- Research article
- Open access
- Published: 21 July 2017

Treatment outcomes in schizophrenia: qualitative study of the views of family carers
- Joanne Lloyd 1 ,
- Helen Lloyd 2 ,
- Ray Fitzpatrick 3 &
- Michele Peters 3
BMC Psychiatry volume 17 , Article number: 266 ( 2017 ) Cite this article
28k Accesses
13 Citations
12 Altmetric
Metrics details
Schizophrenia is a complex, heterogeneous disorder, with highly variable treatment outcomes, and relatively little is known about what is important to patients. The aim of the study was to understand treatment outcomes informal carers perceive to be important to people with schizophrenia.
Qualitative interview study with 34 individuals and 8 couples who care for a person with schizophrenia/schizoaffective disorder. Interviews were transcribed verbatim and analysed by a thematic framework based approach.
Carers described well-recognised outcomes of importance, alongside more novel outcomes relating to: Safety (of the patient/others); insight (e.g. into non-reality of psychotic phenomena); respite from fear, distress or pain; socially acceptable behaviour; getting out of the house; attainment of life milestones; changes in personality and/or temperament; reduction of vulnerability to stress; and several aspects of physical health.
Conclusions
These findings have the potential to inform the development of patient- or carer- focused outcome measures that take into account the full range of domains that carers feel are important for patients.
Peer Review reports
Improving treatment outcomes and quality of life for people with long-term mental health conditions are key aims of health care policy [ 1 , 2 ]. Schizophrenia is a particularly important target, being associated with poor quality of life [ 3 ] and individual and societal impacts [ 4 , 5 , 6 ], and requiring long-term treatment [ 7 ]. Antipsychotic medications can ameliorate some symptoms and improve quality of life [ 3 , 8 , 9 ], but individual responses vary [ 10 , 11 ], and many discontinue medication due to poor efficacy or debilitating side effects [ 12 , 13 ]. Treatment outcomes are often assessed by clinician ratings, and/or symptom scales [ 14 ], but patients and carers may prioritise different outcomes to clinicians [ 15 , 16 , 17 ], and controlling symptoms is not the only outcome of importance [ 14 ]. The recovery literature draws attention to the importance of recognising a broad array of outcome domains in schizophrenia treatment, highlighting the relevance of improved social and domestic functioning, alongside subjective wellbeing, optimism and empowerment (e.g. [ 18 , 19 ]). Patients and relatives, in particular, refer to subjective wellbeing when defining ‘remission’, in contrast to traditional clinical definitions focused around reduced symptom scores [ 17 ]. People with schizophrenia value outcomes such as achieving life milestones, feeling safe, improved physical activity, employment, a positive sense of self and psychosocial outcomes [ 20 ]. Understanding the full range of treatment outcomes important to people with schizophrenia and their carers is key for ensuring that clinical practice, research and assessment are aligned with patient and carer priorities [ 4 , 21 ].
While people with schizophrenia can give valid and reliable accounts of outcomes [ 22 , 23 , 24 ], symptoms can make it difficult to participate in research [ 25 ], and carers represent a valuable additional resource [ 15 , 21 , 26 ]. Furthermore, carers have the potential to influence treatment decisions [ 26 ], and experience, indirectly, the impact of outcomes. This study sought to explore the treatment outcomes that carers feel are important for people with schizophrenia. It used a framework informed by a thematic review of the existing literature on treatment outcomes of importance to patients and carers, and a consensus conference with professionals, carers and patients, and aimed to identify whether carers report any outcome domains that have not been emphasised in the current literature.
Design of the study
A qualitative study using in-depth semi-structured interviews was conducted with self-identified ‘carers’ of a family member with a diagnosis of schizophrenia made at least 2 years previously. Ethical approval was obtained from NHS East of Scotland Research Ethics Service (EoSRES) REC 1 by proportionate review (Application Number 13/ES/0143). All participants gave written informed consent.
Participants and recruitment
A total of 34 individuals and 8 couples were interviewed (i.e. 50 people in 42 interviews). While qualitative methodology papers tend to avoid prescribing hard guidelines for sample sizes for qualitative studies, 25–30 participants have been deemed an acceptable minimum by Dworkin [ 27 ] and this number is usually sufficient for reaching data saturation. An email circulated by charity ‘Rethink Mental Illness’ was responded to by 102 people who were screened via telephone to confirm that they were the carer of someone with a ≥ 2-year diagnosis of schizophrenia or schizoaffective disorder. Within this self-selecting convenience sample, participants were then recruited purposively to generate a relatively heterogeneous final sample, consisting of 38 females and 12 males, aged from 20s–80s (48% in their 60s, 26% in their 50s, and the remainder in their 20s, 40s, 70s or 80s), and coming from urban (e.g. Greater London) and rural (e.g. Wiltshire) locations. Thirty-seven were the mother of a person with schizophrenia, 10 were the father or stepfather, one the husband, one the wife, and one the sibling. Duration of illness of the patients discussed ranged from 2 to 20+ years, with a modal duration of 11–15 years (42%). The majority ( n = 44) cared for someone with schizophrenia, and six cared for someone with schizoaffective disorder.
Most participants chose to be interviewed at home, but approximately 20% chose to come to the University. At the beginning of the interviews, carers re-confirmed that the patient had received a formal diagnosis of schizophrenia or schizoaffective disorder from a GP or psychiatrist, at least two years prior to the interview. Carers were then asked what they felt were important outcomes of treatment for the patient who they cared for: at present; at a time when the patient was particularly ill or unwell; at a time when they were more stable; and at a time when they were doing particularly well. Prompts were designed to encourage participants to discuss both directly-experienced outcomes, and important/desired but unattained outcomes. In addition, a series of prompts relating to key outcomes were compiled based on the conceptual review of the literature and feedback from a consensus conference, but were not in fact utilised in any of the interviews, as participants spontaneously discussed a broad array of outcomes of importance in response to the preliminary, general questions. After the initial 6 interviews, when it became apparent that participants identified multiple outcomes in response to the primary questions, without need for prompts, the researchers agreed that all future interviews in the study would proceed without prompts. Carers were encouraged to expand upon ideas that they themselves raised in relation to outcomes, rather than directed towards any specific topic. It was felt that this strengthened the data, as it reduced the potential for investigator bias. The topic guide, which was reviewed for tone and content prior to use by two carers and one person with schizophrenia, can be found in online Additional file 1 . Interview duration ranged from 40 to 125 min (average, approx. 60 min).
Interviews were transcribed verbatim by a professional transcriber, and anonymised. Transcripts were analysed in NVivo 8 by JL, using a thematic, framework based approach [ 28 ]. This involved the creation of a preliminary framework based on a literature review and consensus conference. Transcripts were then analysed, with themes being coded into appropriate categories within that framework, wherever appropriate categories existed. Where themes did not fit well into an existing category, novel categories were created. Interviews were continued until no further novel categories emerged, by which point all categories had been spontaneously mentioned by several participants, and saturation was deemed to have been reached. Once all interviews had been coded, the categories were reviewed by the research team, to ensure that they were representative of all the statements coded within them. Where categories were ambiguous, e.g. contained material that could potentially be better conceptualised within different domains, or could be better represented by different titles, they were revised, and the material coded within them was re-coded in order to ensure that it was coded within the most appropriate category. A final framework that encompassed the original and the novel categories was then agreed amongst the researchers. All of the interviews were then re-coded, using the final framework. In this second iteration, the majority of the material was coded into the same categories as during the initial coding. However, this process was important to ensure that any statements that had originally been coded into categories within the preliminary framework, but in retrospect better-reflected a novel category that had been added to the final framework, were coded appropriately. RF and MP independently cross-checked the final categorisation by coding a random selection of 6 transcripts, and no disagreements emerged. Categorized data were summarized and synthesized, and the resultant categories (and associations between them) were interpreted in relation to the categories already identified within the literature and consensus conference. After the final coding, the number of interviews in which each category occurred was calculated.
Outcomes of importance in schizophrenia reported by the carers included symptom related outcomes, quality of life, functional outcomes, personal recovery, physical health and lifestyle, and satisfaction with treatment. Table 1 lists these outcomes, and their sub-categories, and the proportion of interviews in which they occurred (using the conventions: ‘few’ for 2–10% ( n = 1–4), ‘some’ for 12–24% ( n = 5–10), ‘many’ for 25–50% ( n = 11–21), and ‘most’ for >50% ( n = 22–42)). It was not necessary for a participant to overtly state that an outcome had been experienced by the person they care for, in order to code their statement as an endorsement of that domain. While ‘endorsement’ of an outcome domain did, in some cases, take this form, any statement that either explicitly or implicitly indicated that a domain was relevant or important to that carer, was also coded within that domain. For example, where a carer identified that the person they cared for experienced ongoing difficulties with engaging in physical activity, or that they wished the person they cared for could have the energy to engage in physical activity, this was interpreted as the carer indicating that being able to engage in physical activity was an important outcome, and hence it was coded within the ‘physical activity’ category.
The categories in Table 1 were first identified through a literature review and consensus conference and subsequently adapted to include the newly identified and/or expanded categories from the interview data reported here. Standard font indicates categories which were pre-identified from the literature review (and replicated in the current study), and italic font indicates novel/ modified categories which emerged from the current study (which are illustrated by quotations in Tables 3 and 4 , and discussed below). All categories in Table 1 were identified as relevant by at least some of the carers interviewed, and the majority were mentioned in >50% of the interviews.
Symptom-related outcomes (Table 2 )
Safety was mentioned in most interviews, and encompassed safety from dangerous behaviours prompted by psychosis (such as absconding/ putting oneself or others into risky situations); from health risks linked to negative symptoms (e.g. not eating, living in squalor); and from potential for deliberate self-harm related to affective symptoms.
‘It's great for it to be diagnosed, to be put on your medication and you're safe’ [C41]
The importance of reduction of, or relief from fear, distress and emotional (or even physical) pain was raised in most interviews, often closely related to positive symptoms, but at the level of their physical and emotional consequences.
‘He was absolutely intimidated by his environment… he felt frightened and threatened’ [C25]
Insight was also mentioned in most interviews, encompassing both recognition that current/prior psychotic phenomena are not real, and understanding that one has a long-term illness. It was described as a gatekeeper to many other treatment benefits, partly through its impact upon treatment adherence, and was important in helping people deal with residual psychotic phenomena.
‘He can rationalise…although he hears the voices he has a sense of reality.’ [C40]
Side-effects are not described in detail here as they are well reported within existing literature (e.g. [ 29 ]), but they were identified as important in the majority of interviews, and in addition to commonly-reported side effects (e.g. weight gain and fatigue), a few participants mentioned negative impact of medication on imagination and/or creativity, and concerns over toxicity of medication during pregnancy and breastfeeding.
Quality of life (Table 2 )
The concept of ‘social acceptability’ was raised in most interviews, i.e. behaving in a socially appropriate way and avoiding bizarre/unconventional behaviour. Many discussed the importance of treatment in helping patients avoid illegal behaviour (sometimes precipitated by symptoms).
‘[When] he's not taking his medication, he occasionally offends people in the street’ [C25]
Functional outcomes (Table 3 )
The domain of ‘life milestones’ was added to encompass many carers’ reports of the importance of reaching key life/developmental milestones, such as attaining qualifications, learning to drive, moving out of the caregiver’s home, or having a family.
‘I think he missed out all his twenties and thirties so maybe catching up in some ways.’ [C03]
Simply ‘getting out’ of the house was mentioned in most interviews, and was consequently added as a sub-category of ‘leisure pursuits’. This encompassed the importance of being well enough to leave the house, which was something many patients needed to achieve before the more ambitious step of engaging in structured leisure activities or even activities of daily living.
‘The worst time that we've had was… when he was so unwell he didn’t go out the house for a year’ [C24]
A novel sub-category of ‘pets’ was added within the ‘role functioning and productivity’ category, because the importance of being able to care for a pet was raised in some interviews.
Personal recovery (Table 3 )
The importance of ‘personality/temperament’ was raised in most interviews, and was often particularly valued by carers themselves. This encompassed emergence of aspects of the patient’s character, such as sense of humour, consideration, and thoughtfulness, and of a generally calmer temperament, more ‘like oneself’.
‘He reverted to his old self. You could reason with him, you could have a laugh with him’ [C46]
The vast majority of carers also mentioned ‘vulnerability/sensitivity’ to all kinds of stress, in most cases as a residual difficulty that treatment failed to resolve, rather than a positive, attained outcome.
‘Although he seems fairly even I don’t think it would take a huge amount to kick him over the edge.’ [C06]
Physical health and lifestyle (Table 4 )
Exercise/physical activity and diet/weight were raised by the majority of carers, who sometimes described how treatment facilitated physical activity and healthy diet (by improving symptoms that create barriers), but also described how side-effects (such as alteration in appetite/metabolism, and fatigue) could act as barriers.
‘On such a high dose… of a sedating medication. Motivation is just not there’. [C46]
Many described the importance of outcomes related to drugs/alcohol/smoking, such as decreased reliance upon substances previously used to self-medicate positive or affective symptoms, or compensate for lack of social/functional activities.
‘She was drinking herself to sleep, I think, mostly because she had recurrent nightmares, and day time nightmares’ [C50]
Daily routine was mentioned in many interviews, in relation to sleep and waking, eating and self-care, and was described both as a factor that contributed to improving other outcomes, and as an outcome in itself.
Principle findings
All the schizophrenia treatment outcomes identified in the literature review and consensus conference preceding the study (i.e. symptom-related outcomes; functional outcomes; personal recovery; quality of life; and satisfaction with treatment) were confirmed in these qualitative interviews, along with several novel sub-categories within existing domains and a novel category of physical health and lifestyle, thus giving a deeper understanding of outcomes in this condition. While a large proportion of the sample endorsed most of the themes, it should be noted that frequency information are indicative of the frequency of these domains within our sample, and cannot be extrapolated from to estimate the prevalence of these concerns in carers of persons with schizophrenia.
While the importance of physical activity for persons with schizophrenia is recognised within the literature [ 30 ], and low levels of physical activity have been demonstrated empirically to be associated with poorer outcomes in schizophrenia [ 31 ], its importance as a treatment outcome is not expressed in existing outcome measures. This highlights the need to consider physical activity as a potentially relevant outcome domain in its own right. Designing interventions for schizophrenia that include attention to physical health and lifestyle, could help improve outcomes for many patients.
Safety of the patient (and those around them), and reduction of their fear, distress or pain, were considered important by most carers, and it is easy to see why they would value these outcomes, relating to resolution of negative practical and emotional consequences of symptoms. While the importance of these outcomes may be intuitive, they are not explicitly represented in current outcome measures, and this study is novel in highlighting their particular salience. These outcomes could be described as ‘secondary’, in the sense that they could be logically expected to follow on from the more ‘primary’ outcome of amelioration of (particularly, positive) symptoms. However, it could also be argued that there are other means of reducing patients’ fear, distress, or pain, aside from by symptom resolution, and thus outcome measures could benefit from assessing the extent to which treatments help to reduce a patient’s experience of these negative states. This could help professionals to gain a fuller understanding of how a given treatment programme is impacting on the individual’s level of fear and distress.
Most carers also valued insight which they often reported to be associated with improved communication with the person with schizophrenia, and a return of their personality and/or of a more favourable, ‘normal’ temperament. This is consistent with findings that insight in schizophrenia is associated with social cognition [ 32 ], and lower scores on an aggression scale [ 33 ]. Carers also described insight’s importance for enabling patients to apply cognitive strategies to counter paranoid thoughts, delusions or hallucinations, consistent with the finding that insight can be predictive of prognosis [ 34 ]. Monitoring level of insight may be beneficial in order to inform decisions about when cognitive interventions may be more effective. Exploring the value of educating carers in ways to cope with poor insight in the person for whom they care, could be another important target for future work.
Within functional outcomes, many carers talked of ‘getting out’ (i.e. leaving the house), similar to the existing domain of engaging in leisure pursuits, but at a more preliminary level. Caring for pets, similarly, could be conceptualised as a specific form of role functioning/productivity. Where residual difficulties are considerable and/or recovery is particularly limited, less ‘ambitious’ functional outcomes such as these may be particularly relevant. This is consistent with the observation that traditional social functioning measures may not be relevant to people with severe disabilities related to schizophrenia [ 35 ], and with carers’ comments about reduced potential and lowering of expectations. From carers’ references to a range of key developmental/life events such as moving out of the family home, getting a job, learning to drive, and having a romantic relationship, we identified ‘reaching life milestones’ as an important and novel outcome. Because schizophrenia onset is typically during adolescence or early adulthood [ 36 ], before traditional milestones have been reached, it is logical that the reaching of milestones would for many be the goal, rather than the resumption of familial, domestic, occupational or educational roles and responsibilities. This highlights the fact that functional outcome measures in schizophrenia may need to take subtle levels of attainment into account, in order to accurately capture small gains.
Within the realm of ‘personal recovery’ many carers highlighted the importance of changes in personality and temperament, and several described the return of the person they used to know as the most important outcome; understandably so, considering that these are good outward indicators of wellness and ‘personal recovery’ and directly impact upon the patient-carer relationship. Indeed, temperament has been linked with functional outcomes and psychological health [ 37 ]. Also relating to personal recovery, many carers discussed patients’ vulnerability (to stress, and in general) and sensitivity, consistent with empirical findings of increased biological reactivity to stress in schizophrenia [ 38 ]. These were typically described as residual unresolved difficulties, and several carers reported that they limited patients’ attainment of functional outcomes and acted as precipitants of relapse, requiring careful monitoring. This could indicate a potential benefit to be found in involving carers, where appropriate, in helping patients to monitor level of stress, and react quickly to try and reduce its impact.
In the sub-category of ‘leading a normal life’, a number of carers spoke of the importance of treatment for helping patients to avoid socially unacceptable/antisocial/illegal behaviours, (often precipitated by positive symptoms), in order to reduce risk of arrest or sectioning, facilitate social interactions and minimise stigma – consistent with findings that socially unacceptable behaviour is strongly associated with stigma in schizophrenia [ 39 ].
