An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts


Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice
Purpose of review.
To briefly review results of the latest research on the contributions of depression, anxiety, and stress exposures in pregnancy to adverse maternal and child outcomes, and to direct attention to new findings on pregnancy anxiety, a potent maternal risk factor.
Recent findings
Anxiety, depression, and stress in pregnancy are risk factors for adverse outcomes for mothers and children. Anxiety in pregnancy is associated with shorter gestation and has adverse implications for fetal neurodevelopment and child outcomes. Anxiety about a particular pregnancy is especially potent. Chronic strain, exposure to racism, and depressive symptoms in mothers during pregnancy are associated with lower birth weight infants with consequences for infant development. These distinguishable risk factors and related pathways to distinct birth outcomes merit further investigation.
This body of evidence, and the developing consensus regarding biological and behavioral mechanisms, sets the stage for a next era of psychiatric and collaborative interdisciplinary research on pregnancy to reduce the burden of maternal stress, depression, and anxiety in the perinatal period. It is critical to identify the signs, symptoms, and diagnostic thresholds that warrant prenatal intervention and to develop efficient, effective and ecologically valid screening and intervention strategies to be used widely.
INTRODUCTION
For more than a decade, psychiatry and related disciplines have been concerned about women experiencing symptoms of anxiety and depression during pregnancy and in the months following a birth. Current Opinion in Psychiatry alone published relevant reviews in 1998, 2000, 2004, 2007, 2008, 2009, and 2011, usually addressing the clinical management of postpartum depression or the effects of antidepressant use on mothers and their babies. Meanwhile, a parallel literature has grown rapidly in other health disciplines, especially behavioral medicine, health psychology, and social epidemiology, regarding stress in pregnancy and the implications for mothers, infants, and development over the life course. The purpose of this article is to briefly review results of the latest research on effects of negative affective states (referring throughout to anxiety and depression) and stress exposures in pregnancy, mainly regarding effects on birth outcomes. We direct attention specifically to recent research on pregnancy anxiety, a newer concept that is among the most potent maternal risk factors for adverse maternal and child outcomes [ 1■■ ]. By highlighting these developments, we hope to encourage synthesis and new directions in research and to facilitate evidence-based practices in screening and clinical protocols.
Psychiatric research on pregnancy focuses mostly on diagnosable mental disorders, primarily anxiety, and depressive disorders [ 2 , 3 ] and somewhat on posttraumatic stress disorder following adverse life events or childbirth experiences. However, a large body of scientific research outside psychiatry provides extensive information on a wide range of clinical symptoms during pregnancy, as measured with screening tools such as the Edinburgh Postpartum Depression Scale (EPDS), for example, the Beck Depression Inventory, or the Center for Epidemiological Studies Depression Scale. Scores on these measures are sometimes dichotomized in order to create depressed/nondepressed groups of women as a proxy for diagnostic categories, but continuous scores of symptom severity are more often used in research. Symptoms typically show linear or dose–response associations with outcomes such as preterm birth (PTB), low birth weight (LBW), or infant abnormalities. Our current understanding of negative affective states in pregnancy is based largely on these studies of symptomatology, not investigations of confirmed diagnoses, perhaps because investigators lacked clinical expertise or funding to conduct diagnostic interviews. More studies of confirmed diagnoses would be helpful, particularly with larger samples and controlling for antidepressant medications and other relevant variables. Nonetheless, research findings on symptoms of anxiety and depression in pregnancy are informative for clinicians regarding prenatal screening, early detection, prevention, and treatment of perinatal mood disturbances among expecting and new mothers.
Estimates of the prevalence of depression during pregnancy vary depending on the criteria used, but can be as high as 16% or more women symptomatic and 5% with major depression [ 2 ]. Firm estimates for prenatal anxiety do not exist, nor is there agreement about appropriate screening tools, but past studies suggest that a significant portion of women experience prenatal anxiety both in general and about their pregnancy [ 1■■ , 3 ]. Evidence of high exposure to stress in pregnancy is more widely available, at least for certain subgroups of women. For example, a recent study of a diverse urban sample found that 78% experienced low-to-moderate antenatal psychosocial stress and 6% experienced high levels [ 4 ]. Some of the stressors that commonly affect women in pregnancy around the globe are low material resources, unfavorable employment conditions, heavy family and household responsibilities, strain in intimate relationships, and pregnancy complications.
A large body of research is now available regarding stress and affective states during pregnancy as predictors of specific pregnancy conditions and birth outcomes [ 5 , 6 ]. The most commonly studied are PTB (<37 weeks gestation) and LBW (≤2500 g). Both are of US and international significance due to high incidence in many parts of the world and also consequences for infant mortality and morbidity. It has been estimated that two-thirds of LBW infants are born preterm. Thus, there are likely to be both common and unique etiological pathways [ 1■■ , 7■■ ]. Current theoretical models emphasize biopsychosocial and cultural determinants and interactions of multiple determinants in understanding these birth outcomes [ 8 , 9■■ , 10 – 12 ].
STRESS IN PREGNANCY
The literature on stress in pregnancy and birth outcomes is reviewed in two subsections, one on PTB and the other on LBW.
Stress and preterm birth
More than 80 scientific investigations on stress and PTB were recently reviewed by Dunkel Schetter and Glynn [ 7■■ ], of which a majority had prospective designs, large samples, and validated measures, and were fairly well controlled for confounds such as medical risks, smoking, education, income, and parity. These studies can be grouped by the type of stress examined. Of the more than a dozen published studies assessing `major life events in pregnancy', a majority found significant effects; women who experienced major life events such as the death of a family member were at 1.4 to 1.8 times greater risk of PTB, with strongest effects when events occurred early in pregnancy. The majority of a second, smaller group of studies on catastrophic, community-wide disasters (e.g., earthquakes or terrorist attacks) also showed significant effects on gestational age at birth or PTB. A third small set of studies on chronic stressors, such as household strain or homelessness, all reported significant effects on PTB. Finally, a majority of past investigations on neighborhood stressors such as poverty and crime indicated significant effects on gestational age or PTB. In comparison, studies on daily hassles and perceived stress did not consistently predict PTB. Thus, of the many distinguishable forms of stress, many (but not all) contribute to the risk of PTB.
Stress and low birth weight
A second area of developing convergence concerns the effects of stress on infant birth weight and/or LBW, reviewed recently by Dunkel Schetter and Lobel [ 9■■ ]. Again these studies can be organized by type of stressor. Evidence suggests that `major life events' somewhat consistently predicted fetal growth or birth weight, whereas measures of `perceived stress' had small or nonsignificant effects. `Chronic stressors', however, have been even more robust predictors of birth weight. For example, unemployment and crowding predicted 2.0 to 3.8 times the risk of LBW among low-income women in one study [ 13 ]. An important source of chronic stress is `racism or discrimination' occurring both during the pregnancy and over a woman's lifetime [ 14 ]. Racism and discrimination contribute to birth outcomes independently of other types of stress [ 15 ]. A growing number of studies have demonstrated that racism and discrimination prospectively predict birth weight, particularly in African–American women [ 16 ]. Although this literature has focused mainly on women in the USA, it is relevant to minority women in other countries [ 17 ].
In summary, chronic strain, racism, and related factors such as neighborhood segregation are significant risk factors for LBW [ 18 ]. Of note, investigations of chronic stress and racism do not usually take into account depressive symptoms. Yet, depression may be an important mechanism whereby the effects of exposure to chronic stress and racism influence fetal growth and birth weight, likely via downstream physiological and behavioral mechanisms [ 9■■ ].
ANXIOUS AND DEPRESSED AFFECT IN PREGNANCY
Recent research on symptoms of anxiety and depression during pregnancy is reviewed similarly within two subsections distinguishing findings on PTB from those on LBW.
Affect and preterm birth
State anxiety during pregnancy significantly predicted gestational age and/or PTB in seven of 11 studies recently reviewed [ 7■■ ], but only in combination with other measures or in subgroups of the sample. More consistent effects have been found for `pregnancy anxiety' (also known as `pregnancy-specific anxiety' and similar to `pregnancy distress'). Pregnancy anxiety appears to be a distinct and definable syndrome reflecting fears about the health and well being of one's baby, of hospital and health-care experiences (including one's own health and survival in pregnancy), of impending childbirth and its aftermath, and of parenting or the maternal role [ 1■■ , 19 ]. It represents a particular emotional state that is closely associated with state anxiety but more contextually based, that is, tied specifically to concerns about a current pregnancy. Assessment of pregnancy anxiety has entailed ratings of four adjectives combined into an index (`feeling anxious, concerned, afraid, or panicky about the pregnancy [ 20 ]' or use of a 10-item scale reflecting anxiety about the baby's growth, loss of the baby, and harm during delivery, as well as a few reverse-coded items concerning confidence in having a normal childbirth) [ 21 ]. Other measures exist as well.
There is remarkably convergent empirical evidence across studies of diverse populations regarding the adverse effects of pregnancy anxiety on PTB or gestational age at birth [ 7■■ , 19 ]. More than 10 prospective studies have been conducted on this topic, all of which report significant effects on the timing of birth. An early study found that the 10-item scale scores combined with a standard measure of state anxiety predicted gestational age of the infant at birth, controlling for medical risk factors, ethnicity, education, and income; these results were also independent of the effects of a woman's personal resources (sense of mastery, self-esteem, and dispositional optimism) [ 21 ]. Use of multidimensional modeling techniques later revealed that state anxiety, pregnancy anxiety, and perceived stress all predicted the length of gestation, but pregnancy anxiety (as early as 18 weeks into pregnancy) was the only significant predictor when all three indicators were tested together with medical and demographic risks controlled [ 20 ]. At least three large, well controlled, prospective studies have replicated these results using similar pregnancy anxiety measures [ 22 – 24 ]. The largest of these was a prospective study of 4 885 births finding that women with high pregnancy anxiety were at 1.5 times greater risk of a PTB, controlling for socio-demographic covariates, medical and obstetric risks, and specific worries over a high-risk condition in pregnancy [ 23 ].
In sum, recent evidence is remarkably convergent, indicating that pregnancy anxiety predicts the timing of delivery in a linear manner. Further, pregnancy anxiety predicts risk of spontaneous PTB with meaningful effect sizes across studies, comparable to or larger than effects of known risk factors such as smoking and medical risk. These effects hold for diverse income and ethnic groups in the USA and in Canada. The consistency of these findings paves the way for investigating the antecedents and correlates of pregnancy anxiety, mechanisms of effects, and available treatments.
In contrast, relatively few of the more than a dozen studies on depressed mood or symptoms of trauma found significant effects on gestational age or PTB [ 9■■ ]. A Swedish study found that elevated antenatal depressive symptoms predicted increased risk for PTB [odds ratio (OR) = 1.56] [ 25 ], and a recent meta-analysis concluded that PTB was associated with depression across 11 studies. However, in general, effect sizes were relatively small across studies with an average OR of 1.13 [confidence interval (CI 1.07–1.30)] [ 26 ].
Affect and low birth weight
Recent evidence points more often to the role of maternal depressive symptoms in the etiology of LBW as compared with the etiology of PTB [ 27■■ ]. The recent meta-analysis on depression in pregnancy, cited earlier, evaluated 20 studies and found that high depressive symptoms were associated with 1.4 to 2.9 times higher risk of LBW in undeveloped countries, and 1.2 times higher risk on average in the USA [ 26 ]. Another recent review found relatively large effects of maternal depressive symptoms on infant birth weight across several studies, with the largest effects for low-income or low social status women and women of color [ 9■■ ]. Furthermore, although there are few studies on diagnosed disorders, one study reported that mothers with a depressive disorder had 1.8 times greater risk of giving birth to a LBW infant [ 28 ]. Thus, evidence appears to be stronger for contributions of depressive symptoms or disorder to slower growth of the fetus and LBW than to the timing of delivery or PTB, and these effects are pronounced for disadvantaged women [ 29 ]. In contrast, very few studies have demonstrated any effects of anxiety on LBW, with rare exceptions [ 30 ].
STRESS AND NEGATIVE AFFECTIVE STATES IN PREGNANCY AND INFANT OR CHILD OUTCOMES
Evidence for effects of maternal stress, depression, and anxiety in pregnancy on adverse neurodevelopmental outcomes for the child is substantial [ 31 ], through a process known as `fetal programming' [ 5 , 32 ]. Research utilizing animal models indicates that maternal distress negatively influences long-term learning, motor development, and behavior in offspring [ 33 , 34 ]. Evidence suggests that this occurs via effects on development of the fetal nervous system and alterations in functioning of the maternal and fetal hypothalamic pituitary adrenal (HPA) axes [ 34 – 36 ]. Maternal mood disorders have also been shown to activate the maternal HPA axis and program the HPA axis and physiology of the fetus [ 37 , 38 ]. In short, a mother's stress exposure and her affective states in pregnancy may have significant consequences for her child's subsequent development and health [ 5 , 39 – 43 ]. This evidence has been reviewed in many articles and spans effects on attention regulation, cognitive and motor development, fearful temperament, and negative reactivity to novelty in the first year of life; behavioral and emotional problems and decreased gray matter density in childhood; and impulsivity, externalizing, and processing speed in adolescents [ 44 – 47 ]. Of note, many of these findings involve the effects of prenatal pregnancy anxiety on infant, child, or adolescent outcomes. Maternal stress has also been linked to major mental disorders in offspring [ 40 , 47 ].
SUMMARY AND KEY ISSUES
In summary, there is substantial evidence that anxiety, depression, and stress in pregnancy are risk factors for adverse outcomes for mothers and children. More specifically, anxiety in pregnancy is associated with shorter gestation and has adverse implications for fetal neurodevelopment and child outcomes. Furthermore, anxiety about a particular pregnancy seems to be especially potent. Finally, chronic strain, exposure to racism, and depressive symptoms in mothers during pregnancy are associated with lower birth weight infants with consequences for development as well. These differential risk factors and related pathways to PTB and LBW deserve further investigation. Beyond this, women with high stress, anxiety, and depressive symptoms in pregnancy are more likely to be impaired during the postpartum period. Postpartum affective disturbance and stress in turn impair parenting quality and effectiveness [ 48 ]. Figure 1 summarizes the evidence that has been briefly reviewed in a simple schematic with connections in bold representing those with notably stronger and more consistent evidence. This simple diagram can be elaborated further to include associations among the various types or forms of stress and to include mediated pathways to birth outcomes. For example, major life events or community catastrophes can be hypothesized to increase pregnancy anxiety, and long-term chronic strain to increase risk of depression. The effects of chronic strain on LBW via depression are also not depicted but are worthy of further research. Together, the evidence and developing consensus that biological and behavioral mechanisms explain these findings lay the groundwork for a next era of psychiatric and collaborative interdisciplinary research on pregnancy.

Summary of evidence on depression, anxiety and stress. GA, gestational age at birth; LBW, low birth weight; PTB, preterm birth.
Why pregnancy anxiety?
It is not clear why `pregnancy anxiety' has such powerful effects on mothers and their babies. In fact, the nature of this concept has not yet received sufficient attention to be fully explicated. Possibly what makes it potent is that measures of pregnancy anxiety capture both dispositional characteristics, or traits, and environmentally influenced states. For example, women who are most anxious about a pregnancy seem to be more insecurely attached, of certain cultural backgrounds, more likely to have a history of infertility or to be carrying unplanned pregnancies, and have fewer psychosocial resources [ 49 ]. These results suggest that existing vulnerabilities that predate pregnancy may interact with the social, familial, cultural, societal, and environmental conditions of pregnancy to increase levels of pregnancy anxiety, producing effects on the maternal–fetal–placental systems, especially during sensitive periods such as early pregnancy. This process can then adversely influence fetal development by programming the fetus's HPA axis and also have effects on the initiation of labor via maternal, fetal, and placental hormonal exchanges. Although there is much we do not know, a worthwhile future goal for clinical researchers may be to identify women high in anxiety before conception, as well as women high in anxiety during pregnancy, and especially those women who are anxious about specific aspects of their pregnancies – about this child and this birth, and about competently parenting with this partner. These women would appear to be targets for early intervention such as evidence-based interventions for stress reduction, mood regulation treatments such as cognitive behavioral therapies, pharmacological treatments, and follow-up care during postpartum to prevent a range of adverse outcomes for mother, child, and family.
Clinical screening for affective symptoms in pregnancy
Clinical screening for depression or anxiety in prenatal and postpartum healthcare has been widely recommended but is also potentially problematic. The issues concern what screening tools to use; what cutoffs to adopt for identifying women at risk; the need for expert clinicians to follow up on those women who score above thresholds to make diagnoses; and, for those who have established diagnoses, the availability of affordable and efficacious treatments [ 50 ]. These issues must be resolved for prenatal (and postpartum) clinical screening to be recommended widely. For example, the EPDS, which is a gold standard used widely in clinic settings for depression screening both prepartum and postpartum, actually measures both depressive and anxiety symptoms, which may contribute to confusion about risks [ 51 ]. In addition, experts have questioned the validity of a diagnosis of depressive disorders using standard diagnostic criteria for mood disturbance because they include typical somatic symptoms of pregnancy such as fatigue, sleep disturbance, and appetite changes [ 52 ]. Also relevant is one recent study reporting that women with both depression and anxiety disorders were at highest risk of LBW, as compared with those with only depressive or anxious symptoms or none [ 53 ]. Combinations of symptoms have received very little research attention. Furthermore, little research thus far has examined the feasibility and utility of screening for prenatal stress or pregnancy anxiety.
If broad screening for affective symptoms during pregnancy results in high rates of false-positive results, low rates of clinical follow-up and referral, insufficient or ineffective education for women about the meaning of screening results, lack of treatment, and/or absence of proven evidence-based interventions, then clinical screening as a standard procedure in specific prenatal settings is of questionable value. Nonetheless, if important preconditions can be met, screening for pregnancy anxiety, state anxiety, depressive symptoms, and stress in pregnancy stands to provide potentially important clinical benefits for mothers and their children [ 54 , 55 ].
The broader context of pregnancy
An essential consideration in implementing widespread effective prenatal screening, diagnosis, and treatment is the context of a woman's pregnancy. The context includes her partner, family, friends, neighborhood, and larger community, all of which are known to influence a woman's mental health and responses to a diagnosis of disorder. Therefore, attention must be paid to these levels of influence in any attempts to screen and treat depression, anxiety, pregnancy anxiety, or stress in pregnancy. For example, a woman's ability to understand or respond to a diagnosis of a mood or anxiety disorder and accept treatment may be facilitated by involving her partner, closest relative, or friend in follow-up after screening. Families and communities can undermine or enhance efforts to screen and treat women in pregnancy as a result of their beliefs, values, and level of information (or misinformation). Although these issues are known barriers to community mental health treatment in diverse populations, they have not yet been addressed in establishing appropriate clinical procedures in pregnancy for follow-up of widespread screening for affective disorders. It may also be useful to identify a range of protective and resilience factors such as mastery, self-efficacy and social support in women for the purpose of intervention planning [ 2 , 56■■ ]. If efforts are directed to strengthening women's psychosocial resources as early as possible, ideally before conception, it is possible that prenatal health and outcomes could be better optimized.
In conclusion, although considerable, rigorous research now demonstrates the potential deleterious effects of negative affective states and stress during pregnancy on birth outcomes, fetal and infant development, and family health, we do not yet have a clear grasp on the specific implications of these facts. Key issues for the next wave of research are as follows: disentangling the independent and comorbid effects of depressive symptoms, anxiety symptoms, pregnancy anxiety, and various forms of stress on maternal and infant outcomes; better understanding the concept of pregnancy anxiety and how to address it clinically; and further investigating effects of clinically significant affective disturbances on maternal and child outcomes, taking into account a mother's broad socio-environmental context. As our knowledge increases, it will be critical to identify the signs, symptoms, and diagnostic thresholds that warrant prenatal intervention and to develop efficient, effective, and ecologically valid screening and intervention strategies to be used widely. If risk factors can be identified prior to pregnancy and interventions designed for preconception, many believe this window of opportunity is our best bet [ 57 ]. Interdisciplinary research and collaboration will be crucial, however, to meeting these objectives and in order to reduce the burden of maternal stress, depression, and anxiety in the perinatal period.
- Anxiety, depression, and stress in pregnancy are risk factors for adverse outcomes for mothers and children.
- Anxiety regarding a current pregnancy (`pregnancy anxiety') is associated with shorter gestation and has adverse implications for preterm birth, fetal neurodevelopment and child outcomes.
- Chronic strain (including long-term exposure to racism) and depressive symptoms in mothers during pregnancy are associated with lower birth weight with many potential adverse consequences.
- These distinguishable risk factors and related pathways to distinct birth outcomes merit further investigation.
- It is critical to agree upon the signs, symptoms and diagnostic thresholds that warrant prenatal intervention and to develop efficient, effective, and ecologically valid screening and intervention strategies that can be used widely.
Acknowledgements
The contributions of collaborators Laura Glynn, PhD, Calvin Hobel, MD, and Heidi Kane, PhD to this program of work are gratefully acknowledged.
Conflicts of interest There are no conflicts of interest .
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as: ■ of special interest ■■ of outstanding interest Additional references related to this topic can also be found in the Current World Literature section in this issue (p. 162).
Depression During Pregnancy
Medical review policy, latest update:.
Updates throughout to text, information, and sources, plus a new medical review.
Recommended Reading
What are the risk factors for depression in pregnancy, what causes depression during pregnancy, what are the symptoms of depression during pregnancy, can depression during pregnancy affect your baby, treatments for pregnancy depression, 1. non-drug treatments, 2. antidepressants, can you prevent pregnancy depression.
Taking action is the first step towards protecting your mental health so you can feel better — and give you and your baby the best possible start together.
Updates history
Jump to your week of pregnancy, trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
- Share full article
Advertisement
Supported by
Depression During and After Pregnancy Can Be Prevented, National Panel Says. Here’s How.
The task force of experts recommended at-risk women seek certain types of counseling, and it cited two specific programs that have been particularly effective.

By Pam Belluck
As many as one in seven women experience depression during pregnancy or in the year after giving birth. Now, for the first time, a national panel of health experts says there is a way to prevent it.
Some kinds of counseling can keep some women from developing debilitating symptoms that can harm not only them but their babies, the panel reported on Tuesday. Its report amounted to a public call for health providers to seek out women with certain risk factors and guide them to counseling programs. The recommendation, by the United States Preventive Services Task Force , means that insurers will be required to cover those services — with no co-payments — under the Affordable Care Act.
“We really need to find these women before they get depressed,” said Karina Davidson, a task force member and senior vice president for research for Northwell Health.
[ Like the Science Times page on Facebook. | Sign up for the Science Times newsletter. ]
Perinatal depression , as it is called, is estimated to affect between 180,000 and 800,000 American mothers each year and up to 13 percent of women worldwide . The condition increases a woman’s risk of becoming suicidal or harming her infant, the panel reported. It also increases the likelihood that babies will be born premature or have low birth weight, and can impair a mother’s ability to bond with or care for her child. The panel reported that children of mothers who had perinatal depression have more behavior problems, cognitive difficulties and mental illness.
The panel emphasized that perinatal depression is shouldn’t be confused with “baby blues” — the tears, irritability, fatigue, and anxiety that many women experience after delivery but which evaporates within 10 days.
The panel evaluated research on numerous possible prevention methods , including physical activity, education, infant sleep advice, yoga, expressive writing, omega-3 fatty acids and antidepressants. Several showed some promise, including physical activity and programs in Britain and the Netherlands involving home visits by midwives or other providers. But only counseling demonstrated enough scientific evidence of benefit.
Women receiving one of two forms of counseling were 39 percent less likely than those who didn’t to develop perinatal depression. One approach involved cognitive behavioral therapy, helping women navigate their feelings and expectations to create healthy, supportive environments for their children. The other involved interpersonal therapy, including coping skills and role-playing exercises to help manage stress and relationship conflicts.
“This recommendation is really important,” said Jennifer Felder, an assistant professor of psychiatry at University of California, San Francisco, who was not on the panel. “This focuses on identifying women who are at risk for depression and proactively preventing its onset, using concrete guidelines.”
The panel recommended counseling for women with one or more of a broad range of risk factors, including a personal or family history of depression; recent stresses like divorce or economic strain; traumatic experiences like domestic violence; or depressive symptom s that don’t constitute a full-blown diagnosis. Others include being a single mother, a teenager, low-income, lacking a high school diploma, or having an unplanned or unwanted pregnancy, panel members said.
