Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines


Phalloplasty for Gender Affirmation
Featured Expert:

Fan Liang, M.D.
Phalloplasty is surgery for masculinizing gender affirmation. Phalloplasty is a multistaged process that may include a variety of procedures, including:
- Creating the penis
- Lengthening the urethra so you are able to stand to urinate
- Creating the tip (glans) of the penis
- Creating the scrotum
- Removing the vagina, uterus and ovaries
- Placing erectile and testicular implants
- Skin grafting from the donor tissue site
Gender affirmation surgery is customized to each individual. Your surgical plan may include more or fewer of these steps and procedures. Fan Liang, M.D. , medical director of the Center for Transgender and Gender Expansive Health at Johns Hopkins, explains what you should know.
Are there different types of phalloplasty?
Phalloplasty involves using skin flaps, which are areas of skin moved from one area of the body to another. The skin flap is then reshaped, contoured and reattached to the groin to create the penis. There are three approaches the surgeon may use to construct the penis, using skin from the arm (radial forearm free flap), leg (anterolateral thigh flap) or side (latissimus dorsi flap).
There are pros and cons to each approach. Factors for choosing skin flap locations include the patient’s health and fat distribution, nerve function, blood flow and desired surgical outcomes.
What is a radial forearm free flap?
A radial forearm free flap (RFFF) involves taking the skin, fat, nerves, arteries and veins from your wrist to about halfway up your forearm to create the penis. Typically, the surgeon will use your nondominant hand so it is easier for you to recover and return to your day-to-day activities.
During your surgical consultation, the doctor will check the blood flow to your arm and hand noninvasively. This involves temporarily putting pressure on arteries then releasing the pressure to test blood distribution in the arm and hand.
There are three stages to this procedure.
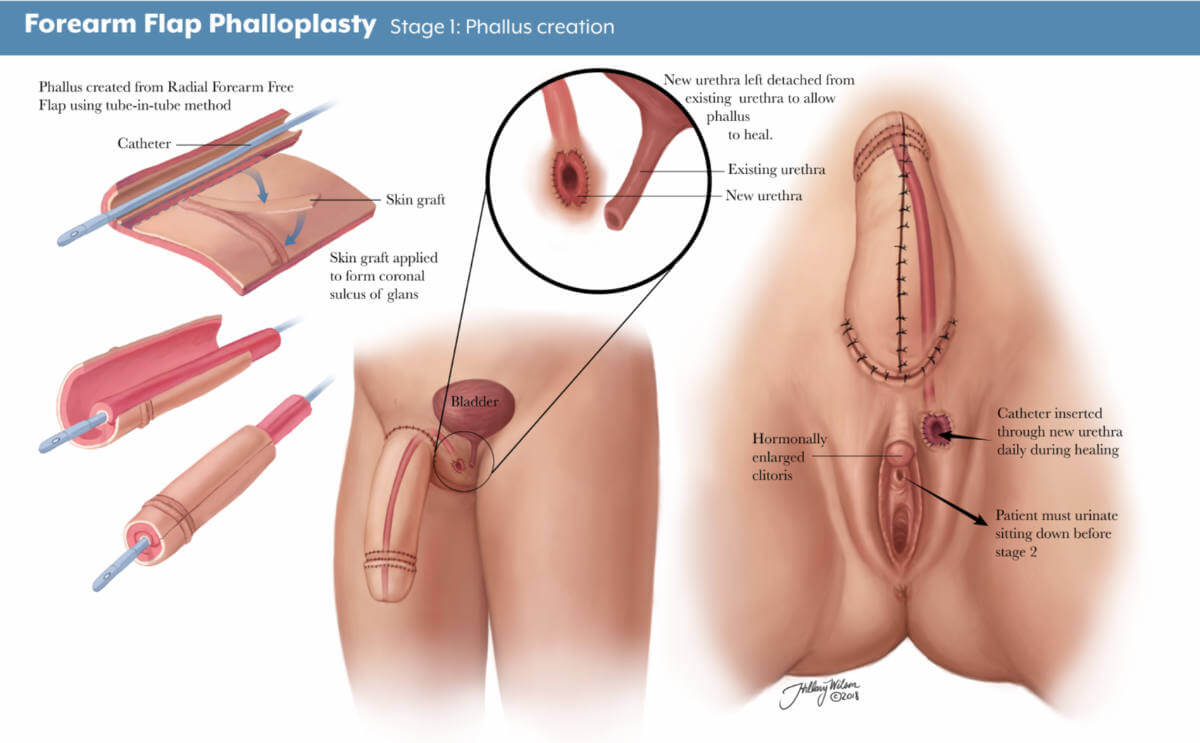
- Stage 1: The first stage of an RFFF approach is creating the penis using tissue from the forearm. The area where the forearm tissue is taken will require a skin graft. This may occur at the time of the initial phalloplasty surgery, or it may occur three to five weeks afterward. If it occurs later, patients will have a temporary skin covering over the forearm to help it heal.
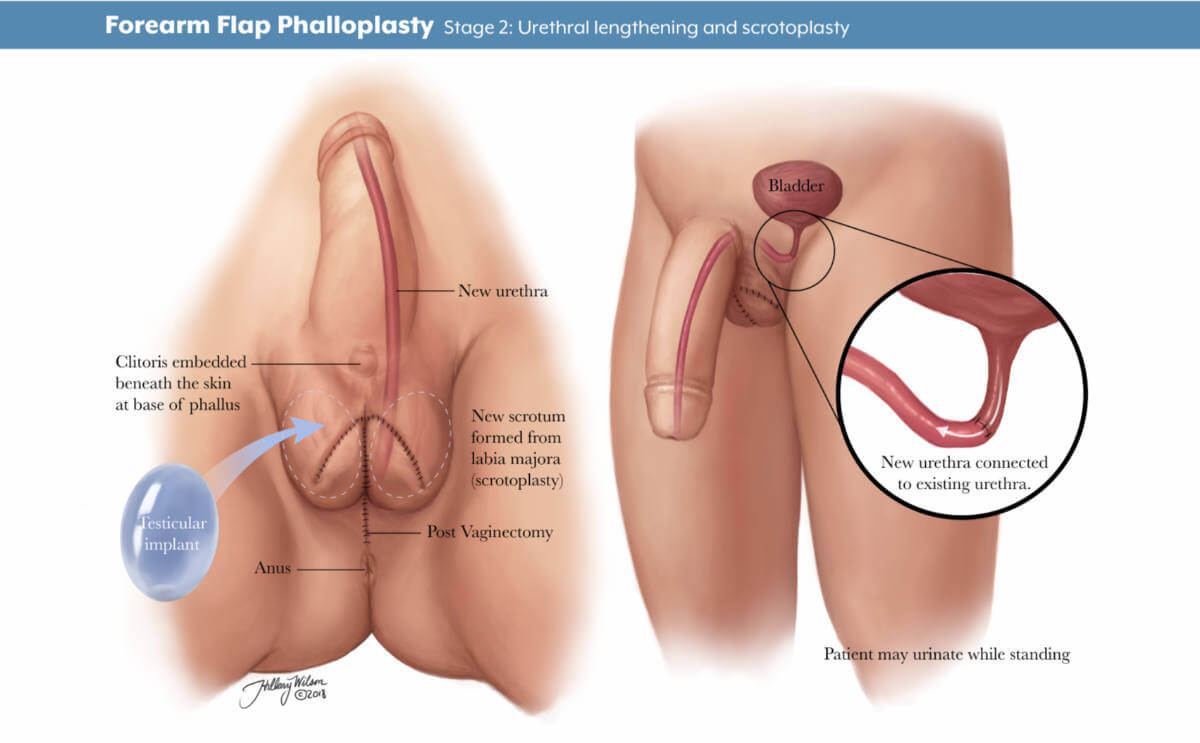
- Stage 2: The second stage, scheduled about five to six months later, may include lengthening the urethra to allow for urination out of the tip of the penis, creating the scrotum and removing the vagina, and other procedures depending on the patient’s individualized plan.
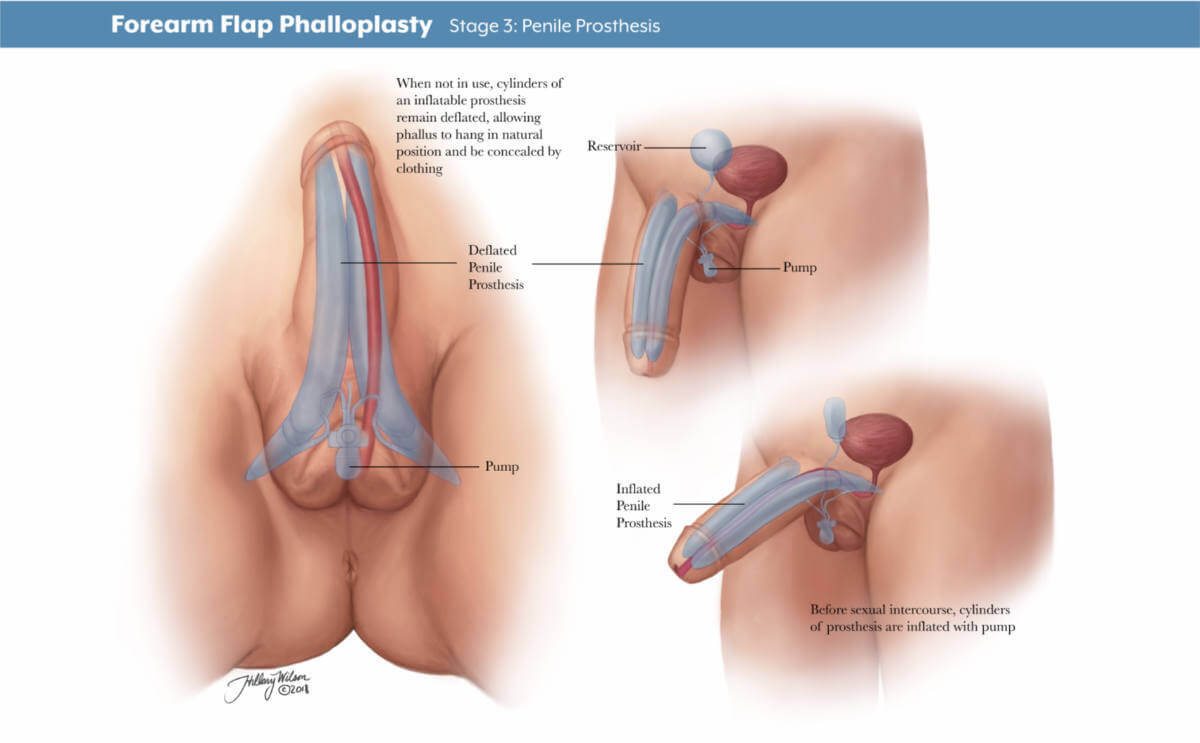
- Stage 3: The third stage of surgery involves putting in place testicle implants and an erectile device to help the patient achieve an erection. The third stage typically takes place 12 months after the second.
Will I have a say in how the phalloplasty is staged and the surgical plan?
Your gender affirmation surgery is highly personalized. Depending on what is most important to you, your surgery team will work with you on a customized plan beforehand. You and your surgeon will discuss your priorities and decide which procedures are right for you. Each stage will be scheduled to ensure your health and safety and provide the best chance of good results.
How long will I be in the hospital?
After your stage 1 surgery, you will stay as an inpatient for four to five days. Your surgical team will frequently monitor the blood supply to the tissue that has been used to create your new penis and ensure you are able to use the bathroom and walk around after surgery. Procedures for stages 2 and 3 do not require a hospital stay.
Will I need a catheter?
During your inpatient stay for stage 1 surgery, you will have a suprapubic tube that goes directly into your bladder and another catheter in your native urethra for at least five days. It is typically removed in the hospital before you go home.
If you decide not to have urethral lengthening as part of stage 2, you will have a Foley catheter placed in the operating room and removed before you leave the hospital. If you decide to have urethral lengthening, you will go home with a Foley catheter in the new urethra and a suprapubic tube. A clamp ensures that the urethra does not leak urine.
What is a suprapubic tube?
A suprapubic tube (SPT) allows urine to drain from your bladder. It is placed in the lower part of your abdomen, below the belly button. The SPT stays in for four to five weeks, depending on your healing and recovery.
When will my SPT be removed?
Before the SPT is removed, around four weeks after surgery, a urologist will perform a retrograde urethrogram. This involves putting dye into the bladder through the new urethra. An X-ray tracks the dye to see if the new urethra is open and ready for urination. If so, the doctor will clamp the SPT and you will be allowed to urinate from your new urethra. If everything looks good after a few days, the SPT is removed.
Forearm Flap Phalloplasty
Stage 1: phallus creation. Enlarged image .
Stage 2: urethral lengthening and scrotoplasty. Enlarged image .
Stage 3: penile prosthesis. Enlarged image .
Other Skin Flaps Used in Phalloplasty
What is an anterolateral thigh flap.
An anterolateral thigh flap (ALT) uses skin, fat, nerves, arteries and veins from the leg to create a penis. A special vascular CT scan can help the surgeon examine the blood supply of each leg to determine which leg will be better for creating the skin flap.
The stage of the ALT phalloplasty are similar to the RFFF. The area where the thigh tissue is taken will also require a skin graft. The resulting scar on the thigh can be covered with shorts.
What is a musculocutaneous latissimus dorsi flap?
A musculocutaneous latissimus dorsi skin flap (MLD) involves the skin, fat, nerves, arteries and veins from the side of your back to create a penis. The surgeon may order a special CT scan to look at the blood flow throughout the donor site area.
The stages of the MLD phalloplasty are similar to the RFFF and ALT. However, the area from which the back tissue is taken usually does not require a skin graft and can be closed in a straight line. The scar can be covered with a shirt. Patients may experience some initial weakness raising their arm, but this improves with time.
How is penis size determined?
Penis size depends on patient preferences and the skin flap harvested from your body. Thinner patients with less fat on the skin flap will have a penis with less girth. Alternatively, patients with a greater amount of fat will have a thicker penis.
The length of the penis depends on the patient’s donor site, but typically it is about 5–6 inches. After the first stage, the penis may decrease in size as postoperative swelling decreases and the tissue settles into its new location.
What determines scrotum size?
Scrotum size is specific to the patient and depends on the amount of skin that is present in the genital area before phalloplasty. The more genital tissue there is, the larger the scrotum and the testicular implants can be.
There are different ways to create the scrotum, including a procedure called V-Y scrotoplasty, a technique that creates a pouch to hold testicular implants. AART silicone round carving blocks have been approved by the FDA to be used as implants.
Procedures to Discuss with Your Physician Before Phalloplasty
Each individual undergoing gender confirmation surgery is different. Your surgeon will work with you to discuss which procedures, and their timing, are best for you and your goals.
Should I have a hysterectomy before phalloplasty surgery?
For those interested in this procedure, hysterectomies are typically done before phalloplasty and do not require a vaginectomy.
Urethral Lengthening Before Phalloplasty
If you choose to have urethral lengthening, this procedure involves lengthening your existing urethra so that you are able to urinate out of the tip of the penis. It involves connecting your current urethra to the new urethra created in the shaft of the penis.
Not all patients choose to have urethral lengthening; however, this will be a necessary step if you want to stand when you urinate. It is also important to know that if you decide not to have urethral lengthening in stage 1 of your phalloplasty, it will not be possible to have the lengthening procedure later.
Complications of Urethral Lengthening
The most common complications for urethral lengthening include urethral strictures (narrowed areas of the urethra), fistula (creation of a passageway between the urethra and another location) and diverticula (formation of a pouch in the urethra). This may require an additional surgical procedure to fix.
What is a metoidioplasty?
A metoidioplasty is a surgical procedure to achieve masculine-appearing genitalia with fewer steps than a phalloplasty. The skin of the labia and around the clitoris is lengthened to achieve the appearance of a penis. Some people prefer to undergo a metoidioplasty if they do not want to use tissue from their arms or legs to create a penis or if they prefer a shorter, more straightforward surgery.
A metoidioplasty procedure has a quicker recovery and fewer complications. Surgeons can discuss metoidioplasty with patients and help them decide if this option is right for them.
Will I need to have hair removal?
Yes, before surgery, after you consult with the surgical team and choose a skin flap site, you will get a template for hair removal that you can give to your hair removal professional.
What if I have a tattoo on my preferred donor site?
As long as there is good blood flow and nerve function, donor sites — even those with a tattoo — can be used.
Penile Function and Sensation After Phalloplasty
What can i do with a reconstructed penis.
Penis function is determined by what you and your surgery team agree on for your surgical plan. If it is important for you to urinate out of the tip of your penis, then urethral lengthening may be a good choice for you. If sensation is most important, your team will focus on a donor site with good nerve innervation. If penetrative sex is most important, and you would like to maintain an erection, then implanting an erectile prosthetic can be part of your surgery plan.
Can I get an erection after phalloplasty?
In stage 3 phalloplasty, a urologist can place a prosthetic erectile device which will allow you to maintain an erection. As of September 2022, no implantable prosthetic devices have been FDA-approved for phalloplasty. Instead, the surgeon can use a device intended for patients with erectile dysfunction to allow transmasculine patients to achieve an erection. There is a risk of infection and implant rejection with an erectile implant . If this happens, it may take six months before another device can be placed into the penis.
What kind of sensation and feeling can I expect?
Sensation recovery varies by patient. Nerve regeneration can begin as early as three weeks after surgery, but it can take longer in some patients. Sometimes sensation can take up to a year or longer. Return of nerve sensation is not guaranteed. As nerves regenerate and strengthen connections, you might experience shooting pain, tingling or electrical sensations. As time goes on, the tingling feeling begins to subside.
What is nerve hookup during phalloplasty?
Nerve hookup involves taking existing nerves from the donor site, such as the arm, and connecting them to nerves located in the pelvis. This allows you to have sensation in the reconstructed penis.
What is clitoral burying during phalloplasty surgery?
Clitoral burying involves moving the clitoris into the base of the penis to increase sensation. This is typically done at stage 2.
Is orgasm possible after phalloplasty?
Orgasm is possible after phalloplasty, especially if your surgery plan emphasizes preserving sensation. It is important to note that your penis will not ejaculate with semen at the time of orgasm.
Find a Doctor
Specializing In:
- Gender Affirmation Surgery
- Transgender Health
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
- Center for Transgender and Gender Expansive Health
- Plastic and Reconstructive Surgery
Find Additional Treatment Centers at:

