We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs


Chapter 1: 10 Real Cases on Acute Coronary Syndrome: Diagnosis, Management, and Follow-Up
Nisha Ali; Timothy J. Vittorio
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion.
- Clinical Symptoms
- Risk Factors
- Classification
- Complications
- Full Chapter
- Supplementary Content
Case 1: Diagnostic Evaluation of Chest Pain
A 65-year-old man presented to the emergency department with a complaint of left-sided chest pain radiating to his left arm. There were no alleviating factors. His past medical history included hypertension, uncontrolled diabetes mellitus, and hyperlipidemia. He denied any toxic habits. His baseline exercise tolerance is 2 city blocks limited by fatigue. Upon presentation, vital signs were stable and the physical examination was unremarkable. The chest pain was partially relieved by sublingual nitroglycerin. The 12-lead ECG showed nonspecific T-wave inversions in the inferolateral leads. He was administered aspirin, and the chest pain resolved shortly thereafter. Subsequently, he was admitted to the telemetry floor for further evaluation and observation. His serial cardiac biomarkers were negative. He did not have any recurrent chest pain and remained hemodynamically stable throughout the hospital stay. How would you manage this case?
In this clinical scenario, the patient does not fit the complete picture of anginal symptoms. However, the key here is the presence of risk factors and subtle 12-lead ECG changes, which place him at an elevated risk for coronary artery disease. He can be further evaluated by stress testing for risk stratification.
Angina consists of retrosternal chest pain increased by activity or emotional stress and generally relieved by rest or administration of nitroglycerin. The evaluation of chest pain begins with a thorough history and physical examination to delineate the etiology. The list of differential diagnoses is vast, and a detailed review of systems about pertinent diagnoses can narrow down the list. The presence of comorbid conditions and risk factors might hint toward a diagnosis of coronary artery disease. Both serial 12-lead ECG and highly sensitive cardiac troponin T testing should be performed before excluding ongoing ischemic coronary artery disease. Prior to stress testing, the patient should be chest pain free for 24 hours, without dynamic 12-lead ECG changes, and the highly sensitive cardiac troponin T level should be negative or trending downward.
The differential diagnosis of chest pain includes the following:
Coronary artery disease
Aortic dissection
Pericarditis
Pulmonary embolism
Costochondritis/rib fracture
Peptic ulcer disease
Acute cholecystitis
Cervical radiculopathy
Herpes zoster
Anxiety disorder
Chest pain should be classified as anginal or nonanginal based on the history.
Anginal symptoms can be considered in the setting of risk factors and should be evaluated by an appropriate stress modality if the symptoms are vague.
Serial 12-lead ECG and highly sensitive cardiac troponin T should be performed to exclude ongoing ischemic coronary artery disease before stress testing is performed.
Case 2: Diagnosis of Acute Coronary Syndrome
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Center for Bloodless Medicine and Surgery
Case study: cardiac surgery, case study 1:, radial artery approach for cardiac catheterization followed by an "off-pump" coronary artery bypass surgery.
A 66-year old male Jehovah’s Witness patient was brought to the hospital with chest pain, and referred for a cardiac catheterization. He had a positive nuclear stress test that showed reduced blood flow to the left ventricle with a high suspicion for coronary artery disease.
Dr. John Resar, the director of the cardiac catheterization lab at Johns Hopkins performed the procedure. In order to reduce blood loss from the cardiac catheterization, the approach was planned through the radial artery (in the arm) rather than the femoral artery (in the groin). This approach is associated with reduced bleeding during and after the procedure. The total blood loss during the cardiac catheterization procedure was 50 mls (1% of total blood volume). As expected, the procedure revealed high-grade triple vessel disease (narrowing) that was not treatable with coronary stents. Coronary artery bypass surgery was recommended.
Dr. John Conte performed the coronary bypass surgery. Of interest is the fact that in 1999, Dr. Conte published a case report of the first ever successful bloodless lung transplant in a Jehovah’s Witness patient. In this case presented here, he decided the patient would be best served by performing an "off-pump" cardiac surgery where the heart lung bypass machine is not used. This technique reduces the blood loss that is commonly associated with the bypass machine, since with traditional bypass a substantial amount of the patient’s blood is left behind in the circuit of the machine and is unrecoverable.
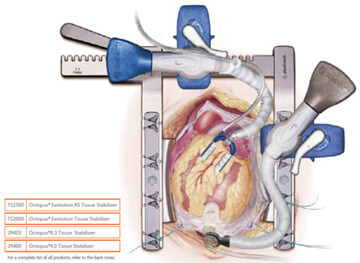
The 4-hour surgery went very well. The saphenous vein from his right leg was harvested using an endoscopic approach. Compared to the traditional technique, this method uses a smaller incision to harvest the vein. The internal mammary artery and the saphenous vein were both used to provide blood flow to the narrowed coronary arteries. A special “octopus retractor” was used to stabilize the heart because during off-pump surgery the heart continues to beat (thus the term “beating heart surgery”), unlike the traditional on-pump method where the heart is arrested and completely still. The hemoglobin level was 13.8 before surgery and 13.0 three days later when the patient was discharged from the hospital. Two weeks after the surgery, the patient attended the open house for our Bloodless Medicine and Surgery Program and looked and felt "as good as ever".
Case Study 2:
Aortic valve and aortic root replacement without blood transfusion.
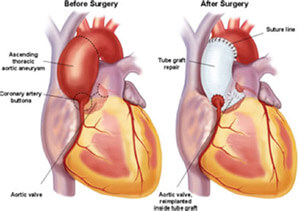
A 46-year old female Jehovah’s Witness patient had severe aortic valve regurgitation along with an ascending aortic aneurysm. She had been seen at two other major academic centers in hopes of having a valve replacement along with repair of her “aortic root” (the section of aorta that joins the heart above the aortic valve), but was unable to find a team of physicians that would perform the surgery without blood transfusion.
Dr. Duke Cameron, the former Chief of Cardiac Surgery saw her along with Dr. Steven Frank, Director of the Johns Hopkins Bloodless Medicine and Surgery Program. With the patient and her family present, they reviewed the echocardiogram and cardiac catheterization report from another hospital. At the time, a discussion took place about the various methods of blood conservation and the various alternatives to transfusion. The patient and her family agreed that blood salvage (Cell Saver) and intraoperative autologous normovolemic hemodilution (IANH) were acceptable options. The patient was sent to the lab for routine blood tests and her hemoglobin level was suboptimal (13.0 g/dL) for this type of surgery. One complicating factor was the patient’s body weight of 95 lbs, which means that her total blood volume and red cell mass was about ½ that of a normal sized adult.
The patient was scheduled for a 3-week course of erythropoietin and intravenous iron at the infusion clinic at Johns Hopkins. The patient responded nicely to the treatments and her hemoglobin level increased to 15.1 g/dL, at which time the surgery was scheduled.

After the patient was under general anesthesia, 2 units of her own blood were removed as part of the IANH technique. These 2 units would be given back to her near the end of the surgery. During surgery, the Perfusionist, who operates the heart lung machine, was able to use a method called retrograde autologous prime (RAP), whereby the patient’s own blood is used to prime the circuit in an effort to conserve the patient’s blood volume.
After the surgical procedure, the patient was noted to have some cardiac ischemia (deficient blood flow to the left coronary artery). She was taken to the cardiac cath lab where a coronary stent was placed by an interventional cardiologist into her left main coronary artery. The next day she was weaned of the ventilator and she recovered nicely. Our Bloodless team Hematology consultant, Dr. Linda Resar guided her postoperative therapy which included IV iron and erythropoietin. She was discharged from the hospital with a hemoglobin of 8.0 g/dL, and she and her family had a Baltimore crab dinner before returning home to Roanoke, VA.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 106, Issue 5
- Angina: contemporary diagnosis and management
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-4009-6652 Thomas Joseph Ford 1 , 2 , 3 ,
- http://orcid.org/0000-0002-4547-8636 Colin Berry 1
- 1 BHF Cardiovascular Research Centre , University of Glasgow College of Medical Veterinary and Life Sciences , Glasgow , UK
- 2 Department of Cardiology , Gosford Hospital , Gosford , New South Wales , Australia
- 3 Faculty of Health and Medicine , The University of Newcastle , Newcastle , NSW , Australia
- Correspondence to Dr Thomas Joseph Ford, BHF Cardiovascular Research Centre, University of Glasgow College of Medical Veterinary and Life Sciences, Glasgow G128QQ, UK; tom.ford{at}health.nsw.gov.au

