- 3-D Printing
- 3T Magnetic Resonance Imaging
- AI / Machine Learning
- Clinical Trial
- Consumer Product
- Forge Alumni
- Imaging Technology
- Intellectual Property
- International
- Internet of Things
- Manufacturing
- McMaster Innovation Park
- medical device design
- Personal Protective Equipment
- Positron Emission Tomography
- Procurement
- product design
- Product Development
- product strategy
- product validation
- products strategy
- Quality Control
- Radiopharmaceuticals
- Regulatory Support
- Research Imaging
- SOPHIE Alumni
- Synapse Competition
- Synapse Consortium Partner
- Testing & Evaluation

🡄 back
The Population Health Research Institute (PHRI) is Canada’s premiere global health research institute and a world leader in large clinical trials and population studies. Through international collaboration and innovation, PHRI explores CVD, diabetes, kidney and lung diseases, brain health, cancer and more.
Originally formed with a focus on cardiovascular disease (CVD) and diabetes, PHRI’s research areas have broadened to include population genomics, perioperative medicine, stroke, thrombosis, CV surgery, renal, obesity, childhood obesity, bone and trauma and implementation science.
Over the years, the PHRI has developed unparalleled expertise in epidemiology, population health and clinical trials. Examining biological and genetic determinants of health, as well as social, environmental and policy factors, the research focuses on the prevention of cardiovascular disease, diabetes and other common conditions. PHRI’s capacity to conduct several international studies concurrently, with tens of thousands of participants in each, is a capability very few organizations in the world can match. To date, PHRI studies have enrolled almost 1,500,000 participants worldwide in 102 countries.
A core strength of the PHRI is the multidisciplinary team of world-class scientists and research support teams. The environment promotes collaboration and a multifaceted approach which allows researchers to capitalize on the wealth of collective knowledge as they each bring areas of expertise to a single study.
- Contract, Professional and Other Services
- Research Centres and Institutes
- Research Institutes & Academic Institutions
- Testing & Medical Laboratories
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Am J Public Health
- v.93(3); Mar 2003
What Is Population Health?
David kindig.
David Kindig is with the Department of Population Health Sciences, University of Wisconsin—Madison School of Medicine, Madison. Greg Stoddart is with the Department of Clinical Epidemiology and Biostatistics, McMaster University Health Science Centre, Hamilton, Ontario.
Greg Stoddart
Population health is a relatively new term that has not yet been precisely defined. Is it a concept of health or a field of study of health determinants?
We propose that the definition be “the health outcomes of a group of individuals, including the distribution of such outcomes within the group,” and we argue that the field of population health includes health outcomes, patterns of health determinants, and policies and interventions that link these two.
We present a rationale for this definition and note its differentiation from public health, health promotion, and social epidemiology. We invite critiques and discussion that may lead to some consensus on this emerging concept.
ALTHOUGH THE TERM “population health” has been much more commonly used in Canada than in the United States, a precise definition has not been agreed upon even in Canada, where the concept it denotes has gained some prominence. Probably the most influential contribution to the development of the population health approach is Evans, Barer, and Marmor’s Why Are Some People Healthy and Others Not? The Determinants of Health of Populations , 1 which grew out of the work of the Population Health Program of the Canadian Institute for Advanced Research. No concise definition of the term appears in this volume, although its authors state the concept’s “linking thread [to be] the common focus on trying to understand the determinants of health of populations.” 1(p29)
The idea that population health is a field of study or a research approach focused on determinants seems to have evolved from this work. Early discussions at the Canadian Institute for Advanced Research also considered the definition and measurement of health and the processes of health policymaking, but the dominant emphasis evolved to the determinants themselves, particularly the nonmedical determinants. John Frank, the scientific director of the recently created Canadian Institute of Population and Public Health, has similarly called population health “a newer research strategy for understanding the health of populations.” 2 T. K. Young’s recent book Population Health also tends in this direction; he states that in Canada and the United Kingdom in the 1990s, the term has taken on the connotation of a “conceptual framework for thinking about why some populations are healthier than others as well as the policy development, research agenda, and resource allocation that flow from this framework.” 3(p4)
However, Young also indicates that in the past, the term has been used as a “less cumbersome substitute for the health of populations,” which is of course its literal meaning. Evans and Stoddart, while supporting an emphasis on “understanding of the determinants of population health,” have also stated, however, that “different concepts [of health] are neither right or wrong, they simply have different purposes and applications. . . . [W]hatever the level of definition of health being employed, however, it is important to distinguish this from the question of the determinants of that definition of health.” 1(p28) The Health Promotion and Programs Branch of Health Canada has recently stated that “the overall goal of a population health approach is to maintain and improve the health of the entire population and to reduce inequalities in health between population groups.” 4(p1) They indicate that one guiding principle of a population health approach is “an increased focus on health outcomes (as opposed to inputs, processes, and products) and on determining the degree of change that can actually be attributed to our work.” (p11)
Dunn and Hayes, quoting the definition of the Canadian Federal/Provincial/Territorial Advisory Committee on Population Health, write that “population health refers to the health of a population as measured by health status indicators and as influenced by social, economic, and physical environments, personal health practices, individual capacity and coping skills, human biology, early childhood development, and health services. As an approach, population health focuses on interrelated conditions and factors that influence the health of populations over the life course, identifies systematic variations in their patterns of occurrence, and applies the resulting knowledge to develop and implement policies and actions to improve the health and well being of those populations.” 5(p57) Kindig has suggested a similarly broad definition: population health is “the aggregate health outcome of health adjusted life expectancy (quantity and quality) of a group of individuals, in an economic framework that balances the relative marginal returns from the multiple determinants of health.” 6(p47) This definition proposes a specific unit of measure of population health and also includes consideration of the relative cost-effectiveness of resource allocation to multiple determinants.
Recently, even in the United States, the term is being more widely used, but often without clarification of its meaning and definition. While this development might be seen as a useful movement in a new and positive direction, increased use without precision of meaning could threaten to render the term more confusing than helpful, as may already be the case with “community health” or “quality of medical care.” For this reason, we propose a definition that may have a more precise meaning for policymakers and academics alike; our purpose is to stimulate active critiques and debate that may lead to further clarification and uniformity of use.
DEFINITION AND CONCEPT
As indicated above, the primary tension or confusion at present seems to be between defining population health as a field of study of health determinants or as a concept of health. The Group Health Community Foundation has recently stated that “some observers see population health as a new term that highlights the influential role of social and economic forces in combination with biological and environmental factors, that shape the health of entire populations . . . others interpret population health primarily as a goal—a goal of achieving measurable improvements in the health of a defined population.” 7(p7)
We think that there are 3 general possibilities: population health (a) is only concerned with the independent variables (the multiple determinants), (b) is only concerned with the dependent variables (health outcomes), or (c) is concerned with both the definition and measurement of health outcomes and the roles of determinants. While none of the three is normatively correct or incorrect, we believe that the latter is more appropriate, primarily because the concept and measurement of health and health outcomes focuses attention and research effort on the impact of each determinant and their interactions on some appropriate outcome. It also allows one to consider health inequality and inequity and the distribution of health across subpopulations, as well as the ethical and value considerations underpinning these issues. 8
While the original Evans and Stoddart “field model” did not discuss a population health concept in these terms, the idea is implicit in the evolution of the dependent variable from “health care” to “health and function” to “well being.” 1(pp33–53) The Institute of Medicine has given serious attention to measuring population health, thereby encouraging some kind of summary measure that includes mortality and health-related quality of life. 9
Given these considerations, we propose that population health as a concept of health be defined as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.” These populations are often geographic regions, such as nations or communities, but they can also be other groups, such as employees, ethnic groups, disabled persons, or prisoners. Such populations are of relevance to policymakers. In addition, many determinants of health, such as medical care systems, the social environment, and the physical environment, have their biological impact on individuals in part at a population level.
Defining population health this way requires some measure(s) of health outcomes of populations, including their distribution throughout the population. We chose the broader term “health outcomes” rather than the more narrow term “health status”; we believe the latter refers to health at a point in time rather than over a period of years. We do not believe that there is any one definitive measure, but we argue that the development and validation of such measures for different purposes is a critical task for the field of population health research.
Our definition does imply the necessity of one or more broad summary measures capable of being a dependent variable for the spectrum of all determinants (generally including length of life and health-related quality and function of those life years), along with a family of other submeasures for different policy and research purposes. For example, the Health Utilities Index is being used in the Canadian National Population Health Survey, 10 Years of Healthy Life have been used in Healthy People 2000, 11 and the EuroQuol has been recently added to the Medical Expenditure Panel Survey. 12
We support the idea that a hallmark of the field of population health is significant attention to the multiple determinants of such health outcomes, however measured. These determinants include medical care, public health interventions, aspects of the social environment (income, education, employment, social support, culture) and of the physical environment (urban design, clean air and water), genetics, and individual behavior. We note with caution that such a list of categories can lead to a view that they operate independently; population health research is fundamentally concerned about the interactions between them, and we prefer to refer to “patterns” of determinants.
Population health researchers tend to use a set of methods and approaches that have the following important characteristics: examination of systematic differences in outcomes across populations, complexity of interactions among determinants, biological pathways linking determinants to population health outcomes, and the influence of different determinants over time and throughout the life cycle. 13– 15
In our view, a population health perspective also requires attention to the resource allocation issues involved in linking determinants to outcomes. Part of the study of population health involves the estimation of the cross-sectoral cost-effectiveness of different types and combinations of investments for producing health. 16 Because improvement in population health requires the attention and actions of multiple actors (legislators, managers, providers, and individuals), the field of population health needs to pay careful attention to the knowledge transfer and academic-practice partnerships that are required for positive change to occur. 17, 18 Figure 1 ▶ shows how we view the field of population health. The field investigates each of the components shown in the figure, but particularly their interactions.