Consistent with other studies, many carers expressed desire for greater monitoring of physical health [ 40 ]. Exercise/physical activity, diet, and weight were all salient concerns; again consistent with findings of elevated obesity [ 41 ] and low activity [ 42 ] in schizophrenia/severe mental illness. A wide range of contributing factors were cited by the carers, including medication side effects, positive, negative and affective symptoms, and eating replacing less attainable leisure pursuits. Several also described patients who used alcohol or drugs to self-medicate and/or compensate for a lack of alternative leisure outlets; consistent with reported motivations for substance use in schizophrenia [ 43 ]. Some carers did describe physical health benefits of treatment, e.g. where it reduced use of drugs or alcohol for self-medication, or reduced symptoms enough to allow patients to exercise or shop for healthy food. In relation to lifestyle more generally, several carers emphasised the importance of routine, as a desirable outcome and useful intervention for facilitating the attainment of other outcomes (consistent with a study where people with schizophrenia rated organization of time as a useful coping strategy [ 44 ]). The discovery that physical health is an important concern in schizophrenia is not novel, but this study does support the growing body of work emphasising the importance of incorporating physical health interventions into schizophrenia treatment programmes (e.g. [ 45 ]).
Strengths and limitations
This study confirms the key treatment outcome categories found in the current literature, and contributes evidence of additional outcomes that carers feel are important for patients but are not apparently captured in current thinking about, and measurement of, schizophrenia outcomes. However, there are some possible biases in the sample. The majority of carers interviewed were parents of a person with schizophrenia, with a gender bias in the sample, such that around three quarters of participants were female. However, this is in line with the gender balance found in other convenience samples of carers of persons with schizophrenia [ 46 ], and reflects the fact that mothers are most frequently the primary carer in schizophrenia [ 47 ]. It is possible that spouses, siblings, or children (or those of a younger age in general) may have different perceptions of what the important outcomes are. Most participants were recruited via Rethink Mental Illness, which may have meant they were particularly well-informed about features of schizophrenia and issues around treatment. Finally, the patients discussed were typically quite advanced in chronicity (in most cases >10 years post-diagnosis). While carers were asked to discuss outcomes that they felt were important at different phases of illness, it is nevertheless possible that carers of patients more immediately post-diagnosis would report different outcomes. Future studies could benefit from exploring outcomes with younger carers with different relationships to the patient, from a range of backgrounds, and those caring for people more early post-diagnosis.
The outcomes carers identified as being important for patients may not be identical to the outcomes that patients themselves would identify. However, there is generally good agreement between the two [ 21 ], and as agents who potentially influence patients’ treatment decisions [ 16 ], and experience the consequences of the illness [ 48 ], carers’ views are important in their own right. Furthermore, we were able to gain insight into outcomes that might not otherwise have been represented, as most of the carers interviewed reported that the patients they were speaking about would have been unwilling/unable to participate (e.g. ‘he hates talking about it when he was really ill… he said, “It makes me feel so ill again” [C41]).
The findings from this study contribute to our understanding of the full range of treatment outcomes that carers feel are important to people with schizophrenia, and could contribute to ensuring research, treatment planning and assessment are aligned with the needs and priorities of patients [ 4 ]. The breadth of information gleaned from these interviews with family carers indicates what an important resource this population represents. Furthermore, it is clear that informal carers typically bear a high burden of care in schizophrenia [ 49 ]. Working with carers to gain insights and coordinate interventions, where appropriate, could be a valuable way for professionals to develop person-centred approaches in schizophrenia. Outcomes of treatment should ideally be assessed with measures that both complement existing clinical scales and incorporate patient and carer priorities. The domains and more specific experience emphasised here should inform the further development of such patient- or carer- focused outcome measures in order to ensure more appropriate and complete evaluation of interventions.
Centre for Mental Health, Department of Health, Mind, NHS Confederation Mental Health Network, R.M. Illness. Turning point: No health without mental health. Implementation framework 2012. London: Department of Health; 2012.
Department of Health. NHS Outcomes Framework 2012/13. London: Department of Health; 2012.
Google Scholar
Bobes J, Garcia-Portilla MP, Bascaran MT, Saiz PA, Bousono M. Quality of life in schizophrenic patients. Dialogues Clin Neurosci. 2007;9(2):215–26.
PubMed PubMed Central Google Scholar
Schizophrenia Commission. The abandoned illness: a report from the Schizophrenia Commission. London: Rethink Mental Illness; 2012.
Eack SM, Newhill CE. Psychiatric symptoms and quality of life in schizophrenia: a meta-analysis. Schizophr Bull. 2007;33(5):1225–37.
Article PubMed PubMed Central Google Scholar
Jin H, Mosweu I. The Societal Cost of Schizophrenia: A Systematic Review. Pharmacoeconomics. 2016.
Ascher-Svanum H, Faries DE, Zhu B, Ernst FR, Swartz MS, Swanson JW. Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J Clin Psychiatry. 2006;67(3):453–60.
Article PubMed Google Scholar
Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, Davis JM. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379(9831):2063–71.
Article CAS PubMed Google Scholar
Wehmeier PM, Kluge M, Schneider E, Schacht A, Wagner T, Schreiber W. Quality of life and subjective well-being during treatment with antipsychotics in out-patients with schizophrenia. Prog Neuro-Psychopharmacol Biol Psychiatry. 2007;31(3):703–12.
Article CAS Google Scholar
Wehmeier PM, Kluge M, Schacht A, Helsberg K, Schreiber WG, Schimmelmann BG, Lambert M. Patterns of physician and patient rated quality of life during antipsychotic treatment in outpatients with schizophrenia. J Psychiatr Res. 2008;42(8):676–83.
Levine SZ, Rabinowitz J, Faries D, Lawson AH, Ascher-Svanum H. Treatment response trajectories and antipsychotic medications: examination of up to 18 smonths of treatment in the CATIE chronic schizophrenia trial. Schizophr Res. 2012;137(1–3):141–6.
Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RS, Davis SM, Davis CE, Lebowitz B, Hsiao J, Severe J. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia: primary efficacy and safety outcomes of the clinical antipsychotic trials of intervention effectiveness (CATIE) schizophrenia trial. Neuropsychopharmacology. 2005;30:S32.
Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, Samara M, Barbui C, Engel RR, Geddes JR, Kissling W, Stapf MP, Lassig B, Salanti G, Davis JM. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;392:951–62.
Article Google Scholar
Mortimer AM. Symptom rating scales and outcome in schizophrenia. Br J Psychiatry. 2007;191(50):s7–s14.
Shepherd G, Murray A, Muijen M. Perspectives on schizophrenia: a survey of user, family carer and professional views regarding effective care. J Ment Health. 1995;4(4):403–22.
Bridges JFP, Slawik L, Schmeding A, Reimer J, Naber D, Kuhnigk O. A test of concordance between patient and psychiatrist valuations of multiple treatment goals for schizophrenia. Health Expect. 2013;16(2):164–76.
Karow A, Naber D, Lambert M, Moritz S, Initiative E. Remission as perceived by people with schizophrenia, family members and psychiatrists. Eur Psychiatry. 2012;27(6):426–31.
Warner R. Recovery from schizophrenia and the recovery model. Curr Opin Psychiatry. 2009;22(4):374–80.
Karow A, Moritz S, Lambert M, Schottle D, Naber D, Initiative E. Remitted but still impaired? Symptomatic versus functional remission in patients with schizophrenia. Eur Psychiatry. 2012;27(6):401–5.
Lloyd H, Lloyd J, Fitzpatrick R, Peters M. The role of life context and self-defined well-being in the outcomes that matter to people with a diagnosis of schizophrenia. Health Expect. 2017; 1–12. doi: 10.1111/hex.12548 .
Balaji M, Chatterjee S, Brennan B, Rangaswamy T, Thornicroft G, Patel V. Outcomes that matter: a qualitative study with persons with schizophrenia and their primary caregivers in India. Asian J Psychiatr. 2012;5(3):258–65.
Voruganti L, Heslegrave R, Awad AG, Seeman MV. Quality of life measurement in schizophrenia: reconciling the quest for subjectivity with the question of reliability. Psychol Med. 1998;28(1):165–72.
Reininghaus U, Priebe S. Measuring patient-reported outcomes in psychosis: conceptual and methodological review. Br J Psychiatry. 2012;201(4):262–7.
Baumstarck K, Boyer L, Boucekine M, Aghababian V, Parola N, Lancon C, Auquier P. Self-reported quality of life measure is reliable and valid in adult patients suffering from schizophrenia with executive impairment. Schizophr Res. 2013;147:58–67.
Kaminsky A, Roberts LW, Brody JL. Influences upon willingness to participate in schizophrenia research: an analysis of narrative data from 63 people with schizophrenia. Ethics Behav. 2003;13(3):279–302.
Rettenbacher MA, Burns T, Kemmler G, Fleischhacker WW. Schizophrenia: attitudes of patients and professional Carers towards the illness and antipsychotic medication. Pharmacopsychiatry. 2004;37(03):103–9.
Dworkin SL. Sample size policy for qualitative studies using in-depth interviews. Arch Sex Behav. 2012;41(6):1319–20.
Ritchie J, Spencer L. In: Bryman A, Burgess B, editors. Qualitative data analysis for applied policy research, in Analyzing qualitative data. London: Routledge; 1993. p. 173–94.
Fischer EP, Shumway M, Owen RR. Priorities of consumers, providers, and family members in the treatment of schizophrenia. Psychiatr Serv. 2002;53(6):724–9.
Soundy A, Freeman P, Stubbs B, Probst M, Coffee P, Vancampfort D. The transcending benefits of physical activity for individuals with schizophrenia: a systematic review and meta-ethnography. Psychiatry Res. 2014;220(1–2):11–9.
Vancampfort D, Knapen J, Probst M, Scheewe T, Remans S, De Hert M. A systematic review of correlates of physical activity in patients with schizophrenia. Acta Psychiatr Scand. 2012;125(5):352–62.
Quee PJ, van der Meer L, Bruggeman R, de Haan L, Krabbendam L, Cahn W, Mulder NC, Wiersma D, Aleman A. Insight in psychosis: relationship with neurocognition, social cognition and clinical symptoms depends on phase of illness. Schizophr Bull. 2011;37(1):29–37.
Ekinci O, Ekinci A. Association between insight, cognitive insight, positive symptoms and violence in patients with schizophrenia. Nord J Psychiatry. 2013;67(2):116–23.
Saravanan B, Jacob KS, Johnson S, Prince M, Bhugra D, David AS. Outcome of first-episode schizophrenia in India: longitudinal study of effect of insight and psychopathology. Br J Psychiatry. 2010;196(6):454–9.
Burns T, Patrick D. Social functioning as an outcome measure in schizophrenia studies. Acta Psychiatr Scand. 2007;116(6):403–18.
de Girolamo G, Dagani J, Purcell R, Cocchi A, McGorry PD. Age of onset of mental disorders and use of mental health services: needs, opportunities and obstacles. Epidemiol Psychiatr Sci. 2012;21(1):47–57.
Eklund M, Hansson L, Bengtsson-Tops A. The influence of temperament and character on functioning and aspects of psychological health among people with schizophrenia. Eur Psychiatry. 2004;19(1):34–41.
Mizrahi R, Addington J, Rusjan PM, Suridjan I, Ng A, Boileau I, Pruessner JC, Remington G, Houle S, Wilson AA. Increased stress-induced dopamine release in psychosis. Biol Psychiatry. 2012;71(6):561–7.
Loganathan S, Murthy SR. Experiences of stigma and discrimination endured by people suffering from schizophrenia. Indian J Psychiatry. 2008;50(1):39–46.
Marder SR, Essock SM, Miller AL, Buchanan RW, Casey DE, Davis JM, Kane JM, Lieberman JA, Schooler NR, Covell N, Stroup S, Weissman EM, Wirshing DA, Hall CS, Pogach L, Pi-Sunyer X, Bigger JT Jr, Friedman A, Kleinberg D, Yevich SJ, Davis B, Shon S. Physical health monitoring of patients with schizophrenia. Am J Psychiatry. 2004;161(8):1334–49.
Scott D, Happell B. The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues Ment Health Nurs. 2011;32(9):589–97.
McNamee L, Mead G, MacGillivray S, Lawrie SM. Schizophrenia, poor physical health and physical activity: evidence-based interventions are required to reduce major health inequalities. Br J Psychiatry. 2013;203(3):239–41.
Gregg L, Barrowclough C, Haddock G. Development and validation of a scale for assessing reasons for substance use in schizophrenia: the ReSUS scale. Addict Behav. 2009;34(10):830–7.
Lee PW, Lieh-Mak F, Yu KK, Spinks JA. Coping strategies of schizophrenic patients and their relationship to outcome. Br J Psychiatry. 1993;163:177–82.
Stubbs B, Firth J, Berry A, Schuch FB, Rosenbaum S, Gaughran F, Veronesse N, Williams J, Craig T, Yung AR, Vancampfort D. How much physical activity do people with schizophrenia engage in? A systematic review, comparative meta-analysis and meta-regression. Schizophr Res. 2016;176(2–3):431–40.
Svettini A, Johnson B, Magro C, Saunders J, Jones K, Silk S, Hargarter L, Schreiner A. Schizophrenia through the carers’ eyes: results of a European cross-sectional survey. J Psychiatr Ment Health Nurs. 2015;22(7):472–83.
Wancata J, Freidl M, Krautgartner M, Friedrich F, Matschnig T, Unger A, Fruhwald S, Gossler R. Gender aspects of parents’ needs of schizophrenia patients. Soc Psychiatry Psychiatr Epidemiol. 2008;43(12):968–74.
Gutierrez-Maldonado J, Caqueo-Urizar A, Kavanagh DJ. Burden of care and general health in families of patients with schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2005;40(11):899–904.
Nordstroem AL, Talbot D, Bernasconi C, Berardo CG, Lalonde J. Burden of illness of people with persistent symptoms of schizophrenia: a multinational cross-sectional study. Int J Soc Psychiatry. 2017;63(2):139–50.
Mojtabai R, Corey-Lisle PK, Ip EH, Kopeykina I, Haeri S, Cohen LJ, Shumaker S. The patient assessment questionnaire: initial validation of a measure of treatment effectiveness for patients with schizophrenia and schizoaffective disorder. Psychiatry Res. 2012;200(2–3):857–66.
Matza LS, Phillips GA, Revicki DA, Ascher-Svanum H, Malley KG, Palsgrove AC, Faries DE, Stauffer V, Kinon BJ, George Awad A, Keefe RSE, Naber D. Validation of a clinician questionnaire to assess reasons for antipsychotic discontinuation and continuation among patients with schizophrenia. Psychiatry Res. 2012;200(2–3):835–42.
Kitchen H, Rofail D, Heron L, Sacco P. Cognitive impairment associated with schizophrenia: a review of the humanistic burden. Adv Ther. 2012;29(2):148–62.
Mueser KT. Should psychosocial treatment for schizophrenia focus on the proximal or distal consequences of the disorder? J Ment Health. 2012;21(6):525–30.
Kirkpatrick B, Fenton WS, Carpenter WT Jr, Marder SR. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. 2006;32(2):214–9.
Kikkert MJ, Schene AH, Koeter MW, Robson D, Born A, Helm H, Nose M, Goss C, Thornicroft G, Gray RJ. Medication adherence in schizophrenia: exploring patients’, carers’ and professionals’ views. Schizophr Bull. 2006;32(4):786–94.
Rogers A, Day JC, Williams B, Randall F, Wood P, Healy D, Bentall RP. The meaning and management of neuroleptic medication: a study of patients with a diagnosis of schizophrenia. Soc Sci Med. 1998;47(9):1313–23.
Weiden P, Rapkin B, Mott T, Zygmunt A, Goldman D, Horvitz-Lennon M, Frances A. Rating of medication influences (ROMI) scale in schizophrenia. Schizophr Bull. 1994;20(2):297–310.
Rosenheck R, Stroup S, Keefe RS, McEvoy J, Swartz M, Perkins D, Hsiao J, Shumway M, Lieberman J. Measuring outcome priorities and preferences in people with schizophrenia. Br J Psychiatry. 2005;187:529–36.
McCabe R, Saidi M, Priebe S. Patient-reported outcomes in schizophrenia. Br J Psychiatry. 2007;191(50):s21–8.
DiBonaventura M, Gabriel S, Dupclay L, Gupta S, Kim E. A patient perspective of the impact of medication side effects on adherence: results of a cross-sectional nationwide survey of patients with schizophrenia. BMC Psychiatry. 2012;12(1):20.
Naber D. A self-rating to measure subjective effects of neuroleptic drugs, relationships to objective psychopathology, quality of life, compliance and other clinical variables. Int Clin Psychopharmacol. 1995;10(Suppl 3):133–8.
PubMed Google Scholar
Wilkinson G, Hesdon B, Wild D, Cookson R, Farina C, Sharma V, Fitzpatrick R, Jenkinson C. Self-report quality of life measure for people with schizophrenia: The SQLS. British J Psychiatry. 2000;177:42–6.
Gerlinger G, Hauser M, De Hert M, Lacluyse K, Wampers M, Correll CU. Personal stigma in schizophrenia spectrum disorders: a systematic review of prevalence rates, correlates, impact and interventions. World Psychiatry. 2013;12(2):155–64.
Cuffel BJ, Fischer EP, Owen RR, Smith GR. An instrument for measurement of outcomes of Care for Schizophrenia: issues in development and implementation. Eval Health Prof. 1997;20(1):96–108.
Andresen R, Caputi P, Oades L. Stages of recovery instrument: development of a measure of recovery from serious mental illness. Aust N Z J Psychiatry. 2006;40(11–12):972–80.
Bullock WA, Young SL. The mental health recovery measure (MHRM). In: Bullock, et al., editors. Measuring the promise of recovery: a compendium of recovery and recovery-related instruments, Part II W.A. Cambridge: Evaluation Center@HSRI; 2005.
Giffort D, Schmook A, Woody C, Vollendorf C, Gervain M. The recovery assessment scale, in can we measure recovery? A compendium of recovery and recovery-related instruments, R.O. Ralph, K. Kidder, and D. Phillips, Editors. Cambridge: Human Services Research Institute; 2000. p. 7–8 52–55.
Resnick SG, Fontana A, Lehman AF, Rosenheck RA. An empirical conceptualization of the recovery orientation. Schizophr Res. 2005;75(1):119–28.
Bloom BL, Miller A. The consumer recovery outcomes system (CROS 3.0): assessing clinical status and progress in persons with severe and persistent mental illness. Colorado Springs: CROS, LLC/Colorado Health Networks; 2004.
Gibson S, Brand S, Burt S, Boden Z, Benson O. Understanding treatment non-adherence in schizophrenia and bipolar disorder: a survey of what service users do and why. BMC Psychiatry. 2013;13(1):153.
McCabe R, Bullenkamp J, Hansson L, Lauber C, Martinez-Leal R, Rossler W, Salize HJ, Svensson B, Torres-Gonzalez F, van den Brink R, Wiersma D, Priebe S, The Therapeutic Relationship and Adherence to Antipsychotic Medication in Schizophrenia. PLoS One. 2012;7(4).
Download references
Acknowledgments
The authors would like to acknowledge the support of Rethink Mental Illness in advertising the study, and the input of all the carers who took part.
This work was supported by EUFAMI, the European Federation of Associations of Families with Mental Illness.
Dr. Joanne Lloyd was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care Oxford whilst working on drafts of this article. Dr. Helen Lloyd was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South West Peninsula whilst commenting on drafts of this paper. Throughout this project, Prof Ray Fitzpatrick and Dr. Michele Peters were supported by the Department of Health funded Policy Research Unit on Quality and Outcomes of Person Centred Care (QORU), a collaboration between the London School of Economics and Political Science (LSE) and the Universities of Kent and Oxford. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Availability of data and materials
Anonymised transcripts are available from the corresponding author.
Author information
Authors and affiliations.
School of Psychology, Sport and Exercise, Staffordshire University, Stoke on Trent, UK
Joanne Lloyd
Peninsula Medical School, Plymouth University, Plymouth, Devon, UK
Helen Lloyd
Nuffield Department of Population Health, University of Oxford, Old Road Campus, Oxford, OX3 7LF, UK
Ray Fitzpatrick & Michele Peters
You can also search for this author in PubMed Google Scholar
Contributions
MP and RF conceived the study and raised the funding. JL and HL conducted the interviews and led the data analysis. MP and RF contributed to the analysis. All authors were involved in writing the publication. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Michele Peters .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from NHS East of Scotland Research Ethics Service (EoSRES) REC 1 by proportionate review (Application Number 13/ES/0143). All participants gave written informed consent.
Consent for publication
Participants have given consent that anonymised quotes can be used in publications.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Lloyd et al., Treatment outcomes in schizophrenia: qualitative study of the views of family carers. Interview schedule. (DOCX 12 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Lloyd, J., Lloyd, H., Fitzpatrick, R. et al. Treatment outcomes in schizophrenia: qualitative study of the views of family carers. BMC Psychiatry 17 , 266 (2017). https://doi.org/10.1186/s12888-017-1418-8
Download citation
Received : 16 December 2016
Accepted : 04 July 2017
Published : 21 July 2017
DOI : https://doi.org/10.1186/s12888-017-1418-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Schizophrenia
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Functioning in schizophrenia from the perspective of psychologists: A worldwide study
Roles Conceptualization, Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft
* E-mail: [email protected]
Affiliations Clinical Institute of Neurosciences (ICN), Hospital Clinic, Barcelona, Spain, Department of Social Psychology and Quantitative Psychology, University of Barcelona, Barcelona, Spain
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Writing – review & editing
Affiliations Department of Social Psychology and Quantitative Psychology, University of Barcelona, Barcelona, Spain, Group on Measurement Invariance and Analysis of Change (GEIMAC), Institute of Neurosciences, University of Barcelona, Barcelona, Spain
Roles Conceptualization, Investigation, Methodology, Writing – review & editing
Affiliations Institute for Medical Information Processing, Biometry and Epidemiology–IBE, Research Unit for Biopsychosocial Health, Ludwig-Maximilians-Universität (LMU), Munich, Germany, Pettenkofer School of Public Health, Munich, Germany, ICF Research Branch, a cooperation partner within the WHO Collaborating Centre for the Family of International Classifications in Germany (at DIMDI), Munich, Germany
Affiliations Hospital Benito Menni CASM, Sisters Hospitallers, Sant Boi de Llobregat, Spain, Department of Psychiatry, International University of Catalonia, Barcelona, Spain
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing
Roles Conceptualization, Data curation, Formal analysis, Resources, Software, Supervision, Writing – review & editing
- Laura Nuño,
- Georgina Guilera,
- Michaela Coenen,
- Emilio Rojo,
- Juana Gómez-Benito,
- Maite Barrios