https://doi.org/10.1136/heartjnl-2018-314661
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- cardiac catheterization and angiography
- chronic coronary disease
- percutaneous coronary intervention
- coronary artery disease
Learning objectives
Around one half of angina patients have no obstructive coronary disease; many of these patients have microvascular and/or vasospastic angina.
Tests of coronary artery function empower clinicians to make a correct diagnosis (rule-in/rule-out), complementing coronary angiography.
Physician and patient education, lifestyle, medications and revascularisation are key aspects of management.
Introduction
Ischaemic heart disease (IHD) remains the leading global cause of death and lost life years in adults, notably in younger (<55 years) women. 1 Angina pectoris (derived from the Latin verb ‘angere’ to strangle) is chest discomfort of cardiac origin. It is a common clinical manifestation of IHD with an estimated prevalence of 3%–4% in UK adults. There are over 250 000 invasive coronary angiograms performed each year with over 20 000 new cases of angina. The healthcare resource utilisation is appreciable with over 110 000 inpatient episodes each year leading to substantial associated morbidity. 2 In 1809, Allen Burns (Lecturer in Anatomy, University of Glasgow) developed the thesis that myocardial ischaemia (supply:demand mismatch) could explain angina, this being first identified by William Heberden in 1768. Subsequent to Heberden’s report, coronary artery disease (CAD) was implicated in pathology and clinical case studies undertaken by John Hunter, John Fothergill, Edward Jenner and Caleb Hiller Parry. 3 Typically, angina involves a relative deficiency of myocardial oxygen supply (ie, ischaemia) and typically occurs after activity or physiological stress ( box 1 ).
Definition of angina (NICE guidelines) 32
Typical angina: (requires all three)
Constricting discomfort in the front of the chest or in the neck, shoulders, jaw or arms.
Precipitated by physical exertion.
Relieved by rest or sublingual glyceryl trinitrate within about 5 min
Presence of two of the features is defined as atypical angina.
Presence of one or none of the features is defined as non-anginal chest pain.
Stable angina may be excluded if pain is non-anginal provided clinical suspicion is not raised based on other aspects of the history and risk factors.
Do not define typical, atypical and non-anginal chest pain differently in men and women or different ethnic groups.
- Download figure
- Open in new tab
- Download powerpoint
Reappraisal of ischaemic heart disease pathophysiology. Distinct functional and structural mechanisms can affect coronary vascular function and frequently coexist leading to myocardial ischaemia. CAD, coronary artery disease.
We begin by classifying angina according to pathophysiology. We then consider the current guidelines and their strengths and limitations for assessing patients with recent onset of stable chest pain. We review non-invasive and invasive functional tests of the coronary circulation with linked management strategies. Finally, we point to future directions providing hope for improved patient outcomes and development of targeted disease-modifying therapy. The aim of this educational review is to provide a contemporary approach to diagnosis and management of angina taking into consideration epicardial coronary disease, microcirculatory dysfunction and coronary vasospasm.
Contemporary angina classification by pathophysiology
The clinical history is of paramount importance to initially establish whether the nature of the presenting symptoms is consistent with angina ( box 1 ). Indeed, recent data supports specialist physicians under-recognise angina in up to half of their patients. 10 Furthermore, contemporary clinical trials of revascularisation in stable IHD including the ISCHEMIA trial highlight the importance of good clinical history and listening to our patients to determine the nature and frequency of symptoms which helps to plan management. We propose a classification of angina that aligns with underlying aetiology and related management ( table 1 ).
- View inline
Classification of angina by pathophysiology
Angina with obstructive coronary artery disease
2018 ESC guidelines on myocardial revascularisation define obstructive CAD as coronary stenosis with documented ischaemia, a haemodynamically relevant lesion (ie, fractional flow reserve (FFR) ≤0.80 or non-hyperaemic pressure ratio (NHPR) (eg, iwFR≤0.89)) or >90% stenosis in a major coronary vessel ( table 1 ). There is renewed interest in NHPRs (iwFR, resting full-cycle ratio (RFR) and diastolic pressure ratio (dPR)) as data have emerged in support of numerical equivalency between these indices suggesting all can be used to guide treatment strategy. 11 Angina with underlying obstructive CAD allows symptom guided myocardial revascularisation (often with percutaneous coronary intervention (PCI)) and is effective in reducing ischaemic burden and symptoms (in many patients). Recent studies have served evidence that functional coronary disorders overlap and may contribute to angina even in patients with obstructive epicardial CAD. Dynamic changes in lesion or vessel ‘tone’ and propensity to vasoconstriction is important and may cause rest angina that is frequently overlooked in patients with obstructive CAD. 12 During invasive physiological assessment of ischaemia during exercise, Asrress et al showed that ischaemia developed at FFR averaging≈0.76 which is not often observed with adenosine induced hyperaemia. 13 This finding implies there are other important drivers of subendocardial ischaemia (myocardial supply:demand factors). Furthermore, it reinforces that angina is not synonymous with ischaemia or flow-limiting coronary disease (eg, abnormal FFR or NHPR). Coronary anatomy and physiology should not be considered in isolation but in the context of the patient.
Angina-myocardial ischaemia discordance
Although obstructive CAD or microvascular dysfunction may be present, the link between ischaemia and angina is not clearcut. The ‘ischaemic threshold’ (the heart rate-blood pressure product at the onset of angina) has intraindividual and interindividual variability. 14 Innate differences in vascular tone and endocrine changes (eg, menopause) may influence propensity to vasospasm while environmental factors including cold environmental temperature, exertion and mental stress are relevant. The large international CLARIFY registry highlighted the importance of symptoms, showing that angina with or without concomitant ischaemia, was more predictive of adverse cardiac events compared with silent ischaemia alone. 15 Other potential drivers of discordance between angina and ischaemia include variations in pain thresholds and cardiac innervation (eg, diabetic neuropathy).
Symptoms and/or signs of ischaemia but no obstructive coronary artery disease (INOCA)
Cardiologists are inclined to adopt a ‘stenosis centric’ approach to patient management; however, as clinicians we must appreciate that all factors are relevant, including coronary anatomy and function but systemic health and the psychosocial background ( figure 2 ). First, systemic factors including heart rate, blood pressure (and their product) and myocardial supply:demand ratio (Buckberg index) are relevant. 16 Reduced myocardial oxygen supply from problems such as anaemia or hypoxaemia should always be considered.
Contributing factors to myocardial ischaemia. The contributors to the physiological myocardial perfusion gradient and resultant ischaemia can be broken down at patient-level into systemic, cardiac and coronary factors. CAD, coronary artery disease; SEVR, subendocardial viability ratio.<Modified with permission from 47 >.
Second, coronary factors are well recognised but certain nuances are overlooked. In 2018, the first international consensus guidelines clarify that a definite diagnosis of MVA may be made in patients with angina with no underlying obstructive CAD, evidence of reversible ischaemia on functional testing and objective evidence of coronary microvascular dysfunction ( table 1 ). 17 ‘Probable MVA’ is defined by three of the above criteria. Coronary microvascular dysfunction may be structural (eg, small vessel rarefaction or increased media: lumen ratio) or functional (eg, endothelial impairment) and these disorders may coexist. Other coronary causes of INOCA include intramyocardial ‘tunnelled’ segments of epicardial arteries (myocardial ‘bridging’) who may have ischaemia on exercise. These segments are particularly susceptible to vasoconstriction due to endothelial impairment. 18 Coronary arteriovenous malformations are rare but may also cause of myocardial ischaemia. Vasospastic angina (‘Prinzmetal’s angina’) is typically described as recurrent rest angina with focal occlusive proximal epicardial often seen in young smokers with characteristic episodic ST segment elevation during attacks. Notably, the more common form of VSA is distal and diffuse subtotal epicardial vasospasm and is characterised by ST segment depression and may occur during exertion. Typical cardiac risk factors and endothelial impairment may be implicated. 19
The long-term (sometimes lifelong) burden of MVA and/or VSA on physical and mental well-being can be profound. Patients with these conditions commonly attend primary care and are repeatedly hospitalised with acute coronary syndromes, arrhythmias and heart failure driving up health resource utilisation, morbidity and reducing quality of life. 20 21
The third and final group of factors that drive ischaemia in patients with angina but without obstructive CAD include cardiac factors . These include left ventricular hypertrophy or restrictive cardiomyopathy where subendocardial ischaemia results impaired perfusion from arterioles penetrating deeper into myocardial tissue with shorter diastole, enhanced systolic myocardial vessel constriction and enhanced interstitial matrix. 22 Heart failure (with reduced or preserved ejection fraction) can lead to elevated left ventricular end diastolic pressure which reduces the diastolic myocardial perfusion gradient. Valvular heart disease (eg, aortic stenosis (AS)) is an important consideration in patients with INOCA. In AS, most experts support haemodynamic factors as the main cause of ischaemia, especially since symptoms and coronary flow reserve (CFR) improve immediately after valve replacement. 23 Patients with INOCA may have increased painful sensitivity to innocuous cardiac stimuli (eg, radiographic contrast) without inducible ischaemia. Furthermore, some affected patients have a lower pain threshold and tolerance to the algogenic effects of adenosine (thought to be the main effector of ischaemia mediated chest pain). 24
Gender differences and angina presentation
The WISE (Women’s Ischemia Syndrome Evaluation) study highlighted that over 2/3 of women with angina had no obstructive CAD and the majority of these had functional impairments in the coronary microcirculation associated with significant impairments in health-related quality of life. 25 Indeed, women have more non-obstructive CAD and functional IHD which are frequently overlooked and hence undertreated. 26 27 Over time and at different ages, women have a similar or slightly higher prevalence of angina than men across countries independent of diagnostic and treatment practices. 28 Different patterns of IHD may be anticipated to cause different angina symptoms between genders. Nonetheless, recent evidence moves the field away from the ‘male-typical, female-atypical’ model of angina towards a ‘gender continuum’ whereby the objective reports between men and women’s symptoms are more similar than treating physicians perceive. Interestingly, dyspnoea was a feature in around ¾ of angina presentations without any significant difference between the sexes. 29
Assessment: current guidelines
Assessment strategies in current major international guidelines focus on the detection of underlying obstructive CAD. European and American guidelines (ESC and ACC/AHA, respectively) favour a Bayesian approach whereby overall probability of obstructive CAD after testing is determined from pretest probability modified by the diagnostic test results. The ACC/AHA guidelines determine pretest risk from a modified Diamond Forrester model, 30 whereas the Europeans favour the CADC (Coronary Artery Disease Consortium) model which avoids overestimation seen with Diamond-Forrester and appears a more accurate assessment of pretest risk. 31 Both current guidelines stratify pretest risk into low, intermediate or high groups with use of non-invasive testing suggested in the intermediate group (ACC/AHA arbitrarily defined as 10%–90% or 15%–85% in ESC).
In stark contrast, the NICE CG95 2016 update ‘chest pain of recent onset: assessment and diagnosis’ discarded the Bayesian pretest risk assessment. NICE advocates first-line multidetector CT coronary angiography (CTCA) in all patients with typical or atypical chest pain ( box 1 ), those whose history does not suggest angina but who have ST changes or Q waves on a resting ECG. 32 Functional testing (eg, exercise stress echo or stress perfusion magnetic resonance—CMR) are relegated to second-line if CTCA is non-diagnostic or the clinical significance of known CAD needs clarified. Potential benefits of this approach include a much higher diagnostic accuracy for detection of atherosclerotic heart disease than functional testing which potentially carries the best long-term prognostic information for patients with CAD. 27 Extended 5-year outcomes from SCOTHEART showed a reduction in the combined endpoint of death from coronary heart disease or non-fatal myocardial infarction among the group randomised to CTCA compared with standard care (2.3% vs 3.9%; absolute risk reduction (ARR) 1.6% number needed to treat (NNT) 63). This effect was driven by better targeting of preventative therapies. The authors report that although overall prescriptions of preventive cardiovascular medications were only modestly increased (~10% higher) in the CTCA arm, changes in such therapies occurred in around one in four patients allowing more personalised treatment to patients with most coronary atheroma in the CT group.
These results should be considered in relation to design limitations of this trial. There was no control procedure (test vs no test), the threshold for prescribing preventive therapy with statins was 20%–30% likelihood of a CHD event in 10 years (much higher than many contemporary healthcare systems), CTCA was performed on top of treadmill exercise testing which has poor test accuracy in distinct patient groups, notably women, and the procedures were unblinded and open-label. Outcome reporting that is narrowly focused on CHD does not take account of other cardiovascular events, such as hospitalisation for arrhythmias and heart failure, which have implications for quality of life. In PROMISE, a ‘head-to-head’ trial of CTCA versus functional testing, there were no differences in health outcomes. 33 In the interests of providing patients and clinicians with a reliable and accurate test result, a strategy based on anatomical CTCA has fundamental limitations. SCOT-HEART identified that obstructive CAD affects the minority (one in four) patients presenting to the Chest Pain Clinic with known or suspected angina. This means that an anatomical test strategy with CTCA leaving the aetiology and treatment unexplained in the majority of affected patients, which becomes all the more relevant considering that anginal symptoms and quality of life are worse when CTCA is used. 34 Diagnostic options are enhanced by advances in technology and tests for the functional significance of CAD are now feasible, but at significant cost. 35 NICE guidelines state that HeartFlow FFR CT should be considered as an ‘option for patients with stable, recent onset chest pain who are offered CCTA as part of the NICE pathway on chest pain’. Using HeartFlow FFR CT may avoid the need for invasive coronary angiography and revascularisation; however, major randomised controlled trials are ongoing (eg, FORECAST study NCT03187639 ).
We support efforts to provide a definitive diagnosis for patients with ongoing angina symptoms after a ‘negative’ CTCA, initially using non-invasive ischaemia testing. Notably, the recent International Standardised Criteria for diagnosing ‘suspected’ MVA would be met in patients with symptoms of myocardial ischaemia, no obstructive CAD and objective evidence of myocardial ischaemia ( table 1 ). Invasive testing for diagnosis of MVA could be reserved for subjects with refractory symptoms and negative ischaemia testing or diagnostic uncertainty. The criteria for ‘definite MVA’ require the above AND objective evidence of microvascular dysfunction (eg, reduced CFR or raised microvascular resistance).
Limitations of current guidelines
There are limitations to the current NICE-95 guideline, not least the logistics and cost of service provision with an estimated 700% increase in cardiac CT required across the UK. 36 Importantly, what do we report to the majority of patients with anginal chest pain but no obstructive CAD on the CTCA? In fact, only 25% of patients had obstructive CAD and at 6 weeks based on the CTCA findings, 66% of patients were categorised as not having angina due to coronary heart disease. The possibility of false reassurance for the patients with angina and INOCA is an open question and may be one contributing factor for the lack of improvement in angina and quality of life in the CTCA group vs standard care. 34 We must strive to deliver patient-centred care, recognising that most patients seek explanation for their symptoms in combination with effective treatment options. 37 CTCA is an insensitive test for disorders of coronary vascular function, which may affect the majority of patients attending with anginal symptoms. Since the majority of affected patients have no obstructive CAD, and the majority of them are women, an anatomical strategy introduces a sex-bias into clinical practice, whereby a positive test result (obstructive CAD) is more likely to occur in men and a positive test for small vessel disease is less likely to occur in women. Furthermore, patient-reported outcomes including angina limitation, frequency and overall quality of life improve less after CTCA compared with standard care, notably in patients with no obstructive CAD. 34 Non-invasive functional testing with positron emission tomography (PET), echo and most recently stress perfusion CMR has diagnostic value for stratified medicine. Finally, stratification of patients using luminal stenosis severity on angiography overlooks the spectrum of risk associated with overall plaque burden and may miss functional consequences associated with diffuse but angiographically mild disease (particularly when subtending large myocardial mass).
Non-invasive functional testing includes myocardial perfusion scintigraphy, exercise treadmill testing (including stress echocardiography) or contrast-enhanced stress perfusion MRI depending on local availability. Novel pixel-wise absolute perfusion quantification of myocardial perfusion by CMR will likely improve the efficiency of absolute quantification of myocardial blood flow by CMR. 38 PET is the reference-standard non-invasive assessment of myocardial blood flow permitting quantitative flow derivation in mL/g/min. Clinically, PET-derived quantification of myocardial blood flow (MBF) can assist in the diagnosis of diffuse epicardial or microvascular disease; however, limitations include poor availability and exposure to ionising radiation. Non-invasive workup often provides important insights on coronary microvascular function and are reviewed in detail elsewhere. 39
With functional testing relegated to second-line testing, clinicians may forgo additional tests after a negative CTCA particularly in an era of fiscal restraint and if patients’ symptoms are viewed as atypical. One important group that will be disparately affected by an ‘anatomy first’ strategy are women—over half of all patients with suspected angina in the large prospective trials of CTCA are female. While the benefits of CTCA to diagnose CHD and prevent CHD events are similar in women and men, the large majority of patients undergoing CTCA do not have obstructive CAD potentially leading to misdiagnosis and suboptimal management in patients with INOCA. 33 Women, are most likely to have no obstructive CAD and their cardiac risk is associated with severely impaired CFR and not obstructive CAD. 40 Overall, there is growing awareness of sex-specific differences in coronary pathophysiology and potential for different patterns of CAD in women. This is a rapidly evolving fertile area for further research.
Invasive coronary angiography and physiological assessment
UK NICE guidelines suggest that invasive coronary angiography is a third-line investigation for angina when the results of non-invasive functional imaging are inconclusive. Patients with typical symptoms, particularly those in older age groups with higher probability of non-diagnostic CTCA scans, often proceed directly to invasive coronary angiography. During cardiac catheterisation, assuming that epicardial CAD is responsible for their symptoms, visual assessment for severe angiographic stenosis (>90%) is sufficient to establish significance and treatment plan for these patients. Two common pitfalls for visual interpretation of angiograms were recently highlighted by two coronary physiology pioneers Gould and Johnson. Using their quantitative myocardial perfusion database of over 5900 patients showing that occult coronary diffuse obstructive coronary disease or flush ostial stenosis may be both be overlooked on angiography and mislabelled as microvascular angina with suboptimal treatment. 41 The ischaemic potential of indeterminate coronary lesions (~40%–70% diameter stenosis) is best assessed using pressure-derived indices, such as FFR, and non-hyperaemic pressure ratios (NHPR: dPR, nstantaenous wave free ratio (iwFR) and others) to guide revascularisation decisions. However, as is the case with coronary angiography, these indices do not inform the clinician about disorders of coronary artery vasomotion.
Invasive tests of coronary artery function are the reference standard for the diagnosis of coronary microvascular dysfunction 17 and vasospastic angina ( table 1 ; figure 1 ). 42 Coronary microvascular resistance may be directly measured using guidewire-based physiological assessment during adenosine induced hyperaemia. Methods to assess this include using a pressure-temperature sensitive guidewire by thermodilution (index of microcirculatory resistance; IMR) or Doppler ‘ComboWire’ (hyperaemic microvascular resistance; HMR). These metrics have been the focus of a recent review article in Heart. 43 There are several other haemodynamic indices of microvascular function including instantaneous hyperaemic diastolic pressure velocity slope, wave intensity analysis and zero flow pressure. A detailed description of these parameters is out with the scope of this review. 41 Elevated coronary microvascular resistance (eg, IMR >25) carries prognostic utility in patients with reduced CFR but unobstructed arteries. Lee et al found over fivefold higher risk of adverse cardiac events in these subjects compared with controls with normal microvascular function. 44
CFR is the ratio of maximum hyperaemic blood flow to resting flow. CFR in the absence of obstructive CAD can signify impaired microvascular dilation. Lance Gould first introduced this concept almost 50 years ago but more recently proposed that CFR should be considered in the context of the patient and the hyperaemic flow rate. 41 The absolute threshold for abnormal CFR varies depending on the method of assessment, the patient population studies and the controversy reflects the dichotomous consideration of the continuous physiological spectrum of ischaemia. Abnormal CFR thresholds vary from ≤2.0 or ≤2.5 with more restrictive criteria for abnormal CFR (<1.6) being more specific for myocardial ischaemia and worse outcomes but at the cost of reduced sensitivity. On the other hand, studies of transthoracic Doppler derived CFR (which has less reproducibility) often use cut-offs of 2.5 with some observational evidence of worse outcomes in the INOCA population with CFR below this threshold. 45 The influence of rate-pressure product on resting flow and its correction for CFR determination should be considered.
Systolic endocardial viability ratio (SEVR) is a ratio of myocardial oxygen supply:demand derived from the aortic pressure-time integral (diastole:systole). However, it is well known that blood pressure, pulse and SEVR perturbations influence CFR more closely than microcirculatory resistance. Reduced CFR without raised microvascular resistance still portends increased cardiovascular risk 44 and may be a distinct subgroup with different drivers of ischaemia (eg, abnormal supply:demand systemic haemodynamic factors; figure 2 ). Alternatively, these patients may be at an earlier stage of disease prior to more established structural microvascular damage. Sezer et al showed the pattern of coronary microvascular dysfunction early in type II diabetes was driven by disturbed coronary regulation and high resting flow. 46 In longstanding diabetes however, elevated microvascular resistance was observed reflecting established structural microvascular disease. This process matches the paradox of microvascular disease in diabetic nephropathy where increased glomerular filtration rate (GFR) typifies the early stages of disease prior to later structural damage and reduction in GFR.
The third mechanism of microvascular dysfunction is inappropriate propensity to vasoconstriction of the small coronary arteries, typically this is assessed using intracoronary acetylcholine infusions as a pharmacological probe.
Rationale and benefit of invasive coronary function testing in INOCA
We contend that a complete diagnostic evaluation of the coronary circulation should assess structural and functional pathology. 47 The British Heart Foundation CorMicA trial provides evidence about the opportunity to provide a specific diagnosis to patients with angina using an interventional diagnostic procedure (IDP) when obstructive CAD is excluded by invasive coronary angiography. Consenting patients were randomised 1:1 to the intervention group (stratified medical therapy, IDP disclosed) or the control group (standard care, IDP sham procedure, results not disclosed). The diagnostic intervention included pressure guidewire-based assessment of FFR, CFR and IMR during adenosine induced hyperaemia (140 µg/kg/min). Vasoreactivity testing was performed by infusing incremental concentrations of acetylcholine (ACh) followed by a bolus vasospasm provocation (up to 100 µg). The diagnosis of a clinical endotype (microvascular angina, vasospastic angina, both, none) was linked to guideline-based management. The primary endpoint was the mean difference in angina severity at 6 months (as assessed by the Seattle Angina Questionnaire summary score—SAQSS) which was analysed using a regression model incorporating baseline score. A total of 391 patients were enrolled between 25/11/2016 and 11/12/2017. Coronary angiography revealed obstructive disease in 206 (53.7%). One hundred and fifty-one (39%) patients without angiographically obstructive CAD were randomised. The underlying abnormalities revealed by the IDP included: isolated microvascular angina in 78 (51.7%), isolated vasospastic angina in 25 (16.6%), mixed (both) in 31 (20.5%) and non-cardiac chest pain in 17 (11.3%). The intervention was associated with a mean improvement of 11.7 units in the SAQSS at 6 months (95% CI 5.0 to 18.4; p=0.001). In addition, the intervention led to improvements in the quality of life (EQ5D index 0.10 units; 0.01 to 0.18; p=0.024). After disclosure of the IDP result, over half of treating clinicians changed their diagnosis about the aetiology of their patients’ symptoms. There were no procedural serious adverse events and no differences in major adverse cardiac events (MACE) at 6 months. Interestingly, there were sustained quality of life benefits at one year for INOCA patients helped by correct diagnosis and linked treatment started at the index invasive procedure. 48 Future trials are anticipated to determine the wider external validity of this approach.
Medical therapy to prevent new vascular events should be considered and these include consideration of aspirin, ACE inhibitors (ACEi) and statins. The latter two agents have pleiotropic properties including beneficial effects on endothelial function and so may be helpful in treating coronary microvascular dysfunction. Sublingual glyceryl trinitrate tablets or spray should be used for the immediate relief of angina and before performing activities known to bring on angina.
Non-pharmacological
As with many cardiovascular diseases, lifestyle modification including risk factor control and patient education are key. Lifestyle recommendations are covered in detail in recent ESC guidelines. The adverse effect of angina on patient well-being and quality of life can be substantial. It is crucial that we assess for this and manage appropriately. After diagnosis with angina, cardiac rehabilitation can be useful to educate and build confidence. One useful patient led education aid is called the ‘Angina plan’. This tool is a workbook and relaxation plan delivered in primary care, which helps improve angina symptoms (frequency and limitation) while reducing anxiety and depression. 49 The ORBITA trial highlights the benefits of placebo effect and we support that the positive diagnosis may be therapeutic in itself. Angina symptoms are often subjective and multifactorial in origin, so patient education and validation of symptoms may facilitate further improvement.
Management: Non-obstructive CAD
Generic guidelines on angina management frequently overlooks the precision medicine goal whereby treatment is targeted to underlying pathophysiology. There is a lack of high-quality clinical trial data for treating microcirculatory dysfunction. The current article thus proposes a reasoned approach to management based on evaluation of pathophysiological mechanisms.
We contest that angina and INOCA are syndromes and not a precise diagnosis (akin to myocardial infarction with no obstructive CAD—MINOCA). As such, by stratifying treatment according to underlying pathophysiology, we may realise better outcomes for our patients.
Impaired coronary vasodilator capacity (reduced CFR)
Bairey Merz et al performed a randomised controlled trial of ranolazine in the WISE population. Notably, there was no net benefit effect on the INOCA population as a whole; however, in patients with reduced CFR (<2.5), there was a benefit suggestion of improved myocardial perfusion reserve index (MPRi) after established treatment. 50 Lanza and Crea highlight that subjects with reduced CFR might preferentially be treated with drugs that reduce myocardial oxygen consumption (eg, beta-blockers (BB)—for example, Nebivolol 1.25–10 mg daily). 51 There is accumulating evidence that long acting nitrates are ineffective or even detrimental in MVA. Lack of efficacy may relate to poor tolerability, steal syndromes through regions of adequately perfused myocardium and/or related to the reduced responsiveness of nitrates within the coronary microcirculation. 52 Furthermore, chronic therapy with nitrate may induce endothelial dysfunction and oxidative stress, predominantly via endothelin dependent pathways. 53
Increased microvascular constriction (structurally increased microvascular resistance or functional propensity to microvascular spasm)
Subjects with increased microvascular vasoconstriction may be treated with vasodilator therapies acting on the microcirculation. These include calcium channel blockers (CCB—for example, amlodipine 2.5–10 mg daily) or nicorandil (eg, 5–30 mg two times a day). Hyper-reactivity to constrictor stimuli resulting in propensity to microvascular spasm may be provoked by endothelial dysfunction. This was first described my Mohri et al over three decades ago with recent physiological studies suggesting treatment aimed at improving endothelial function (eg, ACEi, Ramipril 2.5–10 mg) may improve the microvascular tone and/or the susceptibility to inappropriate spasm. 54 55 A detailed discussion of all potentially therapeutic options for coronary microvascular dysfunction is beyond the scope of this article; however, a systematic review by Marinescu et al may be of interest to readers wishing further information. 56
Epicardial spasm (vasospastic angina)
The poor nitrate response or tolerance seen in MVA contrasts with patients with vasospastic angina, in whom nitrates are a cornerstone of therapy and BB are relatively contraindicated. 7 Dual pathologies (VSA with underlying microvascular disease) is increasingly recognised. A diagnosis of VSA facilitates treatment using non-dihydropiridine calcium antagonists (eg, diltiazem-controlled release up to 500 mg daily). Overall, CCB are effective in treating over 90% of patients. 57 High doses of calcium antagonists (non-dihydropiridine and dihydropyridine) may be required either alone or in combination. Unfortunately, ankle swelling, constipation and other side effects may render some patients intolerant. In these cases, long-term nitrates may be used with good efficacy in this group. In about 10% of cases, coronary artery spasm may be refractory to optimal vasodilator therapy. Japanese VSA registry data shows nitrates were not associated with MACE reduction in VSA, and importantly when added to Nicorandil were potentially associated with higher rates of adverse cardiac events. 58 Alpha blockers (eg, clonidine) may be helpful in selected patients with persistent vasospasm. In patients with poor nitrate tolerance the K+-channel opener nicorandil (5–10 mg two times a day) can be tried. Consider secondary causes in refractory VSA (eg, coronary vasculitis) and in selected patients with ACS presentations, coronary angioplasty may be considered as a bailout option.
Management: Obstructive CAD
Pharmacological.
Although NICE guidelines offer either BB or CCB first line, although we support BB initially because they are generally better tolerated ( table 2 ). 59 Long-term evidence of efficacy is limited between BB and CCB and there are no proven safety concerns favouring one or the other. Dihydropyridine calcium may be added to BB if blood pressure permits. NICE CG126 states third line options can be either added on (or substituted if BB/CCB not tolerated). These include nitrates (eg, isosorbide mononitrate 30–120 mg controlled release), ivabradine (eg, 2.5–7.5 mg two times a day), nicorandil (5–30 mg two times a day) or ranolazine (375–500 mg two times a day). These are all third line medications that can be used based and combined with BB and/or CCB depending on comorbidities, contraindications, patient preference and drug costs ( figure 3 ). The RIVER-PCI study found that anti-ischaemic pharmacotherapy with ranolazine did not improve the prognosis of patients with incomplete revascularisation after percutaneous coronary intervention. 60 This was a reminder that alleviation of ischaemia may not improve ‘hard’ endpoints in patients with chronic coronary syndromes but helps us to remain focused on improving their quality of life.
Angina pharmacotherapy
Empirical pharmacological treatments for patients with angina. ACEi, Angiotensin converting enzyme inhibitor; ASP, aspirin; BB, beta-blocker; Endo, endothelial; IVA, ivabradine; MVA, microvascular angina; NIC, nicorandil; NIT, nitrate; Obs CAD, obstructive coronary artery disease;, RAN, ranolazine; RF, risk factor.
Revascularisation
Recently revised 2018 ESC guidelines suggest that myocardial revascularisation is indicated to improve symptoms in haemodynamically significant coronary stenosis with insufficient response to optimised medical therapy. Patients’ wishes should be accounted for in relation to the intensity of antianginal therapy as PCI can offer patients with angina and obstructive CAD a reduced burden from polypharmacy. Angina persists or recurs in more than one in five patients following PCI and microvascular dysfunction may be relevant. Guidelines support consideration of revascularisation for prognosis in asymptomatic ischaemia in patients with large ischaemic burden (left main/proximal left anterior descending artery stenosis >50%) or two/three vessel disease in patients with presumed ischaemia cardiomyopathy (LVEF<35%).
Refractory angina is common in patients with complex CAD including those with previous coronary artery bypass grafting (CABG) and chronic total occlusions (CTOs). Over the last decade, vast strides in technique, training and tools have delivered major increases in the success of CTO PCI. These angina patients often have incomplete revascularisation with lesions or anatomy previously considered ‘unsuitable for intervention’ but now amenable to treatment by trained operators. A recent review article in Heart summarises non-pharmacological therapeutic approaches to patients with refractory angina including cognitive behavioural therapy (CBT), stellate ganglion nerve blockade, Transcutaneous Electrical Nerve Stimulation (TENS)/spinal cord stimulation and pain modulating antidepressants (eg, imipramine). 61 Of note, coronary sinus reducers deployed using a transcatheter venous system have shown early promise in clinical studies.
Future directions
Based on test accuracy, health and economic benefits, non-invasive and invasive functional tests should be considered a standard of care in patients with known or suspected angina, especially if obstructive CAD has been excluded by CT or invasive coronary angiography. Computational fluid dynamic modelling of the functional significance of CAD, notably with FFRct, is an emerging option and clinical trials, including FORECAST (ClinicalTrials.gov Identifier: NCT03187639 ) and PRECISE ( NCT03702244 ), are ongoing. The use of computational modelling as a diagnostic tool in patients with microvascular angina or coronary vasomotion disorders remains to be determined.
Systemic vascular abnormalities were recently highlighted in patients with INOCA potentially supporting a therapeutic role for targeted vascular therapy, for example, using selective endothelin-A receptor antagonists. 19 The MRC Framework for Stratified Medicine is applicable to patients with angina and we believe genetic testing with precision medicine holds future promise.
The optimal management of patients with known or suspected angina begins with establishing the correct diagnosis.Around one half of angina patients have no obstructive coronary disease; many of these patients have microvascular and/or vasospastic angina.Non-invasive assessment with CTCA is a sensitive anatomical test for plaque which assists in initial treatment and risk stratification. Anatomical imaging has fundamental limitations to rule in or rule out coronary vasomotion disorders in patients with symptoms and/or signs of ischaemia but no obstructive CAD (INOCA). Women are disproportionately represented in this group with MVA and/or VSA, the two most common causes of diagnoses. A personalised approach to invasive diagnostic testing permits a diagnosis to be made (or excluded) during the patients’ index presentation. This approach helps stratify medical therapy leading to improved patient health and quality of life. Physician appraisal of ischaemic heart disease (IHD) should consider all pathophysiology relevant to symptoms, prognosis and treatment to improve health outcomes for our patients. More research is warranted, particularly to develop disease modifying therapy.
ESC curriculum: stable CAD
Precipitants of angina.
Prognosis of chronic IHD.
Clinical assessment of known or suspected chronic IHD.
Indications for, and information derived from, diagnostic procedures including ECG, stress test in its different modalities (with or without imaging, exercise and stress drugs) and coronary angiography.
Management of chronic IHD, including lifestyle measures and pharmacological management.
Indications for coronary revascularisation including PCI/stenting and CABG.
Angina pectoris is a clinical syndrome occurring in patients with or without obstructive epicardial coronary artery disease.
Diagnostic testing in angina is symptom driven and so should provide patients and their physicians with an explanation for their symptoms and used to stratify management and offer prognostic insights.
Microvascular and/or vasospastic angina are common disorders of coronary artery function that may be overlooked by anatomical coronary testing, leading to false reassurance and adverse prognostic implications.
CME credits for Education in Heart
Education in Heart articles are accredited for CME by various providers. To answer the accompanying multiple choice questions (MCQs) and obtain your credits, click on the 'Take the Test' link on the online version of the article. The MCQs are hosted on BMJ Learning. All users must complete a one-time registration on BMJ Learning and subsequently log in on every visit using their username and password to access modules and their CME record. Accreditation is only valid for 2 years from the date of publication. Printable CME certificates are available to users that achieve the minimum pass mark.
Supplemental material
- Naghavi M ,
- Allen C , et al
- ↵ Cardiovascular Disease Statistics 2018 . London : British Heart Foundation , 2018 .
- Kligfield P
- ↵ Cine-coronary arteriography . Circulation . 227 East Washington Square, Philadelphia, PA 19106. : Lippincott Williams and Wilkins , 1959 .
- Kaski J-C ,
- Gersh BJ , et al
- Saraste A , et al
- Montalescot G ,
- Sechtem U ,
- Achenbach S , et al
- Corcoran D ,
- Peterson ED ,
- Dai D , et al
- Arnold SV ,
- Grodzinsky A ,
- Gosch KL , et al
- Park J , et al
- Asrress KN ,
- Williams R ,
- Lockie T , et al
- Garber CE ,
- Carleton RA ,
- Camaione DN , et al
- Greenlaw N ,
- Tendera M , et al
- Johnson NP ,
- Nitroglycerine JNP
- Camici PG ,
- Beltrame JF , et al
- Corban MT ,
- Prasad M , et al
- Rocchiccioli P ,
- Good R , et al
- Maddox TM ,
- Stanislawski MA ,
- Grunwald GK , et al
- Tavella R ,
- Tucker G , et al
- Raphael CE ,
- Parker KH , et al
- Pasceri V ,
- Buffon A , et al
- Kelsey SF ,
- Matthews K , et al
- Stanley B ,
- ↵ Ct coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial . The Lancet 2015 ; 385 : 2383 – 91 . doi:10.1016/S0140-6736(15)60291-4 OpenUrl
- Hemingway H ,
- Langenberg C ,
- Damant J , et al
- Kreatsoulas C ,
- Shannon HS ,
- Giacomini M , et al
- Diamond GA ,
- Forrester JS
- Bittencourt MS ,
- Polonsky TS , et al
- (NICE) NIfHaCE
- Douglas PS ,
- Hoffmann U ,
- Patel MR , et al
- Williams MC ,
- Shah A , et al
- Leipsic J ,
- Pencina MJ , et al
- Nicol EPS ,
- Roobottom C , British Society of cardiovascular Imaging/ British Society of cardiovascular computed tomography
- Richards T ,
- Coulter A ,
- Hsu L-Y , et al
- Szymonifka J ,
- Twisk JWR , et al
- Taqueti VR ,
- Cook NR , et al
- Beltrame JF ,
- Kaski JC , et al
- Aetesam-ur-Rahman M , et al
- Hwang D , et al
- Hachamovitch R ,
- Murthy VL , et al
- Kocaaga M ,
- Aslanger E , et al
- Berry C , B
- Sidik N , et al
- Robinson J , et al
- Bairey Merz CN ,
- Handberg EM ,
- Shufelt CL , et al
- Horowitz JD
- Kröller-Schön S , et al
- Koyanagi M ,
- Egashira K , et al
- Fearon WF ,
- Kobashigawa JA , et al
- Marinescu MA ,
- Löffler AI ,
- Ouellette M , et al
- Nishigaki K ,
- Yamanouchi Y , et al
- Takahashi J ,
- Takagi Y , et al
- Généreux P ,
- Iñiguez A , et al
- Sainsbury PA ,
- Jolicoeur EM
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Twitter @tomjford
Contributors TJF devised and wrote the article and figures. CB edited and approved the final manuscript.
Funding British Heart Foundation (PG/17/2532884; RE/13/5/30177; RE/18/634217).
Competing interests CB is employed by the University of Glasgow which holds consultancy and research agreements with companies that have commercial interests in the diagnosis and treatment of angina (Abbott Vascular, AstraZeneca, Boehringer Ingelheim, GSK, Menarini, Opsens, Philips and Siemens Healthcare.)
Patient consent for publication Not required.
Provenance and peer review Commissioned; externally peer reviewed.
Read the full text or download the PDF:

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
A 52-Year-Old Man With Atherosclerosis
A 52-year-old executive was referred to our clinic for risk factor management after undergoing coronary computed tomography angiography (CTA) as part of an Executive Physical. He has no history of coronary artery disease and exercises regularly without experiencing anginal symptoms.
His family history is notable for a myocardial infarction (MI) in his father at the age of 52 years. He is a lifelong non-smoker. He does not take medications.
His blood pressure was 110/75. His exam was notable for being overweight with a BMI of 27, but was otherwise unremarkable.
His total cholesterol is 206 mg/dL, HDL-C is 46 mg/dL, triglycerides are 178 mg/dL, calculated LDL-C is 124 mg/dL, and non HDL-C is 160 mg/dL. His fasting glucose is 86 mg/dL. His Hgb A1c is 5.6%.
His 10-year risk based on the 2013 ACC/AHA pooled ASCVD risk estimator is 3.7%.
His coronary artery calcium (CAC) score is 120, which places him in the 87th percentile for his age, gender, and ethnicity.
His coronary CTA shows the following in the proximal LAD:
In addition to maximizing therapeutic lifestyle changes (exercise, weight loss), what is the next step in this patient’s management?
- A. There is nothing more to do since his estimated 10-year risk is low.
- B. Maximize risk factor modification by starting a low-dose aspirin and statin therapy.
- C. Pursue stress testing.
- D. Pursue coronary catheterization.
- E. B and C.
Show Answer
The correct answer is: B. Maximize risk factor modification by starting a low-dose aspirin and statin therapy.
Atherosclerosis is necessary for nearly all coronary events. The development of atherosclerosis is multifactorial. There is significant heterogeneity in the contribution of common traditional modifiable risk factors including apolipoprotein B (apoB)-containing lipoproteins, smoking, diabetes, hypertension, and sedentary lifestyle to atherogenesis. 1 In participants from the Multi-Ethnic Study of Atherosclerosis (MESA) without atherosclerosis as measured by coronary artery calcium (CAC), even the presence of multiple modifiable risk factors was associated with low event rates (3.1%). In contrast, in those with elevated CAC and no modifiable risk factors, the event rates were significantly higher at nearly 11%. 1
While risk estimators are improving in accuracy, 2,3 the presence of subclinical atherosclerosis (primarily by CAC) has consistently been an additive predictor of coronary events in individuals and further discriminates between those at higher and lower risk for events. 4-6 The case patient is at elevated risk because of the burden of subclinical atherosclerosis and, therefore, answer choice A is incorrect.
The recent 2013 ACC/AHA guidelines on cholesterol treatment take a risk-based approach to recommendations for statin therapy. 7 The patient in this case has a low estimated 10-year risk at 3.7%. The current guidelines suggest a risk discussion in this case based on the patient's family history of premature coronary heart disease (CHD). Subclinical atherosclerosis imaging by CAC scanning can help with this discussion. 8
Recently, eight-year follow-up from the Dallas Heart Study showed that among participants with a family history of MI, those without CAC experienced a significantly lower CHD event rate of 1.9% compared to 8.8% in those with any CAC. 9 The case patient has a CAC score >100 that places him above the 75th percentile for his age, gender, and ethnicity. We would recommend moderate- or high-intensity statin therapy during a risk discussion based on an estimated 10-year event rate that exceeds 7.5%. Furthermore, recent data support the use of aspirin in those with CAC >100. Therefore, answer choice B is the correct answer.
Subclinical atherosclerosis imaging with CAC scanning has been endorsed by several committees to assist with risk assessment. The 2010 ACC/AHA risk assessment guidelines gave CAC scanning a IIA recommendation in those deemed to be at intermediate risk for CHD events. 11 In the 2010 appropriate use criteria for cardiac CT endorsed by multiple societies, CAC scanning was deemed appropriate among low-risk asymptomatic patients with a family history of premature CHD in addition to those at intermediate risk. 12 Most recently, the 2013 ACC/AHA risk assessment guidelines gave CAC scoring a IIB recommendation. Specifically, the committee suggests that if there is uncertainty about whether to start pharmacotherapy after risk estimation, then CAC scoring could be considered. 2
An important consideration in this case is the use of CTA to identify subclinical atherosclerosis. While coronary CTA is a more specific and sensitive test for atherosclerosis, there is no evidence that CTA adds significantly to CAC scanning in an asymptomatic population. However, CTA may identify vulnerable features of plaque that are not picked up by CAC scanning, such as those present in the case example. 13 Motoyama et al. identified high-risk features for acute coronary syndromes (ACS) in asymptomatic subjects on CTA including positive remodeling and low-attenuation plaque, in addition to spotty calcification in those presenting with ACS. 14,15 A small preliminary study suggested a benefit of statin therapy on plaque volume and the amount of low-attenuation plaque. 16 The role of CTA in asymptomatic, primary prevention patients is actively under investigation. 17 The benefits of CTA should be weighed against exposure to contrast, expense, and the need to train readers. With rapidly advancing technology, CTAs can now be performed with the equivalent radiation exposure of two mammograms. 18
Currently, the use of CTA is useful in appropriate symptomatic patients, particularly in chest pain protocols in the emergency department. 19 Many of these patients have mild or moderate, non-obstructive atherosclerosis that is unlikely to be the cause of their presenting symptoms, but should be managed with aggressive preventive therapies. In symptomatic patients from the CONFIRM registry, there is an increased hazard of mortality in those with non-obstructive atherosclerosis on CTA compared to those without atherosclerosis on CTA. 20
Some have advocated for stress testing in those with CAC scores > 400; however, the patient in this case does not meet this criteria. 21,22 Therefore, answer choices C and D are incorrect as the patient is asymptomatic.
- Silverman MG, Blaha MJ, Krumholz HM, et al. Impact of coronary artery calcium on coronary heart disease events in individuals at the extremes of traditional risk factor burden: the Multi-Ethnic Study of Atherosclerosis. Eur Heart J. 2013 Dec 13 [Epub ahead of print].
- Goff DC, Jr., Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2935-59.
- Muntner P, Colantonio LD, Cushman M, et al. Validation of the atherosclerotic cardiovascular disease Pooled Cohort risk equations. JAMA 2014;311:1406-15.
- Polonsky TS, McClelland RL, Jorgensen NW, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 2010;303:1610-6.
- Erbel R, Möhlenkamp S, Moebus S, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol 2010;56:1397-406.
- Yeboah J, McClelland RL, Polonsky TS, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA 2012;308:788-95.
- Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2889–934.
- Nasir K, Budoff MJ, Wong ND, et al. Family history of premature coronary heart disease and coronary artery calcification: Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 2007;116:619-26.
- Paixao AR, Berry JD, Neeland IJ, et al. Coronary artery calcification and family history of myocardial infarction in the Dallas Heart Study. JACC Cardiovasc Imaging . 2014 June [Epub ahead of print].
- Miedema MD, Duprez DA, Misialek JR, et al. Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes 2014;7:453-60.
- Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2010;56:e50-103.
- Taylor AJ, Cerqueira M, Hodgson JM, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol 2010;56:1864-94.
- Voros S, Rinehart S, Qian Z, et al. Coronary atherosclerosis imaging by coronary CT angiography: current status, correlation with intravascular interrogation and meta-analysis. JACC Cardiovasc Imaging 2011;4:537-48.
- Motoyama S, Sarai M, Harigaya H, et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol 2009;54:49-57.
- Motoyama S, Kondo T, Sarai M et al. Multislice computed tomographic characteristics of coronary lesions in acute coronary syndromes. J Am Coll Cardiol 2007;50:319-26.
- Inoue K, Motoyama S, Sarai M, et al. Serial coronary CT angiography-verified changes in plaque characteristics as an end point: evaluation of effect of statin intervention. JACC Cardiovasc Imaging 2010;3:691-8.
- U.S. National Institutes of Health.Detection of Subclinical Atherosclerosis in Asymptomatic Individuals (Decide CTA). (ClinicalTrials.gov website). 2009-2014. Available at: http://clinicaltrials.gov/ct2/show/NCT00862056?term=DECIDE-CTA . Accessed June 22, 2014.
- Achenbach S, Marwan M, Ropers, D et al. Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J 2010;31:340-6.
- Hoffmann U, Truong QA, Schoenfeld DA, et al. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med 2012;367:299-308.
- Min JK, Dunning A, Lin FY, et al. Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol 2011;58:849-60.
- Hendel RC, Berman DS, Di Carli MF, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. J Am Coll Cardiol 2009;53:2201-29.
- Berman DS, Hachamovitch R, Shaw LJ, et al. Roles of nuclear cardiology, cardiac computed tomography, and cardiac magnetic resonance: Noninvasive risk stratification and a conceptual framework for the selection of noninvasive imaging tests in patients with known or suspected coronary artery disease. J Nucl Med 2006;47:1107-18.
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Contact Member Care
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
- Search Menu
- Sign in through your institution
- Volume 2024, Issue 5, May 2024 (In Progress)
- Volume 2024, Issue 4, April 2024
- Bariatric Surgery
- Breast Surgery
- Cardiothoracic Surgery
- Colorectal Surgery
- Colorectal Surgery, Upper GI Surgery
- Gynaecology
- Hepatobiliary Surgery
- Interventional Radiology
- Neurosurgery
- Ophthalmology
- Oral and Maxillofacial Surgery
- Otorhinolaryngology - Head & Neck Surgery
- Paediatric Surgery
- Plastic Surgery
- Transplant Surgery
- Trauma & Orthopaedic Surgery
- Upper GI Surgery
- Vascular Surgery
- Author Guidelines
- Submission Site
- Open Access
- Reasons to Submit
- About Journal of Surgical Case Reports
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, conflicts of interest, giant coronary artery aneurysm occluded completely by a thrombus.
- Article contents
- Figures & tables
- Supplementary Data
Shinichi Ishida, Genki Maeno, Aoi Kato, Yuson Wada, Hideyuki Okawa, Takahisa Sakurai, Toshimichi Nonaka, Giant coronary artery aneurysm occluded completely by a thrombus, Journal of Surgical Case Reports , Volume 2024, Issue 5, May 2024, rjae355, https://doi.org/10.1093/jscr/rjae355
- Permissions Icon Permissions
A coronary artery aneurysm is an uncommon vascular disorder, and it can be a life-threatening disease when associated with rupture or an embolism. A 52-year-old man was found to have a 50-mm coronary artery aneurysm at the right coronary artery, and the aneurysm was completely occluded by a thrombus. He had no symptoms after arriving at our hospital, and his hemodynamics was stable. Therefore, initially, we administered anticoagulation therapy involving heparin. After therapy, the distal coronary artery was detected when the thrombus dissolved, and elective surgery was planned. Coronary artery bypass grafting, ligation of the inflow and outflow vessels, and resection of the aneurysm were performed. Early anticoagulation therapy and surgical aneurysm resection were effective for treating the completely occluded coronary artery aneurysm. We herein report this rare case of a giant coronary artery aneurysm occluded completely by a thrombus and treated successfully by anticoagulation therapy and surgical aneurysm resection.
A coronary artery aneurysm (CAA) is an uncommon vascular disorder, and it can be a life-threatening disease when associated with rupture or an embolism [ 1 ]. In particular, a giant CAA that >20 mm is very rare. Moreover, a CAA completely occluded by a thrombus is even more uncommon. We herein present a rare case of a patient with a 50-mm CAA at the right coronary artery (RCA), which was completely occluded by a thrombus at detection.
Case report:
A 52-year-old man with transient ischemic attack was transferred to our hospital. He had a history of hypertension and dyslipidemia. He was conscious and had no particular symptoms after arriving at our hospital; however, an electrocardiogram showed ST-segment elevation in leads II, III, aVF, and V1–4. Enhanced computed tomography revealed a giant CAA at the RCA ( Fig. 1 ). The aneurysm measured 50 mm in diameter and was completely occluded by a thrombus. Additionally, the coronary artery distal from the CAA did not show contrast. Emergency coronary angiography was performed. The RCA was occluded at segment #2 proximal to the CAA, and the CAA did not show contrast ( Fig. 2A ); however, the artery distal to the CAA showed contrast via a collateral artery from the left circumflex artery ( Fig. 2B ). Anticoagulation therapy involving intravenous heparin was started. After several hours, the ST-segment elevation disappeared quickly, and there were no particular symptoms. The creatine kinase level spiked to a maximum of 1475 IU/L, which then decreased to 432 IU/L on the next day. Four days after starting therapy, enhanced computed tomography and coronary angiography were performed again. They showed slight contrast in the CAA and the distal coronary artery ( Fig. 3 ). Thus, surgery was performed to prevent the CAA from rupturing.