A schematic definition of the field of population health.
We expect and welcome critiques of the definition presented here. As noted above, one critique will be that the tasks of defining and measuring concepts of health are large enough to constitute a subject of their own, rather than being combined with the study of determinants of health. We have already given our rationale for including them in population health as a field of study, but we would add that the need for accountability argues strongly for the inclusion of outcome and distributional considerations if a population health approach is to be useful in guiding policymaking regarding resource allocation across determinants and sectors. Without such a framework, advocacy and financial incentives for individual determinants can proceed independently of their impact, as some would argue is now the case for some medical care expenditures in the United States.
A second critique is that such a definition and concept is so broad that it includes everything and is therefore not useful to guide either research or policy. We understand this concern but do not agree with it. We believe that a guiding synthesis is essential for considering both the relative impacts of the pattern of determinants and their interactions. Integration of knowledge about health and its multiple determinants seldom occurs. Policy managers typically have responsibility for a single sector; advocacy groups typically have an interest in only one disease or determinant. No one in the public or private sectors currently has responsibility for overall health improvement. We suggest that the importance of a population health perspective is that it forces review of health outcomes in a population across determinants. For population health research, specific investigations into a single determinant, outcome measure, or policy intervention are relevant, and may even be critical in some cases, but they must be recognized as only a part and not the whole.
Those in public health or health promotion may legitimately feel that population health is simply a renaming of what has been their work or legacy. Hamilton and Bhatti have attempted to show the complementarity and overlap between population health and health promotion, 19 building on the Canadian Achieving Health for All Framework for Health Promotion 20 and the World Health Organization Ottawa Charter on Health Promotion. 21 Frank has indicated that historic concepts of public health were similarly broad, until the biomedical paradigm became dominant. Those who define public health as the “health of the public” would not disagree with the definition of population health proposed here; in the words of Frank, the “shift in thinking entailed in population health should be a small one for public health workers . . . in fact it is not so much a shift as a return to our historical roots encompassing all the primary determinants of health in human populations.” 22(p163)
However, much of public health activity, in the United States at least, does not have such a broad mandate even in the “assurance” functions, since major determinants such as medical care, education, and income remain outside of public health authority and responsibility, and current resources do not even allow adequate attention to traditional and emerging public health functions. Similarly, we believe that the emerging prominence of social epidemiology is a very important development for population health but does not have the breadth, or imply all of the multiple interactions and pathways, of the definition proposed here for population health.
We believe that the time has come for a clarification of the meaning and scope of the term “population health.” We have offered a clarification of the term that combines the definition and measurement of health outcomes and their distribution, the patterns of determinants that influence such outcomes, and the policies that influence the optimal balance of determinants. We welcome discussion and debate regarding these suggestions as a way of moving toward some consensus on this important and emergent concept.
Acknowledgments
D. Kindig was funded in part by the Robert Wood Johnson Health and Society Scholars Planning Grant to the Department of Population Health Sciences at the University of Wisconsin Madison School of Medicine.
We acknowledge the helpful comments of John Mullahy, Stephanie Robert, Donn D’Alessio, John Lavis, and many members of the Robert Wood Johnson Foundation Health and Society Scholars Planning Group.
Both authors contributed equally to the planning and writing of this article.
Peer Reviewed
The Center for Interdisciplinary Population and Health Research (CIPHR) designs, supports, and conducts innovative research and evaluations to improve population health. We focus on
Improving patient-centered outcomes,, partnering with communities,, addressing health disparities,, educating, training & mentoring,, implementing & evaluating evidence-informed interventions, and disseminating findings., ciphr areas of research, biobehavioral cancer research, community engagement, health disparities, emergency medicine, infectious disease, implementation science, clinical and population health.

Staff Retreat 2023

CIPHR Research

CIPHR Resources

>CIPHR Investigators
>ciphr staff.

Key Partners
Ciphr office 1 riverfront plaza, fl 4 westbrook, maine 04092.