It highlighted two specific programs, which were similarly successful, Dr. Davidson said. They counsel first-time mothers and those who already have children. They are available in Spanish and focus on low-income women, about 30 percent of whom develop perinatal depression, experts say.
One program, “ Mothers and Babies ,” includes cognitive behavioral therapy in eight to 17 group sessions, often delivered in clinics or community health centers, primarily during pregnancy with at least two sessions postpartum.
“It’s really meant to break down this idea that talking about your thoughts and behaviors is scary,” said Darius Tandon, an associate professor at Northwestern University’s Feinberg School of Medicine and principal investigator of several “Mothers and Babies” studies.
So far, health and human service agencies in over 175 counties in 21 states have been trained to implement the program. It is also being evaluated in Florida and the Midwest to see if it works when administered one-on-one by home visiting caseworkers instead of groups run by psychologists or social workers, Dr. Tandon said.
The other program, “ Reach Out, Stay Strong, Essentials for New Moms ” or ROSE, typically delivered in four sessions during pregnancy and one postpartum, can be administered in groups or one-on-one by nurses, midwives or anyone trained to follow the manual, said Jennifer Johnson, a professor of public health at Michigan State University.
So far, women in Rhode Island, Mississippi and Japan have participated, said ROSE’s creator, Caron Zlotnick, a professor of psychiatry and human behavior at Brown University. She and Dr. Johnson are testing its expansion to 90 clinics throughout the country.
Karla Manica, 30, a single mother of four in Detroit, participated in “Mothers and Babies” when pregnant with her youngest, who is now 1. She said she experienced abuse as a child and in relationships, attempted suicide by drinking cleaner, lived in homeless shelters after being laid off from her job as a dementia caregiver, and has had bipolar depression.
“It was good to come to the table and share,” Ms. Manica said. The counselor texted uplifting messages between sessions, and “homework assignments” to engage in stress-relieving activities were useful. When Ms. Manica learned her baby’s father had another girlfriend, she said, the group “gave me hope.”
After her daughter Kathryn was born, “I was well,” Ms. Manica said. “If I hadn’t got with the Mothers and Babies, would I have been prepared, would I have gotten the confidence I have now? No.”
Experts and leaders of the programs, whose curriculums and counselor training are free, said financial and other obstacles exist.
“Cost is definitely still an issue,” said Dr. Tandon. He said one prenatal session costs clinics delivering the counseling $40 to $50 to provide mothers’ transportation and child care, and Medicaid doesn’t have a reimbursement code for preventive counseling, so clinics often absorb the cost of staff time to provide it.
Access to counseling also can be difficult. “Especially when you’re pregnant and you have competing demands on your time and energy, or if you have a little one at home,” said Dr. Felder, who wrote an editorial about the recommendation. Offering it online or through apps may help.
Even in some cases in which it doesn’t prevent depression, counseling may be beneficial, said Dr. Melissa Simon, a task force member and vice chairwoman of research at Northwestern’s Feinberg School of Medicine’s obstetrics and gynecology department. “It provides the pregnant person with education and coping strategies,” she said, and can encourage those who develop depression to seek treatment faster.
Captoria Porter, 28, of Bolingbrook, Ill., who has seven children, ages 2 months to 11, experienced no depression during or after her first five pregnancies. But during her sixth, life became more tumultuous, with marital problems and the need to move in with her sister because the housing project where she was living was closing.
After the birth of Myla, now 1, “I think I had symptoms of depression,” said Ms. Porter, who has worked as a telemarketer selling sanitizer dispensers. “I was really sad.”
Fortunately, the pre-birth “Mothers and Babies” sessions helped her recognize signs like “you don’t want to brush your hair or you don’t want to be bothered with the baby,” she said. “I would find myself feeling that way.”
Ms. Porter met twice with a community center counselor, but realized the program had already taught her the practices he recommended: “Reaching out to family and friends. Learning that I can’t control everything. Eating when the baby eats, sleeping when the baby sleeps, laying the kids down for a nap and calling it ‘me time.’”
That warded off full-blown depression. “I caught it early,” she said.
The panel encouraged more research on all prevention approaches. In reviewing 50 studies of various methods, it found negative effects only in the two small studies with antidepressants. One study reported instances of dizziness and drowsiness among women who took Zoloft. The other reported that more women taking Pamelor experienced constipation.
“Some people have asked, ‘Why aren’t you just recommending antidepressants?’” Dr. Davidson said. “Of course, antidepressants were developed and studied for someone who has depression. We need to consider possible benefits and possible harms to parent and fetus when someone is not depressed and you’re giving them a drug to treat depression on the off-chance it prevents depression.”
Beth Sanfratel, 43, a preschool teacher in Birmingham, Ala., said she wished she’d had a counseling program when pregnant with the second of three sons, Mac, now 10.
“I don’t even think postpartum depression was mentioned,” she said. Several months after Mac was born, Ms. Sanfratel, usually upbeat and social, said she began having crying spells. “I was having trouble getting up and in general just being really bummed out.”
Ultimately, Ms. Sanfratel, a former social worker, recognized she needed help and took antidepressants for about a year, resuming them shortly before her third son, Beau, was born in 2011.
“Getting moms figuring out what’s going on ahead of the actual delivery, it’s a great, great thing,” she said.
Pam Belluck is a health and science writer whose honors include sharing a Pulitzer Prize and winning the Nellie Bly Award for Best Front Page Story. She is the author of Island Practice, a book about an unusual doctor. More about Pam Belluck
Pregnancy, Childbirth and Postpartum Experiences
Aspirin’s Benefits: Not enough pregnant women at risk of developing pre-eclampsia, life-threatening high blood pressure, know that low-dose aspirin can help lower that risk. Leading experts are hoping to change that.
‘A Chance to Live’: Cases of trisomy 18 may rise as many states restrict abortion. Some women have chosen to have these babies , love them tenderly and care for them devotedly.
Teen Pregnancies: A large study in Canada found that women who were pregnant as teenagers were more likely to die before turning 31 .
Weight-Loss Drugs: Doctors say they are seeing more women try weight-loss medications in the hopes of having a healthy pregnancy. But little is known about the impact of those drugs on a fetus.
Premature Births: After years of steady decline, premature births rose sharply in the United States between 2014 and 2022. Experts said the shift might be partly the result of a growing prevalence of health complications among mothers .
Depression and Suicide: Women who experience depression during pregnancy or in the year after giving birth have a greater risk of suicide and attempted suicide .
- Search Menu
- Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Politics of Development
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >
7 Depression During Pregnancy and the Postpartum Period
Shaila Misri, M.D., Reproductive Mental Health Program, B.C. Children’s and Women’s Hospital, St. Paul’s Hospital; Department of Psychiatry, Faculty of Medicine, University of British Columbia; and B.C. Mental Health and Addiction Services, Provincial Health Services Authority.
Jasmin Abizadeh, Reproductive Mental Health Program, B.C. Children’s and Women’s Hospital, St. Paul’s Hospital; Department of Psychiatry, Faculty of Medicine, University of British Columbia; and B.C. Mental Health and Addiction Services, Provincial Health Services Authority.
Sonya Nirwan, Reproductive Mental Health Program, B.C. Children’s and Women’s Hospital, St. Paul’s Hospital.
- Published: 05 December 2014
- Cite Icon Cite
- Permissions Icon Permissions
Depression affects 9–13% of pregnant women and 12–16% of postpartum women. Rates vary depending on whether depressive symptoms or DSM diagnoses of depression are considered. Risk factors of perinatal depression include socioeconomic status, social support, personality style, personal and family history of depression, and hormonal changes. The Edinburgh Postnatal Depression Scale (EPDS) is a self-report instrument commonly used to assess for perinatal depression. The treatment of perinatal depression with antidepressant medication is controversial. Most guidelines recommend psychotherapy for mild to moderate depression and medication for moderate to severe depression. Established psychotherapies include interpersonal psychotherapy and cognitive behavioral therapy, as well as alternative therapies such as infant massage in the postpartum. Although extensive research on perinatal depression has been conducted over the past two decades, future research could include designing prospective, methodologically sound studies with larger samples to compare treatment modalities, teratogenicity associated with pharmacotherapy, and prevalence of perinatal depression in various cultures.
Although the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) includes the specifier “with peripartum onset” for a diagnosis of major depressive disorder (MDD), it does not acknowledge postpartum depression (PPD) with an onset beyond 4 weeks ( American Psychiatric Association [APA], 2013 ). The revisions however from the DSM-IV to the DSM-5 now account for MDD during pregnancy compared to just a postpartum onset before. In clinical practice, PPD has been noted to occur at any time within the first 12 months following childbirth. Terms used synonymously to describe perinatal depressive illness include antenatal or prenatal depression (i.e., depression during pregnancy) and postpartum or postnatal depression (i.e., depression after childbirth). In this chapter, we use all of these terms.
Perinatal Prevalence Rates
In pregnancy, depressive symptoms generally have a prevalence rate of 20%, whereas MDD during this time period ranges from 9–13% ( Bowen & Muhajarine, 2006 ; Faisal-Cury & Rossi Menezes, 2007 ; Marcus, Flynn, Blow, & Barry, 2003 ). The rate of 13% in pregnancy is based on a meta-analysis of 30 studies by Gaynes et al. (2005) . The National Epidemiological Survey on Alcohol and Related Conditions (NESARC) yielded a figure of 12.4% in 1,524 women, whereas the lower rate of 9% was found in a smaller study of 326 women ( Benute et al., 2010 ; Le Strat, Dubertret, & Le Foll, 2011 ). Although the rates of subclinical depressive symptoms may be higher in the pregnant population, the reported rates of MDD in pregnancy are not dissimilar to those reported in the non-childbearing population (7–13% of the global female population; Blehar, 2001 ; Berardi et al., 2002 ; Lepine, Gastpar, Mendlewicz, & Tylee, 1997 ; Statistics Canada, 2002 ).
Furthermore, some studies have described a variation of rate in each trimester, whereas others do not. In their systematic review of the literature, Bennett, Einarson, Taddio, Koren, and Einarson (2004) described a depression prevalence rate of 7.4% in the first, 12.8% in the second, and 12.0% in the third trimesters on the basis of observational studies and surveys using validated screening instruments. The authors cautioned interpretation of the lower rate of 7.4% in the first trimester due to the availability of few studies and the small number of study participants. Clinically, the underreporting of depression in the first trimester is not uncommon due to the symptom overlap between signs of pregnancy and symptoms of depressive illness specifically in primiparous women. The higher prevalence rates in the second and third trimester may be a reflection of greater demands of advancing pregnancy being responsible for increasing the risk of depression. Another explanation for why depression rates may peak in the second and third trimester is that women are more likely to seek medical care in the second and third trimester than in the first, so those at risk may be more easily identified ( Kelly et al., 1999 ). Other authors have found a peak in the first trimester only, including findings from two longitudinal studies by Kitamura, Shima, Sugawara, and Toda (1993 ; n = 120), which used a structured diagnostic interview to identify depression, and Kumar and Robson (1984 ; n = 119), which used a semistructured interview as well as a self-rated questionnaire. Lastly, a study by Ancill, Hilton, Carr, Tooley, and McKenzie (1986) found a peak only in the third trimester using a similar sample size ( n = 108) and a prospective longitudinal design. Authors of this paper cautioned that the higher prevalence of third-trimester depression could have resulted from the misidentification of physical discomforts of pregnancy as somatic signs of depression in pregnancy, as identified with the Hamilton Rating Scale for Depression (HAM-D; Hamilton, 1960 ).
There is an increased rate of depressive symptoms in the postpartum period (i.e., 19.2%) in comparison to MDD, where the most commonly cited rate is between 12% and 16% ( Gavin et al. 2005 ; Mori et al., 2011 ; O’Hara & Swain, 1996 ). Variability in prevalence rates depends on whether researchers report depressive symptoms or the diagnosis of MDD. Additional factors that affect the variation of the reported rate in postpartum women include methodological differences (e.g., prospective vs. retrospective design), the use of different screening measures, differences in the definition of depression, and the onset of the episode. PPD can occur early or late in the first 12 months after childbirth. In a prospective study, Mori et al. (2011) showed that the prevalence rate of PPD was 11% for early onset and 4% for late onset when using the Edinburgh Postnatal Depression Scale (EPDS; Cox, Holden, & Sagovsky, 1987 ) as the screening instrument.
PPD rates also fluctuate as a function of the country in which the epidemiological data are collected ( Goldbort, 2006 ; Halbreich & Karkun, 2006 ). Halbreich and Karkun (2006) reviewed 143 studies of postpartum prevalence in 40 countries and found a range of 0% to 60%, concluding that the frequently reported range of 10–15% is not representative of the rates worldwide. Researchers examining depression in countries such as Singapore (0.5%), Malta (3.9%), Malaysia (3.9%), Austria (5.0%), and Denmark (5.5%) reported a much lower rate in comparison to researchers examining depression in Brazil (42.8%), Guyana (57.0%), Costa Rica (34.0–48.0%), Italy (38.1%), Chile (37.4%), South Africa (36.5%), Taiwan (34.5%), and Korea (36.1–48.0%).
The disparity in findings may have been due to cultural issues surrounding the conceptualization of mental illness, accompanying stigma, differences in reporting style, and socioeconomic/biological vulnerability factors; for example, the term PPD may be unknown or unacceptable to some non-Western cultures, and the Western diagnostic standards may not be applicable to other cultures ( Posmontier & Horowitz, 2004 ). Specifically, Asian women tend to express depression in somatic terms versus affective symptoms. This may contribute to overdiagnosis if a questionnaire is used that assesses affective and somatic symptoms; it may lead to underdiagnosis if the clinician does not interpret the somatic symptoms as an expression of PPD ( Lee, Yip, Chiu, Leung, & Chung, 2001 ; Park & Dimigen, 1995 ; Yoshida et al., 1997 ). For example, Japanese women may be more likely to focus on their physical problems instead of their depression, and Chinese women may be more likely to complain about physical symptoms, such as “wind inside the head” or head numbness, to describe their depression ( Lee et al., 2001 ; Yoshida et al., 1997 ). Reported rates of depression may vary from one culture to another depending on the perceived stigma, the reporting style, and varying cutoff scores on a screening tool ( Dankner, Goldberg, Fisch, & Crum, 2000 ; Stuchbery, Matthey, & Barnett, 1998 ). In addition, in their view, Halbreich and Karkun (2006) concluded that certain rituals, recognition of role transition, and the mobilization of support and help for the new mother may serve as protective factors for PPD, as seen among Koreans, Chinese, Japanese, Mexicans, Nigerians, and others. In Western culture, mothers have little time to recover from childbirth, are often socially isolated, and are expected to juggle multiple roles soon after delivery, which could contribute to an increased prevalence of PPD.
The course of perinatal depression is affected by the age of onset, time of onset, hormonal changes, severity of symptoms, duration of illness, and the number of previous episodes. In addition, psychiatric and medical/obstetric comorbidities govern the course of perinatal depression. The age of onset of MDD for females is in their early 20s to 30s, and peak incidence occurs at 30 years, which falls during the childbearing years ( Eaton et al., 1997 ; Weissman et al., 1996 ). Early onset of the disease leads to repeated relapses and recurrences throughout life and the reproductive period, particularly if the first episode occurs before 18 years of age ( Coryell et al., 2009 ; Klein et al., 1999 ; Zisook et al., 2007 ).
Hormonal changes throughout the female life cycle have a crucial effect on the emergence and progression of the mood disorder. After menarche, the mood changes can present as premenstrual symptoms and, in severe cases, may meet the DSM-5 criteria for a mood disorder called premenstrual dysphoric disorder (PMDD; Biggs & Demuth, 2011 ; Gonda et al., 2008 ). PMDD may increase the risk of PPD and affect the course of depression in the perinatal period as a result. One study prospectively diagnosed postpartum mood disorders in women and also retrospectively reported PMDD in two groups of women, identified as either at low risk ( n = 109) or at high risk of postpartum mood disorders ( n = 133; Bloch, Rotenberg, Koren, & Klein, 2005 ). Results showed that 23% of women with PMDD also experienced depression in the postpartum period. Pregnancy and childbirth is a time of highest vulnerability, with rapid hormonal escalation and decline ( Marcus, 2009 ). Repeated pregnancies and childbirths increase the frequency and duration of the illness. Those with a history of PPD with the first child have a 25–50% recurrence of the disease with their second pregnancy ( Altshuler, Hendrick, & Cohen, 1998 ). In one study, multiparous depressed women were found to be at an increased risk for experiencing the depressive episode more intensely than primiparous women ( Righetti-Veltema, Conne-Perréard, Bousquet, & Manzano, 2002 ).
Another important factor that impacts the course of perinatal depressive illness is the presence of a personality disorder. Women with MDD and a personality disorder have more frequent episodes lasting more than 1 year, inadequate response to pharmacotherapy, and poorer recovery after hospital discharge compared to those with MDD but no personality disorder ( Black, Bell, Hulbert, & Nasrallah, 1988 ; Newton-Howes, Tyrer, & Johnson, 2006 ). In another study in which depressive symptoms and personality disorder were assessed in postpartum women at 6 weeks and 12 months after childbirth, those with dependent and obsessive-compulsive personality disorder (71.4%) were more depressed compared to those without these disorders (5%; Uguz, Akman, Sahingoz, Kaya, & Kucur, 2009 ). In this study, the presence of the personality disorder alone was an independent predictor of PPD at 1-year follow-up. Thus, it seems that women with personality disorders have more severe and persistent depression than do those without personality disorders.
Treatment of depression also impacts its course. The average length of an untreated episode can last between 6 and 12 months, as shown by a cross-national epidemiologic survey involving about 38,000 community subjects across 10 different countries ( Weissman et al., 1996 ). Even after treatment, relapse rates may be high and occur quickly. In a naturalistic study of depressed patients, 12% relapsed within 4 weeks after recovery from an episode of depression and 25% relapsed within 12 weeks ( Keller, Shapiro, Lavori, & Wolfe, 1982 ).
Correlates and Risk Factors
Demographic and socioeconomic risk factors.
The NESARC reported that relationship status significantly correlates with perinatal depression. Specifically, depressed pregnant women were 2.05 times more likely to be never married and 3.30 times more likely to be widowed, divorced, or separated ( Le Strat et al., 2011 ).
In addition, socioeconomic status (SES) is an important risk factor related to depression. However, not all aspects of SES are associated with depressive illness, as findings have been mixed. For example, lower income and lower educational level were related to depressive symptoms, whereas unemployment was not related to depressive symptoms in a meta-analysis of studies that evaluated associations between prenatal depressive symptoms and risk factors ( Lancaster et al., 2010 ).
Melville, Gavin, Guo, Fan, and Katon (2010) found ethnicity to be also a major risk factor in pregnant women, with Asian and African Americans having a 2.98- to 5.81-fold increased risk. There was a 2.50-fold greater propensity for Hispanic women. In addition, age is another factor that can impact PPD, with a U-shaped pattern showing an increased association of PPD with younger and older maternal age ( Milgrom et al., 2008 ; Mori et al., 2011 ).
Thus, the existing literature suggests that whereas the correlation between SES and depression is mixed, ethnicity, age, and relationship status appear to have a clearer association. It is important to be aware of demographic and socioeconomic variables as potential risk factors for perinatal depression and evaluate their impact for each patient.
Psychosocial Risk Factors
Numerous psychological and social factors that can affect perinatal depression include life stressors, situational stressors, presence of social support, quality of relationships, and personality traits. With regard to life stressors, one study reported that depressed women who were pregnant in the past year had a 2.59 to 9.15 greater likelihood of reporting at least one stressful life event during their pregnancy compared to women who were pregnant but not depressed ( Le Strat et al., 2011 ). In their review, Lancaster et al. (2010) also found a medium association between increased life stress and antenatal depression in 18 studies assessing life events and daily hassles.
The psychological response to unplanned pregnancy is an important factor that can increase the vulnerability to perinatal depression. In clinical practice, often these are single mothers who conceive when the relationship is ending and have little to no family support. A previous history of depressive illness in such a woman, with an unpredictable course of the mood disorder in the perinatal period, can be a further complicating factor. Empirically, Benute et al. (2010) found that 86.2% of depressed women had an unplanned pregnancy compared to 68.4% of women without depression.
Social support is another important variable in contributing to the onset of perinatal depression. In a review of 20 studies that examined social support and depression during pregnancy, a correlation was found between the two ( Mori et al., 2011 ). Specifically, lack of emotional social support during pregnancy was found to be significantly correlated with the development of early-onset PPD (odds ratio [OR] = 2.3) as well as late-onset PPD (OR = 3.3). Among the types of social support, lack of partner support was most strongly correlated with early- or late-onset PPD ( Mori et al., 2011 ). In addition to the availability of social support, the quality of the partner relationship is also linked to the outcome of PPD ( Brugha et al., 1998 ; Pope, 2000 ), with studies showing that the closeness of the relationship with the partner seems most consequential in explaining PPD ( Beck, 2001 ; Boyce et al., 1998 ; Segre, O’Hara, Arndt, & Stuart, 2007 ). In a new mother who is psychologically vulnerable, a supportive and appreciative partner may serve as a protective factor against PPD ( Marks, Wieck, Checkley, & Kumar, 1996 ). For example, Misri, Kostaras, Fox, and Kostaras (2000) used the Dyadic Adjustment Scale (DAS; Spanier, 1976 ) to measure the change in the marital relationship over seven study visits. Postpartum women were assigned either to a control group, in which the patient attended therapy sessions alone, or to a support group, in which the patient’s partner also attended select therapy sessions. The patients in the support group showed greater cohesiveness in their relationship and a decrease in depressive symptoms compared to the control group.
Domestic violence may play an important role in women who experience antenatal depression. A review by Lancaster et al. (2010) showed a small association between domestic violence and depressive symptoms in six studies that were reviewed. However, one study found that domestic abuse in the year prior to pregnancy was associated with nearly 2.5 times more of a likelihood of being diagnosed with depression in pregnancy. This latter study was conducted with a sample of women ( n = 130) from an urban low-income population and may not have been representative of the population of perinatal women in general ( Jesse, Walcott-McQuigg, Mariella, & Swanson, 2005 ). Similar results were reported in a recent study where women who experienced domestic violence had a 3.45-fold increased risk of experiencing antenatal depression relative to antenatal women who did not experience domestic violence ( Melville et al., 2010 ).
Personality and cognitive style have been examined as possible risk factors for perinatal depression. In a study by Jones et al. (2010) , those women with depression during pregnancy were seen to have higher levels of neuroticism and dysfunctional beliefs, but lower levels of self-esteem and extraversion. The findings of this study further illustrate that women who have a history of depression in the perinatal period tend to demonstrate greater negative evaluation of self, dependency on others, and need for control. Perfectionism and high interpersonal sensitivity may also heighten the risk for the onset and recurrence of PPD, with an increased risk of 1.26 of endorsing a higher EPDS score in those women with perfectionistic traits ( Boyce, Parker, Barnett, Cooney, & Smith 1991 ; Milgrom et al., 2008 ).
Biological Risk Factors
Biological factors play a considerable role in the onset and perpetuation of maternal psychiatric illness. Among the important factors that govern vulnerability to depressive illness is a positive family and personal history of depression. In the perinatal population, studies have shown that there is a twofold risk of recurrence of the illness in those with a previous episode of depression ( Banti et al., 2011 ; Pope, 2000 ). The presence of a medical disorder is another noteworthy risk factor for depression in pregnant women, as shown by Benute et al. (2010) in a study of pregnant women with a medical disorder ( n = 326). In this study, MDD was diagnosed in 7.1% of women with preeclampsia or chronic hypertension, 12.1% with cardiac disorder, 7.1% with diabetes mellitus, 6.3% with anemia, 8.3% with collagenosis, and 12.5% with premature delivery. The authors recommended that depression should be routinely screened for in pregnant women presenting with a medical disorder. Another interesting biological correlate—lower plasma oxytocin and antenatal depression—was demonstrated in a study by Skrundz, Bolten, Nast, Hellhammer, and Meinlschmidt (2011) . According to this study, low plasma oxytocin concentrations before childbirth significantly predicted PPD symptoms at 1 weeks postpartum.
The risk of pregnancy loss has a biological as well as psychological component to it. Although repeated miscarriages may have a medical etiology, the subsequent psychological trauma can lead to MDD in a vulnerable woman. Blackmore et al. (2011) found that the number of previous miscarriages and stillbirths was correlated with depressive symptoms (β = 0.14, s.e. = 0.07, p < .01) and anxiety (β = 0.14, s.e. = 0.05, p < .01) in a subsequent pregnancy ( n = 13,133). Interestingly, the birth of a healthy child did not mitigate the negative impact of a previous perinatal loss in this study.