Enhanced computed tomography shows a giant coronary artery aneurysm (arrow) at the right coronary artery, which is occluded completely by a thrombus.

(A) Coronary angiography shows occlusion of the right coronary artery proximal to the aneurysm (arrow). (B) The artery distal to the aneurysm shows contrast via a collateral artery from the left circumflex artery (arrow).

A second coronary artery angiography shows slight contrast in the aneurysm (arrow head) and in the distal coronary artery (arrow head).
After a median sternotomy, the right gastroepiploic artery was harvested. Cardiopulmonary bypass was established with ascending aortic cannulation and bicaval drainage. The giant CAA was present at the right ventricle ( Fig. 4A ). The inflow and outflow coronary arteries surrounding the CAA were identified, and the heart was arrested with antegrade cardioplegia. Coronary artery bypass grafting (CABG) was performed (right gastroepiploic artery–RCA distal to the CAA), and the CAA was cut after ligating the inflow and outflow vessels. The inner area of the CAA was filled with a thrombus, and the thrombus was removed immediately. There was no ostium of the other vessels ( Fig. 4B ); thus, the CAA wall was resected and the remnant wall was sutured. The postoperative course was uneventful. Postoperative computed tomography showed shrinkage of the CAA and no contrast in it, and confirmed patency of the bypass graft. The histopathological findings of aneurysm wall revealed that it was the pseudoaneurysm.

Intraoperative image from the surgeon’s perspective. (A) There is a giant coronary artery aneurysm (arrow) on the right ventricle. (B) A view of the inside of the aneurysmal sac (arrow).
A CAA can be induced by atherosclerosis, Kawasaki disease, trauma, infection, etc. [ 2 ]. In the present case, the patient had hypertension and dyslipidemia, with no other relevant medical history. Therefore, the patient’s CAA was assumed to be associated with atherosclerosis.
The treatment strategy for a CAA is controversial, and several approaches have been reported, including conservative treatment with anticoagulation, catheter intervention or surgery, and emergent or elective intervention [ 3 , 4 ]. Most reports have mentioned non-occluded or partially occluded CAAs. However, in the present case, the CAA was occluded completely by a thrombus when it was detected. Our patient had no symptoms after arriving at our hospital, and his hemodynamics was stable. In addition, the coronary artery distal from the aneurysm was unclear, and it was probably small. Therefore, we first decided to perform anticoagulation therapy. As a result, the distal coronary artery was detected when the thrombus dissolved, and elective surgery could be planned. There is a paucity of data and no randomized controlled study available to determine their efficacy, specifically in coronary aneurysm patients. In this case, it showed that early anti-coagulants therapy would be effective in patients with large coronary aneurysm occluded by a thrombus. We assumed that the occlusion of RCA has less influence for blood supply to anterior and lateral left ventricle, which was evident from the electrocardiogram showing ST-elevation in, leads V1-V4. Regarding anticoagulation therapy, aspirin, warfarin, and heparin are common pharmacological treatments to dissolve a thrombus and promote ischemia reperfusion in cases of a coronary aneurysm. We used intravenous heparin early, and it was effective against the thrombus.
Regarding the surgical strategy for a CAA, most reports describe ligating the CAA or inflow and outflow vessels at the same time as CABG, closing the CAA with a stent through catheter intervention, performing CABG followed by stenting, etc. [ 4–6 ]. In the present case, the CAA was completely occluded by a thrombus, and the presence of inflow vessels other than the main coronary artery was not clear. Therefore, to surely stop blood flow into the CAA, we opened the lumen of the CAA and checked that there was no inflow vessel. With this approach, we could close the ostium of other inflow vessels easily if present and perform CABG if necessary.
In conclusion, in patients with a CAA occluded by a thrombus, early anticoagulation therapy is effective. Furthermore, to surely stop blood flow into the CAA, it is important to open it and check that there is no other inflow vessel.
The authors declare that there is no conflict of interests.
None declared.
Pahlavan PS , Niroomand F . Coronary artery aneurysm: a review . Clin Cardiol 2006 ; 29 : 439 – 43 . https://doi.org/10.1002/clc.4960291005 .
Google Scholar
Nichols L , Lagana S , Parwani A . Coronary artery aneurysm: a review and hypothesis regarding etiology . Arch Pathol Lab Med 2008 ; 132 : 823 – 8 . https://doi.org/10.5858/2008-132-823-CAAARA .
Everett JE , Burkhart HM . Coronary artery aneurysm: case report . J Cardiothorac Surg 2008 ; 3 : 1 . https://doi.org/10.1186/1749-8090-3-1 .
Sheikh A , Hailan A , Kinnaird T , et al. Coronary artery aneurysm: evaluation, prognosis, and proposed treatment strategies . Heart Views 2019 ; 20 : 101 – 8 . https://doi.org/10.4103/HEARTVIEWS.HEARTVIEWS_1_19 .
Crawley PD , Mahlow WJ , Huntsinger DR , et al. Giant coronary artery aneurysms: review and update . Tex Heart Inst J 2014 ; 41 : 603 – 8 . https://doi.org/10.14503/THIJ-13-3896 .
Sundhu M , Yildiz M , Saqi B , et al. Coronary artery aneurysm presenting as non-ST elevation myocardial infarction . Cureus 2017 ; 9 : 1436 . https://doi.org/10.7759/cureus.1436 .
Email alerts
Citing articles via, affiliations.
- Online ISSN 2042-8812
- Copyright © 2024 Oxford University Press and JSCR Publishing Ltd
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Cardiac comorbidities in McArdle disease: case report and systematic review
Affiliations.
- 1 Department of Clinical and Experimental Medicine, Neurological Institute, University of Pisa, Via Roma 67, 56100, Pisa, Italy.
- 2 Department of Clinical and Experimental Medicine, Neurological Institute, University of Pisa, Via Roma 67, 56100, Pisa, Italy. [email protected].
- 3 Department of Internal Medicine, University of Genova, Genoa, Italy.
- PMID: 38802689
- DOI: 10.1007/s10072-024-07600-x
Introduction and methods: Myophosphorylase deficiency, also known as McArdle disease or Glycogen Storage Disease type V (GSD-V), is an autosomal recessive metabolic myopathy that results in impaired glycogen breakdown in skeletal muscle. Despite being labelled as a "pure myopathy," cardiac involvement has been reported in some cases, including various cardiac abnormalities such as electrocardiographic changes, coronary artery disease, and cardiomyopathy. Here, we present a unique case of a 72-year-old man with GSD-V and both mitral valvulopathy and coronary artery disease, prompting a systematic review to explore the existing literature on cardiac comorbidities in McArdle disease.
Results: Our systematic literature revision identified 7 case reports and 1 retrospective cohort study. The case reports described 7 GSD-V patients, averaging 54.3 years in age, mostly male (85.7%). Coronary artery disease was noted in 57.1% of cases, hypertrophic cardiomyopathy in 28.5%, severe aortic stenosis in 14.3%, and genetic dilated cardiomyopathy in one. In the retrospective cohort study, five out of 14 subjects (36%) had coronary artery disease.
Discussion and conclusion: Despite McArdle disease primarily affecting skeletal muscle, cardiac involvement has been observed, especially coronary artery disease, the frequency of which was moreover found to be higher in McArdle patients than in the background population in a previous study from a European registry. Exaggerated cardiovascular responses during exercise and impaired glycolytic metabolism have been speculated as potential contributors. A comprehensive cardiological screening might be recommended for McArdle disease patients to detect and manage cardiac comorbidities. A multidisciplinary approach is crucial to effectively manage both neurological and cardiac aspects of the disease and improve patient outcomes. Further research is required to establish clearer pathophysiological links between McArdle disease and cardiac manifestations in order to clarify the existing findings.
Keywords: Cardiac comorbidities; Coronary artery disease; McArdle disease; Myophosphorylase deficiency.
© 2024. The Author(s).
Publication types
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 30 May 2024
Pharmacogenomics of coronary artery response to intravenous gamma globulin in kawasaki disease
- Sadeep Shrestha ORCID: orcid.org/0000-0002-7002-357X 1 ,
- Howard W. Wiener 1 ,
- Sabrina Chowdhury 1 ,
- Hidemi Kajimoto 2 ,
- Vinodh Srinivasasainagendra 3 ,
- Olga A. Mamaeva 1 ,
- Ujval N. Brahmbhatt 1 ,
- Dolena Ledee 2 ,
- Yung R. Lau 4 ,
- Luz A. Padilla 1 ,
- Jake Y. Chen 5 ,
- Nagib Dahdah 6 ,
- Hemant K. Tiwari 3 &
- Michael A. Portman 2
npj Genomic Medicine volume 9 , Article number: 34 ( 2024 ) Cite this article
Metrics details
- DNA sequencing
- Risk factors
- Sequence annotation
Kawasaki disease (KD) is a multisystem inflammatory illness of infants and young children that can result in acute vasculitis. The mechanism of coronary artery aneurysms (CAA) in KD despite intravenous gamma globulin (IVIG) treatment is not known. We performed a Whole Genome Sequencing (WGS) association analysis in a racially diverse cohort of KD patients treated with IVIG, both using AHA guidelines. We defined coronary aneurysm (CAA) ( N = 234) as coronary z ≥ 2.5 and large coronary aneurysm (CAA/L) (N = 92) as z ≥ 5.0. We conducted logistic regression models to examine the association of genetic variants with CAA/L during acute KD and with persistence >6 weeks using an additive model between cases and 238 controls with no CAA. We adjusted for age, gender and three principal components of genetic ancestry. The top significant variants associated with CAA/L were in the intergenic regions (rs62154092 p < 6.32E–08 most significant). Variants in SMAT4, LOC100127 , PTPRD, TCAF2 and KLRC2 were the most significant non-intergenic SNPs. Functional mapping and annotation (FUMA) analysis identified 12 genomic risk loci with eQTL or chromatin interactions mapped to 48 genes. Of these NDUFA5 has been implicated in KD CAA and MICU and ZMAT4 has potential functional implications. Genetic risk score using these 12 genomic risk loci yielded an area under the receiver operating characteristic curve (AUC) of 0.86. This pharmacogenomics study provides insights into the pathogenesis of CAA/L in IVIG-treated KD and shows that genomics can help define the cause of CAA/L to guide management and improve risk stratification of KD patients.
Introduction
Kawasaki disease (KD) is a life-threatening acute vasculitis that diffusely affects multiple organ systems in children. Coronary artery dilatations and aneurysms can occur and represent the most serious KD complications 1 , 2 . For most patients, KD is self-limited and lacks the chronic nature of other autoimmune diseases; however, the pathological walls of afflicted vessels show a propensity for forming thrombosis and aneurysms 3 . If untreated or treatment fails, the vasculitis can lead to coronary aneurysm or thrombosis in 20–25% of cases, potentially resulting in ischemic heart disease, myocardial infarction, or death 4 , 5 . Clinical trials conducted in the 1980s and 1990s showed that IVIG treatment dramatically reduced occurrence of persistent CAA defined, primarily by Japanese Ministry of Health criteria 6 , 7 . These criteria stated that coronary artery diameters ≥3 mm in children <5 years and ≥4 mm in children ≥5 years were classified as abnormal. Echocardiographic detection and definition of significant CAA has dramatically improved over the past 2 to 3 decades. A 2007 study by the National Heart Lung and Blood Institute (NHLBI) showed that approximately 18 to 20% of patients had persistent CAA determined using coronary artery z scores 8 , 9 . The 2017 AHA guidelines adjusted the definition for CAA as z score ≥ 2.5 and ≥5 defines a medium to large CAA 1 . Although these coronary abnormalities show higher prevalence in IVIG refractory patients, they can still occur in patients seemingly responsive and showing fever resolution. Most of these children with large aneurysms require daily lifelong anti-coagulation, often with twice daily painful low molecular weight heparin injections, as warfarin is difficult to maintain within therapeutic range in children.
A study based on a large-scale Japanese cohort reported that coronary events did not occur in patients with small CAA; however, 5% of patients with medium CAA and 35% of patients with large CAA had coronary events 10 . North American studies support these data from Japan 11 . The most severe form, giant coronary artery aneurysm (GCA), has been shown to be associated with complications such as luminal narrowing, thrombosis, and major cardiac events 11 , 12 , and substantially alters quality of life for KD patients. Children with GCA require lifelong anti-coagulation, exercise restrictions, and often treatment for ischemic heart disease such as coronary stenting and/or bypass grafting 1 . The majority of patients with GCA develop clinically important stenosis from intimal hypertrophy during the late convalescent phase 13 . Japanese males with coronary artery involvement have a mortality rate 2.4 times higher than expected in general population 14 , but the overall impact on KD patients in the U.S. still requires definition. A recent systematic review showed that mid- to large-sized CAA provided the most significant risk factor for reducing survival of patients with KD 15 . Mid- to large-sized CAA showed a slower recovery with worse prognosis than smaller CAA 16 . Another study reported that the high persistence probability of mid- to large-sized CAA significantly increased the cardiovascular risk at 1 year after KD onset, when approximately two-thirds of the acute myocardial infarction cases occur 17 .
Predicting increased risk for persistent large (medium to giant) size coronary aneurysms despite IVIG treatment is clinically important for intensification of treatment and disease management. Algorithms combining clinical and lab data in Japanese populations predict risk with respect to persistent CAA 18 . However, the Japanese algorithms show poor predictive value for risk in North American and European cohorts 8 , 19 , and fail even in some Asian populations 20 , 21 . Thus, no universal biomarker or algorithm accurately predicts risk for persistent CAA in North America 22 .
A single U.S center retrospectives study showed that presence of early coronary artery dilation is moderately useful in predicting persistent dilation. However, that study did not specifically evaluate for larger higher risk aneurysms 23 . Currently available data indicate that KD susceptibility and treatment response depend on an individual patient’s genetic background 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 . Discrepancies among races or ethnicities also suggest that pathogenesis of KD might vary 34 , 35 . To date, very few studies have focused on genetic risk factors for CAA development in KD patients. We performed the first Whole Genome Sequencing (WGS) association analysis in a cohort of KD patients in a racially diverse North American population exhibiting differences in artery aneurysm formation. We identified multiple loci associated with CAA formation among a pediatric KD population receiving IVIG that can inform on risk stratification; potentially serve as treatment response predictors and guidance toward new therapeutic targets.