- Published: June 6, 2019
- https://doi.org/10.1371/journal.pone.0217936
- Reader Comments
Schizophrenia is a severe mental disorder associated with impairment in functioning. A multidisciplinary approach is essential to help individuals with this health condition, and psychological interventions are considered a priority. The International Classification of Functioning, Disability and Health (ICF) offers a theoretical framework for assessing functioning and disability. The ICF Core Sets for schizophrenia are a list of ICF categories describing the most common problems in functioning of persons affected by this health condition. This study aimed to explore the content validity of these ICF Core Sets and to identify the most common problems in people with schizophrenia from the perspective of psychologists. Psychologists with experience of schizophrenia treatment were recruited for a three-round Delphi study in order to gather their views regarding the problems commonly presented by these patients. A total of 175 psychologists from 46 countries covering the six WHO regions answered the first-round questionnaire, and 137 completed all three rounds. The 7,526 concepts extracted from first-round responses were linked to 412 ICF categories and 53 personal factors. Consensus (≥75% agreement) was reached for 76 ICF categories and 28 personal factors. Seventy-three of the 97 ICF categories that form the Comprehensive ICF Core Set for schizophrenia achieved consensus, and only three categories that yielded consensus do not feature in this Core Set. These results support the content validity of these ICF Core Sets from the perspective of psychologists. This provides further evidence of the suitability of the ICF framework for describing functioning and disability in persons with schizophrenia.
Citation: Nuño L, Guilera G, Coenen M, Rojo E, Gómez-Benito J, Barrios M (2019) Functioning in schizophrenia from the perspective of psychologists: A worldwide study. PLoS ONE 14(6): e0217936. https://doi.org/10.1371/journal.pone.0217936
Editor: Eduardo Fonseca-Pedrero, University of La Rioja, SPAIN
Received: January 26, 2019; Accepted: May 21, 2019; Published: June 6, 2019
Copyright: © 2019 Nuño et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data will be held in the University of Barcelona's repository by clicking this link: http://hdl.handle.net/2445/127181 .
Funding: This work was supported by Spain’s Ministry of Economy and Competitiveness [grant PSI2015–67984-R], and by the Agency for the Management of University and Research Grants of the Government of Catalonia [grant 2017SGR1681]. J. Gómez-Benito was the author who received the funding. The grants financed the preparation of the materials in the five languages in which it was applied, the Qualtrics platform through which the data were collected, and the linguistic revision of the manuscript. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Schizophrenia is a severe mental disorder that afflicts more than 21 million people worldwide [ 1 ]. It has a multifactorial etiology, with numerous individual variables interacting with several environmental factors [ 2 ]. Its lifetime prevalence is estimated at between 0.3% and 0.7%. The disorder is characterized by the presence of delusions, hallucinations, disorganized thinking, abnormal motor behavior (including catatonia), and negative symptoms[ 3 ]. Although this wide range of symptoms can be present in different combinations[ 4 ], patients across the schizophrenia spectrum commonly experience impairments, limitations, and restrictions in major areas of functioning (such as education, work, interpersonal relations, or self-care). Better and more targeted treatment of these areas would help to decrease the stigma that surrounds this illness and empower patients to improve their quality of life [ 5 ].
A multidisciplinary approach to both assessment and clinical intervention is essential to support individuals with this health condition. Worldwide clinical guidelines consider psychological interventions to be one of the mainstays of treatment and emphasize the importance of cognitive-behavioral therapy, cognitive remediation, and family intervention [ 6 – 8 ]. The goals of these interventions are manifold, with key targets being to improve psychological wellbeing and quality of life, neurocognition, and family communication. Other main objectives include training in social skills and problem solving, reducing positive and negative symptoms, and modifying contextual factors to facilitate recovery [ 9 ]. Psychological assessment focuses on the same areas and encompasses both neuropsychological testing and the evaluation of psychosocial functioning [ 10 ].
Achieving these therapeutic goals requires a proper understanding of each patient’s functioning and health status. At the 54th World Health Assembly on 22 May 2001 the International Classification of Functioning, Disability and Health (ICF) was officially endorsed (resolution WHA 54.21 ) by all 191 member states of the World Health Organization (WHO) as the international standard to describe and measure health and disability [ 11 ]. The ICF is based on a multidimensional, biopsychosocial approach (see Fig 1 ) and considers a patient’s functioning as a dynamic interaction between the underlying health condition and specific personal and environmental contextual factors. Its worldwide acceptance and applicability to all health conditions is one of its main contributions in comparison with other evaluation systems. Another key strength is its multidisciplinary approach, insofar as it provides a common language that can be used by all the professionals and healthcare disciplines involved in a person’s care. A comprehensive framework employing a universal language that is understood by all actors could improve the implementation of care plans, leading to a common understanding and shared goals between all health professionals. The ICF provides just such a framework.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0217936.g001
The ICF as a whole includes more than 1400 categories and hence is not suited to application in everyday clinical practice. Consequently, the WHO has established a protocol to develop ICF Core Sets (ICF-CSs) for specific health conditions. Each ICF-CS comprises a selection of ICF categories that are considered essential for describing the functioning of a person living with the corresponding health condition. Following the methodology endorsed by the WHO [ 12 ], the ICF-CSs for schizophrenia have already been developed through a formal decision-making consensus process, integrating evidence from four preparatory studies and expert opinion [ 13 ]. The Comprehensive ICF-CS for schizophrenia consists of 97 categories covering the characteristic spectrum of problems in functioning and health that are experienced by individuals with this disorder; it also includes environmental factors. The Brief ICF-CS for schizophrenia includes just 25 of these categories, the ones considered most important for the purposes of assessment and treatment. The two ICF-CSs for schizophrenia are available for free download at: https://www.icf-research-branch.org/icf-core-sets-projects2/mental-health/icf-core-set-for-schizophrenia .
A basic requirement for the implementation of these ICF-CSs in clinical practice is their validation from different perspectives. The content validity of the ICF-CSs for schizophrenia has already been examined and supported from the perspective of psychiatrists [ 14 ]. The goal of the present study was to build on this by exploring content validity from the perspective of psychologists, another group of health professionals closely involved in the care of individuals with schizophrenia. Specifically, our two objectives were: 1) to identify the problems, personal characteristics/resources, and aspects of the environment that psychologists regard as most important for understanding functioning in people with schizophrenia; and 2) to analyze the extent to which the problems and aspects identified are represented in the ICF-CSs for schizophrenia.
We conducted a three-round worldwide Delphi study by means of an e-mail survey. This is a multistage process in which each stage or round builds on the results of the previous one in order to gather and provide information about a particular subject [ 15 ]. The purpose is to achieve consensus from a panel of individuals with knowledge of the topic of interest (hereinafter, experts). The Institutional Review Board Committee of University of Barcelona approved the Study IBR00003099. Participants were provide with a written consent form. The study procedure was the same as that used in the validation study of the ICF-CS for schizophrenia from the perspective of psychiatrists, and hence further details can be consulted in Nuño et al. (2018) [ 14 ].
Recruitment of participants
Expert psychologists from around the world were recruited by contacting international associations of psychologists, universities with health professional training programs, and hospitals. We also made use of literature searches, LinkedIn contacts, and personal recommendations. To ensure that study participants were all “informed individuals” with regard to the treatment of individuals with schizophrenia, the initial invitation letter specified that they should be “psychologists experienced in the treatment of schizophrenia”. In addition, it was made clear that they should have at least one year experience of treating adults with schizophrenia.
Our aim was to recruit a panel of experts as broad and heterogeneous as possible and to achieve consensus and common opinion despite and across this variability. Indeed, we sought to obtain a sample of experts that, as far as possible, reflected worldwide variety in all the variables considered (e.g., gender, age, years of experience, and region). Furthermore, experts did not need to have specific knowledge about the ICF, and they were selected without taking into account their therapeutic orientation or training background. It was made clear that they should base their answers on their clinical experience. Those psychologists who had participated in any earlier stage of developing the ICF-CS for schizophrenia were not eligible for the present study.
All potential participants received an invitation with basic information about the study and what would be required of them. They were also asked to provide demographic and professional data. Of the 1,555 health professionals who agreed to take part and who provided demographic and professional data, 223 were psychologists who met the eligibility criteria and who were therefore invited to begin round one of this study.
A total of 175 psychologists from 46 countries covering the six WHO regions answered the first-round survey (78.5% of the 223 who were sent the survey material). They primarily worked in clinical practice (mean 46.3% of their time), followed by research (28.1%), teaching and training (16.9%), management (7.8%), and other tasks (0.9%). Table 1 shows participants’ demographic and professional characteristics. The second-round survey was answered by 151 psychologists, and 137 completed the third round, with a response rate across rounds one to three of 78.3%.
https://doi.org/10.1371/journal.pone.0217936.t001
There were no statistically significant differences in age, gender, or population treated (urban, rural, acute, and chronic) between psychologists who responded in the first round and those were invited to take part but did not do so. However, there was a significant difference between these two groups in years of experience (p < .01), since the invited experts who did not respond were less experienced than those who did take part. Specifically, 52% of invited experts who did not respond had less than five years’ experience in the treatment of individuals with schizophrenia, while this was the case for only 20% of the experts who did take part in the first round.
There were no significant differences in age, gender, or years of experience in treating individuals with schizophrenia between the groups that responded across rounds 1 to 3.
Material and data collection
With the aim of avoiding language barriers and encouraging participation by experts from different world regions, the study was conducted in five languages (Chinese, English, French, Russian, and Spanish). The survey materials were independently translated and supervised by at least two native speakers. The Delphi process is shown in Fig 2 . Data were collected between March and June 2017, with participants being allowed two weeks to respond in each round.
https://doi.org/10.1371/journal.pone.0217936.g002
Responses in the first Delphi round were logged using an online survey system ( www.qualtrics.com ). Participants were sent an e-mail with a link to the survey homepage and instructions (i.e., to list all the aspects they considered to be relevant when assessing and/or treating individuals with schizophrenia). To help them with this survey they were asked to consider six open-ended questions that covered all four components of the ICF-CS; the Environmental factors component was divided into supportive and hindering factors (survey questions can be consulted in S1 Text ). The expected completion time for each survey round was about 15 minutes.
The responses gathered in the first round were then linked to ICF categories using established ICF linking rules [ 16 , 17 ]. All categories reported by at least 5% of the experts were listed and presented to the panel in the second Delphi round. Specifically, all the panelists who had responded in the first round were sent a list of the selected ICF categories linked to the responses of all participants, as well as a list of the categories proposed for Personal factors , along with their respective definitions. The categories included in the ICF-CSs for schizophrenia were also listed. For each category, they were asked to indicate whether it was relevant from their perspective as a psychologist to the assessment and/or treatment of individuals with schizophrenia. They were reminded that the aim was to obtain a final list that was both short enough to be applicable in clinical practice and sufficiently comprehensive to cover the most important needs of people with schizophrenia. Participants in the third round were asked to evaluate the same list of categories again, this time taking into account the feedback they were sent concerning the responses of the panel and their own previous responses.
All components of the ICF, except Personal factors , are organized hierarchically in an exhaustive list of categories (see Fig 3 ). Third- and fourth-level categories are more specific than second-level categories, and they share the attributes of the second-level category with which they are associated. Therefore, their use implies that the corresponding second-level category is applicable.
https://doi.org/10.1371/journal.pone.0217936.g003
Two health professionals with experience of treating persons with schizophrenia and trained in the use of the ICF independently linked all responses from the first Delphi round to the corresponding ICF categories. For instance, if the reported problem was ‘executive dysfunction’, the concept ‘executive function’ was extracted and assigned to the ICF category b164 Higher-level cognitive functions . Any disagreements between the two independent coders were reviewed and discussed by two other health professionals with the aim of achieving consensus.
Personal factors were defined as the particular background of an individual’s life and living situation (e.g., age) [ 18 ]. Personal traits that constitute a premorbid predisposition of individuals and which affect how they cope with their illness were considered as Personal factors , whereas personality traits that are altered due to the illness were coded under category b126 of Body functions . As Personal factors are not currently categorized in the ICF, they do not feature in the ICF-CS for schizophrenia. However, as they are relevant to assessment and intervention planning, concepts related to Personal factors were summarized and considered in rounds two and three of the Delphi study. The proposed categorization of Personal factors was developed by consensus among three psychologists (L.N., M.B., G.G.) based on previously proposed categorizations of personal factors [ 14 , 18 , 19 ] and on the experts’ responses to the question about personal factors.
Data analysis
We calculated descriptive statistics for the sociodemographic characteristics of participants and the frequencies of ICF categories. In order to be able to compare our findings with the ICF-CSs for schizophrenia, which comprise solely second-level categories, all third- and fourth-level categories identified in the Delphi process were aggregated to their corresponding second-level category.
Based on previous studies [ 14 , 20 ], consensus was defined as agreement among at least 75% of participants. Inter-coder reliability was assessed by calculating the delta statistic and 95% confidence intervals (95% CI) [ 21 ]. In order to facilitate comparison with previous studies that use the kappa index, we also calculated this statistic and its 95% CI [ 22 ].
The categories for which there was agreement in the third round were compared with the categories included in both the Brief and Comprehensive ICF-CSs.
Linking process
From the experts’ answers in round one, a total of 7,526 concepts were extracted and linked to 412 ICF categories (219 second-level, 189 third-level, and 4 fourth-level). Fifty-three categories were proposed for the Personal factors identified. Aggregation of third- and fourth-level categories to their corresponding second-level category yielded a list of 223 second-level ICF categories. Those ICF categories and Personal factors that were reported by less than 5% of the experts (98 ICF categories and 20 personal factors) were excluded from the second round; ICF categories coded as ‘other specified’ or ‘unspecified’ at the second-level ( n = 11 ICF categories) were also excluded. This meant that in round two, the panel had to consider a list of 114 second-level ICF categories and 33 Personal factors . In the third round, consensus (i.e., agreement of at least 75%) was reached for 76 ICF categories and 28 Personal factors . Data regarding the categories presented to experts in rounds two and three and the degree of consensus reached are shown in the first two rows of Table 2 . Applying the delta statistic method, a general index of .90 [95% CI: .89 - .91] was obtained, indicating that 90% of agreements were not due to chance. The kappa coefficient for the linking process was .90 [95% CI: .88 - .92].
https://doi.org/10.1371/journal.pone.0217936.t002
Correspondence between panel responses and the ICF core sets for schizophrenia
Agreement of 75% or higher was reached for 75.3% of the categories included in the Comprehensive ICF-CS for schizophrenia and for all the categories in the Brief version. Therefore, the following analysis refers solely to the Comprehensive ICF-CS. A summary of the results is shown in the third and fourth row of Table 2 . More detail regarding the categories listed by the experts and the corresponding percentage analyses is provided in S1 – S5 Tables. Table 3 lists the categories that did not match in the two sets of data (the set of categories included in the ICF-CS for schizophrenia and the set of categories that reached consensus).
https://doi.org/10.1371/journal.pone.0217936.t003
With respect to the Body functions component, an agreement of 75% or higher was achieved for 14 categories. Of these, only one ( b126 Temperament and personality functions ) does not feature in the ICF-CS for schizophrenia. Four of the 17 categories that are included in the ICF-CS for schizophrenia ( b330 Fluency and rhythm of speech functions , b530 Weight maintenance functions , b640 Sexual functions , and b765 Involuntary movement functions ) did not achieve consensus in the Delphi study (see S1 Table for more details).
Regarding the Body structures component, the ICF-CS for schizophrenia does not contain any category from this component. However, one of its categories ( s110 Structure of brain ) reached an agreement of 90% in the Delphi study (for more details, see S2 Table ). With respect to the Activities and Participation component, all the categories that reached consensus ( n = 32) form part of the ICF-CS for schizophrenia. Sixteen categories from this component that are included in the ICF-CS for schizophrenia did not yield consensus (see S3 Table for more information).
Twenty-nine categories from the Environmental factors component yielded agreement of at least 75%, and only one of them ( e135 Products and technology for employment ) is not included in the ICF-CS for schizophrenia. Four categories from this component that do feature in the ICF-CS for schizophrenia did not reach consensus in the Delphi study (see S4 Table ).
In summary, only three of the 76 categories that yielded an agreement of at least 75% do not feature in the Comprehensive ICF-CS for schizophrenia. Twenty-four categories that form part of the ICF-CS did not achieve consensus among the experts. Regarding Personal factors , which are not classified in the ICF, 33 concepts were presented to the experts, and 28 of these yielded consensus (see S5 Table ).
This validation study highlights the functioning-related issues that psychologists encounter in their work with individuals with schizophrenia and considers the extent to which these aspects are covered by the ICF Core Sets for schizophrenia. All categories included in the Brief ICF-CS for schizophrenia were selected by 75% or more of participating experts, thus supporting the relevance of the categories that form this ICF-CS. We will therefore focus on comparing our results with the categories featured in the Comprehensive ICF-CS for schizophrenia. As many of the categories listed in that Core Set were considered important by more than half the experts but did not reach the threshold for consensus (75% agreement), the results are discussed by considering categories that were clearly excluded (50% or less of agreement), those whose relevance appears to be ambiguous (between 50% and 75% of agreement), and those for which there was consensus (75% or more agreement).
Concerning the Body functions component, all the categories that yielded consensus belong to chapter b1 Mental functions . Some of the categories that achieved higher consensus refer to cognitive functions, such as b164 Higher-level cognitive functions . This area is one of the main targets of psychological interventions such as cognitive remediation therapy (CRT), which aims to improve neurocognition and other functional outcomes in individuals with schizophrenia [ 23 ]. Psychological interventions also address other categories that were associated with high agreement, namely psychosocial functions ( b122 Global psychosocial functions [ 24 ]), functions affected by negative symptoms (e.g., b130 Energy and drive functions and b152 Emotional functions [ 25 , 26 ]), and classical symptoms in schizophrenia such as delusions and hallucinations (e.g. b156 Perceptual functions [ 27 ]). These results differ slightly from those obtained from the perspective of psychiatrists [ 14 ]. Although psychiatrists highlighted the importance of many categories from chapter b1 Mental functions , they also emphasized other categories from the Body functions component, such as b530 Weight maintenance functions or b765 Involuntary movement functions . This is consistent with the more biomedical perspective of psychiatrists.
Only one of the categories from the Body functions component ( b126 Temperament and personality functions ) that reached an agreement of at least 75% is not included in the ICF-CS for schizophrenia. As this category also reached consensus in the validation study from the perspective of psychiatrists it clearly reflects a problem area for these patients [ 28 , 29 ], and therefore its exclusion from the ICF-CS for schizophrenia should be reconsidered. Four categories from the Body functions component of the ICF-CS (i.e., b330 Fluency and rhythm of speech functions , b530 Weight maintenance functions , b640 Sexual functions , and b765 Involuntary movement functions ) did not achieve consensus in the Delphi study but were considered important by more than half the experts. This suggests that these categories are relevant to the assessment of and intervention with persons with schizophrenia, but that they may not be the most common target of psychologists’ interventions, which focus primarily on mental rather than other body functions [ 23 ]. In fact, these functions are mainly assessed by other professionals, such as endocrinologists (weight maintenance) or physiotherapists (movement abnormalities).
Although no category from the Body structures component is currently included in the ICF-CS for schizophrenia, 90% of the psychologists agreed that brain structure ( s110 Structure of brain ) is an essential aspect to consider when treating individuals with schizophrenia. The relevance of this category was likewise noted in the Delphi study from the perspective of psychiatrists [ 14 ], where agreement was even higher (97%). The literature also supports the idea that the brain is the main altered structure in this illness and it is considered to be the basis of other dysfunctions such as neuropsychological impairment [ 30 ]. There is also evidence that psychological interventions produce changes in brain structure and its functioning [ 31 ], with this being the goal of interventions such as cognitive remediation. Thus, from the perspective of psychologists, inclusion of this category in the ICF-CS for schizophrenia should be considered.
The component with the largest number of categories achieving consensus was Activities and Participation . These categories covered all its chapters and focused especially on learning and applying knowledge (e.g., d160 Focusing attention ), interpersonal interactions (e.g., d720 Complex interpersonal interactions ), and major life areas such as education (e.g., d830 Higher education ) and employment (e.g., d845 Acquiring , keeping and terminating a job ). Once again, these results are consistent with those obtained in the validation of the ICF-CS for schizophrenia from the perspective of psychiatrists. All categories of the Activities and Participation component for which consensus was reached are listed in the ICF-CS for schizophrenia. This reflects the fact that schizophrenia has a major impact on everyday functioning in all these areas, and illustrates why the main long-term therapeutic goals in the psychological treatment of these individuals are not limited to specific symptoms, but rather focus on improving patients’ psychosocial functioning [ 32 , 33 ]. Sixteen categories that are included in the Activities and Participation component of the Comprehensive ICF-CS for schizophrenia were initially referred to by many of our experts but did not reach the threshold for consensus. Of these, the ambiguous categories (i.e., those selected by more than 50% but less than 75% of the expert panel) mainly belong to chapter d6 Domestic life (e.g., d640 Doing housework ) or are related to employment (e.g., d855 Non-remunerative employment ). It is worth noting that these categories did yield agreement of 75% or higher in the Delphi study from the perspective of psychiatrists, thus highlighting how different professional views may complement one another. The Comprehensive ICF-CS categories that were selected by fewer than 50% of psychologists mainly referred to simple activities such as d210 Undertaking a single task and d330 Speaking , whereas consensus was achieved for the equivalent more complex categories (e.g., d220 Undertaking multiple tasks ). These results offer a more positive view of the abilities of people with schizophrenia, since it suggests that their difficulties mainly depend on the complexity of the task.
As in the previous study from the perspective of psychiatrists, the component with the second highest number of categories showing agreement of at least 75% was Environmental factors . The agreed-upon categories especially concerned support and relationships (e.g., e320 Friends ), attitudes ( e410 Individual attitudes of immediate family members ), and the accessibility of health services ( e580 Health services , systems , and policies ). These results suggest that psychologists ascribe considerable importance to the impact of environmental factors on the functioning of a person with schizophrenia, a point already made by other authors [ 34 , 35 ]. Of the 29 categories from this component that yielded consensus in the Delphi study, only one (i.e., e135 Products and technology for employment ) is not included in the ICF-CS for schizophrenia. This category belongs to chapter e1 Products and Technology , and it should be noted that the ICF-CS for schizophrenia already contains four categories from the same chapter (i.e., e110 Products or substances for personal consumption , e125 Products and technology for communication , e130 Products and technology for education and e165 Assets ). Given that an ICF-CS needs to be as short as possible, this domain may already be sufficiently covered by these four categories. Four categories from the Environmental factors component of the ICF-CS for schizophrenia did not achieve consensus but were selected by more than 50% of the experts surveyed. This suggests that these categories (e.g., e555 Associations and organizational services , systems , and policies ) may be relevant to the assessment and treatment of individuals with schizophrenia, but that they are not primary targets of psychological intervention. Once again, these categories did yield agreement of at least 75% in the Delphi study from the perspective of psychiatrists, underlining the importance of analyzing functionality from a multidisciplinary point of view.
Concerning the Personal factors component, we drew up a proposed list of 33 personal factors, 28 of which achieved consensus in the third Delphi round. This level of agreement supports the relevance of personal factors to the assessment and treatment of individuals with schizophrenia. Personal factors, such as resilience [ 36 , 37 ], premorbid cognitive skills [ 38 ], premorbid social skills [ 39 ], personal history and biography [ 40 ], premorbid drug use and lifestyle [ 41 ], and premorbid personality [ 42 ] have been considered to influence how people with schizophrenia cope with their illness. Most of the categories that psychologists regarded as important coincide with those identified in the validation study from the perspective of psychiatrists [ 14 ], suggesting that the proposed list of Personal factors captures the aspects that merit particular consideration in this population. In light of these results, it would be useful if the ICF included comprehensive specifications of ‘Personal factors’, or at least a list of such factors, so as to enable more systematic reporting of the personal factors that influence functioning and health and to further stimulate research in this important area [ 43 ].
Twenty-four categories that feature in the ICF-CS for schizophrenia did not achieve agreement of 75% in the present Delphi study. This is likely due to the multidisciplinary approach that was used to develop this ICF-CS, which aims to cover the main intervention targets not merely of a specific professional group (in this case, psychologists) but of all health professionals involved in the treatment of individuals with schizophrenia [ 11 ].
A particular strength of the present study is that the panel of experts comprised 175 psychologists from 46 countries covering all six WHO regions. Such a large sample is not common in this kind of study [ 44 , 45 ]. Furthermore, all the experts surveyed had considerable experience (54.7% with 10 or more years) in the treatment of patients with schizophrenia, both acute and chronic and from both rural and urban settings. Another strength of the study is that participation was possible in any of five languages, and this is likely to have been a key factor in achieving such a multicultural and multinational representation. It should also be noted that the response rate across rounds one to three was 78%, considerably higher than the mean across rounds of 50% that is reported in the literature [ 46 ]. The primary limitation of the study concerns the representativeness of the panel of experts. Although psychologists from all over the world took part, the Eastern Mediterranean, Western Pacific, and African WHO regions were under-represented, and this may limit the external validity of our results. Possible reasons for this under-representation include limited internet access and lower numbers of psychologists in these regions.
To conclude, the results of this study provide strong support for the content validity of the Comprehensive ICF-CSs for schizophrenia as they were obtained by surveying psychologists from all six WHO regions. Of the ICF categories that were selected by at least 75% of experts in the Delphi study, 96% feature in the Comprehensive ICF-CS for schizophrenia. Consensus was achieved for 75.3% of the ICF categories included in the Comprehensive ICF-CS, and 100% of those in the Brief ICF-CS. These results are in line with those obtained in the validation study from the perspective of psychiatrists, where all the categories of the Brief ICF-CS and 90% of those in the Comprehensive version yielded consensus. The fact that there are also some differences in emphasis between psychologists and psychiatrists highlights the importance of considering different professional points of view in order to achieve a fuller picture of how functioning is affected in this population. Taken together, these results suggest that the ICF-CSs for schizophrenia provide a clinically relevant framework for organizing information about this health condition. Having a basic set of categories that addresses a particular patient population at different stages of an illness and that helps both to improve communication within multi-professional teams and to guide the management and treatment of patients by different health professionals is important for ensuring optimal care [ 47 ]. The ICF-CSs for schizophrenia can be used as a standard set of ICF categories to facilitate the assessment of functioning in real-life clinical practice by using the ICF qualifiers, which are codes used to record the extent of functioning or disability in a domain or category, or the extent to which an environmental factor is a facilitator or barrier. Importantly, improvement and decline in aspects of functioning can be displayed in a functioning profile over the course of treatment or over the life span. The ICF-CSs for schizophrenia may also be used as a framework for analyzing the content of patient-reported outcome measures or to inform instrument developers about what needs to be included in tools designed to assess the functioning of persons with schizophrenia. Further validation studies from the perspective of other professionals (i.e., nursing, occupational therapy, social work, and physiotherapy) are now needed in order to complement the present findings and to move a step closer towards a definitive version of the ICF-CS for schizophrenia.
Supporting information
S1 text. survey questions (round 1)..
https://doi.org/10.1371/journal.pone.0217936.s001
S2 Text. Acknowledgments.
https://doi.org/10.1371/journal.pone.0217936.s002
S1 Table. Body functions component.
https://doi.org/10.1371/journal.pone.0217936.s003
S2 Table. Body structures component.
https://doi.org/10.1371/journal.pone.0217936.s004
S3 Table. Activities and participation component.
https://doi.org/10.1371/journal.pone.0217936.s005
S4 Table. Environmental factors component.
https://doi.org/10.1371/journal.pone.0217936.s006
S5 Table. Personal factors component (proposed categories).
https://doi.org/10.1371/journal.pone.0217936.s007
Acknowledgments
The authors would like to thank all the participating experts for their commitment and the time spent, without which the study would not have been possible. Further information about the experts who formed part of this study is available as supplementary data ( S2 Text ).
- 1. World Health Organization (WHO) | Schizophrenia. In: World Health Organization. World Health Organization; 2016.
- View Article
- PubMed/NCBI
- Google Scholar
- 3. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5). American Psychiatric Pub; 2013.
- 11. ICF; World Health Organization. International Classification of Functioning, Disability and Health: ICF. World Health Organization; 2001.
Schizophrenia Research: Latest Findings
Schizophrenia research is ongoing, and new developments are consistently being made. For some people with schizophrenia, findings can introduce new interventions that may significantly affect their lives at critical points, possibly improving schizophrenia symptoms and functioning.
Researchers suggest that genetic and environmental factors play a role in the development course of schizophrenia and look to examine the ways such factors might be mitigated with interventions. Other research might focus on prevention, brain changes in particular stages of the illness, or psychotic symptoms.