The role of parity with regard to its impact on PPD is unclear because findings are mixed in terms of the differential effects of primiparity versus multiparity in depressive illness. Some studies have found that primiparous women are at an increased risk for PPD within the first 4 weeks postpartum ( Tamaki, Murata, & Okano, 1997 ; Mori et al., 2011 ). Mori et al. (2011) reported that primiparous postpartum women had an adjusted risk of 2.6 for early-onset depression compared to multiparous women. In contrast, other studies have found that multiparity increases the risk for depression within the first 3 months of childbirth, yet these studies only report findings at the univariate level; thus, other risk factors may have impacted the relation ( Chandran, Tharyan, Muliyil, & Abraham, 2002 ; Milgrom et al., 2008 ).
Research to date demonstrates that there is a complex interaction between hormonal changes, their effect on neurotransmitters, and MDD. Our knowledge in this area is evolving. Studies have suggested that disturbances in the serotonin system and limbic-hypothalamic-pituitary-adrenal axis are the neurobiological basis for mood changes ( Nemeroff, 1998 ; 2002 ). MDD seems to be related to the manner in which the brain responds to stress as corticotropin-releasing hormone (CRH) levels increase ( Farvolden, Kennedy, & Lam, 2003 ). Because CRH regulates the limbic axis, increased stress will impact the entire cycle of emotion regulation. Progesterone, estradiol, CRH, corticotropin, and cortisol levels increase during pregnancy and decrease acutely in the postpartum period, which could potentially trigger depressive symptoms in vulnerable women ( Meltzer-Brody, 2011 ).
Finally, nutritional intake has also been examined as a contributor in increasing vulnerability of perinatal depression. De Vriese, Christophe, and Maes (2003) showed that women who developed PPD had significantly lower levels of omega-3 fatty acids consumption. Beard et al. (2005) conducted a prospective, randomized, controlled intervention trial of new mothers from 10 weeks to 9 months postpartum. Results showed that there is a strong relation between iron levels, depression, stress, and cognitive functioning. Those women who showed iron deficiency and were treated with iron improved by 25% in their depressive symptoms. Serum zinc levels may also play a role in depressive symptoms. In a study that assessed depressive symptoms a month before delivery, as well as 3 and 30 days afterward, low zinc levels were correlated with higher depressive symptoms both at the assessment just before and after childbirth ( Wójcik et al., 2006 ). Vitamin D deficiency has also been associated with exacerbation of depression, especially during times when levels of 25-hydroxyvitamin D are low ( Eskandari et al., 2007 ). Low vitamin D has been shown to correlate with premenstrual mood symptoms in women, and increasing its intake via supplementation or photo intake has been found to improve depressive symptoms in two randomized controlled trials ( Gloth, Alam, & Hillis, 1999 ; Jorde, Sneve, Figenschau, Svartberg, & Waterloo, 2008 ; Thys-Jacobs et al., 1995 ).
Comorbidity
Anxiety disorders.
Although anxiety disorders occur frequently either by themselves or comorbid with depressive illness, they are often underdiagnosed and undertreated. The symptoms of anxiety are often “normalized” and typically confused as being an inherent presentation of a pregnant or postpartum mother. When present, they are disabling and can potentially interfere with the maternal–infant relationship.
Several studies demonstrate a close link between mood and anxiety disorders in perinatal women. Antenatal anxiety has been shown to be a risk factor for PPD ( Skouteris, Wertheim, Rallis, Milgrom, & Paxton, 2009 ). A longitudinal study by Coelho, Murray, Royal-Lawson, and Cooper (2011) showed that antenatal generalized anxiety disorder (GAD) independently predicted PPD at various time points after childbirth. In prospective study by Skouteris et al. (2009) , mid-trimester depression was associated with anxiety in late pregnancy. This, in turn, predicted more intense illness even after controlling for social support and sleep quality.
Comorbid anxiety and depression rates were also reported in a longitudinal study of a large sample of postpartum women ( n = 1,024) who were screened for depression and anxiety ( Reck et al., 2008 ). Results showed that 18.4% of women with an anxiety disorder also had a diagnosis of depressive disorder and that 33.9% of depressed women also had an anxiety disorder in the postpartum. Overall, the authors estimated that 2.1% of women had comorbid anxiety and depression at 3 months postpartum. Anxiety was assessed with the Structured Clinical Interview for DSM-IV ( Wittchen, Wunderlich, Gruschwitz, & Zaudig, 1997 ) for panic disorder, agoraphobia, social phobia, specific phobia, and GAD; the Anxiety Screening Questionnaire ( Wittchen & Boyer, 1998 ) was used to assess current anxiety and GAD. Depression was assessed with the Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001 ) and the EPDS.
Matthey et al. (2003) also found a similar overall depression and anxiety comorbidity rate of 2.1–4.2% at 6 weeks postpartum ( n = 408). These women had a significantly higher EPDS score in pregnancy compared to women who did not experience comorbid disorders. Mothers experienced a threefold risk of a postpartum mood disorder when anxiety was assessed in addition to depression. Anxiety was defined as per the DSM-IV criteria for panic disorder, phobia, and acute adjustment disorder with anxiety.
Wenzel, Haugen, Jackson, and Brendle (2005) assessed depression and anxiety in 147 women at 8 weeks postpartum. Depending on the particular domain of anxiety, 10–50% of women who experienced symptoms of anxiety in the postpartum also had concurrent symptoms of depression. Specifically, in women with a GAD diagnosis, 75% had depressive symptoms, and more than 40% of women with a subsyndromal diagnosis had depressive symptoms as well. In a prospective, longitudinal Swedish study 1,224 women were assessed for mood and anxiety disorders in pregnancy at 12 to 20 weeks, 32 weeks, and 1 month postpartum ( Soderquist, Wijma, Thorbert, & Wijma, 2009 ). This study found a significant positive correlation between posttraumatic stress disorder (PTSD) and depression. Specifically, 58% of women with PTSD also had depression at 1 month postpartum, and 13.72% of women with depression also had PTSD at 1 month postpartum. Measures that were used included the DSM-IV for diagnosis of the PTSD and the Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961 ) for diagnosis of depression. Thus, women diagnosed with anxiety disorders often display accompanying symptoms of depression; conversely, women presenting with perinatal mood disorders can also have accompanying anxiety disorders, as shown in these studies.
Eating Disorders and Childhood Sexual Abuse
Studies have shown that women with lifetime eating disorders have reported more severe perinatal depression than women with no prior eating disorder history ( Meltzer-Brody et al., 2011 ). In addition, women with lifetime eating disorders are more likely to report a history of childhood sexual or physical abuse compared with women without such a history ( Bulik, Sullivan, & Rorty, 1989 ; Rayworth, Wise, & Harlow, 2004 ). Thus, there appears to be an association among symptoms of perinatal depression, eating disorder, and childhood sexual or physical abuse. Clinically, these associated conditions must be recognized in order to institute a multimodal treatment plan. Unfortunately, routine screening for eating disorders in pregnancy and postpartum is not common; therefore, the percentage of women who seek treatment for perinatal depression who have eating disorder histories is unknown ( Andersen & Ryan, 2009 ; Leddy, Jones, Morgan, & Schulkin, 2009 ; Meltzer-Brody et al., 2011 ). Micali, Simonoff, and Treasure (2011) demonstrated that women with current or past histories of an eating disorder reported a sixfold increase in depression and anxiety symptoms at 18 weeks of gestation and 8 months postpartum. In a population-based sample, Mazzeo et al. (2006) reported that 39.1–66.7% of women with a lifetime eating disorder suffered from depression in pregnancy compared to 45.5–70.0% during the postpartum. Occasionally, women report remission of eating disorder symptoms in pregnancy ( Bulik et al., 2007 ). In a relapsed state, however, women engage in dietary restraint and increased purging behavior, leading to poor nutrition ( Bulik et al., 2007 ).
The prevalence of sexual and physical abuse in a study sample by Meltzer-Brody et al. (2011) was as high as 81.3% in those with anorexia nervosa and 75.0% in those with bulimia nervosa. A systematic review by Leeners, Richter-Appelt, Imthurn, and Rath (2006) showed that women with a history of childhood sexual abuse are more likely to present with a variety of long-term outcomes related to pregnancy, delivery, and early parenthood including increased stress, anxiety, and depression. Buist (1998) found, in a sample of depressed postpartum women ( n = 56), that 28.6% had a history of childhood sexual abuse. These women also tended to have a more severe depression compared to women without a history of abuse. In a study by LaCoursiere, Hirst, and Barrett-Connor (2012) , sexual abuse history was identified as one of the important psychosocial risk factors in 11.7% of postpartum women and was associated with an increased rate of PPD (OR = 2.05).
Substance Abuse
Women with preexisting substance abuse histories frequently do not disclose this information to their clinicians. Often, substance abuse in pregnancy and postpartum is seen as a means to self-medicate in order to relieve mood and anxiety symptoms. Pregnancy-related complications and detrimental effects on the developing fetus were seen in women abusing substances in a study by Bolton, Robinson, and Sareen (2009) . These consequences include spontaneous abortions, stillbirths, fetal growth restrictions, and fetal anomalies ( Muzik, Marcus, Flynn, & Rosenblum, 2010 ). Treating substance abuse is imperative when women present with comorbid mood depression and anxiety symptoms, especially because studies have shown that cigarette smoking, alcohol consumption, and illicit drug use in pregnancy are positively correlated with PPD ( Barnet, Duggan, Wilson, & Joffe, 1995 ; Ross & Dennis, 2009 ).
A retrospective study by McCoy, Beal, Shipman, Payton, and Watson (2006) found a statistically significant correlation between cigarette smoking and the development of PPD based on data obtained from routine 4-week postnatal visits ( n = 209). Specifically, the authors found that those women who smoked had a higher incidence of PPD compared to nonsmokers, with an EPDS score of greater than 13 (indicating possible depression). In this sample of women with marginalized socioeconomic backgrounds, the relative risk of depression with cigarette use was 1.58. In another study, Homish, Cornelis, Richardson, and Day (2004) prospectively identified antenatal factors at each trimester that predicted postpartum comorbid alcohol use and symptoms of depression ( n = 595). Results indicated that women were significantly more likely to be engaging in substance use and experiencing depression symptoms 8 months after childbirth if there was a presence of binge drinking, depressive symptoms, or tobacco use at any time in pregnancy.
There are varied opinions on who should be screened for depression in the perinatal period and at what time (prenatal vs. postpartum). Options are to implement universal screening for all women, to screen only those with known risk factors and/or presenting symptoms, or to conduct a diagnostic assessment if symptoms of depression are present instead of screening for symptoms. The American College of Obstetricians and Gynecologists (ACOG) published a committee opinion in which it stated that there is insufficient evidence to support a firm recommendation for universal perinatal screening, while at the same time acknowledging that screening and treating depression has the potential to benefit a woman and her family ( ACOG, 2010 ). A systematic review by Thombs et al. (2014) presented a similar viewpoint. However, others have cautioned that screening should not be dismissed so easily and that “when making recommendations about screening, investigators must consider the breadth of research and the suffering that exists with undiagnosed and untreated perinatal depression” ( Chaudron & Wisner, 2014 ). The Marcé International Society published a position statement on universal perinatal depression screening and concluded that universal psychosocial assessment acknowledges the critical role of psychosocial well-being in maternal and infant outcomes and that when undertaken within an integrated care model it can serve as a point of education for both women and their families ( Austin, 2014 ). At the Reproductive Mental Health Program located at British Columbia Children’s and Women’s Hospital in Vancouver, B.C., Canada, screening is recommended at 28 weeks of gestation and at 6–8 weeks postpartum. These recommendations have been written up in a clinical guideline manual called Best Practice Guidelines for Mental Health Disorders in the Perinatal Period ( BC Reproductive Mental Health Program & Perinatal Services BC, 2014 ). There is no doubt that perinatal depression screening remains a controversial topic.
Properly identifying women with a mental illness during the perinatal period is one way of facilitating treatment of mental illness in the obstetrical outpatient population ( Kim et al., 2009 ; Miller, Shade, & Vasireddy, 2009 ; Muzik et al., 2010 ). In one study, the rate of detection and treatment of women presenting with mood disturbances at obstetric clinics was assessed ( Smith et al., 2004 ). Results indicated that only 26% of women who screened positive for a mood or anxiety disorder were properly identified as suffering with a mental illness by their health care provider (with the exception of a high accuracy rate in identifying symptoms of panic disorder due to their somatic presentation). Without proper identification, treatment cannot be initiated in a timely manner.
One screening tool that is routinely used in the detection of possible depressive symptoms in the perinatal period is the Edinburgh Postnatal Depressive Scale ( Cox et al., 1987 ). The EPDS is a brief 10-item self-rated measure of depression commonly utilized in the postpartum period. This screening tool is relatively easy to administer and has become the gold standard for assessing perinatal depression ( Murray & Cox, 1990 ). A score above 12 (out of 30) indicates that a repeat screening is recommend two weeks later as the score can be a sign of possible or likely depression of varying severity ( Jolley & Betrus, 2007 ). It has been translated into more than 20 languages, although not all translated versions have been validated (Eberhard-Gran, Eskild, Tambs, Opjordsmoen, & Samuelsen, 2001). The effectiveness of the EPDS was tested in a study in which the scale was compared to the PHQ-9 and the Postpartum Depression Screening Scale (PDSS; Beck & Gable, 2000 ; Hanusa, Scholle, Haskett, Spadaro, & Wisner, 2008 ). Results showed that both the EPDS and PDSS were more accurate in screening for depressive symptoms in the perinatal population than the PHQ-9. The EPDS can be an invaluable tool both in pregnancy and the postpartum period as it promotes the initiation of treatment in a timely manner, especially in rural areas. Choosing the right screening tool is challenging because symptoms of depression and signs of pregnancy overlap ( Muzik et al., 2010 ). Some health care professionals may also feel more comfortable than others in screening for mood and anxiety symptoms in perinatal women, based on their amount of training in this area ( Olson, Dietrich, Prazar, & Hurley, 2006 ).
The treatment of depression in pregnancy and postpartum involves pharmacotherapy, psychotherapy, and adjunctive therapies to achieve successful outcomes. In clinical practice, psychotherapy is the first line of treatment for mild to moderate depressive illness, whereas antidepressants are usually considered for the management of severe depression and in those in whom other modalities of treatments have failed ( Yonkers et al., 2009 ). Decisions are made on a case-by-case basis, weighing the risks and benefits of the treatment versus exposure to the disease itself.
At present, there is an ongoing debate regarding the institution of pharmacotherapy in the perinatal period. The current literature is fraught with controversies, methodologically limited research, and unaccountability for confounding factors with regard to perinatal pharmacotherapy. Although no causal relation has been demonstrated with adverse neonatal health with medication use thus far, women are still concerned about its safety in pregnancy and lactation.
Antenatal Pharmacotherapy
Most pregnant women are resistant to taking medications despite illness severity, and clinicians are also not always comfortable in prescribing them. Exposure to medications in perinatal women raises doubts and concerns that include (a) effects of medication on pregnancy, (b) birth defects related to first-trimester use, (c) side effects encountered in the newborn, and (d) potential long-term neurobehavioral impact on the children.
The choice of an antidepressant depends on the efficacy and tolerability of the particular medication and response to previous trials. At times, successful treatment of a family member with a specific medicine can be a guide. If the patient has had no prior exposure to antidepressant medication, the principles of the Canadian Network for Mood and Anxiety Treatments (CANMAT) should be considered ( Lam et al., 2009 ). These evidence-based guidelines make recommendations for treatment in the general population, with a subsection referring to the perinatal population. For the general population, the CANMAT guidelines recommend the following antidepressants as the first-line treatment: escitalopram, citalopram, fluoxetine, and sertraline (selective serotonin reuptake inhibitors [SSRIs]); venlafaxine (serotonin norepinephrine reuptake inhibitor [SNRI]); and bupropion (noradrenaline reuptake inhibitor). In the perinatal population, a similar choice of antidepressants is frequently recommended. According to the and the ACOG, approximately 13% of women took an antidepressant at some point in pregnancy in 2003, a rate that has doubled since 1999 ( Cooper, Willy, Pont, & Ray, 2007 ; Oberlander, Warburton, Misri, Aghajanian, & Hertzman, 2006 ). However, it is important to note that all psychotropic medication use in pregnancy and postpartum has an “off-label indication,” which means that these medications are not indicated for use in this population. We recommend that clinicians have up-to-date information to assist with decisions surrounding medication use in pregnant and breastfeeding women when they are dealing with moderate to severe depressive illness.
Pregnancy Outcomes and Antidepressants
Preterm birth and low birthweight has been the subject of mixed reviews in the literature. Of 12 prospective cohort studies reviewed by Udechuku, Nguyen, Hill, and Szego (2010) , nine demonstrated a statistically significant increase in preterm birth rates with antidepressant use. Two of these studies showed a correlation between late exposure and increased preterm delivery rates. Five out of six retrospective cohort studies reviewed also demonstrated positive findings. It is important to note that many of these studies did not account for other drug exposure or control for confounders such as smoking ( Udechuku et al., 2010 ). Oberlander et al. (2006) examined prescription records matched with hospital separation records and found that SSRI-exposed babies had a higher rate of preterm birth than did babies exposed to depression alone. No specific studies focused on the impact of antidepressants on spontaneous abortions themselves; however, two meta-analyses showed spontaneous abortion to be a secondary outcome ( Hemels, Einarson, Koren, Lanctot, & Einarson, 2005 ; Rahimi, Nikfar, & Abdollahi, 2006 ). There have been no studies that have specifically examined the risks of stillbirths upon antidepressant exposure. None of the large birth registry studies has shown any increased incidence of stillbirth in exposed infants ( Udechuku et al., 2010 ).
Birth Defects and Antidepressants
With regard to the correlation between birth outcomes and antidepressant use, research shows mixed results. Some studies show a negative correlation, such that negative birth outcomes were associated with antidepressant use, whereas others found no correlation and viewed them as safe to take during pregnancy. Udechuku et al. (2010) systematically reviewed 35 studies, many cohort (prospective and retrospective) and case–control studies, to investigate the association between antidepressant use and congenital malformations. They found a significant association between antidepressant use and congenital malformations in 12 out of 35 studies. Other studies were also found to have an association between paroxetine, fluoxetine, and cardiac defects ( Chambers, Johnson, Dick, Felix, & Jones, 1996 ; Murray & Cooper, 1997 ). It is important to note that these studies had a wide range of 95% confidence intervals, indicating less precision or confidence around the estimated associations and greater variability among the studies. In contrast, a birth registry by Källén and Otterblad Olausson (2003) demonstrated no increased risk associated with SSRIs, including paroxetine, in relation to cardiac malformations, as did a study by Cole, Ephross, Cosmatos, and Walker (2007) . At present, paroxetine is listed in Category D (contraindicated in pregnancy; Alwan, Reefhuis, Rasmussen, Olney, & Friedman, 2007 ). Alwan et al. (2007) recorded rare infant outcomes in a small sample exposed to paroxetine or citalopram, which included anencephaly (214 infants, 9 exposed), craniosynostosis (432 infants, 24 exposed), and omphalocele (181 infants, 11 exposed). However, it is important to note that the authors warned against viewing their findings as strong evidence given the small number of exposed infants with rare outcomes. Finally, persistent pulmonary hypertension (PPHN) was recently reported (with minimal absolute risk) with antenatal SSRI use based on a limited retrospective dataset ( Chambers et al., 2006 ), yet many factors associated with depression itself may account for the association ( Occhiogrosso, Salehi Omran, & Altemus, 2012 ). The U.S. Food and Drug Administration released a revised statement in 2011 acknowledging the conflicting findings of studies that have evaluated the risk of SSRI use during pregnancy and the potential risk of PPHN and stated that it is premature to reach any conclusion about a possible link ( U.S. Food and Drug Administration, 2012 ). In a study by Grigoriadis et al. (2014) , the statistical association between infants exposed to SSRIs in late pregnancy and an increased risk of PPHN was significant, but “clinically the absolute risk of PPHN of the newborn remained low even in the context of late exposure to SSRIs.”
With respect to the concerns about paroxetine and other SSRIs during pregnancy, a recent report by Adrienne Einarson of Motherisk concluded that “accumulated evidence from different types of studies does not suggest that paroxetine is associated with an increased risk of heart defects” ( Einarson, 2010 ). In addition, three meta-analyses found no risk of major or cardiac malformations with first-trimester exposure to paroxetine or other SSRIs ( Einarson & Einarson, 2005 ; O’Brien, Einarson, Sarkar, Einarson, & Koren, 2008 ; Rahimi et al., 2006 ). Another study found no association with first-trimester SSRI use overall and congenital anomalies ( Louik, Lin, Werler, Hernández-Díaz, & Mitchell, 2007 ). Thus, when antidepressants are indicated in a pregnant woman, a consensual discussion between the clinician and the patient is recommended to facilitate an informed decision by the patient to engage in pharmacotherapy.
Adverse Neonatal Outcomes
Poor neonatal adaptation syndrome with antenatal antidepressant exposure has been rated to be 13.9% ( Oberlander et al., 2006 ). This is a transient phenomenon commonly characterized by tremors, abnormal tone, slow respiration, and other nonspecific symptoms. Very few infants need clinical intervention. Most studies conducted thus far with regard to side effects in the newborn involve maternal exposure to SSRIs and venlafaxine, which is a SNRI.
Long-Term Neurobehavioral Teratogenicity
The majority of the studies that have examined long-term developmental outcomes of children exposed to antidepressant medication report no differences between children who were and were not exposed to SSRIs in utero ( Casper et al., 2003 ; Udechuku et al., 2010 ). Two prospective cohort studies by Oberlander et al. (2007) and Misri and Kendrick (2007) illustrated that the best predictor of externalizing and internalizing behaviors at age 4 was maternal mood, not SSRI treatment during pregnancy.
Recent literature surrounding the use of tricyclic antidepressants (TCAs) in pregnancy is sparse because TCAs are prescribed less frequently than newer antidepressants, such as SSRIs, in the treatment of depression. The few older studies are retrospective, with some case reports ( Cole et al., 2007 ; Källén & Otterblad Olausson, 2007 ). At present, TCAs are generally avoided because of their unfavorable side effects of orthostatic hypotension, conduction defects of the heart, sedation, and weight gain ( Wisner, Parry, & Piontek, 2002 ). The majority of studies have not found any significant association between prenatal TCA use and structural malformations, but in utero exposure to TCAs has been linked to perinatal complications that include jitteriness, irritability, and (rarely) seizures in newborns ( Altshuler et al., 1996 ; Källén, 2004 ; Simon, Cunningham, & Davis, 2002 ). In one prospective study, no significant link was found between TCAs in pregnancy and differences in behavior, cognition, and temperament in children ( Nulman et al., 2002 ). This study utilized mother–child dyads (46 were exposed to TCAs prenatally; 40 exposed to fluoxetine; 36 controls not exposed to any teratogenic medication). TCAs in this study included amitriptyline, imipramine, clomipramine, desipramine, nortriptyline, doxepin, and maprotiline. Clomipramine was, however, associated with an increased likelihood of any cardiovascular defect (odds ratio = 1.77; Källén & Otterblad Olausson, 2007 ).
Given the conflicting knowledge surrounding antidepressant use in pregnancy, clinicians are faced with the difficult task of treating moderate to severely depressed women who are in need of such treatment. Clinically, this treatment option remains one of the most controversial issues at present.
Pharmacotherapy in the Postpartum
A large percentage of women continue to nurse newborns while on antidepressant medications. In the extant literature, sertraline and paroxetine seem to be described as the safest pharmacotherapeutic agents and are used with little risk. This is due to their weakly active metabolite generally not detectable in infant plasma. No statistically significant adverse events have been reported with their use ( Wisner et al., 2002 ). On the contrary, fluoxetine and citalopram have been shown to have a slightly higher secretion through breast milk, with rates of 2–7% for fluoxetine and 3.5–8% for citalopram, relative to 0.5–1% for sertraline and 1.4% for paroxetine ( Berle et al., 2004 ; Fitelson, Kim, Baker, & Leight, 2011 ; Franssen et al., 2006 ; Heikkinen, Ekblad, Kero, Ekblad, & Laine, 2002 ; Kim et al., 2006 ; Kristensen et al., 1999 ; Lanza di Scalea & Wisner, 2009 ; Oberlander et al., 2005 ; Stowe et al., 2003 ; Weissman et al., 2004 ). Unlike most antidepressants, fluoxetine has a highly active metabolite (norfluoxetine), and both agents have very long half-lives (84 and 146 hours, respectively; Wisner, Perel, & Findling, 1996 ). With regard to the TCAs, most studies have focused on nortriptyline because it has the most data on safety during breastfeeding ( Fortinguerra, Clavenna, & Bonati, 2009 ). It is classified as one of the safer drugs in breastfeeding women based on a limited number of women without an increase in adverse effects in the infant ( Hale, 2012 ).
