their hands or use waterless, alcohol-based hand-hygiene products after contact with animals.
3. Service Animals
Although this section provides an overview about service animals in health-care settings, it cannot address every situation or question that may arise (see Appendix E – Information Resources). A service animal is any animal individually trained to do work or perform tasks for the benefit of a person with a disability. 1366, 1376 A service animal is not considered a pet but rather an animal trained to provide assistance to a person because of a disability. Title III of the "Americans with Disabilities Act" (ADA) of 1990 mandates that persons with disabilities accompanied by service animals be allowed access with their service animals into places of public accommodation, including restaurants, public transportation, schools, and health-care facilities. 1366, 1376 In health-care facilities, a person with a disability requiring a service animal may be an employee, a visitor, or a patient.
An overview of the subject of service animals and their presence in health-care facilities has been published. 1366 No evidence suggests that animals pose a more significant risk of transmitting infection than people; therefore, service animals should not be excluded from such areas, unless an individual patient's situation or a particular animal poses greater risk that cannot be mitigated through reasonable measures. If health-care personnel, visitors, and patients are permitted to enter care areas (e.g., inpatient rooms, some ICUs, and public areas) without taking additional precautions to prevent transmission of infectious agents (e.g., donning gloves, gowns, or masks), a clean, healthy, well-behaved service animal should be allowed access with its handler. 1366 Similarly, if immunocompromised patients are able to receive visitors without using protective garments or equipment, an exclusion of service animals from this area would not be justified. 1366
Because health-care facilities are covered by the ADA or the Rehabilitation Act, a person with a disability may be accompanied by a service animal within the facility unless the animal's presence or behavior creates a fundamental alteration in the nature of a facility's services in a particular area or a direct threat to other persons in a particular area. 1366 A "direct threat" is defined as a significant risk to the health or safety of others that cannot be mitigated or eliminated by modifying policies, practices, or procedures. 1376 The determination that a service animal poses a direct threat in any particular healthcare setting must be based on an individualized assessment of the service animal, the patient, and the health-care situation. When evaluating risk in such situations, health-care personnel should consider the nature of the risk (including duration and severity); the probability that injury will occur; and whether reasonable modifications of policies, practices, or procedures will mitigate the risk (J. Wodatch, U.S. Department of Justice, 2000). The person with a disability should contribute to the risk-assessment process as part of a pre-procedure health-care provider/patient conference.
Excluding a service animal from an OR or similar special care areas (e.g., burn units, some ICUs, PE units, and any other area containing equipment critical for life support) is appropriate if these areas are considered to have "restricted access" with regards to the general public. General infection-control measures that dictate such limited access include
- the area is required to meet environmental criteria to minimize the risk of disease transmission,
- strict attention to hand hygiene and absence of dermatologic conditions, and
- barrier protective measures [e.g., using gloves, wearing gowns and masks] are indicated for persons in the affected space.
No infection-control measures regarding the use of barrier precautions could be reasonably imposed on the service animal. Excluding a service animal that becomes threatening because of a perceived danger to its handler during treatment also is appropriate; however, exclusion of such an animal must be based on the actual behavior of the particular animal, not on speculation about how the animal might behave.
Another issue regarding service animals is whether to permit persons with disabilities to be accompanied by their service animals during all phases of their stay in the health-care facility. Healthcare personnel should discuss all aspects of anticipatory care with the patient who uses a service animal. Health-care personnel may not exclude a service animal because health-care staff may be able to perform the same services that the service animal does (e.g., retrieving dropped items and guiding an otherwise ambulatory person to the restroom). Similarly, health-care personnel can not exclude service animals because the health-care staff perceive a lack of need for the service animal during the person's stay in the health-care facility. A person with a disability is entitled to independent access (i.e., to be accompanied by a service animal unless the animal poses a direct threat or a fundamental alteration in the nature of services); "need" for the animal is not a valid factor in either analysis. For some forms of care (e.g., ambulation as physical therapy following total hip replacement or knee replacement), the service animal should not be used in place of a credentialed health-care worker who directly provides therapy. However, service animals need not be restricted from being in the presence of its handler during this time; in addition, rehabilitation and discharge planning should incorporate the patient's future use of the animal. The health-care personnel and the patient with a disability should discuss both the possible need for the service animal to be separated from its handler for a period of time during non-emergency care and an alternate plan of care for the service animal in the event the patient is unable or unwilling to provide that care. This plan might include family members taking the animal out of the facility several times a day for exercise and elimination, the animal staying with relatives, or boarding off-site. Care of the service animal, however, remains the obligation of the person with the disability, not the health-care staff.
Although animals potentially carry zoonotic pathogens transmissible to man, the risk is minimal with a healthy, clean, vaccinated, well-behaved, and well-trained service animal, the most common of which are dogs and cats. No reports have been published regarding infectious disease that affects humans originating in service dogs. Standard cleaning procedures are sufficient following occupation of an area by a service animal. 1366 Clean-up of spills of animal urine, feces, or other body substances can be accomplished with blood/body substance procedures outlined in the Environmental Services section of this guideline. No special bathing procedures are required prior to a service animal accompanying its handler into a health-care facility.
Providing access to exotic animals (e.g., reptiles and non-human primates) that are used as service animals is problematic. Concerns about these animals are discussed in two published reviews. 1331, 1366 Because some of these animals exhibit high-risk behaviors that may increase the potential for zoonotic disease transmission (e.g., herpes B infection), providing health-care facility access to nonhuman primates used as service animals is discouraged, especially if these animals might come into contact with the general public. 1361, 1362 Health-care administrators should consult the Americans with Disabilities Act for guidance when developing policies about service animals in their facilities. 1366, 1376
Requiring documentation for access of a service animal to an area generally accessible to the public would impose a burden on a person with a disability. When health-care workers are not certain that an animal is a service animal, they may ask the person who has the animal if it is a service animal required because of a disability; however, no certification or other documentation of service animal status can be required. 1377
4. Animals as Patients in Human Health-Care Facilities
The potential for direct and indirect transmission of zoonoses must be considered when rooms and equipment in human health-care facilities are used for the medical or surgical treatment or diagnosis of animals. 1378 Inquiries should be made to veterinary medical professionals to determine an appropriate facility and equipment to care for an animal.
The central issue associated with providing medical or surgical care to animals in human health-care facilities is whether cross-contamination occurs between the animal patient and the human health-care workers and/or human patients. The fundamental principles of infection control and aseptic practice should differ only minimally, if at all, between veterinary medicine and human medicine. Health-care– associated infections can and have occurred in both patients and workers in veterinary medical facilities when lapses in infection-control procedures are evident. 1379–1384 Further, veterinary patients can be at risk for acquiring infection from veterinary health-care workers if proper precautions are not taken. 1385
The issue of providing care to veterinary patients in human health-care facilities can be divided into the following three areas of infection-control concerns:
- whether the room/area used for animal care can be made safe for human patients,
- whether the medical/surgical instruments used on animals can be subsequently used on human patients, and
- which disinfecting or sterilizing procedures need to be done for these purposes.
Studies addressing these concerns are lacking. However, with respect to disinfection or sterilization in veterinary settings, only minimal evidence suggests that zoonotic microbial pathogens are unusually resistant to inactivation by chemical or physical agents (with the exception of prions). Ample evidence supports the contrary observation (i.e., that pathogens from human- and animal sources are similar in their relative instrinsic resistance to inactivation). 1386–1391 Further, no evidence suggests that zoonotic pathogens behave differently from human pathogens with respect to ventilation. Despite this knowledge, an aesthetic and sociologic perception that animal care must remain separate from human care persists. Health-care facilities, however, are increasingly faced with requests from the veterinary medical community for access to human health-care facilities for reasons that are largely economical (e.g., costs of acquiring sophisticated diagnostic technology and complex medical instruments). If hospital guidelines allow treatment of animals, alternate veterinary resources (including veterinary hospitals, clinics, and universities) should be exhausted before using human health-care settings. Additionally, the hospital's public/media relations should be notified of the situation. The goal is to develop policies and procedures to proactively and positively discuss and disclose this activity to the general public.
An infection-control risk assessment (ICRA) must be undertaken to evaluate the circumstances specific to providing care to animals in a human health-care facility. Individual hospital policies and guidelines should be reviewed before any animal treatment is considered in such facilities. Animals treated in human health-care facilities should be under the direct care and supervision of a licensed veterinarian; they also should be free of known infectious diseases, ectoparasites, and other external contaminants (e.g., soil, urine, and feces). Measures should be taken to avoid treating animals with a known or suspected zoonotic disease in a human health-care setting (e.g., lambs being treated for Q fever).
If human health-care facilities must be used for animal treatment or diagnostics, the following general infection-control actions are suggested:
- whenever possible, the use of ORs or other rooms used for invasive procedures should be avoided [e.g., cardiac catheterization labs and invasive nuclear medicine areas]
- when all other space options are exhausted and use of the aforementioned rooms is unavoidable, the procedure should be scheduled late in the day as the last procedure for that particular area such that patients are not present in the department/unit/area;
- environmental surfaces should be thoroughly cleaned and disinfected using procedures discussed in the Environmental Services portion of this guideline after the animal is removed from the care area;
- sufficient time should be allowed for ACH to help prevent allergic reactions by human patients [Table B.1. in Appendix B];
- only disposable equipment or equipment that can be thoroughly and easily cleaned, disinfected, or sterilized should be used;
- when medical or surgical instruments, especially those invasive instruments that are difficult to clean [e.g., endoscopes], are used on animals, these instruments should be reserved for future use only on animals; and g) standard precautions should be followed.
5. Research Animals in Health-Care Facilities
The risk of acquiring a zoonotic infection from research animals has decreased in recent years because many small laboratory animals (e.g., mice, rats, and rabbits) come from quality stock and have defined microbiologic profiles. 1392 Larger animals (e.g., nonhuman primates) are still obtained frequently from the wild and may harbor pathogens transmissible to humans. Primates, in particular, benefit from vaccinations to protect their health during the research period provided the vaccination does not interfere with the study of the particular agent. Animals serving as models for human disease studies pose some risk for transmission of infection to laboratory or health-care workers from percutaneous or mucosal exposure. Exposures can occur either through
- direct contact with an infected animal or its body substances and secretions or
- indirect contact with infectious material on equipment, instruments, surfaces, or supplies. 1392
Uncontained aerosols generated during laboratory procedures can also transmit infection.
Infection-control measures to prevent transmission of zoonotic infections from research animals are largely derived from the following basic laboratory safety principles:
- purchasing pathogen-free animals,
- quarantining incoming animals to detect any zoonotic pathogens,
- treating infected animals or removing them from the facility,
- vaccinating animal carriers and high-risk contacts if possible,
- using specialized containment caging or facilities, and
- using protective clothing and equipment [e.g., gloves, face shields, gowns, and masks]. 1392
An excellent resource for detailed discussion of these safety measures has been published. 1013
The animal research unit within a health-care facility should be engineered to provide
- adequate containment of animals and pathogens;
- daily decontamination and transport of equipment and waste;
- proper ventilation and air filtration, which prevents recirculation of the air in the unit to other areas of the facility; and
- negative air pressure in the animal rooms relative to the corridors.
To ensure adequate security and containment, no through traffic to other areas of the health-care facility should flow through this unit; access should be restricted to animal-care staff, researchers, environmental services, maintenance, and security personnel.
Occupational health programs for animal-care staff, researchers, and maintenance staff should take into consideration the animals' natural pathogens and research pathogens. Components of such programs include
- prophylactic vaccines,
- TB skin testing when primates are used,
- baseline serums, and
- hearing and respiratory testing.
Work practices, PPE, and engineering controls specific for each of the four animal biosafety levels have been published.1013, 1393 The facility's occupational or employee health clinic should be aware of the appropriate post-exposure procedures involving zoonoses and have available the appropriate post-exposure biologicals and medications.
Animal-research-area staff should also develop standard operating procedures for
- daily animal husbandry [e.g., protection of the employee while facilitating animal welfare]
- pathogen containment and decontamination;
- management, cleaning, disinfecting and/or sterilizing equipment and instruments; and
- employee training for laboratory safety and safety procedures specific to animal research worksites.1013
The federal Animal Welfare Act of 1966 and its amendments serve as the regulatory basis for ensuring animal welfare in research.1394, 1395
- Reptiles include lizards, snakes, and turtles. Rodents include hamsters, mice, and rats.
Infection Control
CDC provides information on infection control and clinical safety to help reduce the risk of infections among healthcare workers, patients, and visitors.
For Everyone
Health care providers, public health.
- Open access
- Published: 13 May 2024
Assessment of tumor hypoxia in spontaneous canine tumors after treatment with OMX, a novel H-NOX oxygen carrier, with [ 18 F]FMISO PET/CT
- Sangkyung Choen 1 ,
- Michael S. Kent 1 ,
- F. Alexandra Loucks 2 ,
- Jonathan A. Winger 2 &
- Allison L. Zwingenberger 1
BMC Veterinary Research volume 20 , Article number: 196 ( 2024 ) Cite this article
169 Accesses
1 Altmetric
Metrics details
Hypoxia is a detrimental factor in solid tumors, leading to aggressiveness and therapy resistance. OMX, a tunable oxygen carrier from the heme nitric oxide/oxygen-binding (H-NOX) protein family, has the potential to reduce tumor hypoxia. [ 18 F]Fluoromisonidazole ([ 18 F]FMISO) positron emission tomography (PET) is the most widely used and investigated method for non-invasive imaging of tumor hypoxia. In this study, we used [ 18 F]FMISO PET/CT (computed tomography) to assess the effect of OMX on tumor hypoxia in spontaneous canine tumors.