MHIR Contact Info
81 Research Drive | Scarborough, ME | 04074
Phone: 207.396.8100
Email: [email protected]
- Donate to Research
- Research Navigation Request Form
- MaineHealth Investigator Guide
Air pollution accounted for 8.1 million deaths globally in 2021, becoming the second leading risk factor for death, including for children under 5 years
Featured stories, advancing public health through data – a partnership spotlight on ephi’s national data management and analytics center for health (ndmc).

Partnering with Aga Khan University to further public health in Pakistan

The Lancet Public Health: Global study reveals stark differences between females and males in major causes of disease burden, underscoring the need for gender-responsive approaches to health

The number of people experiencing poor health and early death caused by metabolism-related risk factors such as high blood pressure, high blood sugar, and high BMI has increased by 50% since 2000, reveals new global study

Recent publications
Cost-effectiveness of interventions for hiv/aids, malaria, syphilis, and tuberculosis in 128 countries, evaluating scope and bias of population-level measles serosurveys, the state of health in the european union (eu-27) in 2019, burden of disease scenarios for 204 countries and territories, 2022–2050, hear from experts.
Get expert insights on trending topics in global health.
From air pollution to smoking, which risk factors contribute the most to health loss?

Forecasting the state of world health in 2050

Why is tuberculosis still a major cause of death? An interview with Dr. Hmwe Hmwe Kyu

Why PEPFAR matters, with Dr. Anthony Fauci

Explore the latest health trends with new GBD 2021 results

Popular pages and tools
View our most-visited pages in the last 30 days.
Global Burden of Disease (GBD)
The Global Burden of Disease (GBD) study provides a comprehensive picture of mortality and disability across countries, time, age, and sex. It quantifies health loss from hundreds of diseases, injuries, and risk factors, so that health systems can be improved and disparities eliminated.
On gun violence, the United States is an outlier
When we look exclusively at high-income countries and territories with populations of 10 million or more, the US ranks first for its high levels of gun violence.
The Lancet: Dramatic declines in global fertility rates set to transform global population patterns by 2100
By 2050, over three-quarters of countries will not have high enough fertility rates to sustain population size over time. This will increase to 97% of countries by 2100.
Health by location
Discover IHME's research on focus countries and health profiles for all countries.
Subscribe to our newsletter
- Skip to main content
- Skip to "About this site"
- Departments
Language selection
- Search and menus
Institute of Population and Public Health

The Institute of Population and Public Health launches at the Université de Montréal

Congratulations to the 2024 Applied Public Health Chairs!
The mandate of the Institute of Population and Public Health (IPPH) is to support research into the complex biological, social, cultural and environmental interactions that determine the health of individuals, communities and global populations; and to apply knowledge to improve the health of individuals and populations through strategic partnerships with population and public health stakeholders and innovative research funding programs. IPPH’s mission aims to improve the health of populations and promote health equity in Canada and globally through research and its application to policies, programs, and practice in public health and other sectors.

Dr. Katherine Frohlich

Université de Montréal
Suite 2043 7077 Avenue du Parc Montreal, QC H3N 1X7
Subscribe to our mailing list

- UH Population Health
UH Population Health to Host Scholars Focused on Obesity Health Disparities
Federal Grant Supporting Ongoing Training for Emerging Researchers
April 29, 2024
By Mike Emery
University of Houston Population Health (UHPH) has focused programming and research on cardiovascular health including obesity. Soon, it will begin a new phase in its efforts to facilitate the development of scientific investigations addressing this worldwide epidemic.
A recent grant from the National Heart, Lung, and Blood Institute (one of the National Institutes of Health), will provide UHPH with resources to further train and mentor new generations of obesity researchers.
This is the third time that Bettina Beech, UH Chief Population Health Officer and UHPH founder and colleagues have been awarded this grant, which supports Obesity Health Disparities Programs for Inclusion and Diversity Among Individuals Engaged in Health-Related Research (OHD PRIDE). Through OHD PRIDE, UH Population Health will work with early career investigators from around the nation to help them develop and share their research.
“UH Population Health will contribute to the next generation of scientists who are focusing their energies on health issues such as obesity,” said Marino Bruce, director of UH Population Health Collaboratories and OHD PRIDE Multiple Investigator. “We’re helping them launch their careers as early faculty members and assisting them to develop research studies designed to reverse disturbing global trends in obesity.”
Beech, Bruce and Roland J. Thorpe Jr. at Johns Hopkins Bloomberg School of Public Health are multiple principal investigators of OHD PRIDE. Rosenda Murillo, Associate Professor in the UH College of Education along with a national team of mentors and program faculty will work with early career scholars as OHD PRIDE Fellows. OHD PRIDE mentors and program faculty are scientists from leading research universities who have distinguished careers in obesity-related cardiovascular research. This group will deliver presentations on the latest developments in obesity science and provide feedback to Fellows about their research ideas in group and individual settings. OHD PRIDE mentors and program faculty will work with Fellows to produce competitive research grants and high impact peer-reviewed publications; the primary elements of an independent research career.
UHPH will welcome the next cohort of OHD PRIDE Fellows during a 10-day summer institute this June. Additional follow-up meetings will be scheduled both virtually and on campus through 2025. OHD PRIDE will mentor and train four cohorts of Fellows over the next five years.
“Fellows will not only master the nuts and bolts of manuscript and grant writing; they also will learn the nuances of biomedical, behavioral and social science research,” Bruce said. “They need to understand that revisions and rewrites are common, and research writing is a marathon … not a sprint.”
Beyond developing fellows’ writing and research skills, OHD PRIDE aims to continue making contributions the research literature and bringing awareness to the health risks associated with obesity in the U.S. and around the world.
“Obesity has been an international epidemic for two decades … going on three,” Bruce said. “It is one of the major risk factors for hypertension, diabetes, chronic kidney disease, heart disease and some forms of cancer. This has affected marginalized populations more than others.”
According to data from the Centers for Disease Control (CDC), adult obesity is most prevalent among Black and Hispanic adult populations. Bruce added that social and economic factors also affect obesity rates. Living in areas that are not conducive to walking or basic exercise contributes to obesity as do communities without access to fresh, healthy food options.
“There is not a ‘one size fits all’ solution for obesity,” Bruce said. “That’s why we need a diverse biomedical research workforce to collaborate, produce, and disseminate research on this weight related outcomes.”
While obesity has long contributed to several cardiovascular diseases and cancers, new developments related to the disease are affecting communities. Bruce cites the rise in weight loss drugs as offering scientists new opportunities to conduct obesity prevention and intervention studies. The jury is still out on medications such as Ozempic, he said.
“We simply don’t know what the long-term effects of these drugs are,” Bruce said. “Initiatives like OHD PRIDE can help the next generation of scientists produce research about accelerated weight gain and weight loss ensure that is accessible to and understood by the general public.”
OHD PRIDE perfectly complements the mission of UH Population Health. Since its introduction at the University, UHPH has addressed quality of life and has launched academic health programs. In doing so, Beech, Bruce and others within UHPH examine the myriad factors affecting health—physical, social, environmental, economic, spiritual and more.
“There is so much to understand with regard to health, nutrition and obesity,” Bruce said. “We are looking forward to continuing to work with early career researchers who are ready to explore these areas, establish careers as successful independent investigators, and share their discoveries with the world.”
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
research@BSPH
The School’s research endeavors aim to improve the public’s health in the U.S. and throughout the world.
- Funding Opportunities and Support
- Faculty Innovation Award Winners