The most commonly used psychotherapeutic modalities are interpersonal psychotherapy (IPT) and cognitive behavioral therapy (CBT). In mild to moderate PPD, both individual and group therapy have been shown to be an effective form of treatment. For moderate to severe PPD, a combination of psychotherapy and pharmacotherapy is recommended ( Hirst & Moutier, 2010 ).
Interpersonal Psychotherapy
IPT, a time-limited and problem-focused therapy, works well with the demands of a postpartum mother ( Fitelson et al., 2011 ). Specific areas of conflict such as the mother–infant relationship, mother–partner bond, and transitioning back to work can be addressed with IPT ( Stuart & O’Hara, 1995 ). In a randomized controlled trial, 120 women with PPD received either 12 weekly sessions of IPT by a trained therapist or were assigned to a waitlist control condition ( O’Hara, Stuart, Gorman, & Wenzel, 2000 ). A significant decrease in depressive symptoms and improvement in social functioning was seen in the group of women who received IPT, relative to those in the waitlist condition, as measured by the HAM-D, BDI, Postpartum Adjustment Questionnaire ( O’Hara, Hoffman, Phillips, & Wright, 1992 ), and Social Adjustment Scale–Self-Report ( Weissman & Bothwell, 1976 ). In a recent meta-analysis, systemically oriented psychotherapies, including individual IPT and various relational interventions, produced similar therapy outcomes to medication and cognitive behavioral therapies ( Claridge, 2014 ).
Research has also shown that group IPT is advantageous over individual IPT as it offers increased social support, normalization of problems, development of interpersonal skills in a group setting that can be translated to outside relationships, and minimization of stigma associated with PPD ( Reay et al., 2006 ). In a randomized controlled trial by Reay et al. (2012) , the long-term (i.e., 2 years posttreatment) efficacy of group IPT in a group of postpartum depressed women ( n = 44) was examined. Women who had received group IPT improved significantly faster in the short term and had a lower likelihood of experiencing persistent depressive symptoms in the long term. Remission was maintained over the course of the 2-year follow-up period by 57% of women who received IPT. Similar findings were found in another randomized controlled trial of mothers with PPD ( n = 50) who were divided into either a treatment group of 8 weeks of group IPT or a treatment-as-usual group ( Mulcahy, Reay, Wilkinson, & Owen, 2010 ). Mothers in group IPT had significantly greater symptom relief, as measured by the HAM-D, and were much more likely to have continued improvements at 3 months after therapy compared to the treatment-as-usual group. They also showed significant improvements in terms of marital functioning and positive perceptions of the mother–infant relationship. An Austrian study also supported these findings; women with PPD ( n = 17) reported significant improvements in their depressive symptoms after 12 weeks of group-based IPT, with the majority reaching full remission (59%) or partial remission (29%; Klier, Muzik, Rosenblum, & Lenz, 2001 ).
Cognitive Behavioral Therapy
CBT aims to help depressed patients to modify distorted patterns of negative thinking and make behavioral changes that enhance coping and reduce distress ( Hollon, 1998 ). CBT can be utilized alone or in combination with medications to achieve maximum results. For example, Misri, Reebye, Corral, and Milis (2004) randomized 35 women with PPD and comorbid anxiety either to paroxetine monotherapy or paroxetine combined with 12 weekly manualized CBT sessions. Results indicated that the combination therapy did not offer any additional advantage in treatment of MDD in the postpartum period. In other words, the addition of CBT did not yield any significant difference in the average dose of paroxetine required to achieve remission, nor did it shorten the length of treatment for the combination therapy group. However, both treatments resulted in statistically significant improvements in maternal mood and anxiety symptoms between the baseline and final visits. Milgrom, Negri, Gemmill, McNeil, and Martin (2005) randomized 192 postpartum depressed women to CBT, counseling, or routine primary care for 12 weeks. Mood was assessed with the BDI and Beck Anxiety Index (BAI; Beck, Epstein, Brown, & Steer, 1988 ) for outcome measures. The authors did not find significant differences in outcomes in women who were randomized to CBT or counseling groups, but found both to be helpful in decreasing symptoms of depression. Similar results were found by Cooper, Murray, Wilson, and Romaniuk (2003) in that women with PPD who received CBT did not significantly differ from those receiving nondirective counseling or psychodynamic therapy when compared with the control group (receiving routine primary care). On the other hand, Honey, Bennett, and Morgan (2002) found that women with PPD who received a brief, group-based psychoeducation intervention (which included cognitive behavioral techniques) fared significantly better than those in routine care.
Nondirective Counseling
Nondirective counseling is also referred to as “person-centered” counseling and is based on the use of empathic and nonjudgmental listening and support ( Fitelson et al., 2011 ). Recent literature examining the efficacy of this form of therapy is sparse; however, past studies have shown high rates of improvement in recovery for postpartum women. For example, one study by Wickberg and Hwang (1996) randomized 31 women with PPD to receive six nondirective counseling sessions or routine primary care. Eighty percent of women in the treatment group remitted from depression versus 25% of women who received routine primary care.
Peer and Partner Support
Interventions aimed at increasing social support are an important part of treatment for perinatal depression because a lack of social support has been identified throughout the literature as a risk factor ( Beck, 2001 ; Horwitz, Briggs-Gowan, Storfer-Isser, & Carter, 2007 ; Xie, He, Koszycki, Walker, & Wen, 2009 ). Misri et al. (2000) examined the impact of partner support in the treatment of PPD. Participants were randomly assigned to either a patient-only group (control) or a group consisting of patients and their partners (support group). Each group participated in seven psychoeducational visits with partners participating in four of the seven visits. Patients in both groups were administered a set of questionnaires, including the EPDS, Kellner Symptom Questionnaire ( Kellner, 1987 ), the DAS, and the Parental Bonding Instrument ( Parker, Tupling, & Brown, 1979 ). Furthermore, during visits 1 and 7, all patients underwent assessment using the Mini International Neuropsychiatric Instrument ( Sheehan et al., 1998 ). The partners of women in both groups completed the DAS and the General Health Questionnaire (GHQ; Goldberg & Hillier, 1979 ). By visit 6, there was a statistically significant difference in depressive symptomatology and DAS scores in the support group relative to the control group. The health of the control group partners was also significantly poorer than that of the support group partners, as indicated by the higher scores of control group partners on the GHQ. This study conveyed the importance and significance of partner support and the impact it has on women experiencing PPD. The results also indicate that women experience a more rapid recovery when the partner is supportive.
Alternative Therapies
Alternative therapies are widely used and may be of benefit to women with perinatal depression, particularly for those who are concerned about engaging in pharmacotherapy. Several complementary and alternative therapies have been reviewed for their effectiveness for perinatal depression, and some are discussed here ( Freeman, 2009 ; Weier & Beal, 2004 ).
Acupuncture has been investigated as an adjunctive form of treatment in pregnancy for symptoms of nausea, pain, and breech presentation, as well as for induction of labor ( Smith & Cochrane, 2009 ). One pilot study ( n = 150) compared the use of targeted acupuncture for symptoms of depression versus controls of a nontargeted acupuncture (i.e., acupuncture that did not target depression) and massage for 8 weeks ( Manber et al., 2010 ). Results indicated that active acupuncture significantly outperformed a massage intervention in terms of reduction on a depression symptom rating scale (i.e., HAM-D) in depressed pregnant women. In a randomized controlled trial, women with PPD ( n = 61) were randomized to one of three treatment groups for 8 weeks (active acupuncture, active control acupuncture, massage; Manber, Schnyer, Allen, Rush, & Blasey, 2004 ). In the active control acupuncture group, women still received acupuncture but not in a way in which depression symptoms were specifically addressed. Acupuncture was delivered in a double-blind fashion. Results indicated that women in the active acupuncture group had a significantly higher rate of decreased BDI scores compared to the other two control groups ( Manber et al., 2004 ).
Several studies have shown massage to be an effective treatment for perinatal depression. Specifically, techniques of therapeutic, partner-delivered, and infant massage in the postpartum period have been utilized ( Field, Diego, Hernandez-Reif, Deeds, & Figueiredo, 2009 ; Field, Grizzle, Scafidi, & Schanberg, 1996 ). A study by Field et al. (1996) found a significant improvement in depression ratings in a massage group versus a relaxation technique group in which 10 sessions were utilized for each. There was no long-term follow-up of this study. A more recent study investigated maternal massage therapy administered by the women’s partner for 12 weeks in depressed pregnant women. Results from this study demonstrated benefits in the massage group in depression during late pregnancy and immediately postpartum ( Field et al., 2009 ). Again, there was no long-term follow-up in this study. Several studies have also found infant massage to promote maternal–infant bonding, particularly for women experiencing moderate levels of perinatal depression ( O’Higgins, St. James Roberts, & Glover, 2008 ; Onozawa, Glover, Adams, Medi & Kumar, 2001 ; Underdown, Norwood, & Barlow, 2013 ).
Omega-3 fatty acids have been shown to have great health benefits for pregnant and postpartum women. However, studies examining the use of this supplement have had mixed results. One pilot study assessing omega-3 fatty acids as an intervention for perinatal depression during pregnancy showed a 40.9% mean decrease in depressive symptoms on the EPDS, whereas a second randomized dose-ranging study found no significant difference between control and study groups. Importantly, both studies had small sample sizes and no placebo group ( Freeman, Hibbeln, Wisner, Watchman, & Gelenberg, 2006 ).
Exercise is important in ensuring physical health and well-being, but it also has beneficial effects on mood. The UK National Institute for Health and Clinical Excellence (NICE) has recommended exercise to be beneficial in women experiencing mild to moderate depression ( Daley, Macarthur, & Winter, 2007 ). For pregnant women, the ACOG recommends 30 minutes of exercise per day ( Artal & O’Toole, 2003 ). One specific form of exercise that has shown promise both for depression and in pregnant women is yoga ( Rakhshani, Maharana, Raghuram, Nagendra, & Venkatram, 2010 ; Uebelacker et al., 2010 ). In fact, yoga has been suggested as a second-line adjunctive treatment for mild to moderate MDD by the CANMAT guidelines ( Ravindran et al., 2009 ).
In summary, mild mood and anxiety disorders in pregnancy and postpartum often respond to nonpharmacological treatments. Patients often choose to engage in CBT or IPT for the treatment of their symptoms. Pharmacotherapy is warranted when these treatments do not produce an adequate response or if the disease worsens. Ideally, a combination of pharmacotherapy and psychotherapy produces the best result. Any adjunctive therapy, such as exercise, yoga, acupuncture, massage, and others, can provide additional relief to perinatal women who are treated by conventional treatment modalities.
Untreated Maternal Depression
Maternal depression during pregnancy can adversely affect the mother, her child, and the family if left untreated. Poor prenatal attendance, lack of nutrition, increased risk of smoking, alcohol/drug abuse, and self-harm are some of the important consequences in an untreated mother ( Bonari et al., 2004 ; Oates, 2003 ; Shadigian & Bauer, 2005 ). Poor maternal–infant attachment, delays in infant growth and development, and an increased risk of anxiety and depressive symptoms in later life are also related to untreated postpartum maternal illness. In one study, 2-month-old infants of postpartum depressed women displayed four times as much negative expression and affect compared to infants of nondepressed mothers ( Cohn, Campbell, Matias, & Hopkins, 1990 ). In another study, children of depressed mothers were 1.61 times more at risk for being stunted in growth compared to children of nondepressed mothers ( Avan, Richter, Ramchandani, Norris, & Stein, 2010 ). Additionally, a 20-year follow-up study has shown that children of depressed mothers had a three times higher risk of mood and anxiety disorders compared to children of nondepressed mothers ( Weissman et al., 2006 ).
Studies of biochemical markers have been an important development in understanding the link between maternal untreated illnesses and the baby. Higher cortisol levels in prenatally depressed women have been shown to be associated with delayed fetal growth, prematurity, and impaired fetal brain development ( Field & Diego, 2008 ; Van den Bergh, Mulder, Mennes, & Glover, 2005 ; Weinstock, 2005 ). In another study by Field et al. (2004) , infants born to depressed mothers were found to have higher cortisol and lower dopamine and serotonin levels, mimicking their mother’s prenatal levels. In addition, these newborns also presented with greater relative right frontal electroencephalography activation and lower vagal activity associated with chronic depression.
Maternal depression has been shown to be related to infant avoidant and disorganized attachment, with negative mother–infant interactions ( Korja et al., 2008 ; Martins & Gaffan, 2000 ). These, in turn, have been linked to externalizing behavior problems during toddlerhood ( Madigan, Moran, Schuengel, Pederson, & Otten, 2007 ). Another study by Trapolini, McMahon, and Ungerer (2007) found that by the preschool years, children who were exposed to chronic depression had higher levels of internalizing and externalizing behaviors as reported by parents and teachers and as measured by the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001 ). The rates of clinically elevated scores were much higher than population-based norms and also higher than expected in this socioeconomically low-risk sample. On the basis of maternal reports, 10% of the exposed children had internalizing scores (i.e., self-directed and quiet behaviors where feelings are kept inside, such as sadness and guilt, which may result in withdrawal, unexplained physical symptoms, and depression) that were in the clinical range, and 7% of children had externalizing scores (i.e., disruptive, overt, attention-seeking behaviors such as irritability, anger, and aggression) in the clinical range. Rates of internalizing behaviors were five times higher than those in the general population, and rates of externalizing behaviors were three times higher.
More research is needed to examine the association between maternal depression and adverse child outcomes as a function of gender. Some studies show that boys are more adversely affected by prenatal and postpartum maternal depression than are girls, whereas others do not detect gender differences ( Bagner, Pettit, Lewinsohn, & Seeley, 2010 ; Carter, Garrity-Rokous, Chazan-Cohen, Little, & Briggs-Gowan, 2001 ). Some have concluded that maternal MDD during the first year of life is associated with maternal report of child internalizing behavior problems regardless of gender.
Conclusion and Future Directions
The current definition of PPD does not reflect the clinical picture in its entirety. Consequently, health care providers are unable to identify psychiatric illnesses adequately during this sensitive, vulnerable, and critical period in the mother’s life. Delay in diagnosis and treatment is the rule rather than the exception. Because the management of this illness is not standardized, women frequently encounter obstacles to finding appropriate health care providers, further complicating their recovery. Recognizing the serious impact of an untreated mother on the fetus, the newborn, the toddler, and the adolescent is gaining momentum and raising the awareness of timely intervention of this disease. Much needs to change in the future in regards to destigmatizing maternal mental illness by instituting early screening and engaging in a consensual treatment plan.
With regard to future research, designing studies that are methodologically sound could potentially lead to important findings. Recruitment of a prospective perinatal sample is preferred to examining retrospective data. Moreover, every effort should be made to investigate a reasonably large trial to understand and evaluate the effects of research. In addition, duplication of population-based studies in different cultural contexts would help in determining the prevalence of this disease more clearly. Head-to-head comparison of different modalities of treatment, such as comparing psychotherapy versus pharmacotherapy, should be undertaken in a prospective manner in order to institute appropriate treatment and reduce a high rate of attrition. Additionally, advances can be made in researching teratogenicity associated with pharmacotherapy, given the current controversy that exists with antidepressant medication use in pregnancy and lactation. Studies with a strong educational component could potentially reduce the biases held by committees that have the power to influence research decisions in the perinatal population. Active campaigning needs to be undertaken to reduce the sense of shame and embarrassment that prevents mothers from admitting their illness and accessing help when needed. They tend to suffer in silence—a reality hidden in plain sight.
Achenbach, T. M. , & Rescorla, L. A. ( 2001 ). Manual for the ASEBA school-age forms & profiles: An integrated system of multi-informant assessment. Burlington, VT: University of Vermont Research Center for Children, Youth, & Families.
Google Scholar
Google Preview
Altshuler, L. L. , Cohen, L. , Szuba, M. P. , Burt, V. K. , Gitlin, M. , & Mintz, J. ( 1996 ). Pharmacologic management of psychiatric illness during pregnancy: Dilemmas and guidelines. American Journal of Psychiatry, 153(5), 592–606.
Altshuler, L. L. , Hendrick, V. , & Cohen, L. S. ( 1998 ). Course of mood and anxiety disorders during pregnancy and the postpartum period. Journal of Clinical Psychiatry, 59(Suppl 2), 29–33.
Alwan, S. , Reefhuis, J. , Rasmussen, S. A. , Olney, R. S. , & Friedman, J. M. ( 2007 ). Use of selective serotonin-reuptake inhibitors in pregnancy and the risk of birth defects. New England Journal of Medicine, 356(26), 2684–2692.
American College of Obstetricians and Gynecologists, Committee on Health Care for Underserved Women. ( 2006 ). Committee opinion no. 343: Psychosocial risk factors: Perinatal screening and intervention. Obstetrics and Gynecology, 108(2), 469–477.
American College of Obstetricians and Gynecologists, & Committee on Obstetric Practice. ( 2010 ). Committee opinion no. 453: Screening for depression during and after pregnancy. Obstetrics and Gynecology , 115 (2 Pt 1), 394.
American Psychiatric Association. ( 2013 ). Diagnostic and statistical manual for mental disorders (5th ed.). Washington, DC: Author.
Ancill, R. , Hilton, S. , Carr, T. , Tooley, M. , & McKenzie, A. ( 1986 ). Screening for antenatal and postnatal depressive symptoms in general practice using a microcomputer-delivered questionnaire. Journal of the Royal College of General Practitioners, 36(287), 276–279.
Andersen, A. E. , & Ryan, G. L. ( 2009 ). Eating disorders in the obstetric and gynecologic patient population. Obstetrics and Gynecology, 114(6), 1353–1367.
Artal, R. , & O’Toole, M. ( 2003 ). Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period. British Journal of Sports Medicine, 37(1), 6–12.
Austin, M. P. ( 2014 ). Marcé International Society position statement on psychosocial assessment and depression screening in perinatal women. Best Practice & Research Clinical Obstetrics & Gynaecology , 28 (1), 179-187.
Avan, B. , Richter, L. M. , Ramchandani, P. G. , Norris, S. A. , & Stein, A. ( 2010 ). Maternal postnatal depression and children’s growth and behaviour during the early years of life: Exploring the interaction between physical and mental health. Archives of Disease in Childhood, 95(9), 690–695.
Bagner, D. M. , Pettit, J. W. , Lewinsohn, P. M. , & Seeley, J. R. ( 2010 ). Effect of maternal depression on child behavior: A sensitive period? Journal of the American Academy of Child and Adolescent Psychiatry, 49(7), 699–707.
Banti, S. , Mauri, M. , Oppo, A. , Borri, C. , Rambelli, C. , Ramacciotti, D. , … Cassano, G. B. ( 2011 ). From the third month of pregnancy to 1 year postpartum. Prevalence, incidence, recurrence, and new onset of depression. Results from the perinatal depression–research & screening unit study. Comprehensive Psychiatry, 52(4), 343–351.
Barnet, B. , Duggan, A. K. , Wilson, M. D. , & Joffe, A. ( 1995 ). Association between postpartum substance use and depressive symptoms, stress, and social support in adolescent mothers. Pediatrics, 96(4 Pt 1), 659–666.
BC Reproductive Mental Health Program & Perinatal Services BC. ( 2014 ). Best practice guidelines for mental health disorders in the perinatal period. Author.
Beard, J. L. , Hendricks, M. K. , Perez, E. M. , Murray-Kolb, L. E. , Berg, A. , Vernon-Feagans, L. , … Tomlinson, M. ( 2005 ). Maternal iron deficiency anemia affects postpartum emotions and cognition. Journal of Nutrition, 135(2), 267–272.
Beck, A. T. , Epstein, N. , Brown, G. , & Steer, R. A. ( 1988 ). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897.
Beck, A. T. , Ward, C. H. , Mendelson, M. , Mock, J. , & Erbaugh, J. ( 1961 ). An inventory for measuring depression. Archives of General Psychiatry, 4(6), 561–571.
Beck, C. T. ( 2001 ). Predictors of postpartum depression: An update. Nursing Research, 50(5), 275–285.
Beck, C. T. , & Gable, R. K. ( 2000 ). Postpartum depression screening scale: Development and psychometric testing. Nursing Research, 49(5), 272–282.
Bennett, H. A. , Einarson, A. , Taddio, A. , Koren, G. , & Einarson, T. R. ( 2004 ). Prevalence of depression during pregnancy: Systematic review. Obstetrics and Gynecology, 103(4), 698–709.
Benute, G. R. G. , Nomura, R. M. Y. , Reis, J. S. , Fraguas, Junior R. , Lucia, M. C. S. , & Zugaib, M. ( 2010 ). Depression during pregnancy in women with a medical disorder: Risk factors and perinatal outcomes. Clinics (Sao Paulo), 65(11), 1127–1131.
Berardi, D. , Leggieri, G. , Ceroni, G. B. , Rucci, P. , Pezzoli, A. , Paltrinieri, E. , … Ferrari, G. ( 2002 ). Depression in primary care: A nationwide epidemiological survey. Family Practice, 19(4), 397–400.
Berle, J. Ø ., Steen, V. M. , Aamo, T. O. , Breilid, H. , Zahlsen, K. , & Spigset, O. ( 2004 ). Breastfeeding during maternal antidepressant treatment with serotonin reuptake inhibitors: Infant exposure, clinical symptoms, and cytochrome p450 genotypes. Journal of Clinical Psychiatry, 65(9), 1228–1234.
Biggs, W. S. , & Demuth, R. H. ( 2011 ). Premenstrual syndrome and premenstrual dysphoric disorder. American Family Physician, 84(8), 918–924.
Black, D. W. , Bell, S. , Hulbert, J. , & Nasrallah, A. ( 1988 ). The importance of Axis II in patients with major depression. A controlled study. Journal of Affective Disorders, 14(2), 115–122.
Blackmore, E. R. , Côté-Arsenault, D. , Tang, W. , Glover, V. , Evans, J. , Golding, J. , & O’Connor, T. G. ( 2011 ). Previous prenatal loss as a predictor of perinatal depression and anxiety. British Journal of Psychiatry, 198(5), 373–378.
Blehar, M. C. ( 2001 ). The NIMH women’s mental health program: Establishing the public health context for women’s mental health. Trends in Evidence-Based Neuropsychiatry, 3 , 42–43.
Bloch, M. , Rotenberg, N. , Koren, D. , & Klein, E. ( 2005 ). Risk factors associated with the development of postpartum mood disorders. Journal of Affective Disorders, 88(1), 3–8.
Bolton, J. M. , Robinson, J. , & Sareen, J. ( 2009 ). Self-medication of mood disorders with alcohol and drugs in the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Affective Disorders, 115(3), 367–375.
Bonari, L. , Pinto, N. , Ahn, E. , Einarson, A. , Steiner, M. , & Koren, G. ( 2004 ). Perinatal risks of untreated depression during pregnancy. Canadian Journal of Psychiatry, 49(11), 726–735.
Bowen, A. , & Muhajarine, N. ( 2006 ). Antenatal depression. Canadian Nurse, 102(9), 26–30.
Boyce, P. , Harris, M. , Silove, D. , Morgan, A. , Wilhelm, K. , & Hadzi-Pavlovic, D. ( 1998 ). Psychosocial factors associated with depression: A study of socially disadvantaged women with young children. Journal of Nervous and Mental Disease, 186(1), 3–11.
Boyce, P. , Parker, G. , Barnett, B. , Cooney, M. , & Smith, F. ( 1991 ). Personality as a vulnerability factor to depression. British Journal of Psychiatry, 159(1), 106–114.
Brugha, T. S. , Sharp, H. M. , Cooper, S. A. , Weisender, C. , Britto, D. , Shinkwan, R. , … Kirwan, P. H. ( 1998 ). The Leicester 500 Project. Social support systems and the development of postnatal depressive symptoms, a prospective cohort survey. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences, 28(1), 63–79.