Thirteen canine patients with various tumors ( n = 14) were randomly divided into blocks of two, with the treatment groups alternating between receiving intratumoral (IT) OMX injection (OMX IT group) and intravenous (IV) OMX injection (OMX IV group). Tumors were regarded as hypoxic if maximum tumor-to-muscle ratio (TMR max ) was greater than 1.4. In addition, hypoxic volume (HV) was defined as the region with tumor-to-muscle ratio greater than 1.4 on [ 18 F]FMISO PET images. Hypoxia was detected in 6/7 tumors in the OMX IT group and 5/7 tumors in the OMX IV injection group. Although there was no significant difference in baseline hypoxia between the OMX IT and IV groups, the two groups showed different responses to OMX. In the OMX IV group, hypoxic tumors ( n = 5) exhibited significant reductions in tumor hypoxia, as indicated by decreased TMR max and HV in [ 18 F]FMISO PET imaging after treatment. In contrast, hypoxic tumors in the OMX IT group ( n = 6) displayed a significant increase in [ 18 F]FMISO uptake and variable changes in TMR max and HV.
Conclusions
[ 18 F]FMISO PET/CT imaging presents a promising non-invasive procedure for monitoring tumor hypoxia and assessing the efficacy of hypoxia-modulating therapies in canine patients. OMX has shown promising outcomes in reducing tumor hypoxia, especially when administered intravenously, as evident from reductions in both TMR max and HV in [ 18 F]FMISO PET imaging.
Peer Review reports
Hypoxia, a partial oxygen pressure (pO 2 ) below physiological demand, is a common feature of most solid tumors, with its development typically attributed to two factors: diffusion-limited and perfusion-limited oxygen delivery [ 1 , 2 ]. These arise due to aberrant tumor vasculature, disrupted blood flow, and elevated oxygen consumption by rapidly proliferating tumor cells [ 2 , 3 ]. Tumor hypoxia has been closely correlated with unfavorable prognosis, exhibiting an aggressive phenotype, increased risk of invasion and metastasis, and resistance to chemotherapy and radiotherapy [ 3 , 4 ].
Reducing tumor hypoxia may therefore enhance the efficacy of tumor treatment [ 2 ].
OMX is a novel tunable oxygen carrier derived from the heme nitric oxide/oxygen-binding (H-NOX) protein family. OMX has previously been shown to be well-tolerated, attenuate hypoxia-induced myocardial dysfunction in lambs during acute global hypoxia [ 5 ] and preserve ischemic brain tissue in a canine model of acute ischemic stroke [ 6 ]. Preliminary studies in mouse tumor models have also indicated that OMX is long-lasting in circulation and tumors, and it penetrates deep into tumor tissue reducing hypoxia and altering the hypoxic phenotype by downregulating the hypoxia-inducible factor 1 alpha (HIF-1α) pathway [ 7 , 8 , 9 ]. In a preclinical study in tumor-bearing mice, the administration of OMX resulted in a reduction in hypoxic tumor area, and coupling OMX with radiation therapy led to an approximately 3-fold extension in both tumor growth delay and survival time [ 9 ]. Another study showed that OMX reduces hypoxia levels and thereby reverses the immunosuppressive tumor microenvironment in GL261 tumor-bearing mice [ 8 ]. These results indicated OMX may be a promising treatment for reducing hypoxia in spontaneous tumors.
Several methods exist to measure hypoxia directly or indirectly. The “gold standard” uses polarographic electrode needles that allow direct measurement of the pO 2 [ 3 , 4 ]. This method, however, is invasive and can only be used in superficial tumors. Consequently, non-invasive approaches are necessary to detect the distribution of hypoxic cancer cells within the body. One such advanced technique is positron emission tomography (PET), which enables a 3-dimensional quantitative assessment of vascular, molecular, and cellular oxygen changes in hypoxic tumors using hypoxia-imaging probes [ 1 , 4 ]. [ 18 F]Fluoromisonidazole ([ 18 ]FMISO) is the most widely used radiolabeled imaging tracer for hypoxia among several others [ 4 , 10 ]. It is a lipophilic compound that diffuses passively into the tissue and undergoes initial reduction via nitroreductases. When oxygen is abundant, in normally oxygenated cells, the parent compound is quickly regenerated by reoxidation and can diffuse out of the cells [ 10 ]. However, in hypoxic cells, the low pO 2 prevents reoxidation of [ 18 F]FMISO metabolites, leading to the accumulation of the tracer. Consequently, [ 18 F]FMISO PET imaging provides the opportunity to measure hypoxia noninvasively and monitor the magnitude and 3-dimensional pattern within patients sequentially over time during treatment [ 4 , 11 ].
Our previous study demonstrated the feasibility of hypoxia PET/CT (computed tomography) imaging to detect and quantify the extent of hypoxia in a variety of spontaneous canine tumors [ 4 ]. To the authors’ knowledge, no study has assessed and monitored the response of spontaneous canine tumors to hypoxia-modulating drugs using [ 18 F]FMISO PET/CT. The objectives of this study were to determine whether [ 18 F]FMISO PET/CT can be used to monitor tumor hypoxia before and after OMX administration and to assess the efficacy of intratumoral (IT) and intravenous (IV) OMX administration methods in reducing tumor hypoxia in spontaneous canine tumors. We hypothesized that [ 18 F]FMISO PET/CT imaging provides a valuable method for monitoring tumor hypoxia during treatment and that OMX decreases tumor hypoxia, potentially leading to an improved response to radiotherapy.
Patient and tumor characteristics
A total of 13 canine patients were enrolled in this study. The enrolled animals were randomly divided into blocks of two, with the treatment groups alternating between receiving IT OMX injection (OMX IT) and IV OMX injection (OMX IV). However, one dog (Dog 8) was reassigned to the OMX IV group due to suspected metastasis in the abdominal lymph node, precluding intra-tumoral treatment given its anatomical location within a concealed body cavity. The dogs represented various breeds and had an age range of 9 to 15 years (mean ± SD, 12 ± 2.3 years). Six were female (5 spayed) and seven were neutered male. The weights of the dogs ranged from 8.1 kg to 43 kg (mean ± SD, 28.9 ± 10.3 kg). Table 1 provides detailed information about the canine patients, including tumor location and volume, as well as histocytological diagnosis within the OMX IV and OMX IT groups. All tumors were histologically confirmed, with the exception of one tumor (IV 1). We confirmed the presence of metastasis in the lymph node of dog 8 with hepatoid gland carcinoma, and included this tumor in our analysis.
[ 18 F]FMISO distribution and static PET analyses
The injected dose of [ 18 F]FMISO ranged from 54 to 227 MBq (4.6–5.5 MBq/kg), and there was no statistically significant difference in the injected dose between the [ 18 F]FMISO PET/CT scans before OMX injection ([ 18 F]FMISO Pre−OMX ) and [ 18 F]FMISO PET/CT scans 24 h after OMX injection ([ 18 F]FMISO Post−OMX ). The results of [ 18 F]FMISO PET image analysis for all hypoxic tumors are presented in Table 2 .
Tumor hypoxia was detected in 6 out of 7 tumors in the OMX IT group and 5 out of 7 tumors in the OMX IV group. Dogs 3, 12, and 13 were excluded from the analysis because their lesions were non-hypoxic or diagnosed as benign upon histological evaluation. No significant differences were observed in maximum standardized uptake value (SUV max ), maximum tumor-to-muscle ratio (TMR max ), tumor volume (TV), and hypoxic volume (HV) between hypoxic tumors in each group prior to treatment. When correlations among all analyzed values were investigated in hypoxic tumors ( n = 11) before treatment, only TMR max showed the strongest correlation with HV (rho = 0.87, p < 0.001).
After treatment, SUV max decreased in most hypoxic tumors (4/5) in the OMX IV group, but it was not statistically significant due to the small sample size, whereas all hypoxic tumors ( n = 6) in the OMX IT group showed an increase in SUV max . In the OMX IT group, no significant changes were observed in TMR max and HV after treatment (Fig. 1 ), although dog 4 (IT 4) showed a substantial decrease in hypoxic volume despite an increased TMR max . Interestingly, IT 3 exhibited multifocal hypoxic regions in an area that was suspected to correspond with the locations of the IT injections (Fig. 1 . middle row).
[ 18 F]FMISO PET images of canine spontaneous tumors before (left) and 24 h after (right) OMX Intratumoral (IT) injection. Hypoxic tumors (arrows) displayed heterogeneous distribution and increased uptake of [ 18 F]FMISO after treatment. Dog 4 showed multifocal regions of increased [ 18 F]FMISO uptake (dashed circle), suspected to be at the injection site locations. Dog 2 (top): soft tissue sarcoma in the abdominal wall. Dog 4 (middle): Soft tissue sarcoma in the pelvic limb. Dog 7 (bottom): squamous cell carcinoma in the mandible
In the OMX IV group, all hypoxic tumors ( n = 5) showed a reduction in both TMR max and HV ( p < 0.05) (Fig. 2 ). However, for IV 1 and IV 3, the reduction in tumor hypoxia was not as pronounced due to their lower baseline TMR max (< 1.6) and smaller initial hypoxic volumes (< 1 cm 3 ) compared to the rest. Following treatment, the change in HV ranged from − 100% to -8.6% (mean: -53.8%) in the OMX IV group and from − 57.6 to 132.2% (mean: 15%) in the OMX IT group.
[ 18 F]FMISO PET images of canine spontaneous tumors before (left) and 24 h after (right) OMX intravenous (IV) injection. Hypoxic tumors (arrows) displayed decreased [ 18 F]FMISO uptake and HV after treatment. Dog 9 (top): soft tissue sarcoma in the thoracic limb. Dog 10 (middle): adenocarcinoma in the nasal cavity. Dog 11 (bottom): carcinoma in lung
Several clinical studies have consistently demonstrated that tumor hypoxia is related to an unfavorable prognosis across various tumor types, resulting in adverse outcomes such as poor locoregional control, disease-free survival, and overall survival [ 3 , 4 , 10 , 12 ]. The detection and assessment of tumor hypoxia have become crucial steps in the validation and development of hypoxia-modulating treatments, ultimately leading to their integration into standard clinical practice [ 3 ]. A practical, reliable, and consistently replicable method for detecting and measuring hypoxia could improve patient outcomes by enabling the selection of more suitable therapies to counter the impact of hypoxia or by facilitating patient classification for more precise prognostic assessments [ 10 ]. In this regard, hypoxia PET imaging has gained prominence, as it allows visualization of the hypoxic status across the entire tumor and associated lesions in cases of metastatic or locally advanced cancer, offering a repeatable, 3-dimensional depiction of hypoxia that is not achievable with electrode- or biopsy-based methods [ 4 ]. [ 18 F]FMISO PET is the most widely used and investigated method for non-invasive imaging of tumor hypoxia in multiple studies both in animals and humans [ 3 , 4 , 10 , 12 , 13 ]. Additionally, recent studies have demonstrated the high reproducibility of intratumor distributions of [ 18 F]FMISO, confirming its suitability for delineating HVs for dose escalation, patient stratification in hypoxia-targeted therapies, and monitoring therapeutic response [ 14 , 15 ]. For small tumor metastases, integrating [ 18 F]FMISO imaging with [ 18 F] fluorodeoxyglucose ([ 18 F]FDG) PET scans and post-contrast CT scans could provide a more detailed assessment, thereby improving the development of targeted treatment strategies in a clinical setting [ 16 , 17 ].
To our knowledge, this is the first study to assess and monitor the response of spontaneous canine tumors to hypoxia-modulating drugs using [ 18 F]FMISO PET/CT imaging. In this study, we investigated the potential of [ 18 F]FMISO PET imaging for monitoring tumor hypoxia, as well as the efficacy of IT and IV OMX administration methods in reducing tumor hypoxia. Hypoxic metrics including SUV max , TMR max , and HV were employed to evaluate changes in tumor hypoxia before and after OMX-4.80P treatment. These metrics possess independent and robust prognostic value in hypoxia PET imaging and have been associated with a poor prognosis [ 10 , 12 , 15 ]. While the precise quantitative relationship between [ 18 F]FMISO uptake and pO 2 remains to be fully elucidated, a study reported a strong correlation between the TMR max obtained from [ 18 F]FMISO PET scans after 2 h and the different parameters of the hypoxic fraction, which were measured using polarographic needle electrodes [ 18 ]. Additionally, our previous [ 18 F]FMISO study demonstrated that TMR max is comparable to hypoxic kinetic parameters in spontaneous canine tumors [ 4 ]. Furthermore, there has been a strong relationship between HV defined with [ 18 F]FMISO PET and the volumes derived from pimonidazole and carbonic anhydrase IX immunohistochemical staining [ 13 ]. In a previous study involving head and neck cancer patients, the hypoxia PET parameters (SUV max and TMR max ) showed a moderate correlation with TV, and the strongest correlation was observed with HV [ 12 ]. However, in this study, only TMR max exhibited the strongest correlation with HV. The inclusion of a variety of spontaneous tumors, rather than being restricted to a specific type of lesion, might account for these different results.