Conducting Research That Addresses Public Health Issues Worldwide
Systematic and rigorous inquiry allows us to discover the fundamental mechanisms and causes of disease and disparities. At our Office of Research ( research@BSPH), we translate that knowledge to develop, evaluate, and disseminate treatment and prevention strategies and inform public health practice. Research along this entire spectrum represents a fundamental mission of the Johns Hopkins Bloomberg School of Public Health.
From laboratories at Baltimore’s Wolfe Street building, to Bangladesh maternity wards in densely packed neighborhoods, to field studies in rural Botswana, Bloomberg School faculty lead research that directly addresses the most critical public health issues worldwide. Research spans from molecules to societies and relies on methodologies as diverse as bench science and epidemiology. That research is translated into impact, from discovering ways to eliminate malaria, increase healthy behavior, reduce the toll of chronic disease, improve the health of mothers and infants, or change the biology of aging.
120+ countries
engaged in research activity by BSPH faculty and teams.
of all federal grants and contracts awarded to schools of public health are awarded to BSPH.
citations on publications where BSPH was listed in the authors' affiliation in 2019-2023.
publications where BSPH was listed in the authors' affiliation in 2019-2023.
Departments
Our 10 departments offer faculty and students the flexibility to focus on a variety of public health disciplines
Centers and Institutes Directory
Our 80+ Centers and Institutes provide a unique combination of breadth and depth, and rich opportunities for collaboration
Institutional Review Board (IRB)
The Institutional Review Board (IRB) oversees two IRBs registered with the U.S. Office of Human Research Protections, IRB X and IRB FC, which meet weekly to review human subjects research applications for Bloomberg School faculty and students
Generosity helps our community think outside the traditional boundaries of public health, working across disciplines and industries, to translate research into innovative health interventions and practices
Introducing the research@BSPH Ecosystem
The research@BSPH ecosystem aims to foster an interdependent sense of community among faculty researchers, their research teams, administration, and staff that leverages knowledge and develops shared responses to challenges. The ultimate goal is to work collectively to reduce administrative and bureaucratic barriers related to conducting experiments, recruiting participants, analyzing data, hiring staff, and more, so that faculty can focus on their core academic pursuits.

Research at the Bloomberg School is a team sport.
In order to provide extensive guidance, infrastructure, and support in pursuit of its research mission, research@BSPH employs three core areas: strategy and development, implementation and impact, and integrity and oversight. Our exceptional research teams comprised of faculty, postdoctoral fellows, students, and committed staff are united in our collaborative, collegial, and entrepreneurial approach to problem solving. T he Bloomberg School ensures that our research is accomplished according to the highest ethical standards and complies with all regulatory requirements. In addition to our institutional review board (IRB) which provides oversight for human subjects research, basic science studies employee techniques to ensure the reproducibility of research.
Research@BSPH in the News
Four bloomberg school faculty elected to national academy of medicine.
Considered one of the highest honors in the fields of health and medicine, NAM membership recognizes outstanding professional achievements and commitment to service.
The Maryland Maternal Health Innovation Program Grant Renewed with Johns Hopkins
Lerner center for public health advocacy announces inaugural sommer klag advocacy impact award winners.
Bloomberg School faculty Nadia Akseer and Cass Crifasi selected winners at Advocacy Impact Awards Pitch Competition