Buist, A. ( 1998 ). Childhood abuse, parenting and postpartum depression. Australian and New Zealand Journal of Psychiatry , 32 (4), 479-487.
Bulik, C. M. , Sullivan, P. E. , & Rorty, M. ( 1989 ). Childhood sexual abuse in women with bulimia nervosa. Journal of Clinical Psychiatry, 50(12), 460–464.
Bulik, C. M. , Von Holle, A. , Hamer, R. , Knoph Berg, C. , Torgersen, L. , Per Magnus, M. D. , … Reichborn-Kjennerud, M. D. ( 2007 ). Patterns of remission, continuation, and incidence of broadly-defined eating disorders during early pregnancy in the Norwegian Mother and Child Cohort Study (MoBa). Psychological Medicine, 37(8), 1109–1118.
Carter, A. S. , Garrity-Rokous, F. E. , Chazan-Cohen, R. , Little, C. , & Briggs-Gowan, M. J. ( 2001 ). Maternal depression and comorbidity: Predicting early parenting, attachment security, and toddler social-emotional problems and competencies. Journal of the American Academy of Child and Adolescent Psychiatry, 40(1), 18–26.
Casper, R. C. , Fleisher, B. E. , Lee-Ancajas, J. C. , Gilles, A. , Gaylor, E. , DeBattista, A. , & Hoyme, E. ( 2003 ). Follow-up of children of depressed mothers exposed or not exposed to antidepressant drugs during pregnancy. Journal of Pediatrics, 142(4), 402–408.
Chambers, C. D. , Hernandez-Diaz, S. , Van Marter, L. J. , Werler, M. M. , Louik, C. , Jones, K. L. , & Mitchell, A. A. ( 2006 ). Selective serotonin-reuptake inhibitors and risk of persistent pulmonary hypertension of the newborn. New England Journal of Medicine, 354(6), 579–587.
Chambers, C. D. , Johnson, K. A. , Dick, L. M. , Felix, R. J. , & Jones, K. L. ( 1996 ). Birth outcomes in pregnant women taking fluoxetine. New England Journal of Medicine, 335(14), 1010–1015.
Chandran, M. , Tharyan, P. , Muliyil, J. , & Abraham, S. ( 2002 ). Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India. British Journal of Psychiatry, 181(6), 499–504.
Chaudron, L. H. , & Wisner, K. L. ( 2014 ). Perinatal depression screening: Let’s not throw the baby out with the bath water! Journal of Psychosomatic Research , 76 (6), 489.
Claridge, A. M. ( 2014 ). Efficacy of systemically oriented psychotherapies in the treatment of perinatal depression: a meta-analysis. Archives of Women’s Mental Health , 17 (1), 315.
Coelho, H. F. , Murray, L. , Royal-Lawson, M. , & Cooper, P. J. ( 2011 ). Antenatal anxiety disorder as a predictor of postnatal depression: A longitudinal study. Journal of Affective Disorders, 129(1-3), 348–353.
Cohn, J. F. , Campbell, S. B. , Matias, R. , & Hopkins, J. ( 1990 ). Face-to-face interactions of postpartum depressed and nondepressed mother-infant pairs at 2 months. Developmental Psychology, 26(1), 15–23.
Cole, J. A. , Ephross, S. A. , Cosmatos, I. S. , & Walker, A. M. ( 2007 ). Paroxetine in the first trimester and the prevalence of congenital malformations. Pharmacoepidemiology and Drug Safety, 16(10), 1075–1085.
Cooper, P. J. , Murray, L. , Wilson, A. , & Romaniuk, H. ( 2003 ). Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression: 1. Impact on maternal mood. British Journal of Psychiatry, 182(5), 412–419.
Cooper, W. O. , Willy, M. E. , Pont, S. J. , & Ray, W. A. ( 2007 ). Increasing use of antidepressants in pregnancy. American Journal of Obstetrics and Gynecology, 196(6), 544.e1–5.
Coryell, W. , Solomon, D. , Leon, A. , Fiedorowicz, J. G. , Schettler, P. , Judd, L. , & Keller, M. ( 2009 ). Does major depressive disorder change with age? Psychological Medicine, 39(10), 1689–1695.
Cox, J. L. , Holden, J. M. , & Sagovsky, R. ( 1987 ). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry, 150(6), 782–786.
Daley, A. J. , Macarthur, C. , & Winter, H. ( 2007 ). The role of exercise in treating postpartum depression: A review of the literature. Journal of Midwifery and Women’s Health, 52(1), 56–62.
Dankner, R. , Goldberg, R. P. , Fisch, R. Z. , & Crum, R. M. ( 2000 ). Cultural elements of postpartum depression. A study of 327 Jewish Jerusalem women. Journal of Reproductive Medicine, 45(2), 97–104.
De Vriese, S. R. , Christophe, A. B. , & Maes, M. ( 2003 ). Lowered serum n-3 polyunsaturated fatty acid (PUFA) levels predict the occurrence of postpartum depression: Further evidence that lowered n-PUFAs are related to major depression. Life Sciences, 73(25), 3181–3187.
Eaton, W. W. , Anthony, J. C. , Gallo, J. , Cai, G. , Tien, A. , Romanoski, A. , … Chen, L. S. ( 1997 ). Natural history of Diagnostic Interview Schedule/DSM-IV major depression: The Baltimore Epidemiologic Catchment Area follow-up. Archives of General Psychiatry, 54(11), 993–999.
Einarson, A. ( 2010 ). Paroxetine use in pregnancy and increased risk of heart defects: Evaluating the evidence. Canadian Family Physician, 56(8), 767–768.
Einarson, T. R. , & Einarson, A. ( 2005 ). Newer antidepressants in pregnancy and rates of major malformations: A meta-analysis of prospective comparative studies. Pharmacoepidemiology and Drug Safety, 14(12), 823–827.
Eskandari, F. , Martinez, P. E. , Torvik, S. , Phillips, T. M. , Sternberg, E. M. , Mistry, S. , … Cizza, G. ( 2007 ). Low bone mass in premenopausal women with depression. Archives of Internal Medicine, 167(21), 2329–2336.
Faisal-Cury, A. , & Rossi Menezes, P. ( 2007 ). Prevalence of anxiety and depression during pregnancy in a private setting sample. Archives of Women’s Mental Health, 10(1), 25–32.
Farvolden, P. , Kennedy, S. H. , & Lam, R. W. ( 2003 ). Recent developments in the psychobiology and pharmacotherapy of depression: Optimising existing treatments and novel approaches for the future. Expert Opinion on Investigational Drugs, 12(1), 65–86.
Field, T. , & Diego, M. ( 2008 ). Cortisol: The culprit prenatal stress variable. International Journal of Neuroscience, 118(8), 1181–1205.
Field, T. , Diego, M. , Dieter, J. , Hernandez-Reif, M. , Schanberg, S. , Kuhn, C. , … Bendell, D. ( 2004 ). Prenatal depression effects on the fetus and the newborn. Infant Behavior and Development, 27(2), 216–229.
Field, T. , Diego, M. , Hernandez-Reif, M. , Deeds, O. , & Figueiredo, B. ( 2009 ). Pregnancy massage reduces prematurity, low birthweight and postpartum depression. Infant Behavior and Development, 32(4), 454–460.
Field, T. , Grizzle, N. , Scafidi, F. , & Schanberg, S. ( 1996 ). Massage and relaxation therapies’ effects on depressed adolescent mothers. Adolescence, 31(124), 903–911.
Fitelson, E. , Kim, S. , Baker, A. S. , & Leight, K. ( 2011 ). Treatment of postpartum depression: Clinical, psychological and pharmacological options. International Journal of Women’s Health, 3 , 1–14.
Fortinguerra, F. , Clavenna, A. , & Bonati, M. ( 2009 ). Psychotropic drug use during breastfeeding: A review of the evidence. Pediatrics, 124(4), e547–e556.
Franssen, E. J. , Meijs, V. , Ettaher, F. , Valerio, P. G. , Keessen, M. , & Lameijer, W. ( 2006 ). Citalopram serum and milk levels in mother and infant during lactation. Therapeutic Drug Monitoring, 28(1), 2–4.
Freeman, M. P. ( 2009 ). Complementary and alternative medicine for perinatal depression. Journal of Affective Disorders, 112(1-3), 1–10.
Freeman, M. P. , Hibbeln, J. R. , Wisner, K. L. , Watchman, M. , & Gelenberg, A. J. ( 2006 ). An open trial of omega-3 fatty acids for depression in pregnancy. Acta Neuropsychiatrica, 18(1), 21–24.
Gavin, N. I. , Gaynes, B. N. , Lohr, K. N. , Meltzer-Brody, S. , Gartlehner, G. , & Swinson, T. ( 2005 ). Perinatal depression: A systematic review of prevalence and incidence. Obstetrics and Gynecology, 106(5, Pt. 1), 1071–1083.
Gaynes, B. N. , Gavin, N. , Meltzer-Brody, S. , Lohr, K. N. , Swinson, T. , Gartlehner, G. , … Miller, W. C. ( 2005 ). Perinatal depression: Prevalence, screening accuracy, and screening outcomes. Evidence Report: Technology Assessment ( Summary ), 119 , 1–8.
Gloth, F. M. 3rd, Alam, W. , & Hollis, B. ( 1999 ). Vitamin D vs broad spectrum phototherapy in the treatment of seasonal affective disorder. Journal of Nutrition Health and Aging, 3(1), 5–7.
Goldberg, D. P. , & Hillier, V. F. ( 1979 ). A scaled version of the general health questionnaire. Psychological Medicine, 9(1), 139–145.
Goldbort, J. ( 2006 ). Transcultural analysis of postpartum depression. American Journal of Maternal/Child Nursing, 31(2), 121–126.
Gonda, X. , Telek, T. , Juhász, G. , Lazary, J. , Vargha, A. , & Bagdy, G. ( 2008 ). Patterns of mood changes throughout the reproductive cycle in healthy women without premenstrual dysphoric disorders. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 32(8), 1782–1788.
Grigoriadis, S. , VonderPorten, E. H. , Mamisashvili, L. , Tomlinson, G. , Dennis, C. L. , Koren, G. , … & Ross, L. E. ( 2014 ). Prenatal exposure to antidepressants and persistent pulmonary hypertension of the newborn: systematic review and meta-analysis. BMJ: British Medical Journal , 348 .
Halbreich, U. , & Karkun, S. ( 2006 ). Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. Journal of Affective Disorders, 91(2), 97–111.
Hale, T. W. ( 2012 ). Medications and mothers’ milk: A manual of lactational pharmacology (15th ed.). Amarillo, TX: Hale Publishing.
Hamilton, M. ( 1960 ). A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry, 23(1), 56–62.
Hanusa, B. H. , Scholle, S. H. , Haskett, R. F. , Spadaro, K. , & Wisner K. ( 2008 ). Screening for depression in the postpartum period: A comparison of three instruments. Journal of Women’s Health ( Larchmont ), 17 (4), 585–596.
Heikkinen, T. , Ekblad, U. , Kero, P. , Ekblad, S. , & Laine, K. ( 2002 ). Citalopram in pregnancy and lactation. Clinical Pharmacology and Therapeutics, 72(2), 184–191.
Hemels, M. E. H. , Einarson, A. , Koren, G. , Lanctot, K. L. , & Einarson, T. R. ( 2005 ). Antidepressant use during pregnancy and the rates of spontaneous abortions: A meta-analysis. Annals of Pharmacotherapy, 39(5), 803–809.
Hirst, K. P. , & Moutier, C. Y. ( 2010 ). Postpartum major depression. American Family Physician, 82(8), 926–933.
Hollon, S. D. ( 1998 ). What is cognitive behavioural therapy and does it work? Current Opinions in Neurobiology, 8(2), 289–292.
Homish, G. G. , Cornelis, J. R. , Richardson, G. A. , & Day, N. L. ( 2004 ). Antenatal risk factors associated with postpartum comorbid alcohol use and depressive symptomatology. Alcoholism: Clinical and Experimental Research, 28(8), 1242–1248.
Honey, K. L. , Bennett, P. , & Morgan, M. ( 2002 ). A brief psycho- educational group intervention for postnatal depression. British Journal of Clinical Psychology, 41(Pt. 4), 405–409.
Horwitz, S. M. , Briggs-Gowan, M. J. , Storfer-Isser, A. , & Carter, A. S. ( 2007 ). Prevalence, correlates, and persistence of maternal depression. Journal of Women’s Health ( Larchmont ), 16 (5), 678–691.
Jesse, D. E. , Walcott-McQuigg, J. , Mariella, A. , & Swanson, M. S. ( 2005 ). Risks and protective factors associated with symptoms of depression in low-income African American and Caucasian women during pregnancy. Journal of Midwifery and Women’s Health, 50(5), 405–410.
Jolley, S. N. , & Betrus, P. ( 2007 ). Comparing postpartum depression and major depressive disorder: Issues in assessment. Issues in Mental Health Nursing, 28(7), 765–780.
Jones, L. , Scott, J. , Cooper, C. , Forty, L. , Smith, K. G. , Sham, P. , … Jones, I. ( 2010 ). Cognitive style, personality and vulnerability to postnatal depression. British Journal of Psychiatry, 196(3), 200–205.
Jorde, R. , Sneve, M. , Figenschau, Y. , Svartberg, J. , & Waterloo, K. ( 2008 ). Effects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: Randomized double blind trial. Journal of Internal Medicine, 264(6), 599–609.
Källén, B. A. ( 2004 ). Neonate characteristics after maternal use of antidepressants in late pregnancy. Archives of Pediatrics and Adolescent Medicine, 158(4), 312–316.
Källén, B. A. , & Otterblad Olausson, P. ( 2003 ). Maternal drug use in early pregnancy and infant cardiovascular defect. Reproductive Toxicology, 17(3), 255–261.
Källén, B. A. , & Otterblad Olausson, P. ( 2007 ). Maternal use of selective serotonin re-uptake inhibitors in early pregnancy and infant congenital malformations. Birth Defects Research. Part A: Clinical and Molecular Teratology, 79(4), 301–308.
Keller, M. B. , Shapiro, R. W. , Lavori, P. W. , & Wolfe, N. ( 1982 ). Recovery in major depressive disorder: Analysis with the life table and regression models. Archives of General Psychiatry, 39(8), 905–910.
Kellner, R. ( 1987 ). A symptom questionnaire. Journal of Clinical Psychiatry, 48(7), 268–274.
Kelly, R. H. , Danielsen, B. H. , Golding, J. M. , Anders, T. F. , Gilbert, W. M. , & Zatzick, D. F. ( 1999 ). Adequacy of prenatal care among women with psychiatric diagnoses giving birth in California in 1994 and 1995. Psychiatric Services, 50(12), 1584–1590.
Kim, J. , Riggs, K. W. , Misri, S. , Kent, N. , Oberlander, T. F. , Grunau, R. E. , … Rurak, D. W. ( 2006 ). Stereoselective disposition of fluoxetine and norfluoxetine during pregnancy and breast-feeding. British Journal of Clinical Pharmacology, 61(2), 155–163.
Kim, J. J. , La Porte, L. M. , Adams, M. G. , Gordon, T. E. J. , Kuendig, J. M. , & Silver, R. K. ( 2009 ). Obstetric care provider engagement in a perinatal depression screening program. Archives Women’s Mental Health, 12(3), 167–172.
Kitamura, T. , Shima, S. , Sugawara, M. , & Toda, M. A. ( 1993 ). Psychological and social correlates of the onset of affective disorders among pregnant women. Psychological Medicine, 23(4), 967–975.
Klein, D. N. , Schatzberg, A. F. , McCullough, J. P. , Dowling, F. , Goodman, D. , Howland, R. H. … Keller, M. B. ( 1999 ). Age of onset in chronic major depression: Relation to demographic and clinical variables, family history, and treatment response. Journal of Affective Disorders, 55(2-3), 149–157.
Klier, C. M. , Muzik, M. , Rosenblum, K. L. , & Lenz, G. ( 2001 ). Interpersonal psychotherapy adapted for the group setting in the treatment of postpartum depression. Journal of Psychotherapy Practice and Research, 10(2), 124–131.
Korja, R. , Savonlahti, E. , Ahlqvist-Bjorkroth, S. , Stolt, S. , Haataja, L. , Lapinleimu, H. , … Lehtonen, L. ( 2008 ). Maternal depression is associated with mother-infant interaction in preterm infants. Acta Paediatrica, 97(6), 724–730.
Kristensen, J. H. , Ilett, K. F. , Hackett, L. P. , Yapp, P. , Paech, M. , & Begg, E. J. ( 1999 ). Distribution and excretion of fluoxetine and norfluoxetine in human milk. British Journal of Clinical Pharmacology, 48(4), 521–527.
Kroenke, K. , Spitzer, R. L. , & Williams, J. B ( 2001 ). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613.
Kumar, R. , & Robson, K. M. ( 1984 ). A prospective study of emotional disorders in childbearing women. British Journal of Psychiatry, 144(1), 35–47.
LaCoursiere, D. Y. , Hirst, K. P. , & Barrett-Connor, E. ( 2012 ). Depression and pregnancy stressors affect the association between abuse and postpartum depression. Maternal and Child Health Journal , 16 (4), 929–935.
Lam, R. W. , Kennedy, S. H. , Grigoriadis, S. , McIntyre, R. S. , Milev, R. , Ramasubbu, R. , … Ravindran, A. V. ( 2009 ). Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. III. Pharmacotherapy. Journal of Affective Disorders, 17(Suppl. 1), 26–43.
Lancaster, C. A. , Gold, K. J. , Flynn, H. A. , Yoo, H. , Marcus, S. M. , & Davis, M. M. ( 2010 ). Risk factors for depressive symptoms during pregnancy: A systematic review. American Journal of Obstetrics and Gynecology, 202(1), 5–14.
Lanza Di Scalea, T. , & Wisner, K. L. ( 2009 ). Antidepressant medication use during breastfeeding. Clinical Obstetrics and Gynaecology, 52(3), 483–497.
Leddy, M. A. , Jones, C. , Morgan, M. A. , & Schulkin, J. ( 2009 ). Eating disorders and obstetric-gynecologic care. Journal of Women’s Health, 18(9), 1395–1401.
Lee, D. T. S. , Yip, A. S. K. , Chiu, H. F. K. , Leung, T. Y. S. , & Chung, T. K. H. ( 2001 ). A psychiatric epidemiological study of postpartum Chinese women. American Journal of Psychiatry, 158(2), 220–226.
Leeners, B. , Richter-Appelt, H. , Imthurn, B. , & Rath, W. ( 2006 ). Influence of childhood sexual abuse on pregnancy, delivery, and the early postpartum period in adult women. Journal of Psychosomatic Research , 61 (2), 139–151.
Lepine, J. P. , Gastpar, M. , Mendlewicz, J. , & Tylee, A. ( 1997 ). Depression in the community: The first pan-European study DEPRES (Depression Research in European Society ). International Clinical Psychopharmacology, 12(1), 19–29.
Le Strat, Y. , Dubertret, C. , & Le Foll, B. ( 2011 ). Prevalence and correlates of major depressive episode in pregnant and postpartum women in the United States. Journal of Affective Disorders, 135(1-3), 128–138.
Louik, C. , Lin, A. E. , Werler, M. M. , Hernández-Díaz, S. , & Mitchell, A. A. ( 2007 ). First-trimester use of selective serotonin-reuptake inhibitors and the risk of birth defects. New England Journal of Medicine, 356(26), 2675–2683.
Madigan, S. , Moran, G. , Schuengel, C. , Pederson, D. R. , & Otten, R. ( 2007 ). Unresolved maternal attachment representations, disrupted maternal behavior and disorganized attachment in infancy: Links to toddler behavior problems. Journal of Child Psychology and Psychiatry and Allied Disciplines, 48(10), 1042–1050.
Manber, R. , Schnyer, R. N. , Allen, J. J. B. , Rush, A. J. , & Blasey, C. M. ( 2004 ). Acupuncture: A promising treatment for depression during pregnancy. Journal of Affective Disorders, 83(1), 89–95.
Manber, R. , Schnyer, R. N. , Lyell, D. , Chambers, A. S. , Caughey, A. B. , Druzin, M. , … Allen, J. J. ( 2010 ). Acupuncture for depression during pregnancy: A randomized controlled trial. Obstetrics and Gynecology, 115(3), 511–520.
Marcus, S. M. ( 2009 ). Depression during pregnancy: Rates, risks and consequences—Motherisk Update 2008. Canadian Journal of Clinical Pharmacology, 16(1), e15–e22.
Marcus, S. M. , Flynn, H. A. , Blow, F. C. , & Barry, K. L. ( 2003 ). Depressive symptoms among pregnant women screened in obstetrics settings. Journal of Women’s Health ( Larchmont ), 12 (4), 373–380.
Marks, M. , Wieck, A. , Checkley, S. , & Kumar, C. ( 1996 ). How does marriage protect women with histories of affective disorder from post-partum relapse? British Journal of Medical Psychology, 69(Pt. 4), 329–342.
Martins, C. , & Gaffan, E. A. ( 2000 ). Effects of early maternal depression on patterns of infant-mother attachment: A meta-analytic investigation. Journal of Child Psychology and Psychiatry and Allied Disciplines, 41(6), 737–746.
Matthey, S. , Barnett, B. , Howie, P. , & Kavanagh, D. J. ( 2003 ). Diagnosing postpartum depression in mothers and fathers: whatever happened to anxiety? Journal of Affective Disorders , 74 (2), 139-147.
Mazzeo, S. E. , Slof-Op’t Landt, M. C. , Jones, I. , Mitchell, K. , Kendler, K. S. , Neale, M. C. , … Bulik, C. M. ( 2006 ). Associations among postpartum depression, eating disorders, and perfectionism in a population-based sample of adult women. International Journal of Eating Disorders, 39(3), 202–211.
McCoy, S. J. B. , Beal, J. M. , Shipman, S. B. , Payton, M. E. , & Watson, G. H. ( 2006 ). Risk factors for postpartum depression: A retrospective investigation at 4-weeks postnatal and a review of the literature. Journal of the American Osteopathic Association, 106(4), 193–198.
Meltzer-Brody, S. ( 2011 ). New insights into perinatal depression: Pathogenesis and treatment during pregnancy and postpartum. Dialogues in Clinical Neuroscience, 13(1), 89–100.
Meltzer-Brody, S. , Zerwas, S. , Leserman, J. , Holle, A. V. , Regis, T. , & Bulik, C. ( 2011 ). Eating disorders and trauma history in women with perinatal depression. Journal of Women’s Health ( Larchmont ), 20 (6), 863–870.
Melville, J. L. , Gavin, A. , Guo, Y. , Fan, M. Y. , & Katon, W. J. ( 2010 ). Depressive disorders during pregnancy: Prevalence and risk factors in a large urban sample. Obstetrics and Gynecology, 116(5), 1064–1070.
Micali, N. , Simonoff, E. , & Treasure, J. ( 2011 ). Pregnancy and post-partum depression and anxiety in a longitudinal general population cohort: The effect of eating disorders and past depression. Journal of Affective Disorders, 131(1-3), 150–157.
Milgrom, J. , Gemmill, A. W. , Bilszta, J. L. , Hayes, B. , Barnett, B. , Brooks, J. , … Buist, A. ( 2008 ). Antenatal risk factors for postnatal depression: A large prospective study. Journal of Affective Disorders, 108(1-2), 147–157.
Milgrom, J. , Negri, L. M. , Gemmill, A. W. , McNeil, M. , & Martin P. R. ( 2005 ). A randomized controlled trial of psychological interventions for postnatal depression. British Journal of Clinical Psychology, 44(Pt. 4), 529–542.
Miller, L. , Shade, M. , & Vasireddy, V. ( 2009 ). Beyond screening: Assessment of perinatal depression in a perinatal care setting. Archives of Women’s Mental Health, 12(5), 329–334.
Misri, S. , & Kendrick, K. ( 2007 ). Treatment of perinatal mood and anxiety disorders: A review. Canadian Journal of Psychiatry, 52(8), 489–498.
Misri, S. , Kostaras, X. , Fox, D. , & Kostaras, D. ( 2000 ). The impact of partner support in the treatment of postpartum depression. Canadian Journal of Psychiatry, 45(6), 554–558.
Misri, S. , Reebye, P. , Corral, M. , & Milis, L. ( 2004 ). The use of paroxetine and cognitive-behavioral therapy in postpartum depression and anxiety: A randomized controlled trial. Journal of Clinical Psychiatry, 65(9), 1236–1241.