Schizophrenia research
Considered the official journal of the Schizophrenia International Research Society (SIRS), the Schizophrenia Research journal gathers findings from multiple studies in one place, featuring various clinical trials, systematic reviews, and meta-analyses.
For example, one recent study focused on the relationship between negative symptoms and motivation toward monetary rewards. The study in question looked at both bipolar disorder and schizophrenia and suggested that negative symptoms were linked with lower motivation for goal-oriented, monetary rewards.
Early psychosis research
A global network of researchers called Accelerating Medicines Partnership Schizophrenia (AMP SCZ), which was launched in 2020, is presently working to study young, at-risk people for schizophrenia .
Mount Sinai has announced that this network of researchers is entering a new phase of testing preventive measures and interventions for addressing schizophrenia symptoms. According to Mount Sinai, "MP SCZ is collecting data on biomarkers that could predict which individuals are at risk for developing psychosis." The participants, who are between 12 and 30, are spread across 13 countries.
On June 2023, Mount Sinai researchers from around the world presented findings on "new psychosis risk biotypes, cannabidiol as a novel treatment for psychosis, and new clinical interventions for early-stage mental illness."
First episode psychosis
One recent study involving 404 persons aged 15 to 40 years old with non-affective first episode psychosis (FEP) participated in a program called the Recovery After Initial Schizophrenia-Early Treatment Program. The program notes that early intervention services have been shown to improve symptoms and functioning in (FEP), but research hasn't yet examined these services' impact on cognitive functioning. To test their theory, participants were put in either community care (CC) or an early intervention program called NAVIGATE for a period of two years.
The program's findings suggest that early intervention programs may not be as significant in improving cognitive functioning for older FEP patients but showed effectiveness in improving working memory in younger FEP patients. Participants aged 15 to 19 in the early intervention program indicated significant improvement in working memory. Moreover, improvements in cognitive functioning noted in the first year correlated with reduced symptom severity. The study concluded that "interventions targeting cognition may be required to enhance cognitive functioning in most FEP patients."