The results of this study revealed that the OMX IV group exhibited a significant reduction in tumor hypoxia, as confirmed by a decrease in both TMR max and HV on [ 18 F]FMISO PET imaging, which is consistent with a preclinical study conducted in multiple orthotopic and immunocompetent mouse and rat models of glioblastoma, as well as in spontaneous canine brain tumors in veterinary patients [ 7 , 8 , 9 ]. The administration of OMX in mice with individual orthotopic glioblastoma tumors resulted in a reduction of over 50% in the hypoxic tumor area, as evidenced by immunostaining with glucose transporter 1 (Glut1) and HIF-1α markers [ 9 ]. Despite the inclusion of various tumor types and sizes in this study, the IV group exhibited similar outcomes, with an average reduction in tumor hypoxia of approximately 54%.
Before OMX treatment, no significant differences were observed in TV and hypoxic measures between the hypoxic tumors in each group. However, despite this, the OMX IT group displayed heterogeneous alternations in tumor hypoxia. The OMX IT injection was administered at a rate of 0.5 mg/cm² (20 µl/cm²) to the tumors. However, tumors with considerable depth, in contrast to those with diffuse infiltration, exhibited a smaller tumor surface area despite their larger volume, leading to a relatively lower quantity of OMX administered. It is also noteworthy that the use of a 25-gauge needle with a length of 16 mm for the IT injection of OMX may be insufficient to adequately diffuse the drug into the deep hypoxic areas of large tumors. Furthermore, the majority of tumors in the IT group were soft tissue sarcomas, while those in the IV group predominantly consisted of carcinomas. These distinct tumor types in each group might have contributed to variations in the treatment efficacy. Finally, a separate study reported a transient increase in hypoxia levels following IT injection, with levels rising from 18 to 70%, particularly in the tumor cells located along the path of the needle [ 19 ]. In the present study, IT 3 exhibited multifocal hypoxic regions, suspected to correspond to the locations of the IT injections.
The present study has several limitations. First, this prospective randomized clinical trial included a small number of patients and differences in the major tumor types between the IT and IV OMX groups, resulting in the failure to compare and detect a statistically significant difference between the OMX IT and OMX IV groups. Additionally, Dog 8, which presented with a metastatic carcinoma in an abdominal cavity, was reassigned to the OMX IV group. The metastasis rate can vary depending on the types of cancers, but generally, carcinomas may exhibit a higher metastasis rate compared to soft tissue sarcomas, which could contribute to the difference in the major tumor types between groups [ 20 ]. Second, there are limited clinical data, and no reports are available on the reproducibility of [ 18 F]FMISO PET scans in spontaneous canine tumors [ 14 , 15 ]. Further research is essential to investigate and reduce the variability in PET hypoxia measurements, with the aim of providing greater clarity and accuracy in the quantification of tumor hypoxia. Third, while oxygen electrodes are often considered the gold standard for tumor hypoxia measurement, this study did not incorporate this invasive technique, which could be limiting in a veterinary clinical trial involving client-owned dogs, as well as potentially leading to transient increases in hypoxia levels [ 19 ]. Fourth, canine patients were maintained under anesthesia using 1–2% isoflurane in 100% oxygen. Previous studies have found that the introduction of 100% oxygen or anesthetics reduced the [ 18 F]FMISO TMR in CaNT-bearing CBA mice, while CT26 colorectal carcinoma-bearing mice exhibited higher TMR when breathing air compared to following 100% oxygen breathing protocols [ 4 ]. Finally, given the limited number of canine patients enrolled, there was no control group for either IT or IV administration, and therefore no ability to compare OMX-dependent changes in tumor hypoxia over 24 h to naturally-occurring changes in tumor hypoxia over that same time period.
The use of [ 18 F]FMISO PET/CT imaging presents a promising non-invasive method for monitoring tumor hypoxia and assessing the efficacy of hypoxia-modulating therapies in canine patients, which may facilitate the development of more individualized treatment strategies for patients afflicted with hypoxic tumors. OMX exhibited promising results in the reduction of tumor hypoxia, particularly in the IV injection group, as indicated by significant reductions in both TMR max and HV on [ 18 F]FMISO PET imaging. These findings are consistent with preclinical studies conducted in various animal models, highlighting the potential efficacy of OMX in reducing tumor hypoxia and the potential benefit of using [ 18 F]FMISO PET imaging to stratify patient selection for therapeutic treatment based on baseline tumor hypoxia levels.
Patient population
This was a prospective clinical observational study involving companion dogs that were referred to the University of California, Davis Veterinary Medical Teaching Hospital for evaluation and treatment of spontaneous tumors. The research protocol was approved by the UC Davis Animal Care and Use Committee and Veterinary Clinical Trial Review Board (protocol number 22,126). Additionally, all dog owners signed a provided written informed consent form. All dogs enrolled in this study had at least one spontaneous primary tumor located in the head, lung, body wall, or limb. The inclusion criteria were as follows: solid tumors confirmed through tissue biopsy or fine needle aspiration with measurable disease by caliper or previous imaging; body weight greater than 5 kg; absence of critically concomitant systemic diseases (diabetes, liver failure, or renal failure); and no previous history of radiation therapy to the anatomic area. The sample size for this study was determined based on the sample size of our previous study, and as a result, we planned to recruit 14 dog patients [ 4 ].
OMX treatment
While the patients were under anesthesia, OMX (25 mg/ml) was administered either through IV injection at a dose of 100 mg/kg given over 40 min or via IT injection dosed at 0.5 mg/cm 2 (20 µl/cm 2 ) of the tumor once following the first PET scan. For IT injections a 1 cm grid was placed over the tumor and 20µls of OMX was injected into each cm 3 of tumor volume using a 25 gauge needle and a 1 cc syringe. The intravenous dose of 100 mg/kg was chosen based on preliminary preclinical efficacy data in mouse and canine tumor models (unpublished data). The intra-tumoral dose was selected based on maximum feasible dose/cm 2 of tumor area. Dogs were recovered from anesthesia and monitored for any adverse events.
Imaging procedure
PET/CT imaging was performed using a Mini-EXPLORER II (United Imaging Healthcare, Shanghai, China) PET/CT scanner [ 21 ]. Patients underwent two FMISO PET/CT scans: [ 18 F]FMISO Pre−OMX PET imaging to measure [ 18 F]FMISO tumor uptake before OMX treatment and [ 18 F]FMISO Post−OMX PET imaging 24 h after OMX treatment. Canine patients fasted for at least 12 h prior to the scan and were injected intravenously with [ 18 F]FMISO, 2 h prior to PET/CT imaging. The dogs were premedicated with midazolam and butorphanol, then induced with a bolus injection of propofol, and anesthetized with isoflurane (1–2%) in 100% oxygen via an endotracheal tube 90 min after [ 18 F]FMISO injection. To prevent the shine-through artifact caused by a highly radioactive bladder during PET scans, urinary catheterization was performed on anesthetized dogs with tumors located around the urinary bladder. A pre-contrast CT scan was obtained for attenuation correction and image analysis purposes (120 kVp,175 mA). Next, 30-minute static PET images were acquired for a single bed position centered over the tumor starting 2 h after the injection of [ 18 F]FMISO. Following this, a post-contrast CT scan was obtained 1 min after IV administration of a bolus of contrast medium (Ultravist 370) at a dose of 660 mg Iodine/kg with the use of manual injection. Immediately after completing the PET/CT imaging, the dogs were administered OMX either intravenously or intratumorally, and then awakened from anesthesia.
The second [ 18 F]FMISO PET/CT scan was performed 24 h after the administration of OMX. The same imaging procedures were repeated, with the exception of the post-contrast CT scan that followed the PET imaging. Radioactivity levels were expected to be within normal limits on the subsequent day and all dogs were scanned with a Geiger counter prior to release to ensure radioactivity was below the institutions release reading of < 2 mCi/hr at skin surface. The animals were discharged to their owner or referring service for further treatment.
All PET images were reconstructed into a 128 × 128 × 206 matrix (voxel dimensions, 2 × 2 × 2.34 mm3) using a 3D time-of-flight list-mode ordered-subset expectation maximization method provided by the scanner manufacturer (4 iterations, 20 subsets, and post-reconstruction non-local means filtering).
Volume-of-interest (VOI) definition and image analysis
All post-imaging analyses were conducted using PMOD, version 4.3 (PMOD Technologies Ltd., Zürich, Switzerland). The images of PET/CT were interpreted in an unblinded fashion by a veterinarian with 7 years of diagnostic imaging experience. Considering that the main aim of this study was not to compare diagnostic performance, but rather to conduct a quantitative analysis between the two scans, the unblinded interpretation of the imaging likely did not introduce interpretation bias. To quantitatively evaluate [ 18 F]FMISO radioactivity, VOIs were placed to cover the entire tumor and non-hypoxic reference tissue. Using the fused PET/CT images, the tumor margin on each slice was drawn manually, and contrast CT images were used for better delineation in cases where the tumor margin was unclear. For the non-hypoxic reference tissue, spherical VOIs with a radius of 10 mm were placed in the skeletal muscle on the opposite side of the tumor. The selection of muscle was determined by the tumor location: neck muscle for tumors in the head, supraspinatus muscle for tumors in the thoracic wall and lung, and gluteal muscle for tumors in the flank, anal sac, and pelvic limb.
Standardized uptake values (SUVs) and tumor-to-muscle ratio (TMR) were calculated. Tumors were regarded as hypoxic if TMR max was greater than 1.4, following a similar approach as previous canine studies [ 4 , 22 ]. In addition, HV was defined as including the voxels within the TV having a TMR greater than 1.4 on both [ 18 F]FMISO Pre−OMX and [ 18 F]FMISO Post−OMX images. The change in HV was calculated as follows: change in HV (%) = 100 × (HV post-OMX treatment - HV pre-OMX treatment)/HV pre-OMX treatment.
Statistical analysis
Data were analyzed using SPSS, version 25 (IBM Corp, NY, USA). The Mann-Whitney U tests were used to investigate intergroup differences in SUV max , TMR max , TV, and HV in the [ 18 F]FMISO Pre−OMX image. To assess the correlation between SUV measures, TV, and HV in the [ 18 F]FMISO Pre−OMX images, the Spearman’s correlation coefficient (rho) was used as the index for the correlation. The value of this coefficient ranges from 0 to 1, with a strong correlation defined as rho ≥ 0.7, a weak one as rho < 0.3, and values in between as moderate. Because of the small sample size, the Wilcoxon signed rank test was used to compare the differences in SUV max , TMR max , and HV between [ 18 F]FMISO Pre−OMX and [ 18 F]FMISO Post−OMX images in the same patient. P-values < 0.05 were considered statistically significant for all analyses.
Data availability
This article contains all the data that were created or evaluated during the research.
Sorace AG, Syed AK, Barnes SL, Quarles CC, Sanchez V, Kang H, et al. Quantitative [18F]FMISO PET imaging shows reduction of Hypoxia following Trastuzumab in a murine model of HER2 + breast Cancer. Mol Imaging Biol. 2017;19:130–7.
Article CAS PubMed PubMed Central Google Scholar
Graham K, Unger E. Overcoming tumor hypoxia as a barrier to radiotherapy, chemotherapy and immunotherapy in cancer treatment. Int J Nanomed. 2018;13:6049–58.
Article CAS Google Scholar
Walsh JC, Lebedev A, Aten E, Madsen K, Marciano L, Kolb HC. The clinical importance of assessing tumor hypoxia: relationship of tumor hypoxia to prognosis and therapeutic opportunities. Antioxid Redox Signal. 2014;21:1516–54.
Choen S, Kent MS, Chaudhari AJ, Cherry SR, Krtolica A, Zwingenberger AL. Kinetic evaluation of the Hypoxia Radiotracers [18F]FMISO and [18F]FAZA in dogs with spontaneous tumors using dynamic PET/CT imaging. Nucl Med Mol Imaging. 2023;57:16–25.
Article CAS PubMed Google Scholar
Boehme J, Le Moan N, Kameny RJ, Loucks A, Johengen MJ, Lesneski AL et al. Preservation of myocardial contractility during acute hypoxia with OMX-CV, a novel oxygen delivery biotherapeutic. PLoS Biol. 2018;16.
Shazeeb MS, King RM, Anagnostakou V, Vardar Z, Kraitem A, Kolstad J, et al. Novel oxygen carrier slows Infarct Growth in large vessel occlusion dog model based on Magnetic Resonance Imaging Analysis. Stroke. 2022;53:1363–72.
Krtolica A, Le Moan N, Getz J, Davis T, Ng S, Bedard C, et al. Abstract 3003: OMX-4.80P, a novel H-NOX oxygen carrier that oxygenates hypoxic tumors in multiple tumor models and canine cancer patients, downregulates HIF-1 pathway and increases response to radiation therapy leading to cures. Cancer Res. 2015;75(15Supplement):3003.
Article Google Scholar
Moan N, Le, Leung P, Ng S, Davis T, Liang C, Winger JW, et al. Abstract 4686: Omx a hypoxia modulator reverses the immunosuppressive glioblastoma microenvironment by stimulating T cell infiltration and activation that results in increased number of long-term survivors. Cancer Res. 2017;77(13Supplement):4686.
Krtolica A, Le Moan N, Serwer L, Yoshida Y, Ozawa T, Butowski N, et al. TUMOR-PENETRATING TUNABLE OXYGEN CARRIER, REDUCES TUMOR HYPOXIA AND DRAMATICALLY ENHANCES RADIATION THERAPY IN INTRACRANIAL MODELS OF GLIOBLASTOMA. Neuro Oncol. 2014;16:1–112.