Mori, T. , Tsuchiya, K. J. , Matsumoto, K. , Suzuki, K. , Mori, N. , Takei, N. , & The HBC Study Team. ( 2011 ). Psychosocial risk factors for postpartum depression and their relation to timing of onset: The Hamamatsu Birth Cohort (HBC) Study. Journal of Affective Disorders, 135(1-3), 341–346.
Mulcahy, R. , Reay, R. E. , Wilkinson, R. B. , & Owen, C. ( 2010 ). A randomised control trial for the effectiveness of group interpersonal psychotherapy for postnatal depression. Archives of Women’s Mental Health, 13(2), 125–139.
Murray, L. , & Cooper, P. J. ( 1997 ). Postpartum depression and child development. Psychological Medicine, 27(2), 253–260.
Murray, D. , & Cox, J. L. ( 1990 ). Screening for depression during pregnancy with the Edinburgh Depression Scale (EPDS). Journal of Reproductive and Infant Psychology, 8(2), 99–107.
Muzik, M. , Marcus, S. M. , Flynn, H. , & Rosenblum, K. L. ( 2010 ). Depression during pregnancy: Detection, comorbidity and treatment. Asia-Pacific Psychiatry, 2(1), 7–18.
Nemeroff, C. B. ( 2002 ). Recent advances in the neurobiology of depression. Psychopharmacology Bulletin, 36(Suppl. 2), 6–23.
Nemeroff, C. B. ( 1998 ). The neurobiology of depression. Scientific American, 278(6), 42–49.
Newton-Howes, G. , Tyrer, P. , & Johnson, T. ( 2006 ). Personality disorder and the outcome of depression: Meta-analysis of published studies. British Journal of Psychiatry, 188(1), 13–20.
Nulman, I. , Rovet, J. , Stewart, D. E. , Wolpin, J. , Pace-Asciak, P. , Shuhaiber, S. , & Koren, G. ( 2002 ). Child development following exposure to tricyclic antidepressants or fluoxetine throughout fetal life: A prospective, controlled study. American Journal of Psychiatry, 159(11), 1889–1895.
Oates, M. ( 2003 ). Suicide: The leading cause of maternal death. British Journal of Psychiatry, 183(4), 279–281.
Oberlander, T. F. , Grunau, R. E. , Fitzgerald, C. , Papsdorf, M. , Rurak, D. , & Riggs, W. ( 2005 ). Pain reactivity in 2-month-old infants after prenatal and postnatal serotonin reuptake inhibitor medication exposure. Pediatrics, 115(2), 411–425.
Oberlander, T. F. , Reebye, P. , Misri, S. , Papsdorf, M. , Kim, J. , & Grunau, R. E. ( 2007 ). Externalizing and attentional behaviors in children of depressed mothers treated with a selective serotonin reuptake inhibitor antidepressant during pregnancy. Archives of Pediatric and Adolescent Medicine, 161(1), 22–29.
Oberlander, T. F. , Warburton, W. , Misri, S. , Aghajanian, J. , & Hertzman, C. ( 2006 ). Neonatal outcomes after prenatal exposure to selective serotonin reuptake inhibitor antidepressants and maternal depression using population-based linked health data. Archives of General Psychiatry, 63(8), 898–906.
O’Brien, L. , Einarson, T. R. , Sarkar, M. , Einarson, A. , & Koren, G. ( 2008 ). Does paroxetine cause cardiac malformations? Journal of Obstetrics and Gynaecology Canada, 30(8), 696–701.
Occhiogrosso, M. , Omran, S. S. , & Altemus, M. ( 2012 ). Persistent pulmonary hypertension of the newborn and selective serotonin reuptake inhibitors: lessons from clinical and translational studies. American Journal of Psychiatry , 169 (2), 134-140.
O’Hara, M. W. , Hoffman, J. G. , Phillips, L. H. C. , & Wright, E. J. ( 1992 ). Adjustment in childbearing women: The Postpartum Adjustment Questionnaire. Psychological Assessment, 4(2), 160–169.
O’Hara, M. W. , Stuart, S. , Gorman, L. L. , & Wenzel, A. ( 2000 ). Efficacy of interpersonal psychotherapy for postpartum depression. Archives of General Psychiatry, 57(11), 1039–1045.
O’Hara, M. W. , & Swain, A. M. ( 1996 ). Rates and risk of postpartum depression—a meta-analysis. International Review of Psychiatry, 8(1), 37–54.
O’Higgins, M. , St James Roberts, I. , & Glover, V. ( 2008 ). Postnatal depression and mother and infant outcomes after infant massage. Journal of Affective Disorders , 109 (1), 189-192.
Olson, A. L. , Dietrich, A. J. , Prazar, G. , & Hurley, J. ( 2006 ). Brief maternal depression screening at well-child visits. Pediatrics, 118(1), 207–216.
Onozawa, K. , Glover, V. , Adams, D. , Modi, N. , & Kumar, R. C. ( 2001 ). Infant massage improves mother–infant interaction for mothers with postnatal depression. Journal of Affective Disorders , 63 (1), 201-207.
Park, E. H. M. , & Dimigen, G. ( 1995 ). A cross-cultural comparison: Postnatal depression in Korean and Scottish mothers. Psychologia: An International Journal of Psychology in the Orient, 38(3), 199–207.
Parker, G. , Tupling, H. , Brown, L. B. ( 1979 ). A parental bonding instrument. British Journal of Medical Psychology, 52(1), 1–10.
Pope, S. ( 2000 ). Postnatal depression: A systematic review of published scientific literature to 1999. Canberra: National Health and Medical Research Council.
Posmontier, B. , & Horowitz, J. A. ( 2004 ). Postpartum practices and depression prevalences: Technocentric and ethnokinship cultural perspectives. Journal of Transcultural Nursing, 15(1), 34–43.
Rahimi, R. , Nikfar, S. , & Abdollahi, M. ( 2006 ). Pregnancy outcomes following exposure to serotonin reuptake inhibitors: A meta-analysis of clinical trials. Reproductive Toxicology, 22(4), 571–575.
Rakhshani, A. , Maharana, S. , Raghuram, N. , Nagendra, H. R. , & Venkatram P. ( 2010 ). Effects of integrated yoga on quality of life and interpersonal relationship of pregnant women. Quality of Life Research , 19 (10), 1447–1455.
Ravindran, A. V. , Lam, R. W. , Filteau, M. J. , Lespérance, F. , Kennedy, S. H. , Parikh, S. V. , & Patten, S. B. ( 2009 ). Canadian Network for Mood and Anxiety Treatments (CANMAT). Clinical guidelines for the management of major depressive disorder in adults. V. Complementary and alternative medicine treatments. Journal of Affective Disorders, 117(Suppl. 1), S54–S64.
Rayworth, B. B. , Wise, L. A. , & Harlow, B. L. ( 2004 ). Childhood abuse and risk of eating disorders in women. Epidemiology, 15(3), 271–278.
Reay, R. , Fisher, Y. , Robertson, M. , Adams, E. , Owen, C. , & Kumar, R. ( 2006 ). Group interpersonal psychotherapy for postnatal depression: A pilot study. Archives of Women’s Mental Health, 9(1), 31–39.
Reay, R. E. , Owen, C. , Shadbolt, B. , Raphael, B. , Mulcahy, R. , & Wilkinson, R. B. ( 2012 ). Trajectories of long-term outcomes for postnatally depressed mothers treated with group interpersonal psychotherapy. Archives of Women’s Mental Health, 15(3), 217–228.
Reck, C. , Struben, K. , Backenstrass, M. , Stefenelli, U. , Reinig, K. , Fuchs, T. , … Mundt, C. ( 2008 ). Prevalence, onset and comorbidity of postpartum anxiety and depressive disorders. Acta Psychiatrica Scandianavica, 118(6), 459–468.
Righetti-Veltema, M. , Conne-Perréard, E. , Bousquet, A. , & Manzano, J. ( 2002 ). Postpartum depression and mother-infant relationship at 3 months old. Journal of Affective Disorders, 70(3), 291–306.
Ross, L. E. , & Dennis, C. ( 2009 ). The prevalence of postpartum depression among women with substance use, an abuse history, or chronic illness: A systematic review. Journal of Women’s Health, 18(4), 475–486.
Segre, L. S. , O’Hara, M. W. , Arndt, S. , & Stuart, S. ( 2007 ). The prevalence of postpartum depression: The relative significance of three social status indices. Social Psychiatry and Psychiatric Epidemiology, 42(4), 316–321.
Shadigian, E. , & Bauer, S. T. ( 2005 ). Pregnancy-associated death: A qualitative systematic review of homicide and suicide. Obstetrical & Gynecological Survey, 60(3), 183–190.
Sheehan, D. V. , Lecrubier, Y. , Sheehan, K. H. , Amorim, P. , Janavs, J. , Weiller, E. , … Dunbar, G. C. ( 1998 ). The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(Suppl. 20), 22–33.
Simon, G. E. , Cunningham, M. L. , & Davis, R. L. ( 2002 ). Outcomes of prenatal antidepressant exposure. American Journal of Psychiatry, 159(12), 2055–2061.
Skouteris, H. , Wertheim, E. H. , Rallis, S. , Milgrom, J. , & Paxton, S. J. ( 2009 ). Depression and anxiety through pregnancy and the early postpartum: An examination of prospective relationships. Journal of Affective Disorders, 113(3), 303–308.
Skrundz, M. , Bolten, M. , Nast, I. , Hellhammer, D. H. , & Meinlschmidt, G. ( 2011 ). Plasma oxytocin concentration during pregnancy is associated with development of postpartum depression. Neuropsychopharmacology, 36(9), 1886–1893.
Smith, C. A. , & Cochrane, S. ( 2009 ). Does acupuncture have a place as an adjunct treatment during pregnancy? A review of randomized controlled trials and systematic reviews. Birth, 36(3), 246–253.
Smith, M. V. , Rosenheck, R. A. , Cavaleri, M. A. , Howell, H. B. , Poschman, K. , & Yonkers, K. A. ( 2004 ). Screening for and detection of depression, panic disorder, and PTSD in public-sector obstetric clinics. Psychiatric Services, 55(4), 407–414.
Soderquist, J. , Wijma, B. , Thorbert, G. , & Wijma, K. ( 2009 ). Risk factors in pregnancy for posttraumatic stress and depression after childbirth. An International Journal of Obstetrics & Gynecology, 116(5), 672–680.
Spanier, G. B. ( 1976 ). Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family, 38(1), 15–28.
Statistics Canada. (2002). Health indicators (Report No. 82-221-XIE). Retrieved from http://www.statcan.gc.ca/pub/82-221-x/00502/4149152-eng.htm
Stowe, Z. N. , Hostetter, A. L. , Owens, M. J. , Ritchie, J. C. , Sternberg, K. , Cohen, L. S. , & Nemeroff, C. B. ( 2003 ). The pharmacokinetics of sertraline excretion into human breast milk: Determinants of infant serum concentrations. Journal of Clinical Psychiatry, 64(1), 73–80.
Stuart, S. , & O’Hara, M. W. ( 1995 ). Interpersonal psychotherapy for postpartum depression: A treatment program. Journal of Psychotherapy Practice and Research, 4(1), 18–29.
Stuchbery, M. , Matthey, S. , & Barnett, B. ( 1998 ). Postnatal depression and social supports in Vietnamese, Arabic and Anglo-Celtic mothers. Social Psychiatry and Psychiatric Epidemiology, 33(10), 483–490.
Tamaki, R. , Murata, M. , & Okano, T. ( 1997 ). Risk factors for postpartum depression in Japan. Psychiatry and Clinical Neurosciences, 51(3), 93–98.
Thombs, B. D. , Arthurs, E. , Coronado-Montoya, S. , Roseman, M. , Delisle, V. C. , Leavens, A. , … & Zelkowitz, P. ( 2014 ). Depression screening and patient outcomes in pregnancy or postpartum: a systematic review. Journal of Psychosomatic Research , 76 (6), 433-446.
Thys-Jacobs, S. , Silverton, M. , Alvir, J. , Paddison, P. L. , Ricco, M. , & Goldsmith, S. J. ( 1995 ). Reduced bone mass in women with premenstrual syndrome. Journal of Women’s Health, 4(2), 161–168.
Trapolini, T. , McMahon, C. A. , & Ungerer, J. A. ( 2007 ). The effect of maternal depression and marital adjustment on young children’s internalizing and externalizing behaviour problems. Child: Care, Health and Development, 33(6), 794–803.
Udechuku, A. , Nguyen, T. , Hill, R. , & Szego, K. ( 2010 ). Antidepressants in pregnancy: A systematic review. Australian and New Zealand Journal of Psychiatry, 44(11), 978–996.
Uebelacker, L. A. , Tremont, G. , Epstein-Lubow, G. , Gaudiano, B. A. , Gillette, T. , Kalibatseva, Z. , … Miller, I. W. ( 2010 ). Open trial of vinyasa yoga for persistently depressed individuals: Evidence of feasibility and acceptability. Behavior Modification, 34(3), 247–264.
Uguz, F. , Akman, C. , Sahingoz, M. , Kaya, N. , & Kucur, R. ( 2009 ). One year follow-up of post-partum-onset depression: The role of depressive symptom severity and personality disorders. Journal of Psychosomatic Obstetrics and Gynaecology, 30(2), 141–145.
Underdown, A. , Norwood, R. , & Barlow, J. ( 2013 ). A realistic evaluation of the processes and outcomes of infant massage programs. Infant Mental Health Journal , 34 (6), 483–495.
U.S. Food and Drug Administration. (2012, January 9). FDA Drug and Safety Communication: Selective serotonin reuptake inhibitor (SSRI) antidepressant use during pregnancy and reports of a rare heart and lung condition in newborn babies. Retrieved from www.fda.gov/Drugs/DrugSafety/ucm283375.htm
Van den Bergh, B. R. , Mulder, E. J. , Mennes, M. , & Glover, V. ( 2005 ). Antenatal maternal anxiety and stress and the neurobehavioral development of the fetus and child: Links and possible mechanisms. A review. Neuroscience & Biobehavioral Reviews, 29(2), 237–258.
Weier, K. M. , & Beal, M. W. ( 2004 ). Complementary therapies as adjuncts in the treatment of postpartum depression. Journal of Midwifery & Women’s Health, 49(2), 96–104.
Weinstock, M. ( 2005 ). The potential influence of maternal stress hormones on development and mental health of the offspring. Brain, Behavior, and Immunity, 19(4), 296–308.
Weissman, M. M. , Bland, R. C. , Canino, G. J. , Faravelli, C. , Greenwald, S. , Hwu, H. G. , … Yeh, E. K. ( 1996 ). Cross-national epidemiology of major depression and bipolar disorder. Journal of the American Medical Association, 276(4), 293–299.
Weissman, M. M. , & Bothwell, S. ( 1976 ). Assessment of social adjustment by patient self-report. Archives of General Psychiatry, 33(9), 1111–1115.
Weissman, A. M. , Levy, B. T. , Hartz, A. J. , Bentler, S. , Donohue, M. , Ellingrod, V. L. , & Wisner, K. L. ( 2004 ). Pooled analysis of antidepressant levels in lactating mothers, breast milk, and nursing infants. American Journal of Psychiatry, 161(6), 1066–1078.
Weissman, M. M. , Wickramaratne, P. , Nomura, Y. , Warner, V. , Pilowsky, D. , & Verdeli, H. ( 2006 ). Offspring of depressed parents: 20 years later. American Journal of Psychiatry, 163(6), 1001–1008.
Wenzel, A. , Haugen, E. N. , Jackson, L. C. , & Brendle, J. R. ( 2005 ), Anxiety symptoms and disorders at eight weeks postpartum. Journal of Anxiety Disorders, 19(3), 295–311.
Wickberg, B. , & Hwang, C. P. ( 1996 ). Counselling of postnatal depression: A controlled study on a population based Swedish sample. Journal of Affective Disorders, 39(3), 209–216.
Wisner, K. L. , Parry, B. L. , & Piontek, C. M. ( 2002 ). Clinical practice. Postpartum depression. New England Journal of Medicine, 347(3), 194–199.
Wisner, K. L. , Perel, J. M. , & Findling, R. L. ( 1996 ). Antidepressant treatment during breast-feeding. American Journal of Psychiatry, 153(9), 1132–1137.
Wittchen, H. U. , & Boyer, P. ( 1998 ). Screening for anxiety disorders: Sensitivity and specificity of the anxiety screening questionnaire (ASQ-15 ). British Journal of Psychiatry, 173(34), s10–s17.
Wittchen, H. U. , Wunderlich, U. , Gruschwitz, S. , & Zaudig, M. ( 1997 ). SCID. Structured clinical interview for DSM-IV, axis I. Goettingen: Hogrefe.
Wójcik, J. , Dudek, D. , Schlegel-Zawadzka, M. , Grabowska, M. , Marcinek, A. , Florek, E. , … Nowak, G. ( 2006 ). Antepartum/postpartum depressive symptoms and serum zinc and magnesium levels. Pharmacological Reports, 58(4), 571–576.
Xie, R. H. , He, G. , Koszycki, D. , Walker, M. , & Wen, S. W. ( 2009 ). Prenatal social support, postnatal social support, and postpartum depression. Annals of Epidemiology, 19(9), 637–643.
Yonkers, K. A. , Wisner, K. L. , Stewart, D. E. , Oberlander, T. F. , Dell, D. L. , Stotland, N. , … Lockwood, C. ( 2009 ). The management of depression during pregnancy: A report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. General Hospital Psychiatry, 31(5), 403–413.
Yoshida, K. , Marks, M. N. , Kibe, N. , Kumar, R. , Nakano, H. , & Tashiro, N. ( 1997 ). Postnatal depression in Japanese women who have given birth in England. Journal of Affective Disorders, 43(1), 69–77.
Zisook, S. , Lesser, I. , Stewart, J. W. , Wisniewski, S. R. , Balasubramani, G. K. , Fava, M. , … Rush, A. J. ( 2007 ). Effect of age of onset on the course of major depressive disorder. American Journal of Psychiatry, 164(10), 1539–1546.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Patient Care & Health Information
- Diseases & Conditions
- Postpartum depression
The birth of a baby can start a variety of powerful emotions, from excitement and joy to fear and anxiety. But it can also result in something you might not expect — depression.
Most new moms experience postpartum "baby blues" after childbirth, which commonly include mood swings, crying spells, anxiety and difficulty sleeping. Baby blues usually begin within the first 2 to 3 days after delivery and may last for up to two weeks.
But some new moms experience a more severe, long-lasting form of depression known as postpartum depression. Sometimes it's called peripartum depression because it can start during pregnancy and continue after childbirth. Rarely, an extreme mood disorder called postpartum psychosis also may develop after childbirth.
Postpartum depression is not a character flaw or a weakness. Sometimes it's simply a complication of giving birth. If you have postpartum depression, prompt treatment can help you manage your symptoms and help you bond with your baby.
Products & Services
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- A Book: Mayo Clinic Guide to Your Baby's First Years
- A Book: Obstetricks
Symptoms of depression after childbirth vary, and they can range from mild to severe.
Baby blues symptoms
Symptoms of baby blues — which last only a few days to a week or two after your baby is born — may include:
- Mood swings
- Irritability
- Feeling overwhelmed
- Reduced concentration
- Appetite problems
- Trouble sleeping

Postpartum depression symptoms
Postpartum depression may be mistaken for baby blues at first — but the symptoms are more intense and last longer. These may eventually interfere with your ability to care for your baby and handle other daily tasks. Symptoms usually develop within the first few weeks after giving birth. But they may begin earlier — during pregnancy — or later — up to a year after birth.
Postpartum depression symptoms may include:
- Depressed mood or severe mood swings
- Crying too much
- Difficulty bonding with your baby
- Withdrawing from family and friends
- Loss of appetite or eating much more than usual
- Inability to sleep, called insomnia, or sleeping too much
- Overwhelming tiredness or loss of energy
- Less interest and pleasure in activities you used to enjoy
- Intense irritability and anger
- Fear that you're not a good mother
- Hopelessness
- Feelings of worthlessness, shame, guilt or inadequacy
- Reduced ability to think clearly, concentrate or make decisions
- Restlessness
- Severe anxiety and panic attacks
- Thoughts of harming yourself or your baby
- Recurring thoughts of death or suicide
Untreated, postpartum depression may last for many months or longer.
Postpartum psychosis
With postpartum psychosis — a rare condition that usually develops within the first week after delivery — the symptoms are severe. Symptoms may include:
- Feeling confused and lost
- Having obsessive thoughts about your baby
- Hallucinating and having delusions
- Having sleep problems
- Having too much energy and feeling upset
- Feeling paranoid
- Making attempts to harm yourself or your baby
Postpartum psychosis may lead to life-threatening thoughts or behaviors and requires immediate treatment.
Postpartum depression in the other parent
Studies show that new fathers can experience postpartum depression, too. They may feel sad, tired, overwhelmed, anxious, or have changes in their usual eating and sleeping patterns. These are the same symptoms that mothers with postpartum depression experience.
Fathers who are young, have a history of depression, experience relationship problems or are struggling financially are most at risk of postpartum depression. Postpartum depression in fathers — sometimes called paternal postpartum depression — can have the same negative effect on partner relationships and child development as postpartum depression in mothers can.
If you're a partner of a new mother and are having symptoms of depression or anxiety during your partner's pregnancy or after your child's birth, talk to your health care provider. Similar treatments and supports provided to mothers with postpartum depression can help treat postpartum depression in the other parent.
When to see a doctor
If you're feeling depressed after your baby's birth, you may be reluctant or embarrassed to admit it. But if you experience any symptoms of postpartum baby blues or postpartum depression, call your primary health care provider or your obstetrician or gynecologist and schedule an appointment. If you have symptoms that suggest you may have postpartum psychosis, get help immediately.
It's important to call your provider as soon as possible if the symptoms of depression have any of these features:
- Don't fade after two weeks.
- Are getting worse.
- Make it hard for you to care for your baby.
- Make it hard to complete everyday tasks.
- Include thoughts of harming yourself or your baby.
If you have suicidal thoughts
If at any point you have thoughts of harming yourself or your baby, immediately seek help from your partner or loved ones in taking care of your baby. Call 911 or your local emergency assistance number to get help.
Also consider these options if you're having suicidal thoughts:
- Seek help from a health care provider.
- Call a mental health provider.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential. The Suicide & Crisis Lifeline in the U.S. has a Spanish language phone line at 1-888-628-9454 (toll-free).
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
Helping a friend or loved one
People with depression may not recognize or admit that they're depressed. They may not be aware of signs and symptoms of depression. If you suspect that a friend or loved one has postpartum depression or is developing postpartum psychosis, help them seek medical attention immediately. Don't wait and hope for improvement.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
There is no single cause of postpartum depression, but genetics, physical changes and emotional issues may play a role.
- Genetics. Studies show that having a family history of postpartum depression — especially if it was major — increases the risk of experiencing postpartum depression.
- Physical changes. After childbirth, a dramatic drop in the hormones estrogen and progesterone in your body may contribute to postpartum depression. Other hormones produced by your thyroid gland also may drop sharply — which can leave you feeling tired, sluggish and depressed.
- Emotional issues. When you're sleep deprived and overwhelmed, you may have trouble handling even minor problems. You may be anxious about your ability to care for a newborn. You may feel less attractive, struggle with your sense of identity or feel that you've lost control over your life. Any of these issues can contribute to postpartum depression.
Risk factors
Any new mom can experience postpartum depression and it can develop after the birth of any child, not just the first. However, your risk increases if:
- You have a history of depression, either during pregnancy or at other times.
- You have bipolar disorder.
- You had postpartum depression after a previous pregnancy.
- You have family members who've had depression or other mood disorders.
- You've experienced stressful events during the past year, such as pregnancy complications, illness or job loss.
- Your baby has health problems or other special needs.
- You have twins, triplets or other multiple births.
- You have difficulty breastfeeding.
- You're having problems in your relationship with your spouse or partner.
- You have a weak support system.
- You have financial problems.
- The pregnancy was unplanned or unwanted.
Complications
Left untreated, postpartum depression can interfere with mother-child bonding and cause family problems.
- For mothers. Untreated postpartum depression can last for months or longer, sometimes becoming an ongoing depressive disorder. Mothers may stop breastfeeding, have problems bonding with and caring for their infants, and be at increased risk of suicide. Even when treated, postpartum depression increases a woman's risk of future episodes of major depression.