Differences in brain structure
A structural and functional MRI study sought to examine progressive changes in the brain throughout the illness course. The study had 115 participants with different stages of schizophrenia, divided according to how long they've had the illness (five, 15, and 25 years). These three groups were matched with a control group of 230 people without schizophrenia or another mental disorder.
All groups were evaluated using two structural and functional MRI analysis methods, and each group of patients with schizophrenia was compared with the control groups. These methods indicated that brain abnormalities become present at different stages of the illness. The researchers noted that "individual functional abnormalities occur in limited brain areas initially, functional connectivity and gray matter density abnormalities ensue later in wider brain areas, and structural connectivity abnormalities involving almost all white matter tracts emerge in the third decade of the course in schizophrenia."
The study tested the possible effect of long-term usage of antipsychotic medication on the brain. Its findings suggested no "significant correlation" between accumulative exposure to medication and observed brain abnormalities. Currently, brain scans are not considered a reliable method of diagnosis for any mental illness.
Cognitive symptoms
The cognitive impairment associated with schizophrenia symptoms has been a source of interest for researchers. Current findings suggest that cognitive impairment seems to be distinct from positive and negative symptoms . Using a five-factor model (positive, negative, disorganized, excited, and depressed), the Positive and Negative Syndrome Scale (PANSS) is often used to assess the structure of symptoms. Research indicates the disorganized factor is associated with more cognitive impairment.
Mental health services
A cross-sectional observational study assessed how diagnosed schizophrenia patients had their first contact with mental health services . The study included 150 schizophrenia patients between 12 and 60 years old. It found that faith healers were the most common "pathway to care," and factors such as family members' education and socioeconomic background influence the choice and perception of psychiatric care. The researchers suggest that "while planning mental health services, emphasis should be made on collaboration between psychiatric and nonpsychiatric services."
Healthcare providers
A systematic review of the role of primary care physicians in managing schizophrenia in low- and middle-income countries suggests that appropriate training of primary care physicians to address schizophrenia may reduce the treatment gap and introduce interventions for improving quality of life. The review indicates a need for more integrated care of various professionals who encounter individuals at risk for schizophrenia.

Safeguarding your mental health
Speaking to a therapist may be valuable when struggling with daily life challenges. A therapist can help clients manage stress and find ways to navigate symptoms. If in-person sessions are inconvenient or not easy to access, online therapy can be an accessible way to receive therapy.
Online therapy through platforms like BetterHelp can be a convenient and easy-to-use option for some people grappling with schizophrenia symptoms across the spectrum. Clients can choose between phone, video, or in-app messaging sessions and access resources like support groups and worksheets.
A review and synthesis of relevant factors of online psychosocial interventions for psychosis noted that "increased engagement is associated with improved outcomes," but other factors (individual, environmental, and type of intervention) also influence engagement. The synthesized findings suggest that "interventions should be flexible, easy to use , aim to promote motivation, and incorporate some form of support."
Schizophrenia research findings may introduce new interventions that may significantly affect the lives of people with schizophrenia at critical points, improving symptoms and functioning.
Researchers suggest that genetic and environmental factors play a role in the development course of schizophrenia and look to examine the ways such factors might be mitigated with appropriate interventions. Research may focus on various areas related to schizophrenia, including brain changes in particular stages of the illness, psychotic symptoms, and environmental factors.
Considered the official journal of the Schizophrenia International Research Society (SIRS), the Schizophrenia Research journal gathers findings from multiple studies into one place — a source for those looking for the latest on schizophrenia-related findings. Schizophrenia research is ongoing, and new developments are on their way. Speaking to a therapist can also be helpful when struggling with challenges that affect your well-being, regardless of your diagnostic status.
- How To Establish A Schizophrenia Care Plan Following Diagnosis Medically reviewed by Andrea Brant , LMHC
- Schizophrenia Suicide Rate: How To Address Risk Medically reviewed by April Justice , LICSW
- Schizophrenia
- Relationships and Relations

8 Ways to Know if Your Schizophrenia Treatment Is Helping
The effects are rarely immediate, but treatment can relieve many symptoms of schizophrenia.
Some people may notice improvements within weeks of starting treatment, says Joel Frank, PsyD , a psychologist in Los Angeles. For others, it may take several months to a year to feel the full effects.
“The initial [treatment] steps often involve finding the right combination of medication and therapy that works best. This process can vary significantly from one person to another,” says Dr. Frank.
Sticking to your treatment plan is important and may bring benefits sooner than expected. “Some people might notice an effect from the medications right away, within days,” says Bruce Bassi, MD , a psychiatrist based in Chicago.
The following clues can help you determine when your treatment is working.
1. Hallucinations and Delusions Occur Less Frequently
“For some individuals living with schizophrenia, they might not understand their hallucinations or delusions are symptoms of their diagnosis. The easing of such symptoms could … be the first time a person understands the full scope of their schizophrenia,” says Frank, who adds that with medication specifically, these symptoms are often the first to abate.
2. You’re Sleeping Better
As your treatment starts to work and your hallucinations and delusions become less frequent, you may notice less psychological distress in general and greater mental clarity, says Frank, which can allow you to relax and sleep more easily.
3. Tough Days Don’t Get to You as Easily
“Through the combined efforts of therapy and medications, individuals living with schizophrenia can learn the necessary skills for managing emotional reactivity and how to challenge distressing thoughts and beliefs.” With practice, it becomes easier to handle tough days — a sure sign your treatment is helping.
4. You Have More Energy
5. it’s easier to focus.
Bassi, who treats patients with schizophrenia in an inpatient setting, says he also notices that people can focus on questions and answer them more logically after a few weeks of treatment.
6. You Want to Be Around People Again
Getting back into the social game may come with some adjustment and anxiety at first, says Bassi. “Allow yourself to see how socialization affects other parts of the mental illness, such as hallucinations," he says. "Some individuals find that talking to other people is very helpful to lessen and distract them from the voices in their head.”
7. Your Loved Ones Notice You’re More Expressive
This type of symptom can take longer — often months — to improve, says Bassi. But after some time, your friends and family may tell you they’ve noticed a change in your voice and expression, which means your treatments are helping.
8. It’s Easier to Take Care of Yourself
With the boost in energy that tends to result from treatment, you may notice you can perform daily tasks more easily. Bassi says that treatment can lead to fewer distracting thoughts, improved ability to stay on tasks, and a better ability to take care of yourself.
Once you realize you want to brush your hair, cook a meal, or take a shower again, you can feel confident your schizophrenia treatment is starting to work.
Questions to Ask Your Doctor
- How will I know if the treatment is working?
- When should I start seeing results?
- Is there a chance the symptoms will go away altogether?
- What should I do if I continue to have hallucinations or other symptoms?
- Could another condition be causing or worsening my symptoms?
Editorial Sources and Fact-Checking
Everyday Health follows strict sourcing guidelines to ensure the accuracy of its content, outlined in our editorial policy . We use only trustworthy sources, including peer-reviewed studies, board-certified medical experts, patients with lived experience, and information from top institutions.
- Schizophrenia. National Institute of Mental Health. April 2024.
- Oh S et al. Effectiveness of Antipsychotic Drugs in Schizophrenia: A 10-year Retrospective Study in a Korean Tertiary Hospital. Nature . November 19, 2020.
- Modesti MN et al. A Systematic Review on Add-On Psychotherapy in Schizophrenia Spectrum Disorders. Journal of Clinical Medicine . February 2023.
- Waite F et al. Sleep and Schizophrenia: From Epiphenomenon to Treatable Causal Target. Schizophrenia Research . July 2020.
- Sharma A et al. Emotional and Behavioral Dysregulation in Severe Mental Illness. Child and Adolescent Psychiatric Clinics of North America . April 2021.
- Leucht S et al. Long-Term Efficacy of Antipsychotic Drugs in Initially Acutely Ill Adults With Schizophrenia: Systematic Review and Network Meta-Analysis. World Psychiatry . June 2023.

Related Topics
- What Can Trigger a Psychotic Episode?
- Tardive Dyskinesia
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 9, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
New treatment could reverse hair loss caused by autoimmune skin disease alopecia areata
by Anne Trafton, Massachusetts Institute of Technology

Researchers at MIT, Brigham and Women's Hospital, and Harvard Medical School have developed a potential new treatment for alopecia areata, an autoimmune disorder that causes hair loss and affects people of all ages, including children.
For most patients with this type of hair loss , there is no effective treatment. The team has developed a microneedle patch that can be painlessly applied to the scalp and releases drugs that help to rebalance the immune response at the site, halting the autoimmune attack.
In a study of mice, the researchers found that this treatment allowed hair to regrow and dramatically reduced inflammation at the treatment site, while avoiding systemic immune effects elsewhere in the body. This strategy could also be adapted to treat other autoimmune skin diseases such as vitiligo, atopic dermatitis , and psoriasis, the researchers say.
"This innovative approach marks a paradigm shift. Rather than suppressing the immune system, we're now focusing on regulating it precisely at the site of antigen encounter to generate immune tolerance," says Natalie Artzi, a principal research scientist in MIT's Institute for Medical Engineering and Science, an associate professor of medicine at Harvard Medical School and Brigham and Women's Hospital, and an associate faculty member at the Wyss Institute of Harvard University.
Artzi and Jamil R. Azzi, an associate professor of medicine at Harvard Medical School and Brigham and Women's Hospital, are the senior authors of the new study , which was published in the journal Advanced Materials . Nour Younis, a Brigham and Women's postdoc, and Nuria Puigmal, a Brigham and Women's postdoc and former MIT research affiliate, are the lead authors of the paper.
The researchers are now working on launching a company to further develop the technology, led by Puigmal, who was recently awarded a Harvard Business School Blavatnik Fellowship.
Direct delivery
Alopecia areata, which affects more than 6 million Americans, occurs when the body's own T cells attack hair follicles, leading the hair to fall out. The only treatment available to most patients—injections of immunosuppressant steroids into the scalp—is painful and patients often can't tolerate it.
Some patients with alopecia areata and other autoimmune skin diseases can also be treated with immunosuppressant drugs that are given orally, but these drugs lead to widespread suppression of the immune system, which can have adverse side effects.
"This approach silences the entire immune system, offering relief from inflammation symptoms but leading to frequent recurrences. Moreover, it increases susceptibility to infections, cardiovascular diseases, and cancer," Artzi says.
A few years ago, at a working group meeting in Washington, Artzi happened to be seated next to Azzi (the seating was alphabetical), an immunologist and transplant physican who was seeking new ways to deliver drugs directly to the skin to treat skin-related diseases.
Their conversation led to a new collaboration, and the two labs joined forces to work on a microneedle patch to deliver drugs to the skin. In 2021, they reported that such a patch can be used to prevent rejection following skin transplant. In the new study, they began applying this approach to autoimmune skin disorders.
"The skin is the only organ in our body that we can see and touch, and yet when it comes to drug delivery to the skin, we revert to systemic administration. We saw great potential in utilizing the microneedle patch to reprogram the immune system locally," Azzi says.
The microneedle patches used in this study are made from hyaluronic acid crosslinked with polyethylene glycol (PEG), both of which are biocompatible and commonly used in medical applications. With this delivery method, drugs can pass through the tough outer layer of the epidermis, which can't be penetrated by creams applied to the skin.
"This polymer formulation allows us to create highly durable needles capable of effectively penetrating the skin. Additionally, it gives us the flexibility to incorporate any desired drug," Artzi says.
For this study, the researchers loaded the patches with a combination of the cytokines IL-2 and CCL-22. Together, these immune molecules help to recruit regulatory T cells, which proliferate and help to tamp down inflammation. These cells also help the immune system learn to recognize that hair follicles are not foreign antigens, so that it will stop attacking them.
Hair regrowth
The researchers found that mice treated with this patch every other day for three weeks had many more regulatory T cells present at the site, along with a reduction in inflammation. Hair was able to regrow at those sites, and this growth was maintained for several weeks after the treatment ended. In these mice, there were no changes in the levels of regulatory T cells in the spleen or lymph nodes, suggesting that the treatment affected only the site where the patch was applied.
In another set of experiments, the researchers grafted human skin onto mice with a humanized immune system. In these mice, the microneedle treatment also induced proliferation of regulatory T cells and a reduction in inflammation.
The researchers designed the microneedle patches so that after releasing their drug payload, they can also collect samples that could be used to monitor the progress of the treatment. Hyaluronic acid causes the needles to swell about tenfold after entering the skin, which allows them to absorb interstitial fluid containing biomolecules and immune cells from the skin.
Following patch removal, researchers can analyze samples to measure levels of regulatory T cells and inflammation markers. This could prove valuable for monitoring future patients who may undergo this treatment.
The researchers now plan to further develop this approach for treating alopecia, and to expand into other autoimmune skin diseases.
This story is republished courtesy of MIT News ( web.mit.edu/newsoffice/ ), a popular site that covers news about MIT research, innovation and teaching.
Explore further
Feedback to editors

Visual experiences unique to early infancy provide building blocks of human vision, study finds
5 hours ago

Study points to personalized treatment opportunities for glioblastoma

Research team introduces new tool to boost battle against childhood undernutrition

How herpes hijacks a ride into cells
6 hours ago

How the brain is flexible enough for a complex world, without being thrown into chaos

Researchers create AI model to understand how brain activity relates to illness

Study reveals need to review temperature control measures in hospitals to manage Legionella

'What was that?' How brains convert sounds to actions
8 hours ago

ERR-gamma 'trains' stomach stem cells to become acid-producing cells

Scientists make progress on new charged particle therapy for cancer
Related stories.

Causes of hair loss (alopecia) in children
Mar 25, 2024

Treating the 'root' cause of baldness with a dissolvable microneedle patch
Aug 12, 2021

Scientists develop a skin patch that painlessly delivers drugs into the body
Oct 18, 2023

Hair-raising research: Scientists find surprising link between immune system, hair growth
Jun 23, 2022

Microneedle patch delivers antibiotics locally in the skin
May 10, 2021

Skin patch could painlessly deliver vaccines, cancer medications in one minute
Aug 25, 2019
Recommended for you

Unobtrusive, implantable device could deepen our understanding of behavioral responses
9 hours ago

Using MRI, engineers have found a way to detect light deep in the brain

Flicker stimulation shines in clinical trial for epilepsy

'Smart' contact lenses could someday enable wireless glaucoma detection
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Switch language:

- Analyst Comment
Insmed’s brensocatib: A candidate for bronchiectasis treatment, closer to approval
Brensocatib is also in Phase II clinical trials for cystic fibrosis and chronic rhinosinusitis without nasal polyps.

- Share on Linkedin
- Share on Facebook

Insmed has been in the spotlight over the past few years for its pipeline agent, brensocatib, which has previously shown promising Phase II results, generating anticipation within the medical community ahead of the Phase III results for the treatment of bronchiectasis.
The positive outcomes from the Phase III trial could pave the way for regulatory approval, potentially transforming the therapeutic landscape for bronchiectasis, a disease that currently lacks approval of any therapeutic treatment globally.
Go deeper with GlobalData

LOA and PTSR Model - Brensocatib in Chronic Obstructive Pulmonary D...
Loa and ptsr model - brensocatib in cystic fibrosis, premium insights.
The gold standard of business intelligence.
Find out more
Related Company Profiles
Boehringer ingelheim international gmbh, chiesi usa inc.
Other therapies are also being developed and are currently competing to demonstrate promising results from their Phase II trials, including Boehringer Ingelheim’s BI-1291583, Sanofi ’s itepekimab, Chiesi’s CHF-6333, and Armata Pharmaceuticals’ APPA-02, as well as Renovion’s ascorbic acid.
The field may be considered attractive for pharmaceutical companies as there is a significant opportunity to acquire patient shares in a market that lacks approved therapies.
Brensocatib is an investigational anti-inflammatory molecule that inhibits the activity of neutrophil serine proteases (NSPs), as a dipeptidyl peptidase-1 reversible inhibitor, therefore suppressing neutrophils that contribute to the inflammatory environment present in non-cystic fibrosis bronchiectasis (NCFB) patients.
The previous Phase II study (WILLOW) demonstrated the efficacy of brensocatib in prolonging the time to first exacerbation and in reducing the frequency of exacerbations, through eliminating the numbers of multiple NSPs, including neutrophil elastase, proteinase 3, and cathepsin G, which have been previously implicated in the promotion of NCFB progression.
How well do you really know your competitors?
Access the most comprehensive Company Profiles on the market, powered by GlobalData. Save hours of research. Gain competitive edge.

Your download email will arrive shortly
Not ready to buy yet? Download a free sample
We are confident about the unique quality of our Company Profiles. However, we want you to make the most beneficial decision for your business, so we offer a free sample that you can download by submitting the below form
As of now, Phase III clinical trials are ongoing for the assessment of brensocatib’s efficacy, safety, and tolerability in patients with bronchiectasis, which were expected to have been completed by the first quarter of 2024, the results of which are highly anticipated by the medical community.
The outcomes will determine the future of brensocatib in the treatment landscape of bronchiectasis, as the presence of promising findings will progress the agent closer to market authorisation.
According to leading data and analytics company GlobalData ’s Sales and Forecast Database, brensocatib’s sales are anticipated to reach $1.2bn by 2030, subject to approval.
In addition to bronchiectasis, brensocatib is also in Phase II clinical trials for cystic fibrosis and chronic rhinosinusitis without nasal polyps, highlighting possible opportunities for Insmed to expand the agent’s label into these indications.
As expected, the competition in the bronchiectasis treatment landscape has increased over the years, with multiple pharmaceutical companies entering the race to obtain approval for their respective pipeline agents.
As the treatment landscape for bronchiectasis is currently governed by off-label therapies, there is an urgent need in the field for the development of advanced therapies that can target the disease at a cellular level, highlighting an opportunity for pharmaceutical companies to enter a market with potential for rapid expansion within the bronchiectasis field.