Request an Appointment

Vaginoplasty for Gender Affirmation

Top Surgery

Facial Feminization Surgery (FFS)
Related Topics
- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
- Social and Public Health
What Is Gender Affirmation Surgery?
:max_bytes(150000):strip_icc():format(webp)/KP-Headshot-IMG_1661-0d48c6ea46f14ab19a91e7b121b49f59.jpg)
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary, to change one or more of their sex characteristics. This type of procedure offers a person the opportunity to have features that align with their gender identity.
For example, this type of surgery may be a transgender surgery like a male-to-female or female-to-male surgery. Read on to learn more about what masculinizing, feminizing, and gender-nullification surgeries may involve, including potential risks and complications.
Why Is Gender Affirmation Surgery Performed?
A person may have gender affirmation surgery for different reasons. They may choose to have the surgery so their physical features and functional ability align more closely with their gender identity.
For example, one study found that 48,019 people underwent gender affirmation surgeries between 2016 and 2020. Most procedures were breast- and chest-related, while the remaining procedures concerned genital reconstruction or facial and cosmetic procedures.
In some cases, surgery may be medically necessary to treat dysphoria. Dysphoria refers to the distress that transgender people may experience when their gender identity doesn't match their sex assigned at birth. One study found that people with gender dysphoria who had gender affirmation surgeries experienced:
- Decreased antidepressant use
- Decreased anxiety, depression, and suicidal ideation
- Decreased alcohol and drug abuse
However, these surgeries are only performed if appropriate for a person's case. The appropriateness comes about as a result of consultations with mental health professionals and healthcare providers.
Transgender vs Nonbinary
Transgender and nonbinary people can get gender affirmation surgeries. However, there are some key ways that these gender identities differ.
Transgender is a term that refers to people who have gender identities that aren't the same as their assigned sex at birth. Identifying as nonbinary means that a person doesn't identify only as a man or a woman. A nonbinary individual may consider themselves to be:
- Both a man and a woman
- Neither a man nor a woman
- An identity between or beyond a man or a woman
Hormone Therapy
Gender-affirming hormone therapy uses sex hormones and hormone blockers to help align the person's physical appearance with their gender identity. For example, some people may take masculinizing hormones.
"They start growing hair, their voice deepens, they get more muscle mass," Heidi Wittenberg, MD , medical director of the Gender Institute at Saint Francis Memorial Hospital in San Francisco and director of MoZaic Care Inc., which specializes in gender-related genital, urinary, and pelvic surgeries, told Health .
Types of hormone therapy include:
- Masculinizing hormone therapy uses testosterone. This helps to suppress the menstrual cycle, grow facial and body hair, increase muscle mass, and promote other male secondary sex characteristics.
- Feminizing hormone therapy includes estrogens and testosterone blockers. These medications promote breast growth, slow the growth of body and facial hair, increase body fat, shrink the testicles, and decrease erectile function.
- Non-binary hormone therapy is typically tailored to the individual and may include female or male sex hormones and/or hormone blockers.
It can include oral or topical medications, injections, a patch you wear on your skin, or a drug implant. The therapy is also typically recommended before gender affirmation surgery unless hormone therapy is medically contraindicated or not desired by the individual.
Masculinizing Surgeries
Masculinizing surgeries can include top surgery, bottom surgery, or both. Common trans male surgeries include:
- Chest masculinization (breast tissue removal and areola and nipple repositioning/reshaping)
- Hysterectomy (uterus removal)
- Metoidioplasty (lengthening the clitoris and possibly extending the urethra)
- Oophorectomy (ovary removal)
- Phalloplasty (surgery to create a penis)
- Scrotoplasty (surgery to create a scrotum)
Top Surgery
Chest masculinization surgery, or top surgery, often involves removing breast tissue and reshaping the areola and nipple. There are two main types of chest masculinization surgeries:
- Double-incision approach : Used to remove moderate to large amounts of breast tissue, this surgery involves two horizontal incisions below the breast to remove breast tissue and accentuate the contours of pectoral muscles. The nipples and areolas are removed and, in many cases, resized, reshaped, and replaced.
- Short scar top surgery : For people with smaller breasts and firm skin, the procedure involves a small incision along the lower half of the areola to remove breast tissue. The nipple and areola may be resized before closing the incision.
Metoidioplasty
Some trans men elect to do metoidioplasty, also called a meta, which involves lengthening the clitoris to create a small penis. Both a penis and a clitoris are made of the same type of tissue and experience similar sensations.
Before metoidioplasty, testosterone therapy may be used to enlarge the clitoris. The procedure can be completed in one surgery, which may also include:
- Constructing a glans (head) to look more like a penis
- Extending the urethra (the tube urine passes through), which allows the person to urinate while standing
- Creating a scrotum (scrotoplasty) from labia majora tissue
Phalloplasty
Other trans men opt for phalloplasty to give them a phallic structure (penis) with sensation. Phalloplasty typically requires several procedures but results in a larger penis than metoidioplasty.
The first and most challenging step is to harvest tissue from another part of the body, often the forearm or back, along with an artery and vein or two, to create the phallus, Nicholas Kim, MD, assistant professor in the division of plastic and reconstructive surgery in the department of surgery at the University of Minnesota Medical School in Minneapolis, told Health .
Those structures are reconnected under an operative microscope using very fine sutures—"thinner than our hair," said Dr. Kim. That surgery alone can take six to eight hours, he added.
In a separate operation, called urethral reconstruction, the surgeons connect the urinary system to the new structure so that urine can pass through it, said Dr. Kim. Urethral reconstruction, however, has a high rate of complications, which include fistulas or strictures.
According to Dr. Kim, some trans men prefer to skip that step, especially if standing to urinate is not a priority. People who want to have penetrative sex will also need prosthesis implant surgery.
Hysterectomy and Oophorectomy
Masculinizing surgery often includes the removal of the uterus (hysterectomy) and ovaries (oophorectomy). People may want a hysterectomy to address their dysphoria, said Dr. Wittenberg, and it may be necessary if their gender-affirming surgery involves removing the vagina.
Many also opt for an oophorectomy to remove the ovaries, almond-shaped organs on either side of the uterus that contain eggs and produce female sex hormones. In this case, oocytes (eggs) can be extracted and stored for a future surrogate pregnancy, if desired. However, this is a highly personal decision, and some trans men choose to keep their uterus to preserve fertility.
Feminizing Surgeries
Surgeries are often used to feminize facial features, enhance breast size and shape, reduce the size of an Adam’s apple , and reconstruct genitals. Feminizing surgeries can include:
- Breast augmentation
- Facial feminization surgery
- Penis removal (penectomy)
- Scrotum removal (scrotectomy)
- Testicle removal (orchiectomy)
- Tracheal shave (chondrolaryngoplasty) to reduce an Adam's apple
- Vaginoplasty
- Voice feminization
Breast Augmentation
Top surgery, also known as breast augmentation or breast mammoplasty, is often used to increase breast size for a more feminine appearance. The procedure can involve placing breast implants, tissue expanders, or fat from other parts of the body under the chest tissue.
Breast augmentation can significantly improve gender dysphoria. Studies show most people who undergo top surgery are happier, more satisfied with their chest, and would undergo the surgery again.
Most surgeons recommend 12 months of feminizing hormone therapy before breast augmentation. Since hormone therapy itself can lead to breast tissue development, transgender women may or may not decide to have surgical breast augmentation.
Facial Feminization and Adam's Apple Removal
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers, botox, fat grafting, and liposuction may also be used to create a more feminine appearance.
Some trans women opt for chondrolaryngoplasty, also known as a tracheal shave. The procedure reduces the size of the Adam's apple, an area of cartilage around the larynx (voice box) that tends to be larger in people assigned male at birth.
Vulvoplasty and Vaginoplasty
As for bottom surgery, there are various feminizing procedures from which to choose. Vulvoplasty (to create external genitalia without a vagina) or vaginoplasty (to create a vulva and vaginal canal) are two of the most common procedures.
Dr. Wittenberg noted that people might undergo six to 12 months of electrolysis or laser hair removal before surgery to remove pubic hair from the skin that will be used for the vaginal lining.
Surgeons have different techniques for creating a vaginal canal. A common one is a penile inversion, where the masculine structures are emptied and inverted into a created cavity, explained Dr. Kim. Vaginoplasty may be done in one or two stages, said Dr. Wittenberg, and the initial recovery is three months—but it will be a full year until people see results.
Surgical removal of the penis or penectomy is sometimes used in feminization treatment. This can be performed along with an orchiectomy and scrotectomy.
However, a total penectomy is not commonly used in feminizing surgeries . Instead, many people opt for penile-inversion surgery, a technique that hollows out the penis and repurposes the tissue to create a vagina during vaginoplasty.
Orchiectomy and Scrotectomy
An orchiectomy is a surgery to remove the testicles —male reproductive organs that produce sperm. Scrotectomy is surgery to remove the scrotum, that sac just below the penis that holds the testicles.
However, some people opt to retain the scrotum. Scrotum skin can be used in vulvoplasty or vaginoplasty, surgeries to construct a vulva or vagina.
Other Surgical Options
Some gender non-conforming people opt for other types of surgeries. This can include:
- Gender nullification procedures
- Penile preservation vaginoplasty
- Vaginal preservation phalloplasty
Gender Nullification
People who are agender or asexual may opt for gender nullification, sometimes called nullo. This involves the removal of all sex organs. The external genitalia is removed, leaving an opening for urine to pass and creating a smooth transition from the abdomen to the groin.
Depending on the person's sex assigned at birth, nullification surgeries can include:
- Breast tissue removal
- Nipple and areola augmentation or removal
Penile Preservation Vaginoplasty
Some gender non-conforming people assigned male at birth want a vagina but also want to preserve their penis, said Dr. Wittenberg. Often, that involves taking skin from the lining of the abdomen to create a vagina with full depth.
Vaginal Preservation Phalloplasty
Alternatively, a patient assigned female at birth can undergo phalloplasty (surgery to create a penis) and retain the vaginal opening. Known as vaginal preservation phalloplasty, it is often used as a way to resolve gender dysphoria while retaining fertility.
The recovery time for a gender affirmation surgery will depend on the type of surgery performed. For example, healing for facial surgeries may last for weeks, while transmasculine bottom surgery healing may take months.
Your recovery process may also include additional treatments or therapies. Mental health support and pelvic floor physiotherapy are a few options that may be needed or desired during recovery.
Risks and Complications
The risk and complications of gender affirmation surgeries will vary depending on which surgeries you have. Common risks across procedures could include:
- Anesthesia risks
- Hematoma, which is bad bruising
- Poor incision healing
Complications from these procedures may be:
- Acute kidney injury
- Blood transfusion
- Deep vein thrombosis, which is blood clot formation
- Pulmonary embolism, blood vessel blockage for vessels going to the lung
- Rectovaginal fistula, which is a connection between two body parts—in this case, the rectum and vagina
- Surgical site infection
- Urethral stricture or stenosis, which is when the urethra narrows
- Urinary tract infection (UTI)
- Wound disruption
What To Consider
It's important to note that an individual does not need surgery to transition. If the person has surgery, it is usually only one part of the transition process.
There's also psychotherapy . People may find it helpful to work through the negative mental health effects of dysphoria. Typically, people seeking gender affirmation surgery must be evaluated by a qualified mental health professional to obtain a referral.
Some people may find that living in their preferred gender is all that's needed to ease their dysphoria. Doing so for one full year prior is a prerequisite for many surgeries.
All in all, the entire transition process—living as your identified gender, obtaining mental health referrals, getting insurance approvals, taking hormones, going through hair removal, and having various surgeries—can take years, healthcare providers explained.
A Quick Review
Whether you're in the process of transitioning or supporting someone who is, it's important to be informed about gender affirmation surgeries. Gender affirmation procedures often involve multiple surgeries, which can be masculinizing, feminizing, or gender-nullifying in nature.
It is a highly personalized process that looks different for each person and can often take several months or years. The procedures also vary regarding risks and complications, so consultations with healthcare providers and mental health professionals are essential before having these procedures.
American Society of Plastic Surgeons. Gender affirmation surgeries .
Wright JD, Chen L, Suzuki Y, Matsuo K, Hershman DL. National estimates of gender-affirming surgery in the US . JAMA Netw Open . 2023;6(8):e2330348-e2330348. doi:10.1001/jamanetworkopen.2023.30348
Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8 . Int J Transgend Health . 2022;23(S1):S1-S260. doi:10.1080/26895269.2022.2100644
Chou J, Kilmer LH, Campbell CA, DeGeorge BR, Stranix JY. Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria . Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX.0000944280.62632.8c
Human Rights Campaign. Get the facts on gender-affirming care .
Human Rights Campaign. Transgender and non-binary people FAQ .
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877–84. doi:10.21037/tau.2016.09.04
Richards JE, Hawley RS. Chapter 8: Sex Determination: How Genes Determine a Developmental Choice . In: Richards JE, Hawley RS, eds. The Human Genome . 3rd ed. Academic Press; 2011: 273-298.
Randolph JF Jr. Gender-affirming hormone therapy for transgender females . Clin Obstet Gynecol . 2018;61(4):705-721. doi:10.1097/GRF.0000000000000396
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD. Hormonal treatment strategies tailored to non-binary transgender individuals . J Clin Med . 2020;9(6):1609. doi:10.3390/jcm9061609
Van Boerum MS, Salibian AA, Bluebond-Langner R, Agarwal C. Chest and facial surgery for the transgender patient . Transl Androl Urol . 2019;8(3):219-227. doi:10.21037/tau.2019.06.18
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):248–53. doi:10.21037/tau.2019.06.12
Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML. Metoidioplasty: surgical options and outcomes in 813 cases . Front Endocrinol . 2021;12:760284. doi:10.3389/fendo.2021.760284
Al-Tamimi M, Pigot GL, van der Sluis WB, et al. The surgical techniques and outcomes of secondary phalloplasty after metoidioplasty in transgender men: an international, multi-center case series . The Journal of Sexual Medicine . 2019;16(11):1849-1859. doi:10.1016/j.jsxm.2019.07.027
Waterschoot M, Hoebeke P, Verla W, et al. Urethral complications after metoidioplasty for genital gender affirming surgery . J Sex Med . 2021;18(7):1271–9. doi:10.1016/j.jsxm.2020.06.023
Nikolavsky D, Hughes M, Zhao LC. Urologic complications after phalloplasty or metoidioplasty . Clin Plast Surg . 2018;45(3):425–35. doi:10.1016/j.cps.2018.03.013
Nota NM, den Heijer M, Gooren LJ. Evaluation and treatment of gender-dysphoric/gender incongruent adults . In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext . MDText.com, Inc.; 2000.
Carbonnel M, Karpel L, Cordier B, Pirtea P, Ayoubi JM. The uterus in transgender men . Fertil Steril . 2021;116(4):931–5. doi:10.1016/j.fertnstert.2021.07.005
Miller TJ, Wilson SC, Massie JP, Morrison SD, Satterwhite T. Breast augmentation in male-to-female transgender patients: Technical considerations and outcomes . JPRAS Open . 2019;21:63-74. doi:10.1016/j.jpra.2019.03.003
Claes KEY, D'Arpa S, Monstrey SJ. Chest surgery for transgender and gender nonconforming individuals . Clin Plast Surg . 2018;45(3):369–80. doi:10.1016/j.cps.2018.03.010
De Boulle K, Furuyama N, Heydenrych I, et al. Considerations for the use of minimally invasive aesthetic procedures for facial remodeling in transgender individuals . Clin Cosmet Investig Dermatol . 2021;14:513-525. doi:10.2147/CCID.S304032
Asokan A, Sudheendran MK. Gender affirming body contouring and physical transformation in transgender individuals . Indian J Plast Surg . 2022;55(2):179-187. doi:10.1055/s-0042-1749099
Sturm A, Chaiet SR. Chondrolaryngoplasty-thyroid cartilage reduction . Facial Plast Surg Clin North Am . 2019;27(2):267–72. doi:10.1016/j.fsc.2019.01.005
Chen ML, Reyblat P, Poh MM, Chi AC. Overview of surgical techniques in gender-affirming genital surgery . Transl Androl Urol . 2019;8(3):191-208. doi:10.21037/tau.2019.06.19
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P. Male-to-female vaginoplasty: Preecha's surgical technique . J Plast Surg Hand Surg . 2015;49(3):153-9. doi:10.3109/2000656X.2014.967253
Okoye E, Saikali SW. Orchiectomy . In: StatPearls [Internet] . Treasure Island (FL): StatPearls Publishing; 2022.
Salgado CJ, Yu K, Lalama MJ. Vaginal and reproductive organ preservation in trans men undergoing gender-affirming phalloplasty: technical considerations . J Surg Case Rep . 2021;2021(12):rjab553. doi:10.1093/jscr/rjab553
American Society of Plastic Surgeons. What should I expect during my recovery after facial feminization surgery?
American Society of Plastic Surgeons. What should I expect during my recovery after transmasculine bottom surgery?
de Brouwer IJ, Elaut E, Becker-Hebly I, et al. Aftercare needs following gender-affirming surgeries: findings from the ENIGI multicenter European follow-up study . The Journal of Sexual Medicine . 2021;18(11):1921-1932. doi:10.1016/j.jsxm.2021.08.005
American Society of Plastic Surgeons. What are the risks of transfeminine bottom surgery?
American Society of Plastic Surgeons. What are the risks of transmasculine top surgery?
Khusid E, Sturgis MR, Dorafshar AH, et al. Association between mental health conditions and postoperative complications after gender-affirming surgery . JAMA Surg . 2022;157(12):1159-1162. doi:10.1001/jamasurg.2022.3917
Related Articles
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 16 May 2017
An overview of female-to-male gender-confirming surgery
- Shane D. Morrison 1 ,
- Mang L. Chen 2 &
- Curtis N. Crane 2
Nature Reviews Urology volume 14 , pages 486–500 ( 2017 ) Cite this article
2669 Accesses
62 Citations
13 Altmetric
Metrics details
- Reconstruction
- Sexual behaviour
Gender-confirming surgery is becoming a more frequently encountered procedure for urologists, plastic surgeons, and gynaecologists
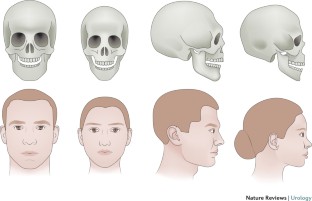
Female-to-male gender-confirming surgery consists of facial masculinization, chest masculinization, body contouring, and genital surgery
Metoidioplasty (hypertrophy with systemic hormones and mobilization of the clitoris with urethroplasty) can produce a sensate microphallus
Phalloplasty can produce an aesthetic and sensate phallus with ability to micturate in a standing position and engage in penetrative sexual intercourse if proper nerve coaptation and prosthetic insertion are performed
Urethral complications following genital surgery in transmen are generally higher than 30% and include urethral fistulas and strictures; revisional urethroplasty can address most urethral complications following genital surgery
Advances in basic sciences, transgender-specific prostheses, and patient-reported outcomes will continue to offer options for improvements in gender-confirming surgery
Gender dysphoria is estimated to occur in approximately 25 million people worldwide, and can have severe psychosocial sequelae. Medical and surgical gender transition can substantially improve quality-of-life outcomes for individuals with gender dysphoria. Individuals seeking to undergo female-to-male (FtM) transition have various surgical options available for gender confirmation, including facial and chest masculinization, body contouring, and genital surgery. The World Professional Association for Transgender Health guidelines should be met before the patient undergoes surgery, to ensure that gender-confirming surgery is appropriate and indicated. Chest masculinization and metoidioplasty or phalloplasty are the most common procedures pursued, and both generally result in high levels of patient satisfaction. Phalloplasty, with a resultant aesthetic and sensate phallus along with implantable prosthetic, can take upwards of a year to accomplish, and is associated with a considerable risk of complications. Urethral complications are most frequent, and can be addressed with revision procedures. A number of scaffolds, implants, and prostheses are now in development to improve outcomes in FtM patients.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Male-to-female gender affirmation surgery: breast reconstruction with Ergonomix round prostheses