Genetic association analysis between individual SNPs and the risk of large (medium/giant) aneurysm
To identify SNPs associated with KD-associated large (medium/giant) coronary aneurysm (CCA/L), clinical data were linked in KD patients with whole genome sequencing data, nested in a clinical cohort as previously described 36 . Basic demographics of the study population with CCA/L ( N = 91) and no aneurysm ( N = 278) are described in Table 1 . Principal component analysis confirmed a good match between KD patients with CCA/L and those without any aneurysm. However, 3 PC were adjusted for in the analyses, as estimated in previous study 36 . A quantile-quantile plot indicated that population stratification had negligible effects on the statistical results (λ genomic control = 0.955). There were several SNPs that exhibited suggestive statistical significance ( p < 10 –5 ) in the additive genetic model, as shown in the Manhattan plot (Fig. 1 ). Of all the SNPs examined, rs62154092 in the intragenic region (nearest gene ACTR3BP2 ) was the most statistically significant (6.32E–08). Among the overall top 10 most significant SNPs, 5 SNPs (all intergenic rs1424006606, rs1396081550, rs1258107032, rs1379390981, rs1424309393) were in chromosome 20, although in different regions. All SNPs statistically significant at p < 10 –4 are listed in Supplementary Table S1 . Among the non-intergenic SNPs, rs28730284 upstream of KLRC2 gene was the most statistically significant (2.20 E-07) and among the top 15 non-intergenic, they were mostly intronic (rs9643846, rs9643847, rs57504215, rs60545202, rs59556769, rs73677451, rs12676292, rs4332118, rs6988966) located in SMAT4 and others in LOC100127 (non-coding RNA rs10276547, rs10280266), PTPRD (intronic rs600075, rs5896385) and TCAF2 (intronic rs1218424730) genes. The most significant exonic SNPs (rs11259953 and rs11259954) were in WHAMM gene (Supplementary Table S1 ). Regional association plots with cluster of SNPs in LD in chromosomes 7, 8 and 9 are shown in (Fig. 1b–d ). Results of corresponding single SNP association with developing any CAA ( N = 233), any persistent CAA ( N = 145) for 2 years, and P-CCA/L for 2 years ( N = 79) vs no aneurysm ( N = 276) are shown in Fig. 2 and Supplementary Table S1 .

a Manhattan Plot displaying Whole Genome Sequence Association results with—Large (medium/giant) Coronary Aneurysm ( N = 92) vs no Coronary Artery Aneurysm ( N = 276). Negative log 10 -transformed P values from the logistic regression model (additive model) are plotted on the y- axis and the SNP genomic locations on the x-axis (colors representing different autosomal chromosomes). Locus Zoom plots for selected gene regions in ( b ) Chromosome 7 with rs10276547 the most significant SNP in the region, ( c ) chromosome 8 with rs9643846 the most significant SNP in the region, ( d ) Chromosome 9 with rs600075 the most significant SNP in the region. Vertical axis (on the left) is the –log 10 of the p-value, the horizontal axis is the chromosomal position. Each dot represents a SNP tested for association with large coronary aneurysm. Linkage disequilibrium between the most significant SNP, listed at the top of each plot, and the other SNPs in the plot is shown by the r 2 legend in each plot. Vertical axis (on the right) is the recombination—the site and rate are represented by red curves.

The outer plot is the association of large aneurysm ( N = 92), the next inner plot is the association of persistent large aneurysm ( N = 79), the next inner plot is the association of any coronary aneurysm ( N = 233) and the fourth inner plot is the association of persistent any coronary aneurysm vs no coronary aneurysm (for each outcome). The innermost plot indicates if SNPs were associated in 1–4 outcomes with p < 1.0E–05.
Gene mapping
Using three gene mapping strategies (position mapping, eQTL mapping and chromatin interaction mapping) in FUMA, we mapped the significant association variants ( P < 10 –5 ) to genes and identified 12 genomic risk loci (Supplementary Table S2 ) and 48 mapped genes associated with CCA/L (Fig. 3 , Supplementary Table S3 ). None of the genes were mapped by all three strategies. Three genes NDUFA5 , ZMAT4 and MICU2 were mapped by physical and eQTL - NDUFA5 is located at the chromosome 7, and its lead SNP rs34163760 is located in the intron of the gene ( P = 4.84E-06). An eQTL analysis showed that with the increasing number of risk alleles of rs34163760, there was a higher mRNA level of NDUFA5 in the Esophagus. The CADD score of rs34163760 is 14.39 indicating a deleterious mutation. ZMAT4 is located in chromosome 8, and its lead SNP rs9643846 is located in the intron of the gene ( P = 6.57E-07). An eQTL analysis showed that with the decreasing number of risk alleles of rs9643846, there was a higher mRNA level of ZMAT4 in thyroid. CADD score of rs9643846 is 15 indicating a deleterious mutation. The third gene MICU2 is located in chromosome 13, and its lead SNP rs12585631 is located in the intron of the gene ( P = 4.11E-06). An eQTL analysis showed that with the decreasing number of risk alleles of rs12585631, there was a higher mRNA level of MICU2 in thyroid. The CADD score of rs12585631 is 15.22 indicating a deleterious mutation. Several genes in chromosomes 4, 7 and 13 were also identified to interact with the chromatin at those sites (Fig. 3 , Supplementary Table S3 ).

The most outer layer is the Manhattan plot (only SNPs with P < 0.05 are displayed). Genomic risk loci are highlighted in blue and the strength of linkage disequilibrium r 2 between each SNP to the lead SNP is given by the following color code: red (r 2 > 0.8), orange (r 2 > 0.6), green (r 2 > 0.4), blue (r 2 > 0.2) and gray (r 2 ≤ 0.2). Genes are mapped by 3-D chromatin interaction (orange) or eQTLs (green), or both (red). a Circos plot for Chromosome 13 with lead SNP rs12585631, ( b ) Circos plot for Chromosome 7 with lead SNP rs10276547, and ( c ) Circos plot for Chromosome 4 with lead SNP rs62330192.
Expression patterns of the 48 prioritized genes were estimated in 54 different tissues (Supplementary Table S4 Supplementary Fig. S1 ). Several of these genes show high expression in aorta and coronary artery tissues.
Genetic risk score (GRS)
Twelve genomic risk loci identified from FUMA yielded an AUC of 0.86. As shown in Fig. 4 , based on the empirical distribution of the AUC from the permutation test, eP was <0.0001, suggesting highly significant genetic risk score from the 12 genomic risk loci. For sensitivity analyses, when GRS for CCA/L was conducted separately in four specific races, AUC of 0.83, 0.78, 0.81 and 0.97 were obtained among White, Asian, Hispanic and African American KD patients.