LOA and PTSR Model - Brensocatib in Chronic Obstructive Pulmonary Disease (COPD)
More relevant.
Can-Fite receives FDA IND clearance for Phase IIb MASH treatment trial
Neushen begins dosing for phase i trial of schizophrenia treatment, sign up for our daily news round-up.
Give your business an edge with our leading industry insights.
Sign up to the newsletter: In Brief
Your corporate email address, i would also like to subscribe to:.
I consent to Verdict Media Limited collecting my details provided via this form in accordance with Privacy Policy
Thank you for subscribing
View all newsletters from across the GlobalData Media network.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 10 May 2024
Behavioral evidence of impaired self-referential processing in patients with affective disorders and first-episode schizophrenia
- Yanli Zhao 1 ,
- Jiahua Xu 1 ,
- Jiangyue Hong 1 ,
- Xuejing Xu 2 ,
- Hongzhen Fan 1 ,
- Jinguo Zhang 1 ,
- Dong Li 1 ,
- Jingxu Chen 1 ,
- Yaxue Wu 1 ,
- Yanli Li 1 ,
- Yunlong Tan 1 &
- Shuping Tan 1
Scientific Reports volume 14 , Article number: 10754 ( 2024 ) Cite this article
Metrics details
- Bipolar disorder
- Cognitive neuroscience
- Human behaviour
- Schizophrenia
- Social neuroscience
Despite the critical role of self-disturbance in psychiatric diagnosis and treatment, its diverse behavioral manifestations remain poorly understood. This investigation aimed to elucidate unique patterns of self-referential processing in affective disorders and first-episode schizophrenia. A total of 156 participants (41 first-episode schizophrenia [SZ], 33 bipolar disorder [BD], 44 major depressive disorder [MDD], and 38 healthy controls [HC]) engaged in a self-referential effect (SRE) task, assessing trait adjectives for self-descriptiveness, applicability to mother, or others, followed by an unexpected recognition test. All groups displayed preferential self- and mother-referential processing with no significant differences in recognition scores. However, MDD patients showed significantly enhanced self-referential recognition scores and increased bias compared to HC, first-episode SZ, and BD. The present study provides empirical evidence for increased self-focus in MDD and demonstrates that first-episode SZ and BD patients maintain intact self-referential processing abilities. These findings refine our understanding of self-referential processing impairments across psychiatric conditions, suggesting that it could serve as a supplementary measure for assessing treatment response in first-episode SZ and potentially function as a discriminative diagnostic criterion between MDD and BD.
Introduction
Self-disturbance constitutes a salient transdiagnostic feature across a wide array of mental health conditions. The concept of the self is multifaceted, as posited by various theoretical frameworks 1 , 2 . Among its diverse dimensions, two central aspects are the pre-reflective and reflective selves 1 . The pre-reflective or minimal self facilitates an immediate sense of being the experiencer, existing in the present moment without temporal extension, while the reflective or narrative self encompasses the totality of one's identity, enabling comprehension of oneself within the continuum of time 3 .
In the present study, we specifically direct our attention to the reflective self dimension, operationalized through the self-reference effect (SRE) paradigm 4 in patients diagnosed with affective disorders and schizophrenia. The SRE task typically consists of dual stages: encoding and recognition. During the encoding stage, participants are tasked with judging whether a series of trait adjectives apply to themselves or another individual, thus engaging both self-reflection (often referred to as self-referential processing) and reflection on others (referred to as other-referential processing). Subsequently, an unanticipated recognition phase follows after a brief interval, where participants must discern which words were previously encountered during the encoding session. Empirical evidence from studies involving healthy adult populations has consistently demonstrated that recognition performance is significantly enhanced when items have been encoded under self-referential conditions relative to other-referential contexts, a phenomenon widely recognized as the SRE 5 . The manifestation of the SRE critically depends upon an individual's intact capacity for self-referential processing, i.e., the conscious cognitive appraisal of information relevant to the self 6 , 7 . Therefore, any impairment in the SRE can serve as a reliable behavioral marker indicative of compromised self-referential processing functionality.
Self-referential processing constitutes a fundamental aspect of social cognition and is pivotal for social adaptation 8 , 9 . Its impairment is pertinent to the manifestation of psychosis, maladaptive social functioning, and diminished illness awareness in schizophrenia (SZ) 10 , 11 . Major Depressive Disorder (MDD) is marked by an intensified self-focused cognitive pattern, i.e., the tendency for individuals to engage in a persistent and repetitive form of self-referential processing, frequently accompanied by a self-critical perspective and the growing empirical evidence supports the critical involvement of self-referential processing mechanisms across various stages of MDD 12 . Consequently, the study of self-referential processing in mental health disorders has attracted substantial interest from numerous scholars. Previous research on self-referential processing in affective disorders and schizophrenia has largely employed functional magnetic resonance imaging (fMRI) or event-related potential (ERP) methodologies to directly probe this process, offering neurobiological evidence for the anomalies observed in self-referential processing within these conditions 13 , 14 , 15 , 16 , 17 , 18 . Despite their value, these techniques are often time-consuming and demand higher participant compliance compared to behavioral tasks, which offer a more straightforward and expedient experimental avenue. However, there is currently a scarcity of behavioral research specifically addressing the SRE in psychiatric populations. Findings from prior studies 19 have indicated abolished SRE and compromised self-referential processing in SZ patients. Conversely, certain investigations have shown that first-episode SZ patients maintain intact SRE and self-referential processing abilities but exhibit deficits in mother-referential (intimate other) information processing when compared to healthy controls (HC) 20 . A small-scale study on bipolar disorder (BD) has revealed that impairments in self-referential and other-referential processing may be exclusive to BD patients with comorbid psychotic symptoms, whereas those without accompanying psychotic features exhibit intact self-referential processing capabilities 18 . More recent work has revealed an amplified self-referential advantage in MDD patients over HC, suggesting excessive self-focus in MDD 21 , although some studies do not report such augmentation 17 .
In summary, the current body of behavioral research exploring self-referential processing in schizophrenia and affective disorders is relatively sparse and exhibits inconsistencies. To our knowledge, few studies have systematically investigated the presence and nature of self-referential processing impairments in affective disorder and first-episode SZ patients using a common behavioral task. This lack of comparative data is crucial for enhancing diagnostic precision, differential diagnosis, and the design of efficacious therapeutic interventions in mental health disorders. Notably, previous literature suggests that the Chinese self-concept embodies an interdependent self where the self includes the mother 22 . Therefore, for a comprehensive understanding of self-disturbances in Chinese cultural contexts, it is essential to consider mother-referential processing. Addressing these gaps, the present study adopted an established SRE task 20 to explore whether patients with affective disorders and first-episode SZ exhibit impairments in interdependent self-representation, i.e., dysfunctional self- and/or mother-referential processing. Given that self-referential processing abnormalities in BD may be influenced by the presence or absence of psychotic symptoms 18 and the phase of the disorder (depressive or manic episode), we refrained from formulating specific hypotheses regarding BD outcomes. We anticipated that MDD patients would display better recognition scores in self- and/or mother-referential processing due to heightened self-focus 12 . Furthermore, we hypothesized that first-episode SZ patients would reveal dysfunction in intimate other-referential processing 20 .
Encoding phase
The results of the 4 (group:HC/MDD/BD/first-episode SZ) × 3 (condition: self/mother/other) repeated measures ANOVA on RT revealed a significant interaction between condition and group [ F (6286) = 2.30, P = 0.035; Table 1 ; Fig. 1 A]. Simple effects analyses disclosed that in the HC group, participants exhibited significantly longer RT during other-referential processing compared to mother-referential processing, P = 0.035; however, there was no significant difference between self-referential and other-referential processing, P = 0.471. Moreover, no significant difference in RT was observed between self- and mother-referential processing, P = 0.777. For MDD, BD, and first-episode SZ groups, RT were significantly longer during other-referential processing than during both self-referential and mother-referential processing (all P < 0.01). In contrast, no significant differences in RT were detected between self- and mother-referential processing within these clinical groups (all P > 0.1).
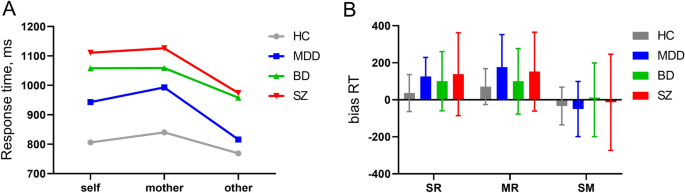
The behavioral performance during encoding phase. ( A ) The line graphs depict the response time (RT) among patients with first-episode schizophrenia (SZ), bipolar disorder (BD), major depressive disorder (MDD) and healthy controls (HC). In the context of mother-referential processing, RTs were longer for patients with MDD compared to HC. Under all three experiment conditions, both first-episode SZ and BD patients exhibited prolonged RTs relative to HC. Within self-referential processing conditions, MDD patients showed shorter RTs than first-episode SZ patients. When it came to other-referential processing, MDD patients demonstrated shorter RTs compared to first-episode SZ and BD patients. In patient cohorts, there is no discernible difference in RTs between the self-referential and mother-referential processing conditions; however, both consistently exhibit longer RTs than those recorded under the other-referential condition. In contrast, among the control group, a clear distinction exists such that RTs are significantly longer under the mother-referential condition relative to the other-referential condition alone. ( B ) The bar graphs depict the group differences of bias RT among first-episode SZ, BD, MDD and HC. The normal group had lower bias RT compared to first-episode SZ patients and MDD patients. ** p < 0.01; * p < 0.05. SM: self-mother, MR: Mother-other, SR: self-other.
In the context of self-referential processing, while there was no significant difference in RT between the HC and MDD groups ( P = 0.115), the controls had significantly shorter RT compared to those with BD and first-episode SZ (both P < 0.001). Additionally, the RT for the MDD group were significantly lower than those for the first-episode SZ group ( P = 0.021); notably, no significant difference was found between the BD and first-episode SZ groups ( P = 1.000). Under mother-referential processing conditions, the HC group displayed shorter RT than those in the MDD ( P = 0.071), BD ( P = 0.003), and first-episode schizophrenic groups ( P < 0.001); however, among the three patient groups, no significant differences in RT were observed (all P > 0.1). Regarding other-referential processing, no significant difference in RT was detected between the HC and MDD groups ( P = 1.000); however, the control group showed significantly shorter RT when compared to BD and first-episode schizophrenic groups (both P < 0.001). Furthermore, the RT for the MDD group were also significantly shorter than those for the BD and first-episode SZ groups (both P < 0.05). As before, no significant difference in RT emerged between the BD and first-episode SZ groups for other-referential processing ( P = 1.000).
The results of the repeated-measures ANOVA on bias RT revealed a significant main effect of condition [ F (2286) = 33.08, P < 0.001]. Further pairwise comparisons disclosed that the SM bias RT values were significantly shorter than those of SR bias and MR bias ( P -values for both comparisons were less than 0.001); however, no significant difference was found between SR bias and MR bias, P = 0.341. Moreover, a significant main effect of group was observed [ F (3, 143) = 3.17, P = 0.026; Table 1 ; Fig. 1 B]. Subsequent post-hoc tests indicated that the normal group had significantly lower bias RT compared to first-episode SZ patients ( P = 0.029) and MDD patients (marginally significant at P = 0.099). For all other pair-wise comparisons among groups, no statistically significant differences were detected with p-values being greater than or equal to 0.547.
Recognition phase
The results of a 4 (group: HC/MDD/BD/first-episode SZ) × 3 (condition: self/mother/other) repeated measures ANOVA on recognition scores revealed a significant interaction between condition and group [ F (6, 286) = 3.06, P = 0.006; Table 2 ; Fig. 2 A]. The simple effect analysis indicated that the recognition scores in all participants revealed significant difference across the three conditions: self-referential = mother-referential (pairwise P ≥ 0.257) > other-referential (pairwise P ≤ 0.004).
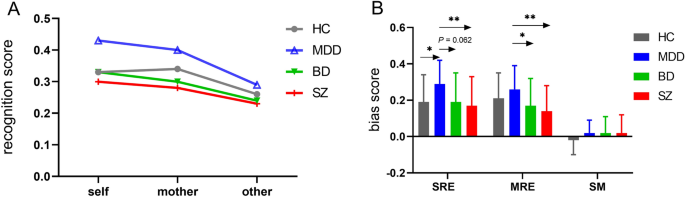
The behavioral performance during recognition phase. ( A ) The line graphs depict the recognition score among patients with first-episode schizophrenia (SZ), bipolar disorder (BD), major depressive disorder (MDD), and healthy controls (HC). All participants, including HC and patients with MDD, BD, and first-episode SZ, displayed both self-referential and mother-referential bias in recognition memory, characterized by a pattern where scores for self- and mother-referenced items were higher than those for other-referenced items (self-recognition = mother-recognition > other-recognition). Additionally, participants with MDD exhibited significantly elevated self-referential recognition scores compared to HC, first-episode SZ, and BD patients. While MDD patients outperformed first-episode SZ and BD patients in recognizing information related to their mothers, no statistically discernible difference was found when comparing MDD patients to HC. ( B ) The bar graphs depict the group differences of bias score among first-episode SZ, BD, MDD, and HC. Patients with MDD exhibit higher SRE bias scores compared to those with first-episode SZ, BD, and HC. Meanwhile, Patients with MDD exhibit higher MRE bias scores compared to those with first-episode SZ and BD. ** p < 0.01; * p < 0.05. SM: self-mother, MRE: Mother-referential effect, SRE: self-referential effect.
Moreover, it was found that MDD patients demonstrated higher self-referential recognition scores compared to first-episode SZ ( P = 0.004), BD ( P = 0.064), and HC participants ( P = 0.051). Regarding maternal-referential recognition scores, MDD patients scored significantly higher than those with first-episode SZ ( P = 0.001) and BD ( P = 0.029), yet no significant difference was observed when compared to the HC ( P = 0.490). Additionally, a lack of statistically discernible disparities in mother-referential processing recognition performance has been observed among individuals diagnosed with BD relative to their counterparts with first-episode SZ, and this pattern persists when contrasting each patient cohort against a matched group of HC (all [ P -values being ≥ 0.256). No significant differences in other-referential recognition scores were detected among the four groups, with all p -values being ≥ 0.285.
The results of the repeated measures ANOVA on bias score revealed a significant interaction between condition and group [ F (6286) = 4.20, P = 0.003; Table 2 ; Fig. 2 B]. The results from simple effects analyses revealed that patients with MDD exhibited significantly higher self bias compared to individuals with first-episode SZ ( P = 0.004), as well as those with BD ( P = 0.062) and HC ( P = 0.036). Concurrently, MDD patients also displayed a mother bias that was elevated in comparison to first-episode SZ ( P = 0.002) and BD ( P = 0.031) patients; However, no statistically significant difference was found when contrasting MDD patients against the normal control group ( P = 0.453). Furthermore, for both self and mother biases, no other group comparisons reached statistical significance as all corresponding P -values exceeded the threshold of 0.304. Moreover, there were no discernible statistically significant differences among any two groups concerning the differential scores under self-mother referential conditions, referred to as the SM bias, with all P -values exceeding the minimum threshold of 0.269. Additionally, for all participants, the self bias and mother bias values were consistently higher than the SM bias values (all p -values < 0.001), and no statistically significant differences were observed between the self bias and mother bias scores (all P -values ≥ 0.257).
To the best of our understanding, this research pioneers the use of a unified behavioral paradigm to systematically and comparatively assess potential impairments in self-referential processing among first-episode SZ, BD, and MDD patients. The study's outcomes reveal that individuals across all three patient groups—first-episode SZ, BD, and MDD—exhibit comparable SRE and MRE patterns to those seen in HC, indicative of preserved preferential processing for information pertaining to both the self and mother domains. Furthermore, akin to HC participants, the self-conceptualization in patients also includes a mother-referential component. Notably, this investigation has revealed unique profiles of self-referential processing abilities across distinct psychiatric conditions, uncovering novel insights that deviate from previous findings in the literature.
Firstly, this study demonstrates a significantly heightened self-recognition and augmented SRE bias in MDD patients when compared to HC. However, no significant variations were observed between these groups concerning recognition performance for mother-referential or other-referential information, suggesting that MDD individuals exhibit a selectively amplified memory preference specifically for self-related content. This observation corroborates earlier behavioral research on MDD 21 as well as prior fMRI data indicating abnormal hyperactivity within the anterior cingulate cortex during self-referential processing in MDD 12 . It is pertinent to mention that some studies have reported inconclusive results with no discernible differences in self-relevant information retrieval between acute or remitted MDD patients and HC 17 . The divergent findings might stem from the utilization of disparate behavioral instruments, particularly free recall tasks as opposed to the recognition tasks employed herein.
During the encoding phase, our analysis unveiled longer RTs among MDD patients under mother-referential conditions, coupled with increased RT biases for SR, MR, and SM relative to HC. Importantly, no significant difference was detected in RTs for tasks involving other-referential processing between the two cohorts, potentially implying an enhanced duration spent elaborating or organizing self- and mother-related information in MDD patients.
Secondly, our results indicate that there are no significant differences in any bias measures or self- and mother referential recognition between first-episode SZ patients and HC, suggesting an intact SRE and interconnected self-concept at the early stages of SZ. This contrasts with previous research 20 that suggested preserved fundamental self-function but altered relational aspects of self in initial SZ episodes. The present study is the first to provide empirical evidence that not all individuals experiencing a first episode of schizophrenia show deficits in processing information related to intimate others, specifically mother-referential processing. Earlier studies have shown a detrimental association between recognition performance in tasks involving self- and mother-referential processing and total PANSS scores among first-episode SZ patients 20 , pointing towards a relationship where more severe symptoms are linked with poorer recognition under both self- and mother-related conditions. In this particular investigation, the symptom severity as measured by the PANSS total score for the first-episode SZ group was notably lower (51.93 ± 25.64) compared to prior literature (75.90 ± 10.41). This reduced symptomatology could potentially explain the maintenance of unimpaired self- and mother-referential processing capabilities found here.
Consistent with earlier findings 16 , 20 , 23 , during the encoding phase, behavioral data from this study demonstrated extended RTs across all experimental conditions for first-episode SZ patients relative to HC, confirming compromised processing speed in both early-stage and chronic SZ.
Thirdly, akin to the findings in first-episode SZ patients, this study reveals that individuals with BD also exhibit intact self-referential and mother-referential processing abilities, which contrasts with prior research 18 suggesting impaired self-referential processing in BD relative to HC. Concurrently, earlier studies have indicated a negative correlation between self-referential bias scores and manic symptomatology in BD, meaning that more severe manic symptoms are associated with a greater degree of impairment in self-referential processing 18 .
In the present sample, BD participants were predominantly experiencing depressive episodes characterized by heightened depressive symptom severity (HAMD score: 20.67 ± 11.37 versus 6.2 ± 8.61), whereas past investigation 18 involved subjects with more profound manic symptoms (YMRS score: 18.2 ± 10.53 compared to 8.00 ± 5.99). This difference in patient profiles may underlie the inconsistency between these two sets of findings. Moreover, previous literature 18 has suggested that impairments in self-referential processing could be exclusive to BD cases accompanied by psychotic features. However, despite the presence of psychotic symptoms in our BD cohort as measured by a PANSS total score of 48.76 ± 8.80, no deficits in self-referential processing were detected. This implies that the relationship between self-referential processing capabilities and psychotic symptoms in BD might not be as strong as previously thought, and instead suggests that the phase of illness (i.e., manic or depressive episode) and the severity of related symptoms play a more substantial role. These observations underscore the need for further research to elucidate the complex relationship between BD's different phases, symptom severity, and self-referential processing functions. Future studies should delve deeper into this issue to clarify these dynamics.
Consistent with past literature 18 , BD patients displayed prolonged RTs across all experimental conditions during the encoding phase compared to HC, indicative of compromised information processing speed in this population.
Lastly, patients with MDD exhibited significantly superior recognition performance and corresponding bias indices for both self- and mother-referential processing when compared against those diagnosed with first-episode SZ and BD.
Notably, during the encoding phase of self-referential processing, individuals in the first-episode SZ group displayed longer RTs relative to their MDD counterparts. Furthermore, both first-episode SZ and BD patient groups demonstrated a more extended engagement duration when engaging in tasks requiring other-referential processing as compared to the MDD group. These findings suggest that at early stages of SZ and BD patients exhibit potentially reduced cognitive efficiency compared to MDD patients.
The clinical implications arising from this study are multifaceted. Initially, the present research enhances our comprehension of rumination symptoms by demonstrating that individuals with MDD exhibit a pronounced self-referential advantage effect, spending more time and engaging more deeply during encoding and retrieval of information pertaining to themselves. Secondly, this work, in conjunction with prior literature, underscores the heterogeneity among first-episode SZ patients regarding self-referential processing impairments. The variability observed may be linked to the severity of symptoms experienced by these patients. Consequently, assessing self-referential processing capacity could serve as a potential metric for gauging the effectiveness of pharmacological interventions in early-stage schizophrenia. Thirdly, while rumination has been recognized as a prevalent symptom across both BD's depressive and manic phases, as well as MDD 24 , 25 , our findings suggest distinct patterns of impairment in self-referential processing between these two psychiatric conditions. Notwithstanding the observation that BD participants in our study manifested more severe depressive symptoms than those in the depression group (mean scores: 20.67 ± 11.37 versus 15.57 ± 6.13), no impairments were detected in their self-referential processing abilities. The present study's findings, alongside previous research findings 18 , suggest that self-referential processing may serve as a potential adjunctive biomarker for differentiating between BD and MDD in diagnostic settings.
The present study has several limitations that warrant consideration. Firstly, the inherent cognitive disparities between patients and HC are substantiated by our findings, where both first-episode SZ and BD participants exhibited significantly prolonged RTs across all three experimental conditions during the encoding phase as compared to normal controls, indicative of compromised basic information processing in these patient populations. However, a notable distinction emerged during the recognition phase; while differential recognition scores were observed exclusively under self- and/or mother-related conditions for patients, no significant differences transpired in other-referential processing between the patient groups and normal controls. This observation suggests, to some extent, that the obtained results do not solely emanate from fundamental cognitive capacity discrepancies between patients and controls. In future research endeavors, it is crucial to incorporate a comprehensive cognitive assessment within the study design to more effectively control for potential confounding variables. Another limitation herein is the lack of consideration for the potential influence exerted by varying clinical symptomatology on the impairment patterns of self-referential processing in BD patients. Addressing this knowledge gap is essential for refining our understanding of the disorder-specific expressions of self-referential processing deficits. Lastly, the results of this study should be interpreted with caution, and future research necessitates the replication and validation of our findings in larger, more extensive cohorts.
In summary, the present study provides preliminary evidence for unique patterns of self-referential processing abilities in MDD, BD, and first-episode SZ. It emphasizes the potential different roles that self-referential processing may have in evaluating treatment response and aiding in discriminative diagnosis among these conditions.
Material and methods
The calculation of sample size.
A power analysis was conducted using the G*Power software 26 to ascertain the requisite sample sizes necessary for discerning significant differences between HC and patient cohorts with BD, first-episode SZ, and MDD. The principal outcome measure in these calculations was the recognition scores obtained from previously reported self-referential processing tasks 18 , 20 , 21 , which exhibited the following means and standard deviations: HC versus BD: 0.45 ± 0.03 vs. 0.26 ± 0.03; HC versus SZ: 0.47 ± 0.15 vs. 0.35 ± 0.18; and HC versus MDD: 0.36 ± 0.13 vs. 0.44 ± 0.13. With an alpha level set at α = 0.05 to maintain statistical significance, and a desired power (1 − β) of 0.90 to ensure adequate statistical power, the estimated minimum required sample sizes were determined as follows: 11 participants for the BD group, 33 participants for the first-episode SZ group, and 44 participants each for both the MDD group and the HC group.
Participants
In the current study, guided by the aforesaid power analysis and sample size estimation standards, we recruited 41 patients with first-episode SZ, 33 individuals diagnosed with BD, and 44 participants suffering from MDD from Beijing HuiLongGuan Hospital. Concurrently, 44 HC were enrolled through local community advertisements.
Diagnoses of first-episode SZ, BD, and MDD were established according to the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) criteria 27 , with each diagnosis confirmed by both an attending psychiatrist and subsequently verified by a senior psychiatrist.
For the first-episode SZ cohort, additional inclusion criteria included: (1) experiencing their inaugural episode of illness, operationally defined as either their initial treatment contact or an illness duration not exceeding three years since symptom onset; (2) being antipsychotic-naive, meaning no prior exposure to antipsychotics, or having minimal exposure quantified as a cumulative treatment period of ≤ 2 weeks. Regarding BD participants, they had to be in the acute phase or remission stage of a depressive episode. Exclusionary criteria applied specifically to those in a current manic episode or mixed affective state. Common exclusion criteria for both SZ and BD groups encompassed conditions such as overt brain injury, diagnosed neurological disorders, intellectual disability ascertained by an IQ score below 70, substance abuse or dependence within the last six months, and receipt of electroconvulsive therapy within the preceding six months. First-episode SZ and BD patients were drawn from the inpatient population. Enrollment was carried out after a well-defined period of relative clinical stability post-hospitalization, ensuring that SZ subjects displayed sufficient communicative competence and had comprehended the nature and implications of our experimental protocols to provide fully informed consent. This interval between hospital admission and study enrollment consistently averaged approximately 2–3 weeks.
For outpatient MDD participants, specific inclusion criteria required them to exhibit mild to moderate depression, evidenced by a Hamilton Depression Scale 17 items (HAMD-17) score of ≥ 7 but < 24 points 28 . Exclusions for MDD patients included: (1) meeting DSM-IV axis I diagnostic criteria for any other mental disorder; (2) presenting with suicidal tendencies or scoring item 3 ≥ 3 on the relevant assessment tool; (3) showing psychotic symptoms or psychomotor retardation/hyperactivity symptoms.HC were free from DSM-IV Axis I disorders, had no history of substance abuse or dependence within the previous six months, and lacked first-degree relatives with a history of psychotic or affective disorders.
All participants were aged between 18 and 55 years, had completed at least 12 years of education, and possessed normal or corrected-to-normal visual acuity. Each participant voluntarily gave informed consent and received compensation for their participation. The entire research process strictly adhered to the ethical principles outlined in the Declaration of Helsinki (1964) and its subsequent revisions. Ethical clearance was granted by the Research Ethics Committee of Beijing HuiLongGuan Hospital on July 5th, 2016, under the assigned ethical approval number 2016–26.
In the overall study group, four MDD participants did not complete the full experimental procedure. Moreover, five MDD patients and three HC were excluded from statistical analyses due to their exceptionally high educational attainment that necessitated their removal during matching procedures to maintain homogeneity. Additionally, technical issues led to incomplete data for three HC, resulting in their exclusion. Therefore, the final dataset consisted of 41 first-episode SZ patients, 33 BD patients, 35 MDD patients, and 38 HC for subsequent statistical evaluations. No significant differences in age, education level, or sex distribution were detected across the four diagnostic categories. Clinical symptom ratings were carried out by a panel of four attending psychiatrists, achieving acceptable inter-rater reliability (kappa = 0.83). Symptom severity in SZ patients was evaluated using the Positive and Negative Syndrome Scale (PANSS) 29 , BD patients were assessed using both the Hamilton Depression Rating Scale (HAM-D) and the Young Mania Rating Scale (YMRS) 30 , while MDD patients were rated using the HAM-D and the Hamilton Anxiety Rating Scale (HAM-A) 31 . A comprehensive overview of the demographic and clinical characteristics of the study participants is presented in Table 3 .
The SRE task
We used the SRE task previously described by our research group 20 (Fig. 3 ). Briefly, the task consisted of two stages: an encoding phase and a recognition phase. In the encoding phase, the participants were asked to evaluate whether a certain personality-trait adjective presented in Chinese was appropriate to describe themselves, their mothers, and ‘other’, that is a well-known public figure (Hu Jintao, former President of the People's Republic of China). A total of 180 words were randomly selected for the encoding phase and there were 60 words in each condition (30 positive and 30 negative words). Each trial began with a gaze crossover of 600–1000 ms, followed by a “cue” word (self, mother, or other) above the adjective feature for a maximum of 4000 ms. Participants were required to respond as quickly and accurately as possible by pressing buttons on the response box with their left and right index fingers. The assignment of left and right button presses was counterbalanced across all participants. The target word disappeared when the participant indicated their response, and the next trial began 1000 ms later.
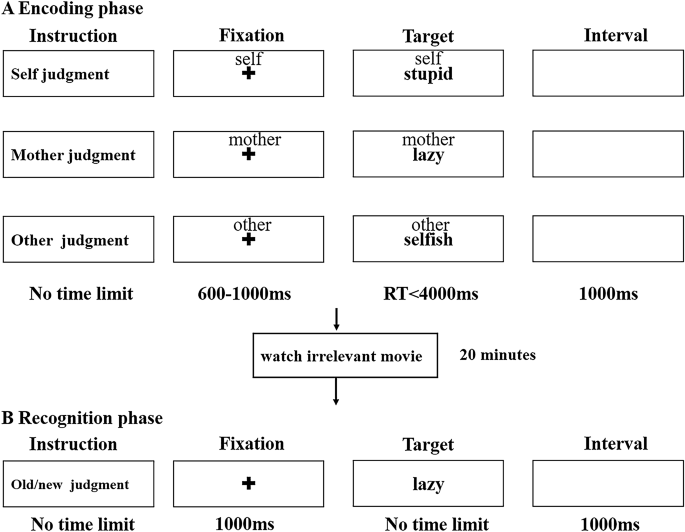
The general procedure of Self-referential effect task. An illustration of general procedure of self-referential effect task. Participants were instructed to finish encoding phase and recognition phase separated by irrelevant movie watching.
After the encoding session, the participants were asked to watch an unrelated video for 20 min, after which they completed an unexpected new/old word recognition test. All 180 words were included, along with 120 new characteristic adjectives. The participants were required to determine whether certain words had been present during the encoding phase.
Behavioral measures
E-Prime software (Version 3.0, Psychology Software Tools, Inc., Pittsburgh, PA, USA) was used for stimulus display and data acquisition. Data analyses were conducted using SPSS Statistics 20.0 (IBM, USA).
During the encoding phase, apart from the average RT per task condition, we calculated the differential RT by subtracting the RT under the other-referential condition from the corresponding RT in the self-referential (yielding SR bias RT) and mother-referential conditions (yielding MR bias RT), as well as the difference between the self-referential and mother-referential RT (designated as SM bias RT).
During the recognition phase, we adhered to signal detection theory as previously established 4 , 7 , 9 to operationalize two pivotal indices: the first being the sensitivity index d', which is computed as the difference between the hit rate and false alarm rate; a higher d' signifies superior recognition performance, indicating an enhanced ability to discriminate signals from noise. The second critical variable was the response bias or criterion value. In the present investigation, we derived three unique response bias scores based on these calculations: the SRE bias score, the Mother-Referential Effect (MRE) bias score, and the Self-Mother (SM) bias score. These were respectively defined as the difference between the “self-referential d” and the “other-referential d” (“self-referential d” minus “other-referential d”), the difference between the “mother-referential d” and the “other-referential d” (“mother-referential d” minus “other-referential d”), and the difference between the “self-referential d” and the “mother-referential d” (“self-referential d” minus “mother-referential d”).
In the context of behavioral data collected during the encoding phase, a 4 (group: HC, MDD, BD, and first-episode SZ) × 3 (encoding condition: self-referential, mother-referential, and other-referential) repeated-measures analysis of variance (ANOVA) was employed to meticulously examine RT. The independent between-subjects factor reflected group membership, while the within-subjects factor denoted the different encoding contexts. This rigorous analytical approach was specifically tailored to discern potential interaction effects between diagnostic groups and various encoding conditions.
Furthermore, a separate 4 × 3 repeated measures ANOVA was conducted to scrutinize RT biases corresponding SR bias RT, MR bias RT, and SM bias RT. This investigation aimed at revealing any diagnostic category-specific variations in the distinct patterns of bias that emerged during the encoding process.
During the subsequent recognition phase, analogous repeated measures ANOVAs with an identical design as used in the encoding stage were applied independently to recognition scores and bias scores. Throughout this study, statistical significance was set at α = 0.05. Whenever significant interactions were detected, post-hoc analyses were conducted using simple effects models, accompanied by appropriate adjustments for multiple comparisons to mitigate family-wise error rate.
Data availability
The raw data and/or analyzed datasets of the present study will be made available by the corresponding author on reasonable request.
Gallagher, I. Philosophical conceptions of the self: Implications for cognitive science. Trends Cogn Sci 4 , 14–21 (2000).
Article CAS PubMed Google Scholar
Damasio, A. Feelings of emotion and the self. Ann. N. Y. Acad. Sci. 1001 , 253–261 (2003).
Article ADS PubMed Google Scholar
Esslen, M., Metzler, S., Pascual-Marqui, R. & Jancke, L. Pre-reflective and reflective self-reference: A spatiotemporal EEG analysis. Neuroimage 42 , 437–449 (2008).
Article PubMed Google Scholar
Mu, Y. & Han, S. Neural oscillations involved in self-referential processing. Neuroimage 53 , 757–768 (2010).
Symons, C. S. & Johnson, B. T. The self-reference effect in memory: A meta-analysis. Psychol. Bull. 121 , 371–394 (1997).
van der Meer, L., Costafreda, S., Aleman, A. & David, A. S. Self-reflection and the brain: A theoretical review and meta-analysis of neuroimaging studies with implications for schizophrenia. Neurosci. Biobehav. Rev. 34 , 935–946 (2010).
Kelley, W. M. et al. Finding the self? An event-related fMRI study. J. Cogn. Neurosci. 14 , 785–794 (2002).
Shad, M. U. et al. Neurobiology of self-awareness in schizophrenia: An fMRI study. Schizophr. Res. 138 , 113–119 (2012).
Article PubMed PubMed Central Google Scholar
Philippi, C. L., Duff, M. C., Denburg, N. L., Tranel, D. & Rudrauf, D. Medial PFC damage abolishes the self-reference effect. J. Cogn. Neurosci. 24 , 475–481 (2012).
Modinos, G., Renken, R., Ormel, J. & Aleman, A. Self-reflection and the psychosis-prone brain: An fMRI study. Neuropsychology 25 , 295–305 (2011).
Murphy, P., Bentall, R. P., Freeman, D., O’Rourke, S. & Hutton, P. The paranoia as defence model of persecutory delusions: A systematic review and meta-analysis. Lancet Psychiatry 5 , 913–929 (2018).
Nejad, A. B., Fossati, P. & Lemogne, C. Self-referential processing, rumination, and cortical midline structures in major depression. Front. Hum. Neurosci. 7 , 666 (2013).
Lemogne, C. et al. Self-referential processing and the prefrontal cortex over the course of depression: A pilot study. J. Affect. Disord. 124 , 196–201 (2010).
Holt, D. J. et al. An anterior-to-posterior shift in midline cortical activity in schizophrenia during self-reflection. Biol. Psychiatry 69 , 415–423 (2011).
Blackwood, N. J. et al. Persecutory delusions and the determination of self-relevance: An fMRI investigation. Psychol. Med. 34 , 591–596 (2004).
Zhao, Y. et al. Neural correlates of the abolished self-referential memory effect in schizophrenia. Psychol. Med. 44 , 477–487 (2014).
Article ADS CAS PubMed Google Scholar
Shestyuk, A. Y. & Deldin, P. J. Automatic and strategic representation of the self in major depression: Trait and state abnormalities. Am. J. Psychiatry 167 , 536–544 (2010).
Zhao, Y. et al. Behavioral and neural correlates of self-referential processing deficits in bipolar disorder. Sci. Rep. 6 , 24075 (2016).
Article ADS CAS PubMed PubMed Central Google Scholar
Harvey, P. O., Lee, J., Horan, W. P., Ochsner, K. & Green, M. F. Do patients with schizophrenia benefit from a self-referential memory bias. Schizophr. Res. 127 , 171–177 (2011).
Zhao, Y. et al. Impaired emotional self-referential processing in first-episode schizophrenia. Front. Psychiatry 12 , 591401 (2021).
Liu, P. et al. Behavioral and electrophysiological analyses of self-referential neural processing in major depressive disorder. Asian J. Psychiatr. 79 , 103401 (2023).
Zhang, L. et al. In search of the Chinese self: An fMRI study. Sci. China C Life Sci. 49 , 89–96 (2006).
Jimenez, A. M., Lee, J., Wynn, J. K. & Green, M. F. The neural correlates of self-referential memory encoding and retrieval in schizophrenia. Neuropsychologia 109 , 19–27 (2018).
Ghaznavi, S. & Deckersbach, T. Rumination in bipolar disorder: Evidence for an unquiet mind. Biol. Mood Anxiety Disord. 2 , 2 (2012).
Pavlickova, H. et al. The dynamics of mood and coping in bipolar disorder: Longitudinal investigations of the inter-relationship between affect, self-esteem and response styles. PLoS One 8 , e62514 (2013).
Faul, F., Erdfelder, E., Lang, A. G. & Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39 , 175–191 (2007).
APA. Diagnostic and Statistical Manual of Mental Disorders 4th edn. (American Psychiatric Association, 1994).
Google Scholar
Hamilton, M. Development of a rating scale for primary depressive illness. Br. J. Soc. Clin. Psychol. 6 , 278–296 (1967).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13 , 261–276 (1987).
Young, R. C., Biggs, J. T., Ziegler, V. E. & Meyer, D. A. A rating scale for mania: Reliability, validity and sensitivity. Br. J. Psychiatry 133 , 429–435 (1978).
Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 32 , 50–55 (1959).
Woods, S. W. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J. Clin. Psychiatry 64 , 663–667 (2003).
Download references
Acknowledgements
This research was supported by Beijing High Level Health Technology Talent Construction Project Training Plan (Discipline Leader -02-03; Subject Backbones -02-09).
Author information
Authors and affiliations.
Beijing HuiLongGuan Hospital, Peking University HuiLongGuan Clinical Medical School, Beijing, 100096, People’s Republic of China
Yanli Zhao, Jiahua Xu, Jiangyue Hong, Hongzhen Fan, Jinguo Zhang, Dong Li, Jingxu Chen, Yaxue Wu, Yanli Li, Yunlong Tan & Shuping Tan
Temple University, Philadelphia, PA, 19122, USA
You can also search for this author in PubMed Google Scholar
Contributions
The study was conceived and designed by Y.L.Z. and S.P.T. The analysis was carried out by Y.L.Z. and J.Y.H. Y.L.Z. took the lead in drafting the initial version of the manuscript. Critical revisions were provided by J.H.X. and S.P.T., while X.J.X., J.G.Z., D.L., J.X.C., Y.X.W., and Y.L.L. significantly contributed to participant recruitment and the acquisition of behavioral and clinical data. H.Z.F. and Y.L.T. offered crucial insights into data interpretation. All authors participated in the final review process, providing approval for the submission and publication of this manuscript.
Corresponding author
Correspondence to Shuping Tan .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zhao, Y., Xu, J., Hong, J. et al. Behavioral evidence of impaired self-referential processing in patients with affective disorders and first-episode schizophrenia. Sci Rep 14 , 10754 (2024). https://doi.org/10.1038/s41598-024-60498-5
Download citation
Received : 05 May 2023
Accepted : 23 April 2024
Published : 10 May 2024
DOI : https://doi.org/10.1038/s41598-024-60498-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Self-reference effect
- Major depressive disorder
- Self-referential processing
- Mother-referential processing
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Share full article
Advertisement
Supported by
N.Y. Prisons Holding Mentally Ill People in Solitary, Lawsuit Says
A complaint filed by the Legal Aid Society and others accuses the state prison system of holding mentally ill and disabled people in isolation despite a law against the practice.