Overview on metoidioplasty: variants of the technique

Masculinizing genital gender-affirming surgery: metoidioplasty and urethral lengthening
World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. 7th Version (World Professional Association for Transgender Health, 2011). Standards of care for transgender and gender nonconforming patients to assist all providers caring for patients within this population.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Benjamin, H. The Transsexual Phenomenon (Julian Press, 1966).
Google Scholar
Byne, W. et al . Report of the American Psychiatric Association task force on treatment of gender identity disorder. Arch. Sex. Behav. 41 , 759–796 (2012).
Article PubMed Google Scholar
Dhejne, C. et al . Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PLoS ONE 6 , e16885 (2011).
Article CAS PubMed PubMed Central Google Scholar
Dhejne, C., Oberg, K., Arver, S. & Landen, M. An analysis of all applications for sex reassignment surgery in Sweden, 1960-2010: prevalence, incidence, and regrets. Arch. Sex. Behav. 43 , 1535–1545 (2014).
Lawrence, A. A. Gender assignment dysphoria in the DSM-5. Arch. Sex. Behav. 43 , 1263–1266 (2014).
Leiter, E., Futterweit, W. & Brown, G. R. in Reconstructive Urology Vol. 2 (eds Webster, G., Kirby, R., King, L. & Goldwasser, B.) 921–932 (Blackwell Scientific Publications, 1993).
Winter, S. et al . Transgender people: health at the margins of society. Lancet 388 , 390–400 (2016). Evaluation of the difficulties experienced by transgender patients in seeking healthcare.
Wylie, K. et al . Serving transgender people: clinical care considerations and service delivery models in transgender health. Lancet 388 , 401–411 (2016).
Gooren, L. J. Clinical practice. Care of transsexual persons. N. Engl. J. Med. 364 , 1251–1257 (2011).
Article CAS PubMed Google Scholar
Deutsch, M. B. et al . Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J. Am. Med. Inform. Assoc. 20 , 700–703 (2013).
Article PubMed PubMed Central Google Scholar
Morrison, S. D. The care transition in plastic surgery. Plast. Reconstr. Surg. 136 , 861e–862e (2015).
Morrison, S. D. & Swanson, J. W. Surgical justice. Plast. Reconstr. Surg. 136 , 291e–292e (2015).
De Cuypere, G., Elaut, E. & Heylens, G. Long-term follow-up: psychosocial outcome of Belgian transsexuals after sex reassignment surgery. Sexologies 15 , 126–133 (2006).
Article Google Scholar
De Cuypere, G. et al . Sexual and physical health after sex reassignment surgery. Arch. Sex. Behav. 34 , 679–690 (2005).
Hage, J. J. & Karim, R. B. Ought GIDNOS get nought? Treatment options for nontranssexual gender dysphoria. Plast. Reconstr. Surg. 105 , 1222–1227 (2000).
Lawrence, A. A. Sexuality before and after male-to-female sex reassignment surgery. Arch. Sex. Behav. 34 , 147–166 (2005).
Wierckx, K. et al . Sexual desire in female-to-male transsexual persons: exploration of the role of testosterone administration. Eur. J. Endocrinol. 165 , 331–337 (2011).
Wierckx, K. et al . Sexual desire in trans persons: associations with sex reassignment treatment. J. Sex. Med. 11 , 107–118 (2014). Evaluation of the sexual desires experienced by transgender patients after gender-confirming surgery.
Wierckx, K. et al . Long-term evaluation of cross-sex hormone treatment in transsexual persons. J. Sex. Med. 9 , 2641–2651 (2012).
Wierckx, K. et al . Quality of life and sexual health after sex reassignment surgery in transsexual men. J. Sex. Med. 8 , 3379–3388 (2011).
Zaker-Shahrak, A., Chio, L. W., Isaac, R. & Tescher, J. Economic impact assessment: Gender nondiscrimination in health insurance. (ed. Department of Insurance) (State of California, 2012).
Monstrey, S. et al . Surgical therapy in transsexual patients: a multi-disciplinary approach. Acta Chir. Belg. 101 , 200–209 (2001).
CAS PubMed Google Scholar
Selvaggi, G., Dhejne, C., Landen, M. & Elander, A. The 2011 WPATH standards of care and penile reconstruction in female-to-male transsexual individuals. Adv. Urol. 2012 , 581712 (2012).
Gooren, L. J. Management of female-to-male transgender persons: medical and surgical management, life expectancy. Curr. Opin. Endocrinol. Diabetes Obes. 21 , 233–238 (2014).
Davis, S. R. et al . Testosterone for low libido in postmenopausal women not taking estrogen. N. Engl. J. Med. 359 , 2005–2017 (2008).
Gooren, L. J. & Giltay, E. J. Review of studies of androgen treatment of female-to-male transsexuals: effects and risks of administration of androgens to females. J. Sex. Med. 5 , 765–776 (2008).
Gooren, L. J., Giltay, E. J. & Bunck, M. C. Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience. J. Clin. Endocrinol. Metab. 93 , 19–25 (2008).
Mueller, A. & Gooren, L. Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. Eur. J. Endocrinol. 159 , 197–202 (2008).
Van Caenegem, E. et al . Bone mass, bone geometry, and body composition in female-to-male transsexual persons after long-term cross-sex hormonal therapy. J. Clin. Endocrinol. Metab. 97 , 2503–2511 (2012).
Monstrey, S. J., Ceulemans, P. & Hoebeke, P. Sex reassignment surgery in the female-to-male transsexual. Semin. Plast. Surg. 25 , 229–244 (2011).
Morrison, S. D., Perez, M. G., Carter, C. K. & Crane, C. N. Pre- and post-operative care with associated intra-operative techniques for phalloplasty in female-to-male patients. Urol. Nurs. 35 , 134–138 (2015).
Morrison, S. D., Perez, M. G., Nedelman, M. & Crane, C. N. Current state of female-to-male gender confirming surgery. Curr. Sex. Health Rep. 7 , 38–48 (2015).
Selvaggi, G. & Bellringer, J. Gender reassignment surgery: an overview. Nat. Rev. Urol. 8 , 274–282 (2011).
Morrison, S. D. et al . Educational exposure to transgender patient care in plastic surgery training. Plast. Reconstr. Surg. 138 , 944–953 (2016). Evaluation of resident exposure to transgender patient care in plastic surgery.
Obedin-Maliver, J. et al . Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA 306 , 971–977 (2011).
Dy, G. W. et al . Exposure to and attitudes regarding transgender education among urology residents. J. Sex. Med. 13 , 1466–1472 (2016). Evaluation of resident exposure to transgender patient care in urology.
Morrison, S. D. et al . Facial feminization: systematic review of the literature. Plast. Reconstr. Surg. 137 , 1759–1770 (2016).
Ousterhout, D. K. Dr. Paul Tessier and facial skeletal masculinization. Ann. Plast. Surg. 67 , S10–S15 (2011).
Deschamps-Braly, J. C., Sacher, C. L., Fick, J. & Ousterhout, D. K. First female-to-male facial confirmation surgery with description of a new procedure for masculinization of the thyroid cartilage (Adam's apple). Plast. Reconstr. Surg. 139 , 883e–887e (2017). First report of facial masculinization in transmen.
Monstrey, S. et al . Chest-wall contouring surgery in female-to-male transsexuals: a new algorithm. Plast. Reconstr. Surg. 121 , 849–859 (2008). Algorithmic approach to chest wall masculinization.
Richards, C. & Barrett, J. The case for bilateral mastectomy and male chest contouring for the female-to-male transsexual. Ann. R. Coll. Surg. Engl. 95 , 93–95 (2013).
Berry, M. G., Curtis, R. & Davies, D. Female-to-male transgender chest reconstruction: a large consecutive, single-surgeon experience. J. Plast. Reconstr. Aesthet. Surg. 65 , 711–719 (2012).
Colic, M. M. & Colic, M. M. Circumareolar mastectomy in female-to-male transsexuals and large gynecomastias: a personal approach. Aesthetic Plast. Surg. 24 , 450–454 (2000).
Nelson, L., Whallett, E. J. & McGregor, J. C. Transgender patient satisfaction following reduction mammaplasty. J. Plast. Reconstr. Aesthet. Surg. 62 , 331–334 (2009).
Vukadinovic, V., Stojanovic, B., Majstorovic, M. & Milosevic, A. The role of clitoral anatomy in female to male sex reassignment surgery. ScientificWorldJournal 2014 , 437378 (2014).
Weyers, S. et al . Gynaecological aspects of the treatment and follow-up of transsexual men and women. Facts Views Vis. Obgyn. 2 , 35–54 (2010).
CAS PubMed PubMed Central Google Scholar
Ergeneli, M. H., Duran, E. H., Ozcan, G. & Erdogan, M. Vaginectomy and laparoscopically assisted vaginal hysterectomy as adjunctive surgery for female-to-male transsexual reassignment: preliminary report. Eur. J. Obstet. Gynecol. Reprod. Biol. 87 , 35–37 (1999).
Weyers, S., Selvaggi, G. & Monstrey, S. Two-stage versus one-stage sex reassignment surgery in female-to-male transsexual individuals. Gynecol. Surg. 3 , 190–194 (2006).
Morrison, S. D. et al . Phalloplasty: a review of techniques and outcomes. Plast. Reconstr. Surg. 138 , 594–615 (2016). Contemporary evaluation of techniques and outcomes of phalloplasty.
Perrone, A. M. et al . Hysterectomy and bilateral salpingoovariectomy in a transsexual subject without visible scaring. Diagn. Ther. Endosc. 2010 , 845029 (2010).
Chen, Y. J. et al . Single-port compared with conventional laparoscopic-assisted vaginal hysterectomy: a randomized controlled trial. Obstet. Gynecol. 117 , 906–912 (2011).
Bogliolo, S. et al . Robotic single-site surgery for female-to-male transsexuals: preliminary experience. ScientificWorldJournal 2014 , 674579 (2014).
Obedin-Maliver, J., Light, A., Dehaan, G., Steinauer, J. & Jackson, R. Vaginal hysterectomy as a viable option for female-to-male transgender men. Obstet. Gynecol. 123 (Suppl. 1), 126S–127S (2014).
Djordjevic, M. L. et al . Urethral lengthening in metoidioplasty (female-to-male sex reassignment surgery) by combined buccal mucosa graft and labia minora flap. Urology 74 , 349–353 (2009).
Djordjevic, M. L. & Bizic, M. R. Comparison of two different methods for urethral lengthening in female to male (metoidioplasty) surgery. J. Sex. Med. 10 , 1431–1438 (2013). Assessment of outcomes of urethral lengthening following metoidioplasty.
Zhang, Y. F. et al . Is vaginal mucosal graft the excellent substitute material for urethral reconstruction in female-to-male transsexuals? World J. Urol. 33 , 2115–2123 (2015).
Hage, J. J. & Bloem, J. J. Review of the literature on construction of a neourethra in female-to-male transsexuals. Ann. Plast. Surg. 30 , 278–286 (1993).
Hage, J. J., Bouman, F. G. & Bloem, J. J. Construction of the fixed part of the neourethra in female-to-male transsexuals: experience in 53 patients. Plast. Reconstr. Surg. 91 , 904–910 (1993).
Rohrmann, D. & Jakse, G. Urethroplasty in female-to-male transsexuals. Eur. Urol. 44 , 611–614 (2003).
Selvaggi, G. & Elander, A. Penile reconstruction/formation. Curr. Opin. Urol. 18 , 589–597 (2008).
Salgado, C. J., Chim, H., Tang, J. C., Monstrey, S. J. & Mardini, S. Penile reconstruction. Semin. Plast. Surg. 25 , 221–228 (2011).
Hage, J. J. & De Graaf, F. H. Addressing the ideal requirements by free flap phalloplasty: some reflections on refinements of technique. Microsurgery 14 , 592–598 (1993).
Monstrey, S. et al . Penile reconstruction: is the radial forearm flap really the standard technique? Plast. Reconstr. Surg. 124 , 510–518 (2009). Largest evaluation of outcomes of RFFF phalloplasty.
Zhang, W. R., Garrett, G. L., Arron, S. T. & Garcia, M. M. Laser hair removal for genital gender affirming surgery. Transl Androl. Urol. 5 , 381–387 (2016).
Durfee, R. & Rowland, W. in Proceedings of the Second Interdisciplinary Symposium on Gender Dysphoria Syndrome (eds Laub, D. R. & Gandy, P.) 181–183 (Stanford Univ. Press, 1973).
Lebovic, G. S. & Laub, D. R. in Reconstructive and Plastic Surgery of the External Genitalia (eds Ehrlich, R. M. & Alter, G. J.) 355–360 (WB Saunders, 1999).
Hage, J. J. Metaidoioplasty: an alternative phalloplasty technique in transsexuals. Plast. Reconstr. Surg. 97 , 161–167 (1996).
Hage, J. J. & van Turnhout, A. A. Long-term outcome of metaidoioplasty in 70 female-to-male transsexuals. Ann. Plast. Surg. 57 , 312–316 (2006).
Oakley, S. H. et al . Innervation and histology of the clitoral-urethal complex: a cross-sectional cadaver study. J. Sex. Med. 10 , 2211–2218 (2013).
Djordjevic, M. L. et al . Metoidioplasty as a single stage sex reassignment surgery in female transsexuals: Belgrade experience. J. Sex. Med. 6 , 1306–1313 (2009).
Perovic, S. V. & Djordjevic, M. L. Metoidioplasty: a variant of phalloplasty in female transsexuals. BJU Int. 92 , 981–985 (2003).
Takamatsu, A. & Harashina, T. Labial ring flap: a new flap for metaidoioplasty in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62 , 318–325 (2009).
Bogoras, N. Über die volle plastische Wiederherstellung eines zum Koitus fähigen Penis (Peniplastica totalis) [German]. Zentralbl. Chir. 63 , 1271–1276 (1936).
Gillies, H. & Millard, R. The Principles and Art of Plastic Surgery Vol. II 369–388 (Little, Brown and Company, 1957).
Kaplan, I. A rapid method for constructing a functional sensitive penis. Br. J. Plast. Surg. 24 , 342–344 (1971).
Puckett, C. L., Reinisch, J. F. & Montie, J. E. Free flap phalloplasty. J. Urol. 128 , 294–297 (1982).
Hu, W. et al . A preliminary report of penile transplantation: part 2. Eur. Urol. 50 , 1115–1116 (2006).
Hu, W. et al . A preliminary report of penile transplantation. Eur. Urol. 50 , 851–853 (2006).
Morrison, S. D. et al . Penile replantation: a retrospective analysis of outcomes and complications. J. Reconstr. Microsurg. 33 , 227–232 (2017).
Monstrey, S. et al . Radial forearm phalloplasty: a review of 81 cases. Eur. J. Plast. Surg. 28 , 206–212 (2005).
Bettocchi, C., Ralph, D. J. & Pryor, J. P. Pedicled pubic phalloplasty in females with gender dysphoria. BJU Int. 95 , 120–124 (2005).
Shaeer, O. & El-Sebaie, A. Construction of neoglans penis: a new sculpturing technique from rectus abdominis myofascial flap. J. Sex. Med. 2 , 259–265 (2005).
Terrier, J. E., Courtois, F., Ruffion, A. & Morel Journel, N. Surgical outcomes and patients' satisfaction with suprapubic phalloplasty. J. Sex. Med. 11 , 288–298 (2014).
Alanis, S. Z. An innovation in total penis reconstruction. Plast. Reconstr. Surg. 43 , 418–422 (1969).
Davies, D. Phalloplasty. S. Afr. Med. J. 31 , 990–991 (1957).
Davies, D. M. & Matti, B. A. A method of phalloplasty using the deep inferior epigastric flap. Br. J. Plast. Surg. 41 , 165–168 (1988).
Dubin, B. J., Sato, R. M. & Laub, D. R. Results of phalloplasty. Plast. Reconstr. Surg. 64 , 163–170 (1979).
Santi, P. et al . Immediate reconstruction of the penis using an inferiorly based rectus abdominis myocutaneous flap. Plast. Reconstr. Surg. 81 , 961–964 (1988).
Zhang, Y., Lu, L., Zhang, W., Jiang, H. & Zhu, X. A simple and effective method for phalloplasty in female-to-male transsexuals. Plast. Reconstr. Surg. 126 , 264e–265e (2010).
Lumen, N., Hoebeke, P. & Oosterlinck, W. Urethroplasty for urethral strictures: quality assessment of an in-home algorithm. Int. J. Urol. 17 , 167–174 (2010).
Krauss, E. M., Tung, T. H. & Moore, A. M. Free functional muscle transfers to restore upper extremity function. Hand Clin. 32 , 243–256 (2016).
Ranno, R. et al . Neo-phalloplasty with re-innervated latissimus dorsi free flap: a functional study of a novel technique. Acta Chir. Plast. 49 , 3–7 (2007).
Ranno, R., Hyza, P., Vesely, J., Dessy, L. A. & Kadanka, Z. An objective evaluation of contraction power of neo-phallus reconstructed with free re-innervated LD in female-to-male transsexuals. Acta Chir. Plast. 49 , 8–12 (2007).
Mori, R. L. & Angermeier, K. W. Staged urethroplasty in the management of complex anterior urethral stricture disease. Transl Androl. Urol. 4 , 29–34 (2015).
PubMed PubMed Central Google Scholar
Djordjevic, M. L., Bumbasirevic, M. Z., Vukovic, P. M., Sansalone, S. & Perovic, S. V. Musculocutaneous latissimus dorsi free transfer flap for total phalloplasty in children. J. Pediatr. Urol. 2 , 333–339 (2006).
Lin, C. T. & Chen, L. W. Using a free thoracodorsal artery perforator flap for phallic reconstruction — a report of surgical technique. J. Plast. Reconstr. Aesthet. Surg. 62 , 402–408 (2009).
Perovic, S. V., Djinovic, R., Bumbasirevic, M., Djordjevic, M. & Vukovic, P. Total phalloplasty using a musculocutaneous latissimus dorsi flap. BJU Int. 100 , 899–905 (2007).
Vesely, J. et al . New technique of total phalloplasty with reinnervated latissimus dorsi myocutaneous free flap in female-to-male transsexuals. Ann. Plast. Surg. 58 , 544–550 (2007).
Kessler, T. M. et al . Long-term results of surgery for urethral stricture: a statistical analysis. J. Urol. 170 , 840–844 (2003).
Mathur, R. K. et al . Single-stage preputial skin flap urethroplasty for long-segment urethral strictures: evaluation and determinants of success. BJU Int. 113 , 120–126 (2014).
Taguchi, H., Saito, K. & Yamada, T. A simple method of total reconstruction of the penis. Case reports. Plast. Reconstr. Surg. 60 , 454–456 (1977).
Hage, J. J., Winters, H. A. & Van Lieshout, J. Fibula free flap phalloplasty: modifications and recommendations. Microsurgery 17 , 358–365 (1996).
Sadove, R. C., Sengezer, M., McRoberts, J. W. & Wells, M. D. One-stage total penile reconstruction with a free sensate osteocutaneous fibula flap. Plast. Reconstr. Surg. 92 , 1314–1323 (1993).
McRoberts, J. W. & Sadove, R. C. Penile reconstruction with a free sensate osteocutaneous fibula flap in the surgical management of the intersex patient. Adv. Exp. Med. Biol. 511 , 283–287 (2002).
Sengezer, M., Ozturk, S., Deveci, M. & Odabasi, Z. Long-term follow-up of total penile reconstruction with sensate osteocutaneous free fibula flap in 18 biological male patients. Plast. Reconstr. Surg. 114 , 439–450 (2004).
Dabernig, J., Chan, L. K. & Schaff, J. Phalloplasty with free (septocutaneous) fibular flap sine fibula. J. Urol. 176 , 2085–2088 (2006).
Papadopulos, N. A., Schaff, J. & Biemer, E. The use of free prelaminated and sensate osteofasciocutaneous fibular flap in phalloplasty. Injury 39 (Suppl. 3), S62–S67 (2008).
Salgado, C. J., Rampazzo, A., Xu, E. & Chen, H. C. Treatment of dyspareunia by creation of a pseudojoint in rigid bone following total penile reconstruction with fibular osteocutaneous flap. J. Sex. Med. 5 , 2947–2950 (2008).
Sun, G. C. & Huang, J. J. One-stage reconstruction of the penis with composite iliac crest and lateral groin skin flap. Ann. Plast. Surg. 15 , 519–528 (1985).
Cutting, C. B. & McCarthy, J. G. Comparison of residual osseous mass between vascularized and nonvascularized onlay bone transfers. Plast. Reconstr. Surg. 72 , 672–675 (1983).
Weiland, A. J., Phillips, T. W. & Randolph, M. A. Bone grafts: a radiologic, histologic, and biomechanical model comparing autografts, allografts, and free vascularized bone grafts. Plast. Reconstr. Surg. 74 , 368–379 (1984).
Zielinski, T. Phalloplasty using a lateral groin flap in female-to-male transsexuals. Acta Chir. Plast. 41 , 15–19 (1999).
Akoz, T., Erdogan, B., Gorgu, M., Kapucu, M. R. & Kargi, E. Penile reconstruction in children using a double vascular pedicle composite groin flap. Scand. J. Urol. Nephrol. 32 , 225–230 (1998).
Akoz, T. & Kargi, E. Phalloplasty in a female-to-male transsexual using a double-pedicle composite groin flap. Ann. Plast. Surg. 48 , 423–427 (2002).
Puckett, C. L. & Montie, J. E. Construction of male genitalia in the transsexual, using a tubed groin flap for the penis and a hydraulic inflation device. Plast. Reconstr. Surg. 61 , 523–530 (1978).