X-axis is the AUC value after a random permutation of the outcome variable (medium to large coronary aneurysm, z > 5.0) based on the 12 genomic loci from FUMA in predicting the risk score of having a large aneurysm and Y-axis is the frequency. Empirical P-value (eP) is proportion of permutations resulting in a larger AUC than original data.
We analyzed a relatively large North American KD cohort using whole genome sequencing. Treatment with IVIG during the acute phase was an inclusion criterion, so lack of treatment was not a confounding factor. Additionally, persistent coronary artery aneurysm (P-CAA or P-CCA/L) should be considered a failure of IVIG therapy. As noted in Table 1 , the vast majority of medium to giant coronary aneurysms persisted. We identified for the most part novel gene loci that appear to have a relationship with coronary artery aneurysm formation and persistence in KD patients. We have used this same WGS strategy to identify genes related to IVIG refractoriness as defined by AHA guidelines 1 . Prior studies searching for CAA genetic risk variants have used either hypothesis driven strategies or genome-wide association strategy with their inherent limitations. In this study, we specifically used the newest AHA classifications, and sought to determine genetic associations with CCA/L (Z ≥ 5) as these show a lower chance for early regression than do smaller aneurysms (Z ≥ 2.5, but < 5). However, we also found that statistical genetic associations were consistent among all coronary phenotype groups as shown in Table 2 and Fig. 2 . This suggests that pathobiology or at least genetic risk is consistent regardless of size of the aneurysm or propensity for regression.
The most significant SNP related to moderate to giant aneurysm was located in the intergenic region with the closest gene being ACTR3BP2 , a pseudogene with unknown function. However, among the top SNPs in the gene region, rs28730284 was located just upstream of the KLRC2 gene and has intriguing potential biological relevance to KD. The KLRC2 gene encodes the C-type lectin NKG2C (Killer cell lectin receptor-2). Natural Killer (NK) cells mediate innate immune responses against virally infected and malignant cells 37 , 38 , 39 . NK cell function such as production of proinflammatory cytokines, depends on a balance between activating and inhibiting signals triggered by multiple surface receptors, including NKG2C 40 . Polymorphisms in KLCR2 have been shown to influence both function and expression of NK cells. Furthermore, SNPs in KLRC2 are associated with microvascular inflammation during renal graft transplant rejection. Importantly, all type NK cell (CD56 ++ CD16 +− , CD56 + CD16 + , CD56 − CD16 + ) expression is reduced in KD patients compared to febrile or non-febrile controls, while CD56 − CD16 + NK cell expression was significantly lower in IVIG-resistant patients than in the IVIG-responsive 41 .
Multiple intronic SNPs were found in ZMAT4 gene, which encodes the Zinc Finger Matrin-Type 4 protein. This gene was also identified by FUMA. SNPs within ZMAT4 are associated with diseases such as Spinocerebellar Ataxia and Myopia 42 , and copy number variations are associated with hematological malignancies 43 . Function of this particular Zinc-Finger protein remains undefined, so a potential biological role in KD would be unclear. The top two exonic SNPs were in the WHAMM gene. This gene encodes a protein nucleation-promoting factor that regulates the Actin-related protein 2/3 complex, but any biological relevance to KD would be highly speculative. Additionally, we found SNP (rs1052373) within the MYBPC3 exon region as marginally significant. MYBPC3 (myosin binding protein c3) function is well established and mutations are involved in the pathology of hypertrophic cardiomyopathy 44 , 45 . This particular SNP has also been associated with athletic endurance 46 . However, any suggestion of biological relevance for these exonic SNPs to KD would be highly speculative.
Multiple SNPs were also found in regions near Facioscapulohumeral muscular dystrophy (FSHD) region-1( FRG1DP ). FRG1 acts on upstream of FGF2, which signals activation of the AKT/ERK signaling axis in endothelial cells. Interestingly, we previously reported that this gene is associated with IVIG response in KD patients. FRG1DP has been linked to angiogenesis and retinal vasculpathy in FSHD patients including development of micro aneurysms. Additionally, altered expression for FRG-1 protein leads altered angiogenesis in human umbilical vein endothelial cells (HUVECs).
Using FUMA we found several genes potentially related to CAA/L in IVIG-treated KD patients. MICU2 is a calcium sensitive regulatory subunit of the mitochondrial calcium uniporter and is important for reducing oxidative stress particularly in endothelial cells. MICU 2 −/− mice exhibit abnormal cardiac diastolic relaxation but also develop abdominal aortic aneurysms, which spontaneously rupture with only modest increases in blood pressure. NDUFA5 encodes NADH dehydrogenase [ubiquinone] 1 alpha subcomplex subunit 5, a critical component of mitochondrial respiratory complex 1, which facilitates the translocation of protons across to the mitochondrial inner membrane. A SNP in NDUFA5 was also a top hit in a small Taiwanese KD study evaluating genetic risk for CAA formation 47 . Thus, our findings for these two genes regulating oxidative stress response suggest that mitochondria play a role in development of CAA and should be a target for future research 48 .
We previously published a WGS pharmacogenomics analyses of IVIG response in KD using “persistent or recurrent fever” as the benchmark for IVIG resistance 36 . Data suggests that IVIG resistance or refractoriness is a risk factor for persistent CAA. However, we did not find numbers of variants that were associated with both coronary aneurysms and IVIG resistance. This lack of genetic association uniformity between these two different outcomes suggests that their biological pathways and mechanisms may be different. However, the list of novel genes provides new insights into the pathogenesis of KD.
Genetic analyses of coronary aneurysms in KD are complicated by multiple potential confounding factors. Prior studies, which have identified numerous significant variants associated with coronary aneurysms, did not account for the IVIG therapeutic effect 49 , 50 , 51 . Clinical trials clearly show that IVIG reduces the risk of CAA 52 . However, those previous genetic studies for the most part do not clarify whether study participants received appropriate IVIG treatment. Thus those prior cohorts could and probably do include patients whom did not receive timely IVIG. We used strict criteria for IVIG treatment in our study subjects in accordance with pharmacogenomics design. Accordingly, our results using different design and methodology did not replicate findings from prior studies such as associations with coronary aneurysms for variants in ITPKC 51 , KCNN2 50 , NEBL and TUBA3C 47 , SLC8A1 53 , and the matrix metalloproteinase ( MMP ) gene family 54 . Likewise, Huang et al 55 reported TET mRNA levels associated with IVIG and DMNT1 mRNA levels with CAA; however, there were no SNPs in these gene regions that were statistically significant in our study.
Two other studies indicated association of TIFAB 56 and PLCB1 57 genes. Although the same SNPs were not replicated in our study, we found several SNPs in these gene regions that were associated with CAA in our study (Table S1 ). Unlike studies predominantly using Asian populations, our cohort included 4 races (Whites, Asians, African-Americans, and Hispanics). We had fewer cases of African-Americans and Hispanics and we were underpowered to conduct race-specific analyses (Supplementary Table S5 ). However, in the main combined cohort, we adjusted for three principal components which resulted in λ genomic control = 0.955, suggesting no major confounding factors (Supplementary Figure S2 ).
We also used 12 genomic loci from FUMA to test for overall prediction of risk for developing CAA/L, a genetic predictive risk score. The AUC based on these markers is promising and the empirical risk models based on 10,000 simulated cases and controls had considerably higher AUC than theoretically achievable. Although sample size is small, all race-specific analyses also showed similar trends with high AUC. These specific markers need to be validated in different IVIG-treated KD populations; however, there is potential clinical utility in developing a point-of-care assay based on panels of genetic risk markers to predict who will develop CAA/L and/or other sequalae. Accurate prediction can assist in developing a treatment plan during the acute KD phase 58 .
The main limitation for this study is the lack of a validation cohort. This is a common limitation of clinical trials and pharmacogenomics studies of rare diseases, although our cohort is the largest reported to date with a clear IVIG treatment phenotype. Further validations as well as functional studies of these variants will be needed in the future.
In summary, using WGS we have identified several novel genes and loci, which could have a functional impact on coronary artery response to IVIG in KD. Additionally, these loci could be used in identifying new personalized therapeutic avenues as well as developing an important predictive risk score for persistence of coronary artery aneurysms despite IVIG treatment.
Study populations and primary outcome
We performed whole genome sequencing in 504 KD patients who were diagnosed and treated with IVIG (2 g/Kg on a single infusion) and aspirin 36 , both using the American Heart Association (AHA) criteria 1 , 59 . All patients included in the study had echocardiography data that assessed for coronary artery aneurysm (CAA) (212 Whites, 75 Asians, 50 Hispanics and 32 Blacks). Coronary artery internal diameters in the left main coronary artery (LMCA), left anterior descending artery (LAD), and right coronary artery (RCA) obtained by echocardiography. Coronary artery dimensions were normalized for body surface area and converted to z- scores (SDs from a predicted normal mean) based on nonlinear regression equations derived from a normal nonfebrile population 60 . Echocardiographic data were collected at baseline, at 2 weeks, and 5–6 weeks or after following fever onset. The > 5 -6 week echocardiograms were assessed for persistence of the CAAs. We used the Boston z -score model 1 and as defined by AHA, coronary abnormality or aneurysm was considered if z ≥ 2.5. According to AHA guidelines, we categorized positive or negative coronary artery aneurysm (CAA) occurring at any time point with z score ≥ 2.5 as “CAA”. Persistent CAA (P-CAA) was defined as any aneurysm z ≥ 2.5 for upto 5–6 weeks. We also categorized large CAA (CAA/L) as medium to giant coronary aneurysm for a z score ≥5.0 at any time; and then persistent CCA/L (P-CCA/L) if aneurysm z ≥ 5.0 remained for upto 5–6 weeks. Genomic comparisons were made for each of the 4 categories versus those without any aneurysm (z < 2.5).
The parent cohort/study and this pharmacogenomic study conformed to the procedures for informed consent (parental permission) approved by institutional review boards at all sponsoring organizations .The pharmacogenomic data management and analysis procedure was approved by the University of Alabama at Birmingham Institutional Review Board (IRB). The study was conducted in accordance with the local legislation and institutional requirements following the ethical guidelines of the Declaration of Helsinki. Written informed consent for minor participation (children) in this study was provided by the participants’ legal guardians/next of kin.
Whole genome sequencing and variant calling
With consent from the parents or legal guardian, whole blood or saliva was collected to extract genomic DNA, as previously described 36 . PCR-free libraries were generated using the BGI DNBSEQ True PCR-Free platform (Beijing Genomics Institute; Guangdong, Shenzhen, China) and whole genome sequencing was performed on the MGISEQ-2000 instrument (Beijing Genomics Institute; Guangdong, Shenzhen, China) to generate 100 bp paired-end reads, as previously described 36 . All reads that passed were aligned to the human reference genome (hg38) using Burrows-Wheeler aligner (BWA) v 0.7.17. The average sequencing depth was 30x per individual. Broad Institute’s Genome Analysis Tool Kit (GATK) best practices workflow was used for quality control and informatics pre-processing of the data. Variant-level QC was performed using the Variant Quality Score Recalibration tool (VQSR) from the Genome Analysis Toolkit (GATK), using the recommended threshold of 99% sensitivity for the “true” variant. As we previously reported, we included 5 duplicate samples, which showed overall high SNP genotype concordance, with a kinship coefficient estimate, Φ > 0.497 between duplicates. For the SNPs we report association, the concordant genotypes were confirmed between all duplicate samples.
Whole genome sequencing (WGS) association—single-variant analysis
Intensive quality control of the genetic data including minor allele frequency (MAF), call rate (CR), and p values of Hardy-Weinberg equilibrium (HWE), were applied to filter uncertain SNPs as described previously 36 , resulting in 46,718,826 variants (21,675,492 singletons) and 25,043,334 polymorphic SNPs were included in the analysis. Logistic regressions models were conducted using PLINK 1.90 to examine the association of individual autosomal SNPs using an additive model in a case/control design, for the main outcome (medium/giant aneurysm, 91 cases (52 W, 3AA, 20His, 16As) and 278 controls (160 W, 29AA, 30His, 59As) and the three secondary outcomes (Table 1 ). Age, gender and three principal components (PCAs) of genetic ancestry were adjusted in the models. Quantile-quantile (QQ) plots and Manhattan plots were produced with the qqman package in R. The crude and adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were also calculated for the top hits using unconditional univariate logistic regression analysis to evaluate the associations between genotypes and medium/giant aneurysm.
Identification of genes and their roles using FUMA
Functional annotation was conducted in Functional Mapping and Annotation (FUMA) v1.3.0 61 , using variants of interest from the WGS association analysis ( p < 1.0 × 10 −5 and all variants in r 2 < 0.6 with them). Lead SNPs were defined from these independent statistically significant SNPs if pairwise SNPs had r 2 < 0.1. The maximum distance between LD blocks to merge into a genomic locus was 250 kb. The genetic data of mixed population in 1000 G phase3 were used as reference to estimate LD. Three methods were used to map SNPs to genes: (a) physical distance (within a 10-kb window) from known protein-coding genes in the human reference assembly, (b) expression quantitative trait loci (eQTL) variant mapping using 62 , and (c) 3D chromatin interaction mapping (Hi-C) 63 . Combined Annotation-Dependent Depletion (CADD) analysis 64 with a minimum score of >12.37 (considered to be suggestive deleterious) was used to filter the variants. Annotation of enhancers 65 , tissue-specific expression of genes identified via Hi-C and eQTL mapping 62 were queried in FUMA tool and Genotype Tissue Expression (GTEx) database ( https://gtexportal.org/home/ ).
Genetic risk score computation
All genomic risk loci from FUMA were used to estimate gene risk score (GRS) by a simple risk alleles count method. Discriminative power attributable to the GRS was estimated and compared by plotting receiver operating characteristic (ROC) curves and calculating the area under the curve (AUC) for the case-control samples. The AUC compares the rates of true positives (sensitivity) and false positives (1—specificity) and assesses the overall performance of genetic risk score models. Next, case and control status was randomly permuted 10,000 times and AUC was estimated with each pseudo case-control status. An empirical p-value (eP), which is the proportion of AUC based on randomization distribution of cases and controls that are more extreme than our observed AUC from the actual case (medium/giant aneurysm) and control (no aneurysm) status, was then calculated.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data have been deposited with links to BioProject accession number PRJNA1055092 in the NCBI BioProject database ( https://www.ncbi.nlm.nih.gov/bioproject/ ). The datasets used and/or analyzed in this study are also available from the corresponding author on reasonable request.
Code availability
Analytical codes will be available upon request from the Corresponding author.
McCrindle, B. W. et al. Diagnosis, treatment, and long-term management of Kawasaki disease: A scientific statement for health professionals From the American Heart Association. Circulation 135 , e927–e999 (2017).
Article PubMed Google Scholar
Kawasaki, T. [Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children]. Arerugi 16 , 178–222 (1967).
CAS PubMed Google Scholar
Orenstein, J. M. et al. Three linked vasculopathic processes characterize Kawasaki disease: a light and transmission electron microscopic study. PLoS One 7 , e38998 (2012).
Article CAS PubMed PubMed Central Google Scholar
Kato, H. et al. Long-term consequences of Kawasaki disease. A 10- to 21-year follow-up study of 594 patients. Circulation 94 , 1379–1385 (1996).
Article CAS PubMed Google Scholar
Burns, J. C. & Glode, M. P. Kawasaki syndrome. Lancet 364 , 533–544 (2004).
Newburger, J. W. et al. A single intravenous infusion of gamma globulin as compared with four infusions in the treatment of acute Kawasaki syndrome. N. Engl. J. Med . 324 , 1633–1639 (1991).
Newburger, J. W. et al. The treatment of Kawasaki syndrome with intravenous gamma globulin. N. Engl. J. Med. 315 , 341–347 (1986).
Sleeper, L. A. et al. Evaluation of Kawasaki disease risk-scoring systems for intravenous immunoglobulin resistance. J. Pediatr. 158 , 831–835.e3 (2011).
Newburger, J. W. et al. Randomized trial of pulsed corticosteroid therapy for primary treatment of Kawasaki disease. N. Engl. J. Med. 356 , 663–675 (2007).
Miura, M. et al. Association of severity of coronary artery aneurysms in patients with kawasaki disease and risk of later coronary events. JAMA Pediatr. 172 , e180030 (2018).
Article PubMed PubMed Central Google Scholar
McCrindle, B. W. et al. Medium-term complications associated with coronary artery aneurysms after Kawasaki disease: A study from the international kawasaki disease registry. J. Am. Heart Assoc. 9 , e016440 (2020).
Friedman, K. G. et al. Coronary artery aneurysms in Kawasaki disease: Risk factors for progressive disease and adverse cardiac events in the US population. J. Am. Heart Assoc. 5 , e003289 (2016).
Patel, A. S., Bruce, M., Harrington, W. & Portman, M. A. Coronary artery stenosis risk and time course in Kawasaki disease patients: Experience at a US tertiary pediatric centre. Open Heart 2 , e000206 (2015).
Newburger, J. W. et al. Summary and abstracts of the Seventh International Kawasaki Disease Symposium: December 4-7, 2001, Hakone, Japan. Pediatr. Res 53 , 153–157 (2003).
PubMed Google Scholar
Lee, J. J. Y. et al. The long-term cardiac and noncardiac prognosis of Kawasaki disease: A systematic review. Pediatrics 149 , e2021052567 (2022).
Hu, J. & Ren, W. Analysis of the risk factors in prognosis of Kawasaki disease with coronary artery lesions. Front Pediatr. 9 , 798148 (2021).
Lin, M. T. et al. Acute and late coronary outcomes in 1073 patients with Kawasaki disease with and without intravenous gamma-immunoglobulin therapy. Arch. Dis. Child 100 , 542–547 (2015).
Kobayashi, T. et al. Risk stratification in the decision to include prednisolone with intravenous immunoglobulin in primary therapy of Kawasaki disease. Pediatr. Infect. Dis. J. 28 , 498–502 (2009).
Davies, S. et al. Predicting IVIG resistance in UK Kawasaki disease. Arch. Dis. Child 100 , 366–368 (2015).
Fu, P. P., Du, Z. D. & Pan, Y. S. Novel predictors of intravenous immunoglobulin resistance in Chinese children with Kawasaki disease. Pediatr. Infect. Dis. J. 32 , e319–e323 (2013).
Shin, J., Lee, H. & Eun, L. Verification of current risk scores for Kawasaki disease in Korean children. J. Korean Med. Sci. 32 , 1991–1996 (2017).
Portman, M. A. & Shrestha, S. One size does not fit all: Genetic prediction of kawasaki disease treatment response in diverse populations. Circ. Cardiovasc Genet 10 , e001917 (2017).
Son, M. B. F. et al. Predicting coronary artery aneurysms in Kawasaki Disease at a North American Center: An assessment of Baseline z Scores. J. Am. Heart Assoc. 6 , e005378 (2017).
Makowsky, R. et al. FcgammaR gene copy number in Kawasaki disease and intravenous immunoglobulin treatment response. Pharmacogenet Genomics 23 , 455–462 (2013).
Shrestha, S. et al. Role of activating FcgammaR gene polymorphisms in Kawasaki disease susceptibility and intravenous immunoglobulin response. Circ. Cardiovasc Genet 5 , 309–316 (2012).
Shrestha, S. et al. Functional FCGR2B gene variants influence intravenous immunoglobulin response in patients with Kawasaki disease. J. Allergy Clin. Immunol. 128 , 677–680 (2011).
Wu, S. F., Chang, J. S., Wan, L., Tsai, C. H. & Tsai, F. J. Association of IL-1Ra gene polymorphism, but no association of IL-1beta and IL-4 gene polymorphisms, with Kawasaki disease. J. Clin. Lab Anal. 19 , 99–102 (2005).
Minami, T. et al. A polymorphism in plasma platelet-activating factor acetylhydrolase is involved in resistance to immunoglobulin treatment in Kawasaki disease. J. Pediatr. 147 , 78–83 (2005).
Burns, J. C. et al. Family-based association analysis implicates IL-4 in susceptibility to Kawasaki disease. Genes Immun. 6 , 438–444 (2005).
Burns, J. C. et al. Genetic variations in the receptor-ligand pair CCR5 and CCL3L1 are important determinants of susceptibility to Kawasaki disease. J. Infect. Dis. 192 , 344–349 (2005).
Khor, C. C. et al. Genome-wide association study identifies FCGR2A as a susceptibility locus for Kawasaki disease. Nat. Genet. 43 , 1241–1246 (2011).
Onouchi, Y. et al. A genome-wide association study identifies three new risk loci for Kawasaki disease. Nat. Genet 44 , 517–521 (2012).
Elakabawi, K., Lin, J., Jiao, F., Guo, N. & Yuan, Z. Kawasaki disease: Global burden and genetic background. Cardiol. Res 11 , 9–14 (2020).
Holman, R. C. et al. Racial/ethnic differences in the incidence of Kawasaki syndrome among children in Hawaii. Hawaii Med J. 69 , 194–197 (2010).
PubMed PubMed Central Google Scholar
Padilla, L. A. et al. Kawasaki disease and clinical outcome disparities among black children. J. Pediatr. 229 , 54–60 e2 (2021).
Shrestha, S. et al. Pharmacogenomics of intravenous immunoglobulin response in Kawasaki disease. Front. Immunol. 14 , 1287094 (2024).
Herberman, R. B., Nunn, M. E., Holden, H. T. & Lavrin, D. H. Natural cytotoxic reactivity of mouse lymphoid cells against syngeneic and allogeneic tumors. II. Characterization of effector cells. Int J. Cancer 16 , 230–239 (1975).
Kiessling, R., Klein, E. & Wigzell, H. “Natural” killer cells in the mouse. I. Cytotoxic cells with specificity for mouse Moloney leukemia cells. Specificity and distribution according to genotype. Eur. J. Immunol. 5 , 112–117 (1975).
Trinchieri, G. & Santoli, D. Anti-viral activity induced by culturing lymphocytes with tumor-derived or virus-transformed cells. Enhancement of human natural killer cell activity by interferon and antagonistic inhibition of susceptibility of target cells to lysis. J. Exp. Med. 147 , 1314–1333 (1978).
Long, E. O., Kim, H. S., Liu, D., Peterson, M. E. & Rajagopalan, S. Controlling natural killer cell responses: integration of signals for activation and inhibition. Annu. Rev. Immunol. 31 , 227–258 (2013).
Choi, I. S. et al. Circulating immune cell profile and changes in intravenous immunoglobulin responsiveness over the disease course in children With Kawasaki Disease. Front Pediatr. 9 , 792870 (2021).
Cheong, K. X., Yong, R. Y. Y., Tan, M. M. H., Tey, F. L. K. & Ang, B. C. H. Association of VIPR2 and ZMAT4 with high myopia. Ophthalmic Genet 41 , 41–48 (2020).
Wan, J. et al. The association between the copy-number variations of ZMAT4 and hematological malignancy. Hematology 16 , 20–23 (2011).
Helms, A. S. et al. Effects of MYBPC3 loss-of-function mutations preceding hypertrophic cardiomyopathy. JCI Insight 5 , e133782 (2020).
van Velzen, H. G. et al. Clinical characteristics and long-term outcome of hypertrophic cardiomyopathy in individuals with a MYBPC3 (myosin-binding protein C) founder mutation. Circ. Cardiovasc. Genet 10 , e001660 (2017).
Al-Khelaifi, F. et al. Genome-wide association study reveals a novel association between MYBPC3 gene polymorphism, endurance athlete status, aerobic capacity and steroid metabolism. Front Genet 11 , 595 (2020).
Kuo, H. C. et al. Genome-wide association study identifies novel susceptibility genes associated with coronary artery aneurysm formation in Kawasaki disease. PLoS One 11 , e0154943 (2016).
Beckley, M. A., Shrestha, S., Singh, K. K. & Portman, M. A. The role of mitochondria in the pathogenesis of Kawasaki disease. Front Immunol. 13 , 1017401 (2022).
Hoggart, C. et al. Identification of novel locus associated with coronary artery aneurysms and validation of loci for susceptibility to Kawasaki disease. Eur. J. Hum. Genet 29 , 1734–1744 (2021).
Kim, J. J. et al. Identification of KCNN2 as a susceptibility locus for coronary artery aneurysms in Kawasaki disease using genome-wide association analysis. J. Hum. Genet 58 , 521–525 (2013).
Liu, J., Yuan, P., Pang, Y. & Su, D. ITPKC polymorphism (rs7251246 T > C), coronary artery aneurysms, and thrombosis in patients with Kawasaki disease in a Southern Han Chinese population. Front Immunol. 14 , 1184162 (2023).
Oates-Whitehead, R. M. et al. Intravenous immunoglobulin for the treatment of Kawasaki disease in children. Cochrane Database Syst. Rev. 2003 , CD004000 (2003).
Shimizu, C. et al. Genetic variation in the SLC8A1 calcium signaling pathway is associated with susceptibility to Kawasaki disease and coronary artery abnormalities. Circ. Cardiovasc Genet 9 , 559–568 (2016).
Shimizu, C. et al. Matrix metalloproteinase haplotypes associated with coronary artery aneurysm formation in patients with Kawasaki disease. J. Hum. Genet 55 , 779–784 (2010).
Huang, Y. H. et al. Decreased DNA methyltransferases expression is associated with coronary artery lesion formation in Kawasaki disease. Int J. Med. Sci. 16 , 576–582 (2019).
Kwon, Y. C. et al. Identification of the TIFAB gene as a susceptibility locus for coronary artery aneurysm in patients with Kawasaki disease. Pediatr. Cardiol. 40 , 483–488 (2019).
Lin, Y. J. et al. Genetic variants in PLCB4/PLCB1 as susceptibility loci for coronary artery aneurysm formation in Kawasaki disease in Han Chinese in Taiwan. Sci. Rep. 5 , 14762 (2015).
Wu, J., Pfeiffer, R. M. & Gail, M. H. Strategies for developing prediction models from genome-wide association studies. Genet Epidemiol. 37 , 768–777 (2013).
Newburger, J. W. et al. Diagnosis, treatment, and long-term management of Kawasaki disease: A statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 114 , 1708–1733 (2004).
McCrindle, B. W. et al. Coronary artery involvement in children with Kawasaki disease: Risk factors from analysis of serial normalized measurements. Circulation 116 , 174–179 (2007).
Watanabe, K., Taskesen, E., van Bochoven, A. & Posthuma, D. Functional mapping and annotation of genetic associations with FUMA. Nat. Commun. 8 , 1826 (2017).
Consortium, G. T. Human genomics. The genotype-tissue expression (GTEx) pilot analysis: Multitissue gene regulation in humans. Science 348 , 648–660 (2015).
van Berkum, N. L. et al. Hi-C: a method to study the three-dimensional architecture of genomes. J. Vis. Exp. 6 , 1869 (2010).
Kircher, M. et al. A general framework for estimating the relative pathogenicity of human genetic variants. Nat. Genet 46 , 310–315 (2014).
Roadmap Epigenomics, C. et al. Integrative analysis of 111 reference human epigenomes. Nature 518 , 317–330 (2015).
Article Google Scholar
Download references
Acknowledgements
The parent cohort/study and this genomic study conformed to the procedures for informed consent (parental permission) approved by institutional review boards at all sponsoring organizations and to human-experimentation guidelines set forth by the United States Department of Health and Human Services. We thank the participating patients and their parents. This study was supported by the National Institutes of Health grant NHLBI-1R01HL146130.
Author information
Authors and affiliations.
Department of Epidemiology, School of Public Health, University of Alabama at Birmingham, Birmingham, AL, USA
Sadeep Shrestha, Howard W. Wiener, Sabrina Chowdhury, Olga A. Mamaeva, Ujval N. Brahmbhatt & Luz A. Padilla
Division of Cardiology, Seattle Children’s and University of Washington Department of Pediatrics, Seattle, WA, USA
Hidemi Kajimoto, Dolena Ledee & Michael A. Portman
Department of Biostatistics, School of Public Health, University of Alabama at Birmingham, Birmingham, AL, USA
Vinodh Srinivasasainagendra & Hemant K. Tiwari
Division of Pediatric Cardiology, Heersink School of Medicine, University of Alabama at Birmingham, Birmingham, AL, USA
Yung R. Lau
Department of Biomedical Informatics and Data Science, Heersink School of Medicine, University of Alabama at Birmingham, Birmingham, AL, USA
Jake Y. Chen
Division of Pediatric Cardiology, CHU Ste-Justine, Universite de Montreal, Montreal, QC, Canada
Nagib Dahdah
You can also search for this author in PubMed Google Scholar
Contributions
SS: Conceptualization, Study design, Funding acquisition, Methodology, Analysis, Overall supervision, Results validation & visualization, Manuscript writing – original draft. HW: Data management & pre-processing, WGS analysis, Writing – review & editing. SC: Results tabulation and visualization, Writing – review & editing. HK: Clinical data management, Biospecimen handling, Writing – review & editing. VS: Data pre-processing, Bioinformatics, Results tabulation and visualization, Writing – review & editing. OAM: Sample processing, DNA extraction & quantification, Writing – review & editing. UNB: Results tabulation and visualization, Writing – review & editing. DL: Clinical data management, Project administration, Writing – review & editing. YL: Phenotyping and clinical validation, Writing – review & editing, LAP: Data management, Methodology, Writing – review & editing. JC: Supervision of genomic data pre-processing, Writing – review & editing. ND: Phenotyping and clinical validation, Methodology, Writing – review & editing. HT: Supervision of genomic data pre-processing & analysis, Methodology, Writing – review & editing. MP: Conceptualization, Phenotyping and clinical validation, Funding acquisition, Investigation, Methodology, Clinical Supervision, Results validation & visualization, Writing – review & editing
Corresponding author
Correspondence to Sadeep Shrestha .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplemental material, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Shrestha, S., Wiener, H.W., Chowdhury, S. et al. Pharmacogenomics of coronary artery response to intravenous gamma globulin in kawasaki disease. npj Genom. Med. 9 , 34 (2024). https://doi.org/10.1038/s41525-024-00419-7
Download citation
Received : 31 January 2024
Accepted : 09 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1038/s41525-024-00419-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 24, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
Researchers study indicators of coronary obstructions in women with established coronary artery disease
by Bentham Science Publishers
Researchers in medicine have been studying the composition of biochemical markers to determine correlations between during health and disease for several decades. The data helps health care professionals to accurately diagnose and treat diseases, some of which are life threatening.
A team of researchers from Brazil has studied biomarkers, ratios, and indexes as indicators of coronary obstructions in women with established coronary artery disease , regardless of whether they have diabetes.
The paper is published in The Open Biomarkers Journal .
A cross-sectional study was conducted on 42 women with confirmed atherosclerotic coronary disease, divided into diabetic and non-diabetic groups, who were scheduled for angioplasty or coronary bypass surgery. Blood samples were taken right before the coronary procedures to measure various lab values, including blood sugar, HbA1c, insulin, HDL-C, PON-1, free cholesterol , LDL-C, Apo A-1, Apo B, and triglycerides.
In diabetic patients , insulin levels were positively correlated with triglycerides (p < 0.0108; r = 0.2009), apo B (p < 0.0006; r = 0.3737), non-HDL cholesterol (p < 0.0084; r = 0.2156), and free cholesterol (p < 0.0084; r = 0.3251). Using a linear regression model, insulin in diabetic patients was linked to blood sugar, triglycerides, and HOMA-IR (p < 0.001, R2 = 0.9868).
In non-diabetics, insulin was only associated with HOMA-IR (p = 0.002, R2 = 0.9031). When triglycerides were used as the dependent variable, they were associated with HOMA-IR in both groups (diabetics: p = 0.006, R2 = 0.2504; non-diabetics: p = 0.014, R2 = 0.4697). Additionally, the TG/HDL-C ratio was higher than 2.5 in 90% of diabetics and 83.33% of non-diabetic patients.
The high number of women with a TG/HDL-C ratio over 2.5, along with the links between insulin, HOMA-IR, and TG/HDL-C, as well as the correlations with apoB, non-HDL-C, and free cholesterol, should be considered as indicators of early coronary atherosclerosis in women .
Explore further
Feedback to editors