Fleming IN, Manavaki R, Blower PJ, West C, Williams KJ, Harris AL, et al. Imaging tumour hypoxia with positron emission tomography. Br J Cancer. 2015;112:238–50.
Serganova I, Humm J, Ling C, Blasberg R. Tumor hypoxia imaging. Clin Cancer Res. 2006;12:5260–4.
Article PubMed Google Scholar
Zschaeck S, Löck S, Hofheinz F, Zips D, Saksø Mortensen L, Zöphel K, et al. Individual patient data meta-analysis of FMISO and FAZA hypoxia PET scans from head and neck cancer patients undergoing definitive radio-chemotherapy. Radiother Oncol. 2020;149:189–96.
Dubois L, Landuyt W, Haustermans K, Dupont P, Bormans G, Vermaelen P, et al. Evaluation of hypoxia in an experimental rat tumour model by [ 18F]Fluoromisonidazole PET and immunohistochemistry. Br J Cancer. 2004;91:1947–54.
Nehmeh SA, Lee NY, Schröder H, Squire O, Zanzonico PB, Erdi YE, et al. Reproducibility of Intratumor distribution of 18F-Fluoromisonidazole in Head and Neck Cancer. Int J Radiat Oncol Biol Phys. 2008;70:235–42.
Okamoto S, Shiga T, Yasuda K, Ito YM, Magota K, Kasai K, et al. High reproducibility of tumor hypoxia evaluated by 18F- fluoromisonidazole pet for head and neck cancer. J Nucl Med. 2013;54:201–7.
Bandurska-Luque A, Löck S, Haase R, Richter C, Zöphel K, Perrin R, et al. Correlation between FMISO-PET based hypoxia in the primary tumour and in lymph node metastases in locally advanced HNSCC patients. Clin Transl Radiat Oncol. 2019;15:108–12.
PubMed PubMed Central Google Scholar
Sato J, Kitagawa Y, Yamazaki Y, Hata H, Abe T, Kitamura T, et al. FMISO PET reflects the pathological findings with cervical lymph node metastasis in oral squamous cell carcinoma. J Nucl Med. 2012;53(supplement 1):392.
Google Scholar
Gagel B, Reinartz P, DiMartino E, Zimny M, Pinkawa M, Maneschi P, et al. pO2 polarography versus positron emission tomography ([ 18F] fluoromisonidazole, [18F]-2-fluoro-2′- deoxyglucose): an appraisal of radiotherapeutically relevant hypoxia. Strahlenther Onkol. 2004;180:616–22.
Olive PL, Luo C-M, Banáth JP. Local hypoxia is produced at sites of intratumour injection. Br J Cancer. 2002;86:429–35.
Biller B, Berg J, Garrett L, Ruslander D, Wearing R, Abbott B, et al. 2016 AAHA oncology guidelines for dogs and cats. J Am Anim Hosp Assoc. 2016;52:181–204.
Lv Y, Lv X, Liu W, Judenhofer MS, Zwingenberger A, Wisner E, et al. Mini EXPLORER II: a prototype high-sensitivity PET/CT scanner for companion animal whole body and human brain scanning. Phys Med Biol. 2019;64:0–12.
Bruehlmeier M, Kaser-Hotz B, Achermann R, Bley CR, Wergin M, Schubiger PA, et al. Measurement of tumor hypoxia in spontaneous canine sarcomas. Veterinary Radiol Ultrasound. 2005;46:348–54.
Download references
Acknowledgements
We thank Lisa Carstens for her assistance in the PET/CT imaging, and Emily Phenix for recruiting patients.
This study was supported by the National Cancer Institute of the National Institutes of Health under Award Number R01CA20472. This work utilized the UC Davis Comprehensive Cancer Center’s In Vivo Translational Imaging Shared Resource which is supported by the NCI Cancer Center Support Grant (CCSG; NCI P30CA093373). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and affiliations.
Department of Surgical and Radiological Sciences, School of Veterinary Medicine, University of California, 1 Shields Ave, 2112 Tupper Hall, Davis, CA, 95616, USA
Sangkyung Choen, Michael S. Kent & Allison L. Zwingenberger
Omniox, Inc., San Francisco, CA, USA
F. Alexandra Loucks & Jonathan A. Winger
You can also search for this author in PubMed Google Scholar
Contributions
SC, MSK, FAL, JAW and AZ contributed to conceptualization, study design, methodology, data interpretation, and project administration. SC, MSK, and AZ were responsible for study execution, data curation, data analysis and data visualization. SC, MSK, and AZ wrote the original draft, and FAL and JAW substantively revise it. All authors contributed to review, editing, and approval of the final manuscript.
Corresponding author
Correspondence to Allison L. Zwingenberger .
Ethics declarations
Ethics approval and consent to participate.
We confirm that all experimental protocols were reviewed and approved by the Institutional Animal Care and Use Committee (IACUC) and Veterinary Clinical Trial Review Board of the University of California Davis (#20831). We confirm that all procedures were carried out in accordance with the ARRIVE criteria. An informed consent from the owner(s) to use the animals in our study was obtained.
Consent for publication
Not applicable.
Competing interests
JAW and FAL are employees of Omniox, Inc. and hold shares/options in Omniox, Inc. JAW is eligible to receive a portion of royalties from patents relating to uses of OMX products. The other authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Choen, S., Kent, M.S., Loucks, F.A. et al. Assessment of tumor hypoxia in spontaneous canine tumors after treatment with OMX, a novel H-NOX oxygen carrier, with [ 18 F]FMISO PET/CT. BMC Vet Res 20 , 196 (2024). https://doi.org/10.1186/s12917-024-04061-4
Download citation
Received : 11 December 2023
Accepted : 06 May 2024
Published : 13 May 2024
DOI : https://doi.org/10.1186/s12917-024-04061-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Tumor hypoxia
- Oxygen carrier
- H-NOX protein
- Canine tumors
- [18F]Fluoromisonidazole ([18F]FMISO)
- Positron emission tomography (PET)
- Computed tomography (CT)
- Therapy resistance
- Non-invasive imaging
BMC Veterinary Research
ISSN: 1746-6148
- General enquiries: [email protected]
- Reference Manager
- Simple TEXT file
People also looked at
Conceptual analysis article, dogs supporting human health and well-being: a biopsychosocial approach.

- 1 Department of Psychiatry, Center for Human Animal Interaction, School of Medicine, Virginia Commonwealth University, Richmond, VA, United States
- 2 Human-Animal Bond in Colorado, School of Social Work, Colorado State University, Fort Collins, CO, United States
- 3 Department of Education, California State Polytechnic University, Pomona, CA, United States
- 4 Division of Social Sciences and Natural Sciences, Seaver College, Pepperdine University, Malibu, CA, United States
Humans have long realized that dogs can be helpful, in a number of ways, to achieving important goals. This is evident from our earliest interactions involving the shared goal of avoiding predators and acquiring food, to our more recent inclusion of dogs in a variety of contexts including therapeutic and educational settings. This paper utilizes a longstanding theoretical framework- the biopsychosocial model- to contextualize the existing research on a broad spectrum of settings and populations in which dogs have been included as an adjunct or complementary therapy to improve some aspect of human health and well-being. A wide variety of evidence is considered within key topical areas including cognition, learning disorders, neurotypical and neurodiverse populations, mental and physical health, and disabilities. A dynamic version of the biopsychosocial model is used to organize and discuss the findings, to consider how possible mechanisms of action may impact overall human health and well-being, and to frame and guide future research questions and investigations.
Introduction – A Historical Perspective on Dog-Human Relationships
The modern relationship between humans and dogs is undoubtedly unique. With a shared evolutionary history spanning tens of thousands of years ( 1 ), dogs have filled a unique niche in our lives as man's best friend. Through the processes of domestication and natural selection, dogs have become adept at socializing with humans. For example, research suggests dogs are sensitive to our emotional states ( 2 ) as well as our social gestures ( 3 ), and they also can communicate with us using complex cues such as gaze alternation ( 4 ). In addition, dogs can form complex attachment relationships with humans that mirror that of infant-caregiver relationships ( 5 ).
In today's society, dog companionship is widely prevalent worldwide. In the United States, 63 million households have a pet dog, a majority of which consider their dog a member of their family ( 6 ). In addition to living in our homes, dogs have also become increasingly widespread in applications to assist individuals with disabilities as assistance dogs. During and following World War I, formal training of dogs as assistance animals began particularly for individuals with visual impairments in Germany and the United States ( 7 ). Following World War II, formal training for other roles, such as mobility and hearing assistance, started to increase in prevalence. Over the decades, the roles of assistance dogs have expanded to assist numerous disabilities and conditions including medical conditions such as epilepsy and diabetes and mental health disorders such as posttraumatic stress disorder (PTSD). At the same time, society has also seen increasing applications of dogs incorporated into working roles including detection, hunting, herding, and protection ( 8 , 9 ).
In addition to these working roles, dogs have also been instrumental in supporting humans in other therapeutic ways. In the early 1960s, animal-assisted interventions (AAI) began to evolve with the pioneering work of Boris Levinson, Elizabeth O'Leary Corson, and Samuel Corson. Levinson, a child psychologist practicing since the 1950s, noticed a child who was nonverbal and withdrawn during therapy began interacting with his dog, Jingles, in an unplanned interaction. This experience caused Levinson to begin his pioneering work in creating the foundations for AAI as an adjunct to treatment ( 10 ). In the 1970s, Samuel Corson and Elizabeth O'Leary Corson were some of the first researchers to empirically study canine-assisted interventions. Like Levinson, they inadvertently discovered that some of their patients with psychiatric disorders were interested in the dogs and that their patients with psychiatric disorders communicated more easily with each other and the staff when in the company of the dogs ( 11 , 12 ). Over the following decades, therapy dogs have been increasingly found to provide support for individuals with diverse needs in a wide array of settings ( 13 ).
Theoretical Framework for Dog Interaction Benefits
For over 40 years, the biopsychosocial model ( 14 ) has been widely used to conceptualize how biological, psychological, and social influences combine to determine human health and well-being. Biological influences refer to physiological changes such as blood pressure, cortisol, and heart rate, among others; psychological influences include personality, mood, and emotions, among others; and social influences refer to cultural, socio-economic, social relationships with others, family dynamics, and related matters. Figure 1 presents a graphical illustration of the relationship among these three influences in determining overall health and well-being. Although the model has dominated research and theory in health psychology for decades, more recently, it was re-envisioned as a more dynamic system ( 15 ) that construes human health as the result of the reciprocal influences of biological, psychological and social factors that unfold over personal and historical time. For example, if a person breaks his/her arm, there will be a biological impact in that immune and muscle systems respond and compensate. Social, or interpersonal, changes may occur when support or assistance is offered by others. Psychological changes will occur as a result of adjusting to and coping with the injury. Thus, the injury represents a dynamic influence initiated at one point in time and extending forward in time with diminishing impact as healing occurs.
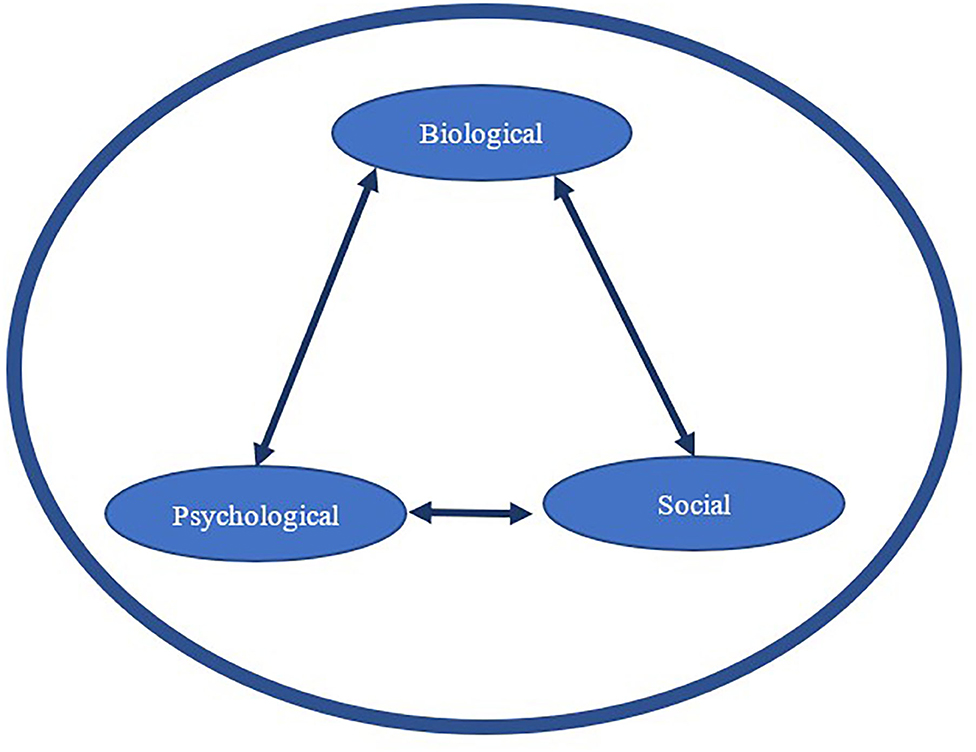
Figure 1 . A biopsychosocial perspective of how biological, psychological, and social influences may impact one another (solid lined arrows) and influence human health and well-being (represented here by the large thick circular shape).