Felici, N. & Felici, A. A new phalloplasty technique: the free anterolateral thigh flap phalloplasty. J. Plast. Reconstr. Aesthet. Surg. 59 , 153–157 (2006).
Lee, G. K., Lim, A. F. & Bird, E. T. A novel single-flap technique for total penile reconstruction: the pedicled anterolateral thigh flap. Plast. Reconstr. Surg. 124 , 163–166 (2009).
Hasegawa, K., Namba, Y. & Kimata, Y. Phalloplasty with an innervated island pedicled anterolateral thigh flap in a female-to-male transsexual. Acta Med. Okayama 67 , 325–331 (2013).
PubMed Google Scholar
Morrison, S. D. et al . Modification of the tube-in-tube pedicled anterolateral thigh flap for total phalloplasty: the mushroom flap. Ann. Plast. Surg. 72 (Suppl. 1), S22–S26 (2014).
Mutaf, M. A new surgical procedure for phallic reconstruction: Istanbul flap. Plast. Reconstr. Surg. 105 , 1361–1370 (2000).
Hoebeke, P. B. et al . Erectile implants in female-to-male transsexuals: our experience in 129 patients. Eur. Urol. 57 , 334–340 (2010).
Lumen, N. et al . Erectile implants in female-to-male transsexuals: our experience in 130 patients [abstract]. Eur. Urol. Suppl. 7 , 117 (2008).
Neuville, P. et al . Surgical outcomes of erectile implants after phalloplasty: retrospective analysis of 95 procedures. J. Sex. Med. 13 , 1758–1764 (2016). Recent evaluation of outcomes of prosthetics in phalloplasty.
Gurjala, A. N., Nazerali, R. S., Salim, A. & Lee, G. K. World's first baby born through natural insemination by father with total phalloplasty reconstruction. Ann. Plast. Surg. 76 (Suppl. 3), S179–S183 (2016).
Sinove, Y. et al . Preoperative planning of a pedicled anterolateral thigh (ALT) flap for penile reconstruction with the multidetector CT scan. Handchir. Mikrochir. Plast. Chir. 45 , 217–222 (2013).
Liu, C. Y., Wei, Z. R., Jiang, H., Zhao, Y. Z. & Zhang, Y. F. Preconstruction of the pars pendulans urethrae for phalloplasty with digestive mucosa using a prefabricated anterolateral thigh flap in a one-arm patient. Plast. Reconstr. Surg. Glob. Open 1 , e53 (2013).
Rubino, C. et al . Innervated island pedicled anterolateral thigh flap for neo-phallic reconstruction in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62 , e45–e49 (2009).
Chang, T. S. & Hwang, W. Y. Forearm flap in one-stage reconstruction of the penis. Plast. Reconstr. Surg. 74 , 251–258 (1984).
Monstrey, S. et al . Radial Forearm Phalloplasty: a Review of 91 Cases. ANIR-ANHP 6 , 193–199 (2004).
Selvaggi, G. et al . Genital sensitivity after sex reassignment surgery in transsexual patients. Ann. Plast. Surg. 58 , 427–433 (2007). Evaluation of genital sensitivity following phalloplasty for transmen.
Fang, R. H., Kao, Y. S., Ma, S. & Lin, J. T. Phalloplasty in female-to-male transsexuals using free radial osteocutaneous flap: a series of 22 cases. Br. J. Plast. Surg. 52 , 217–222 (1999).
Kim, S. K. et al . The etiology and treatment of the softened phallus after the radial forearm osteocutaneous free flap phalloplasty. Arch. Plast. Surg. 39 , 390–396 (2012).
Trost, L., Wanzek, P. & Bailey, G. A practical overview of considerations for penile prosthesis placement. Nat. Rev. Urol. 13 , 33–46 (2016).
Biemer, E. Penile construction by the radial arm flap. Clin. Plast. Surg. 15 , 425–430 (1988).
Doornaert, M. et al . Penile reconstruction with the radial forearm flap: an update. Handchir. Mikrochir. Plast. Chir. 43 , 208–214 (2011).
Matti, B. A., Matthews, R. N. & Davies, D. M. Phalloplasty using the free radial forearm flap. Br. J. Plast. Surg. 41 , 160–164 (1988).
Salgado, C. J. et al . Immediate pedicled gracilis flap in radial forearm flap phalloplasty for transgender male patients to reduce urinary fistula. J. Plast. Reconstr. Aesthet. Surg. 69 , 1551–1557 (2016).
Selvaggi, G. et al . Donor-site morbidity of the radial forearm free flap after 125 phalloplasties in gender identity disorder. Plast. Reconstr. Surg. 118 , 1171–1177 (2006).
Bardsley, A. F., Soutar, D. S., Elliot, D. & Batchelor, A. G. Reducing morbidity in the radial forearm flap donor site. Plast. Reconstr. Surg. 86 , 287–292 (1990).
Boorman, J. G., Brown, J. A. & Sykes, P. J. Morbidity in the forearm flap donor arm. Br. J. Plast. Surg. 40 , 207–212 (1987).
Richardson, D., Fisher, S. E., Vaughan, E. D. & Brown, J. S. Radial forearm flap donor-site complications and morbidity: a prospective study. Plast. Reconstr. Surg. 99 , 109–115 (1997).
Van Caenegem, E. et al . Long-term evaluation of donor-site morbidity after radial forearm flap phalloplasty for transsexual men. J. Sex. Med. 10 , 1644–1651 (2013).
Rieger, U. M. et al . Comparative study of the free microvascular groin flap: optimizing the donor site after free radial forearm flap phalloplasty. Urology 95 , 192–196 (2016).
Fang, R. H., Lin, J. T. & Ma, S. Phalloplasty for female transsexuals with sensate free forearm flap. Microsurgery 15 , 349–352 (1994).
Gottlieb, L. J. & Levine, L. A. A new design for the radial forearm free-flap phallic construction. Plast. Reconstr. Surg. 92 , 276–283 (1993).
Hage, J. J., Bouman, F. G., de Graaf, F. H. & Bloem, J. J. Construction of the neophallus in female-to-male transsexuals: the Amsterdam experience. J. Urol. 149 , 1463–1468 (1993).
Kim, S. K., Lee, K. C., Kwon, Y. S. & Cha, B. H. Phalloplasty using radial forearm osteocutaneous free flaps in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62 , 309–317 (2009).
Koshima, I., Tai, T. & Yamasaki, M. One-stage reconstruction of the penis using an innervated radial forearm osteocutaneous flap. J. Reconstr. Microsurg. 3 , 19–26 (1986).
Leriche, A. et al . Long-term outcome of forearm flee-flap phalloplasty in the treatment of transsexualism. BJU Int. 101 , 1297–1300 (2008).
Ma, S., Cheng, K. & Liu, Y. Sensibility following innervated free radial forearm flap for penile reconstruction. Plast. Reconstr. Surg. 127 , 235–241 (2011).
Ma, S., Liu, Y., Chang, T. & Cheng, K. Long-term follow-up of sensation recovery of the penis reconstructed by Cheng's method. Plast. Reconstr. Surg. 127 , 1546–1552 (2011).
Papadopulos, N. A., Schaff, J. & Biemer, E. Usefulness of free sensate osteofasciocutaneous forearm and fibula flaps for neophallus construction. J. Reconstr. Microsurg. 17 , 407–412 (2001).
Sasaki, K., Nozaki, M., Morioka, K. & Huang, T. T. Penile reconstruction: combined use of an innervated forearm osteocutaneous flap and big toe pulp. Plast. Reconstr. Surg. 104 , 1054–1058 (1999).
Song, C., Wong, M., Wong, C. H. & Ong, Y. S. Modifications of the radial forearm flap phalloplasty for female-to-male gender reassignment. J. Reconstr. Microsurg. 27 , 115–120 (2011).
Vriens, J. P., Acosta, R., Soutar, D. S. & Webster, M. H. Recovery of sensation in the radial forearm free flap in oral reconstruction. Plast. Reconstr. Surg. 98 , 649–656 (1996).
Waits, C. A., Toby, E. B., Girod, D. A. & Tsue, T. T. Osteocutaneous radial forearm free flap: long-term radiographic evaluation of donor site morbidity after prophylactic plating of radius. J. Reconstr. Microsurg. 23 , 367–372 (2007).
Ma, S., Cheng, K., Liu, Y. & Chen, F. A new surgical procedure for penile reconstruction by combined free radial forearm flap and dorsalis pedis flap. Urology 97 , 232–237 (2016).
Hoebeke, P., de Cuypere, G., Ceulemans, P. & Monstrey, S. Obtaining rigidity in total phalloplasty: experience with 35 patients. J. Urol. 169 , 221–223 (2003).
Selvaggi, G. et al . Scrotal reconstruction in female-to-male transsexuals: a novel scrotoplasty. Plast. Reconstr. Surg. 123 , 1710–1718 (2009). Presentation of the novel technique for transman scrotoplasty.
Hage, J. J., Bouman, F. G. & Bloem, J. J. Constructing a scrotum in female-to-male transsexuals. Plast. Reconstr. Surg. 91 , 914–921 (1993).
Millard, D. R. Jr. Scrotal construction and reconstruction. Plast. Reconstr. Surg. 38 , 10–15 (1966).
Reid, C. F. & Wright, J. H. Jr. Scrotal reconstruction following an avulsion injury. J. Urol. 133 , 681–682 (1985).
Sengezer, M. & Sadove, R. C. Scrotal construction by expansion of labia majora in biological female transsexuals. Ann. Plast. Surg. 31 , 372–376 (1993).
Still, E. F. II & Goodman, R. C. Total reconstruction of a two-compartment scrotum by tissue expansion. Plast. Reconstr. Surg. 85 , 805–807 (1990).
Lumen, N., Monstrey, S., Goessaert, A. S., Oosterlinck, W. & Hoebeke, P. Urethroplasty for strictures after phallic reconstruction: a single-institution experience. Eur. Urol. 60 , 150–158 (2011). Analysis of outcomes and techniques for urethral fistula and stricture repair in phalloplasty.
Wilson, S. C. et al . Fasciocutaneous flap reinforcement of ventral onlay buccal mucosa grafts enables neophallus revision urethroplasty. Ther. Adv. Urol. 8 , 331–337 (2016).
Dabernig, J., Shelley, O. P., Cuccia, G. & Schaff, J. Urethral reconstruction using the radial forearm free flap: experience in oncologic cases and gender reassignment. Eur. Urol. 52 , 547–553 (2007).
Garaffa, G., Ralph, D. J. & Christopher, N. Total urethral construction with the radial artery-based forearm free flap in the transsexual. BJU Int. 106 , 1206–1210 (2010).
Kim, S. K., Moon, J. B., Heo, J., Kwon, Y. S. & Lee, K. C. A new method of urethroplasty for prevention of fistula in female-to-male gender reassignment surgery. Ann. Plast. Surg. 64 , 759–764 (2010).
Bayramicli, M. & Akdeniz, Z. D. Urethra reconstruction with lateral pectoral flap in female-to-male transsexual patients. J. Plast. Reconstr. Aesthet. Surg. 69 , 1558–1560 (2016).
De Filippo, R. E., Yoo, J. J. & Atala, A. Urethral replacement using cell seeded tubularized collagen matrices. J. Urol. 168 , 1789–1792 (2002).
Chen, K. L., Eberli, D., Yoo, J. J. & Atala, A. Bioengineered corporal tissue for structural and functional restoration of the penis. Proc. Natl Acad. Sci. USA 107 , 3346–3350 (2010).
Joo, K. J. et al . Porcine vesical acellular matrix graft of tunica albuginea for penile reconstruction. Asian J. Androl. 8 , 543–548 (2006).
Kwon, T. G., Yoo, J. J. & Atala, A. Autologous penile corpora cavernosa replacement using tissue engineering techniques. J. Urol. 168 , 1754–1758 (2002).
Kropp, B. P. et al . Use of small intestinal submucosa for corporal body grafting in cases of severe penile curvature. J. Urol. 168 , 1742–1745 (2002).
Raya-Rivera, A. M. et al . Tissue-engineered autologous vaginal organs in patients: a pilot cohort study. Lancet 384 , 329–336 (2014).
Sopko, N. A. et al . Ex vivo model of human penile transplantation and rejection: implications for erectile tissue physiology. Eur. Urol. 71 , 584–593 (2017).
Tuffaha, S. H. et al . Using the dorsal, cavernosal, and external pudendal arteries for penile transplantation: technical considerations and perfusion territories. Plast. Reconstr. Surg. 134 , 111e–119e (2014).
Selvaggi, G., Branemark, R., Elander, A., Liden, M. & Stalfors, J. Titanium-bone-anchored penile epithesis: preoperative planning and immediate postoperative results. J. Plast. Surg. Hand. Surg. 49 , 40–44 (2015).
Selvaggi, G., Elander, A. & Branemark, R. Penile epithesis: preliminary study. Plast. Reconstr. Surg. 126 , 265e–266e (2010).
Massie, J. P., Morrison, S. D., Smith, J. R., Wilson, S. C. & Satterwhite, T. Letter to the editor regarding “Surgical outcome after penile inversion vaginoplasty: a retrospective study of 475 transgender women” by Buncamper et al . Plast. Reconstr. Surg. http://dx.doi.org/10.1097/PRS.0000000000003479 (2017).
Berli, J. U. et al . What surgeons need to know about gender confirmation surgery when providing care for transgender individuals: a review. JAMA Surg. 152 , 394–400 (2017).
Download references
Author information
Authors and affiliations.
Division of Plastic and Reconstructive Surgery, Department of Surgery, University of Washington School of Medicine, 1959 NE Pacific Street, Seattle, 98195, WA, USA
Shane D. Morrison
Brownstein & Crane Surgical Services, 575 Sir Francis Drake Blvd, Ste 1, Greenbrae, 94904, CA, USA
Mang L. Chen & Curtis N. Crane
You can also search for this author in PubMed Google Scholar
Contributions
S.D.M., C.N.C and M.C. researched data for article, made substantial contributions to discussions of content, and reviewed and edited the manuscript before submission. S.D.M. and M.C. wrote the article.
Corresponding author
Correspondence to Curtis N. Crane .
Ethics declarations
Competing interests.
The authors declare no competing financial interests.
PowerPoint slides
Powerpoint slide for fig. 1, powerpoint slide for fig. 2, powerpoint slide for fig. 3, powerpoint slide for fig. 4, powerpoint slide for fig. 5, powerpoint slide for fig. 6, powerpoint slide for fig. 7, powerpoint slide for table 1.
Inherent discordance of a patient's gender expression and their anatomy leading to distress
Tissue forming the nipple and surrounding areola on the breast or chest
A physical examination test to determine the patency of the palmar or plantar arches as a correlate for the dominant inflow vessel to the hand or foot. Most commonly it is used in the hand where the radial and ulnar arteries are both occluded with pressure from the examiners hand and each is released sequentially while maintaining the pressure on the other artery. The perfusion of the hand is monitored to ensure both vessels can perfuse the hand.
A person born as a male and whose gender identity is male.
Urological procedure for urethral strictures, in which the ventral aspect of the phallus is opened through the urethra. The urethra is secured to the skin and urine is diverted. A second stage completed months later is used to repair the urethra with grafted tissue over a catheter.
Flaps containing multiple tissue types (skin, bone, mucosa.) based on a single angiosome used for complex reconstruction.
Local flap used for advancing tissue generally to cover a wound, but can be used in other procedures. An incision shaped like a V is made through the subcutaneous tissue, advanced into its new position relying on subcutaneous perfusion, and closed in a Y pattern.
Closure of a urethral stricture with a longitudinal incision followed by a transverse closure.
A person born with female sexual organs, but whose gender identity is male
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Morrison, S., Chen, M. & Crane, C. An overview of female-to-male gender-confirming surgery. Nat Rev Urol 14 , 486–500 (2017). https://doi.org/10.1038/nrurol.2017.64
Download citation
Published : 16 May 2017
Issue Date : August 2017
DOI : https://doi.org/10.1038/nrurol.2017.64
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Geschlechtsinkongruenz – definition, diagnosestellung und transitionsoptionen.
- Antje Feicke
- Barbara Mijuskovic
Urologie in der Praxis (2023)
(De-)centralized health care delivery, surgical outcome, and psychosocial health of transgender and gender-diverse people undergoing vaginoplasty: results of a retrospective, single-center study
- Andreas Koehler
- Bernhard Strauß
- Timo O. Nieder
World Journal of Urology (2023)
Gender Affirmation Surgery for the Transmasculine Patient
- Michael Callegari
- Gaetan Pettigrew
- Shubham Gupta
Current Obstetrics and Gynecology Reports (2022)
Urethral complications after gender reassignment surgery: a systematic review
- L. R. Doumanian
International Journal of Impotence Research (2021)
Suprapubic phalloplasty in transmen: surgical results and critical review
- Manon Terrier
- Nicolas Morel-Journel
- Paul Neuville
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Female to Male Surgery for Trans Men
As a transgender male, your goal for female to male surgery (FTM) for gender-confirmation can involve top surgery, bottom surgery, or both. You may or may not want facial procedures. It’s up to you.
Female to Male Surgery at UVA
We’re here to offer consultations, second opinions, and information to help you choose and plan. Come to us with your questions and concerns. We’ll explain:
- Procedure options and details
- Recovery and healing
- What to expect of your results
We want you to feel confident about the direction and quality of your care.
Charley's Gender-Confirmation Surgery
From a young age, Charley Burton knew that his body did not match his gender identity – a struggle he kept inside for 50 years. With the help of family nurse practitioner Reagan Thompson, FNP, MSN, RN, and a whole team of caring providers, Charley found a safe place to become his true self. View Charley's story transcript.
FTM Top Surgery
To give you a flatter chest, we’ll have to remove breast tissue. We might also need to move and shrink your areolas.
If you have smaller breasts, we can sometimes use liposuction, which doesn’t involve many incisions.
Larger breasts may require the “double incision” technique. This method saves the pectoralis major muscle, the most defining characteristic of a male chest.
Whatever your breast size, we will use the techniques that optimize the results.
FTM Bottom Surgery
We can give you male genitalia in two different ways:
- Phalloplasty creates a penis and urethra (to stand while urinating). We use tissue from your forearm or thigh. We do this in 2 stages.
- Metoidioplasty takes your existing genital tissue and makes it longer, turning it into a defined phallus. This needs only one surgery.
You may or may not want to also have an operation to remove your internal reproductive organs. A hysterectomy takes out your uterus, fallopian tubes, and ovaries.
Facial Masculinization
Through a combination of procedures, we can sculpt your chin, jaw, and cheeks to appear more masculine. We can also reshape your nose and make your Adam’s apple look bigger. We can use synthetic implants for this work.
Questions? See our transgender surgery FAQs .
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
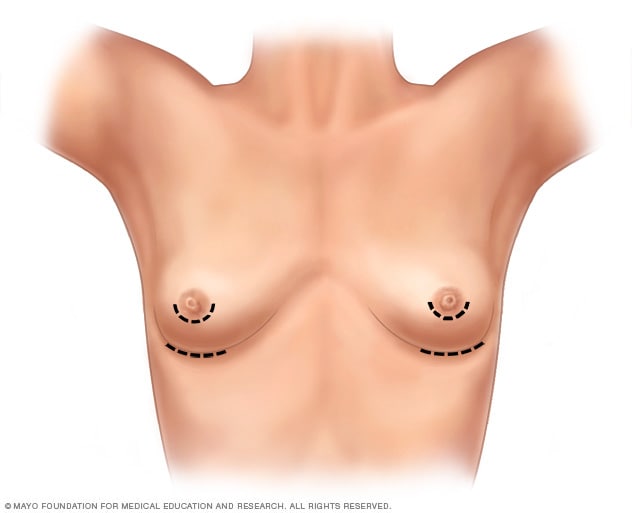
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
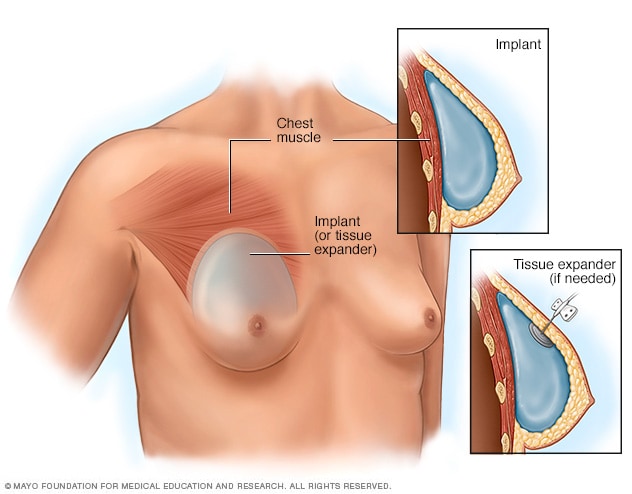
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
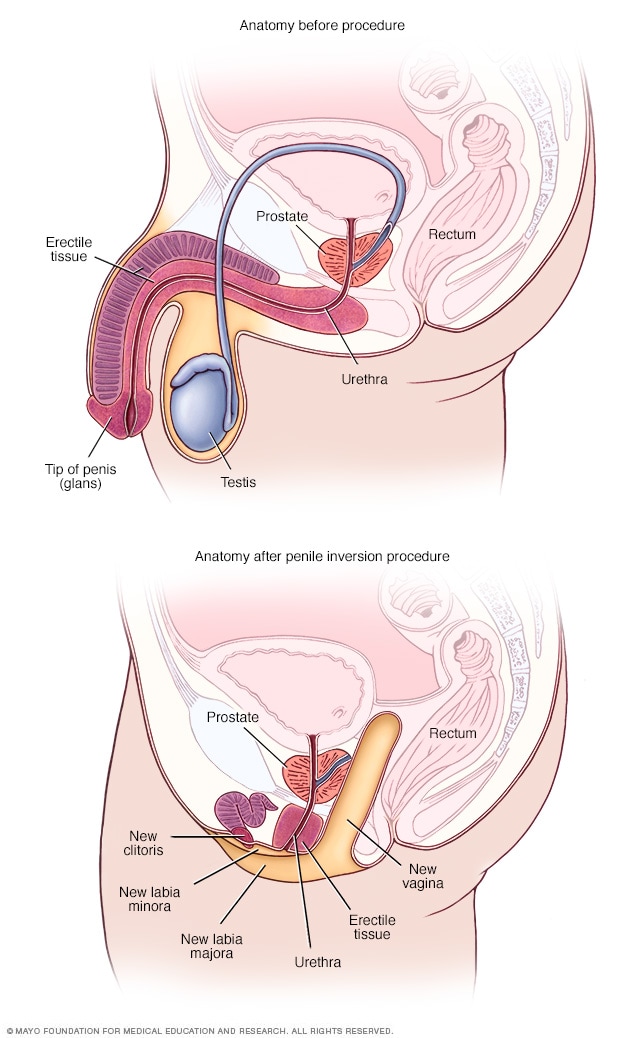
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
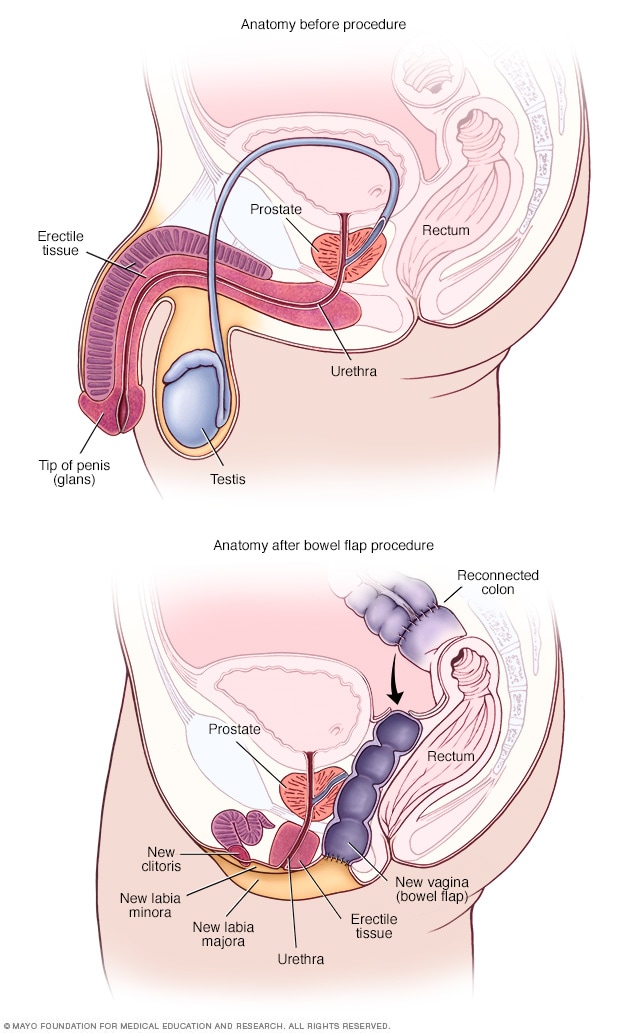
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Do I need a referral to see a specialist? Learn more here . Explore the Department Directory Learn more about Telehealth Appointments Protect Yourself from West Nile Virus
How to schedule your APPOINTMENT at Denver Health: CURRENT PATIENTS: Login to MyChart to schedule appointments or call 303-436-4949 . NEW PATIENTS: Schedule an appointment online or call 303-436-4949 . NEED CARE? Schedule a Virtual Urgent Care appointment or click here to find an Urgent Care clinic .
MyChart Login
Login to MyChart
MyChart for Mobile
Download the MyChart mobile app for access to your healthcare information. Managing your healthcare has never been more simple. Download for iPhone and Android .
MyChart Sign Up
Learn about MyChart features , and sign up for an account .
Virtual Urgent Care Now Available for Denver Health MyChart Users
Denver Health MyChart users can now have a virtual urgent care visit with one of our expert providers. It’s easy and convenient to get the urgent care you need from the comfort of your home, using your smartphone, tablet or computer.
Click here for more details