Tobacco firms invest billions in medical products: Call for journals to ban research by the firms, their subsidiaries
3 hours ago

New avenues to developing personalized treatments for schizophrenia
4 hours ago

Study: Access to targeted lung cancer drug is cost-prohibitive globally

Researchers identify factors that heighten risk for catheter-associated urinary tract infections and sepsis
5 hours ago

'Sticky and strain-gradient artificial epineurium' can heal severed nerves in only one minute, study claims

Could ultra-processed foods be associated with your insomnia?
6 hours ago

Tiny worm helps uncover long-lasting prenatal effects from amphetamines

PTSD, anxiety is rising among college students

Study confirms effectiveness of 'watch-and-wait' approach to prostate cancer

Cause of common type of heart failure may be different for women and men
Related stories.

Do sex differences in how adipose tissue responds to insulin explain why type 2 diabetes is more common in men?
May 10, 2024

Women with heart disease are less likely to receive life-saving drugs than men, researchers find
Apr 25, 2024
Insulin resistance under-diagnosed in non-diabetics with Parkinson's disease
Aug 2, 2018

Moving more may match focused exercise in prediabetes
Dec 7, 2017

Risk predictive model developed for patients with multivessel coronary artery lesions
Jan 29, 2024

Diabetics more likely to experience high blood sugar after joint surgery
Mar 15, 2019
Recommended for you

Mummies study finds heart disease plagued the ancients, too
15 hours ago

Study finds older adults hospitalized for heart failure had high risk of kidney complications
May 29, 2024

Study shows orange peel extract may improve heart health
May 28, 2024

Study finds blood clot risk is influenced by angle at which pulmonary veins reach the heart

Promising results for hyperlipidemia treatment reduce risk of cardiovascular events
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Arq Bras Cardiol
- v.103(3); 2014 Sep

Case 4/2014 - A 66-Year-Old Man with Acute Myocardial Infarction and Death in Asystole after Primary Coronary Angioplasty
A 66-year-old man sought medical care at the hospital due to severe chest pain lasting for 24 hours. The patient was aware of being hypertensive and was a smoker. Without any prior symptom, he started to have severe chest pain and sought emergency medical care after about 24 hours, due to pain persistence.
At physical examination (August 13, 2005, 10 PM) he had a heart rate of 90 bpm and blood pressure of 110/70 mmHg. Lung examination showed no alterations. Heart assessment showed a systolic murmur in the lower left sternal border and mitral area.
The initial electrocardiogram (August 13, 2005, 22 h) showed HR of 100 bpm, sinus rhythm, 1 st -degree atrioventricular block (PR 240 ms), low-voltage QRS complexes in the frontal plane, QRS complex electrical alternans and extensive ongoing anterior wall infarction (QS V1 to V6, ST elevation in the same leads and QS in the inferior wall, II, III and aVF) ( Figure 1 ).

ECG: low QRS voltage in the frontal plane, electrical alternans of QRS complexes, electrically inactive lower wall area and extensive ongoing myocardial infarction.
Acetylsalicylic acid by oral route and 5 mg of intravenous metoprolol were administered. The patient had bradycardia and cardiorespiratory arrest in pulseless electrical activity, reversed after five minutes. He developed hypotension and peripheral hypoperfusion and was transferred to InCor (The Heart Institute).
On admission he had received heparin and continuous intravenous norepinephrine. BP was 60/30 mmHg.
The ECG (August 13, 2005, 11:36 PM) disclosed heart rate of 116 bpm, junctional escape rhythm with sinus arrest and atrial extrasystoles); low-voltage QRS complex in the frontal plane, extensive ongoing anterior acute myocardial infarction, inactive area in the inferior wall; presence of ST elevation at V1 to V5 and ST depression in leads I, II and aVF; ST elevation in aVR ( Figure 2 ).