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Generalized Anxiety Disorder
Generalized anxiety disorder is characterized by excessive anxiety and worry about a variety of events or activities (e.g., work or school performance) that occurs more days than not, for at least 6 months. People with generalized anxiety disorder find it difficult to control their worry, which may cause impairment in social, occupational, or other areas of functioning.
Additional information about generalized anxiety disorder can be found on the NIMH Health Topics page on anxiety disorders .
Prevalence of Generalized Anxiety Disorder Among Adults
- An estimated 2.7% of U.S. adults had generalized anxiety disorder in the past year.
- Past year prevalence of generalized anxiety disorder among adults was higher for females (3.4%) than for males (1.9%).
- An estimated 5.7% of U.S. adults experience generalized anxiety disorder at some time in their lives. 2
| Demographic | Percent | |
|---|---|---|
| Overall | 2.7 | |
| Sex | Female | 3.4 |
| Male | 1.9 | |
| Age | 18-29 | 2.0 |
| 30-44 | 3.5 | |
| 45-59 | 3.4 | |
| 60+ | 1.5 | |
Generalized Anxiety Disorder with Impairment Among Adults
- Of adults with generalized anxiety disorder in the past year, degree of impairment ranged from mild to serious, as shown in Figure 2. Impairment was determined by scores on the Sheehan Disability Scale. 3
- Impairment was distributed evenly among adults with generalized anxiety disorder. An estimated 32.3% had serious impairment, 44.6% had moderate impairment, and 23.1% had mild impairment.
| Severity | Percent |
|---|---|
| Mild | 23.1 |
| Moderate | 44.6 |
| Serious | 32.3 |
| Total | 100 |
Prevalence of Generalized Anxiety Disorder Among Adolescents
- An estimated 2.2% of adolescents had generalized anxiety disorder, and an estimated 0.9% had severe impairment. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria were used to determine impairment.
- The prevalence of generalized anxiety disorder among adolescents was higher for females (3.0%) than for males (1.5%).
| Demographic | Percent | |
|---|---|---|
| Overall | 2.2 | |
| With Severe Impairment | 0.9 | |
| Sex | Female | 3.0 |
| Male | 1.5 | |
| Age | 13-14 | 1.0 |
| 15-16 | 2.8 | |
| 17-18 | 3.0 | |
Data Sources
- Harvard Medical School, 2007. National Comorbidity Survey (NCS). (2017, August 21). Retrieved from https://www.hcp.med.harvard.edu/ncs/index.php . Data Table 2: 12-month prevalence DSM-IV/WMH-CIDI disorders by sex and cohort.
- Harvard Medical School, 2007. National Comorbidity Survey (NCS). (2017, August 21). Retrieved from https://www.hcp.med.harvard.edu/ncs/index.php . Data Table 1: Lifetime prevalence DSM-IV/WMH-CIDI disorders by sex and cohort .
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005 Jun;62(6):617-27. PMID: 15939839
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010 Oct;49(10):980-9. PMID: 20855043
Statistical Methods and Measurement Caveats
National comorbidity survey replication (ncs-r).
Diagnostic Assessment and Population:
- The NCS-R is a nationally representative, face-to-face, household survey conducted between February 2001 and April 2003 with a response rate of 70.9%. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) mental disorders were assessed using a modified version of the fully structured World Health Organization Composite International Diagnostic Interview (WMH-CIDI), a fully structured lay-administered diagnostic interview that generates both International Classification of Diseases, 10 th Revision, and DSM-IV diagnoses. The DSM-IV criteria were used here. The Sheehan Disability Scale (SDS) assessed disability in work role performance, household maintenance, social life, and intimate relationships on a 0–10 scale. Participants for the main interview totaled 9,282 English-speaking, non-institutionalized, civilian respondents. Any anxiety disorder was assessed in a subsample of 5,692 adults. The NCS-R was led by Harvard University.
- Unlike the DSM-IV criteria used in the NCS-R and NCS-A, the current DSM-5 no longer places post-traumatic stress disorder or obsessive compulsive disorder in the anxiety disorder category. They are listed in new DSM5 categories.
Survey Non-response:
- In 2001-2002, non-response was 29.1% of primary respondents and 19.6% of secondary respondents.
- Reasons for non-response to interviewing include: refusal to participate (7.3% of primary, 6.3% of secondary); respondent was reluctant- too busy but did not refuse (17.7% of primary, 11.6% of secondary); circumstantial, such as intellectual developmental disability or overseas work assignment (2.0% of primary, 1.7% of secondary); and household units that were never contacted (2.0).
- For more information, see PMID: 15297905 .
National Comorbidity Survey Adolescent Supplement (NCS-A)
- The NCS-A was carried out under a cooperative agreement sponsored by NIMH to meet a request from Congress to provide national data on the prevalence and correlates of mental disorders among U.S. youth. The NCS-A was a nationally representative, face-to-face survey of 10,123 adolescents aged 13 to 18 years in the continental United States. The survey was based on a dual-frame design that included 904 adolescent residents of the households that participated in the adult U.S. National Comorbidity Survey Replication and 9,244 adolescent students selected from a nationally representative sample of 320 schools. The survey was fielded between February 2001 and January 2004. DSM-IV mental disorders were assessed using a modified version of the fully structured World Health Organization Composite International Diagnostic Interview.
- The overall adolescent non-response rate was 24.4%. This is made up of non-response rates of 14.1% in the household sample, 18.2% in the un-blinded school sample, and 77.7% in the blinded school sample. Non-response was largely due to refusal (21.3%), which in the household and un-blinded school samples came largely from parents rather than adolescents (72.3% and 81.0%, respectively). The refusals in the blinded school sample, in comparison, came almost entirely (98.1%) from parents failing to return the signed consent postcard.
- For more information, see PMID: 19507169 and the NIMH NCS-A study page .
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
News Release
Thursday, June 6, 2024
NIH launches $30 million pilot to test feasibility of a national primary care research network
Initiative aims to improve health outcomes by integrating research in everyday primary care settings.
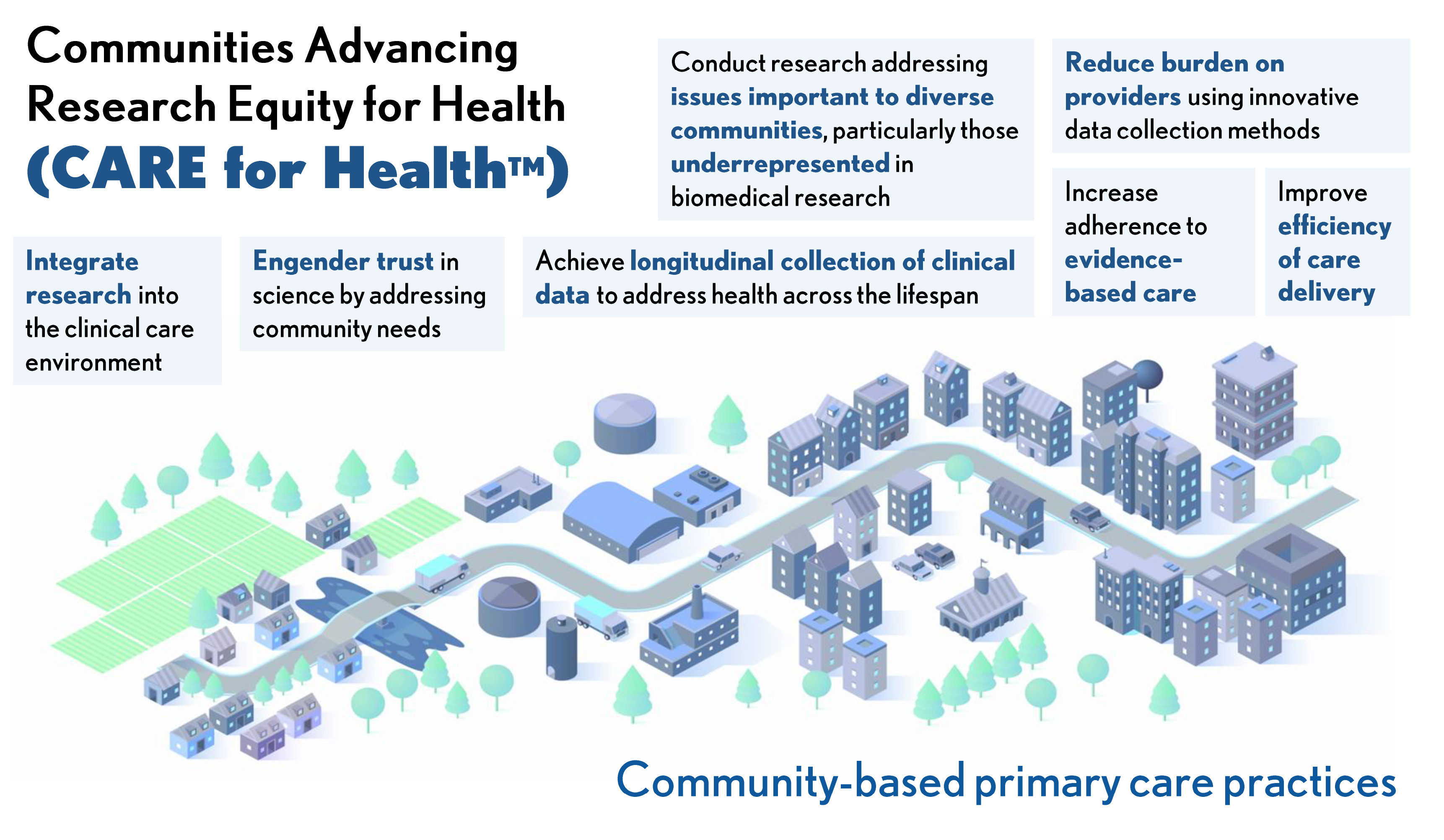
CARE for Health infographic
The National Institutes of Health (NIH) is investing approximately $30 million in total over fiscal years 2024 and 2025 to pilot a national primary care research network that integrates clinical research with community-based primary care. The new initiative called Communities Advancing Research Equity for Health – or CARE for Health – seeks to improve access to clinical research to inform medical care, particularly for those in communities historically underrepresented in clinical research or underserved in health care. Informed by the health needs of these communities, CARE for Health will help to grow an evidence base that contributes to improved patient outcomes, provide communities access to the best available scientific research and expand opportunities to participate in clinical trials and studies. NIH Director Monica M. Bertagnolli, M.D., lays out her vision for CARE for Health in a Science Editorial that was published today.
“Despite tremendous scientific progress, the health of important segments of the U.S. population is getting worse, not better,” said Dr. Bertagnolli. “Health is dependent upon many factors. We recognize that environmental and societal factors are very important, and that each community is unique. Because of this, we must adapt our research to be more inclusive and more responsive to the needs of communities currently underserved in health research. Our vision for CARE for Health is to help primary care providers and their patients contribute to knowledge generation, and to deliver evidence back to them to achieve better care.”
Supported through the NIH Common Fund, CARE for Health will initially leverage existing NIH-funded clinical research networks and community partners to establish the infrastructure that will support research at select primary care sites. Initial awards will fund organizations that serve rural communities and are expected to be made in fall 2024.
“Health research should be accessible to all populations. Clinical trials should reflect the diversity of Americans – because we know that delivers the best results,” said HHS Secretary Xavier Becerra. “We are taking a big step towards ensuring communities that are historically underrepresented in clinical research are fully included and have the same access to the best available results and analysis. There has never been more potential for progress than we have today.”
Participating clinical sites will be able to choose research studies based on health issues affecting and prioritized by their communities. Patients will be able to contribute their data to research in order to generate results that are clinically meaningful to them. Final study findings and aggregate results will be shared with research participants. CARE for Health will expand NIH-funded research studies to increase engagement with people from communities historically underrepresented or underserved in health care and clinical research. This includes people from certain racial and ethnic groups, those who are older, those who live in rural areas and those who have low socioeconomic status or lower educational attainment. Studies will seek to address common health issues, as well as disease prevention.
“Community-oriented primary care not only provides essential health services, but it also engenders trust among those who lack confidence in recommended medical care or science,” said Dr. Bertagnolli. “In fact, greater availability of primary care services in communities is associated with fewer disparities in health outcomes and lower mortality. We earn people’s trust when they get access to the care they need and when they can see direct benefits from their participation in research.”
As CARE for Health expands, the program will launch new studies across the network and further establish study sites, training capabilities, data management and increased interoperability. By expanding collaborations to integrate research data into clinical practice and clinical data collection into research studies, the network will facilitate the use of innovative practices and trial designs to minimize burden of research on primary care providers and patients.
“The goal is to create a learning health system in which research informs clinical practice and clinical data informs research,” said NIH Deputy Director for Program Coordination, Planning, and Strategic Initiatives Tara A. Schwetz, Ph.D. “As the program grows, sites and their communities will help design new clinical studies reflecting their specific health needs, and results from those studies will inform the care they receive.”
The NIH is hosting a public workshop on Friday, June 7 from 10 a.m. to 12:30 p.m. EDT to share findings from a series of listening sessions on the challenges and opportunities for integrating research into primary care. Learn more about the workshop and register for the event .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
Connect with Us
- More Social Media from NIH
- Operational Excellence
- Lab Services
- Lectureships
- Collaborations
- Outlook.com
- PHRI Intranet
- McMaster Intranet
- HHS COVID-19 self assessment
- DFexplore/ iDataFax