This dynamic biopsychosocial approach to understanding health and well-being is appealing to the field of human-animal interaction (HAI) because of the dynamic nature of the relationship between humans and animals. For example, a person may acquire many dogs over his/her lifetime, perhaps from childhood to old age, and each of those dogs may sequentially develop from puppyhood to old age in that time. Behaviorally, the way the human and the dog interact is likely to be different across the lifespans of both species. From a biopsychosocial model perspective, the dynamic nature of the human-canine relationship may differentially interact with each of the three influencers (biological, psychological, and social) of human health and well-being over the trajectories of both beings. Notably, these influencers are not fixed, but rather have an interactional effect with each other over time.
While a person's biological, psychological, and social health may affect the relationship between that person and dogs with whom interactions occur, the focus of this manuscript is on the reverse: how owning or interacting with a dog may impact each of the psychological, biological, and social influencers of human health. We will also present relevant research and discuss potential mechanisms by which dogs may, or may not, contribute to human health and well-being according to the biopsychosocial model. Finally, we will emphasize how the biopsychosocial theory can be easily utilized to provide firmer theoretical foundations for future HAI research and applications to therapeutic practice and daily life.
Psychological Influences
Much research has been conducted on the impact of dog ownership and dog interactions on human psychological health and functioning. Frequent interactions with a dog, either through ownership or through long-term interventions, have been associated with positive psychological outcomes across the lifespan [for a systematic review of this evidence see ( 16 )]. One psychological aspect of interest to many HAI researchers is depression, especially among older adults. However, the relationship of pet dog ownership and depression over the lifespan continues to have inconsistent and inconclusive findings ( 16 ). Nevertheless, there are examples in the literature highlighting the beneficial role of dog ownership in reducing depression. As is frequently the case in HAI, the evidence from intervention studies is stronger than that of pet ownership studies ( 16 ), with the preponderance of this evidence linking animal-assisted interventions to a decrease in depression, as measured by self-report indices. Among the mechanisms for this reduction in depression are biological and social influences. For example, one such study found that an attachment relationship with a pet dog may serve as a coping resource for older women by buffering the relationship between loneliness (also measured by self-report indices) and depression, such that the presence of the pet dog appears to ameliorate the potential for loneliness to exacerbate depression ( 17 ). A causal relationship between dog ownership and mental health is difficult to determine. Not only may owning a pet dog increase stress, but those who are already suffering from loneliness or depression may be more inclined to have a pet dog than those who do not.
Another psychological outcome related to dog interaction that receives considerable research attention is anxiety. Studies have found that short-term, unstructured interactions with a therapy dog can significantly reduce self-reported anxiety and distress levels [e.g., ( 18 )]. For example, children with their pet dog or a therapy dog present during a stressful task exhibit lower perceived stress and more positive affect compared to when alone ( 19 ), when a parent was present ( 20 ), or when a stuffed dog was present ( 21 ). In addition to psychological mechanisms, there are social and biological mechanisms at play as well. In these short-term stressful contexts, a dog may serve as both a comforting, nonjudgmental presence as well as a positive tactile and sensory distraction. Dog interaction might also reduce anxiety and distress by influencing emotion regulation while coping with a stressor ( 22 ). During animal-assisted therapy, having a dog present during psychotherapy such as cognitive behavioral therapy can aid in decreasing self-reported anxious arousal and distress for patients who have experienced trauma, making the therapeutic treatment process more effective ( 23 ).
In addition to the negative aspects of psychological functioning, HAI research has also aimed to quantify the effects of dog interaction and ownership on positive psychological experiences such as happiness and well-being. Some studies have found that dog ownership is associated with higher life satisfaction and greater well-being ( 24 ), while other studies show that this is the case only when the dog provided social support ( 25 ) or satisfied the owner's needs ( 26 ). However, other large-scale surveys have found no significant differences in self-reported happiness between dog owners, cat owners, and non-pet owners ( 27 ), contributing to mixed findings. Recent discussions argue that too much focus has been placed on the relationship between mental health and the simple variable of dog ownership, when the specific activities that owners engage in with their dogs (e.g., walking, tactile interaction, and shared activities,) may be more important in explaining positive well-being ( 28 ). Further, many other factors may be driving these inconsistent findings in depression, anxiety, and well-being, including the owner's personality ( 24 ), gender and marital status ( 29 ), and attachment to the dog ( 30 ).
Dogs may also provide a source of motivation; for example, people with dogs are more likely to comply with the rigors of their daily life ( 31 ). The relationship with a pet dog may provide motivation to do things that may be less desirable. For example, for older adults who own pets, it is not uncommon for them to be more involved in daily life activities because of the need to take care of their animals ( 32 ). Likewise, children also complete less desired activities due to their relationship with the dog [for a discussion of this topic see ( 33 )].
An accumulation of research also suggests that dog interaction may have specific psychological benefits for individuals with physical disabilities and chronic conditions. Cohabitating with a specially trained assistance dog, including guide, hearing, and service dogs, can be associated with increased psychological and emotional functioning among individuals with disabilities ( 34 ). For individuals with mental disorders such as posttraumatic stress disorder (PTSD), recent research has also found that having a psychiatric service dog is associated with fewer PTSD symptoms, less depression and anxiety, and better quality of life [For a review see ( 35 )]. These benefits appear to be due to a combination of the service dog's specific trained tasks and aspects inherent to cohabitating with a pet dog, including having a source of love, nonjudgmental social support, and companionship ( 36 ).
Similar research has also highlighted the value of dogs for children with disorders of executive functioning and self-regulation, especially autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD). For some children with ASD, dogs may provide a calming and positive presence ( 37 ) and may both reduce anxiety ( 38 ) and improve problematic behaviors ( 39 ). Parents report that both pet dogs and service dogs can provide certain benefits for children with ASD, including benefits to children's moods, sleep, and behavior ( 40 , 41 ). Therapy dogs have also been found to be impactful in supporting children with ADHD in their emotional regulation ( 42 ) and aspects of character development ( 43 ). Nevertheless, the outcome of dog interactions may not be positive for all individuals with ASD and ADHD; despite evidence of psychological benefits of dog interaction for some children, others may be fearful or become over-stimulated by dogs ( 44 ).
In addition to impacts on psychological health, dog interaction can also impact psychological functioning, cognition, and learning. Among children, emerging research suggests short-term interactions with a therapy dog may lead to improvements in specific aspects of learning and cognition. A recent systematic review of research on therapy dog reading programs indicated that reading to a dog has a number of beneficial effects including improved reading performance ( 45 ). Studies suggest that interacting with a therapy dog may also improve speed and accuracy on cognitive (e.g., memory, categorization, adherence to instructions) and motor skills tasks among preschool-aged children compared to interacting with a stuffed dog or human ( 46 ). Similarly, a recent study showed that 10–14-year-old children had greater frontal lobe activity in the presence of a real dog as compared to a robotic dog, indicating a higher level of neuropsychological attention ( 47 ).
Among young adults, similar effects on cognition and learning have been found. Numerous colleges and universities now offer interactions with therapy dogs, typically during high stress times (such as before exams). In this sense, a biological mechanism through which dog interaction may positively impact cognition and learning is via stress reduction and improvement in positive affect. Even such short and infrequent interactions with therapy dogs may decrease perceived stress and increase perceived happiness in college students [e.g., ( 48 , 49 )]. Further, some institutions have permanent resident therapy dogs and/or long-term intervention programs; one such program showed that students who interacted with therapy dogs for 8 weeks reported significantly less homesickness and greater satisfaction with life than wait-listed controls ( 50 ). These effects may translate to additional effects on students' academic success, learning, and cognition. For instance, a recent randomized controlled trial ( 51 ) paired a standard academic stress management program with therapy dog interaction; the pairing produced significantly higher levels of self-reported enjoyment, usefulness, self-regulation, and behavior change than the stress management program or dog interaction alone. However, when therapy dog interaction is closely paired with more specific learning experiences, beneficial effects on stress remain, but benefits to academic performance may not manifest. For example, a recent study showed that interacting with a therapy dog resulted in significant improvements in students' perceived stress and mood, but not in actual exam scores ( 52 ). Similarly, interacting with a therapy dog during the learning and recall phase of a memory test did not improve memory compared to a control group ( 53 ). Taken together, dog interaction may improve stress and affect among college-aged adults as well as dimensions important for academic success and learning, but these results may or may not translate to cognitive performance benefits.
Biological Influences
The psychological and biological effects of HAI are often closely interwoven, as seen in the Psychological Influences section above and as demonstrated by the frequency with which psychological effects are evaluated using biological assessments of stress, anxiety, and arousal ( 54 ). For example, a plethora of studies have examined how short-term interactions with dogs can influence stress by measuring physiological biomarkers. Studies have found that dog interaction can influence parameters such as blood pressure, heart rate, and electrodermal activity ( 55 ) as well as neurochemical indicators of affiliative behavior [e.g., beta-endorphins, prolactin, and dopamine; ( 56 )].
However, one of the most popular physiological measures in HAI research is the stress hormone cortisol ( 57 ). Studies have found that short-term interactions with a dog can decrease both subjective stress and circulating cortisol concentrations [e.g., ( 58 )]. Cohabitating with a dog has also been found to impact circulating cortisol after waking among children with ASD ( 39 ) and military veterans with PTSD ( 59 ). Experimental studies have also examined how having a dog present may modulate the stress response and cortisol secretion among individuals undergoing a stressful situation. Among adults, studies have found that having a dog present during a socially stressful paradigm can attenuate cortisol compared to when alone or with a human friend ( 60 ). A recent randomized controlled trial similarly found that interacting with a therapy dog, for 20 min, two times per week, over a 4-week period resulted in reduced cortisol (basal and diurnal measurement) among typically developing and special needs school children compared to the same duration and length of delivery for a yoga relaxation or a classroom as usual control group ( 61 ). However, it is of note that many methodologically rigorous studies have not found significant effects of interacting with a dog on physiological parameters, including salivary cortisol ( 21 , 62 , 63 ). A recent review of salivary bioscience research in human-animal interaction concluded that significant variation exists with regards to sampling paradigms, storage and assaying methods, and analytic strategies, contributing to variation in findings across the field ( 57 ).
As research quantifying the physiological outcomes from dog interaction continues to increase, so does research attempting to understand the underlying mechanisms of action leading to stress reduction. One theoretical rationale for dogs' stress-reducing benefits consists of the dog's ability to provide non-judgmental social support ( 60 ), improve positive affect ( 64 ), and provide a calming presence ( 22 ). Dogs may also contribute to a feeling of perceived safety and provide a tactile and grounding comfort ( 65 ). For these reasons, dogs are often incorporated into treatment and recovery for individuals who have experienced a traumatic event ( 66 ). Another mechanism contributing to these stress reducing benefits may be tactile stimulation and distraction derived from petting or stroking a dog. For example, Beetz et al. ( 67 ) found that the more time a child spent stroking the dog before a stressful task, the larger the magnitude of cortisol decrease. In fact, calming tactile interactions such as stroking, touching, and petting may be a key mechanism explaining animal-specific benefits to stress physiology, as touch is more socially appropriate in interactions with animals than as with other people ( 22 ). While there are many hypothesized mechanisms underlying positive psychophysiological change following human-dog interaction, more research is needed to determine how individual differences in humans, animals, and the human-animal relationship affects outcomes ( 21 , 57 , 62 , 63 ).
Another mechanism in which positive dog interaction may result in psychophysiological benefits is via the secretion of oxytocin. Oxytocin not only buffers the stress response and cortisol secretion ( 68 ) but is also involved emotion, trust, and bonding ( 69 ). The oxytocin system has been hypothesized to be a primary mechanistic pathway involved in human-dog interactions ( 70 ). Positive dog-owner interactions including stroking, petting, and talking have been shown to result in increased oxytocin levels in both dog owners and dogs, which has been related to the strength of the owner-dog relationship ( 71 ) and dog-human affiliative behaviors ( 72 , 73 ). Some studies have also found differential effects in oxytocin reactivity after dog interaction between human males and females ( 74 ), giving context to potential gender and/or hormonal differences in dog-human interactions. However, even though the oxytocin system exhibits potential as a pathway by which dogs provide psychophysiological benefits, it should be noted that mixed findings and methodological and measurement differences limit strong conclusions ( 75 ).
In regards to pet dog ownership, many studies have also sought to understand the biological effects of long-term interactions with a pet dog. Some research suggests that sharing animal-associated microbes with a pet dog can have long-term impacts on human health ( 76 ) while others have found that cohabitating with a pet dog can be beneficial for child allergies ( 77 ) and immune system development ( 78 ). However, most research on the long-term health impacts of pet dog ownership has focused on cardiovascular functioning. Epidemiological research suggests that dog ownership is linked to greater physical activity levels (presumably linked to dog-walking), and reduced risk for cardiovascular disease, stroke, and all-cause mortality [for a summary see ( 79 )]. A recent meta-analysis of ten studies amassing data from over three million participants found that pet dog ownership was associated with a 31% risk reduction for mortality due to cardiovascular disease ( 80 ). However, dog ownership research of this nature will always suffer from an important chicken and egg type question: do dogs make us healthier, or do healthy people opt to own dogs?