- Departments & Services
- Conditions & Treatments
- Our Locations
- Find a Provider
- Pharmacy / Prescriptions
- Pay my bill
- Main Campus (303) 436-6000
- Appointments (303) 436-4949
- Lean Academy 855-888-5326
- Nurseline (303) 739-1211
- Pharmacy (303) 389-1390
- Telehealth (303) 436-4949
Make an Appointment
Hours of operation, gender affirming surgery (sex reassignment surgery).
Thank you for your interest in gender affirming surgery at Denver Health. There is no one-size-fits-all approach for the gender affirmation process and we are here to support you in your journey. We are proud to offer surgeries with a truly talented multi-disciplinary team of surgeons. Our services are growing as the unique needs of each individual evolve. Currently we offer the following gender affirming surgeries: MTF Top Surgery , FTM Top Surgery , Orchiectomy , FTM Hysterectomy , and Vaginoplasty surgeries.
What is Gender Affirming Surgery?
Gender affirming surgery, also known as sex reassignment surgery (SRS) or confirmation surgery, is the surgical procedure(s) by which a transgender or non-binary person’s physical appearance and functional abilities are changed to align with the gender they know themselves to be.
Complete Our Surgical Interest Form
If you are interested in a gender affirmation surgery at Denver Health, please complete one of the following forms.
Top Surgery and Hysterectomy
For vaginoplasty, breast augmentation and orchiectomy, our approach to surgical assessment.
Denver Health adheres to the guidelines for surgical assessment as described in the World Professional Association for Transgender Health Standards of Care, 8th Version . The standards were created by international agreement using the latest scientific research on transgender health so that doctors can best meet the unique health care needs of transgender and gender-nonconforming people. Most insurance companies also adhere to these guidelines.
Patients may provide referral letters from their own outside mental health providers, or the assessment process via our Behavioral Health team. Patients seeking to undergo the assessment at Denver Health should make an appointment with our Behavioral Health Team .
Read more about common frequently asked general surgery questions:
How long will my hospital stay be.
Hospital stays will vary based on specific patient response.
MTF top surgery, FTM chest surgery, FTM Hysterectomy, and orchiectomy surgery patients are usually released from the hospital the same day of surgery. Vaginoplasty patients typically spend 3 days in the hospital during recovery.
What medications will I be prescribed after surgery?
You will likely receive painkillers and antibiotics to reduce the chance of infection.
- 0 && newsLoaded" class="" data-id="{044698B9-FA04-4636-994D-47662155601F}" ref="news"> News
- 0 && blogLoaded" class="" data-id="{9AB9C6CB-06BD-4D71-867F-FAB69D88F93C}" ref="blog"> Blog Articles
- 0 && storiesLoaded" class="" data-id="{71E64EA2-1956-4F7C-A67D-579E0BB54378}" ref="stories"> Patient Stories
- May 15 Labor and Delivery Tour for Expectant Families
- May 18 Boot Camp for New Dads ®
- May 22 Labor and Delivery Tour for Expectant Families
- May 29 Labor and Delivery Tour for Expectant Families
How Gender Reassignment Surgery Works (Infographic)
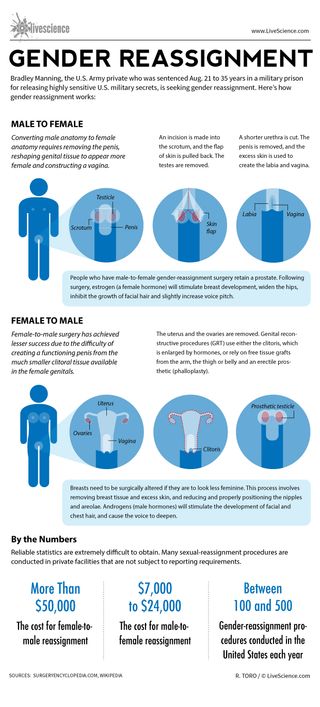
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Man's years of premature ejaculation had a rare cause
Viagra alternatives? Study of mouse erections hints at new ways to treat erectile dysfunction
Earth from space: Majestic 'yin-yang' crater sits atop a dormant volcano in Turkey
Most Popular
- 2 32 of the most colorful birds on Earth
- 3 Can mirrors facing each other create infinite reflections?
- 4 See stunning reconstruction of ancient Egyptian mummy that languished at an Australian high school for a century
- 5 New invention transforms any smartphone or TV display into a holographic projector
- 3 Space photo of the week: 'God's Hand' leaves astronomers scratching their heads
- 4 Why can't we see the far side of the moon?
- 5 Papua New Guineans, genetically isolated for 50,000 years, carry Denisovan genes that help their immune system, study suggests
clock This article was published more than 9 years ago
Here’s how sex reassignment surgery works