By Jan Ransom
Each time Stephanie Peña was placed alone in a prison cell the length and width of a parking spot, she could feel herself losing it.
Ms. Peña, 23 and living with post-traumatic stress and antisocial personality disorders, would recoil from the bloodstained mattress and the feeling of pests crawling over her as she slept. Desperate, she sometimes tried to harm herself just so her guards would let her out.
When New York banned the use of long-term solitary confinement in its prisons and barred the practice entirely for certain people, including mentally ill prisoners like Ms. Peña, it was hailed as a groundbreaking measure that would fundamentally change life behind bars.
But since the law took effect two years ago, prison officials have refused to implement it and have continued to hold incarcerated people with disabilities in solitary and in cells in specialized disciplinary units for most of the day, according to a class-action lawsuit filed on Tuesday in State Supreme Court in Brooklyn.
Ms. Peña is one of hundreds of prisoners who have been held in isolation or in solitary-like conditions for more than 17 hours at a time in violation of the new state law, according to the lawsuit filed by the Legal Aid Society, Disability Rights Advocates and the law firm Winston & Strawn.
“Solitary confinement is extremely harmful for people generally and, of course, for people with disabilities specifically,” said Stefen Short, a lawyer working on behalf of the Prisoners’ Rights Project of the Legal Aid Society. “Really what the agencies are doing here is flouting the will of the Legislature and by extension flouting the will of the people.”
Over the past two years, state legislators and oversight agencies have sounded the alarm in reports and letters to the New York Department of Correction and Community Supervision and the state’s Office of Mental Health, warning that the agencies were violating the law.
On any given month from May 2022 to April of this year, more than a quarter of the inmates in solitary had a diagnosed mental illness, according to the lawsuit, in violation of state law.
Representatives of the state prison system and Office of Mental Health said they could not discuss the suit because the agencies do not comment on pending litigation.
A spokesman for the prison system said officials had updated internal policies and added procedures last year to ensure that those held in segregated confinement meet all of the requirements under state law.
A spokesman for the Office of Mental Health, Justin Mason, said the department’s “top priority is ensuring that all New Yorkers have access to adequate mental health care, including those involved with the criminal justice system.”
He said the agency “is committed to treating those individuals entrusted to its care in the most clinically appropriate setting that is most likely to help them onto the path toward recovery.”
For years, advocates for incarcerated people had sought restrictions on the use of solitary confinement, citing research showing that prolonged isolation exacerbates mental illness, increases the risk of self-harm and suicide and leads to higher rates of death after release.
A survey in 2005 found that nearly half of the suicides in New York prisons had occurred in solitary, which the lawsuit described as “among the most extreme form of punishment which can be inflicted on human beings short of killing them.”
In 2021, legislators approved the law over fierce objection from the unions representing correction staff. The law barred the officials from placing any person with any disability in segregated confinement for any amount of time, and it also restricted the maximum length of time a person could be held in isolation to no more than 15 consecutive days.
Before the law was enacted, thousands of prisoners had been held in solitary or kept in their cells for 22 or 23 hours a day, sometimes for months or even years on end. They were forced to eat alone and prohibited from seeing other prisoners, working prison jobs or attending programs and other rehabilitative activities.
The new law required the state to create specialized disciplinary units for people with mental illness where they would receive intensive programming to address their behaviors, including at least seven hours of out-of-cell time. But the lawsuit said that people have instead been held in these cells for most of the day and with little access to services, in what amounted to solitary confinement “by another name.”
Prisoners in Residential Mental Health Treatment units were disciplined at the highest rates in the system, the lawsuit said, and they were assigned, on average, eight times more time in segregated confinement than the prison population as a whole.
Eric Lee, one of the nine plaintiffs named in the lawsuit, had been diagnosed with bipolar disorder and schizophrenia as a child. But Mr. Lee, 32, who is serving 23 years to life in prison for murder and robbery, had been held in solitary confinement at the Shawangunk Correctional Facility for about two weeks. Later, at other prisons, he was kept in cells in alternative disciplinary units for 17 hours a day for months at a time.
During one stint in isolation while at Attica Correctional Facility, Mr. Lee, who had become desperate and paranoid, attempted to kill himself.
“Staring at a blank wall all day everyday just makes me want to give up,” he said, according to the lawsuit.
The Department of Corrections and Community Supervision, which operates the state’s 44 prisons, and the Office of Mental Health, which provides psychiatric services to thousands of prisoners, have also relied on policies that ensure some people who otherwise would have been shielded from solitary-like confinement were held under those conditions.
For example, the Office of Mental Health allows people who it does not deem to be “seriously mentally ill” to be held in solitary confinement. The agency has adopted a very narrow definition of serious mental illness, limiting it to just a small number of diagnoses such as schizophrenia and bipolar disorder, rather than the full spectrum of mental health disabilities that are covered under the law, the lawsuit said.
Other psychiatric problems like post-traumatic stress disorder, generalized anxiety disorder and adjustment disorder are not considered serious mental illness, and prisoners with those conditions are not protected under the mental health agency’s interpretation of the law, the suit says.
In fact, despite her diagnoses, Ms. Peña had been held in solitary confinement several times since being sent to the Albion Correctional Facility in 2022. On several occasions, she said, she was disciplined for behavior that stemmed from her mental illness. But she should never have been held in solitary in the first place, the lawsuit said.
“It’s just seriously affected me,” Ms. Peña, a plaintiff in the case who was convicted of attempted robbery and remains in custody, said in a response sent through her lawyer. “I will never be the same.”
People with physical, medical and sensory disabilities have also been held illegally in solitary, the lawsuit said.
One man, Maurice Anthony, 42, is legally blind and was approved by the correction department to receive accommodations for his disability. Even so, he has been held in isolation for as many as 23 hours a day for various periods over the past three years. The only recreation he was permitted was by himself in a small semi-outdoor portion of his cell. More recently he has only been allowed one hour a day in a small 10-by-10 foot cage.
Isolation, Mr. Anthony said, is like being kept in a coffin.
Research has shown that solitary can be especially harmful for prisoners like Mr. Anthony, the lawsuit said, because it can worsen vision problems.
The lawsuit seeks a court injunction to prohibit prison officials from placing people with any type of disability in solitary, and to bar the correction department and the mental health agency’s use of policies that narrow the number of people protected under the law.
“They’ve been causing unimaginable harms,” said Joshua Rosenthal, supervising attorney with the nonprofit Disability Rights Advocates.
“There is no rationale,” he added, that the state could give “that would justify the torture of people with disabilities in this way.”
Jan Ransom is an investigative reporter on the Metro desk focusing on criminal justice issues, law enforcement and incarceration in New York. More about Jan Ransom
Politics in the New York Region
A Thorny Mayoral Race: Zellnor Myrie, an Afro-Latino state senator from Brooklyn known for backing progressive causes, announced that he is moving to challenge Mayor Eric Adams in next year’s Democratic primary in New York City.
Special House Election: Timothy Kennedy, a Democratic New York State senator, easily won a special House election to replace a retiring congressman in western New York, narrowing the Republican majority in Washington.
A $237 Billion Budget: Gov. Kathy Hochul and New York City emerged as two of the winners from a budget process that blew past the April 1 deadline. Here’s a look at how things went .
Concessions From N.Y. Lawmakers: Hochul used the budget to wedge in contentious issues like extending Adams’s control over New York City schools.
More Scrutiny of Judges: A group that helped thwart the confirmation of Hochul’s choice to lead New York’s highest court last year is pushing elected officials to more closely scrutinize judicial nominees .