We’re better together. Scientists, investigators, fellows, study teams, and operational experts at PHRI – all dedicated to excellence in research

Salim Yusuf
Executive Director; Senior Scientist
Salim Yusuf chairs our five-member Executive Committee, and the Leadership Council comprised of 12 members of PHRI management.
Researchers
Senior Scientists, Scientists, Investigators, Research Fellows, Associates and PHRI International Fellows.

Muhammad Hameed
Head of Operations
Operational teams at PHRI work as an integrated whole to innovate and support clinically relevant, effective and optimal study processes, for our researchers in Hamilton and at sites around the world.
Back To Top
Sign up for the PHRI Pulse Newsletter
Don't miss out on the latest health research news from the Population Health Research Institute in Hamilton, Canada
- Full Name *
- Comments This field is for validation purposes and should be left unchanged.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Alcohol's Effects on Health
Research-based information on drinking and its impact.
National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Alcohol facts and statistics.

Updated: 2024
Learn up-to-date facts and statistics on alcohol consumption and its impact in the United States and globally. Explore topics related to alcohol misuse and treatment, underage drinking, the effects of alcohol on the human body, and more.
Find up-to-date statistics on lifetime drinking, past-year drinking, past-month drinking, binge drinking, heavy alcohol use, and high-intensity drinking.
Learn how many people ages 12 to 20 engage in underage alcohol misuse in the United States and the impact it has.
Explore how many people ages 18 to 25 engage in alcohol misuse in the United States and the impact it has.
Find out how many people have alcohol use disorder in the United States across age groups and demographics.
Discover how many people with alcohol use disorder in the United States receive treatment across age groups and demographics.
Discover the effects that alcohol consumption has on the human body such as increased risk for diseases and injuries.
Learn statistics about alcohol use during pregnancy.
Discover the impact alcohol has on children living with a parent or caregiver with alcohol use disorder.
Explore statistics on alcohol-related deaths and emergency visits in the United States.
Learn more about the financial impact of alcohol misuse in the United States.
Learn more about impacts of alcohol misuse globally.
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Endocrine Diseases
- Hashimoto's Disease
- Español
Hashimoto's Disease
On this page:
What is Hashimoto’s disease?
How common is hashimoto’s disease.
- Who is more likely to develop Hashimoto’s disease?
What are the complications of Hashimoto’s disease?
What are the symptoms of hashimoto’s disease, what causes hashimoto’s disease, how do doctors diagnose hashimoto’s disease, how do doctors treat hashimoto’s disease, how does eating, diet, and nutrition affect hashimoto’s disease, clinical trials for hashimoto’s disease.
Hashimoto’s disease is an autoimmune disorder that can cause hypothyroidism , or underactive thyroid. Rarely, the disease can cause hyperthyroidism , or overactive thyroid.
The thyroid is a small, butterfly-shaped gland in the front of your neck. In people with Hashimoto’s disease
- the immune system makes antibodies that attack the thyroid gland
- large numbers of white blood cells, which are part of the immune system, build up in the thyroid
- the thyroid becomes damaged and can’t make enough thyroid hormones
Thyroid hormones control how your body uses energy, so they affect nearly every organ in your body—even the way your heart beats.