ECG: low QRS voltage in the frontal plane, electrically inactive lower wall area and anterior myocardial infarction with increased ST elevation, still with positive T waves, "hyperacute phase of myocardial infaction".
Coronary angiography was indicated, which disclosed anterior interventricular branch occlusion and images suggestive of intracoronary thrombus, lesion of 70% in the circumflex artery, 50% in the right coronary artery and 70% in the ostium of the right posterior descending branch. Angioplasty was performed with stent implant in the anterior interventricular artery, but distal flow was not restored. This was followed by cardiac arrest in asystole, which did not respond to treatment and the patient died.
Clinical Aspects
This clinical case reports on a 66-year-old hypertensive patient, long-term smoker, who sought medical care due to acute chest pain. The main diagnostic hypothesis for this clinical case is of acute coronary syndrome.
Chest pain is one of the most common reasons for seeking emergency care and remains a challenge for the clinician, due to the difficulty in differentiating between non-emergency diagnoses and those of high morbidity and mortality, such as acute coronary syndrome (ACS), aortic dissection and pulmonary thromboembolism.
In the assessment of acute chest pain, there are three basic parameters for its management: clinical examination (clinical history and physical examination), electrocardiogram (ECG) and myocardial necrosis markers. They should be analyzed together to provide a safer approach to the patient, especially when it is necessary ruling out ACS. Chest radiography, chest Computed Tomography Angiography (CTA), echocardiography and other tests may be useful in the differential diagnosis.
Approximately 15-25% of patients presenting in the ER with chest pain are diagnosed with acute coronary syndrome, and this represents its more frequent clinical manifestation 1 . Therefore, in the first step of the evaluation, which is the clinical examination, the greater determinant of an ischemic etiology is the characteristic presence of angina.
Angina is often described as a burning or compression sensation or difficulty breathing, located in the precordial region or any other region of the chest, radiating to the neck, shoulder and left arm. It usually increases in intensity within minutes and may be accompanied by symptoms such as nausea and sweating. It can be triggered by physical or emotional stress and relieved by rest or use of nitrates. It should also be remembered that ACS can occur without obvious precipitating factors and be asymptomatic or present as ischemic equivalent, especially in the elderly and diabetic patients with autonomic dysfunction (dyspnea, syncope and pre-syncope).
On the other hand, there are characteristics of pain that make the diagnosis of ACS unlikely, such as pleuritic pain (reproduced by respiratory movements) located with the fingertip, pain in meso/hypogastrium region and reproduction of pain with local palpation or movement. These features raise the suspicion of other differential diagnoses such as pericarditis, pleuritis, gastrointestinal or musculoskeletal diseases.
In the present case report, the patient presented with prolonged chest pain, which does not rule out acute coronary syndrome (ACS), but raises the possibility of some condition associated with this coronary picture, such as pericarditis or mechanical complications.
Among the most important risk factors for atherosclerotic disease risk are dyslipidemia, diabetes mellitus, hypertension, male gender, older age, obesity/metabolic syndrome, smoking, sedentary lifestyle, chronic kidney disease, depression and stress. This patient had some risk factors that contributed to the development of coronary artery disease: age, male gender, hypertension and smoking.
Patients with chest pain and ACS often have a nonspecific physical examination, with less than 20% of them showing significant alterations in the initial evaluation 2 . This becomes important by helping in the detection of differential diagnoses (e.g., pericardial friction rub in pericarditis) or by inferring the presence of risk factors for coronary artery disease (abdominal or carotid murmur, among others).
However, when findings resulting from an ACS are present, they indicate a worse prognosis due to mechanical complications or due to a large area of myocardium at risk and ventricular dysfunction (hypotension, tachycardia, pulmonary edema and mitral regurgitation murmur secondary to ischemia).
The electrocardiogram is important in the diagnostic, prognostic and therapeutic approach and must be obtained within 10 minutes after the presentation of patients with ongoing chest pain 2 . A normal electrocardiographic tracing does not exclude the possibility of ACS and a serial ECG is indicated, which increases its sensitivity and helps differentiating between acute and chronic alterations.
The patient reported in this clinical case had, at the admission ECG performed at another service, ST-segment elevation in the anterior wall, suggesting the hypothesis of acute coronary syndrome with ST-segment elevation. However, this ECG also showed low voltage and electrical alternans of the QRS complex, which suggests large pericardial effusion or even cardiac tamponade.
The main hypothesis for this pericardial effusion is a mechanical complication of myocardial infarction: left ventricular free wall rupture. It occurs within 24 hours after infarction or between the third and fifth day, has an incidence of 0.8 to 6.2% and is more common in an extensive myocardial infarction, in the elderly, women and hypertensive patients. Its clinical course is variable 3 and may be acute and severe, leading to sudden death or subacute, with nonspecific clinical manifestations.
Other mechanical complications that may be present in myocardial infarction are papillary muscle and interventricular septum rupture. These complications do not present with significant pericardial effusion and normal pulmonary auscultation in this patient also makes the diagnosis of papillary muscle rupture less likely. This clinical condition presents with pulmonary congestion due to volume overload secondary to acute mitral regurgitation.
Another diagnostic hypothesis for this patient presenting with chest pain and pericardial effusion would be aortic dissection. Pain, in these cases, is usually of sudden onset and strong intensity since the beginning (unlike angina pain, which often increasingly escalates). It is often described as excruciating and its location reflects the site and progression of the dissection. Autonomic signs (pallor, profuse sweating) are greatly associated.
In aortic dissection, physical examination may disclose hypertensive crisis, differences between limb pulses, signs of pleural and pericardial effusion, diastolic murmur of aortic regurgitation, different from the systolic murmur detected in this clinical case. The extension of the dissection to other vessels can lead to other symptoms corresponding to ischemia of the organs irrigated by them: cerebrovascular accident, acute myocardial infarction, mesenteric ischemia, etc.
Another diagnostic hypothesis for the clinical case is pulmonary embolism. The absence of pulmonary symptoms, mainly dyspnea, makes this hypothesis less likely. It is the most common symptom of this disease, occurring in over 78% of the patients 4 . Sudden chest pain of sudden onset and very often pleuritic, affects up to 44% of patients 4 . Cough and hemoptysis may also occur. Additionally, there was no mention is made on admission at the other service, of right ventricular dysfunction manifestations, such as jugular stasis and hypotension.
The patient, an hour and 36 minutes after his admission at the Heart Institute, was submitted to coronary angiography with left anterior descending artery angioplasty. However, he developed asystole and cardiac arrest.
The main diagnoses for the final clinical picture are cardiogenic shock and/or distributive shock due to cardiac tamponade, discussed below.
The hypothesis of cardiogenic shock should be considered, as the patient had an extensive acute myocardial infarction without culprit artery reperfusion even after percutaneous revascularization attempt. However, this diagnosis cannot fully explain the patient's clinical condition, such as the absence of pulmonary congestion, which usually follows an acute myocardial failure.
Considering the patient's history, late cardiac tamponade seems to have been the main precipitating factor of the final clinical picture in this case. The electrocardiographic findings commonly observed in cardiac tamponade are low voltage and electrical alternans of the QRS complex, observed in the case. Although physical examination made no reference to clinical findings suggestive of tamponade, such as jugular stasis or muffled heart sounds, we cannot exclude this diagnostic hypothesis.
An echocardiography could have been performed to confirm this diagnosis, which is the most widely used noninvasive method for diagnostic investigation of this pathology. The ventriculography in this context would not be informative, as it was a free wall rupture with cardiac tamponade and thus, it would not allow the visualization of contrast leakage into the pericardial cavity.
This is a patient with myocardial infarction that came at the emergency room more than 24 hours after the onset of the event and who probably had a mechanical complication of myocardial infarction: ventricular free wall rupture.
Most deaths from myocardial infarction occur in the first hours of disease onset, with 40-65% occurring within the first hour and approximately 80% in the first 24 hours 5 , 6 . The recently implemented therapies for MI treatment have been proven to modify patient evolution and prognosis. However, the effectiveness of most of these measures is time-dependent and delay in seeking medical care may have been the factor that likely contributed to the clinical outcome of the patient in this case report. (Dr. Wilma Noia Ribeiro, Dr. Alice Tatsuko Yamada)
Diagnostic hypotheses: Acute myocardial infarction with mixed shock (cardiogenic - distributive) by mechanical complication - free wall rupture with tamponade (Dr. Wilma Noia Ribeiro, Dr. Alice Tatsuko Yamada)
The heart weighed 414 g. The myocardium of the left ventricular anterosseptal wall and right ventricular anterior wall was softened, slightly yellowish in color, characterizing extensive transmural acute myocardial infarction. There was an obvious narrowing of the affected anterosseptal wall, with ventricular septum rupture in the anterior region of its mid portion, with a ventricular septal defect measuring 10 mm in its longest axis. The other left ventricular walls showed to be slightly hypertrophic and there was a small area of fibrosis in the postero-inferior region of the ventricular septum. There was also moderate right ventricular dilation ( Figure 3 ).

Cross-section of the ventricles showing left ventricular transmural infarction of the anterosseptal wall (asterisks) and of the right ventricular anterior wall (arrows). The explorer shows the VSD secondary to septal rupture. Observe the ventricular wall thinning and the small area of fibrosis in the ventricular septum (arrowhead).
Histological analysis confirmed the presence of myocardial infarction, with marked neutrophil infiltration, confirming histological dating of 24-48 hours of onset. Another small ongoing microinfarction was observed in the posterior region of the ventricular septum, in addition to the previously described small area of fibrosis (healed infarction), compatible with approximately 7-10 days of evolution.
There was superficial fibrin deposition in the epicardium, with the presence of reactive inflammatory infiltrate. Examination of the initial segment of the left anterior descending artery showed fatty atherosclerotic plaques with areas of marked thinning of the fibrous cap that covered the lipid core and 80% of obstruction.
There were also areas of plaque rupture and hemorrhage, with acute thrombosis in the first and second centimeters of that artery ( Figs. 4 and and5 5 ).

Histological section of the first centimeter of the left anterior descending artery showing large lipid-core atherosclerotic plaque, with internal area of fibrin deposition and hemorrhage (asterisk). Observe the area with marked thinning of the fibrous cap of the lipid core plaque (arrow), site of potential rupture and thrombosis. Hematoxylin-eosin, 2.5×.

Histological section of the second centimeter of the anterior interventricular artery showing large lipid-core atherosclerotic plaque with ruptured area (arrows) and occlusive luminal thrombosis (asterisk). Hematoxylin-eosin, 2.5×.
The lungs weighed 1,208 g together and showed alveolar edema. The kidneys showed irregular surface and retention cysts, with hyaline arteriolosclerosis on histological examination. The aorta showed mild / moderate degree of atherosclerosis. (Dr. Luiz Alberto Benvenuti)
Anatomopathological diagnoses. Coronary atherosclerosis; acute myocardial infarction involving the left ventricular anterosseptal wall and the right ventricular anterior wall; rupture of the ventricular septum, with VSD; acute pulmonary edema (cause of death) (Dr. Luiz Alberto Benvenuti) .
This is the case report of a 66-year-old man with systemic hypertension and a chronic smoker that presented with acute severe chest pain. After medical assessment, he was diagnosed with acute myocardial infarction and the patient underwent coronary angiography, which disclosed proximal occlusion of the left anterior descending artery with images suggesting the presence of thrombi. He was submitted to balloon-angioplasty in the affected segment without restoration of distal coronary flow (unsuccessful procedure) and the patient developed irreversible cardiac arrest and died.
The autopsy confirmed acute myocardial infarction, which was very extensive, affecting the left ventricular anterosseptal wall and the right ventricular anterior wall. Histological dating was 24-48 hours of onset, consistent with the clinical history. It is noteworthy the fact that the detailed examination of the ventricular septum showed the presence of two previous microinfarctions, an old (healed) one and an ongoing one.
The presence of atherosclerosis of the coronary arteries was identified, with massive plaques in the proximal segment of the left anterior descending artery, which resulted in chronic obstruction of 80% of the lumen. The fatty plaques had extensive lipid cores and there were areas of marked thinning of the fibrous cap that covered the cores, as well as areas of rupture associated with acute thrombosis of the remaining lumen in the first two centimeters of the left anterior descending artery. It is known that acute coronary occlusions with luminal thrombosis are usually associated with large lipid-core plaques, which undergo rupture due to the instability of their thin fibrous cap 7 , as observed in this case.
Aside from the great extent of the infarcted area, the patient developed an important mechanical complication of acute myocardial infarction, the occurrence of ventricular septal rupture with the establishment of VSD 8 - which certainly aggravated his hemodynamic condition, progressing to cardiogenic shock -, acute pulmonary edema and death. It should be emphasized that the patient had two classic risk factors for atherosclerosis and myocardial infarction: systemic hypertension and chronic smoking 9 . (Dr. Luiz Alberto Benvenuti)
Section Editor: Alfredo José Mansur ( rb.psu.rocni@rusnamja )
Associated Editors: Desidério Favarato ( rb.psu.rocni@otaravaflcd )
Vera Demarchi Aiello ( rb.psu.rocni@arevpna )

COMMENTS
A telemedicine visit was arranged as part of a local public health strategy to reduce the spread of coronavirus disease 2019 (Covid-19), the disease caused by severe acute respiratory syndrome ...
A 67-year-old woman sought emergency medical care due to prolonged chest pain. In April 2009 the patient had prolonged chest pain and at that time she sought medical care. She was admitted at the hospital and diagnosed with myocardial infarction. The patient had hypertension, diabetes mellitus, dyslipidemia and was a smoker.
The recommendation of optimized drug treatment as the initial option for patients with chronic coronary artery disease is supported by a meta-analysis with 63 studies (1852 symptomatic and asymptomatic patients diagnosed with chronic coronary artery disease, mean age ranging from 56 to 65 years), comparing four possibilities of procedures ...
We report a case of coronary artery disease, which rapidly progressed and led to severe ischemic cardiomyopathy. Based on the risk factors, typical symptoms of angina, and the results of the first angiography, the initial stenosis was most probably caused by atherosclerosis and was managed with a DES followed by dual antiplatelet therapy.
Both serial 12-lead ECG and highly sensitive cardiac troponin T testing should be performed before excluding ongoing ischemic coronary artery disease. Prior to stress testing, the patient should be chest pain free for 24 hours, without dynamic 12-lead ECG changes, and the highly sensitive cardiac troponin T level should be negative or trending ...
Part 4. He was taken to the catheterization lab where the left anterior descending coronary artery (LAD) was shown to be completely occluded. Following successful percutaneous intervention and one drug eluding stent implantation in the LAD normal flow is restored (Thrombosis in myocardial infarction, TIMI = 3). 72 hours later, he is ready to be discharged home.
Case Study 1: Radial Artery Approach for Cardiac Catheterization followed by an "Off-Pump" Coronary Artery Bypass Surgery ... He had a positive nuclear stress test that showed reduced blood flow to the left ventricle with a high suspicion for coronary artery disease. Dr. John Resar, the director of the cardiac catheterization lab at Johns ...
Design of the Coronary Artery Disease Genome-Wide Replication and Meta-Analysis (CARDioGRAM) Study, Clinical Perspective: a genome-wide association meta-analysis involving more than 22,000 cases and 60,000 controls. ... Association of HDL cholesterol efflux capacity with incident coronary heart disease events: a prospective case-control study ...
Although 195 coronary artery lesions were analyzed in this trial by quantitative coronary angiography, this study was limited in terms of the few patients evaluated (intervention group: n=22; control group: n=19); one patient died during the study period, and several angiograms were lost. 95 However, the Stanford Coronary Risk Intervention ...
Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet. 1994; 344:563-570. doi: 10.1016/s0140-6736(94)91963-1 Crossref Medline Google Scholar; 24.
Subsequent to Heberden's report, coronary artery disease (CAD) was implicated in pathology and clinical case studies undertaken by John Hunter, John Fothergill, Edward Jenner and Caleb Hiller Parry.3 Typically, angina involves a relative deficiency of myocardial oxygen supply (ie, ischaemia) and typically occurs after activity or ...
An observational, retrospective case series study was conducted. Patients who had low and moderate cardiac surgical risk (less than 8% mortality risk on the STS score) and had the concomitant indication for CABG and AAOR between December 2005 and August 2021 were included.
<Learning objective: This case report reveals an exceptionally young Caucasian man presenting with stable angina and found to have multivessel coronary disease. The patient received a coronary artery bypass surgery at just 21 years of age. He exhibits traditional risk factors of CHD; hypertension, dyslipidemia, cigarette smoking, and obesity.
Given his symptoms, coronary disease risk factors and ECG changes, he undergoes a one-day exercise Tc-99m myocardial perfusion study. He exercises a total of seven minutes, 49 seconds on a standard Bruce protocol and achieves 9.8 METS. Peak heart rate is 135 bpm (86% of his maximum predicted heart rate).
This chapter illustrates various general issues in genetic epidemiology in relation to coronary artery disease (CAD). This is a disease strongly influenced by environmental/lifestyle factors, such as smoking, but with substantial estimated heritability. ... Coronary artery disease: an example case study Methods Mol Biol. 2011:713:215-25. doi ...
Congenital agenesis of the right coronary artery (RCA) is a coronary anomaly characterized by a single coronary ostium from which the whole coronary tree takes origin. Coronary anomalies are often incidental findings in patients undergoing coronary angiography for coronary artery disease (CAD) exclusion. Cardiovascular computed tomography ...
Cardiovascular manifestations also include valvular heart disease, ventricular thrombi and higher risk for coronary artery disease (CAD). In this case report, we describe a 61-year-old woman who had no significant risk factors for CAD, and presented with aggressive disease in native and graft vessels that required multiple coronary interventions.
A. A. A. A 52-year-old executive was referred to our clinic for risk factor management after undergoing coronary computed tomography angiography (CTA) as part of an Executive Physical. He has no history of coronary artery disease and exercises regularly without experiencing anginal symptoms. His family history is notable for a myocardial ...
A coronary artery aneurysm is an uncommon vascular disorder, and it can be a life-threatening disease when associated with rupture or an embolism. A 52-year-old man was found to have a 50-mm coronary artery aneurysm at the right coronary artery, and the aneurysm was completely occluded by a thrombus.
The study was a case series from a single-center of patients with AKI who required coronary angiography over a 12-month period during 2022-2023. ... Prior coronary artery disease: 25 (2) Prior coronary artery bypass graft: 12.5 (1) Prior cerebrovascular accident: 25 (2) Congestive heart failure:
Coronary artery disease (CAD) is one of the main causes of death in the world. Functional indices such as fractional flow reserve (FFR), coronary flow reserve (CFR) and instantaneous wave-free ratio (iFR) are used to estimate the severity of CAD. Approximately 30-50% of patients have residual myocardial ischaemia even after formally successful percutaneous coronary intervention (PCI ...
However, due to the lack of adequate information on this topic, this study aimed to investigate the relationship between AIP and coronary heart disease risk. Results: This study included 2,226 women and 1,690 men aged 35-70 years who participated in the Bandar Kong Cohort study and met the eligibility criteria. The data was collected using a ...
Here, we present a unique case of a 72-year-old man with GSD-V and both mitral valvulopathy and coronary artery disease, prompting a systematic review to explore the existing literature on cardiac comorbidities in McArdle disease. Results: Our systematic literature revision identified 7 case reports and 1 retrospective cohort study.
Kawasaki disease (KD) is a multisystem inflammatory illness of infants and young children that can result in acute vasculitis. The mechanism of coronary artery aneurysms (CAA) in KD despite ...
A cross-sectional study was conducted on 42 women with confirmed atherosclerotic coronary disease, divided into diabetic and non-diabetic groups, who were scheduled for angioplasty or coronary ...
This patient had some risk factors that contributed to the development of coronary artery disease: age, male gender, hypertension and smoking. Patients with chest pain and ACS often have a nonspecific physical examination, with less than 20% of them showing significant alterations in the initial evaluation 2. This becomes important by helping ...
The remarkable risk discrimination capability of PGS000747 stands out as the most noteworthy outcome of the study. Coronary artery disease (CAD) stands as the most predominant type of cardiovascular disease (CVD). Polygenic risk scores (PRSs) have become essential tools for quantifying genetic susceptibility, and researchers endeavor to improve their predictive precision. The aim of the ...