Social Influences
A final way in which dog companionship and interaction may contribute to human health and well-being is through the social realm. Dogs may impact social functioning by providing direct social support ( 81 ) and a source of an attachment bond ( 82 ) which in turn may contribute to better social and mental health by providing companionship. Acquiring a pet dog has been reported to reduce both short-term and long-term self-reported loneliness ( 83 ). Particularly for those who live alone, dog ownership may serve as a protective factor against loneliness in times of social isolation, such as during the COVID-19 pandemic ( 84 ). Among older adults living in long-term care facilities or who live alone, dog visitation may also decrease loneliness by providing a source of meaningful companionship and social connectedness ( 85 , 86 ). However, the literature on pet dogs and loneliness is also characterized by mixed findings, raising the possibility that dog ownership may be a response to loneliness rather than protection from loneliness. Further, there remains a lack of high quality research in this area which limits any causal conclusions ( 87 ).
Another way in which the social support from a pet dog may benefit social functioning is by facilitating social interactions with others. For example, observational studies have found that being accompanied by a dog in public increases the frequency of received social interactions ( 88 ) and social acknowledgments [e.g., friendly glances, smiles; ( 89 )]. For those who engage in dog walking, social interactions are perceived as a rewarding side effect ( 90 ). Dogs can also provide a source of social capital, defined as the glue that holds society together ( 91 ). The research of Wood and colleagues ( 92 ) suggests that dogs can function as facilitators for social contact and interaction, with pet owners reporting higher perceptions of suburb friendliness and more social interactions with neighbors compared to non-pet owners.
For children and adolescents, pet dog ownership may contribute to healthy social development. Positive child–pet dog interactions have been shown to have benefits to children's social competence, interactions, and play behavior [for a review see ( 93 )]. Not only can children form attachment relationships with dogs ( 94 ), but pet dogs may promote feelings of safety and security ( 95 ) that can facilitate childhood social development. Pet ownership may also help children develop skills to form and maintain social relationships with their peers ( 96 ). For example, cross-sectional studies found that children with a pet dog in the home have fewer peer problems and have more prosocial behavior with children without a dog [e.g., ( 97 , 98 )].
Among children with developmental disorders, dog interaction has also been similarly shown to impact social functioning. For children with ADHD, two randomized controlled trials have found that 12 weeks of visits with a therapy dog, incorporated into curricula designed to improve skills and reduce behavioral problems, can result in improved social skills, prosocial behaviors, and perceptions of social competence ( 42 , 43 ). One potential explanation for these benefits is that children may interpret the dogs' nonverbal communication as less threatening and easier to interpret than human interaction ( 99 , 100 ). A recent eye-tracking study found that children with ASD exhibit a bias in social attention to animal faces, including dogs, compared to human faces ( 101 ). The presence of a dog in clinical applications may also promote more social engagement with a therapist while reducing negative behaviors ( 102 , 103 ). Further, there is some evidence that having a pet dog in the home can have a positive impact on social interactions of children with ASD, especially among verbal children, while teaching children responsibility and empathetic behavior ( 104 , 105 ).
Potential Mechanisms of Action
We have discussed how, in the psychological realm, interacting with a dog can positively relate to depression, anxiety, and well-being as well as psychological functioning in the areas of cognition, learning, and attention. It is interesting to note that most psychological constructs are measured using self-report indices, such as the Beck Depression Inventory ( 106 ) or the UCLA Loneliness Scale ( 107 ), while a smaller group of constructs are measured using speed and accuracy to detect targets (attention) or to remember information (learning and memory). In the biological realm, we discussed how interacting with dogs can influence stress-related physiological parameters and long-term biological and cardiovascular health. Biological measures are often recorded in real-time, such as heart rate or blood pressure, or are collected at critical time points during the study (e.g., saliva, urine, or blood samples for such measures as cortisol or oxytocin). Finally, we discussed the social realm, in which interacting with a dog can provide social support, facilitate social interactions, and improve social development and social skills. Measures used to assess variables in the social realm include self-report indices (e.g., demographics such as marital status, numbers of family members and friends), real time observations of social interactions (e.g., video analyses of interactions using ethograms), and parent/teacher reports of social functioning [e.g., Social Skills Rating System; ( 108 )]. To better understand and organize these various findings, we now consider potential mechanisms of action in the context of the biopsychosocial model, and as part of this discussion we will consider the potential for different types of measurement to have their own influence.
The mechanisms that underly positive human-dog interactions are likely to be interrelated and broadly, yet differentially, impactful across the three influencers of health (biological, psychological and social). According to the biopsychosocial model, impacts on one of the influencers of health is likely to impact the others ( 14 ). Further, an underlying mechanism of change may have a larger immediate impact on one realm than on the other two ( 15 ). Although this applies to the many influences we have discussed above, we will describe a reduction in stress as a more detailed example of how the biopsychosocial model can be considered. Stress is likely to have an immediate and measurable impact on the biological system through endocrinological (e.g., changes in cortisol) and psychophysiological (e.g., changes in blood pressure) processes. This same reduction in stress is likely to impact the psychological system through changes in mood or affect, concentration, and motivation, but that impact may not be immediately measurable or may be smaller in magnitude. This conjectured delay or reduction in effect size stems at least in part, from the way these changes are typically measured and the time course for potential effects to become measurable. For example, some biological changes indicative of increased stress (e.g., heart rate) can be measured in direct correspondence with the experimental manipulations (e.g., interacting with the dog vs. experiencing a control condition), and provide real time biological indications of changes in stress levels. Psychological indications of stress may be measured by a self-report survey instrument assessing state or trait anxiety. This type of measure cannot be completed in real time during the various experimental conditions (e.g., interacting with the dog vs. experiencing a control condition), but must be completed at some point following the experimental manipulation. It is possible that psychological measures are not as immediately sensitive to changes in the constructs they measure because of the required delay between manipulation and measurement. Such a delay may underestimate the real time effect as it may fade over time. Finally, reductions in stress have the potential to impact social systems by increasing social approaches and acceptance of approaches by others, but that impact may be of a small size or require even more time to be measurable. For example, exposure to stress may have immediate physiological effects, but it could take more time (prolonged exposure to stress) for those effects to impact some measures of social influence such as number of friends.
In Figure 2 , the mechanism of stress reduction is used as one example for the purposes of this discussion to exemplify how human-dog interactions may influence human health and well-being, as explained by the biopsychosocial model. Stress reduction may have a more immediate or larger impact on the biological realm as demonstrated by the larger arrow, while having a smaller (or perhaps delayed) impact on the psychological realm and an even smaller (or potentially more delayed) impact on the social realm.
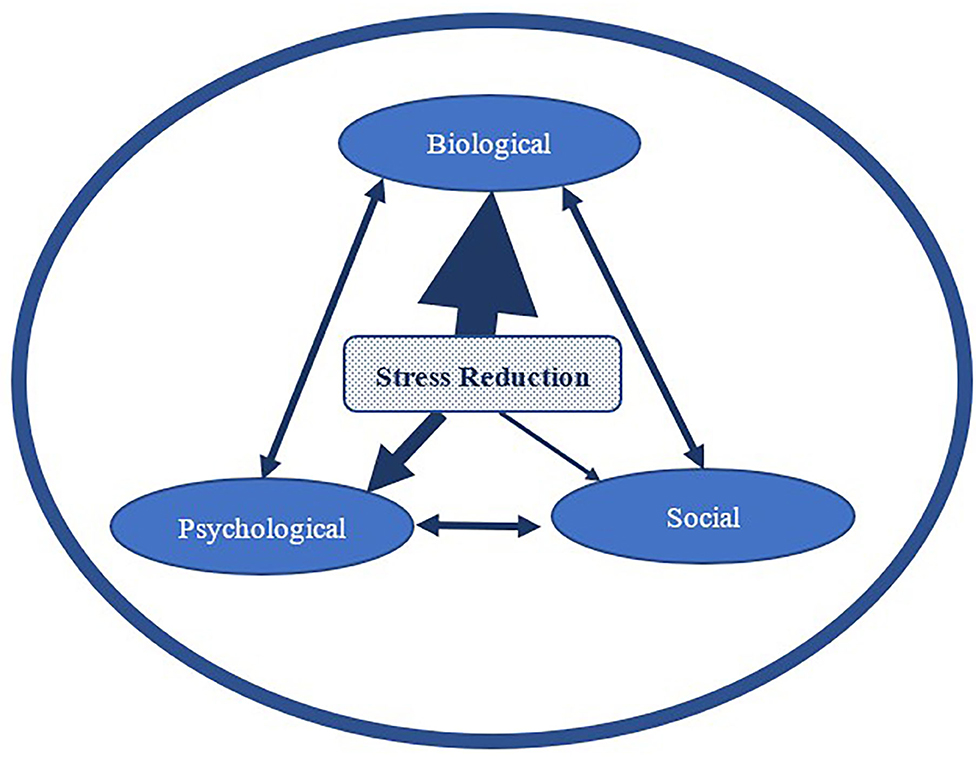
Figure 2 . An example of the potential for differential impact (represented by the different arrow thickness) of one mechanism of action (stress reduction) on the three realms of influence of overall health and well-being (depicted by the larger encompassing circle).
Based on the research described earlier, we have seen that interacting with a dog can have stress reducing impacts in the biological realm such as decreased cortisol, heart rate, and blood pressure, and increases in oxytocin. In the psychological realm, stress reduction can be a driver of immediate improvements in self-report measures of stress, mood, and anxiety and more delayed improvements in overall mental health and quality of life. The social realm is also likely to be directly and indirectly impacted by this stress reduction from both immediate and delayed psychophysiological changes as well as more long-term improvements in social support, social networks, social development, and overall social health. Therefore, it is important to consider the dynamic nature of these three realms in that there may be a strong immediate effect of dog interaction on one realm, but a lesser, delayed impact in the other two realms. Similar to our more detailed example of stress above, other influences we have discussed (e.g., social support, positive affect, etc.) are likewise mechanisms that operate in a similar reciprocal biopsychosocial framework. Further, although it likely that the three influences are interrelated, it is not known from the current evidence the degree to which they may be interrelated and thus have shared and overlapping effects on one another and on overall health and well-being. Therefore, a consideration of mechanisms that influence human-dog interactions from a dynamic and flexible biopsychosocial perspective, instead of from a single realm, is an important addition to the study of human-animal interaction.
Conclusion and Future Directions
In conclusion, the biopsychosocial model is a promising theoretical model to be applied to human-animal interaction research for several reasons. First, the field of HAI has been plagued by mixed findings in which some research suggests that dogs have beneficial effects on human health and well-being and others suggest no effect or even a negative effect [for a discussion see ( 109 )]. This variability in HAI research outcomes caused by differing methodologies, measurement, populations, and interventions is described in detail by Rodriguez et al. ( 110 ). However, we also argue that some of the variability seen in HAI research may be explained by the potential for differential immediate and delayed impacts within each of the three biopsychosocial model realms. For example, if dog interaction shows immediate reduction in physiological measures of stress, how long does that reduction last, and do we see corresponding immediate and/or delayed responses in the psychological and social realms? Therefore, more information about differential impacts of dog interactions on each of the three influencers at various points in time is needed. In addition, it may be necessary to apply a variety of measures (at least one measure per influencer realm) over time to fully disentangle the existing mixed results in the field of HAI.
Secondly, due to the flexibility that this dynamic biopsychosocial model offers in explaining HAI research outcomes, we propose this model as an effective avenue to promote future theoretically grounded research in our field. Saleh ( 111 ) stresses that practice, research, and theory are the corner stones of any field, HAI is not exempt from this consideration. The field of HAI will benefit from applying an accepted model, like the biopsychosocial model, because it provides a useful framework for understanding and predicting how interactions between humans and animals impacts human health and well-being. As Saleh ( 111 ) explains, “it is the result of the relationship between the process of inquiry (research) and the product of knowledge (theory)” that our understanding of a process may become clearer. Therefore, current research should continue to modify and impact a present theory, which should act as a guide for researchers to constantly generate and test the basis of a theory ( 111 ). The findings from such theory-driven research could then help practitioners, as well as health care policy makers, in how to effectively incorporate dogs in therapeutic settings and in homes.
Lastly, the reciprocal relationship of the psychological, biological, and social domains can be used to elucidate the mechanisms that both impact and are impacted by interactions between humans and animals. Theory-driven science (for which we have proposed the biopsychosocial model as a useful framework) should be used to influence and inform research, practice, and policy. Thus, researchers and practitioners applying the biopsychosocial model will be instrumental not only in guiding future research in the field, but also in clarifying existing research as well people's perceptions of benefits derived from canine-human interactions.
Author Contributions
NG provided the initial organization and theoretical framework. All authors wrote and edited the document in shared collaboration and discussed and conceived the idea for the paper.
As part of the conferment of Fellowship status to all authors, the Wallis Annenberg Petspace provided the funding for publication fees of this document.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors wish to express their appreciation to the Wallis Annenberg Petspace for supporting this theoretical framework and exploration of the Human-Canine bond.