Does Hashimoto’s disease have another name?
Hashimoto’s disease is also called Hashimoto’s thyroiditis, chronic lymphocytic thyroiditis, or autoimmune thyroiditis.
The number of people who have Hashimoto’s disease in the United States is unknown. However, the disease is the most common cause of hypothyroidism , which affects about 5 in 100 Americans. 1
Who is more likely to have Hashimoto’s disease?
Hashimoto’s disease is 4 to 10 times more common in women than men. 2 Although the disease may occur in teens or young women, it more often develops in women ages 30 to 50. 3 Your chance of developing Hashimoto’s disease increases if other family members have the disease.
You are more likely to develop Hashimoto’s disease if you have other autoimmune disorders, including 4
- celiac disease , a digestive disorder that damages the small intestine
- lupus , a chronic, or long-term, disorder that can affect many parts of the body
- rheumatoid arthritis , a disorder that affects the joints
- Sjögren’s syndrome , a disease that causes dry eyes and mouth
- type 1 diabetes , a disease that occurs when your blood glucose, also called blood sugar, is too high
Many people with Hashimoto’s disease develop hypothyroidism . Untreated, hypothyroidism can lead to several health problems, including 5
- high cholesterol
- heart disease and heart failure
- high blood pressure
- myxedema , a rare condition in which the body’s functions slow down to the point that it can threaten your life
Left untreated, hypothyroidism can also cause problems during pregnancy .
Many people with Hashimoto’s disease have no symptoms at first. As the disease progresses, you may have one or more of the symptoms of hypothyroidism.
Some common symptoms of hypothyroidism include
- weight gain
- trouble tolerating cold
- joint and muscle pain
- constipation
- dry skin or dry, thinning hair
- heavy or irregular menstrual periods or fertility problems
- slowed heart rate
Hashimoto’s disease causes your thyroid to become damaged. Most people with Hashimoto’s disease develop hypothyroidism. Rarely, early in the course of the disease, thyroid damage may lead to the release of too much thyroid hormone into your blood, causing symptoms of hyperthyroidism. 3
Your thyroid may get larger and cause the front of the neck to look swollen. The enlarged thyroid, called a goiter , may create a feeling of fullness in your throat, though it is usually not painful. After many years, or even decades, damage to the thyroid may cause the gland to shrink and the goiter to disappear.

Researchers don’t know why some people develop Hashimoto’s disease, but a family history of thyroid disease is common. Several factors may play a role, including 2
- viruses , such as hepatitis C
Hypothyroidism can also be caused by
- some medicines used to treat bipolar disorder or other mental health problems
- iodine-containing medicines used to treat abnormal heart rhythm
- exposure to toxins, such as nuclear radiation
Doctors diagnose Hashimoto’s disease based on
- medical history and physical exam . Your doctor will start by taking a medical history and performing a physical exam. In addition to asking about symptoms, the doctor will check your neck for a goiter, which some people with Hashimoto’s disease can develop.
- the thyroid hormones T4 (thyroxine) and T3 (triiodothyronine)
- thyroid-stimulating hormone, or TSH
- thyroid peroxidase antibodies (TPO), a type of thyroid antibody that is present in most people with Hashimoto’s disease
You probably won’t need other tests to confirm you have Hashimoto’s disease. However, if your doctor suspects Hashimoto’s disease but you don’t have antithyroid antibodies in your blood, you may have an ultrasound of your thyroid. The ultrasound images can show the size of your thyroid and other features of Hashimoto’s disease. The ultrasound also can rule out other causes of an enlarged thyroid, such as thyroid nodules—small lumps in the thyroid gland.
How your doctors treat Hashimoto’s disease usually depends on whether the thyroid is damaged enough to cause hypothyroidism. If you don’t have hypothyroidism, your doctor may choose to simply check your symptoms and thyroid hormone levels regularly.

The medicine levothyroxine , which is identical to the natural thyroid hormone thyroxine (T4), is the recommended way to treat hypothyroidism. Prescribed in pill form for many years, this medicine is now also available as a liquid and in a soft gel capsule. 2 These newer formulas may be helpful to people with digestive problems that affect how the thyroid hormone pill is absorbed.
Some foods and supplements can affect how well your body absorbs levothyroxine. Examples include grapefruit juice, espresso coffee, soy, and multivitamins that contain iron or calcium. 1,6 Taking the medicine on an empty stomach can prevent this from happening. Your doctor may ask you to take the levothyroxine in the morning, 30 to 60 minutes before you eat your first meal.
Your doctor will give you a blood test about 6 to 8 weeks after you begin taking the medicine and adjust your dose if needed. Each time you change your dose, you’ll have another blood test. Once you’ve reached a dose that’s working for you, your doctor will likely repeat the blood test in 6 months and then once a year.
Never stop taking your medicine or take a higher dose without talking with your doctor first. Taking too much thyroid hormone medicine can cause serious problems, such as atrial fibrillation or osteoporosis . 5
Your hypothyroidism can be well-controlled with thyroid hormone medicine, as long as you take the medicine as instructed by your doctor and have regular follow-up blood tests.
The thyroid uses iodine, a mineral in some foods, to make thyroid hormones. However, if you have Hashimoto’s disease or other types of autoimmune thyroid disorders, you may be sensitive to harmful side effects from iodine. Eating foods that have large amounts of iodine—such as kelp, dulse, or other kinds of seaweed, and certain iodine-rich medicines—may cause hypothyroidism or make it worse. Taking iodine supplements can have the same effect.
Talk with members of your health care team about
- what foods and beverages to limit or avoid
- whether you take iodine supplements
- any cough syrups you take that may contain iodine
However, if you are pregnant, you need to take enough iodine because the baby gets iodine from your diet. Too much iodine can cause problems as well, such as a goiter in the baby. If you are pregnant, talk with your doctor about how much iodine you need.
Researchers are looking at other ways in which diet and supplements—such as vitamin D and selenium —may affect Hashimoto’s disease. 2 However, no specific guidance is currently available. 3
The NIDDK conducts and supports clinical trials in many diseases and conditions, including endocrine diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for Hashimoto’s disease?
Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about Hashimoto’s disease and improve health care for people in the future.
Find out if clinical studies are right for you .
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for Hashimoto’s disease are looking for participants?
You can find clinical studies on Hashimoto’s disease at www.ClinicalTrials.gov . In addition to searching for federally funded studies, you can expand or narrow your search to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank: Leonard Wartofsky, M.D., M.A.C.P., MedStar Georgetown University Hospital