In this excellent post , my colleague Steven Petrow advised that if you're wondering whether someone you know is transitioning from one gender to the other, it's best to "check your curiosity and hold your tongue." But we all have questions about a subject that is increasingly mainstream. Aside from the recent coverage of Bruce Jenner 's apparent transition , Laverne Cox last year became the first trans person on the cover of Time magazine, and Amazon debuted “Transparent,” a show about a father who is transitioning.
[UPDATE: Bruce Jenner: ‘Call me Caitlyn’ ]
Here are answers to some of the questions surrounding this issue.
How many people are transgender?
The Williams Institute, a think tank at the UCLA School of Law dedicated to research on sexual orientation law and public policy, estimates that 700,000 Americans are transgender . But a good piece last year on fivethirtyeight.com noted that there are no national surveys. And if there were, there is no agreement on what "trangender" means.
How many people have sex reassignment surgery?
It's very difficult to know. The Encyclopedia of Surgery says that "the number of gender reassignment procedures conducted in the United States each year is estimated at between 100 and 500. The number worldwide is estimated to be two to five times larger." At least one other researcher says there are many more. Marci Bowers, a transgender obstetrician and gynecologist in Burlingame, Calif., who performs the surgeries, said in an interview that she does about 200 per year herself, about three quarters of them male to female.
Fred Ettner, a physician in Evanston, Ill., who works with people going through transition, estimated that only about 25 percent to 30 percent of transgender people have any kind of surgery.
How does one begin the process of changing one's sex?
Under the standards of care adopted by the World Professional Association for Transgender Health (WPATH), the first step usually is meeting with a mental health professional for a diagnosis and psychotherapy. A diagnosis of gender identity disorder or gender dysphoria and a letter of recommendation from the therapist allows a person to begin hormone therapy with a doctor. That is usually followed by a period of living publicly as a member of the opposite sex and, finally, surgery to alter the genitalia and other body parts.
What do hormones do?
Androgens are given to women to help them develop secondary male sex characteristics such as a beard and body hair. Estrogen and anti-androgens are given to men to help change their musculature, skin and fat distribution, all of which will make them appear more feminine. Body hair also diminishes.
But Ettner said the hormones' most important contribution is to reduce the dysphoria transgender people have been struggling with all their lives. After a month or two, their bodies and brains begin aligning.
"It's very obvious to the individuals," Ettner said, adding, "Their brain finally is getting this hormone. They feel differently. They behave differently.
"The first effect is the brain effect," he said.
What is the Real-Life Experience (also known as the Real-Life Test)
Surgeons who follow the WPATH standards of care (which some patients and experts consider too strict) usually require candidates for surgery to live for as long as a year in their preferred gender role. They must work or go to school; do volunteer work; change their first names and prove to the surgeon that people other than their therapists know they are successfully living this way.
What happens during surgery?
Male to female genital surgery is easier, less expensive and generally more successful than female to male surgery. That's one reason why fewer women choose to have surgery on their genitals, Bowers said. (Another is cost.)
In male to female surgery , the testicles and most of the penis are removed and the urethra is cut shorter. Some of the skin is used to fashion a largely functional vagina. A "neoclitoris" that allows sensation can be created from parts of the penis. Men retain their prostates.
In female to male surgery, the breasts, uterus and ovaries are removed (in two separate procedures). A "neophallus" can be constructed using tissue from the forearm or other parts of the body that allows sexual sensation, an expensive procedure. Extending the urethra to allow standing urination has proved to be perhaps the most difficult part of the process, Bowers said.
What other kinds of surgery are performed?
Women wishing to live as men often have mastectomies. Men transitioning to women can have plastic surgery to "feminize" their appearance, including work on their eyes, noses, brows, chins and hairlines. They also can have their Adam's apple shaved down so it is less prominent.
Sounds expensive. Is it covered by insurance?
Bowers and Ettner said a woman who chooses the full range of surgical procedures available would spend $75,000 or more to transition to a male. Switching from male to female might cost in the $40,000 to $50,000 range. Some people have the work done in Thailand, which is well known for the surgery and where the cost is much lower.
Insurance is just beginning to cover some of the costs. Last year, Medicare lifted a 33-year ban on coverage for gender reassignment surgery , and the surgery was performed on 74-year-old Army veteran .
Do many people regret having the surgery?
Anecdotal accounts of regret abound, but overall it appears to be rare. Bowers said that only two of the 1,300 people she has operated on have wanted to go back to their old bodies.
But that doesn't mean that surgery is a miracle cure for the difficulties of gender dysphoria. People who make the transition often lose spouses, families, friends and jobs. They may find themselves completely alone if they relocate to start new lives. Johns Hopkins University, which in the 1960s was one of the first medical institutions to perform sex reassignment surgery, halted the practice when officials concluded that it was not helping the transgendered overall.
A 2o11 study of 324 Swedish transsexuals by the Karolinska Institute showed that "after sex reassignment, [they] have considerably higher risks for mortality, suicidal behaviour, and psychiatric morbidity than the general population. Our findings suggest that sex reassignment, although alleviating gender dysphoria, may not suffice as treatment for transsexualism, and should inspire improved psychiatric and somatic care after sex reassignment for this patient group."
The forgotten history of Bruce Jenner
Transgender etiquette 101
Transgender at 7: Tyler gets a legal name change

- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What to Know About Metoidioplasty (Bottom Surgery)
- Who Qualifies?
- Surgical Techniques
- Neophallus Function
- Surgery Follow-Up
- Where to Have Surgery
Metoidioplasty , or "bottom surgery," is a gender-affirming surgical procedure that involves creating a neophallus (new penis) from a hormonally enlarged clitoris . Transgender men and transmasculine people assigned female at birth (AFAB) may elect for a metoidioplasty if they want their genital appearance to align with their gender identity.
In contrast to the more complex phalloplasty that involves several surgeries, metoidioplasty offers a more straightforward phallic reconstruction in one procedure.
During a metoidioplasty, a surgeon cuts the ligaments that connect the clitoris to the pubic bone to release the clitoris and create a penis with erogenous (sexual) sensations. It may also include additional steps, such as urethral lengthening and scrotoplasty (forming a scrotum), to enhance the appearance and functionality of the neophallus.
This article explores metoidioplasty surgical techniques, the recovery process, and what to expect post-surgery.
CarlosDavid.org / Getty Images
Who Qualifies for Metoidioplasty Surgery?
Metoidioplasty is a gender-affirming (sex-reassignment) surgery for transgender men assigned female at birth. According to the 2015 U.S. Transgender Survey, about 4% of trans men have undergone the procedure, while another 53% expressed a desire to undergo metoidioplasty in the future.
The World Professional Association for Transgender Health (WPATH) developed the criteria for gender reaffirmation surgeries to ensure optimal physical and psychological outcomes for those pursuing bottom (genital) surgeries. The eligibility criteria for metoidioplasty include the following:
- Ongoing and well-documented gender dysphoria
- The ability to make informed decisions and provide consent for treatment
- Being 18 years of age or older
- Medical or mental health concerns are well-managed (if applicable)
- At least 12 consecutive months of gender-affirming testosterone therapy
- Living as a male or masculine-presenting person for at least one year in all settings (e.g., work, school, with family members and community)
Though it is not required, regular visits with a mental health or other medical professional are highly recommended before undergoing a metoidioplasty.
Metoidioplasty Surgical Techniques
People can choose a few different metoidioplasty surgical techniques depending on their preferences. Other procedures can occur simultaneously (e.g., hysterectomy) if desired.
Simple Release Metoidioplasty
In the simple release procedure, ligaments attached to the pubic bone are cut and released, and the clitoris is separated from surrounding tissue to enhance the position and visibility of the clitoris. The labia minora are wrapped around the clitoris to create the glans (head) of the newly formed penis.
Ring Metoidioplasty
Similar to the simple release, this technique involves releasing the clitoral ligaments to lengthen the clitoris. This procedure also involves lengthening the urethra using a flap of tissue from the vaginal wall and labia minora. This procedure gives trans men a micropenis with more girth and the ability to stand while urinating.
Belgrade (Full) Metoidioplasty
The Belgrade technique, or full metoidioplasty, involves the removal of the vagina (vaginectomy) and releasing the clitoris to lengthen and straighten the clitoris. The urethra is lengthened using vaginal tissue and buccal mucosa (inner cheek) skin grafts. The penis is reconstructed with the remaining clitoral and labial skin to give it more girth.
Then, the labia minor flaps are joined to create a scrotum (scrotoplasty), and testicular implants may be inserted into the newly created scrotum. A penile pump or vacuum is recommended three weeks post-surgery to lengthen the neophallus and prevent retraction.
Simultaneous Procedures
In addition to metoidioplasty, some trans men may opt for additional procedures performed at the same time to achieve their desired outcomes. These procedures may include:
- Hysterectomy : Removal of the uterus
- Bilateral salpingo-oophorectomy : Removal of the ovaries and fallopian tubes
- Vaginectomy : Removal of the vagina and surrounding tissues
- Scrotoplasty : Forms a new scrotum; testicular implants may be placed to give the appearance of natural testicles
- Erectile implant : A device is placed inside the neophallus to help achieve erections
Metoidioplasty vs. Phalloplasty
Metoidioplasty and phalloplasty are surgical options for transgender men seeking gender-affirming genital reconstruction. Metoidioplasty involves using existing genital tissue, such as the hormonally enlarged clitoris, to create a neophallus. It usually results in a smaller but functional neophallus.
Phalloplasty involves constructing a neophallus using various techniques, including grafting tissue from other body parts. This procedure can provide a larger and more visually realistic phallus but is more complex and may require multiple stages. The choice between metoidioplasty and phalloplasty depends on individual preferences, desired outcomes, and considerations such as surgical risk, recovery time, and aesthetic goals.
Risks to Understand Before Metoidioplasty
While metoidioplasty is generally considered safe, like any surgical intervention, it carries certain risks. Before undergoing metoidioplasty, discuss the risks with a healthcare provider to gain a comprehensive understanding and make an informed decision.
Potential risks include:
- Urethral stricture or stenosis : Narrowing of the urethral passage, leading to difficulty with urination and potential obstruction of urine flow. Sometimes, urine flow may be blocked entirely, requiring surgery to correct the problem.
- Urethral fistula : An abnormal connection or passageway between the urethra and the skin or surrounding tissues. This can result in urine leakage or an abnormal opening along the neophallus.
- Sensation changes : The newly formed penis may have decreased or loss of sensation or feel hypersensitive and tender.
Function of Neophallus Post-Bottom Surgery
Trans men who have undergone metoidioplasty report high levels of satisfaction with the procedure's results, both in appearance and function.
While a neophallus created through metoidioplasty is usually considered a micropenis (1–4 inches), erections and orgasms are achieved by nearly all who have undergone the procedure. Penetrative sex may or may not be possible. Urinating while standing is possible for most men after metoidioplasty.
Metoidioplasty Recovery Period
The recovery period following metoidioplasty depends on the specific surgical technique and can vary from person to person. Most people can expect one week of bed rest immediately following the procedure and gradually resume their activities within about six weeks.
Initially, there will be discomfort, swelling, and bleeding in the genital region, which will gradually subside over time. You may also experience:
- Bruising in the genital area that spreads from the belly down to the legs
- Itching and short, sharp, shooting sensations as the area heals
- Numbness at or near the incision sites, which can persist for months
- Scarring on the genitals that will first appear red or pink and fade over time
Metoidioplasty Follow-Up (and Asking for Help)
You will need assistance and support during the follow-up period after metoidioplasty, as the recovery process can involve discomfort, limited mobility, and restricted activity. You will need a caretaker for at least a week or two after the procedure—someone who can help with daily tasks such as meal preparation, household chores, and running errands.
Your surgeon may restrict certain activities, such as driving, sex, and heavy lifting. You may need help with transportation to follow-up appointments for about six weeks. Most people can resume their normal activities within six weeks post-surgery. Still, getting the OK from a healthcare provider is important to ensure you are properly healed and to lower the risk of complications.
Where to Have Metoidioplasty Surgery
Specialized surgeons with experience in transgender healthcare often perform metoidioplasty surgery. The procedure is usually carried out in a hospital or surgical center with the necessary tools and equipment for the surgery. It is essential to choose a reputable medical facility that is experienced in transgender surgeries and maintains a supportive and inclusive environment.
When considering where to have metoidioplasty surgery, start by asking a mental health professional or another healthcare provider for referrals and recommendations of surgeons who specialize in the procedure. They can provide information and guidance on the options available to you.
Researching and gathering information about the surgeon's qualifications, experience, and success rates, as well as reading reviews or testimonials from other people who have undergone metoidioplasty at the facility, can also help you select the most suitable location for the surgery. Open communication with healthcare providers can ensure that all your questions and concerns are addressed before deciding where to have metoidioplasty surgery.
Metoidioplasty is a gender-affirming surgery for trans-male people assigned female at birth (AFAB). The procedure involves releasing the clitoral ligaments and utilizing the hormonally enlarged clitoris to create a neophallus (new penis).
There are a few different metoidioplasty techniques. Sometimes, people undergo simultaneous procedures, such as hysterectomy and vaginectomy. Metoidioplasty is considered a safe, effective procedure that results in a 1–4 inch functional penis that gives trans men the opportunity to align their physical characteristics with their gender identity.
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: Techniques and outcomes . Transl Androl Urol . 2019;8(3):248-253. doi:10.21037/tau.2019.06.12
Kjölhede A, Cornelius F, Huss F, Kratz G. Metoidioplasty and groin flap phalloplasty as two surgical methods for the creation of a neophallus in female-to-male gender-confirming surgery: A retrospective study comprising 123 operated patients . JPRAS Open . 2019;22:1-8. doi:10.1016/j.jpra.2019.07.003
Stojanovic B, Bencic M, Bizic M, Djordjevic ML. Metoidioplasty in gender affirmation: A review . Indian J Plast Surg . 2022;55(2):156-161. doi:10.1055/s-0041-1740081
National Center for Transgender Equality. Injustice at every turn: a report of the national transgender discrimination survey .
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people .
Heston AL, Esmonde NO, Dugi DD 3rd, Berli JU. Phalloplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):254-265. doi:10.21037/tau.2019.05.05
Alberta Medical Association. Metoidioplasty .
Bordas N, Stojanovic B, Bizic M, et al. Metoidioplasty: Surgical options and outcomes in 813 cases . Front Endocrinol (Lausanne) . 2021;12:760284. doi:10.3389/fendo.2021.760284
TransCare BC. Provincial Health Services Authority. Metoidioplasty .
Michigan Medicine: University of Michigan. What to expect: Metoidioplasty at Michigan Medicine .
TransHealthCare. Metoidioplasty - list of surgeons in the USA .
By Lindsay Curtis Curtis is a writer with over 20 years of experience focused on mental health, sexual health, cancer care, and spinal health.
- Search Close Search submit
Join our Resident Webinar this Saturday, May 18th
Female to Male Gender Reassignment Surgery (FTM GRS)
Female-to-male gender reassignment surgery (FTM GRS) is a complex and irreversible genital surgery for female transsexual who is diagnosed with gender identity disorder and has a strong desire to live as male. The procedure is to remove all female genital organs including the uterus, ovaries, and vagina with the construction of male genitalia composed of the penis and scrotum.
The patient who is fit for this surgery must strictly follow the standard of care set by the World Professional Association of Transgender Healthcare (WPATH) or equivalent criteria; Express desire or live in another gender role (Female gender) long enough, under hormonal replacement therapy, evaluated and approved by a psychiatrist or other qualified professional gender therapist.
Apart from genital surgery, the patient would seek other procedures to allow them to live as males smoothly such as breast amputation, facial surgery, body surgery, etc.
Interested in having this procedure?
Useful Information
Ensure you consider all aspects of a procedure. You can speak to your surgeon about these areas of the surgery in more detail during a consultation.
The surgery is very complicated and only a handful of surgeons are able to perform this procedure. It is a multi-staged procedure, the first stage is the removal of the uterus, ovary, and vagina. The duration of the procedure is 2-3 hours. The second and later stages are penis and scrotum reconstruction which is at least 6 months later. There are several techniques for penile reconstruction depending on the type of tissue such as skin/fat of the forearm, skin/fat of the thigh, or adjacent tissue around the clitoris. This second stage of surgical time is between 3-5 hours. A penile prosthesis can be incorporated simultaneously or at a later stage. The scrotal prosthesis is also implanted later.
The procedure is done under general anesthesia and might be combined with spinal anesthesia for faster recovery by reducing the usage of anesthetic gas.
Inpatient/Outpatient
The patient will be hospitalized as an in-patient for between 5-7 days for each stage depending on the technique and surgeon. The patient will have a urinary catheter at all times in the hospital.
Additional Information
What are the risks.
The most frequent complication of FTM GRS is bleeding, wound infection, skin flap or graft necrosis, urinary stenosis and fistula, unsightly scar, etc. The revision procedure is scar revision, hair transplant, or tattooing to camouflage unsightly scars.
What is the recovery process?
During hospitalization, the patient must be restricted in bed continuously or intermittently for several days between 3-5 days. After release from the hospital, the patients return to their normal lives but not having to do physical exercise during the first 2 months after surgery. The patient will have a urinary catheter continuously for several weeks to avoid a urinary fistula. If the patient has a penile prosthesis, it would need at least 6 months before sexual intimacy.
What are the results?
With good surgical technique, the result is very satisfying with an improved quality of life. The patient is able to live in a male role completely and happily either on their own or with their female or male partners.
- Patient Information
- Global Statistics
- Media Centre
- World Congress
- Global Sponsors
- Privacy Policy
19 Mantua Road, Mount Royal, NJ 08061 United States
Registration number: 0330131
US Office: +1-603-643-2325
UK Office: +44 20 7038 7812
© 2022 International Society of Aesthetic Plastic Surgery. All Rights Reserved.
- Create an account
Log into My ISAPS
Forgot your password? Reset it here
Join the ISAPS Community
All members will continue to receive information relevant to their membership and ISAPS events.
I confirm by clicking below I would like to receive information about:
Welcome to the ISAPS community
By creating an account, you can:.
- Register for events
- Update your personal details
- Gain access to ISAPS publications and video library
- Become a member (explore our memberships here)
ISAPS Members can also:
- Access your member benefits
- Secure discounted member rates for events
- Read the Aesthetic Plastic Surgery Journal
- Gain full access to the video library
- View the Members Directory
- Update your 'Find a Surgeon' profile details
- Renew/Upgrade your Membership
The first step to becoming a part of the community is creating an account, so join us!
Medindia » Articles » Procedure » Gender-Reassignment Surgery: Everything You Need to Know
Gender-Reassignment Surgery: Everything You Need to Know
- Indications
Non-Surgical Procedures
- Surgical Procedures
Risks in Non-Surgical and Surgical Procedures
- Whom to consult?
- Pre-Op Considerations
- Post-Op Considerations
Impact on Mental Health
- Cost of the Surgery
Gender reassignment surgery, also known as gender-affirming surgery, is a medical procedure or series of procedures aimed at altering an individual's physical appearance and sexual characteristics to align with their gender identity.
In Simple words, it can be defined as the alteration of a person's physical sex characteristics by surgery in order to match the personâs gender identity
This transformative process is often pursued by transgender individuals, as well as some cisgender and non-binary individuals. It involves various surgical interventions to modify primary and secondary sexual characteristics, thereby affirming an individual's gender identity( 1 ✔ ✔ Trusted Source Sex Reassignment Surgery in the Female-to-Male Transsexual Go to source ).
Alternative Names for Gender-Affirming Surgery
- Gender reassignment surgery (GRS)
- Gender-affirmation surgery
- Gender confirmation surgery
- Sex reassignment surgery
Who Can Get Gender Reassignment Surgery?
Transgender individuals.
Transgender individuals are those whose gender identity differs from the sex they were assigned at birth. Many transgender individuals experience gender dysphoria, a condition characterized by distress or discomfort caused by a misalignment between their gender identity and physical body. Gender reassignment surgery is often sought by transgender individuals as part of their transition journey to alleviate gender dysphoria and align their physical appearance with their gender identity.
Trans Women: Assigned male at birth but identify and live as women. Trans women may pursue feminizing surgeries such as vaginoplasty (creation of a vagina), breast augmentation, facial feminization surgery, and voice feminization surgery to affirm their gender identity.
Trans Men: Assigned female at birth but identify and live as men. Trans men may undergo masculinizing surgeries such as chest reconstruction (removal of breast tissue), hysterectomy (removal of the uterus), and phalloplasty or metoidioplasty (creation of a penis) to align their bodies with their gender identity.
Intersex Individuals
Intersex is a term used to describe individuals who are born with variations in their biological sex characteristics (chromosomes, gonads (testes/ovaries), reproductive organs (prostate/uterus) or external genitalia (penis/clitoris)) that do not fit typical definitions of male or female.
Intersex Individuals with Gender Dysphoria: While intersex individuals can be transgender if their gender identity does not match the sex they were raised or assigned as, some intersex individuals may experience distress or discomfort, known as gender dysphoria , due to a misalignment between their gender identity and assigned sex characteristics, and seek gender-affirming surgery to align their physical appearance with their gender identity( 2 ✔ ✔ Trusted Source Gender Affirmation Surgeries Go to source ).
Drag Performers
Drag performers are individuals who utilize clothing, makeup, and performance art to explore and celebrate gender expression. They are typically associated with a gender different from their own. These performers engage in drag for various reasons, including self-expression, artistic exploration, and entertainment purposes.
While some drag performers may identify as transgender or non-binary and use drag as a form of self-expression or exploration of their gender identity, others may identify as cisgender and engage in drag purely for entertainment or artistic expression.
Drag Queens and Drag Kings : Drag queens are typically male individuals who dress in feminine attire and adopt exaggerated female personas for performance. Drag kings, on the other hand, present as male or masculine while performing. While some drag performers may identify as transgender and may ultimately pursue gender-affirming surgeries, the act of performing drag does not inherently imply a desire for surgical intervention.
Individuals with Klinefelter Syndrome
Klinefelter syndrome is a chromosomal condition in which individuals are born with an extra X chromosome (XXY), resulting in differences in sexual development and often leading to infertility and other physical characteristics such as tall stature, reduced muscle mass, and gynecomastia (enlarged breast tissue in males)( 4 ✔ ✔ Trusted Source Klinefelter syndrome Go to source ).
While not directly related to transgender identity, some individuals with Klinefelter syndrome may experience gender dysphoria and seek gender-affirming treatments, including surgery. These individuals may undergo procedures to modify their physical characteristics to better align with their gender identity and alleviate distress associated with gender dysphoria.
Non-Binary Individuals
"Non-binary" is a term used to describe individuals whose gender identity does not exclusively align with the categories of male or female. This is a deeply personal and internal sense of one's own gender. Non-binary individuals may identify as both, neither, a combination of both, or as a gender entirely different from male or female.
Bigenital Operation: Bigenital operations allow individuals to construct a penis or vagina and retain their original organs. Some non-binary individuals may opt for these surgeries to achieve a physical presentation that aligns with their gender identity while maintaining aspects of their original anatomy. These surgeries cater to the diverse spectrum of gender identities and expressions and provide options for individuals who do not fit within the traditional binary understanding of gender.
"Cisgender" is a term used to describe individuals whose gender identity aligns with the sex they were assigned at birth. In other words, someone who is cisgender identifies as the gender typically associated with the biological sex they were born with. For example, a person who was assigned female at birth and identifies as a woman is considered cisgender. The term "cisgender" is often used in contrast to "transgender," which describes individuals whose gender identity differs from the sex they were assigned at birth
While gender dysphoria is often associated with transgender individuals, cisgender people can also experience it. In some cases, cisgender individuals with severe gender dysphoria may seek gender-affirming surgeries to alleviate their distress and bring their physical appearance into alignment with their gender identity. These surgeries are typically pursued after extensive evaluation and therapy, and they can significantly improve the mental health and well-being of individuals experiencing gender dysphoria.
Is Gender Dysphoria the only Reason for Gender Reassignment Surgery?
No, not only gender dysphoric individuals seek gender reassignment surgery. While gender dysphoria is a common reason why individuals pursue gender-affirming surgeries, it's not the only factor. Some people may choose to undergo these surgeries for reasons beyond alleviating distress associated with gender dysphoria.
For example, individuals with intersex variations may seek gender-affirming surgeries to align their physical appearance with their gender identity, even if they do not experience gender dysphoria. Similarly, some non-binary individuals may opt for surgeries to achieve a physical presentation that better aligns with their gender identity, regardless of whether they experience gender dysphoria.
Furthermore, some cisgender individuals may also undergo gender-affirming surgeries for reasons related to body dysmorphia or dissatisfaction with their physical appearance, rather than gender dysphoria.
Ultimately, the decision to pursue gender reassignment surgery is deeply personal and can be influenced by a variety of factors beyond gender dysphoria alone.
Hormonal injections is the only available non-surgical procedure.It isa form of hormone replacement therapy (HRT) commonly used in transgender healthcare to induce and maintain desired physical changes consistent with an individual's gender identity.
These injections typically involve the administration of testosterone for transmasculine individuals (female-to-male, or FtM) and estrogen for transfeminine individuals (male-to-female, or MtF).
Testosterone Injections (for Transmasculine Individuals)
Purpose : Testosterone injections are administered to induce masculine changes, such as increased facial and body hair growth, deepening of the voice, muscle development, and redistribution of body fat.
Types of Testosterone : There are different formulations of testosterone available for injection, including testosterone cypionate, testosterone enanthate, and testosterone undecanoate.
Administration : Testosterone injections are typically administered intramuscularly (into the muscle) in either the gluteal (buttocks) or deltoid (upper arm) muscle.
Dosage and Frequency : The dosage and frequency of testosterone injections can vary depending on individual factors such as age, weight, hormone levels, and desired changes. Typically, injections are administered every one to two weeks to maintain stable testosterone levels in the body.
Monitoring : Regular monitoring of hormone levels, liver function, and other relevant markers is essential to ensure the safety and effectiveness of testosterone therapy. Blood tests may be conducted periodically to assess hormone levels and adjust the dosage as needed.
Estrogen Injections (for Transfeminine Individuals)
Purpose : Estrogen injections are administered to induce feminine changes, such as breastdevelopment, redistribution of body fat, softening of the skin, and reduction of muscle mass.
Types of Estrogen : The most common form of estrogen used in injections is estradiol valerate.
Administration : Estrogen injections are typically administered intramuscularly, similar to testosterone injections, in the gluteal or deltoid muscle.
Dosage and Frequency : The dosage and frequency of estrogen injections vary depending on individual factors and treatment goals. Typically, injections are administered every one to two weeks.
Monitoring : Regular monitoring of hormone levels, liver function, and other relevant parameters is crucial for ensuring the safety and effectiveness of estrogen therapy. Blood tests may be conducted periodically to assess hormone levels and adjust the dosage as needed.
Time Frame of Use of Hormonal Injections
Initiation : Hormonal injections are often initiated after a thorough evaluation by healthcare providers, including discussions about treatment goals, potential risks and benefits, and informed consent. The timing of initiation may vary depending on individual factors such as age, readiness for treatment, and presence of any underlying health conditions.
Duration : Hormonal injections are typically used as part of long-term hormone replacement therapy to maintain desired physical changes and support overall well-being. The duration of hormone therapy may vary from individual to individual and often continues indefinitely, especially for those who desire ongoing maintenance of gender-affirming changes.
Discontinuation : In some cases, individuals may choose to discontinue hormonal injections for various reasons, such as personal preference, changes in health status, or the achievement of desired physical changes. It's essential for individuals to discuss any plans to discontinue hormone therapy with their healthcare provider to ensure proper management of any potential effects or complications.
Surgical Procedures: Gender Affirming Surgery
These surgical procedures play vital roles in gender affirmation for transgender individuals, aligning their physical appearance with their gender identity( 3 ✔ ✔ Trusted Source Gender Confirmation Surgery Go to source ).
Male-to-Female (MtF) Transitions:
- Tracheal Shave: This procedure reduces the prominence of the Adam's apple, a typically male characteristic, to create a smoother, more feminine neck contour.
- Breast Augmentation: Transfeminine individuals undergo breast augmentation to develop fuller, more feminine breast contours. Breast implants are placed behind breast tissue or chest muscle to achieve the desired size and shape.
- Facial Feminization Surgery (FFS): FFS encompasses various surgical procedures aimed at feminizing facial features. Techniques may include forehead contouring, rhinoplasty , cheek augmentation, chin and jaw reshaping, tracheal shave, lip augmentation, and hairline lowering to achieve a more traditionally feminine appearance.
- Male-to-Female Genital Sex Reassignment (Vaginoplasty): This surgical procedure constructs female genitalia for transfeminine individuals seeking alignment with their gender identity. Techniques involve using penile and scrotal tissue to create the vaginal canal, labia, and clitoral hood. The procedure may also include the creation of a neurovascular neoclitoris, providing both aesthetic and functional female genitalia in one operation.
Female-to-Male (FtM) Transitions:
- Hysterectomy and Oophorectomy: This procedure involves the removal of the uterus and ovaries, reducing the production of female hormones (estrogen and progesterone).
- Vaginectomy: Vaginectomy is the surgical removal of the vaginal canal, aligning the physical anatomy with a masculine appearance.
- Chest Reconstruction (Top Surgery): FtM individuals undergo chest reconstruction surgery to remove breast tissue and reshape the chest to achieve a more masculine contour. Techniques include subcutaneous mastectomy or double mastectomy with or without nipple reconstruction.
- Female-to-Male Genital Sex Reassignment (Phalloplasty): Phalloplasty is a surgical procedure to construct a phallus for FtM individuals seeking male genitalia. The radial forearm flap method is commonly used, involving tissue grafting from the forearm to create the phallus and urethra for standing urination. This procedure can be performed concurrently with a hysterectomy/vaginectomy to complete the transition process. A scrotum with testicular implants may be constructed in a second stage.
These surgical interventions are integral to gender affirmation for transgender individuals, helping align their physical appearance with their gender identity and alleviating gender dysphoria. Each procedure is tailored to the individual's unique needs and goals, reflecting the diversity of experiences within the transgender community.
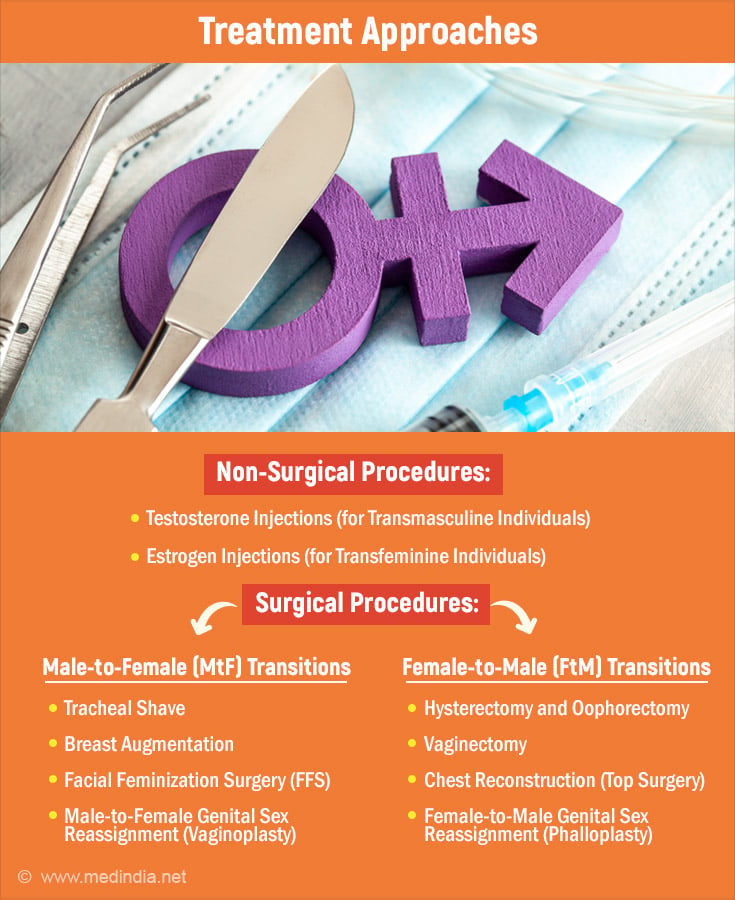
Risks in Hormone Therapies
- Cardiovascular Risks : Hormone replacement therapy (HRT) may increase the risk of cardiovascular events such as heart attacks and strokes, especially in older individuals or those with pre-existing cardiovascular conditions.
- Thromboembolic Events : Estrogen therapy, particularly in forms like oral contraceptives, may elevate the risk of blood clots, leading to thromboembolic events such as deep vein thrombosis (DVT) or pulmonary embolism (PE).
- Endocrine Disruption : Hormone therapies can disrupt the body's natural hormone balance, leading to potential complications such as metabolic disturbances, including insulin resistance and dyslipidemia.
- Breast Cancer Risk : Some studies suggest that long-term use of hormone replacement therapy, especially estrogen-only formulations, may increase the risk of breast cancer in transgender women.
- Liver Dysfunction : Hormone therapies, particularly oral estrogen formulations, may affect liver function and increase the risk of liver disease or dysfunction.
Risks in Gender Reassignment Surgeries
- Surgical Complications : As with any surgical procedure, gender reassignment surgeries carry risks such as infection, bleeding , anesthesia complications, and adverse reactions to medications.
- Scarring : Gender-affirming surgeries, especially those involving breast augmentation, chest reconstruction, or genital reconstruction, may result in visible scarring that could impact body image and self-esteem.
- Loss of Sensation : Surgeries involving genital reconstruction, such as vaginoplasty or phalloplasty, may result in loss of sensation or altered sensation in the genital region, affecting sexual function and satisfaction.
- Functional Complications : Some individuals may experience functional complications post-surgery, such as urinary incontinence , erectile dysfunction, or difficulties with sexual arousal or orgasm.
- Psychological Impact : Gender reassignment surgeries can have profound psychological effects, including adjustment difficulties, post-operative depression, and challenges related to body image and identity.
Guidance on Surgical Procedures: Whom to Consult?
When contemplating gender reassignment surgery, it's essential for individuals to consult with a team of experienced healthcare providers specializing in transgender care. Here's whom to consider consulting:
1. Gender-Affirming Surgeons
Gender-affirming surgeons specialize in performing gender reassignment surgeries and have expertise in various surgical techniques, including chest surgery (for both masculinization and feminization procedures), genital reconstruction, and facial feminization surgery. These surgeons can provide comprehensive information about the surgical options available, discuss the potential risks and benefits, and guide individuals through the decision-making process.
2. Endocrinologists
Endocrinologists play a crucial role in managing hormone therapy for transgender individuals. They can provide guidance on hormone replacement therapy (HRT), including the use of testosterone for transmasculine individuals and estrogen for transfeminine individuals. Endocrinologists can assess hormone levels, monitor any potential side effects, and adjust hormone regimens as needed to support the transition process.
3. Mental Health Professionals
Mental health professionals, such as psychologists, psychiatrists, or licensed therapists, offer invaluable support throughout the gender transition journey. They can assist individuals in exploring their gender identity, coping with gender dysphoria, and addressing any psychological concerns or challenges that may arise before, during, or after surgery. Mental health professionals also play a role in assessing readiness for surgery and providing pre- and post-operative counseling and support.
4. Primary Care Physicians
Primary care physicians are essential members of the healthcare team and can provide general medical care, coordinate referrals to specialists, and monitor overall health and well-being. They can also assist with managing any pre-existing medical conditions and ensuring that individuals are physically fit for surgery.
5. Support Groups and Advocacy Organizations
Support groups and advocacy organizations within the transgender community can offer valuable peer support, resources, and information about gender-affirming surgeries. These groups provide opportunities for individuals to connect with others who have undergone similar experiences, share insights, and seek guidance from those who have navigated the transition process.
Consulting with a multidisciplinary team of healthcare providers ensures that individuals receive comprehensive care tailored to their unique needs and goals. This collaborative approach helps individuals make informed decisions about gender reassignment surgery and supports their overall health and well-being throughout the transition process.
Pre-operative Considerations
1. Medical Considerations
Transgender individuals may have preexisting health conditions like diabetes , asthma , or HIV, which can impact their eligibility for surgery and postoperative care. Surgeons often consult with endocrinologists to assess the patient's physical fitness for surgery, especially considering the complex medication regimens involved in hormone therapy before and after surgery.
2. Fertility Concerns
Patients considering sex reassignment surgery (SRS) are informed about potential infertility, particularly if procedures like orchiectomy or oophorectomy are performed as part of the transition process. Preservation of fertility options may be discussed before surgery.
3. Age and Consent
SRS is generally not performed on children under 18, with rare exceptions made for adolescents based on healthcare provider assessments and potential benefits or risks. Consent from parents or legal guardians is required, along with long-term mental health counseling to confirm persistent gender dysphoria.
4. Intersex and Trauma Cases
Infants born with intersex traits may undergo surgical interventions at or near birth, raising ethical concerns about human rights implications. Trauma cases also require careful consideration, as surgically assigned gender may not align with the individual's gender identity, leading to negative outcomes later in life.
5. Standards of Care
Many regions follow Standards of Care for the Health of Transgender and Gender Diverse People (SOC), such as those published by the World Professional Association for Transgender Health (WPATH). These guidelines outline minimum requirements for treatment, including psychological evaluation and living as the desired gender before surgery.
6. Insurance Coverage
Obtaining insurance coverage for SRS may require documented assessments by mental health professionals, evidence of persistent gender dysphoria, and completion of physician-supervised hormone therapy for a specified duration.
Post-operative Considerations
1. Quality of Life and Physical Health
Studies assessing postoperative quality of life vary, with some reporting similar quality to control groups while others note lower quality in domains of health and limitations. Overall, many individuals report improvements in mental health, satisfaction with physical appearance, and overall well-being after surgery.
2. Psychological and Social Consequences
SRS has been shown to be effective in relieving gender dysphoria, though some studies highlight methodological limitations. Patients often report reduced anxiety, depression , and hostility levels post-surgery, with improvements in self-perceived physical and mental health.
3. Sexuality and Sexual Satisfaction
SRS can significantly impact individuals' sexual experiences and satisfaction. Most transsexual individuals report enjoying better sex lives and improved sexual satisfaction after surgery, with changes in orgasm frequency, intensity, and masturbation habits observed. However, satisfaction levels may vary between trans men and trans women, and expectations for sexual aspects of life may differ from cisgender individuals.
4. Continued Support
Comprehensive postoperative care involves ongoing psychological support, management of any complications, and assistance with adjustment to physical changes. Social support networks play a crucial role in helping individuals navigate their post-surgical experiences and integrate their gender identities into their daily lives.
The denial or limited access to gender-affirming surgeries can have severe consequences for the mental health and well-being of transgender individuals.
1. Persistent Gender Dysphoria
Without access to surgery, transgender individuals may continue to experience intense distress and discomfort due to the misalignment between their gender identity and physical characteristics. This persistent gender dysphoria can lead to heightened anxiety, depression, and a sense of hopelessness.
2. Heightened Anxiety
Living in a body that does not align with one's gender identity can contribute to persistent anxiety. The frustration of being unable to access necessary medical care and the ongoing struggle to navigate societal expectations can exacerbate feelings of stress and worry.
3. Increased Depression
Untreated gender dysphoria and the inability to undergo gender-affirming surgeries can lead to deepening feelings of depression and despair. Transgender individuals may struggle with low self-esteem, feelings of worthlessness, and a sense of isolation from not being able to live authentically.
4. Social Withdrawal
The distress caused by the incongruence between one's gender identity and physical appearance can result in social withdrawal and avoidance of social interactions. Transgender individuals may feel ashamed or uncomfortable in social settings, leading to further isolation and loneliness.
5. Suicidal Ideation
The lack of access to gender-affirming surgeries and the ongoing struggle with gender dysphoria can significantly increase the risk of suicidal thoughts and behaviors. Without the hope of being able to live authentically and alleviate their distress, transgender individuals may experience profound feelings of hopelessness and desperation.
Click here to know more about Mental health in transgender community
Affordable Surgery Options
Gender-affirming surgeries, including gender reassignment surgery (GRS), vary widely in cost globally. Affordable options exist in countries like Turkey, Brazil, Argentina, and Belgium. Turkey offers the most budget-friendly option, followed by Brazil, Argentina, and Belgium. While these countries provide competitive prices, individuals should consider factors beyond cost, such as healthcare quality and legal protections.
Click here for detailed information on the global cost of these surgeries and to find out which options are more affordable
In summary, gender reassignment surgery serves as a vital tool in validating the gender identities of transgender and intersex individuals, enabling them to harmonize their external appearance with their innate sense of self. Despite its transformative potential, many face obstacles in accessing this essential care, including financial constraints, inadequate insurance coverage, and legal hurdles.
As society progresses towards greater awareness and acceptance of transgender rights, it's imperative to prioritize equitable access to gender-affirming treatments and offer unwavering support to individuals throughout their transition journey. By dismantling these barriers and fostering inclusivity within healthcare systems, we can empower transgender individuals to live authentically and flourish in their gender identity.
Html.Raw(Model.contents.ToString())
- Sex Reassignment Surgery in the Female-to-Male Transsexual - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3312187/)
- Gender Affirmation Surgeries - (https://www.hopkinsmedicine.org/health/wellness-and-prevention/gender-affirmation-surgeries)
- Gender Confirmation Surgery - (https://www.uofmhealth.org/conditions-treatments/transgender-services/gender-confirmation-surgery)
- Klinefelter syndrome - (https://www.nhs.uk/conditions/klinefelters-syndrome/)
Please use one of the following formats to cite this article in your essay, paper or report:
Dr. Preethi Balasubramanian. (2024, May 08). Gender-Reassignment Surgery: Everything You Need to Know . Medindia. Retrieved on May 13, 2024 from https://www.medindia.net/health/procedure/gender-reassignment-surgery-everything-you-need-to-know.htm.
Dr. Preethi Balasubramanian. "Gender-Reassignment Surgery: Everything You Need to Know". Medindia . May 13, 2024. <https://www.medindia.net/health/procedure/gender-reassignment-surgery-everything-you-need-to-know.htm>.
Dr. Preethi Balasubramanian. "Gender-Reassignment Surgery: Everything You Need to Know". Medindia. https://www.medindia.net/health/procedure/gender-reassignment-surgery-everything-you-need-to-know.htm. (accessed May 13, 2024).
Dr. Preethi Balasubramanian. 2024. Gender-Reassignment Surgery: Everything You Need to Know . Medindia, viewed May 13, 2024, https://www.medindia.net/health/procedure/gender-reassignment-surgery-everything-you-need-to-know.htm.
- Neuroscience for Kids - (http://faculty.washington.edu/chudler/words.html)
- What the Stroop Effect Reveals About Our Minds - (https://lesley.edu/article/what-the-stroop-effect-reveals-about-our-minds)
- The Emotional Stroop Effect Is Modulated by the Biological Salience and Motivational Intensity Inherent in Stimuli - (https://www.frontiersin.org/articles/10.3389/fpsyg.2019.03023/full)
- Numerical stroop effect - (https://pubmed.ncbi.nlm.nih.gov/15058867/)
- The Emotional Stroop Task: Assessing Cognitive Performance under Exposure to Emotional Content - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4993290/)
- The Stroop Effect - (https://www.simplypsychology.org/stroop-effect.html)
- Ask an Expert: How does Stroop Effect apply to real life situations? - (https://www.sciencebuddies.org/science-fair-projects/ask-an-expert/viewtopic.php?t=6139)
- Stroop Effect - (https://conductscience.com/portfolio/stroop-effect/#:~:text=Stroop%20effect%20has%20many%20practical,bipolar%20disorder%2C%20or%20major%20depression.)
- Stroop Test - (https://www.sciencedirect.com/topics/psychology/stroop-test)
- Clinical Application of the Modified Stroop Test to Children with Attention Deficit/Hyperactivity Disorder - (https://www.researchgate.net/publication/47792734_Clinical_Application_of_the_Modified_Stroop_Test_to_Children_with_Attention_DeficitHyperactivity_Disorder)
Anita Ramesh. (2021, September 17). Stroop Effect . Medindia. Retrieved on Apr 21, 2023 from https://www.medindia.net/patients/lifestyleandwellness/stroop-effect.htm.
Anita Ramesh. "Stroop Effect". Medindia . Apr 21, 2023. <https://www.medindia.net/patients/lifestyleandwellness/stroop-effect.htm>.
Anita Ramesh. "Stroop Effect". Medindia. https://www.medindia.net/patients/lifestyleandwellness/stroop-effect.htm. (accessed Apr 21, 2023).
Anita Ramesh. 2021. Stroop Effect . Medindia, viewed Apr 21, 2023, https://www.medindia.net/patients/lifestyleandwellness/stroop-effect.htm.