1. Thalmann O, Shapiro B, Cui P, Schuenemann VJ, Sawyer SK, Greenfield D, et al. Complete mitochondrial genomes of ancient canids suggest a European origin of domestic dogs. Science. (2013) 342:871–4. doi: 10.1126/science.1243650
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Albuquerque N, Guo K, Wilkinson A, Savalli C, Otta E, Mills D. Dogs recognize dog and human emotions. Biol Lett. (2016) 12:20150883. doi: 10.1098/rsbl.2015.0883
3. Hare B, Brown M, Williamson C, Tomasello M. The domestication of social cognition in dogs. Science. (2002) 298:1634–6. doi: 10.1126/science.1072702
4. Miklósi Á, Kubinyi E, Topál J, Gácsi M, Virányi Z, Csányi V. A simple reason for a big difference: wolves do not look back at humans, but dogs do. Curr Biol. (2003) 13:763–6. doi: 10.1016/S0960-9822(03)00263-X
5. Payne E, Bennett PC, Mcgreevy PD. Current perspectives on attachment and bonding in the dog–human dyad. Psychol Res Behav Manag. (2015) 8:71. doi: 10.2147/PRBM.S74972
6. American Pet Products Association. 2019–2020 APPA National Pet Owners Survey . Stamford, CT: American Pet Products Association (2019).
Google Scholar
7. Fishman GA. When your eyes have a wet nose: the evolution of the use of guide dogs and establishing the seeing eye. Surv Ophthalmol. (2003) 48:452–8. doi: 10.1016/S0039-6257(03)00052-3
8. Cobb M, Branson N, McGreevy P, Lill A, Bennett P. The advent of canine performance science: offering a sustainable future for working dogs. Behav Process. (2015) 110:96–104. doi: 10.1016/j.beproc.2014.10.012
9. Cruse SD. Military working dogs: classification and treatment in the US Armed Forces. Animal. (2014) 21:249.
10. Levinson B. Pet-Oriented Child Psychotherapy . Springfield, IL: Charles C Thomas (1969).
11. Corson S, O'leary Corson E, Gwynne P. Pet-facilitated psychotherapy. ln: Anderson RS, editor. Petanimals and Society . London: Baillière Tindal (1975). p. 19–35.
12. Corson SA, Arnold LE, Gwynne PH, Corson EOL. Pet dogs as nonverbal communication links in hospital psychiatry. Compr Psychiatry. (1977) 18:61–72. doi: 10.1016/S0010-440X(77)80008-4
13. Fine AH. Handbook on Animal-Assisted Therapy: Foundations and Guidelines for Animal-Assisted Interventions . New York, NY: Academic Press (2019).
14. Engel GL. The clinical application of the biopsychosocial model. Am J Psychiatry. (1980) 137:535–44. doi: 10.1176/ajp.137.5.535
CrossRef Full Text | Google Scholar
15. Lehman BJ, David DM, Gruber JA. Rethinking the biopsychosocial model of health: understanding health as a dynamic system. Soc Person Psychol Compass. (2017) 11:e12328. doi: 10.1111/spc3.12328
16. Gee NR, Mueller MK. A systematic review of research on pet ownership and animal interactions among older adults. Anthrozoös. (2019) 32:183–207. doi: 10.1080/08927936.2019.1569903
17. Krause-Parello CA. Pet ownership and older women: the relationships among loneliness, pet attachment support, human social support, and depressed mood. Geriatr Nurs. (2012) 33:194–203. doi: 10.1016/j.gerinurse.2011.12.005
18. Kline JA, Fisher MA, Pettit KL, Linville CT, Beck AM. Controlled clinical trial of canine therapy versus usual care to reduce patient anxiety in the emergency department. PLoS ONE. (2019) 14:e0209232. doi: 10.1371/journal.pone.0209232
19. Kerns KA, Stuart-Parrigon KL, Coifman KG, Van Dulmen MH, Koehn A. Pet dogs: does their presence influence preadolescents' emotional responses to a social stressor? Soc Dev. (2018) 27:34–44. doi: 10.1111/sode.12246
20. Kertes DA, Liu J, Hall NJ, Hadad NA, Wynne CD, Bhatt SS. Effect of pet dogs on children's perceived stress and cortisol stress response. Soc Dev. (2016) 26:382–401. doi: 10.1111/sode.12203
21. Crossman MK, Kazdin AE, Matijczak A, Kitt ER, Santos LR. The influence of interactions with dogs on affect, anxiety, and arousal in children. J Clin Child Adolesc Psychol. (2020) 49:535–48. doi: 10.1080/15374416.2018.1520119
22. Crossman MK. Effects of interactions with animals on human psychological distress. J Clin Psychol. (2017) 73:761–84. doi: 10.1002/jclp.22410
23. Hunt MG, Chizkov RR. Are therapy dogs like Xanax? Does animal-assisted therapy impact processes relevant to cognitive behavioral psychotherapy? Anthrozoös. (2014) 27:457–69. doi: 10.2752/175303714X14023922797959
24. Bao KJ, Schreer G. Pets and happiness: examining the association between pet ownership and wellbeing. Anthrozoös. (2016) 29:283–96. doi: 10.1080/08927936.2016.1152721
25. Mcconnell AR, Brown CM, Shoda TM, Stayton LE, Martin CE. Friends with benefits: on the positive consequences of pet ownership. J Person Soc Psychol. (2011) 101:1239. doi: 10.1037/a0024506
26. Luhmann M, Kalitzki A. How animals contribute to subjective well-being: A comprehensive model of protective and risk factors. J Positive Psychol. (2018) 13:200–14. doi: 10.1080/17439760.2016.1257054
27. Taylor P, Funk C, Craighill P. “Are We Happy Yet?” . Washington, DC: Pew Research Center (2006).
28. Barcelos AM, Kargas N, Maltby J, Hall S, Mills DS. A framework for understanding how activities associated with dog ownership relate to human well-being. Sci Rep. (2020) 10:1–12. doi: 10.1038/s41598-020-68446-9
29. Cline KMC. Psychological effects of dog ownership: role strain, role enhancement, and depression. J Soc Psychol. (2010) 150:117–31. doi: 10.1080/00224540903368533
30. Wanser SH, Vitale KR, Thielke LE, Brubaker L, Udell MA. Spotlight on the psychological basis of childhood pet attachment and its implications. Psychol Res Behav Manag. (2019) 12:469. doi: 10.2147/PRBM.S158998
31. Barker SB, Wolen AR. The benefits of human–companion animal interaction: a review. J Vet Med Educ. (2008) 35:487–95. doi: 10.3138/jvme.35.4.487
32. Raina P, Waltner-Toews D, Bonnett B, Woodward C, Abernathy T. Influence of companion animals on the physical and psychological health of older people: An analysis of a one-year longitudinal study. J Am Geriatr Soc. (1999) 47:323–9. doi: 10.1111/j.1532-5415.1999.tb02996.x
33. Melson GF, Fine AH. Animals in the lives of children. In: Fine AH, editor. Handbook on Animal-Assisted Therapy. New York, NY: Elsevier (2015). p. 179–94.
34. Rodriguez KE, Greer J, Beck A, O'haire ME. The psychosocial effects of service dogs on individuals with physical disabilities: a systematic literature review. PLoS ONE. (2020) 15:e0243302. doi: 10.1371/journal.pone.0243302
35. Krause-Parello CA, Sarni S, Padden E. Military veterans and canine assistance for post-traumatic stress disorder: a narrative review of the literature. Nurse Educ Today. (2016) 47:43–50. doi: 10.1016/j.nedt.2016.04.020
36. Rodriguez KE, Lafollette MR, Hediger K, Ogata N, O'haire ME. Defining the PTSD service dog intervention: perceived importance, usage, and symptom specificity of psychiatric service dogs for military veterans. Front Psychol. (2020) 11:1638. doi: 10.3389/fpsyg.2020.01638
37. Silva K, Lima M, Santos-Magalhães A, Fafiães C, De Sousa L. Can dogs assist children with severe autism spectrum disorder in complying with challenging demands? An exploratory experiment with a live and a robotic dog. J Alternative Comp Med. (2018) 24:238–42. doi: 10.1089/acm.2017.0254
38. Wright H, Hall S, Hames A, Hardiman J, Mills R, Team PP, et al. Pet dogs improve family functioning and reduce anxiety in children with autism spectrum disorder. Anthrozoös. (2015) 28:611–24. doi: 10.1080/08927936.2015.1070003
39. Viau R, Arsenault-Lapierre G, Fecteau S, Champagne N, Walker C-D, Lupien S. Effect of service dogs on salivary cortisol secretion in autistic children. Psychoneuroendocrinology. (2010) 35:1187–93. doi: 10.1016/j.psyneuen.2010.02.004
40. Burrows KE, Adams CL, Spiers J. Sentinels of safety: Service dogs ensure safety and enhance freedom and well-being for families with autistic children. Qual Health Res. (2008) 18:1642–9. doi: 10.1177/1049732308327088
41. Carlisle GK. The social skills and attachment to dogs of children with autism spectrum disorder. J Autism Dev Disord. (2014) 45:1137–45.
PubMed Abstract | Google Scholar
42. Schuck SE, Emmerson NA, Fine AH, Lakes KD. Canine-assisted therapy for children with ADHD: preliminary findings from the positive assertive cooperative kids study. J Attention Disord. (2015) 19:125–37. doi: 10.1177/1087054713502080
43. Schuck SE, Johnson HL, Abdullah MM, Stehli A, Fine AH, Lakes KD. The role of animal assisted intervention on improving self-esteem in children with attention deficit/hyperactivity disorder. Front Pediatr. (2018) 6:300. doi: 10.3389/fped.2018.00300
44. Grandin T, Fine AH, Bowers CM. The use of therapy animals with individuals with autism spectrum disorders. In: Fine AH, edior. Handbook on Animal-Assisted Therapy . 3rd ed. New York, NY: Elsevier. (2010). p. 247–64.
45. Hall SS, Gee NR, Mills DS. Children reading to dogs: a systematic review of the literature. PLoS ONE. (2016) 11. doi: 10.1371/journal.pone.0149759
46. Gee NR, Fine AH, Schuck S. Animals in educational settings: Research and practice. In: Handbook on Animal-Assisted Therapy . New York, NY: Elsevier (2015). p. 195–210.
47. Hediger K, Turner D. Can dogs enhance children's attention performance? A randomized controlled crossover trial. Hum Anim Interact Bull. (2014) 2:21–39.
48. Ward-Griffin E, Klaiber P, Collins HK, Owens RL, Coren S, Chen FS. Petting away pre-exam stress: the effect of therapy dog sessions on student well-being. Stress Health. (2018) 34:468–73. doi: 10.1002/smi.2804
49. Wood E, Ohlsen S, Thompson J, Hulin J, Knowles L. The feasibility of brief dog-assisted therapy on university students stress levels: the PAWS study. J Mental Health. (2017) 27:263–8. doi: 10.1080/09638237.2017.1385737
50. Binfet J-T, Passmore H-A, Cebry A, Struik K, Mckay C. Reducing university students' stress through a drop-in canine-therapy program. J Mental Health. (2018) 27:197–204. doi: 10.1080/09638237.2017.1417551
51. Pendry P, Carr AM, Gee NR, Vandagriff JL. Randomized trial examining effects of animal assisted intervention and stress related symptoms on college students' learning and study skills. Int J Environ Res Public Health. (2020) 17:1909. doi: 10.3390/ijerph17061909
52. Trammell JP. The effect of therapy dogs on exam stress and memory. Anthrozoös. (2017) 30:607–21. doi: 10.1080/08927936.2017.1370244
53. Trammell JP. Therapy dogs improve student affect but not memory. Anthrozoös. (2019) 32:691–9. doi: 10.1080/08927936.2019.1645514
54. Rodriguez KE, Guérin NA, Gabriels RL, Serpell JA, Schreiner PJ, O'haire ME. The state of assessment in human-animal interaction research. Hum Anim Interact Bull. (2018) 6:63−81.
55. Beetz A, Uvnäs-Moberg K, Julius H, Kotrschal K. Psychosocial and psychophysiological effects of human-animal interactions: the possible role of oxytocin. Front Psychol. (2012) 3:234. doi: 10.3389/fpsyg.2012.00234
56. Odendaal J, Meintjes R. Neurophysiological correlates of affiliative behaviour between humans and dogs. Vet J. (2003) 165:296–301. doi: 10.1016/S1090-0233(02)00237-X
57. Pendry P, Vandagriff JL. Salivary Studies of the Social Neuroscience of Human–Animal Interaction. In: Granger D, Taylor M, editors. Salivary Bioscience. Springer (2020). p. 555–81.
58. Barker SB, Knisely JS, Mccain NL, Best AM. Measuring stress and immune response in healthcare professionals following interaction with a therapy dog: a pilot study. Psychol Rep. (2005) 96:713–29. doi: 10.2466/pr0.96.3.713-729
59. Rodriguez KE, Bryce CI, Granger DA, O'haire ME. The effect of a service dog on salivary cortisol awakening response in a military population with posttraumatic stress disorder (PTSD). Psychoneuroendocrinology. (2018) 98:202–10. doi: 10.1016/j.psyneuen.2018.04.026
60. Polheber J, Matchock R. (2013). The presence of a dog attenuates cortisol and heart rate in the Trier Social Stress Test compared to human friends. J Behav Med. 37:1–8. doi: 10.1007/s10865-013-9546-1
61. Meints K, Brelsford V, Dimolareva M, Gee N. Dog-assisted interventions with children in mainstream and special educational needs schools – what works? In: Paper presented at the International Society for Anthrozoology Annual Conference . Liverpool (2020).
62. Coakley AB, Annese CD, Empoliti JH, Flanagan JM. The experience of animal assisted therapy on patients in an acute care setting. Clin Nurs Res. (2020). doi: 10.1177/1054773820977198. [Epub ahead of print].