Èlektrostal'
Urban District in Moscow Oblast

IMAGES
VIDEO
COMMENTS
Explore Our Studies and Trials. PHRI research activities encompass: ACS and interventional cardiology; arrhythmia and heart failure; biomarkers and genetics; brain health and stroke; cancer survivorship; CVD prevention; diabetes and GI; global and population health; infectious diseases; knowledge translation and health systems; perioperative and surgery; digital health; renal; and thrombosis.
PHRI is a joint initiative of McMaster University and Hamilton Health Sciences, founded by Salim Yusuf in 1999. It conducts large clinical trials, population health studies, and epidemiology expertise in 102 countries on six continents.
Our Story. After starting a preventive cardiology and therapeutic program in Hamilton, Canada in 1993, Salim Yusuf founded the Population Health Research Institute (PHRI) in 1999 to broaden the research agenda. An extensive international network of committed collaborators in 102 countries, and a wide range of types of large trials, studies and ...
PHRI.ca Population Health Research Institute (PHRI) is a joint institute of McMaster University and Hamilton Health Sciences. Founded in 1999 under the leadership of Dr. Salim Yusuf, who continues ...
The Mission of Public Health. In 1988, an Institute of Medicine commission defined the mission of public health as "assuring the conditions in which people can be healthy. ... On the academic side, research in population health has increased dramatically in the United States, partly in response to the evolving policy context of medical care ...
PHRI (Population Health Research Institute), a joint institute of McMaster University and Hamilton Health Sciences, is a world leader in clinical trials and large population health observational ...
The Population Health Research Institute (PHRI) is Canada's premiere global health research institute and a world leader in large clinical trials and population studies. Originally formed with a focus on cardiovascular disease (CVD) and diabetes, PHRI's research areas have broadened to include population genomics, perioperative medicine ...
The Population Health Research Institute (PHRI) is Canada's premiere global health research institute and a world leader in large clinical trials and population studies. Through international collaboration and innovation, PHRI explores CVD, diabetes, kidney and lung diseases, brain health, cancer and more. Originally formed with a focus on cardiovascular disease (CVD) and diabetes, PHRI's ...
Accelerating population health improvement. Pedro Delgado and colleagues describe how applying improvement methods to working with populations could help close equity gaps. As the covid-19 pandemic shines a bright light on longstanding health equity gaps, 1 concerted action around social determinants of health to close these gaps continues to ...
Population health studies involve assessment of diagnostic and therapeutic decisions and evaluation of clinical outcomes using multiple methods, including clinical trials and observational outcome studies. In addition to clinical event outcomes, quality of life, costs, and societal impact are also evaluated. Many social determinants of health ...
John Frank, the scientific director of the recently created Canadian Institute of Population and Public Health, has similarly called population health "a newer research strategy for understanding the health of populations."2 T. K. Young's recent book Population Health also tends in this direction; he states that in Canada and the United ...
The Center for Interdisciplinary Population and Health Research (CIPHR) designs, supports, and conducts innovative research and evaluations to improve population health. ... MaineHealth Institute for Research. 81 Research Drive Scarborough, Maine | 04074 207.396.8100 [email protected]. Search for: Resources + Clinical Trials + Grants ...
A group comprised of members of the MetroHealth Research Institute, the Population Health and Equity Research Institute (PHERI), Center staff, and Center collaborators met to incorporate the findings from the interviews into the strategic planning process. This culminated with a virtual retreat in December that was extremely well attended.
The Institute for Health Metrics and Evaluation ... Discover IHME's research on focus countries and health profiles for all countries. Last updated. March 20, 2024 ... Institute for Health Metrics and Evaluation Hans Rosling Center for Population Health. 3980 15th Ave NE, Seattle WA 98195 UW Campus Box #351615. Phone: +1 (206) 897-2800 Fax : +1 ...
Our collective efforts will establish powerful new models of how to improve the health of different communities in the region, statewide, and nationally. The three Centers within the Population Health and Equity Research Institute have had great success in 2022 with over 40 publications and 34 active grants totaling over $27 million dollars ...
Don't miss out on the latest health research news from the Population Health Research Institute in Hamilton, Canada. Full Name * Email * CAPTCHA. Phone. This field is for validation purposes and should be left unchanged. PHRI is a joint institute of McMaster University and Hamilton Health Sciences.
About IPPH. The mandate of the Institute of Population and Public Health (IPPH) is to support research into the complex biological, social, cultural and environmental interactions that determine the health of individuals, communities and global populations; and to apply knowledge to improve the health of individuals and populations through strategic partnerships with population and public ...
Population Health Research Institute, Canada D-index 75 Citations 35,342 343. 17314 World 719 National. Jackie Bosch Population Health Research Institute, Canada D-index 70 Citations 37,326 217. Our research was coordinated by Imed Bouchrika, PhD, a computer scientist with a well-established record of collaboration on a number of international ...
We are pleased to announce a new Narrative "Summer Series" hosted jointly by UWPHI and DPH/DHS. These 90-minute events will be conversational, workshop-style virtual learning opportunities designed to increase participants' understanding of narrative's connection to specific topics within public health.
University of Houston Population Health (UHPH) has focused programming and research on cardiovascular health including obesity. Soon, it will begin a new phase in its efforts to facilitate the development of scientific investigations addressing this worldwide epidemic. A recent grant from the National Heart, Lung, and Blood Institute (one of the National Institutes of Health), will provide ...
Systematic and rigorous inquiry allows us to discover the fundamental mechanisms and causes of disease and disparities. At our Office of Research (research@BSPH), we translate that knowledge to develop, evaluate, and disseminate treatment and prevention strategies and inform public health practice.Research along this entire spectrum represents a fundamental mission of the Johns Hopkins ...
The NIMH Strategic Plan for Research is a broad roadmap for the Institute's research priorities over the next five years. Learn more about NIMH's commitment to accelerating the pace of scientific progress and transforming mental health care. ... Diagnostic Assessment and Population: The NCS-R is a nationally representative, face-to-face ...
CARE for Health will expand NIH-funded research studies to increase engagement with people from communities historically underrepresented or underserved in health care and clinical research. This includes people from certain racial and ethnic groups, those who are older, those who live in rural areas and those who have low socioeconomic status ...
Maha Mushtaha has been employed by the Population Health Research Institute since 2011, working currently in the global health research group on the following studies: PURE, SCHOLAR-2 and TIMING. She has experience with site and database management of large, international observational studies as well as investigator-initiated clinical trials.
Operations. Operational teams at PHRI work as an integrated whole to innovate and support clinically relevant, effective and optimal study processes, for our researchers in Hamilton and at sites around the world. Meet Operations. Don't miss out on the latest health research news from the Population Health Research Institute in Hamilton, Canada.
Learn up-to-date facts and statistics on alcohol consumption and its impact in the United States and globally. Explore topics related to alcohol misuse and treatment, underage drinking, the effects of alcohol on the human body, and more.
Noginsky District ( Russian: Ноги́нский райо́н) is an administrative [1] and municipal [2] district ( raion ), one of the thirty-six in Moscow Oblast, Russia. It is located in the east of the oblast. The area of the district is 893.90 square kilometers (345.14 sq mi). [2] Its administrative center is the town of Noginsk. [1]
Population. 158,000. Elevation. 166 metres (545 feet) Open Location Code. 9G7WQCRR+56. OpenStreetMap ID. node 156167469. OpenStreetMap Feature. place=city. GeoNames ID. 563523. Wikidata ID. Q198419. Thanks for contributing to our open data sources.
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about Hashimoto's disease and improve health care for people in the future. Find out if clinical studies are right for you.
The population development of the urban and rural places in Èlektrostal'. The icon links to further information about a selected place including its population structure (gender). Name Native Status District Population Census 2002-10-09 Population Census 2010-10-14 Population Census