ASK A DOCTOR ONLINE

What's New on Medindia

Follow @MedIndia
Gender-Reassignment Surgery: Everything You Need to Know - Related News
- Addressing Mental Health Needs in the Transgender Community
- A Global Comparison: Best Countries for Gender Reassignment Surgery
- Transgender Healthcare Disparities Highlighted
- Why is Thyroid Cancer More Common Among Transgender Female Veterans?
- Is Gender Reassignment Surgery Against Nature?
- Consult Online Doctor
- Take Telemedicine course
- Health Centers
- Health Tools
- Health info by Speciality
- Know Your Body
- Health and Wellness
- Web Stories
- Health Tips
- Nutrition Facts
- Lifestyle & Wellness
- Beauty Tips
- Diet & Nutrition
- Home Remedies
- Obesity & Weight Loss
- Complementary Medicine
- Special Reports
- Press Releases
- Health Guide
- Health articles
- Health Quiz
- Health Facts
- Travel Health
- Medicine and Movies
- Symptom Articles
- Diabetes Tools
- Pediatric Calculators
- Men's Health
- Women's Health
- Height Weight Tools
- Cardiac Tools
- Pharma Tools
- Wellness Interactive Tools
- Drug Information
- Drugs by Condition
- Drug Price List - Brand Names
- Drug Interaction with Food
- Drug Price List - Generic Names
- Drugs - Side Effects
- Drug Videos
- Drug Database
- Doctor Directory
- Diagnostic Lab Directory
- Hospital Directory
- Pharmacy or Chemist
- Medical Equipment Suppliers
- Pharma Directory
- Emergency Services
- PG Education
- Family Medicine
- Other Resources
- Medical Aphorism
- Health Acts in India
- Health Quotations
- Medical Conference
- Amazing Body Facts
- Health poll

- Editorial Team
- Exclusive Interviews
- In the News
- Partners & Affiliates
- Advertise With Us
- हिन्दी
- français
- Español
- 中文

IMAGES
VIDEO
COMMENTS
Female-to-male surgery is a type of gender-affirmation or gender-affirming surgery. There are multiple forms of gender-affirming surgery, including altering the genital region, known as "bottom ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning. Often used to refer to phalloplasty, metoidoplasty, or vaginectomy, sex reassignment surgery can also more broadly ...
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
Featured Expert: Fan Liang, M.D. Phalloplasty is surgery for masculinizing gender affirmation. Phalloplasty is a multistaged process that may include a variety of procedures, including: Creating the penis. Lengthening the urethra so you are able to stand to urinate. Creating the tip (glans) of the penis. Creating the scrotum.
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary, to change one or more of their sex characteristics. This type of procedure offers a person ...
Gender transition can substantially improve quality-of-life in individuals with gender dysphoria, and various surgical options are available for female-to-male (FtM) transition, including facial ...
FTM Bottom Surgery. We can give you male genitalia in two different ways: Phalloplasty creates a penis and urethra (to stand while urinating). We use tissue from your forearm or thigh. We do this in 2 stages. Metoidioplasty takes your existing genital tissue and makes it longer, turning it into a defined phallus.
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Gender affirming surgery, also known as sex reassignment surgery (SRS) or confirmation surgery, is the surgical procedure(s) by which a transgender or non-binary person’s physical appearance and functional abilities are changed to align with the gender they know themselves to be.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000. Between 100 to 500 gender-reassignment procedures are ...
The Encyclopedia of Surgery says that "the number of gender reassignment procedures conducted in the United States each year is estimated at between 100 and 500. The number worldwide is estimated ...
Metoidioplasty , or "bottom surgery," is a gender-affirming surgical procedure that involves creating a neophallus (new penis) from a hormonally enlarged clitoris. Transgender men and transmasculine people assigned female at birth (AFAB) may elect for a metoidioplasty if they want their genital appearance to align with their gender identity.
The authors provide a state-of-the-art overview of the different gender reassignment surgery procedures that can be performed in a female-to-male transsexual. Keywords ... Monstrey S, Selvaggi G, Ceulemans P, et al. Chest-wall contouring surgery in female-to-male transsexuals: a new algorithm. Plast Reconstr Surg. 2008; 121 (3):849-859 ...
Female-to-male gender reassignment surgery (FTM GRS) is a complex and irreversible genital surgery for female transsexual who is diagnosed with gender identity disorder and has a strong desire to live as male. The procedure is to remove all female genital organs including the uterus, ovaries, and vagina with the construction of male genitalia ...
During this period, 214 patients underwent penile inversion vaginoplasty. Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18-61 years); the average of operative time was 3.3 h (range 2-5 h); the average duration of hormone therapy before surgery was 12 years (range 1-39).
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
Female-to-Male Genital Sex Reassignment (Phalloplasty): Phalloplasty is a surgical procedure to construct a phallus for FtM individuals seeking male genitalia. The radial forearm flap method is ...