63. Clark S, Martin F, Mcgowan RT, Smidt J, Anderson R, Wang L, et al. The impact of a 20-minute animal-assisted activity session on the physiological and emotional states in patients with fibromyalgia. In: Mayo Clinic Proceedings . Elsevier. (2020). p. 2442−61. doi: 10.1016/mayocp.2020.04.037
64. Lass-Hennemann J, Schäfer SK, Römer S, Holz E, Streb M, Michael T. Therapy dogs as a crisis intervention after traumatic events? An experimental study. Front Psychol. (2018) 9:1627. doi: 10.3389/fpsyg.2018.01627
65. Bleiberg J, Prout M, Debiak D, Lefkowitz C, Paharia I. Animal-assisted prolonged exposure: a treatment for survivors of sexual assault suffering posttraumatic stress disorder. Soc Anim. (2005) 13:275–96. doi: 10.1163/156853005774653654
66. O'haire ME, Philip Tedeschi M, Jenkins MA, Braden SR, Rodriguez KE. The impact of human-animal interaction in trauma recovery. New Direct Hum Anim Bond . (2019) 15:15–53. Available online at: https://library.oapen.org/bitstream/handle/20.500.12657/24992/1005110.pdf?sequence=1#page=30
67. Beetz A, Julius H, Turner D, Kotrschal K. Effects of social support by a dog on stress modulation in male children with insecure attachment. Front Psychol. (2012) 3:352. doi: 10.3389/fpsyg.2012.00352
68. Cardoso C, Kingdon D, Ellenbogen MA. A meta-analytic review of the impact of intranasal oxytocin administration on cortisol concentrations during laboratory tasks: moderation by method and mental health. Psychoneuroendocrinology. (2014) 49:161–70. doi: 10.1016/j.psyneuen.2014.07.014
69. Meyer-Lindenberg A, Domes G, Kirsch P, Heinrichs M. Oxytocin and vasopressin in the human brain: social neuropeptides for translational medicine. Nat Rev Neurosci. (2011) 12:524–38. doi: 10.1038/nrn3044
70. Marshall-Pescini S, Schaebs FS, Gaugg A, Meinert A, Deschner T, Range F. The role of oxytocin in the dog–owner relationship. Animals. (2019) 9:792. doi: 10.3390/ani9100792
71. Handlin L, Nilsson A, Ejdebäck M, Hydbring-Sandberg E, Uvnäs-Moberg K. Associations between the psychological characteristics of the human–dog relationship and oxytocin and cortisol levels. Anthrozoos. (2012) 25:215–28. doi: 10.2752/175303712X13316289505468
72. Maclean EL, Gesquiere LR, Gee NR, Levy K, Martin WL, Carter CS. Effects of affiliative human–animal interaction on dog salivary and plasma oxytocin and vasopressin. Front Psychol. (2017) 8:1606. doi: 10.3389/fpsyg.2017.01606
73. Petersson M, Uvnäs-Moberg K, Nilsson A, Gustafson L-L, Hydbring-Sandberg E, Handlin L. Oxytocin and cortisol levels in dog owners and their dogs are associated with behavioral patterns: an exploratory study. Front Psychol. (2017) 8:1796. doi: 10.3389/fpsyg.2017.01796
74. Miller SC, Kennedy C, Devoe D, Hickey M, Nelson T, Kogan L. An examination of changes in oxytocin levels in men and women before and after interaction with a bonded dog. Anthrozoös. (2009) 22:31–42. doi: 10.2752/175303708X390455
75. Powell L, Guastella AJ, Mcgreevy P, Bauman A, Edwards KM, Stamatakis E. The physiological function of oxytocin in humans and its acute response to human-dog interactions: a review of the literature. J Vet Behav. (2019) 30:25–32. doi: 10.1016/j.jveb.2018.10.008
76. Garcia MCS, Schorr AR, Arnold W, Fei N, Gilbert JA. Pets as a novel microbiome-based therapy. In: Pastorinho M, Sousa A, editors. Pets as Sentinels, Forecasters and Promoters of Human Health. Springer (2020). p. 245–67. doi: 10.1007/978-3-030-30734-9
77. Hölscher B, Frye C, Wichmann HE, Heinrich J. Exposure to pets and allergies in children. Pediatr Aller Immunol. (2002) 13:334–41. doi: 10.1034/j.1399-3038.2002.02063.x
78. Bufford J, Reardon C, Li Z, Roberg K, Dasilva D, Eggleston P, et al. Effects of dog ownership in early childhood on immune development and atopic diseases. Clin Exp Allergy. (2008) 38:1635–43. doi: 10.1111/j.1365-2222.2008.03018.x
79. Friedmann E. The animal-human bond: health and wellness. In: Fine AH, editor. Animal-Assisted Therapy: Theoretical Foundations and Guidelines for Practice . New York, NY: Academic Press. (2019). p. 80–93.
80. Kramer CK, Mehmood S, Suen RS. Dog ownership and survival: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. (2019) 12:e005554. doi: 10.1161/CIRCOUTCOMES.119.005554
81. Beck AM, Katcher AH. Between Pets and People: The Importance of Animal Companionship . West Lafayette, IN: Purdue University Press (1996).
82. Kurdek LA. Pet dogs as attachment figures. J Soc Person Relat. (2008) 25:247–66. doi: 10.1177/0265407507087958
83. Powell L, Edwards KM, Mcgreevy P, Bauman A, Podberscek A, Neilly B, et al. Companion dog acquisition and mental well-being: a community-based three-arm controlled study. BMC Public Health. (2019) 19:1428. doi: 10.1186/s12889-019-7770-5
84. Oliva JL, Johnston KL. Puppy love in the time of Corona: dog ownership protects against loneliness for those living alone during the COVID-19 lockdown. Int J Soc Psychiatry. (2020). doi: 10.1177/0020764020944195. [Epub ahead of print].
85. Stanley IH, Conwell Y, Bowen C, Van Orden KA. Pet ownership may attenuate loneliness among older adult primary care patients who live alone. Aging Mental Health. (2014) 18:394–9. doi: 10.1080/13607863.2013.837147
86. Krause-Parello CA, Gulick EE, Basin B. Loneliness, depression, and physical activity in older adults: the therapeutic role of human–animal interactions. Anthrozoös. (2019) 32:239–54. doi: 10.1080/08927936.2019.1569906
87. Gilbey A, Tani K. Companion animals and loneliness: a systematic review of quantitative studies. Anthrozoos. (2015) 28:181–97. doi: 10.2752/089279315X14219211661615
88. Mcnicholas J, Collis GM. Dogs as catalysts for social interaction: Robustness of the effect. Br J Psychol. (2000) 91:61–70. doi: 10.1348/000712600161673
89. Mader B, Hart LA, Bergin B. Social acknowledgments for children with disabilities: effects of service dogs. Child Dev. (1989) 60:1529–34. doi: 10.2307/1130941
90. Higgins JW, Temple V, Murray H, Kumm E, Rhodes R. Walking sole mates: dogs motivating, enabling and supporting guardians' physical activity. Anthrozoös. (2013) 26:237–52. doi: 10.2752/175303713X13636846944286
91. Lang RE, Hornburg SP. What is social capital and why is it important to public policy? Housing Policy Debate. (1998) 9:1–16. doi: 10.1080/10511482.1998.9521284
92. Wood L, Giles-Corti B, Bulsara M. The pet connection: pets as a conduit for social capital? Soc Sci Med. (2005) 61:1159–73. doi: 10.1016/j.socscimed.2005.01.017
93. Purewal R, Christley R, Kordas K, Joinson C, Meints K, Gee N, et al. Companion animals and child/adolescent development: a systematic review of the evidence. Int J Environ Res Public Health. (2017) 14:234. doi: 10.3390/ijerph14030234
94. Jalongo MR. An attachment perspective on the child-dog bond: Interdisciplinary and international research findings. Children Dogs Educ. (2018) 21–41. doi: 10.1007/978-3-319-77845-7_2
95. Melson GF. Companion animals and the development of children: implications of the biophilia hypothesis. In: Fine AH, editor. Handbook on Animal-Assisted Therapy . New York, NY: Elsevier (2006). p. 375–83. doi: 10.1016/B978-012369484-3/50019-0
96. Mueller MK. Is human-animal interaction (HAI) linked to positive youth development? Init Answers Appl Dev Sci. (2014) 18:5–16. doi: 10.1080/10888691.2014.864205
97. Vidović VV, Štetić VV, Bratko D. Pet ownership, type of pet and socio-emotional development of school children. Anthrozoös. (1999) 12:211–7. doi: 10.2752/089279399787000129
98. Wenden EJ, Lester L, Zubrick SR, Ng M, Christian HE. The relationship between dog ownership, dog play, family dog walking, and pre-schooler social–emotional development: findings from the PLAYCE observational study. Pediatr Res. 1–7. doi: 10.1038/s41390-020-1007-2. [Epub ahead of print].
99. Prothmann A, Ettrich C, Prothmann S. Preference for, and responsiveness to, people, dogs and objects in children with autism. Anthrozoös. (2009) 22:161–71. doi: 10.2752/175303709X434185
100. Solomon O. What a dog can do: Children with autism and therapy dogs in social interaction. Ethos. (2010) 38:143–66. doi: 10.1111/j.1548-1352.2010.01085.x
101. Valiyamattam GJ, Katti H, Chaganti VK, O'haire ME, Sachdeva V. Do animals engage greater social attention in autism? An eye tracking analysis. Front Psychol. (2020) 11:727. doi: 10.3389/fpsyg.2020.00727
102. Martin F, Farnum J. Animal-assisted therapy for children with pervasive developmental disorders. West J Nurs Res. (2002) 24:657–70. doi: 10.1177/019394502320555403
103. Silva K, Correia R, Lima M, Magalhães A, De Sousa L. Can dogs prime autistic children for therapy? Evidence from a single case study. J Alternat Comp Med. (2011) 17:1–5. doi: 10.1089/acm.2010.0436
104. Carlisle GK. Pet dog ownership decisions for parents of children with autism spectrum disorder. J Pediatr Nurs. (2014) 29:114. doi: 10.1016/j.pedn.2013.09.005
105. Hall SS, Wright HF, Hames A, Mills DS. The long-term benefits of dog ownership in families with children with autism. J Vet Behav. (2016) 13:46–54. doi: 10.1016/j.jveb.2016.04.003
106. Beck AT, Steer RA, Brown G. Beck depression inventory–II. Psychol Assess. (1996) 36:221–37. doi: 10.1037/t00742-000
107. Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Person Assess. (1996) 66:20–40. doi: 10.1207/s15327752jpa6601_2
108. Van Der Oord S, Van Der Meulen E, Prins PJ, Oosterlaan J, Buitelaar J, Emmelkamp PM. A psychometric evaluation of the social skills rating system in children with attention deficit hyperactivity disorder. Behav Res Therapy. (2005) 43:733–46. doi: 10.1016/j.brat.2004.06.004
109. Herzog H. The impact of pets on human health and psychological well-being: fact, fiction, or hypothesis? Curr Direct Psychol Sci. (2011) 20:236–9. doi: 10.1177/0963721411415220
110. Rodriguez KE, Herzog H, Gee N. Variability in human-animal interaction research. Front Vet Sci. (2021) 7:619600. doi: 10.3389/fvets.2020.619600
111. Saleh US. Theory guided practice in nursing. J Nurs Res Pract. (2018) 2:18.
Keywords: dog, human health, human-animal interaction, biopsychosocial, canine, mental health
Citation: Gee NR, Rodriguez KE, Fine AH and Trammell JP (2021) Dogs Supporting Human Health and Well-Being: A Biopsychosocial Approach. Front. Vet. Sci. 8:630465. doi: 10.3389/fvets.2021.630465
Received: 17 November 2020; Accepted: 25 February 2021; Published: 30 March 2021.
Reviewed by:
Copyright © 2021 Gee, Rodriguez, Fine and Trammell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nancy R. Gee, nancy.gee@vcuhealth.org
This article is part of the Research Topic
Our Canine Connection: The History, Benefits and Future of Human-Dog Interactions

- News and Media
- Newsletters
- Download a Member Application
- Grants, Awards, and Scholarships
- Access the Phantom Analysis Toolkit
- Membership Directory
- Centers of Excellence
- Member Spotlight
- Women in Nuclear Medicine
- SNMMI Fellow
- SNMMI-TS Fellow
- Council and Center Internships
- Learning Center
- Calendar of Events
- 2024 Annual Meeting
- 2024 Therapeutics Conference
- 2024 Mid-Winter Meeting
- Nuclear Medicine & Molecular Imaging Week
- Coding & Reimbursement
- Legislative Efforts
- Government Relations News
- Radiopharmaceutical Supply News
- Technologist State Issues
- Position Statements
- FDA PET Drug Manufacturing Q&A
- Clinical Guidelines and AUC
- Quality and Patient Safety
- Dose Optimization
- About Quality & Practice
- Clinical Trials Network
- Radiopharmaceutical Therapy Central
- Radiopharmaceutical Therapy Centers of Excellence
- Preclinical Imaging
- Nuclear Medicine Clinical Trial Group, LLC
- Research: Learn More
- Strategic Plan
- Bylaws & Procedures
- Governance - SNMMI
- Governance - SNMMI-TS
- Career Center
- About Nuclear Medicine & Molecular Imaging
- International Collaboration
- Support SNMMI
In This Section
- Press Releases
- Coding & Reimbursement News
- Molecular Imaging News
- Media Center
- Social Media