IMAGES
VIDEO
COMMENTS
2.1. Dopaminergic Hypothesis. The dopaminergic hypothesis of schizophrenia is the fundament of the investigation and treatment of schizophrenia [].The first version of this hypothesis stressed the role of the excess of dopamine but it was developed into an idea linking prefrontal hypodopaminergia and striatal hyperdopaminergia and then to the current aberrant salience hypothesis [].
Introduction. The goal of this guideline is to improve the quality of care and treatment outcomes for patients with schizophrenia, as defined by the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (American Psychiatric Association 2013).Since publication of the last full practice guideline (American Psychiatric Association 2004) and guideline watch (American Psychiatric ...
For treatment-resistant schizophrenia, 15/15 CPGs recommended clozapine. Only 7/19 (38.8%) CPGs included a treatment algorithm. ... Italian guidelines 41, NICE 34, NJDMHS 32, Schizophrenia Patient ...
This paper reports a review of outcomes in schizophrenia in the twenty‐first century and is an extension of the work undertaken by the late Dr ... Sustained favorable long‐term outcome in the treatment of schizophrenia: A 3‐year prospective observational study ... Schizophrenia Research, 107 (2-3), 165-172. 10.1016/j.schres ...
The journal publishes novel papers that really contribute to understanding the biology and treatment of schizophrenic disorders; Schizophrenia Research brings together biological, clinical and psychological research in order to stimulate the synthesis of findings from all disciplines involved in improving patient outcomes in schizophrenia.
The neurobiology of treatment-resistant schizophrenia: paths to antipsychotic resistance and a roadmap for future research. NPJ Schizophr. 6 , 1 (2020). PubMed PubMed Central Google Scholar
The number of published studies in schizophrenia research has been rapidly increasing over the last 25 years and an analysis of medline, a relevant database of international scientific publications, shows that the increase of schizophrenia-related publications since 1990 is much larger than the increase of the total number of all research ...
Read the latest Research articles from Schizophrenia. Variations to plasma H 2 O 2 levels and TAC in chronical medicated and treatment-resistant male schizophrenia patients: Correlations with ...
Objective: The authors of this systematic review (SR) sought to provide evidence for effects of commonly used psychosocial interventions on several outcomes among adults with schizophrenia. Methods: MEDLINE, the Cochrane Library, and PsycINFO databases were searched through July 2020. Eligible studies were SRs and trials of at least 12 weeks duration and with ≥50 participants that compared ...
This paper is predicated on the view that health outcomes and therefore treatment effectiveness are deteriorating over time for people with schizophrenia, although this view may be contrary to the position adopted in the recently published revision of the Royal Australian and New Zealand College of Psychiatrists (RANZCP) Clinical Practice ...
Schizophrenia, characterised by psychotic symptoms and in many cases social and occupational decline, remains an aetiological and therapeutic challenge. Contrary to popular belief, the disorder is modestly more common in men than in women. Nor is the outcome uniformly poor. A division of symptoms into positive, negative, and disorganisation syndromes is supported by factor analysis.
Background Schizophrenia is a complex, heterogeneous disorder, with highly variable treatment outcomes, and relatively little is known about what is important to patients. The aim of the study was to understand treatment outcomes informal carers perceive to be important to people with schizophrenia. Method Qualitative interview study with 34 individuals and 8 couples who care for a person with ...
The Choice of Drugs for Schizophrenia. J.M. DavisN Engl J Med 2006;354:518-520. Schizophrenia is a serious chronic illness that requires lifelong medication. In some patients, the illness is ...
schizophrenia include overt delusions, auditory, visual, and tactile hallucinations, thought disorder, and behavior. that is bizarre when compared to norm al behavior in the culture where it ...
Editor spotlight. Schizophrenia Research and Treatment maintains an Editorial Board of practicing researchers from around the world, to ensure manuscripts are handled by editors who are experts in the field of study.
Schizophrenia is a severe mental disorder associated with impairment in functioning. A multidisciplinary approach is essential to help individuals with this health condition, and psychological interventions are considered a priority. The International Classification of Functioning, Disability and Health (ICF) offers a theoretical framework for assessing functioning and disability. The ICF Core ...
In order to understand schizophrenia, its causes, development, and outcome, and in order to define new subgroups of patients who may be differentially responsive to treatment or, hopefully, prevention interventions, we will need to switch our focus from psychosis to cognition and the related brain development during childhood and early adolescence.
Schizophrenia research findings may introduce new interventions that may significantly affect the lives of people with schizophrenia at critical points, improving symptoms and functioning. Researchers suggest that genetic and environmental factors play a role in the development course of schizophrenia and look to examine the ways such factors ...
Waite F et al. Sleep and Schizophrenia: From Epiphenomenon to Treatable Causal Target. Schizophrenia Research. July 2020. Sharma A et al. Emotional and Behavioral Dysregulation in Severe Mental ...
Schizophrenia is a severe and debilitating psychiatric disorder that involves psychotic symptoms such as hallucinations and delusions, accompanied with regressive behaviour. Latest Research and ...
Researchers at MIT, Brigham and Women's Hospital, and Harvard Medical School have developed a potential new treatment for alopecia areata, an autoimmune disorder that causes hair loss and affects ...
The findings from GWAS studies allow us to identify possible genes for targeted treatment and future research regarding the immune mechanisms of schizophrenia . There are still a number of shortcomings, such as clarification of the pathogenesis, early diagnosis, and the treatment of schizophrenia; hence, the extent of genomics in the treatment ...
Insmed has been in the spotlight over the past few years for its pipeline agent, brensocatib, which has previously shown promising Phase II results, generating anticipation within the medical community ahead of the Phase III results for the treatment of bronchiectasis.. The positive outcomes from the Phase III trial could pave the way for regulatory approval, potentially transforming the ...
Previous research on self-referential processing in affective disorders and schizophrenia has largely employed functional magnetic resonance imaging (fMRI) or event-related potential (ERP ...
A complaint filed by the Legal Aid Society and others accuses the state prison system of holding mentally ill and disabled people in isolation despite a law against the practice.
Abstract. Schizophrenia is a highly disabling disorder whose causes remain to be better understood, and treatments have to be improved. However, several recent advances have been made in diagnosis, etiopathology, and treatment. Whereas reliability of diagnosis has improved with operational criteria, including Diagnostic and Statistical Manual ...