- For the other parent. Postpartum depression can have a ripple effect, causing emotional strain for everyone close to a new baby. When a new mother is depressed, the risk of depression in the baby's other parent may also increase. And these other parents may already have an increased risk of depression, whether or not their partner is affected.
- For children. Children of mothers who have untreated postpartum depression are more likely to have emotional and behavioral problems, such as sleeping and eating difficulties, crying too much, and delays in language development.
If you have a history of depression — especially postpartum depression — tell your health care provider if you're planning on becoming pregnant or as soon as you find out you're pregnant.
- During pregnancy, your provider can monitor you closely for symptoms of depression. You may complete a depression-screening questionnaire during your pregnancy and after delivery. Sometimes mild depression can be managed with support groups, counseling or other therapies. In other cases, antidepressants may be recommended — even during pregnancy.
- After your baby is born, your provider may recommend an early postpartum checkup to screen for symptoms of postpartum depression. The earlier it's found, the earlier treatment can begin. If you have a history of postpartum depression, your provider may recommend antidepressant treatment or talk therapy immediately after delivery. Most antidepressants are safe to take while breastfeeding.
- Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision DSM-5-TR. American Psychiatric Association; 2022. https://dsm.psychiatryonline.org. Accessed May 9, 2022.
- Postpartum depression. Office on Women's Health. https://www.womenshealth.gov/mental-health/mental-health-conditions/postpartum-depression. Accessed May 5, 2022.
- Depression among women. Centers for Disease Control and Prevention. https://www.cdc.gov/reproductivehealth/depression/index.htm. Accessed May 5, 2022.
- What is peripartum depression (formerly postpartum)? American Psychiatric Association. https://www.psychiatry.org/patients-families/postpartum-depression/what-is-postpartum-depression. Accessed Nov. 18, 2022.
- Viguera A. Postpartum unipolar depression: Epidemiology, clinical features, assessment, and diagnosis. https://www.uptodate.com/contents/search. Accessed Nov. 18, 2022.
- Viguera A. Mild to moderate postpartum unipolar major depression: Treatment. https://www.uptodate.com/contents/search. Accessed May 6, 2022.
- Viguera A. Severe postpartum unipolar major depression: Choosing treatment. https://www.uptodate.com/contents/search. Accessed May 6, 2022.
- Faden J, et al. Intravenous brexanolone for postpartum depression: What it is, how well does it work, and will it be used? Therapeutic Advances in Psychopharmacology. 2020; doi:10.1177/2045125320968658.
- FAQs. Postpartum depression. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/postpartum-depression. Accessed May 6, 2022.
- Suicide prevention. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/suicide-prevention. Accessed May 6, 2022.
- Postpartum depression. Merck Manual Professional Version. https://www.merckmanuals.com/professional/gynecology-and-obstetrics/postpartum-care-and-associated-disorders/postpartum-depression#. Accessed May 6, 2022.
- AskMayoExpert. Depression in pregnancy and postpartum. Mayo Clinic; 2022.
- American Academy of Pediatrics. Postpartum care of the mother. In: Guidelines for Perinatal Care. 8th ed. American Academy of Pediatrics; American College of Obstetricians and Gynecologists; 2017.
- Kumar SV, et al. Promoting postpartum mental health in fathers: Recommendations for nurse practitioners. American Journal of Men's Health. 2018; doi:10.1177/1557988317744712.
- Scarff JR. Postpartum depression in men. Innovations in Clinical Neuroscience. 2019;16:11.
- Bergink V, et al. Postpartum psychosis: Madness, mania, and melancholia in motherhood. American Journal of Psychiatry. 2016; doi:10.1176/appi.ajp.2016.16040454.
- Yogman M, et al. Fathers' roles in the care and development of their children: The role of pediatricians. Pediatrics. 2016; doi:10.1542/peds.2016-1128.
- FDA approves first treatment for post-partum depression. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-post-partum-depression. Accessed May 6, 2022.
- Deligiannidis KM, et al. Effect of zuranolone vs placebo in postpartum depression: A randomized clinical trial. JAMA Psychiatry. 2021; doi:10.1001/jamapsychiatry.2021.1559.
- Betcher KM (expert opinion). Mayo Clinic. May 10, 2022.
- 988 Suicide & Crisis Lifeline. https://988lifeline.org/. Accessed Nov. 18, 2022.
Associated Procedures
- Electroconvulsive therapy (ECT)
News from Mayo Clinic
- Mayo Clinic Minute: Postpartum depression is more than baby blues Feb. 02, 2023, 03:00 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Open access
- Published: 26 March 2024
Depression during pregnancy and associated factors among women in Ethiopia: a systematic review and meta-analysis
- Solomon Shitu Ayen 1 ,
- Abebaw Wasie Kasahun 2 &
- Amare Zewdie 2
BMC Pregnancy and Childbirth volume 24 , Article number: 220 ( 2024 ) Cite this article
655 Accesses
1 Citations
Metrics details
A Correction to this article was published on 23 April 2024
This article has been updated
Pregnancy is one of the most remarkable experiences in a woman’s life. Prenatal depression, characterized by stress and worry associated with pregnancy, can reach severe levels. On a global scale, mental and addictive disorders affect more than one billion people, causing 19% of years lived with disability. It is estimated that 25–35% of pregnant women experience depressive symptoms, with 20% meeting the diagnostic criteria for major depression.
A systematic review and meta-analysis were conducted to examine depression during pregnancy in Ethiopia. The search was conducted from March 1–31, 2023. Data extraction used Microsoft Excel, and analysis was performed using STATA version 17. The New Castle-Ottawa Scale quality assessment tool was employed to evaluate the methodological quality of included studies. The Cochrane Q test and I2 statistics were used to assess heterogeneity. A weighted inverse variance random-effects model estimated the pooled level of antenatal depression (APD). Publication bias was detected using a funnel plot and Begg’s and Egger’s tests.
Out of 350 studies searched, 18 were included in the analysis. The overall pooled prevalence of depression in Ethiopia was 27.85% (95% CI: 23.75–31.96). Harari region reported the highest prevalence (37.44%), while Amhara region had the lowest (23.10%). Factors significantly associated with depression included unplanned pregnancies, low social support, low income, previous history of depression, intimate partner violence, and history of abortion.
This systematic review and meta-analysis demonstrate that approximately one-quarter of pregnant women in Ethiopia experience depression during pregnancy. Unplanned pregnancy, low social support, low income, previous history of depression, history of abortion, and intimate partner violence are determinants of depression. To address this high prevalence, the Ethiopian government and stakeholders should develop policies that incorporate counseling during pregnancy follow-ups. Improving the quality of life for pregnant women is crucial for the well-being of families, communities, and the nation as a whole.
Peer Review reports
Introduction
Pregnancy is a significant life event for women, involving numerous physical, emotional, and social changes. This period can heighten the susceptibility of women and their fetuses to mental, physical, and psychological health issues. Among various mental health problems that occur during pregnancy, depression is the most prevalent psychiatric disorder affecting pregnant women. Depression during pregnancy, also known as antenatal depression (APD), is caused by anxiety and stress related to pregnancy and can stem from hormonal fluctuations, psychological disturbances, relationship issues, family or personal history of depression, life stress, low family support, unintended or unplanned pregnancies, and violence. If left untreated, APD can lead to adverse pregnancy outcomes, such as hypertension, low birth weight babies, preterm birth, and postnatal depression.
Depression is characterized by symptoms like excessive sleeping or insomnia, difficulty concentrating, forgetfulness, emotional instability, extreme irritability, fatigue, overeating or appetite loss, decreased interest in sex, feelings of guilt, sadness, suicidal thoughts, or death ideation. Globally, over one billion people suffer from mental or addictive disorders, accounting for 19% of all years lived with disability. Depression affects more than 350 million people across all age groups, with women being more vulnerable than men. Studies suggest that 25–35% of pregnant women experience depressive symptoms, and 20% of them meet the diagnostic criteria for major depression. The prevalence of APD varies in different countries, ranging from 20% in the United States to 30% in Finland and 35–50% in some lower and middle-income countries (LMICs).
In Africa, mental health issues among pregnant women and mothers have been extensively reported. APD is a critical public health concern in developing nations due to its intergenerational impact on mothers, infants, and children. In Ethiopia, the prevalence of APD and its associated factors differ across regions and time. Factors like older age, less education, being single, unemployment, low income, intimate partner violence, lack of social support, unplanned pregnancies, previous pregnancy loss, history of abortion, obstetric complications, and substance abuse contribute to APD.
Previous studies have provided inconsistent findings regarding APD prevalence and predictors at the national level, leaving policymakers with inconclusive information. This systematic review and meta-analysis aim to estimate the pooled prevalence of depression during pregnancy and its predictors among pregnant women in Ethiopia. By including recent studies and a larger sample of research articles (18 in total), this study offers a more comprehensive understanding of APD in Ethiopia.
Study design and setting
To ensure the originality and avoid redundancy of the research, the International Prospective Register of Systematic Reviews (PROSPERO) database was consulted. Upon checking the database ( http://www.library.ucsf.edu/ ), no published or ongoing research related to antenatal depression (APD) in Ethiopia was found. To proceed with the research, the protocol of the systematic review and meta-analysis was registered in the PROSPERO database with the ID CRD42023423700. The study adheres to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines to maintain the highest standards of research transparency and quality [ 1 ].
Data sources and search strategy
Articles included in the review were searched from the following databases: MEDLINE, Scopus, PubMed, Science Direct, Google Scholar, African Journals Online, and Web of Sciences to retrieve related articles. Search terms were formulated using PICO guidelines through online databases. Medical Subject Headings (MeSH) and key terms had been developed using different Boolean operators ‘AND’ and ‘OR’. Each database was searched from its start date to March 2023 by using the following words: Depression (Mesh), depress ∗ (all fields), “antepartum depression” (Mesh), “antenatal depression” (Mesh), Ethiopia(Mesh), “prenatal depression” (Mesh), “pregnancy and depression” (Mesh), mental health (all fields). Furthermore, librarians were consulted to find unpublished research works on our area of interest for this review. The literature search was conducted by two separate researchers (SSA and AWK) to avoid missing articles.
Eligibility criteria
In this systematic review and meta-analysis, the scope was to include all community and facility-based studies that reported the prevalence of antepartum depression (APD) and its determinants. This comprehensive approach aimed to ensure the study captured as much relevant information as possible. Both published and unpublished studies were considered to minimize potential publication bias. If multiple reports of the same study existed, the most recent and comprehensive study was chosen to ensure the analysis was based on the latest and most accurate data available.
The language restriction for the included articles was limited to English to facilitate the understanding and analysis of the data. This decision was made considering the limitations of the research team’s language capabilities and the widespread use of English in academic and scientific publications.
The timeframe for the search and inclusion of studies was set until March 30, 2023. This date allowed for a relatively recent and up-to-date analysis of the prevalence of APD and its associated factors in Ethiopia. As new research continues to emerge, future updates to the review may consider extending the search period or re-evaluating the study to incorporate more recent findings.
Exclusion criteria
To maintain the focus and accuracy of the systematic review and meta-analysis, several exclusion criteria were applied. Articles that did not report the outcome variables of interest, such as the prevalence of antepartum depression (APD) or its determinants were excluded. This ensured that only relevant data was considered in the analysis.
Additionally, certain study types were excluded to maintain the quality and reliability of the review. Systematic reviews, case series, commentaries, conference abstracts, letters to editors, technical reports, qualitative studies, and other opinion publications were not included, as they might not provide sufficient quantitative data or meet the required methodological standards.
To avoid double-counting studies, potential duplicates were also excluded. This involved removing studies conducted in the same area with similar findings during the same study period. This step ensured that the final analysis included a diverse and representative sample of studies, reducing the risk of overrepresentation or redundancy in the data.
Measurement of the outcome of interest
In this systematic review and meta-analysis, the primary focus was on determining the prevalence of antepartum depression (APD) in Ethiopia. The pooled prevalence was calculated as the primary outcome variable to provide an overall estimate of the proportion of affected individuals within the studied population.
The secondary outcome variable was to identify the factors associated with APD. To achieve this, a pooled Adjusted Odds Ratio (AOR) with 95% Confidence Intervals (CIs) was employed. This statistical measure allowed for the estimation of the strength and significance of the relationship between various determinants and the occurrence of APD.
To assess depressive symptoms in the studies, participants were typically asked specific questions. If they responded affirmatively (“Yes”) to these questions, they were considered to be experiencing depression. On the other hand, if they responded negatively (“NO”), they were not classified as depressed. This approach enabled the identification and analysis of individuals with potential APD within the studied population.
Data extraction strategy
To ensure a comprehensive and organized review process, several steps were taken to manage and analyze the collected data. Initially, duplicate articles were identified and removed using EndNote X8, citation management software. This helped to avoid any overlapping data or double-counting of studies in the analysis.
Data extraction was carried out using a Microsoft Excel spreadsheet, which was designed with a pre-settled and piloted format. The format was adapted from the Joanna Briggs Institute (JBI) data extraction format to ensure a standardized and thorough approach to data collection. The extracted information included:
The primary author’s name, publication year, study year, study design, study area, study setup, sample size, response rate, data collection technique, The proportion of APD, adjusted Odds Ratio (AOR) with their 95% confidence interval. To facilitate the data extraction process, multiple researchers (SS, AW, and AZ) worked separately, ensuring a more accurate and reliable data collection. They used 2 by-2 tables for the second objective of the review, which focused on identifying factors associated with APD.
Finally, the data analysis was performed using STATA software version 17. This statistical software allowed for the appropriate handling and interpretation of the collected data, contributing to a more robust and reliable systematic review and meta-analysis.
Quality assessment
The Newcastle-Ottawa Scale (NOS) was employed to assess the quality of the included studies in this systematic review. The NOS is a widely recognized and validated tool that evaluates the quality of non-randomized studies, such as cohort and case-control studies, in a structured manner. It focuses on three main components. The principal component, which evaluates the methodological quality of each primary study and is graded with five stars. The comparability of each study, which is graded from two stars and assesses the similarity of study participants and other factors that may influence the results. The outcomes and statistical analysis of each original study, graded from three stars and examining the adequacy of the reported results and statistical methods. The NOS uses a scoring system with a maximum score of 9 points. The quality of each study was rated based on the following scoring algorithms. A score of 7 points or more was considered “good” quality. A score between 2 and 6 points was considered “fair” quality. A score of 1 point indicated a “poor” quality study [ 2 ].
To ensure the validity and reliability of the systematic review results, only primary studies with fair to good quality were included in the analysis. The quality assessment was conducted by two authors (AW and SS), who evaluated the methodological quality, sample selection, sample size, comparability, and the outcome and statistical analysis of each original study.
Data processing and analysis
After importing the selected articles into a Microsoft Excel spreadsheet, the data was exported to STATA version 17 for statistical analysis. The choice of statistical methods depended on the nature of the data and the presence of heterogeneity between studies.
To estimate the pooled prevalence of APD, a weighted inverse variance random-effects model was used. This model takes into account the variability between studies and provides a more conservative estimate when heterogeneity is present. The presence of statistical heterogeneity across the included studies was determined using Higgins I2 statistics and the Cochran-Q test. The interpretation of I2 values was based on the following criteria. 75–100%: considerable heterogeneity, 50–90%: substantial heterogeneity, 30–60%: moderate heterogeneity, 0–40%: mild heterogeneity [ 3 ].
When studies showed significant heterogeneity, a random-effects model was used. In cases of homogeneous studies, a fixed-effects model was applied. To assess the possibility of publication bias, a Funnel plot and Eggers test were conducted. Publication bias was considered justified if the p -value was greater than 0.05. The results were presented in a forest plot format, which displays the pooled prevalence of APD with its 95% confidence interval (CI).
For the analysis of the adjusted odds ratio (AOR) from eligible studies, along with their 95% confidence intervals, the pooled AORs were computed using either a random or fixed-effect model, depending on the presence of heterogeneity. Finally, forest plots were used to visually represent the pooled estimates for APD and its determinants, along with their respective 95% confidence intervals, allowing for a comprehensive understanding of the relationship between these factors and APD.
Characteristics of included studies
In total, 350 studies were initially identified from various search engines, including 341 from the specified data sets and 9 from other sources. After removing duplicates, 63 studies were excluded, leaving 287 studies. Among these, 201 studies were further excluded based on their titles and abstracts, not meeting the inclusion criteria.
Subsequently, 68 studies were excluded after reviewing their full texts due to insufficient data or not satisfying the predefined criteria. Finally, 18 studies were deemed eligible for inclusion in the analysis (Fig. 1 ). These studies were conducted across different regions of Ethiopia, with four studies each in the South Nations, Nationalities, and Peoples’ Region (SNNPR) and Oromia, three studies each in Amhara and Addis Ababa, two studies in Tigray, and one study in each of Somali and Harari (Table 1 ). The population exposure and outcome (PEO) of the study participants are demonstrated in Table 2 , providing a clear overview of the study population and the outcomes assessed in the included studies.
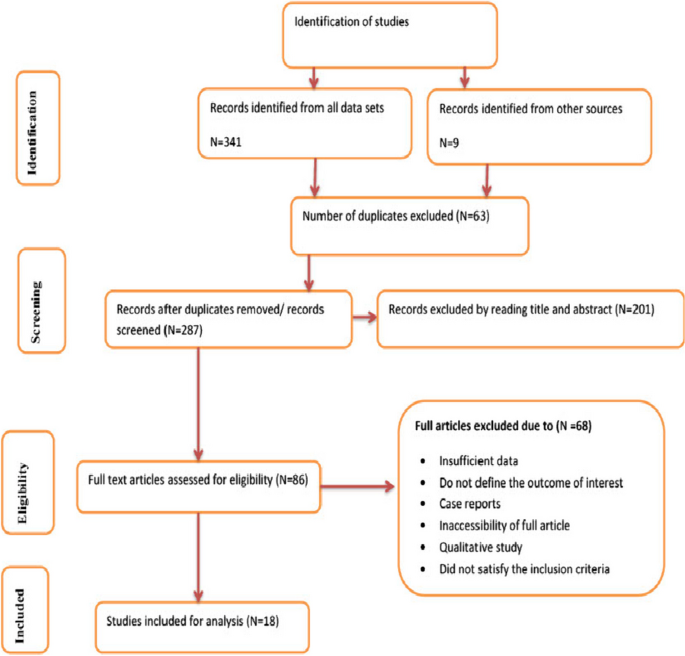
Flow chart of selection for systematic review and meta-analysis on DDP and associated factors in Ethiopia, 2023
Sensitivity analysis
The sensitivity analysis, performed using the random-effects model, aimed to assess the influence of individual studies on the overall estimate of antepartum depression (APD) prevalence in Ethiopia. The results of this sensitivity analysis, presented in Fig. 2 , indicate that no single study significantly impacted or unduly influenced the overall estimate of APD prevalence in Ethiopia. This finding suggests that the results are robust and stable, as the overall prevalence estimate remains consistent even when specific studies are removed from the analysis.
Sensitivity test of studies included in systematic review and meta-analysis on DDP and associated factors in Ethiopia, 2023
Publication bias
To further evaluate the possibility of publication bias, funnel plots were employed to visually inspect the asymmetry of the distribution of study effect sizes against their standard errors. An inverted funnel shape that appears symmetrical suggests a low likelihood of publication bias. In this case, the funnel plot displayed a large, symmetrical inverted funnel shape (Fig. 3 ), indicating that the chance of publication bias is minimal.
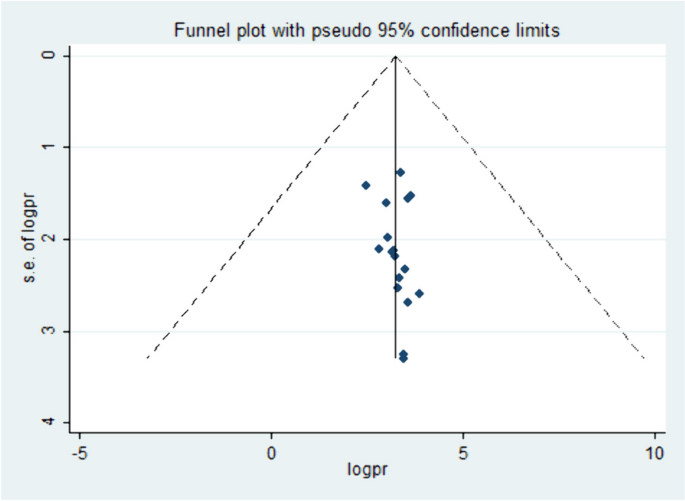
Funnel plot showing the symmetric distribution of articles on DDP in Ethiopia, 2023
In addition to the visual assessment, statistical methods such as Egger’s and Begg’s tests were used to provide supplementary evidence. A p -value less than 0.05 are generally considered statistically significant, and in this context, it suggests that there is no significant publication bias present in the included studies, supporting the visual assessment findings.
The pooled prevalence of APD in Ethiopia
Antepartum depression in Ethiopia varied across the studies, demonstrating significant heterogeneity. The heterogeneity was quite high, with an I2 value of 95.0% and a statistically significant P -value less than 0.000. This high level of heterogeneity indicates that there are substantial differences in the study results that cannot be explained by chance alone. Despite this heterogeneity, the overall pooled prevalence of APD in Ethiopia was estimated to be 27.85% (95% confidence interval: 23.75–31.96). This combined prevalence figure is summarized using a forest plot (Fig. 4 ), which visually represents the individual study results and their contribution to the overall prevalence estimate.
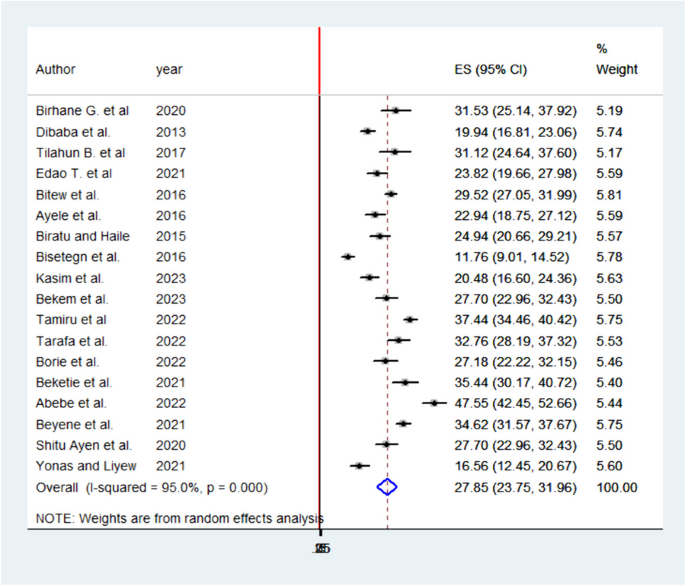
Pooled prevalence systematic review and meta-analysis on DDP and associated factors in Ethiopia, 2023
The high heterogeneity among studies highlights the importance of considering the context and methodology of each individual study when interpreting the overall prevalence estimate. Further research and investigation may be required to understand the factors contributing to this variability and to develop targeted strategies for managing and preventing APD in Ethiopia.
Subgroup analyses of APD in Ethiopia
Subgroup analyses were conducted by the study region. Accordingly, the highest prevalence of APD was reported in Harari and lowest in Amhara regions with prevalence and I 2 of 37.44% (95% CI: 34.46–40.42) I 2 95% P = 0.000 and 23.10 (95% CI: 8.56–37.64) I 2 98.3% P = 0.000 respectively (Fig. 5 ).
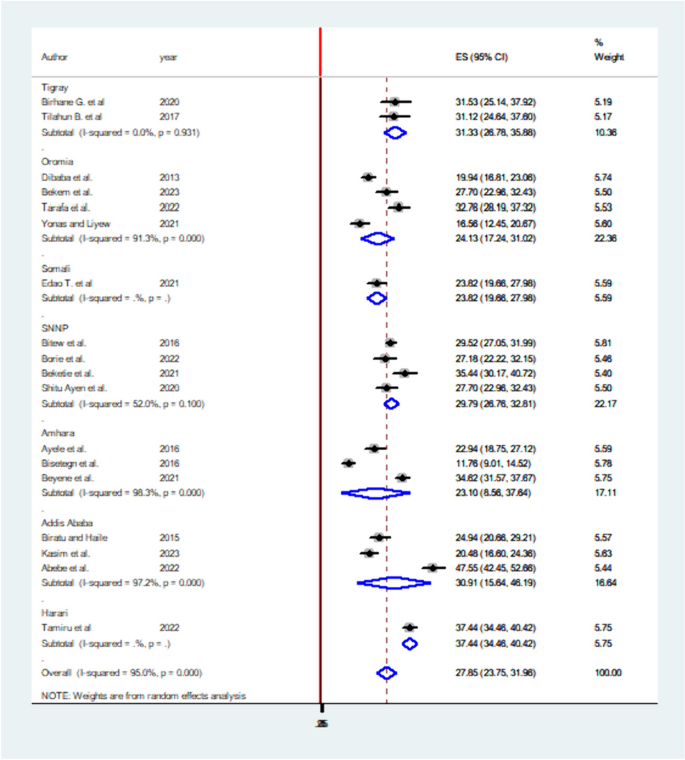
Subgroup analysis of systematic review and meta-analysis on DDP and associated factors in Ethiopia, 2023
Factors associated with APD in Ethiopia
Six significant factors have been identified in this systematic review and meta-analysis to be associated with antepartum depression (APD) in Ethiopia. These factors are unplanned pregnancy, social support, history of abortion, intimate partner violence, low income, and previous history of depression. Each factor’s association with APD is quantified using adjusted odds ratios (AOR) and their respective confidence intervals.
Unplanned pregnancy: Women experiencing unplanned pregnancies have a 2.47 times higher likelihood of developing APD compared to those with planned pregnancies (AOR: 2.47, 95% CI: 1.92–3.19). Low social support and income: Pregnant mothers with low social support and income are 2 times more likely to develop APD than their counterparts (AOR: 2.06, 95% CI: 1.44–2.94 for low social support; AOR: 2.13, 95% CI: 1.54–2.91 for low income). Previous history of depression: Women with a history of depression have a 3 times higher likelihood of developing APD (AOR: 3.49, 95% CI: 2.40–5.08). History of intimate partner violence: Women with a history of intimate partner violence are 2.7 times more likely to develop APD than those without such history (AOR: 2.71, 95% CI: 2.07–3.55). History of abortion: Women with a history of abortion have a 2 times higher likelihood of developing APD compared to those without (AOR: 2.12, 95% CI: 1.392–3.25).
These findings, summarized in Table 3 , provide valuable insights into the potential risk factors associated with APD in Ethiopia. Addressing these factors and implementing targeted interventions could help reduce the prevalence and impact of APD on affected women in the country.
This systemic review and meta-analysis provide valuable insights into the prevalence and associated factors of antepartum depression (APD) in Ethiopia. The pooled prevalence of APD in Ethiopia is 27.85% (95% CI: 23.75–31.96), which is in line with studies conducted in Nigeria, Ghana, and Africa as a whole [ 14 , 15 , 16 ], but higher than studies in Brazil, Nepal, South Africa, and rural Ghana [ 17 , 18 , 19 , 20 , 21 , 22 , 23 ]. The prevalence in Ethiopia might be higher due to differences in study periods, populations, and areas. However, the prevalence of this systemic review and meta-analysis was lower than in studies done in Tanzania, Côte d’Ivoire, Kenya [ 15 , 24 , 25 ] the reason might be due to most of the studies are single area findings which may not be strong too as compared to this systemic review which is pooled prevalence. Also, it may be due to the study period, study population, and study area differences.
Sub-group analysis reveals the highest prevalence in the Harari region (37.44%) and the lowest in the Amhara region (23.1%). Factors significantly associated with APD include unplanned pregnancy, social support, history of abortion, intimate partner violence, low income, and previous history of depression. These associations are quantified using adjusted odds ratios (AOR) and their respective confidence intervals.
Low social support and low income are associated with a twofold increased likelihood of developing APD. This finding is consistent with studies conducted in Nepal, Tanzania, Nigeria, South Africa, and systemic reviews in Africa. Women with unplanned pregnancies have a 2.47 times higher likelihood of developing APD, possibly due to economic stress and concerns related to unplanned pregnancies in developing countries [ 18 , 19 , 20 , 21 , 22 , 24 ].
In this systemic review and meta-analysis, women with low income were two times more likely to develop APD than women with good income AOR 2.13; 95% CI; 1.54–2.91. The finding was in line with studies conducted in Tanzania, Nigeria, and systemic reviews in Africa [ 16 , 21 , 24 ]. This may be due to a family with poor income may be related to the economic problem and she became stressed thinking of how can she give care for the newborn and the family.
Women with a history of unplanned pregnancy were 2.47 times more likely to develop APD than women with planned pregnancy AOR 2.47; 95% CI; 1.92–3.19. The reason may be in developing countries planning to get pregnant will be associated with the economy of the household so women with unplanned pregnancies may be stressed by thinking of economic problems after birth which may lead to depressive conditions [ 21 ].
A previous history of depression has been associated with APD in this review. Women with a previous history of depression had 3.5 times more likely to develop APD than their counterparts AOR 3.49; 95% CI; 2.40–5.08. The finding was consistent with studies done in Brazil and South Africa [ 17 , 20 ]. A possible explanation might be scientifically the reoccurrence of APD is most likely in consecutive pregnancies unless possible risk factors are avoided [ 20 ].
The probability of the women developing APD was 2.71 times more likely with intimate partner violence as compared to their counterparts AOR 2.71; 95% CI; 2.07–3.55. The finding was supported by studies in Kenya, Nigeria, and South Africa. The possible explanation might be as the name indicates violence is violating the rights of the person physically, sexually, or emotionally. Thus, women with violence might be more likely to develop depression. It may also be a partner who violates the rights of the woman may have poor educational conditions and can’t respect others [ 14 , 19 , 25 ].
Women with a history of abortion were two times more likely to develop depression during pregnancy than their counterparts AOR 2.12; 95% CI; 1.39–3.25. The possible reason might be women who experience abortion may be stressed due to fear of repeated abortion and loss of their baby. The finding was supported by a study done in Nigeria [ 21 ].
These findings can help guide interventions and policies to address the factors associated with APD in Ethiopia, ultimately reducing its prevalence and impact on affected women.
Strengths and limitations of the study
The study presents several strengths and limitations. One of the main strengths lies in the comprehensive search strategy employed to retrieve related articles. By searching different databases and following the PRISMA flow charts strictly, the study ensures a systematic and thorough approach to identifying relevant studies. Additionally, including studies published over different years allows for an analysis of potential trends in antepartum depression (APD) during pregnancy in Ethiopia.
However, there are some limitations to consider. Firstly, the study is limited to English-language articles, which might have resulted in excluding relevant studies published in other languages. This could potentially affect the generalizability and comprehensiveness of the findings. Secondly, the absence of studies from some regions of Ethiopia might raise questions about the generalizability of the results across the entire country. This could be due to various factors, such as regional differences in access to healthcare, cultural practices, or research focus. To address these limitations, future studies could consider expanding their search to include non-English articles and aim to include studies from all regions of Ethiopia to enhance the generalizability of their findings.
The findings of this systemic review and meta-analysis highlight the significant prevalence of antepartum depression (APD) in Ethiopia, affecting one-quarter of pregnant women. Addressing the determinant factors of depression, such as unplanned pregnancies, low social support, low income, previous history of depression, history of abortion, and intimate partner violence, is crucial for reducing the prevalence of APD.
To address this issue, the government of Ethiopia and other stakeholders should consider incorporating depression counseling during antenatal care (ANC) follow-ups. By providing information and support to pregnant women, they can better understand and cope with potential risk factors and seek appropriate help when needed. This approach not only improves the well-being of individual women but also contributes to the overall well-being of their families, communities, and the nation.
Incorporating depression awareness and prevention measures into ANC services can help create a supportive environment for pregnant women, empowering them to make informed decisions and seek assistance when facing challenges. This holistic approach to maternal health can lead to better mental health outcomes for pregnant women, ultimately benefiting the entire society.
Availability of data and materials
The result of this systematic review and meta-analysis was extracted from the data gathered and analyzed based on the stated methods and materials. All the relevant data are within the paper.
Change history
23 april 2024.
A Correction to this paper has been published: https://doi.org/10.1186/s12884-024-06506-y
Abbreviations
Adjusted Odds Ratio
Ante Partum Depression
Depression during Pregnancy
Joanna Briggs Institute
Lower and Middle-Income Countries
Newcastle-Ottawa Scale
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
South Nations, Nationalities, and People Region
World Health Organization
Prisma transparent reporting of systematic reviews and meta-analyses. http://www.prisma-statement.org/PRISMAStatement/Checklist.aspx . Cited 2021 Nov 18.
ells GA, O’Connell BSD, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
The Cochrane Collaboration and John Wiley & Sons Ltd, Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews. England: Wiley; 2008.
Google Scholar
Dibaba Y, Fantahun M, Hindin MJ. The association of unwanted pregnancy and social support with depressive symptoms in pregnancy: evidence from rural Southwestern Ethiopia. BMC Pregn Childb. 2013;13(1):1–8.
Article Google Scholar
Bitew T, Hanlon C, Kebede E, Medhin G, Fekadu A. Antenatal depressive symptoms and maternal health care utilization: a population-based study of pregnant women in Ethiopia. BMC Pregn Childb. 2016;16(1):1–1.
Ayele TA, Azale T, Alemu K, Abdissa Z, Mulat H, Fekadu A. Prevalence and associated factors of antenatal depression among women attending antenatal care service at Gondar University Hospital, Northwest Ethiopia. Plos One. 2016;11(5):e0155125. https://doi.org/10.1371/journal.pone.0155125 .
Article CAS PubMed PubMed Central Google Scholar
Biratu A, Haile D. Prevalence of antenatal depression and associated factors among pregnant women in Addis Ababa, Ethiopia: a cross-sectional study. Reprod Health. 2015;12(1):1–8.
Bisetegn TA, Mihretie G, Muche T. Prevalence and predictors of depression among pregnantwomen in Debretabor Town, Northwest Ethiopia. Plos One. 2016;11(9):e0161108. https://doi.org/10.1371/journal.pone.0161108 .
Tamiru D, Misgana T, Tariku M, Tesfaye D, Alemu D, Weldesenbet AB, Gebremichael B, Theresa M. Prevalence and associated factors of common mental disorders among pregnant mothers in rural eastern Ethiopia. Front Psychiatry. 2022;13:843984.
Article PubMed PubMed Central Google Scholar
Tarafa H, Alemayehu Y, Nigussie M. Factors associated with pregnancy-related anxiety among pregnant women attending antenatal care follow-up at Bedelle General Hospital and Metu Karl comprehensive specialized hospital Southwest Ethiopia. Front Psychiatry. 2022;2133:938277.
Beketie ED, Kahsay HB, Nigussie FG, Tafese WT. Magnitude and associated factors of antenatal depression among mothers attending antenatal care in Arba Minch town, Ethiopia, 2018. Plos One. 2021;16(12):e0260691. https://doi.org/10.1371/journal.pone.0260691 .
Abebe W, Gebremariam M, Molla M, Teferra S, Wissow L, Ruff A. Prevalence of depression among HIV-positive pregnant women and its association with adherence to antiretroviral therapy in Addis Ababa, Ethiopia. Plos One. 2022;17(1):e0262638. https://doi.org/10.1371/journal.pone.0262638 .
Beyene GM, Azale T, Gelaye KA, Ayele TA. The effect of antenatal depression on birth weight among newborns in South Gondar Zone, Northwest Ethiopia: a population-based prospective cohort study. Arch Public Health. 2021;79(1):1–2.
Thompson O, Ajayi I. Prevalence of antenatal depression and associated risk factors among pregnant women attending antenatal clinics in Abeokuta North Local Government Area. Nigeria Depress Res Treat. 2016;2016:4518979. https://doi.org/10.1155/2016/4518979 . (Epub 2016 Aug 18. PMID: 27635258; PMCID: PMC5007324).
Article PubMed Google Scholar
Bindt C, Appiah-Poku J, Te Bonle M, Schoppen S, Feldt T, Barkmann C, Koffi M, Baum J, Nguah SB, Tagbor H, Guo N, N’Goran E, Ehrhardt S, International CDS Study Group. Antepartum depression and anxiety associated with disability in African women: cross-sectional results from the CDS study in Ghana and Côte d’Ivoire. PLoS One. 2012;7(10):e48396. https://doi.org/10.1371/journal.pone.0048396 . (PMID: 23110236; PMCID: PMC3482210).
Dadi AF, Wolde HF, Baraki AG, Akalu TY. Epidemiology of antenatal depression in Africa: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2020;20(1):251. https://doi.org/10.1186/s12884-020-02929-5 . (PMID: 32345263; PMCID: PMC7189721).
Coll CVN, da Silveira MF, Bassani DG, Netsi E, Wehrmeister FC, Barros FC, Stein A. Antenatal depressive symptoms among pregnant women: evidence from a Southern Brazilian population-based cohort study. J Affect Disord. 2017;209:140–6 (Epub 2016 Nov 26. PMID: 27914247; PMCID: PMC5282400).
Joshi D, Shrestha S, Shrestha N. Understanding the antepartum depressive symptoms and its risk factors among the pregnant women visiting public health facilities of Nepal. PLoS ONE. 2019;14(4):e0214992 PMID: 30947251; PMCID: PMC6448918. https://doi.org/10.1371/journal.pone.0214992 .
Govender D, Naidoo S, Taylor M. Antenatal and postpartum depression: prevalence and associated risk factors among adolescents’ in KwaZulu-Natal, South Africa. Depress Res Treat. 2020;2020:5364521. https://doi.org/10.1155/2020/5364521 . (PMID: 32411457; PMCID: PMC7204344).
Sulyman D, Aminu MB, Ayanda KA, Dattijo LM. Antepartum depression among women attending antenatal clinic in a Nigerian teaching hospital. Niger J Med. 2021;30:556–60.
Redinger S, Pearson RM, Houle B, Norris SA, Rochat TJ. Antenatal depression and anxiety across pregnancy in urban South Africa. J Affect Disord. 2020;277:296–305. https://doi.org/10.1016/j.jad.2020.08.010 . (Epub 2020 Aug 13. PMID: 32858310).
Adeoye IA, Sogbesan A, Esan O. Prevalence, associated factors and perinatal outcomes of antepartum depression in Ibadan Nigeria. BMC Pregnancy Childbirth. 2022;22(1):219. https://doi.org/10.1186/s12884-022-04549-7 . (PMID: 35303804; PMCID: PMC8933907).
Weobong B, ten Asbroek AHA, Soremekun S, Manu AA, Owusu-Agyei S, et al. Association of antenatal depression with adverse consequences for the mother and newborn in Rural Ghana: findings from the DON population-based cohort study. PLoS ONE. 2014;9(12): e116333. https://doi.org/10.1371/journal.pone.0116333 .
Rwakarema M, Premji SS, Nyanza EC, Riziki P, Palacios-Derflingher L. Antenatal depression is associated with pregnancy-related anxiety, partner relations, and wealth in women in Northern Tanzania: a cross-sectional study. BMC Womens Health. 2015;15:68. https://doi.org/10.1186/s12905-015-0225-y . (PMID: 26329331; PMCID: PMC4557331).
Tele A, Kathono J, Mwaniga S, Nyongesa V, Yator O, Gachuno O, Wamalwa D, Amugune B, Cuijpers P, Saxena S, McKay M, Carvajal L, Lai J, Huang KY, Merali Z, Kumar M. Prevalence and risk factors associated with depression in pregnant adolescents in Nairobi, Kenya. J Affect Disord Rep. 2022;10:100424 (Epub 2022 Sep 19. PMID: 36970124; PMCID: PMC10038142).
Download references
Acknowledgements
We would like to thank all authors of the primary studies which are included in this systematic review and meta-analysis.
Institutional review board statement
Not applicable.
This systematic review and meta-analysis used and analyzed information obtained from pre-existing studies.
There is no funder for this systematic meta-analysis.
Author information
Authors and affiliations.
Department of Midwifery, College of Medicine and Health Science, Wolkite University, Wolkite, 07, Ethiopia
Solomon Shitu Ayen
Department of Public Health, College of Medicine and Health Science, Wolkite University, Wolkite, Ethiopia
Abebaw Wasie Kasahun & Amare Zewdie
You can also search for this author in PubMed Google Scholar
Contributions
As per the guidelines for authorship, all authors of this study have made significant contributions to the work reported and have fulfilled the following criteria. Conception and design, data extraction and analysis, study design and execution, acquisition of data, interpretation of results, drafting, revising, and critically reviewing the article, final approval of the version to be published, agreement to be accountable for all aspects of the work, taking responsibility for the integrity and accuracy of the research and its presentation. By fulfilling these criteria, all authors have demonstrated their active involvement in various aspects of the research and manuscript preparation, ensuring the quality and reliability of the study's findings.
Corresponding author
Correspondence to Solomon Shitu Ayen .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
All authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: "it was noted that due to a typesetting error the figure legends were paired incorrectly. The figure legends for Figs. 2, 4 and 5 were wrongly given as captions for Figs. 5, 2 and 4 respectively. Also, there are some type errors in the main text submitted which need some modifications. Incorrect and correct data are indicate in bold."
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ayen, S.S., Kasahun, A.W. & Zewdie, A. Depression during pregnancy and associated factors among women in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth 24 , 220 (2024). https://doi.org/10.1186/s12884-024-06409-y
Download citation
Received : 23 October 2023
Accepted : 11 March 2024
Published : 26 March 2024
DOI : https://doi.org/10.1186/s12884-024-06409-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Depression during pregnancy
- Pregnant women
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
The recent meta-analysis on depression in pregnancy, cited earlier, evaluated 20 studies and found that high depressive symptoms were associated with 1.4 to 2.9 times higher risk of LBW in undeveloped countries, ... Papers of particular interest, published within the annual period of review, have been highlighted as: of special interest of ...
Pregnancy can be a time of joy — and stress. Research suggests that about 7% of pregnant women experience depression during pregnancy. Rates might be higher in low and middle income countries. Depression, a mood disorder that causes a persistent feeling of sadness and loss of interest, is the most common mood disorder in the general population.
A new study of more than 7,000 pregnant women found that depression was associated with an 82 percent increased risk of extremely premature birth and a 28 percent increased risk of low birth weight, for instance (Venkatesh et al., Obstetrics and Gynecology , 2016). Yet many pregnant women are reluctant to take antidepressants—for good reason.
Rest as much as you can. Pregnancy fatigue can intensify the mood swings you may be having, so make sure you're getting enough rest. Go to bed early, sleep late, and take naps when you can. Spend time outside. Being outside in nature has been proven to reduce stress and depression symptoms. Opens a new window.
Signs of depression during pregnancy can include: Having recurrent thoughts of death or suicide. Having a depressed mood for most of the day, nearly early day, for the last two weeks. Feeling guilty, hopeless or worthless. Having difficulty thinking, concentrating or making decisions. Losing interest or pleasure in most activities during the ...
Introduction. Depression and anxiety are significant contributors to maternal perinatal morbidity and a range of negative child outcomes. This systematic review and meta-analysis aimed to review and assess the diagnostic test accuracy of selected screening tools (Edinburgh Postnatal Depression Scale [EPDS], EPDS-3A, Patient Health Questionnaire [PHQ-9]-, PHQ-2, Matthey Generic Mood Question ...
Thinking about death or suicide is a sign of depression. If you are in crisis or feel like you want to harm yourself or others, call 988 right away. 988 is the Suicide & Crisis Lifeline, which offers free support and resources.Read the Resources section for other support options, including more helplines you can text or call and online pregnancy support groups.
As many as one in seven women experience depression during pregnancy or in the year after giving birth. Now, for the first time, a national panel of health experts says there is a way to prevent it.
Although the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) includes the specifier "with peripartum onset" for a diagnosis of major depressive disorder (MDD), it does not acknowledge postpartum depression (PPD) with an onset beyond 4 weeks (American Psychiatric Association [APA], 2013).The revisions however from the DSM-IV to the DSM-5 now account for MDD during pregnancy ...
Dr. Neha Hudepohl: So, women who have depression or anxiety during pregnancy present very similarly to depression and anxiety at other times in a woman's life cycle. So, that can often present with sadness or loss of interest or pleasure in things that are normally pleasurable. It can present as, you know, detachment or disengagement from ...
Depression in pregnancy is an illness that can be treated and managed; however, it is important to seek out help and support first. What is depression in pregnancy? Depression during pregnancy, or antepartum depression, is a mood disorder just like clinical depression. Mood disorders are biological illnesses that involve changes in brain chemistry.
Postpartum depression: The birth of a baby can trigger a jumble of powerful emotions, from excitement and joy to fear and anxiety. But it can also result in something you might not expect — depression.
Pregnancy is one of the most remarkable experiences in a woman's life. Prenatal depression, characterized by stress and worry associated with pregnancy, can reach severe levels. On a global scale, mental and addictive disorders affect more than one billion people, causing 19% of years lived with disability. It is estimated that 25-35% of pregnant women experience depressive symptoms, with ...
Activity During Pregnancy and Postpartum Depression. Studies have shown that women's mood and cardiorespiratory fitness improve when they engage in moderate-intensity physical activity in the weeks and months after giving birth to a child. We will write. a custom essay specifically for you by our professional experts.
Perinatal depression refers to depression occurring during pregnancy or after childbirth. The use of the term perinatal recognizes that depression associated with having a baby often begins during pregnancy. (Postpartum depression refers to depression experienced after childbirth.) Perinatal depression is a serious, but treatable medical ...
According to the Cleveland Clinic Journal of Medicine, 1 in 7-10 women will develop a depressive disorder during pregnancy. For reference, 1 in 5-8 women will experience depression postpartum ...
ABSTRACT. Depression is a mood disorder which can affect 1 in every 4 women at some point of life even during pregnancy. Depression is most often not properly diagnosed during pregnancy as it is assumed by people to be just another type of imbalance in hormones. But this assumption can be very dangerous to the mother and the foetus (1).
Among the various pregnancy complications that we know of, postpartum depression is one of the most common with as many as 10-15% of women having been diagnosed (Hantsoo, et al. 2014). While suffering from postpartum depression is undoubtedly difficult, it is important for one to know the signs, symptoms, complications, diagnoses and treatment ...
Essay Examples on Postpartum Depression. Essay examples. Essay topics. 7 essay samples found. Sort & filter. 1 Postpartum Depression and Anxiety Disorders in Women . 4 pages / 1783 words . Pregnancy is a process of bringing a new life into the world. In most situations it is perceived as a joyous time filled with happiness, excitement, and ...
The findings suggest that gut bacteria contribute to allopregnanolone production during pregnancy. Researchers have linked low levels of allopregnanolone to postpartum depression and other mood and psychiatric disorders, and allopregnanolone is used as an FDA-approved drug known as brexanolone to treat postpartum depression.
Causes. Prognosis. Coping. Postpartum depression (PPD) is a type of depression that occurs after giving birth. It's more serious than the "baby blues" as it can interfere with a new mother's ability to function. It's important for new mothers and family members to be on the lookout for signs of postpartum depression.
11/16/10. Depression and Pregnancy 2. For most women the period of growing bellies and growing anticipations is a joyful and exciting time and for others this time may harbor doubt, fear, and depression. "As many as 1 out of 5 women have symptoms of depression during pregnancy. For some women, those symptoms are severe.
It turns out flatulence can serve a purpose beyond being uncomfortable or funny: Gas released by some gut bacteria stimulates other gut bacteria to produce a hormone involved in pregnancy and in an FDA-approved treatment for postpartum depression, according to new research led by Harvard Medical School scientists. The work shows how gut ...
Several aspects of pregnancy and the postpartum period are hypothesized to contribute to the onset of postpartum psychosis. These risk factors include: Primiparity. Being a first-time mother ...
This essay about the Emergency Banking Act of 1933 explores how this pivotal legislation reshaped American finance during the Great Depression. Delving into its enactment and impact, it highlights how the Act stabilized the banking sector, paved the way for regulatory reforms like Glass-Steagall, and established the FDIC.
It is shown that current IUD use 'protects' against interstitial pregnancies, which are the most difficult to manage, and shows that subsequent fertility tends to be higher in women with distal EP. Expand. 651. PDF. Semantic Scholar extracted view of "Spontaneous diaphragm rupture caused by abdominal pregnancy: A case report." by Yi Cao et al.
Essay Example: Bonnie Parker and Clyde Barrow stand as enduring enigmas in the annals of American criminology, their appellations forever enshrined in the folklore of the Depression era. The saga of Bonnie and Clyde epitomizes a narrative steeped in crime, ardor, and the relentless pursuit by. Writing Service; Essay Samples.